PUBLIC HEALTH IN INDIA : CRISIS, CHALLENGES
Item
- Title
- PUBLIC HEALTH IN INDIA : CRISIS, CHALLENGES
- extracted text
-
RF_COM_H_49_SUDHA.
f'
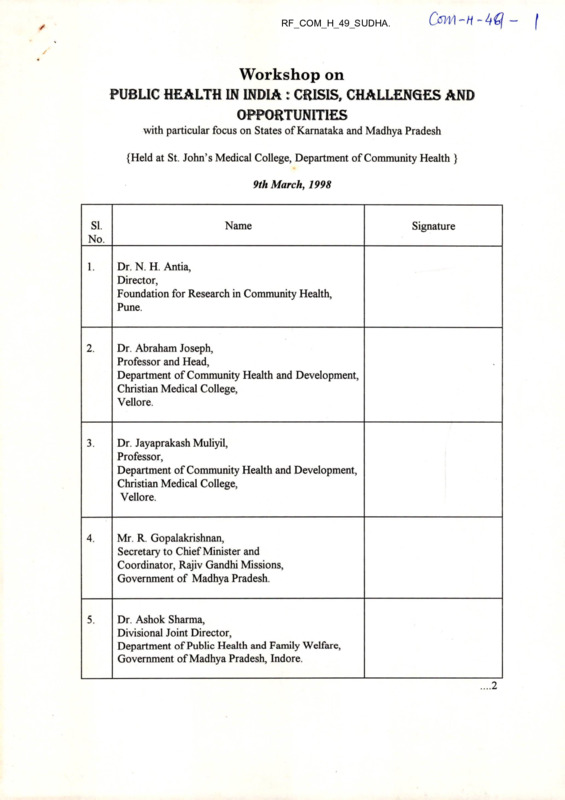
Workshop on
PUBLIC HEALTH IN INDIA : CRISIS, CHALLENGES AND
OPPORTUNITIES
with particular focus on States of Karnataka and Madhya Pradesh
{Held at St. John’s Medical College, Department of Community Health }
9th March, 1998
SI.
No.
Name
1.
Dr. N. H. Antia,
Director,
Foundation for Research in Community Health,
Pune.
2.
Dr. Abraham Joseph,
Professor and Head,
Department of Community Health and Development,
Christian Medical College,
Vellore.
3.
Dr. Jayaprakash Muliyil,
Professor,
Department of Community Health and Development,
Christian Medical College,
Vellore.
4.
Mr. R. Gopalakrishnan,
Secretary to Chief Minister and
Coordinator, Rajiv Gandhi Missions,
Government of Madhya Pradesh.
5.
Dr. Ashok Sharma,
Divisional Joint Director,
Department of Public Health and Family Welfare,
Government of Madhya Pradesh, Indore.
Signature
....2
: 2 :
SI.
Name
Signature
No.
6.
Dr. G.V. Nagaraj,
Additional Director of Health Services,
Government of Karnataka.
7.
Dr. S. Subramanya,
Project Administrator and Ex-Officio Additional
Secretary to Government,
Health and Family Welfare Department,
Karnataka Health Systems Development Project,
Bangalore.
8.
Dr. Murugendrappa,
Joint Director (Malaria & Filaria),
Department of Health and Family Welfare,
Bangalore.
9.
Dr. Mary Olapally,
Principal,
St. John’s Medical College, Bangalore.
10.
Dr. Dara Amar,
Professor and Head,
Department of Community Health,
St. John’s Medical College, Bangalore.
11.
Dr. M.K. Sudarshan,
Professor and Head,
Department of Community Health,
Kempegowda Institute of Medical Sciences,
Bangalore.
12.
Dr. D.K. Srinivasa,
Consultant - Medical Education,
Rajiv Gandhi University of Health Sciences,
Bangalore.
.... 3
: 3 :
SI.
No.
Name
13.
Dr. J.S. Bhatia,
Professor - Health Management,
Indian Institute of Management, Bangalore.
14.
Dr. Ravi Kapur,
Visiting Professor,
National Institute of Advanced Studies,
Bangalore.
15.
Dr. Jayashree Ramakrishna,
Additional Professor & Head,
Department of Health Education,
National Institute of Mental Health and
Neuro Sciences, Bangalore.
16.
Dr. Mohan Isaac,
Professor and Head,
Department of Psychiatry,
National Institute of Mental Health and
Neuro Sciences, Bangalore.
17.
Ms. Sujatha De Magry,
Director,
International Service Association,
Bangalore.
18.
Dr. Sukant Singh,
Consultant - Community Health,
Christian Medical Association of India,
Southern Regional Office, Bangalore.
19.
Dr. Pankaj Mehta,
Associate Dean and Professor and Head,
Department of Community Medicine,
Manipal Hospital, Bangalore.
Signature
.... 4
: 4 :
Name
SI.
No.
20.
Dr. C M. Francis,
Consultant,
Community Health Cell,
Bangalore.
21.
Dr. V. Benjamin,
Consultant,
Community Health Cell,
Bangalore.
22.
Dr. Arvind Kasturi,
Assistant Professor,
Department of Community Health,
St. John’s Medical Colege, Bangalore.
23.
Mr. As Mohammed,
Assistant Professor of Statistics,
Department of Community Health,
St. John’s Medical Colege, Bangalore.
24.
Dr. H. Sudarshan,
President,
V.H.A.Karnataka, Bangalore &
Honorary Secretary,
Vivekananda Girijana Kalyana Kendra,
BR Hills.
25.
Ms. T. Neerajakshi,
Promotional Secretary,
Voluntary Health Association of Karnataka,
Bangalore.
26.
Dr. Kishore Murthy,
Management Consultant,
Bangalore.
Signature
....5
: 5 :
Name
SI.
No.
27.
Dr. Ravi Narayan,
Coordinator,
Community Health Cell,
Bangalore.
28.
Dr. C. Siddegowda,
Additional Director - AIDS,
Department of Health and Family Welfare,
Bangalore.
29.
Dr. B.Y. Nagaraj,
Joint Director - TB,
Department of Health and Family Welfare,
Bangalore.
30.
Dr. S.M. Junge,
Joint Director - Leprosy,
Department of Health and Family Welfare,
Bangalore.
31.
Dr. G. Gururaj,
Head - Dept, of Epidemiology,
NIMHANS,
Bangalore.
32.
Dr. Gita Sen,
Professor - Indian Institute of Management,
Bangalore.
33.
Dr. Lessel David,
Danida Team Member.
Signature
...6
: 6 :
Name
SI.
No.
34.
Ms. Sangeeta Mookherji,
Danida Team Member.
35.
Ms. Victoria Francis,
Danida Team Member.
36.
Dr. Kris Heggenhougen,
Danida Team Member.
37.
Dr. Birte Holm Sorensen,
Danida Team Member.
38.
Dr. Bjarne Jensen,
Danida Team Member.
39.
Dr. Suresh Ambwani,
Danida Team Member.
40.
Mr. Esben Sonderstrup,
Danida Team Member.
Signature
‘A-
«•
—Z
Cow H
i /JL - * 4
IIl "
1! l-^ny G _LAV-'';m i ‘ f- '.
PACTORd i
r-r ■
■illlb
• Lack
i 1
in Formation
of
MiflBfilfRFS
. pjxaVALFNT
4
i
h
. PoftR
Pe.kcef>rion
• Poor
Health
. Lack
f'EHAVJOUR’
Risk
of
of
Risk.
6E£kiN<
behaviour.
EMPOWERMENT
/
• Health - Low PRioRiry,
:■
i
•
iNBQUALiTy - PiNANCML
• Q lai
rfvi
;• » .
[a
. IW bVSTR)AU&ATi6W
• cultural ' SHOCK'f£)
u • Ji
I
T
'I- i
• IjiJiiE POPULATION
]A
•
:L
Iw
8 t.
QuoaRAPHICAL ARfiA.
•Diverse
cultures.
• HIGH ILLirERACy,
• > 45a languages
^ialscts
• urgent need
• Poor aids AWAREtflSj • PERHAPS
l>kfcASE *.
• Behaviour .change bEPsvps ow Too MA^y
«
<
I
Jj .
k-
'• ’''
'•
ON<E
• MEt»'4AL CAR£
HCVv >
l> k.
H)V 4
I ?
If
I
i1 ;
'
• Social
1! ■ I ■'
‘' I
<
J- jI
I
.iMi ?
i W.r
C/n H/v
Crp’-
j
*
TO SINGLE* PAMiLJE^
fl
Ik 5
|b
Ii
J
ll
jJ^aNONli cA L
OF
. COST
- UNMAMAGAiilA
MANAGEMENT
4
OF
• Loss
MT
H. Ne
ti
*• I
<.
Income
m'reoT
l'+
. M vltFsector»al .
A.f PR.OACP
1
■i! ■
f
■
1
fe ll■4
rule
SPiA’-L
J ' '.
=
to
RVLE
TO
C WORK?
biVIIDE
1
■• < i
! '1 ■ i1'* ’
',
vjl’.^r
’ A BEARANT ATTfT. “
■
;
•■’. "I ;r : I
r„
«jjtLAy
LACK
r.H
oru
ZF
®f
1
TIME
i 1 Or™ ’ <4i®
, Mi |4 .;
■ «sP
w
tp»
■■■ h !
4^4
LARQH.
motTvation.
Inertia.
ib Care 4 event relat*z> prev*
I
J.
Ti»f
; SfeiHJw
F
i LE x i B) Lipy
PoftR
In FRASTJWCF
• Small
• Less ka Crass RotfT xv>port;
MU LTl SECTOAIAL
M r’
jWh ’
?»
NGO
C'f^)
ACUs C R £ t>) & i Liry
f
i
L6ST
DIVIDE.
'I ?' r
it;
'
h
ain-SSi
’4'd1 fiw
4,
htfi 4ij^drir
■t
I'
lib’'
It' ■
jww
WiR
hO
!• i grass
'I
i*11 r’lJ
’A-
f
&;
■'.
r,
AxS^MRcEs
.'/?
il.l'
- IWMte
Qurekfi
l/u Ul Ki
i ■ ■■
t
■
HIS
-b
77 M--, ■<-.".■ '
It"}
i
• i ■ MPliinr'
• HIGH’ M&TivATia k/ lySilS
i
• V, *
r’ ’r
|i
H
•More ;N H. P^o^aTM
-1
<HAN
CARE,
Health
pu/s
Mi ii i
I
1
W'pl’ fejiii '.PLUo N6O +
llilj >m
'•ji I
«si
lid'
ni'
iB
Wil
Wil
fl
.-r
'•
'»
i
'
.
-'3
n?- ■
nJ hi •
<1
V
i . If
r-
CAKE.
iv)l'.P)<Au
h|'l
Go
. ' ’. rj r»7 rina!..' ..
•
f
<
PAT1SMT.
Qo
bAS’zj>
.
Mt
"''GO «
G '’ '/N . G. LI.IM^
Imi'./• biSSASE. AVMAR&N2..
ao
N<?0
BlectioWic. *<8hi4
fix
NC&o).
l 'J.
!
i »! - ? r
Go
AGENT
'i
change hjv
op
v< ■
y
WHE^ CAN
IT ft£ EFFeCTl’vE/
■ '.
;.
I .
L j« i> l
?
i
• Commit hoent
i
i
equal
PartneremIp.
. OPTifOUM
FLExiBiL>TX
r-
» SELF- SUFFj’cjENCy _ (pf REcTlOf^)
► I
A
-Mr!-.
M Go
l.h
H ■•
s [ ■
Pl
N GT {,70 R K)N^
- V iyA L
- EXPBRJENCH’
•
PAz,o
POOR ^^TAlVABklTy
• JaaIoua^
• ^'VckJay^,
iH’ *:
CjOMMen
H
i -rv ,
Ci!
J::
I,!
• FLy
By wiSHT
oPERBToAs,
• lyf Rk tJONE tEsi Cs;<;>J+ DU Wtop.CLAIM
- NW>V ? N<0 -
• CORPORATE
NEC's. ? Cbarȣ.
I
14
* A-
h ■
?
cultured
'
z UNG LIS H
. Hi fl
.Local bMo-PMoaMt\
« Program
CHOICE -
? MONi Torino
. Target
groups
Lntens'ive
^^caToRa*
!
Focus
OA/ta
- CAPTIVE f P»SAbvA!VTAGED
• CsWi.
'
• PWA* 'MeSt^yu.
.
/f.
I
• E h->|>©tNer>nent - > blame others
Agencies
Life Piffkvlt.
1
i
X\ b E P£N DENCE
I
b- i
.
I &.
"
«
I
I
Visibility
PRo^'^TE
•
SUFFERS
.
Favouritism
.
Poor
I
z Promise/ 1.VRE
FROM
i
next
'
5 yr
GONSORT/t/M
A«<iste4
h/ACO
but.
?vacp ,
AASlsrRJb
NA\y
•!
•\
Vi
J»)an z We h^e.
WHO
e
id?
2»<5 NO a
-for
you
OR.
•PRobuirivrr^
ajcnc^
DO
A
©N£ o{
^xecuii'n^
ai v
Pay!
’’no
* PaRxJ/vSoM^M.*
(Be
1
I
■
-
but
PRobUcTrv/yy — /hfC£/vT/vfi
Poor
PONb/NcS AGEMCtC^
In The
CWAM^e TMe'sHi^
<
-
't
6vMbR«M».
PUA/fc>Al$
To Halt
ttMfa
.’a
Not
0^71/1 H — ■4^ --'
,'( V •
K
Uh*
■■
■*■■“'
(1'
4
•^*
\
\
V-.-...
4—imrvW-
/w.
.
._■,
-y -ftC.
I
7b e
C ©NTI NP<^
■i
o4 M
PicH c
IM
S <S> C( A- C-
h. bucnnoN^^
y ocr ri on n<~
It
I.
IO «
TP-A iFl »N 6
I
I
Dll/IOUftC
*
I
I ■
H<6>rt£ir
r»e
Pouieie
I
OF-
■J
P UH Lr lONftt* 4
■'
I
I
!
RHHfl-E>/2-/rar»0A/
I
IN
rfpu rnrtoAj
)
J
J
PoAme/^
/6/rr4>
.. 'Uv.ijrj.-... .:.
. PflLi-iftuVzr
w H? H ’
C f\«t
D ecisi oM
IN FOMec>
i
Q uat/ny
f= fA/ft/V 6/ftlL
1 *
Phz-z-inr ii/e
cftKe
I) ?P.0PH'ItR
3-) coftimo^
i TO Bf fo/Nri/Ma^
|NF£CTIOA/S TReATEJi
symptom control
!’
£fj Serious
iNPecno/^;
TRenreb
V
.
^yf-.'T^Sftyrar. -■
‘F \
Home*
I’
3b
$
I
B BSfB t-
’• c
-—4;-UatiX4U.^2XS*».-
tflRE.
|
I
I
V
M
U
*;i
t(
;
I
I
’ X
->!
\) pr U/ifK H1D5
Be/Nt,
2-) ro
Peer
ro
3j
ro
H
M
J
I
A|Oi faf
oibHir'j (/?Fspecr
FRotfips
OPTIf^ufYl comPofc*
HW<hieMB TO AIP5 l//CTI/v>i
:i
i•:
Hopi^
SMPROAT
I A-ND PfRiOA/flc
j
4 CHOICE
e-fAorioNnt-
st/ppoftr to
■'
fl.Nc>
i
i
I
CrtRF C-,>VEft.l
1
'
IaJO8K|?R
- (- OUNifi t-COft-
' PhiroKtL- cnns
£ <£u / pmenr
Pun cn ©/><; A(4
I:
VO LU
- re*
1 V A
COi^ Po ne f<(
op
Home- Cftne
X NVRA/N4)
“
c O VN 5
/N 6
Pasro^n-e
- SOC/^L- SCCPpOJ^r
Po A.r
IN Comc74?N^^hriO/</
WflrF/Mftc
shPPoaf
Rb“L^
S6>C/ftC- CO^^^P'
■ I
C0Srj>
I'toSpI F4-U
*7
i
^74
1/
Ji
j,-..
•
-J
/-
■xh ■
n.
ft&VhNThfoe*
nos f>/rA<JS*ri©A<
t
PF
*)
He
h^s 1 co /mtRo t/ the ou cnrioA/
o
WtiZ
(oM MUNirLj
14 pi f>
S')
FP-Of*
R e t> ucrioN
CO M rytc/Hir<i.
of
3ne»r»tn>
-:
I
<1
D/S nt>VftNTAC7EJ
peNiftu
OP TP EPtTMCAIr
V
HomC v nits
,i
1
i
m ftiNTentrHce
4;
VO L.U nF6ep-j
S')
S FK, Mb•'
A
’
4
|
I
A
r
C AHP
OP
,f .
. / - <.* >,<>*>•« <'
I
>,.w,
Ptf/AT^
co n c e^zt
0_e h©s p/c
Nee d
u PP&Kr
(n Pi O U P3
f^t=~ G, 11//<
- Tkavi rio/^frc.
gottT
DlSf/Vst?
PoLLBH
Nfi^fcs
; PKncncnc
/n dail<^
frwnrnNCG
TAiycK
- KFFP/N£|
- tMtg^cnoN
7
oH/WfO^
Henur^ i<iirsr*
- rsus/j^eii
^©r<oA/^ c.
c= ^r/N e>j
S ca ppo^r Oug/^t,
Petr#
v1'
L-
*b< "T
J
X.
(niveK £Q(»J
-
Aoz-f
0 •P ftfmitroag2J
CftAJRS7<
Aoti?
P e V^LO P&Zrt T'
jf^E’ H IV P°^* 7\Vlf
I
omr
J Msk
D I P de S5I0A/
op
rmeNr
t-O SS
*
shi r
u/m
im
AFiFo/M£iAc/ry
peer & &
N Co/MTpPtusO
^OU7
• -
Co/SPLlC)
T (.(.HL-’b
...
HU-
* y
-x
c Mir o p c
•{h ’.
t r\
I
IJ X N C
z_) Heep
ft C /?
TO
anticiPft-re
re ft ch
q)
$TftR.r«»l^i TO i-OP^MITti
inu l.t)Pt £" P«0 3£.fc^
1
i
f) £ NJievnccz**'-twf' *P^o
i- .
<■
V
i
I
DevEtoP
J
I'!
Is
<
I
]
■
s■
1’Y ‘hif!
COflNb,
h)
COQN iCLLINtj
0
M cr woAKj^t,
He^ti
4
Q Wi ,K SlAdj^Y^
GiROOPJ •
Public hbalj/-/
tbOC^T/ 0/\f
Cwi H
AajD TflA/Alz/vS,
^ SS CjES
B. CUA l L SA! SSS )
• S'C0/>6 OF
•
POVOCACy
PCLUOC PfFP c tai
FoQ Public mb a fry
7/laining,
Poli Gy
P P P Ad a cjjfs
•
to
STP-FAJG,7J.I&A/
OT^FA
7'<Q<9//V//y
^FFTCg
TAG,
• ^rP£SC co )rH
Ppl Qualietab
estabdsa,
school
Public pcacth (
of
m^tj -
2>ISCI Pc/AiAAy j
9
PmiL " 2 y&w
(■ouAse
(c/MKeb Yq f\
ZTATVATOAv Oaji \jC/LS
■ Basic U6> t ps,
»
/VOUCT/^A/
E xPcoajn6)
&.
Distance
^16 bC Qopeaj
---------- ■‘W
7~ A
jy^r. l>Wo.
(Pe^xfw
a
S'f&vgfi
G^i^ov) p Jl
CcWl
Pgprjposg op
A - Access
&•
c- r/AMA^HeAJT-
or-
£>A7A ^keMGRATOAS Tb
A/u/uyse Jut fuse Data at aoc4<
*
4Eu^C&
He ams op
&
G-Gmgaat/as^
?Acw bM
^ulck
deiPoAJse
GA^WAj0ees
• daeArsA oriury
• CjUAtga
z/o\/o4ue«GAjr
’ £MeA<xG/ocy fteAcr/©A>• NoTIUAT/oaJ .
•
/M90A.W A1I0A3 M6eas
• ZoCAK /OGGZ> op /A)9©<«At/«M
• Stats / n)At/oaj^c AJGsi).
He-tHoOS
op
Z>ATA OTlCl&Mod ftT
6euec.
CoNHuMiry
PuMiiive
• >J/
P.e£PoK)se
QoR
1
•
Accou^e^ry
/KJt(5A5Gc.roAA<
Quaut?
MAlOAi/^a.
If^oMvA-VOfQ
~CecH*D/qu6&-
2>cPFeAeAJT
«
CA?/A>6.
UlTM
I
*
C\.
X^oCAt.
CLocceafG^
«
l^^oANATlOf^ i
Pu&LIc
^eAixu
P^O^L£’ti£
b^bGl^tlFl&i
;
• PAT£AAamJUe
SYZTGN&
^>»AH/M€
*
^GACTH
£7AeAj&.TweAJiAJ&.
< i>eu6A0P/^^
JjDC/MJLy .
.
Dp
To
If^^oAHAriOfO-
C.OAAj^fjf
• bex&MiMMa <5^Gt^xiA-L.
p-eebMCK. swrens
K&SeAAO^
IHPCGHGAJte^
• £HPok5£A^^
«
^SALTIA
AesezwicH
III ■l1fllnB1iM,w|———
P£fLcep‘fioKis
ci/a?oaaa
PP Ao PA/OA1C 'Z’o
hcvori
Pop.
iM^wAvioti.
^D^ITopjf^c^
^o- of ^.ecoAZ>£ •
^oth bi/ieaffo^>
CoHHorf H^Gmecrofi.AL bM& 9^^
I5j (j ROUP 3
me
P£cerrTMi,l$/ir/ofJ irr tHB HeMrH
Hnp HoSfi-rAt- pynpot'y.
Pflfi/cpitytr Pkf jT/rsnrvnorJ To pe e/rcouMe-ej)
Pooiet- (,$ driver1 /nretioj t>F Trips, x MohW
Hepp THe^ TO tpermpy THerf. r/eePi, PPr PPior-ines
PF? IaJoPjc-OUT plfiri of PpiTlori za/ ficcof-p
iPrrH
With
THP SrtVPmo/J
to
Kfrf-rJkrPtt.Pi'-
$i>tt-PiN6- of
(VifMfteAS pF
PF-r
' HefirJff- l/J PLfrJrJlrJG' TO P-&Of> irJ J>eci5lO|M MfiXIAte' To CrJT><Jf£ pfifT vpfiTiir! OF rJ<rO,
TrJTFp.rJfiTK>rJAi. Pr'P fl-rref^es
P
- TO P-P^p PRt pt> Cn/^e up
PPoa-P P€\j. ppcrixirrei/ ^>pec\f:ic. PT^irH
pP&.t ir/jpeK KeMM> Pf-(r-
* ft trf 0^0
~
Of
^uTONotfw/
PeOfUc
Ho $f>rrftL5 ■•
c(pj &e
/w-use’ op po^e^
pet-P 7^ PeAI- ■
PPX
U5PP pee j:^$Tifvrio^s rfie-Hr
/AJ f&vrry /A/ seytuices
r>
op Ho$>f>rtALs
])& cerJ-rffir^^FP
1
Cduop 06 Dc/je ^y Co^T\TVT^& fEOftf
F^om T'Hf M&(6H&>ut-Hoop.
USZK pees
'fo e>e Ct^n-eJ>
pfirriz/rt
^fLfirfP, [(■<■■
frfijj)
i.
WAi/JT'eNA'f'JC&) '
fOptUS ^HoopD tPe
d
^ifAP^
rd Off ASM M&JArM^
f’lptiz. RfticwA,&ei-W.f
Pnp fcgLe-Aw).
*
Coaiai <Ja> i-ry ptSAot-fi Sysret'i
I
7>IS PW A^trAS-e-P
Pf- SAS.
(NlT<n-reP
M /Mx4<aV >Zy V&AAvCi^d-) yn ^1§C
* ."TT^
^U^or/ f
* C OhCcpkA&l^&k'Bn
2? /'rex/- AcJiviJ?
r^&ZaJi sy^k'p be&)<2£'K
4y pa^/\
b^ll\
^>k^- 'fvrivi oa^cJj^csn i/s.
Vis£a\
• Or^a^saJSsA ak fbcaX (jqajqJL ~
C£7MXVtu Zfee. y CjTCUM' po^c^aycjub
CjOIa^'cA' Igz/.
CjOCoJ- Iq<O(J2^ </Kejzjjjz
<*■ (i<Jjxc/Yy
40
‘A? C^cA-^^'
^Po
•
-l4?
*
(yij /e Co Ca^>
•
/UycJZcu __ / / - l^u^
/
ojjooa^m^
— /V)Zj2^/ */© TtAxZ^ 'tX
l>0Q/Il^AA’ trtu*’
t) hvixx^ ~/-o /xaJg
1/ fcc-s CZexvfi (5>i
y/l 6JX4^as^v
a^^YO^vi^(& (saJ- oA©
idjzxp/ V° T^'
]^Mc
c 6C-
4>e^cz
C^l^-pol^e^'^ &b*d<&(gjy
•
^C^-uiAiiSh-J a/^s^iiCi
J^cMs^i.,-i
PtJ't' ('ovd —
ppt Q^locdo
• G)ffi<^ /b
I/Ca loe^tr cJkjua.(uu < "
*
B
kM/).
V* 6) )<. K. pyc^eiL/~:
(j&UcJj 6CG'sfrfX
* ^JCdA^XX A?^o
&UA
EQUITY
Commitment to equity
Support for the “All” in
Health for All
* Benevolence
* Non-maleficence
* Justice
* Autonomy
EQUITY ORIENTED POLICIES
* Selection, training and deployment of health
personnel
* Reorienting training
* Selection and use of technologies
* Selection of populations
- greatest burden of ill - health
- disadvantaged and marginalised
* Gender sensitiveness
* Reduction of health disparities
environment: Determinants of
Health
* Physical
* Social
* Economic
* Political
environment : Hazards to
health
Chemical
* Microbiological
* Physical
*
*Local
*GlobaI
Con H
WARNINGS
SINCE 1975
GOVT. EXPERT
COMMITTEE - 1996
ON
Srivastava Report/
ICSSR - ICMR Report,
JNU / FRCH / VHAI/
CHC.
PUBLIC HEALTH
SYSTEM
(GOI / MHFW)
(CRISIS^
IN
PUBLIC
HEALTH
SECUNDERABAD
MEETING - August 1997
EXPERT ARTICLES
-1990S
Public Health Crisis and Challenges
EPW/NMJI
HA/HFM/Lancet
Malaria Report
(CHC/VHAI)
ICHI Report
(Network of Public Health
Professionals
Govt./NGO/ICMR/NPs)
opinion
polls
BANGALORE
DIALOGUE - MARCH
1998
Public Health
Crisis/Challenges/Opportunities
(Dialogue with Danida Health
Sector Mission)
CRISIS IN
PUBLIC
HEALTH
SYSTEM
BREAKDOWN
POLICY
PRIORITY
AND
FINANCING
CRISIS
IN
CRISIS
IN
PLANNING
CRISIS
IN
HUMAN
RESOURCES
DEVELOPMENT
’ CRISIS OF DATA /
HEALTH
INFORMATION
>
PUBLIC
HEALTH
(Dimensions)
CRISIS
IN
RESEARCH
AND
PROBLEM
ANALYSIS
<
CRISIS IN
SOCIETAL AND
SOCIAL CONTEXT
CRISIS IN
ENVIRONMENTAL
CONTEXT
PUBLIC HEALTH SYSTEM BREAKDOWN?
SHORTAGE OF WORKERS / DOCTORS
REDUCTION IN BUDGETS
OVERBURDENED HEALTH WORKERS
(ANMs - EXPLOITATION)
CORRUPTION / SCAMS / MISUSE OF FUNDS
POLITICAL INTERFERENCE
DECISION MAKERS WITHOUT PUBLIC HEALTH
COMPETENCE / ORIENTATION
CENTRALISED TOP DOWN PLANNING
CENTRE / STATE RESPONSIBILITY
- AMBIGUITY
• INADEQUATE / UNREALISTIC PLANNING
Source : Secunderabad Meeting - August 97.
MARKET ECOKOMY IN HEALTH
*
TOP DOWN PROMOTION OF
TECHNOLOGICAL FIXES!
*
MARKET INTERESTS IN DECISION MAKING
*
INTERNATIONAL PUBLIC HEALTH
COLLABORATION / COOPERATION
Often becoming subservient to:
* AGENDAS OF VISITING CONSULTANTS
* RESEARCH PRIORITIES OF COLLOBORATERS
* “GUINEA PIGS” for Research
* FUNDING AGENCY CONDITIONALITIES!
* GRANTS TO LOANS!!
*
ILL HEALTH EFFECTS OF NEO-LIBERAL
ECONOMIC POLICIES
(From Solidarity to exploitation!!)
Source: Secunderabad meeting - Augus: 1997.
HEALTH LOBBY
NETWORKS
•HEALTH POLICYCELL
IN MH & FW___________
- Interdisciplinary
- intersectoral
- Apex body to translate policy
into action
FOCUS ON
* Equity
* Sustainability
* Health as Right
* Gender Sensitivity
* Health central to
Decentralization
STRENGTHEN
PUBLIC HEALTH
EXPERTISE
* Indian Health /Medical
service
* staff college for health
policy
makters/administrators
* New short courses
* Reorient PSM
I
HEALTH PRIORITY i
HEALTH BUDGET T
DEPOLITICISE PUBLIC
HEALTH
CHALLENGES
MONITOR EFFECTS OF NEP
ON HEALTH.
>
CONTINUING
EDUCATION
OF
HEALTH TEAM
ANMs
Other Paramedicals
Nurses
Doctors
SOME
CENTRAL
LEVEL
OPPORTUNITIES
9?
VOLUNTARY
SECTOR
◄—
NEW PARTNERSHIPS
FOR HEALTH
PRIVATE
SECTOR
HEALTH AND
EDUCATION
SECTOR LINKAGES
*
Folk media strategy
* Community based media
approach
* School based Health
Programme
* Youth involvement in
National Health
Programme
OPINION POLL
MARCH 199S
b
STATE / NGO
INVOLVEMENT
CELL
PANCHAYATRAJ
AND
HEALTH CARE
AREA
HEALTH PLANNING
DISTRICT / TALUKA
>
INTEGRATED
HEALTH
INFORMATION
SYSTEM
*
REGIONAL
DISPARITIES
*
RATIONALISATION
OF MIS
*
STATE
HEALTH
PLANNING
CELL
IMPROVING
PRIMARY HEALTH
CARE
INTER
SECTORAL
COORDINATION
* MISSIONS
* APPROACHES
* STRATEGIES
4
STATE
LEVEL
OPPORTUNITIES
ENHANCE
FORECASTING/EPI
DEMIC
SURVEILLANCE
*
HUMAN RESOURCES/
COMMUNITY BASED
*
ANM-CMEs/ Updates
*
ESSENTIAL DRUGS
SUPPLIES
*
HEALTH ACTION
SUPPLIES
PRIVATE SECTOR
- Recognition
- Involvement
- Regulation cost &
quality
- Reorientation
PUBLIC HEALTH
ORIENTATION
Orientation course
Short courses
CMEs
Reorient PSM_______
Public Health Training
Institute/Network
4-
HEALTH WATCH
(OMBUDSMAN)
Enhancing
Accountability to citizen
- Watchdog/countering
* corruption
* commerciali sation
* political
interference
* Market Strategy
-
HEALTH LOK AYUKTA!
PUBLIC HEALTH IN INDIA: CRISIS, CHALLENGES AND OPPORTUNITIES
(with particular focus on States of Karnataka and Madhya Pradesh)
Group I
Group II
Public Health Education &
Training
Health Information System &
Public Health Research
1) Dr. D.K. Srinivasa (Chairperson)
2) Dr. Abraham Joseph (Key discussant)
3) Dr. Murugendrappa
4) Dr. B Y. Nagaraj
5) Ms. Sujatha de Magry
6) Dr. M.K. Sudarshan
7) Dr. Dara Amar
8) Dr. Sukant Singh
9) Danida Team Member
10) Danida Team Member
1) Dr. R.L. Kapur (Chairperson)
2) Dr. Jayaprakash Muliyil (Key discussant)
3) Dr. G.V. Nagaraj
4) Dr. Ashok Sharma
5) Dr. G. Guru raj
6) Dr. Ravi Narayan
7) Mr. As Mohammed
8) Dr. Gita Sen
9) Danida Team Member
10) Danida Team Member
Rapporteur : Dr. A.R. Sreedhara (CHO
Rapporteur : Dr Denis Xavier (CHC)
Group HI
Group IV
Decentralisation in the Health
Sector (including Panchayatraj &
Hospital Autonomy)
Coniniunity Participation &
Communication (including IEC)
1) Dr. J.S. Bhatia (Chairperson)
2) Dr. N.H. Antia (Key discussant)
3) Mr. Gopalakrishnan
4) Dr. S. Subramanya
5) Dr. C.M. Francis
6) Dr. Mary Olapally
7) Dr. Kishore Murthy
8) Dr. H. Sudarshan
9) Danida Team Member
10) Danida Team Member
1) Dr. Mohan Isaac (Chairperson)
2) Dr. Arvind Kasturi (Key discussant)
3) Dr. C. Siddegowda
4) Dr. S.M. Junge
5) Dr. Jayashree Ramakrishna
6) Dr. V. Benjamin
7) Ms. Neerajakshi
8) Dr. Pankaj Mehta
9) Danida Team Member
10) Danida Team Member
Rapporteur : Mr. Murali (CHC)
Rapporteur : Dr. Rajan Patil (CHC)
Z
/
H
Workshop on
PUBLIC HEALTH IN INDIA : CRISIS AND CHALLENGES
: with particular focus on States of Karnataka and Madhya Pradesh
{Held at St. John’s Medical College, Department of Community Health }
9th March, 1998
LIST OF PARTICIPANTS
SPECIAL INVITEES
1.
2.
3.
4.
5.
6.
7.
8.
Dr. N. H. Antia, Director, Foundation for Research in Community Health,
Pune/Mumbai.
Dr. Abraham Joseph, Professor and Head, Department of Community Health and
Development, Christian Medical College, Vellore.
Dr. Jayaprakash Muliyil, Professor, Department of Community Health and
Development, Christian Medical College, Vellore.
Mr. R. Gopalakrishnan, Secretary to Chief Minister and Coordinator, Rajiv Gandhi
Missions, Government of Madhya Pradesh.
Dr. Ashok Sharma, Divisional Joint Director, Department of Public Health and
Family Welfare, Government of Madhya Pradesh, Indore.
Dr. G.V. Nagaraj, Additional Director of Health Services, Government of Karnataka.
Dr. S. Subramanya, Project Administrator and Ex-Officio Additional Secretary to
Government, Health and Family Welfare Department, Karnataka Health Systems
Development Project, Bangalore.
Dr. Mumgendrappa, Joint Director (Malaria & Filaria) , Department of Health and
Family Welfare, Bangalore.
PA\R TICIJPA NTS
9.
10.
11.
12.
13.
14.
15.
Dr. Mary Olapally, Principal, St. John’s Medical College, Bangalore.
Dr. Dara Amar, Professor and Head, Department of Community Health, St. John’s
Medical College, Bangalore.
Dr. M.K. Sudarshan, Professor and Head, Department of Community Health,
Kempegowda Institute of Medical Sciences, Bangalore.
Dr. D.K. Srinivasa, Consultant, Medical Education, Rajiv Gandhi University of
Health Sciences, Bangalore.
Dr. J.S. Bhatia, Professor, Health Management, Indian Institute of Management,
Bangalore.
Dr. Ravi Kapur, Visiting Professor, National Institute of Advanced Studies,
Bangalore.
Dr. Jayashree Ramakrishna, Additional Professor & Head, Department of Health
Education, National Institute of Mental Health and Neuro Sciences, Bangalore.
: 2 :
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
Dr. Mohan Isaac, Professor and Head, Department of Psychiatry', National Institute
of Mental Health and Neuro Sciences, Bangalore.
Ms. Sujatha De Magry, Director, International Service Association, Bangalore.
Dr. Sukant Singh, Consultant, Community Health, Christian Medical Association of
India, Southern Regional Office, Bangalore.
Dr. Pankaj Mehta, Associate Dean and Professor and Head, Department of
Community Medicine, Manipal Hospital, Bangalore.
Dr. C.M. Francis, Consultant, Community Health Cell, Bangalore.
Dr. V. Benjamin, Consultant, Community Health Cell, Bangalore.
Dr. Arvind Kasturi, Assistant Professor, Department of Community Health,
St. John’s Medical Colege, Bangalore.
Mr. As Mohammed, Assistant Professor of Statistics, Department of Community
Health, St. John’s Medical Colege, Bangalore.
Dr. H. Sudarshan, President, Voluntary Health Association of Karnataka, Bangalore
and Honorary Secretary, Vivekananda Girijana Kalyana Kendra, BR Hills.
Ms. T. Neerajakshi, Promotional Secretary, Voluntary Health Association of
Karnataka, Bangalore.
Dr. Kishore Murthy, Management Consultant, Bangalore.
Dr. Ravi Narayan, Coordinator, Community Health Cell, Bangalore.
Dr. C. Siddegowda, Additional Director - AIDS, DHFW, Bangalore.
Dr. B Y. Nagaraj, Joint Director - TB, DHFW, Bangalore.
Dr. S.M. Junge, Joint Director - Leprosy, DHFW, Bangalore.
Dr. G. Gururaj, Head, Dept, of Epidemiology, NIMHANS, Bangalore.
Dr. Gita Sen, Professor, Indian Institute of Management, Bangalore.
Dr. Lessel David, Danida Team.
Ms. Sangeeta Mookherji, Danida Team.
Ms. Victoria Francis, Danida Team.
Dr. Kris Heggenhougen, Danida Team.
Dr. Birte Holm Sorensen, Danida Team.
Dr. Bjarne Jensen, Danida Team.
Dr. Suresh Ambwani, Danida Team.
Mr. Esben Sonderstrup, Danida Team.
Io
PUBLIC HEALTH IN INDIA: CRISIS, CHALLENGES AND OPPORTUNITIES
(with particular focus on States of Karnataka and Madhya Pradesh)
Date
9th March, 1998
Venue
Department of Community Health, St. John’s Medical
College, Bangalore - 560 034.
Facilitation
Society for Community Health Awareness, Research
and Action (CHC), Bangalore in collaboration with
Department of Community Health, St. John’s Medical
College.
Objective
Interactive workshop with Danida Health Sector
Identification Mission
Timings
9 am to 5 pm
Programme
9.15 - 9.45 am
Session I
: Introduction to Workshop
Chairperson
Welcome
: Dr. V. Benjamin
: Dr. Dara Amar, SJMC
Self Introductions
Expectations of Workshop
: Dr. Ravi Narayan, CHC
: Mr. Esben Sonderstrup,
DANIDA Health Sector Mission
9.45-10.45 am
Session II
: Introduction to Theme
I. Crisis & Challenges of : Dr. Ravi Narayan
Public Health in India an overview
II. Core Values in Public : Dr. C.M. Francis
policy
Health
A
reflection
III.Clarifications / comments : Participants
■
2
■
10.45-11.00 am Tea
11.00-12.45 p
Session III
: Group Discussions:
Identifying Opportunities
Group I
: Public Health Education and
Training
Chairperson
Key Discsussant
: Dr. D.K. Srinivasa
: Dr. Abraham Joseph
Group II
: Public Health Research &
Health Information System
Chairperson
Key discussant
: Dr. Ravi Kapur
: Dr. Jayaprakash Muliyil
Group III
: Decentralization in the
Health Sector (including
Panchayatraj & Hospital
Autonomy)
Chairperson
Key discussant
: Dr. J.S. Bhatia
: Dr. N.H. Antia
Group IV
: Community Participation &
Communication (including
IEC)
Chairperson
Key discussant
: Dr. Mohan Isaac
: Dr. Arvind Kasturi
{Each group will have a mix of participants from governmental, non
governmental and. academic/research backgrounds and some
members of the Danida team (see separate list)}
12.45-1.30 pm
Lunch and Fellowship
: 3 :
1.30 - 3.30 pm
Session IV
: Identifying Opportunities for
Strengthening Public Health
Sector
Chairperson
: Dr. C.M. Francis
{A member from each group will present key ideas & suggestions from
that group, followed by clarifications and. interactive discussions with
all the participants}
3.30 - 3.45 pm
Tea
3.45 - 5 pm
Session V
: How could DANIDA assist at
Central & State levels : with
special reference to
Karnataka and Madhya
Pradesh (Wrap up)
Chairperson
: Dr. N.H. Antia
Vote of Thanks
eSOnn h
...iyi
THE PUBLIC HEALTH CRISIS IN INDIA
1.
PREAMBLE
The Re-emergence of Mai ar i a as a significant public health problem in the country' since the
1970s and the increasing occurrence of outbreaks and epidemics especially in the 1990s, is
leading to an urgent reappraisal of the countrys public health policy and a deeper understanding
of the larger ‘public health crisis that has been evolving in the country' over the last two decades.
Some elements of this crisis arc:
LI
The Socio-Epidcniiological Imperative
There is a growing concern (hat the ‘situation analysis and ‘problem solving processes
in the past, with regard to communicable diseases control strategics have focused
predominantly on the techno-managerial aspects and less on the important socio-cconomiccultural-political context of the problem.
There is therefore urgent need to strengthen these dimensions of problem analysis
and solution so that a more comprehensive, effective, sustainable strategy is evolved
to tackle the challenge of Malaria.
1.2
fhe Political Economy of Health
There is a growing concern in health planning and health policy circles that the ‘market
economy often drives policy decisions more significantly, than rigorous socioepidemiological problem analysis. In National health programmes supported by
International public health cooperation and collaboration, this also means that approaches
and priorities arc often promoted that arc at variance from the recommendations of
National expert committees and technical evaluation reports. These distortions taking
place primarily because International public health linkages are themselves getting market
determined.
It is therefore important to understand the political economy of health in rz National
and International context before evolving strategies /programmes.
1.3
The challenge of Deccntralization
There is a growing concern that the country lias reached the limits of National, centralised
planning and with the recognition of the great diversity in situations and challenges at
regional and state levels there is need for a more concerted effort at decentralised
planning with a flexible framework that responds to regional needs and disparities
in the health care situation. This is even more relevant to National disease control
programmes especially when a disease like Malrria shows a diversity and locality in
its epidemiology .
1
1.4
The need to move Primary Health Care beyond rlictoi ic to grassroots initiatiy es
at community level
There is a growing concern that inspite of a National commitment to Primary Health
Care and to integrated, comprehensive health care approaches, National health
programmes arc loo vertical, too top down and inadequately integrated into the basic
health services structure. This also menus that policy alternatives or thrusts such as
Decentralization and Panehayatraj; community participation; community based
approaches; involvement of general practitioners and the NGOs (both voluntaiy sector
and private sector), inter sectoral coordination; and equity issues; arc included in the
formulation of strategics but remain rhetorical and not adequately translated into actual
guidelines for action.
There is therefore need to promote community based approaches that ultimately
strengthen the health infrastructure at the j’rassrouts.
1.5
The Threat of the New Economics
There is a growing concern that larger economic issues be they corruption at all Icxcls
of the delivery system or the more recent trends towards privatization and
commercialization and cutbacks in governmental expenditure on welfare is leading to
a continuous worsening of the general health infrastructure and human power situation
in the country affecting the sustainability and effectiveness of health care programmes.
This is much more than just an infrastructural development or ‘adminislrative/managcmcnt
lacunae issue and there is need to address this matter urgently since it alfccts all health
and welfare programmes in the country.
The effects of the new economic policies need to be monitored carc/ully and the
distortions in the planning process produced by market forces need to be countered.
1.6
he Urgent need for Right of Information
There is a growing realisation that health and development programmes in the country
have failed to make the impact they were expected to, because of the failure to generate
and sustain an awareness creation and educational process that would enable and empower
the people and particularly the more marginalised sections of the community to access
and utilize the services available and actively participate in the development and decision
making processes for the further evolution and growth of such strategics. Without the
spread of‘critical information leading to inadequate public participation programmes
. have floundered on inertia and red-tape. There is therefore need to support a process
of demystification linked to the Hight of information.
1.7
The need to Widen the Dialogue and Participation in the Planning Process
In the light of all these background concerns and emerging needs for cHcclivc policy
responses, and keeping in mind the urgent need to widen the dialogue and participation
in the planning process, we have reviewed the Malaiia situation and are oflcring certain
complcmcntary/supplcmcnlary comments and suggestions in all those areas where wc
feel (here is need tor newer perspectives and alternative approaches. We have drawn
upon the resources of a wide network of individuals/gioups who constitute an altcrnalisc
sector eager to share their experiences and perspectives with the mainstream plaiming
process.
By doing so wc hope that the voluntary sector would have contributed to the development
of some complementary strategics for action, to tackle the Malaria situation in the years
to come and actively supplement the efforts of the NMBP by the evolution of more
indigenously determined responses to problem analyses and problem solving.
Source: TOWARDS AN APPROPRIATE
MAIuARIA CONTROL STRATEGY
Issues of Concern 6< Alternatives
for Action
(A VHAI/CHC PUBLICATION)
Cor^}A 14-^. .t 7-
ISSJliSAiW HECOifMENDAJ'JONS
* * * * *
1. STRENGTHENING THE SOCIO-CULTURAL-ECONOMIC-POLITICAL
DIMENSION OF PROBLEM ANALYSIS
We recommend therefore that Health Economists must be actively identified and involved
in situation assessment and programme planning so that decisions about choices and alter
natives, and effects, are based on more rational economic and socio-cultural indicators.
However , we would caution that the 'economic’ criteria should not supersede other crite
ria and costs should not become the determining factor at the cost of social need and eq
uity issues. The plea is for 'economics’ to be an important complementary part of the
planning process but not the central core.
There is therefore an urgent need to respond to this lacunae and we suggest the fol
lowing:
♦
Behavioural science, approaches and socio-anthropological and socio-economic/health
economic research competence must be urgently built into the 'problem analysis’ and
'problem solving’ structures at all levels.
♦
Well planned, multidisciplinary operations research must be initiated and a more wholistic
effort strongly rooted in the social sciences must be encouraged.
♦
From Action research, practical, realistic operational guidelines can be evolved on all the
above areas and these then incorporated into the planning process, the training process and
the action process at all levels.
2. HEALTH EDUCATION
Creating awareness and building up a knowledge base amongst communities are the com
monly accepted forerunners to the involvement of communities and building up their ca
pabilities to act collectively and individually towards a common goal. Although the need
for the same clearly comes out of all the planning manuals, the commitment to this activity
is not adequately visible in terms of the time, manpower, efforts or budgets earmarked for
the same.
It is suggested that:
♦
There must be a quantum jump on the manpower, effort, time, resources and budgets allocation for Health Education.
♦
The most vulnerable and high risk groups are usually illiterate and have no access to radio
or television. In view of this, socially relevant and low cost alternatives addressing these
particular target groups should be used. Folk artistes, ilinerarant performers and street
theatre artists can be used to pass correct and specific messages to entertainment starved rural communities. These artistes can be employed under various employment
guarantee schemes or tribal development plans.
♦
Posters and videos do have their role but cannot be allowed to overshadow the other
forms of communication mentioned above because of the irrelevance to the most vulner
able and deserving section of the community.
♦
Teachers and school children need to be specifically targeted for specific health education
as the long term effects on their action potential are the most beneficial and effective.
♦
The Government has in recent years produced many useful booklcts/pamphlets, videos and
other useful health education materials. These are however used only within the govern
ment system. There is urgent need to make them available freely on a much more open
basis to all groups outside the government system who wish to be involved in Awareness
building.
♦
Communication centres within the voluntary7 sector may be encouraged to use these mate
rials, adapt them to local/regional needs, translate them into the local vernacular and work
on alternative approaches to communicate the key messages and facts in other interactive,
low cost ways.
3. DISTRICT PLANNING / DECENTRALIZATION
There is a growing realisation that the regional disparities / differences are so wide and the
development process including health service development so diverse that planning at re
gional level and at district level particularly is not only necessary but also relevant.
The whole renewed development and emphasis of the Panchayatiraj concept and structure
also emphasises the urgent need and opportunity for this.
Finally the concept of involving the grassroots community in the planning process now
considered to be more relevant, favours this shift as well.
To support this shift of emphasis, we suggest the following action :
♦ The urgent development of capacities and capabilities to undertake district planning.
♦ The urgent training/orientation of Health Centre staff particularly Mos in the ability to
make local plans based on local data and to involve the panchayat/community in the plan
ning process.
♦ The urgent training/orientation of emerging panchayat leadership to participate meaning
fully in the health planning process.
♦ Community level plans could be a short term goal to support the long term goal of district
plans.
L
4. LOSS OF PUBLIC HEALTH SKILL / COMPETENCE
The health programmes in India is being greatly affected by the crisis of “Public Health” in
the country, marked primarily by the increasing disregard of ‘public health competence’
and public health perspectives in health policy and health care decision making.
At Central and State levels there is increasing marginalisation of technical leadership with
public health competence, by their clinical counterparts and both these groups by lay gen
eralist administrators. Decisions that therefore need sound epidemiological and technical
background are now being increasingly taken by those who are not adequately qualified to
do so. Specious arguments based on management/economic/or other extraneous factors
are therefore being allowed to modify policy planning process.
This is further compounded by the inadequate support to public health training in the
country' whose growth in quantity, quality and diversity today are totally out of context of
the large needs in the country.
It is therefore suggested that:
Serious effort be made to strengthen public health training in the country;
Ensure that key decision makers in health care services and policy making bodies have
public health competence and orientation;
Encourage existing Public Health and Preventive and Social Medicine/Community Medicine/Community Health courses in the country to be more field oriented in their priorities
and skill development; and
Build inservice training and continuing education programmes for all categories of health
personnel in public health skills/knowledge including communicable disease control focuss
ing on national programme related issues.
5. CORRUPTION / POLITICAL INTERFERENCE IN POLICY DECISION MAKING
While techno-managerial and some epidemiological causes of programme inadequacy
and/or failure have been constantly highlighted in all evaluation/reviews/studies of the
‘implementation gap’ in national health programme - two extraneous factors that are im
portant, known to most researchers, experienced by most programme planners and pro
gramme implementors but inadequately tackled or even described because of the difficult
nature of the problem are the following:
a) Corruption manifested particularly at the time of tender, bulk purchase, appointments, and
transfers. These involve bribes and pecuniary benefits to decision making leadership. Of
ten there are well developed systems with the collections shared by a larger section of the
system.
3
b) Political interference in decision making at all levels even to the point of disregarding
technical expertise. This is the bane of Indian Public life today. The involvement of lob
bies of drug companies, insecticide manufacturers, irresponsible trade unionism, staff and
all sorts of extraneous influences seem to be at play when variances from policy statements
and actual realities are discovered by evaluators/researchers.
While these are part of a larger problem, we suggest:
A policy of greater transparency in decision making involving tenders and contracts asso
ciated with drug/pesticide purchases from the private companies.
A greater sharing of information / with increasing emphasis and legal sanction to right of
information. These will go a long way to allow consumer groups and social activists to
play the necessary7 watchdog role on the system particularly in these aspects.
6. INTERNATIONAL PUBLIC MEALTII COLLABORATION
Many major public health problems in India, are serious global problems as well. It will
require concerted national efforts, strengthened by regional collaborative efforts and the
resource support and linkages of international funding agencies and international Public
Health co-operation.
In the present global scenario and the evolving market phenomena, there is a growing dan
ger that funding will get linked to marketing of specific products or approaches at the cost
of a more integrated / comprehensive strategy.
We suggest that the international project linkages, project funding, should primarily
o
Strengthen national capacity to deal with ‘.he problem.
o
Build national infrastructure especially trained and skilled multidisciplinary manpower.
Be rooted in approaches/strategies responding to local needs and socio-economic-culturalpolitical realities of the country and arising primarily out of local experience.
a Prevent national strategies/projects becoming subservient to the priorities/needs of inter
national funding agencies, institutions and resource persons whose understanding of local
socio-epidemiology is often rather limited and who may inadvertently promote the re
search, training and programme agendas of their own institutions/agencies rather than be
ing supportive of local expertise.
a Ensure that projects/linkages are transparent and subject to collective peer group dialogue
and interaction among all those who are seriously involved and interested in the public
health problems in the country.
Source . Towards An Appropriate Malaria Control Strategy
Issues of Concerns and Alternatives for action
(A VHA1 / CI-1C PUBLICATION).
cS.0
K <4-6.11
STA TE OF PEOPLE'S HEAL TH IN HAENA TAKA
The Voluntary Health Association of Karnataka in collaboration with the
Government of Karnataka and the Voluntary health Association of India has
brought out a report entitled the '■State of People's Health in Karnataka’. It was
in response to the needs of the people interested in health of the people of the
State to have a reliable source of information. In 18 chapters contributed by
knowledgeable resource persons, the book deals with various aspects of public
health and health care services in the State and compares it with the situation in
India and the neighbouring states. The book has brought out a number of
recommendations to improve the health of the people.
Regional disparities
The northern districts are backward in health and development. It is necessary
to pay special attention to the people of the area, to enable them to catch up with
the more developed districts. 1It is also necessary to have a more equitable
distribution of health care.
Community Participation
The community must be organised to take action for health. The people and
peoples’ representatives (under Panchayat Raj and Municipalities Act) must be
trained to plan and take decisions. The health functionaries must accept the
rights of the people to plan, make decisions and ensure the implementation of
the plans.
Equity with quality
The quality of care, Governmental, Voluntary or Private must be acceptable.
There has to be equity, with health for all.
Value-based education
The education of all health personnel must be value-based with competence
and commitment and the training must be close to the people to be served. The
practice must be ethical.
Public Health
It is essential to have a public health approach, with improvement in the
environment, reduction in pollution of all kinds and health awareness among all
the people, leading to health action. Lifestyles must be healthy. There is need
for improvement in the quantity and quality of water supply and proper disposal
of waste.
chc/msword/c:/nagaraj/peokar.doc
Nutrition
Malnutrition must be corrected. This is especially important in the early
formative years.
Alternative Systems of medicine
All recognized systems of medicine should be supported, leaving the choice and
utilisation to the people.
Special needs
The special needs of the vulnerable groups such as the tribals, urban poor,
women, children, elderly, disabled and other disadvantaged persons must be met
urgently.
The special needs of the girl child and women during adolescence, reproductive
age and later must be met.
Mental health
Mental health care needs to be integrated with primary health care.
Rational Drug Use
The efforts to have an essential drug list and formulary appropriate for each
level of use and expertise must be supported.
The supply of essential drugs through a revamped Government medical stores
and supply system must be strengthened.
Information regarding Rational Drug Use must be disseminated widely among
all prescribers and users through well-thought out campaigns.
Voluntary Organisations
Karnataka has a large number of voluntary organisations involved in health and
development. Government should see them as equal partners. They should be
seen as innovators, issue raisers, trainers and enablers of people to take action
for better health.
The book is available with
Voluntary Health Association of Karnataka,
#60, Raj ini Nilaya,
2nd Cross, Gurumurthy Street,
Ramakrishna Mutt Road, Ulsoor,
Bangalore - 560 008.
v
chc/msword/c:/nagaraj/peokar.doc
I?
I;
Tiru ^<4 'UUrl
REPORT
OF
r
THE EXPERT COMMITTEE
ON
PUBLIC HEALTH SYSTEiM
I
SOVERNMENT OF INDIA
M1NISTRYOF HEALTH & FAMILY WELFARE
NIRMAN BHAVAN, NEW DELEU-110 Oil.
I
JUNE. 1996
t
Annex -1A
LISI OI- rilE MEMBERS OE THE EXPERT COMMITTEE
1.
Prof. J S Bajaj, Member,
Planning Commission.
Chairman
2.
Dr Jai Prakash Muliyil,
Deplt. of Community Medicine,
Christian Medical College, Vellore.
Member
r
3.
Dr Ilarcharan Singh, Ex-Adviser (Health),
Planning Commission.
4.
Dr N S Deodhar, Ex-Officer on Special Duty,
MOH&FVV, 134/1/20, Baner Road,
Aundh, Pune.
Member
Dr K J Nath, Director,
All India Institute of Hygiene &
Public Health, Calcutta.
Member
5.
6.
Dr K K Datta, Director,
N1CD, Delhi.
Member
Member-Secretary
List of the officials who assisted the committee
1.
Dr. Prema Ramachandran,
Advisor (Health),
Planning Commission
2.
Dr. Dinesh Paul,
Deputy Advisor (Health),
Planning Commission
3.
Dr. A C Dhariwal,
Joint Director,
N.I.C.D., Delhi.
4.
Dr. S P Rao,
Chief Medical Officer,
N.I.C.D.,Delhi.
ii
phsanncx.iloc
<So
H Ms -' 4-
CONTENTS
Description
SI.No.
1.
EXECUTIVE SUMMARY
2.
INTRODUCTORY CHAPTER
1.0
2.0
Background
Introduction
Page
Nos.
1-20
21
22
CURRENT STATUS OF PUBLIC HEALTH
SYSTEM IN INDIA
3.
History
Federal Set-up
Union Ministry of Health & Family Welfare
Department of Health
Department of Family Welfare
Department of Indian System of Medicine and
Homoeopathy
'3.7' Function
3.8 Department of Health
3.9 Computerisation
3.10 Medical Education, Training and Research
3.11 International CO-operation for Health and Family
Welfare
3.12 Facilities for Scheduled Castes and Scheduled
Tribes under special component plan
3.13 Directorate General of Health Services
3.14 Functions of Department of Indian System of
Medicine and Homoeopathy
3.15 Department of Family Welfare
3.16' Planning Commission
3.17 State Level
3.18 District Level
3.19 Community Health Centre/Primary Health
Centre/Sub-Centre
3.20 Observations, Suggestions and Overview
3.21 State Level
3.22 District Level
3.23 Community Health Centres
3.24 PHC/Sub-centre Level
3.1
3.2
3.3
3.4
3.5
3.6
43
44
44
45
45
45
46
48
49
50
51
51
53
58
60
63
64
65
66
66
72
72
73
74
EPIDEMIOLOGICAL SURVEILLANCE SYSTEM
INCLUDING INSTITUTIONAL SUPPORT
SERVICES
4.
General Introduction
Notification System
Diseases that are notifiable
Legal Provisions for Notification
Reporting Agency
Defects in Notification
Epidemiological Units and Investigations
Public Health Laboratories
Isolation and treatment facilities
Quarantine Administration
Anti-Mosquito and anti-rodent measures at Ports
and Airports
4.12 Collection and dissemination of Statistics
4.13 Observations, Suggestions and Overviews
4.14 Institutional Supprt Services
4.1
4.2
4.3
4.4
4.5
4.6
4.7
4.8
4.9
4.10
4.11
76
77
78
78
79
79
81
81
82
82
83
83
96
99
STATUS OF CONTROL STRATEGIES FOR
EPIDEMIC DISEASES
5.
5.1
5.2
5.3
5.4
5.5
5.6
5.7
5.8
5.9
5.10
5.11
General Introduction
Malaria
Kala-azar
Japanese Encephalitis
Dengue
Diarrhoeal Diseases including Cholera
Poliomyelitis
Measles
Viral Hepatitis
Strategy for Control of Epidemic Diseases
Observations, Suggestions and Ovendews
103
105
109
110
111
112
113
114
114
114
116
EXISTING HEALTH SCHEME
6.
6.1
6.2
6.3
6.4
6.5
6.6
6.7
6.8
6.9
6.10
Rural Health Service Scheme
Health Manpower in Rural areas as on 31.03.95
Health Manpower in Tribal areas as on 31.03.95
Training of professionals and para-professionals
Village Health Guide Scheme
Mini Health Centre Scheme of Tamil Nadu
Rehbar-i-Sehat Scheme in J & K
Child Survival and Safe Motherhood Scheme
Universal Immunisation Programme
Suneillance of Vaccine Preventable Diseases
ii
118
123
123
125
126
128
129
129
130
131
6.11
6.12
6.13
6.14
6.15
6.16
6.17
6.18
6.19
6.20
6.21
6.22
6.23
6.24
6.25
6.26
6.27
6.28
6.29
7.
Testing of Oral Poliovaccine
Oral Rehydration Therapy for Diarrhoea control
among children
Programme of Acute Respiratory' Infection
Iron Deficiency
Vitamin A Deficiency
Safe Motherhood Services for Pregnant Women
Care of Newborn and infants
National Malaria Eradication Programme
National Leprosy Eradication Programme
National Tuberculosis Control Programme
National Filaria Control Programme
National Guineaworm Eradication Programme
National AIDS Control Programme
National Kala-azar Control Programme
National Programme for Control of Blindness
National Iodine Deficiency Disorders Control
Programme
National Diabetes Control Programme
National Cancer Control Programme
Observations, Suggestions and Overviews
135
135
136
136
137
139
144
145
146
147
148
150
150
152
154
155
157
NATIONAL FAMILY WELFARE PROGRAMME
7.1 Introduction
7.2 Family Welfare Programme During the First
Seven Five Year Plans
7.3 Observations, Suggestions and Overviews
8.
131
133
161
161
177
ENVIRONMENTAL HEALTH AND SANITATION
8.1 Introduction
8.2 Constitutional Obligations for Environmental
Health and Sanitation
Water
Supply
8.3
8.4 Sanitation
8.5 Hospital Waste Management
8.6 Drinking Water Quality- Surveillance - Legislation
and Standards
8.7 Operation and Maintenance
8.8 Industrial Waste Management and Air Pollution
Control
8.9 Air Pollution control in India
8.10 Observations, Suggestions and Overviews
in
183
185
186
187
191
191
192
192
195
198
EPIDEMIC REMEDIAL MEASURED - ROLE OF
STATE AND LOCAL HEALTH AUTHORITIES
9.
9.1
9.2
9.3
9.4
9.5
9.6
9.7
Introduction
State Health Directorates
Municipal Health Authorities
District Health Authorities
Primary Health Centre Infrastructure
Panchayati Raj System
Observations, Suggestions and Overviews
201
201
202
203
203
204
204
CURRENT STATUS OF HEALTH
MANAGEMENT INFORMATION SYSTEM AND
ITS ROLE
10.
10.1 Introduction
10.2 Evolution of HMIS in India & its current Status
10.3 Current Status of HMIS implementation in
10.4
various states
Observations
206
206
211
211
REC COMMENDATION S
11.
11.1 Short Term
11.1.1 Policy Initiatives
11.1.2 Administrative Restructuring
11.1.3 Health Manpower Planning
11.1.4 Opening of Regional Schools of Public Health
11.1.5 Strenthening & Upgradation of the Departments
of Preventive and Social Medicine in Idetified
11.1.6
11.1.7
11.1.8
11.1.9
11.1.10
11.1.11
11.1.12
11.1.13
11.1.14
11.1.15
11.1.16
11.1.17
11.1.18
Medical Colleges
Reorganised functioning of the Department of
PSM in Medical Colleges
Establishment of a Centre for Diseases Control
Primary' Health Care Infrastructure in Urban
Areas
State Level
District Level
Establishment of a supervisory’ mechanism at.
Sub-district level
Community- Health Centres
PHC/sub-centre level
Village level
Prevention of Epidemics
Upgradation of Infectious Diseases Hospitals
Water Quality Monitoring
Urban Solid Waste
iv
213
213
216
216
217
217
218
218
218
219
219
219
220
220
221
221
224
224
224
v
11.1.19
11.1.20
11.1.21
11.1.22
1 1.1.23
I 1.2
11.2.1
1 1.3
Inter-sectoral co-operation
Nutrition
Decentralised uniform funding pattern
Non Governmental Organisations (NGOs)
Involvement of ISM & Homoeopathy
Long Term
Broad set-up of Ministry'
Funding
o
225
225
226
226
227
227
227
228
12.
ACTION PLAN FOR STRENGTHENING OF
PUBLIC HEALTH SYSTEM
229
13.
ACKNOWLDGEMENT
23S
14.
BIBLIOGRAPHY
239
15.
ANNEXURES
i-lii
v
Cor^i H LhC|.
EXECUTIVE SUMMARY
E-1.0 INTRODUCTION
India is a large country with around 900 million population in 25 states
ami 7 Union Territories. I listoricallv Irmlia had a rich public heath system as
evidenced from the relics of Indus Valley civilisation demonstrating a holistic
approach towards care of human and disease. I he public health system
declined through the successive invasions through the centuries, intrusion of
modern culture and growing contamination of soil, air and water from
population growth. With the establishment of British rule and the initiation
of practice of Western medicines in India strong traditional holistic public
health practice in India went into disuse bringing disease-doctor-drug
orientation. The so-called modern public health practice of the advanced
European and industrialised countries was primarily set up around
cantonments, district and State Headquarters in British India.
E-l.l Bv the time India achieved independence socio-political and economic
degradation reached to an extent where hunger and mal-nutrition were
almost universal; 50% of the children died before the age of five, primary
health care was very rudimentary or non existent and the state of public
health was utterly poor as evidenced through life expectancy at birth around
26, infant mortality rate 162, crude death rate around 22, maternal mortality
rate around 20. Only 4.5% of the total population had access to safe water
and onlv 2% of the people had sewerage facility. Number of medical
institutions were few and trained para professionals like nurses, midwives,
sanitary inspectors were barely skeletal in numbers. The picture on the
nutrition front was very grave. Food production, its distribution and
availability of food per capita were all unsatisfactory. MCH services, school
health services, health care facilities for the industrial workers, environmental
health were all far from satisfactory.
V
E-1.2 Under the Constitution, health is a slate subject and each state has its
health care delivery system. The federal government's responsibility consists
of policy making, planning, guiding, assisting, evaluating and co-ordinating
the work of various provincial health authorities and also supporting various
on-voing schemes through several funding mechanisms. By and large heall r
care delivery system in India in different states has developed following
independence on the lines of suggestions of the Bhore Committee which
recommended delivery of comprehensive health care at the door step of the
population through the infrastructure of primary health centres and sub
centres. During the last eight 5 year plans following independence a large
network of primary health care infrastructure covering the entire country ras
been established. In addition, several national health and disease contio
programmes were initiated to cover a wide range of communicable diseases
namely, malaria, filaria, tuberculosis, several vaccine preventable diseases Ime
diphtheria, pertussis, tetanus, polio, measles etc. and to also cover some
important non-communicable diseases like iodine deficiency cnsort ers,
1
PHSl'ind! j\)C
conlio’ of biinciness, cancer, diabetes etc. The progress was periodically
rcvic’.ved through con.stitution of several committees like Mudaliar
Committee, School Health Committee, Chadha Committee, Mukherjee
Committee etc.
To provide more thrust on Hie improvement of
environmental health and sanitation the responsibilities pertaining to water
supply, s-nutation and enviroiimcntal related issues were tran.sferrcd to the
concerned ministries of Urban Development, Phiral Development and
Environment and Forests.
Major initiatives were taken up in our efforts to
reach Health for /ch by 2001) A.D. on the lines of policv directives enunciated
in National Health Policy. Eighth plan starting in 1992-93 clearly emphasised
that the health facilities must reach trie entire population by the end of Sth
plan and that tire health for all paradigm must not only take into account the
high risk vulnerable group i.e. mothers and children but also focus on the
under privileged segments both within and outside the vulnerable group. All
tiie efforts put through the last four and a half decades following
independence made significant dent in the improvement of health indices
viz. IMR 74 (1994), water suppiv urban area 54.9%, rural area 79.2% (1993),
sanitation urban area 47.9% (1993), rural 14% (1994), crude death rate 9.2%
(1994). expectation of life at birth Male 60.4% (1992-93) and fernale 61.2%
(1992-93). Significant number of doctors and para medical staff are available
and the food productions have been raised from 50 million tonnes in 1950 to
1S2 million tonnes in 1993-91 increasing the per capita availability even in
spite of large population growth from 394.9 gm in 1951 to 474.2 gm in 1994.
E-1.3 In spite of this significant development and impressive growth in
health care, enormous health problems still remain to be tackled and
addressed to.
Though mortality has .declined appreciably yet survival
standards are comparable to the poorest of the nations of the world. Even
within the country wide differences exist in the health status in the states like
Bihar, Orissa, Madhva Pradesh, Rajasthan to that of Karnataka,- Maharashtra
and Punjab which have done exceedingly well in terms of quality of human
life. Major problems facing the health sectors are, lack of resources, lack of
multi-sectoral approach, inadequate 1EC support, poor involvement of NGOs,
unsatisfactory laboratory support services, poor quality of disease
surveillance and health management information system, inadequate
institutional support and poor flexibility in disease control strategy etc.
E-1.4 In the background of the above and also in the light of the observations
in recent times following review of the rural health services, national
programmes like malaria, tuberculosis, UIP etc. concern has been expressed
that whether our efforts will succeed in achieving the goal tor reaching
Health for. All by 2000 A.D. In fact experts are of the opinion that Health tor
All bv 2000 A.D. is not a distinct possibility. It may have to be revised
backwards by a decade or two. The concern has been further compounded
follo’A’ing the recent outbreaks of malaria and plague indicating poor
o
response^ capability of the existing public health system in meeting the
caoabilitv
emergent challenges of the modern days particularly die threat posed by ne^,
A
J
o
phsi'uinl tio<*
emerging and re-emerging human pathogens.
In this context, the
Government of India constituted an expert committee to comprehensively
review the public health system in the country under the chairmanship of
Prof. J.S. Bajaj, Member, Planning Commission to undertake a comprehensive
review of (a) public health system in general and the quality of epidemic
surveillance and control strategy in particular, (b) the effectiveness of the
existing health scheme, institutional arrangements, role of states and local
authorkies in improving public health system, (c) the status of primary health
infrastructure, sub centres and primary health centres in rural areas specially
their role in providing intelligence and alerting system to respond to the
science of outbreaks of disease and effectiveness of district level
administration for timely remedial action and (d) the existing health
management information system and its capability to provide up-to-date
intelligence for effective surveillance, prevention and remedial action. I he
committee had four meetings in addition to interaction between the members
of the expert committee.
The summary of the observations and
recommendations suggested by the committee are summarised here.
E-2.0 PUBLIC HEALTH SYSTEM IN INDIA
E-2.1 Federal Set up
The federal set up of public health system consists of Ministry of
Health & Family Welfare, the Directorate General of Health Services with a
network of subordinate offices & attached institutions and the Central
Council of Health & Family Welfare. The Union Ministry of Health & Family
Welfare is headed by a cabinet minister who is assisted by a Minister of State
It has three departments namely, Department of Health, Department o
Family Welfare and Department of Indian Systems of Medicines. The
Department of Health deals with the medical and public hea th matters
■ including drug control and prevention of food adulteration throug i
e
Directorate General of Health Services and its supporting offices. Director
General of Health Services renders technical advice on all medical and pu ic
health matters and monitors various health schemes. Director General of
Health Services also renders technical advice on family welfare programmes.
The functions of the Union Ministry of Health and Family Wellare are to cany
out activities to fulfil the obligations set out in the 7th Schedule of the Article
246 of the Constitution of India under Union and Concurrent hs .
The federal government has set up several regulatory bodies for
monitoring the standards of medical education, promoting training and
research activities namely, Medical Council of India, Indian Nursing Council
Pharmaceutical Council etc. In addition to the Union Ministry of Health &
Family Welfare, Planning Commission has a Member (Health) o the rank of a
Minister of State who assists the Ministry of Health in formulation of plan
through advice and guidance and the expert guidance is also available for
monitoring and evaluation of the plan projects and schemes.
3
phstinal.doc
E - 2.2 S t a I c 1 c v c 1
i iic Stale governments have full authority and rcsponsibililv for ail the
Health services if' their territory. The State Ministry of Health & Famiiv
Wehaie H headed by a Minister of Health C Family Welfare either of a
Ccbme: rank or a Minister of State. Often he/thev is/are assisted by a Deputy
Ministei depending upon the political situation. The Health Secretariat is the
Official organ of the State Ministry of Health & Family Welfare and is headed
by a Secretary/Principal Secretary/Commissioner as the case may be. State
Health Secretariat is assisted by a technical wing called the State Health
Directorate. Earlier all the functions pertaining to health and family welfare
and medical education were integrated. However, now in manv states
directorates of public health sendees, posts of Director of Public Health,
Director of Family Welfare and Director of Medical Education have been
separated and they report directlv to the Secretary.
E-2.3 District Level
Hie princmal unit of administration in India is the district which is
under-?. Collector/District Magistrate/Dcputv Commissioner. The size of the
districts vary widely from less than 0.1 million to more than 3 million and the
district public health system is headed bj* the Chief Medical and Health
Officer/District Health Officer.
L-2.Communi t v 11 cck: i Ce n trc/i ''ri mai y Heai th Cen tre/Sub Centre
Apart from the headquarters of the district having district hospitals
and the office of the Chief Medical and Health Officer, the district has a
network of hospitals, dispensaries, community health centres, primary health
centres and sub centres to cover the entire population of the district with
regard to health care delivery services. It lias also the network of hospitals
and dispensaries under the Indian Svstems of Medicine and Homoeopathy.
P-?..S Hmlth is a multi-ministerial rcsponsil»ility. Many of the activities
undertaken by the other ministries have tremendous impact on the health of
the people.
Several policy initiatives related to agriculture, urban
development, industrial packages have far reaching health linkages involving
higher morbidity and mortalitv. The same need to be analysed through
appropriate health impact assessment studies for guidance of policy makers.
E-2.6 Many of the areas under the National Health Policy have not yet been
implemented.
During the last decade massive changes have occurred
through destruction of ecological svstem, rapid urbanisation, large population
growth, industrial revolutions etc. leading to changes in health and
demographic scenario. Appearance of new, emerging and re-emerging health
4
phsHnnl doc
problems has been causing concern. This calls for review of the National
Health Policv.
E-2.7 India is a large country with diverse socio economic situations.
I herefore, uniform health care deliverv system is not likely to yield the
desired results. Therefore, continued efforts to develop alternate strategies
should be there so that the same could be appropriately dovetailed within the
overall framework of the health care delivery system to obtain better results.
E-2.8 73rd and 74 Constitutional amendments have provided immense
administrative and managerial authorities to the Panchayats and
municipalities. The same should be fully exploited with appropriate
delegation of financial authorities to improve the public health system.
E-2.9 Several ministries arc involved in public health related activities.
Hardly any appropriate inter-sectoral co-ordination and co-operation
mechanism exists.
E-2.10 In the present organisational set up of the Ministry of Health & Family
Welfare there are several areas of duplications and there is excessive
bureaucracv. Not enough number of senior public health positions exist.
Manv-of the important positions requiring public health responsibility are
being managed through non-Public health professionals. For several key
areas like environmental health & sanitation, manpower planning hardly any
component exists in the DGHS.
E-2.11 Indian Systems of Medicine & Homoeopathy has large number of
professionals. They are not being appropriately exploited to supplement the
modern health care delivery services particularly in the area of awareness,
community participation etc.
E-2.12 Rapid urbanisation has led to phenomenal growth in urban
population. 25-30% live now in urban area. Though tertiary care services are
available but primary care is grossly neglected here leading to higher
morbiditv & higher mortality amongst urban poor and slum dwellers and to
also over straining of tertiary care health services.
E-2.13 Earlier practice of integrated delivery of health care services is being
eroded through creation of separate directorates in several states leading to
disintegrated pattern of medical and health administration, Growth of
bureaucracv as evidenced through placement of bureaucrats as Directors of
Health Services or as heads of primarily medical and health organisations is
also responsible for erosion of public health machinery.
E-2.14 Epidemiological support services and public health laboratory facilities
at the district level is grossly inadequate..
5
phsfinaldoc
E-?.15 Referral services in the communit)' health centre is poor. Public health
specialised services in the community health centre is totally lacking.
o
E-3.0 EPIDEMIOLOGICAL- SUK^'L;IL.LzYNCE 5YSJ_LM
E-3.1 Epidemiological services were grossly inadequate prior to
independence but have since developed to a great extent, concurrently with
th- national control/eradication programmes for various diseases like
malaria, tuberculosis, leprosy, cholera, vaccine preventable diseases filaria
etc However, there is a conspicuous lack of uniformity in the lists of diseases
which are notifiable in different states and also from the view point of
primarv agency responsible for reporting. Cholera, yellow fever and plague
which are under International Health Regulations are notifiable throughout
the country. The other important diseases which are notifiable in one state or
the other are viral hepatitis, enteric fever tuberculosis, influenza, meningitis,
Japanese Encephalitis, rabies, diphtheria, leprosy, measles, poliomyelitis etc. ■
Notification system in operation in various states is usually supporte
through certain legal provisions. The position with regard to legal provisions
also varies from state to state and some state governments do noc have am
specific act excepting invoking the Epidemic Diseases Act 1897. In urban areas
the responsibility lies with the municipal health authorities. Common defects
in notification are delay and inaccuracy in reporting the cases and un
reporting.
E-3.2 Epidemiological investigations have a key role to play in
control of diseases. For co-ordinating and carrying out such mvesUga>1 .
epidemiological units/cells have been established in a number of stales
there are sla’tes where such units have not been established yet. Pubiu. heahh
laboratories plav a premier role in verification of diagnosis, in assisting
epMemioloricartracing of the spread of the outbreak and in underslandin
X natural cvcle of the disease. In most of the stales, pubhc health
laboratories are not functioning very efficiently and there >s hardly an)
facilities for virus isolation work in these public health laboratories.
E-3 3 Wide variation in tire notification system being implemented by
various sta.es/UTs make the data lack in epidemioldg.cal qyahty and bus
hardly offers inputs for an effective response. The data generated y_°“S ‘
massive rural health infrastructure and hospitals and dupensa
.
received late and are non-uniform with scanty laboratory support It: indud
no reporting and truncated reporting from —ra areas due to complete
biackout of surveillance In time & space due to »
of asons - n
availability of health personnel, apathy of health personne, p
management, errors in reporting etc.
■•’ .l‘ • J do
6
E-3.4 Surveillance data generated through the system and through various
programmes are considered at best indicative of trend rather than the actual
situation in the community and mortality and morbidity numbers reported
are grossly under estimated.
E-3.5 Though major national health and family welfare programmes have
institutional support services but such support mechanism is grossly
inadequate to meet the challenging needs of the modern programme
management. With large amount of information being generated covering
various areas of development and various scientific disciplines, there is an
urgent need for their appropriate analysis, understanding and dovetailing to
make the on-going programmes more modern and updated. Unfoi tunately,
in several of the programmes such formal mechanism does not exist. Though
a large number of medical colleges, national and referral institutions are there
not much has been done in the context of harnessing the expertise through a
formal linkage mechanism.
E-4.0 STATUS OF CONTROL STRATEGIES FOR EPIDEMIC DISEASES
E-4.1 /Xppropriate guidelines for detection of outbreak and early warning
signal mechanism for epidemic prone diseases are not nationally available. It
ally provided by NICD on ad hoc basis.
is usually
E-4.2 Though several diseases with epidemic potentiality are covered
through national disease control/eradication programmes like National
Malaria Eradication Programme, Universal Immunisation Programme, there
is no centrallv sponsored or central scheme to tackle epidemic prone diseases
in general. National Malaria Eradication Programme provides guidelines
with respect to detection and containment of epidemic of malaria and kalaazar and so also several of EPI targeted diseases have appropriate guidelines
for epidemiological investigations. Guidelines have provisions of initiating
control measures but none of the guidelines have a component of generating
earlv warning signal and thus helping in identification of outbreaks early.
For many of the diseases like poliomyelitis, cholera, viral hepatitis, adequate
diagnostic support services are not available as a result many of them are not
detected and reported. Even in most of the medical colleges facilities foi
identifying new sero types of cholera are not available.
E-5.0 EXISTING HEALTH SCHEME
E-5.1 There are large number of schemes functioning in the country like
Development of health infrastructure, Training of professionals and para
professionals. Village health guide. Mini health centre, Rehbar-i-Sehat
scheme, Child survival and safe motherhood scheme including HIP,
Programme of Acute Respiratory Infection, ORT, etc. in addition to severa
major diseases control/eradication programmes covering diseases of pu ic
7
phsfinal.doc
health importance like malaria, leprosy, tuberculosis etc. under communicable
diseases and blindness control, iodine deficiency disorders, cancer and
oiaoetcs etc. under chronic diseases. In addition to tlie above programmes
under the Ministry of Health and Family Welfare there are several schemes
under other ministries like Ministry of Rural Development, Ministry of Urban
Development, Ministry of Environmcnl & Forests and Ministry of Welfare to
cover wide areas of environmenta.1
environmental health, water supply, sanitation and child
health.
E-o.2 All the schemes have been aimed to improve the public health system.
Large nurnbci Oi agencies are involved. Co-operation and co-ordination
between these agencies are grossly inadequate and thus many of the
programmes do not give satisfying performance.
E-5.3 Multiplicity of funding mechanism, poor administrative fc-financial
authority’ at the peripheral points,, multiplicity in administrative authority
lead to poor performance.
E-6.0 NATIONAL FAMILY AATLFARE PROGRAMME
E-6.1 •India was tlie first country-’ to have an official family welfare
programme which was initiated in 1952. Since then, during tlie subsequent
eight five year plans, family planning as a measure of population control has
been receiving liigh priority' attention in each of the five year plans. During
tlie 3rd five year plan (1961-66), family planning received a major boost and it
v*as declared the very centre of plan development and in the year 1966 a
separate Department of Family Planning was established in the Ministry of
Health and the extension approach was further modified into an integrated
approach and thus family planning became an integral part of MCH and
nutrition services. Tlie National Health Policy has indicated a long-term
demographic goal of achieving replacement level fertility’ (net reproduction
rate oi 1.0) by the year 2000 A.D. wluch would necessitate achieving a birth
rate of 21 per thousand, death rate of 9 per thousand and annual population
growth rate of 1.2 per cent. The 7th plan document visualised the goal of
icacliing the same by 2006-11. However, keeping in view die level of
acliievement the Sth plan document has envisaged to achieve the same by
2011-16.
E-6.2 lhe family planning programme has not been able to achieve fully the
demograpliic goals which are vitally’ linked with improvement of public
e health system in the country. States which have done exceedingly well on
the demographic front have also done well on the health front.
E-6.3 Creation of a separate department leading, to disintegration of earlier
integrated way of functioning has not improved performance.
g
ph'.rinjl (* DC
E-6.4 Poor referral services to a great extent are responsible for high
maternal and infant mortality Only few first referral units are functional.
E-6.5 India is a vast country. Efforts of the government alone can not meet
the needs. Though a large number of NGOs are functioning well in the
country, not much efforts have been made in that direction to involve them
more effectively in the delivery of health & family welfare services.
E-7.0 ENVIRONMENTAL HEALTH AND SANITATION
Though environmental health and sanitation received priority
attention in all the successive plans but level of environmental health and
sanitation both in rural areas and in urban areas continues to be poor in spite
of significant achievements in terms of coverage and quality of service. This
has been largely due to large population growth, urbanisation,
industrialisation, population movements and ecological changes. Following
the Bhore Committee recommendations an Environmental Hygiene
Committee was constituted in 1948-49 and in 1953 a national level technical
body (Central Public Health Engineering Organisation) was established in the
Ministry of Health to undertake national water supply and sanitation
programme. In 1973 the subject of water supply and sanitation was
transferred from Ministry of Health to Ministry of Works and Housing and
local self government (presently redesignated as the Ministry of Urban Affairs
and Employment). The Water (Prevention and Control of Pollution) Act of
1974 was another milestone in the prevention and control of water pollution
in the country. For implementation of the Act, a Central Pollution Control
Board at the national level and State Pollution Control Boards at the state
level were established in 1974. The Act was amended in 1988. The Air
(Prevention and Control of Pollution) Act, 1981 amended further in 1987 has
provided an instrumentation to improve the environment. In 1981
International Drinking Water Supply and Sanitation Decade was launched. In
addition to that centrally sponsored rural sanitation programme and several
other programmes were also initiated by different ministries. In spite of all
these efforts, recurring outbreaks of gastrointestinal disorders and
haemorrhagic dengue fever etc. and large scale outbreaks of malaria and
plague in recent years point towards insufficiency in our efforts in improving
environmental health and sanitation. The low level of urban, peri-urban and
rural sanitation is a matter of deep concern. Multiple operating agencies with
poor co-ordination between them have added to poor programme efficiency.
E-8.0 ROLE OF HEALTH AUTHORITIES IN EPIDEMIC REMEDIAL
MEASURES
E-8.1 Health is a state subject and the entire health care delivery services
including epidemic remedial measures are primarily through the State
9
phsl'inal doc
governments v/bo have the constitutional authority and obligations to
implement the health care delivery services. The municipalities and the local
authorities and the State governments though have the constitutional
authority and obligations to effectively implement the public health
programmes but they are unable to function satisfactorily in that direction
because of paucity of resources, non-availability of the expertise in terms of
personnel and institutional support etc. and also due to appiopnate
perception of public health problems. Many of these local bodies cio not have
requisite financial authorities.
E-S.2 ■ Municipal Bye-laws and the local bye-laws are wide!) in variation
from one and another and many of them are outdated. Many Oi the
provisions of municipal bye-laws and local bye-lav/s though tecluiically
sound but do not yield desired results because of poor implementation.
9.1
initially I IMIS was started in the states of Havana, Gujarat, Rajasthan
and Maharashtra on pilot basis Ln one district each of the states, the system
was manual and the data which was generated as a result of implementation
of the pilot project proved very useful. On the basis of the achievement of
HMI5 which was known as HMIS Version 1.0, the programme officers of
. ' State
cl ■ Governments
rfrom th°
various
ana ovnprtc
experts nuin
ui^ related fields were consulted
and the inputs for each level of institution responsible for health care delivery.,
were designed and developed.
E-9 2 During the year 1988-59 National Informatics Centre set up Satellite
bas^d computer communication network called NICNET and the HMIS was
again modified and modified computerised formats designed and developed
m the shape of Version 2.0 were implemented. It has become fully
operahonal'in Haryana, Sikkim and in several other states it is in differen
stages of implementation.
p!i$• • r si w'C
10
CoH: U-t-
11.
RECOMMENDATIONS
11.1
Short-term
11.1.1 Policy Initiatives
11.1.1.1
5
Review of Nati ona 1 IIea 1th Policy
The National Health Policy was formulated and adopted in
1983. During the years since then major changes have occurred
through continuing population growth, rapid urbanisation, industrial
revolution, changing health and demographic scenario, appearance of
new, emerging and re-emerging health problems etc. Two important
constitutional amendments namely 73rd and 74th have been passed
giving more responsibility and authority to municipalities and
panchayats and thus providing appropriate tools to the community to
deal with health, water supply and sanitation etc. more effectively. In
view of the same, the National Health Policy needs a careful and
critical reappraisal.
The committee, therefore, recommends
constitution of a Group of Experts to prepare the draft of the new
National Health Policy by the end of 1996.
Establishment of health impact assessment cell
11.1.1.2
While the link between economic growth and better health is a
strong one, growth in income and a developing economy do not
necessarily ensure improved health status. Many developing countries
are concerned with the possible health impact of economic
restructuring and development policies. The Committee, therefore,
recommends that there is a need to enhance the capacity and capability
of the Ministry of Health & F.W. to undertake health impact
assessment for major development projects, industrial units etc. so that
the project/industrial authorities could be appropriately advised &:
guided to incorporate proper intervention measures/changes as the
case may be. All large projects of different ministries should invariably
have health component in the proposal itself and this should be
examined and approved by the Ministry of Health & Family Welfare.
Regular analysis of various public policies and practices of other
ministries viz. agriculture, industry, urban development, rural
development and environment, which have direct link with the health
of the people, must be considered as an essential prerequisite for a
meaningful inter-ministerial co-ordination.
11.1.1.3
Surveillance of critically polluted areas
In view of the population explosion and unplanned
urbanisation and industrialisation, diseases due to ecological and
213
PHSfmMoc
environmental imbalances arc increasing.
Health impact and
environmental epidemiology related to air, water, and soil pollution
need to be monitored and evaluated particularly in the critically
polluted areas in the country. Ministry of Health and Family Welfare
should initiate actions in this regard urgently, in co-ordination with the
Ministries of Environment, Industry and Urban Development.
Measures such as a properly maintained data-base, mapping of the
vulnerable areas, immediate intervention where possible and
continuing surveillance need to be initiated as a well structured
programme of action.
This is particularly important in view of the large inputs
provided by the Ministry of the Environment and Forests for 100
critically polluted towns and cities. Such surveillance will enable to
understand impact of the interventions made and take appropriate
corrective measures.
11.1.1.4
Search for alternative Strategy/ strengthening of health
serviccs/systcm research
India is a vast country. Uniform health care strategy for the
"entire countrv is not likely to succeed because of a variety of reasons:
geographic, socio cultural, ethnic, economic etc. Therefore, a
continuous search for alternative health care strategies needs to be
undertaken by the health implementing agencies through appropriate
health services research. At present, health system/services research
receives very inadequate support and poor response from the health
directorates.
Therefore, the Committee recommends allocation of
adequate funds to the Centre, UTs and State Directorate of Health
Services enabling them to undertake or commission Health
Services/System Research and Intervention Studies and to ensure that
such research results are utilised to improve the health care delivery
services.
11.1.1.5
Uniform adoption of Public Ilcallh Acl by Hie local health
authorities
Model Public Health Act revised and circulated in 1987 should
be examined by all State health authorities, municipalities and local
health authorities carefully and adopted/enacted to suit local and
national needs. This will give a uniform, updated and modern tool to
tackle many of the old and new, emerging and re-emerging health
problems more efficiently. This is all the more important in view of the
recent 73rd and 74th Constitutional Amendments providing enormous
political, administrative and managerial authorities to local and
municipal bodies so as to enable them to take care of human health and
development.
214
rz/sruhil doc
11.1.1.6
J^abHshing National Notification System/National Health
Regulations
The notification system as it exists today varies vvidelv from
state to state and within the state from area to area. The Committee
recommends the constitution of a Task Force drawing experts from
states, NGOs, and public health institutions to examine the existing
notification system and prepare draft National Health Regulations for
adoption bv all states. This should be time bound and completed bv
1996.
11.1.1.7
Joint Council
Homoeopathy
of Health,
Family Welfare
and
ISM
&
Indian Systems of Medicine and Homoeopathy should be
appropriately involved in strengthening further the public health
system of the country. Therefore, the committee recommends that the
existing Joint Council of Health & Family Welfare should be further
broad based to make a Joint Council of Health, Family Welfare and
.Indian Systems of Medicine & Homoeopathy.
11.1.1.8
Establishing an Apex Technical Advisory Body
In order to ensure a mechanism of continuing review and
appraisal, the committee recommends to establish an broad based
Apex Technical Advisory Body and advise the government
accordingly.
11.1.1.9
Constitution of Indian Medical & II ealthServices
The Committee reinforces in the strongest terms the need to
constitute Indian Medical & Health Services without anv further
delay. This has been a long felt need and was recommended as early
as 1961 by Mudaliar Committee. Many of the central health
programme managers have no formal education in public health and
management and have never worked in the states, as a result they do
not have appropriate perception of the problems of thestates leading
to poor professional communication and understanding between
central and state government health programme managers. 1 Creation
of Indian Medical & Health Services will facilitate bridging this gap
and improve technical leadership and management both at centre and
state levels.
215
PHSMdoc
11.1.2 Administrative restructuring
11.1.2.1
Organisational set up of the ministry
11.1.2.1.1
There are presently three departments in the Union Ministry of
Health & F.W. each headed by a Secretary, and tire DGHS is headed by
a technocrat. Co-ordination between departments is not satisfactory'
and several times it has been seen that they' work in water-tight
compartments and the interaction between different programme
managers has often been found unsatisfactory. Even between the
working of the DGHS and Department of Health there are several
areas of duplication. Most of the functions of the Union Ministry' of
Health and Family Welfare are highly teclinical in nature and,
therefore, require technical leadership of a high quality.
Tire
committee therefore, strongly recommends that tire union Ministry of
Health & Family Welfare may consider merger of the two departments
of Health & Family Welfare and that the single department so created
benefits from technical leadership as indicated above, lhe department
of ISM and Homeopathy may' also be similarly' restructured.
The Department of Health & Family Welfare and DGHS should
11.1.2.1.2
be restructured and reorganised; while doing so emphasis should be
given to strengthen Planning, Food and Drug Division of DGHS. New
Divisions of Environmental Health & Sanitation, Health impact
assessment Cell and Health Manpower Division should be established.
11.1.2.1.3
All the major technical divisions under the Union Ministry' of
Health & Family Welfare and major institutions/organisations should
have an advisory body to periodically- review the functioning of these
divisions, institutions and suggest an appropriate corrective step for
improving their various activities.
11.1.3 Health Manpower Plannin
11.1.3.1
The DGHS should have a strong Health Manpower Planning
......... Division; appropriate institutional support mechanism by creation of a
National Institute of Health Manpower Development may also be
considered.
1-1 i 3 o
The committee reiterate that recommendations contained in
‘ ' ’‘Baja; committee report of 1987 on health manpower planning
' production and management should be implemented in n ht
earnestness which will greatly strengthen public health system in the
country. Primary health care provision being a team f
training and continuing education of the professional and p a
professionals should have components of training/education of the
Pliyinal doe
216
entire team together in addition to training of the individuals. This
multi professional education approach will provide cohesive
functioning of the team and improve quality and coverage of health
services.
11.1.3.3
The Union Ministry of Health & F.W. is primarily responsible
tor public health services but it does not have requisite number of
senior level public health professionals. Many programme managers
at the national level are without any public health orientation or public
health qualifications. The committee, therefore, recommends that
positions requiring public health tasks should be filled by appropriate
qualified public health professionals and until these professionals are
available, these could be operated by general category health
professionals through appropriate training in health services
administration, management and epidemiology.
11.1.4
Openiiig of Regional Schools of Public Health:
There is a need to open new schools of public health so that
more public health professionals and para-professionals • could be
trained. The existing public health schools also be appropriatelv
.strengthened. The committee recommends that at least four more
regional schools of public health are set up in Central, Northern,
Western and Southern regions. Duly modernised schools could be in
the pattern of All India Institute of Hygiene and Public Health,
Calcutta and School of Tropical Medicine, Calcutta.
11.1.5
Strong t hening and upgradation of the Departments of
Preventive and Social Medicine in identified medical colleges
Establishing new schools of public health will require several
years in terms of obtaining resources, construction of buildings etc.
For a vast country like India even establishing few more schools of
public health will not be able to meet the entire needs. Therefore, it is
recommended that some of the existing medical colleges who have
very significant expertise in teaching of preventive and social
medicine/community medicine should be further strengthened in the
form of establishing an advanced centre for teaching of public health or
upgrading the existing departments so that it can take up additional
responsibilities of continuing education in public health subjects for
health professionals and also to undertake responsibilites for
producing more public health professionals to meet the demands of the
countrv. In this context, it is strongly suggested that a centrally
sponsored programme of upgradation of few identified departments of
preventive and social medicine in the medical colleges could be taken
up during the last financial year of this Plan and during the 9th Plan
period at least 25% of existing departments may be similarly upgraded.
217
These centres could be linked through a network so that the facilities
could be maximally utilised.
11.1.6
l<eorg^sjd_JinTCtigriinr of the Department of PSM
Medical Colicqcs:
in
The S v stem of providing an exposure to the community health
care to the physicians through the Department of Preventive and Social
Medicine at the medical college under the ROME scheme has not met
with anticipated success as it provides very limited exposure to
community health programmes. It is suggested that the State/District
National health programme management focal points are posted for
sometime in the Deptt. of PSM in medical colleges so that the
programme managers get the benefit of updated academic and
technical skills and the students are benefited from the practical
experience of the programme managers at the field level Similarly
teachers of Preventive and Social Medicine should be posted in the
district for some time to act as a focal point for national health
programmes.
11.1.7
Establish in!; a Centre for Disease Contro 1
To make the public health system more responsive to the needs
of new, emerging and re-emerging health problems and also to meet
the challenges of escalating
epidemic of non communicable
diseases the need for establishing a Centre for Disease Control at the
national level is strongly felt. The committee, therefore, is of the view
that National Institute of Communicable Diseases, Delhi should be
substantially strengthened through capacity building into a National
Centre of excellence for
__ Disease
---------- Control
--------- 1 on the pattern of similar
advanced centres such as CDC, Atlanta.
11.1.8
Primary Health Care infrastructure in urban are a s:
The basic health care infrastructure in the urban area which
caters to the needs of 25% ■ 30% of the population is grossly deficient.
In view of the recent initiatives to give more financial and managerial
authorities to the municipal bodies, immediate attention need to be
given to develop the health care infrastructure in urban area. The same
.will reduce stress and strain on the secondary and tertiary health care
facilities available in the urban areas. The committee recommends that
an Expert Group be constituted to suggest restructuring or even
redesigning of health care infrastructure including referral and linkage
upto and including tertiary care in urban areas.
218
■
due
11.1.9
State Level:
Creation of several positions of Directors at the State level has
led to disintegration of earlier integrated pattern of medical and health
administration. Earlier practice needs to be restored. It is also
recommended that functioning of the Department of Health being
mostly that of technical nature a technical man should be the head of
the Departmewl of Health instead of a bureaucrat.
The committee recommends that on the general principles
suggested for reorganisation and restructuring of the Central Ministry
ot Health & Family Welfare and the Directorate General of Health
Services, the State/UT health ministries and directorates should also be
reorganised and restructured.
11.1.10
District level:
Every district should have a strong epidemiological services
input through establishment of an epidemiological unit headed bv an
officer of the level of district epidemiologist and supporting staff.
Establishment of this type of unit will also help initiating disease
.surveillance programme including early warning signal mechanism
with appropriate laboratory support.
The committee, therefore,
recommends to establish such units if not already existing under the
National Disease Surveillance Programme.
11.1.11
Establishment of a supervisory mechanism at the Sub-district
level:
In many states district levels officers like district malaria officer,
district family welfare officer and district health officer have been
given
responsibility to supervise all health & family welfare
o
programme in part of the districts in addition to supervising the entire
individual programme for the entire district. This has not given much
dividend, because The officer does not give adequate attention to .
activities other than the specific health & family welfare programme
through which his salary is drawn. In addition disease control
strategies/interventions are becoming complex due to variety of
reasons viz. addition of more and more sophisticated technologies,
problems related to resistance to drugs, resistance to insecticide,
ecological changes, management issues covering logistics, cost
effectiveness etc.
Therefore, supervision of the various health
programmes has been suffering and there is an urgent need to institute
appropriate supervisory mechanism at the sub district level.
219
CHSMdoc .
Community IIcalth Centres:
11.1.12
Community Health Centre is regarded as the first referral unit.
The National Education Policy in Health Sciences as approved by the
Central Council of Health & Family Welfare in 1993 has recommended
placement of one public health specialist at the community health
centre (CHC) level and if this is implemented the same will contribute
immensely in strengthening the public health system and will offer
suitable correction to present hospital based disease cure emphasis in
health care delivery to make it disease prevention and health
promotion oriented as enshrined in the National Health Policy
statement. The availability of additional manpower in form of one
public health specialist in all the CHCs may not appear immediately
feasible at this stage of available public health specialist manpower.
However, once a beginning is made and National Education Policy in
Health Sciences is implemented in a time bound manner through an
appropriate action programme, this will be possible in foreseeable
future and thus disease control activities channelled through CHC will
have more updated professionally competent support for better
management of disease control programme and transfer of newer
technologies for various disease control activities at the grass root
. level.
At the CHC there are four specialists and one PHC Medical
Officer. Until such time as a Public health expert is available at CHC
level, it is suggested that each of the specialists take up the
responsibility of monitoring the public health programme pertaining to
their speciality in the population covered by CHC e.g. obstetrician will
supervise collection and reporting of data pertaining to Reproductive
Health and Family Planning, Paediatrician for immunization and child
survival, physician for communicable and non-communicable disease
control programme, surgeon for disability limitation rehabilitation and
blindness control programmes. The entire data pertaining to all
programmes in the CHC population may be put together and reported
bv the PHC M.O who must be adequately trained in epidemiology and
public health management. Thus with the existing statf impioxement
in MIS, disease surveillance and response and accurate reporting of
data pertaining to PHC can be
1 attempted in the CHC. This would also
bring about increased awareness of the clinicians to the'ongoing public
' in
health programmes and result
i better integration of clinical curative
and preventive medicine com;ponents of the important programmes.
11.1.13
ITIC/Sub-Centre level:
The organisational structure of the health services at village
level should be entrusted to the Panchayati Raj institutions which
should decide the nature structure, and priorities of the organisation of
220
the health care delivery services at the village level depending upon
the local situation, resource availability etc. This would ensure
participatary management by the community with empowerment for
decentralised area specific microplanning. Within such a framework,
further co-ordination must develop at all levels of local self
governance.
11.1.14
\rilla£;e level
With the 73rd and 74th Constitutional Amendments providing
enormous political, administrative and managerial powers to take care
of the health and development of the people, it is very important that
the Village Health Guide scheme continues to be supported with
appropriate strengthening through enhancement of honorarium and
drugs so that they become more effective in handling the local health
problems. The committee is of the considered opinion that the Village
Health Guide in the new envisaged role as Panchayat Swastha Rakshak
will provide useful support to the Panchavat system at the village level
in enhancing community awareness and participation.
11.1.15
Prevention of Epidemics:
11.1.15.1
It may not be possible to completely prevent outbreak of
diseases. However, epidemics can be prevented if an appropriate
surveillance mechanism is established. In fact price of freedom from
disease is appropriate surveillance. The Committee agrees with the
recommendations of the Fourth Conference of the Central Council of
Health & Family Welfare (1995) proposing initiation of a National
Disease Surveillance Programme for strengthening of health
surveillance and support services and recommends that this
programme should be initiated as a centrally sponsored scheme within
the existing health infrastructure with appropriate laboratory support
involving already existing expertise in various national institutes,
medical colleges, and district public health laboratories. Additional
support needs to be provided to modernise laboratory support system
through strengthening of conventional techniques and procedures,
induction of rapid diagnostic tests, molecular epidemiology capability
so that the public health system is updated and modernised to respond
to any eventual public health emergency. Initiation ‘of a national
disease surveillance programme will improve notification system,
institution of early warning signal mechanism and would enhance
prompt response capability.
11.1.15.2
With the establishment of National Disease Surveillance
Programme, several national institutes at the national, regional and
state level alongwith several medical colleges and important public
health laboratories will be appropriately linked so that the response
221
PIISM.doc
capability becomes faster and expertise available in these institutes
promptly could be harnessed by the executive health authorities at the
district level to respond to an epidemic situation. These institutions
should be appropriately linked and strengthened to maintain an
updated expertise for meeting any future challenges.
11.1.15.3
India has established a large number of health institutions at the
national, regional and state level. Many of these institutions are
suffering due to non-availability of resources and, therefore, even if the
human expertise is available the same is unable to provide requisite
response capability because of non-availability of support services and
resources. Alternatively, in several institutions even if the modern
equipments are available they are not being appropriately utilised
because of the non-availability of human expertise because of poor
allocation of resources, poor quality of continuing medical education,
etc. I he Committee, therefore, is of the opinion that during the 9th
Plan a centrally sponsored scheme may be initiated to upgrade these
institutions and laboratories through appropriate allocation of funds so
that these institutions can modernise themselves through capacity
building. This could be appropriately linked with recommendation
under 11.1.7.
11.1.15.4
National Institute of Communicable Diseases prepares
guidelines and procedures for outbreak investigations and epidemic
disease surveillance but the same is either not available through out the
country or not put to practical use under a regularly monitored
programme. At present, such guidelines and procedures are usually
provided on request to various health agencies. To be optimally useful,
these guidelines need to be regularly updated. The entire mechanism
as it exists today is on ad hoc basis. The committee, therefore,
recommends that National Institute of Communicable Diseases.should
prepare these guidelines regularly under the supervison of a National
Task Force, update the guidelines at predetermined interval and send
to all health implementing agencies. The guidelines should include
details of the mechanism of detection of outbreak and detection of
early warning signal.
11.1.15.5
The system of civil registration of deaths, Model Registration
Scheme, Sample Registration Scheme subsequently renamed as Survey
of Causes of Death (Rural), certification of causes of death should be
continuously improved by enlarging its scope and coverage so that it
gives more relevant data in the context of the entire country.
11.1.15.6
The processing of weekly epidemiological statistics being
provided by CBHI lacks an appropriate feed back channel to the
various peripheral agencies. The same need to be developed in the
pattern of MMWR (Morbidity Mortality Weekly Report) published by
PHS/maLdoc
CDC and National Institute of Communicable Diseases may take up
the responsibility for the same and initiate action in this regard to
prepare an MMWR type of Bulletin for rapid feed back to all
participating agencies, experts etc. CBHI may continue to act as a
nodal agency for diseases which arc being reported on a monthly basis.
The diseases under International Health Regulations and the diseases
under National Health Regulations having epidemic potentiality
should be Inc responsibility of N1CD which has the due expertise in
appreciating the problem and initiating action accordingly.
11.1.15.7
National Institute of Communicable Diseases, Delhi and
Christian Medical College, Vellore have worked on ' Models of
obtaining information involving peripheral health workers and
physicians in the private sector respectively and if both the models
with necessary mollifications if any, can be appropriately dovetailed
within the existing HMIS, the same will provide early warning signals
for detecting an impending epidemic.
The HMIS was also reviewed recently in the 4th Conference of
the Central Council of Health & Family Welfare held in New Delhi
from 11-13 October, 1995 and the Council recommended undertaking
wan urgent expansion of HMIS to other states. It is desirable to develop
health information system at the district level in order to improve all
activities related to Community Health including those in the
Environmental, Community Water Supply and Sanitation sectors
which will directly lead to an improvement in the health and
environmental status of the district's population. Population based
information in respect of socio economic, environmental, cultural,
demographic and epidemiological issues is vital for choosing priority ..
areas of action and planning public health interventions and evaluating
progress.
With the expansion of HMIS to other states and its
establishment on a firm basis the epidemic -intelligence component
could be appropriately dovetailed within the HMIS and a few districts
in some states be taken up where HMIS has been satisfactorily
established incorporating the epidemic intelligence component in the
light of the experiences of NICD epidemic prone disease surveillance
project and NADHI Projects of CMC, Vellore on a pilot basis. If found
successful, it will further strengthen the HMIS in its response
capability. This could form part of operational research support to the
proposed National Disease Surveillance Programme.
Epidemic Diseases Act 1897 covers the entire country. This Act
11.1.15.8
is about 100 years old.
However, not many times regulatory
mechanisms are clamped under this Act because of improper
professional perception of the nature and spread of the epidemic. If
223
PliyM.Joc
appropriate provisions under the Act are clamped in time major
epidemics could be averted. Therefore, the committee recommends
that the Epidemic Diseases Act provisions should be made available to
all the health authorities and the provisions under the Act could be
continuously reviewed by a designated group to make it more
comprehensive in the light of the latest scientific information available.
11.1.16
Ul^radalicm of Infectious Diseases Hospitals
Every State has got one or more ID Hospitals. Most of these
hospitals are inadequately staffed with poor maintenance. Many of
them lack the basic diagnostic support services. There is an urgent
need that facilities in these hospitals are appropriately reviewed and
modernised to meet the requirements of infectious diseases
management. These hospitals should also have some provisions
particularly in the major metropolitan cities for management of cases
suffering from dangerous human pathogens.
11.1.17
Water quality monitoring
Inspile of significant progress in the coverage of Urban and
J\ural Population with public water supply, reduction in the morbidity
ol water borne diseases, has not been commensurate with the
investment made in the water supply sector. One of the key factors
behind this failure is the total lack of water quality monitoring and
surveillance in most of the rural areas and majority of cities and towns.
A recent study by the UNICEF and the All India Institute of Hygiene &
Public Health, Calcutta, has demonstrated the feasibility of a
community based and affordable model of water quality monitoring
and surveillance. Ministry of Health & Family Welfare should take up
the matter with the Ministry of Rural Affairs and Employment and
Urban Affairs and Employment to initiate a few pilot studies in
different locations in the country to examine the feasibility of the same
and develop National Action Plan, in this regard.
For lull benefits of supply of safe and adequate water, domestic
and personal hygiene should be of high order.
Therefore, the
committee recommends to launch massive IEC programme on
personal, domestic and food hygiene practices including excreta
disposal.
11.1.18'
Urban Solid Waste
I he committee endorses the recommendations of the 1995 Bajaj
Committee Report of the High Power Committee on Urban Solid
Waste Management in India, constituted bv the Planning Commission
with regard to collection, transportation and safe disposal of municipal
224
PHSfinal doc
wastes including industrial and hospital wastes etc. The committee
also endorses the suggestion of the Bajaj Committee, that it is essential
to evolve a National Policy as well as an action plan for management of
solid waste.
11.1.19
Inter-sectoral Co-operation:
Large number of health schemes are implemented through the
Ministry of Health & Family Welfare. In addition, there are large
number of schemes having tremendous impact on human health and
quality of life. These schemes are being implemented through several
other ministries. Some of the important ones which have a direct
bearing on the Public Health System are Rajiv Gandhi National
Drinking Water Mission (RGNDWM), Rural Sanitation, Accelerated
Urban Water Supply Programme, Urban Sanitation, . Urban Basic
Services for the Poor, Urban Solid Waste Management, Sewerage and
Sewage Treatment, Prevention of Water and Air Pollution, Nutritional
Programmes like Integrated Quid Development Services, Special
Nutritional Programme, Balwadi Nutritional Programme, Midday
Meal Programme etc. All these schemes have been conceptualised to
improve the Public Health System. But as different agencies are
^involved and co-ordination between these agencies is not so easily
achieved, tire Committee is of the opinion that until and unless a
formal mechanism of co-ordination arid co-operation is established
involving all concerned and guidelines indicating detailed
responsibilities in respect of all participating units precisely defined,
even inspite of individual schemes appearing to be technically sound,
the same will not be able to deliver what is expected in terms of
effective improvement in the Public Health System. The Committee
fully believe that such mechanism is very vital in tlie implementation
of the health schemes and will strengthen Public Health response
capability significantly. The committee, therefore, recommends
establishment of such mechanism on a formal basis with Ministry of
Health & Family Welfare acting as nodal agency.
11.1.20
Nutrition
Interactive interdependence of nutrition, infection and health
have been well recognised. The National Nutrition Policy formulated
in 1993 has defined the Nutrition goals and the key areas of action.
National Action Plan for Nutrition provides the sectoral and
intersectoral interventions to achieve these goals.
Appropriate
indicators and institutional mechanism . for monitoring the
implementation and impact of the ongoing intervention programmes
at local, district, state and national level need be developed, and
internalised so that the efficacy and efficiency of tire various strategies
225
PHS/inal.doc
can be assessed on a continuing basis and appropriate midcourse
correction can be taken.
India is in a state of demographic, economic and social transformation.
In this context it is essential that a mechanism of nutritional
surveillance at local, district, state and national levels is built up so that
early recognition and rapid remedial interventions of existing and
emerging nutritional problems becomes possible.
11.1.2'1
Decentralised and uniform funding pattern:
Salaries for the ANMs in the periphery come from the family
welfare budget and, therefore, they are subservient to the command of
the Family Welfare Department and do not respond adequately for
related work in the Department of Health for which instructions come
from Department of Health. Similar is the situation in respect of male
health workers who receive their salaries from the health budget and,
therefore, they do not adequately respond to the instructions issued
from Family Welfare Department until and unless specific incentives
are provided and in that case he works for Family Welfare only for
incentives at the cost of health related work. Therefore, this
^fragmentation of tasks and commands grossly affects tire functioning
of the health workers which in turn affects tire efficient functioning of
the public health system. Therefore there is an urgent need that both
the departments are under unified command and the budgetary
provisions are made through unified budgeting system. This will also
enable adjustment of funds at the peripheral points depending upon
the situation which will improve better utilisation of funds etc. There
is also a quantitative distortion in the number of filled posts. As the
salary for ANM comes from FW programme which is a 100% centrally
sponsored one, the posts of ANMS have been created according to the
norms. In contrast the salary for MMPW is from the State budget and
often more than 50% of the posts are vacant and not filled up. This
anomaly needs to be corrected immediately to ensure appropriate
involvement of peripheral level functionaries in disease control
programme as well as in FP programmes.
11.1.22
Non-Govcrnmental Organisations (NGOs):
Non-governmental organisations (NGOs) contribute immensely
in the development of public health system and the practices.
However, the service coverage is limited due to financial and other
constraints. If the NGOs and the private practitioners are effectively
involved tills will strengthen the public health system and significantly
enhance the response capability of the health care delivery system.
Therefore, the committee recommends that the NGOs should be
226
PHSfinal.doc
increasingly involved through an appropriately developed action plan
with suitable funding.
11.1.23
Involvement of ISM
Homoeopathy:
India has over 5 lakh practitioners in indigenous systems of
medicine and homeopathy. Despite the fact that India has a large
number of practitioners in ISM&H, of whom a significant proportion
are institutionally qualified and certified, this potential manpower
resource is yet to be effectively drawn and optimally utilised for
delivery of health care in the country. The committee, therefore,
recommends their involvement in the health care delivery system to
strengthen the public health services and endorses fully the Bajaj
Committee Report on Health Manpower, Planning, Production and
Management in 1987 in this regard. The practitioners of Indian System
of Medicine can be gainfully employed in the area of National Health
Programmes like the National Malaria Eradication Programme,
National Leprosy Eradication Programme, Blindness Control
Programme, Family Welfare and universal immunisation and
nutrition. Within the health care system, these practitioners can
strengthen the components of (i) health education, (ii) drug
.distribution for national control programmes, (iii) motivation for
family welfare, and (vi) motivation for immunisation, control of
environment etc:
J
11.2
J
Lone-term
11.2.1 Broad set up of Ministry:
The vecommendations of the Bhore Committee that the Ministry
of Health should be under the charge of a separate Minister is being
followed and is currently in practice. However, the members of the
committee are of the opinion that the several activities linked with the
human health are presently undertaken by Ministry of Welfare,
Ministry of Human Resource Development, Ministry of Urban
Development, Ministry of Environment, Ministry of Rural
Development etc. The work of sanitation and environmental health
was earlier with the Ministry of Health but now it is being undertaken
by several ministries viz. Ministry of Environment and Forests,
Ministry of Rural Areas and Employment, Ministry of Urban Affairs
' and Employment and Ministry of Chemicals. It has been further seen
that the inter-sectoral co-ordination which is very vital in successful
implementation of various programmes is not readily available
through a formalised mechanism resulting in poor achievements under
various programmes. Therefore, involving all the activities pertaining
to human health, creation of a new ministry such as Human Welfare
mav reauire serious consideration. Alternatively a National Council of
.
*
n27
PMSfbiai doc
I luman Welfare be constituted under the chairmanship of Prime
Minister oi India, and other members being Deputy Chairman,
Planning Commission, Ministers of concerned Ministries, eminent
medical and health professionals and representatives of professional
organisations and NGOs etc.
11.3
Funding
Appropriate budgetary provisions may have to be made in a
phased manner in order to implement the recommendations of the
committee during the 9th Plan and beyond.
228
rH^maldoc
ACTION PLAN FOR STRENGTHENING OF PUBLIC HEALTH SYSTEM
Taking into account the existing resources and manpower
constiaints, certain areas have been identified to strengthen the public
health system in the country. The same have been given in the Short
term recommendations of the committee. The committee also proposes
some action plans to implement the recommendations.
1.
A I ask Force should be constituted to review the National Health
Policy and draft the revised National Health Policy for the
consideration of the government. This could be initiated during the
last year of the 8th Five Year Plan.
(MOH&FW)
2.
Establishment of capacity and capability at the Directorate General of
Health Services to undertake health impact assessment of major
developmental projects to guide the respective ministries accordingly.
Ibis could be taken up during the IXth Plan.
(MOH&FW)
3.
Surveillance activities with regard to human health in and around
.critically polluted areas should be initiated. This could be a part of
overall health surveillance and support services and could be initiated
during the IXth Plan.
(MOH&FW/DGHS)
4.
India is a vast country. Uniform health care strategy’ will not be yield
satisfactory results for all areas. Search for the alternative strategies
needs to be continued on a long term basis to develop situation specific
strategies for such identified areas. States/UTs should strengthen
health system research through appropriate deployment of resources
specially earmarked for the same during the IXth Plan.
(State/UTs)
5.
All the states, municipalities and local health authorities should be
addressed to modify their existing public health laws in the pattern of
the Model Public Health Act revised in 1987 and circulated including
any modification the local situation may demand. The same should be
followed up meticulously so that during the next few years all over the
country uniform public health practice codes are available.
(NICO/DGHS)
6.
National Health Regulations need to be formulated and distributed to
all states, municipalities and panchayats. A Task Force may be
immediately established to draft the National Health Regulations in
the pattern of International Health.Regulations.
(NICD/MOH&FW)
229
PHSfmal. doc
7.
Io involve the Indian Systems ol Medicine more appropriately within
the health care delivery system the e,xisting Central Council of Health
& Family Wellare should be further broad and a Central Council of
Health, Family Welfare and Indian Systems of Medicine and
Homoeopathy may be formed.
(MOH&FW)
8.
An Apex Technical Advisory Body should be constituted to advise the
Ministry of Health & Family Welfare and the Directorate General of
Health Services in all major technical issues periodically and also to
review the major health programmes.
(MOH&FW/DGHS)
9.
Indian Medical and Health Services should be immediately
constituted. I his has been a long pending demand of the medical
professionals and it has been recommended time and again and there
is an urgent need that this is considered immediately by the
government for its implementation.
(iMOH&FW)
10.
. Immediate action needs to be taken to set the process of administrative
reorganisation of the Department of Health & Family Welfare and
Directorate General of Health Services in the light of the
recommendations made.
(MOH&FW/DGHS)
11(a)
A Health Manpower Division should be established in the DGHS; a
National Institute of Health Manpower Development may be
established to provide appropriate institutional support mechanism to
this important activity. This could be initiated during the IXth Plan.
(MOH&FW/DGHS)
11(b) The Baja]' Committee Report on Health Manpower Planning,
Production and Management should be implemented without any
further delay.
(MOH&FW)
11(c)
Positions requiring public health task should be filled by appropriately
trained/qualified public health professionals.
In tliis connection
Central Health Service needs to be appropriately restructured.
(MOH&FW)
12.
Four Regional Schools of Public Health should be set up in the pattern
of All India Institute of Hygiene and Public Health, Calcutta and
School of Tropical Medicine, Calcutta to train more public health
230
PHSJImIdoc
I
professionals to meet the growing demands of the health care delivery
services. This could be taken up during the IXth Plan.
(MOH&FVV)
13.
The existing departments of Preventive & Social Medicine in identified
medical col leges should be strengthened and upgraded to take up the
additional responsibility of continuing education for health and also to
produce more public health professionals. This could also be taken up
during the IXth Plan.
(MOH&FVV/DGH5)
14.
The committee suggest that the state/district national health
programme management focal points are posted for some time in the
Department of PSM in Medical Colleges so that the programme
managers get the benefit of updated academic & technical skills and
the students are benefitted from the practical experience of the
programme managers at the field level. Similarly the teachers of
preventive & social medicine be posted for some time as national
health programme management focal point at district/state level.
(MOH&FW/DGHS)
15.
e A Centre for Disease Control be immediately established in the pattern
of CDC, Atlanta and National Institute of Communicable Diseases
should be substantially strengthened in this direction.
(NICD/MOH&FVV)
16.
The urban areas have very good tertiary facilities but primary health
care infrastructure is very poor. The same needs to be established
particular! v to reach the under privileged, slums etc. The existing
health outposts/dispensaries should be linked to secondary care
centres and these in turn linked to tertiary care centres situated in the
defined geographic area.
(MOH&FW/DGHS)
17.
Reorganisation of the Directorate of Health Services should be
undertaken in the light of the recommendations made. Process could
be initiated immediately.
(MOH&FVV)
18.
A strong epidemiological unit needs to be established at the district
level. The States which have not done so far should establish so under
the National Disease Surveillance Programme. This also could be
taken up during the IXth Plan.
(MOH&FVV/DGHS/NICD)
231
PHSjlnal.ifoc
19.
Evcrv States/UTs should establish a supervisory mechanism at the sub
district level. This could be taken up during the IXth Plan.
(MOH&FW/State/UTs)
20.
One public health specialist should be posted at Community Health
Centre to make the health care delivery team more effective in
delivering the national health projp-ammes and other related services.
(Stale/UTs)
21.
Through the 73rd and 74th Constitutional Amendments, panchayats
have given more administrative and managerial authorities. Io fulfil
their obligations towards public health services, the health care
delivery system should be channellised tlirough them. This will
necessitate establishment of health care delivery component at the
panchayat level. This may require provision of some funds as one time
grant to the panchayats.
(Planning Commission/ MOH&TW)
Village Health Guide Scheme should be strengthened and revamped to
make it more functional to meet the demands of the health care
delivery services. This will necessitate enhancing their honorarium
and also the budgetary allocation for procurement of common drugs.
(MOH&FW/Planning Commission)
23(a). National Disease Surveillance Programme be initiated immediately
with establishment of District Epidemiology^ Cell, establishment of
linkage mechanism involving the medical colleges, referral institutions,
district public health laboratories etc. Microbiology investigative
facilities be also established at the district level.
(NICD/MOH&FW)
23(b). The coverage and scope of the Model Registration Scheme and sample
Registration Scheme should be enlarged to generate more scientifically
valid data in the context of the entire country.
(RGI)
24.
State ID Hospitals need to be upgraded and modernised to meet the
reuirements of the infectious disease management. 'This could be taken
up during the IXth Plan.
25.
/Trre'>
(Planning Commission/States/U Is)
In consultation with the ministries of Urban Affairs and Employment
and Rural Affairs and Employment, the Ministry of Health shou
water quality monitoring on the pilot basis —ely
26.
Ministry of Urban Al fairs and Employment should implement the
recommendations of the Bajaj Committee on Urban Solid Waste
Management.
(MOUA&E)
27.
Health being a multi ministerial responsibility a formal mechanism of
inter-sectoral co-operation and co-ordination needs to be established
involving all the concerned ministries.
(MOH&FW)
28.
Nutrition surveillance shall be in-built part of National Health
Surveillance and Support Services.
(MOH&FW/DGHS)
29.
The female multi-purpose workers are funded through the National
Family Welfare Programme and due to paucity of resources, the state
health authorities have not been able to fill up the positions of male
multi purpose health workers. This should receive high priority
through higher allocation of funds.
(MOH&FW/State/UTs)
30.
.Involvement of NGOs is very important. They have been providing
very useful services to the people at large. More of their involvement
within the health care delivery system will improve the functioning of
the various programmes. Therefore, every effort should be taken to
involve the NGOs and to meet that higher allocation of funds are
necessarv.
(State/UTs)
31.
The country has large number of practitioners of Indian System of
Medicine and Homoeopathy. They should be appropriately involved
within the health care delivery system to make it more effective.
(State/UTs)
233
PHSfinal.doc
<Sorv> h
1-4
PUBLIC HEALTH IN INDIA: CRISIS AND CHALLENGES
(with particular focus on States of Karnataka and Madhya Pradesh)
WORKSHOP in BANGALORE ON 9TH MARCH 1998
VENUE: COMMUNITY HEALTH DEPT., ST.JOHN’S MEDICAL COLLEGE,
BANGALORE - 560 034.
FACILITATION: SOCIETY FOR COMMUNITY HEALTH AWARENESS,
RESEARCH AND ACTION, BANGALORE (CHC)
IN COLLABORATION WITH:. COMMUNITY HEALTH DEPT., ST. JOHN’S
MEDICAL COLLEGE, BANGALORE.
TIME: 9 AM TO 5 PM
For: Danida Health Sector Identification Mission to India
(16th February - 20th March 1998)
*****************
BACKGROUND
® In June 1996, an Expert Committee on Public Health System constituted by the
Ministry of Health and Family Welfare, Government of India, reviewed the ‘situation’
of the public health system’ in the country and recommended an Action plan for
strengthening of the public health system. In a comprehensive report, the Committee
reviewed, the current status of public health in India; the epidemiological surveillance
system including institutional support sendees; status of control strategies for epidemic
diseases; the existing health schemes and National programmes; environmental health
and sanitation; epidemic remedial measures and role of State and local health
authorities; current status of health management information system and its role and
derived short term and long term recommendations. Unfortunately, this report was
not circulated and discussed as widely as it should have been.
On 19th August, 1997, a year later ‘public health’ policy makers, trainers, researchers
from Governmental and non-governmental background met in National Institute of
Nutrition, Hyderabad for a Ross Centenary celebration workshop on the theme Public
Health in India: Crisis and Challenges . This meeting which was a networking
event of the Indian Alumni of the London School of Hygiene and Tropical Medicine,
explored the crisis of public health in all its dimensions and considered some challenges
for policy and action. It was a multidisciplinary dialogue and brought together
resource persons working on malaria, tuberculosis, Kalazar, AIDS, filariasis, women
and children health, reproductive health, IDD, nutrition disorders, cardiovascular
disease, occupational health, health management, health economics, health planning
and financing, vector control and international health. The proceedings of this
chc/msword/c: /o fice/tra i ni ng/da nida.doc
1
dialogue are to be released shortly at some launch workshops in different parts of the
country in the next few months.
® The Danida Health Sector Identification mission which will be visiting India in the next
few weeks will be exploring different options for possible future health sector
programme support to India, especially pertaining to the States of Madhya Pradesh
and Karnataka. The Society for Community health Awareness, Research and Action,
Bangalore, which primarily facilitated the Hyderabad workshop, has been requested to
host a one day interactive dialogue and workshop on 9th March 199(8 bringing
together public health professionals’ and health policy makers who have multisectoral
and multiregional experience to discuss the same theme particularly in the context of
the states of Karnataka and Madhya Pradesh.
OBJECTIVES
The objectives of the workshop/interactive dialogue are:
1) To provide an opportunity for the Danida Mission to meet with knowledgeable Indian
health professionals and discuss the state of public health in India, particularly in the
context of the Expert Committee recommendations.
2) To discuss more specifically the state of health information systems, public health
education and management training; public health research and the scope of
decentralisation, including Panchayat Raj in health care.
3) To identify and informally discuss how Danida could be of assistance in a National or
State health sector context.
PREPARA TION ANO METHODS
1) Invitees to the meeting will be a cross section of resource persons who have concern
and commitment to improve the ‘public health system ’ in India. Within the short time
available, an attempt will be to bring together a multidisciplinary group with
experience, particularly in Karrnataka and Madhya Pradesh.
2) All invitees are requested to complete a short opinion poll on the key elements of the
crisis and the challenges. This will be summarised in the introductory session to
enhance the participatory nature of the dialogue.
3) All invitees will be sent summaries of the Expert Committee report (1996) and the
Hyderabad workshop proceedings (1997) as background.
chc/msword/c:/ofice/training/danida.doc
z.
4) At the workshop, after the introduction , an initial presentation 'the Crisis and
Challenges of Public Health in India', will bring together the expert
recommendations, opinion polls and literature review including proceedings of
earlier workshops. In addition another reflection will emphasise the core values
that should be central to policy^strategy and action.
5) The dialogue will then proceed in brainstorming sessions devoted to specific issues
as indicated. For each issue, one resource person will make a 10-15 minute
presentation to introduce the issue and its context and challenges. After these,
participants will brainstorm and contribute to the identification of possible
initiatives.
6) A final session will prioritize ail the specific ideas which have emerged in the
workshop with particular reference to the States of Karnataka and Madhya Pradesh
and in the context of the Danida Mission.
7) To ensure the interactive nature of the workshop, Danida Mission team members
will be invited to share their own observations and responses throughout the
consultations, in the context of the discussions they have had at various levels
during the travels in India.
****************
{A tentative programme is enclosed}
For the small number of outstation participants, suitable air/rail travel and local hotel
accommodation will be provided.
****************
All confirmations, clarifications and follow-up may please be addressed to:
Dr. Ravi Narayan,
Society for Community Health Awareness, Research and Action,
Attention: Public Health Workshop,
367, Srinivasa Nilaya, Jakkasandra I Main,
I Block Koramangala,
Bangalore - 560 034.
Fax: (080) 55 333 58 (Mark Attn: CHC)
Tel: (080) 55 315 18 (Off).
Email: tnarayan@giasbg01.vsnl.net.in
chc/nisword/c:/ofice/lraining/danida.doc
H
Workshop theme: Public Health in India: Crisis and Challenges
(with special reference to Karnataka and Madhya Pradesh)
9th March, 1998
Venue: Department of Community Health,
St John’s Medical College, Bangalore.
Programme Schedule
Time
9 am - 9.30 a m.
9.30 a.m. - 10.30
a.m.
Welcome, Introductions, and Objectives of Workshop.
SESSION : 1
1. Crisis and Challenges of Public Health in India
2. Core values in Public Health - A policy reflection
(Clarifications / Comments)
10.30 a.m. - 10.45
a.m.
10.45 am - 12.45
p.m.
12.45 p.m - 1.30
pm
1.30 p.m - 3.30
p.m
SESSION II
Identifying Opportunities for Strengthening
♦ Public Health Education and Training .
♦ Public Health Research and Health Information System
Lunch
SESSION III
Identifying Opportunities for strengthening
♦ Decentralization in the Health Sector (including Panchayat raj
institutions and Hospital autonomy)
♦ Community Participation and communication (including IEC)
3.30 p.m. - 3.45
p.m.
3.45 p.m, - 5 p.m
How could Danida assist at Central and State levels (with special
reference to Karnataka & Madhya Pradesh)_________________
chc/msword/ci/ofice/training/danida.doc
. |G
H
I
An opinion poll
labile Health in India: Crisis ajnd. Challenges
(with particular focus on status of Karnataka and Madhya Pradesh)
A. The 'crisis’ in Public health in India’ is evident from:
1.
2.
3.
B. The causes of this crisis, today, are:
1.
2.
3.
C. To meet the challenges, the following initiatives should be taken:
Central level
1.
3.
State level (keep Karnataka & Madhya Pradesh in focus)
1.
2e
3.
Date:
Note:
1. If space is not enough, please use reverse of the sheet.
2 The idea of restricting it to 3 responses on each section is to get a sense of priority, so
please mention the top three ideas you would suggest in order of priority.
3. Please return this to Community Health Cell by 2nd March, 1998, Monday, by post or by
fax.
Fax No: (080) 55 333 58 (Kindly mark Attn: CHC)
Postal Address: Community Health Cell, #367, Srinivasa Nilaya, Jakkasandra I
Main, I Block Koramangala, Bangalore - 560 034.
chc/msword/c:/ofice/training/danida.doc
I
•DECCAN HERALD, SATURDAY, DECEMBER 6, 1997
Call for laws
to curb danger to
public health
v
fA
I
B*
•a ALC
1 ?
aj
NEW DELHI, Dec 5 (PTI)
President K R Narayanan, said
here today that laws and
legislations will have to address
the problem of regulating the gen
eral conditions which give rise to
dangers to public health as well as
the particular reasons that pro
duce specific illnesses.
Inaugurating a three-day interlational conference on global
health law, organised by the In
dian Law Institute (ILI) and co
sponsored by the World Health Or
ganisation (WHO). Mr Narayanan
said in today’s world, not only
peace and prosperity were indivis
ible, but the health of the people
■4^
is also indivisible.
i
Observing that the law of public
health is based fundamentally on
the laws of nature and on the prin
ciples of good living, Mr
* Narayanan said “public health
law will have to leap the frontiers President K R Narayanan, Prime Minister I K Gujral and Chief Justice of India, Justice J S Verma
of countries and encompass the applaud at the International Conference on Global Health Law organised by the Indian Law Institute
whole globe and humanity.”
x
in New Delhi on Friday.
PTI photo
.t
AL'
m iMiw
■JIB
■J
■
7.
■<-
-
■■■
' H
■
T TQ rnmmPTrp QprrptrJf'z
■
1_______ a
j-i
IM
j ___ -
PUBLIC
i
HEALTH
(_O
National pipedreams
Governments make annual policy pronouncements on everything from industry to
sport. But strangely, public health policy is assumed to be the responsibility of the
World Bank. The government’s last statement on health, the National Health Policy
document of 1983, must be the nation’s most forgotten and forsaken document
by V R Muraleedharan
Z^Xnc can say very little that is positive about the current
I
ktate of the public health care system in India, despite
the fact that an enormous amount of investment has
been made by the central and state governments over the last
50 years. The contribution of the Primary Health Centres
(PHCs) to public health has been dismal. For example, a 1998
World Bank study has shown that there is no correlation
between the availability of sub-centres and PHCs and child
survival among either the poor or the non-poor This lack of
impact of PHCs on child survival was largely attributed to
the fact that services are not oriented to the type of care needed
and/or that these services are not functioning as they should
be. Overall, the World Bank study has this to say: “India is
not getting the returns it should from its spending on public
health. And more importantly, the poor are not benefiting
much from that spending.” Indeed this would not be surprising
to those who have some familiarity with
what goes on at the ground level.
It does not follow, however,
.
that the private health sector’s
contribution to peoples’
health is much greater,
or even that it is better
than that of the
public health care
system. The sad I
part of the story of /
the health care \
system in India is
'
that no one has any
clue, in empirical
terms, about the
health of the country’s
people over the last five
decades. And. the saddest
part of the story is that there
has hardly even been an attempt
to find out. This speaks volumes for
the state of health policy planning in
this country.
Health policy outlook: a dismal reality
The health care sector has the dubious
distinction of not having any overall policy
guidelines to direct its growth ana development..
\V
That job, it has been assumed, is the responsibility I I
of the World Bank. The Bank in the recent past has \l
come out with a few reports on various aspects of >
health care financing and provision and how the system
should be (re)organized in order to be efficient, equitable,
a
1\
etc. 2 Periodically (almost yearly, in fact) governments make
policy pronouncements on a variety of subjects such as tiny,
small, medium- and large-scale industries, agriculture,
insurance, financial institutions, tourism, sports,
transportation, import of gold, telecommunications — the list
can go on to include at least a dozen other items. But for the
health sector, there was just .the infamous, forgotten and
forsaken 1983 National Health Policy document produced
by the Government of India 3. That was the only policy
direction on health care services from the central government
to the state governments, and that was more than 15 years
ago.
In keeping with our tradition of declaring “sound policy
statements”, the NHP 1983 also contained several wellarticulated visions, goals arid possible strategies that various
state governments should adopt to achieve these goals. But
the NHP is one of the most forgotten and ignored documents
in the history of health care policy in independent India.
Amazingly, even the most responsible persons sitting in
►
the government’s administrative hierarchy do not
<
know of the NHP’s existence, much less its
i
contents. I have experienced thrs personally
some senior personnel in the
government. Isn’t that a great tribute to our
1 nX
parliamentarians who had debated and
formulated the 1983 NHP?
U i
Why has this happened? Why has this
~
/ //
document been thus ignored? What does
it contain, of what does it not contain, to
/z ///
warrant such scant attention from
academics, bureaucrats, activists and others
fj/
*n l^e past? One reading could be that it had
///
literally nothing to guide the actions of planners
/f
and executives. Another reading could be that its
y.
recommendations.were good but they were not
implementable for various reasons. Did the NHP
contain anything worth recalling? Let’s find out.
A sample of pipedreams:
The NHP was broadly committed to attaining the goal of
“Health for all by the Year 2000” through the universal
provision of comprehensive primary health care services.
The document
k clearly
recognized
g that such a
f goal can be
attained only
through
“a
l h o r o u g h
faizana
HUMANSCAPE ■ MAY 1999 ■ 6
Tm I<cnr/ v/3/
F'C’r' Lx~)
[opj]£ 0
K-Crr-)
H <+c( '
4
PUBLIC
HEALTH
overhaul of the existing approaches to the education, training state has no control whatsoever on the private health sector
ol medical and health personnel and the reorganization of and no clue as to how it should go about building a healthy
the health services infrastructure”. Furthermore, it said, relationship with the private health sector. It should also be
“considering the large variety of inputs into health, it is noted that over the years both private and public health care
necessary to secure the complete integration of all plans for systems have lost credibility in the eyes of the public. No
health and human development with the overall national doubt, they have lost credibility mutually as well.
socio-economic development process...” Needless to say, the
c) Consider just one more pipedream, which relates to
rhetoric included the right dosage of expressions such as, medical research. The NHP said the ultimate test of medical
“(health care services) should be relevant to the needs and research “would involve the translation of available know
priorities of the community”, “should be at a cost which the how into simple, low-cost, easily applicable, appropriate
people can afford”, “should be delivered through the technologies, devices and interventions suiting local
organized involvement and participation of the community”. conditions, thus placing the latest technological achievements
It contained many more eloquent and impressive expressions. within the reach of health personnel and front-line workers
Thus, with a view to putting
in the remotest corners of the
“an end to the existing all-round
country. Therefore, besides
unsatisfactory situation”, the Has any effort been made in the past
devotion to basic, fundamental
NHP proposed a set of
to involve people in the setting of research, high priority would be
approaches to bring about the
accorded to applied, operational,
“urgently
necessary” priorities? Has any effort ever been
research including research for
restructuring in the health
continuously improving costmade
to
involve
social
scientists
in
services. What were they? We
effective delivery of health
shall cite only a few of them
the formulation of state-level
services. Priorities would require
here 4.
planning
in
health
care
services?
to be identified and laid down in
a) To ensure that the proposed
collaboration
with social
Has any operational research study scientists, planners,
set of approaches do not merely
decision
form an assemblage of “disparate ever even been conceived to improve
makers and the public” (NHP,
health interventions” the NHP
P-51)
the cost-effectiveness of health
emphasized the formation of “a
Il would require tremendous
nation-wide chain of sanitary- programmes? You can stick your neck
dedication and effort on the part
cum-epidcmiological stations.
of the state to instill confidence
out and say, ‘No
The location and functioning of
in the minds of the people who
these stations may be between the
are expected to identify priorities
primary and secondary levels of the hierarchical structure,
structure, and participate in decision-making. But has any effort been
depending upon the local situations and other relevant made in the past to involve people in the setting of priorities?
considerations. Each such station would require suitably Has any effort ever been made to involve social scientists in
trained staff equipped to identify, plan and provide preventive, the formulation of state-level planning in health care services?
promotive and mental health care services. It would be Has any operational research study ever even been conceived
beneficial, depending upon the local situations, to establish to improve the cost-effectiveness of health programmes? You
such stations at Primary Health Centres. The district health can stick your neck out and, say, “NO”.
organisation should have, as an integral part of its set-up, a
The proof of the pudding...
well-organised epidemiological unit to coordinate and
More than 65 per cent of children under five suffer from
superintend the functioning of the field stations....” (NHP, p malnutrition. Not more than 30 per cent of the population
42)
has access to sanitation facilities. The under-five mortality
The question is: Where are all these sanitary-cum- rate per 1000 is still above 85. The infant mortality rate is
epidemiological stations? Why were they not established around 65. The public health care system continues to suffer
anywhere at all? If they were, what was their experience? from an inadequate number of physicians and nurses despite
The fact remains that this approach has not taken any shape a high annual production of these personnel. A substantial
as visualized by the NHP.
part of per capita health expenditure (even for primary care)
b) Take another example: The NHP proposed that to “reduce is borne by individuals. A large proportion of India’s
governmental expenditure and fully utilise resources, planned population continues to seek care from the private sector even
programmes may be devised, related to the local requirements for diseases (malaria and tuberculosis, for example) for which
and potentials to encourage the establishment of practice by national programmes have been in operation for several years.
private medical professionals, increased investment by non The medical education system continues to lean heavily
governmental agencies in establishing curative centres...” towards curative care. The public health care system continues
(NHP, p 43)
to suffer from lack of intersectoral cooperation — often one
This was another pipedream. Nothing to date has happened directorate of the health and family welfare department does
in terms of actively encouraging the establishment of private not know what another directorate of the same department is
heahh institutions/facilities, The state has happily slept over doing! Very few would try to deny such facts. We are far
this proposal of the NHP. Over the last couple of years, some removed from considering health insurance schemes (one of
initiatives have been made by a few state governments in the pipedreams of the NHP 1983) for rural areas. In fact, there
getting to know how the private sector is organized and has been no attempt so far in this direction, let alone the
working. Much less effort is being made to witness its healthy feasibility of sustaining such schemes.
growth and development. It is common knowledge that the
But we have tottered along, despite poorly executed (and
HUMANSQAPE ■ MAY 1999 .J 7
♦ 4
i
PUBLIC
HEALTH
often unexecuted) intentions over the years and (not
surprisingly) have even shown some impressive
improvements. For example, life expectancy has gone up
substantially over the last 40 years. Crude birth and death
rales have gone down significantly. But as said earlier, we
shall never be able to prove adequately how many of these
improvements have occurred due to specific policies, although
scholars have a knack of making models out of nothing! For
example, quite an amount of scholarly work has been
produced on the remarkable fall in the total fertility rate (TFR)
in the state of Tamil Nadu to 2.1. There is no definitive
explanation as yet (and possibly can never be), but attention
to this question has already started waning. In the absence of
any concrete evidence, one can safely attribute it to the
“invisible hand” of god, although there are competing interest
groups — the bureaucrats, for example — who appropriate
all,the credit for themselves!
One concluding thought:
Since independence, we have produced several policy
documents, one of which we commented upon briefly in this
essay. There is plenty of food for thought and action in these
reports, and it would be worthwhile for policy-makers to pore
over these policy documents and reflect carefully as to where
and why we have gone wrong and re-establish our goals and
approaches.
References
1. Governmenl of India. National Health Policy, 1983, New Delhi
2. World Bunk (1995), India: Policy and Finance Strategics loi
Strengthening Primary Health Care Services, Washington DC.
3. (1997), India: New Directions in Health Sector Development at the
State Level: An Operational Perspective, Washington DC.
4. (1998), Reducing Poverty in India: Options for More Effective
Public Services, Washington DC.
NOTES
1 World Bank (1998), chapter-3.
2 The three noteworthy reports are: World Bank (1995), World Bank
(1997) and World Bank (1998)
3 The National Health Policy was endorsed by parliament in December
1983. We shall hence call this tlie 1983 NHP.
4 For want of space, we have not gone into the details of other
approaches. The reader is advised to go through the original document
of the 1983 NHP.
V R Muralcedharan, associate professor of economics
at the Indian Institute of Technology, Chennai, is one of
India’s best-known health and medical historians. He is a
doctorate in economics, and one of the few economists in
India who has made the health sector his field of
research.
Manufacturers of
High Frequency Dielectric Preheaters
And Induction Heaters
/
s
ectroni
vices
B
22, Mistry Industrial Complex, M.I.D.C.,
Cross Road A, Andheri (E), Mumbai 400093
Tel: 8221649 / 8349383 Fax: 8349383
T?
HUMANSCAPE ■ MAY 1999 ■ 8
II
hie
-
POVERTY, DISEASE AND NATIONAL AND INTERNATIONAL
POWER STm’CTURE
THE CASE OF INDIA
Debabar Banerji*
SOME CONCEPTUAL ISSUES
It is necessary to understand at least the key quantitative and qualitative issues involved
in the phenomena of poverty and health in a population, and in their interrelation. Both
these areas of study are very complex and multi-dimensional. There have been numerous
instances of distortion of the concepts concerning these areas because many writers have
fallen to the temptation of adopting what amounts to a rather simple and fragmentary
approach to very complex issues. This has automatically distorted their analysis of the
interrelation between the two. Matters have been worse confounded when they set out to
use such flawed ideas to make international comparisons. It is contended that despite all
the efforts at the improvement of what the United Nations Development Programme
(UNDP) has called Human Development Index (HDI), it still suffers from some major
infirmities for comparing relative levels of 'development' in different countries of the
world.
POVERTY
It is not intended to go into the highly controversial area of measurement of poverty.
Even some carefully chosen statistical indices (which are not necessarily exhaustive
enough in capturing the key variables), that arc used to draw up profiles of poverty
stricken people in a population, give only a part of the picture; sometimes it can even be a
deceptive picture. Poverty, in whatever way it is defined, has a number of deep human
dimensions in the form of the way it affects individuals and groups; it has deep cultural,
social and human ecological implications. Over and above, it has roots in the history,
international politics and trade, geography, economy and power relations which
determine the political setting. These obviously cover too wide an area. It is,
nevertheless, contended that at the very least these dimensions are kept in mind while
making judgements and conclusions about individual countries and populations. Very
often this is not done.
Gunnar Myrdal was among the early scholars to draw attention to the complex nature of
poverty of a community and the social, cultural, economic and political implications that
flow from that condition. He had articulated his thinking in 1944 in the famous book,
American Dilemma, the Negro Problem and Modern Democracy to analyse the causes of
* Professor Emeritus, Jawharlal Nehru University, New Delhi.
Nucleus for Health Policies and Programmes, B-43 Panchsheel Enclave, New Delhi 110 017.
Tel: 648 0851; Telefax: 649 8538; Email: nhpp@bol.net.in
- i
American Dilemma, the Negro Problem and Modem Democracy to analyse the causes of
backwardness of the American Negro, as he was then called. He had contended that the
'Negro’ was caught in a vicious circle of poverty, apathy, ill-health, crime, illiteracy,
family instability and many other such negative attributes, which form a vicious circle.
Here, one attribute gets accentuated by the influence of many others.
Myrdal had based his findings on the plight of the American Negro to propound his
theory of Cumulative Causation in his book, Economic Theory and Underdeveloped
Regions: the negative attributes feed on one another to form a vicious cycle, making the
community more backward. He suggested that this vicious cycle can be reversed by what
he termed as 'purposive intervention’ in carefully chosen 'key variables' in the process of
cumulative causation and thus turn it into a 'virtuous cycle’. He had identified
intervention for improvement of health status as one of the key variables.
Persistence of poverty and ill-health and other social and economic maladies is due to the
failure of those who command authority to translate this concept of purposive
intervention into action. This is essentially a political question.
HEALTH
Focusing on issues concerning community health, the great German medical scholar and
political activist, Rudolf Virchow, had asserted as early as in 1848 that 'health is nothing
but practice of politics on a larger scale’. Thomas McKeown has provided ample
historical and epidemiological evidence to conclude that socio-economic factors have
more to do with the decline in the death rates in Europe, than the public health measures
undertaken during that period. Walshc McDermott has marshalled convincing c\ idcncc
to show that the sharp fall in the infant mortality rates in New York City in the 1920s can
be explained essentially by the socio-economic changes that had taken place at that time.
As will be discussed in detail at a later stage, this does not imply that no action need be
taken to protect, promote and alleviate health problems of people through integrated
public health services. As with many other socio-economic variables, interventions
through health services has a positive role in contributing to converting the vicious cycle
into a virtuous one. As has been pointed out earlier by many scholars, properly designed
health services to alleviate the sufferings of the poor due to health problems have a
positive role in preventing people from going below the 'poverty line’, in increasing their
capacity to fight for their causes, increasing their capacity to earn more and in acting as
entry points or a 'lever’ to stimulate development in other poverty related areas of action.
WHO’S APPROACH TO POVERTY AND HEALTH
The oft quoted WHO’s definition of health as a state of complete physical, social and
mental wellbeing, and not mere absence of disease’ (the word 'spiritual' was added later)
also commits that organization to a wider scope of activities in the field of health. For all
its efforts of the past half a century and the catchy slogan of Health For All by AD 2000,
using the approach of Primary Health Care (HFA-2000/PHC), WHO has a great deal of
- z
catching up to do in assisting its member states to reach even the goal of ensuring 'mere
absence of preventable diseases’. It is worthwhile to recall that WHO had taken some
major inititiatives to grapple with twin and interrelated problem of poverty and health.
The first among them was in 1975-76, when WHO joined the World Bank in launching a
proposal to concurrently deal with the problems of poverty and health. That this initiative
was to aborted within a short time ought to have served as a warning signal to them about
the challenge of undertaking such ventures.
Undaunted, WHO launched its famous programme of HFA 2000/PHC in 1977. This was
followed in 1978 by the Alma-Ata Declaration of 1978, signed by all the countries of the
world. The Declaration marked a watershed in public health practice, both at the national
and international levels - health as a fundamental human right of all the peoples of the
world, people as the prime movers for giving shape to their health services, intersectoral
action in health, social control over the health services, are some of the principal elements
of the Declaration. For reasons that need not be gone into here, HFA-2000/PHC never
took off; a feeble gesture was made by WHO to have a World Conference at Riga,
Latvia, in 1988 to mark the tenth anniversary of the Declaration; it was almost totally
forgotten by the time the twentieth anniversary came in 1998. The recent declaration by
thepresent director-general of WFIO, in the World Health Report of 1999 as well as in her
address to the South-East Asian Regional Committee meeting at Dhaka in September,
1999, about the primacy of linking health with poverty removal, while insisting on the
vertical programmes concerning tobacco, AIDS, tuberculosis and malaria, provides a
good instance of ambivalent approach of WHO towards the problem. Significantly, as
will be discussed below, Amartya Sen's Keynote Address to the 52nd World Health
Assembly, entitled 'Health in Development', which is also published in the WHO
Bulletin, also reflected a similar ambivalent line of thinking.
AMARTYA SEN ONTIEALTH IN DEVELOPMENT’
Sen makes the usual correct remarks about curtailing military expenditure, skilful social
allocation of resources to support to a 'support-led' process to provide basic health and
education and other relevant social arrangements, informed public discussion in the form
of participatory politics, 'development as freedom', liberation from 'misery and
unfreedom', and so on. He also refers to a 'variety of historical reasons' for the
spectacular economic growth in the East and South East Asian countries and devotes an
entire section to 'the economics and politics of health care'. It is ironical that having made
all these lofty pronouncements, he did not think it worthwhile to make a deeper analysis
of the historical, political and socio-cultural forces and the forces generated by
international politics, trade and military pacts, which led to the neglect of the 'social
support systems'in many poor countries.
His approving references to South Korea, for instance, do not take into account the
impact of the Korean War, economic benefits of locating a huge US military base in that
country, propping up of dictators like Syngmen Rhee, huge foreign direct investment for
politically and socially correct behaviour of the Syngman Rhee's government and
5 -
formation of an export-led economy. Similar is the history of Chiang-ki-Seik's
Formosa/Taiwan, or Lee Kwan Yew's Singapore and the Crown colony of Hong Kong.
Unleashing of the Viet Nam War led to yet another bout of economic 'prosperity' of the
countries of this region, including the not so famous rest and recreation industry of
Thailand and the dictatorial regime of Suharto in Indonesia. These features did not seem
to come in the way Sen's praise for economic development of such countries.
How could Sen shower praise for achievements of 'pre-reform' China when he is well
aware of the 'misery and unfreedom' of a totalitarian approach to the economy, politics,
judiciary, access to information and administration, and the disastrous failures of the
movements of 'let hundred flowers bloom', 'the great leap forward', the great Chinese
famine, the cultural revolution and the Tianenman Square incident of 1989?
He greatly emphasises the importance of'informed public debate', but which 'public' has
he in mind in the vast majority of the poor countries of the world where a minuscule elite
has a vicious grip over the levers of power to make public policy decisions? Another
major problem with Sen’s presentation is his idea of measuring 'health'. While at the start
of his address he mentions the idea of capability of'living really long and to have a good
life while alive', he ends up in measuring health in terms of mortality rates and life
expectancy. How do his data capture his idea of good life while alive and liberation from
misery and unfreedom? How do these apply to South Korea, Taiwan, China, Indonesia
and other Asian Tigers? Do even the peoples of the oft quoted Kerala State of India, Sri
Lanka, Jamaica (which incidentally has one of the highest homicidal rates in the world)
and Costa Rica enjoy 'a good life while alive'?
Talking to a global audience, Sen made no mention of the devastating impact on the poor
peoples of the world of the World Bank/IMF inspired programmes of globalisation,
structural adjustment programmes and cost recovery for social services from the people
and encouragement of the private sector in health; the World Trade Organisation has
added to the predicament of the poor by imposing many trade regimes which affect their
lives. For instance, in the Indian Union budget for 1992-93, the well known welfare
economist and the then finance minister, Manmohan Singh, had imposed a drastic cut of
20 percent on the health budget as a whole (without taking into account the inflation of
1991-92); the cut was still more severe on the communicable disease control programmes
which are of particular relevance to the hapless poor. There were also cuts in other social
services; but the defence budget was virtually left untouched. Sen has described
elsewhere Manmohan Singh as a 'dear friend’ and he would like to have him as a future
Prime Minister of India!
QUANTITATIVE
DATA
USED
BY
INTERNATIONAL ORGANIZATIONS
UNDP
AND
OTHER
The foregoing analyses reveal serious infirmities in the use of quantitative indices for
measuring development by UNDP and other international organizations. Besides, there is
the very serious question of reliability of the data that are made available to these
organizations by the national governments. Finally, there is the key question of
- 4- -
comparability of data from one country with others and wide differences in the
endowments of different countries. Sen, for instance, has pouted out the incongruity of
comparing a country like India with, say, Maldives.
Taking just one example among the poor countries of the world, one can ask: how many
countries have even the quantitative data which can be comparable to the almost half a
century series of the National Sample Surveys on a wide range of socio-economic
problems? Very few, if any of them have the time series data on vital events through
Inida’s Sample Registration Systems. Yet information from the NSS and SRS in India is
compared on equal terms of reliability and validity with countries with very poor and, not
infrequently, doctored quantitative data.
One can also point to the other problem of bias, unintended or otherwise, which tend to
package some data in alarmistic terms. For instance, with many highly populated
countries of the located in the South-Eastern region of WHO, intellectual fairness
demands that disturbing situations are depicted as population ratios, rather than in
hyperbolic terms as 'containing the largest number of the poor of the world’. They
conviently overlook that they have no access to corresponding data from China. There is
a strong undercurrent of cheap public relations exercises in presenting various conditions
in many international organisations. This ought to be curbed.
The recent commissioned report, Poverty and Health - Regional Issues: South-East Asia,
brought out by the South-East Regional Office of the WHO, reflects most of the flaws
referred to in the previous paragraph; that is, reliability, validity and comparability of the
information base. On the other side, WHO/SEARO does not make any mention of the
reasons why it had not been able to implement HFA-2000/PHC and other anti-poverty
initiatives taken by WHO, both before and after Alma-Ata. That is a more important issue
than playing with quantitative data of limited value.
There is, however, one set of quantitative data from the Human Development Report
1998 of UNDP which reasonably captures the real situation. Il says that the countries
which account for 20 percent of the population of the world consume as much as 86
percent of the world resources. Of the remaining 80 percent of the population, it can
easily be surmised from numerous sources of information that the upper crust forming
barely the 5-10 percent of them consume seven percent of the resources, thus leaving a
mere seven percent for anywhere between 90-95 percent of the population of the residual
80 percent of the world population. This set of data is being presented to underline the
awe-inspiring nature of distribution of resources between and within different countries
in this world. Is this the vision of the global village, of the rulers of the rich countries?
The horrendous maldistribution indicates the very dangerous trend of how a small
fraction of the population of the rapidly polarising world is so thoroughly brainwashed so
as to wallow in the in the mindless consumption of such utterly frivolous and
aggressively marketed 'products’ as designer merchandise, brand name values, prize
Fights and other big money sports events, fashions and cosmetics and a powerful industry
built on most outlandish noises that go in the name of pop and reggae music, on the one
side, and a huge mass of the population living under most degrading conditions of
- 5 -
poverty, ill-health and destitution, on the other. Inadequate recognition of this alarming
situation explains why the authorities concerned have repeatedly failed to come to grips
with problems of poverty and health. The approach has to be different. The forces
engaged in the frenzied creation of markets have to be tamed. For this purpose, the
affected people themselves will have to get together to wrest (heirrights from their rulers.
A liger can not be expected to become a vegetarian!
POVERTY AND HEALTH IN INDIA HISTORICAL BACKGROUND,
HUMAN ECOLOGICAL CONDITIONS AND DEVELOPMENT
Considering the global and the national economic order, India, with a population of one
billion, has a very large number of those who are poor. This problem of poverty and its
relation to health is being analysed here very briefly in the perspective that has been
developed at the beginning of this presentation.
When the country gained independence in 1947 after two centuries of British colonial
rule, the nature and extent of poverty was much more severe and extensive than what
exists today. The health services too were in a very rudimentary form, leaving an
overwhelming proportion of the poor to their fate. There were frequent outbreaks of
epidemic diseases which were mostly left unchecked. Twenty mothers lost their lives for
every 1000 childbirths. Only half of the children born, after such colossal sacrifice of
lives by the mothers, were alive ten years after their birth. Expectancy of life al birth as
measured in 1941-1951 national census was 32.1 years.
Since then, despite assigning overwhelming priority to family planning in resource
allocation, the size of the population has shot up from 351 million in 1951 to the present
figure of a billion. This addition of an extra 650 million people in a country which was
already overpopulated in 1951 has been a very significant feature of human ecology in
the country. It is indeed a remarkable achievement that the already overpopulated and
poverty stricken country managed to absorb an additional 650 million people over a
period ol half a century, thus belying the grim Malthusian forebodings; the country also
managed not only to retain, but actually deepen the democratic system of government;
infant and other mortality rates have shown significant decline all over the country;
despite increase in population, the proportion of the poor has been reduced from around
half to about a third of the population; there has been a sustained growth in the per capita
income in fixed prices; the latest NSS figures show that the literacy rate have gone up to
74 percent in 1998 from 62 percent in 1991; the life expectancy was 57.7 in the 1971-80
census and it has now risen to 63 years; and so on.
UNEQUAL
SERVICES
STRUGGLE
FOR
DEVELOPMENT
OF
HEALTH
A mention is made here of some positive achievements to underline the fact that the poor
have been able to wrest some of their rights from the minuscule elite who control the
levers of power of the country. Looking at the opposite side, if one goes beyond the
criteria of defining a poor as one who gets two square meal a day all round the year to
- 6 -
one getting some pioteins in his diet, has access to protected water supply, basic
conditions of housing, including toilet facilities and environmental sanitation and access
to basic education and health services, as reflected in the UNDP assessment of
distribution of the global resources, some three-fourths or more of the present population
will be branded as poor.
The task of alleviating poverty-disease syndrome is thus an uphill one. The deprived have
to struggle hard to impel the ruling elite and their abroad to make what Sen has called
judicious social allocations for this purpose. Manmohan Singh did not do so. This has
been a difficult task because of the distribution of political power in the population. It has
been compounded because of severe cuts in the budgetary allocation for health and other
social seiwices, increasing inefficiency in the use of whatever is allocated and gross
inadequacies in finding more cost-effective programmes for social interventions to break
the vicious cycle of poverty and ill-health.
In the health services sector, for instance, there has been severe erosion even of some
modest gains that were made during the first two decades after Independence. Giving
over-riding priority to resource allocation for implementation of the very defectively
designed and extremely expensive and wasteful family planning programme for more
than three decades has grievously damaged almost all the components of the health
service system. As if that was not enough, international agencies then came in with their
own prefabricated tcchnocentric global agenda against some specified diseases and
managed to get the politician/burcaucrat diad to accord these unsuitable programmes
priority over the basic health activities.
HERITAGE OF ENDOGENOUS IIEALT1I SERVICE DEVELOPMENT
The net result was a virtual decimation of the philosophy of health service development,
which was so painstakingly built up during the first two decades. This 'philosophy' was
evolved as a part of an overall philosophy for development in consonance with the socio
cultural and economic conditions. Very briefly, developing people-oriented technology,
providing promotive, preventive (including family planning) and curative services in an
integrated form, training of manpower in consonance with the tasks to be performed and
undertake research to make the system cost-effective (optimisation), and later on,
entrusting "people’s health in people's hands”, were some of the major elements of the
public health philosophy that was endogenously developed in India. It may be noted in
passing that this philosophy has had strong resonance in the postulates of Primary Health
Care contained in the Alma Ata Declaration. One possible reason for this could be that
the moving spirit behind the Declaration, Halfdan Mahler, had his public health baptism
in India at that time.
In fact, moving a step forward, the public health workers in India questioned the then
conventional wisdom of economists in the Planning Commission to consider health
services as a 'consumption item' for national planning. It was argued by public health
workers that alleviation of suffering due to health problems strengthens the people to
fight for their democratic rights and increase their productivity in the bargain; it was also
considered as levers or 'entry points' for workers from other fields of social development
- 7 -
to more effectively bring about developments in their respective areas, such as education
and cooperative movements. Sen has added yet another economic argument by stating
that investment in health services for the poor is labour intensive and very cost-effective.
COUNTERPRODUCTIVE ROLE
OTHER GLOBAL INITIATIVES
OF
FAMILY PLANNING AND
The feai of population explosion was invoked by some foreign consultants, with
enthusiastic concurrence of the elite class subservient political leadership, to vivisect the
composite ministry of health into department of family planning and that of health. This
was done in 1967. do enforce the population control programme, the political leadership
brought in bureaucrats to make people accept sterilisation for population control. They
were considered by the politicians and their advisors from outside agencies more suitable
to'get the job done'.
In the course of time the bureacrats spread their tentacles more extensively. The situation
now is that these bureaucrats have acquired dominant positions in decision making
processes in complex fields of both health and population for which they have no
competence; they arc certainly not equipped for making what Sen has termed sound
social allocations on the basis of cost-effective studies. They can not even be held
accountable for their actions because they arc frequently transferred to other departments.
Reference has also been made earlier to the devastating impact on lhe health services of
implementation of the plans for structural adjustment, globalisation and encouragement
of private sector and cost recovery from lhe people for public financed health services.
There is also the impact of WTO. There appears to be a deterministic streak all these
decisions which adversely affect the poor.
1 he net result ol all these acts of omission and commission was that desperately poor
people were literally thrown to the wolves’ in the garb of unregulated, greedy, private
sector. The predicament of the poor was dramatically demonstrated by similar findings
from two nationwide surveys on utilisation of medical services in India in the late 1980s one by the NSS and the other by the National Council of Applied Economic Research
(NCAER): 90 percent of them had lost their indigenous mechanisms for coping with their
medical problems and depend on Western medicine; only around 3 per cent sought help
from primary health centres; and most ominous of all, among the poor, meeting the cost
of buying' services from hospitals was the second most important cause of rural
indebtedness, lhe last item shows how important is access to public funded health
services for countering the problem of poverty in the country.
At long last, the World Bank has conceded in The World Development Report, 1999 that
the anti-poverty programmes that had been implemented for half a century by the Bank
have not been very effective. If the Bank and other organisations are keen on 1following
up on these conclusions, then they must look inwards for the causes. There is; a crying
need for fundamental 'structural change’ in the Bank and other international
organisations.
8 -
As early as in the early 1970s, warnings were sounded loud and clear about the
infirmities in design of the Bank’s India Population Project-I. These warnings were
simply ignored. Taking the more recent example of the global programme of
tuberculosis, it has been repeatedly pointed out to the Bank and other 'authorities'
concerned, on the basis of sound scientific data, that the programme is ill-conceived, illplanned, ill-designed and extremely wasteful. For instance, there had been no evidence
which made WHO declare tuberculosis as a global emergency in 1993. How can a once
respected organisation make such a sweeping declaration without a sound data base?
What has happened to that emergency? Similarly, while the AIDS epidemic in SubSaharan Africa has precipitated a human tragedy unprecedented dimensions, affecting
tens of million of people, UNAIDS was conferring to India the dubious and totally
unsubstantiated distinction of being 'the AIDS capital of the world'. There seems to be
some deep seated malady in the working of international agencies in the poor countries
of the world. The Bank, the WHO and other agencies must find out why scientific data
questioning their programmes were suppressed and why those who dared to produce
scientific evidence to raise doubts were systematically ostracised as 'untouchables'?
There appears to be a whiff of totalitarianism in their actions.
CONCLUSIONS: AGENDA FOR ACTION FOR INDIA
Perhaps the most urgent task in the field of poverty and health will be to provide relief to
the poor for their medical problems. This, as has been repeatedly pointed out earlier, is
essentially a political question; the democratic forces in the country must impel the
political leaders to reverse the trends of the past three decades. This, as has been shown
by the NSS and NCAER data, will make significant contribution to alleviating poverty
and destitution. Specifically, this might include the following steps:
1. Many health activities can be decentralised to villagc/slum levels, depending on the
level of community organisation and political action for devolving power to the people.
Local communities can be encouraged to: (a) set up reasonably clean living space for
conduct of normal childbinhs; (b) have locally trained girls for giving immunization,
keeping stores and overseeing the administration of anti-tuberculosis drugs to diagnosed
patients, providing family planning services and advice and implementing child feeding
and other programmes under the Intergratzd Child Development Projects; (c) keeping
records of births and deaths; (d) checking the visits’of village/slum-level health workers
and obtaining their assistance for more complicated problems; (e) maintaining reasonably
good village/slum sanitation levels, including working of tube wells and providing
drainage; (f) imparting education and information on health and development matters to
the population; (g) arranging for transport of needy patients to the nearesHiealth facility
and ensuring that the personnel in those facilities adequately respond to the people's
needs. The list can go on, depending more on the capacity of the community
organisation, than on funds.
2. Concurrent!v. urgent steps can be taken to rectify the anomalies that have crept into the
health services, from the ven- top to the bottom. Some of the priority areas for action
could be:
- 9 -
T-o
a. Strengthening education, training and research capabilities of health administrators by
rejuvenating
the existing public health institutes, so that they can occupy key positions in the health
administration.
b. rolling back generalist administrators from positions for which they do not have the
needed competence.
c. integrate the family planning department with the health department.
d. Integrate the vertical programmes with general health services.
e. Initiate health system research to improve the efficiency of the system.
The list is obviously incomplete. Many other actions can be added on the basis of deeper
studies and analyses. It must be made explicit that these programmes will be integrated
with other programmes directed towards dealing with the problem of rural poverty.
October 30 1999
\
Dr Ravi Narayan, CHC.
- IO ~
8
Com H
HEALTH POLICY AND PLANNING; 10(4): 333-349
© Oxford University Press 1995Xs*^^j^^L fl
(380
Review article
I
i ha role of private medical practitioners and
their interactions with public health services
in Asian countries
SYED ALJUNID
Health Economics and Financing Programme, Heaith Policy Unit, London Schoo! of Hygiene and
Tropica! Medicine, UK
p ..
IMM
I
This paper aims to review the role of private practitioners and their interactions with public health services
in developing countries, focusing largely on the Asian region. Evidence on the distribution of health
facilities, manoower, health exoenditures and utilization rates shows that private practitioners are signifi
cant health care providers in many Asian countries. Limited information has been published on interac
tions between public and private providers despite their co-existence, issues related to enforcement of
regulations, human resources, patient referrals and disease notifications, are examined.
Introduction
This paper examines evidence on the role of
private practitioners and their interactions with
public sector providers in developing countries
iodising primarily on Asia, though information
on other countries is included when helpful. The
private sector is defined as all those organiza■jon-. and individuals working outside the direct
control of the state, that is both for-profit com
panies and individuals, and not-for-profit
private organizations (Bennett 1991). In health
.■are. this is a heterogeneous group consisting of
a wide range of providers with different motives.
Claouin (1981) defined private practitioners as
‘.nc. .-iduals who were perceived by the com
munity to provide resources and assistance in ill
ness but were not employed by the government
health service’. This definition makes a clear
distinction between public and private practi
tioners in relation to their employer. Following
this, he grouped private practitioners in Bangla
desh into 7 categories: allopathic practitioners
with MBBS qualification or Medical Board
license, unqualified allopathic practitioners,
homeopathic practitioners, ayurvedic or unani
practitioners, spiritual healers, traditional mid
wives and others that do not fall into any of the
earlier categories such as bone setters.
R
i
The private practitioners or providers that form
the object of this paper are those who are
allopathic practitioners with MBBS qualifica
tions or equivalent. Within this group, the pro
viders may have either a profit or non-profit
motive. The former usually have financial gain
as their dominant objective in contrast to the lat
ter who provide health care for humanitarian,
religious, charitable or other non-specified
reasons. For-profit private practitioners include
general practitioners in group or solo practice
and doctors working in private clinics and
hospitals. Church and mission hospitals and
clinics are examples of non-profit providers. To
add to the complexity, some non-profit providers
may identify their organizations as such only for
tax purposes, since in many countries non-profit
organizations are given tax relief and subsidies
(Green 1987).
1
i
< ■
1
1
fe-
Ji
II
Significance of private health care in
Asian countries
There is limited information published on private
practitioners in Asian countries. A brief review,
however, shows that private practitioners are
heavily used, although sometimes for particular
..
.
~
i
S
..
■
&
334
Syed Aljunid
complaints. An example of information
available is the Malaysian National Morbidity
Survey conducted by the Ministry of Health in
1986-87. This nationwide household survey used
a two-week recall period, and showed that
private clinics were most commonly utilized for
out-patient care. During the two-week period,
for every 100 ill persons, 5.2 visits were made to
the private clinics as compared to 2.1 visits to
health centres, 1.4 visits to government hospitals
and 0.4 visits to traditional practitioners (MOH
1988a). One obvious limitation of this study was
the use of health workers as the interviewers,
which might have affected the way respondents
reported. An example of this problem is shown
in a study in rural Kenya by Schulpen and
Swinkels (1980), where they found gross under
reporting ot the use of traditional healers when
health personnel were employed as interviewers.
Another study, conducted in two rural villages in
the state of Selangor in Malaysia, found that
32.of adults above 18 years of age utilized
the public services, 22.2(J7o sought treatment at
private clinics, 33.6°7o used self-medication and
11.7^o visited traditional healers (Aljunid and
Norhassim 1992). The study was limited by the
use of a six-month recall period which would
lead to under-reporting, especially of visits for
trivial conditions.
In Indonesia, most of the doctors and a lame
number ot nurses and other paramedical staff
working at private hospitals are public sector
employees either seconded or working part-time
in the private sector. Only I5°7o of the country’s
health workers are directly employed full-time in
private institutions (Gish et al. 1988). Berman et
al. (198/) showed that in Western Java, among
the 3322 treatment contacts, 12.8^0 were made
with private providers (doctors and paramedics),
Ib.S^o with public providers and the rest with
traditional healers or self-treatment. In 1986, the
private sector accounted for 63.2% of the total
health expenditure ot Indonesia (Brotowasisto et
al. 1988).
'Among 132 physicians in the Northern Thailand
Provinces, more than two-thirds of the public
sector doctors reported having after hours
private practice (Smith 1982). In 1985 it was
estimated that there were more than 12 000
private clinics in the country compared to 7800
public health centres (Griffin 1989). Private
health care expenditure in Thailand increased
from 66.7% of the total health expenditure in
1978 to 73.2% in 1987 (Wibulpolpraset 1991a).
In 1974, 69% of primary care facilities in the
rural areas of the Philippines were owned and
run by private practitioners (Griffin and Paqueo
1993). A study among 399 households in the
Bicol region, a poor rural region of the Philip
pines, showed that 31% of the adults visited
private practitioners compared to 18% using
government clinics; the remainder visited tradi
tional healers or did not seek any medical help
(Akin et al. 1986). In 1980, the per capita expen
diture on health for the country was USS18.23;
US$13.39 was spent in the private sector and on
ly US$4.84 in the public sector (World Bank
1987). Roemer (1991) reported that in 1981, 59%
ot physicians in the Philippines were engaged en
tirely in private practice. Among the 41^0 public
doctors, nearly all did some private practice part
of the time.
In India, 56% of hospitals and 49% of dispen
saries in the country were owned by private
organizations in 1988. Furthermore, it was
thought that the figures for private ownership
were even greater as information on clinics and
nursing homes which exhibited strong private
ownership were not available (Bhat 1991). It was
estimated that about /?% ot qualified physicians
in the allopathic system were in private practice
and only 27% worked in public services (Bhat
1993). In a household survey in a rural district of
Maharastra, Duggal and Amin (1989) found that
■ ■% of the iilness episodes were presented to
private practitioners and hospitals compared to
only 13% to government facilities. In another
study (Visvanathan and Rohde 1990) it was
shown that 65% of diarrhoeal cases sought
medical treatment, 80% of these cases went to
private practitioners and only 10% to govern
ment health facilities. In terms of health expen
ditures, Nichter (1980) found that 82 poor
families in South Kanara district of Karnataka
spent 7% of their family expenses on health,
60% of which was spent for private consultations
and drugs.
In Papua New Guinea, Kolehmainen-Aitken et
al. (1990) reported that the percentage of doctors
Private practitioners and public health services
in full-time private practice increased from IS^o
to 18^0 between 1984 and 1990. In 1974 only
15^o of the patients of all expatriate private prac
titioners were nationals; 10 years later this had
increased to 50a7o.
Hillier and Zheng (1990) reported that China has
1^60 000 private doctors (including paramedics).
Seventy per cent of them worked in rural areas
and 45T) of villages had at least one private doc
tor.
These studies show that private practitioners in
Asia are important health care providers besides
the government and indigenous healers. In some
or these studies, private practitioners were utiliz
ed more frequently than the government services.
Factors influencing utilization of health
services
ms section reviews evidence of factors which
mfluence the utilization of private and public
services. Identifying such factors assists in under
standing the barriers faced by users of the ser
vices. These barriers which limit accessibility to
services need to be considered by policy-makers
when promoting private or public sector services.
1 he classification of Kroeger (1983) was used to
isiess factors influencing utilization of health
services: characteristics of the subjects, the
disorder and the service.
Characteristics of the subjects
Socioeconomic status
Socioeconomic status is commonly mentioned as
an important factor affecting the choice of pro
vider in rural communities. More importantly it
•■'O affects the decision of whether or not to seek
tr-vmment (Fiedler 1981).
Cortinovis et al. (1993) argued that developed
country socioeconomic classifications based on
income, occupation and literacy are inap
propriate in developing countries because of
structural and economic heterogeneity between
the countries. However, many studies in develop
ing countries do use income or occupation as
socioeconomic indicators but tailor them accor
ding to the local situation (Benyoussef and
335
Wessen 1974; Heller et al. 1981; Berman et al.
1987). Others use a combination of more than
one variable, such as occupation, ownership of
land, and educational level, to classify
socioeconomic status (Cortinovis et al. 1993;
Ramachandran and Shastri 1983; Amin et al*
1989). Recently, Dye and Lee (1994) reported us
ing only ownership of cows and sheep as an ade
quate indicator of the socioeconomic status of
households in rural Kashmir.
Heller (1982) found that households with higher
income levels shifted their demand from public
to private clinics in Malaysia. The National Mor
bidity Survey by the MOH showed that lower in
come groups (monthly income of RM 500 and
below) had lower utilization rates and higher
tendency to use public services than higher in
come groups (MOH 1988a). However,^private
clinics were utilized by 35J7o of those in the lowest
income groups (less than RM 300 per month)
while 25*0 of those in upper income groups (RxM
2000 and above per month) used the subsid
ized public facilities. These two studies did not
disaggregate urban and rural areas.
A community-based study in a rural village in
Malaysia showed that utilization of private
clinics by adults aged 18 years and above in
creased significantly as income increased (Aljunid and Norhassim 1992). The percentage of
respondents who utilized private clinics increased
from 7*70 for those with monthly per capita in
come of less than RM 50.00 to 36.507o for the
group with income of RM 150.00 and above. The
percentage of respondents who visited traditional
practitioners decreased as income increased.
Berman et al. (1987) showed that in Indonesia,
at all levels of severity of illness, higher income
groups were more likely to seek treatment; he
pointed out that the use of private physicians was
primarily restricted to the upper income group.
Heller et al. (1981) found that in Mexico, those in
lower socioeconomic classes were less likely to
have a stable source of medical care and more
likely to use public rather than private facilities.
Ethnicity
Different ethnic groups have different patterns
of utilization. In Malaysia, Heller (1982) found
that Chinese people used out-patient services
more frequently than Malays and Indians even
1
3
I
1
I i
#11!
iSI
,O|
I
.-l--:'
• I®
I
T
-o
336
Syed Aljunid
after controlling for socioeconomic status. No
explanation was offered for these findings. The
National ^Morbidity Survey in Malaysia also
showed that the Chinese were more likely to use
private care facilities than Malays and Indians
(MOH 1988a). These findings are likely to be
confounded by income, not controlled in the
analysis. The explanation offered for the ethnic
differentials in this study was the distance to ser
vices: the Chinese population is more urbanized
than the other two population groups. Kroeger
(1983) suggested that differences in symptom
sensitivity in different ethnic groups may be one
explanation for inter-ethnic variations in utiliza
tion. The patients’ desire to choose doctors from
the same ethnic group who speak the same
language might be another reason for the observ
ed ethnic pattern of utilization.
groups within the home. Another interesting fin
ding was that those aged 5-15 and those over 45
were more likely to use traditional medical care
rather than modern treatment. The latter finding
might be due to the confidence of older age
groups in traditional practitioners but the former
finding could not be explained by Heller.
Senior and Bhopal (1994) recently suggested
four problems in using ethnicity as a variable in
research: difficulty of measurement, hetero
geneity of populations being studied, lack of
clarity about the research purpose, and ethnocentricity affecting the interpretation and use of
data. Among other things, they suggested that
ethnicity should be perceived as different from
race, that researchers should appreciate the
complex and fluid nature of ethnicity, and that
higher priority be given to research on methods
tor ethnic classifications. Such issues are as
relevant in industrialized as in less developed
countries.
Gender
Studies from various countries have shown dif
ferent utilization patterns between males and
females. In Tunisia, for instance, it was found
that females had higher rates of utilization than
men in both rural and urban areas in almost all
age groups (Benyoussef and Wessen 1974).
Age
Health needs at different ages influence utiliza
tion patterns. A study by Benyoussef and Wessen
(1974) in Tunisia found a ‘U* shape utilization
rate with peaks at both extremes of age; this was
explained by the high morbidity rates in the very
young and the elderly.
®j
Heller (1982) found that the schoolchildren
and household members in the working age
group in Malaysia were more likely to consume
out-patient services (public or private services)
despite their relatively lower morbidity rate. He
showed that the high morbidity group in the age
groups 0-4 years and more than 45 years con
sumed the smallest amount of out-patient care.
He postulated that this unusual finding might be
due to household choices to treat a significant
fraction of minor illnesses of these dependent age
In Singapore, Fong and Phua (1985) found that
at all age groups, private general practitioners
were more frequently utilized than government
out-patient services. For both services, their
utilization rate peaked at the age groups 5-9 and
over 50. There was another peak in the utiliza
tion rate of private general practitioners at the
20-30 age group. The researcher suggested that
this peak might be due to employees who require
a medical certificate for absences from work.
Akin et al. (1986), in their study on the demand
for adult out-patient services in the Philippines,
reported a statistically significant increase in the
probability of a private versus a public sector
visit if the sick person was male. They suggested
that such findings may be indicative of a diver
sion of resources towards males to improve the
quality of their care.
The priority of men over women in receiving
health care was also found by Feldman (1983) in
his study in Bangladesh. He found that men are
more likely to use allopathic treatment than
women. He suggested that allopathic medicine,
which has a quicker effect and is more powerful,
may be reserved for the males since male labour
is assumed to be of greater value than women’s
labour. This is particularly true for poor families
where males seek quick cures in order to be
available for employment opportunities. It is
also possible that when men control the family
finances, they might give priority to their own
health needs.
In contrast, Fong and Phua (1985) in Singapore
found that females visited private general practi-
s
Private practitioners and public health services
'.ioners 1.7 times more often than males. Women
Also visited government out-patient services 1.6
.imes more often than men.
Sources of finance
Source of finance is one barrier to use of private
leaith care providers in developing countries.
Third party payment mechanisms, such as health
nsurance coverage, are poorly developed though
developing rapidly in some richer developing
rountries. Coverage of suc*h schemes tends to be
.imited to certain sections of the population,
asually those employed in the formal sector. Ser■ ices covered tend to be mostly hospital admis;ions rather than ouf-p&tient services. Ron et al.
1991/ reviewed health insurance schemes in 14
■.eveieping countries and reported that in most
.ouniries public services were utilized to deliver
•ervices under the scheme, except in South
Korea, the Philippines and Thailand where
private practitioners were selected through an ac
creditation process. Bennett and Tangcharoenathien *1993) noted that in Thailand, formal
ector employees covered by national health inurance demanded access to the private sector in
■eturn for their contribution.
n Malaysia, only 6.5% of users of government
acilities paid through third parties, "O^o had
Tee services and the remainder paid out-ofoocket. Among the users of private facilities,
20.9^0 paid through third parties and the majorty paid out-of-pocket. Most with third party
coverage in the private sector received this
privilege as an employee benefit (MOH 1988a).
n Indonesia, 13% of the population, almost all
cf them government employees and their
families, were covered by some form of health
msurance (Brotowasisto et al. 1988). Direct outjf-pocket payment comprised by far the greatest
cart of all household payments to public and
Arivate sector facilities.
I
337
Malaysia, Heggenhougen (1979) found that most
people used the public clinic for minor problems
and presented their more serious health problems
directly to a private physician.
Lim (1991) reviewed 3164 patients attending 8
private clinics in two rural districts of Pahang, an
east coast state in Malaysia, and found that 87
of patients came for medical treatment and only
13*70 for preventive care. Minor conditions,
mostly acute illnesses, represented 82% of the
cases; major disorders (mainly chronic illnesses
such as hypertension, asthma and diabetes
mellitus) accounted for 18% of cases. Upper
respiratory tract infections were the commonest
minor conditions while hypertension was the
most common major condition. He suggested
that chronic illnesses were not commonly treated
in the private sector because of the expense of
obtaining long-term treatment which was provid
ed free of charge in the public sector.
In Kenya, Mwabu (1986) reported that different
illnesses gave rise to different consultation pat
terns. He found that although government clinics
were more frequently visited on first consulta
tion, villagers visited private mission clinics for
diseases like diarrhoea, malaria, leprosy and
tuberculosis.
A disease-specific utilization pattern emerged
in a study by Sarder and Chen (1981) in
Bangladesh. They found that although some pro
blems like diarrhoea and fever were treated by all
practitioners, others such as respiratory infec
tions and parasitic diseases were treated by
allopaths and homeopaths while jaundice, snake
bites and headache were treated by traditional
healers. They stated that client selection of
practitioners was influenced by availability, cost
and the perceived effectiveness of technology in
relation to a particular disease.
J
1
■1
it
I!
4
■!
-1
1
Yesudian (1994), in his study in Bombay, India,
showed for all socioeconomic strata that patients
Characteristics of the disorder
with minor and chronic illnesses more commonly
in a study in a Malay rural village in Malaysia,
Colson (1971) found that acute and fatal disease
vere presented more frequently to modern pracitioners, whereas chronic non-fatal illnesses
vere presented to traditional healers. In another
■.tudy among villagers attending a rural clinic in
used private sector providers than other sources.
However, for acute illnesses, the level of utiliza
tion of private health care increased with
socioeconomic status. Criteria for grouping the
diseases into minor, acute or chronic were not
stated.
II
■w
tW
I
b 'A
'
■
...
ST
PT;
I
'
i
I
.'M
til- ■ I
-
<r
i
'
'i
I
i
to«
fggti
•H T" <
338
Syed Aljunid
Characteristics of the service
Studies in developed countries, such as Joseph
and Bantock (1982) in Canada, Dutton (1986) in
the USA, and Haynes and Bentham (1982) in the
UK, have also found that distance is a barrier to
utilization or affects the poor more.
Geographical accessibility
In rural areas of developing countries, a low
degree of geographical accessibility to modern
health services is a major reason for use of other
services such as traditional care. In a study in
rural Nigeria, Stock (1983) found that rural
populations living further from health facilities
tend to delay using these services and preferred
alternatives such as self-treatment with tradi
tional or patent medicines. He also noted that
various factors atfect utilization in relation to
distance, including perceived effectiveness of
Western-type treatment and perceived quality of
service. Males travelled further than females to
obtain treatment. This was attributed to the
religion of the Hausa people in which married
women must obtain permission from their
husbands before leaving their homes. Adults
were found to travel further for treatment than
children.
Quality of care
Patient satisfaction, a component of quality of
care, has been given high priority in developed
countries. Fitzpatrick (1991) cited three reasons
for the importance of patient satisfaction: it
determines compliance with recommended treat
ment and influences patient choice of provider; it
is a measure of patient involvement in decisions
about care; and it can be used to choose alter
native methods of organizing and providing
health care.
Research in developed countries has focused at
tention on the theoretical and methodological
issues in assessing patient satisfaction. Pascoe
(1983) suggested that research on patient
satisfaction has not been guided by a wellsupported definition or psychological model of
satisfaction. Williams (1994) supported Pascoe’s
views on the theoretical weaknesses and iden
tified the impact of different methodological ap
proaches on the results of patient satisfaction
research. He showed that in quantitative studies,
satisfaction tended to be high while greater levels
of disquiet were revealed through qualitative
methods.
In the West Indies, a study by Poland et al.
(1990) showed that distance to permanent health
care services was a significant predictor of
utilization. This was supported by a study in
Southern Iraq which noted a decline in utiliza
tion rates at modern health care centres (both
public and private) with increasing distance
travelled. The authors concluded that the single
most important factor related to variation in
utilization was distance travelled by people to
reach the service, once variation due to sickness
or need was taken into account (Habib and
Vaughan 1986).
A few studies on patient satisfaction in develop
ing countries have exposed the weakness of
public services and higher patient preference for
private health care. Gilson et al. (1994), using
both quantitative and qualitative methods,
studied community satisfaction with primary
care facilities in Tanzania and found that services
provided by church dispensaries were ap
preciated much more than government facilities.
Drugs were more consistently available and
health workers in these services exhibited more
positive attitudes towards their patients.
Mode of transport also affects utilization. In
Ethiopia, patients in the cities use private or
government cars to get to private clinics; those in
the periphery make the trip on foot, by over
crowded buses or taxi and use a mix of govern
ment facilities and traditional remedies (Kloos et
al. 1987).
In Malaysia, it was found that utilization rates of
both government and private clinics decreased
with increasing travel time and travel cost (MOH
1988a). Earlier, in 1982, Heller reported that
among households using both government and
private clinics, an increase in travel time lowered
the utilization rate of government clinics but not
of private facilities.
Long waiting times, shortage of drugs, and poor
attitudes of nurses and physicians were among
the complaints about public facilities gathered in
group discussions in a study in Mali (Ainsworth
1983). The respondents indicated that personal
connections were important in skipping registra
tion queues and that the only way to obtain ade-
■
;
■......................................... ■
.
.
■
■
339
Private practitioners and public health services
quate care was to arrange for private care after
office hours.
Kloos et al. (1987), in a household study in a
suburb of Addis Ababa and four rural villages,
showed that patients preferred services from
private physicians rather than government clinics
because of their personalized services and shorter
waiting times. He found that 6O*ro of wealthy
traders and 13% of people from other
socioeconomic groups used private services, even
though the charge was 10 to 15 times higher than
in government facilities.
In Malaysia. 9O,ro of the patients bypassed the
community clinics manned by community nurses
to seek treatment at health centres, district
hospitals and private clinics where doctors were
available (MOH 1988a). Patient perceptions on
the quality of services provided by doctors might
be one reason for this finding. On average,
patients have to spend longer in government
health centres compared to private clinics (MOH
1988a).
Annis : 1981) reported poor utilization of govern
ment health posts due to understaffing, badly
unuerequipped services and poor quality of <er:es in rural Guatemala, in rural Mexico, people
preferred private physicians over the more ac
cessible health centres which were staffed by
young and inexperienced doctors (Walt 1977).
In most of the studies mentioned above, patients
rei- ed the quality of care given by private
providers to be higher than in public services.
?rowever, some studies using professionally
def’ned criteria for quality of care have found
contrary results. Uplekar and Siiepurd ‘1991)
studied the prescribing patterns of 143 private
allopathic and non-allopathic doctors in the
treatment of tuberculosis in a slum area of Bom
bay. They found that the doctors prescribed
three times more expensive drugs than the na
tional standard and also used unnecessary drugs.
Eighty different regimes were used by the doc
tors, although only four of these conformed with
the regimes used by the National Tuberculosis
Programme. They suggested that poor participa
tion of private doctors in continuing medical
education and the lack of integration with the na
tional health system were the reasons for the
poor quality. In another study on management
I
-UK
. .
.
of leprosy by 106 private practitioners from the
same area, Uplekar and Cash (1991) found that
none of them followed the WHO recommended
regime for treating leprosy.
3
Recently, Hooi (1994) reported that of 100 tuber
culosis cases treated in a public hospital in
Malaysia, 48 of them had consulted private prac
titioners and
of these had had delays in
diagnosis and treatment compared to only 15 ,J7o
of those in the government facilities. Further
more he showed that only Id.b^o of those who
had first consulted private practitioners had
undergone chest X-rays and only 2.1% had
undergone sputum analysis on their first visit. He
suggested that private practitioners may be
unaware of proper diagnostic and management
regimes for tuberculosis. This study suffered
from selection biases as only those cases even
tually treated in public hospitals were studied.
■i
Ij
1fe'
i
A study in India showed that private doctors
prescribed a greater number of drugs and injec
tions than public doctors and that the most com
monly prescribed drugs were vitamins and
tonics. Among the patients who visited private
practitioners, 55lT7o were given an antibiotic; of
these. 23% received two or more types. In con
trast. only lS,ro of patients who attended govern
ment primary health care centres were prescribed
antibiotics; of these only 6% received more than
one drug (Greenhalgh 1987). This study did not
indicate whether the type and severity of illness
suffered by both groups of patients were com
parable. In the same study, the management of
diarrhoeal cases differed, with private doctors
being less likely to recommend oral rehydration
therapy and more likely to prescribe an inhibitor
of gut motility or a binding agent than the sec
tors in government primary health care centres
and teaching hospitals.
w
■.
w,,
Wyatt (1992) suggested that injections were very
popular in developing countries because these
may epitomize Western medicine, reinforce
traditional beliefs about healing and disease, and
may be the most profitable part of doctors’
work, especially in the private sector. She cau
tioned against the excessive use of injections
because of the danger of provocation of paralysis
in poliomyelitis cases and transmission of
hepatitis B and HIV virus if unsterile needles and
syringes were used.
F
.. .
./
I
I
i.
340
Ahmad and Bhutta (1990) studied the prescrip
tion of four types of non-essential drugs (antidiarrheals, appetite stimulants, multivitamins
and brain tonics) promoted by the pharma
ceutical industry among 100 private physicians in
Karachi. Most of these drugs were ineffective
and some may be hazardous: 55°7o of all drugs
prescribed by the doctors were in this category.
He suggested that poor prescribing resulted from
the dependence of doctors on salesmen and pro
motional materials from drug companies, the
lack of involvement in continuing medical educa
tion among private practitioners, and the
absence of a national drug policy in the country.
No comparison was made with doctors in public
services and the information was gathered by
questioning the practitioners rather than study
ing their actual prescribing habits.
A- '-'k
.■
■■
■
:
■
Gilson et al. (1993), using retrospective data
from patient registers, compared drug prescrip
tions trom tour church dispensaries and 16
government facilities in Tanzania. Church
dispensaries prescribed 2407o more drugs per visit
than government units. Antibiotics, chloroquine
and injections were given in higher proportions
by church dispensaries compared to government
units. Most ot the non-essential drugs were given
m church dispensaries. It was suggested that the
prescribing pattern observed was due to the suc
cess of the Tanzanian Essential Drugs Pro
gramme (EDP) in the government services.
Church dispensaries, which were outside the
EDP system, charged fees for treatment and may
prescribe more drugs to gain revenue and to
satisfy patient demand resulting from payment
of fees.
•
f, II
-
Syed Aljunid
S'-'-" ■■
Price of care
In most developing countries, public services are
usually highly subsidized and private health care
is often expensive. The high utilization rate in
private sector facilities, despite the high charges,
has been used as evidence that demand for ser
vices was not primarily determined by the price
of care. For example, Akin et al. (1986), in the
rural Bicol region of the Philippines, showed that
private clinics and hospital charges were over 28
times higher than charges at government clinics
and hospitals. Despite this, private facilities were
still utilized more frequently than public
facilities.
I
I
■
■
! k A
In Malaysia, almost all out-patient visits to
government health centres are free, and in 60<7o
of visits to government hospitals the charge is
only RxM 1.00 for both consultation and medica
tion. The average payment in a private clinic was
RM 12, with 32To paying RM 5 to RM 9 and a
further 30% paying RM 10 to RM 14. Despite
the great differences in the fees, private clinics
were utilized twice as frequently as public clinics
(MOH 1988a). Heller (1982) showed that de
mand for out-patient and in-patient care among
Malaysian users was highly inelastic to cash price
(price elasticity of demand measures the respon
siveness of demand to changes in price). He con
cluded that the demand for out-patient and in
patient care in Malaysia was not responsive to
changes in the price of care. A 10% increase in
the price of public out-patient care would reduce
demand by only 1.5%. Nevertheless, consumers
were responsive to the relative cash prices of
private and public out-patient clinics. Heiier
showed that the cross price elasticity of demand
tor public care due to changes in private out
patient prices was approximately +0.15. Cross
price elasticity of demand measures the response
in quantity demanded of a certain good or ser
vice which arises from a change in the price of
other goods or services. In this study, a 10% in
crease in the price of private out-patient care
increased the demand for public out-patient
services by 1.5%.
Gilson (1988) and McPake (1993) criticized
studies by both Akin et al. (1986) and Heller
(1982) for their failure to estimate the impact of
price on demand for different income levels. The
impact on utilization resulting from price
changes would probably be greater in lower than
upper income groups. Akin et al. (1986) at
tributed their findings of low price elasticitv
partly to the differences in quality of care bet
ween the public and private sector and severity of
illness. These two factors were not controlled in
their demand model: it is possible that patients
are willing to pay more for higher quality care
and when their disease is severe.
Yoder (1989) showed that in Swaziland the in
crease of fees in government services led to a
32.407o decline in the attendance at government
facilities and an increase of 10% in attendance at
mission facilities. There were also declines in pa
tient visits to both government and mission
!t4
•
■
...
z
I
■
.
.
■
_______________________
.
_
.
.
__________________________________________________
'y!
I
■
Private practitioners and public health services
facilities for BCG, DPT immunizations, and for
treatment of dehydration in children, each show
ing substantial declines in average attendances of
16, 19 and 24% respectively. The negative impact
of user fees on utilization of public facilities has
also been shown in Kenya (Moses et al. 1992),
Zimbabwe (Hongoro and Chandiwana 1994) and
Zaire (Bethune et al. 1989; Haddad and Fournier
l°95).
Types of services available
The types of service available also affect the
choice of facility. In developing countries the
: pes of service -*of private providers have
-arely been documented. This is basic informaicn, needed before a greater role of private proGuers can be considered in developing countries.
T'-ai and Donaldson (1987) suggested that lack of
systematic and careful record-keeping by private
nractitioners was one reason for poor documen
tation of services provided by private providers.
it is generally assumed that curative services are
the main focus of private practitioners' activities,
a/hough the actual nature and extent of services
has been little documented. In a survey in tne
state of Perak, Malaysia, 17 private practitioners
ere asked to list their services (Diong 1988). The
'."ictitioners indicated curative and preventive
services, including procedures and diagnostic in
vestigations. The list has limited value since it did
not really reflect what was actually provided by
me private doctors. Some of the procedures
IZted (e.g. deep lymph node biopsy and re
moval of breast lump.) can only be carried out by
■rained specialists. The profile of the providers
was not given in this study.
Leopando (1988) reported that 74% of family
physicians (mostly private practitioners) in the
Philippines provided immunization services in
addition to other curative care.
Family planning services are widely provided by
,?r:vate practitioners in developing countries. \
study in Kenya among 592 private physicians
using mailed questionnaires showed that family
planning services were being dispensed on patient
demand, the pill was the method largely pre
scribed, and sterilizations were being done for
older female clients (Mugo-Gachuhi 1977).
Surveys carried out in 25 countries in Africa.
Asia, Latin America and the Middle East bet-
341
ween 1979 and 1984 showed that an average of
13% of rural and 18% of urban family planning
users reported using private clinics (London et al.
1985).
Antenatal services have also been reported to be
provided by private practitioners. In Egypt 71%
of the households in a rural area received
antenatal services from government facilities as
compared to 21% from private clinics (Abu-Zeid
and Dann 1985). The extent and comprehen
siveness of this service by private practitioners
were not reported. Among the urban poor in
Kuala Lumpur, 13% of pregnant mothers
received antenatal care in private clinics and
hospitals, and 11.5% of children were delivered
in these facilities (Gan and Yusof 1993).
!'
■
bbiii
L
«<4;;
'
'
i
Private practitioners were also found to provide
services not provided by government facilities.
House calls by doctors are common among
private practitioners in Indonesia (Berman et al.
1987). In the Philippines, private clinics generally
operate longer hours than public clinics. Accor
ding to Griffin and Paqueo (1993), almost ail
private clinics (96%) opened on holidays
compared to only 10% of the public clinics, and
nearly three-quarters of the pri'-ate clinics pro
viced services after office hours compared to
only 6% of the public clinics.
Interactions between public and private
providers
Interactions between health workers in the public
and private sector have been poorly documented,
particularly in developing countries, yet it could
be argued that interactions between the two pro
viders are inevitable and it is surprising that so
little information exists (EPU 1985). Given that
many health programmes affect both private and
public providers, understanding the kinds of in
teractions and problems faced by them provides
valuable feedback to health planners seeking to
improve the effectiveness and efficiency of such
programmes.
-
zS
■
i
a MW
ig
■■
Due to limited evidence in the literature, the in
teractions between the two sectors on enforce
ment of regulations, human resources, patient
referrals and diseases notification only will be
discussed.
III
342
I-■'"
W':''
Syed Aljunid
Enforcement of regulations
Perhaps the commonest form of interaction
between the public and private health sector is
through the regulation of private health care.
Extreme proponents of the market approach are
not in favour of regulation, even in the presence
of market failure, as state intervention is not
seen as providing any better solution than that
reached by market adjustment (Bennett 1991).
They blame excessive government regulation as
the cause of many of the current problems in
health care. Regulation of health services has
been argued to cause greater administrative
costs, greater inequality in attendance access,
greater chance of unnecessary or iatrogenic in
ter ventions, and unjustified development of
inadequately evaluated, complex technology
(Belmartino 1994).
Roemer and Roemer (1982) believe that the ex
istence of a free market in health care provision
may lead to monopoly or oligopoly, turbulent
competitive disequilibrium in favour of pro
viders, and long-term contractual arrangements
between consumers and providers. They further
suggest that these outcomes might be very
deleterious to consumers unless regulated. It has
been argued that the government is responsible
tor regulating the private health sector because it
has obligations to protect its citizens and to en
sure that resources are not wasted (Garner and
Thaver 1993).
Regulation ot the private health sector in many
developing countries is weak because of lack of
resources, poorly decentralized government ser
vices, lack of information on activities of private
providers and professional self-interests of the
regulatory agency (Bennett et al. 1994). The
World Bank, while suggesting a greater role for
the private health sector, recognizes the need for
governments to strengthen their capacity to
regulate the private sector in order to ensure
quality of care (World Bank 1993).
Registration of doctors and other health workers
is usual in most countries. In Malaysia, under
the Medical Act (1971), the Malaysian Medical
Council (MMC) was established to register the
practitioners and take care of ethical issues.
The MMC is a quasi-governmental body with
government maintaining control through the
nomination of 13 of 24 members. The nominated
members are government officers in the MOH
and the remaining members are elected by the
profession. Reports of the activities of the MMC
showed that, despite many complaints of medical
negligence in the media, very few cases were
reported and investigated. Between 1989 and
1991, 72 cases were reported to the MMC, only
35 were investigated and disciplinary action was
taken against only 7 doctors (/Vew Sunday
Tinies, 1993).
In India, Yesudian (1994) reported that people’s
confidence in the Maharasta Medical Council
had decreased because it tended to protect the
doctors rather than the public in cases of medical
negligence. He cited a case of medical malprac
tice where the Council had to be forced to take
action through court orders.
In 1990 in Malaysia there were 79 health laws and
regulations and 36 health-related laws: it is com
monly held that these are poorly enforced. The
Private Hospital Act (1971) is the main act
regulating the private hospitals in the country. It
has provision for annual inspections and
registration of private hospitals. This is enforced
by the Ministry of Health. This Act is now being
amended to extend its coverage to private clinics.
It was envisaged that under the amended act the
minimum standards for private clinics and their
distribution in the country would be spelled out
(MMA 1993). The existence of similar regula
tions have been reported in Thailand (Bennett
and Tangcharoensathein 1994), Singapore
(MMA 1993) and Malawi (Ngalande-Banda and
Walt 1995).
Regulation regarding location of practice is ap
plied in developed countries but has rarely been
reported in developing countries. In Tanzania,
regulations to control the location of clinics and
types of personnel to be employed were present
but not properly enforced (Mujinja et al. 1993).
Under the Medical Practitioners and Dental Act,
1987, paramedicals in Malawi were allowed to
open private clinics but only in rural areas. This
regulation was not strictly enforced as most
paramedicals opened their clinics in peri-urban
areas (Ngalande-Banda and Walt 1995).
Government control over new investments has
been applied in many countries through cer
tificates of need. This is aimed at controlling cost
Private practitioners and public health services
escalation due to excessive use, particularly of
expensive medical equipment. In developed
countries such as France and Canada, in
vestments in expensive medical technology are
controlled by the government. Yang (1993)
reported that Magnetic Resonance Imaging
(MRI) in Korea had not been regulated by the
state and the service was more accessible to the
rich than the poor. He further suggested the
formation of a corporate body responsible for
assessing new technologies before adoption.
Foote (1986) assessed the Medical Device
Amendments of 1976 which authorized the Food
and Drug Administration in the USA to regulate
medical equipmerft for safety, but concluded that
it was not effective and failed to stop the entry of
unsafe medical devices into markets.
Bhat (1991) raised the issue of uncontrolled use
of high technology equipment in private ciimcs
to attract customers. He argued that this would
lead to unnecessary waste of resources and ex
posure of patients to unnecessary risks. In the
USA. Hillman et al. (1990) found that patients
were at least four times as likely to have
diagnostic imaging (ultrasonography and
rauiography) done if they sought care from a
physician who had the facilities in his office
rather than from one who referred patients to a
radiologist. This suggests the presence of
supplier-induced demand.
In Thailand, where there is no legislation to con'roi the purchase of sophisticated medical equip
ment, 35 out of 57 CAT scanners in the country
were in private hospitals. Six out of the total of 8
MRI scanners in the country were owned by
private hospitals (Wibulpolpraset 1991b). Where
populations are less vigilant and knowledgeable,
:mscrupulous practitioners may rake advantage
of rhe situation for their own gain.
Human resources
Tcemer (1984) expressed concern about how the
private health sector competes with public ser
vices to attract trained workers in developing
countries. He stated that most developing coun
tries spent only
of the GNP on the public
health sector, leading to low salaries for public
health workers. Health workers such as physi
cians and nurses are normally trained by govern
ment to serve the public health sector. The
private health sector attracts these trained and
343
sometimes experienced workers by offering high
incentives which cannot be offered by the
government services.
One way of retaining health workers is through
regulation, where health workers are required to
serve in the;public sector for a certain period of
time before being allowed to leave for the private
sector. In Malaysia, the Medical Act (1971) re
quires all doctors to serve three years in govern
ment services. This was extended to five years in
1992. Those sponsored by government for their
training are bonded for between 7 to 10 years to
serve in government services. Nevertheless, many
doctors leave the public services after the com
pulsory service period and some pay their bond
to be released to work in the private sector
(MOH 1988b).
Incentives to retain doctors in the public services
by allowing them :o work in private clinics after
office hours were reported in Jamaica, Egypt, Sri
Lanka, Thailand, Indonesia and Malawi
•'Roemer 1984; Ngalande-Banda and Walt 1995).
However this is not favoured in some countries
for fear of abuse or neglect of government
facilities. In Nigeria, government doctors
reportedly referred patients they see in govern
ment facilities to their own private clinics (Attah
1986). In Egypt, even though newly graduated
doctors are required to work for at least two
years in government health units in rural areas,
they only saw public patients in a few hours in
the morning and spent the afternoon in private
clinics where they could earn more than their
government salaries (Roemer 1984).
-
-!lll
■ IB 1
' Hi
<?e
H
i
-
To solve shortages of manpower, private doctors
are sometimes employed to work in public
facilities. In India, for example, private
specialists were employed as honorary con
sultants in public facilities. However, these
honorary consultants abused their position by
admitting their private patients to government
facilities and charging them (Yesudian 1994).
■
I
s
■
The Malaysian Medical Association has been
urging the government to allow government doc
tors to work part-time in private clinics to reduce
the influx into the private sector (MMA 1991).
This suggestion was turned down by the MOH
on the grounds that public services would be
neglected (The Star, 1992).
-W’
■
s
i
'~i
Il--
•■Oi
r
344
In India and the Philippines government doctors
were not allowed to open private practice
(Roemer 1984). Nepal, Pakistan and Thailand
had similar regulations and paid non-private
practice allowance incentives to public doctors.
However, this financial incentive failed to stop
government doctors engaging in private practice
(Bennett et al. 1994).
• <
y
■
Syed Aljunid
:
-
IOS
I
Patient referrals
The referral system is the most important link
between different health providers and is the
system through which medical practitioners com
municate with one another. Private practitioners
refer two groups of patients to public providers:
those who cannot afford to be treated by private
practitioners and those who cannot be treated or
^investigated due to lack of facilities and expertise
(Lachman and Stander 1991).
In rural areas ot Malaysia, private practitioners
do not normally have in-patient services. Since
most private hospitals are located in urban areas,
private patients needing secondary care and in
patient services will be referred to public
hospitals (Ming 1982).
I
KM
-v-'H $
■
"
■ i
;
|
Interaction between providers has been studied
through analysis of referral letters in many
studies in developed countries. For example,
studies in the UK and Netherlands have focused
mostly on interactions between general practi
tioners and their colleagues in hospitals. The
complaints of general practitioners include the
tailure of hospital doctors to return the patient to
their care and the failure of hospital doctors to
read the referral letters (Doeieman 1987).
General practitioners have also accused hospital
doctors of not understanding the problems of
the patient outside the hospital (Grace and
Armstrong 1987) and considered the replies to
referral letters by specialists to be irritating,
discourteous and belittling (Western et al. 1990).
Grace and Armstrong (1986) studied 213 refer
rals in rhe UK and found that in only 48.4% of
the cases was there agreement between hospital
consultants and general practitioners on the
reasons for the referrals. The hospital con
sultants criticized the general practitioner’s
management of patients before the referral and
felt that most ot the referrals were unnecessary
(Grace and Armstrong 1986).
The quality of referral letters by general practi
tioners has also been studied. Creed et al. (1990)
found that doctors who write detailed referral
letters refer the least patients. Westerman et al.
(1990) showed that 60% of referral letters sent
by general practitioners to specialists in the
Netherlands were of poor quality.
A standard referral letter has been introduced in
some settings to improve the quality of com
munication between providers. Jones et al.
(1990) showed that despite the introduction of a
standard ophthalmic referral form, 19.2% of the
general practitioners did not use it when referring
patients to an eye hospital in Manchester, UK.
The studies reviewed so far have been carried out
in developed countries. In developing countries,
assessment of referrals between public and
private practitioners has rarely been reported. In
South Africa, of 1143 referral letters received in
a children’s hospital, only 4.8% were considered
to be complete in terms of patient history, ex
amination, diagnosis, appropriate investigations
and treatment at primary level (Lachman and
Stander 1991). It was suggested that the varying
quality of reterral letters found in this study was
due to the workload of referring doctors, lack of
understanding of the need for comprehensive
details about patients and lack of contact
between the hospital and referring doctors. Yesudian (1994) reported medical malpractice in
reterral in India where money was paid to
general practitioners to encourage referrals to
certain consultants.
Disease notification
Disease notification is one component of com
municable disease surveillance programmes in
many countries. Since disease surveillance pro
grammes are normally carried out by the public
sector, public and private providers may interact
through this programme. Disease notification is
useful in advising appropriate medical therapy,
detecting outbreaks, and for planning and evalu
ation of prevention and control programmes
(Chorba et al. 1989).
Despite the importance of reporting, under
reporting of notifiable diseases has been iden
tified in many developing countries. Studies in 7
East Mediterranean countries (Pakistan, Sudan,
Somalia, Syria, Yemen Arab Republic,
Private practitioners and public health services
Democratic Yemen and Egypt) and five Asian
countries (Bangladesh, Bhutan, India, Indonesia
and Thailand) showed that only 2-5% of
neonatal tetanus cases in 1980-81 were notified
(WHO 1982). This estimate was based on the
number of deaths from neonatal tetanus in the
various countries and the total number of
reported cases. The low percentage of notifica
tions may also be due to people not seeking
medical treatment at all because of poor ac
cessibility to health services. However, a study in
the Philippines in 1980-81 found that 85% of
polio cases were seen by medical practitioners
during the acute phase, but only 12% of cases
were notified (WHO 1981a). Whether a correct
diagnosis was made by the medical practitioners
during the initial consultation was not reported.
Under-reporting of notifiable diseases is also
faced by health authorities in developed coun
tries. In the USA, for example, a study of
discharge records in 11 hospitals in Washington
DC revealed that only 35% of selected notifiable
diseases were officially reported (WHO 1982). In
the Netherlands, it was estimated that oniy 3'ro
of measles cases were reported by general practi
tioners (WHO 1981b). Clarkson and Fine (1985)
estimated that 4O-6O(ro of measles cases and only
5—25% of pertussis infections were notified in
England and Wales in the period 1957-1980.
Although the various studies reviewed here
remonstrated under-reporting of notifiable
diseases, none has shown concrete evidence that
medical practitioners are wholly responsible for
this, even though they are required to notify
once they are suspicious or have diagnosed a
notifiable disease (Galbraith 1990). Several
events must occur before correct notification by
a medical practitioner is made: 1) the infected in
dividual must suffer some clinical disease; 2) the
parent must be seen by a medical practitioner; 3)
the practitioner must make a correct diagnosis
and then notify the case (Clarkson and Fine,
1985). The first two steps are beyond the control
of medical practitioners. However, Konowitz et
al. (1984) found that medical practitioners in the
USA failed to report notifiable diseases despite
making the diagnosis. They found that some
practitioners did not know which diseases should
be reported, others assumed that the laboratory
workers would notify the case. Practitioners
may also fear that notification will affect their
345
I
patient’s confidentiality and may violate the
doctor-patient relationship (Rothenberg et al.
1980; Clere et al. 1967).
Lack of uniformity in case definition also leads
to confusion among medical practitioners as to
whether or not to notify. For example, in some
states in the USA, Salmonellosis infections are
required to be notified if culture results are
positive; in other states, notifications are re
quired only when culture results are positive and
the individual is symptomatic (Chorba et al.
1989).
Kirsch and Harvey (1994) suggested that private
physicians failed to notify cases because it was
time consuming, and because of lack of reward,
feedback and supervision. Nevertheless, as with
all the literature reviewed earlier, there was no
evidence that private practitioners were any
worse than those in the public sector in disease
notification.
Various ways to improve notification rates
have been reported, such as sending stamped
reporting forms to practitioners (Hall and
Douglas 1976), actively telephoning practitioners
(Rothenberg et al. 1980; Weiss et al. 1988; Vogt
et al. 1983), sending them feedback (Spenser and
Warren 1979) and paying them (McCormick
1987). Except for actively telephoning practi
tioners, all the other methods failed to increase
the notification rates significantly. In developing
countries, efforts to encourage notification and
problems facing medical practitioners in disease
notification have not been reported.
-r
•r.
1
to
I
h': .
.■
■ w
•s
1
Conclusion
n
Medically qualified for-profit private practi
tioners have been the main focus of this paper.
There is evidence to show that private practi
tioners are important health care providers :n
many Asian countries, e\en in rural areas. Ex
isting literature shows that patient characteristics
(socioeconomic status, ethnicity, age, gender,
source of finance), types of illnesses and
characteristics of the service (geographical ac
cessibility, quality of care, price and types of ser
vices offered) influence the relative utilization of
public and private health care.
W--
s
Very little information is available on interac
tions between public and private providers. In
u&ii
..... IfcB
346
"r:;
i -
i
-/■’
■WW^•j
• ■;
most developing countries, regulations on the
private health sector are either absent or poorly
enforced. An influx of human resources trained
at the public expense into the private sector is
common in developing countries. Mandatory
public service, payment of non-private:practice
allowances, a requirement to seek permission to
work in the private sector, are among the means
governments have used to seek to retain health
personnel in the public sector. When private
practitioners are primary care providers, they
may interact with public providers through the
referral system. In communicable disease
surveillance, public and private providers may
interact through disease notification.
In all these areas, research is required to docu
ment and analyze existing interactions if policies
are to be developed which identify the ap
propriate role of private practitioners and en
courage good quality, cost-effective care in the
private sector.
WO
■:
Syed Aljunid
References
Abu-Zeid HA, Dann WM. 1985. Health services utilization
and cost in Ismaiiia, Egypt. Social Science and Medicine
21(4): 451-61.
Ahmad SR, Bhutta ZA. 1990. a survey of paediatric
prescribing and dispensing in Karachi. Journal of
Pakistan Medical Association June: 126-30
Ainsworth M. 1983. The demand for health and schooling in
Mali: Results of community and service provider survev.
'Acrid Bank Discussion Paper 1983-', Washington DC.
In: World Bank. 1987. Financing health services in
developing countries. An agenda for reform. Washington
DC: World Bank.
Akin JS. Griffin CC. Guilkey DK. Popkin BM. 1986. The
demand tor adult outpatient services in the Bicol region
of the Philippines. Social Science and Medicine 22(3):
321-8.
Aljunid SM, Norhassim I. 1992. Utilization of health
facilities by the Malays of Kuala Selangor. Journal of
UKM Medical Faculty 14(1): 43-52.
Amin R, Chowdhury SA, Kamal GM, Chowdhury J. 1989.
Community health services and health care utilization in
rural Bangladesh. Social Science and Medicine 29(12):
1343-9.
Annis S. 1981. Physical access and utilization of health ser
vices in rural Guatemala. Social Science and Medicine
15(D): 515-23.
Attah EB. 1986. Underutilization of public sector health
facilities in Imo State, Nigeria. World Bank PHN
Technical Note Series No. 86-1. Washington DC: World
Bank.
Belmartino S. 1994. The role of the state in the health
systems. Social Science and Medicine 39(9): 1315-21.
Bennett S. 1991. The mystique of markets: Public and private
health care in developing countries. PHP Departmental
.< -
Publication No. 4. London: London School of Hygiene
and Tropical Medicine.
Bennett S, Tangcharoensathien V. 1994. A shrinking state?
Politics, economics and private health care in Thailand.
Public Administration and Development 14: 1-17.
Bennett S, Tangcharoensathien V. 1993. Health insurance
and private providers: a study of the civil servants’
medical benefit scheme in Bangkok, Thailand. Interna
tional Journal of Health Planning and Management 8:
137-52.
Benyoussef A, Wessen AF. 1974. Utilization of health ser
vices in developing countries — Tunisia. Social Science
and Medicine 8(5): 287-304.
Berman P, Ormond BA, Gani S. 1987. Treatment use and
expenditure on curative care in rural Indonesia. Health
Policy and Planning 2(4): 289-300.
Bethune XP, Alfani S, Lahaye J. 1989. The influence of an
abrupt price increase on health service utilization:
evidence from Zaire. Health Policv and Planning 4( 1);
"6-81.
Bhat R. 1991. The private health care sector in India: some
policy concerns. Research Paper No. 54, Takemi Pro
gram in International Health. Boston: Harvard School of
Public Health.
Bhat R. 1993. The public/private mix in health care in India.
Health Policy and Planning 8(1): 43-56.
Brotowasisto. Gish O. Malik R, Sudharto P. 1988. Health
care financing in Indonesia. Health Policv and Planning
3(2): 131-40.
Chorba TL, Berkelman RL. Safford SK. Gibbs NP. Hull
HF. 1989. Mandatory reporting of infectious diseases ny
clinicians. Journal of American Medical Association
262(2;): 3016-26.
Claquin P. 1981. Private health care providers in rural
Bangladesh. Social Science and Medicine 15(B): 153-'.
Clarkson JA, Fine PEM. 1985. The efficiency of measles and
pertussis notification in England and Wales. Interna
tional Journal of Epidemiology 14(1): 153-68.
Cere RL. Dougherty WJ. Fiumara N.J. Jemke C. Lentz IW,
Rose NJ. 1967. Physicians' attitude towards venereal
diseases reporting. Journal of American Medical Associa
tion 2O2( 10): i l"-22.
Colson AC. !9‘T1. The differential use of medical resources in
developing countries. Journal of Health and Social
Behaviour 12(3): 226-37.
Cortinovis I, Vella, V, Ndiku J. 1993. Construction of socio
economic index to facilitate analysis of health data in
developing countries. Social Science and Medicine 36(8):
1087-9'.
Creed F, Gowrisunkur J, Russell E, Kincey J. 1990. General
practitioner referral rates to district psychiatry and
psychology services. British Journal of General Practice
40(340): 450-4.
Diong KI. 1988. Services in general practice. The Family
Practitioner 22(1 £2): 56-9.
Doeleman F. 1987. Improving communication between
general practitioners and specialists. Familv Practice 4(3):
1'6-82.
Duggal R, Amin S. 1989. Cost of health care: a household
survey in an Indian District. The foundation for research
in community health, Bombay. In: Bhat R. 1991. The
private health care sector in India: some policy concerns.
Research Paper No. 54, Takemi Program in International
Health. Boston: Harvard School of Public Health.
••■
'
'
'■•■.•<-•<
■..
■
-
■<-.
.
-
’____I
Private practitioners and public health services
Dutton D. 1986. Financial, organizational and professional
factors affecting health care utilization. Social Science
and Medicine 23(7): 721-35.
Dye TD, Lee RV. 1994. Socio-economic status: developing a
quantitative, community based index in rural Kashmir.
Journal of Epidemiology and Community Health 48(4):
Economic Planning Unit, Malaysia. 1985. Malavsia health
services financing study report. Kuala’ Lumpur:
Economic Planning Unit.
Feldman S. 1983. The use of private health care providers in
rural Bangladesh: A response to Claquin. Social Science
ana Medicine 17(23): 1887-96.
Fieuier JL. 1981.
review of literature on access and
utilization of medical care with special emphasis on rural
primary care, iociat Science and Medicine 15(C): 129-42.
Fitzpatrick R. 1991. Surveys of patient satisfaction:
1 — Important general considerations. British Medial
Journal 302: 887-9.
Fong NP. Phua KH. 1985. Utilization and expenditure on
neuical services in a local community. Singapore Medical
Journal 26(2): 131-8.
Fooie SB. i986. Coexistence, conflict and cooperation:
public policies toward medical devices. Journal of Health
Politics. Poiicv and Law 11(3): 501-23.
Gaibraith NS. 1990. Infectious disease control. British
Medical Journal 300: 1477-8.
Gar. ; . Yusof K. 1993. Utilization of maternal and chiid
Health facilities by the urban poor of Kuala Lumpur.
South-East Asian Journal of Tropical Medicine and
Puoiic Health 24i2): 302-6.
Garner P. Thaver I. 1993. Urban slums and primary health
care: :he orr-ate doctor's role. British Medical Journal
306: do?.
Gilson L. 1988. Government health care charges: Is equity
being abandoned? Evaluation and Planning Centre for
Health Care Publication No. 15. London: London School
of Hygiene and Tropical Medicine.
•mison L. Aiiiio M, Heggenhougen K. 1994. Community
satisfaction with primary health care services: an evalua
tion undertaken -n the Morogoro region of Tanzania.
Suciat Science ana Medicine 39(6): "67-80.
Gilson L. Jaffar S. Mwankusye S. Teuscher T. 1993. \sses.^ing prescribing practice: A Tanzanian example. Interna
tional Journal of Health Planning and Management 8:
37-58.
Gish O. Malek R. Sudharto P. 1988. Who gets what? Utiliza
tion of health services in Indonesia. International Journal
oj Health Planning and Management 3: 185-96.
Grace JF. Armstrong D. 1987. Referral to hospital: percep
tions of patients, general practitioners and consultants
about necessity and suitability of referral. Familv Practice
4(3): 170-5.
Grace JF. Armstrong D. 1986. Referral co hospital: extent of
agreement between the perceptions of patients, general
practitioners and consultants. Family Practice 3(3): 143-7
Green A. 1987. The role of non-governmental organizations
and the private sector in the provision of health care in
developing countries. International Journal of Health
Planning and Management 2: 37-58.
Greenhalgh T. 1987. Drug prescription and self-medication
m India: An exploratory survey: Social Science and
Medicine 3: 307-18.
S.7^
347
Griffin CC, Paqueo VB. 1993. The development, growth and
distribution of public and private medical resources in
Philippines. In: Mills A, Lee K (eds). 1993. Health
economics research in developing countries. Oxford: Ox
ford University Press.
Griffin CC.19S9. Strengthening health services in developing
countries through the private sector. International
Finance Corporation Discussion paper No. 4. World
Bank. Washington DC.
Habib OS. Vaughan JP. 1986. The determinants of health
services utilization in Southern Iraq: a households inter
view survey. International Journal of Epidemiology
15(3): 395-103.
Haddad S, Fournier P. 1995. Quality, cost and utilization of
health services in developing eountries. A longitudinal
study m Zaire. Social Science and Medicine 40(6): "43-53.
Hall CB, Douglas RG. 1976. Respiratory syncytial virus and
influenza: practical community surveillance. American
Journal of Disease of Childhood 130: 615-20.
Haynes RM. Bentham CG. 1982. The effects of accessibility
on general practitioner consultations, out-patient atten
dances and in-patient admissions in Norfolk. England.
Social Science and Medicine 16: 561-69.
Heggenhougen HK. 1979. Altitudes on health care of vil
lagers attending a rural clinic in Malaysia. Medical Jour
nal oj Malaysia XXXIV (2): 108-15.
Heller PS. 1982. A model of the demand for medical and
neatth services in Peninsular Xlaiaysia. Social Science and
Medicine 16(3): 267-84.
Heller PL, Chalfant HP. Queseda GM. Rivera-Worley MC.
1981. Class, familism and utilization of health services in
Durango, Mexico: a replication. Social Science and
Medicine 15(A): 539-41.
Hilleir S. Zheng X. 1990. Privatisation of care in China.
Lancet 335(8686): 414.
Hillman BJ, Joseph CA. Mabry MR. Sunshine JH, Kennedy
SD. Noether M. 1990. Frequency and costs of diagnostic
imaging in office practice — a comparison of self'eferring and radiologist-referring physicians. The .\ew
England Journal of Medicine 323(23): 1604-8.
Hchgoro C. Chandiwana SK. 1994. The effects of ne ntorcement of user fees on me aealm care delivery -.vsiem
:n Zimbabwe. Report of a ■4udy financed oy UNICEF.
Ministry of Health and Child Welfare. Harare.
Hoot LN. IQ94. Case finding for pulmonary tuberculosis in
Penang. Malaysian Medical Journal 49(3): 223-30.
Jones NP, Lloyds IC. Kwartz J. 1990. General practitioner
referrals to an eye hospital: a standard referral form.
Journal of the Royal Society of Medicine 83: 770-2.
Joseph EA. Bantock PR. 1982. Measuring potential physical
accessibility to general practitioners in rural areas. Social
Science and Medicine 16(1): 85-90.
Kirsch TD, Harvey M. 1994. A role for the private sector in
poliomyelitis surveillance.
240-3.
World Health Forum
11
1i
I
7
11
■i
I
J
;f|
$ SH
i
15-
Kloos H, Elea A. Degefa A et al. 1987. Illness and health
behaviour in Adis Ababa and rural Central Ethiopia.
Social Science and Medicine 25(9): 1003-19.
Kolehmainen-Aitken RL, Modia P. Marjen C. 1990. A
survey of Papua New Guinea medical practitioners.
Papua Hew Guinea Medical Journal 33: 12-22.
Konowitz PM. Petrossian GA. Rose DN. 1984. The under
reporting of disease and physicians' knowledge of repor
ting requirements. Public Health Report 99(1): 31-5.
. Si
'
I £' -
348
If < c-y
<■ '1
I
te^i-
Syed Aljunid
Kroeger A. 1983. Anthropological and socio-medical health
care research in developing countries. Social Science and
Medicine 17(3): 147-61.
Lachman PI, Stander IA. 1991. The referral letter — a prob
lem of communication. South African Medical Journal
79(19): 98-100.
Leopando ZE. 1988. A study of family physicians in the
Philippines. The Filipino Familv Physician XXVI(4):
23-32.
Lim TO. 1991. Content of general practice. Medical Journal
of Malaysia 46(2): 155-62.
London K. Cushing J. Rutstein S et al. 1985. Fertility and
family planning surveys: an update. Population Reports,
Series M, No 8. Population Information Program. The
John Hopkins University Press. Baltimore. In: Lapham
RJ. Simmons GB (eds). 1985. Organizing for effective
family planning programs. Washington DC: National
Academy Press.
Malaysian Medical Association. 1991. Berita MMA 23(5):
September.
Malaysian Medical Association. 1993. Berita MMA 25(7):
December.
McCormick A. 1987. Notification of infect ious disease: the
effect of increasing the fee paid. Health Trends 19: 7-8.
McPake B. 1993. User charges for health services in develop
ing countries: a review of the economic literature. Social
Science and Medicine 36(11): 1397-405.
Ming HT. 1982. General practice today: a profession in
disarray. The Family Practitioner 5( 1): >9-101.
Ministry of Health Malaysia. 1988a. national health and
morbidity survey 1986-87. Overview of findings and
recommendations. Kuala Lumpur: Ministry of Health.
Ministry of Health Malaysia. 1988b. Review of :he Fifth
Malaysia Plan: towards the preparation of the Sixth
Malaysia Plan. Kuala Lumpur: Ministry of Health.
MMA: see Malaysian Medical Association.
MOH: see Ministry of Health.
Moses S, Manji F. Bradley JE. Nagelkerke NJD. Malisa MA.
Plummer FA. 1992. Impact of user fees ?n attendance at
a referral centre lor sexually transmitted diseases in
Kenya. Lancet 340: 463-6.
Mugo-Gachuhi. 1977. The role of private medical practi
tioners in provision ot family planning. Surgical con
traception in Sub-Saharan Africa. Proceedings of a con
ference. In: Tsui AO, Donaldson PJ. 1987. The role of
private physicians and clinics in third world family plann
ing. In: Lapham RJ, Simmons GB. ^S7. Organizing for
effective family planning programs. Washington DC:
National Academy Press.
Mujinja PGM, Urassa D, Mnyika KS. 1993. The Tanzanian
public/private mix in national health care. In: Bennett S.
Mills A. 1993. Proceedings from the workshop on the
public/private mix tor health care in developing coun
tries, Health Policy Unit Report, 1993. London: London
School ot Hygiene and Tropical Medicine.
Mwabu GM. 1986. Health care decisions at the household
level: results of a rural health survey in Kenya. Social
Science and Medicine 22(3): 315-19.
New Sunday Times. 1993. Lee: Register nursing aides too.
21 March 1993. Kuala Lumpur, Malaysia.
Ngalande-Banda E, Walt G. 1995. The private health sector
in Malawi: opening pandora’s box? Journal of Interna
tional Development. In press.
Nichter M. 1980. Health expenditure report. USAID
(Mimeo), New Delhi. In: Bhat R. 1991. The private health
care sector in India: some policy concerns. Research
Paper No. 54. Takemi Program in International Health.
Boston: Harvard School of Public Health.
Pascoe GC. 1983. Patient satisfaction in primary health care:
a literature review and analysis. Evaluation and Program
Planning 6: 185-210.
Poland BD, Taylor SM, Hayes MV. 1990. The ecology of
health services utilization in Granada, West Indies. Social
Science and Medicine 30(1): 13-24.
Ramachandran H, Shastri GS. 1983. Movements for medical
treatment. Social Science and Medicine 17(3): 177-87.
Roemer MI. 1984. Private medical practice: obstacle to
health for all. World Health Forum 5: 195-210.
Roemer MI. 1991. Motional health system of the world.
Volume I: The countries. New York: Oxford University
Press.
Roemer Ml. Roemer JE. 1982. The social consequences of
free trade in health care: a public health response to or
thodox economics. International Journal of Health Ser
vices 12(1): 111-29.
Ron A, Abel-Smith B, Tamburi G. 1991. Health insurance in
developing countries: the social security approach.
Geneva: International Labour Office.
Rothenberg R, Bross DC, Vernon TM. 1980. Reporting of
gonorrhoea by private physicians: a behavioral study.
Journal of American Medical Association 70(9): 983-86.
Sarder AM, Chen LC. 1981. Distribution and characteristics
ot non-government health practitioners in a rural area of
Bangladesh. Social Science and Medicine 15(A): 543-50.
Schulpen TWJ, Swinkels WJ. 1980. Machakos project
studies XIX. The utilization of health services in a rural
area or Kenya. Tropical Geographical Medicine 32:
340-9.
Senior PA, Bhopal R. 1994. Ethnicity as a variable in
epidemiological research. British Medical Journal 309:
327-30.
Smith HE. 1982. Doctors and society: a Northern Thailand
study. Social Science and Medicine 16: 515-26.
Spenser L, 'Aarren GR. 19~9. New reporting system aids
epidemiologist. Hospitals 53: 105-6. In: K.m.iwitz PM.
Petrossian GA. Rose DN. 1984. The under-reporting of
disease and physicians' knowledge of reporting re
quirements. Public Health Report 99(1): 31-5.
Stock R. 1983. Distance and utilization of health facilities
in rural Nigeria. Social Science and Medicine 17(9):
563-"0.
The Star. 1992. Government docs can’t work part-time. 11
November 1992. Kuala Lumpur, Malaysia.
Tsui AO, Donaldson PJ. 1987. The role of private physician
and clinics in third world family planning. In: Lapham
RJ. Simmons GB (eds). Organizing for effective family
planning programs. Washington DC: National AcademyPress.
Uplekar MW, Cash RA. 1991. The private GP and leprosy: a
study. Leprosy Review 62: 410-9.
Uplekar MW, Shepard DS. 1991. Treatment of tuberculosis
by private general practitioners in India. Tubercle 72:
284-90.
Visvanathan H, Rohde JE. 1990. Diarrhoea in rural India: A
nationwide study of mothers and practitioners. Vision
Books, New Delhi. In: Bhat R, 1991. The private health
care sector in India: some policy concerns. Research
Paper No. 54, Takemi Program in International Health.
Boston: Harvard School of Public Health.
——
■ ...A x-x;; a,;-;.. .
.M'M xx-
'
;.
? ii'.'j ■' . ' '
x'-txx\<'.T
•..>/>
; .
■
■'
■
•
...
:
'
'■
A
Srt?
If
;rfA.A/-..A<.
'.<x-A
■j
,r.
jA_____________
■" •
I
Private practitioners and public health services
Vogt RL. LaRue D, Klaucke DN, Jillson DA. 1983. Com
parison of an active and passive surveillance system of
primary care providers for hepatitis, measles, rubella and
salmonellosis in Vermont. American Journal of Public
Health 73(7): ’95-7.
Walt KM. 1977. The illness no longer understand: changing
concepts of health and curing in a rural Mexican com
munity. Medical Anthropology Newsletter 8: 5-11. In:
Kroeger A. 1983. Anthropological and socio-medicai
health care research in developing countries. Social
Science and Medicine 17(3): 147-61.’
Weiss BP. Strassburg MA. Fannin SL. 1988. Improving
disease reporting in Los Angeles Countv: trial and results
Public Health R9p^ts 103(4); 415-2!
Westerman RF. Hull FM. Bezember Pd’ Gort G. 1990. A
study of communication between general practitioners
and specialists. British Journal uf General Pracice
40(3-10): 445-9.
WHO. 1981a. Expanded programme^n immunisation: poiiomveutis prevalence surveys. UeeATv Epidemiological
Record 56(48): 3 7’-84.
WHO. 1981b. Expanded programme on immunisation: rhe
nc:dence of live vaccine preventable diseases and im
munization coverage. Weekly Epidemiological Record
?6(4,): 369-'6.
Wr/j. 1982. Expanded programme on immunisation: the
use ot survey data to supplement disease surveillance.
Weekly Epidemiological Record 57(a'">: 361-68.
W.nulpolpraset S. 1991a. Community financing: Thaiianu’,
"■■mer-.ence. Health Policy and Planning 6(4)- 3^4-60
'A ibmpoipraset S. 19u!b. Health statu>. leaith poiicv objecnves. health services infrastructure and utilization n
■ ••Jiianu. unpubli'hed report.
Vi.uams B. 1994. Patient satisfaction: A
A valid concent?
Scciai Science and Medicine 38(4;: 'Po.
--:6.
W-. rla Bank. 198’. Financing health ■e-'.-ice^ n leceionmg
•oun tries. An agenda j or reform. Washington DC World
□a n k.
World Bank. 1993. World Development Report 1993
Investing in Health. Washington DC: World Bank.
349
Wyatt HV. 1992. Mothers, iinjections
J '______
and poliomyelitis.
Social Science and Medicine 35(6): 795-98.
Yang BM. 1993. Medical technology and inequity in health
’8^'9^ CaSe
K°rea’
Policy and Planning 8(4):
I
i
J
> .J
t-y
A
■
I
Yesudian CAK. 1994. Behaviour of the private sector in rhe
health market of Bombay. Heairh Poiicv and Planning
9(1): 72-80.
'
S
Yoder RA. 1989. Are people willing and able to pay for
health services? Social Science and Medicine 29( 1): 35-42
A -
*
p ■ w
F'A
A
Acknowledgements
The author would like to thank Anthony Zwj and Gill Walt
!‘or their valuable comments on earlier drafts of this paper
This rev<ew is based on a study of the role of private practi
tioners .n rural districts of Malaysia and their interactions
with public health services, funded by Lniversiti Kebangsaan
Malaysia and the Health Economics and Financing Pro
gramme. London School of Hygiene & Tropical Medicine.
■ ne Health Economics and Financing Programme is sup
ported by the Overseas Development Administration (LK)
-•
Bxa.
3
ft'h;A
x-
AM
i
: F
?:
' 1'
i
ft'
Biography
Sved Aijunid. MD. MSc (Public Health), is a oublic health
specialist and lecturer in the Department of Community
Health. Lniversiti Kebangsaan Malaysia. His research in
terest is in the role ot private medical practitioners and health
■ector reform :n devclooing countries. He has recently com
pleted his PhD in the Health Economics and Financing Pro
gramme. London <cnool of.’•> giene and frcpical Medicine.
A,
i
I
Correspondence-. Dr Syed Aijunid. Department of Com
munity Health, Universiti Kebangsaan Malaysia, 50300 Jalan
Raia Muda Musa. Kuala Lumpur. Malaysia.
if
r •
..'di
I
J
^>3
http://bmj .com/cgi/content/full/30. . .te= 1/1/1965&tdate=6/30/2002&jc=al I
bmj.com Smith 309 (6962): 1168
Com h
Home
Help
Search/Archive
Feedback
.
Search Result
BMJ 1994:309:1168 (29 October)
Views and reviews
Autumn books: The Fight for Public Health:
Principles and Practice of Media Advocacy
Simon Chapman, Deborah Lupton BMJ Publishing Group, pounds
sterling 19.95, pp 270 ISBN 0-7279-0849-9
Email this article to a friend
Respond to this article
Download to Citation Manager
Search Medline for articles by:
Smith. G D
Alert me when:
New articles cite this article
How do you translate the findings of epidemiological studies into policies that actually improve
population health? Chapman and Lupton's ambitious efforts to "examine both the why and how of the
ways that particular public health issues become prominent and politically actionable in an issue-rich
political and news environment" should greatly help. Their strategy is "media advocacy" - the use of
mass media to influence public, health policy. Through many case studies, mostly concerning smoking,
the prevention of accidents, and gun control in Australia, they show how creative use of the media can
play an important part in public health campaigns.
There are, of course, powerful forces opposing the potentially positive effects of media coverage of
health issues. Not least of these is the economic clout of the manufacturers of health damaging products.
Threats by tobacco companies to pull advertising from magazines will influence the decision to publish
articles about the damaging consequences of smoking.
Rich corporations can simply buy plenty of media space for their efforts to confuse what are essentially
straightforward facts, such as that smoking shortens average life expectancy by several years and (more
obviously still) guns are used to kill people. Even more cheaply, a rather sad list of’’experts" can be
found who will cloud these issues on television or in print. The fact that the central social dynamic of
capital is that it is required to make more capital, whatever the consequences, aids the process.
The intrinsic processes of producing news can also act against the goals of public health. It is
newsworthy when a few children have apparently been harmed by vaccinations, while the prevention of
epidemic childhood diseases, in part by immunisation programmes, receives no coverage at all.
Uncommon diseases, of low public health importance, receive an inordinate amount of media attention,
while the toll from common conditions is, by definition, simply not news. High technology medical
breakthroughs, applicable to relatively few people, will produce a better story than the workaday
activities of disease prevention.
The ways in which it is possible to win against vested interests within the constraints of how the media
operate are illustrated extensively in the book's main section, "The A-Z of public health advocacy."
BUGA UP (Billboard Utilising Graffitists Against Unhealthy Promotions) simply changed the messages
of posters paid for by the tobacco companies. Thus "Have a Winfield" was changed to "Have a Wank if s healthier," the Benson and Hedges slogan "Gold is the perfect mixer" to "Cancer is the perfect fixer,"
and "Marlboro" to "It’s a bore." Strategic research can also be used, as was recently shown in Britain by
the killing of the "Reg" campaign for Regal cigarettes through a study showing how this appealed
particularly to children, against the voluntary code governing tobacco advertising.
1 of2
6/20/02 2:15 PM
bmj.com Smith 309 (6962): 1168
http://bmj.com/cgi/content/full/30... te= 1/1/1965&tdate-6/30/2002&jc all
As well as these high profile activities, more routine methods of optimising media coverage are given.
Good interview technique, the use of press releases, the incorporation of props to grab attention, and the
involvement of celebrities are discussed.
The only disappointing aspects of the book relate to issues that may be considered outside its intended
scope but that should at least be acknowledged. Firstly, there is no discussion of evaluating whether
campaigns are successful in the final aim of improving public health. Indeed, John Snow's removal of
the handle from the Broad Street pump and hence his stemming of London’s cholera epidemic is yet
again given as an example of successful public health practice. The epidemic was, however,
disappearing, and Snow's action probably had little if any influence even though it would have provided
a wonderful photo opportunity. The same may be the case today, and some campaigns could be
successful at getting television coverage but have no influence on health outcomes. Secondly, little
attention is paid to the views of the public. A detailed analysis of the often complex ways in which
health and disease are popularly conceptualised should be at least as important an aspect of public health
advocacy as knowing the fax numbers of a pack ofjournalists.
The limited impact of conventional health education is shown by the high regard in which it is held by
the tobacco companies. A Rothman’s spokesperson wrote of "fully supporting sensible and effective
public education," and others wrote that "the industry wholeheartedly supported any sensible campaign
to discourage school children from smoking." Teaching of health promotion often emphasises that
simple educational activities have little effect, without offering any real alternatives. The Fight for Public
Health shows that feasible alternatives exist and can even be fun.
G D Smith
Email this article to a friend
Respond to this article
Download to Citation Manager
Search Medline for articles by:
Smith, G D
Alert me when:
New articles cite this article
Home
2 of 2
Search Result
6/20/02 2:15 PM
Corv) H -
6
HEALTH POLICY AND PLANNING; 12(4): 296-311
. 66^
© Oxford University Press 1997
Reform follows failure:
I. Unregulated private care in Lebanon
W VAN LERBERGHE,1 W AMMAR,2 R EL RASHIDI,3 A SALES,3 AND A MECHBAL4
'Department of Public Health, Institute for Tropical Medicine, Antwerp, Belgium, Ministry of Health,
Republic of Lebanon, 3The World Bank, Washington DC, and 4World Health Organization, Beirut,
Lebanon
This first of two papers on the health sector in Lebanon describes how unregulated development of
private care quickly led to a crisis situation. Following the civil war the health care sector in Lebanon
is characterized by (i) ambulatory care provided by private practitioners working as individual entre
preneurs, and, to a small extent, by NGO health centres; and (ii) by a fast increase in hi-tech private
hospitals. The latter is fuelled by unregulated purchase of hospital care by the Ministry of Health and
public insurance schemes. Health expenditure and financing patterns are described. The position of
the public sector in this context is analyzed. In Lebanon unregulated private care has resulted in major
inefficiencies, distortion of the health care system, the creation of a culture that is oriented to secondary
care and technology, and a non-sustainable cost explosion. Betvyeen 1991 and 1995 this led to a financ
ing and organizational crisis that is the background for growing pressure for reform.
Introduction
Many European countries have been or are presently
going through a process of reform of the health care
sector. The impetus for such reform comes from the
inability to control costs, criticism of bureaucratic
rigidity, and the impression of getting poor value for
money (Dekker 1994). Most attention goes to the
supply side, and the reform debate is dominated by
a focus on administrative/financial and organizational
issues (Oevretveit 1994). There is a characteristic
shift towards market-derived incentives in pursuit of
micro-economic efficiency (Saltman 1994) and con
trol of expenditure.
Developing countries are increasingly interested in
following similar approaches in order to control costs,
but also, and this is much more a central issue than
in Europe, in order to correct obvious government
failures in financing and provision of health care
(World Bank 1993). As in Europe, reliance on the
private sector and managed markets is supposed to
enhance provider efficiency through competition and
the substitution of direct management with contrac
tual relationships.
A growing number of developing countries are now
embarking on reforms in which contracting out
clinical services - and specifically hospital care - is
a key element. The speed with which these ap
proaches have been endorsed in development circles
is in sharp contrast with the lack of actual experience
and empirical evidence for success (Carr-Hill 1994).
The do’s and don’ts, the approaches that work and
those that do not, have not been clearly identified in
the industrialized world (Petchey 1995; Saltman
1994), let alone in developing countries. What little
evidence there is to date indicates that in developing
countries the conditions for successful introduction
of such reforms are often not in place (Broomberg
1994). Appropriate regulation technologies and
capacities need to be developed. Reforming the health
care sector in developing countries is indeed subject
to specific constraints that centre around the govern
ment’s regulatory capacity and the strength of its
Health sector reform in Lebanon. I.
bargaining position (McPake and Hongoro 1995). If
ultimately reform has to be evidence-based, documen
tation of present pragmatic efforts is essential.
In most developing countries the original impetus for
health care reform comes from a reaction to the
government’s failure to deliver health care, combined
with a crisis in the financing of the health sector.
Scaling down public delivery of services and the
introduction of private sector competition in the pro
vision of health care with retention of public financ
ing is usually seen as the way to address public sector
inefficiencies whilst retaining a tool for ensuring
equity (Birdsall and James 1992). Privatization is fur
ther to be seen in an ideological context of shift from
welfarism to monetarist macro-economics (Price
1989) but, as in the industrialized world, the debate
is now moving from ideological positioning to opera
tional questions (Belmartino 1994). In practice,
reform mainly addresses urban health care systems
where it focuses on introducing purchaser-provider
splits so as to induce supply-side efficiency through
competition, whilst keeping the State in a monopsonistic power position.
297
sector. It shows that public financing per se, without
the institutional capacity and proper attention for the
mechanics of regulation, does not provide sufficient
leverage to avoid predictable market failures.
Although the staring point for the Lebanese health
care reform is different from most other developing
countries engaging in reform (down-scaling public
care provision is not an issue), the question of the
regulation of a partly publicly financed private sec
tor is of wider relevance.
Lacking regulatory authority - and essential reliable
information - the Ministry of Health (MOH) was
forced to adopt a reform strategy wherein the prob
lems of financing of the health sector are not dealt
with head-on. Tackling the organizational problems
of health care delivery first provided an opportunity
for building up alliances and pressure that should
allow it to tackle finance at a later stage. A second
paper documents the way pressure for reform has
built up, and identifies the key elements on the reform
agenda (Van Lerberghe et al. 1997).
Health care delivery and the civil war
In Lebanon the impetus for health care reform also
starts from the recognition of an unchecked growth
of expenses for medical care. In contrast with many
developing countries, however, it is not a reaction
against the government’s inefficiency in delivering
services. In Lebanon, indeed, the State has only a
marginal role in delivering health care, and a
purchaser-provider split exists de facto. Both am
bulatory and hospital care are almost exclusively
private. Ambulatory care is essentially provided
through private clinics financed through out-of-pocket
payments. Hospital care is provided through (small)
private (for-profit and not-for-profit) hospitals. For
about half of the population, hospital care is covered
by private or public insurance schemes. For the rest
of the population, it is purchased by the State. Private
hospitals are thus heavily dependent on public fund
ing. This arrangement has proven highly inefficient,
the absence of self-regulation of the private svstem
being compounded by the absence of adequate public
sector regulatory mechanisms and capacities.
This first paper documents how, in a very short
time-span, unregulated privatization has created an
inefficient and distoned health care system, and a
non-sustainable cost explosion. The Lebanese case
illustrates the strategic importance of the regulation,
planning and policy setting functions of the public
Once a prosperous, upper-middle-income country,
Lebanon declined during the war of 1975-1990.
About one-quarter of the population emigrated dur
ing these 15 years. A 1992 study, two years after the
end of the war, classified 450 000 individuals as
displaced (Feghali 1992). This is a very large number
considering the relatively small population of the
country-approximately 3 million. Reliable demo
graphic figures are politically sensitive and hard to
come by: the last population census in Lebanon dates
back to 1932. Furthermore there are some 900 000-1
200 000 Unregistered foreign workers (mainly from
Syria), and some 400 000 Palestinian refugees.
Economic activity is picking up fast again following
the cessation of internal fighting, and GDP increased
from around USS 1500 in 1992 to around USS2300
in 1994 (different sources mention different figures).
In real terms, however, the per capita income is still
below the pre-war level.
The war was a period of an accelerated urbanization:
85 % of the population now lives in towns. It was also
a period of demographic and epidemiological transi
tion. Only 9.6% of the population is younger than
five years, as opposed to the 12-13% that is com
mon in the region. Infant mortality increased from
48 per 1000 in 1975 to 57 in the middle of the war.
but then dropped to 44 in 1990. By 1992 it was down
298
W Van Lerberghe et al.
to 34, concentrated in a limited number of areas.
Preliminary results of the 1996 PAP-Child survey
show an infant mortality rate (IMR) of 28 per 1000.
Infectious and parasitic diseases are on the decline.
The pattern of demand for care is now dominated by
chronic diseases and problems related to the urban
environment. For example, the most consistent find
ing in an analysis of the reasons for encounter in
health centres in Lebanon was the high frequency of
diagnosis and treatment of hypenension and diabetes
(Adib 1994).
With a culture of trade and commerce, and delicate
religious and denominational balancing acts that
determine politics and administration, Lebanon has
a strong tradition of individualism, self-reliance and
private initiative. The private sector - with privatefor-profit (PFP) and community-linked not-for-profit
non-governmental organizations (NFP-NGO) dominates in most fields, including health and educa
tion. Although traditionally considered reasonably
competent, effective and even an attractive career
possibility, public administration in Lebanon has
never played a dominant role in the health sector.
Public services in Lebanon were severely affected and
weakened by the war (Kronfol and Bashshur 1989).
Buildings and equipment were destroyed, looted or
damaged. Trained and capable people left the country
(Kronfol et al. 1992), whilst those who stayed had
to struggle to survive on inadequate salaries. There
has been little opportunity for modernization of ideas,
skills or style of work. For all practical purposes, the
MOH disintegrated during the war. There was no
clear policy, no means to implement it, no informa
tion to work on. The public health programmes that
were active during the war period were donor driven
- with major roles for WHO and UNICEF - and
channelled through NGOs of various denominations.
Considering the circumstances, this proved highly ef
fective; NGOs proved to be highly flexible and able
to deliver results - 89% vaccination coverage with
an ongoing civil war. The MOH, however, had only
a marginal role in all this.
The MOH activities were limited to contracting with
private hospitals in order to deal with emergencies.
This was in fact a continuation of the policy of
contracting-out that already existed before the war,
when the government paid the bill for some 40 000
acute care hospitalizations per year in the private sec
tor. During the war, direct involvement of the MOH
in direct provision of hospital care became marginal.
By the mid-1980s, seven of the public sector hospitals
had been destroyed. At some point the public sector
could avail of only 200 beds in Beirut. The share of
the public sector in national hospital bed capacity thus
fell to less than 10% by 1984 (Anonymous 1987).
By the end of the war public hospitals had only 700
partly operational beds left of the 1870 they had in
the early 1970s.
In contrast, the private sector remained very dynamic
throughout the war. For example, 56% of the present
private hospital capacity was created during the war
years. Most of this represented development of
business opportunities by private entrepreneurs for
whom the war provided fresh investment capital.
But the war was also a period of major expansion for
NFP-NGOs. These set up a network of health centres
and dispensaries, and carried out public health pro
grammes. Lebanese and international NGOs under
took emergency programmes with the support of
donors through financial grants designated for short
term emergency aid. International NGOs expanded
from 28 to 171 services. There was also an exponen
tial growth of national NFP-NGOs. These were
mainly small-scale organizations, working in under
served rural and urban poverty pockets, with em
phasis on Beirut and Mount Lebanon. They focused
on emergency relief and humanitarian assistance,
rarely on community development work. For
example, in the mid-1980s, 43 % of their clients were
health service and 47 % relief assistance beneficiaries
(Ministry of Labour and Social Affairs and
Norwegian People’s Aid 1985). Most NFP-NGOs
depended on donations from foreign NGOs and sup
port from political panics and factions. During the
war these NGOs gained high visibility and credibility,
although many were mere propaganda machines or
even fronts for commercial organizations. After the
war, however, this credibility was not translated into
involvement in planning or policy discussions.
In summary, over the last 20 years the Lebanese
health care system has developed in a largely
unregulated way, following private initiative and in
vestment. The public sector has been absent, but the
country has a NFP-NGO health care delivery network
with a public sector logic that has been developed on
the basis of the relief operations during the war.
Ambulatory care in private clinics
Private practice has been the main source for
ambulatory medical care for the Lebanese. Roughly
Health sector reform in Lebanon. I.
299
12
10
'
8
Established
!
.. market ♦........
economies
I
6
"O
4
§
.
...................................... ■:..............................................
Middle East * Latin Amenca
tn
I
........
|
|Lebanon
Turke;
2
Syria* ;
0
Formerly L
socialist .
economies!
0
1
Jordan
2
3
Doctors /1000 inhabitants
4
5
"Lebanon ratios are given as a range to take into account uncertainties in the data
Figure 1. Doctor and hospital bed per population ratios in Lebanon and selected other countries’
NGO health centres
10%
Hospital OPD___ H
Other
3%
Private clinics
79%
Figure 2. Sources of ambulatory care
one out of five households identifies with one medical
practitioner as its 'family physician’, very much in
a West-European fashion though with less reliance
on house calls - less than 5 % of contacts are house
calls (Abyad 1994; Kronfol et al. 1985).
There is an ample supply of physicians: some 8-9000,
i.e. a ratio that comes close to three doctors per 1000
inhabitants. This is higher than most of the rest of
the world outside the formerly socialist economies
of Europe (Figure 1). The doctor/bed ratio of 0.88
is also among the highest in the world, almost three
times that of OECD countries. This relative over-
supply of doctors makes ambulatory care a natural
career perspective.
Most ambulatory care is provided in private clinics
(Figure 2). Hospital outpatient departments capture
8% and health centres, whose number increased spec
tacularly during the war, have expanded their share
to 10%. Most of these health centres are run by NFPNGOs: the few public health centres and dispensaries
offer services of poor quality and are barely used.
Health care delivery by NFP-NGOs is strategically
important since in many cases their health centres are
the only accessible option for the poor. Also, they
300
W Van Lerberghe et al.
14000
12000
I -1 Long stay beds, private
EZJ Acute beds, private
Y/A Acute beds, public
10000
8000 -
I
I
6000 -
4000 -
2000 -
0
1972
1^1
1^1
1^1
1983
1994
1996
Figure 3. The expansion of hospital bed capacity in Lebanon
remain a key vehicle for programme activities such
as vaccination. The set-up of these health centres is
very varied and flexible. There are major institutions
with lots of staff, various specialities and extensive
equipment; others operate out of a rented apartment
and offer only essential amenities. Some of these
health centres function poorly; others offer services
of a better quality level than the average private prac
titioner - at a lower price to ±e patient.
is rented out to private practitioners who carry out
the NFP-NGO’s mission, but at the same time use
the infrastructure to build up a private clientele. This
phenomenon has now become so extensive - also in
the government health centres - that some of the
NGOs are looking for ways to limit the fragmenta
tion of care that is the result of the multiplication of
doctors who use the health centres as a recruitment
basis.
On the whole, however, the profile of care offered
by NFP-NGO health centres increasingly looks like
that of private clinics. This is a consequence of the
changes in the environment in which the NFP-NGOs
operate. Since the end of the war they have been ex
periencing growing difficulties in securing funds. In
puts from foreign donors to Lebanon have diminished
and the trend has been to redirect funds towards the
government. Furthermore, political funding related
to the various factions in the war dwindled. Conse
quently, the importance of ensuring cost recovery
became paramount. Since there is an amply supply
of physicians, the NFP-NGO health centres can
afford to rely more and more on non-salaried parttime physicians: an average of 8.4 per centre. Pro
ceeds of fee-for-service payments are split between
the physician and the NGO, for example on a 50/50
or 75/25 basis. The NFP-NGO health centres are thus
progressively transforming into an infrastructure that
When not working in a NFP-NGO setting, private
practitioners function essentially as individual private
entrepreneurs, most often with some specialist label,
but without accreditation, control or regulations.
There is thus a continuum between health centres and
private practice that affects the way both function:
practice in most NFP-NGO health centres becomes
more ‘commercial’, while the PFP sector cannot
ignore the de facto quality standards some of these
NFP-NGO health centres are setting.
Hospital care in subsidized private
hospitals
There are at present approximately 3.4 beds per 1000
inhabitants in Lebanon (Figure 1), more than in the
rest of the region but less than in other countries with
similar doctor/population ratios. The number of beds
increased both during and after the war (Figure 3).
Health sector reform in Lebanon. I.
301
35
I 30-
LI
C
20 -
i
I15’
o
10 -
J
5
0
Figure 4.
In 46
hospitals
< = 25
beds
In 41
hospitals
26-50
beds
In 37
hospitals
51-100
beds
In 13
hospitals
101-200
beds
_I
In 4
hospitals
>200
beds
Most acute care beds are in small hospitals: bed share of hospitals of various sizes
More than half of the private hospitals became opera
tional during this period. At the same time ±e number
of public beds shnmk, both in absolute and in relative
terms.
The long stay hospitals belong to the NFP-NGO sec
tor. The short stay hospitals belong either to the public
sector (6% of the total number of beds), NFP-NGOs
(22%) or for-profit (FP) private organizations: in
dividual doctors or groups of businessmen that in
clude doctors. Most of the expansion over the last
15 years took place in the form of small-scale private
acute care hospitals: 87 out of 140 have less than 50
beds. Almost one-third of all acute beds are in
hospitals of 50 beds or less (Figure 4). On the
average, FP-NGO hospitals are smaller than those
owned by NFP-NGOs or universities.
In the 1980s, 61 % of patients were admitted to volun
tary and teaching NFP private hospitals, 37% to other
private hospitals and less than 2 % to public hospitals
(Kronfol et al. 1985). The latter have now become
even more marginal; since 1992 the numbers of
hospitalizations, outpatient consultations, x-rays,
laboratory examinations, etc. have declined by
10-20% each year. Many of these public hospitals
now have bed-occupation ratios of less than 5-10%.
In the meantime, the smaller PFP hospitals seem to
increase their market share. This evolution is linked
to the way health care is financed in Lebanon.
Health expenditures in the 1990s
It is extremely difficult to know who spends how
much on health care in Lebanon. Data are incomplete
and contradictory. The 1992 estimate is of USS 301
million, i.e. about USS 100 per person per year
(Posarac 1994). Triangulation of information from
various sources on 1995 yields a range of between
USS 600-862 million (Table 1): USS 200-300 per
person. Around 60% of expenditures is private
money in the strict sense of the word (out-of-pocket
and private insurance), while one-third is paid for
from public sources (MOH and public insurance
schemes, i.e. the National Social Security Fund
(NSSF), the army and the Civil Services Cooperative
(CSC)).
Obviously the situation is changing very fast, not only
in absolute terms (doubling in less than three years),
but also as a percentage of GDP. Table 2 shows that
in 1992 private health expenditures were at the same
level, in terms of GDP, as in established market
302
Table 1.
W Van Lerberghe et al.
Who pays the health bill?*
Public insurance schemes
Public funding: MOH
Lebanese NGOs and international donors
Private insurance
Out-of-pocket
Total
1992
1993
1994
49.0 (16%)
45.1 (15%)
29.0 (10%)
41.6 (14%)
136.4 (45%)
301
71.0
62.8
72.1
1995
130.8 (15-22%)
98.2 (11-16%)
41.6 (5-7%)
151-207 (24-25%)
179-381 (30-^4%)
601-859
* USS million; estimates adapted from Posarac 1994 and other sources
Table 2.
Public and private expenditures for health (excluding donor assistance), as percentage of GDP
Area
Total
(% of GDP)
Public
(% of GDP)
Private
(% of GDP)
Lebanon (1992 estimate)
Lebanon (1995 estimated range)
Syrian Arab Republic
Jordan
Turkey
China
Middle East Crescent (weighted)
Latin America (weighted)
Sub-Saharan Africa (weighted)
Asia (weighted)
India
Established market economies (weighted)
4.8
6.4-9.1
2.0
3.8
4.0
3.5
4.1
4.0
4.5
4.5
6.0
1.6
2.4
0.4
1.8
1.5
2.1
2.4
2.4
2.5
1.8
1.3
5.6
3.2
3.9-6.6
1.6
2.0
2.5
1.4
1.7
1.6
2.0
2.7
4.7
3.5
economies, and higher than in most of the rest of the
world. Public expenditures, on the other hand, were
among the lowest. By 1995, overall health expen
diture in GDP terms in Lebanon appears to close the
gap with the established market economies; mainly
through an increase in private expenditures but also
by catching up in public.
Not all these resources are uniformly distributed.
Figure 5 shows who paid for whom in 1992 and 1995.
NFP-NGO and donor expenditures were assigned to
the whole population. MOH expenditures were allot
ted to the uninsured population, except for the
disbursements for cardiac surgery, kidney dialysis
and cancer treatment, which benefit ±e entire popula
tion (see below). Expenditures of the various public
9.1
insurance systems were allotted to the beneficiaries
of these systems and their dependants. The same goes
for the expenditures of private insurance schemes.
No account is taken of the possibility that some may
benefit from a number of insurance schemes at the
same time. Nevertheless, in Figure 5, 25 % of private
insurance expenditures are arbitrarily distributed over •
both privately and publicly insured, to take account
of the increasingly common practice of subscribing
to complementary insurance. Both expenditure and
coverage data are rough estimations, with a con
siderable amount of uncertainty, indicated by the
arrows in Figure 5. This makes a precise interpreta
tion of expenditure levels difficult. With this caveat,
the figure nevertheless illustrates present trends in
financing.
Health sector reform in Lebanon. I.
500
1000 F7
4
1992
« 400
“
s$2
S
Sa Spent by donors and NGOs
^3 Spent by MOH
i-c- l Spent hv
by nrn/att
private insurance schemes
EZ3 Spent by public insurance schemes
---- .
300
2
1995
s 400^-
I
f 300 f 5■
s
OT
.£
S>
303
.s
200
■g
o
iS 100 ~ \
9%
46%
45%
covered
covered
uninsured
by private by public
insurance insurance
Distribution of the population by insurance status
I
UJ
200
100
5-17%
26-52%
private
public
insurance insurance
(11%)
(41%)
32-63%
no
insurance
(48%)
Distribution of the population by insurance status
' Abscissa: proportional to number of population covered; ordinate: USS per inhabitent per year within the? coverage group
NB: The arrows indicate the range of uncertainty on expenditures and proportion of population covered. W
Where relevant.
the average of vanous estimates of expenditure or population coverage has been used.
Figure 5.
Non-out-of-pocket expenditures on health per person in Lebanon in 1992 and 1995, according to type of coverage’"
Between 5% and 17% of the Lebanese population
have private insurance coverage - estimates range
widely but there is a consensus that the sector is ex
panding. If one assumes that private insurance
coverage has gone up from 8% in 1992 to 11% in
1995, average non-out-of-pocket expenditure for this
pan of the population in 1995 was around USS 460
per person (but may be as high as USS 950 accor
ding to some estimations). Of this, USS 13.8 was
donor money or NFP-NGO expenditure, and the
MOH paid between USS 10-14 (a conservative
estimate: the real figure may be significantly higher)
in hospitalization costs for cardiac surgery, kidney
dialysis and a number of other specific conditions.
The rest, over USS 430 per person in 1995, nearly
three times as much as in 1992, was accounted for
by private insurance. The latter mainly covers
hospitalization, but not exclusively.
Nearly half of the population is covered by one of
the three public insurance systems: army, public ser
vice (CSC), and employees (NSSF). These insurance
systems were created in the 1960s following Euro-
pean models (Kronfol and Bashshur 1989). They
more than doubled their expenditures between 1992
and 1995 (Table 1), and now reach around USS 74
per person per year. About 40% of their expenditures
are for inpatient care. People in a public insurance
scheme also may carry a complementary (private) in
surance (estimated here, rather arbitrarily, to con- ■
tribute USS 29 per person), and benefit from MOH
(low-end estimate between USS 10-14) and donorNGO inputs (USS 13.8). Total expenditure would
then be around USS 129 per person (with a range of
USS 112-168).
The rest of the population is uninsured. The MCH
spent around USS 55 per person in reimbursements
to private hospitals for inpatient care for the unin
sured. It does not reimburse them for outpatient care.
The only other non-out-of-pocket contribution to
financing health care for this part of the population
is that of donors and NGOs. Overall non-out-ofpocket expenditures for the uninsured were around
USS 69 (range USS 58-89) in 1995: more than double
the figure for 1992. Sening aside ±e de facto, but
304
W Van Lerberghe et al.
Out-of-pocket
74%
No or > 1 answer 2%
Aid 1%
7MOH3%
Public insurance
schemes
16%
Private insurance
4%
Adapted from Firkh et al. 1996
Figure 6. How people pay for ambulatory care
limited, subsidies by NFP-NGOs, the uninsured have
to pay out-of-pocket for all of their ambulatory care.
The overall impression is one of an explosion of ex
penditures that is most marked for the population with
private insurance, but touches the rest of the popula
tion as well. If coverage for ambulatory care was
eliminated, very similar expenditure levels would be
expected for both the uninsured and those with public
insurance, roughly between USS 50-70 per person
per year; for the privately insured, non-out-of-pocket
expenditures are probably well above USS 300.
Financing
Only one-fifth of the population relies mainly on third
party payment for its ambulatory care: 16% through
public insurance and 4% through private insurance
(Figure 6) (Firkh et al. 1996). Ambulatory care is
essentially paid out-of-pocket by 77% of the users.
Ten per cent of the population rely on NFP-NGO run
health centres where financial barriers can easily be
overcome (low fees, possibility of free care); the
rest of the population uses the services of (expensive)
private practitioners. Out-of-pocket payment is the
source of 74% of expenditures on laboratory services,
79% of those on drugs and 92% of those on dentistry.
Ambulatory care (slightly over half of total non-donor
funded expenditure in 1992-93) is therefore fairly
independent from public funding. Public insurance
schemes contributed around USS 40 million to non
hospital care in 1993. The rest was made up by
private insurance, NGOs (whose contribution was
estimated at USS 6 million, probably targeting mainly
the uninsured) and out-of-pocket payments. The latter
have increased with the expansion of the supply of
doctors, whereas the MOH was nearly completely
absent (Figure 7).
The situation was very different for hospital care. The
share of the public sector in directly providing
hospital care is marginal. The State, however, makes
use of non-public hospitals through three
mechanisms. The first is the various public insurance
schemes. These have arrangements ro reimburse
Health sector reform in Lebanon. I.
305
100
90
80
53 oop
EZ3 NGOs and donations
Osl Private insurance
Public insurance
70
60
% 50
40
30
20
10
0-
Hospital
Ambulatory
care
care
•Estimations based on aggregate 1993 data; OOP: out-of-pocket; NGO: private non-for-profit only
Figure 7. How hospital and ambulatory care are paid for*
itemized expenses made at outpatient consultations
and for hospitalizations in private hospitals. They are
independent from the MOH.
Secondly, the MOH pays, through its budget, for par
ticular categories of treatment (cardiac surgery,
kidney dialysis and cancer treatment). A political
decision in 1990 led the MOH to pay for such inter
ventions in the private sector for all Lebanese
citizens. This now mobilizes between one-third and
half of MOH expenditure for reimbursement of in
patient care: low-end estimates range between USS
10-14 for 1995, up from USS 8.5 in 1992. It is not
known whether beneficiaries of this MOH financing
are concentrated among a particular class, or equally
distributed.
The final mechanism is contracting with private
hospitals that provide for reimbursement of
hospitalization costs of the uninsured population.
Such treatment in the private sector, paid for by the
government, concerned around 40 000 patients per
year during the war, and rapidly increased after
wards: 64 200 patients in 1990, 65 800 in 1991,
80 000 in 1992, 90 000 in 1995. The MOH earmarks
a number of beds for subsidized patients. Each
hospital is graded, and a room rate and tariffs of
charges for tests, drugs, use of the operating theatre,
etc. are agreed. The MOH has to give authorization
for admission - based on a very cursory referral note.
After hospitalization of an authorized patient, the
MOH will receive an extremely detailed bill, which
it has to pay without being able to exercise any conttol (up to 1993-95) over the justification of the cost
items. There are probably no or very few countries
in the world that have a billing system that is both
as complicated and as uncontrollable as the Lebanese
system. Misuse is rife, but although public insurance
has in two instances cancelled contract arrangements
with hospitals, the MOH has never been in a posi
tion to do so.
Almost half of non-donor-funded expenditure is for
hospital care. The public sector provides some USS
12 per person per year for the (affluent) privately
insured through reimbursement of heart surgery,
kidney dialysis and cancer treatment. It spends USS
50-60 per person per year for the publicly insured
(employees and military with their dependants), and
around USS 55 per person per year for the uninsured.
All in all, public insurance and the MOH paid about
USS 80 million for hospital care provided in private
hospitals in 1992, and almost twice as much in
1995. The rest came from private insurance and from
the users through out-of-pocket payments. In
1992-93, 65% of private hospitals’ income came
from MOH and public insurance, 18% from four
private health insurance schemes and only 15% from
W Van Lerberghe et al.
306
Table 3.
Sources of income of four hospitals in 1995
82 hospitals in 1994
Hospital 1. 1995
Hospital 2, 1995
Hospital 3, 1995
Hospital 4. 1995
out-of-pocket payments. Donations account for 3%
of their income (Figure 7) (Posarac 1994). A study
of 82 hospitals in 1994 (Juijus 1994) and detailed data
on four hospitals in 1995 (Ramaddan 1996) confirm
this pattern (Table 3).
Health care delivery, both hospital based and am
bulatory, is thus essentially private and unregulated.
Ambulatory care has developed outside public financ
ing considerations. Hospitals, on the other hand,
depend very much on public financing. Reimburse
ment of hospitalization expenses by public and private
insurance schemes, and by the MOH, has been the
motor of the expansion of the private hospitals.
Without it, the survival of the smaller hospitals would
probably be immediately endangered.
Institutional bargaining capacity
The dependency of private hospitals, and especially
of the smaller ones, on public funding should put the
MOH in a strong bargaining position. Nevertheless,
the MOH has been unable to restrain the growth of
the cost of the hospital care it contracts for in the
private sector. Hospital care is putting an increasing
strain on its budget, as it does on public insurance
(Abyad 1994). Before the war, payment of hospital
care accounted for roughly one-third of the MOH
budget. This then increased considerably, and since
the end of the war hospital care has consistently
mobilized more than three-quarters of the budget, in
cluding salaries. That is considerably higher than the
OECD mean share for hospitals, excluding
ambulatory care, in total public recurrent health ex
penditure (54% in the 1980s). Out of 60 low, middie and high income countries (Bamum and Kutzin
1993), only Malawi allocates as high a proportion of
recurrent public spending to hospitals. The MOH’s
reimbursement to hospitals has tended to grow over
MOH and public
insurance schemes
Private
insurance
Out-of-pocket
payments
67.1%
88.4%
76.1%
46.0%
51.0%
17.6%
6.1%
16.9%
25.0%
30.8%
15.3%
5.5%
6.9%
20.0%
18.2%
the years, both in absolute and relative terms (Figure
8). In the 1970s this made up one-third of the MOH
budget. Since 1991 hospitals have absorbed over 80%
of the budget, peakins at 86% in 1994 - rising from
USS 18.6 million in 1990 to USS 62.5 million in 1994
and USS 82.4 in million in 1995. The scope for
developing the other activities of the MOH within this
budget frame is limited and shrinking.
The MOH is having increasing problems in obtain
ing the budgets to keep up with the growing requests
for reimbursement of private hospital care. Public in
surance schemes are also, experiencing problems in
securing the required government contributions. On
the other hand, the MOH is unable to exen the
necessary pressure to control the amounts paid to
private hospitals, neither through rationing nor
through the pricing mechanisms.
In theory Lebanon’s MOH could have leverage over
what happens in the field of hospital care, through
its crucial role in the financing of hospital income
(Figure 7). This leverage is, however, limited by the
fact that the MOH has no authority over public in
surance. It can only use its own inputs and technical
authority as a basis for influencing hospital care in
the private sector. In practice it has very little effec
tive influence, for technical, administrative and
political reasons, and coordination in this matter only
started timidly in 1996.
Technically, the asymmetry of information available
to the purchaser (MOH and public insurance) and the
provider (the private hospitals) makes it difficult for
competition, in the form of preferred contracting, to
occur. Lebanon’s MOH has no inside knowledge on
the functioning of the hospital sector. The complexity
of the payment mechanism and the absence of
adequate technology and trained personnel make it
Health sector reform in Lebanon. I.
307
100
90
80 -
I
70 -
__
I
I
60
50
40
30
20 -
10 0
1990
1991
t
1992
Purchase of care
1993
|
| Salaries
1994
Programmes
1995
1996
Other
"1991 expenditures include catch-up expenditures for under-budgeting in 1990; figures for 1996 are budgeted expenditures
Figure 8. Ministry of Health expenditure, in USS millions, for reimbursement of hospital care in private hospitals, as pan of
overall MOH budget*
impossible even to identify blatant misuse or inap
propriate billing (Kronfol and Bashshur 1989), let
alone issue guidelines for standard treatment pro
tocols or costing norms. This deprives the MOH of
control over the pricing mechanism, which, as Euro
pean experience shows, is a critical tool for balanc
ing supply and demand in regulated markets (von
Otter and Saltman 1992).
The MOH thus has little information on which to base
a regulation or control function. This is compound
ed by the fact that the MOH budget offers little scope
for a personnel policy that would increase its capacity.
In terms of purchasing power, the 1994 personnel
budget is only 67.5% of the 1990 level. This also
represents a shrinkage in relative terms: from 15.3 %
of the budget down to only 8.9%. With such a budget
(an overall average of about USS 3600 per employee
for 1994), it is obviously difficult to retain, and near
impossible to anract new, qualified staff, let alone
maintain any illusion of setting up a health care pro
vision system based on public sector employed staff.
As such, the budget for personnel would be sufficient
to hire staff to fulfil a regulatory role. However, this
would require the MOH to rid itself of excess staff
presently assigned to health care delivery, which is
politically difficult. A 50% increase (in USS terms)
in the budget for salaries in 1995 brought purchas
ing power back to 1990 levels. This, however, does
not fundamentally alter the situation, given the ad
ministrative constraints on hiring personnel in the
public service.
Politically, the MOH is being urged to further pro
mote expansion of hospital capacity rather than
regulate it, and to refrain from showing preferences
between potential provider-hospitals. The choice of
hospitals to be contracted is basically a question of
denominational and political considerations. The
MOH thus cannot restrict market entry on technical
4
♦
308
W Van Lerberghe et al.
grounds. When a new small hospital starts activity,
it is near impossible for the MOH to impede this,
especially since it cannot provide alternative public
hospital care possibilities.
Furthermore, non-market pressures and concerns
with continuity of care and accessibility prevent
hospital closure or stopping of reimbursement ar
rangements, even when market conditions suggest
otherwise. Only once has the NSSF, over which the
MOH has no control, had the political clout to stop
purchasing care in a hospital for reasons of persis
tent false billings. In the Lebanese context, where
denominational and political balances are allimportant, the MOH itself has never been in a
position to do this. Even a hospital that constantly
overcharges by 60% or more remains contracted by
the MOH. Theoretically the MOH has the admini
strative authority to intervene, but it does not have
the technical means or information to make a case.
The lack of technical prestige and credibility of a
public service that has been absent from health care
delivery and policy making for the last decade or
more, further weakens its capacity to resist pressure
on technical grounds. Both participation in and
exclusion from the health care market are thus
politically constrained. In such circumstances, it is
unavoidable that there is little control over the size
of costs, over their justification and over quality of
care (Maynard 1991).
K
*
Without financial leverage, Lebanon’s MOH has even
less control over what happens in the field of
ambulatory care. Even though there has been a slight
improvement over the last five years, the MOH still
spends less than 4% of its budget for technical
activities and programmes. Primary health care
accounted for only USS 21 000 in 1991. Their share
of the budget has since increased to USS 1 500 000
in 1995, but this remains a marginal amount com
pared to the bill for hospital treatment. As is the case
in the field of hospital care, the MOH does not have
technical authority since it has not been a significant
actor in health care delivery over the last decades.
And its administrative authority is extremely limited
and almost impossible to carry through in a context
of political interference and delicate denominational
balances.
The MOH is thus left with (i) a budget that does not
provide enough funds to ensure its own activities,
including competitive payment of its personnel;
zii) a growing demand for reimbursement of care
provided by private hospitals; and (iii) limited scope
for increasing the total budget, or for further cuts in
budget lines other than those for reimbursement of
private hospital care. In the meantime, the economic
and cultural effects of the unregulated expansion of
the private sector are becoming apparent.
Incentives for inefficiency and distortion
In the aftermath of the war, the switch from emer
gency relief to health care delivery was to be based
on a self-regulated system of private care providers,
fuelled by public funds, where competition would en
sure quality of care and affordability. Within five
years the assumption that the sector would self
regulate (provide good quality care in an affordable
and efficient way) proved false. There is ample anec
dotal evidence that technical quality of care is want
ing, especially in many of the smaller hospitals. There
is no real evidence of growing consumer dissatisfac
tion as yet, but this can be expected as soon as pro
blems with sustainability become more evident.
Indeed, the mechanisms for regulation of the health
sector (or rather their absence) act as incentives
towards inefficiency and distort rational organization
of health care delivery. They promote, and are
reinforced by, a specialist-centred and secondary care
oriented culture among both professionals and the
public.
There are no incentives to expand the private pro
vider’s or health centre’s responsibility for care
beyond that of responding to immediate demand.
Continuity of care is absent; for example, less than
2% of the contracts with private practitioners are
revisits. Many health centres offer specialist consulta
tions, but, in contrast, leave prenatal care to hospitals.
This implies a tendency to medicalize, irrational use
of drugs, and reliance on technology at the expense
of communication. Hospital pharmacies have an
average of 514 different items, up to 8000 in one
hospital. Public funds pay for half of the 1.5 million
x-ray acts made in Lebanon every year (Juijus 1994).
There are more health centres or private clinics with
ECG services than with family planning activities.
Little or no work is done in the field of health pro
motion, such as prevention of smoking. The priority
given to kidney dialysis is in contrast with the absence
of diabetes programmes (diabetes being the underly
ing aetiology for over one-quarter of kidney failure
patients); the priority given to open heart surgery con
trasts with the lack of primary preventions.
Health sector reform in Lebanon. I.
NFP-NGOs are presently offering an alternative of
reasonably cheap and, in cases of need, free access
to care for the poor. They, rather than government
services, make up the social safety net for the poor
in Lebanon. Their way of operating has led them to
accept comprehensive responsibility for the care of
certain population groups. This situation is now
changing. Since their traditional sources of funding
are withering, NGOs increasingly copy the work
style of private practice: exclusive focus on those ac
tivities that have immediate income generating poten
tial. The financial predicament of NGOs, combined
with a de facto restriction of their mission, results
in erosion of the social safety net as well as in gradual
elimination of examples and models of better prac
tice at primary care level.
These changes are clearly dependent on the absence
of public funding to sustain structures accessible to
the poor, and on the inability of government to in
fluence or rationalise the way the private practitioners
operate. The lack of guidelines and regulation is fuel
ling prescription panems that merely respond to
demand, without elements of rationalization or con
straints other than the patient’s ability to pay. This
is preoccupying, for example, in the field of treat
ment of hypertension and diabetes, which was donorsponsored for the last few years. The government is
now contributing USS 1.5 million per year to this pro
gramme, but still without treatment policy guidelines
that would make it possible to control rising costs.
The lack of tools or levers for rationalizing am
bulatory care is compounded by the type of political
and financial incentives for hospital care. Hospitals
and first level care in Lebanon are completely
unrelated subsystems, both operationally and in the
way they are financed. Since quality or cost
effectiveness are not determinants for purchase of
hospital care, there is no real competition among
hospitals. On the other hand, public subsidy for
hospitalization, but not for ambulatory care, results
in a de facto competition for patients between
hospitals and first line services. This distortion carries
an opportunity cost in terms of missed possibilities
for efficiency gains through a division of labour
between complementary first, second and ternary
care levels.
The expansion of the hospital network has taken place
in an inefficient way, sacrificing overall sustainability
for shon-term return on singular investments. The
creation of a large number of small private hospitals
ggg
has resulted in an excess bed capacity in relation to
the level of demand, as evidenced by a low bed oc
cupancy (56%, compared to an OECD average of
81 %), a short average length hospitalization stay of
4.8 days (less than half of that of OECD countries)
(Juijus 1994) and a hospitalization rate of 13.9 that
approaches the OECD median of 16.1. A large pro
portion of hospitalizations in the small hospitals have
no medical justification.
Lebanon now has three times more physicians per
inhabitant than the average for the other countries in
the Middle East. This can be expected to further fuel
the growth of expenditure and the increase in hospital
beds: new hospitals are already under construction.
Most are so small that economies of scale are dif
ficult. This results, for example, in under-utilization
of equipment: CT scans in the smaller hospitals per
form only between three and eight (often un
necessary) examinations per day. Kidney dialysis
facilities could handle double the present patient load
(Juijus 1994), though the 400 dialysis patients per
million inhabitants is already above the OECD
median of 360.
Although manpower imbalances (e.g. only 2000
qualified nurses compared to 8-9000 doctors) will
make it difficult to sustain proper functioning,
hospitals aim for a level of technology that is way
above that of many developed countries. The finan
cing structure provides an incentive for the private
hospitals to invest in heavy technology, since its
operation will be preferentially subsidized by public
funds. This has led to very rapid expansion, with lit
tle techmeal or economic justification. There are now
five MRI in Lebanon, all located within a few
kilometres from each other. At 240 cases per week
the total cost can be estimated at USS 4 400 000 per
year: the equivalent of 5% of the MOH budget. There
are 27 CT scans, six centres for in-vitro fertilization,
and ten centres for litotripsy (Juijus 1994). The fastest
expansion is in cardiac surgery and cardiac
catheterization, techniques that are automatically
reimbursed by the MOH. Heavy medical technology
is now more available in Lebanon than in many in
dustrialized countries (Figure 9). Apart from the ex
pected iatrogenic effects, this expansion of technology
will further reinforce a culture of hospitalocentrism
and fuel the cost explosion.
These considerable investments gamble on a con
tinued growth of the health care market to ensure
returns. Even compared to established market
*
310
W Van Lerberghe et al.
3.5
3.0
I n
2.5
2.0
1 1.5
10“
z
0.5 -
I
Ol—Lii
Cardiac
surgery
MRI
Cardiac
catheteriast
ion
i&S&l Lebanon
\///A Canada
1
Lithotripsy
Radiation
therapy
Germany
Figure 9. Selected medical technology: availablicy in Lebanon as compared to Canada and Germany
economies, however, private expenditures are already
high in terms of GDP (Table 2), and public expen
diture is growing too fast for the government to sus
tain. The present predicament is that without proper
regulating mechanisms, an unbearable strain will be
put on the MOH and social security schemes, whereas
rationing or regulating mechanisms would endanger
returns on private investment.
References
.
,■
Abyad A. 1994. The Lebanese health care system. Fam Pract 11:
159-61.
Adib SM. 1994. Most common diseases treated in primary health
care facilities in Lebanon. Report to the World Bank. Beirut:
American University of Beirut; pp.1-20.
Anonymous. 1987. Lebanon ar present and its needs for rehabilita
tion and development. Beirut: Harin Foundation; pp.182.
Barnum H, Kutzin J. 1993. Public Hospitals in Developing Coun
tries: Resource Use. Cost. Financing. Baltimore and London:
Johns Hopkins University Press.
Belmartino S. 1994. The role of the State in health systems. Soc
Sci Med 39: 1315-21.
Birdsall N, James A. 1992. Health, government and the poor: the
case for the private sector. Washington DC: World Bank. Un
published report.
Broomberg J. 1994. Managing the health care market in develop
ing countries: prospects and problems. Health Pol Plann 9:
237-51.
Carr-Hill R. 1994. Efficiency and equity implications of the health
care reforms. Soc Sci Med 39: 1189-201.
Dekker E. 1994. Health care reforms and public health. Eur J
Public Health 4: 281-6.
Feghali K. 1992. Displacement in Lebanon: Facts and Figures.
Beirut: Ministry of Displaced People; pp.1-44.
Firkh M. Sinno Z, Ziade F. 1996. Malcassed Health Programme
Health Maintenance Organisation Survey. MOH-WHO un
published report, Beirut; pp.1-33.
Jurjus AR. 1994. Hospital and heavy technology in Lebanon.
MOH-WHO unpublished report, Beirut; pp.1-18.
Kronfol NM, Bashshur R. 1989. Lebanon’s Health Care Policy:
a case study in the evolution of a health system under stress.
J Public Health Policy 10: 377-96.
Kronfol N, Muawwad-Jarawan E, Lockwood-Hourani L. 1985.
The utilization of health services. In: Zurayk HC, Armenian
HK (eds). Beirut 1984: a population and health profile. Beirut:
American University of Beirut; pp. 119-56.
Kronfol NM, Sibai AM, Rafeh N. 1992. The impact of civil distur
bances on the migration of physicians: the case of Lebanon. Med
Care 30: 208-15.
Maynard A. 1991. Developing the health care market. Economic
Journal 101: 1277-86.
McPake B, Hongoro C. 1995. Contracting out of clinical services
in Zimbabwe. Soc Sci Med 41: 13-24.
Ministry of Labour and Social Affairs, Lebanon, and Norwegian
People’s Aid. 1985. Social Welfare Services in Lebanon. Beirut,
unpublished report.
Oevretveit J. 1994. Values in European health care markets: choice,
equity and competition. Eur J Public Health 4: 294-300.
Petchey R. 1995. General practitioner fundholding: weighing the
evidence. The Lancet 346: 1139-42.
Posarac A. 1994. Health Sector Financing in Lebanon. Washington
DC: World Bank: pp.1-48.
Price M. 1989. Explaining trends in the privatization of health
services in South Africa. Health Pol Plann 4: 121—30.
Ramaddan S. 1996. Sources of funds for four private hospitals
in 1995. Personal communication.
Saltman RB. 1994. A conceptual overview of recent health care
reforms. Eur J Public Health 4: 287-93.
Van Lerberghe W, Ammar W, El Rashidi R, Awar M, Sales A,
Mechbal A. 1997. Reform follows failure, n. Pressure for
change in the Lebanese health sector. Health Pol Plann
12(4): 312-319.
Health sector reform in Lebanon. I.
311
von Otter C, Saltman RB. 1992. Planned markets and public com
petition. Strategic reform in Northern European health systems.
Buckingham. UK: Open University Press.
World Bank. 1993. World Development Report 1993: Investing
in Health. New York and Oxford: Oxford University Press.
Lebanon he directed a Social Security Fund and worked as a
hospital director. Since 1993 he has been Director General of the
Ministry of Health in Beirut. He lectures at the National Institute
of Administration and Development and at the School of Public
Health of the Lebanese University.
Acknowledgement
Randa El Rashidi is a Human Resource specialist at the World
Bank. Her field of interest covers social funds and the role of NGOs
in social development in various Middle-Eastern countries.
Pan of this research was supported by a grant of the European
Union. General Directorate XU (Avicenne Project), contract
ERB A VI* CT93-0012.
Biographies
Albert Sales, MD. MPH. started working in West Africa for the
Belgian Cooperation and WHO. He then joined the Asian Develop
ment Bank and is currently a Public Health Specialist with the
World Bank.
Wim Van Lerberghe, MD, PhD. is currently chairman of the
Department of Public Health of the Institute of Tropical Medicine
in .Antwerp. Belgium. His field of interest is the interface between
health care organization and health care reform in Africa, the Mid
dle East and South-East Asia.
Abdelhai Mechbal, MD. was trained in Health Planning in Mex
ico. He is a former Technical Director of the Ministry of Health
in Morocco, and currently WHO representative in Lebanon.
Walid .Ammar, MD, MPH, graduated from the Universite Libre
de Bruxelles. After working as a GP in a community hospital in
Correspondence: Dr W Van Lerberghe, Dept of Public Health.
Institute of Tropical Medicine, Nationalestraat 155, B-2000
Antwerpen. Belgium.
us
HEALTH POLICY AND PLANNING; 12(4): 312-319
© Oxford University Press 1997
Reform follows failure:
II. Pressure for change in the Lebanese health sector
W VAN LERBERGHE,1 W AMMAR,2 R EL RASHIDI,3 M AWAR,2 A SALES,3 AND A MECHBAL4
'Department of Public Health, Institute for Tropical Medicine, Antwerp, Belgium, 2Ministry of Health,
Republic of Lebanon, 3The World Bank, Washington DC, and 4Wor!d Health Organization, Beirut,
Lebanon
This paper describes how, against a background of growing financial crisis, pressure for reform is
building up in the Lebanese health care system. It describes the various agendas and influences that
played a role. The Ministry of Health, backed by some international organizations, has started taking
the lead in a reform that addresses both the way care is delivered and the way it is financed. The
paper describes the interventions made to prepare reform. The experience in Lebanon shows that
this preparation is a process of muddling through, experimentation and alliance building, rather than
the marketing of an overall coherent blueprint
•
Introduction
In the aftermath of the civil war in Lebanon, the
health care system was characterized by a very rapid
expansion of private health care provision. In the
absence of any regulation, this has led to a crisis situa
tion. Private expenditures on health care are already
high in terms of GDP (Van Lerberghe et al. 1997),
and public expenditure is growing too fast for the
government to sustain. Rationing or regulating
mechanisms would endanger returns on private in
vestment, and generate strong opposition from in
terest groups. On the other hand, ±e strain on the
Ministry of Health (MOH) and social security
schemes is rapidly becoming unbearable. The MOH
is faced with (i) a budget that does not leave enough
funds to ensure its own activities, including com
petitive payment of its personnel; (ii) a growing de
mand for reimbursement of care provided by private
hospitals; and (iii) limited scope for increasing the
total budget, or for further cuts in budget lines other
than those for reimbursement of private hospital care.
In the meantime, the economic and cultural effects
of the unregulated expansion of the private sector are
becoming apparent.
A first paper (Van Lerberghe et al. 1997) has
described how this crisis developed between 1991 and
1995. This second paper documents how pressure for
reform built up between 1994 and 1996, and iden
tifies the key issues that, for better or worse, are on
the reform agenda today. It is a reconstruction of
events and positions in a rapidly changing environ
ment, based on a reconstruction of the sequence of
events, document analysis and their (often contradic
tory) interpretation in discussions with key players.
It suffers from the biases of participant observation.
Putting reform on the policy agenda
Recognition of the need for reform usually emerges
gradually among various actors with different and
often contradictory agendas. It is the work of coali
tions, by no means always led by the same groups.
The MOH in Lebanon, which initially had a marginal
role, has come to have a central position in the health
reforms, using an alliance with some of the interna
tional organizations present in Lebanon. This is
unusual since reform is usually put on the agenda by
politicians (Hunter and Stockford 1996), profes
sionals (von Otter and Saltman 1991) or, in develop
ing countries, by the international development
agencies, often in the wake of structural adjustment
programmes (Okuonzi and Macrae 1995).
This central role for the MOH was possible because
the ministry filled a policy vacuum. There is no easily
Health sector reform in Lebanon. II
identifiable leadership in the sector. The actors are
extremely diverse and fragmented, and none em
erges with recognized authority. Whereas NGOs had
prestige and authority during the war, both opera
tionally and in the eyes of the public, this diminished
afterwards. Professional organizations play only a
limited role, and each private hospital looks after its
own immediate interests. Lay politicians in Lebanon
are rather indifferent to the organizational structure
of health care delivery, or to proposals for change.
They look at the health care system basically as one
of the tools to help ensure political equilibrium.
Ideologically biased in favour of hospitals, technology
and private enterprise, they seem unaware of the
financial predicament of the health care sector - con
sidered a marginal problem compared to the political
and economical challenges of reconstruction. Dis
satisfaction with health care delivery is interpreted
as an expression of the need for expansion of health
care supply (physicians and hospitals), rather than as
a need for rationalization and a change in policy and
the health care provision model.
The ideological climate in Lebanon clearly favours
private sector development, making it difficult to
restrain expansion of the private sector hospital
capacity or equipment. At the same time, the strategy
for economic reconstruction is to be driven by public
works. In the case of the health sector this means that
the major focus is on hospital construction. Saudi,
Kuwaiti and OPEC grant and soft-loan money is
presently being used for the construction of seven,
and possibly more, new public hospitals. This is
clearly done more with a view to creating oppor
tunities for public works than with a health sector
development rationale.
Managers within the MOH view the prospect of hav
ing to operate these hospitals as a ftiture budgetary
and manpower nightmare. They find it difficult to en
visage how they will recruit the necessary staff and
liberate the operating funds, given (i) the MOH’s
track record in the operation of existing public
hospitals; (ii) the restricted margin for reallocation
of binds in a budget tied up by the present system
of care purchasing in private hospitals; (iii) the
scarcity of nursing staff; and (iv) the already existing
hospital over-capacity in the private sector. On the
other hand, they see the political necessity to (i) main
tain some negotiation power by offering an alternative
to the private sector; (ii) be able to deal with emer
gencies in case of armed conflict; and (iii) be able
to refer patients that need secondary level care.
313
Conflicting agendas within the MOH
The current predicament of the health care sector
within the MOH is by no means universally agreed.
The main lines of thinking and the influences are
schematized in Figure 1.
A first agenda is that of transforming Lebanon into
a ‘hospital for the Middle East’. In line with the
private sector ideology that fuels the reconstruction
policies in Lebanon today, this is an agenda that those
in the MOH with a political constituency share with
lay politicians. It receives support from different
groups: political parties, the majority of the private
sector medical establishment, interest groups within
the MOH and, given the prevailing specialist and
secondary care oriented ideology, the public as well.
This agenda results in policy options favouring ex
pansion of hospitals and a status quo in matters of
regulation and financing mechanisms. It is made
possible by the easy availability of both Lebanese and
donor capital for heavy investments, and is fuelled
by the high short-term returns on investment. A major
advantage is that it responds to the political constraints
typical for Lebanon. Decisions on hospitals and
financing can be used as ways to obtain short-term
political goals of maintaining or shifting equilibria
within an extremely heterogeneous ‘house of many
mansions’ (Salibi 1993).
The same group also has an agenda of reorientation
towards PHC in response to pressure from their con
stituencies, e.g. for care for chronic patients. On this
agenda they are in concordance with those within the
MOH who have a more technocratic and managerial
outlook. This agenda is supported by part of the
medical establishment and academia: family medicine
concepts are not dominant but do exist (Abyad et al.
1992). Reorientation towards PHC is also advocated
by the NFP-NGOs (not-for-profit non-governmental
organizations), and those within the MOH who pro
mote it found allies in agencies like the World Health
Organization (WHO) and, at a later stage, the World
Bank.
The third agenda is that of control of the financing
crisis. For the managers within the MOH the main
impetus for reform has come from the budgetary
predicament. As of 1992 the consequences of the
political decision of unlimited reimbursement of cer
tain types of care had become apparent.
314
W Van Lerberghe et al.
Positions
within MOH
ns
■ !■I
''
Lebanon
as the
’ ’ t"1 ' S ‘hospital’
for the
Middle East’
Offl
Illi
Illi
Reorientation
towards
Primary
Health
Care
I ■...
Political Parties
The Public
The Medical Establishment
Interest Groups within MOH
,
Policy
Options
Easy Capital
for investment,
Lebanese &
foreign
I
I__StatusandQuo
Expansion
of Hospitals
Part of the Medical Establishment
NFP - NGOs
Academia
UNICEF |
Research
Studies
WHO WB
■
I;
Enabling
Conditions
& Support
Politicians Technocrats/
Managers
: A-/
Influences
Agendas
Control
of the
financing
crisis
I
f
Preparation
of World Bank
project
Pressure
for
Reform
and
Regulation
Figure 1. Agendas and conflicting policy directions with the Ministry of Health
This was not, however, the only element. The MOH
also wanted to find a new and more rational equili
brium between primary, secondary and tertiary care,
and to address the challenges of the epidemiological
transition. Furthermore, some of these managers have
a strong ideological tradition of public service, rein
forced through their links with the NFP-NGOs dur
ing the war period. This makes the MOH one of the
only organized groups concerned with equity and ac
cess, a concern reinforced through its links with
WHO and academia.
The fusion of the second and third agenda items,
reorientation towards PHC and control of the financ
ing crisis, led to increasing pressure for reform and
- regulation. The challenge is to do this in a political
environment with little awareness of the need and the
stakes of reform, and with powerful interests pushing
. towards the status quo. Part of the private sector, for
example, would like to get managerial control of the
public insurance funds, as a way of streamlining
bureaucracy and guaranteeing subsidies to hospitals.
The major constraint was the MOH’s lack of
recognized leadership, institutional capacity and
authority to put the need for reform on the political
agenda and to shape the orientation of the reform
(Kronfol and Bashshur 1989). The MOH itself had
little technical authority, limited political weight and
few qualified professionals. Only a handful had an
overview of the problems of the sector and a vision
of possible ways out. Much of this had to do with
the absence of information on what went on. It is
revealing that even senior public insurance manage
ment staff are unable to provide a clear image of
money-flows, and that the MOH has no updated in
ventory of health centres or hospitals in the country.
Despite its political and institutional fragility, the
MOH has been taking the lead, being the body most
immediately confronted with the financial conse
quences of the evolution of the last five years. For
the MOH, both the way health care is delivered (with
issues such as the equilibrium between hospital and
community care, quality of care, access and equity)
and the administrative-financial aspects of regulation,
cost-containment and efficiency, were at stake. Very
early on its priority option was one of regulation,
rather than direct involvement in health care provi
sion. This evolution was made possible by the fact
Health sector reform in Lebanon. II.
that the MOH had a better insight into the problems
of the sector, which accelerated during the prepara
tion of a World Bank loan for the reform of the health
sector.
The need for information and alliances
In the first phase of putting health care reform on the
agenda, research and information gathering have
played a crucial role. This consisted essentially of
documenting the extent of the cost explosion; the ef
ficiencies and contradictions the health care system was
heading for; and the extent of the problem of chronic
diseases and ill health related to the urban environ
ment. A flurry of research activities, funded through
WHO, were contracted out to academic circles, but
in close collaboration with the MOH. Besides provid
ing information and evidence for the double agenda
of organizational and financial reform, this research
phase has had several important spin-offs.
First, knowledge provided the MOH with new
leverage.. It allowed the MOH administration to make
the case for reform and, by the mere fact of knowing
the sector, to progressively gain the authority to take
a leadership position. Second, it fostered alliances out
side the MOH and, within the ministry, a new sense
of purpose. Third, this phase - with all the discus
sions with academia, NGOs and the international scene
- allowed the MOH to make a basic strategic choice:
it would aim to strengthen its policy-making and
regulation functions rather than try to build a public
sector delivery system.
This phase of awareness creation went on into 1994
and beyond. From 1994 onwards the MOH used the
preparation of a World Bank loan as an opportunity
to launch the process of reform. The aim was two
fold: reorient the way health care is provided and rec
tify the financing structure. In order to do that the
MOH had to improve its bargaining position and its
policy leadership.
In current health sector reforms in industrialized
countries the focus is on the pursuit of micro
economic efficiency on the production side, and on
the allocation mechanisms that link finance to pro
duction (Saltman 1994). Most attempts start by con
centrating on economic incentives and the financial
operation of the health care system (Oevretveit 1994)
in order to respond to fiscal pressure (Beaglehole and
Davis 1992). Characteristic of the reform agenda
in Lebanon is the sequencing of health care organiza
315
tion and health financing reform. Both are obviously
interrelated, but the accent was put on health care
reform first (with actual interventions), whilst in the
field of financing, actions were limited to the prepara
tion of future macro-level reform proposals.
Hospitals and the way they are financed are clearly
at the heart of the problems of cost explosion and
distortion of the Lebanese health system. This does
not mean, however, that these problems can be
tackled head on. The strategic role of public funding
provides the MOH, a priori, with a good bargaining
position towards the hospitals, and should allow it
to eliminate major inefficiencies, control costs, and
provide incentives for quality assurance. In particular,
the smaller, inefficient private hospitals would be
very vulnerable to financial incentives and disincen
tives. But the MOH controls only its own inputs, not
those of public insurance, and moreover, although
potential and willingness are there, it is too weak
technically and politically to enforce changes in the
financing structure on its own. There is some margin
for controlling costs, and some steps have been taken
in 1994-96, but a thorough restructuring requires
stronger pressure and alliances.
Such pressure does not come from ambulatory private
practice as it functions now. Lebanon has some tradi
tion of family medicine (Abyad et al. 1992) that has
been built up in academic circles, but over the last
year hospitalocentrism, reduction of ambulatory care
and technology consumption have become dominant.
Public sector health centres are not a credible alter
native, and few or no officials believe that they have
the potential to become so rapidly, even with major
resource inputs. One of the major impediments to im
proving quality of care at first contact level, and to
using first contact level care as a lever to rationaliz
ing hospital care, is the absence of an organizational
model as an alternative to the present situation. For
family doctors or general practitioners to put pressure
on hospitals, they need first to start working in a dif
ferent way themselves.
Currently, it appears that influencing the private
sector will not be possible through mere financial
mechanisms, certainly not in the short term. This
would require massive state intervention, which is
unrealistic given the budgetary situation and the
weakness and lack of authority of the MOH. It will
therefore be possible only to work through forms of
pressure that are not exclusively dependent on MOH
316
Table 1.
W Van Lerberghe et al.
Interventions to prepare reform
Problem area
Interventions
Expected shon-term
results
Expected medium
results
Hospital care:
cost and
quality
1994 onwards: Control billing
and change price structure
1995: Autonomous public hospitals
1995: Feasibility study HMO
—►Cost containment
Negotiated contracting
conditions: gains in
quality and efficiency
-►Regain credibility for
public hospitals
Ability to negotiate with
private sector
—►Get more options
First contact
level care:
quality and
access
Regulation
capacity
Preparation of
financial
reform
Pressure for
sector reform
1993: WHO PHC Report
1995 onwards: Formulate
programmes for control of chronic
diseases
1995-6 onwards: Contracting
N'FP-NGO health centres: support
in exchange for registration,
minimum package and quality care
1992 onwards: Studies and research
1994 onwards: Control billling
and change price structure
1995 onwards: Institutional
strengthening
1996 onwards: Infrastructure
coverage planning
1996 onwards: focus of studies
and research on problems of
financing
Capacity building (human resources
documenution, information)
administrative mechanisms: pressure from the
medical community and pressure from user demand
for accessible quality care.
Interventions to build pressure for reform
Pressure for reform in Lebanon built up through a
series of parallel and phased interventions rather than
through the marketing of an overall plan. A number
of interventions were put in place in order to build
a capacity, in terms of personnel and knowledge of
the system, that would make it possible to create a
—►Create demand for quality
care
Pressure on private
practitioners to improve
quality
-►Accessible quality care
-►Capacity to manage
responsibility for a defined
population
Social safety net
Fundholding type pressure in
negotiations with hospitals
-►Alliances (especially with
with social security system)
and expertise
Ability to lead
financing reform
-►Tools for regulation
-►Recognition of
leadership and authority
Better control over system
Ability to negotiate with
private sector
-♦Recognition of
leadership and authority
Ability to market reform
proposals
-►Knowledge on the
functioning of the system
Ability to formulate a
reform proposal
Favourable environment
and increased control
Ability to formulate,
to lead and to negotiate
favourable environment and gain some degree of con
trol over the system. The aim is to provide the MOH
with the ability to formulate, lead and negotiate
overall proposals for reform. These different inter
ventions are presented in Table 1.
In the field of hospital care, public hospitals became
autonomous, and attempts are being made to improve
their management. A major stumbling block is the
absence of any links with the health centres. A
feasibility study on establishing an HMO (health
maintenance organization) in a Beirut suburb (Firkh
Health sector reform in Lebanon. II.
317
Computerized billling
!
Information on price structures
1
Transparent codification system
Alliance with public
insurance schemes
Eliminate
gross abuse
Gain in technical
capacities and authority
I
Change principle of pricing
from item based to case mix,
and to standard treatment based
Plan
expenditures
Use pricing as incentive/
disincentive in negotiations
Inbed in discussion on the
financing of the sector
Figure 2. The strategy followed to control billing and pricing of purchased hospital care
et al. 1996) contributed in broadening the range of
options that can be considered.
The key intervention, however, was the attempt at
controlling the billing and pricing structure of pur
chased hospital care (Figure 2). Initially, this was a
technical response to the budgetaiy emergency caused
by increasing costs of purchasing care in private
hospitals. A computerized system was created to
allow identification of abuse and misappropriation,
to get a thorough knowledge of the cost structure of
hospital expenditure, and to transform the principles
of reimbursement from an item-by-item to a case-mix
basis. This, in turn, must make it possible to introduce
elements of rationalization into hospital care (e.g. in
troduction of day-care) and to improve micro-level
efficiency.
Transforming the pricing system requires techno
logies and capacities that were not available in
Lebanon a few years ago but that are now being in
troduced gradually. It also requires the authority to
follow-up on decisions made possible through this
regulation technology, and to re-negotiate conditions
of purchase of care in rational treatment norms - and
despite its lack of authority, the MOH was able to
negotiate a 13% rebate on the bills submitted for
1995. This new strategy has been crucial in creating
an alliance with the NSSF, over which the MOH has
no formal control, for a common position in the
negotiation of prices with private hospitals.
A second area of intervention concerns ambulatory
health care. The beginning of the 1990s saw the first
studies on the health sector and initial attempts to for
mulate disease control programmes. A further, more
radical step was taken in 1995-96, when the MOH
negotiated contracts with NFP-NGO health centres.
In exchange for logistic support (drugs, training,
i
318
W Van Lerberghe et al.
equipment etc.) NFP-NGOs are supposed to provide
an agreed package of care for their population
(Bobadilla et al. 1994), and to introduce quality
assurance in a planned way.
With these contractual arrangements the MOH hopes
for a triple effect. First, accessible quality care would
be assured for the health centre’s population. This
answers the MOH’s preoccupation with maintaining
a social safety net for the poorest. Second, providing
quality care is expected to enhance demand for quality
care, putting consumer pressure on private care pro
viders. A climate of changed consumer-provider ex
pectations would be the best bet for rationalizing
health care provided by individual private practi
tioners. Third, gradual introduction of registration
combined with support on a capitation basis would
give the possibility of enabling health centres to make
contractual arrangements for hospital care for their
registered population. These health centres would
then have a role similar to that of general practitioner
fundholders in the UK or primary care gatekeepers
as used by some health maintenance organizations in
the USA (Enthoven 1991). Pressure for a rationaliza
tion of hospital care would then come not only from
the MOH, but also from part of the health care com
munity in the capacity of patient advocates.
With this stratep' towards NFP-NGOs, the MOH has
a first entry point in the ambulatory care market. An
overall strategy towards regulating and rationalizing
private ambulatory care is still missing. At this stage
it is very much an approach of seizing opportunities
and creating a favourable environment. As a strategy,
however, starting with the NFP-NGO health centres
offers only limited perspectives. NFP-NGO health
centres only cater for some 10% of the first level con
tacts. Fundholding in the UK, however, only covered
3 % of practices three years after its introduction, and
major expansion was decided when only 15% of prac
tices were enrolled (Petchey 1995). Thus, going by
this example, even with a small section of the market
it should be possible to wield significant influence.
LL17.6Registration of the population and capitation
payment are likely to meet with considerable resistance
(Blecher et al. 1995). The technical aspects of the con
tractual arrangements are crucial to the success of the
strategy, and still need to be tested. Politically it will
probably be difficult to introduce and enforce perfor
mance-linked incentives. Nevertheless, the plethora of
doctors is a favourable factor. With the high doctor
population ratio (close to 3:1000; Van Lerberghe
et al. 1997), a certain degree of proletarization, or
possibly even pauperization, of doctors is likely. This
would create a pool of doctors among which the MOH
could find candidates for collaboration in a supportin-exchange-for-quality scheme.
The major bottleneck in creating a regulatory capacity
and preparing the reform of health sector financing
is the lack of institutional capacity and system intelli
gence. Drastic change is unlikely in a fragmented
society such as in Lebanon, where everything is linked;
incremental change, on the other hand, would not pro
duce results without a strong sense of direction. The
MOH has had to develop and provide that sense of
direction.
The interventions concerning hospital and ambulatory
care have provided the MOH with a first set of in
struments to initiate sector regulation. In order to
capitalize on the first successes, the MOH has had
to recruit new, technically qualified staff, mainly with
an NGO or academic background. These new recruits
have brought technical expertise and a new man
agerial culture. There has been visible progress in
streamlining MOH administration and in its perfor
mance in monitoring, evaluation and planning. Com
bined with the alliances the MOH has created during
the research and documentation efforts of the first half
of the 1990s, this accelerated modernization is start
ing to pay off. The MOH now has the best, if still
very inadequate, knowledge of the situation. It is now
technically capable of commissioning and leading
studies that give an insight into the national health
accounts, health expenditure and provider patterns.
This increased system intelligence does not mean that
the MOH has the capacity to plan and implement a
comprehensive reform, but it is now in a position to
mobilize pressure for reform and to push its own
public sector agenda.
Seizing opportunities to prepare for
reform
The strategy of the MOH is not merely one of mud
dling through (Bennet and Holland 1977; Lindblom
1959), but rather of seizing opportunities to make
headway where progress or experimentation is pos
sible. The major weaknesses of this approach are that
there is as yet no clear view on the future of health
sector financing and no vision of how to restructure
ambulatory care. Delay in tackling the financing
issues is also the major criticism made by the inter
national community. This weakness, however, may
Health sector reform in Lebanon. II.
be the strength of the MOH strategy: the groundwork
is being done, and there is time for experimentation
and analysis. There will thus be less risk of import
ing ready-made solutions which are not adapted to
the Lebanese situation. This is turn will increase
chances that reforming health sector financing will
not merely aim at cost containment, but will actually
improve health care delivery. More important still,
especially in Lebanon’s fragmented society, there is
time for creating the necessary alliances. By the time
there is an overall vision of reform, not only of health
care but also of the sector’s financing, the balance
of power will have changed.
The key issue in the Lebanese health crisis is that of
the role of the public sector. Before the war this was
limited to purchase of hospital care and lip-service
to providing universal access (Hayek 1980). With the
war, there has been the implosion of the MOH and
the expansion of the private sector, presenting a situa
tion which is becoming untenable: the extent of the
problem in financing the present system is now such
that it is increasingly difficult to justify further ex
pansion for mere reasons of political equilibrium. It
seems clear now that the public sector in Lebanon
will remain a marginal health care provider but that
there is some scope to redefine its role in financing
and regulating the sector. There is thus hope that
elements of public sector rationality will be injected
into what is now, still, essentially a seller’s market.
References
Abyad A, Zoorob R, Sidani S. 1992. Family medicine in Lebanon:
the 10th anniversary. Fam Med 24: 575-9.
Beaglehole R, Davis P. 1992. Setting national health goals and
targets in the context of a fiscal crisis: the politics of social choice
in New Zealand. Int J Health Serv 22: 417-28.
Bennet AE, Holland WW. 1977. Rational planning or muddling
through. The Lancer. 464-6.
Blecher MS, Bachman MO, McIntyre D. 1995. Acceptability to
general practitioners of national health insurance and capitation
as a reimbursement mechanism. S Afr Med J 85: 847-51.
Bobadilla JL, Cowley P, Musgrove P, Saxenian H. 1994. Design,
content and financing of an essential national package of health
services. Bull World Health Organ 72: 653-62.
Enthoven AC. 1991. Internal market reform of the British National
Health Service. Health Affairs 10: 60-70.
Firkh M, Sinno Z, Ziade F. 1996. Makassed Health Programme
Health Maintenance Organisation Survey. Unpublished report.
Beirut; pp. 1-33.
Hunter D. Stockford D. 1996. Health care reform in the United
Kingdom. International Workshop on Health Care Reform at
the Frontier of Research and Policy Decisions. MOH, Bangkok;
pp. 1-41.
Hayek EF. 1980. Notre chaos medical. Essai sur le Systeme de
Same du Liban. Publications de 1’Universite Libanaise, Libraire
Orientale, Beirouth.
319
Kronfol NM, Bashshur R. 1989. Lebanon’s health care policy:
a case study in the evolution of a health system under stress.
J Public Health Policy 10: 377-96.
Lindblom CE. 1959. The science of “muddling through'. Publ Ad
min Rev 19: 79-88.
Oevretveit J. 1994. Values in European health care markets: choice,
equity and competition. Eur J Public Health 4: 294-300.
Okuonzi SA, Macrae J. 1995. Whose policy is it anyway? Inter
national and national influences on health policy development
in Uganda. Health Pol Plann 10: 122-32.
Petchey R. 1995. General practitioner fundholding: weighing the
evidence. The Lancet 346: 1139-42.
Salibi K. 1993. A House of Many Mansions. The History of
Lebanon Reconsidered. London: I B Taurus & Co.
Saltman RB. 1994. A conceptual overview of recent health care
reforms. Eur J Public Health 4: 287-93.
Van Lerberghe W, Ammar W, El Rashidi R, Sales A, Mechbal
A. 1997. Reform follows failure. I. Unregulated private health
care in Lebanon. Health Pol Plann 12(4): 296-311.
von Otter C, Saltman RB. 1991. Towards a Swedish health policy
for the 1990s: planned markets and public firms. Soc Sci Med
32: 473-81.
Acknowledgement
Part of this research was supported by a grant of the European
Union, General Directorate XII (Avicenne Project), contract
ERBAVI-CT93-0012.
Biographies
Wim Van Lerberghe, MD, PhD, is currently chairman of the
Department of Public Health of the Institute of Tropical Medicine
in Antwerp, Belgium. His field of interest is the interface between
health care organization and health care reform in Africa, the Mid
dle East and South-East Asia.
Walid Ammar, MD, MPH, graduated from the University Libre
de Bruxelles. After working as a GP in a community hospital in
Lebanon he directed a Social Security Fund and worked as a
hospital director. Since 1993 he has been Director General of the
Ministry of Health in Beirut. He lectures at the National Institute
of Administration and Development and at the School of Public
Health of the Lebanese University.
Randa El Rashidi is a Human Resource specialist at the World
Bank. Her field of interest covers social funds and the role of NGOs
in social development in various Middle-Eastern countries.
May Awar holds a Masters in Public Administration, from the
American University of Beirut. She works as an executive assis
tant in the Ministy of Health, Beirut, where she deals with the health
sector rehabilitation project.
Albert Sales, MD, MPH, started working in West Africa for the
Belgian Cooperation and WHO. He then joined the Asian Develop
ment Bank and is currently a Public Health Specialist with the
World Bank.
Abdclhai Mechbal, MD, was trained in Health Planning in Mex
ico. He is a former Technical Director of the Ministry of Health
in Morocco, and currently WHO representative in Lebanon.
Correspondence: Dr W Van Lerberghe, Dept of Public Health. In
stitute of Tropical Medicine, Nationalestraai 155, B-2000 Antwerpen,
Belgium.
SECTION - A : RESULTS OF THE FIRST ROUND
Total Questionnaire sent: 130
Total responses received: 64 (49 %)
Total responses analysed as on 26th December - 59
(The rest of the responses were received after the analysis was done They would be
included in the final Analysis. A quick look at them suggests that their inclusion is not
likely to change the results)
Age Distribution : (Range 28 yrs to 72 yrs)
35 yrs
6
35-44 yrs
16
45-54 yrs
23
54+ yrs
14
Gender: 7 females and 52 males
59
Job profile:
Sector
Academic
30
Government
32
Administrative
21
Private
7
Others
8
NGO
10
Others
10
59
59
Level:
Community
State
District or below
Centre
Medical College
International
Zone
12
15
3
10
14
5
59
North
18
South
23
East
3
West
9
Central
3
International - 3
59
Health Priorities:
The top three priorities identified based on the proportion of people identifying it as one
of the priorities were
1. Improving the quality of services under the primary health care - 75%
2. Improving medical education to suit country’s requirement - 36%
3. Setting up a disease surveillance system
- 28%
The issues that were accorded least priority were
1.
2.
3.
4.
De-linking public health and hospital services at all level and
Creation of separate public health cadre in the health ministry.
Creation of regulatory mechanism for private sector - 33%
Instituting cost recovery mechanism in health sector - 33%
- 55%
Now, let us look at the section wise comments. In all ten sections were there. Each
section has two subsections. First sub-section gives the actual results and the second has
our comments. These comments are based on the above data and the perusal of the open
ended comments given by you)
I. Medical Education : While 71% of the respondents opined that Government should
not open new medical colleges, 56% of them were of the opinion that medical colleges
should not be opened even in Private sector. Regarding the subsidy in medical education,
the group was almost vertically split with 42% in favour of and 49% against the subsidy.’
Almost 60% opined that medical education should be subsidized only for those who opt
to work in government sector or in rural areas. 85% of respondents were dissatisfied with
the undergraduate medical curriculum
Comments:
1. Opinion seems to be against opening any medical college, both in private and public
sector.
2.While the group was divided on the issue of subsidy in medical education, the opinion
seems to be that the subsidy has to be recovered by making the graduates work in the
government sector or rural areas, if necessary, by a bond.
3. Medical education system came under severe criticism. Some people appreciated the
recent initiatives of MCI, but felt more needed to be done. The issues identified in the
open section mainly pertained to
3.1 Selection criteria - caste based reservations/ need for merit/ assessment of aptitude
3.2 Upgrading the PSM/ Community medicine/public health content in the curriculum,’
coupled with a better “status” for the subject.
3.3 More skill based teaching and assessment rather than theoretical foundations.
H. Public Health Administration : Only 36% believed that Water supply should be a
part of Health ministry. Majority (75%) opined that there is no need for a separate
division of Family Welfare. An overwhelming 81% of the respondents felt that, it should
be made mandatory for government doctors to serve in rural areas for a fixed period of
service. However, 90% also felt that these people should be given major incentives in
terms of better pay scale ( even 20% higher basic pay) and preference for higher
education. 58% of the respondents did not believe that curative and public health services
should be separated at all levels. However 60% believed that within the Ministry, there
should be a separate public health cadre and DGHS should be selected from them.
Comments:
1. Need for Integration between Family Welfare and Health Division in the Ministry
was strongly felt.
2. Most people believed that government doctors should be made to work in the rural
are and major incentives should be given for the same.
3. There was a strong opinion that all people in ministry or in posts that deal with public
health ( rather than hospital) should have formal training in Public Health.
HI. Health Care Delivery System: The opinion on the performance of the current
health care delivery system was almost equally divided. Majority (64%) agreed that
campaign approach affects the heath services, its need was not doubted by 72% of the
respondents. The house was divided with roughly 45% vote on either side for the need for
vertical health programs in the country.. 78% believed that Health workers should carry
out domiciliary visits.
Comments:
1. Most people seem convinced that theoretically, horizontal programs and routine health
care delivery systems are needed. However, their confidence in the system to actually
deliver seems to be not that great. Thus, they feel that campaign approach as well as
vertical programs do have place. These measures should be restricted to major public
health problems so that some immediate impact of control measures is seen.
IV.Investing in Health and role of Subsidy : About three fourths of the respondents
believed that the government should focus only on the primary and secondary level
health care and 51% believed that Government should invest in tertiary level hospitals
/
j
“T °f ,henl (s2%) were °fOP™"” "■<» talth
services should not be provided free of cost. About 70% felt that partial cost recovery
mechanism could be instituted at primary level, 72% for frill cost recovery at secondary
level and 55/o at tertiary level with the caveat that really poor patients should be exempt
Comment:
The level of cost recovery from primary to tertiary could be graded one.
2.The need for cost recovery was justified on two grounds'
1
SSXSb”0” "°“ld res“"in be“er vaI“,i<>n of the 80ve^™'",
ii..
The resources recovered by this procedure should be used for improving the
quality of services.
3.However, it was also felt that some objective criteria for
“really poor” should be made
and strictly enforced - free of unwanted influences.
V. Health Insurance : Two thirds of the respondents believed that introduction of
insurance would increase in health care costs. Only 53% believed that poor would
upon favourably by 65% of them.
Comment:
1. The need for insurance as a protective measure was accepted by most. However the
class only6 What" ^Id^b blV"
s
ryrozvgebde ’
”y “w,s ,hefor—ity based
sVoS 0fMultipUrPOSe Workers: Two thirds of the respondents believed that MPWs
each 176% beHeVed that We have no other choice> - the
reach of other health personnel is very poor. Almost 50% agreed that the quality of
curative services by the workers was better than the “quacks” who are practising in the
rural areas. The need for better training of the MPWs with an upgradation of their status
was very strongly felt (88%). 56% of the respondents also believed that we should have a
three year medical course. 74% believed that the Male MPWs should be retained.
Comment:
1. It is quite clear that we have no choice but the MPWs, for the delivery of health care
in rural areas and to some extent in urban
slums. Therefore,
urban slums.
Therefore, we need to greatly
improve their training and skills..
&
y
2. There appears to be schism in the role of MPWs in the system. Traditionally, a
predominantly promotive and preventive role was envisaged for MPWs. To this
subsequently curative role has been added, mainly due to lack of any alternatives.
While for the first they require mainly communication skills, for the later they
require more technical skills. The scheme seems to have fallen between the two
stools. Currently, they neither have sufficient communication skills, nor adequate
technical skills.
3. It was also felt that their adequate supervision was the weakest link in the chain with
Medical Officers of the PHCs failing in this aspect.
4. There is a clear need for a complete overhaul of the system from training needs to
their status in the health system hierarchy
VII. Community Participation: Three fifths of the respondents believed that it was a
good idea to have PHCs under Local Self Governments (LSGs). 83% believed that we
should involve LSGs inPHC/CHC management. However, the respondents were
divided (43% on each side) over doctors being accountable to them. It was felt by 60%
of the respondents that the community volunteer scheme has failed. 51% agreed that we
should focus on other developmental issues like education.
Comments:
1. The consensus seems to be that community participation should be welcome and it is
time that the health sector made them equal partners. Without their involvement, it is
difficult to make much headway.
2. However, it was also felt that the Panchayats and other LSGs are not yet ready to
take upon this role. There is still too much unwanted influence on them and therefore,
doctors should-not be made -accountable to them.
3. There is a need to carry out training activities for the local leaders on health related
issues-so -that, they -appreciate -the issues involved in decision making.
4. It was also felt that the failure of the Community Health Volunteer scheme was more
because of poor implementation rather than a failure of the concept.
VIIL Private Sector: 70% of the respondents felt that NGOs and Private sector should
be allowed to adopt communities on a large scale. An overwhelming majority believed
that there should be a formal interaction between a Government Hospital and private
practitioners working in that area. 90% believed that Government should take tough steps
to ban the practice of unqualified practitioners of medicine. 50% believed that we should
carry out training of unqualified practitioners. The need for an accreditation system for
both private and public sector was thought to be equally important by an overwhelming
majority of the respondents.
Comments:
1. An important role of private sector was envisaged by most. However, it should be
restricted to qualified people only. But knowing the realities of India, they also felt
that thisunay^-not-be-possible4o implement. Therefore, we should train the existing
practitioners, irrespective of qualifications.
2. The need for government hospitals to regularly interacLwith the private, practitioners
waS-Yery strongly .felt. This way it could serve both the training and the monitORng
needs of the private sector.
IX. Modern Technology j 78.%^agreed that increasing use of modem technology is a
welcome step. However, 93% believed the inappropriate use of this technology has
increasedlhe health care costs. 72% felt that, as a step towards makingdhU-technology
available to all. Government should invest in modem technology. Half of the
respondents believed that doctors of Indian System of Medicine should he posted at
PHCs.
Comment:
1 The need for investing and using modem technology in health care was strongly felt
by majority ofihe respondents. However,They felt very strongly that there should he
some control over the use of technology. Most of them suggested an independent
body at central and local levels for deciding on policy of allowinglhe use of newer
medical technologies, based on some objective assessment
2. Included in this was issue, related to Indian System of Medicines. Majority-felt that
they should be encouraged. Though as a trial such facilities should be provided at
CHC level rather than at PHC level.
X.Others: 69% of the respondents disagreed that we should close the national level
institutions. 61%_felt lhat the priorities identified by the international agencies wgre not
the real needs of the countiy. 85%. felt that a Disease Surveillance system should receive
top priority. 67%_felt thaLeven Government Institutions should be brought under
Consumer Protection Act (COPRA). Only 36% agreed that our health services have
focused on MCH services at the cost of others.
Comment:
1 The consensus seems to be that the national Institutions have not really performed
well. Though, this does not mean that they do noihave a role but that they should be
strengthened.
2. The Disease Surveillance system should receive top priority was also reflected in the
list of priorities.
]
Areas of Consensus: ( defined as > 75% responses)
1.
2.
3.
4.
5.
Improving the quality of Primary health care services
Reassessing the role and the training needs of MPW
Increasing community participation at local level
Revamping the medical education for the country’s needs
Making rural posting compulsory for government doctors with a concomitant
incentive in remuneration
6. Instituting Cost recovery systems in Government sector
7. Formal channel of Interaction between Government hospitals and private doctors in
that area
8. Practice by ‘"Unqualified “ practitioners to be banned
9. Setting up an Independent body for assessment of introduction of technology at
various levels.
10. An accreditation system for both Government and private hospitals
11 COPRA to cover both private and government hospitals
12. Setting up an disease surveillance system
Aregs of Clear Discord (defined as both sides having > 35% responses)
1.
2.
3.
5.
6.
7.
8.
Subsidy in Medical Education — Whether it should continue or not
Role of vertical versus horizontal programs
Training of Unqualified practitioners
Water supply to be part of Health Ministry
Health Insurance’s role in protecting the poor from the medical costs
Doctors being accountable to Sarpanches/ Zila Parishad Chairman etc.
Too much focus on MCH services
1
Section — B — Your Response needed
.
ou have read the report. You may have had your own priorities. Now that the group
has identified the priorities, we want that you should respond to the list Whether you
agree or not, we are interested in receiving your comments. If you agree, please write
very briefly why you agree and if you do not, then why not? Please restrict your
comments to the box provided
1.Improving quality of services under the primary health care
2. Improving medical education to suit country’s requirement
3. Setting up a disease surveillance system
2. We would now like you to please give three most important steps that needs to be
taken in order to achieve these objectives.
1 .Improving quality of services under the primary health care
2. Improving medical education to suit country’s requirement
3. Setting up a disease surveillance system
THANKS FOR RESPONDING AGAIN.
CENTRE FOR COMMUNITY MEDICINE
ALL INDIA INSTITUTE OF MEDICAL SCIENCES, NEW DELHI
201H January 20001
Dear Colleagues,
We take this opportunity to wish you all a HAPPY NEW YEAR 2001.
11
S S‘ eat pjeasure to share with you the results of our first round of Delphi Survey
on Health priorities for India”. This was possible entirely due to the response from all of
you. We received responses from a wide range of people from academicians to
grassroots workers, from local NGOs to International agencies.
We are aware that you would be very keen to go through the report. It would be obvious
from the report that we need to go further than what we did in the first round. Some areas
have been identified where we would like to probe more deeply and request you to
respond again. We would be eagerly awaiting your responses as you so wonderfully did
m the first round.
We hope to share the results of the foil survey including the second survey during the
Indian Public Health Congress to be held in Delhi in mid April 2001. We have written to
them in this regard. We therefore, request you to kindly respond at the earliest so as to
give us time to analyze the data for presentation. We look forward to receive your
responses by 28th February. As always, your contribution will be duly acknowledged.
Thanking you in anticipation.
With Warm Regards.
Dr. K. Anand
Dr. S.K. Kapoor
Enclosure . Section — A ; Results of the first round
Section- B : Questions for tne second round
fa
C.S. Pandav
DES NO.
government OF KARNATAKA
I
1
'Ip.,
1111
I
H t X-
r&
•w-
M’
’.v’ylWX; X
4. '•
STATISTICAL abstract
OF
KARNATAKA
1983-84
%r'.
i
ti 'i
!
I I
■
fr ‘
’
’
I
V
'Ww\
ri-l,
TK'
I
M
directorate of economics and statistics
BANGALORE
'i
te
579
Ily-
XXVIII - PUBLIC ICALTII
Table No. 28.1 HOSPITALS {AND DISPENSARIES BY MANAGEMENT, 1979 - 81. (contd.J
(in No.)
■.
State Government
Year/
Division/
District
1
Subsi Primary
Health
diary
Units
Health
Centres +
Hospi- Primary
tals Health
Centres
269
300
305
315
328
1152
1215
1274
1244
1303
E.S.I.
Hospi- Dispentals saries
Hospi- Dispentals saries
13
13
13
13
13
11
11
11
11
11
140
137 a
136 8
137
137
I. BANGALORE DIVISIO?^
32
92
9
446
7
4
1. Bangalore
2. Chitradurga
3. Kolar
4. Shinoga
5. Tumkur
12
2416
18
14
20
2 .
2
4
5
2
1
1
113
82
79
87
35
87
13
257
c
n
11. BELGAUM DIVISION:
2
2
106
n
106
106
106
ws
2
2
Hl
2
1
1
6. Belgaum
7. Bijapur
8. Dharvad
9. Uttara Kannada
4
6
11
6
25
23
26
13
2
3
6'
2
78
66
72
41
HI. GULBARGA DIVISION:
21
64
13
181
1
10. Bellary
11. Bidar
12. Gulbarga
13. Raichur
11
3
4
3
.13
11
22
18
2
3
7
1
42
32
56
51
4
IV. MYSORE DIVISION:
57
85
15
419
5
12
4
22
2
12
11
19
13
6
13
23
4
3
4
62
93
78
11
70
105
14. Chikmaga1ur
15. Dakshina Kannada
16. Hassan
17. Kodaqu
18. r
19.
197
198(
198
198'
1983
1983-
7
1979- 80
1980- 81
1981- 82
1982- 83
1983- 84
1983-84 :
50 +
50
1
1
HI 11. BELGM D
15
6. Bel gaum
7. Bijapur
8. Dharwad
9. Uttara
7
1
6
1
11
3
1
3
2
1
p
5
3
IB
9
i
1
7
2 •
1. Bangal
2. Chitra
3. Kolar
4. Shieog
5. Tumkur
5
4
2
1
B.
|i£?;lll. GULBARGA D
'IBfc
ISt' ww-I
1
I
11. Bidar
12. Gulbar<
• 13. Raichur
®|.». MYSORE
D1VI
—
I'
.....
B; 14, Chiknaga
15. Dakshina
SV ’ I6* Hassan
17. Kodagu •
•?)
|8||t IS. Mandya
■>
2
2
Y
Div
Dis
■'3
Central
Government
6
5
4
3
' 2
<
.
■
■
aBfe-.-- I9, Mysore
-------
ii
Decrease
■I S and
1981-
50 PHUs. |i
strenght h
BH': * One Hospit
Directorate
.Jr' Karnataka,
■i »V-
• s'<A-
■
600
Table No. 28.1 HOSPITALS AND DISPENSARIES BY MANAGEMENT,
1979 - 84. (concld..)
(in No.)
■1.3
No.)
■
E.S.I.
Year/
Division/
District
' -A
—w
■I'. I
—- - ■ '3
2
2
2
2
2
106
106
106 ; ; 4
1'
so;
L. 3 / ;
Hospi- Dispentals
saries
Hospi- Dis pen
tals
saries
1
10
11
12
15
233
233
233
233
233
1636
1730
1794
1804
1676
-751'! '
-HKt
85
85
85
65 »
65
I. BANGALORE DIVISION:
33
25
13
4
86
642
1. Bangalore
2. Chitradurga
3. Kolar
4. Shimoga
5. Tumkur
32
13
1
1
10
8
2
4
1
2
58
4
15
7
2
206
107
108
114
107
II. BELGAUM DIVISION:
’2
21
13
44
373
6
2
3
10
5
1
5
2
9
8
18
9
118
95
113
67
2
3
26
283
1
1
1
13
4
6
3
67
48
92
76
77
558
5
48
7
26
4
17
79
129
98
25
88
139
1
III. GULBARGA DIVISION:
2
5
10. Bellary
11. Bidar
12. Gulbarga
13. Raichur
1
3
1
.
3 ' :
ll
.5-::5 ’b
.4
■5
3 -J
LOB
■ '1
i
•13
13
43
43
43
11
11
11
11
11
7V f
IV. MYSORE DIVISION:
1
1
■
1
1
1
1
3
14
15
4
6
3
4
3
2
1
i
i
f- -LU
•
■
■!1
14
•37
40
41
40 *
40
I - ir
«
13
1979- 80
1980- 81
1981- 82
1982- 83
1983- 84
1983-84 :
MBb
■
' '‘Si
1
Hospi- Dispenlals
saries
6. Belgaurn
7. Bijapur
8. Dharwad
9. Uttara Kannada
■
1
Total
I
■
1
Organisations
5
■
’"’X
Departments
' 3'
?
; x
J
I
■t. wi w
14. Chiknagalur
15. Dakshina Kannada
16. Hassan
17. Kodagu '
18. Mandya
19. Mysore
2
1
2
1
8
2
1
Note : 3 Decrease in No. of Stale Government Hospital s During 1980-81
and 1981-82 is due to the fact that they were taken over by other depts
+ 50 PHVs. Were upgraded.as subsidiary health centre ( Along with the bed
strenght ) during 1982-83.
* One Hospital A 20 Dispensaries were taken over by the State Government.
Source: Directorate of Health and Family Welfare Servu-s, Government of
Karnataka, Bangalore.
-J
84
■ ■□gl
W
|
601
f Bl
■.fri
Table No. 2fi.2 MEDICAL INS1IHHI0MS IN RWAL AND URBAN AREAS, 197? - 04. (could..)
K'l
K-'1
ite1'
(in Ho.)
Year/
Division/
District
■ 1
Rural
Urban
Rural
Ur ban
Rural
Urban
Rural
Urban
1
2
3
4
5
b
7
3
?
1979- 80
1980- 81
1981- 82
1982- 83
1983- 84
33
33
33
■ 33
33
.
155
155
155
135 i
135
7
7
7
?
7
4
4
4
4
*
72
13
76
1
3
50
4
8
7
1
1
4
1
2
6
-
10
6
2
58
7
3
7
5
26
3
10
18
18
6. Belgaum
7. Bijapur
8. Dharwad
9. Uttara Kannada
3
2
1
7
2
4
1
4
7
9
6
HI. GULBARGA DIVISION:
1
20
1
10. Bellary
11. Didar
12. Gulbarga
13. Raichur
4
9
3
5
3
1
IV. NYSORE DIVISION:
23
3?
10
4
5
8
4
1 '
1 •
g
*
1
1. Bangalore
2. Chitradurga
3. Kolar ,
4. Shimoga'#^
5. Tumkur
IL BELGAUH DIVISION:
A
14. Chikmagalur
15. Daksbina Kannada
16. Hassan
17. Kodagu
18. Mandya.
19. Mysore
I
Sfe.
i
1983-84 :
I. BANGALORE DIVISION:
.gw
•'Yl
29 ' 49
47
29
4?
29
'W
29
49
2?
14
14
14
14
14
157
157
157
157
157
K
s
' ft.n--'
■
Private
Government
Private
Government
Hift
Dispensaries
Hospitals
1
K--’
. .... Efe','..-.
■iW
;'
I ’
2
|„ £>
1
**
n
9
1
3
19
3
3
7
1
6
5
1
1
1
22
3
1
2
1
5
1
14
8
4
2
3
3
2
12
1
i®
■ 4 7;.:
6
1
9
2
5
2
1
1
1
13
2
2
5
3
1
9
3
3
■i
It'
K
I
I
h
JSv
siv
lit
IB,
i
I®
7
Ilk
I’
■J
___-
'
■
■L
s
B
“
-r—7
'■^1
602
..
V
’
•
Table No. 25.2 MICf-L INSIIIUIIONS IN RURAL
AND UPr.U fFEAS, 1979 - 84. (concld.J
(in No;)
Yr;-1 /
Division/
District
Primary Health Centres
Subsidiary Health Centres
and Primary Health Units
Government
Urban
4 ,'v
-
4
A ■
Rural
Ur bin
1
10
11
1979- fO
1980- 81
1981 82
V02-83
' 1983-81
1255
1348
1409
1419
1191
166
167
170
190
199
I. BA.NGAL03E DIVISION:
474
73
1. Bangalore
2. Chitradurga
3. Kolar
103
89
90
94
93
36
11
11
7
11. BELGAUN PIVISIOU:
317
40
6. Belgern
7. Dijapur
8. Dhar^ad
9. Uttar a Kannada
93
89
90
52
10
12
11
III. GULBARGA DIVISION:
231
23
10. Bellary
11. Bidar
12. Gul barga
13. Raichur
47
44
79
63
10
IV/ MYSORE DIVISION;
467
52
70
113
90
13
75
106
7
2
5
4
10
24
>•7
1983-81 :
3
1
2
4. Shir?o■a
5. Tuml 'ir
1
: i ’ 1
. ■ wa
14. Chikmagalur
15. Dakshina Kannada
16. Hassan
17. Kodagu
18. Mandya
19. Mysore
8
A
/
2
6
7
Note : + Reduction as a Conseqence of taking over of 20
Dispensaries run by 'Other Departments’ by
State Government.
Source: Directorate of Health i Family Welfare
Services, Government of Karnataka, Bangalore.
»
■
«-
fe4"
^03
^Table NO. 28.3 BED STRENGTH IN HOSPITALS ETC.., 1979 - 84. (coiftd..) .
(in No.)
Central Govt. E.S.I. ‘ Other Dept.
State Governaent
Year/
Division/
District
Hospi- Primary Subsidiary Primary Hospi- Dispentals Health Health
Health
tals saries
Centres Centres Units
3
20068
19830
19099
19490
19607
2552
2744
3003
3226
3342
107
123
1. BANGALORE DIVISION:
7325
1275
2
1. Bangalore
2. Chitradurga
3. Kolar
4. Shiaoga
5. Tumkur
4015
1420
878
625
387
325
306
281
136
227
2
II. BELGAUM DIVISION:
3413
644
28
6. Bel gaum
7. Bijapur
8. Dharwad
9. Uttara Kannada
830
601
1655
327
174
212
180
78
28
III. GULBARGA DIVISION:
2591
416
10. Bellary
11. Bidar
12. Gulbarga
13. Raichur
1294
308.
774
215
108
66
132
110
IV. MYSORE DIVISION: *
6278
428
14. Chikmagalur
15. Dakshina Kannada 1569
582
16. Hassan
1142
x 17. Kodagu
350
18. Mandya
2207
19. Mysore
1979- 80
1980-81
1981- 82
1982- 83
1983- 84
8
7
b
5
4
2
Hospi- Dispentals saries
'.s
if w
9
2023 1730
2023 1730
2436 1730
2531 1730
2798 • 1730
438
438
138
438
438
1031
1269
2154
2109
2109
328
328
328
126
126-
837
1472
414
1975
16
244
94
103
205
191
1170
414
1825
687
137
I;
•Mb
1983-84 :
I. BA
302
24
150
16
56
96
f »
BEL
27
192
176
169
150
137
18
534
25
46
26
12
41
89
294
110
25
6
1007
75
740
96
134
162
98
104
171
338
18
39
10
74
68
243
8
234
121
32
24
24
20
96
32
26
b
32
37
1.
2.
2
4.
5.
1
-
6. E
7. E
8. D
9. U
HI. GULE
!
•10. E
11. B
12. C
13. R,
IV, MYSOR
14. Ch
15. Da
16. Ha
17. Ko.
18. Mar
19. Mys
>------------Source: Dire
Kar,
.■Qi
s
■w
-'i
.:9-
:
V
604
1
H
Table No. 28.3 EES STRENGTH IN HOSPITALS ETC.. 1979 - 84. (cancld.J
(in No,)
IM
Dispensaries
-T
9__
*328
Year/
Division/
District
Private
Total
Hospi- Dispentals
saries
Hospi- Dispentals
saries
1
10
1979- 80
1980- 81
1981- 82
1982- 83
1983- 84
6408
6408
6408
6584
6584
4
4
4
4
4
29237
29237
29391
29913
30030
I. BANGALORE DIVISION:
2630
4
1. Bangalore
2. Chitradurga
3. Kolar
4. Shimoga
5. Tumkur
2224
4
II. BELGAUM DIVISION:
11
12
Of Which
Rural
Urban.
I
!
13
14
15
5345
6209
6432
6831
5220
5406
5622
5864
6134
25368
29368
29978
30481
30727
13402
2548
982
14968
’420
987
400
387
386
357
418
292
126
170
202
192
9929
1694
1752
980
613
1268
4874 .
1479
1643
4710
6. Bel gaum
7. Bijapur
8. Dharwad
9. Uttara Kannada
719
53
446
50
1549
636
2262
377
393
388
409
289
921
152
338
232
1021
922
2333
434
III. GULBARGA DIVISION:
142
2804
968
723
3049
10. Bellary
11. Bidar
12. Gulbarga
13. Raichur
50
92
1345
358
886
215
149
161
426
232
176
101
298
148
1318
418
1014
299
IV. MYSORE DIVISION:
2544
8950
1836
2786
8000
428
3564
732
1231
. 376
12619
226
281
351
104
415
112
1557
261
359
229
268
542
2288 ’
822
976
562
2810
:
328
:
2.
126-
5537
I1
1983-84 :
■ 16
356
50
825
■
27 ■ ' / r k
32
37
-■
- 1
. "J
" I
II
■I
' 1
'S" J
'■ '• 'iI
• 1
ag|
i
14. Chikmagalur
15. Bakshina Kannada 1995
16. Hassan
17. Kodagu
150
89
18. Mandya
19. Mysore
$
310
459
□uiirce: Directorate of Health and Family Welfare Services, Government of
Karnataka, Bangalore.
I
.
I
K ■
■ J.
«-
1R-'
I
1^
It
1 ,'A
605
Table No. 28.4 MEDICAL INSTITUTIONS, FOR SPECIALISED KEAWENT, 1979 - 81.
rear/
Division/
District
f
1
Health
Leprosy
LB.
■
I"
(in No.I
i
Cancer
HospiBed
Bed
Hospitals
Bed
HospiBed
Hospitals Strength
Strength tals Strength tals Strength
3
2
4
6
5
7
9
8
13
13
13
13
13
2644
2644
2674
2676
2676
1
1
1
1
260
260
260
260
260
I. BANGALORE DIVISION:
5
1143
1
'•260
1. Bangalore
2. Chitradurga
3. Kolar
4. Shimoga
5. Tuakur
3
1 .
1
Z19
80
264
1
260
II. BEL6AVM DIVISION:
3
525
1
375
1
110
6. Belgaun
7. Bijapur
8. Dharvad
9. Uttara Kannada
1
1
1
363’ .
100
62
1
375
1
110
III. GULBARGA DIVISION:
1
288
10. Bellary
11. Bidar
12. Gulbarga
13. Raichur
1
288
IV. HYSC^E DIVISION!
4
720
2
150
1979-80
1980- 81
1981- 82
1982- 83
1983- 84
j
2
2
2
2
2
1260
1260
1260
1260
1260
1
1
2
2
2
EC!)
200
275
310
310
1
885
1
1
885
1
1. Inf
2. Neo;.
tW'
I®'-'
3. Endc
meta
200
IIf
4. Dise
form
ECO
rW’
5. Hen!
1983-84 :
r
ft
B.
Bb
6. Disc;
sense
■i
7. Disej
14. Chikraagalur
15. Dakshina Kannada
16. Hassan
17. Kodagu
18. Handya
19. Mysore
ft' 6. Di sea
...... .
w
■
w"
9. Disea
10. Di sea?
syster
11. Compli
birth
12. Diseas
subcul
13. Disease
system
V 14. Congent
15. Certain
Rorbidi
1
1
100
. 470
Source : Directorate of Health and Family Welfare Services, Government of Karnataka, Bangalore.
| 16. Symptom;
conditic
17. Accidentviolence-
TOIL
Source:
|«l
-
•
■
"
■
■ £______________
H'
606
■w
!
•;:‘O
'!wa
Table llo. 28.5 rnWHIS lIT-'fllED IN HOSrilALS AND DIWWMJES W CAUSES 1779 -83.
.
•* .
V* •’
->1 ••
I
(In no.)
Fed
snglh
S
9
"
Causes
-- 1
ECO
209
275
/
-
i
310 "al
3K)
1
200
I
ZOO
I^B
110
110
-
r
«■
1979
1980
1981
1983
1983
2
3
4
5
6
1. Infective amt parasite I'irmses
1664029
1101912
1243632
1012292
741126
5765991
2. Neoplasms
44391
72633
83-30
30347
46281
2772.^2
3. Endocrine nutritional and
metabolic Diseases
281711
176161
24J74?
198531
111519
1012171
4. Diseases of Blood and Blood
forming organs
660292
449673
516i?6
475977
575205
2677783 .
5. Mental Disorder
28848
56711
27376
8992
528748
650V8
6. Diseases of nervous sys:??. and
sense organs
71238?
401118
313327
245367
2175721
7. Diseases of circnlalery system
207038
1178")
roiss
131034
178118
811353
8. Diseases of Respiratory system
2141931
11825:2
13671n2
1030779
659528
63875-12
9. Diseases of Dig-stive Systn
2278116
351217
410157
302630
2262jI
73S8113
10. Diseases of Gsnito Urinary
system
11. Complication of pregnanty child
birth and the puerperi^
1583C2
9:025
1C2830
71707
821v-
515210
162038
25052
19L^
86315
101571
567037
415604
410301
50-336?
233580
193?*;?
1815213
Tola)
Mi
■
.
• "
-
t
■wl
12. Diseases of skin and
subcultaneous tissue
13. Diseases of the musculosklnlal
system and connective tissue
14. Congential Anomalies
15. Certain causes of perinatal
morbidity and mortality
16. Symptoms of ill Defined
conditions
17. Accidents poisionings and
violence (External only)
—
ore.
•■•■rV’W?
T01AL 1 to 17 —>
I,
f!
j
j
255133
130012
133101
93129
38073 ‘ 650078
5585
5141
6741
2376
1287?
32943
<
18965
11114
22657
77651
47563
177955
117539
96242
143996
731357
573311
1662975
1022290
1157219
1337056
522820
515301
455468? '
10209302
5877863
6967903
33/6084
4899267 3333341?
Source! Directorate of Health and Family Welfare Services, Government of Karnataka,
Bangalore.
•1
■ I
I;
Si
607
V ■
Table No. 28.6 FAMILY WELFARE PROGRAMME AND USERS OF CONTRACEPTIVES, 1979 - 84.
(conld..)
Tabi
f-
(in No.)
Sterlisations
Year/
Division /
District
Family
Welfare
Centres
Achievement
Target
Vasec
tomy
Tubectomy
Total
X
I
1
2
3
1979- 80
1980- 81
1981- 82
1982- 83
1983- 84
400
428
428
503
5l6
166000
190400
190400
305000
417000
4
5
6
5584
4785
- 2498'
2332
5060
111583
138111
186322
230682
234829
117167
142896
188820
233014
239889
J-
1983-84:
b
II
198:
1.
I. BANGALORE DIVISION:
169
137700
1173
892E5
81378
1. Bangalore
2. Chitradurga
3. Kolar
4. Shimoga
5. Tuakur
70
24
22
25
55100
20000
21400
18650
22250
431
7?
554
42
67
30108
11581
13267
10861
13807
30537
11660
11121
10'/L’6
13874
II. BELGAVM DIVISION:
132
105650
1770
60710
39
32
43
18
33500
27000
33100
12050
170
1005
411
133
1958?
13726
21417
6178
1977?
147.7.2 ’
213.3
6311
II1.GULBARGA DIVISION:
89
71350
623
27318
28171
10. Bellary
11. Bidar
12. Gul barga
13. Raichur
21
15
30
23
16750
11200
23350
20050
138
200
167
98
7352
5296
7176
7724
75 '0
51:-6
73'3
7822
IV. MYSORE DIVISION:
126
102300
1494
66146
67610
IV. MY'
13
31
18
9
17
38
10200
26700
15200
5200
15900
29100
145
585
293
23
109
339
8427
11337
12324
3165
13351
17542
8572
1197?
12617
3183
13460
17881
14.
15.
16.
17.
18.
19.
6. Belgaua
7. Bijapur
8. Dharwad
9. Uttara Kannada ’
14. Chikusagalur
15. Dakshina Kannada
16. Hassan
17. Kodagu
18. Mandya
'• 19. Mysore
28 ■
1
i
3
4
5
B,
II. F
wr
S’
I.
1
6
7
8.
9
■
III.GUL
K
10
11
12
•13
^4'
Source:
_
H"
________ .
_
608
Table No. 28.6 FAMILY WELFARE PROGRAHHE AND USERS OF CONTRACEPTIVES,
(concld.J
79 - 84.
1 uD
Year/
Division /
Total
Esti»ated
C.c.Users C.C.Users
(Target) (Achieve-
Rent
■
6
1
7
8
9
117167
142896
188820
233014
239839
1979- 80
1980- 81
1981- 82
1982- 83
1983- 84
67000
55000
55000
102000
170000
50776
54657
55448
68877
97097
79400
123600
123600
136000
170000
83285
88293
89236
94165
108865
I. B^NGALOHE DIVISION:
MOO
39915
56100
28072
1. Bangalore
2. Chitradurga
3. Kolar
4. Shir-oga
5. Tunkur
22850
8250
8800
• 7700
9200
19050
4192
7324
3214
6135
22600
8150
8700
7600
9030
8191
2613
5613
4375
6915
11. BELGAtfl DIVISION:
43600
18146
43050
25423
6. B^.guM
7. Bijapur
8. Dharvad
9. Uttara Kannada
13800
11150
13650
5000
6857
4013
4490
3086
13650
11000
13500
4900
7014
7626
6623
4158
28171
III.GULBARGA DIVISION;
27400
9155
29100
19915
73 *0
51-6
73-:3
7822
10. Bellary
11. Bidar
12. Gulbarga
13. Raichur
6900
4600
7650 •
8250
3446
1193
1925
2591
6800
4550
9550
8200
5271
2015
5211
7418
IV. MYSORE DIVISION:
42200
29581
41750
35455
4200
11000
6300
2150
6550
12000
3248
4420
4183
1525
7109
9096
4200
109W
6200
2100
6500
11850
4536
6358
4615
2585
7303
10058
fe--|
-
i
I
1983-84:
81378
30337
116'0
11121
10306
13874
- S3
—Sfi
i
"f 3I
197/7
1473.2 •
213:3
63H
67640
8572
4 rrrn
1I
12617
3188
13160
17881
■
■ .
14. Chik»agalur
15. Dakshina Kannada
16. Hassan
17. Kodagu
18. Mandya
19. Mysore
Source: F*
Directorate of Health and Family Welfare Services, Governffieni
of Karnataka, Bangalore.
B5
<
«
609
ilF
Table No. 28.7 STERILISATIONS CONDUCTED, 1979 - 84.
F
k-i• £3
(in No.)
Category
1979-80
1980-81
1981-82
1982-83
1983-84
1
2
3
4
5
6
i
¥
f
I1I-
STERILIZATION COtWCTED
I. By Religions
117142
142896
189820
233014
239889
a. Hindus
b. Muslifis
c. Chirisians
d. Sikhs
e. Others
f. Not Known
103831
6247
2024
28
278
4734
126924
8408
2693
18
148
4705
168878
12572
3260
25
£ 306
4779
179279
13879
3502
70
563
35721
213645
18083
6437
42
374
1308
II. By Educational Status:
117167
142896
188820
233014
' 239889
a. migrate
b. Primary
c. Middle
d. Secondary
f. College A Above
g. Not Known
62089
22217
13907
10430
2601
5923 |
72784
41151
12356 ■
9262
1778
5565
133714
23171
14894
9712
2662
4667
140053
26287
16880
10329
2589
36876
.21552
74333 *
24307
14881
2782
2034
Ill. By living children:
117167
142896
188820
233014
239889
a. 0
b. 1
c. 2
d. 3
e. 4
f.5 and above
g. Not Known
82
2228
21638
40223
29727
17841
5428
19
1538
23843
51072
3796&
23339
5119
29
1986
35403
.67692
45848
33649
4213
141
3796 •
•10814
69991
47183
35006
36080
20
4917
54519
85862
55573
37468
1530
t
B8
r.
A. Malar
1 No. O'
A. Total
B. Attac
C. Const
D. Manit
2 No. o<
A. Colk
B. Exani
C. Posit
D. Treat
E. Death
3 (a) No
spra
iii.
■ i: ■
1 W"’"'
1 Bf.
if
WV! w-
| hB'"
Note : » Includes Literates but not completed primary level.
<■* Includes persons Whose Education Status has not been stated.
Source: Directorate of Health and Family Welfare Services, Government of Karnataka,
Bangalore.
!F
(b) NO. L
iii.
II Schoola. No. of
b. No. of
c. No. of
d. No. Ex
e. No. Fo
f. No.of
i. D
ii. F
iii. S
iv. T
2 Tubercu
Note: 1
■j
Source:, D
B
Bb
_•
610
Table
No. 28.8 PUBLIC HEALTH COVERAGE UNDER MAJOR PROGRAMMES, 1979 - 1983.
z
Item
1979
1980
1981
1932
1983
2
3
4.
5
6.
19.13
19.13
19.13
19.13
19.13
r
A. Malaria (in thousand )!
13645
18083
6437
42
374
1308 .
39889
21552
74333 ♦
24307
14881
2782
2034 **
1 No. of Units in Different Phase:
A. Total
B. Attack Phase
C. Consolidation Phase
D. Manitenance Phase
3.57
15.56
3.57
15.56
3.57
15.56
3.57
15.56
3.57
15.56
2 No. of Blood Smears ( in ’000 I:
A. Collected
B. Examined
C. Positive Cases
D. Treated
E. Deaths
4283
4109
277
258
Nil
4722
4491
225
205
Nil
5268
5162'
158
144
Nil
5198
5198
102
96
Nil
5485
5485
62
59
Nil
3 (a) No. of Structure Targeted for
spraying (in ’000)
i. DDT
ii. BBC
iii. Malthion
4460
4665
679.
4513
2822 ‘
662
4973
2210
742
5624
5407
- 894
15025 .
12375
1522
3146
1957
404
3131
1511
471
3917
3911
570
8975
7306
697
105
1461
84000
30988
7119
300
22577
781140
80427
8741
90
8270
306065
63453
13421
90
90/5
312750
22283
3103
90
9091
323800
34633
2689
24260
283348
113668
.93655
73011
20827
7622
3997
246036
23324
117232
102746
10177
37192-
74283 ’
7237
71295
71736
8723
33426
■
(b) NO. OF STRUCTURE SPRAYED (IN ’000) :
3525
i. DDT
3539
ii. BHC
510
iii. Malthion
39889
20 ■
4917
>4519
45862
>5573
J746B
1530
?■
(
II School Health Progam^e:
a. No. of PHCs Selected
b. No. of Schools Selected
*
c. No. of Trageted Children
d. No. Examined
e. No. Found Defective
f. No.of Children Immunised Against:
i. Diptherja & Tetanus
ii. First Doze
iii. Second Doze
iv. Third Doze (Booster Doze)
2 Tuberculusis
<ataka,
Note: 1. Since state ^as delcared free frorv 'Snail Pox' during May 1974 due item
has not been included.
Source^Directorate of Health and Family Welfare Services, Government of Karnataka,
Bangalore.
1
1
■
■
'
1
a
I
611
Table No. 28.9 MEDICAL AND PARA MEDICAL PERSONNEL,
1979 - 84. (contd..)
(in No.
)
i
1979-&0
1980-81
Parlicualrs
Pari
Sanctioned Position
1
Sanctioned Position
2
3
1 Doctors
2910
2696
2960
2730
1 Doctors
2 Dentists
91
90
91
78
2 Dentists
3 Staff Nurses
2839
2777
2839
2777
3 Staff Wur
4 Compounders /
Pharmacists
1985
1626
1985
1495
4 Compounder
Pharmacist
5 Midwives /A.N.M.s
5690
5600
5786
5435
F 5 Midwives /
6 Lady Health Visitors
920
860
920
860
6 Lady Healt
7 Health Inspects.
1170 +
1170 +
1170 +
1147 +-
7 Health Ins
8 School Health
Assistants I
105
105
9 Laboratory\Technician
882
835
832
835
9 Laboratory
10 B.C.6.Technicians
137
131
137
130
10 B.C.G.Teci
11 Heath Visitors (IB)
50
50
5?
58
. 11 Heath Vis;
12 X-Ray Technicians
140
120
145
117
R 12 x“Ray Tect
13 Other Para-Technical
Personnel
N.A
N.A
N.A.
N.A
13 Other Par?
Personnel
________
4
5
I
Hea
Assistants
<
® Note: +* perta
Incluc
■..7
A’.
K.
1I • •
■
•<:
M&v
BCG te
Hence
8 Fall i!
Willin
$ The po
Scheme
Mot Avr"
■Source: Directs
B'
K fcI■S'
■
'J
■
1
.
.A
TT» .
5” ' . I
IS
O
■■
■ P1' r-5- ■ •
Bii
___
ll■
. '
‘ 612
■
Table ho. 28.9 hEDICAl AND PARA iOICAL PERSIHIEL, 1979
I
■
- 84. (conoid..)
..
(in No.)
1981-62'
1982-83
Particualrs
Sanctioned Position
-I
1
M
i
■ s
;5
Sanctioned Position
I
7
8
9
10
11
2960
2730 3
1384
3299
4725
4157
91
73
130
51
131
91
3 Staff Nurses
2862
2797
3074
3065
3204
3114
4 Compounders /
Pharmacists
2077
1587
2043
1749
2169
1795
5 Midwives /A.N.M.s
7624
7074
7924
7574
8380
7458.
6 Lady Health Visitors
1030
890
1115
890
1215
916
7 Health Inspectors
975 *
905 »
981 J
984 *
984 «
964 #
2 Dentists
■
Sanctioned Position
6
1 Doctors
1
1983-81
j.
i
■
\
8 School Health
Assistants $
9 Laboratory Technician
882
835
■ 969
10 B.C.G.Technicians
135 #
130
135
130
125
120
11 Heath Visitors (IB)
59
57
59
59
j?
.5?
147
127
185
127
185
'105
6507
7514
6507
7514
12 X-Ray Technicians
; ' Si
i
13 Other Para-Technical
Personnel
■a.—-—
- ■ J
Th
Bl
31?=’
. 7514
835
1026
830
•
I
; -|b
J
■■
|i
I
I
« !
. 'lhI
6507
Note: * Pertains to only Senior Health Inspectors.
4
1jn5pector5 (TB)’ SR* Hcallh Inspectors, SR A JR Non-lledial Supervisors,
BCG technical Leaders (Broadly dassifed under one head Viz., Health Assistants (Male).
Hence the difference in No. sanctioned and in position.
» Fall in Sanctioned Strenght During 1981-82 is Due to Abolition of 2 Posts in Lady '
Willington TBTDTC, Bangalore during 1981.
$ The post was Abolished Since 1.4.1980 and was merged under Multipurpose workers
Scheme as Health Workers (Females).
N.A. Not Available.
Source: Directorate of Health and Family Welfare Services, Government of Karnataka, Bangalore.
1I
I
I91
/
■
J
I
‘K
w
K
613
ftI:
I
’ Table No. 28.10 EXPENDITURE ON MEDICAL i HEALTH SERVICES, 1979 - 81.
I
i"
(Rs in lakhs)
Particulars
1979-80
1980-81
1981-82
1982-83
1983-84
1
2
‘3
4
5
6
Parti
1 Medical Relief
2 Medical Education^
Training & Research
2329.49
485.75
2605.12
566.73
3527.45
579.52
4060.31
774.35
4190.07
765.34
1. Ag:
3 E.S.I. Scheme
4 Ayurvedic
5 Homoepathy
6 Unani
7 Sidda & Other Systems
8 Stores
9 Others
385.68
117.82
2.92
3.40
278.08
38.38
435.40
129.60
2.36
4.67
0.47
■267.32
157.50
605.06
152.23
2.79
8.49
0.50
187.04
45.41
888.91
229.84
3.80
11.18
1.56
364.48
51.91
759.06
236.40
5.19
13.70
0.67
185.85
62.38
Total - I
3642.08
4169.17
5103.49
6386.34
6218.66
1. Medical Services
0.56
11. Health Services
1 Public Health
Sanitation and
Water Supply J
a. Pevention and
Control of Diseases
b. Rural Wale? Supply
Scheme
c. Others .
2 Family Welfare
■ 1
11|
i
B
1 Bf
2 15
3 2C
4 30
5 40
6 50
7 Al
8 Ag
tf
S:
t
II. Rel
1 Hii
525.64
737.38
1148.95
1203.99
1058.23
451.55
709.23
658.33
1093.32
1125.34
765.45
803.22
602.12
825.05
837.45
964.17
970.36
1277.95
1651.10
Total - Il
2545.86
2873.78
3603.90
4545.62
GRAND TOTAL I + II
6187.94
7042.93
8717.39
10931.96
Source^ A Picture of Karnataka Budget.
1035.92
1W57.25
2 Mus
3 OIL
F
fe
Sb
III. Tr
1 Cur
2 Impr
3 Slit
4 Non5 Left
Medi
6 Othc
7 Tran
8 Died
9 Not I
Note ! J
S
Source :
II
r
614
■
•
--g
■'w ■
fI t;.
Table No. 28.11 IN-FAriEMTS TREATED AT THE MENTAL HOSPITAL, BANGALORE, 197? - 82.
11!
(in No.)
1979-80
1981-82
1980-81
Particulars
1
4190.07
,l5.3(
Males
Females
Males
Females
Males
Females
2
3
4
5
6
7
1. Age Group :
ni.ii
236.40 •;
5.17
13.70
0.67 ".'■3'J
1S5.85
I
1 Below 15 Years
2 15 - 19
3 20 - 29
4 30 - 39 ’
5 40 - 49
6 50 - 59
7 Above 60
8 Age not Known
80
1218
70
662
646
393
163
89-
393
194
101
41
Total - I
2589
123
294
874
610
362
91
133
74
170
510
351
203
82
52
171
231
906
599
343
127x
3
89
206
460
279
198
65
35
2
2487
1442
2446
1334
3441 i
283 *
324 *
2080
234
173
.1203
119
90
2099
208
139
1114
113
77 ‘
4018 *
2487
11V.
2446
1331
152
1767
136
1035
170
1621
414
172
29
70
934
1461
■-
II. Religion :
•1058.23
1 Hindus
2 Muslims
3 Others
•
1123.31
4J
Total - II
|.r;
■
4935.92 1
1651.10
OS
w
III. Treatment Conditions:
1 Cured
2 Improved
3 Slightly Improved
4 Non-Iraproved
5 Left Hospital Against
Medical Advice
6 Otherwise Discharged
7 Transferred
8 Died
9 Not Known
20
2520
Total - III
8
3
9
1422
8
i
206
a
481
26
22.2
18
36
20
20
5
11
10 4
7
34
6
20
8
10
2
3
5
1
2587
1461
2487
1142
2146
1334
'3
72
15
Note : * Sex-Wise Breakups are not Available.
3 The Figures are included in item No. 2. of II! Since the Breakups are not available.
Source : Directorate of Health and Family Welfare Services, Goverir ‘nt of Karnataka,
Bangalore.
’
./
.1
I
*
6b
I
¥
lable No. 28.12 INDIAN RED CROSS SOCIETY, PANGALORE, 1979 - 83.
g.
t■
(in th,)
■
Particulars
1979
1980
1981
1982
1983
1
2
3
4
5
6
r
I
1. Sub Branches
1 District Branches
2 Taluk Branches
16
26
16
26
16
26
16
26
I
r
18
26
t
■II. Memberships
ii a
I
r
ii a
1
7
8
707
1620
58
1016
205
36
1
6
8
710
1648
79
233
254
84
1
6
8
757
1765
22
109
228
75
6
13
1242
2351
755
2886
342
70
6
14
1410
2508
63
3220
325
16
III. Income (in Rs.)
266438
281811
325836
3999999
24E027
IV. Expenditure
(in Rs.)
223333
244859
317478
■ 358157
328562
1 Vice-President
2 Patrons
3 Vice Patrons.
4 Life Members
5 Life Associates
6 Annual Members *
7 Annual Associates *
8 Institutional Members
9 JR. Red Cross Groups
£
IB'
1. BAT^G/
IB.
' 2.
3. K:
4. S!
5. I
sm■
Note’, a Includes Hon-Vice President (i.e. those who have paid Rs 10,000/- or
more to the society).
« Refers to During each Year.
Source: Indian Red Cross Society, Karnataka Branch, Bangalore.
1983:
1. P
II. BELGf.'.
ir'.‘.ts, •
6. B
7. Di
8. D’
9. IM
III. GULBAR
10. Be
11. Bit
12. Gul
13. Rai
IV. MYSORE
14. Chi
15. Dak
16. Has
17. Kod.
18. Man.
19. Myst
Source: Di rec
■1-1
'wB j
616
Table Mo. 28.13 REGISIERED LWBER OF BIRTHS, DEATHS, STILL BIRTHS, ETC., 1979 - .1983,
in
1
--- L-fg
1983
(In L'o.)
Year/
Division/
District
18
26
ii a
6
14
1410
2508
63
3220
325'
16
242027
Live Still Birth Deaths Death Infant Infant
Births Births rate
'Rate Death mortali
ty rate
2
3
1979
1980
1981
1982
1983
455663
460295
466387
480337
406812
7714
7673
7036
4420
5921
12.68 87566 2.41 9075
12.56 150526 4.06 14714
12.66 150003 3.96 15251
10.51 124115 3.21 10190
I. BANGALORE DIVISION
122746
2705
9.55
35364 2.75
1. Bangalore
2. Chilradurga
3. Kolar
4. Shinoga
5. Tumkur
75614
1220?
1989
14235
18331
65
607
2557
4
14.36
6.58
7.18
10.61
1.25
22464
4370
3577
4119
834
II. BELGIUM DIVISION
167263
1599
17.14
6. Bel gaum
7. Bijapur
8. Dharwad
9. Vttara Kannada
47339
3 ?81S
62580
1/418
301
15.33
371
16.03
750 .20.41
174
15.62
16377
12032
17697
4382
III. GULBARGA DIVISION
39763
204
10. Belllary
11. Bidar
12. Gulbarga
13. Raichur
10610
10136
11877
6810
83
74
■O.
4
5
b
7
Mater- Maternal
nal Mortali
ty rate
8
9
W
39.05
19.71
31.54
31.75
25.05
774
577
583
528
356
1.70
1.25
1.25
1.09
0.83
4706
. 38.27
93 .
0.76
4.27
2.36
1.80
2.38
0.41
3860
378
183
226
59
51.04
30.96
12.85
12.33
33
27
7
8
23.07
18
0.44
2.21
0.49
0.44
7.64
50488 5,17
3252
19.44
160
0.96
5.30
4.84
5.77
3.92
761
931
1406
154
16.06
23.36
22.46
8.83
53
4V
56
7
1.12
1.10
O./i?
0.40
6.02
14000 2.12
779
20.09
51
1.28
4120
3110
43'10
2130
2.83
3.02
2.02
1.15
294
15
6.79
10.13
5.53
3.68
177
227
101
27.70
16.96
19.11
14.76
13
11
11
11
1.69
1.05
0.93
1.61
76340 ' 1413
8.12
24263 2.56
1433
18.65
52
0.68
2.68
13.95
7.16
8.03
3.61
7.66
1131 1.19
8405 3.41
3905 2.77
1180 .2.46
1939 1.32
7703 2.85
103
610
171
39
48
462
40.63
17.74
16.96
10.14
3
15
9
1.18
0.44
0.89
9.04
1
24
0.19
1.16
12.08
163296 4.06
1933:
Is
328562 '
jr
: 3
■ 1
J
IV. MYSORE DIVISION
40
27
■
J ■
.1
14. Chiknagalur
2535
15. Dakshina Kannada 34382
16. Hassan
10080
17. Kodagu
3315
18. Mandya
5310
19. Mysore
20688
16
344
717
52
121
163
22.33
I
I
Source* Directorate of Economics and Statistics, Government of Karnataka, Bangalore.
I
9
88
k
I
ri
617
r
Table No. 28.14 ESTIMATED LIVE BIRTH RATE, DEATH RATE ETC., 1979 - 1983.
(per thousand)
Natural
Birth Death Growth
Rate ''Rate Rate
col.2col.3)
Year/
Residence
General
Fertili
ty Rate
Grpss
Total
Reproduc- Fertition
lily
Rate
Rate
Infant
Horatality
Rate
1
2
3
4
5
1979
Rural
Urban
Combined
29.0
25.9
28.1
11.8
6.4
10.4
+17.2
+19.5
+ 17.7
119.8
100.3
114.2
1.9
1.4
1.8
3.9
3.0
3.6
94.3
50.9
83.4
1980
Rural
Urban
Coiibinet
28.9
24.1
27.6
10.7
6.6
9.6
+18.2
+17.5
+18.0
118.5
95.9
112.2
1.8
1.4
1.7
3.8
2.8
3.5
79.1
45.0
.70.9
1981
Rural
Urban
Combined
29.2
25.7
28.3
10.2
6.3
§.1
+19.0
+19.4
+ 19.2
119.0
100.9
113.9
1.8
1.5
1.7
3.8
3.0
3.6
77.1
45.0
69.1
1982
Rural
Urban
Combined
28.8
25.7
27.9
10.2
6.4
9.2
+ 18.6
+ 19.3
+ 18.7
118.2
101.0
111.3
1.8
1.5
1.7
3.8
3.0
3.6
71.1
46.6
65.0
1983
Rural
Urban
Combined.
30.2
26.0
29.1
10.6
6.'0
9.3
+ 19.6
♦20.0
+ 19.8
126.9
102.8
120.1
1.9
1.4
1.8
4.0
3.0
3.7
80.4
41.4
71.0
6
7
A
(
8
Source: Office of the Census Operations in Karnataka,
Sample Registration System Report.
i
5
I
6
■
Table Ho. 28.15 AGE SPECIFIC FERHLITY RATES, 1979 - 1983.
":v
--------- ------1980
1981
1979
AgeMothers
Group
of
AL
(Per thousands)
■y~-
1983
1982
(in years) Rural Urban Rural Urban Rural Urban Rural Urban Rural Urban
1
15 - 19
20 - 24
25 - 29
30 - 34
35-39
40 - 44
' 45-49
2
3
4
5
6
7
8
9
10 .
11
76.1 62.5 79.4 67.6 73.2 75.5 72.9 59.7 83.6 60.5
210.6 185.5 208.3 172.9 213.3 174.2 198.0 181.1 227.8 196.9
211.5 165.1 ‘201.2 148.7 203.0 164.1 201.0 177.8 204.4 160.4
142.2 96.1 138.0 97.8 142.8 114.0 140.1 104.6 138.8 101.2
85.9 54.7 83-. 8 .51.6 83.5 61.4 90.9 55.3 83.1 47.0
32.8 25.9 34.6 24.2 30.9 26.0 39.3 18.5 35.1 26.0
8.9
17.6 15.4 14.8
5.0 14.7
6.4 15.1
8.7 19.0
Source: Office of the Census Operations in Karnataka,
Sample Registration System Report.
f
I
Note : 1.
Source:7
I
- V;
618
<)
ant
ata-
s
Table No. 28.16 AGE SFECIFICED DEATH RATES, 1979 - 1980.
1
(per thousand)
1979
Age group
(in years)
74.3
i0.9
83.4
'9.1
5.0
0.9
1
7.1
5.0
9.1
I
• J-'..-
1.1
5.6
5.0
).4
4.4
■1.0
Males 3
1989
Females 3 Combined Males 9
Females 9 Combined
2
3
4
5
6
7
• 0-4
29.3
32.7
31.0
25.4
27.5
26.4
9
3.5
4.3
3.9
3.6
3.2
3.4
10-14
1.6
1.4
1.6
1.6
1.5
1.6
15-19
1.6
2.1
1.8
1.5
1.7
1.6
20-24
1.8
2.9
2.4
2.4
3.3
2.8
25-29
2.4
3.9
3.1
1.9
2.6
2.2
30-34
3.9
4.5
4.2
3.7
3.4
3.5
35-39
4.7
4.1
4.6
4.8
4.0
4.5
40-44
6.4
4.8
5.6
5.9
3.2
4.5
45-49
9.0
6.6
7.8
9.8
5.5
7.7
50-54
15.5
7.7
1.1.7
13/1
12.4
12.7
55-59
23.7
22.4
23.1
20.4
13.8
17.1
60-64
35.9
36.0
36.5
37.5
28.4
33.9
65-69
47.6
5 31.7
39.5
42.8
36.9
39.8
70 f
102.1
85.5
95.1
45.1
79.9
82.2
All ages
10.6
10.6
10.6
9.2
9.5
9.3
!■
u
I
I
Note : 1. 3 Sample value derived from MTP of Bureau of Economics and Statistics.
Source:'Report on Sample
f ' Registration
“
System 1971-80, (Published by the
Director of Census Operations, Karnataka.)
an
■
.5
.9
.4
2
0
0
9
w
W
w
1
d
1
I
I
61?
Table No. 28.17 PERCENTAGE OF LIVE BIRIHS BY ORDER OF BIRTH
1981 - 1983.
1981
1982
act i
and
The
of S
a by
1983
Birth
order
Rural
Urban
Rural
Urban
Rural
Urban
1
2
3
4
5
6
7
27.23
22.94
18.43
13.99
6.94
3.67
2.38
.1.27
0.62
0.31
0.14
2.08
22.28
20.04
16.38
13.61
10.47
7.72
3.32
1.98
25.98
23.72
18.94
12.81
7.19
4.26
2.08
1.39'
0.65
33.70
25.90
20.45
17.90
14.00
4.16
2.08
4.13
1.93
0.50
0.30
0.13
0.72
23.90
33.78
25.92
Tabl
2.
3.
4.
5.
6.
7.
8.
9.
10.
Above 10.
Not stated
18.15
9.85
4.83
plan
year
84.
"'1.
0.47
0.30
0.21
0.32
0.23
2.43
3.22
19.07
12.58
6.94'
4.05
2.03
1.30
0.63
0.31
0.21
3.08
2.41
1.10
0.67
0.35
0.16
0.09
2.69
Tabl
de ve
unde
1983
Tabb
Source: Directorate of Economics & Statistics,
Government of Karnataka, Bangalore.
cast;
stud,
s cho
yea r <
Table
Table No. 28.18 PROJECTED VALUES OF
EXPECTATION OF LIFE AT BIRTH, 1961-90.
Year
Males
Females
Go ve r
tri be
such
1
2
3
Tabb
1961-70
1971-75
1976-80
1981-85
1986-90
47.1
50.9
53.4
55.9
58.4
45.9
50.0'
52.8
55.6
58.3
di s t r
Tabl c
ex pen
Sche d
1981-
Source: Census of India 1971
India Series - I, Paper -1 of
1979.
Report of the Expert Committee on
polulation projections.
Table
water
s ched
Tabl e
of
s
Cover
years
I"
fr'
i
Dear Sir,
Kindly find attached a Note on the proposed restructuring of the Group A medical
•
posts in the Health and Family Welfare Department. The Note is in line with the broad
recommendations of the Task Force on Health and Family Welfare and seeks to address
concerns expressed at various fora by elected legislators.
The Note is a follow up of the discussion at my level with DHS, Mr. Ramnath, former
Joint Secretary DPAR, and CAO -I. It is suggested that you may kindly agree to chair a
meeting where the following is discussed:
1) Appointment and terms of reference of Shn Ramnath as Consultant to draft the
C&R rules for Group A as well as other posts to form the proposed District cadre
along with time frame and estimated amount for the consultancy; and,
2) The proposed structure of the reorganized Group A medical cadre.
It would be useful to have the DPAR (Service Rules) involved in the discussion at
this stage itself. In view of this, the following could be invited:
1) DHS, 2) Shri Ramnath, 3) Shri A. Kadeer, JS DPAR, 4) CAO -1, 5) Shri
Padmanabha, Member, Task Force, 6) PD 1PP-IX, 7) PA, KHSDP and 8) DS (H).
f
In view of the complex nature of the subject to be discussed a minimum of two
hours may kindly be earmarked for the discussion. A date and time may kindly be
indicated to enable me to the circulate the note in advance of the meeting.
With kind regards,
Yours sincerely,
il
(Sanjay Kaul)
-1
Shri A.K.M. Nayak,
Principal Secretary, HFW,
MS Buildings, Bangalore.
I
-----------» “A” MEDICAL AND PUBLIC HEALTH
Restructuring of the
group
POSTS IN THE DEP.ARTMENT
----------- OF HEALTH AND FAMILY WELFARE
Need and justification for Organizational Reform
There is an unequivocal feeling that the present organizational structure of the deP^^
of health and family welfare needs urgent restructuring, particularly in respect of
Group A posts. The need for restructuring has arisen on account of the following.
(a) The public health element in the department has become devalued and needs to
be reinstituted.
.
(b) There is reluctance on the part of doctors to opt for non-chmcal posts.
(c) There is lack of management expertise in the cadre.
(d) There is a reluctance of doctors to work in backward districts and remote places.
(e) There is need to recognise talent and specialization outside the department and
(f) Xm^rneertoTdurtpmfessionalism in both the medical and public health
spheres.
(g) There is need to make changes to suit the Zilla Panchayat system.
Elected legislators as well as the Task Force on Health and Family Welfare have also
voiced the above concerns. The restructuring proposed is in keeping with the broad
suggestions made by the Task Force.
f
Proposed wings in the Medical and Public Health cadres
All posts of doctors and specialists will be reclassified into the following three services.
1. Karnataka District health service.
2. Karnataka Health service (public health).
3. Karnataka Health service (medical)
The Karnataka District Health Service (KDHS)
The KDMPHS will have the following categories and numbers of posts. These posts will
SeoXted into separate district cadres. The district cadres will have the followrng two
categories of posts:
1. All posts of GDMOs - approx, number 2400.
2. All posts of specialists in CHCs and Taluka hospitals - approx, number 1400.
The method of recruitement will be as below:
1
GDMOs- All vacancies of GDMOs in each district will be notified by the
respective DHOs. Selections will be made based on the qualifying percentage of
marks secured by the candidates in the MBBS examination Reservation would be
provided to SC/ST/BCs as per the prevailing Government Orders. 30 /o of posts m
category would be reserved for women. There would be no written exam or
interview.
Time bound promotions: GDMOs would be eligible tc, two time-bound promotions,
and the second on completion of
y
spgpiglte 50% of posts of specialists> m CH^aud ™"*£c^
^^Tfor such GDMOs who complete then PG in tne sp^
50%
The balance 50% posts will be Direct ecrmun
>
degree/diploma
weightage each for the mark.s s=^
MBBjS^d m .
examination as the case may be. Al
resnective DHOs. If there are
recruitment, speciality-wise, wil e no 11
specialities available
no qualified candidates in a
posts would be filled by
from among GDMOs for J'11^ "P
“
adeq„ate number of specialists in
^^“““^ofo^ngbyp—
aT‘I to a
specialist
55K4O^toh^mpleted 6 years of service A GDMO promore
ipective of the number of years
would also be given the same specialist pay scale irresi
of service rendered by him/her as a GDMO.
Direct recruit specialists
Specialists will be entitled to “XmGDMOs'wUl
^^fc^Tfhose specialists who have been I romot d^f
completion of 13 years of service.
• j ah nnMOs/soecialists who have less than 13 years of service
Transition period; All GDMOs/specia
KHS(M) will be automatically
inducted into the ™S(PH) or KHofM)
inducted into the KDHS in the districts: where tae are^of seeking a
XXXSisJdSmahe an
SXgXoZe^S’^cts concerned and the seniority ofthe Doctor.
Karnataka Health Service (public health) [KHS(PH)]
The KHS(PH) will be comprise the following posts:
1. Taluka Health Officers;
2. Programme Officers;
3. Principal DTCs;
4. District surveillance officers;
. , #
f .
5. DHOs;
Deputy
Directors
and
other
equivalent
posts,
6.
7. Joint Directors;
8. Additional Directors;
L.
9. Director, Public Health Services.
!
//
Method of recruitment: The posts at SI Nos. 1-4 will be equivalent posts carrying an
identical pay scale. 80% of the posts will be filled by promotion on the basis of semontycum-merit from among GDMOs belonging to the KOHS and who have completed their
Post graduation in Public Health or possess a DPH/PESM degree. However, if there are
no suitable qualified persons, then these posts will be filled by promotion on the basis of
seniority-cum-merit from among GDMOs who opt for the KHS(PH). Thu(optioni would
be irrevocable, and no member of KHS(PH) will be eligible to change to KHS(Medical
in his subsequent career. 20% of the of the posts at SI. Nos. 1-4 will be filled by direct
recruitment based on 50% weightage for MBBS marks and 50% weightage for a written
examination to be conducted by the Rajiv Gandhi University of Health Sciences
Commissioner Health & Family Welfare will be the recruiting authority. GDMOs would
also be eligible to apply for the DR posts and would also be eligible for age relaxation ot
upto 5 years.
In respect of Doctors who have completed 13 years in service, all Doctors not possessing
a PG degree and all Doctors having a DPH/PESM degree will be automatically inducted
into the KHS(PH), except for such Doctors who decline to opt for the Service, subject to
the availability of vacancies. Doctors not possessing a DPH/PESM degree will be give
suitable training in Public Health A seniority list of such members of the service will be
published soon after the final notification of the revised C&R rules.
Inter-se seniority among GDMOs serving in various districts.
The inter-se seniority among GDMOs for their promotion into the KHS(PH) will be
decided in the following manner:
1
A list of GDMOs serving in various districts in the KDHS will be
compiled based on their year of recruitment. They will be asked to give
their irrevocable option with regard to joining the KHS(PH). A common
seniority list will be compiled. Those possessing a DPH/PESM degree will
be placed on top and the remaining on the basis of their existing seniority
position. In respect of fresh recruitments made after the revised C&R rules
are notiied, the list of all doctors recruited in the various districts will be
clubbed year-wise and seniority determined according to their marks in the
MBBS examination. In respect of those possessing a DPH/PESM degree,
such persons will be placed on top while others will be placed according
to their year of recruitment and their MBBS marks.
2. Promotions from the KDHS into the KHS(PH) will be done on the basis of
seniority-cum merit according to the seniority list generated as above.
KHS(PH) Probationers
Candidates selected through Direct recruitment into the KHS(PH) will be on
probation for two years. During this period they will be undergo a one year s DPH
programme at the State Institute of H&FW and will receive a DPH certificate recognized
by the Rajiv Gandhi University of Health Sciences. Selected Candidates already
possessing a DPH/PESM degree will also undergo this Course. The University in
consultation with the State Institute, will conduct the examination, and will also decide
the curriculum. Other institutions apart from the State Institute recognized by yhe
University can also conduct the DPH programme. Candidates successfully passing the
DPH examination and other prescribed examinations shall undergo training as a GDMO
for one year before being given regular charge as Taluka Health Officer/Programme
Officer.
Karnataka Health Service (Medical)
The Karnataka Health Service (Medical) will comprise the following posts:
1.
2.
3.
4.
5.
6.
Senior specialists;
District surgeons or equivalent posts;
Chief Surgeons;
Joint Directors;
Additional directors;
Director, Medical Services.
Method of Recruitment
All specialists on completion of 13 years of service or direct recruit specialists on
completing 7 years of service in the KDHS will enter the KHS (Medical) on giving a bond
that they are willing to serve anywhere in the State, subject to available vacancies. There
will be no Direct recruitment into the KHS(M). Promotions to the different cadres will be
on the basis of seniority-cum-merit. Chief Surgeons are upgraded posts equivalent in rank
and pay to that of Joint Director created to ensure a reasonable balance of promotional
opportunities between the two services. District Surgeons or equivalent officers in this
higher grade will be designated as Chief Surgeons, though they will continue discharging
their earlier responsibilities, in addition to new responsibilities given to them. Some
senior specialist positions will be made available at Taluka hospitals/CHCs also.
Promotions in the KHS(PH) and KHS(M)
All promotions into the various posts in the KHS(PH) and KHS(M) will be based on
semority-cum-merit.
- Media
 RF_COM_H_49_SUDHA.pdf
RF_COM_H_49_SUDHA.pdf
Position: 2182 (5 views)