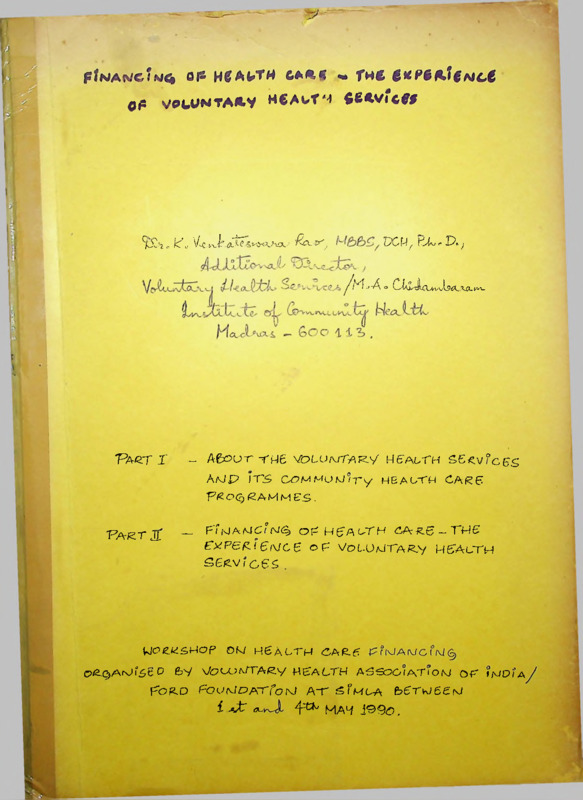
FINANCING OF HEALTH CARE - THE EXPERIENCE OF VOLUNTARY HEALTH SERVICES
Item
- Title
-
FINANCING OF HEALTH CARE - THE EXPERIENCE
OF VOLUNTARY HEALTH SERVICES
- extracted text
-
ofi v^tUHTA*y hcautm fietvicfj
5l£? .- k\' V<C vv^tfCfes^O^ViXIL? ’Rq_,V';
DCU f TT *■ D> )
^/M-’-A<»
Faqt !
CAiJLuvvU£1.'UU','-k-
- Aftoor YM6 VoLU/MTA^y MeAizTH ££<v°c,ES
A/JP ITS CTMMUM/ry MEAUTH CARE
T^O^SaMMES.
Pa^T jl
_
FTmaMC’a/^ O^Mg'AATH ^A^e-TPS
eyPEfli 6i\JC6 op' VoL.(J/UTA^.y MgAcTM
SS/2.V/C6S .
VJC’g.tdg.MCp
C>ie.C)A^r5t D
OM H6ALTM £A£-(5
fcV VC’t-OAATAe.y HEALTH A5S9GATIOM Of t^OiA
^OfLO
FOHMCATfobJ AT sFmla
£ -vt” Ck-
&6TvJ6£M
4^ MAH jO9(9,
COMMUNITY HEALTH CLU
67^1,(First !-!oor)3t. Marks Road
BAWGAtOBE - 56U 601
FINANCING OF HEALTH CARE - THE EXPERIENCE
OF VOLUNTARY HEALTH SERVICES
Dr.K. Venkateswara Rao, MBBS,DCH,Ph.D.
Additional Director
Voluntary Health SerMces/M.A.Chidambaram
Institute of Community Health
Madras 600 113
PART I
ABOUT THE VOLUNTARY HEALTH SERVICES
AND ITS COMMUNITY HEALTH CARE
PROGRAMMES
PART II
FINANCING OF HEALTH CARE - THE
EXPERIENCE OF VOLUNTARY HEALTH
SERVICES
WORKSHOP ON HEALTH CARE FINANCING
ORGANISED BY VOLUNTARY HEALTH ASSOCIATION OF INDIA/
FORD FOUNDATION AT SIMLA BETWEEN
1ST AND 4TH MAY 1990
PART I
ABOUT VOLUNTARY HEALTH SERVICES AND ITS COMMUNITY
HEALTH CARE PROGRAMMES
The Voluntary Health Services Medical Centre (VHS) is
a
comprehensive
community hospital housing
all
the
specialities and superspecialities except cardio-thoracic
surgery and maternity at present. The medical centre has all
the
modern facilities expected of a referal
hospital
including preventive,
promotive, diagnostic, curative and
rehabilitative services.
The VHS was registered as a non-profit society on
July 14, 1958. The in-patient services commenced from the
year 1963.
Right from the inception, the VHS has been modelled
to deliver comprehensive and continuous health services
having several concepts which are unique not only in the
delivery of services but also in the matter of financing of
health care in the country.
The main
i.
concepts of Voluntary Health Services are:
Prevention and Cure of serious illness
The first concept of the society is that in a country
with so many preventable diseases, and deaths,
the
emphasis should be on prevention of serious illness
to the comparative exclusion of minor or day-to-day
illness.
It is felt that the latter can be handled
by the large number of public dispensaries and
unaided private practitioners who are welcome to
utilise the services of the Medical Centre.
ii.
Family as a Unit
The second concept is that the family should be the
unit for medical care and that every family should be
attached to a combined public health and curative
centre and should learn about all diseases and their
prevention from the same Social Worker,
Health
visitor or Public Health Nurse attached to the
Medical Centre to which the family knows it belongs.
iii.
Community Participation
One
of the many ways in which the
community
participation is secured is by enrolling families in
the 'different income groups as subscribers to the
Medical Aid Plan.
2
iv.
Maintenance of family health records
It is absolutely essential to have a comprehensive
and continuous record of the medical and health
history of each member of the family from birth.
This health information system will go a long way in
the provision of continuous and quality services and
ensure proper follow up.
The most unique feature of the VHS is that, every
brick is donated by individual donors, trusts and societies.
The VHS has been supported by the successive Tamil Nadu State
and Central Governments in the form of bed maintenance and
support to individual projects.
The entire society is
functioning with the concept of 'Shram Daan' and if it is
what it is today, is due to the cumulative efforts of several
medical and para medical workers ably supported by several
philanthropists.
I.
GENERAL SERVICES
1. Medical Aid Plan: The services to the families are
rendered through a medical aid plan which is a unique pre
payment concept which has been formulated to popularise
sharing of the burden of maintenance of one's own health care
by the families, as they do for their own food, clothing and
shelter.
Under this plan, families will have to become
subscribers by paying a nominal subscription for the entire
family at the rate of 0.75% of their annual income.
Families
earning below Rs. 300/- per month need not have to pay any
further charges for OP and IP care which includes free diet.
Subscribers above this income level will have to pay graded
charges on a sliding scale even for which a concession of
25% is available.
Services are not refused to those who do not want to
become subscribers.
Though they may not get the concession
eligible for subscribers, the charges for these categories
are moderate when compared to the market rates.
Even here
there is a gradation in the charges.
2. Out-patient Department: A well equipped O.P.
for all
departments
including indigenous systems of
medicines,
functions in two well laid out buildings.
As soon as a family becomes a subscriber, the health
records of all the members of the family are maintained by
compulsory examination.
By this method, we are able to
uncover the hidden ice berg of diseases.
The services start
with preventive measures like inocculations, nutrition advice
and
health education.
Based on the findings of
the
3
examination, OP and IP care is given as per exigencies of the
condition.
The families are encouraged to bring the other
members of the family for compulsory examination.
Other
services in the form of examination of Blood Pressure,
Urine
analysis and 70 mm X-ray chest are also offered for
early detection of Hypertension, Diabetes and Tuberculosis.
3. Day Care Centre: The day care centre,
donated by M/s
Larsen & Toubro,is a new concept in the health care process.
There are several trivial conditions which do not necessitate
admission for longer periods in IP set up.
Conditions like
Diarrhoea, vomiting, minor surgical and medical conditions
can be kept under observation and treated at the
OP
department itself.
Such a measure not only reduces the load
on the IP services but also cuts down the cost and the
record work.
4.
In-patient Services: We have 240 inpatient beds of which
60% are for poor patients.
This includes 19 beds in Deluxe
special wards and 18 beds for paying patients in A and B
class special wards.
The general medical and surgical departments cater to
all
types of medical and surgical problems
including
emergencies.
Individual departments are also conducting
research programmes.
The wards and rooms are large and airy
with a minimal risk of cross infection.
This has been
appreciated by several national and international visitors.
The Surgical Department is backed by three well equipped and
air conditioned theatres.
II.
SPECIALISED SERVICES
1.
Intensive Care Unit: With kind munuficience
of T.S
Srinivasan
(Cheema)
of M/s. Sundaram Clayton,
this unit
caters to the medical and surgical emergencies and has modern
equipments for resuscitation and continued monitoring.
2. Neurosurgery:
The Achanta Lakshmipathy Neurosurgical
Centre has won national and international recognition.
This
department not only provides clinical and diagnostic services
of excellence but also conducts research in several areas
like Epilepsy, Yoga and nonvolitional Bio-feed back etc.
3. Neurology Department: The K. Gopalakrishna Department of
Neurology
has been specialising in the diagnosis
and
treatment of neurological disorders and has become well noted
for the comprehensiveness of approach. Several international
visitors have appreciated the quality of its work.
Special
emphasis is being paid by this department for the study,
4
control and rehabilitation of stroke patients
dystrophy.
and
muscular
4. Nephrology: The Bhagavan Adinath Jain Department of
Nephrology has been donated
by Shri.
Sugalchand Jain.
Though this department has been started recently, it has made
giant strides in a very short time.
It is doing very useful
work to the community by undertaking renal dialysis and has
so far successfully completed 30 renal transplants
in
collaboration with surgical and urological services of the
VHS.
The unique feature of these services is the low cost
for dialysis and transplants.
5.
Urology: This department has modern equipments and is
conducting routine and trans-urethral surgery.
This unit
collaborates actively with the department of Nephrology for
renal transplants.
6.
Diabetic Department: From the modest beginning in 1965,
when only OP services were available, the T.G.K.
Raman
Diabetic Department has grown into a centre of excellence and
now as a Ramabadran Research Laboratory is doing pioneering
work in the detection and control of diabetes with a special
emphasis on research on juvenile diabetes.
7.
Cardiology: This department conducts routine clinical,
diagnostic and curative work in collaboration with the
community health department.
The J.
Srinivasan Cardiac
Research Wing has been studying the problem of causal factors
associated with coronary thrombosis in the City of Madras.
8.
Psychiatry: The usual psychiatric services including
counselling,
diagnostic and curative services including ECT
therapy are provided in this department. The main emphasis
is on community psychiatry.
9.
Dermatology: Routine dermatology services are available in
this department.
10. Gynaecology: Routine gynaecological services
provided at this department.
are
being
11. ENT: This department was built through the munificience
of Madras Round Table No.I and has been doing pioneering work
in the treatment of deafness through Stapedectomy.
This
centre was nurtured and developed by Dr. V.S.
Subramaniam.
To this, is attached the Venky's department, donated by Mr.V.
Arunachalam.
It
is doing work on deafness among school
children and advising appropriate management.
5
12. Opthalmology:
This department supported by R.R.
Iyer
Charities
and
Shri.
V.
Sundaram,
gives
routine
ophthalmological services. Cataract surgery including intra
ocular
lens implantation is being undertaken at
this
department.
13. Orthopaedics: This department is undertaking routine
orthopaedic services and is specialising in partial hip
replacement and spinal surgery.
14. Leprosy: The VHS is attending to several leprosy patients
living in and around Adyar directly.
In addition,
through
its project aided by USAID through Government of India for
control of Leprosy and Tuberculosis, it is taking care of
about 2000 leprosy patients living in the adjacent parts of
the Chingleput district.
This unit treats the leprosy
patients using the modern multi drug regimen. The patients
having
ENL
reactions,
ulcers
and
those
requiring
reconstructive surgery are admitted in the leprosy inpatient
block.
Leprosy Research: For the past few years, the VHS is involved
in the laboratory culture of M. Leprae. At present,
various
synthetic media are being studied by Dr.N. Veeraraghavan for
the speedy culture of the organism in the laboratory.
In
addition,
this department is testing out new combination of
durgs using the concept of cell Mediated Immunity.
15. Tuberculosis: The VHS is a recognised peripheral health
institution of the Tuberculosis centre at Madras. The unique
feature of this department is the low defaulter rate when
compared to the other similar facilities elsewhere consequent
to the assured follow up services to the cases through the
community health care programme.
16. Geriatrics: The VHS is first among the agencies to have
thought about the need for provision of Geriatric services
especially in a society where values are changing fast.
Towards this end, the VHS through the kind courtesy
of
several philanthropists and Helpage has constructed eight
geriatric cottages and two dormitories for the care of the
elderly.
Provision for cooking is available at the geriatric
cottages.
There are attractive schemes for the continued
geriatric care on both short and long term basis.
17. The Urban Family Welfare Centre: This centre is serving a
population of 25,000 living in slums adjacent to the medical
centre.
This has recently been upgraded as an Urban Health
Post
under the World Bank Assisted
India
Population
Project V. The VHS believes in family welfare services being
6
part and parcel of comprehensive
instead of a vertical approach.
health
care
programme
18. Diagnostic Centre: Jadavbai Nathmal Singhvee Diagnostic
Centre donated by Shri. Sugalchand Jain undertakes all types
of clinical, bio-chemical and histopathologic investigations.
The reports of this centre are accepted by the medical
profession as authentic.
Research work is being done for
culture of M. Tuberculosis using Veeraraghavan's medium,
in
addition to other microbiological research.
A unit of
diagnostic centre is functioning at Luz, Mylapore.
19. Radiology: The department has three X-ray machines with
screening
facilities
donated by CARE,
Government
of
India/Arogya ashrama samithi and USAID.
20. Endoscopy Centre: It is a full fledged centre with modern
equipments for doing upper gastroscopy,
retroduodenoscopy,
proctocolonoscopy, bronchoscopy investigations. It goes a
long way in the early detection of ulcers, malignancies and
multi tissue diagnosis. The cost for these investigations is
very low.
This has been made possible3 by the donation from
Jindal Aluminium Company.
21. Blood Bank:
Dr. K.S. Ranganathan Blood Bank has won
laurels for its original studies regarding the Rh factor and
for propagation of the voluntary blood donation.
This centre
can aptly be described as the Father of Voluntary Blood
Donation Movement in India.
22. Physiotherapy: This department has all facilities for
traction,
heat treatment and exercises therapy for both
orthopaedic and neurological problems.
III.
TRAINING
The Voluntary Health Services believes in undertaking
job oriented training for medical and paramedical workers.
It has been our view that we cannot afford to train medical
and para medicals for UK and USA. The entire training must
be directed towards tackling the day-to-day problems which
these categories will encounter.
The
following
undertaken at the VHS:
training
programmes
are
being
1. For the Grass-root level workers: These are middle aged
women identified from the community with a basic educational
qualification of 8th standard.
They are trained as Lay First
Aiders.
They act as informants of the health events in the
7
village to the Multipurpose Workers, in addition to providing
first aid during times of need.
2.
Multipurpose Workers: An Eighteen
Months
training
programme for Multipurpose Worker (Female)
candidates who
have passed 10th Standard is undertaken.
This training is
recognised by the Tamil Nadu Nurses and Midwives Council.
The annual intake of candidates for this course is,
two
batches of ten each.
Multipurpose Training Programme for males of one year
duration is also being conducted.
3. Training programme for Non-medical Graduates: Non-medical
graduates are eligible for admission to one year P.G.
Diploma Course recognised by the Government of Tamil Nadu in
the following three disciplines:
i. Medical Laboratory Technology
ii. Nutrition and Dietetics
iii. Health and Hospital Administration
4.
Post-graduate Training of Medical Officers: The VHS is
recognised by the National Board Examination for the award of
the degree of diplomate of National Board in the following
disciplines:
General Medicine,
General Surgery,
Neurosurgery,
Community Health,
Family Medicine,
Social and Preventive Medicine and
Health Administration.
5.
Others:
In addition to
programmes are organised for:
the
above,
several
training
Postgraduate doctors from National Institute
of
Nutrition;
M.A. students of Madras School of Social Work; Stella
Maris College;
Nava Nirmana, Madras; P.S. Senior Secondary School
Orientation training to students and doctors from
Ramachandra Medical College, Madras and Centre for
Development studies, Ulloor, Trivandrum.
This institute has undertaken the responsibility for
conducting examinations for the Nursing Assistant students
from Khajamalai Ladies Association and Holy Cross Convent
Association, Trichy.
8
IV.
RESEARCH PROGRAMMES
The Voluntary Health Services does not believe in
undertaking
sophisticated research of little
practical
relevance.
On the other hand, it actively promotes research,
directed towards the commonly prevailing problems in the
community.
V.
ALTERNATIVE SYSTEMS OF MEDICINE
Though the institution is devoted to modern medical
care, VHS has been encouraging the growth of alternative
systems of medicine. The Achanta Lakshmipathy Centre for
research in Ayurveda and Siddha is the centre of excellence
for research in those branches. This centre has won a number
of gold medals for its original research. The VHS also has
got centres for magneto-biology, Acupuncture etc.
The
acupuncture training was given to doctors of VHS
and
outsiders by Chinese team of experts in Acupuncture.
VI.
COMMUNITY HEALTH
The VHS from the beginning has been modelled as a
community hospital intended for taking care of the community
living in areas adjacent to it. With this area concept in
view, the community health department was one of the first
departments to be started.
The Mini Health Centre model for the delivery of
comprehensive health services at a low cost was evolved after
a series of operational experiments to work out the ideal
population coverage and the staff to be deployed.
These
experiments
were
conducted at the St.
Thomas
Mount
Community Development Block of Chingleput District in the
mid-sixties.
Dr. K. S. Sanjivi and Dr. K. Venkatesware, Rao
are the authors of these concepts and experiments.
In the late 1960s the model of the Mini Health
Centres took shape and were put on ground in some rural areas
of Chingleput District of Tamil Nadu State.
The ideal set up for Mini Health Centre as evolved is:
A health post manned by Lay First Aider for every
1000 population.
b) A male and a female Multipurpose Worker for every
5000
population.
c) A doctor being available at the Mini Health Centre
(MHC)
level for at least three hours a day on
three days a week.
a)
9
d)
The identification of, and liaison with, a referal
hospital within a reasonable distance.
In the mini health centre, the family is the unit of care.
The essential concept is that, every family should set apart
a small amount within its ability to pay towards the health
care as it does for its food, clothing and shelter.
Dr. Sanjivi believes that health cannot be delivered
in a neat gift packet.
It is essentially 'a do it yourself'
proposition in which every one should participate.
Health alone cannot stand in isolation.
It is
essentially a part and parcel of socio-economic development.
The ideal combination of socio economic development and
medical technology will ensure better primary health care.
There is an increasig tendency of the politicians to
medicalise
the socio economic problems.
Health
care
programmes will not be meaningful until and unless a strong
base is laid by the political will and bureaucratic support
in association with the enabling and empowering process of
the
community
aimed
at
ensuring
better
community
participation.
The first and foremost activity in the mini health
centre is to determine the target groups for the various
health activities by taking a numerical count of the people
living within the jurisdiction of the mini health centre.
This enumeration is done having the family as a unit for
purposes of identification and comprehensiveness of coverage
and follow up.
The families are enrolled as subscribers in the
prepayment plan.
The amount of subscription paid varies
according to the income status of the family.
It amounts to
0.75% of the annual income.
Enrolment as subscriber will
entitle the family to receive curative care and services at
the referal institution without their having to pay further
subscription. The preventive and promotive care is given to
all inhabitants in the mini health centre area irrespective
of their membership status. The Curative care is provided to
non subscribers also but after receiving a fee per service.
We believe in checking up all the individuals in a
family once a year as a routine measure to detect the hidden
problems.
By this approach, we find that more than 95% of
the population require some type of assistance or the other.
The people may not readily come forward to seek medical
assistance unless the suffering caused by the
illness
prevents them from earning their livelihood.
In a programme
10
aiming at prevention, this approach will go a long way in
avoiding the development of chronic and intractable problems.
Family folders are maintained and the
complete
medical and developmental history of all the members of the
family is entered in these folders. This, we believe,
is
very important for the development of health information
system and for ensuring the continuity of follow up.
The Primary Health Care system starts at the remote
villages at the hands of the Lay First Aider manning the
health post.
This LFA is always a middle aged woman who acts
as an health informant and communicates the health events to
the multipurpose workers.
In addition,she will also visit
the houses to know the current health status, as well as for
follow up, to ensure professionals at the Mini health centre.
She also provides basic medicines at times of need at her
health post.
a.
Maternal Services
Based on the information provided by Lay first
aiders,pregnant mothers are registered and followed up by
routine antenatal care until the delivery.
Disposable Delivery Kit is provided to each pregnant
mother to be given to the birth attendant during the time of
delivery.
Skilled assistance is provided for the conduct of
aseptic deliveries.
The health workers liaise with the
Traditional Birth Attendants and give training to them in the
conduct of safe and aseptic deliveries. High Risk mothers
having previous bad obstetric histories, severe anaemias and
other medical problems are referred to the hospital.
b)
Child Health Services
The children are assured of total protection against
vaccine preventable diseases as per the prescribed time
schedule.
Growth of the children is monitored regularly.
Nutritional supplements are provided to children of Grade
III malnutrition. Appropriate nutritional supplements are
also given to pregnant mothers during the last trimester to
combat the problem of low birth weight.
The mothers are educated about the oral rehydration
therapy
in the prevention of morbidity and
mortality
following diarrhoea.
Preparation of sugar and salt solution
is demonstrated to them in the health education sessions.
Periodic deworming
health status of children.
is
attempted
to
improve
the
11
Health check up for school children is an
activity of the mini health centre in the area.
c)
important
Control of Communicable Diseases:
Prevention of communicable diseases as an integral
part of the comprehensive health services is a sheet-anchor
of the mini health centre activities.
Consequent to the
regular house visiting,
screening for malaria,
leprosy,
tuberculosis and other communicable diseases, becomes a
routine.
Sputum
cups
are distributed
to
all
the
symptomatics. The sputum smear is fixed and examined for the
presence of Tubercle bacilli. Then suspected cases are taken
to the referal hospital for an X-ray for the detection of
radiologically positive cases.
After confirmation,
the
patients are put on domiciliary treatment on
standard
regimens. The patients are regularly followed up for control
and treatment default and examined at prescribed intervals to
assess the progress of treatment.
All the cases suspected to be having a patch are
examined for the presence of anaesthesia and treatment
offered at the door steps without much publicity to avoid
their social stigmatisation. The patients are put on modern
multi-drug
regimen.
Microcellular
rubber
shoes
are
distributed to the leprosy patients to prevent trophic
ulceration.
d)
Family Welfare:
Target
couples are identified from
among
the
eligible couples for family planning advice and services.
Conventional Contraceptives and oral pills are distributed at
the door steps.
IUD insertions are also done at the local
areas and cases requiring sterilisation are referred to
urban family welfare centre attached to Voluntary
Health
Services.
e)
Laboratory Support:
Laboratory support is available at the local and
the referal hospital levels.
f)
at
Registration of vital events
Vital events such as births and deaths are identified
and registered with the Village Administrative Officer.
12
g)
Environmental Sanitation
Bad environmental sanitation and bad personal hygiene
are the root causes for the spread of communicable diseases.
Though it is realised that ideal environmental sanitation is
closely linked to socio economic development, as a short term
interim measure, the community is encouraged to dig soakage
pits for the drainage of waste water. They are advised on
the disposal of garbage in the compost pit and the usage of
sanitary latrines.
These facilities are demonstrated at
the Environmental Sanitation demonstration plot at the model
health cum training centre in Thuraipakkam Mini Health
Centre.
h)
Health and Nutritional Education
Health education is a regular activity in the mini
health centre.
In addition to person to person approach,
group discussions and audio visual shows are conducted.
Nutrituion education is provided for the usage of
locally available food stuffs and in the preparation of low
cost weaning foods. Regular nutrition demonstration sessions
are organised at the village level. Weaning food packets are
available at subsidised rates with Lay First Aiders.
These
foods are very popular with the villagers.
Seeds for the development of kitchen gardens are
distributed free of cost to the community. The emphasis is
on the growth of dark green leafy vegetables.
i)
Curative Care
The
medical
officer conducts clinics
at
the
headquarters of the mini health centre on two days a week and
on the third day they conducts clinic at one of the villages
served by that mini health centre by turns, to ensure greater
peripheralisation of health care as well as for providing
'on
the spot' health education and follow up.
In our experience,it has been found that slightly
more than 92% of the medical problems can be dealt with at
the mini health centre level itself.
Only 8% require referal
to an institution for higher level diagnosis and care.
A
mere 1.5% of the total disease load requires actual in
patient care.
j)
and
Referal Chain
The poor villager is not exempt from getting serious
chronic ailments. In the event of such an occurrence,
13
the health care system must rise up in providing the best
possible care as is available for their urban counterparts.
The acute problems that arise at the health posts, should be
in the hands of the physicians or surgeons at the referal
hospital within three to four hours and the cold problems
within a week.
We believe that, families in a defined geographical
area must be attached to an identified referal hospital
through the mini health centres, instead of, their being made
to seek medical and health care through institutions based on
their emp1oyment.
The Voluntary Health Services with its specialities
and super specialities,
is the referal hospital for all
the mini health centres in the area and provides tertiary
support to the rural health posts/mini health centres.
The mini health centre scheme envisages the laying on
ground of an ideal referal system on an area concept.
In our
programme,
even the lay first aider can refer medical
problems
which in her opinion require higher
medical
attention. The referal hospital has been instructed to give
priority attention irrespective of the time of the day even
though they appear trivial in nature to the medical officers
at the referal institution to maintain the credibility of the
village level workers.
k)
Community Participation
The mini health centre scheme emphasises
participation which is three fold. The community
accommodation and minimal furniture.
community
provides
A non political local action committee is constituted
for a two way liaison between service providers and the
beneficiaries.
There is financial participation by the
community in the form of subscriptions or fee for service.
1)
Urban Health Care
As already stated, health care of the people living
in urban slums is also considered a priority. In addition
to all the problems faced by their rural counterparts, the
urban slum dwellers are prone to more air and noise pollution
and accidents. They also suffer from higher degree of mental
trauma due to the gap between anticipation and achievement.
The urban health care model evolved by the Voluntary Health
Services is currently being implemented in several urban
slums of Madras city by several voluntary organisations.
14
m)
Financing
Both
the Central
and State
Governments
have
solicited voluntary organisation to supplement governmental
efforts,
as no country in the world can afford to provide
total health care all by itself.
The successive governments
both at Tamil Nadu and at the Centre have encouraged our
concepts and schemes.
Currently, the expenditure
for
running a mini health centre is being shared on a 1:1:1 basis
by the Central Government, the State Government and the
Community.
We believe that if 0.75% of our GNP is available as a
part of community contribution by way of supplementation of
governmental spending, health care services can be organised
in a planned manner through the community health
and
educational development combines.
n)
Achievements of Community Health Project of VHS
1977
Crude Birth Rate
Crude Death Rate
Infant Mortality Rate
Couple protection rate
:
:
:
:
39.7/1000 pop.
16.9/1000 pop.
134/1000 LBS
Could not be
ascertained
%of immunisation coverage
among eligible children & :
2
AN mothers
% of antenatal registration
of pregnant women
: Negligible
% of deliveries conducted
by trained health workers:
8
% of mothers receiving
postnatal care
:
Negligible
% of children covered by
child welfare services
:
5
1989
21.4
7.0
36.5
40.2
80
94
40
90
80
These achievements of our mini health centres within
a short span of a decade reveal that there has been
measurable
impact
on the overall
health
status
of
the community served by the project as
evidenced by the
reductions in the birth, death and ifant mortality rates and
the other parameters regarding the provision of various
services.
There cannot be any further proof for the success of
the scheme beyond the fact that 261 mini health centres are
functioning
in Tamil Nadu on the pattern evolved
by
the Voluntary Health Services.
15
Mini health centre scheme has been commended by the
Planning Commission and World Bank. Several National and
International organisations and visitors have shown keen
interest in the programme.
o)
Replication
India is also a signatory to Alma Ata Declaration.
Mere declarations,
slogans, Working Groups,
Task Forces,
Workshops,
Symposia,
Seminars and Discussions will
not
produce the desired result.
It is only the concrete plans of
action at the grass root level that can yield specific
results.
The Voluntary Health Services firmly believes that
the mini health centre model if replicated throughout the
country will not only result in making the comprehensive
health services available at the doorstep of the family but
also generate the much needed additional resources thereby
ensuring community participation.
Several physical and operational targets have been
prescribed for achieving Health For all by 2000 AD by the
Government of India.
We strongly believe that if our
approach is adopted, these targets can be achieved much
earlier than the scheduled date.
The Voluntary Health Services strongly believes that
organisation of mini health centres in the private sector is
not at all difficult.
If sufficient number of voluntary
organisations is not available the local bodies can play the
role of voluntary agency. The service organisations like the
Lions
and
Rotaryclubs,
instead
of
conducting
adhoc
camps,medical camps and project reliefs,
should underwrite
mini health centres which ensure permanancy of the service
and their name.
VII.
M.A. CHIDAMBARAM INSTITUTE OF COMMUNITY HEALTH
The M.A. Chidambaram Institute of Community Health,
which is a unit of VHS supported by the M.A.C.
Educational
and Medical Foundations is totally devoted to-a.
b.
c.
d.
Development of low cost Alternative approaches to
Primary Health Care.
Research into the commonly prevalent community
health problems of the day.
Training of health manpower for the meaningful
delivery of health care programmes.
Consultancy for the propagation of community
health concepts.
The model health cum training centre at Thuraipakkam
has become a trend setter for several national organisations,
individual societies and trusts.
16
PART II
FINANCING OF HEALTH CARE-THE EXPERIENCE OF
VOLUNTARY HEALTH SERVICES
A.
GENERAL OBSERVATIONS ON FINANCING OF HEALTH CARE IN INDIA
The Financing of Health Care in our country
discussed under the following heads:
-------
can
be
Central
State
Jointly by Central and State
Organised Sector
Private
a. Purely Private
i. Private practitioners
ii. Nursing Homes
iii. Private Hospitals
-Five Star
-Three Star
b.
c.
d.
e.
Purely voluntary
Voluntary aided by Government
Spending by individual families
Health Services by industries
While it may be possible to get
data for the
Central,
State, Jointly Central and State sectors
and
organised Sectors for knowing the level of expenditure it is
difficult to study the private spending consequent to:
a.
b.
c.
d.
Number of service out-lets
Non standard pattern of expenditure
Confidentiality of expenditure
Miscellany of activities
Health expenditure of private individuals can only be
guessed.
There are various determinants
for
private
expenditure:
a.
b.
c.
d.
e.
The number of individuals having illness
The episodes of illness
Types of illness
The place of re-dressal
The individual providing attention,
logistics
etc.
17
The health expenditure in the various
plans as a percentage of total public sector
indicated below:
five year
outlay is
Health
Family
Welfare
Total
1st Plan
(1951-56)
3.3
-
3.3
2nd Plan
(1956-61)
3.0
0.1
3.1
3rd Plan
(1961-66)
2.6
0.3
2.9
Annl.Plan
(1966-69)
2.1
1.1
3.2
4th Plan
(1969-74)
2.1
1.8
3.9
5th Plan
(1974-79)
1.9
1.3
3.2
1979-80
1.8
1.0
2.8
6th Plan
(1980-85)
1.9
1.0
2.9
7th Plan
(1985-90)
1.9
1.8
3.7
Period
A perusal of the table reveals that
financial
allocation for the health sector as a percentage of the
overall public sector outlay has never been more than 4%.
In
US it is 10.81% of their much higher income of the total
government expenditure; in Australia it is 9.99%.
Even in
Kenya and Mauritius it is more than 7.0% and in Burma it is
6.96%.
Per capita expenditure
Calculating the percapita expenditure on health by
simple arithmetic is obviously a misleading information.
According to Planning Commission the per capita expenditure
on health has been 46.23 and on Family Welfare 7.19. As 80%
of the health services are in the urban areas,
80% of the
18
expenditure naturally goes to urban areas and a greater
proportion of this goes to the maintenance of multimillion
chromium plated, ivory tower institutions.
The
following
table highlights
expenditure of Maharashtra State:
Total
-
3 cities Bombay Poona Nagpur -
the
percapita
Rs. 156 million
Rs. 14.6
Rs. 12.17
Rs. 6.09
District towns
..
Other Miscellaneous centres
Villages
80.0%
6.2%
9.3%
4.5%
A perusal of the table reveals that in
areas a mere 13 paise is available per person.
the
z'ural
Break-down of Health Rupee
A perusal of the expenditure pattern indicates that
more than 85% of the expenditure goes to maintenance of staff
and only 14% goes to drugs. The question that crops up is
how much of this expenditure really results in accrual of
benefit and of what kind to the ultimate recipients of the
services for whom the entire health hierarchy exists.
Is it possible for the benefits to be quantified
economic terms?
in
Will a mere increase in the allocation of rupees and
consequent increase in the per capita health expenditure
result in tangible benefits in terms of reduction
of
morbidity and mortality? If yes for how long ?
The determining factors seem to be minor ailments
which keepon recurring, Higher threshold for suffering; Low
priority to Health. What would be the proportional costing
of Health rupee ? - Salaries Vs Services/Benefits, Preventive
Care Vs Curative Care.
B.
FINANCIAL ASPECTS OF VOLUNTARY HEALTH SERVICES
I.
Sources of income
There are five major sources of revenue of which the
single largest is through direct patient collections, It
accounted for 55.6% of total income in the calender year
1989.
Other sources of income were, government grant 17.5%;
interest earnings 5.7%; private recurring donations 0.5% and
miscellaneous receipts 4.8%; deficit 15.8%.
The funding
sources are described in detail below:
19
1.
Patient collections
These include actual cut of pocket collections
from patients. They can be differentiated into three
types.
i.
ii.
iii.
made
main
collections from the Medical Aid Plan Scheme
service user charges and
revenue generated from commercial schemes
Each is described in turn.
i.
Medical Aid Plan (MAP)
It was conceived along the lines of
a voluntary
health insurance scheme.
Pre-payment to the plan was to be
made by clients in anticipation of the need for health
services.
The annual premia per household is
graded
The income categorization
according to joint monthly income.
and corresponding membership fee is as follows:
Group
F
PIII
PII
PI
NS
Income
Below Rs. 300/Rs. 301/-750/Rs. 751/-1500/Rs. 1501/-3000/Rs. 3001/-and above
Subscription amount
Rs.
Rs.
Rs.
Rs.
Rs.
24/50/100/200/400/-
Membership to the scheme entitles all household
members to a free annual health checkup.
Curative and
diagnostic services for both out-patient
and in-patient
services are offered at concessional rates to
members.
Assessment of income has always been a challenge.
Evidence of socio-economic status is got in the form
of an income certificate from those in formal employment and
a ration card from those in the casual sector.
The task of income assessment is difficult and
sometimes traumatic one, and that there is a tendency on the
part of patients to cheat whilst declaring their incomes.
Almost 70 to 80% of members are in the lowest socio
economic group, those earning Rs. 300/- or less a month. The
number
of
members in each
category
renewing
their
subscription during the year is low. This suggests that most
members enrol only at the time of an episode of illness when
they require health services.
20
ii.
Service user charges
Fees are levied for all direct personal services.
There is a two tier tariff schedule, where charges are graded
firstly on the basis of whether there is membership to the
MAP scheme,
(which entitles the patient to concessional
health care), and secondly according to income.
There is
thus,
a sliding fee scale for both subscribers and non
subscribers of MAP.
At out-patient department, general consultation is
provided free of charge to all subscribers of MAP.
Non
subscribers are charged for both general and specialist
consultations. All out-patients are charged for drugs at full
cost plus a 10% mark up, except for a few basic drugs which
are provided to the lowest income group at a nominal charge.
Fees for diagnostic investigations, such as X-ray and
laboratory tests are graded by MAP membership and income.
There is an admission charge of Rs. 10/- for all in patients, this is a
flat rate regardless of the length of
stay.
Deluxe Unit patients are charged an admission fee of
Rs. 20/-.
Subsequent in-patient care,
including food,
for
members in the lowest MAP income group('F1)
is free of
charge. Most patients earning less than Rs. 300/- per month
join the MAP on admission. Other categories of patients
(both subscribers and non-subscribers) are charged per item
of service, fee levels are graded to income and membership.
Fees are levied for: bed and medical attendance, operations,
diagnostic investigations and other services.
The pricing
strategy on drugs is identical to the outpatient department,
i.e.,
110% of cost. All categories of patients are charged
the same amount, with the exception of the 1F' group.
Pricing Strategy
Fee levels are set on the basis of an initial market
survey of comparable services in the private sector.
For
example,
for fixing a fee for a chemical pathology test, the
prices
charged
by
closely
located
competitors
are
investigated. Voluntary Health Services sets an identical
fee, or slightly lower, to be competitive, as their fee for
the highest income group in the non-subscriber category.
This charge is then gradually reduced for lower income groups
and MAP members. There has to be an appreciable difference
between
the two fees scales of subscribers and
non
subscribers for the necessary incentive to join the MAP
scheme.
Fees
are revised
technique and rationale.
periodically
using
the
same
21
iii.
Income (revenue) generating schemes
Voluntary
Health Services is operating
several
enterprising schemes which have the sole aim of income
generation.
They are:
a.
The Deluxe Unit - This is comparable to a private nursing
home. Patients are charged commercial rates for rent and
extra medical attendance.
They are charged for all other
services utilised at the highest rate in the
non
subscriber category. The majority of Deluxe residents are
private patients of the doctors serving at VHS under
honorary status.
b.
"A" and "B" class wards - These are special category wards
of Madras Race Club (MRC) hospital.
They are smaller in
size than the general wards and they offer more private
facilities.
There are eight beds of "A" class and twelve
beds of "B" class in the hospital. These are available to
all non "F" group patients who are willing and able to pay
for them.
Bed charges are graded to income and MAP
membership.
c.
Diagnostic Centre-Mylapore - This is located in rented
premises a few kilometers from the hospital. The centre
conducts
laboratory investigations
for
neighbouring
private practitioners and individuals. charges are at
commercial rates.
2.
Donations
Voluntary Health Services receives donations from
private individuals, companies and charitable organisations.
Subscription collections for Society membership are also
included in this category.
Donations are both capital and
recurrent,
although in the previous year there were no
capital
donations.
Most donations are
earmarked
for
specific health activities.
A third category of donation is received 'in-kind',
that is not in direct money terms. A substantial in-kind
donation is the voluntary service of many of the doctors.
There are a number of part time medical officers who are paid
a conveyance allowance only
and some medical officers
receive no compensation whatsoever for their services, they
are accorded honorary status.
3.
Interest on deposits
Voluntary Health Services currently possesses nine
lakhs worth of endowments which are invested in fixed
deposits.
The interest earned from these comprise
a
r&o
22
substantial
proportion of total
recurrent donations,
are usually
activities.
4.
income.
earmarked
These,
like
for specific
Government Grant
The Government of Tamil Nadu has accepted
the
responsibility of contributing to the bed-maintenance costs
of the MRC hospital. This is subject to a bed ceiling of 240
and a cost ceiling per bed day of 15 rupees.
The annual
grant is disbursed in four instalments, the fourth being paid
on
submission of the annual audited
accounts.
This
disbursement procedure leads to considerable delays which
often results in payments in arrears of six months or more.
The State Government also meets,
in part,
the
maintenance costs of Family Planning cases including drug and
supply
costs.
There is a similar
delay
in
grant
disbursement.
In addition to recurring costs, the VHS gets building
and equipment grant on 50:50 basis subject to a ceiling of
Rs.30 lakhs.
II•
Cost Structure
Total expenditure of VHS hospital and medical centre
in 1989 was 41.67 lakhs, which was distributed amongst the
major heads as follows:
Establishment
General Administrative expenses
Repairs and Renewals
Sundries and Linen
Consumable and Services
Utilities
Drugs
Diet
44.2%
1.4%
4.5%
10.9%
7.2%
9.5%
19.4%
2.9%.
Cost Components
1. Establishment Charges
Establishment costs consume the largest share of
budget at Rs.41.67 lakhs.
the
The above figure does not include the imputed cost of
donated medical staff time. The full time salaried staff at
VHS are receiving wages considerably lower than equivalent
government employees. As an example, the wage bill for fulltime doctors at VHS is estimated to Rs.1.5 lakhs below its
equivalent government salary level.
23
2.
General Administrative Costs
This expense head includes printing and stationary
costs, postage and telegram, freight, cooly and conveyanca
allowance, advertisement charges, bank and overdraft costs,
audit fee, subscription and miscellaneous expenses.
3.
Consumable and Services
Under this head, are costs of X-ray and chemicals,
blood transfusion charges, medical gas, fuel gas, washing
charge and ambulance expenses.
4.
Utility expenses
This includes electricity and telephone charges.
5.
Diet
This head includes the cost of feeding 'F' group
patients and the few non 'F' group patients who request food.
C.
FINANCIAL ASPECTS OF MINI HEALTH CENTRE SCHEME
I. Sources of Income
Under the Government of Tamil Nadu pattern, the Mini
Health Centres get 2/3rds grant i.e., Rs.18,000/- (Rs.9,000/from Centre, Rs.9,000/- from State Government).
The VHS
share
(Rs.9000/-)
comprises, Mini Health Centre
(MHC)
collections,
interest earnings, donations in cash and kind,
the
shortfall
in the cash contribution
is
met
by
miscellaneous receipts.
Mini Health Centre collections are of two types:
i. The Medical Aid Plan (MAP) subscriptions
ii. Non subscriber user charges.
The Mini Health Centre MAP scheme is similar in
concept to the Hospital and Medical Centre plan. Pre-payment
to the plan entitles members to concessionary or free health
care.
Free service entitlement at the Centre includes health
record
maintenance,
Doctor
and
Multipurpose
Worker
consultation,
drugs and referal to the hospital,
free
outpaient and in-patient care. The scheme enrolment fees are
identical to those of the hospital and are similarly graded
by income.
The majority of MHC members are in the lowest
income category, earning less than Rs.300/- a month.
Total
membership in each centre is low. There is great resistance
to join the scheme, unless there is need for referal
treatment at the hospital. This may be a reflection of the
community's willingness to pay for curative care which shows
24
tangible results and not for preventive care where the
benefits are not so easily identifiable. VHS has found the
task of selling the concept of insurance a difficult one.
II.
Cost Structure
Under
the government funded scheme the
annual
estimated budget of each centre is subject to a cost ceiling
of Rs.27,000/-. The estimated distribution of costs under
various expense heads is shown below:
Annual Budget per Mini Health Centre:
2 MPWs (@ Rs.400/- per month)
3 LFAs (@ Rs.50/- per month)
Drugs in LFA kit
Doctor (part time) @ Rs.300/- per month
Drugs at Mini Health Centre
Supervision, contingencies
Provision for accommodation
D.
9,600/1,800/600/3,600/6,000/3,600/1,800/-
FACTORS CONTRIBUTING TO THE SUCCESS OF VHS
PARTICULAR REFERENCE TO GENERATION OF REVENUE
-
WITH
1. Board of Trustees
The affairs of VHS is overseen by a Board of Trustees
consisting
of eminent individuals,
industrialists
and
philanthropists.
The
Accountant/Auditor
General
of
Government of Tamil Nadu is a member of the Board of
Trustees. This Board plays a paternalistic watchful role.
2.
A Strong Central Committee
The general directory for conducting the affairs of
the institution comes from a Central Committee of both
elected
and nominated members.
The nominated
members
represent large donors whereas the elected members are drawn
from cream of medical professionals, businessmen and those
in other professions.
The members of this committee, in
addition to giving broad direction help to a certain extent
in locating sources of resources, for tapping.
3.
Charisma of Individuals
The success of VHS to a large extent is due to
personalities, notable among whom is Dr. K.S. Sanjivi.
The
individual consultants like Dr. Murali, Dr. B. Ramamurthi and
others have also contributed in no less a measure not only
for the attraction of resources but also in the matter of
utilisation of the facilities as well.
25
4.
Good accounting system
The accounting system of the VHS has been flawless
and
has contributed to a large extent in
instilling
confidence among various donors - institutional,
individual
and
governmental, that the money donated is
properly
accounted and utilised for the purposes for which it has been
given, keeping the overheads low.
5.
Openness
The VHS has been absolutely open in receiving ideas
and in contributing to the growth of similar organisations
elsewhere in the State. The approaches, the flexibility and
the humaneness have been the hall-marks of success.
6.
Lack of bureaucratisation
The voluntary spirit has to be inhibited by one and
all
once they have agreed to serve the
institution.
Sacrifice is universal in the campus and only the degree
varies.
The entire administration at the top level is by a
system of understanding and mutual love. Even today, after
twentysix
years of establishment we do not
have
an
administrative manual or a detailed charter of delegation of
powers.
The decision regarding staff matters are taken in a
spirit of understanding. Anybody can approach anybody else
in the organisation without inhibition.
7.
Administrative and Academic freedom
The top level professionals of the institute are
attracted for service because of the administrative and
academic freedom they normally enjoy.
8.
Income Tax exemptions
The success of VHS to a large measure is due to
Income
Tax
exemption provided to
individual
donors,
institutions,
trusts, and foundations. Two types of Income
Tax
exemptions are available.
For
research
oriented
programme 100% exemption under 35, l(ii) is available and for
other donations 80G facility is available.
9.
Honesty in approach
The
Philanthropy
that has been
generated
is
singularly
based on the honesty in approach
of
the
administration.
The records of VHS are open and can be
scrutinised
by any one and this frankness
has
been
appreciated by one and all. Whatever little we are able to
pay our staff we pay in full inspite of non receipt of
grants etc. in time as a rule.
26
10.
Dedicated and committed staff
The dedication and the commitment exhibited by the
core group of the professionals and para professionals is
another source of strength to the VHS.
11.
Poor pay-scales
The low establishment charges are due to poor pay
scales when compared to similar categories in Government
service.
Though we began with Government scales, we are
unable to keep pace with governmental scales due to obvious
reasons.
12.
Shram Dan
Majority of staff
are working in an
honorary
capacity, getting a so called conveyance allowances which in
affect in a lighter vein amounts to radiator water allowance.
As already stated, the Shram Dan is universal in the campus,
only the degree varies.
Because of the voluntary nature, the
over heads of several items like drugs,
linen,
laundry,
stores, electricity, telephone are comparatively less due to
economy of expenditure.
13.
System of control
The inventory control at various levels
though
manually done help in the reduction of costs and unnecessary
waste of resources and also avoids blockage of resources.
14.
Government Support
The success of the VHS cannot be as what it is today
but for the support extended to it, by successive Governments
at the State and Central levels. The Tamil Nadu Government
gives a bed-maintenance grant of Rs. 15/- a bed per day.
In
addition,
it also gives 50% of the capital expenditure
subject to a ceiling.
E.
THE DRAWBACKS
1.
Turnover of staff
Due to poor pay scales and due to young age, the
lower categories of staff work for a short time,
while
awaiting for a Government job or for a job better prospects.
This is even more in the case of the projects undertaken by
the VHS, consequent to lack of job security.
2.
Lack of finance for further expansion
Though the VHS has got a number of ideas for making
available health care services within the
reach of the
27
common man and it has got both land and infrastructure
facilities for further growth; lack of adequate finance
hampers its enthusiasm for rapid expansion. Nevertheless the
VHS
has
expanded
through dedicated
work
aided
by
philanthropy.
3.
Thinning away of committed people
The old band of committed and dedicated workers is
thinning away due to attrition by age and death. Though a
majority among the younger generation do not lack in honesty
and sincerity, due to the pressures of day to day life and
rising costs, the ability of people for continually doing
dedicated and committed services without meaningfull returns
is causing a problem.
4.
Not being able to keep pace
As Medical science is expanding rapidly and more and
more sophisticated gadgets are becoming available, the VHS is
not able to keep pace with the five star hospital culture.
VHS realises that most of the gadgets may not be necessary
for purposes of diagnosis of a majoraty of illnesses.
Due
to a process of comparison the referral organisation gets
singled out by not possessing them.
5.
Thinning of philanthropy
The main handicap is the inadequacy of financial
resources
available and this inadequacy is
increasing
continuously because private charity is being spread too
thinly
over
an ever increasing number
of
voluntary
organisations.
It is obvious therefore that the voluntary
organisations
can
play
a very vital
part
in
the
reconstruction of health care, if the three principal assets
are recognised and
developed to the full and if their
principal handicap is obviated through special financial
assistance.
6.
Impact of corporate/organised sector
Because
of
the advertisement
technology
and
different value orientation corporate sector is able to
attract even the middle class. The VHS has been established
to serve the underprivileged community and the middle class
people living around it on an area concept.
But due to
development of organised sector on an occupational concept,
the VHS finds it difficult to attract clientece from those
sectors who are living around it.
7.
Low priority to health
In our country health is not a priority. It becomes
a priority only if the illness causes considerable amount of
28
suffering and the poor in the countries have a high threshold
for suffering due to our more pressing needs. To-day, people
visiting hospitals are bothered about quick attention of
their ailments and even quicker cure.
It may not be out of
place to mention here that the morbidity load in the
community at any given point is 94% and 92% of this,
is
formed by minor ailments.
8.
Failure to appreciate value of medical records
The VHS has a laudable objective of developing much
needed health information through the evolution of family
oriented health records from womb to tomb.
Today people
visiting hospitals are bothered about quick attention of
their ailments and even quicker cure. Nobody else seems to
emphasise on the value of records.
9.
Paying for health care
For centuries, people have been told that health care
will be free. Nothing in the world is free except air and
that is polluted.
It costs somebody to provide for the
health care. While people derive pride in spending for food,
clothing and shelter they resent paying for their health.
Even those in higher income brackets, do not feel shy to
underquote their salaries when it will cost them less than
what it would, had they declared their true income.
This
'cheating'
has become universal with the result,
true
asessment of income is becoming well neigh impossible.
This
results in short-fall of the anticipated expenditure. We are
of the firm opinion that if the rich and poor alike
contribute 0.75% of their annual income, quality primary
health care services can be made available to one and all
irrespective
of their economic status
and
geographic
domicile.
The under mentioned plan for 'Community Health
Development and Education Combines' of ours still remains on
paper for want of seed money for trying it out on an area
concept.
It is our dream that all the health expenditure by
the. Central,
State and local bodies organised sectors and
voluntary
spending should be pooled into a common resource
pool and there should be a single uniform channel for
providing primary health care services, irrespective of their
economic
status
or
geographic
domicile.
Community
contribution should also be pooled into this resource pool.
This Community Health and Education Development Combines
(COHEDEC)
will be totally responsible for the delivery of
health services on an area concept.
If necessary
for
mobilising
resources,
a
small health
cess
may
be
contemplated.
- Media
 4559.pdf
4559.pdf
Position: 1903 (6 views)