TRAINING COURSE FOR HEALTH WORKERS IN COMMUNITY HEALTH MEDICINE
Item
- Title
- TRAINING COURSE FOR HEALTH WORKERS IN COMMUNITY HEALTH MEDICINE
- extracted text
-
4
RF_COM_H_32_SUDHA
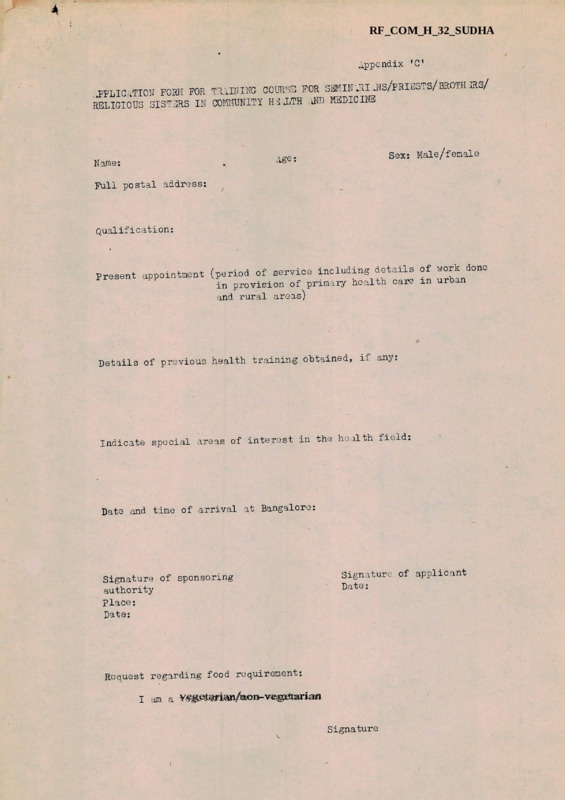
Appendix ’C*
----------- 3EMIN ^1.J(S/PRII3STS/BROTH JRS/
J?PLIC kTION FORM FOR TRAINING COURSE FOR S.
..i ND MEDICINE
RELIGIOUS SISTERS IN COMMUNITY
C----------
Sex: Male/female
Age:
Name:
Full postal address:
Qualification:
Present appointment (period of"* service including details of work done
in provision of primary health care in urban
and rural areas)
Details of previous health training obtained, if any:
Indicate special areas of interest in the health field:
Date and time of arrival at Bangalore:
Signature of sponsoring
authority
place;
Date:
Signature of applicant
Date:
Request regarding food requirement:
I am a vegetarian/non-vegetarian
Signature
r'V hl 3^^
o?T“s
ST JOHN’S MEDIC kL COLLEGE /IND ITS HOSPITALS^
=-=-=-.-
1. Venue;
St John’s Medical College and Hospitals
2. Faculty;
i. Dean, St John’s Medical College
ii. Hospital Administrator and staff of
St John’s Medical College Hospital (SJIdCHJ
iii. Staff of Depts of Anatomy, Medicine,
physiology, Surgery, paediatrics,
Obst & Gynae., Orthopaedics, Dermatology,
ENT, Opthalmology and Psychiatry
iv. Staff of Dept of Community Health and
Ross Institute Unit of Occupational Health
v. Medical Officer in charge of Primary
Health Centre/Units at Dommasandra
and Mallur
vi. Visiting Lecturers from the Indian
Institute of Management, Bangalore,
Govt. Health and other Departments,
Natural Family Planning Unit and
St John Ambulance Brigade
5. Programme Director:
Major General B Mahadevan, PVSM 1VSM
Director of Rural Health Services and Training
Programmes, St John’s Medical College Hospital
4. Duration of Course:
12 weeks (72 working days)
5. Course Components:
i. Concepts of Community Health C-are total health care, maternal and child
health, family welfare, nutrition and
food hygiene, environmental sanitation
including village and home sanitation,
health education, control of communicable
diseases
ii. Clinical sessions in management of common
problems and emergencies in Medicine 9
Surgery, Paediatrics, Psychiatry,
Orthopaedics, Obst & Gynae both in the
hospital and community. Treatment of
common ailments with simple drugs.
iii. Organization and management of health
services — simple techniques involved
in the delivery of Primary Health Care
to individuals and community. Maintenance of
medical records - basic concept of health
economics- social security - health
legislation
6. Course Capacity
Date of commencement
84 Date of completion
25
April
1978
June 24, 1978
I
:3:
(g) Participate in community development activities by
discussing community problems with local leaders and
working out solutions for improving the quality of
life of the population
(h) Refer to appropriate centres all cases and problems
outside or above his/her competence
(i) Maintain basic medical records of vital events (births
and deaths in the community)
3. Course Components
A programme of lectures/group and trainee/staff discussios,
visits, practical sessions and films on community
clinics, field
:
health subjects as per attached appendix ‘’A' & ’B*. The whole course
is designed and spread out over a period of 12 weeks of which 3 weeks
will be at the urban location and 9 weeks at a rural set up. While
certain topics and training will be imparted at St John’s Medical
College and its Hospitals, most of the subjects pertaining to
community health matters will bo dealt with in the rural field
centres, where it will be possible to expose the trainees to problems
and various approaches in community health. Participants will be
involved in practice of actual procedures like immunizations,
disinfections, conduction of antenatal and under five clinics and
treatment of patients for common complaints with simple drugs. The
acquisition of basic knowledge, attitude and skills will receive
full attention throughout the course. Time will be given for
participants to speak, so tha>t the faculty gets to k.now their problems
and find solutions to the same. Their active participation at all
stages will be ensured.
4. Registration
All candidates attending the course will duly fill in the
attached proforma (Appendix ’C’) and mail the same along with boarding
and lodging charges for the period of the entire course in favour
of Bean? St John’s Medical College, through their Biocese, before the
end of March 1978.
5. Boarding and Lodging
Wwill be provided at St John’s Medical College Hostel/Hospital
at the following rates:
Room - Rs.5/Meals etc. - Rs.?/-
(The duration of the course will be for 12 we^ks)
6. Transport
Transport for trips between the college and hospitals and
for field visits to rural areas, will be provided for tne participants
and accompanying staff members.
7, Library facilities, teaching aids and equipments
The course participants may use the library during the
duration of their stay. Loan cards for reference in the library will
:4:
The necessary teaching aids and equipments available
in the hospitals and in the Depts of Anatomy, Physiology, Pathology,
Microbiology, Preventive and Social Medicine of St John’s Medical
College will be made use of.
8. Venue
For all lectures/discuss!ons/films shows will bo in
room nos. 116, 117 of the ground floor and 241 of the first floor of
St John’s Medical College.
Clinics will be arranged at S.JMCH. Suitable plaxes will
be earmarked for teaching at the various rural health centres and
Action Group Areas.
9. Expenditure
Expenditure incurred on transport, audiovisual equipment,
stationery and faculty time is expected to be Rs.900/- per participant
for the entire course and must be paid in advance along with the boarding
and lodging charges.
N.B.
During the course, summer conditions will prevail in Bangalore
temperature varying from 16 deg C« to 55 deg C* Summer clothing
will suffice. Candidates are requested to bring mosquito nets,
bedding and linen*
Appendix IAI
SUmftRY OF CONTENT OF | FftRNING OF COmilUITY HEALTH UORKER
(Mainly extracted from the Manual for Community Health
Worker issued by Ministry of Health and Family Welfare,
New Delhi)•
1. Malaria
a. Identify fever cases
b. Make thick and thin ^lood films of all fever
c. Send the slides for laboratory examination
d. Administer presumptive treatment to fever cases
e. Keep a record of the persons given presumptive treatment
•
■ •
-names
ar)cj
addresses of cases
i—----------f. Inform the Health Worker
(Hale)\ of- the
from whom blood slides have been taken
g. Assist the Health Worker(Male) and the spraying teams in spraying
Assist the } ----- .
and larvicidal operations
h. Educate the community on how to prevent malaria
2. SmanJinx.
of fever with rash and report them to the Health
a« Identify cases
Worker (male)
b.
Inform the Health Worker of infants aged zero to one year requiring
primary vaccination as follows?
i. In the intensive area inform the Health
Worker(female)
li.Hn the twilight area inform the Health Worker(male)
Assist the Health Worker (male/female) in arranging for primary
c.
vaccination
.
d. Follow up cases who have been given primary vaccination
primary
vaccination
the
of
importance
e. Educate the community about 1 ...
3. Communicable,
^is.eases.
Inform the Health Worker(male) immediately an epidemic occurs
in his/her area
b. Take immediate precautions to limit the spread of disease
c. Educate the community about the prevention and control of
a.
communicable diseases
4. Environmental sanitat.ion_^and_j?ersonal_jT
i§ne_
a. Chlorinate drinking water sources at regular intervals
- record of the number of wells chlorinated
b. Keep a
c<. Assist the Health Worker ( male) in arranging for the
const)ruction of the following?
i. Soakage pits?
iii. Compost pits;
v. Smokeless chulhas
ii. Kitchen gardens
iv. Sanitary latrines
d. Educate the community about the followings
i. Safe drinking water
ii. Hygiene methods of disposal of liquid waste
iii. Hygienic methods of disposal of solid waste
iv.
vvi.
vii.
viii.
ix»
Home sanitation
Kitchen gardens
Advantages and use of sanitary latrines
Advantages of smokeless chulhas
Food hygiene
Control of insects, rodents and stray dogs
:2:
5o
Immunization
a. Assist the Health Worker(male/Female) in arranging for
immunization
b. Educate the community about immunization against diphtheria,
whooping cough, tetanus, smallpox, tuberculosis, poliomyelitis,
cholera and typhoid
6. Family planning
ao Spread the message of family planning to the couples in
his/her area and educate them about the desirability of the
small family norm
b. Educate the people about the methods of family planning which
are available
c. Act as a depot holder, distribute nirodh to the couples and
maintain the necessary records of nirodh distributed
d. Inform the Health Worker(male/female) of those couples who
are willing to accept a family planning method so that he/she
can make the necessary arrangements
e« Educate the community about the availability of services for
Medical Termination of Pregnancy(MTP)
7. Maternal and child care
a* Advice pregnant women to consult the Health Worker( female)
or the trained dai for prenatal, natal and postnatal care
b. Advise pregnant women to get immunized against tetanus
Co Educate the community about the availability of maternal and
child care services and encourage them to utilize the
facilities
d. Educate the community about how to keep mothers and children
healthy
8. Nutrition
a.
Identify cases with signs and symptoms of malnutrition among
pre-school children (one to five years) and refer them to the
Health Worker (male/female)
Identify cases with signs and symptoms of anaemia in pregnant
and nursing women and children and refer them to the Health
Worker(male/female) for treatment
c. Assist the Health Worker(male/female) in administering vitamin A
b.
solution as prescribed to children from one to five years
of age
d. Teach families about the importance of breast feeding and the
introduction of supplementary weaning foods
e. Educate the community about nutritious diets for mothers and
children
9* Vital events
a. Report all births and deaths in his/her area to the Health
Worker(male)
b. Educate the community about the importance of registering all
births and deaths
10- £i£st aid in emergencies
ao Give emergency first aid for the following conditions, refer
these cases to the Primary Health Centre as necessary and inform
the Health Worker(male/female)
If Drowning?
ii. Electric shock
vi.
.Insect stings;
v. v». Scorpion sting;
viii. Accidents
vii. Dog bite;
b. Carry out procedures in dealing with accidents
c. Keep a record of first aid given to each patient
11. Treatment of minor ailments
a. Give simple treatment for the following signs and symptoms
and refer cases beyond his/her competence to the Subcentre
or Primary Health Centre
i.
iii.
iv.
vi.
viii.
x.
xii.
xiii.
Fever;
ii* Headache;
Backache and pain in the joints
Cough andcold
v. Diarrhoea;
Vomiting
vii. Pain in the abdomen
Constipation
ix. Toothache;
Earache
xi. Sore eyes
Boils, abscesses and ulcers
Scabies and ringworm
b. Keep a record of the treatment given to each
patient
12. Mental Health
a. Recognize signs and symptoms of mental illness and refer
cases to the Health Worker(malc/fomalo)
b. Give immediate assistance in emergencies associated with mental
illness
c. Educate the community about mental illness
13. Community Bevelopment
s
a. Block Developmental activities
b. Extension
IEducation
c. Agriculture, Pisciculture, Veterinary and live stock
d» Transportation
i
*
Appendix ’B’
PROGR.OTIB FOR TRAINING 0? SH-IIIURI JTs /p RIESTS/b ROTHSRS/ r ELIGIOUS
SISTERS IN COMMUNITY HE -LTH .JTO MEDICINE, ORG.JJIZED BY ST JOHN'S
MEDIC IL tOLLEGE
FIRST
B1Y
9.00 an to 12 noon
1.00 pm to 4x0Q„pm
MONO l Y
Inauguration, Registration and
pro-evaluation
St John’s Medical College (SJMC)
TUaSPAY
Common ailments - Out Patient
(MedAcal)
St Martha’s Hospital (SMH)
Anatomy
Physiology
n
H
First
Aid
H
WEDNESDAY
-do-
ii
THURSDAY
-do-
ti
it
I!
n
it
it
FRIDAY
SATURDAY
Common ailments - Out Patient
(Psychiatry) ‘
SMH
it
Group discussions on common
ailments - SMH
SECOND WEEK
DAY
9.00 am to 12 noon
1.00 pm to 4.00 pm
Common ailments - Out patient
(ent ) - SMH
.anatomy
TUESDAY
Common ailments - Out patient
(Oph) - SMH
First .lid lecture demonstration
WEDNESDAY
Common ailments - Out patient
(Surg/Ortho) - Accidents
MOND l Y
SMH
Physiology
First Aid
Population Dynamics and Family
Planning (Natural Methods)
THURSDAY
Common ailments - Out patient
(Dermatology) - SMH
1.00-2.30 pm
.jiatomy Test
PT?IDiy
Con'.wn ailments - Out patient
(Obst & Gynaec) - SMH
First Aid test
S iTURDAY
Group Discussion
3.00-4.30 pm
Physiology Test
2
: 2:
THIRD IJEEK
TOPIC
DAY
General management of patients - Home Nursing St John’s Medical College Hospital (SJMCH)
MONDAY
Lecture Demonstration at SJMCH
TUESDAY
Multiple etiology
OJ' of diseases
economic ------factors
Role of socio-c—---in health and disease
WEDNESDAY
Visit to Community Development Block, Yelahanka
THURSD lY
Visit to Poultry, piggery, Fishery etc.
FRID kY
Visit to Poultry, Piggery, Fishery etc.
Group Discussion (socio-economic aspects and heapth)
SATURDAY
FOURTH 5/EEK
- (RURAL HEALTH CENTRE)
TOPIC
D kY
MONDAY
Introduction to Rural Health - role of Health Care Administration, Organization and Functions
Health and Environment (introduction) - and survey and
discussion
TUESDAY
Water supply and waste disposal - survey and discussion
T/EDNESDAY
Insects, rodents and live stock - survey and discussion
THURSDAY
Industries
FRID kY
Housing and accommodation
SATURDAY
Survey of major resources and facilities for health
and welfare
- survey and discussion
survey .and discussion
FIFTH DnSEK
- —=-2^2^-=-=-=-=-=-=-=
MONDAY
Introduction to Maternity and
Child Health
Maternity and Child Health
Services and Components*
TUBSD vY
Survey of antenatals
Registration
WEDNESDAY Survey of .antenatals
Registration
THURSDAY
intenat il Clinic
Discussion
SIXTH WSEK
/
OTERNOON
MORNING
DAY
MONDAY
Water borne diseases
(brief introduction)
Survey of drinking water wells
TUHSDa Y
Disinfection of water in
wells
Discussion
WEDNESDAY
Faecal borne diseases
Survey of latrines and methods
of waste disposal (manure pits,
compost etc)
-do-
-do-
THURSDAY
FRIDAY
Laboratory examinations
of urine and faeces
SATURDAY
Group discussions
Analysis of findings
SEVENTH 1-IEEK
TOPIC
D..Y
MONDAY
TUESDAY
WEDNESDAY
I
THURSDAY
FRIDAY
SATURDAY
5
Relation of food and nutrition with health
(Topics: Introduction, balanced diet, energy require
ments, dietary patterns, infancy (well fed and ill
fed), pregnancy, lactation, cocking and culinary
practices, food hygiene and food borne diseases,
malnutrition and under nutrition, education on
nutrition and national applied nutrition programme
<, films, discussions etc
survey, lectures, dciaonstration
<-------
EIGHTH WEEK
DAY
afternoon
MORNING
MOND i.Y
School health - introduction
Visit to school and check up
of environmental factors etc
TUESDAYS
Immunizations - procedures
and practice
Visit to School and other
community he ilth organizations
T'JEDNESDAY
-do-
THURSDAY
-do-
-do-
FRIDAY
-do-
-do-
SATURDAY
Group discussions -
-do-
:4:
NINTH Wi£EK
.JPTERNOON
MORNING
DAY
Education in community,
Personal hygiene, diarrhoea,
vomitting
MONDAY
Clinic - study of common
diseases and treatment
TUESDAY
-do-
Pregnant women, lactating
mother
WEDNESDAY
-do-
Diet and nutrition
THURSDAY
-do-
Diet and nutrition
FRIDAY
-do-
Scabies, leprosy etc.
SATURDAY
Group discussion on common diseases and their treatment
TENTH TJEEK
TOPIC
DAY
J
MONDAY
TUESDAY
WEDNESDAY
THURSDAY
FRIDAY
SATURDAY
I
jj Morbidity enquiry in the community - Drugs & Treatment
ELEVENTH
TOPIC
DAY
MONDAY
TUESDAY
WEDNESDAY
THURSDAY
FRIDAY
SATURDAY
Assignment of studies and data collection -
5
5
analysis and report writing
TWELTH WEEK
TOPIC
DAY
MONDAY
TUESDAY
WEDNESDAY
THURSD kY
FRIDAY
SATURDAY
i
$ Visit to Primary Health Centre - Study of structure
y and functions, job responsibilities
Group discussion on primary health centre
Appendix rC’
JPLIC '.TION FOBM FOR TRAINING COUR'S FOR SEHIN ARI. JSTS/PRIISSTS/BROTH ats/
RELIGIOUS SISTERS IN COMMUNITY H3iTH JTO MEDICINE
Sex: Male/female
Age;
Name:
Full postal address:
Qualification:
Present appointment (period of service including details of work done
in provision of primiry health care in urban
and rural areas)
Details of previous health training obtained, if any;
Indicate special ireas of interest in the health field:
Date and time of arrival at Bangalore:
Signature of sponsoring
authority
Place:
Date:
Signature of applicant
Date:
Request regarding food requirement:
I am a vegetarian/non*vegetarian
Signature
dept of community medicine
st johnts medical college,
BANGALORE 560034
Date:
INTERIMS POSTING
Name of intern,:
Date of duty report at the Dept of Community Medicine:
The above intern is posted for training at the following
Centres and Institutions for the period shown against each. The intern
will report himself/herself for duty to the Officer-in-Charge of the
Centres/lnstitutions. Detailed instructions will be issued separately.
(Maj Gen B Mahaaevan PVSH AVSM)
Professor and Head of the Dept of Cocuunity Medicine
L„LRURALTo
31. Institution x>r Centre] From
No_..
1.
Mallur
2.
Siluvepura
URBAN
From
To
Remarks
Uttarahally
4.
Action Group Area:
5.
Student Health
Service
plannins
6-
=-<=—=—=— .l.=—=—=—5:—=—=—=—1=—=—=—=—=
7. National Tuberculosis
Institute
8.
9.
10.
cc to: 1.
The attendance of the interns with their dates of relief at
Centres may be despatched along id.th other technical, project and
administrative reports etc., etc.
2. Intern's file
Februaiy
, 1978
Tour Lordship,
Sub: Training of Seminarians/priests/Brothers/
Religious Sisters
in village level health work
Ref: Correspondence resting with my letter
NO.3/BC/5048/77 dated August 17, 1977
I am attaching herewith a copy of the programme we have arranged
for training of seminarians/priests y^^brothers/religious sisters
in Community Health and Medicine. The programme includes organizational
details. I hope the schedule meets the requirement.
//We will undertake this training course more as a pilot project
and consider the feasibility of conducting more three months courses
at Bangalore for various dioceses in India* Once a nucleus of Communiy
Health Workers is built up, refresher courses could be conducted at
other centres in India.
//We should also, in due course of time, consider the feasibility
of building up a cadre of teachers in Community Health and Medicine
by organising suitable teacher training programmes at Bangalore, for
selected supervisory staff of dioceses including doctors and nurses.
Such trained teachers could then assist the mobile teams from this
college and hospital in running refresher courses for their community
health workers^from time to time.
//if the dates scheduled for this course disapproved, participants
may please be asked to comply with the organizational instructions
contained in the same. Selection may be made from amongst persons who
are motivated and dedicated to serve, especially those who are already
serving in peripheral areas.
//With best wishes,
Yours sincerely.
(CM Franc: e MBBS PhD)
Rt Rev Patrick D*Souza
Bishop of Vamasi
Bishop's House
45 Varanasi 221002
■?r
/
MINUTE SHEET
Ref: P.U.C. (1)
Placed opposite is the letter
addressed to Rt Rev Patrick D»Souza,
Bishop of Varnasi, regarding training
of seminarians/priests/brothers/religious
.x
'
sisters.
For your signature please.
Director of Rural Health Services and
Training Programmes
11.2.78
Dean
’C Bangalore
©
f C^rrvx. 7T>tT>i
6e ^CLodJr UrJj^
"T^sC S
Crwi . 1
“t^eA.wx_-
‘
\Axxew$.
"^•Cxj Xaxx I^v vixo^r
C*>lWAU*AM.C4^K<rt
J 'Mj C(Ll ^4a ^<S
) 2XtzUA^e^M>9
’’T^-*^ 4“c<J^vv<-^. 4
VtxJcxA^,
| M /vLl^ 4 £ c ^aa |^
Q^ULq
iVT^uXAA-.
ft
&■
( Lv /^<x\4 <5t-^ zzx«41r J)l
UU4
^C7V^-v Aaaa -4aa -^
^Ux4kx^-^£4- VrUrxA- V-v cL-o r>4 4-«*^ 1
C^uXr/
Xu
JI _
e
.
. .
.
.-O'
i
A
v-’-^Oa ^.
(^) A^tzxg^jty^
M^VJ U-t> tJ^Z’ i CL U
b XOa ,' r>^» 6^_ AZv-JVJHC
&|>Z Xaxaa 4^-
(ViA<o (S) \ZvU^^C
v(
Li
H-ih4 4^f -n<4v4ce
WtU-<A-^V-t^ ^1
PyLtAxVet plv^Trzc^-^
cAXop^^'
/7.,
Uj
. V
’
r ~
Cx Xaj Cu A
Slc^ (<y , u-e^)^
fcu^/i *UV<
U-l
; V^tcUuo4 • TOvil^iXo
a-
^-tjvO 4-o br-C^^- c*. t
IV
z^S'K^.X.cf. (^4<
PvT|iu4L>^
Cel^U~
oLo Uax ^ Wo <4^
Uttw to }3<4rUU-i*-x«-4-
^TvC>M a
A-—
■■ V- P>*
z •
(*) (*) (*) (*) (*) (*)*(*) (*) (*) (*) (*) (*) (*) (*) (*) (*) (*) (*) (*) (*) (*) (*) (*P) (*) (*) (*) (#) ( *)
.
T
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
ST.OOHN'S MEDICAL COLLEGE AND HOSPITAL
BANGA LORE-560 034
ORIENTATION COURSE F OR COmUN IT Y H EA LTH WO R KE RS
I (*)
|
■
(*)
■(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
•
*)
<*)
(*)
(*)
(*)
(*)
<*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
*)
l K*)
[ (*)
TRAINING MANUAL
(*)■
Rjstck.
Ct/
r'lc^Ken^i
II (#)
(*)
(*)
• (*)
■
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
m
- — —... MANUAL FOR COMMUNITY
, W1, j. i |
)HEALTH
| i_f-i t_ f 11 mu
WORKER,
xtracted
from
, V\~'
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(f)
(*)
(•*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
;*)
'.*)
(*)
(*)
(*)
Tfa’lsno.
&As'fec\. ^>y
C esnfa h m
er
l-io.
ifa l-lc^ce A
a
fl i7'aha
P^o
Pref 6
far^
fj&'j'i
5/^
WbJ 6
pvtyecf
E&p^
<^CT^z»zO ^O
I
,
T^^h/STP
sxjs ^Tr-ic
7& -
> J)
5^, oh
/5o GHtJs
%
ls -j
^Ll
TVteJ^tirG
C^llC^e
Me it
/ZoP
PK a ^CfZj yi^-p kxj
Cg 11
rC L^. k
7)<^
?4e^ h^J /''Lf'chc*
ervC^
I
I
Pr^ec^
(/
tP& CV C^l'VXS)
Ou .y '
y
s
y
kl<rr->
I
<
-•- k
x*
z ■
k
(*)(
(*)
*)
(*)
(*)
*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
*)
(*)
(*)
k!.
(*)
(*)
(*)
(*)
(*)
(*)
4
■
*)(*)(*)(*)(«)(*)(*)(*)(*)(*)(*)(*)(*)(*)(*)
INDEX
Introduction - Orientation Course for Community Health Workers
I* Malaria
2. Smallpox
Communicable Diseases
4- Environmental Sanitation and Personal Hygiene
5. Immunization
6. Population and Famil^r Planning Information in India
(Booklet made available by N.F.P.A., Bangalore)
Maternal and Child Care
8. Nutrition
9. Vital Events
10. First Aid in Emergencies
11• Treatment of Kinor Ailments
(*)
(*)
12. Mental Health
(*)
(*)
(*)
(*)
*)
(*)
(*)
(*)
(*)
$(.
I
(*)(-)(*)(*)(*)(*)(-■)( ’•) (*)(*)
)(*)(*)(*)(*)(-:(-)(*)(*)(*)(*)(*)(*)(*)(*)(-x-)(^)(*)(*)(*)(*)(*)(*)('‘0(^)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
*)
(*)
(*)
:!
I
(*)
(*)
(*)
(*)
(*)
(*)
(*)
(*)
( *)
(4
(*)
(*)
(*)
(*)
(*)
■
ZT
VA 3 '2—
i
O'
O
INDO-DUTCH PROJECT FOR CHILD WELFARE
( STICHTING NEDERLANDS KINDERHULR FLAN )
6-3-885,
SOMAJIGUDA
HYDERABAD - 500004
PHONE OFF. 35938
TRAINING
PROGRAMME
I “o
GRAM
r
SVASTHIKAS
(Village Health Agents)
*
*******
*****
*
*
B y
Dr. H. W. Butt
Director , Indian Bureau
I
\
RES. 33408
TRAINING PROGRAMME FOR ’’GRAM SVASTHIKAS”
(Village Health Agents)
I
INTRODUCTION:
For
the past 5-6 years the Indo Dutch Project has been function-
i’.ig in U 7 villages ox
the Chevella Block focusing attention
health, education and nutrition.
on
For the health inputs,
the Niloufer health team has been paying regular visits twice a week to
four subcentres.
The Auxiliary Nurse Midwife experiment with
an
extra input of training in skills as well as by reducing the area
of operation of each ANM to a population of 5,000 has helped in
using this important functionary more effectively for health edu
cation, care of minor ailments, referrals, family planning, health
and sanitation with a greater emphasis on the preventive sice.
Emphasis on health education and nutrition has been stressed not
only by the ANM but also
so the balsevika and the mother
teacher s
which has resulted in a multi-pronged impact on the rural families. This experiment has now been spread to
the entire Block
und er the new Multipurpose Health Scheme.
The Project Working
Group consisting of representatives from the National Institute
of Community Development, Niloufer Health Team, Department of
Heal th and family Planning, College of Nursing, College of Home
Science, the District and Block staff reorganised the
centres of
Twenty four subcentres have been now formed to
be manned by a male and female health worker to cover a
population
of 5,000 per unit,
Six zones have been formulated with a male
and a female health supervisor to be in charge of each zone to
the entire Block.
provide guidance and supervision to the health workers in four
subcentres in each zone. This new scheme was inaugurated by the
Minister for Health, Andhra Pradesh at Shankerpalli in September
1976 when all the sixty health workers were provided newly design
ed kits with drugs by the Project in addition to the special
training organized for them by the Medical Department.
I
5 2.:
ROLE OF H-IE NILOUFER TEAM:
Instead of the regular visits to the four subcentres, the new role
of the Niloufer Team will be monitoring, training, evaluation and
on the spot guidance to the Health staff of two zone s
covering
eight subcentres manned by 16 health workers and four health supervisors covering an area of J4 villages.
the
VILLAGE LINK — GRAM SVASTKIKA:
One of the main objectives of the Project has been to encourage
local mothers to con.'o forward to take up responsibilities connect
ed with health, education and nutrition,
Local mothers have been
trained by the project totrun creches and ba1wadis as mother tea
cher s •
In order to strengthen the hands of the health workers, it
has been decided to select and train suitable village women who
have the minimum educational standards (at least 5th grade) for
one month to serve as effective assistants to the health workers of
the new scheme in two zones. After considering several names for
this village woman the Working Committee felt that the term ’’GRAM
SVASTHIKA ” would be appropriate to bring out the main concept of
a village health worker who will have complete information about
the pregnant and lactating mothers, number of malnourished children
and the details of births and deaths in the village.
This GRAM
SVASTHIKA will be expected to fill in the cultural gap that exists
between the city doctor/nurse/paramedical workers and the illite
It is planned to select 34 village vzonien to
serve in the 34 villages of the two zones after they have been
rate rural families.
trained at Shankerpalli for a period of one month.
The main role
of the GRAM SVASIHIKA will be to carry the message of health, education, nutrition and family planning to the rural families and
act as a guide providing the elementary information required for
health education so that the time of the health programmes could
be better utilised during their visits to the concerned villages.
:3»
Preference in selecting suitable women will be given to those who
have already been trained as mother teachers or indigenous mid
wives.
An honorarium ranging from Rs. 30 to 5 0/~ for parttime work
will be given to these women which will not be considered as a
salary but as an incentive for the work and interest shown by them.
FUNCTIONS:
a. The worker should have details of the names of families and
houses specially of women who are in the age
group of 15-^4;
also vital statistics (births and deaths).
b. She should make home visits on a regular basis to build up a
close rapport with the families and be informed of their welfare and supervise the under five feeding programme; indentification of malnourished children.
c. She should be able to attend to minor ailments, dressing first
aid etc. and give necessary advice for maternal and child care,
deworming, vitamin A, follow up T.B. and leprosy patients a nd
family planning.
d. She should have complete information about the programme of
doctors’ visits to the key villages as well as the working
hours of the Auxiliary Nurse Midwife/Balsevika and Craft Teacher.
e. On a routine basis she should take with her a few families to
the ANN subcentre for health checkups.
f. In case of emergency, she should inform the ANM/Health Visitor
to visit the village and also to inform the Medical Officers.
g. In case of referrals and complications,
she should accompany
the cases to the primary health centre.
She should act as a n agent for family planning and use indirect
methods to encourage families to use the proper method suitable
to them.
i . She should provide necessary information with the help of flash
cards, flannel graphs to the families in the village for health
education and emphasize on the priorities of the Project viz.,
encouraging antenatal care for expectant mothers, nutrition
and immunisation.
J•
She should be aware of the type of diseases, epidemics and any
other outbreaks in the village so that she could inform the
subcentre and the primary health centre.
k.
In addition to health, she should also
encourage mahila mandais (womenr s clubs) and balwadis
on the same lines as in the
key village.
1.
senT; L
She should act as an =,
o provide
agent
provide the
to
the necessary informa
tion about the integrated programme.
programme. The rural families should
look up on her as a guide in cases of health, education
and
nutrition.
TRAINING PROGRAMME FOR.GRAM SVASTHIKASi
Period of training: 12 working days on every Mondays, Wednesdays
and Saturdays during the period from 19th February
to 21st March
1977 excluding holidays.
Venue:
Shankerpalli, Chevella Block,
Trainers: Niloufer eHealth Team, PHC Staff, Block Staff and Specialists from the Department of Health and Family Planning,
the College of Home Science and the College of Nursing.
METHODOLOGY:
The syllabus for this course has been designed according to the
jobs to be performed by the Gram Svasthika. The following are
the units showing the weightage given to each in terms of days
and hours»
:5 i
No.of days
Units
Maternal care
2. Child care
3. First aid
1 .
4. Nutrition education
5. Health and sanitation
6. Family Planning
7. Records, reports and
vital statistics
8. Collaboration with PHC
workers and other IDP
workers in the Block
Total
No. of hours for
Theory
Practicals
4
4
1
6
6
3
6
3
3
1
3
2
2
6
1 2
36
2
2
1
2
1
2
4
2
2
24
After a brief introduction the trainers will spend more time in
demonstrations and field practicals.
Each trainee will be given
an opportunity to complete the registers and other data as group
assignments in Shankerpalli village and as individual assignments
in her own village under the guidance of the concerned multipurpose
workers.
nee along
A set of simple registers will be prepared for each trai-
with simple visuals that she could make use of in her
village .
JOB FUI’JCTIONS:
1 .
The Gram Svasthika will make frequent visits to houses in the
village, assigned to her, in such a way that each child and
each wo ma n ar e seen at least once in a month,
and that those
needing special care are seen every week.
2.
She will detect pregancies early and fill in the list of pre
gnant women, so that early care during the antenatal period and
labour can be provided.
3. She will ensure monthly sequential weighing of children atthe
time of visit by Multipurpose worker and recording of their
weights on charts for evaluation of their growth and nutrition.
4. She will maintain a list of children ’at risk’ and a list of
other persons in need of special attention.
3• She will render first aid where necessary and refer sick children
mothers and other adults to the Multipurpose Health Supervisor
: 6 :
(male and female) for checkup and treatment.
6. She will help the Multipurpose Health Worker (female) in examination
of arm-girth of children with coloured bands etc. and distribute
nutrition supplements like tablets, protein packets (Hyderabad Mix)
entrusted, if any, to her, and ensure on the spot consumption of
the material by the beneficiaries, as far as possible, either indi-
vidualljr or. in groups.
7. She will organise immunisation compaigns with the help of the
local community, and will collect children and women for immuni
sation when the Multipurpose health worker visits the place.
8. She will give nutrition education to the families based on food
materials available easily in the village ard teach them better
methods of cooking to ensure balanced diet and demonstrate the pre
paration of weaning diets and supplementary diets.
9. She will educate the families on Health and Sanitation with parti
cular reference to personal hygiene, clean drinking mter, treat
ment for scabies and other minor ailments of common occurrence.
10. She will motivate the people to plan their families and bring to
the notice of the Multipurpose health supervisors (male and female)
such cases of eligible couples as are not neadily coming forward
to accept one or
the other method of Family Planning.
It within
a fortnight of a missed period, termination of pregnancy is desired,
she will refer the case to Multipurpose worker for menstrual
regulation.
11 .
She will collect information on births and deaths occurring in the
village and maintain a record of the events.
12. She will help the Multipurpose Worker (female) in examination of
pregnant women and will distribute under guidance of the Multi
purpose Worker (female) Iron and Folic acid tablets for 100 days
possible as
from the seventh month of pregnancy or to the extent nossiblo
instructed by the Multipurpose Worke r (f emalo) .
RECORDS TO BE MAINTAINED?
1. List of regnant women
2. List of children under five
3. List of other unhealthy persons needing attention
4. ; List of births and deaths
and issue of Hyderabad Mix.
5. particulars of
---c- immunisation
received
and extent of utilisation.^-^
6. Drugs and equipment
(H.W. Butt)
y
<
DETAILED SYLLABUS FOR TRAINING OF GRAM SVASTHIKAS (VILLAGE V/ELFARE
AGENTS) WORKING UNDER THE INDO DUTCH PROJECT - HYDERABAD,
SI.No.
Name of the
Session
1 .
Ma t or na 1 Car e :
1• Antenatal care
Theory
practicals•
1. Importance of early
registration of all
Antenatal cases
1 • Prepare a lis^t
of pregnant
women
2. Make sure that
they are regi
stered by the
Multipurpose
Worker (F)
3. Ensure that they
are getting
antenatal care
2. Detailed examination
4. Take the list
of all high risk
of all Antenatal cases
cases from the
at frequent intervals
to take extra care on
Multipurpose
Worker and see
the high risk cases
that they get
special atten
tion.
3* Systematic follow un
of the cases with ad
ministration of Teta
nus toxoid Vitamin
tablets, Iron & Folic
acid tablets etc.
2. Postnatal care
5 • Act on instruc
tions of the
Muitipurpose
Worker in distri
buting Iron &
Folic Acid
tablets.
1 .
1 . Importance of watching the health of the
mother and child during:
and also after delivery
Report emergen
cies connected
with delivery
to the MPW(F)
or MPS(F) or
the Medical Of
ficer of the
PHC
2. Report all cha
nges in the
health of the
mother and chil*
to the MPW(f)
2. Taking care of the
3. Report delive
ries conducted
health of mothers deli
by local dai
vered by dais & Un
to the MPW(f)
skilled persons.
I
:2 :
3 Care of lacta
ting mothers.
2. Child Caro;
The need for nutritional
supplements to lactating
mother, the advisability
of breast feeding
1 Act on instructions
of MPW in distribu
ting iron and folic
acid tablets and
other nutrition supple
ment to lactating
mother.
2 Introduce the right
technique of breast
feeding.
1 Importance of special
care for the health of
all children under five
years of age.
1 Prepare a list of
children under five
years of age.
2 Get them registered
with MPW (F)
3 Assist the MPW(F) to
take the weight and
give the card by
charging 25 paise
2 Combating malnutrition
in children under 5
£+ Identify cases of
malnutrition with
the help of arm bands
and prepare a list
of children needing
protein packets.
3 Special care to ensure
proper growth and deve
lopment in children
5 Airange for procuring
Hyderabad Mix packets
from Mahila mandals
thro ugh the PHC Medi
cal Officer and dis
tribute these to the
needy cases as inst
ructed by the MPW(F)
4 Checking eye diseases &
defects in children
6 Prepare a list of
children needing va
rious kinds of immu
nisation & administer
oral Vitamin A once
in 6 months to cases
requiring it.
5 Preventing infections
diseases
7 Collect children for
immunisation against
infectious diseases
& particularly DPT
and Polio
6 Treatment against worm
infections.
7 Collect children for
de-worming when MPW
(F) visits the villa
ge.
:3«
3 , Fir st Aid t
1. First Aid in General
emergencies
1. Attend on cuts, burns, falls
& fractures, Dro wining-bi tes •
2 . First aid in communi
cable diseases
2. Attend on scabies/conjunctivi tis
3. Attend on fever, diarrhoea
and vomitings
3. First aid in other
minor illnesses lead
ing to de-hydration etc
. Nutrition
Education; 1• Knowledge about foods
available in villages
2. Balanced diet
Prepare a list of sick per
sons (other than under fives
and pregnant women) who re
quire special attention by
the M.P.Ws.
1 . Promote the practice of grow
ing plants of papaya and drum
stick etc.
2. Advise the families on bet
3. Supplementary and weanter methods of cooking for
i ng foods
•’l . Advice on infa nt feeding
prevention of loss of vita
mins and minerals.
5. Beliefs and taboos about 3 • demonstrate the prepara
food practices
tion of supplementary and
weaning
diets.
6. Importance of green leafy
vegetables.
5> Health &
Sanitation: 1 . Personal Hygiene
2. Clean drinking water
3. Disposal of waste
wa ter
1. Give proper bath-Keep nails
teeth skin and hair clean.
Put on clean cloths.
2. prevent water pollution and
drink purified water.
3 * Educate the families on pros
per utilisation of latrines,
drains & soakage pits.
6. Family
Planning:
Preparation and maintenance
of family survey registers
and eligible couple regi
sters; and using them as
the basis for deriving from
them the lists of couples
that can be treated as tarT
get for any particular
method of Family Planning.
Prepare lists of target
couples in consultation wi th
MPW(f) and MPW(M) based up
on the eligible cntple
register.
Educate the couples regard
ing the DF.P. method appro
priate to each one of them.
(Permanent-Semipermanent or
temporary as the case may
be )
y-
r.
s4s
Circumstances in which it
is advisable to recommend
induced abortion or men
strual regulation.
Motivate the families to adopt
Family Planning and bring to the
notice of MPW (F) and MPW (m)
those that are re sistent.
Refer willing cases for menstrual
regulation to MO, PEC early after
15 days of missing periods and if
abortion is desired arrange for it
early preferably within 3 months
of gestation.
7. Records, Reports
and Vital statistics:
1. Basic records like Family
Health Registers, Family
holders, Individual cards
and charts and daily diaries.
2. Reports such as monthly
progress reports.
3. Importance of vital stati
stics and prompt and com
plete registration of births
and deaths.
■.
Prepare list of births and
deaths occuring in the village
and show it to MPW(f) to fa
cilitate follow up action whe
rever necessary.
Maintain a record of the
supplies of medicines and
equipment received showing
therein the extent, to which
each of these items are
utilised .
8. Co 11 a bo r a t io n ' > i th o th er
workers of the PHC and
other institutions of the
Indo Dutch Project:
1. Organisational set up of
the PHC and particularly
that under the MPW Scheme
and the activities.
2. The set up of Indo Butch
Project Institutions like
balwadis creches mahila
mandals & youth clubs and
their activities.
3. The concept of Integrated
approach for development
of child welfare and improved
socio-economic status of the
rural folk.
k. Collaboration with all other
wor ker s .
-: : :*ssr :
n'l
Observe the activities of
MPW (M&F), BaIsevika, Craft
teacher, mother teacher and
associate with them.
.
H 6_> 6
v
u
Q^cxc fcg rCXx-ricA)
-
#------------------31 tz C /‘5o^ ^/ 7 7
Axc^ / 7__Z9_77_
( 'D-eo^y
rSc^f herjo /Tt^^z 'ek. ^)
-X . ^rT/e^ rJ&re ^r-y
Psm Ji^loSil?)
/O>n
&f Kcju ^7^
Ccyz^^^C
J^cjiyr
le,*cJ
3^a
H^rry Pizf SVfl
hz T^^C^y-
ePl v^OJ Fc^ c^ #y
C?kh
3. _Jk5 JI o c^e. A-«2^ve I
^c^/u?
h7~
/g
Trc*~*-f~) Cn
Ljl 7>^ c .'!
Z/ .
. 3/£ c
~r<^-p>
7%. ola.
-7 7 ~7*
CTTvn .O tf*ozo
So-h ■
/y
j7>ya
ur?<Z;&‘f-r'Lcs'} d -V? C'.'-io)PrCiL^U^
K/k
) iZejfa
b re/
ll-e^ //A
7^vt ^^Lf^^jry^rVyJZ. ^Q k-ii-,')
>•”
O*T>Co CA
~5<CA^T)
cf
|
CXJQI ctff
cj Z^ O.A>txzi f
(C-e/)
J 2. C^Qi^ prOtZj'YC^^
O-pp 1 > C aptejvo
A-n
Cyde^^e^
R:
)& (11)
I have prepared a short brochure on the training
programme for Community Health Workers in Community
Health and Medicine(P<U.C. 1).
I would like you to go through it and make any changes
you desire.
For the time being, we could cyclostyle about 100 copies
of this training programme brochure and send it to all
concerned. The cover page would
ould have to be printed with
the College emblem.
c
^The detailed training programme of lectures, clinics etc.
could be handed over to the trainees when they report at
the Institution.
Tou may like to have a look at the Indo-Dutch Project
for Child Welfare brochure which is placed below on which
our brochure has been patterned to some extent(p.U«C.ll)
19.5.78
The Dean
St.John1© Medical College
Bangalore.
2^
Hospital Administrator
SJMC Hospital
Bangalore
Director of Rural H^-bh SQFVUfcfc
And Training
3^^
ATiwm of w >
ys-uf<r
ST.JOHN’S
MEDICAL
COLLEGE
AUD
TEACHING HOSPITALS/RUHAL HEALTH CENTRES
i
Johnnagara
Bangalore - 34
Phone: 40561 & Ext: 265
TRAINING
PROGRAMME
for
COMMUNITY HEALTH WORKERS
1 n
f
COMMUNITY HEALTH AND MEDICI N S
♦
*****
*#*
*
B y
Major General B Mahadevan
PROGRAMME DIRECTOR
32-
/
TRAIHnJG C0URS3 FOR COMMUNITY HSALTH
WORKERS IN COMMUNITY HBALTH & MSDICINK
I y T R0 D P c T I 0 N 8
Our Country is hopefully entering an era of social
and economic revolution. The Union Minister for Health and Family
Welfare, Sri Raj Narain, has said in this context that "The soul
of our country lives in the villages. The progress of the country
depends on the progress of the villages. Unfortunately the steps
taken so far for the development of villages have not been adequate*
la fact, people’s cooperation was not sought to make rural development
a success.
They vere not given the opportunity to participate
in the activities sponsored by the Government nor >ere they given
the opportunity for doing theee jobs thereeelver?”*
Since independence, we have made substantial
investments in the production of medical manpower but the health
status of our people is still far from satisfactory* Health service
hithertofore has been basically a service ’’distributed’' by a group
of health professionals to a community rhose role was that of a
passive recipient. There has been very little participation from
the community in solving its own problems. It is true that Primary
Health Care delivery is a difficult task. Health is not a primary
felt need.
Economic development and agricultural improvements are
two more important eectors to the people and only after improvement
of these priority sectors, would health became a relevant issue for
the community.
In many gigantic tasks in the control of important
social diseases like tuberculosis and leprosy and in nation wide
programmes connected with Maternity and Child Health(including family
planning). Care of the Handicapped, Rehabilitation ^nd Nutrition,
Voluntary Agencies all ov^r the world, including our own country,
have provided the necessary lead. In the field of medical and
paramedical education also,missionary educational institutions
have contributed a great deal in suppltyienting ^•wr’xiental efforts
and programmes and h«ve functioned as active partners in such
enterprises.
Teaching institutions should play their role in
...2A
-i
: 2 :
training the required number and type of Community Health Workers
to participate as "Comprehensive Grass-roots health agents within
the Community” who will find the needs, problems and potentials in
the Community in the field of health as well as other aspects of
life, thereby giving the required priority to community participation
in the planning and implementation of various nation building
programmes.
The Community Health Workers Training Programme
being organised at St.John’s Medical College and associated Teaching
Hospitals/Rural Health Centres envisages such a coordinated effort.
Our Community Health Workers will Join the Army of Community Health
and Multipurpose Workers being trained by Government to develop,
expand and extend Primary Health Cax’e Services in rural areas and
urban slums. They wil?. function as essential links between the
Community md established health agencies to make rural health
programmes effective. This programme cf training has become possible
due to the dynamism and perseverance of our administrators, the
Dean, Dr.C.M.Francis and the Hospital Administrator, Sr.Carmelann
ably supported by the Governing Body of the Catholic Bishops
Conference of India Society for Medical. Education and various
sponsors.
The training programme of ^months duration has
been made as practical, problem solving and action oriented in
nature as possible. Bmphat s is being laid on understanding basic
health measures, nutrition education, under five care, family
planning and welfare and environmental sanitation. Nearly two
months of their training is in rural areas, and therefore, the
boundaries of problem solving and action are limited to actual village
situations, avoiding unnecessary general and Macaderaicrt discussions*
The workers will be given various practical, assignments to equip
them with the necessary skills for identifying and solving health
problems.
Selection of trainees is made farom amongst persons
with a basic qualification of SSLC or equivalentf motivated and
dedicated to serve and who are already engaged in social, developmental
and health fields, in peripheral areas*
: 3 :
After conducting an adequate nuuoer of such
Basic Courses, it is proposed to run Refresher Courses for these
workers and finally Teaching Training Courses for Doctors, Nurses
and selected CHWs. Refresher Courses will be conducted at suitable
centres in India.
As the trainees hail from all p&rt of India, the
medium of instruction is necessarily in English* For the time being*
selection for Basic Courses is being made from asnongst seminarians/
Priests/Brothers/neligioue sisters of various Diocese and Congregations
in India.
LSARNIHG OBJSCTIW 0? THE COWS s
Ilxe training
vll 1
th 3 worker serving
a Coiraunlty to
(a) Control conaunicfble dlaeaeeB byI
- identifying, treating, advising and when necessary,
referring patients with fever, diarrhoea and respiratory
diseases
• preventing the spread of epideiuics and notifying
such diseases
• undertaking vaccinations as approved
(b) Provide maternal care by:
•• identifying pregnant women in the oommunity, advising
them and referring abnormal
to the health centre
or to the hospital
** preparing for delivery, assistance st child birth,
giving first care to tha anther and baby, calling for
aasiatance or referring cases when T«ecessary
- giving poat natal care, advice and family planning
information
•• advising, treating or sending siok irciaen to the hospital
(c) Provide child care by caring for both well and badly
fed children, and promoting nutrition education
(d) Give primary care in case of limrMSf wounds, fractures,
bites, accidents and refer them when aecoasafy
(e) Concern himself with environmental health problem by
advising the community on water sunrly« excreta and waste
disposal, food protection and by pxsMAoting health
education in these areas.
...4/-
: *
i
(f) (Mpe with the following health probleu by identifying,
treating with staple nedioinee provided and referring
oaeea when neoeseaxyl akin diseases, eye diseases,
headaches, belly pains, pains in the joints, intestinal
woms, weakness and tiredness, diseases of the south and
teeth, lumps under the skin, mental and venereal diseases
(g) Take an interest in and participate in oomnnmity
development activities of various types including animal
husbandry, agricultural, horticulture, poultry,
plsciculturo, piggery and so on, by discussing community
problems with local leaders and working out solutions
for improving the quality of life of the population
(h) Refer to appropriate centres all cases and problems
outside or above his/her competence
(i) Maintain basic medical records of vital events(births
and deaths in the ooiamunity).
CQHPQHSNTS :
A programme of locture/group and trainoe/staff
discussions, clinics, field visits, practical sessions and films on
community medicine and health subjects has been organised* Ths whole
course is designed and spread ott over a period of 12 weeks of idiich
3 weeks will be at the urban location and 9 weeks at a rural set up*
While certain topics and training will be imparted at St*John's Medical
College and its Hospitals, most of the subjects pertaining to community
health matters will be dealt with in the rural field health centres,
where it will be possible to expose V.e trainees to problems and
various approaches in community health* Participants will be
involved in practice of actual procedures like immunisations,
disinfections, conducting of antenatal and under five clinics and
treatment of patients for common complaints with staple drugs* The
acquisition of basic knowledge, attitude and skills will receive full
attention throughout the course. Time will be given for participants
to speak, so that the faculty gets to know their problems and find
solutions to the same. Their active participation at all stages will
be ensured.
I 5 l
One of the highlights of the training programme is
the intensive exposure of trainees to various modal development
activities in Karnataka’s rural areas, including economics of the same.
Information on how to start snail scale projects in rural areas on
Poultry, Piggery, Dairy* Agriculture, Horticulture(Applied Nutrition
Programmes), Pisciculture and Animal Husbandary is provided to them.
The Community Health Workers thereby understand that Health^Development
are closely linked areas for the total development of a Community,
In the words of the Dean, Dr.C,M«Francie* the
participants will have at the end of the training " 1. an elementary knowledge of the working of the body in health
and disease
2. acquired the attitude, skills and knowledge fo^liealth education
at the individual and group levels in the caanunity
J. developed an attitude of nocial concern for the disadvantaged
and sick
4. obtained sone insight into the social effects of illness on
the individual and the family and the role of socio econosio
factors in health and disease
5. acquired skills in making out the signs and symptoms of the
conaon ailsenta in the coffttunity and the general wanagenent of
patients
6. an elementary knowledge in the organisation and management of
primary health care for a community, including water supply,
environmental sanitation and Immunisation
7. knowledge of the working of the national health programmes
including nutrition and maternal and child health programmes
8. obtained an idea of population dynamics and family planning and
9. developed an attitude of thinking of development as a whole
and not health in isolation".
Venue i
1) SfJohn'g Medical College and Hospital* Johnnagara,
Bangalore 34
11) Hural Health Centres, Karnataka 0 - DomaswuidTa(Anekal Taluk)
- Mallur(sidlaghatta Taluk)
...6/-
: 6 $
FACULTY :
(i) Dean, St.John's Medical College
(ii) Hospital Administrator and staff of St •John* 3 Kedioal
College Hospital (SJMCH)
(lii) Staff of Departments of Anatos®’, Physiology, Medicine,
Surgery, Paediatrics, Obst & Gynae, Orthopaedics,
Dermatology, Otorhinolaryngology, Ophthalmology and Psychiatry
(iv) Director, Hural Health Services and staff of Department of
Cohnunity Medicine and Ross Institute Unit of Ocot^ational Health
(▼) Medical Officers and staff of Primary Health Centre/Unit at
Dommasandra and Mallur
(vi) Staff of Providence Convent and Holy Cross Convent
(vii) Visiting Lecturers from:
Indian Institute of Managmmt» Bangalore
National Institute of Mental Health and Neuro Seienaes,Bangalore
Natural Family Planning Association of Indiaf Bangalore
St.Johns Ambulance Brigade^ Bangalore
(viii) Directorate of Animal Husbandry and Veterinary Services,Bangalore
Ministry of Agriculture and Irrigation (Regional Home Sconomist),
Bangalore
Directorate of Indian Institute of Horticulture Research(ICAR),
Hessraghatta, Bangalore
Director, Indo-Dane Projectt Hessraghatta, Bangalore
Water Supply and sewerage Board, Bangalore
Social Welfare and Labour Dept, Bangalore
v'1 * ei
Directorate of Health and Family Welfare Services, Bangalore
Directorate of Fisheries, Bangalore
Dept of women and Children's welfare. Bangalore
Dept of Public instructions, Bangalore(Chief School
Medical Inspector)
Duration of pour a e
12 weeks
Course Capacity
20
• 7 i
Boarding and Lodging s
Course is fully residential. Trainees are
accosmodated at St.John's Medical Cdlego Hospital/Rural Health
Centres( Dosnasandra and Mallur)
Maala
Rs. 5/- per day
Rs. 7/- per day
Transport t
Transport for trips between the College and
Teaching Sospitale/Rural Health Centres and for field visits, will
be provided, for the participants and accompanying staff members.
Library Facilities s
Course participants are permitted to use the
College Library for the duration of the Course.
SXPfflfDITORB 1
^^endMhroJjaeurredoa, transport, ®Miovi^u^l/
/ 'S
equipment, stauondry awTfacuHy 'time.
'
Baah participant is required to pay Bhe Course
Foes of Rs.900/- to meet the expenditure incurred on transport,
audiovisual equipment, stationexy and faculty time. The course
fees will be paid in advance along with the boarding and lodging
charges.
Kegiatration $
All candidates selected for the course are required
to fill in the attached proforma(Appendix a) and mall the same
along with the boarding and lodging charges for the period of the
entire course in favour of the Dean, St.John's Medical College,
through their Diocese/Congregation.
Training Programme ;
The detailed Training Programme of Lectures,
Clinics, field visits, practical sessions, film* on Community
Medicine and health subjects, Topics of Group/Tyainee and staff
discussions, will be handed over to the candidates on joining the
course.
8/4)
V
I 8 |
COORSK CKHTIFICATKS :
Course Certificates will be presented to
candidates successfully completing the course in Community Health
and Medicine, First Aid and Natural Family Planning.
/////////
ee
r <~^a~^1
GD
C(^r>^>^
----- /?^,<^<^v>oz?>^-z-7cd S
PAe^p^^'-
jcr^cx I
._ pPx^o-
y7^xr
Y-i"" YP-^^
p
Ypy
i (^
p-rcs^x'P& '
/q7?_—
bJ Pq >^Op^ C^IIX^
r^
Pe /
C.f3 <S I
<
p-V-eC^-^
cj
^> ca
, r
IfU
e^erp &. -\ n x^e? ^
Ao
^Sc^pe^k
tz cX^.A edK
A'Vef^U czcxl
r
p£_X->
L-/'~)
•C5^>^
^'L<
C-,
)
t
st P^>
a hj ec ^1
.c-J
(py-Y^y^C
1
af
'P) ■ P^l o
^p
&v
}ct'17-7eif 1
Yc^
r
-o e c Ycry ^C
,y‘^
p ’C^j
l'-Y^P<~>
5?(a C
Q) A x^H_^e7
CC^^>
P^p.-oy
U-^'P
ic^CJi)
'
pY c^-r^c. ^- ^ ,
TJy c • H
r>
1 j -.p^, y
cP><~P^
-x I
zp
1
<S^-a
H., ^T5Ci
a
L
.
'YP)
&rcp^~) . 3 '
Zzk
lc
cY^ c^uz'
i
■ Pi^. 17^ y
-
•
iz
-7O?'^k
)
J
Auc 1
renr
l-te^p
j
'
/<
xe^’^
p
4. P/
/< ■
P<P
C^f
7 7-7^- )
ci^.^c^L
r
pUz.
\
ex)
/3<^o
C-Hi^. ip- c^s")
’-j
C. ctca
•>< £»
< CST'l
<^A
ioc^nicz.
r.ii
TD<z
Ci^
e^L^ci^cii
■)
■3 ^-Zbua^A-^^
/< CP^p
610^^ s^-o
)
c^LCo O-^-ooezi
^cs-y^
c?) f—ytp!
<S/7 Pi I
Cc^ck^cy
‘■<J
ex
{ (jrr^o
Moht 1^
.V
h>ili^
i<^ >
p^<p^
/
Clvi
7^’’crCj2-^>o
/-Sc-vJ lci-x--^’^j
'
<d^
j,
/= xp-^.-—"■
I
c^
II
ppM^
^^3 , ,
pI^
Z- pyOrcl''^ ArrO^'j
y
pollahcpcy^
•o
C
Ic^lc^
(g)
Ax Aev^
<T
/
/c>
<S^)
£—^;Z> ,
Ku
lC^~
CzO'/^
ci
f'/^Q
hj2C> 'l^
par
c
/65
ik^2.
^xQv-exx
lc^>!'
pM
h
fcn^~>
kJ<
lo
O P
L^)
MP QO
(J ®
Pn
„.Axx U*)
P .)
t^;h
/O
ri<^p l-^
CP-n^yo
~
AS^^/c. - 7
pl^ho.y^^ ' "7
K
cxfo">
p-' U Z
A/ey^>f z
fc) <>yoiC-
O-^'P\ .
Fk I i e
C=xL^i eta I LzO
3
-^--y^p(c jrn en
_________
6xsLAr5e
c\-
§
C^cyt^r'mf^>'')
pi ^y p
cry^e-Lex
YC In ~f^
idt^TY^
f
> /c5^uo
$»c_xCS /o
z ' y
Cc^Lx-ye^o^^-r'
^C>
Cirfl j
i^Si .
ly -)
p' J^Y-t cA-^: o. .
3
3
•
Cc^y^ pC.yKec^^
rOc^O‘ cl
Pt
ex
la~>€
c>^^
rj^oA-eo
iPsynn
*ruczn <2 c <ta TS^-e?
l^>e I
IBi^jl^-^pl
5.
oY .-A-1'
HyeG-zx^o
tTl^i e>-ck^L
(Scsv/Z
kc ^>d
rr>rn----z*Ottnu^y?u^zdl o^-? tA
C5r)1^\Jp LZ-o
<JL hj^PifL
eLcls
Tib^l nnc-
^7
Ca Y rL 'cST-eOC-^?
Ua-^e/
^/-/Xj J S As C^5Z^yJ<2_
Col Ic^.focTi'C^Kci^-) <Z-
cb-^ eY
/A^^_ p^y
2 T)-e^
/^xu.'C
Pcx-Yy-
St^ 'PcSr-l'OY^.
/er<7<c/-i-rr'
/xfuo-^exj/c
- ------**
/h J»by
C o/)<r^
I
1
C5~^)ly
pYy'Y^KPb
3/Yo
IcrepP^r^p)
L C.
A A ret PT^rm
> O eye
j b~YaPc2i-y^Z> / pQ I>'pt
0^5 <=^
3.
UJtcsy''
L] .
Nc?
6-
z>p
f
'*'
'jej
b-^
(^iz> I'Sa -A C
<y^
<^~Y^
Lsfe-. (jy>^
y
[ <rp rv^-n ip
p Y-yt ^C.^)
p ^pp,
y .^p I
c yy^e^y bo p a>^\
.
1^ 7^^^
dLcxJ
!.
i3<^ c-k.^i voi^-o^A-
p
1^7^) —
^5-r i VcLoriv v<^
p
O^-> cA.
Xerr-y
p<^ '
'S^pp^A'
ho-oeA- -
Av'ovx-/-~7 tyQ £-j
rO
pY<ii
<1
x=> p'T&W c.
e-
h
vn C (2^)
'T^Y' <2 ‘ M
Io)
dx
H7 7-
71^2.
h^c<xlfK
\^l ICX
CX
Lj-sveb^ l/c*l''G>
CJ
p-nxp<^X<x I
A
/4 77-7g
D r <S-M
^df
^.y i<t>rr>
TP) Le> hc p
i 'c^-
/^o-^evo ,
I X^.KcrY->
f-
pot 1^J
.
,M^
rxo
(B Mo’
cl>e^ ^p
^t
C^i
e*-~>
ec
(_pj2
C’
- •
C>-^7
yp
7<r
i<
P.
p( exh
V
/-I^CrjA
c
)Z4O
Xx p
C crcA>
e
7^7 O- vc /-> ~7 "t?
<—-">
p^c
~3
flxso Auzidl
;|€<)
iv-£e’
'C^ I
C^
Pcrr”
____
P)i
P^b
'fj2/7 CJ2
VjEC jiO^^fj 7'7^)
CA.
>
yircc^
oc^b
e
*Co* o
£^7^
Ccy ^ /
y^_>-i cj
y^)
CtLs-b c 'i
e
3
Se.|^c
dy^C
i
O- .
BC-/
'l^^n
ho.^ ^a,i Z1 'Ctx. f ‘ crr->
h) esLC-
/g >)A
L^arX^n^ p^&i^Le^'p
ffp
aj
rr~Le. eXt'Cc’'-
r4o
ir f
p^^^^
P)
h)
I
G^C'P'C
h
p
ex
a^
PU2^l^>-^J
pe^'P
tq-
fcC-G
7
I
t?G>
pcv^>^,€:<:^~
'Di CTCjz ^x o^
IlLXn CJ2=_
oy p^^P
) P)^^c;p I
I
CTrry
'±^
C
hJcrr>
k/UMx
I
X
Med ye
-3^
3i -Lto
'3
i
I
3
6
I
I
13
I
/
c
I 3-f-l
~)
//
/3
~~H
io
IQ
7
3
S
%
7
%
53
16
15 7
vV An o
(_ A^Zca /
C^/^l'e
SA^Ae/X?;^^^
A
<~^e^JL'^■
L/ .
c KC5>-»
J
/) Z?^
i,) ri re&k
Typ^
ck PK^^
r-O^p^^^Zj
r-'ichf -c^
Sc.)^ <^=>1
, .
(jZehc^J
r
G
A
I
ex')
/^tc^f^
C<^y^
d>
C
o
PIc^J
p/^
a)
7
Z-^ tK^^0
C
c d^rz-?A^c^
r^c
c
O1
°
'■ -1'
/e /
/o
&--7J
j,)
’’^
I
^^=> (jpy foeJ^JiO
or-)<jL OrOi oJ/J)
tx)
f3c-l
2.
ti.
5
C
i
IgT^J
tz
*
hj S/^l^e-/^'.
(^) ■fhttZ ahe^‘
1
^Zo- 3o
M^4
“2? o
T7o-6^
3i;
CCDr-y
f^-). rn.
— 5
Sm)
H
/
r<^~>
| cs~>o -
4
Mz>^y
5 ioJ^571^0
flppUA /Setac^M.
______ _
lif )
S’cJ^
3, Reh&h G2^\
)s
kx^>
5. C>jh-
b)
i ,
Cc^~
Type V
3 •
k
p^/Kcrry
(3^
---- Cytk-e^^
Ck H
C^j~Gr^l< (^J-kt^.^
/ke kv^^-
I
De
fv
/kill
a) 7
h)
(7^ ;•
?H~C
r^L^n FA^r
^rv^
CJ
Cr^j2^76-^-x
Pio/"}
>
<^l
&-1 o>z
0kjlc5~>~>
o)
/
l
^c> !/gs -l ^'<>^^
s^b
K-rO^JZ^
by
i
[/^n^uzjcx^; I
I
Ro-nd^^
fAc^
4
7
l^/^l^l^l
f <r/C—
/ ~f'l
f ^1 4- i -W-H
i
L h^l>G^c>cjo
Cu.^clc If&w* ^)'
-/ 4-/
Cj C^k • 2
'i
Co mH- 32_-
The visit of the Advisory Committee for planning the peripheral
health facilities and the>Community Health Department of the
proposed Christian Institute of Health Sciences, Miraj.
Members:
Drs. R.S. Arole, George Joseph. Abraham Joseph, Kalindi
Thomas and P. Zachariah. (Dr. Irwin Samuel had been
invited but was unable to come).
The group met together for the first time on the evening of
February 2, 1989 in Solapur. (Dr. Arole joined the group the next
day at Pandharpur.) The plans for the field visits were finalised
and the demographic data and health statistics which had been
collected on these areas were circulated. There was also an
opportunity for meeting the Dean and Professor of Community Health
of the Solapur Medical College, Dr. Mrs. Shantabai Warerkar.
Traveling down from Solapur by road, the group stopped at the
Rural Hospital at Mangal Wedha in Solapur District. The hospital
was in a hired building, but a permanent Community Health Centre
with about 30 beds was under construction. The doctor in charge
was able to provide a good account of the organisation of the health
care system at the level of the Rural Health Centre (Cottage
Hospital/Community Health Centre) and the Primary Health Centres,
its administrative structure, its strengths and weaknesses. The
adequacy of the present MBBS programme and internship in preparing
graduates for work at this level was discussed.
The group then visited the former Mission Hospital Compound in
Pandharpur also in Solapur District, about 125 KM along good roads
from Miraj. This is a well-planned and well constructed hospital
complex with space for about 50 general beds, quarters for staff and
about 7 acres of land. The whole complex is not in use and is in
the possession of the elderly Christian doctor who was running it
successfully for a long time. If desired, it would probably be
available as a long-term lease. The surrounding community is not
impoverished and this hospital does not have any outreach work.
About one KM from this hospital, a well designed P.H.C. with
accommodation for staff etc. is almost complete in Kasegau. The
group also visited the Pradhan of the neighbouring rural community
as well as the present P.H.C. for Kasegau and the new one under
construction. The Pandharpur town is a famous pilgrimage centre
for Hindus and the local community is predominently Hindu. The
local Christian congregation has only some 10 to 15 families.
Reviving the Christian Hospital under the auspices of MMC would
certainly be possible, but it will to begin a new. Developing a
community health project attached to this hospital will not be easy
and perhaps not relevant because of the new PHC coming up next door.
After considerable discussion, the group felt that in spite of the
ready availability of the physical infrastructure, Pandharpur would
not be the first choice for development into the "independent"
peripheral facility (see below).
(Dr. George Joseph had to leave at the end of the first day
(Dr
due to unavoidable reasons of a personal nature).
On the second day, the group visited Kavathe Mahankal, a partly
developed Taluka in Sangli District, 45 KM to the northeast of Miraj
accompanied by the District Health Officer. There is a well
developed Community Health Centre there with provision for three.
doctors and about 30 beds, and three outlying Primary Health Centres
- 2.-
of the Co-operative Sugar Mill in the neighbourhood. Though this is
not exactly an impoverished area, its optimal distance from Miraj,
the good physical infrastructure for CHC and PHC*s and the co-operati
and effective local leadership make this a good governmental taluka
health care set up for use by MMC, provided it can be completely
handed over to MMC. Atpadi is a neighbouring taluka to the north of
Kavathe Mahankal (85 KM from Miraj) with similar socio-economic,
health care and leadership characteristics. Jath Taluka is less
developed and sprawling taluka about 80 KM from Miraj. The need for
health care is greater there and the socio-economic conditions more
adverse. It is on. the border of Karnataka State and the two language
groups are vying for dominance. So there is no stable political
leadership with which a voluntary agency like MMC can easily
co-operate.
The group was also informed of the centre being developed by
MMC in Bedag, 12 KM outside Miraj with a grant of Rs. 21 lakhs from
DANIDA. A PHC type facility with a few inpatient beds and
accommodation for one doctor, one public health nurse and 20 students
is being-built. It will also have its own conveyance for serving
the surrounding population of 25,000. The Community Health Unit of
MMC has fairly good roots in this community and this miniblock is
within easy access from Miraj.
Following these visits, the group had extensive discussions at
MMC, in which the Director Dr. C. Thomas and Dr. Shaila Jacob,
Nutriionist in the Community Health Unit of MMC, also participated.
SUMMARY
of
RECOMMENDATIONS
A. Clinical and Community Health facilities
For the purpose of the proposed undergraduate programme, the
following structure of health care is suggested:
I. Referral Centre: This may consist of the subspeciality
departments in Wanless Hospital or, eventually, a separate
Speciality Hospital. Undergraduates will have only limited
contact with this area, but should learn at what point cases
must be referred to this level.
II . The Tertiayy Care Centre* This would consist of the Departments
in Wanless Hospital dealing with the subjects in which an
undergraduate is normally examined. Eventually, this may become
a separate General Hospital with only these departments. Such
a hospital, physically separate from the Speciality Hospital
and in the same campus as the Medical College, will have a
number of advantages. Especially, the students could see the
basic clinical specialities taking care of most needs of patients
while also referring patients to subspecialists where necessary-.
(According to the MCI requirements, Departments of Radiology
and Anaesthesiology and Units of Chest Diseases, Dermatology,
Psychiatry and Dentistry must also be available for undergraduatt
teaching. Some of them like Radiology and Anaesthesiology may
have to be duplicated. Others may be based in the Speciality
Hospital, but also serve the General Hospital as necessary).
The undergraduate should not spend more than 50% of bis
"contact" hours (i.e. hours spent in health care facilities of
all kinds) in the Tertiary Care Centre.
III. "Peripheral facilities."
3 Obstetrician) and acting as referral centre for the PHCs or
other primary care facilities serving a rural community of 75
to 100,000. The nursing and paramedical services in these
areas should be fully integrated with the clinical and community
health services and accountable to the heads of these two
services. At the community level, health care should be
integrated as far as possible with comprehensive multisectorial
development activities.
The "integrated" peripheral area should be a relatively
underdeveloped taluka in the Sangli District between 30 to 50 KM from
Miraj, where MMC should receive from the government the whole health
care infrastructure and organise it as effectively as possible. The
Community Health Centre in this block should be manned by the four
basic specialists! MD/MS for Surgery and Medicine and diplomates for
Child Health and Obstetrics. If possible, this Centre should be built
up to a bed strength of 50 to 60. It would be good to keep the staff
strength and budget as close to the governmental pattern as possible
exceeding them only if that becomes indespensable for the efficiency
and effectiveness of the programme as a model programme for the
training of students. Of the three talukas of Sangli District
mentioned earlier, Kavathe Mahankal Seems to be the most suitable for
the field area which is to T5e incorporated into the medical college
programme in co-operation with the government.
It is expected that many of the MMC students will later serve in
health facilities set up by the churches or other voluntary agencies.
Therefore it would be good for them to have part of their peripheral
training in a suitable Christian hospital with its own outreach
programme and adapted for this role. Such an arrangement would also
make up for any deficiencies that may develop in the other "integrated"
peripheral programme. This "independent"•peripheral programme could
be based on the St. Luke’s Hospital in Vengurla, Sindhudurg District,
which is in the underdeveloped Konkan coast, This hospital with
about 100 beds and a school of nursing has a considerable clinical
load from the surrounding area where the health care facilities are
inadequate. It has.a modest community health progra'inr-e in neighbouring
villages. MMC is to come to an agreement with the present management
of the hospital such that it can be incorporated into the medical
college project. The staffing of the hospital is to be increased to
the five basic specialists (including Community Health) and the outreach
work expanded to cover about 70 to 100,000 population.
The main function of the two base hospitals (in Kavathe Mahankal
and Vengurla) should be to train the students in good secondary level
care outside the tertiary care centre, offering experience of almost
all clinical material that an undergraduate should reasonably know.
The student should not only observe the clinical work but increasingly
share in it. Though the clinicians have expertise in one speciality
or other, they must practise and teach multicompetent clinical care.
These hospitals should also demonstrate the referral chain from the
community to secondary level hospital to tertiary care centre. The
clinical staff of the MMC should spend about 25% of their working time
in the base hospitals of the peripheral areas demonstrating the
challenge of delivering fairly expert care under the limited conditions
in these hospitals. The student should be posted for 25% of their
practical hours in these hospitals, and another 25% in the community
itself (i.e. in the Primary Health Care facilities and other activities
relevant to the promotion of health).
It would be good to begin MMC’s involvement in these communities
through health related developmental activities so as to develop
meaningful links with the people and to ensure that the programme
4 -
Both these secondary care centres would be so distant
for some weeks at a time (’’block postings )•
As soon as government sanction for starting the medical college
was assured, MMC should appoint two suitable Project Officers for
developing the two field areas as outlined above.
There would be aspects of CH teaching in which field exposure
is needed as a regular part of the schedule while the students are
at Mirai. It mayalso be good for each student to have some families
they are related to throughout the MBBS course.4 For these purposes,
Bedag should
the clinical facilities and the field programme in Bedaa^Jould
continue to be developed as presently envisaged, with staffing from
the CH Department of MMCr
B.
The Community Health Department
It was suggested that MMC should plan for the following faculty
for a large Community Health Department.
(1) Head of -the Department: A Senior Professor with commitment to
the goals of this venture, and the necessary experience and
expertise.
Four lower level faculty members, each chosen with expertise in
(2) one of the following special areas, with the intention that each
will develop his subspeciality within the larger department:
Biostatistics
Epidemiology
Health Education
Behavioural Sciences
Health care management
Nutrition
Dr. Kalindi Thomas has been associated with the Community Health
’sS’lWoSi; b^ennabled to
tbe
take’™ In PSM through a nolbourlng medleal
inoicatea xnai
Of the National
Board in Community
Health. She .ubseetlon
b". re.pon.lble
for th. Bpldemlology
of th.
jLld^h^n
Department. Dr. Shaila Jacob, also on the start oixn
,^^5 ?equl?e ! SeogSable postgraduate
Health Unit
SKm So Jhain PsS an°d
in charge
the Nutrition
subsection of the Department*
C.
The Presfriflction sandwich Progr^nyn^
....
the 4X2 years MQBS programme.
It^innS!uh,£b^S,D-ln;
(,)
° ^se should be selected for
™
f
.ty
community
The students should r.cele. a good exposure to
what eon-un
to what
5 j
oriented Medicine really means and what the role of the doctor
is in such an approach. They can then decide with greater
understanding whether they wish to be trained for such a career.
(2) The college can also assess the candidates for their suitability
for such a programme in terms of their maturity, motivation and
commitment.
(3) The candidates should also acquire the following knowldege and
skills to prepare them for the proposed "innovative" MBBS
programme:
(a) Working knowledge of local language
(b) Knowledge of English sufficient for acquiring necessary
information from standard soufces.
(c) Basics of the following three Bs:
e
(i) Behavioural Sciences
(ii) Biostatistics
(iii) Biology (human) - This is to facilitate
problem-based, student-centred learning
from the first year of MBBS.
*
*
#
*
O M’H -37-
Working Towards Rt- □ogjiition
Of Dai Tradition
A Report on a Consultative Meet of NGOs working with Dais
(Traditional Midwives) in Gujarat State
India
§
CD
C
’cz
I
fcT
Q
CD
CD
&
X
TS
• o£
o
o
o.
co
May 2000
CHETNA, Ahmedabad
Women’s Health and Development Resource Centre Chaitanyaa
2
Background
In most rural and remote areas of India,
traditional midwives, popularly known as
dais play a critical role during
pregnancy, childbirth and in newborn
care. They are respected and trusted for
the care they give to the people. In
addition they are easily available,
affordable and culturally acceptable
particularly in interior tribal areas.
Dais are an integral part of the
community health resource and
therefore their support in reaching out to
people is greatly sought. Despite their
valuable contribution at the community
level, Dais continue to work in isolation
from the mainstream primary health
care system. Their integration with the
primary health care system is not
formalized and their role in preventing
deaths in rural and tribal areas is
questioned by several experts.
Before and soon after independence, the
Government of India (GOI) initiated
efforts to train the Dais with a view to
reach out to the community and make a
significant difference in the high
maternal and infant mortality rates.
During the second five-year plan, in
1957 the Government of India initiated
Dai training program under the Maternal
and Child Health Scheme. The effort was
to train women from rural areas for a
period of six months and a remuneration
system was worked out. In the
subsequent plans, various changes were
introduced and in the fifth five-year plan,
the duration of training was reduced to
one month and work in association with
the Primary Health Center, under the
supervision of ANM/LHVs. Other
changes include strengthening her
information base, involvement in Ante
natal and post natal care, family
planning counseling, provision of
delivery kits and remuneration for
normal child births and referrals.
Despite various efforts, not all the dais
could be trained. Little efforts were
made to make Emergency Obstetric Care
(EmOC) accessible in remote and rural
areas. (For detail information please refer
in Annexure-II)
While the Government Dai training
program has yet to show significant
changes, the NGO experiences have been
largely positive indicating the need to
integrate the Dais in the primary health
care system. A need to systematically
document these experiences has been
felt.
For more than a decade, CHETNA has been
actively involved in building capacities of
Dais and the Trainer’s of Dais. The
experiences have lead to a realization of the
critical role that Dai play in reproductive
health of women and men. Their role has
been important to reduce the neonatal and
infant mortality, and also in reducing
maternal deaths when supported up by
Emergency Obstetric Care (EOC). There is a
need to recognize the role of Dais and
integrate them with the Government primary
health care system. Dai is a traditional
resource and her training needs to build on
her traditional knowledge, skills and wisdom.
Keeping the above in view, CHETNA
organized this consultation.
Objectives of the meeting
♦ To share experiences and concerns that
relate to Dais, their needs and problems.
•
To review dais’ role in the
Reproductive and Child Health
(RCH) program.
•
To design strategies to identify Dais
role in primary health care system
3
Background of the participants
A total of 23 participants comprising
activists, researchers, medical
practitioners and consultants from
various NGOs across the state of Gujarat
participated. Most NGOs were pioneers
in initiating Dai programs in remote and
rural areas. The discussions were held in
Gujarati. (Please refer to Annexure-I for
the list of participants).
Proceedings
Ms. Pallavi Patel, Deputy Director,
Women ’s Health and Development
Center (WHDRC) of CHETNA warmly
welcomed the participants. She
highlighted the critical need for Dais in
the coming years and expressed a
concern over lack of recognition of Dais
in the primary health system. She also
pointed out the need to define the role of
traditional systems in understanding Dai
practices and building their skills and
capacities.
After introduction, Vd. Smita Bajpai,
Coordinator (traditional health
practices), WHDRC- CHETNA, traced the
role of dais in a historical perspective.
The presentation highlighted the fact
that how, through the process of change,
people’s knowledge and wisdom has
been grossly marginalised. She explained
at length how, since time immemorial
dais particularly in rural and remote
areas have been performing a critical role
particularly during pregnancy and
childbirth. Though majority of Dais is
women, men were also called in some
interior adivasi and tribal areas to give a
helping hand in case of difficult birth.
Giving details about their social and
economic profile, she added that dais
generally belong to the oppressed classes
with little or no education, are poor
because they work mostly as agricultural
workers and cater to the poor class and
receive very little money in return for
their services.
Considering that Dai conduct 60-70
percent of deliveries in rural and remote
areas of India, she elaborated on the
efforts of the government to train dais
and involve them in providing health
care to women and children under the
various five-year plans. The government
initiated Dai training and has provided
them with safe delivery kits and
remuneration.
But of late, a shift in governmental policy
from home to institutionalized deliveries
(in order to bring down infant and
maternal mortality rate), dais have
received a major setback, their
significance notwithstanding. Vd. Bajpai
also discussed in brief the role played by
various NGOs in promoting dais firstly
through training them and secondly
through linking them up with the health
system for services and supplies.
In the discussion that followed, the
participants shared their experiences
and expressed opinions and concerns
about dais, their involvement and future.
4
Highlights of the Experiences of Working with Dai
•
SEWA-Rural, Jhagadia, Bharuch is a pioneering organization that has effectively
demonstrated the functioning of the primary health car e system. Dai has been
identified as a key resource at-the field level and her capacities have been
strengthened. Coordination between Dai, Angan Wadi Workers and Auxiliary Nurse
Midwives has been strengthened and the Dai is actively involved with the Primary
Health Center.
•
SEWA (Self-Employed Women's Association) Ahmedabad has been training
Dai and strengthening linkages with the primary health center. They are
actively involved in registration of the Dai by regular contact and
dissemination of information of the Government Dai training in their area. In
addition they have organized Dai and formed their cooperatives to ensure
quality care from Dai and coordination with Government functionaries.
•
St. Xaviers Social Service Society, Ahmedabad are identifying Dais in
Ahmedabad slums and upgrading her information and skills. They have
observed that registration of Dais and getting a registration card has build
the self-esteem of Dai.
• Tribhuvandas Foundation, Anand, Kheda have strengthened the
coordination between the Dai and gramin swasthya sahayika or village
health worker and they are able to bring down the Infant Mortality Rate in
their area.
•
SARTHI, Panchmahals has identified Dai in the remote tribal areas and
trained them. They are linking the Dai with the Primary Health Care system
by taking a proactive role in registration of Dai and ensuring appropriate
remuneration.
•
CHETNA has been actively involved in building capacities of Dai in Gujarat
and Rajasthan in association with local NGOs. The training is based on
strengthening her traditional knowledge, skills and wisdom. Dai trainers in
the two states have been trained and efforts are being made to strengthen
Dai training programs. A comprehensive, multimedia kit has also been
developed, which is useful in building the capacities of Dai.
5
FRU level,''often she receives
humiliating treatment from the
medical professionals. This adversely
affects her self-esteem and self image
at the village level.
Major concerns and issues raised by
the participants are:
Remuneration that dais receive from
the government is very little and also
irregular, and so is the community
contribution.
A strong emphasis on referral has
started posing serious problems to
dais as they have started losing their
self-confidence and esteem. Many Dais
have now started referring cases to
First Referral Units (FRUs), even if it is
normal and within their capacity to
manage. What was once available at
the doorstep has now become outside
the reach and expensive.
•
While the need for referring critical
cases and making EOC accessible
cannot be overlooked, in the present
state of primary health care system,
when even Dais, who are already
playing a critical role in reproductive
health of women and men, start to
shrug their responsibilities, the poor
communities are at loss.
•
Delivery kits always seem to be in
short supply. Tribhuvandas
Foundation, involved in producing and
distributing Disposable Delivery Kits,
shared that indent for the delivery kit
from government comes very late and
thus it affects the regular and timely
supply.
The requirement could directly reach the
production unit rather than going through
the bureaucratic system.
•
In the primary health care system dais
are viewed as mere appendages than
integral part of the health system.
Very often, they are not even allowed
in the labor rooms and although they
are an integral part of the primary
health care delivery system, they are
not recognized or appreciated. When
the Dai brings the women at PHC or
A need to sensitize the doctors and other
health functionaries and create a positive
environment was strongly expressed.
There is a need to ensure better
coordination of PHC with the local Dai.
Where available, ANMs, Dai andAWWs
need to work, together at the field level.
Biases based on caste and class and
attitudinal problem often leads to the
poor treatment or neglect of dais. She
is viewed as one who collects and
cleans dirt. The consequence is that
her health needs remain largely
ignored. There is no provision of
health check up of the dais. Many
traditional Dais, who are good in
their work, are facing health
problems like cataract, which directly
affects their profession.
There is a need for special health care for
Dais.
•
With modem medicines making deep
inroads, the indigenous treatment
adopted by dais, which is in-built in
their system, is on a decline.
Therefore, Dais are finding them
delinked in the process of delivering
primary health care.
Dai training needs to be sensitive to Dais
worldview and knowledge systems.
Involvement of other traditional systems
viz. Ayurveda, Unani, Siddha could
contribute a great deal in strengthening
Dais capacities.
Dais and communities, in some areas
are practicing some harmful methods
like applying pressure on abdomen
during childbirth and giving
injections to speed up the process
labor.
6
Continuous training and monitoring on
the same is required.
Action plan for promoting Dai
tradition
The later part of the session was chaired
by Ms. Mirai Chatterjee, Secretary, SEWA
who revealed that most government
officials felt that despite extensive
training and special fund allocation to Dai
training, they have not been able to
reduce the mortality rates of new-borns
and the mothers. The environment is not
in favor of promoting Dai traditions and
practice.
Training of TBA alone, in the absence of
back up support from a functioning referral
system and support from professionally
trainbed health workers is not effective in
reducing maternal mortality- WHO 1999
felt that dais should be involved in
treating minor ailments by way of which
their acceptance in the community will
improve. There were some who also felt
their integration in the primary health
care system is possible if they are made
to work along with Auxiliary Nurse
Midwives or Angan Wadi Workers in a
team.
All the participants agreed that there
should be a regular updating of
statistical information on dais and they
should be given identity cards as a token
of recognition as well as incentives for
referrals.
Regarding Dai training
•
Dai usually does not receive regular
refresher training. She needs to be
invited to the Primary Health Center
(PHC) meeting wherein she can share
her experiences, difficulties and
coordinate effectively with other team
members of PHC. During Dai training
they need to be made aware that for
what kind of condition, where to refer
the patient. This will save the time
and lives of women.
•
Dai training needs to include
information on preparation of women
and helping families plan for delivery,
importance of motivating pregnant
woman for saving for emergency and
updated information on available
communication facilities to contact
PHC or FRU (which telephone at the
village is in a working condition,
phone numbers of PHC and FRU etc).
•
Dai has knowledge of the structure
and function of the reproductive
system, some common complaints of
Reproductive Tract and of the people
in the communities who are suffering
from it. This situation can be
strategically utilized in treatment and
prevention of Reproductive Tract
Ref: Reduction of maternal MortalityWHO/ UNFPA/ UNICEF
The group very strongly expressed that
maternal mortality is a complex issue,
which cannot be addressed, by dais
alone. It has to be linked with
strengthening the referral system and
making emergency obstetric care
available in remote and rural areas.
However, a positive experience has been
observed in reducing Infant Mortality
Rate by NGOs. However they need to
strengthen their information base
regarding Dais and develop proper
intervention tools.
Some suggestions to strengthen Dai’s
role
Most of the participants suggested that
dais should be involved in ante and post
natal care after receiving adequate and
appropriate training, guidelines and basic
information. A suggestion was made to
involve the Dai in reproductive health
care. There were several participants who
"7
Infections, particularly in the RCH
program.
suggested that
•
Linking up with the Panchayat system
•
Panchayats can play an important role
in providing necessary facilities and
support to the Dai. The women
member of the Panchayat can be
motivated to take up this issue at the
Panchayat level.
Institutions such as the Indian
Institute of Management can be
approached to mediate and organize
a meeting between GOs and NGOs
where these case studies can be
presented. The presence of dais and
beneficiaries can be worked out to
strengthen case studies.
Providing Delivery kits
Each district needs to calculate the
local birth rate and estimate the
requirement of delivery kit. 25% extra
delivery kit can be added to the
calculated figure and the kits could be
regularly supplied at the district level.
•
•
•
Supplying deliveiy kit to the woman,
during pregnancy is essential and it
has proved to be useful in the past.
There was a further suggestion that all
the family members need to be made
aware of its use. This will generate
awareness among the community
members and they will start
demanding the same.
Registration with Government Health
System
The group felt that NGOs working with
Dai should take up a campaign to
register their names. For registration
it is mandatory that Dai participate in
the Government training. The NGOs
need to make sure that their dais
attend this program and as a result of
which become eligible for registration.
Meanwhile, NGOs can continue
providing training input and identity
cards to Dais in their area. An idea of
creating training schools for Dais also
came up.
The participants strongly felt the need to
discuss Dai experiences with the health
department. In this context, it was
NGOs involved in working with Dai
should prepare case studies and
substantiate the findings with
statistics to lend authenticity to
advocacy.
A list of traditional/Ayurvedic/herbal
medicine, which can be provided to
the Dai’s for primary health care
needs to be prepared. Its affordability
and availability needs to be ensured.
They will try to provide necessary
statistics and research data. The
Government Ayurvedic department
can also develop a training
curriculum for Dai based on the
principles of Ayurveda. Similarly
other indigenous systems can be
involved in strengthening the Dai
tradition.
(Vd. Parul Joshi and Vd. Ila Deshpande
from Akhand Anand Ayurvedic College
have taken a lead to suggest herbs to be
kept with Dai)
•
The group decided on a coordinating
committee consisting of the following
NGOs:
Tribhuvandas Foundation at Kheda;
SEWA in Ahmedabad; SEW A-Rural at
Jhagadia; SARTHI at Panchmahals, Dr.
P.C. Shah, Public Health Consultant,
Crime Prevention Trust and CHETNA.
8
Role of coordination Committee
♦
Contribute in planing and organizing
the GO-NGO meeting.
♦
Finalize case studies of NGOs on
experiences of NGOs.
CHETNA's Role
•
Overall facilitator of the process and
information dissemination.
Edit the case studies and coordinate
with the NGOs, if additional
information is required.
•
Organize a meeting with Dr.Dilip
Mavlankar, IIM and discuss the
possibility and details of GO-NGO
meeting.
Conclusion
Over the entire group expressed that the
Dai training can be effective when
supported with a program to ensure
better care during pregnancy and after
childbirth and with Emergency Obstetric
Care within reach. While sharing the
training experiences the NGOs actively
involved in this area mentioned that
practical exposure of Dai in a hospital
situation is critical to strengthen her
skills.
If the Dai, as a resource has to be utilized
optimally, then certain issues need to be
debated and clarified at the conceptual
level. Some of these issues relate to the
integration of Dai in the primary health
care system, role of traditional formal
systems of health care in Dai training,
skills enhancement, remuneration,
sustainability and linkages with the
health system.
The meeting provided an unique
opportunity to share experiences and
concerns related to Dai tradition and
how to strengthen it. Willingness of
NGOs to coordinate and work on this
issue is bound to bring effective results
to strengthen the role of Dai.
Update
•
CHETNA has already communicated
to the participants as well as other
organizations that have been working
with Dais inviting them to join this
collective effort.
•
A preliminary meeting with Dr.Dilip
Mavlankar, IIM Ahmedabad has been
organized. IIM has shown keen
interest to host the meeting where in
the NGOs working with Dais and
concerned government functionaries
can be invited for a day’s meeting
with an objective to develop a
concrete strategy to strengthen the
role of Dai in health programs. He
suggested that once we receive the
documents from NGO’s, a planning
meeting could be called to review the
case studies and plan the meeting.
He suggested having the preliminary
meeting in the month of June 2000
and the final GO - NGO meeting in
the month of August 2000.
9
ANNEXURE-I
LIST OF PARTICIPANTS
Ms. Manjula Patel
Ms. Mercy Christian
St. Xavier’s Social Service Society,
Post Box No. 4088, Navrangpura,
Ahmedabad- 380009
Gujarat
Phone: 7417654
Dr. Ranjani V.
Family Planning Association of India,
FPAI
Nashabandhi Compound,
Lal Darwaza,
Ahmedabad- 380001
Gujarat
Ph: 5507230
Ms.Mirai Chatteijee
Ms. Madhu Solanki
Dr. Renuka Patwa
Self Employed Women’s Association(SEWA),
Victoria Garden, Ellisbridge,
Ahmedabad-38000 1
Gujarat
Dr. Shobha P. Shah
SEWA-Rural
Jhagadia- 393110 District Bharuch
Gujarat
Ph: 20021
Dr. P.C. Shah
(Public Health Consultant)
Crime Prevention Trust(CPT)
42/436, Green Park Apartment Sola Road,
Naranpura
Ahmedabad- 380063
Gujarat
Mr. Rajendra Dabhi
Kharid Vechan
Gramvikas Seva Trust
Sangh, S.T. Road,
Idar
Taluka Sabarkantha -383430
Gujarat
Mr. Swami Jivapuri
Bhansali Trust
Taluka Radhanpur,
Highway Charasta, Radhanpur-385340,
Banaskantha
Gujarat
Ph:77391
10
Ms. Mandaben Rishi
State Programme Director Mahila Samakhya
Society (MSS)
Govt. Polytechnic Compound
Ahmedabad -380013
Gujarat
Phone: 6306762/2935
Dr. Nikhil Kharod
Tribhuvandas Foundation Rajodpura, Anand
-388001,
Kheda
Gujarat
Ph: 51166/51266
Ms. Reshamben Kalaswa
Mr. Lakshmanbhai Paggi
SARTHI
Godhar (West)
Taluka Santrampur
District Panchamhal
Gujarat
Ph:02675-39306
Ms. Dharmishtha
Narrotam Lalbhai Rural Development Fund;
Taluka Khedbrahma,
Dist. Sabarkantha
Gujarat
Ph: 20039
Ms. Parul Bhavsar
Ms. Ketaki Desai
SRISHTI
Indian Institute of Management
Vastrapur,
Ahmedabad- 380015
Gujarat
Ph: 6758235
Vd. Ilaben Deshpande
Vd. Parul Joshi
Akhand Anand Ayurvedic College
Lal Darwaza, Ahmedabad- 380001
Gujarat
Ph: 6753303
Ms. Pallavi Patel
Ms. Ila Vakharia
Vd. Smita Bajpai
Vd. Lakshmi Bhatt
Dr. G.K.Trivedi
CHETNA
Lilavati Lalbhai Bunglow
Civil Camp Road, Shahibaug
Ahmedabad 380004
Gujarat
Ph: 2866695/8856
Strengthening Dai (traditional midwife) Tradition
Vd.Smita Bajpai and CHETNA team
(Draft not to be quoted)
The Historical Perspective
Since ancient times, pregnancy and childbirth has been women’s domain.
Women conceive and give birth in homes, with support and encouragement of
elderly, experienced and skilful women in neighborhood. They are called Dai,
Dayan or Dai Maa, meaning one who gives. Women have been nurturing the
communities since thousands of years, throughout Asia. In most rural and
remote areas of India, particularly where modernization has not yet reached,
Dai play a critical role to support other women in giving birth. Exclusively
handled by women otherwise, men are sometimes called to give a helping hand
in case of difficult birth or to expedite the process.
The Social and Economical profile of a Dai
Dai or Dayan is usually a middle-aged woman of Dalit or the oppressed caste
and poor. In the lower strata of the society, certain sub-castes perform the role
of Dai. In many states, women of the naai (barber) caste may perform the Dai's
role perhaps because of the association with their surgical tradition and
instruments. Similarly, women from chamar, basod or vankar (weaver) caste
may perform the role of Dai. In some communities, Dai is a member of the
community.
Among Rajput Thakurs, experienced and wise women of the house support
childbirth and Dai is called to cut the cord and clean up. In some tribal areas,
men may perform the role of Dai.
Most Dai's have hardly got an opportunity to go to school. Hence most of them
are illiterate or barely literate. However, their learning from life experiences
provides necessary skills to be able to support pregnancy and childbirth.
Mostly, the Dai learn her skills through apprenticeship and experience. A Dai
usually has the experience of giving birth to several children of her own.
As a young girl she accompanies her mother, mother-in-law or an elderly aunt
and observes. Gradually she starts assisting her and later on when she gains
the confidence, delivers the child on her own, with another learner by her side.
Usually, the Dai have a 5-10 years of formal learning, before she takes on the
tradition. However, some start the work, when they are compelled to support a
woman in crisis.
I
Most of them are engaged in labor or agriculture work. They support labor as a
part of their duty towards the community and assisting the woman in need.
Hence most of the Dai are economically poor. They cater to the poor class and
therefore and expect remuneration according to the condition of the family.
Many times they wait for hours together, barely drink a cup of tea and rarely get
enough money. With more and more families adopting the small family norm, the
number of deliveries is also reducing, which directly affects their meager
income.
We do this work because it is dharam ka kaam. We walk distances, wait for
hours together, risk our lives to go at any time and toil with the woman, still we
get paid very little. If the family is poor, we get a cup of tea or not even that.
Some families give us little grains or clothes whereas some give us 50-60
rupees. (A Dai from Maharashtra during healers meet organized by CHETNA)
Where as some Dai’s do benefit from the remuneration provided by the
Government, but for most, this money is difficult to obtain. At times, she has to
wait for an entire year before she gets money for her work.
Realizing the potential role of Dai during childbirth, the Government as well as
NGOs has made various efforts to strengthen the Dai tradition. This is in terms
of training, providing delivery kits, remuneration and referral services.
Government’s Efforts to Strengthen Dai Tradition
Dais represents the critical role being played by women in nurturing the health
of communities, particularly around pregnancy, childbirth and newborn care.
There are about 60,000 Dais in India. Official sources state that 50-60% of birth
are attended by Dais in rural areas (NIHFW, 1983). Studies indicate that as high
as 90% or more of births are attended by Dais (Kakar, 1972).
Over the years there has been a change in this practice to some extent. In the
areas where obstetric care is available within community’s reach, the number
of deliveries in the hospital has been on rise. With more and more families
accepting the small family norm, the number of births being facilitated by the
Dai’s is gradually declining.
During the pre independence, Dai training program were organized as an
integral part of maternity and child welfare. During the early post Independence
days, the Government of India initiated Dai training under the purview of the
MCH (Maternal and Child Health) program by the state Government.
During the second five-year plan, the Government of India initiated Dai training
program under the MCH programs as a centrally sponsored scheme. UNICEF
2.
assisted project of training Dais began in 1957 and a remuneration system for
referring women for ANC or PNC was worked out. However, not all the dais
identified could be trained
The scheme continued during the subsequent five-year plans and during the
fourth five-year plan period it was transferred to the family planning
department. Till the end of 4“’ plan, only 40-42% of the set target was achieved
(15,000/35,000).
During 1967, the Government of India, through a program assisted by USAID
made efforts to stimulate the Dai training program. Components like provision
of special midwifery kit were added with a focus on motivation for family
planning. India was probably the first country to utilize Dai’s in a national family
planning program. Another effort to boost the scheme was made in 1971 by a
decision to train 75,000 Dais. However, due to various reasons like duration of
the training, lack of backup support, delay in distribution of kits and stipend etc.
the scheme did not catch up.
During 1973, the Government of India appointed a subcommittee to examine the
functioning of Dai training scheme. As a consequence, in the fifth five year plan,
the training content was expanded to include reproductive system, and care of
mother and child during pregnancy, birth and after birth. The duration was
reduced from six to one month and dais were to attend the PHC/SC twice a
week and for remaining four days under the supervision of the ANM/LHVs. The
stipend was revised to Rs.300/-- per month and a kit was provided free of
charge at the end of training. In addition she was entitled to a payment of Rs.
21- for registration of each antenatal case at PHC and Rs. 1/- after each delivery.
Its emphasis from April 1978, financially supported by UNFPA, has been to
promote acceptability of small family norm, reduction in the rate of Infant
mortality and to improve community participation in Government health
services delivery.
Subsequently, The Government of India’s prospective pan for development of
health humanpower seeks to...’’ensure one TBA for every 1,000 population
(India, 1981)
These efforts continued in the subsequent years, with changes in Dai’s
remuneration, introduction of Disposable Delivery Kits and training with an
emphasis on coordination with the local health care system.
With the Government of India’s decision of implementing the Reproductive and
child health program in 1997, the role of Dai has become all the more critical to
address women’s health concerns. Under this program, efforts are being made
to identify and register Dai’s in every village. These Dais’, after training are
3
being recognized by the Government and paid due remuneration. With a view to
institutionalize all deliveries, a decision has been made to stop training and
recognizing new Dais.
Efforts of NGOs to strengthen Dai tradition
Realizing the crucial role of Dai in the community and the inadequacy of
Governments Dai training, various NGOs all over the country are training and
supporting Dai’s. Most of the training follow the curriculum laid down by the
Government. Additionally, there is a lot of follow up support.
NGO initiated efforts can be broadly categorized in to two
■
■
Providing training input to Dais and linking up with the health system for
services and supplies.
Initiating their own program including services, supplies and training.
Specific efforts have been made to organize Dais and form their cooperatives
(Sewa in Gujarat) with a view to empower Dais and make them self-reliant.
Few NGOs have researched for Dai practices and are making efforts for
evolving a more sensitive and appropriate model for Dai training.
Discussion and concerns
A case of mismatch
Dai training in India, by the Government and to some extent by the NGOs, has
been a case of mismatch. We have linked a traditional practitioner, who has her
own worldview, experience and way of thinking and working view with a system
based on an entirely world, view. This system fails to understand and do justice
to the Dai tradition. Hence most Dais a re laden with information that has been
given to them with little effort to learn what they know and practice. The
training has almost no space for Dais knowledge and expertise of herbs and
rituals. Some practices like applying force and pressure on the abdomen, lack
of emphasis on asepsis, calling a person to give stimulating drugs have adverse
effects on woman and the baby but there are quite a few like giving stimulating
and energy promoting decoctions, providing support and encouragement to the
woman, massage, stimulating the placenta for new born resuscitation are a few
to indicate the positive aspects of Dai practices.
The formal traditional systems of medicine have been isolated and hardly
contributed to the Dai program, an area where their contribution could be
maximum.
Often, one gets to hear that they have to counteract with a variety of deeprooted traditions, which are difficult to change. Despite this fact, the Dais
continues to be trained byANMs/LHVs/Medical doctors who have little or no idea
of Dai practices.
The outlook towards Dai
Most communities have the idea that the woman is untouchable during
menstruation and childbirth and therefore is isolated. Some argue that these
practices allow rest and prevent infections. However, such practices lead to a
demeaning attitude towards women throughout their lives. The Dai supports
women when their families, but even she isolate them, as a woman has to bear
the brunt. Class, caste and gender biases lead to shabby treatment towards the
Dai. She is viewed as one who collects and cleans the dirt, which has been
collected since nine months. The consequence is that her own need remain
largely ignored.
In a healer’s meet organized by CHETNA during 1999, the Dai’s voiced the
following needs:
We want to get a health check up done, we require transportation to move to far
places, we need torch to be able to see in bad light, we need foot wear, glasses
to wear to be able to see clearly. But where do we get these
This attitude also affects the decision for referral. More often that not, the Dai is
held responsible for delay in referral in case of complications. However, a study
done by LSPSS/CHETNA in 12 states indicated that the Dais are generally
aware of their limits, however, the decision to take the women to the hospital
largely depends on the money available in the house, the family’s attitude and
value for the woman, available of the transport system and the distance of the
hospital.
The formal health care system views Dais as community workers who are
obliged and expected to support the program and accomplish the task allotted
to them. As a result Dais are made appendages to the formal health system
with few efforts to integrate them in the program. On the contrary, Dai’s have
been meeting the community’s health needs since thousands of years and they
need the support of strong and functional back-up systems.
$
The impact of Dai training
The impact of Dai training has been felt in two clear-cut areas, one reduction in
neonatal mortality due to Tetanus and in improving the referral system. The
most common criticism to the Dai training scheme has been the fact that it has
not been able to reduce maternal mortality rates. It is important to note that for
almost 50 years after independence, we have concentrated to training Dai’s
with little or no efforts to strengthen the referral system and making obstetric
care available in the remote and rural areas. In addition, maternal mortality is a
complex issue, which cannot be addressed with a one-point intervention.
Dai’s have surely benefited from the training in terms of increased recognition
in the community, breaking the barriers of class, caste and religion, learning
aseptic measures and so on. However, it is important to note that this has to
some extent hampered the Dai profession. As a Dai in Gujarat says:
Now we do not do much work. We do not like to take the risk, so when a woman
comes to us, we ask her to go to the hospital. We are not responsible if
something happens afterwards.
This standardization of referral has proved costly to the community. What once
was available at the doorstep has now become distant and costly. As is clear
from the statement of a Dai in Gujarat.
If they go to the Doctor, they would easily have to spend one to two thousand
rupees help them at their door step and they need to spend a hundred rupee or
so.
Conclusion
The Dai’s have a critical role to play in the coming generations. It is important
that the tradition of giving births at home continues in the years to come.
However, there is a need to strengthen and upgrade the skills of Dais on an
ongoing basis.
1
It is important that the Dai training is based on her own knowledge, skills,
practices and experiences. The traditional systems of medicine (Ayurveda,
Siddha, Unani, Yoga, and homeopathy) play a critical role in understanding the
Dai practices and designing the curriculum of Dai training.
The Dai training program should be backed by strong and competent referral
system, including transport and obstetric care.
Economic viability of Dai tradition is another area, which requires lot of thought.
While the remuneration provided by the Government is essential but
inadequate, community remuneration is essential. There is a need to work out
locally acceptable remuneration systems, in terms of cash and kind. This will
also help to portray Dai tradition as a trade and encourage new Dais to take up
this profession.
Lastly, meeting the Dais own needs of health care and other supplies besides
the delivery kit is another concern. Some of the needs could be taken care if an
acceptable remuneration system is set up. However, there is a need to look
seriously to the health needs of the Dai.
References:
Her Healing Heritage; Vd. Smita Bajpai and Dr. Mira Sadgopal; CHETNA; 1996
Traditional Practices in the area of Mother and Child Health Care; A review of
literature; Lok Swasthya Parampara Samwardhan Samiti; 1989
A report on Guni Sammelan; CHETNA; 1999
1
NGO organises meet for
midwives in Ahmedabad
EXPRESS KEWS SERVICE
/-;C, '•/ The main aim of the development
I AHMED.A3W1. aPRiL 18
''
'and support of dai programme is ta .
’
'
' bring a reduction in both female and -'
TN a firf-g tribute to dais (mid- infant mortality rate, - j," j: ’ /
1 I wives), tee Centre for Health Ed’Since 100 per. cent institutionJLucatiom Training and Nutrition.:. alisc(} deliveries are not possible in
Awareness fCHETNA), a non-gbyg^j j|jc country, efforts are being made to.
delivery easier for the women
ernmental neganisation, orgariisea. a;-A
■ meet for them on World Heritage '?• far.pun£, comers of the country.
About 30 dais and several nonDay in Ahmedabad. C.;
? • More that 70,000 dais play a
governmental organisations working
cal role in pregnancy and childbinh^ towards training the midwives atin the remote rural areas as welfasj’ tended the day-long meet to exthe city slums in the
change views and debate one the ex> . The-Centre has been taking var^ .sting prob]ems.
. . ' ■
The rCpresentatives of SEWA
ous efforts tp strengthen the traciitio^
... ...
Rural, a pioneering non-goveimmenof dais,
P
In Gujarat alone, out of 12 lakh^ taJ orgaAisation the field of tram-,
ing midwives, brought relevant points
deliveries annually, eight lakh take
place in the rural areas and 80 per
, . C"
,
to notice/ ;
cent of the-rural deliveries are as- /
The organisation has taken tn
( help of the local hospital in training
sisted by the midwives.
midwives.
;
. ? , . . n
Even in urban areas, about 50 per ' dais.
*~i—'—"
Swatiben said this ensured that a
place in
. cent of-the child-births-take
the slums and are assisted by the midy - rapport and co-ordinatiom evolved
bctweenthemidwivcsandthehospi' wiyes^T- ■-! <; •.. z r. ■- ■ ; .iSv-y
;
7'Mirai'Chatteriec of .SEWA re- -' tai authorities and nurses besides givVailed that most government officials .< inc the former more credibility.
^Apart from this, the expectant
; feTfthatthe dais. irt spite of extensive y.
ttrafeirig and speoi^lfund.allocation, - mother and her family members are
.
trained to handle delivery’ in emer^ve not been4lfle to curb the mor-'
gency situations.
cates of botfi the new-bqms and
r^uiuuiwii
•-•7-r
•
•being provided to
kits are also
Dai...
; themotiK:rs. ;/X' '\■ ?.
Another participant in the meet ‘ expectant mothers to facilitate easy
C.Shah, however, pointed out
T?>Ff QShah,
delivery. However, it was largely obthat'a significant rise inihe number ! served that the 'injection culture’ is
present among the rural population.
of gynaecologists also has not
Concerns were also raised about
brought down the mortality rates.
i
the
prevalent dai-dqctor nexus.
’
Dr Shah felt that midwives could
A
representative said that these
contribute to reduction in reduction
unauoiviuw^v.
. • f doctors are called after the delivery
■ of
. ■...
.•
female mortality.
Shah felt that midwives, should- ■ and they gave injections which
have
information about
adequate information
the JJ not
have adequate
about th£
not required and charged a ht^fy fee
facilities available at various Primary j for the same.
Health. Centres (PHCj ^nd Civil j
.
■ 7
//
rV;
Hospitals. V 7 /7-.
...
•
_
Z
.
V
V.-*.
'r«
'r-
I. LAW! **
--
•
.
• «.
___ .^L _'*«•». am ♦■Ka
— — —- - —
-
J
* .
nlim^/»r
’ J.
*.
/
f
Centre For Health Education/Training & Nutrition Awareness,Lilavatiben
Lalbhai's
Bungalow,Civil Camp Road, Shahibaug, Ahrnedabad-300 004, Gujarat, India .
Ph: 91-079-2866095/ 2868856 / 2865636 Fax ; 91-079-2866513
Email : chetna@icenet.net Website-^www.icenet.neLhi/chetna
Website : »ww.iccnet.net.ln/clieln»
Position: 2598 (4 views)