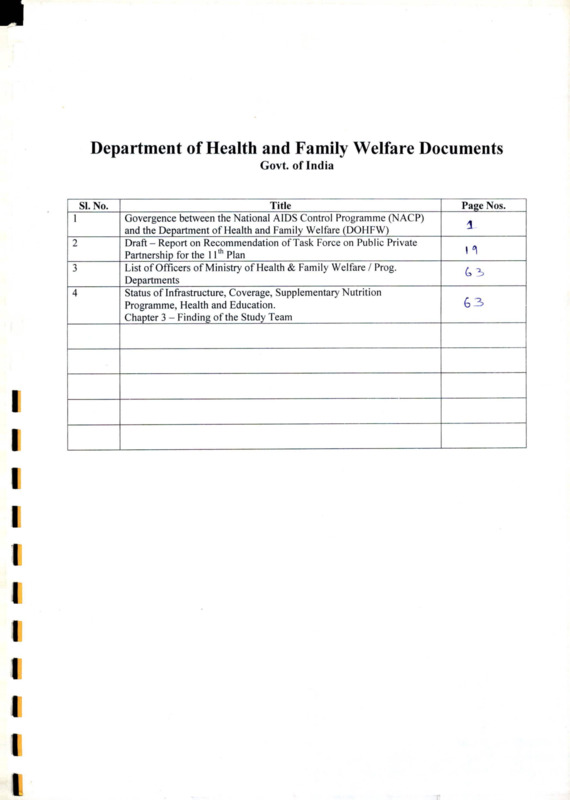
Department of Health and Family Welfare Documents
Item
- Title
- Department of Health and Family Welfare Documents
- extracted text
-
Department of Health and Family Welfare Documents
Govt of India
SI. No.
1
2
3
4
I
1
I
I
_________________________ Title_______________________
Govergence between the National AIDS Control Programme (NACP)
and the Department of Health and Family Welfare (DQHFW)______
Draft - Report on Recommendation of Task Force on Public Private
Partnership for the 11th Plan_______________________________
List of Officers of Ministry of Health & Family Welfare / Prog.
Departments___________________________________________
Status of Infrastructure, Coverage, Supplementary Nutrition
Programme, Health and Education.
Chapter 3 - Finding of the Study Team
Page Nos.
3
I °\
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 1 of 17
CONVERGENCE BETWEEN THE NATIONAL AIDS CONTROL PROGRAMME (NACP)
AND THE DEPARTMENT OF HEALTH AND FAMILY WELFARE (DOHFW)
1.
INTRODUCTION
1.1 The HIV/AIDS epidemic in India is complex, with intense focal epidemics among sub groups
(IDUs, Sex workers, Truckers, Men who have sex with Men) in some states, situations where
prevalence is over 1% in the general population, and low prevalence in some others states. In states
like Andhra Pradesh, Karnataka, Tamil Nadu, Maharashtra, Manipur, and Nagaland, prevalence
among antenatal women (based on sentinel surveillance data (2003) located in ANC clinics),
considered representative of the general population, is around 1.25%. Annexure 1 provides state
wise HIV prevalence levels from 455 sentinel surveillance sites, for the year 2003. NACO has
classified states as high prevalent, medium prevalent, highly vulnerable and vulnerable states
(Annexure 2). The index of vulnerability is based on extent of migration, size of population, and
poor health infrastructure. Among highly vulnerable states are: Bihar, Rajasthan, MP, UP,
Uttaranchal, Chhatisgarh, Jharkhand, Orissa, and Assam. This includes all the EAG states of the
DHFW.
1.2 There is a pressing need to scale up prevention strategies based on factors of risk, vulnerability, and
impact, expand delivery of interventions and ensure that populations at risk and vulnerable groups
are reached. India is at a stage in the epidemic where all sexually active individuals must be offered
information and services on preventive interventions. Sexually active youth, particularly girls are at
high risk given the paucity of needs specific information and services. HIV/AIDS infection
prevalence is increasingly acquiring gender connotations. Sentinel surveillance data also show that
women account for more than half of all infections in rural areas (nearly 60%) and about two fifths
of all infections in urban areas. Sentinel surveillance sites are located mainly in either Antenatal
clinics or in STD clinics. Given the evidence that most STD clinic attendees are men, it can be
assumed that most women who are positive are also pregnant, a rather ominous portent for risk of
transmission to newborns, and a substantial justification to expand the number of sites offering
PPTCT.
1.3 Convergence between the National AIDS Control Programme (NACP) with over a decade of
experience and technical competence in HIV/AIDS prevention and care interventions and the Health
and Family Welfare programmes (HFW) with its infrastructure, human resources and capacity
reach to every village and community is critical to ensure scaling up and effective service delivery.
1.4 Behavior Change, prevention/management of RTI/STI and condom promotion are the cornerstones
of HIV/AIDS prevention. All three areas have a significant degree of overlap with interventions in
the Reproductive and Child Health programme, since target groups and services fall in the same
arena. Other areas of prevention linked to HIV/AIDS interventions and which have implications for
services in the HFW are Voluntary Counseling and Testing, (VCTC), Prevention of Parent to Child
Transmission (PPTCT), and ensuring safety of blood and blood products. Comprehensive
HIV/AIDS Programmes include components of both prevention and care. VCTC and PPTCT are
two areas of overlap between prevention and care strategies. Areas of cross cutting importance that
need to be addressed in prevention and care strategies include: gender, private sector involvement,
and reduction of stigma and discrimination among health care providers and communities.
(Figure 1)
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
I
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 2 of 17
Prevention Strategies
Behaviour Change
RTI/STI management
Condom Promotion
Blood Safety
Harm Reduction
VCTC
PPTCT
Stigma
ovc
Care Strategies
Clinical Mgmt.-OI,
ARV
Home/Community
Care- nutrition
asepsis, psychosocial.
Referral Networks
strengthening,
Legal Support
2, CONVERGENT TECHNICAL STRATEGIES AND PROGRAMMATIC INTERVENTIONS
OF NACO AND HIAV
2 1 The National AIDS Control Organization (NACO) is the implementing agency for the NACP. At
the state level, State AIDS Control Societies (SACS) implement HIV/AIDS interventions.
Currently NACO and the SACS support about 900 NGOs for targeted interventions aimed at
reaching the so-called high-risk groups, (those with high numbers of sexual encounters increasing
possibility of transmission, such as Sex Workers, Truckers, Men who have sex with Men,
Intravenous Drug Users, Adolescents, Migrant men and women,). They also support behaviour
change communication aimed at the general population through variety of mechanisms. The reach of
the NACP to men and in urban areas is significant.
2 2 In the public sector, NACO and the SACS support RTI/STI management, VCTC, PPTCT, Blood
Safety, and several other interventions. However the reach of these interventions through the health
system is primarily through teaching hospitals and medical colleges, district hospitals and in the case
of the six high prevalence states, taluk hospitals as well. The SACS in the high prevalence states
(most of which are the ones with better health infrastructure and moderate to high care seeking) are
also active in implementing HIV/AIDS interventions.
2 3 The Department of Health and Family Welfare at National and State levels (with state specific
variations) supports a range of services for improving primary (including reproductive) health care at
community primary, secondary and tertiary levels. Community based interventions are pnmarily
provided by the Auxiliary Nurse Midwife located at the sub center. The coverage of the sub centre
is about 5000 (3000 in tribal areas) and covers about the area of three to four gram panchayats.
Service delivery is through the sub center on fixed days, supplemented by outreach visits to the
coverage area. At the village level, the Anganwadi Worker (AWW) and/or the Traditional Birth
Attendant (TBA) often assist the ANM. With the advent of the National Rural Health Mission it is
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 3 of 17
expected that the ANM will soon be supported by a female community health volunteer (ASHA), and
assisted by the AWW and TEA. Thus the potential reach of the system will be to every community
and habitation. In addition to the public sector health system, the DHFW supports NGOs (through
the Mother NGO scheme) to implement a range of RH interventions (Safe motherhood, family
planning, adolescent health, RTI/STI management, child health, and male involvement) in areas
underserved or not served by the public sector system. While the DHFW through its flagship RCH
project does include enhancing male responsibility as a key intervention, the emphasis is on women
and children. Urban health is a component of the RCH 2 programme.
2.4 The following areas of convergence have been identified
for scaling up HIV/AIDS prevention
responses: RTI/STI management, Condom Promotion, Voluntary Counseling and Testing,
Prevention of Parent to Child Transmission, Behaviour Change Communication, Blood Safety,
Training, and Management Information Systems. In addition male involvement and ensuring
convergence of NACP and DHFW through strengthening urban health infrastructure and reach are
two additional strategies, which are common to the major areas identified above.
2.5 This paper provides a broad framework for action to address the major convergence areas. The
effectiveness of convergence of key interventions is dependent on several factors, but critical is the
operationalization of convergence within well functioning health systems and programme
management structures at all levels. RCH II has been designed to address reproductive and child
health interventions through a framework of health sector reforms at various levels. It is opportune
that NACO and DHFW jointly look for ways to improve reach, enhance access and coverage,
provide quality services, address synergistic intervention elements, and prioritize interventions
based on prevalence, infrastructure, current programme efficacy, and resources. It must be
emphasized that this framework is proposed at the National level and state level consultations with
key stakeholders are necessary to operationalize the plan in the context of state realities.
2.6 Section 3 provides substantive details on each convergence area, with a brief technical background
for each area, highlights current interventions of NACO and DHFW, identifies points of
convergence in order to reach groups and communities that are at risk and vulnerable, and defines
broad areas for operationalizing these strategies. Section 4 includes operationalization of
convergence and details institutional mechanisms to facilitate convergence. Section 4 is
supplemented by a matrix, which summarizes key convergence areas, primary responsibility, and
convergence aspects. Section 5 briefly discusses next steps.
3. OPPORTUNITIES AND ISSUES FOR CONVERGENCE
3.1
RTI/STIprevention and management
3.1.1
Background: RTI/STI has a severe impact on the reproductive health of individuals as well
as significantly enhances the risk of transmitting or acquiring HIV/AIDS. Women are
biologically more vulnerable to acquiring RTI/STI and consequences of STI in women are
more serious (ectopic pregnancy, pelvic inflammatory disease, still births). Unequal gender
relations resulting in sexual coercion is more pronounced among women, and women often
have limited access to care. There is evidence that RTI/STI care is more often sought in the
private sector than in the public sector and in several places from untrained practitioners as
well as chemists. There is little published comparable and reliable data on RTI/STI in the
country. Efforts at programme planning have been based on micro studies conducted with
different methodologies, using varying criteria and for clinical and laboratory diagnosis.
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
3
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 4 of 17
3.1.2
DHFW strategies: The National STD control programme has been in place since 1946.
However, it was only in the RCH 1 programme, that RTI/STI management was includedion
a national scale. Many donor-funded programmes in states have also supported Rll/S
services through state health and family welfare programmes. While there are no formal
evaluations to assess the performance effectiveness of these efforts, anecdotal evidence
suggests that several lacuna hampered these efforts and they remained largely out of the
reach of women and men in need of services. Current policy guidelines stipulate that only
medical officers are allowed to prescribe RTI/STI drugs, thus limiting the reach of effective
RTI/STI services.
3.1.3 NACP strategies-. RTI/STI management has been attempted through several approaches:
a. NGOs working with High Risk Groups on targeted interventions are provided with support for
medical personnel, clinics, and Drugs for RTI/STI. In some instances NGOs collaborate with the
public health system or private providers to provide STI diagnostic and treatment services.
b. Annual Family Health Awareness Campaigns are held across the country. These are two week
campaigns which are period of heightened activity at the district level and below when the
machinery of the HFW system is expected to conducts house to house and group education, media
and advocacy events and promote care seeking for RTI/STI. Patients are referred to PHC and
above, where RTI/STI are treated using the syndromic approach. Annexure 3 provides details of
the achievements of FHAC from 1999 to 2003. Coverage increased from 100 districts to 572
districts.
.
.
c. NACO has provided support to establishing STD clinics at hospitals upto and including district
hospitals. By the end of fiscal 2004, NACO had supported 735 STD clinics in all medical
colleges and in most district hospitals. Each STD clinic includes a qualified STD specialist and
laboratory support for diagnosis and treatment of STI. NACO also ensures a continuous supply of
STI drugs. (Annexure 4 provides details of number of STD clinics in each state)
NACO
supported training of a range of HFW providers (MO, ANM, LHV, Laboratory
d.
technicians) in areas such as RTI/STI, universal precautions, nature and content of HIV/AIDS
programming, stigma and discrimination. Annexure 5 provides details of personnel trained.
3.1.4
Core Convergence Recommendations for RTI/STI:
From the above data it is clear that NACP interventions in the public sector system reach only the
district hospitals and are not programmed to be gender sensitive. Although Medical officers have been
trained in syndromic diagnosis, they are located in primary health centers and above. Current utilization
of PHCs is low. Thus the benefit of the knowledge and skills of the medical officers does not reach
communities in many parts of the country. The FHAC could do a good job of spreading awareness but
services are still provided at the district level, reducing reach. DFW interventions are also primarily
through medical officers. Grass roots workers such as the ANM in most areas are not empowered to
provide information and services for RTI/STI. There is little by way of health education at the
community level on RTI/STI, which highlights issues of risk and vulnerability, male responsibility, and
the use of condoms for dual protection. This varies from state to state and in high prevalence states,
awareness levels are high, but access to services remains low. One of the challenges that needs to be
taken into account while converging the programme into the DHFW programme is that the reach to
important core and bridge groups such as: “sex workers, men who have sex with men, men in the
general population, and youth. RCH II does include interventions to address youth, enhance male
responsibility, and health in urban areas and care must be taken to ensure that convergence mechanisms
address the inclusion of such groups.
a. Public Sector interventions from district to peripheral level for RTI/STI to be implemented
through DHFW, in line with the RCH II design document. RTI/STI prevention, management of
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 5 of 17
b.
c.
d.
e.
f.
3.1
the client, partner notification, treatment, and follow-up are the key components of an RTI/STI
programme. Comprehensive RT/STI treatment will be provided at CHC and 24 hour PHC
(clinical and etiologic) and first line drugs at the PHCs.
RTI/STI control among High Risk Groups through NGOs with funding support for RTI/STI
diagnosis and treatment, to continue through NACO and SACS, but reporting also to HFW.
It is expected that ASHA will be provided with enough information/supplies to support health
education, prevention advice and treatment facilitation (through referral) at the village level.
Presently the closest possible site for services by trained personnel is the sub center level. The
ANM/Male MPW will be the frontline service providers for RTI/STI management, MO/SN/LHV
at the PHC level, and MO/Ob-Gyn. at the CHC/FRU level. It is expected that over time, with
strengthened Primary Health Care, laboratory based management of RTI/STI will be the norm
rather than the syndromic approach. At the CHC level, basic screening tests for RTI/STI will be
made available. At the district level, RTI/STI will be managed by STD specialists supported by or
linked through referral to high quality laboratory services supporting the full complement of
laboratory tests for RTI/STI.
At the community health centers and district hospitals, RTI/STI management has to be included in
protocols in Ob/Gyn and Medicine departments. Medical and paramedical professionals to be
oriented to risk identification and referral to VCTC.
NGOs under HFW to include RTI/STI in their package of interventions, with referral or services
as appropriate.
Private providers (reached through Indian Medial Association (IMA) and Federation of Obstetrics
and Gynaecology-FOGSI ) to be part of RTI/STI management strategy for training and to ensure
appropriate reporting and notification, particularly in the case of sexually transmitted infections
and drug resistance surveillance. This will also need to be implemented through DHFW.
Voluntary Counseling and Testing Centers (VCTC)
3.2.1
Background: Voluntary Counseling and Testing is now acknowledged as an efficacious and
pivotal strategy for prevention and care for HIV/AIDS. Counseling is an important skill and is a
necessary part of interventions for several areas within Family Welfare, family planning, safe
motherhood, RTI/STI, and in dealing with youth. It is also more cost effective to integrate VCT
into sexual and reproductive health services, rather than support them as freestanding sites.
Counseling requires specialized skills and attitudes, space to assure confidentiality, laboratory
services for testing, adequate reporting systems.
3.2.2
DHFW strategies: While counseling is an important element of several reproductive health
services, counselors are not part of the health provider cadre. ANM, LHV and other providers
have been trained in basic motivation, interpersonal skills, but these are not dealt with in any
depth, nor are they geared toward attitudinal change. It has thus far formed part of an integrated
training package. In some states donors have supported separate training to improve counseling
and motivation skills of ANM and LHV (UNFPA through IPD projects, USAID in SIFPSA), but
only in selected districts.
3.2.3
NACP strategies: NACO and the SACS have established 650 VCTCs across the country with
about half of them located in high and medium prevalence states. They are primarily located in
medical colleges and district hospitals. Annexure 6 provides state wise details of numbers of
VCTC. Each VCT includes one male and one female counselor, and one laboratory technician.
NACO and SACS supply testing kits for these VCTCs. In the medical colleges, the VCTC are
located within the microbiology departments (with counselors reporting to the HOD,
Microbiology) and in charge of the Pathologist in a district hospital. Currently the view of the
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 6 of 17
State AIDS Control Societies is that VCTC utilization is low, particularly in the low prevalence states.
3,2.4
Core Convergence Recommendations for VCTC
The NACP will manage the VCTC in collaboration with the key staff of the facility in which
the VCTC is located. Youth information centers to be established with the VCTC to increase
access of young people to information and referral for services for a range of reproductive
and sexual health issues.
b. NACP will support the staff of VCTC and supplies required with DHFW will provide the
physical infrastructure.
c. It is proposed that the district VCTC function as a satellite center to coordinate, support and
supervise operations of the VCTC’s located in the CHC and 24 hour PHC. This internal
coordination is important for several reasons- to maintain quality of services at all sites, to
ensure uninterrupted supplies, link with PPTCT at district and CHC levels, and to enable
referral linkages of clients that test positive to appropriate centers.
d. VCTC’s will not function as sites for counseling of HIVAIDS alone. Counselors in VCTC,
particularly at secondary and primary health care levels should be able to counsel for family
planning, RTI/STI prevention, safe delivery, and male responsibility. A cadre of counselors
could be established who would serve the RH needs of women and men, including
HIV/AIDS, and the RH information and service for young people. It is hoped that this
measure will increase utilization of VCTC.
e. Expand the number of VCTC sites. The expansion should be informed by a rapid
assessment of VCTCs in low and high prevalence areas, and identify systems issues, human
resource training gaps, and logistics. The expansion is proposed in a phased manner, and
will be governed by the following: prevalence, physical infrastructure, human
resources, and community use of facilities. Fortunately the high prevalence states also
have better infrastructure and increased utilization (higher rates of antenatal coverage,
institutional deliveries, and overall increased care seeking behaviour). As a long-term plan,
(by 2012) it is expected that all PHCs will have VCTC facilities that will cover a range of
services beyond just HIV/AIDS counseling. The expansion process is proposed as follows:
Phase 1: (2005-2008) In the high prevalence states, district hospitals, all CHCs and all 24
hour PHCs will have Voluntary Counseling and Testing Centers, staffed by a full
complement of male and female counselors; separate space and laboratory back up. In
the low prevalence centers, VCTC could be located at the district level and at all CHCs.
In high prevalence districts within low prevalence states, the choice of whether 24 hour
PHCs could offer VCTC could be left to the state.
Phase 2: (2008-2010) All PHCs in high prevalence states and 24 hour PHCs in other
states will have VCTC.
Phase 3: (by 2012): PHCs, all CHCs and district hospitals, will offer VCTC services.
Expansion will be based on review of past experience, utilization and need.
f. Basics of Counseling for all cadres of staff (sub center to CHC) to be included in training
package, so that at the very minimum all staff have the skills to enable clients to understand
risk perception, motivate them to seek services, and finally be able to facilitate informed
referral.
g- Involvement of private providers and private laboratories, through IMA, FOGSI, and
pathologists Association, where testing takes place to ensure that their clients also are
counseled and their data is reported at district and state levels.
h. NGOs under HFW programme and NGOs working with High Risk Groups to include
information on VCTC functions and sites so that they can carry the message to the
community, and increase utilization as appropriate.
a.
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 7 of 17
3.3 Prevention ofParent to Child Transmission (PPTCT)
3.3.1
Background: Core PPTCT interventions need action in the community, and depending on the
package of services offered, at the levels of the sub center, Primary Health Center and at the
Community Health Center. PPTCT interventions for HIV positive women relate to a range of
services provided in the HFW system: antenatal, delivery, and postpartum care, abortion
services, VCTC, Management of STIs in pregnancy, Antiretroviral therapy based on current
policies- (currently Nevirapine), Family planning counseling and easy access to services,
Expansion of well baby clinics, high quality education and information provision on nutrition,
breastfeeding, RTI/STI, and HIV/AIDS, male involvement in MCH care, and linkages to
community based care and support programs for HIV/AIDS.
3.3.2
DHFW Strategies: DHFW per se does not implement PPTCT interventions. Currently PPTCT
interventions are being provided in selected locations through the health facilities of HFW.
However, training, supplies and logistics, and drugs are primarily supplied through NACO.
3.3.3
NACP strategies: Currently NACO is providing PPTCT services in 273 units across the country
of which 234 are located in high prevalence states. Annexure 7 provides details of PPTCT in the
country presently. They are primarily located at the medical colleges of high and low prevalence
states and at district hospitals only in the high prevalence states. They are located in the Ob/Gyn
department. A counselor, mostly female and one laboratory technician staff each PPTCT. Staff
of PPTCT sites (PPTCT team- Ob/Gyn, Microbiologist, Paediatrican, Staff nurse, and one health
educator) are trained for five days. Counselors of PPTCT are trained for a ten-day period.
Sensitization training of other staff in the facility where the PPTCT site is located is also
conducted.
3.3.4
Core Convergence Recommendations for PPTCT
a. The management of PPTCT sites should continue to be with the NACP, since all clients of the
PPTCT will need to be followed up for care and support. At the institution level, the PPTCT staff
will continue to report to the Head of Ob/Gyn. PPTCT at the district level will function as the hub
or satellite center to coordinate quality, supplies, reporting and facilitation of referral.
b. NACP will fund the counselor and laboratory technician in the PTCT and the supplies required for
the PPTCT programme. The PPTCT will be located in the Ob/Gyn department of the CHC and
will function through existing staff.
c. PPTCT sites should be expanded in a phased manner. Since PPTCT is a function of the obstetric
department, and since RCH II is focusing on improving/strengthening access and quality of
institutional deliveries, PPTCT can be implemented within the framework proposed for RCH II.
Phase 1 (2005-2008): All district hospitals and CHCs to offer PPTCT, regardless of prevalence.
Phase 2 (2008-2010) In high prevalence states, 24 hour PHCs, should also offer PPTCT.
Phase 3(by 2012 years): 24 hour PHCs in all states to offer PPTCT services, based on
prevalence, utilization, and need.
d. At the community level, ASHA/ANM will be trained through health education and motivation
among women and men for risk perception, risk identification, facilitation in accessing VCTC,
and thus identifying positive women in need of PPTCT. Para medical and medial providers at the
PHC level will also be trained in similar areas to facilitate referral to PPTCT and enable follow
up.
e. Positive women will be followed up through pregnancy by ANM/ASHA and encouraged to opt
for institutional delivery in district or CHC/FRU.
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 8 of 17
f. PPTCT programmes should establish linkages with the Integrated Management of Neonatal and
Childhood Illnesses (IMNCI) component of RCH II, to address issues of infant feeding, nutrition,
and infections.
g. All providers would need sensitization on issues of stigma and discrimination, so that positive
women do not fear institutional deliveries. PPTCT teams should be specially trained in areas of
infection prevention, and stigma and discrimination attitudes, as well as the specific technical
aspects of PPTCT
h. Institutions to be strengthened to adopt universal precaution measures and waste management.
Delivery kits to be made freely available under the PPTCT programme.
i. Orientation and sensitization of private providers (through IMA, FOGSI, Indian Health Care
federation, Hospital forums and associations) and involvement of private hospitals in VCTC and
PPTCT as appropriate.
j. NGOs supported by DHW and NGOs working with high-risk groups to be provided with
information on location of PPTCT sites and encouraged to facilitate referral and follow up.
3.4 Behavior Change Communication
3.4.1
3.4.2
3.4.3
3.4.4
Background: Changing individual and community behaviour is critical to HIV
prevention In order to impact the epidemic it is necessary to target behaviour change
interventions at the individual level to increase knowledge, enhance risk perception, and
develop safe sex skills. These are primarily through interpersonal communication and
small group discussions and peer education. Such efforts at the individual level need to
be reinforced by community level interventions to increase understanding of a supportive
environment to reduce risk and vulnerability, and influence societal norms. Messages
that are targeted to sexually active individuals include: postponing age of sexual activity,
using condoms correctly and consistently, decreasing number of sexual partners,
increasing STI and TB treatment seeking and prevention behaviors.
DHFW strategies: HFW has not integrated HIV/AIDS messages in BCC material till
date. However, in the past few months, efforts are on to integrate HIV/AIDS prevention
messages in some initiatives of the HFW department- wall calendar and diary for 2005 of
the MOHFW includes HIV/AIDS messages. Adolescent health education and life skills
programmes have included HIV/AIDS content quite substantially, especially in the
adolescent friendly health clinics, piloted by MOHFW.
NACP strategies: At the National level, NACO frames guidelines for IEC activities
countrywide and undertakes multimedia campaigns along with political and media
advocacy. NGOs working with high-risk groups for targeted interventions develop their
own BCC strategies. SACS in each state have mass media campaigns and other activities
for general population- varied across states and school AIDS Education programmes.
Core Convergence Recommendations for BCC
Create a mechanism to ensure that the leadership for developing BCC strategies and
programmes for DHFW and NACP is vested with one authority.
Joint (NACO, DFW) behaviour change communication strategy to be developed based on
commonality of target groups, and tailored for reach of general as well as high-risk
populations. This needs to take place at state level as well between State AIDS Control
Societies and State IEC bureaus.
3.5
Condom promotion
3.5.1
Background: Currently the male condom is the most widely available effective protection
•8
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and the ... Page 9 of 17
I
method against HIV and other STI. Condom distribution can be through free or social marketing
channels. They could be through community based distribution systems, depot holders, health
facilities, pharmacies, and village stores. For any scaled up prevention response it is important
to improve access and availability of condoms to all communities (rural and urban) and groups.
3.5.2 DHFW Strategies: In the family welfare programme, male condoms are promoted as a method
of contraception. In order to improve the use of condoms as a contraceptive, several initiatives at
social marketing and distribution through government and NGOs are being undertaken. Thus
DFW is the repository of substantial experience in promoting condom use as well as condom
procumbent and distribution. However the use of condoms as a method of dual protection has
not been promoted so far. About 25% of the overall condoms procured are distributed as free
supplies with 75% being programmed though social marketing agencies. Of these 25 %, over
three quarters are channeled to NACO for distribution to HRG through NGOs.
3.5.3 NACO strategies: Currently NACO procures and supplies condoms to the NGOs working with
HRG. Primarily NACO and the SACS obtain their supplies through the DHFW. NGOs also
directly access social marketing agencies. NACO and SACS ensure hat there is adequate supply
of condoms in STD clinics, VCTC, and Ob/Gyn clinics. SM condoms are made available at
outlets situated near state highways and in areas where TI projects are underway. NGOs are
encouraged to use a mix of free and SM approaches.
3.5.4
Core Convergence Recommendations for Condom promotion
Create a mechanism to ensure that condom programming for NACP and DHFW is managed
within a single entity to provide leadership and direction. This integration will greatly facilitate
streamlining the condom promotion strategy between the FW and HIV/AIDS programmes.
Joint development of a strategy on condom procurement and distribution to meet the needs of
sexually active women and men as a contraceptive method, as a method of dual protection and to
meet the needs of high-risk groups.
Condom supplies for NGO s involved in TI to be through NACO and SACS.
HFW to promote condoms as dual protection method through improved distribution channels.
Pilots to promote female condom use among general population as well sex workers both as a
contraceptive and barrier method.
3.6
Safety of blood and blood products
3.6.1
Background: In addition to ensuring blood safety, other strategies to reduce transmission
include: reducing the need for transfusions, educating and motivating low risk individuals to
donate blood.
DHFW strategy: Currently blood banks are located at state and at district levels. Stringent
guidelines for blood banks are in place. In the RCH II programme, DHFW has planned blood
storage centers at FRU level. However the procurement of blood will be primarily from the
blood banks certified by NACO, so quality control appears to be taken care of.
NACP Strategy: NACO has been involved in developing a blood safety policy and guidelines
for blood banks. Annexures 8 and 9 provide state wise details of blood banks supported and
strengthened by NACO respectively.
3.6.2
3.6.3
3.6.4
Core Convergence Recommendations fro Blood Safety
It is recommended that this policy be continued so that stringent quality controls are maintained at
the district levels, and high quality blood is available at secondary levels of care.
file ://C :\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr. .. 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and t...
Page 10 of 17
Training
3.7
DHFW strategies: In RCH 1, Medical Officers, Staff Nurses, Lady Health Visitors and ANMs
were trained for periods of between 4 to 6 hours (depending on job profiles) in the area of
HIV/AIDS and RTI/STI. In RCH II, four core committees are currently reviewing the content of
training for each level of provider.
3.7.2 NACP strategies: NACO, SACS (and partner agencies- NGOs) have developed modules for
training in a range of areas- prevention, universal precautions care and support, PPTC 1 tor all
providers. These have been implemented separately from the HFW trainings.
3.7.1
3.7J
Core Convergence Recommendations for training
NACP to designate an officer to coordinate with the groups responsible for ongoing module
development for RCLIII and ensure that HIV/AIDS training inputs cover all areas of concern
adequately.
• Joint finalization of areas of training with respect to content, duration, mix of knowledge and
skills, for all cadres of health and community workers.
• NACO and DHFW to jointly develop a specific plan to train staff of PPTCT and VCTC to
ensure that these functions include other HFW elements as well.
. Finalized modules to be shared with private sector and NGO partners supported by HFW and
NACP.
•
3.8
Management Information Systems
3.8.1
DHFW strategies: As part of the RCH II programme a Management Information System is
being designed. An Integrated Disease Surveillance Project is also underway. Both these
systems will essentially capture data on an ongoing basis at all levels for programme
implementation and ongoing monitoring. Small and large scale surveys such as the NFHS and
District level HH surveys are also conducted periodically.
NACP strategies: The nationwide sentinel surveillance system captures data on an annual basis
from about 455 sites across the country. In addition, VCTC, blood banks and PPTC serve as a
reporting base. Programme supported NGOs also report on STI treated, condoms distributed and
coverage of high-risk groups.
3.8.2
3.8.3
Core Convergence Recommendations for Management Information Systems.
• Joint working group to review data needs, assess ongoing sources, and finalize requirements to fit
into RCH II MIS, so that all facilities report service performance on RTI/STI, VCTC and PPTCT
as part of routine reporting, while maintaining confidentiality.
. State and national level surveys (NFHS III, DLHS) designed to provide information on KAP
related to RTI/STI/HIV/AIDS
• Research and prevalence studies to assess nature of STIs to develop suitable management
protocols and assess antibiotic resistance patterns. Need to explore linkages with integrated
disease surveillance programme.
• Mechanisms to ensure periodic reporting on STI/HIV/AIDS by private providers
• Include NGO reports as part of district level reporting.
3.9
Male involvement: The case to promote male participation in improving reproductive and
sexual health for women has been articulated in several documents and is being implemented
IO
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and t...
Page 11 of 17
through several community-based initiatives. However, the reach of programmes of the DHFW to men
is low. NACP on the other hand, (given that men are the predominant target group in the general
population) has significant experience in approaches to reach men, through condom promotion,
STI clinics, and mass media. In RCH II, it is proposed to provide gender sensitization training
for all providers. Specific BCC interventions will implemented to increase demand for male
contraceptive methods, male RH services, and to heighten awareness about men’s responsibility
in support of women’s sexual and reproductive health.
Core Convergence Recommendations to improve male involvement
• Ensure that NACP and DHFW training include male responsibility as a key area
• BCC strategies for both NACP and DHFW to address the area of male responsibility and shared
action for improved women’s RH as a major issue- includes partner notification, drug
compliance, safe sexual practices and condom promotion.
3.10
Strengthening urban health services to improve convergence: Urban health particularly among
the poor presents a special challenge to the DHFW. While overall health indicators in rural areas
may be better than in rural areas, they mask significant disparities. The reach of the poor to good
health care is limited, and they are often served by the private sector, poorly regulated and
offering care of questionable quality. Given the increase of slum populations, migrants, and
street children, and that these groups are identified as high risk groups for HIV/AIDS, it is
essential that their access to the services such as RTI/STI, VCTC, PPTCT. condom promotion
and BCC interventions be improved.
The NACP supports several targeted interventions in urban areas, primarily through NGOs, and
targeted at marginalized, high-risk groups, and not often general population based. NACP also
support STI clinics, VCTC and PPTCT in large medical colleges/teaching hospitals. However
primary and secondary health care facilities in urban areas are not as clearly structured or
organized as in rural areas. RCH II proposes a two-tier facility - an urban health center for a
population of 50,000- to address primary health care needs of the population, particularly the
vulnerable, and a second tier (mix of private and public sector) to serve as referral sites.
Core convergence Recommendations to improve reach of urban health
• Strengthening urban health infrastructure, including training of urban providers will have
benefits for urban RCH and NACP.
•
Involvement of urban private sector practitioners in training programmes, through
involvement of IMA and FOGSI. .
• Referral information on sites where RTI/STI, VCTC, and PPTCT are available to be
widely disseminated to both general and high risk populations through NGOs, private
sector, and IEC efforts.
• UHC and Referral sites to offer a range of RCH services without discrimination and in an
equitable manner to general populations and populations at risk.
4. OPERATIONALIZATION OF CONVERGENCE
4.1
Of the key areas identified for convergence, RTI/STI management for the general population
could be integrated within the DHFW. VCTCs and PPTC still need to be managed by
NACO and the SACS to retain focus and ensure referral linkages to care and support. In the
area of blood safety, it is recommended that NACO continue to ensure safe blood supplies at
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and t... Page 12 of 17
district levels, and that blood storage units at secondary levels of care procure supplies from the
district. In the areas of behaviour change and condom procurement/distribution, it is
recommended that the leadership for the programmes be entrusted to one entity to ensure
overall guidance of both areas for Health, Family Welfare and the National AIDS Control
Programme. Male involvement needs to be woven into all components. Strategies to
improve services in rural areas must be replicated/adapted for urban areas. Joint working
groups are recommended at national and state level to ensure that the training plans and
monitoring and reporting systems of the DHFW and NACO (and corresponding groups at the
state levels) are well coordinated, reflect shared concerns and are synchronized at the
delivery levels.
4.2
Recommended Institutional Mechanisms
4.2.1
At the National level a NACP-HFW convergence committee is to be set up at DHFW to
provide policy inputs and oversight to the convergence between NACP and DHFW. The
Convergence Committee will be chaired by Secy, HFW and co-chaired by Project Director
NACO.
4.2.2
At the National level, two joint working groups are visualized comprised of technical and
programme mangers from NACO and DHFW. They include:
1. Joint working group on convergence of RTI/STI, VCTC and PPTCT into DHFW
infrastructure and services. (NACO/DDG/MH)
2. Joint working Group on Training and MIS. (NACO/DC Training, and CD, Statistics)
Broadly the roles of the JWG are to review quarterly performance from each state and jointly
review and prepare a report on performance coverage and quality. Reporting formats would be
developed in conjunction with existing formats or those proposed for larger programmes so that
programme managers at state and district levels are not burdened. It is expected that the NACPHFW Convergence Committee, which meets every quarter, will obtain reports from each of the
National JWG, provide feedback and serve as a problem solving mechanism.
4.2.3
It is recommended that at the state level, a similar mechanism be set up, so that the state and
central level review and monitoring, and information needs and flow are co-ordinated.
4.2.4
At the district level, NACO is considering the appointment of a convergence facilitator who
could ensure coordinated inputs between those programmes directly implemented by
NACO/SACS, between various NGO managed programmes, and finally between those
interventions that depend upon the DHFW resources for effective operationalization. In
addition this individual would follow up on the training plan for the district as well as the
MIS to ensure that there is convergence. This individual would report to the SACS and to
the CMO at the district level. At the district level, the District Health Mission (where all
other programmes of HFW are integrated), will include a sub- group to review HIV/AIDS
and HFW convergence in the major service areas (RTI/STI, VCTC, PPTCT) and NGO
functioning.
5.NEXT STEPS
As pointed out initially, this paper is only a broad framework for actions on convergence. The
framework needs to be validated at state level to ensure that there is ownership of the issues between the
State AIDS Control Societies and the Departments of Health ad Family Welfare. While RCH II is the
focus of convergence since it is due to be launched fairly soon, and there has been significant
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and t... Page 13 of 17
decentralized planning and design, it is emphasized in this document. However there are several other
programmes and partners that also need to be viewed through the lens of convergence to ensure
appropriate and effective local responses to HIV/AIDS.
Role and
DHFW
Functions
of Role and
NACP
Functions
of Convergence
mechanisms/aspects
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
13
Areas of convergence between the National AIDS Control Organization (NACO) and t...
Page 14 of 17
14
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and t...
Area
of
Convergence
-Primary
Responsibility- -Support to HRG-NGOs to
RTI/STI
integrate RTI/STI management continue, Service delivery
at all levels in public sector whether directly through
NGOs or referral to public or
system
-Increase
private
sector private sector.
involvement in high quality -Ensure that all STI service
RT/STI treatment- IMA and data and special studies are
provided to JCWG to enable
FOGSI
-Broadly RCH II strategies reporting at the Convergence
should be followed-At PHC committee level.
level, first line drugs to be
offered,
-District, CHC and FRU to
comprehensive
offer
etiological and lab based
treatment. At district level,
linkages with STD referral labs
to be strengthened.__________
-Infrastructure (space) to be Primary responsibility—
VCTC
increase VCTC sitesprovided in facilities where
expansion in phased manner
VCTC are located.
-Support to ensure referral -NACP support for staff and
supplies,
from other departments
Youth
Friendly
-Overall supervision by head -Include
of facility, in collaboration Information Centers at CHC
with Ob/Gyn, STD, Paed, and and PHC
other
-VCTC to serve
other depts.
-Frontline
providers
to counseling needs.
motivate community at risk for -Cadre/of counselors to staff
the sites.
VCTC
PPTCT
BCC
Page 15 of 17
-At National level,
NACP and DHFW to
set up a JCWG group
to monitor access of
RTI/STI services for
general population and
for HRG. Report to
HIV/AIDS
Convergence
Committee.
-Training of providers
(public, private and
NGO) and lab techs
within purview of
DHFW.
-DDG-MH/NACO
-JCWG
to review
functioning of VCTC
through periodic state
reports.
Report to
HIV/AIDS
Convergence
Committee
-Training of providers
of DHFW at all levels
to include elements of
risk
protection,
motivation for testingthrough DHFW
-NGO
training
facilitated by NACP,
but modules jointly
developed.
NACO/DDG-MH
-Overall supervision by head Primary Responsibility to -JCWG to obtain data
on
functioning
of
ensure functioning PPTCT
of facility
-Located
in
Ob/Gyn -Expand PPTCT sites in a PPTCT and review
performance
department, managed by HOD phased manner
for
all
-Ensure non discriminatory -NACP to support once -Training
counselor and lab. Tech. And providers to• include
practices
attitudinal as well
supplies for PPTCT.
-Ensure universal precautions
technical skills, and
-At the community level,
universal precautions.ANM/ASHA follow up of
DHFW
VCTC clients testing positive
-Private sector through
for ANC, and motivate for
IMA and FOGSIPPTCT
DHFW
NACO/DDG-MH
-All messages for HFW to -Messages for HIV/AIDS -BCC strategy/division
include HIV/AIDS prevention highlight appropriate service for NACP and DHFW
single
and care and support as provision through public and under
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
I
Areas of convergence between the National AIDS Control Organization (NACO) and t...
Condom
Promotion
Training
Reporting
Blood Safety
appropriate
-Ensure that NGO programmes
also use message content as
defined___________________
-Enhance condom use for dual
protection
-Female condoms to be
a
promoted
as
contraceptive/barrier method
Primary Responsibility for
training
of all
service
interventions
(except
VCTC/PPTCT) to be within
DHFW
-Support training content and
technical support for VCTC
and PPTCT training
private health system
-Ensure that NGOs highlight
service access in addition to
prevention messages._______
-Condom promotion key to
prevention
-Female condoms to be
a
promoted
as
contraceptive/barrier method
-Support training in terms of
content and technical support
-Primary responsibility for
training VCTC counselors in
a range of issues including
HIV/AIDS, which include
safe
motherhood,
family
planning
and
childcare.
PPTCT staff training also to
be
conducted
by
NACO/SACS.
Page 16 of 17
management.
Condom procurement
and distribution for
FW and NACO under
single entity.
-NACP to coordinate
with groups working
on RCH II modules to
ensure
HIV/AIDS
content for all workers.
-Joint Working Group
to be instituted to
review and ensure that
HIV/AIDS messages
and content for training
are tailored to each
level of provider
-Ensure that training
modules are shared
with NGO partners of
DHFW and NACP.
-Develop protocols and
guidelines for key
services-Ensure dissemination
of
protocols
and
guidelines to NGOs
and private sector.
DHFW MIS to capture service -Ensure that VCTC, PPTCT, -NACP to coordinate
data- RTI/STI, VCTC, and and sentinel surveillance data with RCH II MIS
convener
(CD,
is reflected in district MIS.
PPTCT
Statistics to ensure that
-MIS to include HIV/AIDS
HIV/AIDS indicators
indicators
are
included in MIS for
-Support sentinel surveillance
RCH
II.
data collection
-Joint Working Group
to review RCH II MIS
and
ensure
that
reporting of RTI/STI,
VCTC, and PPTC is
also included.
-Surveys (NFHS III
and DLHS )to include
information
on
HIV/AIDS as well.
Maintain quality of blood -Primary Responsibility to
taken from blood banks to assure safety of blood at
blood storage centers at banks at district level and
above
secondary levels of facilities.
IG
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr ... 9/3/2007
Areas of convergence between the National AIDS Control Organization (NACO) and t... Page 17 of 17
NACO and the DFW jointly constituted a six member Task Force in late December, 2004 to identify areas of
convergence and develop an operational plan by January 31, 2005.
file://C:\Documents%20and%20Settings\Administrator\Desktop\NRHM%20-%20for%20pr... 9/3/2007
1^-
DRAFT REPORT ON RECOMMENDATION OF TASK FORCE ON PUBLIC PRIVATE
PARTNERSHIP FOR THE 11™ PLAN
The Planning Commission constituted a Working Group on Public Private Partnership to
improve health care delivery for the Eleventh Five-Year Plan
(2007-2012) under the
Chairmanship of Secretary, Department of Health & Family Welfare, Government of India with the
following members:
1.
Secretary, Department of Health & Family Welfare, New Delhi
Chairman
2.
Secretary (Health), Government of West Bengal
Member
3.
Secretary (Health), Government of Bihar
Member
4.
Secretary (Health), Government of Jharkhand
Member
5.
Secretary (Health), Government of Karnataka
Member
6.
Secretary (Health), Government of Gujarat
Member
7.
Director General Health Services, Directorate General of Health Services,
Member
New Delhi
8.
President, Indian Medical Association, New Delhi
Member
9.
Medical Commissioner, employees State Insurance Corporation, New
Member
Delhi
10.
Dr. H. Sudarshan, President /Chairman, Task Force on Health & Family
Member
Welfare, Government of Karnataka, Bangalore
11.
Dr. Sharad Iyengar, Action Research & Training in Health, Udaipur,
Member
Rajasthan
12.
Executive Director, Population Foundation of India, New Delhi
13.
Dr. S.D. Gupta, Director, Indian Institute of Health Management Research,
Member
Member
Jaipur
14.
Ms. Vidya Das, Agragamee, Kashipur, District Rayagada, Orissa
Member
1
Dr. C.S. Pandav, Centre for Community Medicine, All India Institute of
15.
Member
Medical Sciences, New Delhi
Dr. V.K. Tiwari, Acting Head, Department of Planning & Evaluation,
16.
Member
National Institute of Health & Family Welfare, New Delhi.
17.
Dr. A Venkat Raman, Faculty of Management Sciences, University of
Member
Delhi
18.
19.
20.
21.
Dr. K.B. Singh, Technical Adviser, European Commission, New Delhi
Member
Shri K.M. Gupta, Director, Ministry of Finance, New Delhi
Member
Shri Rajeev Lochan, Director (Health), Planning Commission, New Delhi
Member
Joint Secretary, Ministry of Health & Family Welfare, New Delhi
Member
Secretary
The Terms of reference of the Working Group were as under:
To review existing scenario of Public Private Partnership in health care (Public,
C)
Private, NGO) in urban and rural areas with a view to provide universal access to equitable,
affordable and quality health care which is accountable at the same time responsive to the needs
of the people, reduction of child and maternal deaths as well as population stablization and also
achieve goals set under the National Health Policy and the Millennium Development Goals.
(ii)
To identify the potential areas in the health care delivery system where an
effective, viable, outcome oriented public private partnership is possible.
(iii)
To suggest a practical and cost effective system of public private partnership to
improve health care delivery system so as to achieve the goals set in National Rural Health
Mission, National Health Policy and the Millennium Development Goals and makes quantitative
and qualitative difference in implementation of major health & family welfare programmes,
functioning of health & family welfare infrastructure and manpower in rural and urban areas.
(iv)
To deliberate and give recommendations on any other matter relevant to the topic.
2
DEFINING PUBLIC PRIVATE PARTNERSHIP IN HEALTH
Public-Private Partnership or PPP in the context of the health sector is an instrument for
improving the health of the population. PPP is to be seen in the context of viewing the whole
medical sector as a national asset with health promotion as goal of all health providers, private or
public. The Private and Non-profit sectors are also very much accountable to overall health
systems and services of the country. Therefore, synergies where all the stakeholders feel they
are part of the system and do everything possible to strengthen national policies and programmes
needs to be emphasized with a proactive role from the Government.
However for definitional purpose, “Public” would define Government or organizations
functioning under State budgets, “Private” would be the Profit/Non-profit/Voluntary sector and
“Partnership” would mean a collaborative effort and reciprocal relationship between two parties
with clear terms and conditions to achieve mutually understood and agreed upon objectives
following certain mechanisms.
PPP however would not mean privatization of the health sector. Partnership is not meant
to be a substitution for lesser provisioning of government resources nor an abdication of
Government responsibility but as a tool for augmenting the public health system.
THE ROLE OF THE PRIVATE SECTOR IN HEALTH CARE
Utilisation of Hospital Services
I
I
•I
I
i
8,000
7,000
6,000
5,000
■ Private
4,000
3,000
2,000
1,000
Source Pearson M, Impact and Expenditure Review, Part II Policy issues. DFID, 2002
Over the years the private health sector in India has grown markedly. Today the private
sector provides 58% of the hospitals, 29% of the beds in the hospitals and 81% of the doctors.
(The Report of the Task Force on Medical Education, MoHFW)
The private providers in treatment of illness are 78% in the rural areas and 81% in the
urban areas. The use of public health care is lowest in the states of Bihar and Uttar Pradesh. The
reliance on the private sector is highest in Bihar. 77% of OPD cases in rural areas and 80% in
urban areas are being serviced by the private sector in the country. (60th round of the National
Sample Survey Organisation (NSSO) Report.
3
"v
*
■ I
10i82
i(
X0'
.0^
)*
i
The success of health care in Tamil Nadu and Kerala is not only on account of the Public
Health System. The private sector has also provided useful contribution in improving health ca
provision.
Studies of the operations of successful field NGOs have shown that they have Produced
dramatic results through primary sector health care services at costs ranging from Rs. 21 to Rs.
91 per capita per year Though such pilot projects are not directly upscalable they demonstrate
promising possibilities of meeting the health needs of the citizens by focused thrust on primary
healthcare services. (NSSO 60th Round)
India: Percentage of Hospitalizations In The Public and Private
Sector Among Those Below The Poverty Line, According To State
100%
0)
□)
(U
4-»
c
0)
o
u.
CD
Q.
;J
__
80%
—,
60%
..
40%
20%
0%
/
/
// /
/
/
/
/
/
/
States
Public Facilities
Private Facilities i
Source Pearson M, Impact and Expenditure Review, Part II Policy issues. DFID,2002
While data and information is still being collated, the private health sector seems to be the
most unregulated sector in India. The quantum of health services the private sector provides is
large but is of poor and uneven quality. Services, particularly in the private sector have shown a
trend towards high cost, high tech procedures and regimens. Another relevant aspect borne out
by several field studies is that private health services are significantly more expensive than public
health services - in a series of studies, outpatient services have been found to be 20-54 /o higher
and inpatient services 107-740% higher. (Report of the Task Force on Medical Education,
MoHFW.
Widely perceived to be inequitable, expensive, over indulgent in clinical procedures, and
without standards of quality, the private sector is also seen to be easily accessible, better
managed and more efficient than its public counterpart.
4
Given the overwhelming presence of private sector in health, there is a need to regulate and
involve the private sector in an appropriate public-private mix for providing comprehensive and
universal primary health care to all. However there is an overwhelming need for action on
privatization of health services, so that the health care does not become a commodity for buying
and selling in the market but remains a public good, which is so very important for India where
1/3 of the population can hardly access amenities of life, leave alone health care.
In view of the non-availability of quality care at a reasonable cost from the private sector,
the upscaling of non-profit sector in health care both Primary, Secondary and Tertiary care,
particularly with the growing problems of chronic diseases and diseases like HIV/AIDS, needs
long term care and support.
OBJECTIVES OF PUBLIC PRIVATE PARTNERSHIPS
Universal coverage and equity for primary health care should be the main objective of any
PPP mechanism besides:
> Improving quality, accessibility, availability, acceptability and efficiency
> Exchange of skills and expertise between the public and private sector
> Mobilization of additional resources.
> Improve the efficiency in allocation of resources and additional resource generation
> Strengthening the existing health system by improving the management of health within
the government infrastructure
> Widening the range of services and number of services providers.
> Clearly defined sharing of risks
> Community ownership
REVIEW OF EXISTING SCENARIO OF PPP
POLICY PRESCRIPTION
Public-Private Partnership has emerged as one of the options to influence the growth of
private sector with public goals in mind. Under the Tenth Five Year Plan (2002-2007), initiatives
have been taken to define the role of the government, private and voluntary organizations in
meeting the growing needs for health care services including RCH and other national health
programmes. The Mid Term Appraisal of the Tenth Five Year Plan also advocates for
partnerships subject to suitability at the primary, secondary and tertiary levels. National Health
Policy-2002 also envisaged the participation of the private sector in primary, secondary and
tertiary care and recommended suitable legislation for regulating minimum infrastructure and
quality standards in clinical establishments/medical institutions. The policy also wanted the
participation of the non-governmental sector in the national disease control programmes so as to
ensure that standard treatment protocols are followed. The Ministry of Health and Family Welfare,
Government of India, has also evolved guidelines for public-private partnership in different
National Health Programmes like RNTCP, NBCP, NLEP, RCH, etc. However, States have varied
experiences of implementation and success of these initiatives. Under the Reproductive and
Child Health Programme Phase II (2005-2009), several initiatives have been proposed to
strengthen social-franchising initiatives. National Rural Health Mission (NRHM 2005-2012)
recently launched by the Hon’ble Prime Minister of India also proposes to support the
development and effective implementation of regulating mechanism for the private health sector
to ensure equity, transparency and accountability in achieving the public health goals. In order to
tap the resources available in the private sector and to conceptualize the strategies, Government
of India has constituted a Technical Advisory Group for this purpose, consisting of officials of
GOI, development partners and other stakeholders. The Task Group is in the process of finalizing
its recommendation.
5
REVIEW OF PPP IN THE HEALTH SECTOR
, the Centre as well as the State Governments have initiated a wide
During the last few years, J.-------- 1--------------' ’) arrangements
variety of public-private partnership
arrangements to
to meet
meet the
the growing
growing health
health care needs of the
populatronT^der fivebasic mechanisms in the health sector:
Contracting in-government hires individual on a temporary basis to provide services
Contracting out- government pays outside individual to mange a specific function
>
Subsidies-government gives funds to private groups to provide specific services
>
Leasing or rentals-government offers the use of its facilities to a private organization
>
Privatization-government gives or sells a public health facility to a private group
>
An attempt has been made here to encapsulate some of the on-going initiatives in public
private partnerships in selected states.
A. Partnership between the Government and the for profit sector
1. Contracting in Sawai Man Singh Hospital, Jaipur
• The SMS hospital has established a Life Line Fluid Drug Store to contract out low cost
high quality medicine and surgical items on a 24-hour basis ms'de the hosprtai.
a9ency
to operate the drug store is selected through bidding. The successful bidder is a propne y
agency, and the medical superintendent is the overall supervisor in charge of monitoring he
store and it's functioning. The contractor appoints and manages the re™neratl°" °f ‘he st^
from the sales receipts. The SMS hospital shares resources with the drug store such as
electricity water- computers for daily operations; physical space; stationery and medicines.
The contractor provides all staff salaries; daily operations and distribution of medicine,
maintenance of records and monthly reports to SMS Hospital. The SMS Hospital provides a
medicines to the drug store, and the contractor has no power to purchase or sell medicines
himself. The contractor gains substantial profits, could expand his contact and gam
popularity through ULFS. However, the contractor has to abide by all the rules and
regulations as given in the contract document.
. The SMS Hospital has also contracted out the installation, operation and maintenance of
CT-scan and MRI services to a private agency. The agency is paid a month y rent by
hospital and the agency has to render free services to 20% of the patients belonging to the
poor socio-economic categories
2. The Uttaranchal Mobile Hospital and Research Center (UMHRG) ia
among the Technology Information, Forecasting and Assessment Council (TIFAC), the
Government of Uttaranchal and the Birla Institute of Scientific Research (BISR). The motive
behind the partnership was to provide health care and diagnostic facilities to poor and rural
people at their doorstep in the difficult hilly terrains. TIFAC and the State Govt, shares the funds
sanctioned to BISR on an equal basis.
3 Contracting out of IEC services to the private sector by the State Malaria Control Society in
GufaralHs underway in order to control malaria in the state. The IEC budget from various
pharmaceutical companies is pooled together on a common basis and the agencies hired by-the
private sector are allocated the money for development of IEC material through a special
sanction.
Himachal Pradesh; Karnataka; Orissa (cleaning work of Capital Hospital by Sulabh International),
Punjab; Tripura (contracting Sulabh International for upkeep, cleaning and maintenance of the
G.B. Hospital and the surrounding area); Uttaranchal, etc.
5. The Government of Andhra Pradesh has initiated the Arogya Raksha Scheme in collaboration
with the New India Assurance Company and with private clinics. It is an insurance scheme fully
6
funded by the government. It provides hospitalization benefits and personal accident benefits to
citizens below the poverty line who undergo sterilization for family planning from government
health institutions. The government paid an insurance premium of Rs. 75 per family to the
insurance company, with the expected enrollment of 200,000 acceptors in the first year.
The medical officer in the clinics issues a Arogya Raksha Certificate to the person who
undergoes sterilization. The person and two of her/his children below the age of five years are
covered under the hospitalization benefit and personal accident benefit schemes. The person
and/oor her/his children could get in-patient treatment in the hospital upto a maximum of Rs. 2000
per hospitalization, and subject to a limit of Rs. 4000 for all treatments taken under one Arogya
Raksha Certificate in any one year. She/he gets free treatment from the hospital, which in turn
claims the charges from the New India Insurance Company. In case of death due to any accident,
the maximum benefit payable under one certificate is Rs. 10,000.
B. Partnership between the Government and the non-profit sector
1. Involvement of NGOs in the Family Welfare Programme
•
The MNGO (Mother NGO) and SNGO (Service NGO) Schemes are being implemented
by NGOs for population stabilization and RCH. 102 MNGOs in 439 districts, 800 FNGOs,
4 regional Resource Centers (RRC) and 1 Apex Resource Cell (ARC) are already in
place. The MNGOs involve smaller NGOs called FNGOs (Field NGOs) in the allocated
districts.
The functions of the MNGO include identification and selection of FNGOs; their capacity
building; development of baseline data for CAN; provision of technical support; liaison,
networking and coordination with State and District health services, PRIs and other
NGOs; monitoring the performance and progress of FNGOs and documentation of best
practices. The FNGOs are involved in conducting Community Needs Assessment; RCH
service delivery and orientation of RCH to PRI members; advocacy and awareness
generation.
The SNGOs provide an integrated package of clinical and non-clinical services directly to
the community
•
The Govt, of Gujarat has provided grants to SEWA-Rural in Gujarat for managing one
PHC and three CHCs. The NGO provides rural health, medical services and manages
the public health institutions in the same pattern as the Government. SEWA can accept
employees from the District Panchayat on deputation. It can also employ its own
personnel by following the recruitment resolution of either the Government or the District
Panchayat. However, the District Health Officer or the District Development Officer is a
member of the selection committee and the appointment is given in her/his presence. In
case SEWA does not wish to continue its services, the District Panchayat, Bharuch would
take over the management of the same.
2. The Municipal Corporation of Delhi and the Arpana Trust (a charitable organization registered
in India and in the United Kingdom have developed a partnership to provide comprehensive
health services to the urban poor in Delhi’s Molarbund resettlement colony. Arpana Trust runs a
health center primarily for women and children, in Molarbund through its health center ‘Arpana
Swasthya Kendra’. As contractual partners, Arpana Trust and MCD each has fixed
responsibilities and provides a share of resources as agreed in the partnership contract. The
Arpana Trust is responsible for organizing and implementing services in the project area, while
the MCD is responsible for monitoring the project. The MCD provides building, furniture,
medicines and equipment, while the Arpana Trust provides maintenance of the building, water
and electricity charges, management of staff and medicine.
7
MfISSiW
PHC There has been redeployment of the Govt, staff in the PHCs, however some do remain in
deputation on mutual consent. The agency ensures adequate stocks of essential drugs at all
times and supplies them free of cost to the patients. No patient is charged for diagnosis, drugs,
treatment or anything else except in accordance with the Government policy. The staff salaries
are shared between the Govt, and the Trust.
Gumballi district is considered a model PHC covering the entire gamut of primary health care preventive, promotive, curative and rehabilitative
Similarly in Orissa, PPPs are being implemented for safe abortion services and social marketing
of disposable delivery kits. Parivar Sewa Sanstha and Population Services International are
implementing the Sector Investment Plan in the state.
4 The Government of Tamil Nadu has initiated an Emergency Ambulance Services scheme in
Theni district of Tamil Nadu in order to reduce the maternal mortality rate in its rural area. The
major cause for the high MMR is anon-medical cause - the lack of adequate transport facilities to
carry pregnant women to health institutions for childbirth, especially in the tn ba areas. This
scheme is part of the World Bank aided health system development project in Tamil Nadu. Seva
Nilayam has been selected as the potential non-governmental partner in the scheme^ This
scheme is self-supporting through the collection of user charges. The Government supports the
scheme only by supplying the vehicles. Seva Nilayam recruits the drivers, tram the staff, maintain
the vehicles, operate the program and report to the government It bears the entire operating cost
of the project including communications, equipment and medicine, and publicizing the service in
the villages, particularly the telephone number of the ambulance service. However, the project is
not self-sustaining as the revenue collection is lesser than anticipated.
Seva Nilayam also operates another program in the Theni district called the Emergency Accident
Relief Center for which the government has also provided a vehicle.
5. The Urban Slum Health Care Project the Andhra Pradesh Ministry of Health and Family
Welfare contracts NGOs to manage health centers in the slums of Adilabad. The basic objectives
of the project are to increase the availability and utilization of health and family welfare services,
to build an effective referral system, to implement national health programs, and to increase
health awareness and better health-seeking behaviour among slum dwellers, thus reducing
morbidity and mortality among women and children. To serve 3 million People, the project has
established 192 Urban Health Centers. Five ‘Mahila Aarogya Sanghams’ (Womens Wee-Being
Associations) were formed under each UHC, and along with the self-help groups and ICDS
workers mobilize the community and adopt Behaviour Change Communication strategies.
The NGOs are contracted to manage and maintain the UHCs, and based on their performance,
they are awarded with a UHC, or eliminated from the program. Additional District Magistrates and
Health Officers supervise the UHCs at district level and the Medical Officer is the nodal officer at
the municipality level. The District Committee approves all appointments made by the NGOs for
the UHC staff. The Govt, of Andhra Pradesh constructs buildings for the UHCs; provide honoraria
to the Project Coordinators of the UHCs, medical officers and other staff; train staff members; and
supply drugs, equipment and medical registers.
6 In recent examples, collaboration that has developed between Government of Arunachal
Pradesh, VHAI and Karuna Trust in managing significant number of PHCs may be seen at
Annexure IV.
8
2-G
r
C. Partnership between the Government and a private service provider
Several examples for the above partnership could be quoted from the Indian experience:
1. Partnership between the Department of Family Welfare and Private Service Providers:
•
•
•
•
•
•
•
•
•
2.
The DoFW has appointed one additional ANM on contractual basis in the remote sub
centers (which constitute 30% of all sub centers in C category districts in 8 states) to
ensure better emergency obstetric care under the RCH programme. Similarly 140 ANMs
could be appointed in Delhi for extending their services in the slum areas. The scheme
has been extended to the North Eastern states with effect from 1999-2000
Public Health/Staff nurses have been appointed on a contractual basis at PHCs/ CHCs
having adequate infrastructure for conducting deliveries.
In order to plug deficiencies in providing emergency obstetric care at FRU due to non
availability of anesthetist for surgical interventions, states have been permitted to engage
the anesthetist from the private sector on a payment of Rs. 1000 per case at the sub
district and CHC level.
With a view to supplement the regular arrangement, provision has been made for
engaging doctors trained in MTP as Safe Motherhood Consultant who will visit the PHC
(including CHCs in NE states) once a week or at least once in a fortnight on a fixed day
for performing MTP and other Maternal Health care services. These doctors will be paid
@Rs.5OO per day visit.
A scheme for reservation of sterilization beds in hospitals run by government, local
bodies and voluntary organizations was introduced in 1964 with view to provide
immediate facilities for tubectomy operations in hospitals. At present too, beds are
sanctioned to hospitals run by local bodies and voluntary organizations and grant-in-aid is
provided as per approved pattern of assistance.
The Haryana Urban RCH Model is being implemented in 19 urban slums and benefits 15
lakh beneficiaries. In this model, a private health practitioner (PHP) has been identified to
provide comprehensive primary health care service to a group of 1000-1500 targeted
beneficiaries. S/he provides services related to National Disease Control Programme,
contraception, immunization, ambulatory care. The PHP gets an incentive of Rs. 100 p.a.
per beneficiary by the Government. The model is envisioned to be self-sustaining by the
5th year.
A proposal has been submitted by PSS, Rajasthan to the GOI for establishing a
comprehensive RCH clinic in 3 districts, wherein PSS would provide services like
sterilization, MTP, spacing, ante/post natal care, immunization, RTI/STI. The cost to be
borne by the Govt, is Rs. 18 to 20 lakhs p.a. per clinic. With a view to ensure project
sustainability, the user fees is sought to be deposited in a bank account.
The Samaydan Scheme in Gujarat aims to ease the problem of vacancies of specialists
in health and medical services. About 125 honorary and part-time specialists have been
appointed in rural hospitals under the scheme and the removal of age-eligibility criteria for
appointment of doctors in government services is also being considered.
Under the Urban Health Care Project, the community base health volunteers in the urban
areas would roped in to provide primary health care in the urban slums of Gujarat. Their
activities would be monitored by CHC/PHC/PPU/Urban Family Welfare Center/Trust
Hospital and they would be paid a fixed monthly honorarium.
The Department of AYUSH envisages accreditation of organizations with the MoHFW for
research and development in order to be eligible for financial assistance under the
scheme of Extra Mural Research on ISM&H. The eligible organizations include R&D
organizations recognized by the Ministry of Science and Technology, Govt, of India; one
Government or semi-Government or autonomous R&D Institution under the Gol/State
Government/Union Territory; and one private R&D institutions registered under any
State/Central Act as Research Organization.
9
D. Partnership between the Government and a private sector and/or the non-profit sector
and/or a private service provider and/or multilateral agencies
1. The National Malaria Control Programme has involved the NGOs and private practitioners at
the district level for the distribution of medicated mosquito nets. (LOGISTICS)
2. Under the National Blindness Control Programme, District Blindness Control Societies have
been formulated, which are represented by the Government, non-government and private
sectors. The NGOs have been involved for providing a package of services
3. The National AIDS Control Programme has involved both the voluntary and private sector for
outreaching the target population through Targeted Interventions (WIDER COVERAGE)
4. The Revised National Tuberculosis Control Programme has involved the private practitioners
and the NGOs for the rapid expansion of the DOTS strategy. The non-inclusion of the private
providers had been one of the main reasons for the failure of the earlier programme. The private
medical practitioners serve as the first point of contact for more than two-thirds of TB
symptomatics.
The GOI has initiated a Public Private Mix (PPM) pilot project with technical assistance from
WHO in 14 sites across the country viz. Ahmedabad, Bangalore, Bhopal, Chandigarh, Chennai,
Delhi, Jaipur, Kolkata, Lucknow, Patna, Pune, Bhubaneshwar, Ranchi and Thiruvananthapuram.
The areas of collaboration with the NGOs include: community outreach; health education and
promotion; provision of DOTS and in-hospital care for TB disease; TB Unit Model; programme
planning, implementation, training and evaluation.
Presently, there are 550 NGOs and 200 Private Practitioners involved in RNTCP. Attempts are
also underway to involve the medical colleges in the programme.
5. The Rajiv Gandhi Super-specialty Hospital in Raichur Karnataka is a joint venture of the
Government of Karnataka and the Apollo hospitals Group, with financial support from OPEC
(Organization of Petroleum Exporting Countries). The basic reason for establishing the
partnership was to give super-specialty health care at low cost to the people Below Poverty Line.
The Govt, of Karnataka has provided the land, hospital building and staff quarters as well as
roads, power, water and infrastructure. Apollo provided fully qualified, experienced and
competent medical facilities for operating the hospital. The losses anticipated during the first three
years of operation were reimbursed by the Govt, to the Apollo hospital. From the fourth year, the
hospital could get a 30% of the net profit generated. When no net profit occurred, the Govt paid a
service charge (of no more than 3% of gross billing) to the Apollo Hospital.
Apollo is responsible for all medical, legal and statutory requirements. It pays all charges (water,
telephone, electricity, power, sewage, sanitation) to the concerned authorities and is liable for
penal recovery charges in case of default in payment within the prescribed periods. Apollo is also
responsible for maintenance of the hospital premises and buildings, and maintains a separate
account for funds generated by the hospital from fees for registration, tests and medical charges.
This account is audited by a Chartered Accountant engaged by Apollo with approval of the
Governing Council. Likewise, Apollo maintains separate monthly accounts for all materials used
by patients below the poverty line (including diagnostic services), which are submitted to the
Deputy Commissioner of Raichur for reimbursement. Accountability and responsibility for
outsourcing the support services remain with the Apollo.
The controlling authority of the Govt, of Karnataka is vested in its District Commissioner. A
Governing Council is established to review the performance of the hospital periodically (twice a
year), make recommendations to improve the administration and management and also resolve
any disputes that might arise. The ten-member council is chaired by the Karnataka Health
10
1
Minister and includes the Raichur District Collector, the Apollo CEO, the Principal Secretary, the
Health Secretary, the Finance Manager, the Hospital Operations Manager, Medical Directors and
local Members of the Legislative Assembly (as special invitees).
6. The Karuna Trust in collaboration with the National Health Insurance Company and the
Government of Karnataka has launched a community health insurance scheme in 2001. It covers
the Yelundur and Narasipuram Taluks. Underwritten by the UNDP, the Karuna Trust undertook
the project to improve access to and utilization of health services, to prevent impoverishment of
the rural poor due to hospitalization and health related issues, and to establish insurance
coverage for out-patient care by the people themselves. The scheme is fully subsidized for
Scheduled Castes and Scheduled Tribes who are below the poverty line and partially subsidized
for non-SC/ST BPL. Poor patients are identified by field workers and health workers who visit
door-to-door to make people aware of the scheme. ANMs and health workers visiting a village
collect its insurance premiums and deposit them in the bank.
The annual premium is Rs. 22, less than Rs.2 a month. If admitted to any government hospital for
treatment, an insured member gets Rs. 100 per day during hospitalization - Rs. 50 for bed
charges and medicine and Rs. 50 as compensation for loss of wages - up to a maximum of
Rs.2500 within a 25-day limit. Extra payment is possible for surgery. The insurance is valid for
one year. If members want to continue the coverage, they must renew their membership and pay
the full premium.
7. The Government of Karnataka, the Narayana Hrudalaya hospital in Bangalore and the Indian
Space Research Organization initiated an experimental tele-medicine project called ‘Karnataka
Integrated Tele-medicine and Tele-health Project’ (KITTH), which is an on-line health-care
initiatives in Karnataka. With connections by satellite, this project functions in the Coronary Care
Units of selected district hospitals that are linked with Narayana Hrudalaya hospital. Each CCU is
connected to the main hospital to facilitate investigation by specialists after ordinary doctors have
examined patients. If a patient requires an operation, s/he is referred to the main hospital in
Bangalore; otherwise s/e is admitted to a CCU for consultation and treatment.
Tele-medicine provides access to areas that are underserved or un-served. It improves access to
specialty care and reduces both time and cost for rural and semi-urban patients. Tele-medicine
improves the quality of health care through timely diagnosis and treatment of patients. The most
important aspect of tele-medicine is the digital convergence of medical records, charts, x-rays,
histopathology slides and medical procedures (including laboratory tests) conducted on patients.
8. The Yeshasvini Co-operative Farmer’s Healthcare Scheme is a health insurance scheme
targeted to benefit the poor. It was initiated by Narayana Hrudayalaya, super-specialty heart
hospital in Bangalore, and by the Department of Co-operatives of the Government of Karnataka.
The Government provides a quarter (Rs. 2.50) of the monthly premium paid by the members of
the Cooperative Societies, which is Rs. 10 per month. The incentive of getting treatment in a
private hospital with the Government paying half of the premium attracts more members to the
scheme. The cardholders could access free treatment in 160 hospitals located in all districts of
the state for any medical procedure costing upto Rs. 2 lakhs.
The premium is deposited in the account of a charitable trust, the regulatory body for
implementing the scheme. A Third Party Administrator - Family Health Plan Limited that is
licensed by Karnataka’s Insurance Regulatory and Development Authority. The FHPL has the
responsibility for administering and managing the scheme on a day-to-day basis. Recognized
hospitals have been admitted to the network throughout Karnataka, which are called as network
hospitals (NWH). These hospitals offer comprehensive packages for operations that are paid by
Yeshasvini. A Yeshasvini Farmers Health Care Trust is formed to ensure sustainability to the
scheme, which comprises of members of the State Government and the network hospitals. The
Trust monitors and controls the whole scheme, formulates policies, appointed the TPA and
addresses the grievances of the insured members or doctors.
11
2-^1
Only the members of an agricultural cooperative society could j°in this scheme and also all
members of a given cooperative society must become members of Yeashsvmi. This ensures
increase in the enrollment rates. The Government, apart from the premium subsidy has provided
key access to the cooperatives. The Department of Cooperatives has provided an administrative
vehicle to popularize the scheme.
The major drawback of this scheme is that the poor farmers are not covered for all health related
issues but only for out-patient care and all expenses connected with surgery.
9 A Rogi Kalyan Samiti (RKS) was formed in Bhopal’s Jai Prakash Goyernement Hospital to
manage9and maintain it with public cooperation. The RKS or Patient Welfare Committee or
Hospital Management Society is a registered society and the committee acts as trustees for the
hospitals responsible for proper functioning and management of the hospital ItsL^emb6rs are
from local PRIs, NGOs, local elected representatives and government officials. Part cipatio
the local staff with representatives of the loci population has been made essen al to ensure
accountably It functions as an NGO and not a government agency. It may ut.hze all government
assets and services to impose user charges. It may also raise funds additionally through
donations, loans from financial institutions, grants from government as well as o herdonor
agencies The funds received are not deposited in the State exchequer, but are available to be
spent by the Executive Committee constituted by the RKS/HMS. Private’ organ^attons could be
contracted out for provision of the super specialty care at a rate fixed by the RKS/HMS.
At JP Hospital RKS was formed due to lack of resources and other functional problems, which
acted as an impediment to timely, and quality health service delivery. Due to delay or n
disbursement of funds, creation of a hospital management society capable of generating
revenues became imperative. After the formation of RKS, the quality of services increased
terms of 24-hour availability of doctors and medicine, diagnostic facilities, better infrastructure
cXliness maintenance and timeliness of services. Through RKS, the hospital has also been
able to provide free services to patients below the poverty line.
10 A public/private DOTS model was established on a pilot basis in Hyderabad at Mahavir Trust
Hospital, which is a private non-profit hospital. This partnership also invol^®s
®® b|i
providers like doctors and nursing homes. This new approach is known as PPM DOTS (Publ c
Private Mix DOTS). As there are virtually no government services in the area, the pnyate■sectons
a full substitute for the public sector. Individual private practitioners were involved n the DOTS
programme as they form the first point of contact for most of the TB Patients both for quality
health care as well as convenience to refer to the private practitioners rather than the hospitals at
frequent intervals.
The Mahavir Trust Hospital acts as a coordinator and intermediary between thei government and
private medical practitioners (PMPs). It also acts as a supervisor. The PMPs refer_patien s
suspected of having TB to the hospital or to any of the 30 specified neighborhood DOTS centers
operated by PMPs. The patients pay the fees to the PMPs. In addition to providing a referra
center for an hour every morning at their own expense, the doctor gams professional and
commercial benefits to their practice that far outweigh the loss of several patients who cou d
never afford proper treatment in any case. In turn the Mahavir TB clinic informs the pnva
practitioners about the progress of their patients throughout their treatment. The Mahavir Hospital
and the PMPs keep the records for the government. The government provides TB control p
y,
training, drugs and laboratory supplies. Five outreach workers trace late or delinquent patients
and provide community mobilization.
All stakeholders gain an advantage through this partnership. The Mahavir Trust Hospital benefits
because the money spent on the DOTS service cures patients. The government benefits because
the DOTS medicine are properly used instead of being wasted or even contributing to the
development of drug resistant TB. The medicines are curing the patients and the spread of the
12
2>o
disease is being arrested. From tan economic point of view, the PMPs and nursing homes are
able to provide an effective treatment, which enhance their goodwill and affects their business as
a whole too.
The pilot project is aimed at attaining uniformity in the diagnosis, treatment and monitoring, wider
programme coverage; saving the patient’s time and expenditure by a good referral network.
11. Multilateral organizations like the World Bank and the European Commission have supported
the Sector Investment Programme in India and the Department of International Development
(DFID) in the area of health sector reforms in India.
12. In recent examples, the Chiranjeevi experiment of Govt of Gujarat may be seen at Annexure
IV.
CHALLENGES FACED IN THE OPERATIONALISATION: KEY CONCERNS
The existing evidence for PPP do not allow for easy generalizations. However it appears that
despite additional efficiencies, the objective of additional resources is not met, as State revenue
remains the bedrock of all services. The evidence also reveals great disparity in services and in
remuneration. As is evident the objectives of the initiatives have been to overcome some of the
deficiencies of the public sector health systems.
Donations, introduction of user fees, insurance schemes are methods to augment resources.
Contracting out is resorted to when health facilities are either underutilized or non functional while
contracting in is used to improve quality of services or improve accessibility to high technology
service or to improve efficiency. Contractual appointment of staff aims to reduce the negative
impact of vacant positions. Voucher schemes and community based health insurance etc are
invoked to reduce the adverse effects of health care costs on poor patients and improve equity in
health system. Mobile health schemes, involvement of CBOs, health cooperatives etc are models
in improving accessibility, both physical and to the health system. Some of the partnerships are
for a short duration while the other is longer. The thrusts of the partnerships also vary. Some
focus on service delivery, some to augment resources and infrastructure, some towards
organizational and systemic improvements while others are simply advocacy oriented.
Contracting is the predominant model for public private partnerships in India. Some
partnerships are simple contracts (like laundry, diet, cleaning etc) others are more complex
involving many stakeholders with their respective responsibilities. For example the Yeshaswani
scheme in Karnataka includes the State Department of Cooperatives, the Yeshaswani Trust with
its almost 200 private hospitals, a corporate Third Party Administrator and the beneficiaries with
the eligibility conditions.
It is seen that in most partnerships, the State Health Department is the principal partner with
rare stakeholder consultation. In most cases it signs contracts with very few cases of Hospital
Management Societies signing the contracts in a decentralized manner.
In terms of monetary value the contracts at Kolkottta’s Bagha Jatin General Hospital provided
inexpensive dietary services at the rate of Rs 27 per meal for about 30 patients a day and
cleaning service at Rs 24000/- per month. The most expensive partnership was the Rajiv Gandhi
Super Speciality Hospital in Raichur where the Government of Karnattaka has paid several
hundred million rupees to the partner as start up cost plus an assurance to cover future losses.
The above initiatives also show that more than 75% of the projects have been located in
backward areas of the states.
However true partnerships in sense of equality amongst partners, mutual commitment to
goals, shared decision making and risk taking are rare.
The case studies also bring to fore genuine concerns summarized in terms of absence of
representation of the beneficiary in the process, lack of effective governance mechanisms for
accountability, non transparent mechanisms, lack of appropriate monitoring and governance
systems and institutionalized management structures to handle the task
13
31
It is seen that the success or failures of the initiatives are as much dependant upon the above
issues as on the political environment, legal framework of the negotiation, the capabilities of t
partners the risks and incentive each party incurs, funding and the payment mechanisms cost
and price analysis prior to negotiation, standardization of norms, performance measurement and
monitoring and evaluations systems.
POTENTIAL AREAS FOR PARTNERSHIP
Different models of PPP are useful under different circumstances. The PPP lists have a
wide-ranging set of PPP options ranging from options for improved service delivery,
augmentation of resources and infrastructure, organizational and systemic improvement, to
advocacy owever any mechanism of PPP must be based on an assessment of local needs and a
situation analysis. For example strengthening the public health structure would be a more v- ab
option in many of the remote corners of the North Eastern states where the presence of private
sector |Sg>|eve| jt js quite c|ear thaf the private sector is as much responsible for
i a" fam'ij wX^SdlnSnd Uaum?Jnd em“es withinZir geZaphical areas and
. „.r,K .<
The remedies for most of the deficiencies of the health system largely fall within the ambit of
Primary Health Care - whether they are promoting, preventive or curative. Therefore at least in
the next five years the focus should be on augmentation of the primary health care services in
terms of focus on better service delivery options, including ancillary services like ambulance
services^and radiology
requirement of additional manpower in terms of regu'rement.of 3
lakh nurses and 12,000 Specialist doctors under NRHM, it is essential to explore a rang
partnership options in terms of private sector support to nursing institutions and medical schools
and colleges to make available the human resources reguired for NRHM. There would also be
massive requirement of managerial capacities under NRHM, which may be obtained throug
partnerships.
The potential areas may be as follows:
, _
Services, disease control and surveillance, diagnostics and medicines.
>
>
>
>
>
>
............................................................................................................................................................................................................
'
‘
Infrastructure
Health manpower
Behaviour change communication
Capacity building including training and systems development.
Managerial service and auxiliary activities of the health sector
In the initial phase caution should be exercised against expanding into too many sectors.
Government funding should not exceed an overall cap of 15% of the budget al.locatio2Super specialty care is not the goal. The intention is to provide basic health care to all
citizens of this country so that they do not face distress and duress in meeting health care needs.
RECOMMMENDATIONS FOR A PRACTICAL AND COST EFFECTIVE MECHANISM
Framework For Regulation
on
As is evident Partnership mechanisms do not work without quality assurance and an
enabling environment. Government must ensure that providers are accredited, at leastt essential
developed and Xd^and'providerTar^kept^dateT^hrough confining medical education
14
3^
advantages, disadvantages and requirements of partnership. They need to understand that
partnerships are based on common objectives, shared risks, shared investments and
participatory decision-making.
Since there is an element of contradiction in the objective of strengthening of the public
health system by the private sector in which the private sector apparently is the ultimate looser,
therefore it is essential that the framework for the whole process of partnership is not ad- hoc.
Equity, Quality and Regulation should underline the entire deliberation and apply not only to the
Private Sector but also to the Public Sector.
Primary goal of any health system should be assurance of health care professional
competence to the public. For a minimalist regulation system that may be feasible in the current
socio-political environment it is suggested that:
1.
Any Health Care Professional, practicing in any area / institution, should register with the
Primary Health Officer of the Area or the Institution as the case may be. For this purpose an
appropriate officer in the Primary Health Centres / Urban Health Centres may be identified as the
Primary Health Officer. Every Health Care Institution may be required to designate an officer as
the Institution’s Primary Health Officer. The Registers maintained by Primary Health Officers
should be accessible to public. The Register will also help Primary Health Centres and Public
Health Officials to manage public health emergencies and for epidemiological surveillance.
2.
Clinical Establishment Act, requiring registration of Health Care Institutions and Hospitals
with appropriate Health Authority. Clinics, Nursing Homes and Small Hospitals of less than 100
beds may register with Local Health Authority, to be designated for about 5 lakh population
(Revenue Division / Sub Division), larger hospitals may register with District Health Authorities
and Tertiary Referral Hospitals may register with concerned State Health Authority. The Act
should also provide for registration at the district level with the Zilla Parishad or the DHA
wherever capacities of PRIs are wanting and include redressal mechanism for health institutions
(Example diagnostic Centres) owned by a non-medical person.
The registers of professionals practicing in an area or within an institution should in the
public domain available for public use and scrutiny. This would eventually lead to setting up of a
national database on professionals practicing in different areas and institutions in different parts
of the country and will also help in the judicial process. Therefore it is important that Registration
should be in the Government domain and not with an autonomous body
The need for regulation should not only be for providers but also for training educators
and training facilities. There is also a need for a regulatory framework for the proposed Rural
Medical Practitioners as they would be key players in the primary health delivery systems.
Since managerial issues and governance capacities within the public health system are
key issues in determining the effectiveness of registration therefore, in the initial phase, self
registration should be encouraged followed by an interim accreditation mechanism developed
with the help of FOGSI/IMA before a fully e-governed registration system could be
institutionalized.
"Accreditation” as a voluntary process with set standards, provision for external review
etc. must also be supported and incentives for accreditation must be encouraged. The
accreditation initiatives in India at the National level (QCI, NABL) and at the State Level (AP,
Karnataka, Tamil Nadu, Kerela and Maharashtra) are progressive steps.
A range of Accreditation Systems ranging from compulsory accreditation, accreditation by
independent agencies, and facilitation of establishment of State Accreditation Councils to a blue
print developed by the Ministry of Health & Family Welfare may be explored. It is however
important to involve the stakeholders, build capacity, have different bodies at different levels, and
collect evidence base for the whole process. Accreditation should have synergy with Regulation.
15
33
The process of accreditation of Mother and Child Hospital specifying certain minimum
standards had already begun in Tamilnadu for the Janani Suraksha Yojana (JSY) Scheme.
However, in the process of accreditation there should be no fallback to the License R j.
There should be a single window for registration/accreditation of health institutions.
Framework Of Partnership
be understood.^
defjning the specific elements of the partnership from both sides as
many a time the private provider feels that the Government itself does not undertake any
9uarant^|ipppsP®hould
two bagic criteria, name|y (a) Value for Money and (b)
Clearly defined sharing of risks. There is need to develop skills within the government for
assessment of the Value for Money and Risk sharing characteristics of PPPs One common
requirement for assessment of Value for Money proposition is existence ° gooc' c0^Para‘°rSa
For example; NGO Management of PHCs uses current budgetary allocations of PHCs as a
comparator to make financial allocation. Similarly average out patient consultations or suchi other
therapeutic procedures, and public health activities in other PHCs can be used to assess the
oerformance of PHC under PPPs. CAG should be requested to develop specialised skills for
assessment of Value for Money and risk sharing characteristics of PPP projects. Auditing of
government expenditure through PPPs requirement would be different from traditional audit o
expenditure directly made by government departments. Unless the CAG develops capacity for
auditing of public expenditures through private partnerships, large scale expansion of PPPs
would be cnfficuH^^^^ Accountabi|ity, Trust, measurable efficiency parameters and Pricing
remain vexatious issues in the partnership process.
.
. _n<,.ira
The framework of partnership should also provide for the costing of services to ensure
that common citizens can get/buy cost effective services.
The governmental system of fixing rate is fraught with difficulties and it is better to
adopt public costing with moderation and states need to work out the cost effectivenessi very
meticulously. It may be noted that no serious effort at costing of services and standard treatmeat
protocol has been attempted in the government domain. The National Commission on Macro
economics and health (NCMH) is the first attempt to document the cost of services in the public
sector Attempts at costing under various PPP schemes like the Yeshaswam scheme of
Karnattaka and the Chiranjeevi scheme in Gujrat have been attempted. However more> work^s
required to be done in this area and the initiative should be taken by the Ministry and the States.
(Examples of a few cost effective options are at Annexure 1)
Decentralization should be the key in dealing with partnerships as centralizedI modete
suffer from failings enumerated in the aforesaid sections. The challenge under the NRHM is t
operationalise partnerships at the District level. Therefore there is also a requiremen ^ district
level skills and managerial capacity for making the process accountable, affordable and
accessible to common citizens.
The resource support and technical assistance for the PPP mechanism may come from
the National Health Systems Resource Centre (NHSRC), State Health Systems Resource Centre
16
(SHSRC) and the District Health Systems Resource Centre (DHSRC) being set up under NRHM
at the National, State and the District level respectively.
The National Institute of Health & Family Welfare (NIHFW) can be the nodal agency for
guiding PPP Policy at the National level. A PPP Cell at the NIHFW can also function as the
Documentation and dissemination Centre for PPP initiatives in the States. Resource support may
be provided under NRHM to fund this Cell. These Cells may be replicated in the States and the
Districts within the overall umbrella of the State Health Society and District Health Society under
NRHM.
District level Health Resource Centres, can help in developing transparency in PPP and
provide the much needed managerial capacity to manage processes like Accreditation and
Standards.
Public Private Partnership needs to be mutually beneficial to both the parties so that
there is encouragement of enterprises and element of pragmatism. It is important that the health
professionals also earn in the process to sustain the partnership. However, the earning should
be commensurate to the health services provided specially to the poor. This is possible through
the volumes of patients, which the private sector would be getting from the public sector.
There is a need for further documentation of the ongoing experiments in PPP and
evaluation of their impact. The evaluation mechanism should highlight the issues of access,
utilization, sustainability, cost effectiveness and pricing, equity, transparency, audit etc.
Models For Partnership
It is essential to appreciate the diversity in terms of regional variations in the health status
across the country. Therefore, generic models of existing PPP practices like contracting in,
contracting out, social marketing, and social franchising may be modified to suit local variations.
The assumption here is that a homogeneous prescription would not work and therefore the
challenge is to develop the nitty-gritty of a framework allowing for diversity of models esp. at the
District Level.
Public-Private-Partnership Models (Details at Annexure 2)
• Contracting:
Contracting out
Contracting-in
•
Franchising:
Partial franchising
Full franchising
Branded clinics
• Social marketing
• Joint ventures
• Voucher schemes
•
Hospital autonomy
• Partnership with corporate sector/ industrial houses
•
Involving professional associations
•
Build, operate and transfer
• Donation & philanthropic contributions
•
Involvement of social groups
• Partnership with co-operative societies
• Partnership for capacity building
•
Partnership with non-profit community-based organizations
• Running mobile health units
• Community based health insurance
PRINCIPLES OF PPP
17
Although the approaches are different for each typology to resolve the health crisis
principles guiding each of such
currently in hand, there are certain common underlying
i
partnerships, which are enumerated below:
1. Setting up of common goals and objectives, which are committed by all the partners.
2. Outcome based planning
4. cTeatonofTsocialXod by improving the health situation of the poor and underserved as well
as standardization and uniformity of quality health service delivery
5. Accountability and responsibility set out vividly for each partner
.
.
6 Sharing of costs and resources are done on the basis of equity. The same principle is followed
for sharing risk and rewards. Central to any successful public-private partnership initiative is the
identification of risk associated with each component of the project and the allocation of that risk
factor to the public sector, the private sector or perhaps a sharing by both. Thus, the desired
balance to ensure best value (for money) is based on an allocation of risk factors to the
participants who are best able to manage those risks and thus minimize costs while improving
7. Regular meetings among the partners to discuss issues at hand and planning and coordinating
^A^clear understanding of the strengths and weaknesses of the partners among themselves is
essential to understand their roles and responsibilities clearly
9. The monitoring mechanisms are made sound in order to address the diversity of
e
lO^Fi'nandal sustainability is an all-pervading factor, which forms the backbone of all
partnerships. There has to a regular flow of funds in order to meet the personnel and operating
costs. Some programs have become self-sustainable only by involvement of the people. Such
schemes do not require regular funds from the Government
11 Partnerships could be full substitution of the provision of health services, or managing the
operations or monitoring or provision of infrastructure (equipments, manpower etc.)
12 Any vested interest in such structures could destroy the base, and lead to the failure of the
whole institution. Thus, a high level of trust and confidence is required in all the PPP initiatives.
13 Effective communications are key to the public's understanding of public-private partnerships.
Communications are required to be planned and carried out as an integral part of the
management process for any project. It involves timely sharing of information accurate and
consistent messages conveyed to key audiences, realistic messages from trusted sources that
set realistic expectations.
14 ppp involves a long term relationship between the public sector and the private sector. While
the collaboration between the two may take various forms like buyer seller relationship, donor
recipient relationship, the most stable partnership is in the form of “contract binding on both the
parties. The contract mirrors the basic objective of the programme/project, the tenure of
agreement, the funding pattern and of sharing of risk and responsibilities. The need to define the
contract very precisely, therefore, becomes paramount under PPP.
Project/Programmes under PPP may, however, broadly be classified under three heads
namely (i) service contract (ii) operations & maintenance (management) contract and (iii) capital
project, with operations & maintenance contract.
Selection of Service Provider
Transparency in ‘selection’ is an essential feature of PPP. Selection of the developer or the
service provider may be done in any of the following three ways.
(i) Competitive Bidding
This involves it well publicized and a well designed bid process to ascertain financial,
technical and managerial capabilities of the service provider or the developer. Either of the two
18
formats for bidding, namely single round sealed bid auction or multiple round open entry
(ascending) bid auction could be adopted. The appropriate biding process depends on the nature
of the valuation that the bidders place on the concession, that is, on the right to do the job.
In some cases the valuation of the project depends on factors that are within the bidder’s
control, such as construction and maintenance cost of a building or a road. These are also
known as ‘private value items’. In other cases, the valuation does not depend just on the bidders
own assessment, but also on certain unknown factors that need to be anticipated. These
unknown factors are common to all bidders and each bidder may update his/her own assessment
based on the assessment of other bidders. These are know as ‘common value items' and include
factors such as the size of market, willingness to pay of consumers and future behaviour of
regulatory etc.
For private value items, a single round auction is appropriate since bidders do not need
to learn from the revelation of information of other bidders and a sealed bid auction is preferable
since that has the least potential for collusion. Concessions with common value characteristics
on the other hand, are best awarded through multiple round bids since this facilitates the process
of value discovery by bidders, allowing bidders to observe and respond to quotations/prices as
they emerge. Multiple round bid can also be sealed bid but there is opportunity to rebid after the
bids are opened. Moreover, wherever the bid process is characterized by a two stage process
involving for instance, mega infrastructure projects, the bidders are required to obtain from their
prospective lenders the financial terms, expectations regarding state support as well as their
comments on the concession agreement etc.
The final selection of the developer/service provider depends upon one or a combination
of the following (a) lowest capital cost of the prOoject (b) lowest operation and maintenance cost
(d) lowest bid in terms of the present value of user fees (c) lowest present value of payment from
government (d) highest equity premium (c) highest upfront fee (f) highest revenue share to the
Government and or 9g) shortest concession period.
Under situations of only a sole bid being received, the authorities have the choice of
either accepting or rejecting the sole bid. In the case of rejecting the sole bid, or when no bid is
received, the project/programme proposal itsSelf may be modified and the bid process restarted.
Alternatively the selection of the developer/service provider is done through competitive
negotiation with the private sector participants.
(ii) Swiss Challenge Approach
The Swiss Challenge approach refers to suo-moto proposals being received from the
private participant by the government. The private sector thus provides (a) all details regarding
its technical financial and managerial capabilities (b) all details regarding technical, financial and
commercial viability of the project/programme (c) all details regarding expectation of government
support/concessions.
The government may examine the proposal and if the proposal belongs to the declared
policy of priorities, then it may invite competing counter proposals from others (in the spirit of
‘Swiss Challenge’ approach) giving adequate notice. In the event of a better proposal being
received, the original proponent is given the opportunity to modify the original proposal. Finally
the better of the two is awarded the project/programme for execution.
(iii) Competitive Negotiation
Competitive negotiation (direct or indirect) is considered a variant of competitive bidding. The
Government thus specifies the service objective and invites proposals through advertisement.
The government then negotiates/finalise the contract with the selected bidders.
19
The government agency (or the local authority) may select the service provider/developer
through competitive negotiation in the following cases:
a)
b)
c)
d)
e)
Social sector projects and programmes involving VOs/NGOs/Local Community.
Project involving proprietary technology or a franchise;
Linkage project related to a mega project or a major activity.
Projects and programmes which failed to solicit any response to a bidding process.
Su-moto proposal from private participants.
Negotiation may, however, be ‘simple’ (direct) or ‘complex’ (indirect). In the second case,
the government negotiates through a master contractor/mother, NGO. In other words, contracts
for (public) services are contracted out and the master contractor handles all dealings with subcontractors/franchises. While the government reviews the works of the master contractor through
its monitoring (officials) who may visit the site of programme implementation and meet the
beneficiaries, the master contractor may monitor the programme (run by sub-contractors) through
collecting
information
from
the
beneficiaries
selected
randomly,
based
on
questionnaires/interviews.
Advantage of Master Contractor
Some of the advantages mentioned about master contracting are: (a) government has
administrative convenience, and better control in dealing with less number of service providers (b)
funds can be raised from other public and private sources, other than the government (c) decision
can be taken more quickly despite political pressures and (d) training programmes can be
organised for the sub-contractors/service provider/vendors by the master contractor more
innovatively.
However, master contract is not always relevant and negotiation vis-a-vis the contract
ought to be done directly with the community/beneficiaries as for instance, in the case of wild life
protection with the residents living in the vicinity of the forest. Competitive negotiations are,
however, less transparent than competitive bidding. With a view to ensure fairness nonetheless,
it is recommended that the government auditor may audit such contracts.
16 Payment mechanism: Payment to the private sector could take the form of (a) contractual
payments (b) grants-in-aid and 9c) right to levy user charges for the asset created/leased in
Contractual payment may be in the form of advance payment, progress payment, final payment
annuities and guarantees for receivable etc. Annuities, in turn could be with respect to recovering
the fixed cost or for recovering both variable cost and the fixed cost of the project. In the form
case, both the government and the private partner share the risk of running the project.
Grant-in-aid in turn can take different forms such as a block grant, capital grant matching
grant, institutional support etc. Lease agreement license similarly may allow the concessionaire
to recover the cost of construction/operation & maintenance through levying user charges.
Moreover, in the case of lease agreement, the asset reverts to the government after the expiry of
the contract. The agreement ought to also provide for the condition of asset that would be
returned at the end of the contract.
17. Monitoring & Evaluation: It is quite often, thought that the job is over with the signing/finalizing
the contract. Payments have to be, however, linked to performance, which in term requires
monitoring. Performance measurement can be done with respect to measuring efficiency or
measuring effectiveness. While measurement of efficiency entails comparing the unit cost of
providing the service from amongst the various alternatives, measurement of effectivenSess
involves comparing the desired outcomes from amongst the various alternatives.
20
2
Monitoring may be done in either of the following ways (i) by government departments
authorized to do so, based on a standardized scale (ii) by independent agencies/regulators based
on a standardized scale (iii) by the department or independent agencies, based on the simple
criteria of pass and fail by the department or independent agencies, based on the feed back
received from the beneficiaries.
Involvement of third party/independent agencies for monitoring appears to be preferable
as they leave the government hassle free over the project and minimize government control. A
certain percentage of the cost of the project needs to be, therefore, earmarked for contract
management. The government and the developer/service provider could mutually decide the
third party. The third party involvement could be further supplemented with provisions for
adjudication by the highest judiciary.
The following would be useful parameters in monitoring and evaluation of the initiatives:
> Profile of implementing agency: history, organizational structure, management board,
business, service provided
> Procedures followed in signing the partnership- decision making process,
competitiveness and transparency in selection process, criteria for selection and time
taken
> Cope and coverage of services under agreement
> Eligibility conditions for the private agency-minimum investment, proper experience
> Specific clauses in the MOU-maximum duration of the contract, pricing and service
specification, billing and payment mechanism, managerial flexibility, supervision and
monitoring, quality control, employment service conditions of the staff, physical
infrastructure support, subsidies and incentives, penalties and fines, exit clause,
grievance redressal system
> Performance evaluation, renewal of contract
> Public health objective clause- specific services and subsidies to poor, women and
children
> Feedback of stakeholders-state and central bureaucrats, public health facility managers,
private agency managers, beneficiaries, staff in both public agency and private agency,
community leaders
I
Conclusion
The Government plays a predominant role in any PPP. Hence it has to follow certain
successful strategies in order to become a better partner. The key elements of a successful PPP
are as follows:
1. The Government should look at the long-term value in a partnership
2. Selection of the right partner becomes imperative for the government to achieve tangible
outputs and create the ‘best value’. A partner's experience in the specific area of partnership
being considered is an important factor in identifying the right partner.
3. By aligning the stakeholders’ interests, the Government could endeavor better value creation
4. The Government could a adopt a more strategic approach by stepping back from the day to
day management of public enterprises, and instead focusing on the drivers of long term value,
setting targets and encouraging alliances and partnerships with the private sector.
5. The Government should introduce greater transparency. Greater openness about the financial
performance and service delivery of public enterprises will be a useful discipline on managers
within those organizations. Focusing on a few strategic targets will be a start.
6. The Government could introduce greater shareholder expertise by ensuring an appropriate mix
of skills and experience among the partners to help carry out the health objectives more
efficiently.
7. However, if PPPs are genuinely going to deliver better quality services, it is vital that they are
designed with the focus on outputs and performance. The private sector partner or partners need
to be clear about what is expected from them and the implications if they fail to deliver.
8. The Government must recognize that it has a continuing role in the public service element of
essential services. In some cases, this may mean retaining some elements of service delivery in
21
2^
the public sector. Therefore it becomes critical to decide on retaining the control over certain
services, rather than contracting them.
9. The Government could adopt the following approaches to deliver partnerships.
thl UdrcumasktancesPi? whichP^hey6 arePto be implemented and the objectives which they are
the circumstances in which they are to
intended to serve
(b) Creating innovative and imaginative partnerships and creating new ways of working - learning
bv doing - is key, particularly where there is no existing best practice
(c) Designing a holistic approach PPPs by joined-up thinking, reflecting the needs of customers
potential partners and providers, as well as joined-up Government initiatives rather than the
narrowing the objectives to the departmental territory.
The performance of any PPP in the health sector could be evaluated based on the following
building blocks:
1. Beneficence or public health gains
2. Non-malfeasance or not leading to ill health
3. Autonomy enjoyed by each partner
4. Shared decision-making
5. Equity or distribution of benefits to those most in need
However it may be reiterated that the private partnerships are not sufficient to resolve the
dilemma of inadequate health care for the people. The focus of Public policy in the context o
thel 1 th Five Year Plan should be the flagship march for strengthening the public health sector.
22
uo
Annexure-1
MOST PRACTICAL & COST EFFECTIVE MODE OF PPP FOR IMPROVEMENT IN
HEALTH SERVICES DELIVERY
PROBLEM AREAS
AT VARIOUS
LEVELS IN HEALTH
SERVICES
DELIVERY
TYPE OF SUGGESTED
PARTNERSHIP
SHORTAGE/
ABSENCE OF
SPECIALISTS
APPOINTING
SPECIALISTS ON
CONTRACT BASIS ON
WEEK ENDS OR SO.
ABSENCE/ POOR
QUALITY OF RADIO
DIAGNOSTIC i
MACHINERY
INSTALLATION OF
RADIO DIAGNOSTIC
MACHINERY (CT.USG.XRAY) BY PRIVATE
SECTOR ON CONTRACT
IN BASIS IN THE
PREMISES OF THE
HOSPITAL
WORKING MODELS
HOSPITAL SET-UP
GOVT OF GUJARAT
IMPLEMENTED THE
PARTNERSHIP IN
SEP 2002 IN
NARMADA DISTT.
AND LATER
EXTENDED TO
RAJKOT DISTRICT
CT MACHINES HAVE
BEEN INSTALLED
AND ARE BEING RUN
BY PRIVATE
AGENCIES IN 7 GOVT
HOSPITALS IN WEST
BENGAL.
COST EFFECTIVITY
REMARKS
FUND POOLING FROM
UNUSED BUDGET DUE TO
VACANT SPECIALISTS
POSITION TO USE FOR
CONTRACTING PRIVATE
PRACTITIONERS
PARTNERSHIP
IS
ON
CONTRACT
BASIS
AND
RS
500(LATER
EXTENDED TO RS.
1000 PER VISIT)
PER VISIT TWICE A
WEEK
IS
PAID.
EVALUATION
SHOWED
THAT
ARRANGEMENTS
ENSURED ACCESS
TO
SPECIALIST
SERVICES
AT
HOSPITALS.
HOWEVER,
PER
DAY HONORARIUM
SHOULD BE KEPT
EQUIVALENT
TO
ONE DAY SALARY
OF
SPECIALIST
WITH
CONVEYANCE
CHARGES OF RS
500/-
SERVICES ROUND THE
CLOCK AT REDUCED
PRICES, FREE SERVICE FOR
BPL PATIENTS & SENIOR
CITIZENS, A FIXED NO. OF
INVESTIGATIONS/MONTH
/HOSPITAL AFTER WHICH
THEY CAN CARRY AS MUCH
AS THEY WISH BUT THEY
WILL HAVE TO PAY
COMMISSION PER PATIENT
&
CONDITIONS
STATE THAT FREE
SERVICES SHOULD
BE GIVEN TO AT
LEAST
35
PATIENTS/
HOSPITAL AND TO
NOT MORE THAN
615
CASES/
HOSPITAL/ MONTH
AT
APPROVED
GOVT RATES. 25%
COMMISSION
AFTER
THE
SPECIFIED CASES
TO BE PAID TO
STATE
GOVT.
MODEL RESULTED
IN OVERALL COST
REDUCTION
ACROSS THE CITY.
PATIENTS
FEEDBACK
MUST
COMPLIANCE
CONDITIONS
IS
FOR
OF
23
OH
~~~~
ABSENCE OF 24x?
LAB SERVICES
ON THE BASIS OF
CONTRACTING IN
PARTNERSHIP WITH
THE PRIVATE SECTOR
PARTNERSHIP
BETWEEN M/S
THUKRAL
DIAGNOSTICS
CENTRE LUCKNOW &
BMC AND PG
ALIGUNJ
IMPLEMENTED IN
MARCH 2003
NO EXTRA COST ON
STRETCHING THE LAB
SERVICES TO ROUND THE
CLOCK, FREE SERVICES
FOR BPL PATIENTS WHOSE
FEES CAN BE REIMBURSED
FROM THE HOSPITAL
WELFARE COMMITTEE
IN 1994 IN SWEDEN A
FOR PROFIT
LABORATORY
CALLED
MEDANALYZE WAS
AWARDED A
CONTRACT TO
HANDLE LAB TESTS
FOR PRIMARY CARE
PHYSICIAN IN A
DISTRICT OF
STOCKHOLM
COUNTY.
DIFFICULTY IN
ACCESS TO
SUPER-SPECIALIST
HEALTH SERVICES
IN REMOTE AND
HILLY AREAS
SETTING THE TELE
MEDICINE & TELE
HEALTH SYSTEM ON
CONTRACTING OUT
BASIS WITH THE
PRIVATE SECTOR
KARNATAKA
' INTEGRATED TELE
MEDICINE AND TELE
HEALTH PROJECT, IN
KARNATAKA DISTT
HOSPITAL,
NARAYANA
HRUDAYALYA
BANGALORE IN
COLLABORATION
WITH
REDUCED
AND
DUTRAVEL
« rxHVElu. rvlvu*
ELIMINATION OF
UNNECESSARY PATIENT
TRANSFER, LOW CAPITAL
INVESTMENT FOR
ESTABLISHING A CARE
PRESENCE, TRAINING AND
RE-TRAINING AT THE
LEAST COST POSSIBLE
"Tn
case“of
SMALLER
lUNITS,
“'—
GOOD AND> BAD
LOCATIONS
; BE
SHOULD
AWARDED
together
TO
COMPENSATE FOR
POSSIBLE LOSSES
SELECTED
DIAGNOSTIC
CENTRE PROVIDES
3 DIFFERENT
PACKAGES AT
REASONABLE
COST FOR
EMERGENCY
INVESTIGATIONS.
THE
ARRANGEMENT
ENSURES THE
PREGNANT
WOMEN AND
CHILDREN HAVE
THE ROUND THE
CLOCK ACCESS TO
LAB
INVESTIGATIONS
AT AN
AFFORDABLE
COST
THE STOCKHOLM
MODEL FAILED AS
THE COMPANY
WAS UNABLE TO
HANDLE THE
LARGE VOLUME OF
SAMPLES AND
BEGAN
MISHANDLING
SPECIMENS AND
EVEN
FABRICATING
RESULTS AS A
MEAN OF COPING.
EXIT POLICY MAY
BE CONSIDERED.
ONLY ACCREDITED
AND TRUSTED
LABS IN HEALTH
SECTOR SHOULD
BE CONSIDERED.
GOVT MAY
EXEMPT RENT,
WATER CHARGES
ETC FOR REMOTE
AREAS
THE
■ ’ ,u’ 27
TELEMEDICINE
CENTERS IN INDIA
ARE THE LARGEST
E-HEALTH
CENTERS IN THE
WORLD;
SO FAR 16000
HEART PATIENTS
HAVE BEEN
TREATED VIA AN
24
‘E-WAY’.
INDIAN SPACE
RESEARCH
ORGANIZATION.
OPERATIONAL SINCE
2002.
LOW AVAILABILITY
OF DOCTORS AND
MEDICAL
SERVICES
PARTNERSHIP WITH
THE CORPORATE/BOT
FOR MEDICAL/ DENTAL
EDUCATION &
SERVICES
VARIOUS PRIVATE
MEDICAL/ DENTAL
COLLEGES ACROSS
THE INDIA.
NO EXTRA BURDEN IN
CORPORATE AND NO
RUNNING COST IN BOT
NON/LOW
AVAILABILITY
OF MEDICINES
& SURGICAL
ITEMS
PARTNERSHIP OF
SOCIAL MARKETING
TYPE CAN PROVIDE
CHEAPER MEDICINES &
SURGICALS IN
HOSPITAL PREMISES
LIFE LINE FLUID
DRUG STORE IN
SAWAI MAN
SINGH(SMS)
HOSPITAL, JAIPUR,
RAJASTHAN
STARTED IN 1996
WITH NO EXTRA COST
STATE GOVERNMENT CAN
PROVIDE STANDARD STUFF
TO THE PATIENTS AT
REASONABLE PRICE
ROUND THE CLOCK
GOVT MAY OFFER
TAX INCENTIVE OR
SOME OTHER
RELIEF IN LIEU OF
WORKING IN
REMOTE AREAS,
PENALTY CLAUSE
FOR NON
FUNCTIONING OF
FACILITY.
FACILITY CREATED
MAY ALSO BE
OPEN TO OTHER
PYT
PRACTITIONERS IN
SURPLUS TIME.
POLICY FOR
PRIVATE SECTOR
PARTICIPATION IN
MEDICAL/ DENTAL
EDUCATION SEEKS
TO ATTRACT
PRIVATE SECTOR
TO SET UP
COLLEGES IN THE
STATE. CRITERIA
IS LAID DOWN BY
THE STATE GOVT,
MCI & DCI. FINAL
DECISION IS
BASED ON THE
AVAILABILITY OF
LAND WITH THE
ORGANIZATION,
AVAILABILITY OF
HOSPITAL HAVING
MINIMUM 300 BEDS
FOR MEDICAL
COLLEGE
EXISTING
EXPERIENCE
FAILED IN DELHI.
GOVT MAY
PURCHASE
SERVICE FOR
POOR/NHPS ON
PREDETERMINED
RATES. HOWEVER,
GOVT MAY DECIDE
THAT NEW
PHCS/CHCS WILL
BE OPENED BY
PYT PLAYERS AND
GOVT WILL BY
SERVICES ON
YESHASVINI
MODEL
THROUGH OPEN
TENDER , RMRS
INVITE BIDS FROM
SUPPLIERS TO
PROCURE
MEDICINES THAT
LLFS SELLS TO
25
LACK OF
AMBULANCE/
TRANSPORT
SERVICES
PARTNERSHIP WITH
NGOS/CBO.USER
CHARGES/KM SCHEME
EMERGENCY
AMBULANCE
SERVICES, THENI
DISTRICT, TAMIL
NADU,
PARTNERSHIP IS
OPERATIONAL SINCE
2002.
AMBULANCE/TRANSPORT
SERVICES CAN BE
PROVIDED WITH NO EXTRA
EXPENDITURE ON
PURCHASING/
MAINTENANCE OF THE
VANS
LOW
SANITATION
AND LAUNDRY
STANDARDS
CONTRACTING
OUT/NGO PARTNERSHIP
GOVERNMENT OF
UTTARANCHAL HAS
HANDED OVER
LAUNDRY SERVICES
IN 9 BIG HOSPITALS
TO PRIVATE
AGENCIES IN
DECEMBER 2001
WHILE THOSE IN
DOON HOSPITAL
WERE HANDED
OVER IN FEB 2003
IMPROVED SANITATION AND
LAUNDRY
SMS PATIENTS AT
THE
PROCUREMENT
PRICES. RMRS
DECIDES THE
PERIOD OF THE
CONTRACT, WHICH
IS RENEWABLE ON
THE BASIS OF
GOOD
PERFORMANCE.
WITH FIXED
SALARY AND A
ONE - PERCENT
COMMISSION ON
ALL SALES, THE
CONTRACTOR
APPOINTS AND
MANAGES STAFF
FROM THE
RECEIPTS.
WILL BE
SUCCESSFUL
WHERE HIGHER
VOLUME OF SALE
EXIST. SMALLER
HEALTH UNITS
MAY ALSO BE
TAGGED WITH
BIGGER ONE IN
CONTRACT
TOTAL COST OF
THE PROJECT IS
6,50,000. RS. 5 PER
KM AS USER FEE.
FREE SERVICES
TO 10%
CASES,(BPL
PATIENTS).
MEMBERS OF
WOMEN’S SELF
HELP GROUP GET
10% CONCESSION.
THIS TYPE OF
INITIATIVES WILL
BE SUCCESSFUL
IF LARGE NUMBER
OF AMBULANCES
ARE CONTRACTED
WITH LEAST IDLE
TIME AND RATE IS
SUBJECT TO
REVISION WHEN
HIKED BY GOVT
THESE AGENCIES
HAVE BEEN
SELECTED ON THE
BASIS OF THE
COMPETITIVE
BIDDING.
MANPOWER,
CONSUMABLES,
EQUIPMENT AND
SALARY TO
_EMPLOYEE_
26
Q9-
DIETARY
SERVICES
CONTACTING IN WITH
PRIVATE CATERERS ON
COMPETITIVE BIDDING
BASIS
ALONG WITH THE
LAUNDRY/
SANITATION
SERVICES THE
GOVT. OF
UTTRANCHAL
HANDED OVER THE
DIETARY SERVICES
AS WELL IN THE FOR
MENTIONED
HOSPITALS
HYGIENIC AND NUTRITIOUS
FOOD WITHOUT EXTRA
BURDEN ON
INFRASTRUCTURE
HEALTH
INSURANCE
COVERAGE TO
THE STATE
POPULATION
COMMUNITY BASED
HEALTH INSURANCE
ALSO CALLED SELF
FUNDED HEALTH
INSURANCE SCHEME.
HOWEVER THE SCHEME
IS NOT FULLY SELF
FUNDED BECAUSE IT
REQUIRES
GOVERNMENT
CONTRIBUTION
YESHASVINI-COOPERATIVE
FARMER’S HEALTH
CARE, KARNATAKA.
PARTNERSHIP
BETWEEN NARAYAN
HRUDAYLAYA
BANGALORE &
APOLLO HOSPITALS
HYDERABAD, TRUST
WAS LAUNCHED IN
2002
PROVIDE SURGICAL CARE
THROUGH LOW PREMIUM
HEALTH INSURANCE.
COVER NEARLY 1600 TYPES
OF SURGERIES. FREE OUT
PATIENT CONSULTATION.
MEDICAL AND DIAGNOSTIC
INVESTIGATIONS AT
NOMINAL RATES. SCHEME
COVERS EVEN
PREEXISTING ILLNESSES.
SHOULD BE
CAREFULLY
DRAFTED IN
AGREEMENT
OTHERWISE
SITUATION WILL
GET WORST
THE SELECTION
OF THE PRIVATE
PARTNER WAS ON
THE BASIS OF THE
COMPETITIVE
BIDDING BY THE
HOSPITAL
AUTHORITY.
POOLING OF
ANCILLARY
SERVICES WILL
RESULT INTO
BETTER PROFIT TO
CONTRACTOR.
STRICT
CONDITIONS
ABOUT
COMPETENCE OF
CONTRACTOR AND
JOB TO BE DONE
IS NEEDED
1,600 DIFFERENT
SURGERIES
; COSTING UP TO A
MAXIMUM OF RS.
200,000.MEDICAL
TREATMENT NOT
LEADING TO
SURGERY IS NOT
COVERED. GOVT.
OF KARNATAKA
ORIGINALLY
CONTRIBUTED 50%
OF MONTHLY
PREMIUM FOR
EACH MEMBER
NOW ONLY A
CONSOLIDATED
AMOUNT (OF RS.
3.5 MILLION IN THE
SECOND YEAR
AND 1.5 MILLION IN
THE THIRD YEAR).
FHPL IS PAID 4%
OR AROUND RS.
5.9 MILLION AS
THEIR FEE.
COMMITTED GOVT
CONTRIBUTION ON
LONG TERM BASIS
AND TIMELY
COLLECTION OF
CONTRIBUTION IS
MUST. RATHER
CREATING NEW
HOSPITALS, GOVT
MAY ENCOURAGE
SUCH SCHEMES
ON LONG TERM
BASIS
AT CHC/ PHC LEVEL
27
IMPROPER
MANAGEMENT
CONTRACTING OUT
WITH THE PRIVATE
SECTOR
MANAGEMENT OF
PRIMARY HEALTH
CENTERS,KARUNA
TRUST, KARNATKA A
NON PROFIT NGO,
FROM 1996 ON TRIAL
BASIS , BUT BASED
ON FORMAL POLICY
DECISION, SINCE
IMPROVED MANAGEMENT
WITH THE SAME/LOW
BUDGET
2002
POOR
OUTREACH
AND
REFERRAL
SERVICES FOR
SLUM
POPULATION.
CONTRACTING OUT TO
PRIVATE
ORGANIZATIONS
ARPANA SWASTHYA
KENDRA
MOLARBUND, DELHI,
IN PARTNERSHIP
WITH MCD.
PERFORMANCE
MEASURES ARE SET
FORTHETRUST,
INITIAL CONTRACT IS
FOR 5 YEARS.
DISTRIBUTING THE BASIC
HEALTH PRODUCTS SUCH
AS CONTRACEPTIVES, ORS,
CLEAN DELIVERY KITS TO
THE SLUM DWELLERS THRU
EXISTING COMMERCIAL
NETWORK FUNDS POOLED
FROM RS. 10 FOR OPD
CARDS INCLUDING
MEDICINES FOR 3 DAYS, RS.
50 TO 100 FOR EMERGENCY
AMBULANCE SERVICES.
GOVT. PROVIDES
PHC PREMISES,
INITIAL
EQUIPMENTS AND
SUPPLIES,-AND
75% TO 90%
SALARIES.
STAFFING BY THE
NGO. RS. 25000
PER ANNUM AS
CONTINGENCY.
RS. 75000 PER
ANNUM FOR
DRUGS/ SUPPLIES.
FREE HEALTH
CARE TO ALL
PATIENTS.
SELECTION OF
WORKERS
SHOULD BE THE
PREROGATIVE OF
NGO., GOOD
WORKING AND
POOR WORKING
FACILITIES
SHOULD BE
JOINTLY HANDED
OVER. INCREASE
IN SALARY OVER
TIME MAY BE KEPT
IN MIND.
APPRAISAL BY
THIRD PART IS
MUST. GOOD
FINANCIAL MGT IS
KEY TO SUCCESS
PERSONALITY
DRIVEN PROJECT.
LACK OF CLARITY Of
USER-FEE,
SHORTAGES OF
RESOURCES
COMMON. LONG
PROCEDURES,
OVERCROWDING,
LACK OF FOLLOW UF
ACCEPTABLE
QUALITY OF
SERVICES ;
COMMITTED STAFF.
EXISTING PVT
PRACTITIONERS MA’
BE TRAINED AND
INVOLVED WITH
INCENTIVE OF PER
UNIT OF SERVICE.
EXISTING PPM
APPROACH OF
RNTCP CAN BE
HELPFUL
INITIALLY, SOME
SEED MONEY MAY B
GIVEN TO START THI
28
PROJECT
COOPERATIVE
SOCIETIES MAY BE
ROPED- IN
1
UNDER
STAFFING OF
THE MEDICAL
OFFICERS/
ANMS
| APPOINTING MEDICAL"
OFFICERS & ANMS ON
CONTRACTING IN BASIS
UTTRANCHAL GOVT.
HAS MADE EFFORTS
IN APPOINTING
MEDICAL OFFICERS
& ANMS. THIS HAS
BEEN DONE IN VIEW
TO IMPROVE
HEALTH SERVICES
IN REMOTE AREAS
AND GIVEN THE
DIFFICULTY IN
RETAINING
SERVICES OF
PROVIDERS DUE TO
LACK OF
ACCOMMODATION
AND LOW SALARY.
" TO RETAIN THE
SERVICES GOVT.
HAS INCREASED
THE HONORARIUM
OF CONTRACTUAL
MEDICAL
OFFICERS FROM
11,000 PER MONTH
TO RS. 13000 PER
MONTH W.E.F. FEB
2004.IN ORDER TO
PROMOTE
INSTITUTIONAL
DELIVERIES, 24
HOURS DELIVERY
SERVICES ARE
BEING PROVIDED
IN 85 HEALTH
CENTERS AND
CERTAIN
INCENTIVES ARE
PROPOSED FOR
SERVICE
PROVIDERS WHO
CONDUCT
DELIVERIES
BETWEEN 8.00 PM
TO 7.00 AM.
LOCALLY
PRACTICING
DOCTORS AND
STAFF MAY BE
GIVEN PRIORITY
AS THEY MAY FIND
THE AMOUNT
ACCEPTABLE.
REGULAR REVIEW
OF SCHEME IS
NEEDED
NO EXTRA BURDEN ON
INFRASTRUCTURE AS
FUNDS CAN BE POOLED
FROM THE FUNDS UNSPENT
DUE TO VACANT POSITIONS
NATIONAL HEALTH PROGRAMMES
FAMILY
WELFARE
PROGRAMME
CONTACTING
WITH THE
NGOS
1459 PRIVATE
HOSPITALS ARE
APPROVED FOR
PERFORMING
VASECTOMY,
TUBECTOMY, MTP
AND OTHER
CONTRACEPTIVES,
GOVT. PROVIDES BASIC
SERVICES WHERE NGO CAN
PROVIDE BEDS, SURGICAL
ITCMO TA DCDCADM
ITEMS TO PERFORM
STERILIZATION SERVICES
■
CATARACT
CONTRACTING
CERTAIN NGOS LIKE
NGOS CAN PERFORM
DRUGS CHARGES
AND OPERATING
SURGEONS FEES
ARE PAID BY THE
GOVT. PAYING
COMPENSATION
TO STERILIZATION
ACCEPTOR.
OPERATIONAL
COST IN GOVT
SET-UP MAY BE
CONSIDERED AS
SERVICE CHARGE
TO PVT
PROVIDERS.
ADVANCE
PAYMENT WILL
IMPROVE
PERFORMANCE
SOME 100 PRIVATE
29
-
BLINDNESS
CONTROL
PROGRAMME
WITH PRIVATE
SECTOR
(NCOS)
TB CONTROL
PROGRAM
PARTNERSHIP
WITH PRIVATE
PRACTITIONER TO GIVE
IEC ON THE DOTS
SCHEME AND FOR
IDENTIFICATION AND
TREATMENT OF THE
PATIENTS, GOVT. LABS
ARE OPEN FOR THE USE
BY THE PRIVATE
PRACTITIONER FOR TB
DIAGNOSIS
AIDS CONTROL
PROGRAMME
PARTNERSHIP
WITH NGOS TO SPREAD
AWARENESS ABOUT
THE HIV/AIDS , MAKING
FREE CONDOMS
AVAILABLE TO THE
PEOPLE BY NGOS
PARTNERSHIP WITH
PRIVATE DOCTORS /
NGOS. NGOS CAN
CONDUCTS PULSE
POLO CAMPS, PRIVATE
DOCTORS CAN GIVE
POLIO DROPS TO THE
UNDER FIVE CHILDREN
THOSE WHO VISITS
THEM AS PATIENTS OR
WITH PATIENTS
. .. .
CONTRACTING WITH
THE PRIVATE HOSPITAL
PULSE POLIO
PROGRAMME
RCH PROJECT
VHS, CHRISTIAN
MISSION HOSPITAL,
ANDHRA MAHILA
SABHA, F.P.A.I. ETC.
ARE GIVEN ANNUAL
GRANTS BY
GOVERNMENT FOR
THEIR RECURRING
EXPENDITURE. THIS
IS APPLICABLE TO
CERTAIN
DISPENSARIES RUN
BY NGOS IN TRIBAL
AREAS ALSO.
CATARACT SURGERIES,
ARRANGE EYE CAMPS
WHERE GOVT PROVIDES
FINANCE.
MAHAVIR TRUST
HOSPITAL,
HYDERABAD,SEWA
AT AHMEDABAD
AND, MANAV
SARTHAK
KUSTHASHRAM,
JAIPUR ARE SOME
OF THE SUCCESS
STORIES
SPREADING AWARENESS ’
THROUGH PRIVATE
DOCTORS IS COST FREE,
OPENING THE LABS FOR
USE BY THE PRIVATE
DOCTORS CAN DIAGNOSE
MORETB PATIENTS AND
TREATMENT OF THE SAME
UNDER RCH
PROJECT
HOSPITALS ARE
APPROVED FOR
UNDERTAKING
MAJOR
SURGERIES
UNDER THE ABOVE
SCHEME.
ONLY ACCREDITED
NGOS HAVING
SKILLED
MANPOWER
SHOULD BE
CONSIDERED.
HOSPITAL
CREATES A
REFERRAL CARD,
INITIAL DIAGNOSIS
, COUNSELING ,
AND TREATMENT
PROTOCOLAND
REFERS THE
PATIENT TO
DESIGNATED DOTS
CENTER FOR
DRUGS. GOVT
PROVIDES FREE
DRUGS AND
MEDICINES TO THE
DOTS CENTERS
ALSO TRAIN
MEDICAL STAFF,
PROVIDES LAB
SUPPLIES,
PRIVATE MEDICAL
PRACTITIONERS
REFER PATIENTS
MODEL OF RNTCP
HAS STRONG
POTENTIAL FOR
ADOPTION IN ALL
NHPS
WITH NO EXTRA COST
GOVT CAN SPREAD HIV/
AIDS AWARENESS AND
PROVIDE CONDOMS TO THE
PEOPLE
MONITORING IS
MUST
WITH INVOLVEMENT OF
PRIVATE PEOPLE
PROGRAMME CAN BE
IMPLEMENTED MORE
EFFECTIVELY WITHOUT
ANY BURDEN ON EXISTING
INFRASTRUCTURE
VACCINE
PREVENTABLE
DISEASES ARE
ALSO ISSUED
FREE OF CHARGE
TO PRIVATE
NURSING HOMES
FORTHEIR USE
EFFECTIVE AND ECONOMIC
RCH & FAMILY WELFARE
FUNDS FOR THE
SCHEME WILL BE
30
•• •
UNDERTAKE LSCS ’
SURGERIES WHERE
GOVT SERVICES ARE
NOT AVAILABLE, FEES.
ARE MET BY GOVT.
HOSPITAL,
OBSTETRICIANS ,
ANESTHETIST CAN BE
HIRED FOR LSCS
SURGERIES IN GOVT
HOSPITAL WHERE THEY
ARE NOT AVAILABLE.
MTP SERVICES ARE
ALSO PROVIDED IN THE
PRIVATE HOSPITALS
AGAINST THE
VOUCHERS WHICH
REIMBURSED AFTER
EVERY MONTH FROM
THE STATE GOVT.
INNOVATIVE MODEL
LIKE VIKALP ARE
GOING ON.
DELIVERY HUTS MAY
BE HANDED OVER
TO NCOS ALREADY
INVOLVED IN RCH
SERVICES CAN BE
PROVIDED TO THE PEOPLE
PROVIDED FROM
THE DEPARTMENT
OF HEALTH,
HARYANA TO THE
MOTHER NGO FOR
FURTHER
PAYMENT. THE
PAYMENT WILL BE
MADE OUT OF THE
FUNDS AVAILABLE
VOUCHER
SCHEMES UNDER
THE RCH n
PROGRAMME. AN
AMOUNT OF RS 1.5
CRORES IS
AVAILABLE FOR
IMPLEMENTING
VOUCHER
SCHEMES IN THE
YEAR 2005-07. THE
NORMS FOR
PAYMENTS WILL
BE FINALIZED
AFTER
NEGOTIATION
BETWEEN MNGOS
AND PRIVATE
PROVIDERS.
ADVANCE
PAYMENT IN FIRST
QUARTER MAY BE
EXPERIMENTED
31
Annexure-2
MODELS OF PUBLIC PRIVATE PARTNERSHIPS
Various models can be utilized for putting these partnerships into action; some of the
possible mechanisms for implementation of PPP are given below:
1. Franchising
its blueprint for a successful product line with franchisees. The franchisees contribute resources
of their own to set up a clinic and pay membership to franchiser.
Partial Franchising: Most of the social franchising models followed in India are partial
franchising models. Franchiser identifies private hospitals and enters into an agreement wi
franchisee to provide certain services in lieu of payment of fee or commissions from sale o
services and goods. These contracts largely confine to a basket of RCH services. However
franchisee provides many other services that are not part of the contract. There is no control over
quality of services provided by franchisee outside the contract.
Usually one-year subscription fee is given by franchisee to franchiser. In this arrangement,
increased performance of franchisee does not lead to increased revenues to franchiser. There is
no incentive to franchiser to improve performance through promotional activities. One way to
overcome this problem is to have a revenue sharing arrangement between franchiser and
franchisee. However many of the hospitals are not transparent about their financial transactions
or do they maintain complete record of services provided. One of the innovative aspects of these
social franchising efforts is to link rural medical practitioners and/or community based
orqanizations such as SHG to franchisee that has helped to increase the client load for RCH
services The partial franchising efforts in India do not represent public-private partnerships but
offer a model and experiences that are highly relevant. Government can have its own model of
social franchising with franchiser-franchisee-RMP-CBO linkages. Concentration of private
hospitals/ nursing homes in urban areas has to be taken into consideration. In many rural and
inaccessible areas where the need for improved access to services is the highest, there are not
private hospitals/nursing homes.
Full Franchising: Franchisee provides services defined by the franchiser and expansion of
range of services depends on mutual agreement. For existing nursing homes and hospitals this
can mean a considerable revenue loss and this has to be filled in by subsidies till the client load
improves and the hospitals start making operating profits. Time required for transition of oss
making unit to profit making unit depends on a variety of factors such as location of hospitals
demand for services, perceived quality of services and competition. Not many hospitals may opt
for this given the uncertainties in financial returns, unless guarantees are given to sustain the
model for a long period of time.
2. Branded Clinics:
...
A few organizations have started a chain of branded clinics that offer a wide range of reproductive
and child health services. There is scope to expand the range of services provided by these
clinics and add social mobilization efforts to their functions. These branded clinics can be opened
in areas where there is a need with minimum effort. Branded clinics are more sustainable
because of their ability to generate more income than social franchising units.
32
3. Contracting Out
Contracting out refers to a situation in which private providers receive a budget to provide certain
services and manage a government health unit. The two parties usually agree on some or all of
the following: the quantity and the quality and the duration of the contract.
Common criteria for identifying those government health clinics that need to be contracted out are
the first step in this direction. Large number of vacancies for a long period, high absenteeism, and
consistent low performance on all RCH indicators could be the critical criteria.
Some states are more prepared for contracting out services compared to others. Fear of losing
jobs and perceived shrinking role of government in health sector are the main reasons for
resistance. Advocacy efforts are required in those states where resistance levels are high for
contracting out services.
There are several levels at which the contracting out can be done depending on the degrees of
freedom given to the contractor. Higher the freedom, higher should be the performance levels of
key RCH indicators.
Option 1:
Option 2:
Option 3:
Option 4:
Government hands over the physical infrastructure, equipment, budget and
personnel of a health unit to the selected agency.
Government hands over the physical infrastructure, equipment, budget but gives
freedom to the selected agency to recruit personnel as per their terms and
conditions but following the government norms such as one ANM per
5,000/3,000 population.
Government hands over the physical infrastructure, equipment, and budget but
gives freedom the select agency to have their own service delivery models
without following the fixed prescribed pattern.
Government hands over the physical infrastructure, equipment, budget and gives
freedom to the select agency to have their own personnel, service delivery
models, freedom to expand types of services provided and freedom to introduce
user fee and recover some proportion of costs.
4. Contracting In
Contracting in is done for a variety of services particularly in major hospitals. These include:
maintenance of buildings, utilities, housekeeping, meals, medicine stores, diagnostic facilities,
transport, security, communications etc. Hospitals are given freedom to choose the services to be
given to contractors. In many cases they lack comprehensive plans and sound financial analysis.
Nevertheless, contracting in many hospitals has resulted in conservation of resources, improved
efficiency and better quality of services. Contracting in services leads to surplus human resources
and they need to be transferred to other health units to fill in vacant positions, if any. Resentment
of employees and interference of trade unions are some of the major obstacles to this process.
Contracting in does not work in some places for particular types of services. For instance some
state governments could not attract private sector participation for diagnostic services in remote
area hospitals with low client load. One option is to subsidize the equipment purchased by private
agencies and the other is to make services located in government hospitals open to all. Even a
person with prescription from private clinic should be allowed to use privately run diagnostic
facilities in government hospitals. This increases the volume of transactions and makes the unit
financially viable.
Recruiting doctors, technicians and other staff on contractual basis for a stipulated period of time
is widely practiced in several states. In some cases the contracted staff performs all duties of
regular staff and in other instances, their services are contracted for a few days in a month and to
provide services in a particular clinic. In many states, a large proportion of vacant positions were
filled in following this process.
X * )*
G-iov- io
10182
AL '*
> oLZ
gfcsilsRsl
reckon with and gained considerable experience in marketing contraceptive products both social
and commercial. The increasing trend now is to enlarge the basket of products by including ORS,
IFA tablets and other health products to make the marketing efforts more self-sustaining.
Government provides the subsidized contraceptives, and finances brand and point of purchase
promotion schemes of selected marketing agencies.
6. Build, Operate and Transfer
t
Build, operate and transfer (BOT) models are highly successful in infrastructure development
sector in India. BOT requires part financing of projects by the government, financial guarantees
when needed, subsidized land at prime locations and assurance of reasonable returns on
investment. These models could be useful to establish large hospitals and ensure quality services
at reasonable rates to poor people. However these hospitals should be able to withstand market
competition to survive and sustain themselves.
7. Joint Venture Companies
. .
Joint venture companies are companies launched with equity participation of government and
private sector. Proportion of equity of each partner may vary from one venture to another. Joint
venture companies, in most cases in commercial sector, have not succeeded in India due to lack
of understanding and trust between partners, inordinate delays in decision-making and
dominance of government even with low equity. There is even less chance of their succeeding in
health sector.
8. Voucher System
.
A voucher is a document that can be exchanged for defined goods or services as a token of
payment (tied-cash”). This consists of designing, developing and valuing health packages for
various common ailments / conditions (like ANC package / STI package / Teen pregnancy
package / family planning package etc) which can be bought by the people at specific intervals of
time. These vouchers can then be redeemed for receiving a set of services (like 1-2
consultations, lab tests, procedures, counselling and drugs for the condition) from certified/
accredited hospitals or clinics and are to be used within 2-3 months of buying the voucher. This
means that the package can be bought, used as and when required and ensures privacy for the
client.
Regular monitoring is required for ensuring quality standards, training of providers and networking
with the people to ensure that the proper use of vouchers. The vouchers are redeemed to the
clinics for the number utilised depending on the price for each package of
satisfaction can be
Clinics that fail the quality standards of service and do not do well on patient
| 1
removed from the certified services.
9. Donations from individuals
Within a large country like India and with a creditable high income and middle income 9roups
there are many examples of private donors willing to partner with the public sector. Rich
philanthropists, individual donations may be the crucial requirement in areas to make the PPP
initiative effective in delivering health care. Though in some states mechanisms and provisions
are present for utilizing these private donations for improving local health situation, many other
states lack these systems. Efforts have to be made to create simple and transparent institutional
mechanisms to encourage donations to contribute to the growth and improvement in reproductive
and child health services in their area.
34
10. Partnerships with Social Clubs and Groups (e.g. Rotary Club)
Clubs like Rotary and Lion’s played a significant role in immunization campaigns, Pulse Polio
campaign and other health care services. Since these clubs have a nation wide network, their
involvement ensures better coverage. They also bring in their expertise and resources to the
health care services.
11. Involvement of Corporate sector:
The corporate sector has a rich history of being supportive of the health and family welfare
interventions for people that work in and live around its premises. Under Corporate Social
Responsibility, the corporate sector through the Confederation of Indian Industries (CH) and the
Federation of Indian Chamber of Commerce and Industries (FICCI) and several other sector wise
business and industry associations have played a significant role in advocacy efforts, funding
non-government organizations for innovative interventions, introducing new schemes to
encourage service utilization and expending their own resources for promotion of reproductive
and child health services particularly family planning services..
12. Partnership with Professional Associations
There are several professional associations such as Indian Medical Association, Gynaecologists
federation, nurses associations etc. These association from time to tome extended help in
launching new programmes such as Vande Mataram Scheme, Gaon Chalo project and
immunization programme particularly pulse polio. They have technical skills and expertise to
provide advice on various other matters such as setting standard protocols, quality assurance
systems and accreditation. However the managerial capacities of these professional associations
have to be strengthened.
Moreover, with widespread chapters/ branches all over the country and huge membership they
can play a very important on ethical issues.
13. Capacity building of private providers, pharmacists and informal providers (RMPs)
Several initiatives taken by the government in the past to improve the technical and counselling
skills of private medical practitioners particularly rural medical practitioners by providing them
training improved quality of services offered by them. Since they have a huge presence in rural
areas and urban slums and a significant proportion of population depend on them for services,
there is a need to involve them in a significant way to create demand for services and in making
referral system effective. Similarly government medical officers and administrator benefited by
participating in training programmes conducted by private institutions. Consultancy services
offered by private institutions in the areas of communications, systems development etc is
another example of public-private partnership. Another area of partnership is contracting out
management of training institutions such as ANM Training Centres, Regional Training Centres to
NGOs and private agencies.
14. Special “Category Campaigns” with the private sector to improve health
The WHO-ORS campaign and the Goli- ke- Hamjoli campaigns are examples of the use of the
commercial sector to advance national health goals. The category campaigns expand use of a
health/family-planning product, increases the volume and the users for the product. In India, the
Goli ke Hamjoli and WHO-ORS campaigns succeeded in increasing product awareness,
availability, sales, and use. At the same time, this entails using a generic promotional strategy,
increased private-sector investment and the value of the market, policy change; coordination with
partner pharmaceutical firms; affiliation with professional associations; expansion of market
channels; and consumer outreach. Initially, the program should use mass media vehicles to
improve product awareness and contemplation. But, as the program develops, its emphasis
should shift to encouraging product trial, and use interpersonal approaches to reach out to
potential consumers.
35
These special campaigns in partnership with the private sector can focus on demand generation
for refurbished and revitalised public sector, generic promotion of health products (lite saving
ORS, Menstrual Hygiene with Sanitary Napkins etc).
15. Autonomous Institutions
Giving autonomy to public institutions within the system can lead to improvement in qua ity,
accountability and efficiency. It also ensures greater involvement and ownership at the level of
the institution, ensuring greater morale and encouragement to the work-force. Many such projects
have been implemented and have shown to yield excellent results, as the need for the change in
management systems is self-driven. This is also sustainable and easy to replicate.
16. Partnering with CBOs / NGOs
For designing and implementing innovative approaches to RCH services, partnerships with
community based organizations and non-government organizations are a significant step.
Government for long encouraged participation these grass roots organizations in demand
creation and delivery of services. These organizations often worked in remote rural areas where
access to RCH services is difficult. Recent NGO Policy of the MOHFW envisages a scheme
where each district would have a mother NGO and linked to several field NGOs within the district
with greater degree of autonomy and decentralization. Community mobilization efforts yield
effective results and community ownership of the programme is sustainable.
17. Mobile Health Vans
In geographical areas with difficult terrain with no transport facilities and poor road connectivity
usually the outreach and institutional services of PHCs are not to the expected standards. This
has resulted in gross under utilization of services. To overcome this problem, in some states
private sector agencies have taken a lead in launching mobile vans. These vans go to clearly
identified central points on fixed days and provide comprehensive health services including RCH
services to a cluster of villages. While private sector resources were put to use to purchase vans,
the government contributed to these services by deputing medical officers and medicines. This
approach has significantly helped to improve access to quality services.
18. Insurance and Public-Private Partnerships
In one of the recently planned schemes, the government insures and pays health insurance
premium for families below poverty line. These families in turn are insured against expenses on
health and hospitalization, up to a certain amount. On similar principle, it is possible to develop
sustainable health insurance schemes that are community based. In such schemes, the
community members pay a minimum insurance premium per month and get insured against
certain level of health expenditure. This protects them from sudden and unexpected expenditure
on health. Such community based schemes also ensure that the local needs and expectations of
the people are met, by preferentially reimbursing local trained healthcare providers.
CLASSIFYING PPPs
Since public-private partnerships vary significantly, it is necessary to categorize them in order to
understand their nature and thrust areas of partnerships. Some of the partnerships are for short
duration or one time activity and others are for long term. These partnerships also work in specific
thrust areas. Some of the partnerships may cover all thrust areas and others one or more.
Nature of PPP
Examples
One time /Short term
Partnership
Donation of land, money, equipment etc
Participation in campaigns
Continuous / Long term
partnership
Social franchising of service
Contracting In and Out
Social marketing
Capacity building_________
36
Thrust areas of partnership
Examples
Service oriented
Social Marketing
Social Franchising
Contracting healthcare providers
Mobile vans____________________________
Contracting out IEC activities to NGOs
Category Campaigns with Private Partners
Information
oriented/Advocacy oriented
Infrastructure oriented
Capacity building oriented
Construction of buildings
Repairs to buildings
Equipment, Vehicles_____________________
Training for skill development and counselling
Systems development
Managerial capacity
CRITERIA FOR INITIATING PPPs
Types of public-private partnerships relevant for a particular state depend on prevailing
conditions, needs and functional requirements. Some criteria by which the public-private
partnerships should be selected are given below, as follows:
Form of Partnership
1. Franchising
Criteria for initiation
_______ __
• The effort to revitalize the complete govt, infrastructure is time
consuming and a slow process
• Resources required to expand public health infrastructure is
enormous.
• Need for services is enormous and the government health
institutions are not in a position to cater to needs
. Availability of vast network of private hospitals in places needed
. When objective is to improve access to services on immediate basis.
•
Improve quality standards of private sector and provide high quality
■ "care-at affordable
i ■ Ti Ti - • Need to expand services rapidly
. Provide high visibility to clinics
. Offer a package of services selected for the purpose
. High quality services at affordable prices
3, Contracting Out
•
•
.
•
Difficult to manage government health units in remote and
inaccessible areas
Utilization of services and performance levels are consistently low
due to non-availability of staff
Aim is to put government health facilities to optimum use
Increase responsiveness of government health facilities to local
needs through community involvement
37
5
^Contracting In
5. Social Marketing ' ~
6. Build Operate
Transfer (BOT)/Joint
Ventures
Voucher System
8. Donations from
individuals
9. Partnerships with
Social Clubs and
Groups (eg. Rotary
Club)
to” Involvement of
Corporate sector
Improve efficiency levels of services provided
Make management of services more effective
Conserve scarce resources by cutting costs
Try out innovative approaches to improve efficiency and
effectiveness
...... ——---- • Combine service delivery with demand creation
• Availability of products in a vast network of easily accessible retail
outlets
. Encourage brand choices and competition to improve penetration
levels
, 4, 4
. Perceived value attached to priced products than products
—.............
distributed free of cost
.............
-—: -—
number of
of service
service delivery
delivery points
points whether
whether hospitals,
hospitals,
• An enormous number
labs or diagnostic centres have to be constructed within a short span
of time.
When the cost of building and maintaining a unit Is prohibitive for the
govt, to bear alone
• When returns on investment are guaranteed.
• Government treats health as infrastructure industry.-----------------• Improve access to services and provide choice
• Costs act as a major barrier to services
• Existing service delivery points do not have provision to all types of
services
• Inadequate knowledge about the value of service (eg importance of
antenatal care)
• Generate demand for services particularly among poor and
disadvantaged sections
_
• Presence of affluent families, philanthropic organizations
• Identified needs to Improve quality of services
• Clear procedures and guidelines to accept donations
• Transparent and accountable systems that enhance image of
institutions______ ____________
. ------- ----------------- :—7—
• Partnerships to popularise revitalized service points, communication
campaigns and logistics management
• Organization of camps on a large scale
e Neecj for additional resources and also management and technical
expertise
. Need to step up advocacy efforts ..... —
_—
• Resources to outreach services through NGOs in remote areas
• Effective services to employees in organized sector
• Policy advocacy efforts
• Adoption of villages or CHCs/PHCs by corporate health sector to
improve services.
I
___________
p
•
•
•
38
5G
11. Partnership with
Professional
Associations
.
•
•
•
•
.
Presence of active professional associations with clear guidelines
Internal committees to promote ethical practices
Management expertise to implement projects
Need to prepare standard protocols, quality assurance system by
building consensus
Improvement of technical skills of professionals in both private and
public sectors
Improve professional response to programme needs
12. Capacity Building
of Private providers,
pharmacists and
Informal providers
(RMPs
•’
•
•
13.Special “Category
“Campaigns with the
Private Sector to
improve health
•
14.Autonomous
Institutions
T “Need to upgrade~quality of services’and Initiate use of state-of-theart technology in health care delivery
• Provide enough flexibility to health units
• Improve efficiency and effective levels of management
• Reduce costs and facilitate quicker decision-making
. Allow institutions to generate alternate sources of funding
15 Partnering with
NGOs/CBOs
.
•
•
•
16. Mobile Clinics
•
•
■■■■■■■MH
17. Insurance
Schemes
■■■■I
•
•
•
.
High dependence of people on private sector for services
Technical knowledge and skill levels are not to a desirable standard
Improve quality standards of providers and increase access to
quality services
Put in place an effective referral system
Involve services providers in social marketing efforts
When the need to promote a service or health care product is
established
Multiple partner involvement is required to promote a product
Advocacy efforts to make product acceptable at all levels
Encourage community involvement
~
Improve community ownership of programme
Test innovative and cost-effective approaches to service delivery
Cover inaccessible and remote areaMHHMH^
Provide access to services people living in inaccessible terrain
Make services available at central location to reduce travel time and
costs of clients
_•__ Improve utilization of services in remote areas
• Focus on poor and disadvantaged
• Provide services at affordable costs
• Long term solution to health problems
• Improved choice of health units
. Reduce indebtedness among poor due to health costs
■■
39
I
Annexure 3
References:
1.
Prof. N.K. Sethi etall: Public Private Partnership in the Health Sector in India:
Initiatives in selected States
2.
Planning Commission, Gol: Report of the PPP Subgroup on Social Sector
November2004:
3.
Ravi Duggal, VHAI: The Private Health Sector in India: Nature Trends and Critique
4.
NIHFW: National Planning Workshop on Public Partnerships in the Health Sector in
India, 2005
5.
A Venkat Raman and James Warner Bjorkman: Public Private Partnership in Health
Care Delivery in India
6.
MoHFW: The Report of the Task Force on Medical Education, 2006
7.
National Sample Survey Organisation (NSSO): Report on the 60th Round
8.
Source for Graphs. Pearson M, Impact and Expenditure Review, Part II Policy
issues. Draft DFID, 2002
40
a
AnnexureIV
CHIRANJEEVI-THE CONCEPT
• For reduction in maternal and child deaths /
access and equity
• In five backward districts
• For EmOC and Em transport services
• With weak Public Health Facilities in Obstetric
care
• In Partnership with FOGSI
• For making available private specialists to BPL
pregnant woman
• Unit cost Rs 1795/- based on package of
services includes:
CHIRANJEEVI-THE CONCEPT-II
• Rs200/- for transport to pregnant mother
• Rs 50/- for midwife or attendant
• Pvt gynaecologist pays above and avails
reimbursement
• ANC Registration in a Govt facility a must
• Advance of Rs 15000/- to the pvt
gynaecologist
• CDMHO empanels and monitors
41
DISTRICT-WISE PERFORMANCE OF
DELIVERIES UNDER CHIRANJM YOJANA,
GUJARAT
Progress Dec 05- March06
District
Total
number of
Private
specialists
Number of
Private
specialists
enrolled
Deliveries
under
Chiranjivi
Yojana till
Average
performance
per Doctors
Panchmahal
29
27
2313
86
Sabarkhanta
73
46
1897
41
Banaskhanta
50
52
1436
28
Kutch
47
20
726
36
Dahod
16
18
1421
79
Total
215
73.6%
7793
48
CHIRANJEEVI-OUTCOMES
• 163 Molls signed. 76% enrollment
• 87% Normal and 5% Caesarian delivery
• Avg Delivery per specialist is 48
• 31% (2415)of 7793 BPL pregnant mothers have
delivered
• No maternal death reported. As per MMR 30
mothers would have died
• 9 infant deaths reported. As per IMR 350-450
infants would have died
• Access of BPL pregnant mothers to institutional
delivery
42
So
ARUNACHAL PRADESH
EXPERIMENT : THE CONCEPT
• Pilot Project:
90% Govt
10% NGO
• State hand over infrastructure of PHC/SC
to Agency
• State to provide cost towards personnel,
drugs and consumables
THE CONCEPTS)
• Agency to engage its own staff and ensure
availability 24X7
• Staffing Pattern
■=>
MO - 2
Pharmacist - 1
Staff Nurse - 2
ANM - 2 (PHC)Z 6 (SC)
■4> LHV-1
lab tech - 1
■=>
Driver -1
HA(Jr.)-1
=> Group D - 4
43
Si
THE CONCEPT (3)
• Agency to provide all services expected of a PHC
• PHC Management Committee-RKS
• State Steering Committee
• National level NGOs
• Exit policy for Agency and Govt
• Audit and Accounting
• Output based performance indicators
• Outreach Activity
• Implementation of National Programmes
• External Evaluation/Concurrent evaluation
PARTNERS IN AP
• Karuna Trust
: 9 Districts
• VHAI
:5 Districts
• JAC(Prayas)
: 1 District
• FGA, Itanagar
: 1 District
44
Chapter 3
Findings of the Study Team
Status of Infrastructure, Coverage, Supplementary Nutrition Programme, Health
and Education
“I was searchingfor the Anganwadi of Mongolpuri in the middle ofAugust, 2006, hut no
one could give any clue from the address I had in my hand. After a long time I could
identify a group of women sitting outside.
“Can you please tell me where the Anganwadi is? ” I asked.
“ What is that? ”
“Anganwadi is where dali, chana etc are distributed to children. “
“OK, two houses to the left”
“Don I your children go to the Anganwadi? ”
“No, but my sister in law’s sons go. There! ” she pointed out to a lady washing clothes in
one of the municipality taps.
I approached her and said, “Does your child go to Anganwadi? ”
“No, but I bring the khichdi or dalia for him, ” she answered.
“How does it taste? Does your child enjoy it? ”
“Not at all! Its so watery, the dalia swims in the water. ”
I reached the anganwadi centre and could find only the landlady at around 11 am. It
certainly did not look like one. It was just a room with no children, no charts and no toys.
Only two big empty drums were lying there...
Sheeted, Field Investigator
2.1 Infrastructure - Adequate infrastructure is necessary for delivery of services of
SNP, Pre School Education, Growth Monitoring etc. Regarding infrastructure, the
experience in Delhi was varied.
Swarn Park: A Model Anganwadi Centre
During our visit to Swaran Park A WC we were received warmly, in a neat and decorated
Aanganwadi Centre where there was ample space for the children "s activities and play. A
group of happy, chirpy children welcomed us. There was clean drinking water and toilet
and the Aanganwadi Worker, the Supervisor and the CDPO were actively involved in
making it into a model A WC. Later we found out there is only one A WC, which needs
quality improvement in the whole project area.
The A WC was decorated with colourful chains made out of waste material, we sat on
multi coloured “darhi”s made by the women from the community with waste pieces of
clothes andjute bags. There were colourful teaching aids made out ofjute bags in which
SNPs are supplied. Everything in the centre was neat, clean and vibrant. The CDPO, the
63
Supervisors, the A WW and the mothers have joined hands to run the centre in the best
possible manner.
Khanpur: A Centre with no space
In Khanpur, the place used as the premises of the A WC centre, is a 4 ft x 7 ft garage
where the landlord keeps his motorcycle. There is no toilet, no drinking water facilities.
During summer and monsoon it is difficult to have activities outside. Generally the
activities are carried out in the open space which actually meant only for distribution of
SNP, whose quality was questioned by everyone present in the meeting, including
functionaries and beneficiaries.
Issues:
•
Space - Most of the centres in Delhi suffer from a severe inadequacy of space
both for storage and for carrying out activities. 58% AWWs complained of space
constraint. In most centres, due to the inadequacy of space, the number of children
registered is only 20-25 whereas, according to the norms, the number should be
40 for children between 3 to 6 years.
10% of the AWCs have either kutcha infrastructure or they operate from jhopris.
These centres have serious lack of space and cleanliness
Location and access - There were no complaints regarding location and
accessibility of the AWCs other than those in Govindpuri, Khyala and
Jahangirpuri areas where AWCs were located on 3rd or 4th floor making the access
difficult and unsafe.
•
Rent: a) Low allocation for rent: As per our survey, 96% centres are on rent. The
allocation for rent is a meager Rs. 500/- per month (the revised provision of rent
since June 1, 2006). 90% Aanganwadi Workers during their interviews, and 8 out
of 10 group discussions, pointed out that meager allocation for rent is a serious
concern. Within this amount, it is not possible to get an exclusive place in Delhi
for the AWCs, where there is space for equipment, for activities, a kitchen and a
clean toilet. AH the functionaries have expressed that “the rent should be raised to
Rs. 1000/- at least”.
b)Irregular payment of rent - 96% AWWs functioning from rented centres,
said they all said rent is irregular. It is generally allotted once a year. As the rent is
irregular, the landlords prefer not to give out premises exclusively for use of the
AW. So the centre cannot be locked. In these circumstances, the worker and
supervisor do not feel it is safe to keep equipment inside. If the landlord has
guests, or if someone in the house is not well, the centre cannot be opened. This
poses a challenge for the regular functioning of the centre. There have also been
instances of Supervisors and Anganwadi workers being harassed by the landlord
on the ground of irregular payment of rent. Irregular rent is thus an issue of
concern.
•
Drinking water and sanitation: Only 57% of the centres have toilets and 58%
have access to clean drinking water. Most of the toilets are common toilets.
Sometimes the neighbours provide drinking water to the centre.
The AWWs have complained of scarcity of resources to buy essentials like jugs
for water storage. At times they have provided it by spending their own money.
•
Scarcity of equipment: 82.23% of AWWs said there was scarcity of equipment
like weighing machines, education kits, toys etc., and it interferes with the
functioning and compromises the quality of the program.
Table 4:Comparison between Neeve Study, Delhi and FOCUS Report* (Data on
Active and Dormant States) Data on Infrastructure
Active States
(FOCUS )
44%
48%________
57%________
65%________
20%
Delhi
Study
0%
Neenv Dormant
(FOCUS)
22%
29%
55%
70%
20%
States
Own building
Kitchen________
42%
Storage facilities
Drinking water
57%
Toilets________
58%
Note:* FOCUS Report
Table 3 shows that Delhi lags behind even the dormant States studied in the FOCUS
Report as regards infrastructure
2.2 Outreach:
While sharing our findings on outreach we would like to comment that coverage is a
common issue for all components. The children not reached through SNP, Preschool and
Health all throw up concerns related to coverage. In this section we have dealt with
coverage from the aspect of attendance recorded in AWC on the day of the survey. The
sub-section on exclusion is the record of the facts that emerged from focused group
discussions.
The following table records the average number boys and girls available in the AWW’s
area and derived from the surveys done by the AWWs in Column 3. Column 4 and 5
captures the average number of boys and girls registered and the attendance on the day of
the survey. The average has been arrived by dividing the total number of boys/girls by the
number of centres covered. The source of Columns 3 and 4 are AWWs’ registers and
Column 5 is the finding of the research team. Minimum and maximum number of
children found in a centre ranges from 0 to 15.
6^
Table 6: Attendance
Beneficiary
Children between 7
months to 3 years
Children between 3-6
years______________
Pregnant ladies______
Lactating mothers
Adolescent girls
Boys
Girls
Boys
Girls
Average no. per
centre as per
survey done by
AWWs
Registered
as
per
AWW’s
register
(average no.
per centre)
35
27______
25______
16______
31
25
23
10
11
3
15______
9_______
8_______
Noteven 1
Attendance
(average
no.
per
centre) as
observed
on the day
of survey
9_______
9________
7________
6________
_3________
j_________
Not even 1
The above Table highlights the discrepancy between the official data and the reality on
the ground. There is also a glaring contrast between the enrolment recorded in the
registers of A WCs and their number actually found attending.
The surveys made by AWWs are also irregular in Delhi. There are centres where no
survey has occurred for more than three years in a row.
Exclusion - as observed during the survey:
•
Leaving out the poorest of the poor - The AWC at Selampur is accessed by
economically backward communities. The service delivery other than SNP was
observed to be poor. In Nizamuddin area, one meeting took place inside the
Valmiki Mandir. We found a group of rag pickers (they are considered to be
Bangladeshis as they spoke Bengali and were Muslim in religion) who are not
given access to the centre though they lived in the same compound. Within a few
months they were forcibly evicted. Communities in slums who suffer demolitions,
are resettled and then uprooted - are left out of ICDS.
The best AWC we have come across in Kanjhawala was mainly accessed by
children who are from families that are economically comfortable. During
discussions and community meetings, we have seen the poorest of the poor is
often left out. The MLA in Karol Bagh area also hinted that the programme is not
reaching the needy. The Supervisors felt that the performance of the programme
will improve if it really reaches the poorest strata of Delhi.
Exclusion of poverty groups like street children or children from the
construction sites: The presence of the poor migrants, rag pickers, street children
has not been felt during data collection through questionnaires or Focussed Group
Discussions. Most of the AWCs are located in resettlement colonies and slums.
This leaves the child of the migrant labourers in construction sites and the street
children out.
•
Exclusion due to poor service delivery - The poor quality of service delivery is
responsible for denying the children their rights and entitlements. There is poor
attendance due to low quality of service.
2.3 Supplementary Nutrition Programme
The objective of distributing supplementary nutrition (norms in Annexure -A ) through
AWC is to supplement deficient nutrition among children below six years and pregnant
and lactating mother.
According to Secondary data:1
• 63% of Delhi’s children below 3 years suffer from anaemia
• 33% suffer from malnutrition
• 30% children are born underweight
Findings from the study on SNP
Food Quality: Cooked food was started from July 2006. The comments from the
beneficiaries and AWWs are as follows :
o During the summer a number of our beneficiaries have reported that the
food has become rotten food as it was cooked early in the morning.
o The beneficiaries look forward to dry ration as that can be stored as well
as shared within the family for a long period of time.
o The new system requires their presence during daily food distribution and
therefore, being resented as “it adds to the demand to their time”. Even
caste issues came up during discussions. Mothers expressed concerns over
the caste of the cook.
The complaints about irregularity have lessened after cooked food was started.
Complaints of poor quality came from 39% of the centres. One major problem was that
there was no fixed time of supply. There have been days when food has come after 1 pm.
During summer the food has become rotten. Najafgarh area has specifically complained
of insects and dirt found in the food material
1 NFHS III, 2003 (Annexure - IV)
Quantity of SNP distribution - The children followed over six months in case studies
have been receiving food from the centre regularly. Some described the quantity as “one
katori” some as “two karchi”. Only one mother specifically mentioned 200 grams.
The AWWs and helpers during the discussions revealed that the quantity distributed is
variable. Days when the numbers of beneficiaries are more, they distribute less quantities
of food.
Regularity/irregularity in distributing SNP - 26% of the centres who had complained
about irregular supply was mainly surveyed before cooked food was initiated. However,
during the days of polio vaccination, irregularity was observed. The workers either stop
distributing food on those days or they distribute dry foods like biscuits.
Coverage of pregnant women and lactating mothers: On an average only 17 women
under this category are found to be registered in an AWC. On an average 3 to 4 pregnant
women and lactating mothers are attending the centre.
Sharing of SNP: 76% of our beneficiaries were found to be sharing SNP with family
members, hence the targeted nutrition is not reaching the beneficiaries. Only 82
beneficiaries out of 2861 beneficiaries interviewed are taking food in the centre.
The following Table gives a comparison on the status of SNP in Delhi with active and
dormant FOCUS states:
Table 7:Status of SNP: Comparison between Neenv Study and the FOCUS2 States
Active States
Neenv Study
Dormant States
(FOCUS)
(FOCUS)
% Of AWCs 94
100
93
where SNP is
provided
% of AWW 95
74
54
who feel food
distribution is
regular_______
% of AWW 2
39
35
who feel food is
of poor quality
There is 100% coverage by SNP in Delhi, but there are a large number of concerns about
regularity and quality. Complaints about quality of food are higher than those from the
dormant states in the FOCUS Report.
“ FOCUS(Focus on Children under Six) Report is a report on a study on ICDS in nine states of India. The
states where ICDS is functioning efficiently are referred to as Active States and states where the
programme is not runnin efficiently are termed Dormant States
68
2.4 Health and Nutrition Monitoring3
2.4.1 Immunisation
Our survey finds immunization status encouraging. Beneficiaries who are accessing the
PHCs show high rate of immunization than the data represented in MWCD’s Website.
The AWW’s interviews confirm that in 97% projects, immunisation is happening in
Primary Health Centres and Dispensaries.
Table 8: A Comparison between Secondary Data from the Ministry’s Website and
Neenv Findings on Immunisation Status in Delhi.
Immunization
Secondary data %
of 0-3
from
WCD years (Neenv
Ministry(in per Study)
old
centages)
children
%
of 3-6
years (Neenv
Study)
old
children
BCG
Polio
DPT I
DPTII
DPT III
Measles
MMR
TT to PL
Vitamin A
87
79
71.7
98
88
98
98
97
94
68
78
98
88
98
98
96
86
49
%
of
Pregnant
ladies
(Neenv
Study)
88
17.1
25%
Comment: NFHS data shows that the percentage of fully immunized children in Delhi
has declined in NFHS HI from NFHS II whereas the above Table indicates that coverage
of immunization is good.
•
•
AWC-PHC Linkage
Immunisation mostly done by ANMs - 85% of the immunizations are done by
the ANMs. in Primary Health Centres and Dispensaries. This is good news for
campaigns involved in universalisation. It also underlines the role played by
AWC-PHC linkage in this matter.
Discrepancy between data provided by AWWs and that by beneficiaries: The
ten children whom we have followed all had their immunization done and the
parents had immunization cards. 87% AWCs had data on immunization for the
children below 3 years and 67% for the 3-6 year old children. 46% reported TT
immunization of pregnant women where as the beneficiaries’ data shows 88%
pregnant women are immunized. 88% of beneficiaries said that they have
received iron tablets from PHCs. The AWWs records, however, have no data on
' Secondary data and literature survey on this in Annexure - V
•
iron tablet distribution which indicates that the AWWs records are not updated or
there is a gap in linkage.
Coverage of Vitamin A distribution - Data on Vitamin A distribution is
available in 9% of the centres but the survey on beneficiaries reveals that 25% of
the children below 6 have received Vitamin A. This shows that though
immunization is good, Vitamin A distribution has remained low.
2.4.2 Weighing and Growth Monitoring
Most of the centres shared the weighing machines, as they either did not have the
weighing machine or the place to keep it. The data on weighing was not
encouraging.
The table below compares the information given by AWWs and beneficiaries’ on
weighing
Table 9: Weighing of the Beneficiaries as per Information Provided by the
AWWs and the Beneficiaries
Dormant
per Active
As
per As
Item
Focus
Focus
AWW’s
beneficiary’s
survey______ states
states
survey
82%
25%
47%
% of 0-3 years children 81%
weighed_________
25%
% of 3-6 year old 68%
children weighed
0.9%
% of Pregnant women 1.2%
weighed
The Table reveals neglect of growth monitoring and interventions for malnutrition
and support to pregnant women. Our survey finds an average attendance of 3
pregnant and 3 lactating women per centre. Only 9% pregnant women are
weighed.
Among the ten children followed for five to six months for the case studies, 5 of
them had not been weighed during these six months. The sixth child (who
migrated to UPas a result of his father losing his job due to sealing drive in Delhi)
also was not weighed. The reason given was non-availability of weighing
machine or the weighing machine was not in working condition. Out of these 10
children, one nineteen-month old child suffered from calcium deficiency. He had
received intervention at the PHC. Another 5-year old girl, who is weighed every
three months is only 14 kgs at the age of 5 years, whereas the average weight of
an Indian girl at the age of 5 years should he 17.7 kgs. The child is yet to receive
any intervention on malnutrition. Another four-year old child who is weighed
regularly is only 11 kg. She is in Grade II of malnutrition and is treated at the
MCD Centre. She is also identified as an anaemic child and has been given blood
at the MCD hospital.
Issues of Data Discrepancy: There is a serious question about the accuracy of the
records on weighing kept by AWWs and also about the figures quoted by the government
on malnutrition.
Another issue very closely connected to this is the issue of maternal health. Anaemic,
underweight mothers give birth to low birth-weight babies who carry the inheritance of
undernutrition forward. Only 38% mothers as per NFHS III 4 have consumed IFA for 90
days during their pregnancy. Around 30% pregnant women suffer from anaemia. These
are alarming figures. From our findings too, it is clear that the SNP and health
components of Delhi AWCc are not supporting the pregnant women in breaking this
vicious cycle of malnutrition. This indicates that the probability of giving birth to a low
birth weight baby also goes unaddressed. The saga of intergenerational legacy of
malnutrition continues...
2.4.3 Malnutrition
•
Data on malnutrition: When we come to the primary data on malnutrition it
seems to endorse our inference that weighing has actually not occurred. One of
the best AWCs surveyed in Kanjhawala project had data on III rd and IV th grade
malnutrition, while among all other centres surveyed, only 4 centres had data on
grade III and IV malnutrition. 17% of the centres had data on Grade I and 17% on
Grade II malnutrition and only one centre has offered medical intervention and
around 9% offered double SNP to the malnourished children. 55% of the projects
of the 27 projects covered could not provide us with any data on malnutrition at
all. This raises doubts about the accuracy of the number of malnourished children
quoted by Delhi Government.
•
Coverage of the issue in AWW’s training programmes - Out of the 242
AWWs interviewed, 27% had special training on AIDS but only 18% on nutrition
•
Monitoring and supervision mechanism: The monitoring and supervision
mechanism of the scheme demands data on malnutrition from both the AWW’s
report as well as the CDPO’s report. However, that the absence of data for so
many projects goes unnoticed is a proof of negligence in the monitoring
mechanism of malnutrition for the children of the capital.
•
Awareness of beneficiaries on nutrition needs of the children: The focused
group discussions, large number of beneficiaries sharing SNP with other family
members and indifference about the quantity of SNP served shows the lack of
awareness on nutrition needs of children.
The sessions on Nutrition and Health Education also have not been able to
generate much informed participation within the community. The mothers who
participated in Focus Group discussions are largely unaware of the issue of
4 The status of children under six as per NFHS III data is given in Annexure 4
malnutrition. They are irregular participants in the NHE meetings and their lack
of awareness has never been consistently addressed.
2.4.4 Children with Disability and ICDS
In our survey we have not come across even one AWC with a child with disability. Only
2.89% AWWs had special training on Disability. Inclusion of children with disabilities is
national mandate. The system in ICDS does not stress importance of fulfilling this
mandate.
2.4.5 Support of Senior Functionaries such as MO and ANM
84% of AWWs have said that the MO had not visited the centre for more than six
months.
ANMs are more regular visitors. 51% of them visit centres once a month. But as
per the AWW’s experience only 28.5% have been supportive.
•
•
2.5 Pre School5
•
Attendance of AWWs and children:We were unable to interview 11% of
Anganwadi Workers despite making three visits to each of these centres. Out of
the rest 89% anganwadis, 43.38% centres had no children for pre-school on the
day of the survey (the entire survey lasted 8 months). There were no children in
105 out of 242 centres on the day of survey
Table 10:Attendance in Pre-School
Boys
Girls
Total
Registered
as
per
AWW’s
record
Average no of
children
registered per
centre
4234
3930
8164
16
15
31
5 Secondary data available in Annexure - VI
Attending
as per the
attendance
recorded
by
the
surveyor
on the day
of
the
survey
1746
1618
3364
Average
no
of
attending
children
per centre
7
6
13
•
Discrepancy between recorded attendance and attendance observed: An
average of 14 children was observed attending the centres for pre school
education. There was a dismal average of 14 children attending per centre The
attendance register in more than 70% cases show attendance varying from 5 to 20
children on the previous day but 43.38% centres recorded no attendance on the
day of the survey.
•
Availability of space to carry out Pre School activities -57.83% Anganwadis
reported space constraint for activities. Most of the AWC did not even have the
place where 40 children can be made to sit. Focus group discussions have even
brought out that some days classes are carried out in open spaces as there is no
place within the centre. It has come out very strongly during our meetings with all
functionaries and beneficiaries that the major sufferer for inadequate space,
infrastructure and aids has been preschool education.
•
Learning needs of 0-3: None of the Anganwadi gives any ECCE inputs to
children below 3 years of age. The mothers are also not given any inputs on
stimulating exercises for children below three years of age.
Chapter 4
Role of Functionaries and Issues Pertaining to their Role
3.1 The Anganwadi Worker6
The Anganwadi is the place through which services reach the beneficiary families of the
community and the AWW is primarily responsible for service delivery. She is the link
between the community and ICDS, the health functionaries and ICDS and also between
primary education and pre school education. The AWW has perhaps the most important
role in service delivery of this largest government programme for children below six
years. She is largely responsible for service delivery of the components, which are
directly linked to protecting the survival, protection, development and participation rights
of children below six years. Her roles and responsibilities are defined* on the website of
Women and Child Development Ministry
Background and Training - Of the 242 workers interviewed, 33% are in the age group
of 30-40 years and, 46% in the age group of 40-50 years. 32% of the 242 A W Ws are X th
pass, 40% XII th pass and 28% are graduates. 93% have received job training and 82%
have received the week-long refresher course. Apart from that 10% are trained on RCH,
27% on AIDS and 18% on nutrition.
6 Role of AWW in Annexure VII
Ad hoc Status -This functionary has a long list of responsibilities but she does not enjoy
an employee status. She is hired on an ad hoc basis and receives a fixed honorarium of
Rs. 1500 per month. One of the AWWs we met during our FGDs said, “The scheme is
“sarkari”(government), all functionaries except us are “sarkari”. We are the only ones in
this scheme which is “gair-sarkari”(private)”
Late payment of honorarium -There is no security of job. The payments do not come
regularly. Although she is accountable for her regular attendance 96% of the AWWs
interviewed said they are not receiving payment in time. This is a serious issue as the
Worker does not feel motivated to come to the centre everyday. We have come across
workers who feel that since the government is not serious about paying their honororium
every month, they also do not feel the commitment towards coming to the centre
everyday. The Anganwadi Workers de-motivation contributes significantly towards low
quality and irregular (other than SNP) service delivery of the AWCs.
Lack of support - During discussions, the anganwadi workers said that they have to buy
registers with their own money; some have to buy earthen pots and Mayur Jugs for
storing water for the children. Sometimes the AWWs have paid rent to get rid of the
landlord’s harassment. Due to non-permanent status, low wage and irregular payment the
AWWs are not a motivated lot, although they feel that they are respected within the
community.
Extra Responsibilities: All of them during the survey and during the discussions
complained that they have extra responsibilities. These responsibilities include giving
polio drops (a small payment is given for this task), carrying out surveys for widows
pension, poverty survey and all information related to schemes concerning women and
children. As the priority has always been on these surveys, the activities of AWC apart
from SNP distribution take a back seat during these days.
Level of support the AWWs have received from other functionaries and community.
• 14% have expressed that they have received support from CDPOs
• 40% from beneficiary families
• 12% have received support from mahila mandals
• 6% from local MLAs.
• All the AWWs have expressed that they have received support from the
Supervisors and ANMs.
Irregularity in attendance of AWWs: Our survey started in March 2006, before that,
our research investigators visited centres and found mainly only helpers. She is there to
distribute the weekly ration. However, the AWW is more regular in attendance (though
only for a short time) after cooked food has been introduced in the centre.
Hopelessness and demotivation: We observed a tone of hopelessness about the system
in the functionaries. Some even felt Delhi does not need AWCs as there is hardly any
poverty. We would however like to end this chapter in a positive note by quoting one
CDPO who felt our initiative of this study to improve status of ICDS was worthwhile as
the Scheme is very good but it is not reaching the people in its fullest capacity. She said,”
Hum log ummid kar sakte hain aur aplog kaushish kar sakte hain”
3.2 The Helper
The helpers are playing a very major role in AWCs. In most of the days the surveyors
find only the helper at the AWC distributing SNPs. As pre-school activities are highly
neglected due to multiple reasons, the helpers are present most of the time during the day
to keep the AWC functional. As per their role definition they are supposed to cook the
food. However, as NGOs are mainly distributing cooked food in Delhi, their role has
become distribution of food. They also make home visits.
3.3 Monitoring and Supervision by CDPOs and Supervisors
The mechanism of monitoring and supervision and the forms devised for monthly
reporting of CDPOs (refer to Armexure B), Supervisors and AWWs as per the scheme is
comprehensive enough. Yet we observed gaps in the status of monitoring.
Lacuna in the chain of supervision:The first lacuna we observed is that the chain
between CDPO, Supervisor and Anganwadi Workers is not functioning properly.
• 66% of AWWs said the CDPOs have not visited the centre for more than 6
months
• 14% have said that they have received support from the CDPO.
Too many centres to supervise: The Supervisors is the functionary who is giving
support to the AWW on a regular basis. From our Focus Group discussions, we found out
that there are many CDPOs who are willing to provide the support to the Scheme but as
they have too many centres (the norms is 100 centres, but in more than 80% cases the
average number of centres supervised by the CDPO was more than 120) to supervise they
are not able to do justice to their responsibilities (some were supervising more than one
projects). The chain of supervision breaks down here.
There are supervisors who are monitoring more than 50 centres (20-25 is the number
specified by the ICDS norm). We have met supervisors who were monitoring 80 centres,
which means they are monitoring almost the same number of centres (100) specified for
CDPOs. Hence the centres remain unvisited and records unchecked. During group
discussions we also heard that Supervisors are given election duties and other office
duties for a long period of time. Hence they are forced to ignore their roles as ICDS
Supervisors and give their ad hoc roles a priority.
The Anganwadi worker hence remain largely unsupervised. We were unable to meet
AWWs in 28 centres in spite of making three visits.
Lacunae in monitoring record keeping: Absence of malnutrition data in all 10 centres
surveyed in 15 out of 27 projects shows that record keeping has gone unsupervised. With
a 63% prevalence of anaemia among Delhi’s children, this negligence cannot be justified
in any way.
Our survey started in March 2006, before that, our research investigators visited centres
and found mainly only helpers. She is there to distribute the weekly ration. The AWW is
more regular in attendance (though only for a short time) after cooked food has been
introduced in the centre.
Hopelessness and demotivation
We observed a tone of hopelessness about the system in the functionaries. Some even
felt Delhi does not need AWCs as there is hardly any poverty. We would however like to
end this chapter in a positive note by quoting one CDPO who felt our initiative of this
study to improve status of ICDS was worth as the scheme is very good but it is not
reaching the people in its fullest capacity. She said,” Hum log ummid kar sakte hain aur
aplog kaushish kar sakte hain”
Chapter 5
Role of the Community and their Participation
Community participation is an important component in the design of the ICDS
Programme. All through the data collection and focus group discussions the study team
examined the status of community participation.
Community Participation
During our survey we have found community participation is confined to the parents of
the child beneficiaries. They at times help in food distribution and in providing drinking
water to the centre. But this group of people has remained mainly non-participatory. The
community mainly looks at AWCs as a food-distributing centre.
Awareness of the Community:The mothers do not participate regularly in the Mahila
Mandal meetings. The Nutrition and Health Education (NHE) meetings have sensitized
the community on some aspects of nutrition but the mothers are largely unaware about
malnutrition, anaemia, growth monitoring and the role of nutrition in improving health
conditions. To be precise, the community is largely unaware about the objectives of the
scheme and the rights of their children attached to it.
One of the major gaps we noticed is that the community is not aware about the basket of
services offered through AWWs and the objective of the scheme. The lack of information
on the scheme and sensitization on issues of children have has led to lack of constructive
interest and demand for quality services. Lack of knowledge on a scheme which has been
in existence for 32 years can only be explained by lack of interest from both the
community’s and the functionary’s side.
Involvement of community members: The 242 AWWs interviewed said that 40%
centres have received support from the beneficiary families. Only 6% centres said the
local MLA has visited the centre and 10% have received support from the local Pradhan.
Absence of interest of local leaders and non-empowered beneficiaries together are
responsible for low demand and participation from the community.
The focus group discussions endorse this finding. The lack of interest of the community
leaders like MLAs, Ward Councillors and Pradhans indicate that the negligence
happening in service delivery of ICDS is actually not a factor in the voters mind and
plays no part election campaigns. Prevalence of anaemia ( 63% among Delhi’s below 3
children), malnutrition (30% of Delhi’s children are born underweight), low participation
of children in “informal” preschool education, has not become part of the political
agenda.
The MLA we interviewed felt that his area (Karol Bagh) did not require anganwadi
centres. He felt that AWCs are more relevant for villages. Delhi requires proper a survey
and relocation of centres according to need. He had not spent any amount of his
development fund on AWCs.
Howerver, in the entire study one project stood out as an exception. The community in
Khajhawala Block took an active interest in AWC and is an example of the difference
community participation and interest can make to the functioning of the ICDS
programme. However, it may be noted that the economic status of this communitry was
better than in most of the other areas studied
Role of Community in making the Anganwadi function in Khanjhawala Block.
The community in Khanjhawala has shown great initiative and come forward on their
own to help the Anganwadi worker. This was the first AWC that the Study Team found
running well. Despite the problems of low budget, irregular supplies etc., the community
were able to assist the Anganwadi worker to run a lively Anganwadi with good activities,
clean environment, personal hygiene of children, up-to-date records, mother’s meetings
etc.
The above reveals the potential ICDS has of fulfilling Child Rights when local
communities come forward and take an interest.
New Resettlement Colony: Status of AWC
Bawana was chosen as part of the study initially to examine the difference between
ICDS and non- ICDS areas. However, it was found that the newly relocated families had
succeeded in having AWCs opened after a tough struggle. The study team was therefore
able to look at the functioning of newly opened AWCs.
The Bawana AWC was found to have been handed over by the government to NGOs.
This provided the team an opportunity to look at the advantages and disadvantages of
NGO-run ICDS centres which was introduced by the state in 2006.
Our survey findings are not very encouraging regarding the status of implementation,
monitoring and supervision of AWCs run by NGOs. NGOs involvement may not actually
result in quality improvement.
The AWC in Bawana are all functioning under NGOs since November 2006 and they are
providing SNP and pre school facilities to 20-25 children between 3 to 6 years. There are
no health services provided by ICDS and no linkage with health departments. The
beneficiaries access nearby hospitals independently for health check ups and
immunization. The nearby two centres we visited did not have any teaching aids and did
not wear a neat and tidy look. Moreover the only group of beneficiaries is the twenty
children in the age group of 3 to 6 years.
From the above it is evident that the system of NGO run AWCs as observed from the
Focussed Group Discussions conducted in NGO run AWCs have problems and needs to
be looked at very carefully as once an NGO takes over the running of the AWC, the
government brushes off a major part of its accountability. Moreover, the community does
not appear to express its dissatisfaction as NGOs are considered a private domain. Not
much had been done to sensitise the community on the programme. The NGOs role as
implementers of the programme has actually eliminated the role of the community as a
partner and advocate.
c
- Media
 10182.pdf
10182.pdf
Position: 596 (21 views)