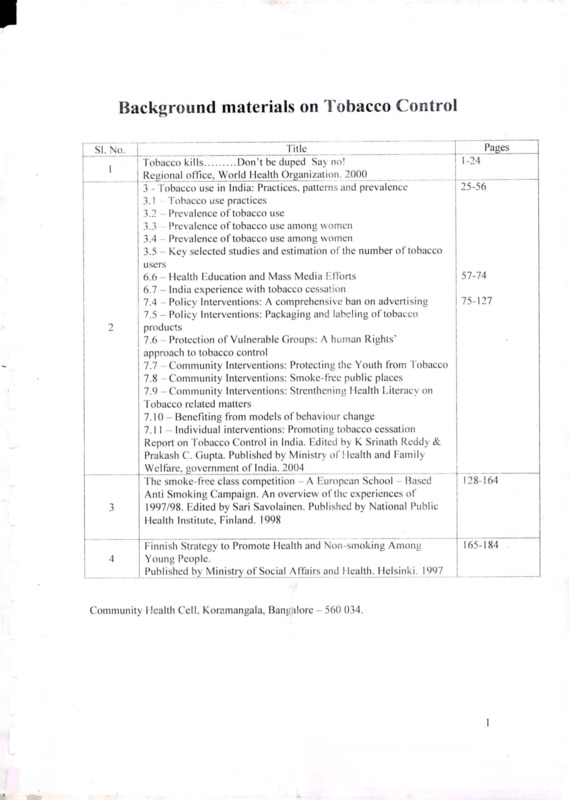
Background materials on Tobacco Control
Item
- Title
-
Background materials on Tobacco Control
- extracted text
-
Background materials on Tobacco Control
SI. No.
I
2
3
4
Title
____
' Tobacco kills
Don’t be duped Say no!
Regional office, World Health Organ[zation. 2000
3 - Tobacco use in India: Practices, patterns and prevalence
3.1 Tobacco use practices
3.2 - Prevalence of tobacco use
3.3 Prevalence of tobacco use among women
3.4 Prevalence of tobacco use among women
3.5 - Key selected studies and estimation of the number of tobacco
users
6.6 - Health Education and Mass Media Efforts
6.7 - India experience with tobacco cessation
7.4 Policy Interventions: A comprehensive ban on advertising
7.5 - Policy Interventions: Packaging and labeling of tobacco
products
7.6 Protection of Vulnerable Groups: A human Rights’
approach to tobacco control
7.7 - Community Interventions: Protecting the Youth from Tobacco
7.8 Community Interventions: Smoke-free public places
7.9 - Community Interventions: Strenthening Health Literacy on
tobacco related matters
7.10 - Benefiting from models of behaviour change
7.1 1 - Individual interventions: Promoting tobacco cessation
Report on Tobacco Control in India. Edited by K Srinath Reddy &
Prakash C. Gupta. Published by Ministry of Health and Family
W el fare, govern men t of India. 2004
The smoke-free class competition A European School Based
Anti Smoking Campaign. An overview of the experiences of
1997/98. Edited by Sari Savolainen. Published by National Public
Health Institute, Finland. 1998
Finnish Strategy to Promote Health and Non-smoking Among
Young People.
Published by Ministry of Social Affairs and Health. Helsinki. 1997
Pages
1 -24
25-56
57-74
75-127
128-164
165-184 .
Community Health Cell, Koramangala, Bangalore - 560 034.
1
H
?
a,
5
6
f
\
7
Control of Tobacco Habits
Smoking habits
Tobacco control in India
Tobacco Research and Interventional Studies in India
Tobacco and ArecaNut by V M Sivaramakrishnan. Published by
Orient Longman, Bangalore. 2001____________ ________
Appendix 3 - Health effects associated with exposure to Second
hand Smoke
Appendix 4 - Countering the opposition
Protection from Exposure to Second-hand Tobacco Smoke - Policy
recommendations. WHO, Geneva. 2007
Crowding out effect of tobacco expenditure and its implications on
household resource allocation in India by Rijo M. John.
Social Science and Medicine, 66 (2008) 1356-1367
185-233
234-241
242-253
2
•y-v- 'S13S'??fSs’5?S!S§
SWMtW
^^aG^-lciliS
;c.7Si K-Tad
J J:
Ml
i■
WBs
twww
I?r
.^3'=
I
v
Q
L Zb/ Fi- (x
hM \ J f
h- • /-'. (
CW.
TWfe
^:^'-. /^7/
J .
£
KJ•*
v^®'"
;?u>;
^®gV1'
■J.
I^Jfc.
I
■PS^
-
VorjiS^Tobacco Day
’
2000
[
3
swg'SasSK;.
1
[ealth Organization
fc MediterraneanIHilfgional Office
Contents
Message from the Director General--------------------
3
Message from the Regional director------ -------------
5
The health dimension of the tobacco problem---------
8
The tobacco industry’s war on public health----------
12
From the horse’s mouth: the tobacco industry speaks
16
Reducing the glamourization of tobacco in movies,
I
on television and on music videos--------------------- -
20
A message to all youth from Duraid Lahham-------
28
Tobacco control legislation and its implementation
30
Islamic rulings on smoking----------------------------
37
The Christian view on smoking-----------------------
43
Celebrities killed by Tobacco
46
Message from
Dr Gro Harlem Brundtland, Director-General
of the World Health Organization for
World No Tobacco Day 2000
Every day, 11000 people die due to a tobacco-related disease.
Tobacco is a communicated disease—communicated through
advertising and promotion for which the tobacco industry spends
billions of dollars. Tobacco advertisements talk to us from our streets,
films, radios, television sets and sports events. Everywhere our
children and we turn, there is something or someone telling you to
smoke.
What -makes all this unacceptable and treacherous is that this
dangerous and addictive product is sold to youth and adolescents as an
assertion of their freedom to choose. One of the primary objectives of
the tobacco industry is to frame tobacco use as an individual and
behavioural decision. The deception in this casting is that it leaves the
tobacco industry’s activities and practices completely out of the
equation. It assumes that people make their decisions in a state of
vacuum, completely uninfluenced by the environment of industry
advertising and marketing.
Research shows that people’s decision to smoke is influenced by
tobacco industry promotion. Tobacco advertising featuring prominent
sports and entertainment figures project and reinforce and image of
tobacco as glamorous, firn, healthy, sophisticated and wealthy. In
countries where advertising bans are beginning to emerge, subtle
product placement in films and film videos continue to send these
messages to young people. By the time people find out, it is often too
late.
So what is it that the tobacco industry spends billions of dollars to
conceal? They want to suppress truth that documents their
manipulation of nicotine to levels that ensure that addiction occurs and
is sustained. Truth that shows us that the tobacco industry privately
3
develops strategies to market to children while publicly claiming the
contrary. Truth, that instructs us that it is hard, if not impossible to
find any parallel in history where people who have gone about in such
a systematic way perpetuating death and destruction have gone
unpunished and unquestioned.
Our decision to focus on the entertainment, films and sports
industry for World No Tobacco Day this year is a carefully thought
one. It is unconventional and unorthodox, but that is precisely why we
have chosen it—the tobacco industry strikes where people least
suspect it to be. Global advertising bans is also one of the early
protocols that will be negotiated by WHO’s 191 Member States
working on the Framework Convention on Tobacco Control. The
decision to highlight that early in the treaty-making process is no
accident—it is our answer to calls from our Member States seeking an
urgent global response to a global menace.
Together, we can hold up mirrors to their practices. Together, we
can buck the tobacco tide that is set to claim 10 million people by
2030, over 70% of them in the developing world. To those young and
not so young who might be debating whether or not to start smoking,
1 would like to say, “tobacco kills—don’t be duped.”
Message by
Dr Hussein A. Gezairy
Regional Director
WHO Eastern Mediterranean Region
on the Occasion of World No Tobacco Day
31 May 2000
As I was completing this message on the occasion of World No
Tobacco Day, a friend of mine asked me the following question: why
does the World Health Organization put such a strong emphasis on
tobacco smoking when everyone is fully aware that smoking is
extremely harmful to health? He added: every smoker knows this fact
and feels it in his poor health and his vulnerability to many diseases
and the rapid deterioration of his health.
That many people are generally aware of the harmful effects of
smoking is one thing, but knowing the full extent of such effects and
the health, social and economic consequences of smoking is
something else. Who, among the vast majority of people, realizes that
in the few minutes a person needs to read this message, smoking will
have killed 60 more people? How many of us realize that tobacco
smoking kills more than 10 000 people every day? As for the diseases
directly related to smoking, these are countless. It is sufficient to state
that if everyone were to stop smoking completely, and if no one were
to light up a cigarette or puff out tobacco smoke, the world would be
spared one-third of all cancer cases, a substantial proportion of
cardiovascular diseases would be prevented, and a further substantial
reduction would be achieved in the number of cases of many serious
and killer diseases. The fact is that smoking is a more fatal killer than
wars, natural disasters and epidemics.
Nevertheless, smoking remains acceptable in many social
environments. Smokers continue to puff away at home and at work,
paying no heed to the extensive and serious harm to which they
4
5
expose their families and colleagues. The tragedy is that the number
of smokers is increasing, and its tragic consequences are rapidly
mounting. According to WHO’s estimates, the number of smokers in
the world today is in excess of 1.25 billion, which is more than
one-third of all people above 15 years of age. If the present trends
continue, this number will continue to rise. By the year 2020, the
number of victims which tobacco kills all over the world will reach 10
million every year, or more than 10 000 every hour of the day and
night.
Despite all the health problems tobacco smoking causes, powerful
interests including multinational companies and prosperous national
industries continue to promote tobacco, targeting adolescents and
women in particular. The tobacco industry is always trying to
compensate for the loss of those of its customers killed by its evil
product. It tries to give smoking a false glamour and an adventurous
aura that it does not have. By so doing, it seeks to attract teenagers
before they gain a full picture of the harmful effects of tobacco and
the hard addiction it causes.
At the same time, officials in certain sectors, such as agriculture,
industry and taxation, imagine that they make large financial and
economic profits from tobacco growing, sale and consumption. But a
proper balance sheet of profits and losses attributed to tobacco will
immediately reveal that the losses incurred by every country of the
world in consequence of smoking far outweigh the profits it makes.
This is true when we include just the hard figures of material gain and
loss. The human loss, in terms of morbidity and mortality, however, is
too great to be balanced against any financial revenue that by contrast
will remain paltry, no matter how high its figures are.
also helps smokers to quit their harmful habit. Such an effort should
also contribute to rescuing the world from the scourge of smoking and
to achieving a tobacco-free world.
But these goals cannot be achieved except through a common
effort in which all take part. Every year the World Health
Organization seeks to enlist the support of one sector of society in the
fight against tobacco with an aim of preventing its promotion. This
year we are trying to enlist the support of all who work in the
entertainment sector, including the media. When we look around, we
find that tobacco promotion seeks to portray smoking as glamorous
and fun. We also see places of entertainment, such as cafes and places
of recreation, providing facilities that encourage people to smoke.
Many hotels and clubs have introduced what they describe as a
Ramadan tent in which the sinful practice of smoking, particularly
waterpipe, is encouraged, and thereby they defile the month of
worship. Women’s smoking of the waterpipe has recently become
very common in these places, while it used to be totally unknown.
The fact is that all this promotion relies on absolute falsehood.
There is in fact no pleasure to be derived from smoking. Pleasure is to
be sought in practices that promote health and prevent disease. Thus
the World Health Organization appeals to all men and women who
work in the entertainment, sector to join it in its strong stand against
tobacco and to contribute to the worldwide effort to protect our young
against the temptation to smoke and to free our world of tobacco. This
is highlighted in the slogan we raise this World No Tobacco Day:
Don’t be duped... tobacco kills.
May God bless you all.
f
C__ , I.
The tragedy represented by tobacco smoking cannot be overcome
except through a collective effort in which all sectors cooperate,
including education, health, media, religion, agriculture, industry and
finance. In this joint effort, measures taken by governments should
support and complement efforts made by individuals and voluntary
organizations. They should all contribute to an integrated effort that
seeks to protect adolescent boys and girls from starting to smoke and
6
Dr Hussein Gezairy
Regional Director
7
The health dimension of
the tobacco problem
Four million people are killed by tobacco every year. For the
smoker, however, this does not happen out of a sudden. Death comes
as the result at the end of a long series of suffering and illness.
Tobacco smoke contains no less than 4000 chemical compounds
which are harmful; 500 of these are very harmful, and 43 are complete
carcinogens, i.e. cancer causing agents, in their own right. Smoking is
also harmful in the short term. The irritant substances in tobacco
smoke can cause a build up of phlegm and a smoker’s cough. Tobacco
smoke also reduces the efficiency of the lungs, making people more
breathless than they would normally be during situations of
rest-exercise, or sudden physical exersion. Furthermore, smoking
reduces the ability of the lungs to fight infection, which makes
smokers more likely to get different types of chest infections.
However, the worst types of the health effects of tobacco smoking
appear only after many years of continuous smoking. This is the
reason why young smokers continue to turn a blind eye to the harm
they inflict on themselves by smoking. The fact remains that a large
number of fatal and life-threatening diseases are caused largely or
entirely by smoking. These include chronic obstructive pulmonary
disease, vascular diseases at various critical sites and several forms of
cancer. A study by the American Cancer Society found that 'cigarette
smokers had ten times the risk of dying from chronic obstructive
pulmonary disease than non-smokers. It also established that about
three-quarters of deaths from this disease were attributable to
smoking. In a prospective study of male British doctors,, cigarette
smokers had 13 times the risk of dying of the disease compared to
non-smokers.
The number and types of cardiovascular diseases caused by
smoking is large indeed. These include coronary artery disease and
heart attacks, aortic aneurysms which can lead to sudden death,
carotid artery disease which can lead to strokes and peripheral
8
vascular disease which, in the lower lipibs, can lead to severe pain in
the leg on walking and may necessitate amputation.
The list of diseases known to be associated with smoking includes
cataracts, hip fracture (osteoporosis), and periodontal disease.
As for cancer, it is well established that smoking is the direct cause
of the overwhelming majority of cases of lung cancer. Smoking and
alcoholic drinks are the two main causes of cancer in the oral cavity
and the larynx. When both risk factors are present, the total risk is
higher than the sum of the two risks taken separately. Other cancers
caused by smoking are those of the pharynx, oesophagus, stomach,
pancreas and bladder. Smoking is also related to other cancers in the
head and neck.
This is a summary of what tobacco smoking causes to smokers.
What it causes to non-smokers is in no way less serious or less
extensive. In its report of 1998, the British Scientific Committee on
Tobacco and Health outlines the effects of environmental tobacco
smoke, making the following conclusions:
® Exposure to environmental tobacco smoke is a cause of lung cancer
and, in those with long term exposure, the increased risk is in the
order of 20%-30%.
Exposure to environmental tobacco smoke is a cause of ischaemic
® heart diseases and if current published estimates of magnitude of
relative risk are validated, such exposure represents a substantial
e public health hazard.
Smoking in the presence of infants and children is a cause of serious
respiratory illness and asthmatic attacks.
Sudden infant death syndrome, the main cause of post-neonatal
• death in the first year of life, is associated with exposure to
environmental tobacco smoke. The association is judged to be one
of cause and effect.
• Middle ear disease in children is linked with parental smoking and
this association is likely to be causal.
9
In addition women g
are at an increased risk i
of cancer of the cervix as ■
a result of smoking. |
Women who smoke and 8
use contraceptive pills 8
run a higher risk of I
Deceptive and
suffering a stroke or a |
alluring
practices
heart attack. Smoking J
employed by
causes
complications |
tobacco
during pregnancy and
companies have
harms the developing baby.
successfully
Mothers who smoke put
drawn women
their own health at great
and girls into the
claws of
risk, and they also expose
smoking
their babies and young
children to all the risks of
passive smoking.
These facts give a clear indication of the magnitude of the
problems faced by health authorities as a result of tobacco smoking.
But the problem is ever on the increase. The number of smokers
throughout the world continues to rise, and a small percentage of
smokers try to quit, with only a moderate rate of success.
yields. People seeking treatment for heroin, cocaine, or alcohol
dependence rate cigarettes as hard to give up as their problem drug.
The aversiveness of nicotine withdrawal is an important factor
underlying the failure of many attempts at cessation."
Furthermore, a habitual smoker more than doubles the risk of
dying before the age of 65. The best health investment anyone can
make is never to smoke. Giving up smoking is the best measure a
smoker can take to improve his or her health. Should all smokers stop
smoking and no one light up again, more than one-third of all cancer
cases would be avoided.
Today, there are different ways to help smokers who wish to quit
the habit. These should be rpade available in hospitals, primary health
centres, pharmacies and oth^r health facilities.
It is important to remember that the choice we have is always one
between tobacco or health. The two are at opposite extremes and
cannot meet up.
Most Member States in the Eastern Mediterranean Region have
taken measures aimed at curbing the spread of the smoking epidemic.
Nevertheless, the problem is still on the increase, due to three highly
important reasons. The first is the fact that tobacco is addictive. The
Report of the British Scientific Committee on Tobacco and Health
states: "Nicotine has been shown to have effects on brain dopamine
systems similar to those of drugs such as heroin and cocaine, and with
appropriate reward schedules it functions as a robust reinforcer in
animals. Dependence on nicotine is established early in teenagers'
smoking careers, and there is compelling evidence that much adult
smoking behaviour is motivated by a need to maintain a preferred
level of nicotine intake, leading to the phenomenon of nicotine
titration, or compensatory smoking in response to lowered nicotine
10
11
Tobacco kills—don't be duped
The tobacco industry's war on public health
The tobacco industry has declared war on public health. A cigarette
is the only consumer product which, when consumed as indicated,
kills. Tobacco is a powerfully addictive substance and the tobacco
industry has subverted science, public health and political processes to
sell a product that addicts its consumer before killing them. Available
data shows that two-thirds of today's smokers started in their teen
years. Far from being a bunch of tobacco leaves rolled into paper
tubes, a <cigarette is a highly engineered product designed to addict and
kill.
Manufacturers are concentrating on the low TPM ["total
^articulate matter] tar and nicotine segment in order to
■reate brands... iwhich aim, in some^ way or another; to
reassure the consumer that these branfls are relatively more
healthy” than orthodox blended cigarettes.
P.L. Short, British American Tobacco Company, "A new Product, 1971
*
*
*
Lies and more lies
One of the primary objectives of the tobacco industry is to frame
tobacco use as an individual and behavioural decision. The deception
in this casting is that it leaves the tobacco industry's activities and
practices completely out of the equation. It assumes that people make
decisions in a state of vacuum, completely uninfluenced by their
environment including industry advertising and marketing.
“The tobacco companies spend US$6 billion a year enticing youth
to smoke. They make you believe that if you smoke, you re going to
be sexy, attractive, successful, accepted by your peers, rocking, and
macho, cool and sassy. They project this image in every media —from
day time movies to night-time movies, magazines and even cartoon
12
characters,” says former “Winston” man turned tobacco control
activist Allan Landers.
Research indicates that the decision to smoke is affected by
tobacco industry promotion. Tobacco advertising featuring prominent
sports and entertainment figures project an image of tobacco use as
glamorous, fun, healthy, sophisticated and wealthy. In countries
where advertising bans are beginning to emerge more subtle product
placement in movies and music videos continue to send these
messages to young people. By the time people find out, it is often too
late.
*
*
*
The threat concerns us all
The tobacco industry acts as a global force sparing no nations and
peoples. There are no true economic or public health arguments in
favour of tobacco as it kills human beings and saps national treasuries.
Tobacco has killed four million people this year. By the 2020s or the
early 2030s, that preventable death toll will rise to 10 million deaths
per year. The tobacco industry and their marketing henchmen need
some 11 000 new smokers every day to replace those they kill. So
they target our children and sell addiction and death as an act of
freedom, rebellion, free choice, sophistication and success.
to ensure increased and longer term growth for the Camel
Filter, the brand must increase its share penetration among
the 14-24 age group which have a set of more liberal values
and which represent tomorrow's cigarette business.
1975 Memo to C.A. Tucker, Vice-President For Marketing, R.J. Reynolds
*
*
13
*
'•#
®
■“
Chuntering the deception
Every eight seconds a person dies of a tobacco-related disease and
almost as quickly another victim is recruited. Big tobacco trades in
death and decepijog^his assault on world health has got to stop. The
WHO has risen to this global challenge. At the core of this response is
the creation of Jhe world’s first legally binding international treaty
dedicated to human health. The WHO Framework Convention on
Tobacco Control (FCTC) will address such issues as advertising bans,
smuggling, taxes and agricultural diversification with a view to
crafting a global response to a global menace.
I
As tobacco control action begins to reduce markets in the west,
transnational tobacco companies are aggressively extending their
global reach. The FCTC will provide a powerful political platform
upon which all the nations of the world can unite and strengthen their
capacities to counter the deadly and deceitful cross border tactics of
the transnational tobacco companies.
If you still believe the industry is simply stuffing tobacco into
paper tubes, not fine-tuning nicotine delivery, consider this
quote from a senior scientist working for a tobacco
company, uncovered recently from a longfhidden document.
In 1972, he said: athe cigarette.should not be construed as a
product but a package. The product is nicotine. Think of the
cigarette as a dispenser of a dose unit of nicotine. Think of a
puff of smoke the vehicle of nicotine. ”
bans, etc) is not known in Sri Lanka or Mexico. On the other hand
unregulated marketing to youth and women in developing and
developed countries in transition (cigarette discos, golden cigarette
contests, etc) which are systematically denied in the west have not
been sufficiently exposed. To ignite this tobacco curtain and build
global support for the FCTC, the WHO has developed the “tobacco
kills-don’t be duped” media initiative.
This new media initiative will systematically attempt to reframe
public perception of the tobacco problem by giving the health and
political community the tools needed to begin to expose and combat
the enormous resources and deceitful tactics of the transnational
tobacco companies.
Obviously there is enormous potential in all these countries.
I would say that the demand for Western cigarettes is
insatiable. It's a fantdstic opportunity for everybody, and
we're talking in any number of countries.
Stuart Watterton, BAT Director of New Business Development speaking of new
opportunities iniEastem Europe and the former Soviet Union, 1995
They've got a good buffer. No matter how badly things go in
the United States, international sales will carry them along.
Allan Kaplan, tobacco analyst at Merrill Lynch & Co. commenting on Phillip
Morris, 1997
WHO Director General Dr Gro Harlem Brundtland to the Ninth International
Conference of Drug Regulatory authorities, Berlin, 27 April 1999
*
*
*
Igniting the tobacco curtain
Key to big tobacco extending its global reach has been aggressive
marketing and advertising and the creation of a new “tobacco iron
curtain”. What is going on in the west (European Union legislation,
huge tobacco company settlements in the United States, advertising
14
15
From the horse’s mouth:
the tobacco industry speaks
I do not believe that nicotine is addictive.
Thomas Sandelfur, Chief Executive of Brown & Williamson
*
*
*
Recent rcvekitions of corporate documents disclosed in litigation
and associated Wstigations, give compelling evidence for the
longstanding interest of various tobacco companies in young smokers.
The following is an ovendew of statements made by these companies.
Evidence is now available to indicate that the 14- to 18year-old group is an increasing segment of the smoking
population. RJR must soon establish a successful new brand
in this market if our position in the industry is to be
maintained over the long term.
RJ Reynolds planning forecast stamped "secret", 15 March 1976
J believe that nicotine is not addictive.
William Campbell, Phillip Morris
*
*
*
And I too believe that nicotine is not addictive.
James Johnston, R.J. Reynolds
CEOs testifying under oath before Congressional Health and Environment
Subcommittee, 1994
Our attached recommendation...is another step to meet our
marketing objective: To increase our young adult franchise.
To ensure increased and longer-term growth for Camel
Filter, the brand must increase its share penetration among
14-24 age group which have ajnew sit of more liberal
values and which represent tomorrow's cigarette business.
23 January 1975
*
*
*
Nicotine is addictive. We are, then, in the business
of selling nicotine, an addictive drug.
Addison Yeaman, Brown & Williamson, 1963
over the iong
...if our company is to survive afid ffrpsper,
term we must get our :share, of the youth market. In my
opinion this will require new brands tailored to the youth
market.
Claude Teague, RJ Reynolds, Researcher, 1973
*
*
*
Smoking and cigarette for the beginner is a symbolic act. 1
am no longer my mother's child, I'm tough, I am an
adventure, I'm not a square... as the force from the
psychological symbolism subsides, the pharmacological
effect takes over to sustain the habit...
Phillip Morris, Vice President for Research and Development,
"Why One Smokes," first draft, 1969
16
If the last ten years have taught us anything, it is that the
industry is dominated by the companies who respond most
effectively to the needs of young smokers.
Overall Market Conditions 1988, Imperial Tobacco Ltd (TTL)
Since how the beginning smoker feels today has implications
of
for the future of the industry, it follows that a study
:
. this
17
Another popular means of keeping cigarette brands in the public
eye and circumventing restrictions on advertising using cigarette
logos on other products such as caps and t-shirts. Many of these
products are popular with children around the world, and they soon
become walking cigarette advertisements.
Counteradvertising can be a useful addition to a tobacco control
campaign
Excitement, adventure and masculinity., harsh
strong psychological pressure is exerted by the
tobacco industry on children and young people
through advertisement
area would be of much interest. Project 16 was designed to
do exactly that-leam everything there was to learn about
how smoking begins, how high school students feel about
being smokers, and how they foresee their use of tobacco in
the future.
Ads for teenagers must be denoted by lack of artificiality,
and a sense of honesty
Serious efforts to learn to smoke occur between ages 12 and
13 in most cases.
The adolescent seeks to display his new urge for
independence with a symbol, and cigarettes are such a
symbol since they are associated with adulthood and at the
same time adults seek to deny them to the young.
Kwechansky Marketing Research Inc, Report for Imperial Tobacco Limited,
Subject: "Project 16", Date: 18 October 1977
18 ,
In countries around the world, young people are exposed to highly
effective tobacco advertising on a daily basis. Tobacco companies
spend billions of dollars each year to promote tobacco products, an
amount which dwarfs the resources available to most tobacco control
programmes. Thus, one important requirement for an effective
prevention programme is to seriously limit the ability of the tobacco
industry to hook a new generation of smokers through advertising.
At the’ same time, a number of countries have produced
anti-tobacco advertisements for distribution via mass media. Many of
these ads are targeted at young people, with the aim of
de-glamourizing tobacco. There are often possibilities for free
distribution of these ads in the form of public service announcements.
However, they are only useful if they are seen, and not broadcast only
during times when most viewers are asleep. In some • situations,
carefully selected paid counter advertising campaigns may be worth
the cost. In the USA, Doctors Ought to Care (DOC) pioneered the
concept of using paid counteradvertising to ridicule brand name
tobacco advertising and promotion.
Health interests can never hope to match the spending by tobacco
interests on paid media advertising, and probably should not try.
However, paid media advertising, when used with precision, can be an
effective tool in a comprehensive effort to discourage tobacco
consumption. One way of funding this would be to use a portion of
increased cigarette taxes for this purpose. Examples of this strategy
may be seen in several states in the USA as well as in other countries,
such as Australia, France and New Zealand.
■*
»
19
Reducing the glamourization
of tobacco in movies,
on television and in music videos
Four steps the entertainment industry can take to reduce the
glamourization of tobacco:
When tobacco is glamourized in movies, on TV and in music
videos, it sends a powerful message to young people that tobacco use
is both appropriate and desirable.
Following are four steps the entertainment industry can take to
discourage teenage tobacco use:
1. Avoid glamourizing tobacco. Refrain from portraying tobacco use
as something that is exciting, cool or sexy and linking tobacco with
adventure, fun and celebration.
2. Creatively substitute other props. Consider means other than
tobacco-type cliches for portraying rebellion, celebration and
relaxation.
3. Portray the reality of tobacco use. People become sick and die from
using tobacco. Most smokers would like to quit but have a difficult
time because of the highly addictive nature of nicotine.
Environmental tobacco smoke impacts the health of non-smokers.
The majority of people in the world do not smoke and prefer to live
in a smoke-free environment.
4. Work toward reducing overall tobacco use. Avoid creating an
image that smoking is a normal, daily activity. Refrain from having
characters use tobacco in inappropriate situations such .as around
children, in medical care facilities and in non-smoking areas.
rarely reflect realityi Tobacco use is not exciting or glamorous. Many
stars have died from tobacco-related diseases.
Encourage others to watch what they are watching. As a young
person, talk with yourfriends about tobacco use in the movies and on
TV. As a family, watch movies or TV and discuss the difference
between the portrayal and reality of tobacco use. As a teacher or youth
group leader, consider teaching a unit on critical viewing skills.
Work to raise public awareness. Host local youth-based media
events around the time of the Oscars or your local award ceremonies.
Contact your local movie and TV critics and ask that they write
articles on the issue. Copy and distribute this packet at health fairs,
World No Tobacco Day, and other events that promote health and/or
tobacco education. Be creative!
Why is tobacco included in movies and on TV?
There are several reasons why tobacco finds its way into movies
and TV programmes.
It is a convenient prop. If yow^anf,,to establish that a teen is
rebellious put a cigarette in his or her fend.
It may depict reality.
It can reflect the personal attitudes alid use of tobacco by writers,
directors, actors and actresses. Itinay result from direct or indirect
influence by the tobacco industry.
It may be used its a marketing tool to reach specific audiences.
Do a study
Watch what you are watching. Inoculate yourself against the
pro-tobacco messages you receive from entertainment productions.
Recognize that movies and TV are for entertainment and that they
Many studies have been conducted to test the manner and
frequency of tobacco usage in the movies and on popular television
programmes. An example of one such study comes out of California
in the United States. It was conducted by Thumbs Up! Thumbs
Down!, a project of the American Lung Association of
Sacramento-Emigrant Trails. The study looked at all movies with a
domestic box office income of more than $5 million in the time frame
from May 1994 through April 1995. It reviewed television shows over
20
21
Three other actions that will make a difference
six-week period in the spring of 1996. These are movies and
programmes that are screened all the world, not just the US, and have
enormous appeal to teenagers everywhere. Following are the key
J
1h
j .•
findings:
. L;-.
Hollywood gets a Thumbs Up! and a Thumbs Down.'m the amount
of tobacco use. Approximately 50% of the 133 movies reviewed had
zero to 10 incidents of tobacco. The other half ranged from a moderate
11—20 incidents to a smoke-filled 100 plus incidents. Television fared
better with only 15% of the 238 episodes watched containing tobacco.
Overall, movies averaged 10 incidents per hour and television two.
Use varies considerably by studio and network. Studios with low
tobacco use included Walt Disney Pictures, Twentieth Century Fox
and Hollywood Pictures. On the high side were Miramax, Castle Rock
and Warner Brothers. On television, ABC had the lowest incidence
while Fox was highest.
Leading actors are more likely to light up in the movies. In the
movies and television programmes which included tobacco use, one or
more leading actors and actresses lit up 82% of the time in movies and
57% of the time on TV.
^.j are the tobacco of choice. In the movies
Cigarettes and cigars
86% displayed
cigarette use, 52% cigar use,
where tobacco was used,
i
...
12% pipe use and 7% smokeless tobacco. On television episodes with
tobacco use, 67% displayed cigarette use, 42% cigar use and 3% pipe
use. There was no smokeless tobacco use displayed.
So what if your favourite actor lights up on screen?
The entertainment industry has a pervasive influence on our
society. While movies and television may reflect our life styles, they
also help define them. The power of the entertainment industry in
influencing young people suggests that it also has a responsibility to
monitor and reduce the potentially negative impact of its messages on
this audience. One area where it can play a particularly important role
is in helping to discourage tobacco use.
22
.jH,
©®
i:.
me iaiiiuus actor auh juiiaiii nas quit smoking, deciding for himself
without waiting for a doctor recommendation. As a respectable
actor, he will surely stop using cigars or cigarettes in the ads for his
works.
Bask tobacco facts
Tobacco kills 4 million people a year around the world. According
to the World Health Organization, it is the single most preventable
cause of death and disease in the world. In addition to the tremendous
suffering it creates, tobacco use costs the United States alone close to
$100 billion annually in health care and days missed from work. Do
you know what the costs are in your own country? It is a price we all
help pay, whether we smoke or not.
Adults don't make the decision to start smoking: young people do
Each day between 82000 to 100000 teenagers light their first
cigarette. Tobacco use starts in early adolescence. Almost all
first-time use occurs before graduation from high school. People who
start smoking at an early age are more likely to develop severe levels
of nicotine addiction and are more likely to die early of a
tobacco-related disease than people who start later.
Why do young people start? A teenager is much more likely to
light up if his or her parents, brothers or sisters smoke. Peer pressure
is also a powerful influence. The most common offer of a first
cigarette is from a friend. Certainly, the massive advertising campaign
carried out by the tobacco- industry plays a part. Billions go toward
23
It represents rebellion. Lighting up becomes a symbol for
challenging a repressive system, whether that system is your parents
or the government.
It's a way of relieving stress. As tension mounts, people light up.
making the Marlboro Man and his counterparts attractive to children.
Whether it is popularity, beauty, adventure, wealth or uniqueness, the
tobacco industry and its legion of public relations firms have a
multitude of ways suggesting it can be had for the price of a puff. Kids
with low levels of self-esteem and a sense of alienation are especially
vulnerable to the industy's relentless campaign.
Che rale off the entertainment industry
What role does the entertainment industry play in this process'?
When tobacco is glamourized in movies, on TV and in music videos,
it provides a powerful message that tobacco use is an appropriate and
even on desirable activity. Whether the glamourization is intentional
or not, it reinforces the multi-billion dollar advertising campaign
carried out by the tobacco industry. In some ways, it may be even
more effective. No warning label is required when actors and actresses
light up. What the young person sees is someone he or she looks up to,
living a life that he or she would like to live, and doing it while using
tobacco.
I
^LM x^|
I
Creativity has nothing to do with smoking. A successful person is not
necessarily a smoker and should not be.
There are three major ways tobacco use is glamourized:
It's fun. Cool, attractive and successful people light up and they use
tobacco while they are doing exciting things.
Advocacy activity for teens
Youth advocacy efforts are an important way to reduce the
influence and amount of positive tobacco portrayal in movies and on
television. Here are some suggestions:
1. Teens can write to the actors and actresses to express their concern
over how tobacco use is portrayed on screen. Simple form or
hand-written statements or letters to actors/actresses, production
companies, or anyone actively involved in decision making, will let
them know that the amount of tobacco use does not go unnoticed
and is undesirable. The youth may also send letters of recognition
to those who convey an anti-tobahco message to encourage and
congratulate their efforts.
2. Produce a slide with an anti-tobacco message that could be shown
prior to movie trailers previews: Contact your local theatre to find
out if they will show it.
'
3. Send it petition to-a particular actorrd^W or producer signed by
youth. This petition can b^fes Otf concern regarding how
tobacco is being portrayed.
4. Do a pre and post test at a movie theatre. Survey moviegoers about
their impression of tobacco and cite some facts. After the movie,
survey the same audience to see if their impression/reaction
changed.
5. Get permission from a movie theatre and hand out a movie
evaluation form for the audience to fill out. For example, the
release of the Hollywood movie "The Insider" may be a good
opportunity to do this.
6. Have youth create a list of movies that contain smoking scenes.
24
25
7. Encourage teens to write letter/article in a school newspaper.
Include a list- of celebrities who have died from smoking related
diseases. (See list of celebrities killed by tobacco)
These are just aTew of ways to encourage critical thinking while
deglamourizing tobacco use. The goal is to encourage the movie and
television industry to stop portraying tobacco as being a desirable
activity.
Watch what you are watching
How do your country’s movies and television programmes fare? It
Would make for an interesting project. Why don't you find out?
Whether you are sending a message to Hollywood or your local
entertainment industry, discussing tobacco use with your family, or
working on a class or group project, the following questions and
methods utilized by the Thumbs Up! Thunks Down! project should
help in your efforts.
How much tobacco use is shown? The easiest way to determine the
extent of tobacco use is to count intfeits. V^ile there are various
ways of counting, the method used by ^umbs^p! Thumbs Down! is
to count each time tobacco is shown pi^f^jp^en as an incident. For
example, two people smoking at ^e^:$^0^finie on screen are
considered two incidents. When a handfhol&rig a cigarette moves off
screen and then back on and when a camera refocuses on a person
smoking are also considered separate incidents. More than 30
incidents in a movie and over 10 incidents on a television programme
reflect relatively high use.
What type of tobacco is being used? The type of tobacco being
used in movies and on TV can encourage or discourage certain trends
in tobacco use. For example, the prominent use of cigars in recent
movies and TV shows in the US has likely played an important role in
the increasing incidence of cigar use in the US.
Who is using tobacco? Major characters who are played by popular
actors and actresses carry out much of the tobacco use in movies and
on TV. Many of these characters, actors and actresses serve as role
26
models to young people. When these role models light up, it sends a
powerful message that smoking is OK.
How is tobacco use being portrayed? The way tobacco use is
portrayed is an all-important factor in encouraging or discouraging
tobacco use. When the entertainment industry shows tobacco use as
fun, it suggests it’s a way of rebelling and establishing independence,
or shows it as a means of relaxing and dealing with stress, it sends a
message that using tobacco is a highly desirable activity. When the
entertainment industry suggests that tobacco use is unhealthy or
addictive, portrays a character strenuously objecting to breathing
second-hand smoke, or shows some of the more unattractive aspects
of tobacco use such as smelly clothes and stained teeth, it sends the
message that one should avoid tobacco use.
1
27
A message to all youth
from Dora'd Lahham
I was a heavy smoker, and I would not
refrain from smoking for any reason despite
my knowledge that it is harmful. I even
realized that smoking could easily send me to
my grave. Later, I began to feel that I should
quit, and made several attempts but withput
success. I asked several people who were
able to quit how did they manage to break
loose of the bondage of this killer, which we
imagine it to be give us enjoyment when it
is truly a killer. Whatever I tried in this
respect ended in failure, until a moment arrived
when my worst fears came true. I suffered a blockage of my arteries
which doctors attributed to smoking. This led to the fact that blood
supply to my heart was severely disrupted. Had it not been for God's
mercy, I would have been one among the millions that tobacco kills
every year.
Smoking is a very deceptive habit. We think of it as a source of
some pleasure or enjoyment, and we take it up unaware of the risks to
which it exposes us. It all starts with a cigarette offered to you by a
friend, which you may wish to try because you think it may be
pleasant, or you may think that it gives you a bridge to cross over in a
few minutes to the stage of being an adult. But it is a bridge of smoke
that kills. It is then a matter of one cigarette after another until we slip
into the stage of nicotine addiction. Then the realization creeps in that
smoking is a total evil, with no positive aspects and no .enjoyment
either. It is simply a mechanical habit that enslaves human beings.
Then the smoker is torn apart between his awareness of the risks that
engulf him and those he loves as a result of continuing to smoke and
his inability to break his chains and quit his habit.
28
Some smokers may do like I have repeatedly done, entertaining a
wish to quit but feeling unable to do so. I would seek help and aids;
such as a nicotine patch or some medication which is supposed to turn
you off smoking. But none of this works, because my resolve to quit
has not been strong enough. Then thoughts of what I may have to
endure after quitting blacken my day and return me back to smoking.
Then the moment of truth arrived. I discovered that it is all a matter
of decision and resolve to break the chains and save myself, my health
and the health of those who are very close and dear to me. I felt that it
is imperative for me to pause and reflect, and to take the decision to
stop once and for all this hazardous and ruinous habit. I felt that I had
to take that decision, even in the form of a vow to commit myself
privately and publicly and to honour my resolve.
The point is that it is all a personal decision, commitment and
resolve. I have made that resolve and I praise God for having enabled
me to quit smoking. As it turned out, nothing of my initial fears have
had any real substance. I have not felt any crave to take up smoking
again. I have not been a victim to intolerable suffering. Now I feel
smoking to be repugnant. I wish I had had the courage to quit earlier.
Indeed I wish I had the courage to say no to the first cigarette when it
was offered to me. I would have then spared myself much trouble and
much suffering.
All that it takes, then, is a little reflection and clear thinking.
Smoking kills in different ways. It destroys our health, wastes our
money and time. All that goes up in smoke. What we are left with is
utter ruin.
A final word to all young men and women:
I was young like yourselves. But now at my age, I remember, with
no good thought, my friend who encouraged me to light up the first
time. Hence, I hope that you have the awareness and the courage to
refuse the first cigarette and save yourself and your friends much
suffering.
29
Tobacco control legislation
and its implementation
By
Abdullah Al-Eissa
Vice President, High Court, Kuwait
i
•I
When the wide range of risks smoking represents became well
established, and the health hazards it poses to smokers and
non-smokers were identified, governments and legislative authonties
began to take measures that seek to contain its effects. Some countnes
issued some laws and regulations which aim to control smoking by
banning tobacco advertising, and restricting smoking in enclosed
public areas. They also made certain specifications with regard to the
contents of tobacco products. Legislation is a good and effective tool
of social control. Legislation may provide for the restriction of certain
practices that are deemed hazardous, or represent an unjustifiable risk
to human life, health or wealth. Its provisions may outline the
principles of accountability and imposes penalties that fit with the
aims and purposes of the legislation. Legislation must always be
suited to the circumstances prevailing in society. It must have some
essential qualities that make it suitable for implementation. Only m
this way can it become an effective way to achieve the purposes for
which it has been promulgated.
While this applies to any piece of legislation that aims to establish
social controls and serve certain public interests, like tobacco control
legislation, a number of prerequisites must be fulfilled for it to work
out. These are:
1. Those who are entrusted with its implementation must have no
personal interest that is contrary to tobacco control;
2 The authority supervising implementation should be seen to
' provide a good example. This is achieved through conviction of its
usefulness and a complete commitment to the fulfilment of its
objectives.
30
3. Maintaining justice in implementation. No piece of legislation
should ever be applied to one sector of the population while others
are exempted. No regulation could apply to one company and not
to another. Yet in practice we see that in both industrial and
developing countries legislation banning tobacco advertising have
been applied to radio and television, but not to press. We also see
that the ban on smoking in public places has been welcomed in
Western countries, while its implementation in the developing
world, including Arab countries continues to leave much to be
desired. It is a simple fact to say that restricting smoking in public
places and transport is the responsibility of three different bodies
which must cooperate to ensure the achievement of the aims of
legislation. These are:
a) The smoker, since he is the one who represents the problem and
bears the burden of compliance with regulations;
b) The non-smoker, who is, in this respect, the victim. The nonsmoker is an important actor in such a situation. He should
make clear his disapproval of smoking, particularly if he
happens to be in close proximity to the smoker, suffering the
effects of passive smoking. He should be able to seek help from
the person in charge of maintaining the regulations in that
place, should the smoker insist on contravening those
regulations. It may be suggested that an effective means to
ensure compliance is to file a case against the smoker, claiming
compensation for what he may cause of health risks to the nonsmoker. This, is correct to some extent. What is needed though
is a proof of the damage that a particular person may
experience, as in the case of both smoker and non-smoker share
the same environment for a certain period of time. Moreover,
the court must conclude that there is a causal aspect that
requires compensation. Needless to say, the difficulty of proof
in such cases makes such a law suit very rare. This means that
seeking compensation through the court is not reliable as a
means of restricting smoking in public places. Nevertheless,
judgement has awarded qgjjiggnsation to those affected as a
11
yarns’
result of passive smoking in the US and Sweden. But this
judgements were not awarded against the smokers but-against
the authorities in charge of the place;
c) The authority responsible for the public place or the means of
transport, as the one responsible to implement the regulations in
that particular environment. Such an authority should always
move to protect non-smokers, taking issue with the smoker who
tries to breach the regulations and pointing out to him the need
to comply. Should he persist, then the punishment specified in
the regulation must be implemented.
That apart, implementation differs according to the provisions of
the law A provision requiring the tobacco industry to reduce nicotine
and tar contents is one for an appropriate government department to
ensure compliance. This may be the ministry of health, a consumers
affairs authority or some other. The same applies to a regulation that
requires staff in restaurants not to smoke when they are preparing
meals for their customers. Since monitoring this aspect falls within the
jurisdiction of the authority in control of food and beverages,
whatever the law provides in this area also falls under its jurisdiction.
Regulations that ban advertising in the media may be primarily
addressed to tobacco companies which are responsible for compliance
with the restrictions imposed. However monitoring implementation is
the responsibility of ministries of information. Certain countries may
issue regulations banning the sale of cigarettes to those below a
particular age. This aims to protect the youth from smoking, and
rightly so. Nevertheless such provisions may remain rather advisory
because of the difficulty of implementation. This is partly due to the
availability of vending machines and the availability of cigarettes in
the supermarkets. It is difficult to require shopkeepers to demand a
proof of age from every young person buying a packet of cigarettes.
Even then it is not difficult to dodge such requirements.
Let us now look at the role of legislation in tobacco control. The
most important points are:
(a) Means of compliance
It is inconceivable that the promulgation of legislation restricting
smoking in certain places and imposing a partial ban on advertising
can achieve the overaU objective of tobacco control. Even the best
legislation will not rid the community of a problem of such a large
magnitude as the tobacco problem. Nor is it possible for the law to
check the tobacco epidemic without concerted efforts exerted by
several sectors working in unison and committed to achieve a tobacco
free society. With such an aim in mind, action must follow two lines
in parallel: firstly, legislation which provides an antismoking legal
forum, and, secondly, an information campaign which supports
legislation by enhancing people's awareness of the hazards of tobacco
and its harmful effects on physical and mental health, as well as its
negative economic and social effects. Such a campaign should benefit
by contributions from medial doctors, religious leaders, media experts,
artists and people who may influence public opinion.
Such efforts must always employ innovative methods and put its
message across in new styles and fresh language.
To fund such efforts, it is most-appropriate that a special tax or
increased custom tariff should be imposed on all tobacco products,
with the revenue allocated for this purpose.
(b) Implementation
When legislation provides for different restrictions and controls
falling within the jurisdiction of different departments and authorities,
responsibility for its implementation will be diverse. However, in the
case of tobacco control we may identify two types of authority:
(1) Authorities that are close to the public, particularly those in
control of public places, such as schools, hospitals, clubs,
government offices, company buildings, etc. Public transport also
comes under this group. Needless to say, implementation in such
places falls on the respective administration of each such place.
(2) Government authorities. Each department or authority should be
assigned responsibility for the enforcement of laws and
33
32
I
regulations that fall within its particular jurisdiction. The
legislature may assign responsibility for issuing enforcement
regulations to different departments. In Kuwait, this role has been
assigned to the Minister of Health. Moreover, article 9 of the
Kuwaiti law gives the Prime Minister and other Ministers
responsibility for implementing the law within their respective
jurisdiction.
(c) Foiling attempts by the tobacco industry to circumvent the
law
Sports
events are
used by the
tobacco
industry to
promote
smoking
j
i
I
d^«
. m ?u
h**
iliXAat £>4 *6-* j-1A-
.X^U-JI jUW<^
*’LJ3
J—*M-*U
wu>
1M
i**U^ Ji^AU
<^* *^*
Ui4^JU^Aa--^
^3<
The tobacco industry utilizes various tools and means to promote
its products, circumventing the laws aimed at tobacco control. In its
attempts to counter the effects of legislation, it employs highly
innovative methods and allocates large budgets. Its efforts include.
© Media advertisments, particularly in papers and magazines,
® Billboards and posters on large buildings and public transport
and in shops and sale outlets;
© Indirect advertising through sponsorship of sports, cultural and
social events;
oo
34
® Promotional products and souvenirs that carry the name of
tobacco brands.
Some countries have enforced strict bans on tobacco advertising in
television^ while others have not imposed such a ban. This limits the
effect of such bans in this age of satellite channels that are monitored
across geographical boundaries. The same applies to the press as
advertising bans apply to national press, while it does not apply to
newspapers and magazines published in other countries. It must be
said that advertising may be very seductive with certain sectors of the
population. Hence very large financial and artistic resources are
allocated to it. Indeed the tobacco industry provides such resources
with the aim of circumventing the law and reaching the public.
This means that we need concerted international efforts, through
the United Nations and its specialized agencies, to work out protocols
that apply to all media channels. Even then the enforcement of such
protocols by private papers and media channels is far from easy.
Nevertheless efforts in this regard must continue, even if that requires
making special agreements with the tobacco industry to stop
advertising for a specified period.
Special efforts should be made to provide the media with
alternative sources of advertising in order to compensate them for the
loss of revenue that results from banning tobacco advertising.
It is my firm conviction that strict implementation of the laws
banning tobacco advertising would have made such promotion efforts
by the tobacco industry a definite breach of the law both in letter and
spirit. It is not to be expected that the tobacco industry will stop its
efforts in this regard, having realized that they are more effective than
direct advertising.
(d) Model integrated legislation
When countries adopt model integrated legislation, numerous
contradictions that now prevail because of the existence of many
different local regulations will be removed. It is important that such
model legislation should incorporate the following principles:
35
Islamic ruling on smoking
(1) The essential rule must be that smoking is banned in any public
place, unless there is a specific exemption allowing it. This is
contrary to what most existing laws provide for, making
smoking in public places permissible unless it is restricted by a
specific legal provision. This rule is the one adopted by the law
in Finland;
(2) Countries that at present do not have tobacco growing or a
tobacco industry should have the right to ban the initiation of
any such activities. On the other hand, the ban should be
limited to any expansion of the present scale of tobacco
growing and tobacco industry in countries where such
activities are at present available. This ban should apply in the
latter group of countries until alternative crops or industries
have been established;
(3) A ban should be imposed on all smoking in all means of
transport including all flights;
By Professor Youssef al Qaradhawi
It is now four centuries since tobacco appeared and began to be
used by people. Scholars at that time felt that they needed to issue a
ruling on tobacco use. As the practice was new and without an earlier
ruling by eminent scholars in previous generations, scholars differed
widely in their ruhngs. Another factor contributing to such differences
was the absence of a proper scientific study explaining the nature of
tobacco and the effects of its smoking. One group felt that it should be
prohibited, another considered it reprehensible or discouraged, and a
third group viewed it as permissible. Some others felt unable to issue a
clear ruling on it, preferring to wait for further evidence about its
effects. In each one of the four Sunni schools of thought we find
scholars adopting any of the aforementioned rulings. This means that
no school of thought was associated with any particular ruling of
permissibility or prohibition of smoking.
(4) A ban on all tobacco advertising should be imposed, whether
direct or indirect, including sponsorship by tobacco companies
of any sports, social or cultural.events;'
Weighing up the arguments
It seems to me that the controversy'among scholars of different
schools of thought at the time when smoking began to spread was not
the result of a difference in the basis on which scholars deduced their
verdicts. It was perhaps due to how they viewed tobacco and its
effects. Some of them felt at the time that smoking resulted in certain
benefits; others thought that its harm was limited and counterbalanced
by some benefits; others still, felt that it had no benefit whatsoever,
but they were unsure that it caused any harm. What this boils down to
is that scholars would have not hesitated to rule that tobacco was
forbidden, had they been aware that it caused definite harm.
(5) Strict limits should be imposed on the nicotine and tar contents
of all tobacco products, including the contents in each
cigarette. These limits should be published on every packet;
(6) Every packet of all tobacco products should carry a health
warning. Regulations may outline the conditions that
such warnings should meet. Health warnings must be
varied, with several warnings given to tobacco
companies for a certain period, then replaced by another
set of warnings for a similar period. The warning should
be prominent on both main sides of the packet, with a
specified perceritage of the area of the packet allocated to
the health warning. The writing should be clear, with
specified colours to make it very prominent.
36
At this point we must make it clear that the task of proving physical
harm caused by tobacco or any other substance is not something that
Islamic scholars should undertake. It is the responsibility of medical
doctors. It is to them that we must refer in this area because they are
a
37
1
L
the experts. Islam requires us to refer to the experts on any matter: Put
your questions to someone in the know (25: 59).
Medical doctors have made clear statements concerning the
harmful effects tobacco smoking causes to man’s general health, and
its particular effects on the smoker’s lungs and respiratory system in
particular. They have emphasized that it is the major cause of lung
cancer. Hence, the whole world has started recently to call for action
against smoking.
II
In our present times, scholars should be unammous in their verdict
on tobacco smoking. A scholarly ruling on this must be based on
medical evidence. Hence, when the doctor says that this practice, i.e.
smoking, is harmful to health, the religious scholar must say that it is
forbidden. Whatever causes harm to human health must be forbidden
in religion.
Yet in respect of smoking, certain aspects of harm need neither a
medical doctor nor a laboratory to confirm. They are well known to
the public at large.
■i
r>
The rationale
Some people may ask: how can you prohibit the use of a plant
without a clear statement? The fact is that it is not necessary that
every prohibited matter should be mentioned by name. Religion lays
down certain rules and principles which may apply to numerous
matters. It is not difficult to outhne the rules, but it is impossible to
enumerate every single matter. It is sufficient to make a rule
prohibiting what is foul or harmful to include under it a large number
of harmful types of food and drink. Hence we find scholars returning
a unanimous verdict of prohibition on cannabis and other drugs,
although there is no statement prohibiting them in particular.
■i.
because the Prophet says, God has decreed that every thing to be done
must be done well. Whoever causes himself or others harm does not
do well. When a person does not do things well, he contravenes God's
decree to do things well. Other evidence that may be cited in support
of this verdict is the Prophet's statement, There shall be no infliction
or harm on oneself or others, and the Quranic verse, Do not kill
yourselves. God is most compassionate to you (4:29).
Among the most comprehensive statements on the prohibition of
eating or drinking harmful substances is this quotation from Imam Al
Nawawi "Whatever causes harm when consumed, such as glass, stone
and poison, is forbidden to eat. Every substance that is not impure and
causes no harm is permissible to eat except what is considered
disgusting, such as semen and mucus. These are certainly forbidden.
It is also permissible to take a medicine that may contain mild poison,
if it is needed and it is, in the considered expert's view, safe to take.
I
The financial aspect
It is not permissible for man to spend his money on something that
brings him no benefit either in this life or in the life to come. Man is
placed as a trustee in charge of his wealth. Thus, both health and
wealth are blessings God has given us. It is not permissible for any
person to impair his health or waste his wealth. The Prophet has
forbidden the wasting of money. A smoker pays his money to buy
what causes him definite harm. That is certainly forbidden. Moreover,
God says: Do not be wasteful, for He does not like those who ate
wasteful. (7:31).
No scholar takes religious statements at face value as strictly as
Imam Ibn Hazm. Nevertheless, he makes it clear that harmful food is
prohibited. In this he rehes on the general sense of religious
statements. To quote Ibn Hazm: ’’Whatever causes harm is forbidden,
The psychological aspect
The psychological aspect of harm is often overlooked by people
who write on tobacco. The point is that when smoking becomes a
habit, the smoker falls in the grip of this habit and cannot get rid of it
easily. It soon becomes an addiction which robs smokers of their will.
Smokers are thus unable to stop it, even when they need to do so,
either because its physical harm becomes excessive, or to set a good
38
39
example for their children, or because they need the money wasted on
tobacco for some beneficial purpose.
In actual fact tobacco enslaves smokers. Hence, a smoker
sometimes gives priority to buying cigarettes rather than spending his
little money on buying food and other essentials for his family.
Should such a person be compelled to refrain from smoking for any
reason, whether personal or enforced, his general condition suffers,
and his judgement becomes easily impaired. He may become highly
irritable. Such harm makes it necessary to issue a ruling concerning
tobacco smoking.
Smoking is foirbidden
There is no way that any scholar could issue a verdict of
permissibility on smoking, after the medical evidence of the harm it
causes has become so strong, and supported by a large number of
medical and scientific authorities. Indeed the extent of the harm
caused by tobacco is now common' knowledge, supported by
indisputable figures.
Since a verdict of complete permissibility of tobacco smoking
cannot be given, then the only verdict possible is to consider smoking
either reprehensible or forbidden. It is already clear that a verdict of
prohibition is more valid and relies on stronger evidence. This is my
ruling, based on the fact that habitual smoking will inevitably cause
certain harm physically, psychologically 'and financially. Indeed
whatever is harmful to health is prohibited in religion.
God says in the Quran: Do not, with your own hands, cast
yourselves to destruction. (2:195) He also says: Do not kill
yourselves; God is ever most merciful to you. (4.29) He also
denounces wasting money in several verses of the Quran: Do not be
wasteful, for He does not like those who are wasteful. (7:31) Do not
squander [your wealth] in the manner of a spendthrift, Indeed
spendthrifts are the brothers of Satan. (17:26-7) The harm caused to
health and wealth by smoking is most definite. Indeed taking any
thing that is injurious to health is forbidden on the evidence of God's
commandment: Do not kill yourselves. (4:29) Hence we must rule that
smoking is definitely forbidden.
In point of fact, medical doctors are unanimous that smoking
causes certain harm. It is true that the harm in this case is cumulative,
not immediate, but a slowly active harmful substance is forbidden in
the same way as a rapidly active one. It is forbidden for anyone to
take a slowly acting poison just in the same way as it is forbidden to
take an instantly killing one. All suicide is forbidden in Islam, whether
slow or instant. A smoker kills himself, or herself, gradually.
Moreover, it is not permissible for a human being to harm or kill
himself or others. Hence the Prophet says: "There shall be no
infliction of harm on oneself or others". As it is unanimously agreed
by medical doctors that smoking represents definite harm to human
beings, countries of the world have required tobacco companies to
include a health warning on cigarette packets, stating that tobacco is
harmful to health. Hence it is not acceptable that religious scholars
should issue any ruling on smoking other than its complete
prohibition.
All five basic needs of human beings are adversely affected by
smoking. These five needs have been identified by religious scholars
as self, mind, offspring, faith and money. It is obligatory for every
human being to preserve these five needs and to take no risks with
them. A man’s faith is adversely affected when we see that some
smokers do not fast in Ramadan, when fasting is obligatory to all
Muslims. Such smokers feel that they cannot refrain from smoking
during the fasting day. Offspring are harmed by the tobacco
consumption of either one or both of their parents. The fetus is
subjected to definite harm when a pregnant woman smokes. Also, a
smoker harms other people in what is known as passive smoking
whereby a non-smoker inhales the smoke of other people s cigarettes
when he or she is in close proximity to them. With all this harm a
smoker causes to oneself and to others, it is not possible to return any
verdict on tobacco smoking other than complete prohibition. Indeed
all Muslim scholars should give a unanimous verdict of its
prohibition.
Some scholars have tied their verdict of smoking to the financial
ability of the smoker, prohibiting smoking to people who cannot
afford it and making it less than prohibited to those who are easily
41
40
able to buy
is incorrect, as it does not look at the problem
of smoking jn its^jofality. The long list of injuries tobacco smoking
presents to phygi^l and mental health must be considered when
giving a ver$p|<^
alongside its financial aspect. Moreover,
it is, not permi||M |fbr a rich person to squander money at will,
because money 1|1( rigs to God in the first place, and then to the
community.
Besides, every Muslim with sound judgement should refrain from
approaching this seriously harmful and foul habit. Tobacco smoking
is definitely foul, not wholesome. It has no material or spiritual
benefit whatsoever.
My advice to Muslim youths in particular is to make sure that they
do not yield to the temptation of taking up this habit which ruins their
health and weakens their bodies. They must not entertain the fallacy
that smoking is glamorous or a mark of independence. Young people
who have started to smoke shoulcktry b^'to get rid of this habit
while they are still at the beginning: Otherwise it will soon become an
addiction that is hard to quit.
>
t i7
The media has an importa1
tobacco. It should include iM
people aware of the harm caused b^tobaQCo. Writers and producers of
soap operas and other entertainr^pt prpgramrpes must stop promoting
tobacco by showing smoking^^^^ffly &ceptable or advantageous.
“SW10 * in ,he f16? aB“lst
Governments should work in cpilaboration to curb the smoking
epidemic, even though this means a loss in revenue. The physical and
mental health of its people should be viewed by a government as far
more valuable than any monetary gain. Indeed all states incur
substantial monetary losses when tobacco smoking is allowed to
spread. The expenditure a state sustains on caring for people with
smoking-caused diseases is far greater than its revenue in tobacco
taxation. The state also incurs loss in productivity because of the
greater absenteeism of smokers.
Finally, I pray to God to give all of us His guidance on all
matters, and to make our judgement sound and correct.
42
Tire Christian view on smoking
By
Father Wissa Gurguis Marcus
As a man of Se church, I believe that smoking is contrary to the
original form of man’s creation. When God created man, He made him
in the highest degree of purity and glory. According to the Scriptures,
“God did not create thorns and bristles until Adam committed his sin
and after his fall.” We realize that Satan, the enemy of all goodness,
tries to spread evil in our world. Smoking ancj other problems we face
in life are part of that evil.
May T begin by saying that Christianity does not forbid matter, but
does forbid that matter should be used for the wrong purposes. Certain
drugs and wines may be used medicinally, as anaesthetists and
surgeons are aware. But it is drug abuse that destroys the mind in
order to give man a distorted image that differs greatly from the image
of his creation. Hence, when we face things that destroy man's health
and ruin his well-being anc| stability, such as tobacco, we remember
the teachings of the Bible that make clear that while “all things are
lawful, not all things are constructive”. Hence, when we say that
everything is lawful, it is important to remember our duty not to allow
anything to hold us in slavery. Since smoking is an addiction, it
certainly enslaves the smoker. The Bible states: “Whoever perpetrates
a sin is a slave of that sin”. Today we see how smoking holds every
smoker in slavery, whether a young person, a man or a woman, youth
or adult. This is clear in the fact that every smoker finds it very hard to
quit.
A smoker may ruin his spiritual life and lose his relationship with
God as a result of smoking. He may not be able to pray or fast or
maintain a good relationship with his Lord because of smoking. The
clearest example is fasting. A person who is addicted to smoking is
unable to'give it up in order to fast. He says: “Fasting is very difficult.
How can I fast when I have to have a cigarette with my morning
coffee. I cannot get through the day unless I have a cigarette. I cannot
43
even lift my head without it”. That is the reason why we look at
smoking as enslavement, because the perpetrator of sin is a slave of
that sin"The same applies to adultery, alcohol and drugs. All are types
of enslavement. Used properly, however, such substances may be
acceptable, in the same way as we use anaesthetics in medicine.
Another point is that one's faith must be clear and free of
ambiguity. Faith presents man's action in a way that glorifies Godwin
the Scriptures we read: “When people see your good actions they
Glorify vour Father in heaven”. Undoubtedly when a human being
resorts to doing what is improper, or doing something that degrades
him in front of others, he actually gives a wrong notion of God, his
faith and of what God does with his life. As such he is not honest. The
Bible teaches us that honesty must remain man’s guide throughout his
life. It says: “Be honest until your death and I will give you-the crown
of life”. This clearly shows that man is placed in a position of trust
with regard to his body, health, property and family.
A priest is also responsible for the people in his community. This
requires that honesty and faithfulness to our trust must be seen m life.
We must, then, combat all bad habits so that we may be known by our
dutiful and pure actions to show God’s beautiful work. Honesty in
human life is not limited to property and health. It also includes the
spiritual aspect and rituals of worship such as prayer and fasting. It is
further concerned with man’s relationship with God, and his love of
other human beings, and every good action. That is why we do not
stand in anyone’s way to prevent him from receiving what is good. On
the contrary, we help people to do good works.
Smoking leads to many sinful actions, because smoking may have
adverse effects on the smoker’s soul, exposing him to problems and
difficulties. Indeed a man may leave God’s house feeling the urge to
smoke, as though his cigarette is more important to him than what
God says and does. That shows that we have a great mission to fulfil.
We are placed in a position whereby people emulate us. This includes
all of us here, whether we are priests, doctors or Islamic scholars. The
task we have to undertake in our community is highly important. This
is particularly true of religious leaders. In our country, an important
44
feature is the fact that both Christians and Muslims have great respect
to priests and scholars, and respect their counsel. People know that
whatever religious leaders say is meant to serve their interests. As
priests, we frequently try to make people understand that it is
imperative to quit smoking because it enslaves the smoker.
%
In the Book of Parables, the Bible says: “A person who has eaten
his fill will not be tempted by honey”. A person who is tempted by
tobacco, drugs, adultery or drinks is a weary person defeated by Satan
and by sin. Hence, we must be ready with our help to try to save him
from evil and transform him to one who is self-sufficient. Our
children must realize that we want them to be self-sufficient to show
them the way to faith and good works. That would help them to
abandon the way of sin and evil so that they may lead a life of purity,
holiness and love of God and man. Thus they will grow in goodness.
One problem that encourages smoking and causes young people to
turn to it is unemployment. Young people <o frequent cafes that are
available everywhere suffer from having npffing to do with their time.
A young man may start to go to a rgll a rton-smoker, but he leaves
it a smoker. This shows the need to-hel^ouf youth to use them time in
a gainful way, so that they may bele^|jiged in work, useful hobbies,
sport, noble concepts, serious read^|g»y religion:s books.
We need to teach them how to appreciate^0M5;blessings which He
has bestowed on all of us. A mind with nothing to occupy it is a
playing field for Satan. When Sataii finds,a person with nothing to
occupy his mind, he hurries to seduce liimthd thus he lands him with
great troubles.
Finally I would like to stress the need to continue our hard work in
combating smoking and all forms of tobacco use. We must remember,
however, that the task we face is a hard one which requires great
perseverance. We must never lose hope. On the contrary, we must
continue our struggle against all social ills, in order that our society,
and human society in general, is based on goodness, peace and love.
45
i
1
<4
^Brities killed by tobacco
Desi Arnaz
Nancy Walker
Buster Keaton Neville Brand
... WArt Blakey
Ed Sullivan
Duke Ellington
John Wayne
Lucille-Ball
Denver Pyle
Lillian Hellman
Robert Mitchum
Arthur Godfrey
John Huston
Bette Davis
■
The foliolist of prominent international celebrities who
have died fror^^®ng, their age, and the cause of death. Please help
list for your own country or region (Courtesy
up put togethej
of die EntertaiJ^nt Industry Council’s Tobacco in the Media Project
and “Cigarette Hall of Fame,” a report by the Roswell Park Memorial
Institute).
{-u -C 4-1*
t_J
4- Zx
Nat “King” Cole
Mary Wells
Steve McQueen
Rod Serling
Eddie Kendricks
Michael Landon
Lee Remick
Betty Grable
Edward R. Murrow
Humphrey Bogart
James Franciscus
Dick Powell
Gary Cooper
Chet Huntley
Dick York
Sammy Davis, Jr.
Walt Disney
Yul Brynner
Tallulah Bankhead
Sarah Vaughan
Colleen Dewhurst
Harry Reasoner
Alan J. Lerner
45
49
50
51
52
54
55
57
57
57
57
59
60
62
63
64
65
65
65
66
67
68
68
Lung Cancer
Throat Cancer
Lung Cancer (also worked with asbestos in shipyards)
Heart Disease (4 packs va.d>y)
Lung Cancer^'■•.
Pancreatlc C£mter'(4'p^Jcs a day)
Lung
Lung Cafii
. I1CM5
Throat ape
Emphyscj
Throaf@g icbr ;
Lung Cahcer
Lung Cancer
Emphysema
Throat Cancer
Lung Cancer
Emphysema
Lung Cancer
Lung Cancer
Lung Cancer
Lung Cancer
Lung Cancer
46
69
69
70
.71
71
, 72
72
72
77
77
79
79
81
81
81
Lung Cancer
Lung Cancer
Emphysema
Emphysema
Lung Cancer
Lung Cancer
Lung Cancer
Had Lung Cancer and survived bypass surgery,
Heart Disease (aortic aneurysm)
Lung Cancer
Emphysema
, Emphysema
Lung Cancer
Emphysema
Stroke
Many of these stars also appeared in ads promoting cigarettes.
Many of the victims were sick for more than ten years before
dying.
••
Ji|jp
Freely adapted from t(Thumbs up! Thumbs Down! Advocacy
Information
Kit”,
Ameripiih
Lung
Association
oj
Sacramento-Emigrant Trails.
47
Tobacco Use in
India: Practices r
Patterns and
Prevalence
3.1 Tobacco use practices
43
3.2 Prevalence of tobacco use
49
3.3 Prevalence of tobacco use among women
57
3.4 Prevalence of tobacco use among the youth
61
3.5 Key selected studies and estimation of
the number of tobacco users
68
Appendix Chemistry and Toxicology of
Tobacco Products Used in India
73
In this chapter, an attempt is made to
understand the magnitude of the problem of
tobacco use in India in qualitative as well as
quantitative terms. This would require focus on
two aspects—the types of tobacco used in India
and the actual prevalence of the different types
' of tobacco used by the population.
In India, tobacco is used in a wide variety of
ways: smoking, chewing, applying, sucking,
gargling, etc. For each type of tobacco use, a wide
range of tobacco products may be available. Some
of these products are industrially manufactured
on a large scale, some locally on a small scale,
some may be prepared by a vendor and some
may be prepared by the user himself or herself.
Newer imperishable forms of tobacco with areca
nut have become very popular and the industry
has grown phenomenally within a few decades.
Secdi smoking is the most popular form of
smoking, while cigarettes form a major tobacco
industry.
While looking at the prevalence of tobacco use in
the population, the pattern among specific
subgroups would be of special interest. In almost
every study, tobacco use was found to be higher
in the lower socioeconomic groups and that
aspect has been dealt with in Section 7.6.
Subgroups that are dealt with in this chapter are:
rural-urban, geographic areas, occupational
groups, etc. Many suiweys on tobacco use have
I
I
•I
_
*'
Tobacco Control in India
been carried out in specific areas—almost
everywhere tobacco use is quite prevalent,
especially among men. Two specific population
groups—youth and women—are given special
attention. On the basis of studies that provide
42
n
the prevalence of tobacco use for the entire
country, the number of tobacco users has been
estimated for India. The scientific reasons for
the harmful effects of tobacco are briefly discussed
in terms of its toxic constituents.
Tobacco Use in India: Practices, Patterns and Prevalence
Cheroots
A cheroot is a roll made from tobacco leaves.
Chuttas
Tobacco Use Practices
Tobacco smoking
Tobacco smoking has been in vogue for
hundreds of years. With the spread of tobacco
to Europe and other parts of the world from the
sixteenth century, tobacco smoking soon gained
popularity in India.1 Tobacco can be smoked in
a wide variety of ways.
Beedis
Beedj's are the most popular smoking form of
tobacco in India. Thirty-four per cent of the
tobacco produced in India is used for making
beedis. Beedis are puffed more frequently than
cigarettes to prevent them from going out.
Beedis are made by rolling a dried, rectangular
piece of tendu leaf with 0.15-0.25 g of sundried, flaked tobacco.2
Cigarettes
Cigarette smoking is the second most popular
smoking form of tobacco used in India after
beedis. In India, cigarette use seems to be
confined to the use of manufactured cigarettes;
there are no reports on the use of roll-your-own
cigarettes. The prevalence varies greatly among
different geographic areas and subgroups such
as rural-urban.
Chuttas are coarsely prepared cheroots. They are
usually the products of cottage and small-scale
industry, or are made at home. Nearly 9% of the
tobacco produced in India is used for making
chuttas. It is estimated that about 3000 million
pieces of chuttas are made annually in India.
Chutta smoking is widespread in the coastal areas
of Andhra Pradesh, Tamil Nadu and Orissa.
Reverse chutta smoking
The term ‘reverse smoking’ is used to describe
smoking while keeping the glowing end of the
tobacco product inside the mouth. Reverse
chutta smoking is practised extensively by
women in the rural areas of Visakhapatnam and
the Srikakulam district of Andhra Pradesh. In
the Srikakulam district, 46% of the 10,169
individuals surveyed smoked reverse and this
practice was more cqmmon among women
(62%) than men (38%).3
Dhumti
Unlike beedis and chuttas, dhumtis are not
available from vendors but are prepared by the
smokers themselves. Dhumti is a kind of a conical
cigar made by rolling tobacco leaf in the leaf of
another plant. In a random sample of about 5400
villagers in Goa, 4% were dhumti smokers.4
Reverse dhumti smoking
Dhumtis may be occasionally smoked with the
lighted end inside the mouth. The overall
prevalence of this form of smoking is 0.5% in Goa.4
Cigars
Cigars are made of air-cured, fermented
tobacco, usually in factories, and are generally
expensive. Cigar smoking is predominantly an
urban practice.
Pipe
Pipe smoking is one of the oldest forms of
tobacco use. The different kinds of pipes used
for smoking range from the small-stemmed
European types made of wood to long-stemmed
pipes made from metal or other material.
43
Tobacco Control in India
Hooklis
Hooklis are clay pipes commonly used in
western India. Once the pipe is lit, it is
smoked intermittently. On an average, 15 g
of tobacco is smoked daily. Hookli smoking
was practised by 11% of the 52^7 men
studied in the Bhavnagar district of Gujarat.5
Recently a herbal beedi (brand name
Vardaan) has been launched. Ostensibly,
these products are marketed as aids to
smoking cessation. No scientific evaluations
have been carried out and little is known
about their efficacy.
Smokeless forms of tobacco
Chillum
Chillum smoking is an exclusively male
practice; it is limited to the northern states
of India, predominantly in rural areas.
Chillum is a straight, conical pipe made of
clay, 10-14 cm long, held vertically. In a
survey on 35,00° individuals in the
Mainpuri district of Uttar Pradesh, 28/6 of
the villagers were found to be chillum
smokers. Chillum smoking requires a deep
pulmonary effort. Often, one chillum is
shared by a group. They are made locally,
are inexpensive and easily available. Chillum
probably predates the introduction of
tobacco to India and was used for smoking
opium and other narcotics.
Hookah
The hookah is an Indian water pipe in which
the tobacco smoke passes through water before
inhalation.
In a random sample of 4859 men and 5481
women from the Darbhanga district of Bihar,
2% and 28%, respectively, reported smoking the
hookah.5 The reason given for this female
predominance is that it is inconvenient for men
to carry a hookah, whereas women remain at
home most of the time. There has been a
considerable fall in the reported consumption
of hookah tobacco. Hookah smoking thus
appears to be on the decline in India.
Non-tobacco smoking products
Non-tobacco smoking products are also
available. An herbal cigarette (brand name
Nirdosh) has been available for a long time.
44
The term ‘smokeless tobacco’ is used to
describe tobacco that is consumed without,
heating or burning at the time of use.
Smokeless tobacco can be used orally or
nasally. For nasal use, a small quantity of
very fine tobacco powder mixed with
aromatic substances called dry snuff is
inhaled nasally. This form of smokeless
tobacco use, although still practised, is not
very common in India. No scientific report
is available in the literature and therefore
nasal inhalation of snuff will not be further
dealt with in this chapter.
The oral use of smokeless tobacco is widely
prevalent in India; the different methods of
consumption include chewing, sucking and
applying tobacco preparations to the teeth and
gums. Smokeless tobacco products are often
made at home but are also manufactured.
Recently, a variety of smokeless tobacco products
have been produced industrially on a large scale,
commercially marketed and are available in small
plastic and aluminium foil packets.
Paao (betel quid) with tobacco
Paan chewing, or betel quid chewing, is often
erroneously .referred to as ‘betel nut chewing’.
Paan consists of four main ingredients—betel
leaf {Piper betle), areca nut {Areca catechu),
slaked lime [Ca(OH2)J and catechu {Acacia
catechu). Betel leaves contain volatile oils such
as eugenol and terpenes, nitrates and small
quantities of sugar, starch, tannin and several
other substances.7 Condiments and sweetening
agents may be added as per regional practices
and individual preferences. Some time after its
•4S
Tobacco Use in India: Practices, Patterns and Prevalence
introduction, tobacco became an important
constituent of paan, and currently most habitual
paan chewers include tobacco.
the villagers used this product.6
Tobacco is the most important ingredient
of paan for regular users. It is used in the
raw state (as in Kerala) as well as after
processing.
Processing,
additives
and
names differ from place to place. Tobacco
is referred to as kaddipudi and hogesoppu in
Karnataka, kadapan in Orissa and West
Bengal, and pattiwala in Uttar Pradesh.
Zarda and kiwam are commercially
manufactured varieties often used as
ingredients in paan.
This preparation contains thin shavings of
areca nut with the addition of some tobacco
and slaked lime. Its use is becoming popular
in Gujarat, especially among the youth.
Mawa use is also prevalent in other regions
of the country. The prevalence of mawa
chewing has increased tremendously in
recent years. Its magnitude can be assessed
from the fact that the Bhavnagar city
administration appealed to the people not
to litter the streets with the cellophane wrappers
of mawa, as they clogged the city drains!
Mawa
Paan masala
Paan masala is a commercial preparation
containing areca nut, slaked lime, catechu and
condiments, with or without powdered tobacco.
Paan masala contains almost all the ingredients
that go into the making of a paan, but are
dehydrated- so that the final product is not
perishable. It comes in attractive sachets and tins,
which can be stored and carried conveniently.
Paan masala is very popular in urban areas and
is fast becoming popular in rural areas. Although
the actual prevalence of this practice is not
known, its popularity can be gauged by the
production figures: according to commercial
estimates, the Indian market for paan masala is
now worth several hundred million US dollars.
Tobacco, areca nut and slaked lime
preparations
Combinations of tobacco, areca nut and slaked
lime are chewed in several regions of north
India, where they are known by different names.
Mainpuri tobacco
In the Mainpuri district of Uttar Pradesh and
nearby areas, this preparation is very popular.
It contains mainly tobacco with slaked lime,
finely cut areca nut, camphor and cloves. In a
study of 35,000 individuals in Mainpuri, 7% of
Tobacco and slaked lime (khaini)
Use of a mixture of sun-dried tobacco and slaked
lime, known in some areas as khaini, is
widespread in Maharashtra and several states
of north India. A regular khaini user may carry
a double-ended metal container, one side of
which is filled with tobacco and the other with
slightly moistened slaked lime. A small quantity
of tobacco is taken in the palm and a little slaked
lime is added. The ingredients are then mixed
vigorously with the thumb and placed in the
mouth. In Maharashtra and Gujarat, khaini is
placed in the premolar region of the mandibular
groove, whereas in Bihar and Uttar Pradesh, it
is generally held in the lower labial groove. In
the Singhbhum district of Bihar, this product is
often kept on the dorsum of the tongue. In a
study of over 100,000 villagers in Pune,
Maharashtra, 28% used tobacco-slaked lime;
the practice was more common among men
(52%) than women (10%). In the Singhbhum
and Darbhanga districts of Bihar, 27% and 44%
of the 4800 and 4856 men, respectively, used
khaini and of the 5248 and 5481 women, 10%
and 7%, respectively, used khaini.3
Chewing tobacco
Small pieces of raw or commercially available
finely cut tobacco are used for this purpose.
45
Tobacco Control in India
Chewing of tobacco alone, however, does
not appear to be very common in India.
Among the 10,000 dental outpatients in
Lucknow, Uttar Pradesh, and 57,000
industrial workers in Ahmedabad, Gujarat,
2.1% and 2.6% chewed tobacco alone,
respectively.9,10
Snus
Swedish snuff called snus is available in
teabag-like pouches. The pouch can be kept
in the buccal or labial groove and sucked.
It is marketed in India by the Swedish Match
Company under the brand name Click.
Tobacco products for application
Several smokeless tobacco preparations such as
mishri, gudhaku, bajjar and creamy snuff, are
intended primarily for cleaning the teeth. Such
use, however, soon becomes an addiction. In
India, there is a widespread misconception that
tobacco is good for the teeth. Many companies
take advantage of this misconception by
packaging apd positioning their products as
dental care products without explicitly stating
so. The reason is that by law, oral care products
cannot contain tobacco. The law is not strictly
enforced and some oral care products may still
contain tobacco.
Mishri
Mishri is a roasted, powdered preparation made
by baking tobacco on a hot metal plate until it
is uniformly black. Women, who use it to clean
their teeth initially, soon apply mishri several
times a day. This practice is common in
Maharashtra. In a survey of 100,000 individuals
in a rural area, 22% were mishri users; the
prevalence was 39% among women and 0.8%
among men.8 Mishri use is also prevalent in
Goa.
Gul
Gul is a pyrolysed tobacco product. It is
marketed under different brand names in small
46
tin cans and used as a dentifrice in the
eastern part of India. In the Global Youth
Tobacco Survey (GYTS), gul use was
reported by 6% in Bihar, 3% each in
Arunachal Pradesh and Nagaland, 2% each
in Assam, UP and Uttaranchal.2,5 In similar
surveys of school personnel in several
northeastern states of India, female school
personnel reported significantly higher gul
use than males; Assam (13.5% vs 0.1%),
Meghalaya (25% vs 1.9%), Nagaland (6.2%
vs 1.4%) and Sikkim (46.5% vs 3.9%).11,12
Bajjar
Bajjar is dry snuff (also known as tapkeerj
applied commonly by women in Gujarat on the
teeth and gums. In a survey of 4844 women in
Bhavnagar district, 14% reported using bajjar?
Lal dantmanjan
Lal dantmanjan is a dentifrice; a red-coloured
tooth powder. Traditionally, it contained tobacco
but after the passage of a law banning the use of
tobacco in dental care products, the listing of
tobacco as an ingredient was stopped. A
laboratory test of five samples of red tooth
powder that did not declare tobacco as an
ingredient found a tobacco content of 9.3-248 mg
per gram of tooth powder.12 The GYTS, which
focuses on school students in the age group of
13-15 years, found the prevalence to be 49% in
Bihar, 29% each in UP and Uttaranchal, 25% in
Orissa, 9% in Mizoram, 5% in Nagaland, 4%
each in Arunachal, Assam and Meghalaya, 3%
in Tripura, and 2% each in Goa, Maharashtra,
Manipur and Sikkim.12
Gudhaku
Gudhaku is a paste made of tobacco and
molasses. It is available commercially and is
carried in a metal container but can be made by
the users themselves. It is commonly used in
Bihar, Orissa, Uttar Pradesh and Uttaranchal.
Gudhaku is applied to the teeth and gums,
predominantly by women. In the GYTS, the
prevalence in these states ranged from 4% to
Tobacco Use in India: Practices, Patterns and Prevalence
16%.l0',, In a survey in the Singhbhum
district of Bihar, 1% of men and 16% of
women used gudhaku.5
Creamy snuff
Commercial preparations of tobacco paste
are marketed in toothpaste-like tubes. They
are advertised as possessing anti-bacterial
activity and being good for the gums and
teeth. These products are thus used like
regular toothpaste, but users soon become
addicted. This practice seems popular with
children in Goa.13
Tobacco water
Tobacco water (known as tuibur in Mizoram
and hidakphu in Manipur) is manufactured
by passing tobacco smoke through water.
Its use was reported by 872 persons (7.2%)
among the 12,185 adults surveyed in the
Aizawl district of Mizoram and 139 persons
(6.5%) among the 2137 adults surveyed in
the Churchandpur district of Manipur; use
was similar among males and females. The
frequency of tobacco water use varied from
1—30 times/day; in Aizawl and Churchandpur
districts, 36.7% and 92.1% reported being
frequent tobacco water users (more than
five times a day), respectively.14
Nicotine chewing gum
Nicotine chewing gum containing 2% nico
tine (brand name good-kha) has been
launched as a help for tobacco cessation.
For chewers, it is available in gutka flavour
and for smokers, in mint flavour.
been evaluated as a human carcinogen by
the World Health Organization (WHO).15 The
use of areca nut by itself appears to be
mildly addictive but when used with
tobacco, the effect multiplies manifold.
Chewing of areca nut products is very
common in India; therefore, a brief resume
of these products is included here.
Areca nut
In addition to being an ingredient of paan,
occasional chewing of areca nut (usually
processed) alone is quite common in India,
but habitual chewing is comparatively rare.
Exclusive areca nut chewing was observed
in 2% of 100,000 villagers in Maharashtra.8
In other rural areas of India also, areca nut
chewing was reported to a limited extent.
In Assam, a fermented form of areca nut,
known as tamol or bura tamol, is chewed
extensively. This is prepared by preserving
raw areca nuts together with areca leaves
in an underground pit with an inner lining
of straw for four months. Bura tamol is often
infected with fungus. This product contains
high levels of arecoline.
Supari
Areca nut is known as supari in several parts
of north India. Some commercial supari
preparations are made by cutting dried
areca nuts into bits and roasting them in fat
to which flavouring, sweetening agents and
condiments are added. Supari is marketed
in attractive aluminium foil packs, in tins
and in simple paper packets. Offering supari
to guests, especially after meals, is a
prevalent and well-accepted social custom.
Areca nut preparations
Some areca nut preparations are chewed
without the inclusion of tobacco, but this
practice may be present concurrently with
the use of smokeless tobacco or tobacco
smoking. Alkaloids present in areca nut are
known to give rise to carcinogenic
nitrosamines and areca nut has recently
Meetha mawa
Meetha (sweet) mawa consists of thin
shavings of areca nut, grated coconut, dried
fruits and other sweetening agents. It is used
commonly in Gujarat and similar prepara
tions with different names are used widely
in other regions.
47
SI
Tobacco Control in India
Paan without tobacco
Occasional paan chewers generally prefer
paan without tobacco. Chewing paan without
tobacco, known as tambula in Sanskrit, is an
ancient practice in India. Areca nut is an
indispensable ingredient of paan. In addition,
a wide range of chewing products including
a chewing gum that may not contain either
areca hut or tobacco but contains strong
betel quid flavours is available in the market.
3.1 TOBACCO USE PRACTICES
KEY MESSAGES
• In India, beedi smoking is the most popular form of tobacco smoking.
• Paan with tobacco is the major chewing form of tobacco.
• Cigarette smoking is the second most popular form of tobacco smoking.
• Dry tobacco-areca nut preparations such as paan masala, gutka and ma wa are also
popular and highly addictive.
• Tobacco dentifrice is popular, especially in some areas and children also use it.
48
2V
Tobacco Use in India: Practices, Patterns and Prevalence
r
3-2
Prevalence of Tobacco
Use
Surveys conducted with the objective of
providing the prevalence of tobacco use are rare
in India. Population-based surveys in limited
areas conducted to study risk factors for various
diseases and mortality have reported informa
tion on tobacco use. Additionally, three major
national surveys have collected limited tobacco
use information. This section presents the
prevalence and trends of tobacco use from some
of these studies, mostly on populations 15 years
of age and above.
Local studies
survey could be in part due to the inclusion of
children in the survey. In the rural part of Delhi,
in a small study conducted in the 1960s, 63.5%
of males aged 25 years and above were smokers.18
Data collected in small surveys in Uttar Pradesh
show a high tobacco use, smoking being more
popular than chewing. In the Sentinel Survey of
individuals 10 years and above in rural Uttar
Pradesh (Allahabad, Bijnor and Mainpuri
districts), 51% of males were tobacco users
(28.2% smokers and 24-5% smokeless users),
while 9.2% of females used tobacco, mainly in
smokeless forms. In the urban areas of the same
districts, 45% of males were tobacco users (24%
smoked; 22.5% used smokeless tobacco), and
8.2% of females were users, again, mainly in
smokeless forms. Smoking in these three
districts consisted mainly of beedi smoking,
especially in rural areas.19 In an earlier study in
Mainpuri district, 82% of men and 21% of
women were tobacco users, mostly in the
smoking form or combined smoking and
smokeless forms.5
■Several rural areas studied in central and north
The most detailed tobacco use information
India appear to have high rates of tobacco usage.
comes from large local surveys (5000-200,000
In a survey in rural Nagaur, Rajasthan, 51% of
respondents). Cross-sectional surveys on heart
males and 5% of females were tobacco users
disease in local communities have mainly
among 3148 respondents 21 years of age and
collected smoking information (1000—2000
above.20 In urban Jaipur, in three successive
respondents), as have surveys on lung diseases
studies about 39%
men and
of ^O2men
(300-15,000 respondents). Studies on lifestyle- .
20 years and above were tobacco users.
In
related factors and drug abuse also report on
Ballabgarh, Haryana, among men 87.6% were
smoking and sometimes on all forms of tobacco
tobacco users and among women 52.9% (55
use (27=100-25,000). The age groups covered
years and above).24
by the various types of studies are diverse and
since tobacco use varies greatly with age,
Low rates in Punjab contrast with the high rates
comparison is problematic.
in other areas of north India. In rural Amritsar,
Ferozepur and Gurdaspur districts, among 3600
In Delhi, a city with a diverse population, two
persons 15 years and above, 19.3% °f males and
large sample surveys were conducted, one in
4% of females were tobacco users.25
1985-1986 and the other in 1992, intended to
be representative of the city. In the first, with
In two large house-to-house surveys of over
14,770 persons in the age group of 25-64 years,
10,000 persons in rural Bihar conducted during
smoking prevalence among men was 45% and
1966-1969, about 80% of the men 15 years and
among women it was 7%«16 the second (10,312
above were tobacco users. Among villagers in
persons, 10 years of age and above), 27.7% of
Singhbhum district, 64% of the men smoked and
males and 2.7% of females were smokers.17 The
in Darbhanga district, 50% men smoked. In
lower prevalence reported from the second
33
Tobacco Control in India
Darbhanga, about half the male smokers also
chewed, while in Singhbum, less than a third of
smokers also chewed, demonstrating that
combined use was common. For women, chewing
was more common in Singhbum and smoking in
Darbhanga.26,27 Thus, Bihar has been shown to
have a high prevalence of tobacco use.
In a recent survey of 12,000 individuals aged
18 years and above in urban Kolkata, smoking
among men was 38% and chewing 36%. Women
users were nearly exclusively chewers (19%).28
In the Sentinel Survey in three districts of
Karnataka of persons 10 years of age and above,
49.2% of males and 16.4% of females in the
rural areas were tobacco users. In the urban
areas, 32.7% of males and 8.5% of females were
tobacco users. In both urban and rural areas,
about two-thirds of male users smoked, while
most female users chewed tobacco.19 In another
study in Kolar district, 30.9% of males were
tobacco users with nearly equal prevalence of
smoking and chewing. Some 38.5% of females
reported chewing tobacco.29
Among rural inhabitants 15 years of age and
above in Ernakijlam district, Kerala during
1966-1969, 81% of males and 39% of females
used tobacco in some form.26,27 Smoking by itself
was practised by 45% of males (15+ years);
additionally, 22% both smoked and chewed, and
14% chewed only. Women’s tobacco use was
essentially confined to chewing (38%). Another
survey in Ernakulam in 1971 showed very similar
results.30 In the 1990s, in rural Thiruvananthapuram (Trivandrum) district, about half
the men aged 35 years and above were smokers.31
In urban Thiruvananthapuram, 43.9% and
55.8% of men smoked in two adjacent areas,
while 26.4% and 26.8% practised smokeless
use.32 The emerging picture from Kerala is one
of high levels of tobacco use, where at least
three-fourths of men use tobacco in some form:
about half the men smoke and about one-fourth
use smokeless tobacco; and among women, a
third to one-fifth chew paan (betel quid) while
smoking is almost negligible among them.
50
~1
A recent survey in South Arcot district, Tamil
Nadu, among men aged 35-69 years, found that
nearly 47% had ever been smokers. During the
same period, a survey in urban Chennai found
that 38% men were ever-smokers.33
In two large surveys in Bhavnagar, Gujarat,
conducted in the late 1960s26,27 and late 1990s,34
overall tobacco use prevalence among men aged
15 years and above was around 70% in both
surveys (71% and 67.6%). Smoking by men,
however, appeared to have significantly
decreased over the years (56% to 35%) and
smokeless tobacco use to have increased (9% to
27%), while mixed use remained nearly the same
(6% and 4.8%). In women, where smoking
remained negligible, smokeless use may have
decreased slightly (15% to 12%). Mawa chewing
was found to have become highly popular among
young men (15-35 years).
In a large survey conducted in rural Pune district
in Maharashtra in the late 1960s, total tobacco
use was 62% among men and 49% among
women aged 15 years and above.7 Most tobacco
use consisted of smokeless forms. Similarly, in
the city of Mumbai, a survey of residents 35
■years and older from the middle and lower
socioeconomic classes found 69% of men and
nearly 58% of women using tobacco, and
smokeless tobacco use predominated. 35 Some
24% men smoked, while smoking was negligible
among women.
Occupational group studies
Occupational groups studied for tobacco use
have included skilled and unskilled industrial
workers, policemen, educational personnel,
doctors, and white-collar workers/professionals,
as shown in Table 3.1. The larger studies are
described here.
In a sutvey of 57,518 industrial workers in
Ahmedabad, Gujarat aged 35 years and above (95%
men), 35.6% smoked exclusively, 22.1% smoked
and chewed paan/supari and 27.1% practised
tobacco use in other ways (chewing tobacco with
or without lime paste, chewing paan/supari or
Tobacco Use in India: Practices, Patterns and Prevalence
I
zzs
,bacco use Prevalence data from urban occupational group studies
Urban workers
n
Age (years)
Smoking (%)
M
Industrial workers50
Ludhiana: Machine
tool factory and woollen
hosieiymill
Ahmedabad: Textile
workers (mainly)’”
1967-1971Policemen51
Bombay
(in 1969)
.
Media personnel52
Patna: Press employees
Chewing (%)
F
M
473
17-64
50.2
NR
57,518
>35
35.6
27.1
F
1
22.1 smk+
chew
3674
>26
26.9
47.0
11.6 smk+
chew
300
10
52
27 smk+
chew
Educational personnel
Chandigarh: Teachers 1
347 M
30-64
—-r
,e,C!'(R 7
19.3
NR
’ 0.0
2159 M
staff and research
scholars . '
Lucknow^ University
Any tobacco
Any tobacco
7X9
33.3
13.9
280 F
471 M
21.4
102 F
. W-'
■
Professionals
College, students
Doctors39
Chandigarh
'
'
.
$
sgg
600
NR
18-25
218
NR
■
All-India’meeting40
In the Global School Personnel Survey (GSPS),
carried out in 2000 in Bihar, 77.6% of the 502
male school personnel interviewed and 77% of
the female personnel interviewed said they were
tobacco users. The break-up by type of tobacco
use was smoking: 47.4% of men (cigarette
r ‘
20.6
30.4
NR
NR
■
■
Sex not stated
53.0 .
48.8
31;6 current
23.3 former
10 current
9 occasional
14 former
2.3
120
102 M
18 F
All-India meeting41
256
26-70
221 M
35 F
NR: not reported; smk: smoking; chew: chewing; M: male; F: female
inhaling snuff). Smoking included beedi, cigarette,
cigar, hookah, chillum and pipe.36
■
NR
NR
NR
NR
0.0
8
8
0.0
NR
NR
smoking: 40-5%) and 31.0% of women (cigarette
smoking: 26.9%). Some 58.7% of men and 53.4%
of women said they used smokeless products.37
The GSPS was also conducted in eight north
eastern states of India during January—March
2001 (Table 3.2). The prevalence of beedi
smoking varied 10% to 40% among school
personnel in this region from. In four of the
.?■
“1
Tobacco Control in India
Table 3.2 Prevalence of current tobacco use among school personnel in eight northeastern states:
Global School Personnel Survey (GSPS), India38
.
~
Women
S—in, (%)
a e. _________ __ .
Smokeless (%)
50.5
49.0
56-6
|raW';' r
- ^7
.
f7.2
IK : •
-■54:2
SWftfB
states, cigarette smoking predominated, while
in four other states, beedi smoking predomi
nated. Other forms of smoking were also found
in the region, like kamchung (a small pipe)
smoking in 6 states and hookah smoking as well
as marijuana smoking with tobacco.38
During a survey conducted in 1986—1987 among
218 doctors in three institutions in Chandigarh,
31.6% were current smokers and 9.6% ex
smokers.39
f
Results of two surveys of professional meetings
of doctors from different parts of India showed
that about 2% and 10% were current smokers
among the male doctors, while none of the
women smoked. In the study with the higher
proportion of smokers, about 8% of men as well
as of women chewed paan with tobacco.40,41
Studies of medical students have shown that
the prevalence of smoking (in all studies) and
intensity of smoking progressively increased
with the number of years in medical college.42
Knowledge of the harmful components of
cigarettes and beedis, and of the health effects
beyond bronchitis and lung cancer was poor,
even among the final-year students.43,44
Regional differences in specific tobacco
practices
Very few studies have reported on specific types
of tobacco use. Beedi smoking was common in
52
—
24.5 ■
--- ---------- —
Box 3.1 Education and tobacco use
six rural areas surveyed during 1966-1969
(Andhra Pradesh, Bihar [two areas], Kerala and
Gujarat) and in 1974 (Goa).4 About 60% of men
smoked beedisin Ernakulam, Kerala; Singhbum,
Bihar and in Goa. However, only 12% of men
smoked beedis in Srikakulam, Andhra Pradesh
where 57% of men smoked chuttas. In
Bhavnagar, Gujarat 11% of men smoked clay
pipes (hookli). In all six areas, only a small
fraction of men smoked cigarettes (up to 6% in
Ernakulam and 5% in Goa), the hookah or
chillum? Chewing was not very prevalent among
men in these areas except in Darbhanga, where
44% of men chewed tobacco with lime, and in
Kerala, where 33% of men chewed paan with
tobacco.2,26
In rural and urban surveys in Maharashtra,
smokeless tobacco use consisted of the
application of mishri (especially among women)
and the chewing of tobacco, mainly in paan.8,35
Trends with age and time
Tobacco use increases with increasing age. In
Tobacco Use in India: Practices, Patterns and Prevalence
the Sentinel Survey, tobacco use prevalence
crossed the 50% level among men in the age
group of 35-39 years in Karnataka, but in Uttar
Pradesh, where the overall prevalence was
higher, it crossed that level in the age group of
25-29 years. Among women in Karnataka and
Uttar Pradesh, the highest prevalence was
reachedTn the age group of 70 years and above,
at levels of 27.6% and 42.6%, respectively,
suggesting that in areas with a high prevalence
of tobacco use, initiation may occur at an early
"vage.19
Types of tobacco use also change with time in
succeeding generations. House-to-house surveys
conducted in random samples of villages in five
districts of Andhra Pradesh, Bihar (2 districts),
Gujarat and Kerala during 1966-1969 among
50,915 villagers aged 15 years and above
indicated that smoking was becoming more
popular among the male youth of those areas
because the average age of men who smoked
was lower than the average age of men in the
entire area’s study population. In all five areas,
the average age of women smokers was higher
than that of the women in the entire study
population, indicating that smoking was
becoming less popular among younger women
in all the areas. On the basis of similar age
considerations, chewing appeared to be
becoming less popular among both men and
women in Ernakulam and Darbhanga, and
among womenin Bhavnagar.2 Thus, tobacco use
patterns change with time.
Traditional forms of tobacco chewing such as in
paan now appear to be mainly an indulgence of
the older generation; the younger generation is
taking up newer forms of tobacco use such as
gutka, tobacco toothpaste and cigarette
smoking.45 In a survey of 1200 college students,
most tobacco users used multiple tobacco
products as well as alcohol.46
National surveys
Efforts to understand the tobacco use scenario
in India by patching together prevalence data
collected in various localities in different age
groups highlight the utility of national survey
data.
The National Household Survey of Drug and
Alcohol Abuse in India (NHSDAA), conducted
in 2002 among males, covered over 40,000
individuals aged 12-60 years in nearly 20,000
households in 25 states.47 The overall prevalence
of current tobacco use from the NHSDAA was
55-8%.
Table 3.3 gives the age-wise break-up of the
NHSDAA data, showing an increase in tobacco
use with age, levelling off after 50 years of age.
This confirms the trend with age shown in the
Sentinel Survey and local surveys.
In India, the National Sample Survey
Organization (NSSO) has been conducting yearly
surveys since 1950-1951.48 Tobacco use is part
of the consumer behaviour component of the
National Sample Survey (NSS), conducted every
five years. Another nationwide survey, the
National Family Health Survey (NFHS), in its
second
round
(1998-1999),
collected
information on tobacco use. It found that
tobacco use among men was 46.5% and 13.8%
among women aged 15 years and above in 19981999/9
Table 3.3 Tobacco use by age category, NHSDAA, 200447
Sample (/7)
Tobacco users (n)
Prevalence
12-18 years
19-30 years
8587
1860
55.8
13216
7026'.
54.9
'
31-40 years
41-50 years
51^60 yeSrs
7805
5920
4193
72.0
5168
8.168
3638
3638
71.5
5186
67.6
Source: Srivastava etal 2004
53
Tobacco Control in India
Table 3.4 Available national data for India on tobacco use
n/aI o r>
of social disapproval. Thus, in the NFHS where
the respondents were mainly females, the
prevalence of smoking among men was reported
to be lower than the NSS (29.3% vs 35-3%) where
most respondents were males, and the
prevalence of smokeless tobacco use among
women higher (12% vs 8.6%).-Part of the
differences may be due to time trends as the
surveys were 3-4 years apart. A time trend of
overall decreasing tobacco use and a specific
increase in smokeless tobacco use is in
consonance with the trends in tobacco
consumption indicated by the NSS from 1987
(see Chapter 2).
Geographic variation
State and regional differences suggested in local
studies have generally been confirmed by the
national studies, with some exceptions. For
example, the NHSDAA found the highest
prevalence of tobacco use in South Bihar
(94-7%), followed by Uttar Pradesh (87.3%) and
high rates in the northeastern states, similar to
findings in local surveys and in the GSPS. The
lowest rate was found in Kerala (20.6%), which
is in contrast to the findings of other recent
local studies.
While the two surveys have similar sampling
methods, it should be kept in mind that in the
NSS, the male head of the household responded
for all members, while in the NFHS, the female
head of the household responded for all
members, an important difference in method
ology. Prevalence rates of tobacco use were
calculated from both the recent NSS 52nd Round
State-wise prevalence using the data of the
and NFHS-2 for the population aged 15 years
NFHS-2 are shown in Table 3.5 and for men,
and above to permit comparison49 and are
graphically displayed in maps (Fig. 3.1). Overall
presented here (Table 3.4).
. tobacco use increases towards the centre of the
country, the north and east. Smoking has an
The surrogate respondent may underreport
increasing gradient towards the north,
tobacco use by younger individuals and the
northwest, northeast and in the two states of
opposite sex either due to ignorance or for fear
Andhra Pradesh and Kerala.
Tobacco Use in India: Practices, Patterns and Prevalence
"able 3.5 State-]
and chewing in India by sex (age 15 years and above)*’9
Smoking
Men
Region/state
North
New Delhi
Harvana;
..
Himachal Pradesh
%
%
Men
95% CI
Women
%
95% CI
%
95% CI
2.5
0.9
0.5
0.9
0.2
3.8
1.9-3.2
0.6-1.3
0.3-0.8
0.6-1.3
0.1-0.4
2.9- 4.9
42.(M6.6
12.2-15.8
35.7- 39.9
1.8
3.5
2.4
8.3
0.3
4.1
1.4-2.2
2.8- 4.3
1.8- 3.1
7.1-9.7
0.2-0.5
3.2- S.2
.13.1
'8.1
7.8
7.3
9.3
19.0
29.4
33,8
27.6-31.1
32.5-35.2
0.9
3.0
0.6-1.2
2.6-3.5
40.3
36.3
34.6-38.0
50.1-53.5
14.4
10.9
12.7-16.2
10.1-11.8
26.3
25,2
39,4
24.8-27.9
23.2-27.2
37.4- 41.5
.6.2
0.9
2.5
5.5-7.0
0.7-1.2
2.07-3,2
• • .'V.
51.8
49.0
23.2
46.7— 51.4
20.9-25.6
44.7- 51.0
6.7
34.3
15.1
6.0-7.6
31.9-36.9
13.5-17.0
2.6
5.6
47.8
51;6
34.1
16.9
60.2
45.0
39.5
10.8
47.9-55.3
31,1-37.3
13.8-20.5
56.5-63.8
41.3-48.8
36.5- 42.7
8,9-13,1
6.0-9.9
24.3
33.1
19,2
27.6
60.7
16 5
18.6
5.2
22.1— 26.6
29.6-36.7
15.5-23.5
23.8-31.7
57.2— 64.0
13.7- 19.7
16.2— 21.2
3.3-8.1
Rajasthan
Central
Madhya Pradesh
Utt3-- Pradesh
East
Bihar
Orissa ;
;
West Bengal ;
North-East
A^achal Pradesh
95% CI
11.5-14.9
6.7- 9.8
6.7- 9.1
5.8-9.1
8.0-10.8
17.7- 20.4
38.7- 42.0
23.9
40.4
38.6
44?3
13.9
37.8
s,ndKas“'
Chewing
Women
31.5
25.6
22.0-25.9
37.7- 43.1
36^40.6^
ManipOr
|f'°
Mizoram
am .. . . .
and
59.4
38.0
.19.4
48.5
28.4- 34.9
23.1-28.2
32.0-38.1
.
5(16 59.7 "
. 57.0-61.8
57
o
34.3-41.8
17,1-22.0
44.9-52.2
bujarat
Maha^shtra
13.3
23.5-27.2
12.1-14.6
South
Andhra Pradesh
Karnataka : ,
Kerala;
Tamil Nadu
2,0
1.4
0.2
1.2-3;2
1.0-1.8
0.1-0.4 ,
7.7
24.6
34.1
22.8-26.4
32.3-36.0
9.4-12,0
8.0
8.0
18.0
6.3-10.2
7.0-9.2
16.1-20.0
35.4
25,7
28.2
27.0
33.4-375
24.1-27.4
26.5-30.0
25.4-28.8
4.2
0.3
0.4
0.3
3.S-4.9
0.2-0.4
0.3-0.7
0.2-0.6
10.7
13.8
9.4
12.9
12.1- 15.6
12.7-15.7
9.1- 11.2
9.3-12.2
9.9
14.1
10.1
10.7
12.7-15.7
9.1-11.2
9.3-12.2
aldyaTAiu1
wrai
West
CI: confidence interval
Source:^ eta/ 2003
m a
22.0
2.4
8.2
'9.7
2.0^3.4
4.2- 7.3
10.0-14.2
4.2-10.6
19.6-24:6
1.3- 4.5
6.9-9,7
6.7-13.9
!
Tobacco Control in India
A
Male tobacco smoking
B
Male tobacco chewing
Male tobacco smoking
prevalence in different
states of India
40.4 to 59.4 (5)
H 35.4 to 40.4 (5)
Hirttot
Punjab’
esh
imu and Kashmir
28.2 to 35.4 (5)
® 25.3 to 28.2 (5)
□ 13.3 to 25.3 (6)
Sikkn
Hi! fiaghal Pradesh
Arundc
ph
Itfor
Male tobacco chewing
prevalence by slates
in India
IS 45 to 60.2 (6)
^36.3 to 45
(3)
IS 16.9 to 36.3 (6)
® 10.7lo 16.9 (5)
□ 7.3 to 10.7 (6)
SiW
Arun;
||j|Naqolond
{BjlNoqalond
LMSnipur
1
1 Tripw
»gal
lizoram
to toaeshj
■Manipur
Tripurt
|al
iizorarr
Orissa
Maharashtr<
laesh
w.
A
Andaman and Nicobar Islands
Keral<
0
Keral
A
Andaman and Nicobar Islands
•r
0
Fig. 3.1. Prevalence of tobacco smoking and tobacco chewing among men aged 15 years and
above in different states of India (brackted numbers denote the number of states)
Source: Rani et al. 2003‘19
3.2 PREVALENCE OF TOBACCO USE IN INDIA
KEY MESSAGES
• About 45 surveys conducted since the 1960s in limited urban and rural areas are available,
covering different age groups, but only a handful were large enough to be representative of
the area studied.
• Male tobacco use prevalence in 1995-1996 was 51.3% and in 1998-1999 it was 46.5%
according to the National Sample Survey 52nd Round and National Family Health Survey2. The prevalence of tobacco use among females was 10.3% and 13.8% in the two successive
surveys.
• The National Household Survey of Drug and Alcohol Abuse conducted in 25 states (excluding
Jammu and Kashmir) in 2002 reports that 55.8% of males 12-60 years of age currently use
tobacco.
• Trends seen in the data include higher tobacco use prevalence among males compared to
females and among older age groups compared to younger.
• Geographic area is a determinant of the type of tobacco use and prevalence of usage; overall
tobacco use increases towards the centre, the north and east. Chewing follows this pattern.
Smoking has an increasing gradient towards the north, northwest, northeast and in the two
states of Andhra Pradesh and Kerala.
Tobacco Use in India: Practices, Patterns and Prevalence
Prevalence and trends of tobacco
use among women in India
Prevalence of Tobacco
Use Among Women
Why focus on women? A global
perspective
Tobacco use plays a pivotal role in perpetuating
health inequalities among different socio
economic groups and between genders. Women
tobacco users not only share the same health
risks as men, but are also faced with health
consequences that are unique to women,
including those connected to pregnancy and
cervical cancer.
Smoking among women in most high-income
countries has increased over the past 20 years,
though there has been a fall in smoking among
men over the same period.58 The number of
women smokers worldwide is projected to
almost triple over the next generation, from the
current 200 million to more than 500 million.59
The biggest rise in female smoking is projected
to be in the less developed countries.
Gender-based psychosocial aspirations are
blatantly exploited to promote tobacco. Almost
all cigarette and chewing tobacco advertising
imagery in India includes women, taking
advantage of the changing position of women
in society, and their increasing socioeconomic
independence. As a result, many educated young
women perceive smoking as a symbol of
liberation and freedom from traditional gender
roles. Peer and advertising pressure encourages
even knowledgeable women to smoke.
Tobacco use among women is prevalent in all
regions of India and among all sections of
society—overall, 2.4% of women smoke and 12%
chew tobacco.49 The prevalence of smoking
among women is low in most areas due to social
unacceptability, but is somewhat common in
parts of the north, east, northeast and Andhra
Pradesh (Fig. 3.2).
A few available studies on pregnant women
suggest that tobacco use prevalence among them
is not different from that of women in the
general population.60’62 This is a cause for
concern, as it indicates no specific tobacco use
prevention efforts during antenatal care. In a
report from a large teaching maternity hospital
in Mumbai, 33.4% of women in the reproductive
age group were smokeless tobacco users.62
Women in many rural areas believe that tobacco
has many magical and medicinal properties;
keeping the mouth clean, getting rid of a foul
smell, curing toothache, controlling morning
sickness, during labour pains, etc.63
Anecdotal evidence points to an increase in
smoking among Indian women64 although the
national surveys do not show a definite trend in
women’s smoking prevalence. (The proportion .
of women smokers of all women tobacco users
was about 20% in 1987-1988 and 1993-1994,48
about 25% in 1995-1996 and 17% in 19981999-49 Though the prevalence of smoking
among Indian women is low at this point of
time, it needs to be tracked carefully due to the
increased marketing efforts and impact of
globalization. There is already an indication that
beedi and cigarette smoking is high (at least
30%) among women in Bihar and the
northeastern states.37*38
In the NFHS 1998-1999, the proportion of
*
Tobacco Control in India
Tripura
Sikkim
Nagaland
Mizoram
Meghalaya
Manipur
Arunachal Pradesh J
Assam J
If
NORTHEAST
West Bengal Orissa I Bihar - ■0
OJ
03
CO
EAST
Uttar Prasesh
Madhya Pradesh
CENTRAL
111 Chewing
Maharashtra
Gujarat
Goa
Tamil Nadu
Kerala
Karnataka
Andhra Pradesh
Rajasthan
Punjab
Jammu and Kashmir
Himachal Pradesh
Haryana
New Delhi
1^1 Smoking
WEST
SOUTH
NORTH
hHBM
ta
is
0
20
40
60
80
Prevalence (%)
Fig. 3.2 The prevalence of tobacco use among women49
regular smokers and chewers among females
increased up to the last age group, 60+, while
that for males increased up to the age of
45-59 years and then tended to flatten out
CFig. 3.3).49 A similar finding has been consis
tently observed in.the other national surveys
and the Sentinel Survey, as well as in several
smaller-scale studies. Among women in Delhi,
the prevalence of smoking increased with age
up to the last age group, but among men,
smoking prevalence was highest in those aged
35 44 years. Thus, initiation of tobacco use in
females may not be limited to childhood and
the teenage years.19
Box 3.2 Women and smoking
Jjea^wp^akat 15-24years of ageWp
Regional differences
Region-specific differences in tobacco use
practices are shown in several large population
based studies. In seven rural surveys conducted
during 1966-1969 (Andhra Pradesh, Bihar [two
areas], Gujarat and Kerala), in Pune district,
Maharashtra and in Goa in 1974, tobacco use
prevalence among women aged 15 years and
above varied from 15% (Gujarat) to 67% (Andhra
Pradesh).2,4’8,27
Among the seven areas, the prevalence of
smoking was 64% among women in Srikakulam
district, Andhra Pradesh (64%), where reverse
chutta smoking was common (59%). Forty-five
per cent of women in Darbhanga district, Bihar
smoked, where ^r7/(i3%) and hookah smoking
(28%) were the most common forms. In these
two areas of high smoking prevalence among
women, smokeless tobacco use was uncommon,
Tobacco Use in India: Practices, Patterns and Prevalence
A Tobacco smoking
B Tobacco chewing
50 7
50 7
40 ;
40 -
40 ;
40 -
35 -
35 -
30 % 25 20 -
30 ~
...... Male respondent
— Male non-respondent
----- Female respondent
—I— Feale non-respondent
/
15 10
5 -
% 25 - /
20
15 -
10 5 -
OH
__ j
cn +
7 7 7 7? ?T?* 5$ ■'t7 7 o
’-I cm
/’
cm
m m xr-finin lom
A ik 00
Age group
0 ta J__ L I XTI cn | . i
? J 7 7?
Ch csi
in o
i-h
rxj
— Male respondent
— Male noh-respondent
...... Female respondent
-4— Feale non-respondent
1! 1! 1r 1 1 1 i ~i1'
4- Tt- in in 10
o in o
cL in O in
in o in o in
ihOLD
co m
vr in in io
r<
10 m
cm
03
Age group
Fig. 3.3 Age-specific prevalence of tobacco smoking
and chewing by men and women in India, aged
15 years and above, during 1998-1999 (NFHS-2)49
but in all the other areas, smokeless use (mainly
chewing) was the most prevalent. Women’s
smoking prevalence was 19% in Goa, where
beedi (12%) and dhumti smoking (6%) were
favoured. Women who smoked dhumtigenerally
smoked one or two per day. Beedi smoking
among women varied from 4% to 13% in the
different districts, while cigarette smoking was
negligible.2,4,8,27
Smokeless tobacco use was more common
among women in all the other areas. The
prevalence of chewing tobacco use, especially
paan with tobacco, was as high as 27% in Goa
and 35% in Kerala. In Bhavnagar, Gujarat, 14%
’of women applied bajjar to the gums, in
Singhbum (Bihar) 16% applied gudhakutQ their
gums and in Darbhanga 7% used tobacco with
lime. In Pune district, Maharashtra, almost
no women smoked but 49% of women were
smokeless tobacco users; altogether 39% used
mishri.2'*’*'27
In an urban survey conducted during 19921994 in Mumbai, 57.5% of women in the age
group of 35 years and above were current
tobacco users, almost all of smokeless tobacco
(only 0.4% smoked).35 The most common form
of smokeless tobacco use was mishri, sometimes
combined with other smokeless tobacco. Over
90% .of women who used mishri applied it less
than 3 times a day. This low frequency is
consistent with the practice of its use as a
dentifrice. Mishri use tended to begin in
childhood, while paan chewing tended to begin
later.
According to NFHS 1998-1999 data, regions in
order of increasing prevalence of tobacco use
among women are the north, south, west,
central, east, and the northeast (Fig. 3.3).
Chewing in various states in 1998-1999 among
women was as follows:
• Up to 61% in Mizoram
• Between 30% and 40% in Orissa and
Arunachal Pradesh
• Between 20% and 30% in Meghalaya and
Assam
• Between 15% and 20% in Manipur, Sikkim,
Nagaland, Madhya Pradesh, Uttar Pradesh,
West Bengal and Maharashtra
• Between 10% and 15% in Karnataka, Kerala
and Tamil Nadu
• Between 5% and 10% in Andhra Pradesh,
Goa, Gujarat, Tripura and Bihar
• Between 2% and 4% in Delhi and Rajasthan
• Less than 1% in Punjab, Himachal Pradesh,
Haryana, and Jammu and Kashmir.
Tobacco Control in India
Smoking in various states among women in
1998-1999 was as follows:
• Between 10% and 25% of women currently
smoked in Mizoram and Manipur.
• Between 5% and 10% of women currently
smoked in Jammu and Kashmir, Bihar,
Tripura, Sikkim, Meghalaya and Arunachal
Pradesh.
• Less than 5% of women currently or ever
smoked in the large majority of states.
As covered in some detail in Chapter 2, women’s
tobacco use is higher in the less educated and
poorer social strata. Yet, the socioeconomic
gradients for tobacco use are steeper for women
than for men.49 In a large study in Delhi, being
a housewife, a student, or being retired had a
protective effect in comparison to being a
professional.16
3.3 PREVALENCE OF TOBACCO USE AMONG WOMEN
KEY MESSAGES
India has a huge problem of widespread smokeless tobacco use among women, particularly
among disadvantaged women.
• The prevalence of smoking is higher among rural women, and women in the north and
northeast.
• Tobacco use in pregnant women is similar to that in non-pregnant women of the same age.
• The difference between male and female smoking rates is narrowing in some areas where
smoking among women has been hitherto uncommon.
Differentials in the prevalence of tobacco use among various socioeconomic groups are much
more acute in women compared with men.
60
I
Tobacco Use in India: Practices, Patterns and Prevalence
Prevalence of Tobacco
Use Among the Youth
A literature review on tobacco use among the
youth revealed that information is limited to
the district or township level and the method
ologies used vary. The Sentinel Survey of the
World Health Organization-South-East Asia
Regional Office (WHO-SEARO) and Indian
Council of Medical Research (ICMR)19 provided
detailed population-based tobacco use preval
ence data for youth in the age group of 10—14
years in two states—Uttar Pradesh (boys 3%;
girls 0.6%) and Karnataka (boys 1.3%; girls
0.1%). The Global Youth Tobacco Survey
(GYTS), supported by the WHO and the Centers
for Disease Control and Prevention (CDC),
conducted during the years 2000-2004, is the
first survey that provides data on youth (13-15
years) for national and international comparison
with standardized methodology. The GYTS data
are available for 26 major states, which represent
94% of the Indian population.
This section provides estimates of tobacco use
among the youth specifically using the school
based GYTS for India.
Objectives and methodology
The objectives of the GYTS were to examine the
prevalence of tobacco use among school-going
youth in the age group of 13-15 years, their
knowledge about the harmfulness of tobacco,
access to tobacco, attitudes towards tobacco use,
social beliefs and perceptions, cessation
behaviour, exposure to tobacco advertisements
and attitudes towards tobacco control.
The GYTS is a school-based, cross-sectional survey
that was independently conducted in different
states of India, using a uniform methodology.65 In
brief, GYTS employed a two-stage cluster sample
design to produce a representative sample of
students in grades eight to ten in both government
and private schools, which roughly corresponds
to the age group of 13-15 years. At the first stage,
the probability of schools being selected was
proportional to the number of students enrolled
in the specific grades. At the second stage, classes
within the selected schools were randomly chosen.
All students from selected classes attending the
school on the day of the survey were eligible to
participate. For estimating the prevalence rates,
weighting factors were applied to each student
record to adjust for non-response (school, class
and student) and variation in the probability of
selection at the school, class and student levels.
For the GYTS data presented here, the school
response rate ranged from 92% to 100% and the
student response rate ranged from 70.1% to 90.6%.
This sample provided responses from 53,654
individual students in 26 Indian states, namely
Andhra Pradesh, Arunachal Pradesh, Assam,
Bihar, Chandigarh, Delhi, Goa, Gujarat, Haryana,
Himachal Pradesh, Karnataka, Madhya Pradesh,
Maharashtra,. Manipur, Meghalaya, Mizoram;
Nagaland, Orissa, Punjab, Rajasthan, Sikkim,
Tamil Nadu, Tripura, Uttar Pradesh, Uttaranchal
and West Bengal.
Results
Tobacco use prevalence and other
variables
The summary of the countrywide results for
GYTS India, 2000-2004, are presented in this
section under important variables:
Ever tobacco use: Ever tobacco use (ever
consumed any tobacco product) was reported
by one-fourth of students (25.1%); the preval
ence ranged from 4.0% (Himachal Pradesh) to
75.3% (Mizoram).
Current use of tobacco in any form:
Students consuming any tobacco products
within 30 days preceding the survey were
61
Tobacco Control in India
I
considered current tobacco users. Among
students in the age group of 13-15 years, 17.5%
Box 3,3 Tobacco use among students
(Grades 8-10)
were current users of tobacco in any form, and
• 17.5% were current users of tobacco
in any form (range: 2.7%-63%);
• 14.6% were current smokeless tobacco users
(range: 2.0%—55.6%);
• 8.3% were current smokers (range: 2.2%34.5%).
current use ranged from 2.7% (Himachal
Pradesh) to 63% (Nagaland).
Current smokeless tobacco use: Among
students aged 13—15 years, 14.6% were current
(GYTS 2000-2004)
smokeless tobacco users. Users ranged from 2%
(Himachal Pradesh) to 55.6% (Bihar).
vs
Smokeless
Clearly,
current
smokeless tobacco use was significantly more
was reported by 8.3% of students. It ranged
from 2.2% in Himachal Pradesh to 34.5% in
Mizoram.
common than current smoking among students
aged 13-15 years (Table 3.6). It is to be noted
rable 3.6 Tobacco
_ ____ __ ...... .
■'
s
smoking:
Current smoking: Current smoking in India
L-.--
'
—-
that the total of smokers and users of smokeless
forms is higher than that of current users of
--- '
■■
■
■ Lowest (State)
-
-'.i '■ •
■%■,
X
•,
:
■
75/3.
(±5.3)28
'-/cp
(±1:0)
(±5.8)
53.7
____
(±0.7)5s
(±0.3)19
(±0.9)'(±4.1)28
if
. 57.8
4.0
?’3
2.0
2.2
0.5
1.6
; (±0.9)’
.13 A
s
_%
'
34.5
22.8
47.4,
94.9
(±4.5)2f
(±3.3)28
,f±lp.6)??,
(±3.§)2'
48;7'■
74.8
(i'1.6)
(±T^..
9.9
23.5
31.4
(±2.9)°
79,0
(±3.9)8
(±7.3)24
84.4
90.9
5.%1
(H4J)
12.1
4.2
(±8.7)>
(±1.7)u
95.7
98.1
0
17.5
14.6 •
Exposure (outside home) ”
s 9 - • a'Fayoprs smoking ban in public places . M ;
. .■
(95% CI)
-• ' • „
Current smoking
Current
./ .
pnt cigarette smoking 1 Current use of non-cigarette
<er needs tobacco
*"i-fe
V-v-x-w ,first
u ; thing in the morning
.
%
_____________________________________
4.2
- <.
.
,,
(95% m
~~
:
(ie.if
(±1.9)21
Access and availability
Notr^ed'blcause'ofage
Tobacco promotion
Percentage who have seen , a lot of advertisements
For cigarettes on billboards
Belongings with cigarette logo
Offered free sample of beedi
Belongings with beedi or paan masala logo
42.1
(±1.4)
(±5.6)10
(±Z.l)22
2.8
0.6
1.1
NA
(±0.5)t8
(±0.8)16
NA
NA
NA
100.0
26.1
(±0.0)24'26'28'29
12.4
8.0
14.6
(±1.3)
(±1.3)
(±1.4)
Cessation
Wants to stop smoking
Tried to quit smoking
68.5:
71.4
(±7.2)
(±11.7)
19.6
8.4.
(±12.5)21
(±3.3)28
88.9
97.8
(±6.9)1
(±3.5)10
Curricular teaching
Taught dangers of smoking in class
Taught effects of tobacco in class
47;4
(±1.6)
2.7
3.1
(±1.9)16
(±2.1)16
75.5
71.4
(±5.2)8
(±5.4)s
50.9
(i'1.5)
(±7.3)28
NA.
NA
States:
Chandigarh
p«HTeM0
nXg,9arrr1 Chhattisgarh
AaulSgarhZ2 Delhi
De,l?f3 Haryana
nanraHa44 Himachal
Himachal Pradesh
Pradesh55 Jam
Jammu and Kashmir6 Madhya .Pradesh7 Punjab8 Rajasthan9 Uttar
a?.^u
. AnclhS Pradesh Karnataka13 Kerala14 Tamil Nadu15 Bihar 16 Orissa17 West Bengal18 Goa19 Guiarat20 Maharashtra21 As
West Bengal18 Goa19 Gujarat20 Maharashtra21 As$am.22
;
Arunachal Pradesh23 Manipur24 Meghalaya25 Mizoram26 Nagaland27 Sikkim28 Tripura29
NA: not available
'
Tobacco Use in India: Practices, Patterns and Prevalence
I
tobacco in any form due to overlap, as a small
proportion of students used both forms.
Current
cigarette
and
non-cigarette
tobacco use: The GYTS India results show
that current non-cigarette. tobacco use (13.6%)
was three times more common than current
cigarette smoking (4.2%). The current prevalence
of cigarette smoking ranged from 0.5% in Goa to
22.8% in Mizoram, whereas the prevalence of
current non-cigarette tobacco use ranged from
1.6% in Himachal Pradesh to 47-4% in Manipur.
Second-hand exposure: Over one-third of
students (36.4%) were exposed to second-hand
smoke inside their homes and nearly half
(48.7%) outside their homes. The exposure to
second-hand smoke inside the home ranged
from 9.9% (Punjab) to 79.0% (Meghalaya) and
outside the home it ranged from 23.5% in
Punjab to 84.4% in Meghalaya.
Factors associate! with tobacco use
The determinants of tobacco use among the
youth are many and varied. First of all, socio
demographic factors such as gender, state and
region, and rural versus urban residence were
found to be related to tobacco use among these
youth. Factors affecting social norms are
described next: family influence and tobacco
use by friends; curricular teaching; exposure to
advertisements in the media and community;
access and availability of tobacco products in
the area of residence; concurrent alcohol and
tobacco smoking; nicotine dependence; desire to
quit tobacco use; levels of awareness about the
harmfulness of tobacco and attitudes towards
government tobacco control policies on access
and availability of tobacco products to minors;
school policies; tobacco control strategies and
tobacco industry tactics to attract the youth.
Gender: Positive responses to all the questions
on tobacco use were reported significantly more
commonly among boys than girls: ever tobacco
■use (boys 30.4 [±2.3], girls 16.8 [±2.2]), current
any tobacco use (boys 22.0 [±2.1], girls 10.3
[±1.9]), current smokeless tobacco use (boys 18.5
Ml m
Cniienr Tobacco Use pot
c
O I-IOS
m 11 22%
Fig. 3.4 Levels of current tobacco use in different-states of
India, GYTS 2000-2004
[±2.1], girls 8.4 [±1.9]), and current smoking
(boys 10.5 [±1.6], girls 4.4 [±1.0]).
State and region: High prevalence (>30%)
was reported in the northeastern states and
Bihar, intermediate prevalence (n%-22%) in
Gujarat, Maharashtra, Madhya Pradesh, Orissa,
Rajasthan, West Bengal, Uttar Pradesh and
Uttaranchal, and low prevalence (i%-io%) in
Andhra Pradesh, Chandigarh, Delhi, Goa,
Haryana, Himachal Pradesh, Karnataka, Punjab,
and Tamil Nadu (Fig. 3,4).
Rural versus urban' residence: The GYTS
results from Karnataka, Bihar and Rajasthan
revealed that there was no statistical difference
in overall current tobacco use among rural and
urban students (rural 59-4%, urban 58.2%);
however, current beedi smoking in rural areas
(5-0%) was significantly higher than in urban
areas (2.4%) in Bihar. Such information was
not available for any other state.
Family,
home,
friends
and
school:
Comparing the GYTS data from 26 states,
current tobacco use was significantly correlated
with variables such as (i) the percentage of
students who have one or more parents using
•IM
S,fci;g
Tobacco Control in India —
I
tobacco (Spearman correlation coefficient=o.77,
Access and availability: Among current
p<o.ooi); (ii) smoking at home was reported
smokers,
65.8% purchased cigarettes in a store
by 36-7% (average) of students, ranging from
(ranging from 53.1% [Nagaland] to 95.7% [Uttar
8.8% in West Bengal to 96.1% in Uttar Pradesh;65
Pradesh])
(Table 3.6). Among students who
(iii) the percentage of students who have most
bought cigarettes in a store in the past 30 days,
or all friends who smoke (Spearman correlation
over 55.1% (average) were not refused purchase
coefficient = 0.85, p<o.ooi); and (iv) exposure
by anyone because of their age (range: 6.2% in
to second-hand smoke inside the home
Uttar Pradesh to 98.1% in Assam) (Table 3.6).
(Spearman correlation coefficient = 0.67,
pco.ooi) and outside (Spearman correlation
Tobacco and co-morbid alcohol use: The
coefficient = 0.70, p<o.ooi); (v) at school, the
GYTS data from the eight northeastern states
level of curricular teaching on topics such as
showed that co-morbid smoking and drinking
the dangers of smoking and chewing (Spearman
ranged from 6.9% in Meghalaya to 13.1% in
correlation coefficient = -0.75, P<o.ooi), and
Sikkim. Among boys it ranged from 8.5% in
the effects on appearance of smoking and
Meghalaya to 19.6% in Manipur, and among
chewing (Spearman correlation coefficient =
girls from 2.9% in Manipur to 7.7% jn
-0.46, pco.ooi) were inversely associated with
Mizoram.67
current tobacco use.
The GYTS data from eight northeastern states
of India showed that tobacco users were more
likely than never-tobacco users to admit that
most or all of their friends smoke. Additionally,
parental tobacco use was reported two to three
times more often by tobacco users as compared
to never-tobacco users.11
Curricular teaching: About half of all
students agreed that they had been taught about
the dangers of smoking (ranging from 2.7% in
Bihar to 75.5% in Punjab) and the effects on
appearance of tobacco use (ranging from 3.1%
m Bihar to 71.4% in Punjab) (Table 3.6).
Media and advertisements: The GYTS
revealed that 42.1% and 38.3% of students
reported seeing pro-cigarette and pro-beedi
advertisements ‘a lot’, respectively. Students
reported being equally exposed to gut/ca
advertisements on billboards and community
events.66 Over 12% and 14% students reported
having some object with a brand logo of
cigarettes/beedi or paan masala, respectively
(Table 3.6). Among the GYTS participants in
India, about 8% of students were offered free
samples of cigarettes and beedis by tobacco
companies (Table 3.6).
Nicotine dependence: Nicotine dependence,
was assessed by one question on whether the
respondent needed tobacco first thing in the
morning. In the northeastern
------- t states, over twothirds of cigarette-smoking students (especially
among boys) and nearly half of smokeless
tobacco users reported needing tobacco first
thing in the morning.11
Desire to quit tobacco use: Attempts
and social support
snH cacioI
The GYTS results revealed that over 68.5%
(average) of students who smoked wanted to
stop (range: 19.6% in Manipur to 88.9% in
Chandigarh), whereas 71.4% (average) had
already tried to stop smoking during the past
year (range: 8.4% in Sikkim to 97.8% in Uttar
Pradesh). For all India, 84.6% of cigarette
smoking students had received help or advice to
stop smoking from family members, community
members, health personnel or friends (range:
10.5% in Sikkim to 97.8% in Uttar Pradesh). In
the northeastern states, however, compared to
the national point estimate, such help was
rePorted to be low (<39% in 5 of 8 states*),
4-^
a
M
,
■
.
.
Tobacco Use in India: Practices, Patterns and Prevalence
Awareness of the dangers of tobacco
and attitudes towards tobacco control
[range: 12.0% in West Bengal to 87.8% in
Manipur]).68 Early initiation before 10 years of
Awareness: Nationwide GYTS data show that
57-9% students agreed that smoke from others is
harmful to them (range: 5.1% to 86.3%). Lower
awareness levels were seen in the northeastern
states as compared to the rest of India.
Attitudes: An assessment of attitudes towards
tobacco control showed that nearly three-fourths
(74-8%) of students (31.4% in Manipur to 90.9%
in Maharashtra) thought that smoking should
be banned in public places (Table 3.6).
Discuss
A review of the GYTS data throws up an
extremely wide range of variations regarding
tobacco use. India, being a country of over one
billion people, has the highest and lowest rates
for current use of any tobacco product in the
world: 3.3% in Goa to 62.8% in Nagaland.68
These wide differences, in prevalence within a
country underscore the importance of
subnational or regional data, for national
estimates can obscure important regional
differences within the country.
Many studies conducted during 1989-2004
using different methods have shown that tobacco
use among girls students in schools13,69-77
colleges76,78 and medical and dental colleges42/44.79-84
was low relative to boys and adults in the general
population. The results of the India GYTS 20002004 are consistent with the above studies;
however, in some of the states, there is no
statistical difference in the use of cigarette and
non-cigarette products between boys and girls.85
This indicates a breakthrough in social norms in
India, where tobacco use by girls and women is
considered taboo.
The average percentage of ever-smoker students
in the GYTS who smoked their first cigarette
before the age of 10 years was 54% (average for
13 states: 8 northeastern states, Bihar Goa
Maharashtra, Tamil Nadu and West Bengal
age was reported to be high in the states where
tobacco use prevalence was high. In the
northeastern states, ever-tobacco users who first
used tobacco before the age of 10 years was
more than 65% in all the states except Mizoram
(23.9%).68 In the present review it is clear that
early initiation is increasing and demands that
environmental factors be properly regulated. A
definite strategy for curricular teaching at all
academic levels is required,
The GYTS in Bihar and Karnataka revealed that
there was no statistical difference in rural-urban
current tobacco use among students 13-15 years
of age. This may be because of the increasing
reach of the tobacco industry in rural areas.
In the GYTS, among students of grades 8-10 in
26 states (53, 654), about 14% of never-smokers
(average 13.8%) (range: 4.55% in Punjab to
46.1% in Sikkim} expressed the opinion that
they were likely to initiate smoking next year.
In Karnataka among college students, although
female students interviewed were non-smokers
several suggested that in the future, smoking
might be an acceptable behaviour among college
going females.78 This indicates that the
marketing effect of tobacco industiy is overriding
prevention strategies.
When asked about their perceptions of smoking
among the youth in western countries, the
majority of college students from different
colleges in Karnataka believed that threequarters of male and female youth in the West
smoked and this perception has been largely
formed through media images, including
satellite television and films. With regard to
addiction, it was widely believed that filter
tipped Cigarettes were one of the most addictive
products because they are made of better quality
tobacco, and are milder and smoother to smoke.
Therefore, a person could easily smoke more of
them, which would lead to addiction. Another
widely held belief was that the more expensive
the cigarette, the less harmful it was for one’s
health.78
j
Tobacco Control in India
In India the misconception is widespread that
tobacco is good for the teeth or health. Specific
teeth-related problems have been assigned as the
reason for starting tobacco use. In the GYTS
reports from the northeastern states of India,
tobacco users reported significantly more often
that tobacco relieves toothache and helps in
morning motions, etc. than did never-tobacco
users.11
Many companies take advantage of these
misconceptions by packaging and positioning
their products as dental care products. In India,
the 1992 amendment to the Drugs and Cosmetic
Act, 1940 prohibits the use of tobacco as an
ingredient in dental care products.12 Tobacco
products are used as a dentifrice in different
parts of India.13,70,75 A laboratory test of five
samples of red tooth powder that did not declare
tobacco as an ingredient, 10 years after the law
had been amended, found a tobacco content of
9.3 to 248 mg per gram of tooth powder.12 A
clear strategy addressing this specific issue needs
to be planned and implemented. In a GYTS
report for 14 states, namely Bihar, Goa,
Maharashtra, Uttar Pradesh, Uttaranchal and
eight northeastern states, current use of tobacco
products as a dentifrice ranged from 6% in Goa
to 68% in Bihar.12
Parents and teachers are the initial role models
for young children. In the northeastern states
, and Bihar, tobacco use among adults48,49,86,87 and
schoolteachers37,38 was found to be high and so
is the current tobacco use prevalence among
students 13-15 years of age. Over 80% of tobacco
users in these states showed that they received
help from someone within the community.11 This
is one example where preaching does not work
unless the role models change themselves too,
and practise what they preach. The GYTS
revealed that those states having higher levels
of curricular teaching have a low prevalence of
tobacco use by students. Bihar (teaching 3%,
tobacco use by students 59%) and Punjab
(teaching 75% and tobacco use by students 3%)
may be taken as examples of two extremes.
From different reports on the Global School
Personnel Survey (GSPS) in India37,38,88
conducted simultaneously with the GYTS, it has
been revealed that tobacco policies in schools
restricting student smoking (28%) and school
personnel smoking (26%) are rarely adopted and
enforced. Tobacco prevention instruction by
teachers on six different teaching and training
measures was low (<35%). A special striking
feature was the lack of teaching material and
training for teachers regarding tobacco legislation
(5%). However, there is evidence that central
government schools that adopt tobacco control
policies had a low prevalence of current tobacco
use among students89 and school personnel90 as
compared to state schools, which had no policies.
A study91 from Kolkata found that increased
tobacco use was associated with government
schools versus private schools. A survey in 45
schools in Mumbai found that tobacco use among
boys in their final year in English medium private
schools (22.5%) was significantly higher as
compared to students from Indian language
private (6.9%) and municipal schools (13.8%).73
The GYTS data show that students in schools
under State Government boards reported
significantly higher current tobacco use than
Union Government board schools in Bihar.75
Goa, Delhi and a few other states have policies
on tobacco control and these states have a low
prevalence of tobacco use among the youth.
However, in Delhi and Goa, over 30% and 20%
students, respectively, reported that they
experienced exposure to second-hand smoke
outside their homes in the week preceding the
GYTS. Apart from this, there is other evidence
that indicates that legislation for tobacco control
is not properly implemented in India.92 About
90% of students in the age group of 13-15 years
supported banning smoking in public places.
For preventing exposure in public places, the
existing law ‘The Cigarettes and Other Tobacco
Products (Prohibition of Advertisement and
Regulation of Trade and Commerce, Production,
Supply and Distribution) Act, 2003 No. 34 of
2003’ needs to be implemented vigorously, while
the public needs to be informed about the
dangers of second-hand smoke.
Tobacco Use in India: Practices, Patterns and Prevalence
3.4 PREVALENCE OF TOBACCO USE AMONG THE YOUTH
KEY MESSAGES
• Tobacco is used by the youth all over India with a wide range of variation among states.
• Two in every ten boys and one in every ten girls use any tobacco product.
• There is no statistical difference in rural-urban current tobacco use among students aged
13-15 years.
• Many youth believe that tobacco is good for the teeth or health.
• Early initiation before the age of 10 years is increasing.
• States having higher levels of curricular teaching have a low prevalence of tobacco use by
students.
roa&iEssi
67
Tobacco Control in India
■
Key Selected Studies and
Estimation of the Number
of Tobacco Users
In this section, key studies selected as a basis
for estimation of the number of tobacco users
are described and an estimate of this number is
attempted.
Key selected studies
The major source material used for this study is
tabulated data from the special report:
Consumption of tobacco in India, 1993~1994
of the National Sample Survey Organization
(NSSO).48 This nationwide survey was
undertaken as the 50th round of the National
Sample Survey (NSS), using statistical sampling
techniques. A total of 115,354 households located
in 6951 villages and 4650 urban blocks were
visited and information on tobacco use including
product types were obtained for all members aged
10 years and above residing in each surveyed
household. In the survey, tobacco use among a
total of 432,393 individuals of all ages was
recorded. This information was obtained from
one member of the household, usually the male
head. The NSSO tabulated the survey results for
urban and rural residents gender-wise and age
wise for 32 states and union territories. In the
report the age groupings were as follows: 10-14,
15-29, 30-44, 45-60 and 60+ years. The NSSO
report also contains prevalence by type among
various social groups.
The second National Family Health Survey
(NFHS-2) was also a nationwide household
survey conducted according to strict statistical
sampling procedures during 1998-1999, on
health-related practices and behaviour in 26
states. Over 90,000 households were surveyed
and information on paa/7/tobacco chewing and
tobacco smoking were obtained for 315,597
persons aged 15 years and above. Information
was collected from the female head on members
aged 15 years and above on tobacco use, and
tabulated data are presented as tobacco chewers
and tobacco smokers in the report. Data are not
presented on the prevalence of combined use in
that report, thus there is an overlap and the
prevalence of chewing and smoking cannot be
added together. However, some combined data .
have been published elsewhere.49 In the NFHS2 report, the age categorization adopted was
15-19,20-24,25-29, 30-39, 40-49, 50-59 and
60 years and above. These data were obtained
from 25 states in the country.
Other thaii the above two nationwide survey
reports, the results of a complete rural
population survey have also been used to
estimate the national prevalence in this section.
This survey was conducted in the entire
Karunagappally population located in Kollam
district of Kerala during 1990-1998. These
results were also used for estimating prevalence
as this was a complete population survey
conducted by face-to-face interviews with results
tabulated for 5-year age groups by gender, which
made it possible to obtain age-specific prevalence
rates for males and females. This area is ‘rural’
according to the government census. The survey
was undertaken to obtain the prevalence of
lifestyle factors associated with cancer
occurrence (personal communication Dr P.
Jayalekshmi, P. Gangadharan and V.S. Binu,
Karunagapally Cancer Registry).93
In Table 3.7 the number of persons interviewed
in the NSS are shown gender-wise and according
to urban-rural residence. The rural population
was only 62% of the total studied.
$
Rural
Urban
iotwl
130,357
78,627
208,984
208,98
223,409
Female
-1999
nW®*
5X
V
(
-
' ....... 'T®
'7^-- iv
Tobacco Use in India: Practices, Patterns and Prevalence
Table 3.9 Percentage of household members above ! 5 y^ars
Table 3.8 Percentage of household members above
10 years of age who regularly use tobacco, by gender
1993-1994 - NSSO 50th round48
of age who currently chew tobacco or smoke by gender 1998-1999 -.NFHS-2"
__
Male
Chewer^okers
Any
Smokers
Agy
Residence
Chew
. .
Female
Currently
Chew
tobacco
Currently
smoke
O-L.O
31.3
32.6
20.8
■ : 21.4
13.8
8.8
20.5
3.1
0.9
16.2
t&te
Rural
Urban
Urban
kuicjix
:
'
20-8
?8 3
29,4
Source: International Institute for Population Sciences, 2000
In the survey of the rural. Karunagappally
population, information was obtained by
interviewing 117,240 men and 138,883 women
above 15 years of age.
Age-specific prevalence
Table 3.10 shows that the prevalence increased
with age. Among males the rates decreased after
60 years but not in females.
Overall urban and rural prevalence
According to the NSSO report, overall in India
in the population aged 10 years and above, 43%
of rural males and 28% of urban males are
regular tobacco users (Table 3.8). Among
females the prevalence in rural areas was 11%
and in urban areas it was 5%. It is evident that
rural prevalence is higher than urban prevalence
for both males and females and that male
prevalence is higher than female prevalence
overall.
Table 3.9 shows the observed prevalence rates of
the NFHS-2 in rural and urban areas for tobacco
chewing and smoking among males and females.
The prevalence in rural areas was 50% higher
than in urban areas for both males and females,
and for chewing tobacco and smoking. Smoking
prevalence among rural females compared to
urban females was more than 3 times higher. On
an all-India level, the NFHS-2 estimated that 21%
of persons aged 15 years and above chew paan
masala or tobacco and only 3% of the women are
reported to have ever smoked but 29% of men are
current smokers. This survey also noted higher
rates among rural and less educated men and
women compared to urban residents.
In the rural Karunagappally population, current
tobacco use prevalence figures in the population
15 years of age and above were 53.8% among
males and 14.2% among females.
Table 3.10 Age-specific prevalence (%) among males and
females of regular tobacco users in rural and urban areas, IMSS
1993-199448
. ...
.
......... '
Age Group
tRSral
' •
T:
. __________
_ __
<:fA<R'uraL
Urban/'
0.9
Mi
4.6
110-14 ~ ~ -15-24
.
0.2
Wl r fc .12.2 '
; 50,9
2Q&
^&1.2 '
■39.5
Source: National Sample Survey Organization, 3998-1999
A similar pattern is seen in the age-specific
prevalence distribution from the NFHS-2, as
shown in Table 3.11.
Table 3.11 Age-specific prevalence of tobacco use in males
i ■
I
/Age group
:/(years).;F
tobacco
4.4
13.7
25.1*
3Z6
. .9.4
6W«
35.6
35.4
28.3
_
2.1
4.3
8.0
123
...
-V - -
'
O
29.4
18,6
0.2
0:6
1.1
: -
• io v
20.5
4.0
5.7
5.3
16.2
,.'.1?
/Source: International Institute for Population Sciences, 2000
69
,v;':
a11®
I
Tobacco Control in India
<p
CD
§
£
80706050403020-
-•-Male (%)
-A-Female (%)
100-1
'T
CD
tn
m
T i
LO
in
LD
I
co
O
TT
<0
rx
4-
In Fig. 3.4, the age-specific prevalence curves
plotted against age for males and females are
shown for the population of Karunagapally
taluk, Kollam district, Kerala. Among males, the
prevalence was above 70% in the age range of
35-69 years. As in the NFHS-2 and the NSS50th, the prevalence declined at older ages in
men but not in women.
Age group
Fig. 3.4 Age-specific prevalence rates among current
tobacco users Karunagappally taluk.
1990-1998
Table 3.12 Prevalence of tobacco use in any form by ever
users per 1000 rural and urban males and females (10+ years
□t age), States and Union Territories, India, NSS, 1993-1994^
State
Male
tobacco
Andhra Pradesh
Arunbchal Pradesh
As^ti
BiMr
Goa
Gtijarat
naryang
Himachal Pradesh
Jammu and Kashmir
Karnataka
Kerala
Madhya Pradesh
Maharashtra
Manipur
Meghalaya
Mizoram
Nagaland
.Orissa
Ra'’^ n
■
-Sikkifn
Tamil Nadu
Tripura
Uttar Pradesh
rWM Bengal
Andaman and Nicobar
^andigarh
:
and Nagar Haveli
if>arriafW)iu
'
"
Lakshadweep
Pondicherry
All
India
„__________
tobacco
toteco.
Urban
tobacco'
users (%) users (%) users (%) users (%)
123 ■'■•TiT
.
43.9
26.2 ’
47.9
37.5
28.8
16.2
52.7
44.6
114 ^■5.3
47.6
33.0
6,0
3.6 .
22.0
23.8
5.5 „ 4;2:v42.9
^8.6
94
3.5 46.8
24
6-2
41,7
28.1
3.8
^1.
38.2
19.8
3.2
0.5
'36.6
24.0
9.6
3.2
34.6
31.5
6.7
4’6
54.Q
33.6
12.0
Z2
45.4
25.4
24.0
8.0
45.5
35.4
21.5
13.2
62.2
53.2
31.9
13.1
69.8
66.9
63.2
57.4 ♦,
31,9
34.1
1.7
' 56-2
41.6
44>8 • ^44
18.0
03 \ 0,3
4^
.31
31.4 ■
4,8 52;6
36.2
4.6
0.6
28.4
23.4
9.2
4.0
56.1
50.7
21.1
24.6
47.6
31.5
7.7
Ms
52.7
<4
10.6
6.6
53.3
43.4
19.9
9.7
384
'r 30.2
1.3
1.3
; 56.7
28.2
5.6
3.1
MS
21.0
7.2
0.5
43.4
25.2
3.5
M
38.3
43.5
21.4
14.3
23.2
16:6
4.8
24
45.3
29.9
11.8
54
National Sample Survey Organization, 1998-1999
70
Female
State-wise prevalence
Table 3-12, the prevalence of tobacco use per
1000 individuals (not percentage) aged 10 years
and above in each state and territory is given.
The variations in tobacco use prevalence that
exist between states are evident. Among rural
males in Punjab, the prevalence was 12.8% but
it was 69.8% in Mizoram. Among urban males,
the lowest rate was seen in Pondicherry at 16.6%
and the highest prevalence of 66.9% was noted
again in Mizoram. Similar variations in
prevalence were noted among women also.
Among the rural and urban women of Punjab
only 0.3% were tobacco users but the prevalence
among rural females in Mizoram was 63.2% and
urban 57.4%. The higher prevalence in rural
areas and among males is true for most states
and territories. Only in Goa, Nagaland, Punjab
and Lakshadweep, the rates in urban males were
higher than in rural males. In Tripura, urban
females had a higher rate than rural ones.
Estimation of tobacco use prevalence
Methods
A simple method is adopted for estimating the
numberjif tobacco users in India for the year
2004. It was thought sufficient to consider only
three variables: rural versus urban residence,
age and gender. State-wise differences and
socioeconomic differences were not considered
in the estimation procedure for the whole
country, given the difficulties involved. The
available rates were projected onto the 2004
population estimated for India in the Registrar
General’s report 1996.95 In this report, the
Tobacco Use in India: Practices, Patterns and Prevalence
estimated population of India (all ages) on
1 March 2004 was 547,55b,000 males and
512,468,000 females. The distribution of the
population by 5-year age groups is also given in
the publication. This estimated population was
proportionately assumed to be composed of 27%
urban and 73% rural in each age group and the
urban and rural age distribution was obtained.
The prevalence of tobacco use for rural and
urban areas of residence obtained from the
NSSO age-specific rates were directly used to
estimate the number of users. These were
obtained separately for males and females in
each age group. A similar compilation was also
done using the Karunagappally age-prevalence
rates of tobacco users for comparison purposes.
Estimations
By using the NSSO age-specific rates, regular
consumers of tobacco (aged 10 years and above)
were 186,482,598 in rural India and 49,337,216
in urban areas. Thus, the total number of tobacco
users was 235,819,814 in 2004.
Age-specific estimation based on the
Karunagappally 5-year age-specific prevalence
rates of current tobacco use yields a total of
195,446,246 male users and 44,607,056 female
users m 2004, totalling 240,053,302 users in
India. It is essential to mention here that the
Karunagappally rates are obtained for the age
groups of 15 years and above, whereas the NSSO
reports are for the ages of 10+ years and above.
Thus, the Karunagappally rates would be lesser
by the number of male and female users in the
10-14 years age group, which would be 4-5
million.
A further estimation was done of the number of
tobacco users (smokers, chewers) among
persons aged 30 years and above. This was used
to estimate chronic disease burdens (Table 3.13).
Prevalence studies of tobacco use in India have
estimated number of users (chewers, smokers)
mtfie 3°+ age groups
--- - ___ _ _
,,
Nep
shown wide variations between urban and rural
areas, regions, age, gender, education^ and other
sociodemographic variables across the country.
Urban-rural differences are an especially
important consideration for estimation, as
several surveys have shown that the prevalence
of tobacco use is higher in rural populations
compared to urban areas arid, in India, 73% of
the population lives in rural areas. Also, tobacco
use is more common among men than women
(NSSO, NFHS-2).48'49
The two estimates of prevalence of the number
of users differ by around 10 million when the
age considered is 10+; thus, the estimated
number indicates that in 2004 there are" about
250 million users aged 10+ years in the countiy.
The NSSO is a nationwide study and is thus
important for such national estimation. The
NSSO estimates gave the number of tobacco
users as 235.8 million.
The Karunagappally area is
is rural,
rural, hence
hence using
using
this the prevalence may have inflated the
estimated number. However, it must be pointed
out that in Kerala there is no ‘rural’ area as seen
in other parts of the country. Sometimes the
entire state is termed as an extended suburban
area. It may also be underscored that there was
a high literacy rate—more than 85% in
Karunagappally, which, is unusual in a rural
setting, rhe prevalence of tobacco use was also
high. Using the age-specific prevalence of
Karunagappally, the estimated number is 250
million users in 2004 in the 10+ years age group.
By a direct estimation using the prevalence
percentage of the NFHS-2, Rani etal^ estimated
t
Tobacco Control in India
that the total number of users were 195 million—
154 million men and 41 million women, probably
using the base year 1998-1999.49 The NSSO
survey was done earlier in 1993-1994 and the
Karunagappally population survey was
undertaken during 1990-1998. Because it was
based on house-to-house visits and face-to-face
interviews it took 8 years to complete.
An earlier estimate made for 1996 was 184
million tobacco users (150 million males and 34
million females).96
It is clear that the estimates obtained here suffer
from limitations. The most important limitation
is that the surveys were not designed to collect
information on tobacco use. Surrogate responses
were used, which can introduce inaccuracies and
biases. Also, the household was used as a
sampling unit rather than an individual, and it
was not possible to make appropriate statistical
adjustments for that while doing the estimation.
It is thus imperative that national-level surveys
be undertaken periodically with the objective of
finding out the prevalence of tobacco use in India.
3.5 KEY SELECTED STUDIES AND ESTIMATION OF THE NUMBER OF TOBACCO USERS
KE¥ MESSAGES
• There are currently an estimated 250 million tobacco users aged 10 years and above in India.
• There are currently about 240 million tobacco users aged 15 years and above (195 million
male users and 45 million female users) in India.
Battle for Tobacco Control—The Indian Experience
6.6
Health Education and
Mass Media Efforts
The primary tool for tobacco control is
comprehensive and active awareness of the
population about the ill effects of tobacco use,
with special emphasis on all aspects of this
impact, i.e. social, physical, financial and
environmental. In the 1960s, when the word
‘prevention’ was added to the health discourse,
the concept referred to a multipronged approach
to disseminate warnings about products and
practices that health professionals considered
potential health hazards along with educating
the youth through school curricula.52
*■"
Efforts made by the government and non
governmental organizations (NGOs) for educat
ing the community on issues related to tobacco
control have intensified in the past few years.
Well-conducted research globally has estab
lished that it is necessary to reduce demand
through such education* married with changes
at the policy level, which also serves to
countervail the industry’s efforts to promote
tobacco. These mass education efforts along with
policy changes are targeted at reinforcing and
changing the social norms towards no tobacco
use. The Centers for Disease Control’s (CDC)
best practice guidelines suggest that public
education is an integral part of the efforts to
both prevent initiation of Tobacco use and to
encourage tobacco cessation.53
Effectiveness of health education
in India
Research studies evaluating the effectiveness of
health education in India have shown successful
results among the youth and adults.
Intervention research on awareness related to
tobacco avoidance and control have shown to
positively alter tobacco use practices among the
youth in India.54 Health education intervention
at the school level has also shown positive results
in India. In a group randomized trial conducted
with seventh grade students in 30 elementary
schools of Delhi, intervention provided at the
school and home level had a significant positive
impact on tobacco use. This intervention
lowered the offers, experimentation and
intentions to use tobacco in the intervention
group as compared to control schools. The
intervention was provided in the form of
classroom curricula, posters, booklets and debate
at the school level, and informative and engaging
materials for families at the home level.54
An intervention study in 3 places—Ernakulam,
Kerala; Bhavnagar, Gujarat; and Srikakulam,
Andhra Pradesh—reported the decline of tobacco
use by 2%, 1% and 5%, respectively, after 1 year.
Additionally, i%-6% of people had reduced their
tobacco 4ise. The intervention was a mix of one
on one discussion along with the use of IEC
materials, individual discussions with a social
scientist, film shows and exhibition of posters.55
In an intervention study among 36,471 tobacco
users, substantially more people stopped the
habit and reduced the frequency of tobacco use
in the intervention cohort than in the control
cohort in Ernakulam (Kerala) and Srikakulam
(Andhra) whereas in Bhavnagar (Gujarat) the
intervention group showed a lesser proportion
of people stopping their tobacco use and there
wasjio difference in the proportion reducing
them after 5 years. The "interventions were in
the form of health education from dentists at
the point of health care delivery. Information
was also disseminated via films, posters, radio
broadcasts and newspaper articles.56
A cohort study was undertaken in Ernakulam.
It showed (on follow up after 8 years) a greater
reduction of tobacco use among intervention
cohort compared to control cohort. Among men,
the decrease was more in smokers and those
with mixed habits compared to ch ewers. The
intervention cohort was subjected to a concen219
Um
•>>'5 ■
Tobacco Control in India
A
trated programme of health education which
included personal as well as mass media
communication concerning tobacco use in
various forms.57
Division, under the Ministry of Information and
Broadcasting (I&B) are creating awareness
among the masses on various public and social
health issues.
Communication inputs designed for these
interventions were personal communication,
films, folk dramas, radio programmes, cessation
camps, etc. and the population was exposed to
them in measured doses. These approaches
brought about-cessation in 14% of the tobacco
users. Personal communication that included
one-to-one interaction was the most preferred
input by the population.58
Traditionally, tobacco never had a prominent
place in the public awareness education
programmes of the Central or State Govern
ments in India. Immunization, tuberculosis and
malaria, alcohol and drug addiction took pride
of place. Tobacco control awareness education
got the least attention, and there is no evidence
of any systematic and concerted effort by either
the Central or State Governments to educate
the masses on tobacco. Its is only recently, after
the setting up of the National Tobacco Control
(NTC) cell under MOHFW, that awareness
educaition through the media such as print and
television has begun in a strategic manner.
However, a sustained visible media awareness
programme or campaign is yet to begin.
Allocation of dedicated funds for tobacco control
education is a major deterrent in achieving this
goal of mass awareness.
Another study was done in Kolar (Karnataka)
to assess the efficacy of anti-tobacco community
education programmes.-Here, health education
including screening of films, exhibition and a
display of photographs on the harmful effects
of tobacco were used. The decline rates in
tobacco use were 10.2% in males and 16.3% in
females, and the quit rates were 26.5% in males
and 36.7% in females compared to the baseline
in the intervention cohort.59
Health education efforts in India have been few
but effective. These efforts have been effective
mainly due to the paucity of information among
the population on the impact of tobacco use.
However, efforts at the national level are
required to counteract this menace which can
be largely curtailed through prevention and
successful quitting as a result of health
education.
Initiatives takes by the Central and
State Government
Under the Ministry of Health and Family
Welfare (MOHFW), the Government of India
has set up the Central Health Education Bureau
(CHEB) and its state chapters called the State
Health Education Bureaus. Every year, the
CHEB conducts an activity of4-6 weeks around
the World No Tobacco Day on 31 May. Similarly,
the Directorate of Advertising and Visual
Publicity (DAVP) and the Song and Drama
Before the establishment of the NTC cell, merely symbolic tobacco control efforts were made by
the Central and State Governments during the
World No Tobacco Day. On that day, the print
and electronic media carried anti-tobacco
messages issued by the government and the
World Health Organization (WHO), as well as
news of seminars and conferences organized by
government agencies to commemorate the day.
The government also conducted a few sporadic
activities against tobacco that appeared on the
national channel (Delhi Doordarshan [DD])
through the DAVP. However, due to non
sustained and disjointed efforts, no tangible
results were gained at the national level.
Efforts undertaken by the Ministry
of Health
In 1984, the Union Ministry of Health launched
the National Cancer Control Programme, which
included a component for educating the public
about the dangers of tobacco to eliminate
S3
KMfc..
Battle for Tobacco Control—The Indian Experience
rtobacco-related cancers.60 This was, however, a
relatively small component of the programme,
which mainly focused on providing clinical care,
establishment of cancer registries and screening
for some cancers.
Collaboration between the Ministry
of Health and WHO
In addition to a few events on the World No
Tobacco Day, the Ministry of Health has reached
out to the rural audience through programmes
such as those listed below.
(i) The South-East Asia Anti-tobacco Flame
rally covered a large number of states in
India during 2000-2001 and later, in its
second phase, in the year 2002. This
campaign was coordinated by the Nehru
Yuva Kendra. Anti-tobacco messages were
disseminated using street plays performed
in the local language, targeting the tobacco
products used locally. This led to greater
penetration of the programme, even in the
remotest parts of the country. All aspects' of
tobacco use were targeted. Apart from the
health impact, concomitant social and
economic burdens of tobacco use were also
highlighted in this anti-tobacco campaign.
(ii) Awareness dissemination was carried out
through 268 field units of the Directorate
of Field Publicity (DFP), which are located
at grassroots levels in villages throughout
the country.
(iii) The World Health Organization-South-East
Asia Region (WHO-SEARO) initiated a year
long campaign in January 2000 to curb
tobacco consumption in South-East Asia.
This campaign included educational
programmes on television in these
countries, including India.
■
'
National Tobacco Control cell
The NTC cell is supported by WHO’s India Office
and is physically located in the MOHFW at New
•‘Tr‘?'’:T
Delhi. This cell has streamlined and intensified
the health education and mass media efforts
related to tobacco control in India in the past
few years. This cell was set up as a result of
collaborative efforts by the Ministry of Health
and WHO in February 2001 to provide impetus
to the tobacco control efforts and to coordinate
these activities at the national level. It also
facilitated the development of a strategic media
plan to provide health education among the
masses. The media plan of the NTC cell focused
specifically on protecting vulnerable segments
such as the youth and passive smokers. There is
no analogous cell in any other ministry. The
Tobacco Free Initiative (TFI) in WHO’s India
Office is one of the largest programmes
worldwide, clearly highlighting tobacco control
to be a high priority for the country and WHO
in India. The focus areas of work in the TFI are:
(i) Planning and executing a comprehensive
information, education and communication
plan;
(ii) Capacity-building among NGOs working in
the field of tobacco control;
(iii) Establishment and strengthening of tobacco
cessation clinics; and
(iv) Undertaking research on policy issues
related to tobacco.
Efforts undertaken by the National
Tobacco Control cell
>
______
•.
■
Developing an India-specific anti-tobacco
logo
In 2001, the NTC cell developed an India-specific
logo and slogan to highlight India’s tobacco
control efforts. The logo is a red circle
surrounding a hand in the gesture of a victory
sign and holding a flower. On the blue
background there are three brushstrokes, of the
three colours in the Indian national flag (saffron,
white and green). This logo has a slogan ‘Choose
Life, Not Tobacco’. The slogan has been
translated into Hindi and other regional
languages as well (Fig. 6.13a and b).
^r"
Tobacco Control in India
I
i
£
(O)
(b)
Fig. 6.13 The logo of the National Tobacco
Control programme
Television and audio advertisements
During 2001-2002, the NTC cell developed 13
ahti-tobacco television advertisements (30
seconds and 15 seconds, duration) targeting the
entire spectrum of tobacco products used in
India-cigarettes, beedis and chewable forms.
Anti-tobacco radio advertisements have also been
developed under the auspices of this cell and
aired on various popular radio channels. The
Ministiy of Health regularly releases anti-tobacco
advertisements on Prasar Bharti (the independent
broadcast corporation that has replaced the state
television and radio services). The frequency of
airing of these advertisements is sparse, due to
the paucity of funds. It usually is a month-long
campaign carried out mostly around the World
No Tobacco Day through the CHEB. The TV
advertisements and infomercials aired during
2002 aimed extensively at popular youth channels
on cable and satellite and on the national channel
to ensure a wider reach of these health messages.
Production of information, education and
. communication (IEC) materials
The DAVP, Ministry of I&B, in coordination
with the NTC cell designed and produced IEC
materials related to tobacco control in all Indian
languages. The IEC materials designed include
posters, flip charts (Fig. 6.14), brochures
Fig. 6.14 A flip chart having an anti-tobacco
message created and distributed by the National
Tobacco Control Cell
• ;• ?22
•;' '
■ter
Fig. 6.15 Sample of a brochure on the ill-effects of
tobacco
(Fig. 6.15; in 16 regional languages), bus panels
(Fig. 6.16), mobile exhibition kits, and stickers
with the logo of the Indian Tobacco Control
Programme. These materials were produced in
2002 and distributed to stakeholders through
DAVP. These are also disseminated across the
country through various health institutions,
NGOs, etc.
Outdoor publicity
Display of anti-tobacco slogans and visuals
through bus panels was coordinated by the NTC
cell in collaboration with the outdoor publicity
unit of the DAVP.
Development of an anti-tobacco mass
media plan
The NTC cell assisted the Ministry of Health in
devising a seamless mass media plan to reach
the rural, semi-urban masses and vulnerable
audience-passive smokers and urban youth.’
(i) Doordarshan: Anti-beedi and anti-^wZAa TV
commercials are aired on the national TV
channels to reach the semi-urban, rural and
marginal populations.
Fig. 6.16 Anti-tobacco message on a bus
Battle for Tobacco Control—-The Indian Experience
I
Organizing health melas
Fig. 6.1 7 Sample of an inland letter bearing an
anti-tobacco message
(ii) Media post: The Department of Posts has
launched an innovative means of taking
messages to the masses called the Media
Post. This media vehicle offers the option
of printing health messages on postal
stationery, i.e. postcards, inland letters
(Fig. 6.17), aeorgrammes, etc. Each postal
stationery item reaches at least 6-7 persons
all over the country and therefore the
impact of the messages is manifold. Since
2003, inland letters bearing anti-tobacco
messages have been used by the postal
department.
(iii) Kalyani Programme: In 2001-2002, the
Ministry of Health, in collaboration with
Prasar Bharti, decided to launch a weekly
health show to be telecast on various
regional Doordarshan kendras. Kalyani is
a health programme aired on the regional
channels of Doordarshan between 7.00 pm
and 7.30 pm for half an hour once a week.
Each of the eight states covered makes its
own programme in the local dialect
revolving around a common theme. It
covers issues related to six diseases
including those related to tobacco use. The
NTC cell contributed to the discussions on
the communication strategy and also
coordinated for inputs in the various
regional workshops. The programme was
launched on the eve of World No Tobacco
Day, 2002. Several anti-tobacco commer
cials are aired during the show and detailed
discussions on the ill-effects of tobacco use
are shown. This programme is largely for
rural audiences in the Hindi-speaking belt,
where tobacco prevalence is high.
The Ministry of Health conducts health melas
(fairs) in 543 parliamentary constituencies of the
country. In these melas, information is
disseminated about various diseases including
non-communicable diseases (NCD) and those
caused due to use of tobacco. These melas include
mobile exhibitions on tobacco, displaying posters,
handouts, audiovisual aids, projectors, movies, etc.
Counter-advertisements in the print media
Other than the regular yearly feature of a half
page advertisement released on the World No
Tobacco Day in all major newspapers, the print
media has been selectively utilized for specific
campaigns, e.g. campaign against passive
smoking. Full page colour advertisements were
released in magazines such as India Today,
Outlook, Femina, etc. The intent of this
campaign was to create public awareness against
passive smoking and empowerment of nonsmokers. This intervention was successfully
implemented and evaluation revealed that the
recall level of both smokers and non-smokers
for the campaign was high (Fig. 6.18).
Felicitation of role models
The World Health Organization recently
awarded Vivek Oberoi, a well-known film star
Fig. 6.18 A counter-advertisement on passive smoking
that appeared in India Today, 2 June 2003
t-V
7
• ' ' •?"*
V"T - r wir '7\- /-<>••
Tobacco Control in India
Fig. 6.19 Felicitation of Bollywood actor Vivek Oberoi
with the World No Tobacco Award 2004
in India, with the ‘World No Tobacco Award’
for the year 2004 (Fig. 6.19). Vivek Oberoi is a
role model for the Indian youth and has been
felicitated with this award for his efforts in and
commitment to fighting the tobacco menace.
He was also instrumental in the production of
an anti-tobacco advertisement featuring other
film stars, which was developed by the Cancer
Patients Aid Association (CPAA) in collaboration
with WHO on World No Tobacco Day 2003.61
Evaluation of these programmes
Evaluation of all these activities is undertaken
on a regular basis to assess the reach it has on
the masses. The print medium, in that context,
loses to the audiovisual channels such as
television and radio, due to its usage being
limited to the literate population only. Television
has a greater reach, even to the rural people of
the country who form the majority of the Indian
population. For them, the impact of such
messages is greater when it can be easily
comprehended through visual aids. Therefore,
television and radio have to be the primary
media for carrying out such activities.
Other efforts in collaboration with
the Ministry of Information and
Broadcasting
Radio-DATE
In 1990, the Indian Council of Medical Research
(ICMR) and All India Radio (AIR) embarked on
1
an innovative and ambitious project called
Radio-DATE (DATE standing for Drugs, Alcohol
and Tobacco Education). The idea was to
produce a series of episodes on drugs, alcohol
and tobacco, intended to reach out to youth
across the country and involve them in
interactive and educational programmes. The
ICMR with assistance from the Voluntary Health
Association of India (VHAI) and several
technical experts developed IEC materials for
the programme, which were mailed to all
registered radio listeners. VHAI designed posters
and informative leaflets on the hazards of using
tobacco. In all, 84 radio stations of AIR
broadcast 30 weekly episodes of the programme.
Regional stations also translated the episodes
into their respective regional languages as per
the guidelines of AIR and ICMR. Listeners were
requested to participate in poster painting
competitions and VHAI was invited to judge
the entries.
Two community-based surveys in rural areas
with no organized anti-tobacco programmes
showed that about 4% of tobacco users in rural
’Goa and about 6% of users in rural Karnataka
quit their habit after hearing the programme. Of
the potential listeners, about 32% in Karnataka
and about 27% in Goa had heard at least one
episode on tobacco.
Commemoration of the World No Tobacco
Day
The Ministry of Health and WHO collaborate
with various agencies to commemorate the
World No Tobacco Day on a large scale each
year for wider dissemination of the theme for
that year. The Union Health Ministers as well
as several State Ministers and Governors have
been involved in the events organized in Delhi
and other states of India on this day.
Health institutions and NGOs in almost every
state of India organize events around the theme
of the World No Tobacco Day every year. The
array of activities ranges from awareness through
rallies, street plays, seminars to advocacy events,
such as submission of anti-tobacco signature
Battle for Tobacco Control—-The Indian Experience
campaigns to government officials and policy
makers.
Efforts undertaken by State
Governments
>
^111
c >.
-x.
The Public Health Department of Maharastra
initiated its tobacco control drive in the year
1986 with a campaign against smoking.
The Public Health Department adopted a slogan
and displayed posters on the impact of passive
smoking. The slogan, ‘Your smoking is injurious
to our health’ was effectively used by nonsmokers to counter the indifference of smokers.
Statewide cancer control programmes
The two-day workshop on cancer, conducted in
Bombay (now Mumbai) by the Tata Memorial
Hospital in 1987, in collaboration with the UICC
(The International Union against Cancer), led
to the formation of statewide cancer control
programmes. One of the strategies developed
under this programme was to initiate aggressive
anti-smoking campaigns in every state of India.
Efforts made by NGOs in education
Interventions made by NGOs in different states
have had different outcomes. Considerable
publicity gets generated locally when there is
press coverage, and serves as the cheapest
medium for generating awareness about
tobacco. Some NGOs also use the local cable
network for making people aware about the
tobacco menace.
Box 6.13 Preferring education over legislation |
.....
Around the World No Tobacco Day, celebrities
from different walks of life, such as cricketers
and film stars come together to conduct
awareness campaigns. The World No Tobacco
Day celebrations begin almost one month in
advance. Different themes are selected by WHO
every year, around which programmes are
conducted in India.
The CPAA developed three TV advertisements
using popular film stars as messengers for anti
tobacco messages. These commercials were done
free of charge by these film stars and the
technical charges were supplemented by WHO.
The Indian Cancer Society also took the initiative
of adapting internationally acclaimed tobacco
control campaigns to the Indian scenario with
the help of WHO/Ministry of Health. All these
advertisements are being widely used not only
through the mass media but also through
dissemination of the same through school- and
community-based interventions.
Initiatives taken by State Voluntary
Health Associations
Many civil society organizations have, on their
own or with support from WHO and the
Ministry of Health, taken up tobacco education
in their constituencies. Many State Voluntary
Health Associations (SVHAs), which are federal
units of the’ VHAI, have integrated tobacco as
part of their ongoing training programmes, are
implementing and monitoring Health Ministryand WHO-supported projects, have conducted
surveys, brought out IEC materials, approached
legislatures and have taken up tobacco
awareness education programmes.
Education to aid enforcement
Though many states have anti-tobacco laws,
their implementation is hardly visible. Political
compulsions overtake public health concerns.
In most states from which information was
sought (Himachal Pradesh, Madhya Pradesh,
Bihar, Gujarat, Sikkim, Kerala, Karnataka, West
.--s-
Tobacco Control in India
Bengal, Orissa, Punjab and Rajasthan), the law
enforcing agency officials were not aware of all
the provisions of the State Act, while most of
the officers were not aware of any such Act.
After the notification of the Tobacco Control
Act in May 2004, the Ministry of Health has
initiated a nationwide public awareness
campaign during August 2004 through
television and radio to educate the public on
the provisions of the Indian Tobacco Control
Act, 2003. The IEC Bureau of MoHFW,
Government of Rajasthan issued posters giving
information about the Act, its provisions and
the officers empowered to take action, to all the
ministries and put them up at public places. It
is also interesting to note here that the
Government of Rajasthan has in place an Act
dating back to 1950, called the Prevention of
Juvenile Smoking Act. An effort is required by
the Union Ministry of Health to sensitize the
health ministries of all State Governments to
ensure effective implementation of the Act.
Efforts need to be made to involve law-enforcing
agencies and related departments of other
Central Government ministries as well.
To promulgate the provisions of the Indian
Tobacco Control Act, civil society groups have
launched efforts to educate the public about the
provisions of the State and Central legislations.
In Delhi, for example, Student Health Action
Network (SHAN), the advocacy wing of Health
Related Information Dissemination Amongst
Youth (HRIDAY), distributed information
brochures detailing the provisions related to the
ban on smoking in public places, to hotels and
restaurants in Delhi and nine other cities of
India, and conducted public awareness
campaigns on the rights of non-smokers.
An effective public education campaign must
use multiple channels to reach the target
audience with messages that are based on
research regarding what is most effective. A welldesigned public education campaign that is
integrated with community- and school-based
programmes, has been demonstrated to lower
smoking among young people. Such effects also
last for a longer time.62
The Massachusetts tobacco control campaign,
which has a sizeable public education
component, has been effective in increasing
public perception of the harms of cigarette
smoking and was associated with a substantial
decline in cigarette consumption.63’64
Considering these best practices, a concerted
effort between the government and civil society
groups needs to be planned to ensure
development and implementation of a
comprehensive health education programme on
tobacco avoidance and tobacco control in India.
Battle for Tobacco Control—The Indian Experience
6.6 HEALTH EDUCATION AND MASS MEDIA EFFORTS
KEY MESSAGES
• The primary tool for tobacco control is to impart comprehensive information to the
population about the ill-effects of tob;•acco use.
• Public education is an iintegral part of the efforts to both prevent initiation of tobacco use
and encourage tobacco cessation.
• Efforts made by the government and NGOs for educating the community on issues related to
tobacco control, although few, have intensified in the past few years.
• NGOs have played a major role in organizing educational activities on the ill-effects of tobacco.
• Evaluation of some of the educational intervention studies has shown a positive impact on
the reduction of tobacco use.
• Various governmental and non-governmental organizations should come together to ensure
the development and implementation of a comprehensive health education programme on
tobacco avoidance and tobacco control in India.
227
G6
Tobacco Control in India
6.7
of initial assessment, three steps of intervention
and evaluation at regular intervals, preferably
with urinary cotinine estimation as an objective
measure of cessation.
Indian Experience with
Tobacco Cessation
Tobacco cessation services are among the areas
that have to be addressed as per the Framework
Convention on Tobacco Control (FCTC). With
the establishment of the National Tobacco
Control Cell as part of the Government of India
and World Health Organization (WHO)
initiative on tobacco control in India, it was felt
that tobacco cessation services have to be
developed to help tobacco users in India give
up their habit. The Ministry of Health and
Family Welfare, Government of India, in
recognition of this need, has started such clinics
on a pilot basis in 13 centres.
In 2002, the WHO supported the setting up of
12 tobacco cessation clinics (TGCs) in diverse
settings (cancer treatment centres, psychiatric
centres, medical colleges and non-governmental
organizations [NGOs]) to help people stop
tobacco use.
Methodology
Initially, 12 centres across India were selected
in various settings such as regional cancer
centres, psychiatry centres, medical colleges and
NGOs. After initial training in Thailand, the
individuals involved were further trained at the
Institute of Human Behaviour and Allied
Sciences, New Delhi. All centres were provided
with support for additional human resources in
the form of a clinical psychologist and medical
social worker. Infrastructure augmentation in
the form of computer and audiovisual
equipment were supplied. Cotinine test kits and
bupropion tablets were also provided. An
algorithm was developed for cessation services
at the various centres. The algorithm consisted
■ a/..................
Extensive community interaction programmes
were organized by all the centres. The clinics
were physically placed within major hospitals
except at the Goa centre. This helped to attract
subjects who presented themselves to the
hospitals as patients or as attendants. Patients
who presented with various co-morbidities were
referred to these clinics for tobacco cessation.
Periodic monitoring of the centres was carried
out and mid-course corrections were introduced
as required. The thirteenth centre was added in
a specialty centre for chest diseases.
Behavioural change counselling was the most
common intervention. Given the varied setting,
pharmacotherapy with bupropion was not
uniformly utilized. Some of the centres with
strong support of the clinical psychiatry
department did introduce pharmacotherapy.
Cotinine tests were tried initially, but did not
add to self-reported cessation.
Self-help tips and behavioural change
counselling modules were developed and over a
period of one year, the centres were stabilized
with regard to the cessation services. Some
centres had large numbers of tobacco chewers
and similar interventions as for tobacco smoking
were used in this group.
The intake and follow-up proforma has been
standardized and will be made available on the
internet shortly with data entry and analytical
facilities. A resource manual for tobacco
cessation services is also being developed. The
centres have developed modules for tobacco
cessation in Indian languages, as per local needs.
Outcome
The tobacco cessation clinics were established
in 2002 and, over the past two years, they have
aggregated a large number of subjects, which
Battle for Tobacco Control—The Indian Experience
w
1400
1200
952
1000
800
500
600
400
263
200
£L
0
Goa
280
292
Mumbai
IHBAS
Delhi
328
714
764
790
Lucknow
Anand
Bhopal
1091
1147
Patna
Cuttack
599
350
VP Chest Bangalore Chandigarh
Delhi
Goa
Chennai
Chimbel
Fig. 6.20 Number of subjects seen at various centres
has provided strength to this initiative. As on
30 September 2003, 8070 subjects were seen
in these clinics with a total of 9551 follow-up
visits. There were 7494 men and 576 women.
The distribution of the subjects seen at the
various centres are given in Fig. 6.20.
As per the original algorithm, a step-wise
approach was suggested, but given the variation
at the centres, an analysis based on the level of
intervention was not carried out. The
interventions were grouped into counselling
alone, and counselling and pharmacotherapy.
The outcome of the intervention was ascertained,
at 6 weeks and was classified as complete
abstinence or reduced to more than 50% of the
initial use. The prevalence of tobacco use by
type is given in Fig. 6.21. The outcomes at 6
weeks are shown in Figs 6.22-6.24.
100 n
138
1725
80 -
g, 60 .
134
13
§ 40 .
1 20-
0 -
Female
Reduced
E3 Quit
No change
Drop-outs
Fig. 6.22 Outcome at 6 weeks by gender
100
727
90
80
70
o> 60
s
OJ
662
373
944
515
188
50
40
30
20
10
0
!E
I 408 - I
Quit @ Reduced
No change
Chewers
Discussion
H
Smoker
Both
Drop-outs
Fig. 6.23 Outcome at 6 weeks by type of
Tobacco cessation services have been found to
be feasible in Indian settings (Table 6.6). The
quit rates achieved with behavioural change
100
90
80
70
£ 60
S 50
8 40
ix 30
20
tobacco use
100
5~
1101
a
90
80
70
<u
cn 60
S
§
2624
40
10
0
Male
Smokers
® Chewers
298
I
178
1162
50
£ 30
20
10
0 -
1056
Female
Counselling
Both
Quit l@ Reduced
250
Pharmacotherapy
No change
Drop-outs
Fig. 6.21 Prevalence of tobacco habits among
Fig. 6.24 Outcome at 6 weeks by type of
attendees
intervention
^'7
Tobacco Control in India
counselling, which is the least expensive and
most feasible option, are satisfactory and
provide scope for further improvement.
16%. The addition of pharmacotherapy improv
ed the quit rates. Counselling is cost-effective
and can be the preferred option for expanding
the services. Pharmacotherapy may be limited
to services which have good clinical support.
The overall quit rate at 6 weeks was around
Table 6.6 List of 13 tobacco, cessation clinics in India
S. No. Contact person(s)
Name of the centre
Contact details
1.
Dr Surendra Shastri
Professor and Head
Tata Memorial Hospital
Department of Preventive Oncology
Dr Ernest Borges Road, Parel, Mumbai 400012
Tel 022-24154379
email: shastri@vsnl.com
2.
Dr Savita Malhotra
Professor and Head
Departmentp^^ychiatry
Dr Anil Malhotta
De-addiction Centre
Postgraduate Institute of Medical Education and
Research
Chandigarh 160012
Tel 0172-2744503
Dr Nimesh G. Desai
Professor and Head of the
Department of Psychiatry
DrS.N.Sengupta
Dr RU A '‘ S-n^0''
R;iZt singn
Associate Professor
PfUdayK; Sinha
Institute of Human Behaviour and Allied Sciences
G.T. Road, Dilshad Garden, Post Box No. 9250, Delhi 95
Tel 011-22113395
email: tccihbasrc@hotmail.com
3.
■
email: savita@chl.dotnet.in
-
'r,
-
: •- ■
. .i;
,
' •/'T'
I
> 7®)Ci^#dfeSsor
-■■■
3 -prD6e|fptva
Assistant FJofessor
2,
Senior kesi
4.
DrGi^M hra
Professor a d Head of
nwlSL-..
Hedd and'Neck Surgery
SW5
.......
gw
’T'
’
^92’22n3^
gm nos: 02692-223254,.
• Mayank Jayant Foundation, Anand
email: dakshaglri@yahoo.com
6.
Dr Mahabir Das
Principal Investigator
7-
I-
r
•
' •
DrB.Sanyal 'W
Radiation Oncologist
Dr K. S. Saluja
Medical Officer
■ S « -Of '-
Acharya Harihar Regional Cancer Centre
Medical Road,
Roach ManglaL.
Manglabad, Cuttack 753007
^feSftStibn Clinic, Sub-centre, Bentkar PHC, Cuttack
• Tobacco Cessation Clinic, Sub-ceritf< Kfchore Nagar PHC
Cuttack
AV
V;t
.•;> <•
ferral Health Centre, Ardr
DrU. R. Parija
Head of the Department
of Head and Neck
Oncology Division
;/
Indira Gandhi Institute of Cardiology
Tel 0671-2302535
email; urparija@csmti^com
'■>
>
''
I
•
.
•- < -.
•:
Tel 0012-2532848
email: mdasnotebihar@sify.com
Chatrapati Shahuji Maharaj Medical University
Lucknow 226016
Jawaha|j^^ru Canosf Hospital ^hd Resedtch Gdntre
1610522-358230 -
Rd. Box N^?, Idgah Hills, Bhopal 462001
Madhya Pradesh
'
email:3n£hwhotcc^sify.cpm
Tql 0755-2666611
>
i.'
230
eg
Battle for Tobacco Control—The Indian Experience
j r I *1 PWmI Ml
ybi
ff
S. No. Contact person_______
Name of the centre
Dr Shekhar Salkar
Surgical Oncologist
General Secretary NOTE
. India
9.
Salgaokar Medical Research Centre
Chicalim, Goa 403711,
Vaidya Hospital, 1st Floor, Panaji, Goa 403001
Tel 0832-2423366
email: sssalkar@yahoo.co.in
• Bambolim: Medicine OPD of Goa Medical College
• Bicholim: Cairo's Hospital
• Chicalihri: Salgaoncar Medical Research Centre (SMRC)
• Vasco: Goa Shipyard Ltd., Vasco
. , Margap: Dr Gopal VaidyatClihic.
• Canacona: Dr Sadanand Prabhu's clinic
• Chimbel: Lifeline Foundation (Community-based unit)
• Mapusa: Teldulkar Hospital
Tel 9829049363
email: vivek_9sharma
©yahoo.com
Bhagwan Mahaveer Cancer Hospital and Eradication
Jawahar Lal Nehru Marg, Jaipur 302017
Pr Vivek Sharma
Consultant Physician
10.
■■■
.
:•
k ',..
.'
'■
<
■
■
-.•» ■
.
■■■.■.■■
■
'.
.
O^S.,nk.
Prqt^rbf Psychiatry;
i.,
Vivek Rew-d -
■
Contact details__________
Satellite centres
-
■■■■
■■
______________________ _
Satellite centres
. Ayurvedic Clinic, University Campus Dispensary'University
than, Jaipur
.
.
•• Rohm No- 217, OPD Block, Sant9^Ppri?.bhjl;MmQfi?l
. I22j5?”','r'htt""'Bh’”"‘an8hMaro
XSS^S^SS^
j ; -Ty 0^26995311
ilSS.
rNIMHANS): Banaalore
k- kVk;;
;
v,.•
■
ema.l. mkl@nImhanS.kar.nlc.in
,,
,
,k,;;
..
'T£ss s~s
ai (private:clinic)k<<,;
k .
/elopment Centre, , . ■
...
.
?;V
■
7
. .
•■
■
13.
■■
K ’.
.
.
Kesearcn^ntre
Anna Nagar (private clinic)
G'schenie< “ty of
'* WdM’^^naf^ Natlona, S
■
■'
.;
A?-
■ •
= Velathery Chennai-42 (NGO) .
■' • • -J • -
.
..
Dr Raj Kumar
Senior Lecturer
.
.
• Presidency College, Chennai 05
• Corporation Dispensary, Kamarajar Nagar, Thiruvanmiyur/Chenhai
• Q^rpOfation Maternity and Child Weifdre Centre, Thiruvanfniytir,
Chennai
• Shree Ramakrishna Institute of OncoloQyxand Research, Coimbatore 44
• Shreerhandfaptabhu Jain College, Minjur 03
• Professor of Radiation Oncology, Cancer Institute
18 Sardan Palil.Road, Adyar, Chennai 600029
•
Department of Respiratory Medicine
Tel 011-27667102
email: rajkumar_27563
Vallabhbhai Patel Chest institute
@yahoo.co.in
. . ,x University, of Delhi, Delhi 110007
231
V-i
Tobacco Control: What Works?
7-4
Policy Interventions:
A Comprehensive Ban
on Advertising
‘Cigarettes are the most marketed products in
the world. There is no reliable estimate of global
cigarette marketing expenditures, but roughly
it is estimated to be in tens of billions of US
dollars a year. Cigarette marketing is bolder and
more aggressive in developing countries than in
developed countries. Tobacco advertising is
common in television, radio, sports, arts, music,
fashion and street events, adventure tours,
contests, give-aways and the internet. There are
also hidden advertisements such as showing of
cigarette smoking scenes and other tobacco
products in films, sponsorship of universities,
good-will donations to community events, and
advertising of other goods and products bearing
the brand name of tobacco products.’73
It has long been recognized that reducing or
eliminating advertising of tobacco products
is important for tobacco control. Many
countries have taken steps to reduce tobacco
advertising, including prohibition of advertis
ing at the point of sale.74 Several countries,
including India, have banned the advertising
of tobacco products to a variable extent.
Recognizing the impact of tobacco
advertisements and promotional activities,
the Framework Convention on Tobacco Control
(FCTC) (Article 13) has called upon countries
to undertake a comprehensive ban of all
tobacco advertising, promotion and sponsor
ship to reduce the consumption of tobacco
products.75 The Indian Act for tobacco control
(Cigarettes and Other Tobacco Products Act,
2003) banned all forms of advertising of
tobacco products—except at the point of
sale.76
Tobacco advertising and promotion
In places where advertising is permitted, the
largest single expenditure of tobacco companies
is devoted to advertising and promotion, which
exceeds the amount spent on purchasing tobacco
leaf.77 A majority of studies have shown that
tobacco advertising leads to an increase in
consumption. Tobacco advertising also has a
powerful effect on young people. Tobacco
promotion activities are causally related to the
onset of smoking in adolescents, and exposure
to cigarette advertising is predictive of smoking
among adolescents. There is an increase in the
prevalence of use of brands, as well as in the
prevalence of smoking altogether, after the
introduction of brand advertisements that
appeal to young people.78
The impact of tobacco advertising
on consumption
Econometric research evidence '
Most econometric studies have found that
increased expenditure on tobacco advertising
increases the demand for cigarettes, while
banning advertising leads to a reduction in
tobacco consumption. A meta-analysis of such
studies found that tobacco advertising signifi
cantly increased tobacco sales.79
Research evidence within a country before
and after a ban on advertisements
Several studies have yielded convincing data that
a complete ban on advertising makes an
important contribution towards reducing the
prevalence of smoking.79 Some of them are
summarized in Table 7.8.
International comparison of trends in
tobacco consumption and anti-tobacco
measures
A study by the New Zealand government, which
examined the trends in consumption and
Tobacco Control in India
I
Table 7.8 Study results within a country before and after a ban on advertising
...
. .
—
. ..
. .
; . 6C
____' .
^O/^^Mpletebanonad
' •
ng.::\ : Long-term reduction ,n tlje'
-nation . premie of sowing by 9%
fiBBSS ■
I®
riiyeductiod'df.4% dn •
alcnce oF smoking '
n-iri tobacco’salesiby:
Fi
ipg in
■ /Reduction Of smokurg prevalence
M
advertising of tobacco in 33 countries during
1970-1986, demonstrated that the higher the
degree of governmental control on tobacco
advertising and sponsorship, the larger the
annual reduction of tobacco consumption. A
cross-sectional time series analysis in 22
Organization for Economic Cooperation and
, Development (OECD) countries, during 19601986, concluded that increasingly strict
regulation of advertising causes corresponding
reduction in tobacco consumption.79
When countries ban tobacco advertising in one
medium, such as television, the industry can
substitute advertising in otheY media with little
or no effect on overall marketing expenditure. If
the most comprehensive restrictions were in
place, tobacco consumption would fall by more
than 6% in high-income countries. Modelling
based on these estimates suggests that the
European Union’s ban on advertising could
reduce cigarette consumption within the
European Union by nearly 7%.80 Another study
in 102 countries compared consumption trends
over time in countries with relatively complete
bans on advertising and promotion, and those
with no such bans. In the countries with nearly
complete bans, the downward trend in
consumption was much steeper (Fig. 7.4). In
Fig. 7.4, it can be noted that the group with
comprehensive bans starts at a higher
consumption level than the non-ban group but
282
at the end of the study period, has a lower
consumption level. This change was due to the
higher negative growth in the countries where
the ban was operable.80,81
Advertising and promotion of tobacco products
attract children’s attention, and they remember
its messages. There is also growing evidence that
£
£
o
o
Q.
1750-1
1700-
Ban
C
O
E
w
1650-
§
1600-
S
1550-
E
No ban
ro
ui
1500-
ro
<
1450
1981
1991
Year
Fig. 7.4 Trends in weighted cigarette
consumption per capita in countries with a
comprehensive ban compared with countries
with no ban00,81
Source: Softer, Henry. The control of tobacco advertising
and promotion. Background paper, cited by Jha and
Chaloupka
— Tobacco Control: What Works?
r
the industry is directing increasing shares of its
advertising and promotion activity toward
markets where there is judged to be growth or
potential for growth, including some youth
markets among whom smoking has until recently
been uncommon.80
jI
i
An Indian study showed very high exposure of
children to tobacco product advertisements. In
Uttar Pradesh, 8 in every 10 boys and girls saw a
tobacco product (cigarette or gutka) advertise
ment on billboards and 6 in every 10 saw such
advertisements in other media. One in every 5
students was offered free cigarettes from a
tobacco company representative. Six out of every
10 students in Uttar Pradesh said they saw
cigarette advertisements on TV, in the
newspapers and at social events.82
Current cigarette smokers are significantly more
likely than never-users to report watching
cigarette advertisements in the print media,
including newspapers. Current cigarette smokers
were 12 times more likely than never-users to
report being offered free cigarette samples by a
tobacco company. Even exposure to gutka/paan
masala advertisements on billboards was
reported to be very high.
Current smokeless tobacco users are significantly
more likely than never-users to report watching
gutka/paan masala advertisements in the print
media, including newspapers. Current smokeless
tobacco users were five times more likely than
never-users to report being offered free gutka/
paan masala samples by a tobacco company. In
Uttar Pradesh, over half of the students (53%)
had seen several beedi advertisements on
billboards and nearly one-third saw them at
social events (31.1%). Current beedi smokers
(69.7%) were significantly more likely than
never-users (36.1%) to report watching beedi
advertisements at social gatherings.82
To achieve an impact on tobacco consumption
by the youth, measures such as increased health
education should be combined with a ban on
advertising. A combination of an increase in
tobacco prices and a complete ban on advertising
has proved to be more effective than either
measure on its own.79
Outdoor advertising
Outdoor advertising (e.g. billboards or posters)
has always been heavily used by the tobacco
industry. Voluntary restrictions on outdoor
advertising, such as agreements not to place
advertisements on billboards within a certain
distance of schools, have not been effective in
international experience. One study showed that
despite such an agreement, during a 6-month
period in 1994, tobacco advertisements were
posted on two-thirds of the billboards near
schools. In 1995, tobacco advertisements were
posted near 40% of the schools.79
Tobacco advertising and display of
tobacco products at the point of sale
Point-of-sale advertising and promotion directly
influence the products and brands that children •
buy and use. Point-of-sale advertising and
promotions target and attract shoppers right at
the places where they can immediately buy the
specific products or brands. More specifically,
point-of-sale tobacco advertising and promotion
may have a direct impact not only on which
brands of cigarettes children buy but also on
the number of children who buy cigarettes.83
Any weakness in the legislation regarding
advertisements would lead to misuse of the gaps
in the tobacco lobby. It has been recommended
that the following fundamentals be incorporated
into legislative drafts:74
• Prohibit any advertisements of any kind
everywhere, including at the point of sale.
• Prohibit advertising of price discounting; for
example, no ‘was/is’ signs, no crossed out
prices with the new price underneath. Price
discounting is attractive to children and
teenagers who are price sensitive.
• Ensure that the prohibition covers all potential
and actual gimcracks, baubles and gimmicks.
2^37;
ft
Tobacco Control in India
•
•
•
•
•
•
•
Ensure that it precludes flags, banners,
clothing, mobiles, wall hangings, carpets, coin
mats, clocks, watches, internally lit revolving
cabinets and objects in associated colours and
themes, as well as colour coding, etc. v
Prohibit lighting directed at product displays.
Prohibit value-added marketing devices such
as give-aways with products; for example,
cigarette lighters, calendars, books, maps,
diaries, CDs, toys or cosmetics. These are
particularly attractive to children.
Prohibit display in association with or near
products marketed for children (such as toys,
videos, candy, sweets, crisps).
Prohibit toys or confectionery that resemble
tobacco or cigarettes.
Prohibit audible as well as visual advertising.
If possible, prevent misleading statements
such as ‘light’ or ‘mild’.
If possible, prohibit the industry from making
false or misleading statements to retailers
about display legislation. This particular
provision in the Tasmanian legislation has
proved invaluable in preventing tobacco
representatives from telling retailers that a
particular display is lawful, when it is not.
This provision has substantially enhanced the
efficacy of enforcement mechanisms.
There are other useful legislative actions that
should be tied or linked to the primary tobacco
legislation. Licensing of tobacco product sellers
might help to find the seller, cancel the license in
case of violation of legislation and generate
revenue from the licensing process, which can
be used for the enforcement process. Infrin
gement notices improve compliance rates, allow
swift and sure ‘punishment’ for breaches of
display provisions, without the complexity and
cost of launching prosecution action, and have
an immediate ‘educative’ effect on retailers.74
There should be large notices in shops regarding
the legislation and should include health
warnings (both graphic and written), as well as
information about who to contact in the
government regarding breaches and access to
cessation programmes.74
284
Nominated officers might be appointed and
trained to undertake enforcement and education
work, and empowered by legislation to issue onthe-spot fines. Such an enforcement regimen
markedly enhances community involvement in
tobacco control activities, and reduces reliance
on governments.74
Other forms of tobacco promotion
As more and more countries impose total or
partial bans on tobacco advertising, the industry
is finding new ways to publicize their brands,
especially among the youth. Such ‘indirect
advertising’ methods include: sponsorship of
sports or cultural events; displays at points of
sale; ‘brand stretching’, where tobacco brand
names are used as part of other product names;
product placement in television and film shows;
direct mailing, special sales promotions and
samples.78
Tobacco companies consistently predict that bans
on advertisement will have a severe adverse
impact on advertisers, the media and the
economy as a whole. In most cases, however,
tobacco advertising constitutes only a small
percentage of the total advertising revenue,
minimizing the economic impact on media
outlets currently accepting tobacco advertise
ments. Several studies have shown that despite a
total ban on tobacco advertising on television
and radio, the advertising revenue went up by
500% in Hong Kong and 42% in Thailand.78
Implications for India
The Cigarettes and Other Tobacco Products Act,
2003 has banned direct and indirect advertising
of all tobacco products. However, advertising has
been permitted at the ‘point of sale’ of tobacco
products. The restrictions placed on display
boards at such sites are not being strictly
observed by vendors and the tobacco industry.
Further, there is the danger that the industry
may rapidly increase the number and type of
outlets where tobacco products are sold and
Tobacco Control: What Works?
festoon markets with display boards at supposed
‘points of sale’. It is, therefore, ideal if the Act is
amended to extend the ban to such ‘point-ofsale’ advertising as well. The danger of cleverly
disguised surrogate advertising also exists and
needs to be carefully monitored and countered
through effective enforcement of the Act.
I
i
It has been found that only restrictions on
content and placement of advertisements or bans
in one or two categories of the media are not
effective. However, the evidence suggests that
tobacco control programmes with comprehensive
advertising bans would reduce tobacco
consumption. Counter-advertising, where the
media is used to promote public health, also
reduces cigarette consumption. The taxation on
advertising has also been found to reduce total
advertising with the additional advantage of
raising revenue that could be used to fund counter
advertising. Therefore, policy options for a
comprehensive ban on tobacco advertising might
include limitations on the content of
advertisements, restrictions on the placement of
advertisements, restrictions on the time that
cigarette advertising can be placed on the
broadcast media, total bans in multiple media,
counter-advertising, taxation on advertising, and
prevention and penalizing of cross-border
advertising (as discussed in Section 6.3)-81
7.4 POLICY INTERVENTION: COMPREHENSIVE BAN ON ADVERTISING
KEY MESSAGES
• There is convincing evidence that tobacco advertising plays an important part in encouraging
non-smokers to begin smoking.
• When countries ban tobacco advertising in one medium, such as television, the industry can
substitute advertising in other media with little or no effect on overall marketing expenditures.
. Comprehensive bans on tobacco advertising and promotion can result in a considerable
reduction of tobacco consumption at the national level.
• A complete ban on advertisements coupled with an intensive public information campaign
on the ill effects of using tobacco products will lead to a reduction in tobacco consumption
by 6%.79
• In India, surrogate advertisements are still prevalent in the media and the existing laws
need to be strengthened and enforced.
Tobacco Control in India
7.5
Policy Interventions:
Packaging and Labelling
of Tobacco Products
statutory warning, ‘Cigarette smoking is
injurious to health’. The Act provided specific
instructions related to minimum font size,
colour contrast, etc. However, these guidelines
were often not followed.85 A recently enacted
legislation for tobacco control, the Cigarettes
and Other Tobacco Products Act, 2003 contains
provisions such as inclusion of a mandatory
health warning, which is legible and conspicuous
(detailed in Section 6.1).86
The FCTC has provided guidelines for the
Several studies have revealed that many smokers
packaging and labelling of tobacco products and
still do not know that tobacco causes disease and
called upon countries to adopt and implement,
premature death, while many others know little
in accordance with their national laws, effective
beyond a vague notion that ‘smoking is bad for
measures to ensure that tobacco product
you’, even in developed countries such as the
packaging and labelling do not promote a tobacco
USA.84 This is even more true of developing
product by any means.87
countries and of non-smoking forms of tobacco ‘
use. Thus, in developing countries such as India,
there is a clear need for effective ways to alert
Effectiveness of health messages
tobacco users about tobacco-related health risks
associated with all forms of tobacco use and inform
There is sufficient evidence to show that
them about the benefits of quitting.84
prominent health warnings and messages on
tobacco product packages increase both the
Consumer protection laws in some countries
awareness of risks and the desire to quit among
require that information be provided to smokers
smokers. The rotation of messages has been
about the health effects of tobacco use.84 A
found to help in keeping this information from
tobacco product manufacturer generally has a
becoming stale and boring. Health messages
legal duty to warn consumers of any foreseeable
continue to be effective, even if the population
hazards associated with the product so that
has become more informed about the dangers of
consumers may exercise ‘informed choice’ in
tobacco use over time, provided the-messages
deciding to use the product. While many tobacco
are sufficiently prominent and contain hard
users in the world generally know that tobacco
hitting factual information. It was reported that,
use is harmful, studies have shown that most
in Brazil, calls to the Quit Tobacco hotline for
smokers are unaware of the true risks, even in
cessation assistance increased by almost 300%
countries in which there is a great deal of publicity
after picture-based warnings were introduced.88
about the health hazards of tobacco. Smokers
tend to be even less aware of the risks of tobacco
The tobacco industry has responded to these
smoke on others.85 The information provided on
packaging regulations by devising methods to
the packaging of tobacco products is an obvious
evade or subvert the spirit of health warnings
and essential mode of communicating these
and reduce their efficacy. In recognition of such
messages to tobacco users.
industry tactics, it is advisable to include
prescribed messages on individual sticks of
Many countries have introduced regulations
smoked products and individual portion pouches
related to the packaging and labelling of tobacco
of smokeless products.88
products. The Government of India, in the
Cigarette Act, 1975 had called upon all packages
In Canada, there has been widespread support
and advertisements of cigarettes to carry a
for the health warnings on cigarette packages.
7^
22a
Tobacco Control: What Works?
r
For most people, these warnings are an accurate
and important source of information. Most
smokers have been found to read the health
messages every day. More than 7 in 10 adult
smokers and almost 9 in 10 youth smokers
consider health warnings to be effective as they
inform them about health effects, compel them
to smoke less around other people, make smoking
less attractive and increase their desire to quit
smoking.89
Smokers who read, think about and discuss
health warnings are more likely to quit, attempt
to quit or reduce their smoking. Health warnings
would be more effective if their content is more
positive and if the negative messages about the
health impacts of smoking are combined with
positive messages about the benefits of quitting
smoking.89
Experience from other countries shows that for
youth smokers, cigarette packaging is a major
source of information about the health effects of
smoking. It is reported that youth smokers look
at the packaging more often than adult smokers
and they are frequent readers of health
information messages on the back panel of
cigarette slide-and-shell packs.89
Studies from Canada indicate that tobacco
labelling should be such that even people with
low literacy skills are able to read and understand
the messages. If the words, images and concepts
used in the health warnings are unable to
communicate the message effectively to this group,
they are more likely to reject the messages than
make an effort to understand them.89
In developing countries, it is important to target
people who consume tobacco products, as not many
of them have access to information about the
hazards of smoking. Large health warnings are
likely to detract them from the glamour and appeal
of tobacco packages, making them less likely to be
seen as stylish accessories. Strong warnings might '
also help to create a social milieu where non
smoking is the norm. They might motivate
smokers to find help if they want to quit.84
Health warnings are weak, small or non
existent in many other parts of the world,
especially in developing countries. It has been
reported that more than 40 developing
countries do not require any warnings at all.84
Developing countries
receive inferior
information about the hazards of smoking,
which is not justifiable, especially since about
80% of the world’s smokers live in developing
countries. Therefore, there is a need for detailed
specifications to be included in the legislation
or regulations governing the information
required on tobacco packs, to prevent
companies from making health warnings
difficult to read or weak in content.84
Health warning message labelling on the product
package is a critical component of a comprehen
sive tobacco control strategy. Health warning
message labels are a cost-effective way to inform
the public, especially smokers, of the hazards of
tobacco use. The impact of health warning
messages should be regularly evaluated for their
effectiveness.90
Characteristics of effective health
warnings
The WHO and World Bank recommended that
effective health warnings should have the
following characteristics.84
Content
To be effective, health warnings should contain
a clear and unequivocal message about the
dangers of tobacco use, in simple and stark terms
(Box 7.7).84 The wording of the message should
be simple, in the principal languages of the
country. The nature and extent of risk, and how
to avoid or reduce the risks should be explained
and addressed directly to the reader using the
word ‘you’. Technical language should always be
avoided. The use of marker words, such as
‘WARNING’, has been suggested.84
Information about sources for help in cessation
(e.g. a toll-free quit line number, an Internet
7r®7
’r
Tobacco Control in India
'1
front and back of the package. The warning
should not be hidden or obscured by other written
or pictorial matter, or when the packet is open.84
IQiih]
•
a ‘hrs
>
I
1
Pictures
Jbbacc-o snide ImiJs Kn
^11
s"'4 Z "'T e
j-JpotLloss; and
:
and/or physical address where more informa
tion is available, quitting tips, and/or advice
which helps in quitting) should also be included.
Misleading terms, such as ‘light’, ‘low tar’, or
‘mild’, which give the wrong impression that
tobacco at lower tar and/or nicotine concentra
tions is safer, should be banned.84
' Format and font
The warning message should be printed in easyto-read black type on a white background (or
vice versa) and large, upper case letters should
be used. Glossy surface coatings and metallic
inks should be avoided. A flat or matte finish
will make the warnings legible under a wide
range of lighting conditions. The text should be
indelible and irremovably fixed, and a black
border should surround the message in a way
that does not interfere with the text of the
warning or the information given.84 There is
also evidence that limiting colour choices to
black and white, to achieve maximum contrast,
also enhances recall. Regulations should be
based on performance standards designed to
ensure that consumers achieve recall rates of
the health warning information comparable to
recall rates for other aspects of the package,
including brand name.91
Location
The health warnings should be on the top of the
Experience with pictograms in Canada and
Brazil shows that large warnings combined with
photos are effective in discouraging smoking and
increasing public awareness of the health effects
of smoking. In a study conducted among 633
Canadian smokers nine months after new, large
pictorial warnings were introduced, 58% reported
that the pictures had made them think more
about the health effects of smoking; 44% said
that the new warnings had increased their
motivation to quit smoking; and 38% of the
smokers who tried to quit said that the new
warnings were a factor in motivating their
attempt.84 In a study conducted in 2002 among
2216 Brazilians 18 years or older, 3 months after
the introduction of new pictorial warnings, 73%
of smokers approved of them, 54% had changed
their opinion on the health consequences of
smoking and 67% said that the new health
warnings made them want to quit.84 There was a
strong impact on low-income and -education
groups. In Australia, it was found that stronger
warning labels resulted in a 29% increase in the
percentage of people who ‘always noticed’ the
warnings, and a 7% increase in people who did
not smoke, at least once due to the warnings.84
In Canada, the top half of the front as well as
back of cigarette packages must show one of 16
picture-based warnings. One of 16 additional
detailed messages is required inside the package,
either on an insert or on the inner ‘sliding’ part
of the package.84
Health, warning messages with pictures are
accessible to illiterate people, and provide
significantly more encouragement to quit and
to not start smoking than messages without
pictures. Pictures will help ensure that even
illiterate people receive important information,
empowering them to better protect their health.
Apart from delivering new information, pictures
elicit a visceral response in viewers, so their
7^
^«s=‘—
Tobacco Control: What Works?
Package inserts
I
impact is both cognitive (intellectual) and
affective (emotional) (Box 7.8). The pictures
should always be colourful and of the largest
size possible to be effective.84
Recently, the European Union come up with 42
hard-hitting picture warnings for cigarette packs
to deter people from smoking. Some of picture
based health warnings in Canada and the
European Union are illustrated in Figs y.s-y.S.
Additional health information could be provided
through inserts similar to those used with
prescription drugs, or on the inner ‘sliding’ part
of packages that have them. Along with textual
information on tobacco addiction and tips for
quitting, inserts should also contain pictures that
illustrate the hazards of tobacco.84
Timing
The time given to companies to implement new
warnings should be ju st enough to use up existing
stocks and print new packages. Although tobacco
companies will typically ask for a longer time, a
time allowance of 3-6 months has been found
to be sufficient.84
WAMHKS .,'2^
TOBACCO^* :e
WJRTSBABli
lift®
HEARTBREAKER
w«tr*ases
Tobswo Jse CM rew1’ i tee clews
•jf jr’ene* m vow Jwjrt. Cogged
> -7
i
■■
-
liSHl
• - S33HP!
.
- •
HMflh Cwadj- »V
’
ill®:
-t-J
S®i®
T^Z.
IK'
■"
Fig. 7.5 Canadian health warning providing
information on the relationship between
smoking and heart attack in Canada92
Fig. 7.6 Canadian health warning providing
information on the harmfuJ effects of smoking
during pregnancy92
_____
CIGARETTES
Cl CARETTES
Brand
:
■
-
Brand r
BMnn
■
f
i
i
:.a'siow .
K;f'“
j
Fig. 7.7 European Union health warning
providing information on the relationship
between smoking and death93
■■
Smoking clogs the arteries
-.
-
and strckss
.
Fig. 7.8 European Union health warning
providing information on the relationship
between smoking and heart diseases93
Tobacco Control in India
Disclosures of toxic substances
Among more than 4000 constituents of tobacco
smoke, over 60 are known or suspected carcino
gens. Studies from other countries have reported
that many smokers are confused about the
constituents of tobacco smoke. Therefore, to
exercise informed choice, it is essential that
tobacco product packages provide tobacco users
with prescribed factual information on the toxic
substances contained in the products and their
smoke.84
However, it is important to recognize the
problem with tar, nicotine and carbon monoxide
(CO) measurements, and disclosures of these
based on current testing methods.88 These
measure-ments are now recognized to be
misleading. Firstly, human smoking patterns vary
greatly and are not mimicked by the machine.
Secondly, modern cigarette designs facilitate
compensatory smoking (over-inhalation), which
may lead to the smoker taking in much greater
amounts of tar and nicotine than are measured
by the machine. The tobacco industry uses the,
measurement for its own benefit by using
descriptors such as ‘light’ and ‘mild’ on packages.
Such terms falsely reassure smokers who might
otherwise have quit the habit.94
Experiences from other countries suggest that
the machine-measured figures for tar, nicotirie
and CO should be removed from the packet,
and a realistic measure must be established for
regulatory purposes. The health warnings
qualitatively deal very well with the risks of
smoking, whereas misleading figures on the
packet can only do harm.94 The WHO’s Scientific
Advisory Committee on Tobacco Product
Regulation (SACTob) also recommends that
placing quantitative estimates of tar and nicotine
on tobacco products should be avoided.
However, consumers should be informed of the
existence, if not the levels, of these and other
hazardous constituents, such as tobacco-specific
nitrosamines, polycyclic aromatic hydrocarbons
and a host of others, and of the dangers they
pose.88
WBSW
Studies have found that smokers clearly support
the inclusion of toxic emissions’ information on
packaging. One-half of adult smokers and 6 in
10 young smokers look at or read the toxic
emissions statements on the side of cigarette
packages.89
A qualitative study has reported that the most
effective texts were short, clear and simple, and
presented only one substance with information
on the impact that the substance has on health.89
Generic packages
From the tobacco industry’s perspective, the
primary job of the package is to create a desire to
purchase and try the product. Therefore, cigarette
packaging can act as an advertisement. When
advertising is banned or strictly regulated, the
package could become a very important
marketing tool. With more and more regulations
coming up for controlling tobacco, tobacco
companies will focus on new areas of opportunity
which do not rely on conventional media, such
as new types and forms of packaging that can act
as a means of communication as well as using
famous trademarks from other fields on tobacco
products and sponsorships.88
Generic packaging is an important tobacco
control measure. Generic packaging for tobacco
products is plain, standardized packaging
stripped of its marketing appeal. The objective
of generic packaging is to ‘denormalize’ tobacco
product use and prevent the tobacco package
from being an alluring advertisement that under
mines health messages, confuses consumers
about the risks of tobacco use and otherwise
detracts from the government’s attempts to
ensure that consumers are aware of the hazards
of tobacco use. It has been suggested that
packages should be generic both inside and
outside.88
Studies in many countries have found that that
plain packaging would reduce experimentation
and ongoing smoking among adolescents.88 A
significant majority of adults refused to buy
§0
—Tobacco Control: What Works?
r
Marlboro cigarettes at half-price when they were
packaged in generic brown boxes, despite the
fact that they were assured of the original
quality. Apart from these, health messages on
plain packages were found to be more noticeable
and their presence more easily recalled than
messages on traditional tobacco packages.88
Labelling as a measure to control
smuggling
Tracking and tracing labelling requirements such
as manufacturer identification, countries of
origin and destination, tax stamp markings, etc.
are important to prevent smuggling. Tracking is
the systematic monitoring of the movement of
tobacco products from the place of manufacture,
where all relevant duties and taxes have been
paid, for the purpose of assisting the competent
authorities to detect, investigate and analyse
illicit manufacture and illicit trafficking. Tracing
means the ability of competent authorities to
recreate the route taken by a tobacco product
’ from the place of manufacture through the
distribution chain to the point where all relevant
duties and taxes have been paid.!8
Many countries have prohibited the sale of single
or unpackaged tobacco products, or packages
below a minimum size, which tend to be more
affordable and accessible to the youth, who are
especially price sensitive. Selling tobacco products
in packages also ensures that consumers are
provided with the prescribed messages, toxic
substance disclosures and other important
labelling information. If sales of single cigarettes
are prevalent because of a large informal sector, it
has been suggested that the manufacturers should
place prescribed messages on individual sticks of
smoked products as well as on packages.88
Belgium has the world’s largest tobacco warnings
(roughly 55% of the package, front and back)
whereas in Brazil, 100% of one principal display
panel must consist of a pictorial health warning.
In Canada, health messages comprise at least
50% of the package’s front and back panels, and
provide graphic pictorial depictions showing the
health effects of tobacco use.88
Ideally, the warning/information label should
cover at least 50% of both the front and back of
the package. Warnings must be large enough to
be easily noticed and read. The credibility of
warning messages, as well as the perceived risks
from tobacco use, increases proportionately with
increases in the size of the warnings.84
The tobacco industry’s tactics
When Brazil enacted its law requiring graphic
pictures on tobacco product packages to
accompany its health warnings, the tobacco
industry tried to delay implementation, arguing
that it did not have the technical capacity to
comply with the new requirements for pictures.^
The tobacco industry often uses such tactics to
delay or prevent the implementation of
stringent laws against tobacco (discussed in
Section 6.5). The industry also argues that there
will be economic and job losses in the packaging
and printing industries, as well as increased
smuggling’ due to labelling requirements.
However, these arguments are without basis
and are merely delaying tactics.88
Experience from many countries shows that the
tobacco industry usually tries to delay or block
more effective warnings. Governments should be
prepared to face these legal challenges, which
are often based on constitutional rights such as
free speech, or trade practices. The case for
tobacco control measures, including stronger
health warnings, is compelling, especially from a
human rights’ and consumer rights’ perspective.
Health-warning regulations should specify that
displaying health warnings on tobacco products
does not relieve tobacco companies of their
liability for damage caused by the use of their
tobacco products.84
■
sa s-
-r—iz
rft
Tobacco Control in India
i
BEEDI
- ________
CIGARETTE
-_____________
Brand Brand
A
Si1
A
It
ATTACK
-•
-
•
-
~
■
‘
KHAINI-GUTKHA
BEEDI
Brand Brand
J
Fig. 7.9 Examples of proposed health warnings on tobacco products in India, which are being
field-tested95
Health warnings on smokeless
I tobacco products
■
"■
?_______________ L_
In India, apart from, cigarettes or other smoking
tobacco products, smokeless tobacco products
should also carry the most effective labels
possible, due to the serious risk of disease and
addiction they pose, and because smokeless
tobacco use is widely prevalent among children
and adolescents.91 Studies on Canadian labels
have found 51% higher total recall rates for oral
snuff packaging, and 65% higher total recall rates
for chewing tobacco packaging, which justifies
the requirement of labels that are at least as
large as those in Canada.91
recognize the warning messages on them.
Therefore, it is advisable to considerably increase
the size of smokeless tobacco packages. In
addition to conveying proper health warning
messages and making them difficult to carry,
bigger packages also increase the cost of
production for tobacco companies.
Health warnings in India
The Cigarettes and Other Tobacco Products Act,
2003, has asked for the inclusion of a mandatory
health warning, which should include a picture
of a skull and cross-bones and may include other
pictorial warnings.86 Figure 7.9 shows some of
the proposed health warnings to be used on
The size of current smokeless tobacco products
packages in India is such that they can easily be
carried in the pockets and it is very difficult to
Indian tobacco packages, which are being fieldtested for their effectiveness.
Tobacco Control: What Works?
r
7.5 PACKAGING AND LABELLING OF TOBACCO PRODUCTS
KEY MESSAGES
• The WHO and the World Bank recommended warning labels on tobacco products, which are
an effective way to inform smokers about the hazards of tobacco consumption, encourage
smokers to quit, and discourage non-smokers from starting to smoke.
. Warnings are effective only if they contain multiple, strong and direct messages that are
prominently displayed.
. Health warning message labelling on the product package is a critical component of a
comprehensive tobacco control strategy. Health warning message labels are a cost-effective
way to inform the public, especially smokers, of the hazards of tobacco use.
"
Stec.’^.
>■■ ' '
«
■-—'
"''
.. .
. ..
-------------- --- . ...-r,
.
--
—7'-—
Tobacco Control in India
7.6
Protection of Vulnerable
Groups: A Human Rights'
Approach to Tobacco
Control
Good health should be an entitlement of every
citizen. However, it is widely recognized that
social, economic, and political conditions and
forces influence both the underlying determinants
of health and public policy, with conflicts of
interest and contradictions featuring as causes
and consequences. These contradictions in public
policy are especially evident in the case of tobacco
and its impact on health.
What is often not recognized, in the context of
tobacco control, is the particular vulnerability of
certain population groups for becoming the
victims of tobacco. These include the poor, the
young and women. In virtually every region of
the world, the poor consume tobacco more
frequently than the affluent sections of the
society. Education, in particular, has a major
effect on tobacco consumption. The higher the
level of education, the less likely is tobacco use.
The poor have less access to education and hence
are more vulnerable to acquiring and
maintaining tobacco use. The youth and women
of all countries, but especially those of develop
ing countries, have become prime targets for
the tobacco industry, which seeks multitudes of
new customers each year to replace the millions
who die from the deadly effects of tobacco. They
too are vulnerable in many respects, especially
when poverty intertwines with their age- or
gender-based susceptibility.
This requires that tobacco control policies must
encompass a human rights’ approach intended
to protect vulnerable groups from the hazards of
tobacco. This is particularly important because
; '
~~1
the tobacco industry frequently raises the bogey
of tobacco control policies infringing the
individual’s right to free choice and also sounds
the false alarm of the poor being adversely
affected by such policies (see Box 7.9). This
section examines the impact of tobacco on the
poor and addresses issues related to tobacco
control from a human rights’ perspective.
Box 7.9 Tobacco control: Resolving the
paradox of poverty_____________________
The poor use tobacco more frequently but the
products that they use most often are not taxed
because policy-makers are wary of increasing the
tax burdens of the poor. However, the high burden
of tobacco-related diseases among the poor, which
will result from such a policy, are ignored. This
paradox, of sparing the poor from tobacco taxes
but not saving them from tobacco-related deaths,
needs to be resolved through a tax policy that taxes
all tobacco products and uses a large fraction of
that revenue for welfare programmes intended to
serve the poor.
The false argument advanced by the tobacco
industry that tobacco control will propel many
farmers and workers into poverty, is unques
tioningly accepted by some policy-makers who
oppose tobacco control measures. Yet, the poor
(who consume tobacco in much larger numbers)
are the worst victims of the tobacco trade, as indeed
are the children who miss school to roll beedis and
remain entrapped in the cycle of poverty. It must
be recognized that tobacco control will alleviate
poverty rather than cause it.
e]«E
A recent report by Economic and Social Council
(ECOSOC) of the United Nations states that
‘Tobacco consumption is a major direct
contributor to increasing noncommunicable
diseases and an associative contributor to
communicable diseases such as tuberculosis.
Poverty facilitates the spread of diseases and
their treatment can impose a heavy financial
burden on poor households. Tobacco entails
heavy opportunity costs for poor households in
which addicted tobacco users spend a significant
amount of household resources on tobacco
consumption. In developing countries, among
<294
I
Tobacco Control: What Works?
F~
poor families, the proportion of household
expenditures used to purchase tobacco products
can easily represent up to 10 per cent of total
household expenditures. This means that these
families have less money to spend on basic items
such as food, education and health care. In
addition to its adverse health effects, tobacco
use can lead to increased health-care costs and
premature death. It also contributes to worsened
malnutrition and a higher illiteracy rate if
money that could have been used for food and
education is spent on tobacco instead’.96
person with postgraduate education.99 The
scheduled castes and tribes, who constitute a
socially and economically vulnerable group, were
also more likely to smoke than other castes. A
similar gradient was observed between the
household standard of living and smoking, with
smoking being 2.5 times more common in the
lowest of five grades compared to the highest."
Smoking was also more common in rural areas
and towns than in large cities.
Similarly, strong gradients were also observed
for chewing of tobacco. The least educated were
1.8 times more likely to chew tobacco than the
Globally and in India, smoking and smokeless
most
educated. Scheduled castes and tribes were
tobacco use is higher among the poor than the
more likely to chew tobacco than other castes,
rich and is accompanied by an increased risk
and the houses with the lowest standard of living
and prevalence of tobacco-related disease and
were twice as likely to chew as compared to the
premature death.97 Beedis and chewed tobacco
houses with the highest standard.99 The National
(gutka, paan masala, etc.) constitute the largest
percentage of tobacco use in India. Cigarettes • Sample Survey of 1995-1996 also reported that,
across India, those below the poverty line have a
used by the richer, more educated social segment
37% higher prevalence of regular use of non
account for only about 20% of tobacco use.
smoking tobacco compared to those below the
Beedis, used to a larger extent by low-income
poverty line, an 8% higher rate of smoking, and
groups, deliver more toxic products to the smoker
a 28% higher rate of regular alcohol consumption.
than other smoked tobacco products. Thus, the
It is therefore likely that the poor will
burden of tobacco-related diseases is higher in
this group. Increased taxes on cigarettes since ' disproportionately suffer the sequelae of these
risks in the future.100
the 1970s resulted in an increased consumption
of beedis, which do not have the same taxation
Studies show that the poor consume the most
or legal requirements for packing and labelling
toxic tobacco products, e.g. unbranded beedis
as cigarettes, thus keeping their costs lower.
manufactured with poor quality control and
sometimes laced with other narcotic drugs.
A study by Gajalakshmi et al. in Chennai,98,
Tobacco quid is used by poor women and men to
found higher smoking rates among less educated
ward off hunger during long tedious work in
men from the lower socioeconomic segments of
agriculture, construction and other labour. Of
society. Among illiterates, 64% of adult men
the pavement dwellers in Mumbai, 86% used
smoked: in those with less than 6 years of
tobacco, 49% consumed raw tobacco 5 times a
schooling 58% smoked; with 6-12 years of
day, 20% chewed 7-8 sachets/day of gutka, 30%
schooling 42% smoked; and with more than 12
smoked 11-12 beedis/^y, 24% chewed paan 4
years of schooling 21% of adult men smoked.
times a day, and 8% smoked cigarettes.101 On an
This marked gradient is in accordance with the
average, 15% of their monthly earnings of Rs
worldwide trend of a higher smoking prevalence
4500 were spent on tobacco, in preference to
among the poor and uneducated.
meeting basic needs. Street children in Mumbai
have a high rate of tobacco usage—46% use
An analysis of the National Family Health
gutka, 39-5% beedi, 28% cigarettes and 14% plain
Survey (NFHS), conducted in 1998-1999, shows
tambaku.™1 In an informal study, 7O%-8o% of
that tobacco smoking is inversely associated
the
over 100,000 street children in Bangalore
with educational status, with an illiterate person
were found to use tobacco products.
being three times more likely to smoke than a
Tobacco Control in India
~l
Table 7.10 Influence of occupation on tobacco consumption in north Indian males
. ...... '
5SiO
■ss/laridlotd
•*'
-
3'
awwsswsse.
f
■
It
SSSflwi
s
v
Cross-sectional surveys conducted by the All
India Institute of Medical Sciences during the
1990s revealed that tobacco consumption among
males was inversely related to the level of
education, with a higher prevalence among the
illiterate and semi-illiterate (Table 7.9). This was
true of urban, rural and industrial populations.102
When analysed by professional class, a similar
inverse relationship was observed, with unskilled
and semi-skilled labourers being the worst
affected by tobacco use (Table 7.10).
The ECOSOC report96 also highlights similar
facts from other developing countries:
• Some street children and other homeless
people in India spend more on tobacco than
on food, education or savings;
• A recent study in Bangladesh showed that
over 10.5 million currently malnourished
people could have an adequate diet if money
spent on tobacco was spent on food instead;
• Poor, rural households in Southwest China
spend over 11% of their total expenditure on
cigarettes;
• Preliminary results from an ongoing study in
3 provinces of Viet Nam found that over the
J;
course of a year, smokers spent 3.6 times
more on tobacco than on education, 2.5 times
more on tobacco than on clothes, and 1.9
times more on tobacco than for health care;
• A study in Poland, in 1996, showed that the
contribution of smoking to the risk of
premature death among males at 35-69 years
of age varies by education level; the risk of
dying during middle age due to tobaccorelated diseases was 5% among people with
higher education and nearly double (9%)
among persons with only primary and
secondary education.
According to the WHO, tobacco and poverty
create a vicious circle, from which it is often
difficult to escape. Tobacco tends to be consumed
by those who are poorer. In turn, it contributes
to poverty through loss of income, loss of
productivity, disease and death.103 Based on this
evidence; WHO observed the World No Tobacco
Day 2004, with the theme of Tobacco and
Poverty, conveying the main message that tobacco
increases the poverty of individuals, families and
nations. This is in contrast to over-simplistic and
widespread arguments that tobacco provides
wealth to governments and growers.
1^--'
Tobacco Control: What Works?
±xrer,yand9ender
_________ y
The ECOSOC report draws attention to the
global upward trend in women smoking, which
is now becoming an issue in the developing
world as well. It states ‘The tobacco industry
has already understood it and is heavily targeting
women to gain a part of the market which was
not available in the past. Tobacco advertising
vehicles images for women featuring vitality,
slimness, glamour, emancipation, etc... The new
gender behaviour can also have adverse social
and economic consequences. For example, it is
known that women often have less disposable
income than men and are more likely to spend
it on their children. When more women start
consuming tobacco at a higher rate, the
diversion of scarce family resources for tobacco
may significantly contribute to malnutrition and
higher rates of school drop-out, with potential
long term negative consequences.’96
Tobacco control and human rights
_________________________________________________________________________________________________________________________________________________________________
■■
In 2001, the National Human Rights
Commission (NHRC) of India considered the
issues related to tobacco control from the
perspective of human rights and concluded that
the following rights of an individual are violated
due to lack of tobacco control mechanisms in
India:104
1. Right to clean air
• A non-smoker is forced to inhale tobacco
smoke in public areas.
2. Rights of children
• Rights of born and unborn children are
violated when they are exposed to tobacco
smoke (active and passive) in the home or
public areas. They are the most vulnerable
and worst affected.
3. Right to information
• Both the smoker and non-smoker are not
provided with adequate information about
the harmful effects of tobacco products
and, in fact, are bombarded with
misinformation about tobacco products
through advertisements/events/celebrityand role model-linked promotion.
4. Right to education
• Both the smoker and non-smoker are not
adequately educated about the drastic illeffects of tobacco on- their personal and
public health.
5. Right to redressal
• Both the smoker/non-smoker do not have
any redressal mechanism for the injuries/
ill-effects suffered by them due to tobacco
products.
6. Right to tobacco cessation programme/
activities (as part of right to health)
• The smoker and his/her family have a
right to have access to various cessation
strategies.
In addition, there are also some rights of the
smoker which may be violated by regulatory
measures intended for tobacco control.
However, these have to be superseded in the
interest of public health and human rights of
the larger community.
Based on this assessment, the NHRC recommen
ded that:
• A comprehensive national tobacco policy
should be evolved at the highest level, in
consultation with all the stakeholders in
public health.
• A multisectoral national-level nodal agency
should be established for tobacco control with
strong representation from the legal, medical
and scientific communities.
• The right of people to access correct informa
tion related to the effects of tobacco
consumption must be promoted through
programmes of information, education and
communication. Such programmes should be
adequately supported through dedicated
resource allocation.
• Assistance for smoking cessation should be
integrated into the health care services.
• e?-
Tobacco Control in India
Role of the government
Given the objectives of protecting and
promoting public health, enabling conditions
need to be created to help individuals make
informed choices, to isolate the changing
patterns of vulnerability and develop effective
response mechanisms for combating the same.
It is important to realize that the human rights’
paradigm cannot operate in a legal vacuum.
Some existing authority needs to enunciate the
law and put into place appropriate enforcement
and redressal mechanisms. This is where the
government (state) comes in. To be able to
respect, protect and fulfil its human rights’
obligations, the government has to bring about
well-defined legislation to facilitate the
functioning of legal systems.
Today, the philosophy of ‘responsive communi
tarianism’ is gaining popularity among wide
sections of society. This essentially means
balancing individual rights with social
responsibilities, or individuality with the
community. The collective rights of the
community must have precedence over the rights
of the individual smoker, especially since tobacco
is now well recognized to be a ‘public bad’. In
asserting these principles, the government must
also recognize the special obligation to provide
for the poor and less educated sections of society
whose right to correct information is least
respected by the tobacco industry. Even in the
safeguarding of rights, special protection needs
to be provided to vulnerable groups.
The fundamental reciprocity between health and
human rights is well estabUshed and the need to
put in place a proper regulatory framework to aid
and nurture this synergy should be the guiding
lights of policy-makers and analysts in this field.
This is even more true of tobacco control than of
many other policies related to public health.
7.6 PROTECTION OF VULNERABLE GROUPS: A HUMAN RIGHTS APPROACH TO TOBACCO CONTROL
KEY MESSAGES
• The poor, the young and women are particularly vulnerable for becoming the victims of
tobacco.
• Tobacco control policies must encompass a human rights’ approach to protect vulnerable
groups from the hazards of tobacco.
• Tobacco smoking is inversely associated with educational status.
• Homeless people in India spend more on tobacco than on food, education or savings.
• Enabling conditions must be created to help individuals make informed choices.
S3
Tobacco Control: What Works?
r~
7.7
Community Interventions:
Protecting the Youth
from Tobacco
In 1996, Peto et al. estimated that unless current
trends changed, some 30%~40% of the 2.3
billion children and teenagers in the world
would become smokers in early adult life. Unless
action is taken now, about 250 million of these
future smokers will be killed by smoking.105
It is estimated that, as in other developing
countries, the most susceptible time for
initiation of tobacco use in India is during
adolescence and early adulthood, i.e. in the age
group of 15-24 years. The majority of users
start using tobacco before the age of 18 years,
while some even start as young as 10 years. It is
estimated that 5500 adolescents start using
tobacco every day in India, joining the 4 million
people under the age of 15 years who already
use tobacco regularly.106 This early age of
initiation points to an urgent need to plan
effective interventions for this vulnerable age
group.
The Government of India has been actively
working towards enforcing legislations to
prevent young people from having any access
to tobacco. The Cigarettes and Other Tobacco
Products (Prohibition of Advertisement and
Regulation of Trade and Commerce, Production,
Supply and Distribution) Act, 2003 enforced
from 1 May 2004 has provisions to protect the
youth in India. The Act prohibits the sale of
tobacco products to minors as well as within
100 yards of any educational institution.
One of the major goals of any tobacco control
effort is to prevent people from starting or
experimenting with tobacco. The target group
KU
should be the youth who are primarily non
users and are vulnerable as the industry
especially targets them.
Issues involved
Availability
The youth start using tobacco even before they
can understand its consequences, and the fact
that tobacco is addictive prevents them from
quitting when they become aware of its harmful
effects later in life. One of the goals of any
tobacco control policy should be to ensure that
tobacco products are neither available by direct
sale nor accessible through other sources to
youth.
Ban on sale to minors
Article 16 of the FCTC mentions about banning
sale to minors. The existing literature provides
mixed evidence on the effects of banning sale to
minors in reducing tobacco use among youth.
Wassermann et al. studied the impact of state
laws that restricted the sale or distribution of
cigarettes to minors. They found that although
these laws reduced the teenager’s probability of
taking to smoking, it did not affect the average
consumption by-young smokers. They attributed .
the latter to the weak enforcement of these laws
and vendors’ poor compliance with the law.107 A
study by Jones et al. showed that enforcement
of youth access laws led to a decrease in minors
purchasing in stores but there was a significant
increase in giving someone else money (social
source) to buy cigarettes for them.108
There have been different viewpoints opposing
the ban on sale to minors. It has been
commented that youth access programmes
which prevent the sale of cigarettes to teenagers
are ineffective and a drain on limited.resources.
It has also been expressed that such bans are
counterproductive because they reinforce the
tobacco industry’s ‘smoking is a way to look
adult’ message.109
Tobacco Control in India
Non-availability of tobacco products around
educational institutions
To restrict free availability of tobacco products
to minors, one easy strategy is to ensure that
tobacco products are not sold near educational
institutions.
Increasing prices through taxation
One of the mechanisms to raise tobacco prices
is taxation. A fundamental principle related to
taxation is that taxes which generate substantial
revenues while minimizing welfare losses
associated with the higher prices resulting from
the taxes, are preferable to those that result in
higher welfare losses. In the short run the
demand for tobacco products is relatively
inelastic. Thus, an increase in tobacco taxes,
although leading to reduction in use, will lead
to significant increases in revenue.110 Increasing
prices through tax increases is the single most
effective intervention to reduce tobacco demand.
It has been seen that a 10% price rise will lead to
a 4% reduction in demand (price elasticity of
-0.4) in high-income countries, and 8%
reduction in low- and middle-income countries
(price elasticity of -0.8). It has been seen that
young people, people belonging to a low
socioeconomic group and less educated people
are more price responsive.111 It has been
estimated that tax increase which would increase
the real price of cigarettes by 10% worldwide will
lead to 42 million smokers of the 1995 cohort
quitting and would prevent 10 million premature
tobacco-related deaths among them.111 In a study
in the USA, it was seen that increasing the price
of cigarettes increases the number of young adults
who quit smoking. The average price elasticity of
cessation was -0.35, i.e. a 10% increase in price
will lead to 3.5% reduction in demand.112
Increases in the price of cigarettes will decrease
the prevalence of smoking and the number of
cigarettes smoked both by the youth and adults.
Lower-income and minority smokers were more
likely than other smokers to be encouraged to
quit in response to a price increase and would
thus obtain health benefits attributable to
quitting.113
The change in smoking behaviour is most
dramatic among the youth exposed to the largest
price increases, suggesting a sustained impact
of higher price on cigarette consumption. Large
cigarette tax increases would result in both
substantially higher quitting rates and a
considerable drop in smoking intensity.114
Gender difference
Young men are much more responsive to
changes in the price of cigarettes than young
women. The price elasticity for young men is
almost twice as large as that for young women.115
Restricting access through regulating
packaging sizes
Ensuring that cigarettes and beedis be sold only
in bigger packs of twenties or more will restrict
purchase by the youth who have limited
resources to buy these products. Similarly,
chewable tobacco (such as gutka, khaini, etc.) is
Box 7,10 Tobacco tax policy
A good tobacco tax policy will seek to do the
following:116
1. Raise the price of tobacco products substantially.
To maximize impact, each tax increase should
increase consumer prices by at least 20%.
2. Ensure that tax levels are not eroded by inflation.
In some countries, for example, in Australia and
New Zealand, tax rates are increased regularly in
line with increases in consumer prices. Tobacco
taxes should be increased frequently and should
account for the rise in disposable incomes.
3. Prevent loopholes that would direct consumers to
switch to cheaper tobacco products. This entails
that there be no price differentiation between
various forms of tobacco products.
4. Link the tobacco tax policies to overall tobacco
control policies to highlight the health basis to
the tax, i.e. to show the health benefits in terms of
reduced consumption and the fact that the revenue
generated can be used for promoting health.
Tobacco taxes should not only be a mechanism
for revenue generation but can also be used for
tobacco control measures,, such as spreading health
awareness among youth and adults, and providing
tobacco cessation strategies such as nicotine
replacement therapy (NRT).
5. Take measures that will prevent the smuggling of
tobacco products.
Tobacco Control: What Works?
c
currently available in sachets, which make these
products available at a very low cost. It is
important that the packaging sizes of all tobacco
products be regulated in India. Increasing the
sizes of tobacco product packages would ensure
that the cost is high enough to make it less
affordable for the youth, who are tempted to
experiment with these tobacco products due to
their small packaging size which makes the
product easily accessible to them for purchase
and concealment.
Awareness and advocacy
It has been well established that awareness and
advocacy related to tobacco avoidance and
control prevents or reduces tobacco use among
youth.117-119 In India, it has been seen that
students in whom school-based interventions
were carried out were less likely to receive offers,
experiment with or intend to use tobacco.117
Among regular smokers, it was found that those
who were engaged in anti-tobacco advocacy were
more likely to reduce their own use. The
decrease was sustained even after six months.
The goal of the advocacy programme was to
increase the student’s awareness of the factors
in the school and community environment that
promote cigarette use.118
A well-designed public education campaign that
is integrated with community- and school-based
programmes, strong enforcement efforts, and
help for smokers who want to quit, can
successfully counter tobacco industry marketing.
Such integrated programmes have been
demonstrated to lower smoking among young
people by as much as 4O%.119 A 15-year follow
up study as part of the North Karelia Youth
Project showed that the reduction in tobacco
use produced by a mass media intervention
combined with a school- and community-based
education programme lasts over time. The mean
lifetime cigarette consumption was 22% lower
among programme subjects than among control
subjects.119
The Massachusetts Tobacco Control Campaign,
which has a sizeable public education
component, has been effective in increasing
public perception of the harms of cigarette
smoking, and is associated with a substantial
decline in cigarette consumption. A 1997
independent evaluation of the Massachusetts
campaign found that tobacco consumption
dropped by 31% from 1992 to the first half of
1997—more than triple the rate of decline
observed for the rest of the nation.119
In its early years, the California Tobacco Control
Programme produced a 10%—13% long term
decline in cigarette consumption, with about a
fifth of the decline caused by the media campaign
alone. A study found that the California anti
tobacco media campaign reduced sales of
cigarettes by 232 million packs between the third
quarter of 1990 and the fourth quarter of 1992.119
A 1995 study of California’s anti-smoking
programme found that anti-smoking media
campaigns are an effective way of reducing
cigarette consumption, and noted that higher
funding levels produced more powerful results.119
A 1994 study determined that anti-smoking
advertising decreased smoking beyond the
effects of school-based interventions. Students
who were exposed to the media plus school
interventions were found to be at lower risk for
smoking than those only receiving school
interventions.119 A 1992 study found that a fiveyear intervention involving a media campaign,
community programmes, and school-based
instruction resulted in significantly lower
smoking rates. At the end of high school, just
14.6% of students in the intervention community
were weekly smokers, compared to 24.1% of those
in the control community.119 A 1997 study found
that, in terms of cost per years of life gained,
mass media and education campaigns are
currently among the most cost-effective methods
available to prevent or reduce tobacco use.119
Researchers have mixed views on the success of
awareness programmes among the youth.
Though some programmes have shown a
positive impact on increasing knowledge,
positively altered attitudes of youth and reduced
tobacco use among them, there have been a few
■
.
l-J «■«■» •->.. .V
'
____ ...
■' ?
Tobacco Control in India
unsuccessful school health programmes that
failed to demonstrate a posi tive impact.
and project the use of tobacco as being socially
acceptable.
An opposite effect was seen in a school-based
programme in Montreal, where it was seen that
children exposed to the programme were more
likely to initiate and continue smoking than
children in the control group. The reason for
this was inadequate attention in programme
development to the diverse cultural origins of
the population targeted.120 Cultural differences
play an important role in comparing school
health programmes globally. The strategies and
channels of intervention delivery are the most
crucial elements to be taken into account. In a
country such as India, involving teachers in
intervention delivery has proven to be very
effective as teachers’ viewpoints are given the
highest priority by the youth when they are in
school. This may not necessarily be true in other
countries, especially in the West.
There is a strong temporal and causal relation
ship between viewing smoking in films and
initiation of smoking among adolescents. For
example, it was shown that 12- and 13-year-old
boys whose favourite television sports included
motor racing (sponsored by tobacco companies)
were twice as likely to become regular smokers
compared to those who did not watch it.123,124
Comprehensive ban on advertisements
and counter advertising
A comprehensive ban includes a ban on
advertisements of tobacco products in all direct
and indirect forms, i.e. print and mass media,
point-of-sale advertisements, ban on surrogate
advertising or brand stretching, and should also
include effective counter-advertising.
Tobacco advertising and promotion increases
the likelihood that adolescents will start to use
the product. The impact of tobacco advertising
on the youth is a well researched area globally.
Non-smoking adolescents who were more aware
of tobacco advertising or receptive to it were
more likely to have experimented with cigarettes
or become smokers at follow-up.121 Receptivity
to tobacco advertising and promotion is an
important factor in progressing from experimen
tation to established smoking among adole
scents.122 Advertising lures gullible youth and
children through glamorous and deceptive
promotional stunts. Advertisements project
tobacco use in congenial surroundings or
associate the brand name with idolized role
models, legitimize the habit in young minds
• 302
Point-of-sale tobacco advertising has the
potential to increase significantly positive brand
user imagery, and hence not only adds to long
term user imagery, but would increase the
likelihood of impulse purchasing.125 This is
relevant to the Indian context, as the Indian
Tobacco Control Bill of 2003 permits point-ofsale advertising while banning all other forms of
advertising.
Evidence suggests that comprehensive bans on
tobacco advertising can reduce tobacco con
sumption. A partial advertising ban has little or
no effect because of the opportunities for
substitution by other forms of advertising.111 In
spite of the fact that anti-tobacco advertising has
a protective effect, it is unable to counteract the
' effects of pro-tobacco advertising.126
Anti-smoking advertising appears to have more
reliable positive effects on those in pre
adolescence or early adolescence by preventing
experimentation. The effects of anti-smoking
advertising on youth smoking can be enhanced
by the use of other tobacco control strategies,
and may be dampened by tobacco advertising
and marketing.127 Because perceived ability to
quit makes adolescents more likely to progress
to experimentation and repeated use, counter
advertising should include messages about
addiction and the difficulties associated with
quitting.122
Advertisements designed to discredit the tobacco
industry should mention specific companies, to
make the counter-advertising more effective.
This will ensure that people know about the
— Tobacco Control: What Works?
tobacco industry’s corporate identities, and
young people who know about these identities
tend to view the company less favourably.128
Intensive and sustained efforts to ‘counter
market’ tobacco among teenagers are essential
to negate the friendly familiarity of the tobacco
industry and to communicate the true health
and social costs of tobacco use. These should
highlight a tobacco-free lifestyle as the majority
lifestyle of diverse and interesting individuals.
Constructive alternatives to tobacco use should
be offered and the dangers of tobacco use
explained in a personal and emotional way.129
Some other examples of the positive effect of
counter-advertising on the youth are discussed
below:”9
1. A 2002 report of the Florida Youth Tobacco
Survey showed that between 1998 and 2002,
current cigarette use among middle school
students declined by 50^, and current
cigarette use among high school students
declined by 35%. These declines followed the
implementation of the Florida Pilot Program
on Tobacco Control, which included an
aggressive
counter-marketing
media
campaign.
2. A 2000 study showed that youth in
Massachusetts, 12-13 years of age, who
reported exposure to anti-smoking television
advertisements at baseline, were significantly
less likely to have progressed to established
smoking at follow up than youth who did
not report exposure to anti-smoking
television advertisements.
Introduction to positive, healthy role models,
added to established anti-tobacco norms, can
tremendously curb the desire of the youth to
experiment with tobacco products.
Restriction of smoking in schools, the
home and public places
Smoke-free workplaces reduce the prevalence
of smoking as well as its consumption. The
combined effect of people quitting smoking and
reducing consumption reduces total cigarette
consumption by 29%.131
Regulations restricting smoking in public places
appear to have a considerable impact on teenage
smoking behaviour. In. contrast to adults,
regulations affect the teenager’s decision to
become a smoker rather than the number of
cigarettes smoked.131 Smoking restrictions in the
home and bans in public places allow a limited
opportunity for smokers to smoke. The mere
existence of a school ban had no effect, but
enforced school bans were associated with up
to 11% reduction in the uptake of smoking.132
Schools with smoking policies have lower rates
of smoking among students.133 Teachers who
smoke make smoking seem safe and acceptable.
The school policy must address both teachers’
and students’ smoking. Colleges with a no
smoking policy for both staff and students have
been shown to have the lowest prevalence and
their students smoke fewer cigarettes.134,135 An
Indian study also revealed that in schools which
have enforced a no-smoking policy, teachers
smoked less compared to schools having no such
anti-smoking policy.136
Establishing anti-tobacco norms
Tobacco cessation
Social group interactions, through family, peer
and cultural contexts, can play an important
role in reinforcing, denying, or neutralizing the
potential effects of anti-smoking advertising.127
It has been seen that peer pressure is an
important influence for tobacco use among
adolescents.’30
Many of the measures mentioned above such as
raising the cost of the product, reducing access,
and comprehensive tobacco education are
effective in reducing tobacco use among the
youth. Additionally, tobacco cessation services
in the form of counselling for behavioural
modification should be provided to the youth.
303
'
■
................................................................
Tobacco Control in India
Tobacco cessation is described in detail in Section
6.7.
Recommendations
Based on the evidence from global and Indian
research, the following measures are
recommended to protect the youth from tobacco:
1. A comprehensive tobacco control programme
(including awareness and well-informed
youth activism) is needed to reduce and
restrict the youth from tobacco use.
2. A comprehensive ban on tobacco advertising
(direct and indirect) is essential to prevent
the youth from associating smoking with their
role models.
3. Raising the prices of tobacco products,
through taxes, and increasing the sizes of the
packages are the most effective ways of
preventing the youth from initiating use, as
they are highly price sensitive.
4. School-based programmes should adopt a
comprehensive intervention approach and
ensure that the modes of communication are
suitable to the targeted group’s characteristics.
5. The youth, especially school students, should
be encouraged to get involved in anti-tobacco
advocacy and discuss policy issues related to
tobacco control. Schoolteachers and parents
should also be involved in these initiatives.
7.7 COMMUNITY INTERVENTIONS: PROTECTING THE YOUTH FROM TOBACCO
KEY MESSAGES
• Based on current trends, some 30%-40% of the 2.3 billion children and teenagers in the
world would become smokers in early adult life.
• The most susceptible time for initiation of tobacco use in India is during adolescence and
early adulthood, i.e. in the age group of 15-24 years.
• Raising the prices of tobacco products through taxes, increasing the size of the packages and a
comprehensive ban on tobacco advertising (direct and indirect) are effective means of
preventing the youth from initiating use.
• Youth involved in anti-tobacco advocacy are more likely to avoid tobacco use.
Tobacco Control: What Works?
I
7.8
Community Interventions:
Smoke-free Public Places
There is now incontrovertible evidence that
exposure to other people’s smoke is dangerous
to health.137 The health consequences of second
hand smoke have already been discussed in
Chapter 4. Exposure to second-hand smoke is
an entirely preventable cause of the substantial
morbidity and mortality associated with tobacco
use.138 A growing number of countries and states
are now implementing restrictions on smoking
in public places. The most obvious benefit of
these restrictions is clearly to non-smokers, who
are spared exposure to the health risks and
nuisance of second-hand smoke. For such
restrictions to work, there must be a general
level of social support for them, and an
awareness of the health consequences of
exposure to second-hand smoke.139
Smoking bans and restrictions are policies and
regulations that ban or limit the consumption of
tobacco products in specific places. These include
private business and employer policies,
organizational regulations, and government laws
and ordinances. Laws and ordinances can
establish minimum standards to protect workers
in private sector workplaces, as well as ban or
restrict smoking in public areas and
workplaces.140
Smoke-free workplaces not only protect nonsmokers from the dangers of passive smoking
but also encourage smokers to quit or reduce
consumption. In one study, the combined effect
of people stopping smoking and reducing
consumption reduced the total cigarette
consumption by 29%.141
The WHO’s Framework Convention on Tobacco
Control (FCTC) has identified the need for
aw
protection from exposure to tobacco smoke. It
states that countries should recognize that
scientific evidence has unequivocally established
that exposure to tobacco smoke causes death,
disease and disability (Article 8).142
Recently, the Government of India has ordered
a ban on smoking in public places. Despite
similar bans imposed earlier by several Indian
State Governments, smoking is still prevalent in
many public places.143 Effective policies for
smoke-free public places are required to guide
implementation at various levels and ensure
strict enforcement of the existing laws.144 The
tobacco industry has often challenged the
rationale and efficacy of such bans. In this
context, it would be useful to review the available
evidence.
Global evidence
Several countries have successfully introduced
smoke-free public places. Regulations restricting
smoking in public places appear to have a
considerable impact on teenage smoking
behaviour. It affects the teenager’s decision to
become a smoker rather than on reducing the
number of cigarettes smoked.141 Smoking
restrictions in the home and bans in public places
allow a limited opportunity for smokers to smoke.
Properly enforced school bans have been found
to be associated with up to 11% reduction in the
initiation of smoking.145 Schools and colleges with
no-smoking policies have been shown to have
the lowest prevalence of tobacco consumption
and their students smoke fewer cigarettes than
others.146-148 Banning smoking in workplaces is a
simple and cost-effective way to encourage
smokers to quit. Banning smoking in restaurants
was found to have either a neutral or beneficial
effect on business arid may increase patronage
by tourists who desire smoke-free restaurants.137
Laws for smoke-free places may also be
associated with a rapid effect on morbidity
resulting from heart disease. A law banning
smoking in public- and workplaces in a localized
community resulted in a sharp decrease in
Tobacco Control in India
hospital admissions for acute myocardial
infarction. The significant decrease in
admissions was from an average of 40
admissions during the same months in the years
before the introduction and after withdrawal of
the law, to a total-of 24 admissions during the
six months when the law was in effect.149
The US Task Force on Community Preventive
Services evaluated the effectiveness of selected
interventions. They strongly recommended
smoking bans and restrictions on the basis that
they reduce exposure to second-hand smoke
when applied: (i) in a wide range of workplace
settings and adult populations; (ii) at different
levels of scale, from individual businesses to
entire communities; and (iii) whether used alone
or as part of a multicomponent community or
workplace intervention.139
In addition to the evidence of effectiveness in
reducing workplace exposure to second-hand
smoke, several studies also observed a significant
reduction in the daily consumption of cigarettes
by workers who are subjected to a smoking ban
or restriction at their workplaces.139
✓
Community education provides information to
parents, other occupants and visitors to the home
that reducing or eliminating second-hand smoke
protects non-smoking adults and children.
Attempts must be made to motivate household
members to modify smoking habits and reduce
the exposure of non-smokers to indoor second
hand smoke by establishing home policies, and
restricting or banning smoking if they cannot
quit entirely.139
Enthusiastic endorsement by and active
participation of the community are essential for
smoking bans to succeed. The ‘top-down’
regulatory approach must be complemented by a
‘bottom-up’ community mobilization approach.
The government and community must constantly
act in concert to enable laws for making public
places smoke free to be enacted and sucessfully
implemented (Fig. 7.10).
9::
IB
E
Indian evidence
There are only a few documented examples in
India of success in achieving smoke-free
environments. A study among youth (in the age
group of 13-15 years), in government and private
schools in Uttar Pradesh, reported that many
students (60.7%) were in favour of banning
smoking in public places.150 A study from Bihar
revealed that in schools that have enforced a
no-smoking policy, teachers smoked less
compared to schools having no such policy.151
Another example is ‘a tobacco-free town’ in
Kerala. The people from Koolimadu village in
Kerala started an anti-smoking movement when
a chain smoker, who was a resident of their
village, died of cancer. The villagers had a typical
example in front of them, so they wete convinced
about the ill effects of tobacco. Due to the
enthusiastic response to the anti-tobacco
movement, the district administration imposed
a total ban on the use and sale of tobacco
products and declared the area a tobacco-free
zone. Some of the youth groups have been given
the responsibility of monitoring the ban. Due to
the success of the movement, the penalty of
being excluded from village life for a day has, so
far, not had to be imposed.152
Before the Government of India banned smoking
in public places, a ban on smoking had existed
in certain areas. The Indian Airlines was one of
the first airlines to ban smoking on domestic
flights. The airlines has now extended the ban
even on its international flights.153 Apart from
these, the Indian railways banned smoking in
all its service areas.154 Some institutions such as
the Lucknow University banned smoking on the
campus.149,154 Although several such bans have
been introduced in India, there is a lack of data
on their effectiveness.
For enforcement of the newly enacted legislation
for tobacco control, there is a need to gather
such evidence of the impact on both active and
passive exposure to tobacco smoke. However,
studies from other countries are sufficient to
?WBBf
Tobacco Control: What Works?
Action at the government level
Action at the community level
Enactment of legislation to ban
smoking in public places
Community support for
the legislation
Framing of rules and design of
implementation pathways
Community consensus on practical
methods of implementation in
different settings
Creation of norms for smoke-free
settings
Community participation and
leadership
Enforcement of rules
Act as a watchdog (monitoring)
Fig. 7.10 Complementary roles of the government and community in making public places smoke free
show the effectiveness of such bans as a
mechanism for tobacco control. In selecting and
implementing interventions, there is a need to
develop a comprehensive strategy to reduce
exposure to second-hand smoke, reduce
initiation and increase cessation. Improvements
in each category will contribute to reductions in
tobacco-related morbidity and death, and
success in one area might contribute to
improvements in other areas as well?55
7.8 COMMUNITY INTERVENTIONS: SMOKE-FREE PUBLIC PLACES
KEY MESSAGES
• Exposure to second-hand smoke is an entirely preventable cause of significant morbidity
and mortality associated with tobacco use.
• Smoke-free workplaces not only protect non-smokers from the dangers of passive smoking,
they also encourage smokers to quit, or reduce consumption.
• For smoking bans to succeed, enthusiastic endorsement by and active participation of the
community and an awareness of the health consequences of exposure to second-hand
smoke are needed.
• The combined effect of people stopping smoking and reducing consumption reduces the
total cigarette consumption by 29%.
• Regulations restricting smoking in public places have a considerable impact on teenage
smoking behaviour. It affects the teenager’s decision to become a smoker rather than the
number of cigarettes smoked.
4K
i
St
Tobacco Control in India
7.9
Community
Interventions:
Strengthening Health
Literacy on Tobaccorelated Matters
A tobacco control programme requires a
multipronged strategy. Increasing the knowledge
and awareness about its harmful effects is one of
the ways of reducing tobacco use among people.
Available global evidence on the impact of
community health education interventions with
regard to tobacco use is summarized here.
Global evidence
-
A well-designed public education campaign that
is integrated with community- and school-based
programmes, strong enforcement efforts and
help for smokers who want to quit, can
successfully counter marketing by the tobacco
industry. Such integrated programmes have been
demonstrated to lower smoking among young
people by as much as 40%.156
A 15-year follow-up study, as part of the North
Karelia Youth Project, showed that the reduction
in tobacco use as a result of a mass media
intervention combined with a school- and
community-based education programme, lasts
over time. In this study, students were taught
about social pressures to smoke exerted by peers,
adults and the mass media, and were trained by
demonstration and role play to deal with them.
The short- and long-term effects of smoking were
also discussed. The mean lifetime cigarette
consump-tion was 22% lower among subjects
who had been in the programme than among
control subjects.157
308
A study done in Minnesota found that a fiveyear intervention involving a media campaign,
community programmes and school-based
instruction resulted in significantly lower
smoking rates. At the end of high school, just
14.6% of students in the intervention community
were weekly smokers, compared to 24.1% of those
in the control community.158
A study conducted in 1997 found that, in terms
of cost per years of life gained, education
campaigns through the mass media were among
the most cost-effective methods to prevent or
reduce tobacco use.159
An effective model for community-based
programmes is the American Stop Smoking
Intervention Study (ASSIST). The primary goal
of this federally funded community-based
programme was to reduce the prevalence of
smoking and cigarette consumption among
adults and youth in the 17 states participating in
the study. By working with community groups,
youth groups and adult organizations, the ASSIST
programme has been able to reach diverse
populations and raise public awareness regarding
the need for tobacco control policies. Outreach
programmes in health care settings and training
programmes for physicians, nurses, dentists and
dental hygienists also increase the potential
public exposure to the dangers of tobacco and
benefits of quitting smoking or avoiding starting
altogether. Within three years of full funding of
the project, per capita tobacco consumption in
the ASSIST states was 7% lower than in nonASSIST states. More than three-quarters of the
intervention states showed some decrease in
cigarette consumption despite decreases in the
price of cigarettes.160
The state of Oregon in the USA has achieved
impressive declines in per capita consumption
after implementing a statewide tobacco control
programme. Oregon’s community activities
include, among others, engaging young people
to plan and conduct community tobacco
prevention and education events and campaigns,
working with judges and retailers to develop
Tobacco Control: What Works?
Increasing excise taxes on cigarettes reduces
tobacco consumption rates, but when the excise
taxes support effective community, media and
school programmes to prevent tobacco use,
decreases in the per capita consumption will
continue even if the industry lowers tobacco
prices to pre-excise tax values.163
education and diversion programmes, conduct
ing a campaign on smoking in the home, and
developing educational presentations and
strengthening tobacco-use policies in schools,
community and day-care centres.
A 1995 study of California’s anti-smoking
programme found that anti-smoking media
campaigns are an effective way of reducing
cigarette consumption, and noted that
funding levels produced more powerful results.5
Goldman and Glantz reviewed research on the
effectiveness of various anti-smoking messages.
They concluded that ‘aggressive’ public
education campaigns that focus on ‘industry
manipulation’ (that is, on the goal of the tobacco
industry to recruit young smokers and the tactics
used to achieve this goal) and the negative effects
of second-hand smoke are more likely to reduce
cigarette consumption and denormalize
A three-month multimedia anti-smoking
campaign conducted in Norway (1977) is credited
with reducing tobacco sales by 4% and
encouraging an estimated 100,000 Norwegian
smokers to attempt to stop smoking.
smoking.164
A two-year anti-smoking television and radio
campaign conducted in Greece between 1978 and
1980 is credited with reducing tobacco sales and
increasing the number of smokers attempting to
stop smoking. In the years before the campaign,
the annual tobacco sales had increased at
approximately 6% per year,' UnnS
tobacco sales were flat.
’
Evaluations of two of the longer running antitobacco campaigns in California and
Massachusetts suggest that the counter
advertising components of their programmes had
contributed to an overall reduction in cigarette
use and greater public awareness of the hazards
of tobacco.162
School-based tobacco prevention programmes
that identify the social influences which promote
tobacco use among youth and teach skills to resist
such influences can substantially reduce or delay
adolescent smoking. Although long-term follow
up of such programmes has indicated that the
effect may dissipate over time, other studies have
shown that the effectiveness of school-based
tobacco prevention programmes is strengthened
by booster sessions and communitywide
programmes involving parents and community
organizations and including school policies, the
mass media and restrictions on youth access.1
Successful health interventions in India have
been cited in Chapter 6.
Effective public education strategy
Available research and experience show that a
public education campaign should include the
following characteristics:156,161
. It must incorporate paid media, public
relations, and special events and
promotions in a coordinated effort that is
integrated with school- and community
based programmes, as well as the other
elements of a comprehensive tobacco
reduction plan.
. It must be well funded so that the media
component can achieve the reach necessary
to be effective. This effort must be sustained
S Zi'H
over the long term.
. The mass media should be used for
dissemination of policies related to tobacco
control. These messages help to reinforce
community campaigns.
• There should be no restrictions on the content
of the messages, and the campaign must
operate completely independent of tobacco
industry input.
309- 9
Tobacco Control in India
• It must be grounded in rigorous, state-ofthe-art research on effectiveness.
• Young people must be involved in the
planning and conduct of community tobacco
prevention and education events and
campaigns.
• Educational presentations should be
developed and tobacco-use policies should
be strengthened in schools, the community
and day-care centres.
• Campaigns should be conducted on stopping
smoking in the home.
• Tobacco advertising should be assessed
locally (at state level) and plans should be
developed to reduce tobacco sponsorship of
public events.
• Smoking cessation programmes should be
' offered.
School-based interventions
These should include the following:156,161
• They should focus on information, attitudes,
and skills to resist social and behavioural
influences, as well as on peer norms, refusal
skills, etc. among others.
• They should be socially and culturally
acceptable to all communities. The lack of this
has seen programmes failing to have the
desired effect.165
• Tobacco-related information should be
included in the curriculum.
• There should be booster sessions, where the
knowledge once imparted can be re
emphasized.
• The information should be imparted by the
teacher rather than an outside health
professional.
• Teachers should be adequately and regularly
trained by health professionals.
• Students should be included in the
dissemination of information to the
community.
• Cessation support should be given to students
and teachers.
• Parents, the community and media should be
involved„in these interventions.
• The programme should be regularly assessed.
7.9 COMMUNITY INTERVENTIONS: STRENGTHENING HEALTH LITERACY ON TOBACCO-RELATED MATTERS
KEY MESSAGES
• Increasing the knowledge and awareness about the harmful effects of tobacco use among
the people is one of the ways to reduce tobacco use.
• Health education leads to a long-lasting reduction in tobacco use, when it is imparted
through the mass media and combined with a school- and community-based education
programme.
. Education campaigns through the mass media are among the most cost-effective methods
currently available to prevent or reduce tobacco use.
• School-based tobacco prevention programmes that identify the social influences which
promote tobacco use among the youth and teach skills to resist such influences can
significantly reduce or delay adolescent smoking, especially if strengthened by booster
sessions and communitywide programmes involving parents and community organizations.
• Public education programmes should be well funded and based on rigorous research.
• The distinct cultural profiles of the targeted population groups should be kept in mind while
designing programmes.
l07>
SS
.’j; _•
Tobacco Control: What Works?
7.10
Benefiting from Models
of Behaviour Change
Health, defined in its broadest conceptualiza
tion, is a dynamic state of complete physical,
psychological, social and spiritual well-being
wherein physiological, psychological, regard for
societal roles and norms, and the transcendent
purpose of existence are incorporated.166 The
maintenance of such a state is dependent on
adopting behaviours that would not compromise
health resulting in pain, disease or death; they
should also foster social, psychological and
spiritual well-being. Thus, the outcomes of highrisk behaviours such as experimenting with
smoking, alcohol, drugs or unsafe sex, which
may appear at first instance to be socially deviant
behaviours, later develop into physical problems.
Influencing behaviours to change them in a
manner that reduces risks would thus seem to
be a necessary step to promote health.
The Ottawa Charter for Health Promotion states
that peace, shelter, education, food, income, equity
and justice are fundamental conditions for health
promotion, which would be fostered by healthy
public policies, supportive environments,
community action and personal skills. Health
behaviour change thus needs to be seen in the larger
comprehensive context of health promotion.167
Health behaviour change is a complex process
and is guided by various empirical constructs
and theories. The change needs to be made at
the community, society (interpersonal) and
individual (intrapersonal) levels. Contemporary
health promotion includes not only educational
activities but. also advocacy, organizational
change efforts, policy development, economic
support, environmental change, and multi
method programmes highlighting the importance
of approaching public health problems at
multiple levels, and stressing the interaction and
integration of factors within and across various
levels. This approach has been referred to as an
ecological perspective. Two key ideas—‘multiple
levels of influence’ and ‘reciprocal causation’between individuals and their environments help
direct the identification of personal and
environmental leverage points for health
promotion interventions.168
This section outlines (i) some of the theoretical
constructs guiding health-related behaviours and
the processes of changing behaviours, and
community and environmental factors that
influence behaviour; (ii) the two prominent
approaches to the development of a framework
in which the theories of behaviour change can be
operational; and (iii) some of the relevant
theories and examples of behaviour change
interventions based on this theoretical framework.
Planning systems/frameworks
Once health communication planners identify a
health problem, they need a planning system that
can help identify the social science theories most
appropriate for understanding the problem or
situation. Two influential methods are: social
marketing and Precede-Proceed. The use of
planning systems such as social marketing and
precede-proceed increases the probability of
programme success by examining health and
behaviour at multiple levels.
Social marketing
Social marketing is not a theory. It does not tell
us how to change a person’s behaviour. Rather, it is
an approach to thinking about and structuring a
social change programme to one that is consumerdriven. Within this framework, a number of social
and behavioural theories can be drawn upon to
develop a strategic course of action.
Kotler (1975) defines social marketing as ‘the
design, implementation, and control of
programmes seeking to increase the acceptability
of a social idea or practice in a target group(s).
Tobacco Control in India
It utilizes concepts of market segmentation,
consumer research, idea configuration, com
munication, facilitation, incentives, and exchange
theory to maximize target group response.’169
Andreasen (1995) defines social marketing as
‘the application of commercial marketing
technologies to the analysis, planning, execution,
and evaluation of programmes designed to
influence the voluntary behaviour of target
audiences in order to improve their personal
welfare and that of their society’.170
The common features of social marketing are:
1. The label is applied to causes judged by
persons in positions of power and authority
to be beneficial to both individuals and society.
2. Unlike commercial marketing, the agent of
change does not profit financially from a
campaign’s success.
3. The ultimate goal is to change behaviours
believed to place the individual at risk and
not simply increase awareness or alter
attitudes.
4. The optimal social marketing campaign is
tailored to the unique perspective, needs and
experiences of the target audience, hopefully
with inputs from representative members of
this group.
5. Social marketing strives to create conditions
in the social structure, which facilitate the
behavioural changes promoted.
6. Social marketing relies on the concepts of
commercial marketing.
It has been said that ‘there is poetic justice in
using the very marketing concepts employed by
such “disease peddlers” as the tobacco and fast
food industries to combat their negative
influences’.171
Social marketing practices are based on
commercial marketing practices that make the
consumer^ the central focus for planning and
conducting a programme. One of the pathways
to information campaigns based on social
marketing is the 5P approach, which addresses
the following components.171
Price: What the consumer must give up to
receive the programme’s benefits (these costs
may be intangible, e.g. changes in beliefs or
habits, or tangibles such as money, time or
travel);
Product: What the programme is trying to
change within the intended audience and what
the audience stands to gain;
Promotion: How the exchange is communicated
(e.g. appeals used);
Place: What channels the programme uses to
reach the intended audience (e.g. mass media,
community or interpersonal); and
Positioning:!^ is a psychological construct that
involves the location of the product relative to
other products and activities with which it
competes. For instance, physical activity could
be repositioned as a form of relaxation, not
exercise.
Lessons learned from social marketing stress the
importance of understanding the target audience
and designing strategies based on their wants
and needs rather than what good health practices
direct them to do.
The Precede-Proceed framework
The Precede model is a framework for the
process of systematic development and
evaluation of health education programmes.172
An underlying premise of this model is that
health education is dependent on voluntary
cooperation and participation of the client in a
process that allows personal determination of
behavioural practices; and that the degree of
change in knowledge and health practice is
directly related to the degree of active
participation of the client. Therefore, in this
model, appropriate health education is
considered to be the intervention (treatment)
for a properly diagnosed problem in a target
population.
This model is multidimensional, founded in the
11)^
Tobacco Control: What Works?
r
social/behavioural sciences, epidemiology,
administration and education. As such, it
recognizes that health and health behaviours
have multiple causations, which must be
evaluated to assure appropriate intervention.
The. comprehensive nature of ‘Precede’ allows
for application in a variety of settings, such as
school health education, patient education,
community health education and direct patient
care settings?72
‘Proceed’ was added to the framework in
recognition of the emergence of and the need
for health promotion interventions that go
beyond traditional educational approaches to
change unhealthy behaviours?73 The administra
tive diagnosis is the final planning step to
‘precede’ implementation. From there, ‘proceed’
to promote the plan or policy, regulate the
environment, and organize the resources and
services, as required by the plan or policy. Figure
7.11 illustrates the Precede-Proceed model.
The Precede-Proceed model directs initial
attention to outcomes rather than inputs. Hence,
PHASE 5
Administration
and policy
diagnosis
PHASE 4
Educational and
organizational
diagnosis
planners focus5 on planning from the outcome
point of view. The model rests on two principles:
1.
The ‘principle of participation’, which states
that success in achieving change is enhanced
by the active participation of members of the
target audience in defining their high-priority
problems and goals, and in developing and
implementing solutions. This principle is
derived from the community development root
theories and the empowerment education
model.
2. The important role of‘environmental factors’,
such as the media, industry, politics and
social inequities, as determinants of health
and health behaviours.
The Precede step of the model ends with the
administrative and policy diagnosis and the
Proceed step then begins with implementation
and evaluation. This model has been applied,
tested, studied, extended and verified in
hundreds of published studies and thousands
of unpublished projects in community, school,
I
I
PHASE 1
Social
diagnosis
PHASE 2
Epidemiological
diagnosis
PHASE 3
Behavioural and
environmental
diagnosis
r
1
1
1
Health
Promotion
Behaviour and
lifestyle
n
? Policy regulation
i organization J
Environment
-------- 1----- --- PHASE 6
Implementation
PHASE 7
Process evaluation
PHASE 8
Impact evaluation
Fig. 7.11 The Precede-Proceed model
1
Hil
PHASE 9
Outcome evaluation
♦ Tobacco Control in India
clinical and workplace settings over the past
decade.173,174 To provide technical guidance and
assistance to those involved in the complex
process of planning and implementing
community-level cancer prevention and control
interventions, the EMPOWER (Enabling
Methods of Planning and Organizing Within
Everyone’s Reach) software was created.173,174
Models/theories of change
There are a number of influential models that
have been proposed and evaluated. Some of these
are as follows:176
I.
The individual (intrapersonal) models are:
1. Health belief, model
2. Transtheoretical model
3. Consumer information-processing model
II. The interpersonal models include:
1. Social learning or cognitive theory
III. Community/organizational network models
include:
Fear (threat) of the consequences of inaction
(e.g. tobacco cessation) are weighed against the
benefits of the action (remaining free of cancer
or other tobacco-related diseases).
Four basic constructs representing the perceived
threat and net benefits in the HBM are:
. — Perceived susceptibility, i.e. one’s opinion of
the chances of acquiring a condition;
— Perceived severity, i.e. how serious a
condition and its sequelae are;
— Perceived benefits, i.e. efficacy of the advised
action to reduce the risk or seriousness of
impact; and
— Perceived barriers, i.e. tangible and
psychological costs of the advised action.
Organizational change theory
2. Community organization theory
3- Diffusion of innovations theory
These are related to ‘readiness to act’ which,
coupled with ‘cues to act’ (including strategies to
activate readiness), will lead to a change in the
behaviour (Fig. 7.12).
I. Individual (intrapersonal) models
Rosenstock178 added self-efficacy, or one’s
confidence in the ability to successfully perform
an action to better fit the challenges of changing
habitual unhealthy behaviours, such as being
sedentary, smoking or overeating.
1.
Health belief model
Developed around the 1950s by Hochbaum,
Kegels and Rosenstock, the Health belief model
(HBM) of influencing behaviours is useful in
analysing asymptomatic yet considerably
diseased persons (e.g. those with hypertension,
diabetes, etc.). It is characterized by inaction
regarding illness or non-compliance to1
intervention and remains one of the most widely
recognized conceptual frameworks of health
behaviour.177
The focus of this model was on increasing the
use of preventive services, such as conducting a
■
chest X-ray examination to screen for tuber
culosis, and immunization such as influenza
vaccines. It was assumed that people feared
diseases and that health actions were motivated
in relation to the degree of fear, i.e. perceived
threat and the expected fear-reduction potential
of actions, as long as the potential outweighed
practical and psychological obstacles to taking
action, i.e. net benefits.
The application of HBM has been primarily in
Perceived severity
Perceived benefits
Perceived barriers
Fig. 7.12 Health belief model
Wil
-JChange
Tobacco Control: What Works?
explaining health-related behaviours but it could
also be a useful framework for designing change
strategies. The most promising application of the
HBM is in helping to develop messages that can
be delivered in the print or electronic media to
persuade individuals to make healthy decisions.
In applying the HBM to a smoker, it would
seem that the messages best suited for health
education would include (i) I can have lung
cancer (susceptible) based on the epidemiology
of the disease, (ii) lung cancer can kill me (the
'severity is great), (iii) quitting can reduce the
chances (how much; benefits), (iv) quitting will
be associated with loss of contacts and perceived
‘pleasure’ of smoking (costs/barriers), and (v) a
strategy to improve self-efficacy in the case of
repeated relapses should be put in place.
The model is particularly useful when the
condition evokes health motivation as well as
social or economic motivation.
Transtheoretical stage of change model
The Transtheoretical stage of change model
developed by Prochaska and DiClemente179,180
evolved from work with smoking cessation and
the treatment of drug and alcohol addiction,
and has recently been applied to a variety of
other health behaviours including substance use
or lifestyle behaviour. The basic premise is that
behaviour change is a ‘process’ and not an event,
and that individuals are at varying levels of
motivation, or ‘readiness’ to change. People at
different points in the process of change can
benefit from different interventions, matched
to their stage at that time.
The four stages in this circular model—pre
contemplation, contemplation, action and
maintenance—are depicted in Fig. 7.13. The
subjects may enter and exit at any stage and go
through the cycle in both directions. They often
go from maintenance back to contemplation
through relapse and onward to action.
Sometimes subjects can go back to
contemplation from action. It seems, however,
that the stages may have a different meaning
for different behaviours.
I
Action
Maintanance
Fig. 7.13 Transtheoretical stage of change model
Readiness to change can be measured by
questionnaires such as the ‘Readiness to Change
Questionnaire’ developed specifically for drugs
of abuse by Rollnick et al.'8i Specifically tailored
programmes can be initiated by knowing the
stage of change the individual is at.
The transtheoretical model is a veiy useful and
influential model of behaviour change. It is used
extensively in drug abuse treatment to ascertain
the stage pf change and use appropriate methods
to change the stage. In relation to tobacco use,
this model helps in understanding change in
the individual as well as the community, and
initiating stage-specific interventions.
Consumer information processing model
This model is based on the fact that information
is important for people to solve problems.
Information is needed for deciding virtually
everything, e.g guidance in choosing treatment
modalities or specific information to choose
foods for therapeutic diets, etc. The human
system, however, is limited by the ability to
process information. Furthermore, information
is necessary but not sufficient for encouraging
healthful behaviours. In the present era of
information explosion, information can increase
or decrease a person’s anxiety, depending on
their information preferences, and how much
and what kind of information they are given.
Misconceptions can lead even motivated
consumers to behave in risky ways.
Tobacco Control in India
■~~1
The Information processing model is governed
by the need for information and motivation to
acquire the information.
Bettman’s model (Fig. 7.14) depicts a cyclical
process of information search, choice, use,
learning and feedback for future decisions.182 To
be used in making decisions for change, the
information must be available, appealing and
novel.
Si
o
Iv
v-'X
Decision process
Fig. 7.14 Consumer information processing model of choice
II. Interpersonal theories of influencing
behaviours
Social learning theory or social cognitive theory
In the 1970s, Bandura published a comprehen
sive framework for understanding human
behaviour, based on a cognitive formulation,
which he named the Social cognitive theory
(SCT).183 This was the first theory to incorporate
the notion of modelling or vicarious learning as
a form of social learning. Whereas strict behavi
ourism supports a direct and unidirectional
pathway between the stimulus and response,
representing human behaviour as a simple
reaction to external stimuli, SCT asserts that
there is a mediator (human cognition) between
the stimulus and response, placing individual
control over behavioural responses to stimuli. A
basic premise of the Social learning theory (SLT)
or SCT is that people learn not only through
their own experiences, but also by observing the
actions of others (vicarious learning) and the
results of those actions. Bandura’s work has
stimulated an enormous amount of research on
learning and behaviour, and has been useful in
developing techniques for promoting behaviour
change.
This theory has been used to study a wide range
of health problems, from compliance to medical
therapy, to alcohol abuse, to immunizations. One
particularly fruitful area of investigation in which
it has been employed is in understanding how
children are socialized to accept the standards
and values of their society. The theory is not
without its limitations, prominent among which
is the theory’s comprehensiveness and complexity,
which make it difficult to operationalize. Further,
many applications of the theory focus on one or
two constructs, such as self-efficacy, while
ignoring the others.
This theory defines human behaviour as a
triadic, dynamic and reciprocal interaction of
personal factors, behaviour, and the
environment, with the individual’s behaviour
being uniquely determined by each of these three
factors. The key constructs include:
(i) Reciprocal determinism, meaning that
behaviour and the environment are
reciprocal systems and that the influence is
in both directions. The environment shapes,
maintains, and constrains behaviour with
people in active interaction in the process,
as they can create and change their
environments.
(ii) Behavioural (symbolizing) capability, which
maintains that symbols serve as the
mechanism for thought and that, through
the formation of symbols such as images
(mental pictures) or words, humans are able
to give meaning, form and contiguity to their
experiences.
5353
Tobacco Control: What Works?
(iii) Expectations, which are the results that a
person thinks will occur as a result of action.
(iv) Self-reflection or self-efficacy, which is the
single most important aspect and a major
determinant of self-regulation.
Observational (vicarious) learning allows one
to develop an idea of how a new behaviour is
formed without actually performing the
behaviour oneself. It is often referred to as
‘modelling’, or learning about what to expect
through the experiences of others. This means
that people can gain a concrete understanding
of the consequences of their actions by observing
others and noting whether the modelled
behaviours are desirable or not, and not
indulging in the behaviour themselves.
Observational learning is governed by four
processes—attention span, retention processes,
motor reproduction processes, and motivational
processes.
Reinforcement is a term from classical
behaviourism and is a response to a person’s
behaviour that affects whether or not the
behaviour will be repeated. Positive reinforce
ments, often called ‘rewards’, increase the
chances that the positive behaviour will be
repeated. They are often useful as motivators for
continued participation but not for sustaining
long-term change.
III. Community/Organizational network
theories
Organizational change theory
Organizations are complex and layered social
systems, composed of resources, members, roles,
exchanges and unique cultures. Thus,
organizational change can best be promoted by
working at multiple levels within the
organization. Understanding organizational
change is important in promoting health to help
establish policies and environments that support
healthy practices and create the capacity to solve
new problems. While there are many theories of
organizational behaviour, two are especially
promising in public health interventions: stage
theory and organizational development (OD)
theory.
Stage theory
The stage theory is based on the idea that
organizations pass through a series of steps or
stages as they change. By recognizing those
stages, strategies to promote change can be
matched to various points in the process of
change. An abbreviated version of the stage
theory involves four stages:
— Problem definition (awareness)
— Initiation of action (adoption)
— Implementation of change
— Institutionalization of change.
Organizational theory
The OD theory grew out of the recognition that
organizational structures and processes influence
worker behaviour and motivation. The OD theory
concerns the identification of problems that
impede an organization’s functioning, rather than
the introduction of a specific type of change.
Human relations and quality of work-life factors
are often the targets of OD problem diagnosis,
action planning, interventions and evaluation. A
typical OD strategy involves process consultation,
in which a specialist from outside the organization
helps to identify problems and facilitates the
planning of change strategies.
When combined, the stage and OD theories have
the greatest potential to produce health
enhancing change in organizations. Such
strategies can be used at various stages as they
are warranted. Simultaneously, the stages signal
the need to involve organization members and
decision-makers at various points in the process.
For example, these could become the guide to
the development of a smoke-free work site
programme.
Community organization theory
This theory emphasizes empowerment and active
participation of communities that can better
evaluate and solve health and social problems.
317
(<H
sag
Tobacco Control in India
This theory emanates from the theory of social
networks and support. Community organization
is the process by which community groups are
helped to identify common problems or goals,
mobilize resources, and develop and implement
strategies for reaching their goals. It has roots in
several theoretical perspectives: the ecological
perspective, social systems perspective, social
networks and social support. It is also consistent
with the SET and can be successfully used along
with SLT-based strategies. Although community
organization does not use a single unified-model,
several key concepts are central to the various
approaches. The process of empowerment is
intended to stimulate problem-solving and
activate community members.
relative advantage (is it better than what was
there before?), compatibility (fit with the
intended audience), complexity (ease of use),
trialability (can it be tried out first?),
observability (visibility of results).
Community competence is an approximate
’ community-level equivalent of Self-efficacy plus
behavioural capability, which include the
confidence and skills to solve problems effectively.
Some illustrative studies of health behaviour
change in smoking and alcohol cessation
described below are taken from the reported
literature and are from settings in the western
world. Available Indian studies are summarized
at the end of this section. These studies illustrate
the use of theoretical models in changing health
behaviours in general, including tobacco use.
Social action approaches to community organizing
go beyond the traditional notion of geographic
and political boundaries. Communities of people
who share common health problems have
coalesced to attract attention and obtain power
to address their needs including health services,
anti-discrimination policies and more research
funding.
Communication channels are a two-way process
of flow of information and they mediate the
impact of the media. The utility of innovation
depends on the innovation (a new idea, product,
practice or technology) as well as communica
tion channels and social systems (networks with
members, norms and social structures).
Illustrative studies
1. Lando et al.184 reported the results of a general
media campaign to compare the number of
people who sent in interest cards and pledged
to stop smoking versus those who sent in cards
but did not pledge to stop smoking in a non
Media advocacy is the strategic use of mass media ,
randomized trial with contemporaneous
as a resource for advancing a social or public
controls, and also compared outcomes from a
policy initiative. The media is an important, and
previous study (historical controls). The
often essential, part of social action and advocacy
campaign was tied to a contest and used
campaigns because it focuses on public concerns
telephone surveys for evaluation. They
and spurs public action. The core components of
compared differences in quit rates between
media advocacy are developing an understanding
pledgers and non-pledgers and the results
of how an issue relates to prevailing public
found that an extended enrolment period and
opinions and values, and designing messages that
intensive campaign increased enrolment and
frame the issues so as to maximize their impact,
overall quit rates. Pledgers had higher self
and attract powerful and broad public support.
reported abstinence rates. The study is,
however, limited by the absence of a control
Diffusion of innovations theory
group (a comparison community without the
intervention), even though the historical
This theory addresses how new ideas, products,
controls may be a good indicator of change.
and social practices spread within a society or
2. Popham185 studied a group of people who quit
from one society to another. Some of the most
smoking from among the entire population of
important characteristics of innovations are their
------- Tobacco Control: What Works?
r
■A
■W
those exposed to California s anti-tobacco
media campaign, to measure the exposure of
those who quit in response to the campaign.
This cross-sectional study determined that
the media campaign had influenced change.
3. Prochaska179’186 used a test of 40 questions to
track subjects for 2 years to determine the
progression through stages of change related
to quitting smoking and outlined processes
by which addictive behaviours are modified
and the stages of change.
4. The World Health Organization sponsored a
study of alcohol education in four countries. .
This pilot study of alcohol education in Sth
grade students in 25 schools in Australia (6),
Chile (3), Norway (14) and Swaziland (2) from
1985 to 1987 used random allocation in each
country to control/teacher-led/peer-led
programmes using social-led influences as the
basis of intervention. Results indicated that
students in the peer-led alcohol education
programme reduced their drinking in all the
four countries. Despite an increase in
knowledge, teacher-led groups had same
drinking status as that of controls.187
5. A Healthy Living Campaign was launched in
Hong Kong in May 1998, as a demonstration
of the stages of change model. The stages of
change model were applied, to measure
changes.188
6. The Indian experience with behavioural
intervention in tobacco use has been
summarized in an annotated bibliography of
tobacco-related research in India.189 Some
reports assessed behavioural variables such
as initiation following exposure to surrogate
advertisement, cessation and prevalence, and
some studies included the incidence of oral
lesions after behaviour change interventions.
Most of the studies used health education as
the intervention. Some used mouth self
examination aS a tool for education and
demonstrated its efficacy.
7.10 BENEFITING FROM MODELS OF BEHAVIOUR CHANGE
KEY MESSAGES
. Influencing behaviours to change them in a manner that reduces risks is a necessary step to
promote health.
• A number of influential models of behaviour change have been proposed and evaluated. These
models provide a framework to show how behaviours can be changed to achieve better health
and social practices.
• The use of communication planning systems, such as social marketing and Precede-Proceed
models, increases the probability of programme success by examining health-related behaviour
_ at multiple levels.
.......... • The Precede-Proceed model directs initial attention to outcomes rather than inputs and hence
planners focus the planning process from the outcome point of view.
• The transtheoretical model of change provides the basis for. stimulating and supporting indi-
vidual efforts at tobacco cessation.
• Lessons learned from social marketing stress the importance of understanding the target audi
ence and designing strategies based on their wants and needs rather than what good health
practice directs them to do.
-
Tobacco Control in India
1
7-11
Individual Interventions:
Promoting Tobacco
Cessation
Why cessation?
Tobacco cessation is essential to reduce the
mortality and morbidity related to tobacco use. It
has been projected that by 2050, if the focus is
only on prevention of initiation and not cessation,
the result will be an additional 160 million deaths
among smokers. The majority of tobacco-related
deaths that can be prevented over the next 40
years will be among current smokers who can be
persuaded to quit, according to projections by the
WHO (Fig. 7.15).190
Tobacco cessation as a strategy is available in
western societies and in Thailand among the
South-East Asian countries. The smoking
cessation guidelines developed in the UK have
300—i
250—
140
200—
’S'
J ISO-
I
to
lOO—
_0J
i
50—
E
d
0-
I
120
Preventable if
adults quit
(halving global
cigarette
consumption by
2020)
Preventable if
young adults do
not start (halving
global uptake of
smoking by 2020)
140 g Other premature
deaths from
tobacco-related
causes
2025-2049
2000-2024
Years
Fig. 7.15 Premature deaths from tobacco use, projections
for 2000-2024 and 2025-2049
evaluated such programmes and have found that
smoking cessation interventions are effective.191,192
They are guaranteed to bring health gains for the
population for a relatively modest expenditure,
and in the long term they reduce smoking-related
health care costs, thereby releasing resources for
other needs.
Tobacco cessation interventions are clinically
effective and cost-effective, relative to other
commonly used disease prevention interventions
and medical treatments. Cost-effectiveness analyses
have shown that smoking cessation treatment
compares favourably with routine medical
interventions such as the treatment of hypertension
or hypercholesterolaemia or preventive inter
ventions such as Papanicolaou smears?93
A recent international review found the median
societal cost of over 310 medical interventions
to be £17,000 per life-year gained discounted at
5% (standard economic practice which weights
immediately saved life-years as more ‘valuable’,
and life-years saved in the future as less
valuable)?94 Discounted results for smoking
cessation interventions in the UK range from
£212 to £873?95 Based on these figures, even
with conservative assumptions, smoking
cessation interventions are considerably more
cost-effective than many medical interventions.
A representative national sample of 893 smokers
in the UK shows that most are disenchanted with
smoking and claim that they would not smoke if
they had their time again?96 The widespread
disaffection with smoking among smokers,
combined with their tendency to be deluded
about how easy and quick it will be to stop,
justifies extra urgency in promoting chances to
stop?97 .
Tobacco cessation will provide the most
immediate benefits of tobacco control and
maximize the advantage for a habituee who quits
the habit. It is also established that a majority of
smokers (as many as 70%) desire to quit, but
only 30% actually try each year, and only 3%5% actually succeed in quitting?98
Source: World Health Report, 1999
"
320
1)0
- Tobacco Control: What Works?
Box 7.11 Effects of quitting tobacco smoking
The first treatment approaches to smoking
cessation that emerged in the 1950s and 1960s
were based principally on behaviour modifica
tion. The 1970s saw a greater emphasis on
cognitive treatments, which achieved greater
momentum in the 1980s. The 1990s witnessed
the introduction of several pharmacological
strategies for nicotine cessation and the
emergence of guidelines for tobacco cessation
from various organizations.
Within. 8 hours: Caxbou^onoxi^lpvel drops in, the bpdy.,.
Within 48 hours: Chancns of hayrng a heart attack start to
decrease, sense of srudl and taste
to iruprove.
j
easier-and mcieasing lung capacity. . ...
Within 2 weeks to 3 months: Circulation improves and lung
functwns xne.ease oy up
g, sipurf congestion, tire’dtfess and
<>
...... boart a,la,:k is cut in
Within 3 to 4 y^ Risk of hC;« at^ck is CW6 toifhat of
0,?,,
.
There is a general consensus that behavioural
methods and pharmacotherapy can contribute
substantially to improved health by enabling
cessation of tobacco use.1" Standard treatment
outcomes include measures such as 7-day point .
been estimated that less intensive interventions
prevalence smoking abstinence at the end of the
such as simple advice by a concerned physician
treatment trial with confirmation of surrogate
can produce quit rates of 5%-io% per year in
measures of smoking such as concentrations of
some individuals. A recent meta-analysis of 7
carbon monoxide in the breath and cotinine in
studies by the Clinical Practice Guideline Panel
the plasma, continuous abstinence from the
reported an abstinence rate of 8% when no
target quit date (TQD) and prolonged abstinence
cessation advice was given, compared with 10%
after a grace period. Long-term abstinence is
with
cessation advice.202 In some more severely
typically evaluated either at 6 or 12 months.
dependent
individuals,
pharmacological
interventions
may
have
to
be
used.
When used
Tobacco (nicotine) dependence treatment
alone,
they
can
produce
quit
rates
of
about 25%
involves a mix of pharmacological and nonbut when combined with behavioural
pharmacological interventions.
Smoking
’
interventions the quit rates can go up to 35%.
cessation clinical practice guidelines was
originally published by the Agency for
Healthcare Research and Quality (AHRQ) in
1999 and was updated in 2000 by AHRQ and a
consortium of 7 government and non-profit
organizations. The 2000 Guidelines urged
clinicians to treat tobacco use disorder as a
chronic disease similar in many respects to other
diseases such as hypertension, diabetes and
hyperlipidaemia, and to provide patients with
appropriate advice and pharmacotherapy.200
A tobacco cessation intervention at an individual
level is' usually undertaken after a thorough
assessment of the intensity of use. The
Fagerstrom Test of Nicotine Dependence is a
commonly used instrument for this purpose.201
Depending on these variables, intervention
programmes can be individually tailored. It has
5‘A’s approach to tobacco cessation
(modified from the United States National
Cancer Institute’s 4‘A’s strategy)203
• Ask every patient about tobacco use status.
It is recommended that this become a part of
the elicitation of vital signs.
• Assess the person’s motivation or willingness
to change. Prochaska and DiClemente offer
a theoretical model of readiness to change.204
Tobacco userss in the pre-contemplation
phase do not consider tobacco use a problem
and are unwilling to address it. Those in the
contemplation phase may be weighing the
pros and cons but have not made any firm
commitment to change. In the determination
321
IK
Tobacco Control in India
(preparation) phase, the person is firmly
committed to stop tobacco use. In the action
phase, the person actually demonstrates
commitment to change and if this is
maintained steadily for a period of time, he
or she is in the maintenance phase. The
model is circular and the person may move
from one phase to another. At any phase,
the person may relapse and re-enter the
cycle.
Assessment also needs to evaluate patient
preferences for behavioural and pharmaco
logical interventions. Measurement of nicotine
and carbon monoxide levels can reflect
smoking over the past few hours.
Measurement of cotinine, a metabolite of
nicotine, can reflect smoking in the past 7
days.205
• Advice to every user must be clear, strong and
personalized. Tobacco users may be helped in
making the transition from a non-committed
phase to a phase of commitment by increasing
their motivation to change. Strategies for
motivation to change include listing the pros
and cons of tobacco use, assessing the person’s
self-efficacy in being able to stop, information
on tobacco-cessation strategies and identifica
tion of a relevant goal. As alcohol is a risk
factor for tobacco relapse, advice to reduce
the alcohol intake or abstain from alcohol is
recommended.206
• Assist a person committed to change by
reinforcing the person’s decision, helping the
person make a plan, including a strategy to
manage withdrawal and triggers for relapse,
Box 7.12 Common questions about tobacco cessation
T clinic
Ml
be‘epcdUrdg6^to MdptJ fiSd^^dy-ekbri^^has.
KiHgeu buuwii to improve tobacco quit rates.210
exploring the possibility of adding
pharmacotherapy to behavioural strategies,
helping the person set a quit date, making
necessary arrangements for the quit date
(informing the family about the decision to
quit; getting rid of all forms of tobacco and
paraphernalia such as lighters or matchboxes,
anticipating and preparing to handle
withdrawal and craving) and identifying
social supports within and outside the family
to assist the person in his or her tobacco
cessation attempts. Both intra-treatment
support (support provided by the physician
or caregiver) and extra-treatment support
(provided by family, friends, employer, etc.)
appear to be critical to the success of a
cessation attempt.
Support within the treatment includes
encouragement to quit tobacco use,
communicating care and concern, encouraging
the patient to talk about the quitting process,
which includes reasons for quitting, concerns
and worries about quitting, and successes as
well as difficulties encountered while quitting.
Assisting can be done as part of a brief or
intensive intervention programme.
• Arrange a specific follow up in the couple of
weeks following the decision to quit to
reinforce the person’s goal, reinforce support,
and intervene in case the person slips and is
unable to achieve the desired goal. Most,
studies suggest that frequent, brief follow up,
including telephone calls to provide support
to the user, increase quit rates.211’212
Interventions to promote tobacco
cessation
Studies on the efficacy of interventions to
promote and maintain tobacco cessation have
mostly been conducted on smoking forms of
tobacco, especially cigarettes. This is because
much of this research has been conducted in
developed countries. The results of several studies
on different types of interventions are
summarized in Table 7.11.
Tobacco Control: What Works?
Psychosocial interventions
The initial goal of psychosocial intervention is to
increase motivation, initiate a quit attempt and
help the patient quit for a short period. The
main goal of psychosocial intervention in tobacco
cessation is sustained abstinence, change of
lifestyle and improved quality of life.
There is a strong dose-response relationship
between the intensity of counselling for tobacco
dependence and its effectiveness. Treatments
involving person-to-person interactions (via
individual, group or proactive telephone
counselling) are consistently effective, and their
effectiveness increases with the.intensity of
I’pTik
Table 7.11 Incremental effects ol
on abstinence for six months or longer213
Effect size3 (%)
95% confidence interval
2
l%-3%
-Moderate to heavy smokers seeking
help with stopping
7
3%-10%
Pregnant smokers
7
5%-9%
Face-to-face intensive behavioural
support from a specialist
Smokers admitted to hospital
4
0%-8%
Proactive telephone counselling6
Smokers wanting help with stopping
but hot r.eceiving-Tace-tb’face support
•-..2
l%-4%
Written self-help materials
Smokers seeking help and not
receiving other support
Nicotinegum
Moderate to heavy smokers receiving
limited behavioural support
5
4%-6%
Moderate to heavy smokers receiving
intensive behavioural support .
Moderate to.heavy smokersTeceiving :
limited behavioural support
.
- .
8
6%-10%
Nicotine transdermal patch
Moderate to heavy smokers receiving
intensive behavioural support
6
5%-8%
Nicotine nasal spray
Moderate to heavy smokers receiving
intensive behavioural support
12
7%-17%
Moderate to heavy smokers receiving
intensive behavioural support
8
4%-12%
Moderate to heavy smokers receiving
intensive behavioural support
8
io/o-14%
Moderate to heavy smokers receiving
intensive behavioural support
9
5%-14%
Moderate to heavy smokers seeking
help from a smokers' clinic
13-19
InferVehtibn
Target population_ ____________
Brief opportunistic advice from a
- physician to stop
Smokers attending GP surgeries or
outpatient clinics
Face-to-fade intensive behavioural
| support from a specialist?
Face-to-face intensive behavioural
{ support from a specialist
Nicotinegum
L'-
■
'
;
■
.
■'
Nicotine tran^dermal-patch
Nicotine inhaler
•
-
Nicotine sublingual tablet
■■/.
■
•
■■
•
*
■
;”
*
Intensive behavioural support
plus NRT or bupropion^
.
/.;T.- ■-
0%-2%
4%-7%
<
' - ; ' - ’
rate between intervention and control/placebo in the studies reported; date from Cochrane meta-analyses
8 Difference in >6-month abstinence
unless otherwise stated
b The range within which one can be 95% confident that the true underlying value lies
more than two subsequent visits.
g Expected effect combining effect of medication with effect of behavioural support
Complete information available from URL: www.thoraxjnl.com
-v
323
Tobacco Control in India
1
treatment (e.g. minutes of interaction). Three
types of counselling and behavioural therapies
have been found to be especially effective, and
are recommended for all patients who are
attempting tobacco cessation:
• Providing practical counselling (problemsolving/skills training)
• Providing social support as part of the
treatment (intra-treatment social support)
• Providing help in securing social support
outside of treatment (extra-treatment social
support).198
Evidence related to specific psychological
therapies are summarized in Table 7.12.
Relapse prevention
Attempts to prevent and manage relapse are
based on a common understanding of the concept
and mechanisms of relapse and lapse. Relapse
may be defined as resumption of frequent,
perhaps uncontrolled tobacco use after a period
of non-use and lapse is considered a single
incident of tobacco use. A lapse (slip) may not
result in a relapse, depending on how the patient
responds to the initial incident. There may be
various reasons for relapse such as withdrawal
symptoms, high-risk situations such as stress,
interpersonal conflict, social pressure and
environmental cues.
The first specific measure in handling a'relapse
is to clearly delineate the contexts/causes for
relapse in that particular case, keeping in view
the common situations and reasons for relapse.
Patients are enabled to anticipate a large number
of situations or processes that are likely to lead
to urges to smoke/chew tobacco or to prompt a
slip. The second step is to reformulate the
treatment plan by which the patients are helped
in planning and developing strategies to cope
with these situations. The patient may be taught
coping skills for ‘high-risk’ situations,
communication skills training, relaxation
techniques, distraction techniques, assertive
training, depending on the pertinent factors
responsible for relapse.
Self-help approaches
The two basic modalities of psychosocial
interventions, i.e. brief and extended, have the
commonality of being therapist mediated. A
third and novel approach in psychosocial
intervention is self-help approaches. These
; Suggest'increased ces^afion
«if.,^hsricontroi/The
0
confidencejnt
85s "S
'e, but hot used by most therapists
J
^rif.prnc216
oliance rconcerns™
■/a/'
vidence192,217
Lacks sufficient evidence W2-2’7
.324
1/^
Tobacco Control: What Works?
include self-help material and self-help groups.
Self-help material: Written manuals are the
most common forms of self-help material,
although computer and video versions are also
available. The major goals of self-help materials
are to increase motivation and impart cessation.
Self-help materials are effective in patients who
are less nicotine dependent and more motivated.
However, without additional contact or support,
the impact of these materials is debatable and
their use is advised as part of a behavioural
treatments emerged primarily for smoking
cessation, but are now also being used for
smokeless tobacco cessation.
therapy programme.21^2'8
• on the
Self-help groups: These mostly operate
principles laid down by the world’s largest self
help group, i.e. the Alcoholics Anonymous (AA).
Several organizations such as Nicotine
Anonymous have outlined how to apply the 12step model to smoking. The aim is to have the
smoker accept that he or she is powerless to stop
smoking and work through 12 goals (or steps)
that help break denial. Though there are no
scientific tests for the 12-step programme for
smoking cessation, it can be a useful adjunct to
other psychosocial treatments.
Other non-pharmacological therapies
Hypnotherapy has been used for tobacco
cessation but reports on its efficacy are
• conflicting, mainly because of methodological
issues. It is still under evaluation as a promising
therapy.216
High-intensity exercise regimens seem to be
helpful in tobacco cessation by increasing selfesteem, relieving stress, managing weight gain
and improving health. Recent findings on highintensity exercise regimens suggest positive
outcomes, but these still need to be evaluated
for sufficient evidence.210’219’220
Pharmacotherapy
Current recommended pharmacotherapy for
nicotine cessation consists of nicotine
replacement therapy (NRT) and the use of the
atypical antidepressant bupropion. These
Extensive randomized, double-blind, placebocontrolled clinical trials have established the
efficacy and safety of NRTs and bupropion in the
treatment of nicotine dependence, by increasing
the quit rates by approximately 1.5-2-fold,
irrespective of the setting.22' The effectiveness of
NRTs appears to be largely independent of the
intensity of additional support provided to the
smoker. Since all the trials of NRT.reported so.,
far have included at least some form of brief
advice to the smoker, this represents the
minimum which should be offered to ensure its
effectiveness. Provision of more intense levels of
support, although beneficial in facilitating the
likelihood of quitting, is not essential to the
success of NRT. There is promising evidence that
bupropion may be more effective than NRT
(either alone or in combination).
Nicotine replacement therapies
These are the most commonly used agents for
quitting tobacco use. Products include nicotine
gums, nicotine patches, nicotine nasal spray,
nicotine inhalers and nicotine lozenges. Details
of the dosages are summarized in Table 7.13Nicotine gum is an over-the-counter
replacement product and is available in a
strength of 2 mg. The dose of gum depends
upon the smoking intensity of the quitter. It is
associated with a quit rate of about 23% as
against 13% with placebo. In one randomized
controlled trial, compliance was highest for the
patch (82%) compared with the gum (38%), the
spray (15%) and the inhaler (11%).,222 Nicotine
patches and nicotine-containing chewing gums
are not available as licenced NRT products in
India.
One important guideline is to advise the patient
to set the TQD before starting NRT. All NRT
formulations have demonstrated superior
efficacy in placebo-controlled clinical trials, with
an odds ratio of 1.5-2.5 at both end-of-trial and
2*^3 “^4
long-term (6- and 12-month) assessments.
325
H
—MFOW’T"’’*
"
Tobacco Control in India
I
Non-nicotine pharmacotherapy
inhibitors [SSRIs]) such as fluoxetine and the
5- HT-ia partial agonist buspirone.226 The opiate
antagonist naltrexone has also been used in
some settings. Mecamylamine, a nicotine
receptor antagonist, has been tried as an aid to
assist smoking cessation, with early trials not
showing a positive outcome when used alone,
and later studies suggesting a positive outcome
on combining it with NRT.226 Lobeline, a non
tobacco drug that shares tolerance with nicotine
on several measures, is available in over-thecounter anti-smoking medications in the US.226
The definite role of these drugs in tobacco
cessation treatments remains to be established.
Bupropion, the phenylaminoketone atypical
antidepressant in the sustained-release form, was
the first agent used in non-nicotine
pharmacotherapy for tobacco cessation, and is
now considered a first-line treatment for nicotine
dependence. A meta-analysis of two placebo
trials of bupropion demonstrated its superiority
over placebo, with the estimated odds ratio of
2.1 (95% confidence interval).202 Nortriptyline, a
tricyclic antidepressant, has also been used and
found to have similar quit rates as bupropion.
Clonidine, an alpha-2 adrenoceptor antagonist
used in opiate and alcohol withdrawal, has also
been shown to diminish some of the tobacco
withdrawal symptoms. The pooled odds ratio for
success in six trials with oral or transdermal
clonidine versus placebo was 1.89 (95%
confidence interval: 1.30-2.74).225
The future holds other promising agents such as
the gamma aminobutyric acid (GABA)-B agonist
baclofen, cannabinoid receptor antagonists,
glutamate receptor agonists, as well as vaccines.
Vaccines, which involve the injection of a
nicotine-like hapten conjugated to a strong
immunogen, and lead to the production of anti
nicotine antibodies and sequestration of
intravascular nicotine after cigarette smoking,
are being developed and phase I studies are in
progress. These novel treatments may be effective
options in both initiating smoking abstinence
and preventing relapse.226
Other pharmacological agents used in nicotine
cessation programmes include doxepin, the
reversible monoamine oxidase (MAO)-A
inhibitor moclobemide, the selective MAO-B
inhibitor and indirect dopamine (DA) agonist
selegeline hydrochloride, 5-HT selective
reuptake inhibitors (specific serotonin reuptake
Table 7.13 Pharmacological agents used for tobacco cessation
t iniiiir r- nr adm rin
mil c—i-iihimritfiiiraiw
mi wairamLw-.-ir'
:
____ ______ _____
— —-
Agent. <
•Nicotine .gum 7 '
Buccal route . —
only after TQD
itch
up to 10 tirries/dayu ■
; ....
trafisderm'al'route
Transdermal route
7-22 mg/day
7 '
6- 12 weeks
'
Local skin
irritation
.. .
-^1
rritranasally
16-32 mg/day
12^24 weeks
'’i
Intranasal or butcal
6-16 mg/day
150 mg o.d. X 3 days,
lease) ' 'intr^d to b.d., ' '
to begin t -2 weeks
before: TQD
..
1 1
: Up to 24 Week?
7- 12 weeks
.'
.
y
;; .ContraindicationS:|77
.^m^htoinlnghp?,:
i..7:tp;i24-weefc777:
________
___
NRT: nicotine replacement therapy; TQD: target quit dat£,
•
5 .
■
Source: Adapted from APA 2004; George and O'Malley 200421W26
.....
...
■I
.
-J ...
■7. 7' .7
/r-ay
326
II G
.
. ... 7
■.
aiw.^
. :
Tobacco Control: What Works?
Strategies for effective tobacco
control
. •_________ ______ -
Various guidelines all emphasize the need for
making tobacco cessation services widely
accessible to tobacco users.191’194’199’227-228 This has
several implications for a developing country
such as India, where identification rates in
clinical settings are low, a negligibly small
number of health professionals have received
training in these areas, availability and
affordability of pharmacotherapy are practical
constraints, a sizeable clientele is likely to be
rural and, as seen from the experience of the
tobacco cessation clinics (TCCs), the acceptance
of pharmacotherapy is low. Several urgent steps
need to be taken to make tobacco cessation
facilities widely available.
Since the problem of tobacco in India is complex,
in view of the varied nature of tobacco use, the
government has realized that the control of
tobacco can effectively be carried out only with
a multisectoral approach, involving the various
concerned sectors. Strategies for different sectors
are being identified for effective tobacco control
in the community, which would help in planning
the national strategy for tobacco control in India.
Tobacco cessation cannot succeed as an isolated
programme. It has to be designed and imple
mented as part of a Comprehensive tobacco
control strategy. This must include the
preventive, curative and rehabilitative aspects of
care. A bold step in this regard is the setting up
of TCC but this endeavour must be extended.
Capacity-building strategies for the identification
and management of tobacco use and disorders
related to its use must be made available through
the existing health care facilities. There must be
a provision for adequate therapeutic interven
tions, including the availability of replacement
therapies for tobacco dependence.
Health care delivery systems
Training medical and other health professionals
in tobacco cessation is critical to expand tobacco
cessation activities in the country. In the medical
sector, from general practitioners to specialists
in different areas, training must address the
attitudes to tobacco use, impart the knowledge
and skills required for intervention, address the
therapeutic nihilism that often surrounds tobacco
cessation interventions and provide updates on
emerging approaches to tobacco cessation.
Training of health professionals is an essential
part of a cost-effective, evidence-based strategy
for smoking cessation and treatment of tobacco
dependence because of their interaction with
smokers and other tobacco consumers as care
providers and their role as health communicators
in societies.229 However, health care providers and
professionals often lack sufficient motivation to
undertake smoking cessation as a means of
prevention. Misinformation about effective
interventions, inadequate training in all health
care settings, lack of support for routine
assessment, and lack of resources and
government funding are a few of the many factors
that impede health care professionals from taking
action.
In addition, professional organizations, such as
medical organizations and those involving
pharmacists, nurses, midwives and dentists,
among others, should become involved in the
training process at the international, regional,
national and local levels. This could include
organizing lectures at workshops and publishing
articles on smoking cessation in bulletins and
journals. They could thus provide basic
interventions as well as background materials
on smoking cessation relevant to the specific
professional groups.
Interventions in diverse, settings and
for diverse populations
The workplace has a captive population where
both tobacco prevention and cessation activities
can be undertaken, and better monitoring of
the effects of intervention is possible. Tobacco
is one of the ‘psychosocial’ problems (along with
stress, alcohol and drugs, violence and HIV/
327
S,.
Tobacco Control in India
AIDS) that is comprehensively addressed by the
International Labour Organization in the
SOLVE (stress, tobacco, alcohol/drugs, violence
and HIV/AIDS prevention) programme for
workplaces.230
More often than not, tobacco interventions
address mainly men who are smokers. It is
important that cessation activities also address
chewers, both men and women, as well as women
smokers. Other groups such as the elderly,
adolescents and patients with psychiatric illness
may require special interventions.
Youth tobacco cessation collaboratives for children
and teenagers begin with intervention through
education. Counselling centres have become
important prerequisites in schools and colleges.
Education Regarding tobacco awareness and
cessation should be imparted first to educators for
effective prevention of tobacco initiation. School
and college science exhibitions today impart
knowledge on tobacco along with subjects such as
cancer, for the benefit of both the thousands of
visitors and the students themselves.
An important strategy for tobacco prevention is
an initiative among the students, such as the
Students Working Against Tobacco (SWAT) in
the US. Student leaders in this group, particularly
ex-smokers, are perfect guides for teenagers
addicted to tobacco. .
Community
Tobacco cessation at the community level is
mandatory. Community participation should be
fortified through the frequency of public
involvement through meetings. Leaders should
not only be popular, committed and convincing,
but should be able to harness the might of the
community members effectively. A counselling
centre in every slum is an achievable goal.231
Community awareness and education should be
enhanced through the role of public and private
agencies, NGOs, the National Service Scheme
and National Cadet Corps, and spiritual leaders.
As in any other important issue, the cessation
strategy can be implemented in a cross-section
of society through a variety of sources. NGOs
are a committed force and empowering them
for tobacco cessation, even in a limited way,
has worked wonders. With the expanding
network of NGOs at every district level, the
cessation movement should be able to take giant
strides.
Quit lines and websites
A toll-free telephone number forms a single
access point to the national network of quit lines.
Of equal importance in tobacco control is the
establishment of quit lines at the national-, stateand local levels. In the US, counsellors have
proved more effective than self-help material.
An online guide to tobacco cessation is available
through websites such as www.smokefree.gov.
Instant messaging with the cessation expert is
made available. Cessation guides that can be
downloaded should also be of great use to the
tobacco user. These websites and guides have
been shown to increase the cessation rates by
40%/Similar use of information technology is
likely to help at least some sections of tobacco
users in India.
Expanding the available approaches
Although nicotine patches were introduced in
different parts of India, the exorbitant costs
limited the acceptance of this form of treatment.
Some pharmaceutical companies introduced
bupropion, but withdrew the product because of
low demand.
Considerable progress has been made in the
provision of effective treatments, both
behavioural and pharmacological, for tobacco
dependence. It is critically important that a wide
range of interventions be used both in general to
support tobacco cessation and specifically to
support those who wish to quit tobacco use even
when medication is not available.231 Social
support for quitting should be possible in all
countries, even those with extremely limited
Tobacco Control: What Works?
resources.231 In the Indian context, research on
the role of indigenous systems such as yoga
and ayurveda as cessation therapies or
facilitators should be systematically designed
and conducted.
According to the United States Clinical Practice
Guidelines, both social support as part of
treatment (intra-treatment social support) and
help in securing social support outside of
treatment (extra-treatment social support) are
especially effective in increasing the rate of
quitting. All countries have laypersons who can
provide informal social support for quitting and
who can be trained to conduct more formal
interventions.
In the background of diverse clinical
recommendations advocating the combined use
of behavioural counselling and pharmaco-therapy for tobacco cessation, it is critical to
develop systematic, large-scale studies in the
Indian context to determine the additive effect
of pharmacotherapy. Alternative ways oi using
nicotine substitutes, e.g. a gum to handle craving
instead of as a complete nicotine replacement
strategy, need to be evaluated.
There would appear to be special challenges in
countries where there- are relatively few ex
smokers and where tobacco prevalence rates are
high among health professionals.231 Ex-smokers
can serve as role models in encouraging quitting
and can provide social support to individuals
who are attempting to quit. They may also reflect
an environment in which quitting is a greater
priority. Attempts must be made to involve such
advocates in cessation programmes in India.
The major challenge for India in the twenty-first
century is to make early tobacco use cessation
treatment available to all tobacco users, evolve
treatments that are culturally relevant and
appropriately tailored to individuals and the
population, and view tobacco cessation in the
wider picture of prevention activities.
7.11 INDIVIDUAL INTERVENTIONS: PROMOTING TOBACCO CESSATION
S3SS3
key messages
. Tobacco use cessation use is an essential component for reducing the mortality and
morbidity related to tobacco use, as the lack of it may lead to an addmonal 160 mrlhon
global deaths among smokers by 2050.
immediate benefits of tobacco control arid
• Tobacco use cessation provides the most
m^dmhes the advantages for a tobacco user who quits the habit.
. Tobacco cessation services should be made widely accessible to tobacco users and should
cater to the wide range of products used in India.
. Capacity-building strategies for the identification and management of tobacco use and
disorders related to its use must strengthen the services avadable through the existing
health care facilities.
• Involvement of the community is an
essential component of a tobacco cessation programme.
329
'' •t1-. 7 (
Hi
•7'7
■
Tobacco Control in India
References
: -I • .-••
7.1 Policy interventions: Taxation
1. World Bank. Curbing the epidemic: Governments
and the economics of tobacco control. Washington,
DC: World Bank;'-1999.
2. Chaloupka F, Jha P (eds). Tobacco control in developing
countries. New York: Oxford University Press, World
Bank; 2000.
3. Guindon E, Boisclair D, Perucic Anne-Marie. Higher
tobacco prices and taxes in South-East Asia—an
effective tool to reduce tobacco use, save lives and
generate revenue. Health, nutrition and population
(HNP) Discussion Paper. Economics of tobacco control,
Paper No. 11. Washington, DC: World Bank; 2003.
4. Blackstone Market Facts. Smokeless tobacco industry
in India—a report. 2003.
5. Tobacco Institute of India. Representations to the
Ministry of Finance before the annual Central Budget,
various years.
6. Karki YB, Pant KD, Pande BR. A study on the economics
of tobacco in Nepal. Health, nutrition and population
(HNP) Discussion Paper. Economics oftobacco control,
Paper No. 13. Washington, DC: World Bank; 2003.
7. Tobacco Institute of India. Tobacco News. SeptemberOctober 2001.
7.2 Tobacco product regulation, testing and
laboratory strengthening
8. National Cancer Institute. Risks associated with smoking
cigarettes with low machine yields of tar and nicotine.
Smoking and Tobacco Control Monograph No. 13.
Bethesda: U.S. Department of Health and Human
Services; NCI; October 2001.
9. Benowitz NL, Hall SM, Kerning RI, Jacob P III, Osman
AL. Smokers of low yield cigarettes do not consume
less nicotine. New England Journal of Medicine
1983;309:139-42.
10. Jarvis MJ, Boreham R, Primatesta P, Feyerebend C,
Byrant A. Nicotine yield from machine-smoked
cigarettes and nicotine intakes in smokers: Evidence
from a representative population study. Journal of
the National Cancer Institute 2001;93:134-8.
11. National Cancer Institute. The FTC cigarette test
method for determining tar, nicotine and carbon
monoxide yields of US. cigarettes. Smoking and
Tobacco Control Monograph No.7. Bethesda: U.S
Department of Health Services, National Institutes
of Health, National Cancer Institute; 1996. NIH
publication 96-4028.39-57.
12. Ashley MJ, Cohen J, Ferrence R. 'Light' and 'Mild'
cigarettes: Who smokes them? Are they being misled?
Canadian Journal of Public Health 2001;92:407-11.
13. Cohen JB. Smokers' knowledge and understanding
of advertised tar numbers: Health policy implications.
American Journal of Public Health 1996;86:18-24.
14. Giovino GA, Tomar SL, Reddy MN, Peddicord JP, Zhu
BP, Escobedo LG. Attitudes, knowledge, and beliefs
about low-yield cigarettes among adolescents and
adults. In: Smoking and tobacco control. Monograph
No. 7: The FTC cigarette test method for determining
tar, nicotine, and carbon monoxide yields of US
cigarettes. Bethesda (MD): US Department of Health
and Human Services, Public Health Service, National
Institute of Health; 1996:39-56.
15. Evans N, Joossens L. Consumers and the changing
cigarette. London: Health Education Authority; 1999.
16. Cohen JB. Smokers' knowledge and understanding
of advertised tar numbers: Health policy implications.
American Journal of Public Health 1996;86:18-24.
17. Gori GB. Consumer perception of cigarette yields:
is the message relevant? Regulatory Toxicology and
Pharmacology 1990; 12:64-8.
18. Pollay RW, Dewhirst T. The dark side of marketing
seemingly 'Light' cigarettes: Successful images and
failed fact. Tobacco Control 2002; 11 (Suppl. 1):
118-31.
19. Wakefield M, Morley C, Horan JK, Cummings KM.
The cigarette pack as image: New evidence from
tobacco industry documents. Tobacco Control2002; 11
(Suppl. l):173-80.
20. Cigarette classification as a consumer- message.
Regulatory Toxicology and Pharmacology
1990;12:253-62.
21. Shiftman S, Pillitteri JL, Burton SL, Rohay JM, Gitchell
JG. Smokers' beliefs about 'Light' and 'Ultra-Light'
cigarettes. Tobacco Control 2001; 10 (Suppl. 1): 117-23.
22. Kozlowski LT, Goldberg ME, Yost BA, White EL, Sweeney
CT, Pillitteri JL. Smokers' misconceptions of light and
ultra-light cigarette may keep them smoking. American
Journal of Preventive Medicine 1998;15:9-16.
23. Canadian Ministerial Advisory Council on Tobacco
Control. Misleading cigarette descriptors: Recommen
dations 2001. Available from URL: http://www.hcsc.gc.ca/English/pdf/media/cig_discrip_repl.pdg
(accessed on 8 November 2004).
24. The European Union Directive. Directive 2001/37/EC
of the European Parliament and of the Council of
June 2001 on the approximation of the laws, regulations
and administrative provisions of the Member States
concerning the manufacture, presentation and sale
of tobacco products. Official Journal of the European
Communities, 18 July 2001.
25. World Health Organization. Framework Convention
on Tobacco Control. Available from URL: http://
www.who.int/tobacco/fctc/text/en/fctc_en.pdf
(accessed on 15 October 2003).
26. Stratton K, Shetty P, Wallace R, Bondurant S (eds).
Clearing the smoke: Assessing the science base for
tobacco harm. Washington, DC: National Academy
Press; 2001.
7.3 Policy interventions: Supply-side actions
27. Chapman S, Wong WL. Tobacco control in the third
world: A resource atlas. Penang, Malaysia: International
Organization of Consumers Unions; 1990.
28. Jha P, Chaloupka FJ. Curbing the epidemic:
Governments and the economics of tobacco control.
Washington, DC: The World Bank; 1999.
U6
Tobacco Control: What Works?
29. Wharton Applied Research Center. A Study of the
tobacco industry's economic contribution to the nation,
its fifty states, and the district of Columbia.
Philadelphia: Wharton Applied Research Center and
Wharton Econometrics Forecasting Associates, Inc.,
45 Vander Merwe R. Employment and output effects for
' Zimbabwe with the elimination of tobacco consumption
and production. Washington, DC: Population, Health
and Nutrition Department, World Bank; 1998.
46 Irvine D, Sims WA. Tobacco control legislation and
Source allocation effects. Canadian Public PoUcy
University of Pennsylvania; 1979.
30 Chase Econometrics. The economic impact of the
tobacco industry on the United States economy in
1983. Bala Cynwyd, PA: Chase Econometrics, 1
31 Pricewaterhouse. The economic impact ofthe tobacco
industry on the United States economy. Arlington,
VA: Price Waterhouse; 1990.
32 Pricewaterhouse. The economic impact ofthe tobacco
industry on the United States economy. Arlington,
VA: Price Waterhouse; 1992.
33. Tobacco Merchants Association. Tobacco's contribution
to the national economy. Princeton, NJ; Tobacco
Merchants Association; 1995.
34. American Economics Group. The US tobacco industry
in 1994: Its economic impact on the states.
Washington: American Economics Group; 1996.
35 PEIDA. The tobacco industry in the European
community, including Portugal and Spain. Edinburgh:
PEIDA; 1985.
36. Agro-Economic Services Ltd., Tabacosmos Ltd. The
employment, tax revenue and wealth that the tobacco
industry creates. London: Agro-Economic Services;
37. Deloitte, Touche. Economic contributions ofthe tobacco
industry in the tobacco growing region of Ontario.
Guelph: Resource Assessment and Planning
Committee; 1995.
38. Coopers and Lybrand.■ A1 study of the economic
advertising in Hong
impact of a ban on cigarette
(
Kong. Coopers and Lybrand; 1996.
39 Price Waterhouse Coopers. The tobacco industry m
’ India: An economic analysis. Canberra, Australia:
Economic Studies and Strategies Unit; 2000.
40. Buck D, Godfrey C, Raw M, Sutton M. Tobacco and
jobs. Society for the Study of Addiction and Centre
for Health Economics. York; University of York; 199 .
41 Vander Merwe R. The economics of tobacco control in
South Africa. In: Abedian I, Vander Merwe R, Wilkins
N Jha P (eds). The economics of tobacco control.
Towards an optima!policy mix. Cape Town: Medical
Association of South Africa Press; 1998:251-71.
42. Vander Merwe R. Employment issues in tobacco control
In: Abedian I, van der Merwe R, Wilkins N, Jha
(eds). The economics of tobacco control: Towards
an optima!policy mix. Cape Town: Medical Association
of South Africa Press; 1998:251-71.
43. Jacobs R, Gale HF, Capehart TC, Zhang P, Jha P. The
supply-side effects of tobacco control policies. In:
Jha P, Chaloupka JF (eds). Tobacco control in developing
countries. Oxford; Oxford University Press; 2002.
44. Warner KE, Fulton GA, Nicolas P, Grimes, DR.
Employment implications of declining tobacco product
sales for the regional economies of the United States.
Journal of the American Medical Association 19 ,
1997;23:259-73.
47 Allen RC. The false dilemma: The impact of tobacco
control policies on employment in Canada. Ottawa,
Ontario: National Campaign for Action on Tobacco;
1993
48 Centre for Multi-disciplinary Development Research
Economic aspects of tobacco cultivation and
consumption. A pilot study. Part of the research
project on Economics of shifting from tobacco
cultivation: An action research project. Karnataka.
Centre for Multi-disciplinary Development Research-.
49 Aberg E, Tedla G. Tobacco and alternative crops.
Report 77. Upsala: Swedish University of Agricultural
Sciences, Department of Plant Husbandry; 1979.
50 Al-Sadat N, Zain Z. Diversification of tobacco farming
in Malaysia. Proceedings of the Tenth World Conference
on Tobacco or Health; 1997 August 24-28; Beijing,
51. Altman DG, Zaccaro DJ, Levine DW, Austin D Woodeli
C Bailey B, et al. Predictors of crop diversification.
A survey of tobacco farmers in North Carolina.
Tobacco Control 1998;74:376-82.
52. Altman DG, Levine DW, Howard G, Hamilton H
Tobacco farmers and diversification: Opportunities
and barriers. Tobacco Control 1996;5:192-8.
53. Yach D. Tobacco in Africa. World Health Forum
1996;17:29-36.
54 Kweyuh PHM. Does tobacco growing pay? The rase
' of Kenya. In: Abedian I, Vander Merwe R, Wilkins
N jha P (eds). The economics of tobacco control.
Towards an optima!policy mix. Cape Town: Medica
Association of South Africa Press; 1998:245 50.
55. Young E. strategic directions for the Philippine tobacco
industry. Washington, DC: Ernst and Young, 19 .
56 Bonoan RR. Rezonification of tobacco-growing areas.
Philippine Journal of Crop Science 1994;19:56.
57 Pan American Health Organization (PAHO). Tobacco
or health: Status in the Americas. Scientific Publication
Number 536;1992.
58. Australia: Total tobacco deregulation has brought
new lease of life to industry and local content rules
are abolished too. Australian Financial Review 19
January 1998.
.
59 Bhat BN, Hundekar AR, Khot RS, Yandgoudar BA
Bidi tobacco. Dharwad: University of Agricultural
Sciences; 1998.
.
60. Satyapriya VS, Govindaraju KV. Economic vMty
of alternative crops to tobacco. Bangui Institute
for Social and Economic Change (ISEC); 1990.
61. Panchamukhi PR, Sailabala Debi, Anmgen VB,
Nayanatara SN. Economics of shifting from tobacco
cultivation. (Unpublished report based on the study
sponsored by IDRC, Canada.) Dharwad: Centre for
Multi-disciplinary Development Research; 2000.
275:1241-6.
.^/
“1
Tobacco Control in India
62. Kaur S. Tobacco cultivation in India: Time to search
for alternatives. In: Efroymson D (ed). Tobacco
and poverty: Observations from India and Bangladesh.
Canada: PATH; 2002.
63. Nagarajan K, Umamaheswara Rao M, Subba Rao R.
Status report on tobacco alternate crops 1995-96.
Central Tobacco Research Institute, Indian Council
of Agricultural Research; 2001.
64. Sharma RS. Hobson's choice for AP tobacco farmers.
Business Line 2000 March 24.
65. Rao P. Flue cured tobacco crop. Its impact on farmer
economics. Tobacco News July-August, New Delhi:
Tobacco Institute of India; 1999.
66. Karnataka State Department of Agriculture. Report on.
region-wise cost of cultivation of crops for the year
igg4-95. Bangalore: Government of Karnataka; 1995.
67. Singh KD, eta!. Studies on feasibility and economic
viability of tobacco based inter-cropping system in
Bihar. Tobacco Research 1998;24.
68. Jaisani BG. Possible substitutes alternate uses of
d/tf/tobacco. In: Sanghvi LD, Notani P (eds). Tobacco
and health—the Indian scene. Bombay: UICC
Workshop, Tata Memorial Centre; 1989.
69. Jacobs R. In: Samet JM, Yoon SY (eds). Economic
policies, taxation and fiscal measures in women and
the tobacco epidemic. Challenges for the 21 century.
The World Health Organization in collaboration with
the Institute for Global Tobacco Control John Hopkins
School of Public Health; 2001.
70. Taylor AL, Bettcher DW. WHO Framework Convention
on Tobacco Control: A global good for public health
review. Bulletin of the World Health Organization
2000;78:920-9.
71. The World Bank. Curbing the epidemic: Governments
and the economics of tobacco control. Series.
Development in practice. Washington, DC: The World
Bank; 1999.
72. World Trade Organization (WTO) agreements and
public health. A joint study by the WTO and WHO
Secretariat. Geneva, Switzerland: WTO Secretariat;
2002. Available from URL: http://www.who.int/media/
homepage/en/who_wto_e.pdf (accessed on 09
November 2004).
7.4 Policy intervention: Comprehensive ban
on advertising
73. Mackay J, Eriksen M. The tobacco atlas. Geneva:
World Health Organization; 2002.
74. Barnsley K, Jacobs M. Special feature. Tobacco advertising
and display of tobacco products at point of sale:
Tasmania, Australia. Tobacco Control 2000; 9:22836. Available from URL: http://tc.bmjjournals. com/
cgi/content/full/9/2/228 (accessed on 17 October 2004).
75. World Health Organization. WHO Framework
Convention on Tobacco Control (FCTC). Article 13.
Geneva: WHO; 2003. Available from URL: http://
www.who.int/tobacco/framework/finaLtext/en/
(accessed on 15 October 2004).
76. The Cigarettes and Other Tobacco Products (Prohibition
:
,332
of Advertisement and Regulation of Trade and Commerce,
Production, Supply and Distribution) Act, 2003, and
rules framed there under. Government of India.
77. World Health Organization (WHO). Guidelines for
controlling and monitoring the tobacco epidemic.
Geneva: WHO; 1998:56.
78. Campaign for Tobacco Free Kids. Tobacco advertising.
Tobacco Fact Sheet. 11th World Conference on Tobacco
or Health. Available from URL: http://tobaccof
reekids.org/campaign/global/docs/advertising.pdf
(accessed on 17 October 2004).
79. Willemsen MC, Blij BD. Tobacco advertising. Tobacco
Control Factsheets. Available from URL: http;//
factsheets.globalink.org/en/advertising.shtml
(accessed on 17 October -2004).
80. World Bank. Curbing the epidemics. Governments
and the economics of tobacco control. In: Measures
to reduce the demand for tobacco. Available from
URL; http://wwwl.worldbank.org/tobacco/book/html/
chapter4.htm (accessed on 17 October 2004).
81. Jha P, Chaloupka F (eds). Tobacco control in developing
countries. New York: Oxford Medical Publications,
The World Bank; 2000.
82. Sinha DN. Report on the results of the Global Youth
Tobacco Survey in Uttar Pradesh, India—2002. United
States Department of Health and Human Services.
Centers for Disease Control and Prevention. National
Center for Chronic Disease Prevention and Health
Promotion. Office on Smoking and Health. Available
from URL: http://www.cdc.gov/tobacco/global/GYTS/
reports/UttarPradeshIndia_2002.htm (accessed on 17
October 2004).
83. Campaign for tobacco free kids. Tobacco marketing
that reaches kids point-of-purchase advertising and
promotions. Available from URL. http.//
tobaccofreekids.org/research/factsheets/pdf/0075.pdf
(accessed on 17 October 2004).
7.5 Packaging and labelling of tobacco
products
84. World Health Organization and the World Bank. Tobacco
pack information at a glance. Available from URL:
http://wbln0018.worldbank.Org/HDNet/hddocs.nsf/0/
00206bce52dl530685256df600554530?
OpenDocument (accessed on 21 October 2004).
85. Choudhry K. Tobacco control in India. 50 years of
cancer control in India. Available from URL: http://
mohfw.nic.in/pg204to219.pdf (accessed on 21 October
2004).
86. The Cigarettes and Other Tobacco Products (Prohibition
of Advertisement & Regulation of Trade and Commerce,
Production, Supply and Distribution) Act, 2003, and
rules framed there under. Government of India.
87. World Health Organization. WHO Framework
Convention on Tobacco Control (FCTC). Article 11.
Geneva: WHO; 2003. Available from URL: http://
www.who.int/tobacco/framework/fi nal_text/en/
(accessed on 15 October 2004).
88. Nathan R. Mode! legislation for tobacco control: A
Tobacco Control: What Works?
policy development and legislative drafting manual.
Tobacco product labeling and packaging. Available
from URL: http://www.fctc.org/modelguide/
Isection08.html (accessed on 21 October 2004).
89. a proposal for new health-related information on
tobacco product labels. Legislation, regulation and
compliance. 2004. Available from URL: http://www.hcsc.gc.ca/hecs-sesc/tobacco/legislation/labelling/#H
(accessed on 20 October 2004).
90. World Trade Organization. Canada's health warning
messages for tobacco products. 2003. Available
from URL: http://www.wto.org/english/tratop_e/tbt_e/
event_oct03_e/case7_e.ppt (accessed on 20 October
care, education and consumer expenditure. National
Sample Survey, 52nd Round, 1995-96 report.
101. Shah S, Vaite S. Pavement dwellers in Mumbai,
India—Prioritizing tobacco over basic needs. In:
Tobacco and poverty: Observation from India and
Bangladesh. Canada: PATH; 2002.63-72.
102. Reddy KS, Prabhakaran D, Shah P, Shrivastava U,
” Prabhakar AK, Shah B, et al. Tobacco consumption
in north Indian imales is inversely related to
educational level: Results of three cross sectional
surveys. World Conference on Tobacco or Health,
2000 (in press).
103. World Health Organization. Tobacco and poverty:
A vicious circle for the Tobacco Free Initiative.
20°4.
L
91 Smokeless tobacco product warning labels. American
Cancer Society. 2000. Available from URL: http://
^w.ftc.gov/os/comments/tobaccocommehts/acs.pdf
(accessed on 20 October 2004).
92. Non-smokers Rights Association. Smoking and Health
Action Foundation. Images of Canadian health
warnings. Available from URL: http://www.nsraadnf.ca/news_info.php?cPath = 22&news_id=78
(accessed on 26 October 2004).
93. Global tobacco control. EU: EC: Warning label images
and tobacco or health report. Available from URL:
http://member.globalink.org/49286 (accessed on 23
October 2004).
94 . Gray N, Boyle P. Publishing tobacco tar measurements
on packets. British Medical Journal 2004;329:81314. Available from URL: http://bmj.bmjjournals.com/
cgi/content/full/329/7470/813 (accessed on 21
October 2004).
95. Health Related Information Dissemination Amongst
Youth (HRIDAY). Tobacco related picture based health
warning messages prepared for the Ministry of Health,
Government of India; 2004.
7.6 Protection of vulnerable groups: A human
rights approach to tobacco control
96. United Nations Economic and Social Council. Report
of the Secretary-General on the Ad Hoc Inter-Agency
Task Force on Tobacco Control. E/2004/55. New
York, 28 June-23 July 2004. Available from URL.
http://ods-dds-ny.un.org/doc/UNDOC/GEN/N04/331/
39/PDF/N0433139.pdf?OpenElement (accessed on
19 October 2004).
97. Jha P, Chaloupka FJ. Curbing the epidemic:
Governments and the economics of tobacco control.
Washington, DC: The World Bank, 1999.
98. Gajalakshmi CK, Jha P, Nguyen S, Yurkeli A. Patterns
of tobacco use, and health consequences.Background
paper. In: Jha P, Chaloupka FJ (eds). Curbing the
epidemic: Governments and the economics of tobacco
control. Washington, DC: The World Bank; 1999.
99. Subramanian SV, Nandy S, Kelly M, Gordon D, Smith
GD. Patterns and distribution of tobacco consumption
in India: Cross sectional multilevel evidence from
the 1998-99 National Family Health Survey. British
Medical Journal 2004;328:801-6.
100. National Sample Survey Organization. Report on health
Geneva: WHO; 2004.
104 . Regional Consultation of Health and Human Rights.
10-11 April 2001, New .DelhU-NaWoal Human
Rights Commission.
7.7
Community interventions: Protecting the
youth from tobacco
?_■„ T, Lopez AD, Boreham J, Thun M, Heath C,
105. Peto R,
Doll R. Mortality from smoking worldwide. British
Medical Bulletin 1996;52:12-21.
106. Arora M, Aghi M, Reddy KS. Global Youth Tobacco
Survey—Delhi report. Available from URL: http.//
www.cdc.gov/tobacco/global/GYTS/reports/pdf/
india_newdelhi_2001_searmo.pdf (accessed on 28
July 2004).
107. Wasserman J, Manning WG, Newhouse JP, Winkler
JD. The effects of excise taxes and regulations on
cigarette smoking. Journal of Health Economics
1991;10:43-64.
108. Jones SE, Sharp DJ, Husten CG, Crossett LS.
Cigarette acquisition and proof of age among US
high school students who smoke. Tobacco Control
2002;11:20-5.
109 Ling PM, Landman A, Glantz SA. It is time to
abandon youth access tobacco programmes. Tobacco
Control 2002;11:3-6.
110. Chaloupka FJ, Hu TW, Warner KE, Jacobs R,
Yurekli A. The taxation of tobacco products. In.
jha P, Chaloupka FJ (eds). Tobacco control in
developing countries. New York: Oxford University
Press, World Bank; 2000:254.
Ill Jha P, Chaloupka FJ. The economics of global
tobacco control. British Medical Journal
2000;321:358-61.
112. Tauras JA. Public policy and smoking cessation
" among young adults in the United States. Health
Policy 2004;68:321-32.
113. Response to increases in cigarette prices by race/
ethnicity, income, and age groups—United States,
1976-1993. Mortality and Morbidity Weekly Report
1998;47:605.
114. Ross H, Powell LM, Tauras JA, Chaloupka FJ. ImpacTeen
Research Papers. New evidence on youth smoking
behavior based on experimental price increases.
Available from URL: http;//www.impacteen. org/
ab_RPNo30_2003.htm (accessed on 26 July 2004).
................... ■’
n
Tobacco Control in India
115. Chaloupka FJ, Pacula RL. Sex and race differences
in young people's responsiveness to price and
tobacco control policies. Tobacco Control
1999;8:373-7.
116. Laugesen M, Scollo M, Sweanor D, Shiftman S,
Gitchell J, Barnsley K, eta!. World's best practice in
tobacco control. Tobacco Control 2000;9:228-36.
117. Reddy KS, Arora M, Perry CL, Nair B, Kohli A, Lytle
LA, et al. Tobacco and alcohol use outcomes of a
school-based intervention in New Delhi. American
Journal of Health Behavior 2002;26:173-81.
118. Winkleby MA, Feighery E, Dunn M, Kole S, Ahn
D, Killen JD. Effects of an advocacy intervention
to reduce smoking among teenagers. Archives
of Paediatrics and Adolescent Medicine
2004;58:269-75.
119. Public education reduces tobacco use. Available
from URL: http://www.tobaccofreekids.org/research/
factsheets/index.php?CategoryID=6 (accessed on
15 August 2004).
120. Renaud L, O'Loughlin J, Dery V. The St-Louis du
Parc Heart Health Project: A critical analysis of the
reverse effects on smoking. Tobacco Control
2003;12:302-9.
121. Lovato C, Linn G, Stead LF, Best A. Impact of
tobacco advertising and promotion on increasing
adolescent smoking behaviors. Cochrane Database
Systematic Review 2003;(4):CD003439.
122. Choi WS, Ahluwalia JS, Harris KJ, Okuyemi K.
Progression to established smoking: The influence
of tobacco marketing. American Journal ofPreventive
Medicine 2002;22:228-33.
123. Rajasekaran A. Cinema smoking encourages the
habit in adolescents. Thorax 2003;58:822.
124. Charlton A, While D, Kelly S. Boys' smoking and
cigarette brand-sponsored motor racing. Lancet
1997;350:1474.
125. Donovan RJ, Jancey J, Jones S. Tobacco point of
sale advertising increases positive brand user imagery.
Tobacco Control 2002;11:191-4.
126. Straub DM, Hills NK, Thompson PJ, Moscicki AB.
Effects of pro- and anti-tobacco advertising on
nonsmoking adolescents' intentions to smoke. Journal
of Adolescent Health 2003;32:36-43.
127. Wakefield M, Flay B, Nichter M, Giovino G. Effects
of anti-smoking advertising on youth smoking: A
review. Journal of Health Communication
2003;8:229-47.
128. Henriksen L, Fortmann SP. Young adults' opinions
of Philip Morris and its television advertising. Tobacco
Control 2002;11:236-40.
129. Mckenna J, Gutierrez K, Mccall K. Strategies for an
effective youth counter-marketing program:
Recommendations from commercial marketing
experts. Journal of Public Health Management and
Practice 2000;6:7-13.
130. Webster.RA, Hunter M, Keats JA. Peer and parental
influences on adolescents' substance use: A path
analysis. International Journal of Addictions
1994;29:647-57.
131. Fichtenberg CM, Glantz SA. Effect of smoke-free
workplaces on smoking behavior: Systematic review.
British Medical Journal 2002;325:188.
132. Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans
CT, Barker DC, Ruel EE. Effect of restrictions on
smoking at home, at school, and in public places
on teenage smoking: Cross sectional study. British
Medical Journal 2000;321:333-7.
133. Rentz MA, Dwyer JH, MacKinnon DP, Flay BR, Hansen
WB, Wang EY, et al. k multicommunity trial for
primary prevention of adolescent drug abuse. Effects
on drug use prevalence. Journal of the American
Medical Association 1989;261:3259-66.
134. Bewley BR, Johnson MRD, Banks MH. Teachers
smoking. Journal of Epidemiology and Community
Health 1979;33:219-22.
135. Charlton A, While D. Smoking prevalence among
16- to 19-year-olds related to staff and student
smoking policies in sixth forms and further education.
Health Education Journal 1994;53:28-39.
136. Sinha DN, Gupta PC, Warren CW, Asma S. Effect of
school policy on tobacco use by school personnel in
Bihar, India. Journal of Schoo! Health 2004;74:3-5.
7.8 Community interventions: Smoke-free
public places
137. Action on smoking and health. Fact sheet-14. Smoking
in workplaces and public places. Available from
URL: http://www.ash.org.uk/html/factsheets/html/
factl4.html (accessed on 15 October 2004).
138. National Library of Medicine. Health services/
technology assessment text. Reviews of evidence
regarding interventions to reduce tobacco use and
exposure to environmental tobacco smoke. Available
from URL: http://www.ncbi.nlm.nih.gov/books/
bv.fcgi?rid=hstat3.section.7463 (accessed on 15
October 2004).
139. World Bank. Curbing the epidemics. Governments
and the economics of tobacco control. In: Measures
to reduce the demand for tobacco. Available from
URL: http://wwwl.worldbank.org/tobacco/book/html/
chapter4.htm (accessed on 17 October 2004).
140. National Guideline Clearing House. Brief summary.
Recommendations regarding interventions to reduce
tobacco use and exposure to environmental tobacco
smoke. Available from URL: http://www.guideline.
gov/summary summary.aspx?doc_id=2614&nbr=
1840#s23 (accessed on 15 October 2004).
141. Fichtenberg CM, Glantz SA. Effect of smoke-free
workplaces on smoking behaviour: A systematic review.
British Medical Journal 2002;325:174-5.
142. World Health Organization (WHO). WHO Framework
Convention on Tobacco Control (FCTC). Article 8.
Geneva: WHO; 2003. Available from URL: http://
www.who.int/tobacco/framework/final_text/en/
(accessed on 15 October 2004).
143. Status of ban on smoking in public places worldwide.
The Tobacco News 2004 March-April.
144. World Health Organization. Prevention and cessation
Y
- Tobacco Control: What Works?
r
of tobacco use. A manual for clinic and community
based interventions. New Delhi: Regional Office
for South-East Asia; 2003.
145. Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans
CT, Barker DC, Ruel EE. Effect of restrictions on
smoking at home, at school, and in public places
on teenage smoking: Cross sectional study. British
Medical Journal 2000;321:333-7. s
146. Rentz MA, Dwyer JH, MacKinnon DP, Flay BR,
Hansen WB, Wang EY, et al. A multicommunity
trial for primary prevention of adolescent drug
abuse. Effects on drug use prevalence. Journal
of the American Medical Association
1989;261:3259-66.
147. Bewley BR, Johnson MRD, Banks MH. Teachers
smoking. Journal ofEpidemiology and Community
Health 1979;33:219-22.
148. Charlton A, While D. Smoking prevalence among
16- to 19-year-olds related to staff and student
smoking policies in sixth forms and further education.
Health Education Journal 1994;53:28-39.
149. Sargent RP, Shepard RM, Glantz SA. Reduced
incidence of admissions for myocardial infarction
associated with public smoking ban: Before
and after study. British Medical Journal
2004;328:977-80.
150. Sinha DN. Report on the results of the Global
Youth Tobacco Survey in Uttar Pradesh, India
2002. Available from URL: http://www.cdc.
gov/tobacco/global/GYTS/reports/UttarPradesh
India_2002.htm (accessed on 15 October
2004).
151. Sinha DN, Gupta PC, Warren CW, Asma S.
Effect of school policy on tobacco use by school
personnel in Bihar, India. Journal of Schoo!
Health 2004;74:3-5.
152. Bhandari U. A tobacco-free town. World Health
Forum 1998;19:301.
153. Rediff on the Net. News. 1998. Available from
URL: http://www.rediff.eom/travel/iaetc.htm#
2008domair (accessed on 18 October 2004).
154. Tobacco News and Information. Smoking ban
on south's trains. Available from URL: http://
www.tobacco.org/news/164057.html (accessed
on 18 October 2004).
155. Strategies for reducing exposure to
environmental tobacco smoke, increasing
tobacco use cessation, and reducing initiation
in communities and health-care systems. A
Reporton Recommendations of the Task Force
on Community Preventive Services. Morbidity
and Mortality Weekly Report 2000;49:1-11.
7.9 Community interventions: Strength
ening health literacy on tobacco-
related matters
156. Public education reduces tobacco use. Available
from URL: http://www.tobaccofreekids.org/
research/factsheets/pdf/0051.pdf (accessed on
15 August 2004).
157. Vartiainen E, Paavola M, McAlister A, Puska P.
Fifteen-year follow-up of smoking prevention effects
in the North Karelia Youth Project. American Journal
of Public Health 1998;88:81-5.
158. Perry CL, Kelder SH, Murray DM,Klepp KI.
Communitywide smoking prevention: Long-term
outcomes of the Minnesota Heart Health Program
and the Class of 1989 study. American Journal of
Public Health 1992;82:1210-16.
159. Seeker-Walker RH, Worden JK, Holland RR, Flynn
BS, Detsky AS. A mass media programme to prevent
smoking among adolescents: Costs and cost
effectiveness. Tobacco Control 1997;6:207-12.
160. Community based programs reduce tobacco use.
Available from URL; http://www.tobaccofreekids.org/
research/factsheets/pdf/0053.pdf (accessed on 16
October 2004).
161. Centers for Disease Control and Prevention (CDC).
National Center for Chronic Disease Prevention
and Health Promotion. Best practices for
comprehensive tobacco control programs. August
1999. Available from URL: http://www.cdc.gov/
tobacco/research_data /stat_nat_data/bestprac.pdf
(accessed on 16 October 2004).
162. The use of counter-advertising as a tobacco use
deterrent. Available from URL: http://www.advocacy.
org/publications/mtc/ counterads.htm (accessed on
16 October 2004).
163. CDC. Cigarette smoking before and after an excise
tax increase and antismoking campaign—
Massachusetts, 1990-1996. Morbidity and Mortality
Weekly Report 1996;45:966-70.
164. Goldman LK, Glantz SA. Evaluation of antismoking
advertising campaigns. Journal of the American
Medical Association 1998;279:772-7.
165. Renaud L, O'Loughlin J, Dery V. The St Louis du
Parc Heart Health Project: A critical analysis of the
reverse effects on smoking. Tobacco Control
2003;12:302-9.
7.10 Benefiting from models of behaviour
change
166. Nutbeam D. Promoting health and preventing disease:
An international perspective on youth health
promotion. Journal of Adolescent Health 1997; 20:
396-402.
167. World Health Organization. Ottawa Charter for Health
Promotion. Geneva: WHO; 1986.
168. McLeroy KR, Bibeau D, Steckler A, Glanz K. An
ecological perspective on health promotion
programmes. Health Education Quarterly 1988;
15:351-77.
169. Kotler P. Marketing for nonprofit organizations.
Englewood Cliffs, NJ: Prentice-Hall; 1975.
170. Andreasen AR. Marketing social change: Changing
behaviour to promote health, social development,
and the environment. San Francisco: JosseyBass; 1995.
171. Alcalay R, Bell RA. Promoting nutrition and physical
activity through social marketing: current practices
335.
Tobacco Control in India
and recommendations. Davis, CA: Center for
Advanced Studies in Nutrition and Social Marketing,
University of California; 2000.
172. Green L. Behavioural health: A handbook ofhealth
enhancement and disease prevention. New York:
Wiley; 1986.
173. Green L, Kreuter M. Health promotion planning.
2nd ed. Mountain View: Mayfield Publishing Co.;
1991.
174. Institute of Health Promotion. Precede: Procede
overview. Available from URL: http://www.ihpr.ubc.
ca./PrecedeRefs.html (accessed on 6 March 2004).
175. Institute of Health Promotion. Precede-Proceed Model
of Health Promotion. Available from URL: http://
www.ihpr.ubc.ca./ProcedePrecede.html (accessed on
6 March 2004).
176. National Cancer Institute. Theory at a glance: A
guide for health promotion practice. Bethesda,
MD: National Institutes of Health, National Cancer
Institute; NIH Publication 95-3896; 1995.
177. Becker MH. The health belief model and personal
health behavior. Health Education Monographs.
Vol. 2\ 1974.
178. Rosenstock IM. The health belief model: Explaining
health behaviour through expectancies. In: Glanz
K, Lewis FM, Rimer BK (eds). Health behaviour
and health education: Theory, research, andpractice.
San Francisco, CA: Jossey-Bass; 1990:39-62.
179. Prochaska JO, DiClemente CC. Stages and processes
of self-change of smoking: Towards an integrative
model of change. Journal of Consulting and Clinical
Psychology 1983;51:390-5.
180. Prochaska JO, DiClemente CC. The transtheoreticai
approach: Crossing traditional boundaries ofchange.
Homewood, IL: Irwin; 1984.
181. Rollnick S, Heather N, Gold R, Hall W. Development
of a short 'Readiness to Change' Questionnaire for
use in brief opportunistic interventions. British Journal
of Addiction 1992;87:743-54.
182. Bettman JR. An information processing theory of
consumer choice. Reading, MA: Addison-Wesley; 1979.
183. Bandura A. Social foundations ofthought and action:
A social cognitive theory. Englewood Cliffs, NJ:
Prentice Hall; 1986.
184. Lando HA, Hellerstedt WL, Pirie PL, Fruetel J,
Huttner P. Results of a long-term community smoking
cessation contest. American Journal of Health
Promotion 1991;5:420-5.
185. Popham W1 Pnttpr i n Hetrick M*, Muthen LK,
Duerr JM, Johnson MD. Effectiveness of the California
1990-1991 Tobacco education media campaign.
American Journal of Preventive Medicine
1994;10:319-26.
186. Prochaska JO, DiClemente CC, Norcross JC. In:
search of how people change: Applications to addictive
behaviours. American Psychologist 1992;47:
1102-14.
187. Perry CL. Creating health behaviour change: How
to develop community-wide programmes for youth.
Thousand Oaks, California: Sage Publications; 1999.
188. The Government of Hong Kong Special Administrative
Region of the Peoples Republic of China. Introduction.
Available at URL: http://www.info.gov.hk/dh/
do_you_k/Surveyreport/report2.PDF (accessed on
21 October 2004).
189. Ray CS, Gupta P, de Beyer J. Research on tobacco
in India (including betel quid and areca nut): An
annotated bibliography of research on use, health
effects, economics, and control efforts. Washington,
DC: Health, Nutrition and Population Family of the
World Bank's Human Development Network; 2003.
7.11 Individual interventions: Promoting
tobacco cessation
190. World Health Organization. The World Health Report
1999. Making a difference. Geneva: WHO; 1999.
191. Raw M, McNeill AD. The prevention of smoking
related disease. Addiction 1994;89:1505-9.
192. United States Department of Health and Human
Services (USDHHS). Clinical practice guideline # 18
smoking cessation. Washington, DC: US Government
Printing Press; 1996.
193. United States Department of Health and Human
Services (USDHHS). Reducing tobacco use: A report
of the Surgeon General. Washington, DC: US
Government Printing Press; 2000.
194. Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V,
Baker T. Cost effectiveness of the Clinical Practice
Recommendations in the AHCPR Guideline for Smoking
Cessation. Journal ofthe American Medical Association
1997;278:1759-66.
195. Parrott- S, Godfrey C, Raw M, West R, McNeill A.
Guidance for commissioners on the cost effectiveness
of smoking cessation interventions. Thorax mS',53
(Suppl. 5):S1-S38.
196. Callum C. The smoking epidemic. London: Health
Education Authority; 1998.
197. Raw M, McNeill A, Watt J, Raw D. National smoking
cessation services at risk. British Medical Journal
2001;323:1140-1.
198. United States Department of Health and Human
Sen/ices (USDHHS). A report ofthe Surgeon General:
The health benefits ofsmoking cessation. Washington,
DC: US Government Printing Office; 1990.
199. World Health Organization. Treatment of tobacco
dependence and smoking cessation methods. In:
Policy recommendations for smoking cessation and
treatment of tobacco dependence. Geneva: World
Health Organization; 2003.
200. Okuyemi KS, Ahluwalia JS, Wadland WC. The
evaluation and treatment of tobacco use disorder.
Journal of Family Practice 2001;50:981-7.
201. Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom
KO. The Fagerstrom test for nicotine dependence:
A revision of the Fagerstrom tolerance questionnaire.
British Journal of Addiction 1991;86:1119-27.
202. Fiore MC. US public health service clinical practice
guidelines: Treating tobacco use and dependence.
Respiratory Care 2000;45:1200-62.
1^
Tobacco Control: What Works?
r
203. Glynn TJ, Manley MW. How to help your patients
stop smoking. Washington, DC: US Government
Printing Office; 1989.
204. Prochaska JO, DiClemente CC. Stages and processes
of self-change of smoking: Toward an integrative
mode of change. Journal of Consulting Clinical
Psychology 1983;51:390-5.
205. Benowitz NL. The use of biologic fluid samples in
assessing tobacco smoke consumption. NIDA
Research Monograph 1983;48:6-26.
206. Shiftman SM. Relapse following smoking cessation:
A situational analysis. Journal of Consulting and
Clinical Psychology 1982;50:71-86.
207. Lando HA. Formal quit smoking treatments. In:
Orleans CT, Slade JD (eds).;. Nicotine addiction:
Principles and management. New York: Oxford
University Press; 1993.
208. Cinciripini PM, Lapitsky L, Seay S, Wallfisch A, Kitchens
K. The effects of smoking schedules on cessation
outcome: Can we improve on common methods of
gradual and abrupt nicotine withdrawal? Journal of
Consulting and Clinical Psychology 1995; 63:388-99.
209. Gritz ER, Klesges RC, Meyers AW. The smoking and
body weight relationship. Implications for intervention ‘
and post-cessation weight control. Annals of
Behavioural Medicine 1989;11:144-53.
210. Marcus BH, Albrecht AE, King TK, Parisi AF, Pinto
BM, Roberts M, et al. The efficacy of exercise as an
aid for smoking cessation in women: A randomized
controlled trial. Archives of Interna! Medicine
1999;159:1229-34.
211. Baillie A, Mattick RP, Hall W, Webster P. Metaanalytic review of the efficacy of smoking cessation
interventions. Drug and Alcohol Reviews
1994;13:157-70.
212. Kottke TE, Battista RN, DeFriese GH, Brekke ML.
Attributes of successful smoking cessation
interventions in medical practice: A meta-analysis
of 39 controlled trials. Journal of the American
Medical Association 1988;259:2882-9.
213. West R, McNeill A, Raw M. Smoking cessation
guidelines for health professionals: An update. Thorax
2000;55:987-99.
214. Law M, Tang JL. An analysis of the effectiveness of
interventions intended to help people stop smoking.
Archives of Interna! Medicine 1995;155:1933-41.
215. Lancaster T, Stead LF. Individual behavioral counselling
for smoking cessation (Cochrane review). In: The
Cochrane Library, Issue 2. Chichester, UK: John
Wiley and Sons Ltd; 2004.
216. American Psychiatric Association. Clinical research/
practice guidelines for nicotine. Arlington, VA:
American Psychiatric Association; 2004. Available
from URL: http://www.psych.org/archives/clin_res/
pract_guide/nicotine/pg_nicotine_2.cfm (accessed
on 3 November 2004).
217. Hajek P, Stead LF. Aversive smoking for smoking
cessation (Cochrane review). In: The Cochrane Library,
Issue 2. Chichester, UK: John Wiley and Sons Ltd;
218. Lancaster T, Stead LF. Self-help interventions for
smoking cessation (Cochrane review). In: The
Cochrane Library, Issue 2. Chichester, UK: John
Wiley and Sons Ltd; 2004.
219. Marcus BH, Albrecht AE, Niaura RS, et al. Exercise
enhances the maintenance of smoking cessation
in women. Addictive
1995;20:87-92.
220. Ussher MH, West R, Taylor AH, McEwen A. Exercise
interventions for smoking cessation. (Cochrane
review). In: The Cochrane Library, Issue2. Chichester,
UK; John Wiley & Sons Ltd; 2004.
221. Lancaster T, Stead L, Silagy C, Sbwden A.
Effectiveness of interventions to help people stop
smoking: Findings from the Cochrane Library. British
Medical Journal 2000;321:355-8.
222. Hajek P, West R, Foulds J, Nilsson F, Burrows S,
Meadow A. Randomized comparative trial of nicotine
polacrilex, a transdermal patch, nasal spray, and
an inhaler. Archives of Interna! Medicine
1999;159:2033-8.
223. Anderson JE, Jorenby DE, Scott WJ, Fiore MC.
Treating tobacco use and dependence: An evidence
based clinical practice guideline for tobacco cessation.
Chest 2002;21:932-4.
224. Fiore MC, Smith SS, Jorenby DE, Baker TB. The
effectiveness of the nicotine patch for smoking
cessation: A meta-analysis. Journal of the American
Medical Association 1994;271:1940-7.
225. Gourlay SG, Stead LF, Benowitz NL. Clonidine for
smoking cessation (Cochrane Review). In: The
Cochrane Library, Issue 2. Chichester, UK: John
Wiley & Sons Ltd; 2004.
226. George TP, O'Malley'SS. Current pharmacological
treatments for nicotine dependence. Trends in
Pharmacological Treatments for Nicotine Dependence
2004;25:42-8.
227. Treating tobacco use and dependence—clinician's
packet. A how-to guide for implementing the public
health service clinical practice guideline, March
2003. U.S. Public Health Service. Available from
URL: http://www.surgeongeneral.gov/tobacco/
clinpack.html (accessed on 3 November 2004).
228. National Institute of Clinical Excellence (NICE).
Guidance on the use ofnicotine replacement therapy
(NRT) and bupropion for smoking cessation.
Technology Appraisal Guideline No. 39. London,
UK: NICE; 2002.
229. Marin Tuya D. Training of health care professionals.
Presentation at the WHO meeting on Global Policy
for Smoking Cessation hosted by the Ministry of
Health of the Russian Federation, Moscow, 14-15
June 2002.
230. International Labour Organization. Addressing
psychosocial problems at work. Geneva: ILO Safe
Work; 2002.
231. Lando HA. Future research needs and capacity
building. Presentation at the WHO meeting on Global
Policy for Smoking Cessation hosted by the Ministry
of Health of the Russian Federation, Moscow, 14-
15 June 2002.
2004. ’
MR
, v....
BACKGROUND
The Smokefree Class Competition originated in Finland, where it has been carried out annually
since the 1989 school year by four NGOs. The competition has been financed by the Ministry
of Social Affairs and Health.
In the competition each class decides to be a non-smoking class for a duration of six months.
Classes in which pupils refrain from smoking can participate in a prize draw. The competition
has been popular in Finland: about half of the targeted age group has participated, annually.
We presented an evaluation of the competition at the Tobacco or Health Conference in Helsinki
in October 1996. Reiner Hanewinkel from Germany and Kamel Abdennbi from France were
at the conference and became interested in the idea. At about the same time the ENYPAT
office moved from ASH Scotland to KTL in Helsinki. We decided to apply Finland’s
competition concept to build a European Smokefree Class Competition. Reiner Hanewinkel
agreed to start as a co-ordinator and soon seven countries submitted an application for the
Europe Against Cancer Programme for March 1997.
The Europe Against Cancer Programme funded the first round 1997/98. Reiner Hanewinkel
and Gudrun Wiborg from IFT-Nord (Institute for Therapy and Health Research) worked hard
with other co-ordinators from Denmark, Finland, France, Italy, Spain and Wales to set up a
well-working project. A total of 3,819 classes and about 100,000 students from 1,040 schools
participated. A German class won the international prize, a trip to Paris.
After the first experience ENYPAT decided to include the competition in the ENYPAT
Framework Project application. Four new countries - Austria, Belgium, Greece and the
Netherlands - are joining the 1998/99 round. This publication presents the experiences of the
first international round in seven countries. We warmly thank all the writers!
Erkki Vartiainen
Project Director
Meri Paavola
Project Manager
European Network on Young People and Tobacco (ENYPAT)
National Public Health Institute (KTL), Finland
7
Gudrun Wiborg and Reiner Hanewinkel
Institute for Therapy and Health Research (IFT-Nord)
Kiel
THE SMOKEFREE CLASS COMPETITION 1997/98
A Summary of the First International Round
1. INTRODUCTION
The Smokefree Class Competition is a school-based smoking prevention pr
year 1997/98 the Smokefree Class Competition was earned out for the first time on a European
tevel; schools in Denmark, Finland, France, Germany, Italy, Spain and UK were invited to
participate. The competition was co-ordinated by IFT-Nord in Kiel, Germany.
The main aims of the competition are the delay and prevention of smoking onset among
pupils who do not smoke, and the reduction and cessation among those who have already
experimented with smoking. Pupils aged 12-14 are the target group, since research has
repeatedly shown that this is the age when pupils begin to expenment with tobacco.
Classes that participated in the competition pledged not to smoke for a period of six months^
Those who succeeded took part in a national prize draw where they could win a number of
attractive prizes for the whole class.
In addition to the national prizes, there was an international prize draw for a class tap to
Paris The international prize draw served to emphasise the European context of the competition
and to enhance communication between pupils of various participating countries. A German
class won the Paris trip and met one of the participating French classes in November 1998.
The competition can be embedded in various subjects in schools and is not particularly time
consuming. The countries involved were able to place the addresses of the participating classes
on the Internet in order to foster communication between the pupils participating in different
countries.
-------
“ -
In this first competition 3,819 classes out of 1,040 schools from the seven countries registered
for participation. In other words, around 100,000 European pupils decided to be smokefree
and enter the competition. On the European level Austria, Belgium, Greece and the Netherlands
will join the competition in the school year 1998/99.
On the national level the competition was earned out in selected regions (except for Finland,
where the whole country participated). In the school year 1998/99, the competition will also
be expanded on the national level.
9
.
- -
---’••• --c
2. BACKGROUND
Cigarette smoking is one major factor promoting the development of chronic diseases such
as cancer, cardiovascular disease and chronic obstructive lung disease. The earlier pupils
start to smoke, the more likely they become regular smokers in future years. Research has
shown that more than half of the regular smokers started smoking at the age of 13. However,
people who start smoking after the age of 20 very rarely become addicted. Moreover, smoking
is often a precursor for taking other kinds of drugs such as marijuana, cocaine or even heroin.
There is a great variety of smoking prevention programmes which are based on information
about the long-term health consequences of smoking. However, it is well understood now
that programmes that concentrate only on information and fear arousal strategies — even
though leading to better knowledge - show very limited effects on attitudinal or behavioural
changes in pupils. In fact, they can even arise pupils’ curiosity to find out what smoking is
about by experiencing it first hand.
The idea of the Smokefree Class Competition is different to traditional approaches. Instead
of using fear arousal strategies, the desired non-smoking behaviour is reinforced: non-smokers
get rewarded if they stay smokefree. It is well known from learning theory that positive
reinforcement enhances the probability of producing a desired behaviour. In this way non
smoking becomes a popular and worthwhile behaviour, and social norms within peer groups
are influenced in a way that non-smoking behaviour becomes more common in classes than
smoking.
3. IMPLEMENTATION< OF THE COMPETITION
3.1. Rules of the competition
The general rules of the competition are similar in each country:
• Classes decide to be a non-smoking class for a period of six months. During this first run,
the duration of the competition differed in the participating countries from 4 to 6 months.
In the school year 1998/99, however, every participating country will carry out the
competition for a period of 6 months.
• Pupils sign a class contract and an individual contract promising not to smoke during the
competition. These contracts serve to underline their commitment.
• The responsibility of controlling smoking lies mainly with the pupils themselves: Pupils
monitor their smoking status and report to teachers regularly whether they have smoked or
not.
• Classes which refrain from smoking for the whole period are rewarded. They participate in
a national as well as a European prize draw in which they can win a number of attractive
prizes.
• National prizes vary by country.
The main prize in the international prize draw is a trip to one of the other participating countries.
10
The competition is flexible so that details can be developed to suit the needs and circumstances
of individual countries. For instance in Denmark, Finland, Italy and Spain classes dropped
out of the competition if a pupil smoked regularly. In France classes in which no one smoked
were awarded the national main prize, classes in which more than one smoked were awarded
the national second prize, etc. A class dropped out if more than five pupils smoked on a
regular basis. In the UK classes were rewarded depending on the time they stayed smokefree.
Moreover, in the UK up to 25% of the pupils in every class were allowed to smoke. In Germany
classes dropped out of the competition if more than 10% of the pupils in a class smoked on a
regular basis. In Denmark all participating classes had to carry out a drug preventive activity,
and in Spain there was a special competition where the best Smokefree Class Competition
slogan was awarded an additional prize.
3.2. Development of the materials
Each of the participating countries developed their own materials for the competition (flyer,
class contract, pupils contract, poster, etc.).
3.3. Teachers’ brochures
Teachers’ brochures were developed to explain the idea of the competition and to advise
teachers on handling the problems that could occur, for instance bullying among pupils, relapses
into smoking or dishonesty.
3.4. Health education materials
In some countries teachers’ manuals were developed consisting of teaching units dealing
with smoking prevention as well as personal and social skills so that teachers could use the
materials in class and carry out further drug preventive activities. In addition, detailed health
education material for teachers and pupils was offered on the Internet in Finnish, Swedish,
English, French, Spanish, German and Italian (www.jyu.fi/no-smoking).
3.5. Promoting the European idea of the Smokefree Class Competition
The Internet was used to promote and enhance communication between pupils in different
countries. Participating schools of all involved countries could place their addresses on aspecial Smokefree Class Internet page (www.jyu.fi/no-smoking). The Internet is a perfect
medium for this purpose as it is becoming increasingly popular among young people and a
growing number of schools in Europe have access to it.
11
19,1
An international flyer was also developed promoting the idea, the principle goals and the
rules of the competition and providing the addresses of all European partners. At the end of
the competition there was an international prize draw, in which one class could win a trip to
one of the participating countries, in order to familiarise pupils with other European cultures.
3.6. Meetings of the project team
Regular meetings were held by the co-ordinators and ENYPAT:
London, September 4, 1997
This first meeting was carried out during the planning stage of the competition.
Matters discussed:
• Current status of the competition plans in the countries involved (e.g. recruitment of schools,
co-financing, etc.)
• Rules of the competition
• National and international prizes
• Presentation of the project on the Internet
• Translation of materials
• Evaluation of the project
London, January 30,1998
The meeting was held right after all countries had started the competition or were just about
to start it. Matters discussed:
• Current status of the competition: Recruitment of schools, participation rate, problems.
• Introduction of new partners for the next run: The Netherlands, Belgium, Austria, Greece.
Barcelona, June 26, 1998
This meeting took place right after the competition had terminated in all countries.
Matters discussed:
• Drop-outs
• Problems encountered during the competition:
- Bullying in school
- Dishonest pupils
- Lack of external control
- Lack of motivation of teachers
• Suggestions for improvement of the rules and implementation of the competition in the
school year 1989/99
12
13^
Table 1: European co-ordinators and institutions involved
Country
Co-ordinator
Institution
Denmark
Mr. Joergen Falk
Danish Council on Smoking and Health,
Copenhagen
Finland
Mrs. Heli Tyrvainen
Mrs. Meri Paavola
Finnish Health Association, Jyvaskyla
KTL, Helsinki (ENYPAT)
France
Dr. Kamel Abdennbi
Association Institut Coeur et Vaisseaux,
Paris
Germany
Mrs. Gudrun Wiborg
Dr. Reiner Hanewinkel
Institute for Therapy and Health Research,
Kiel
Italy
Dr. Elizabeth Tamang
Dr. Giovianni Pilati
Centro di Educazione alia Salute, Padova
Spain
Dr. Manel Nebot
Institut Municipal de la Salut, Barcelona
UK
Mrs. Sue Bowker
Mr. Ceri Breeze
Health Promotion Wales, Cardiff
4. RESULTS OF THE SMOKEFREE CLASS COMPETITION 1997/98
4.1. Participating schools and classes
The competition was carried out in selected regions. The only exception was Finland, where
schools from the whole country were invited to participate. Finland has carried out the
Smokefree Class Competition since 1989/90 and has a wide experience in organising the
competition on a large scale. In future years all participating countries plan to expand the
competition.
Europe-wide about 100,000 pupils from nearly 4,000 classes participated in the competition.
This means that more than 1,000 schools were involved.
Table 2: Participating schools and classes in the school year 1997/98
Country
Number of participating
schools
Denmark
128
145
Finland
503
2.688
France
31
91
Germany
227
462
Italy
82
141
Spain
25
88
UK
44
204
Total
1.040
3.819
13
Number of participating
classes
4.2. Drop-outs
The drop-out rate ranged from 30% to 42% of the registered classes for Spain, Italy, Ger
many and France and nearly or more than 60% for Denmark and Finland. The UK had the
lowest drop-out rate: only about 17%.
Table 3: Number and percentage of drop-outs in the school year 1997/98.
Country
Number of dropped-out
classes
Percentage of dropped-out
classes
Denmark
84
57.9 %
Finland
1,822
67.7 %
France
36
39.5 %
Germany
191
41.2%
Italy
46
32.6 %
Spain
37
42.0 %
UK
34
16,6 %
To assess the pupils’ smoking status, they were asked to monitor their smoking behaviour
(or non-smoking behaviour) and report it to their teachers regularly. No external control was
undertaken. Looking at the percentage of classes which dropped out of the competition, the
figure seems to be quite high. The results indicate that the pupils tended to tell the truth.
4.3. Presentation of the project
Newspapers, radio or TV
Each of the involved countries presented the Smokefree Class Competition in a number of
regional newspapers, and in some cases in national newspapers. Moreover, the Smokefree
Class Competition was presented on radio and TV on several occasions.
International conferences
Conference
Date
Place
1. The Fifth International Congress
of Behavioural Medicine
19-22 August 1998
Copenhagen,
Denmark
2. Working Together for Better
Health
23-25 September 1998
Cardiff, UK
14
International publications
Hanewinkel, R., Wiborg, G„ Paavola, M. (1997). What is the idea behind the “Smokefree
Class Competition44? Tobacco-free healthy cities, December issue.
Hanewinkel, R., Wiborg, G., Tamang, E„ Paavola, M. (1998). Smokefree Class Competi
tion: Germany won the international prize. Tobacco-free healthy cities, June issue.
Hanewinkel, R„ Wiborg, G. (1998). The Smokefree Class Competition. ENYPATNewsletter Interaction, 9.
Hanewinkel, R., Wiborg, G., Paavola, M., Vartiainen, E. Smokefree Class Competition - a
European school-based anti-smoking campaign. Tobacco Control, 7(2).
Vartiainen E., Paavola M., Vertio H. “No Smoking Class” competitions in Finland: their
value in delaying the onset of smoking in adolescence. Health Promotion International,
1996:3 (11):189-192.
15
A
7
Xi
Q'
for Rog
m
e fi
I u r
Paris
klasser pS Fyn
lland. For at vaere med i
konkurrencen skal du og din
andre
klasser
E u r o p
Mgsse dels holde jer regfri •
irrenceperioden og dels
et projekt, som far betyd-
k I a s s e o P 9 a v e
i v e
wn
or
pj
klasser
i. I kan sam-
si
med
Bnke d
Mi
k AV
Bi
7^
andre
iJ
r*
16
Jorgen Falk
Danish Council on Smoking and Health
Copenhagen
THE SMOKEFREE CLASS COMPETITION 1997/98 IN DENMARK
The Danish competition was carried out as a pilot project among 7lh graders in one part of the
country. The competition was linked to one of the existing Danish projects “Smoke Free Year
Group 2001” which is targeted at the same age group.
In Denmark the design of the project somewhat differed from the other countries: in order to
participate in the lottery, the classes had to work with the subject “smoking” in a way that
would involve or be visible for other classes of the school - or even the local community.
Therefore the invitation to participate was followed by a “catalogue of ideas”, out of which
the teachers could choose activities for this purpose. Another difference was the absence of
contracts and that pupils’ smoking habits were monitored once a month. At the end of the sixmonth period the teacher gave a brief report to the Danish Council about the activity carried
out.
About 1700 classes from about 1200 schools were invited to participate. 145 classes from
128 schools took the challenge. 84 classes dropped out. 71 classes participated in the lottery.
There were 5 prize winners. The main prize was 4000 ECUs and the winning class was from
Nyborg. We had expected to involve a greater number of classes, and we found that the drop
out rate was too high.
A process evaluation was made after the competition. Every participating teacher received a
questionnaire. 86 teachers answered (most of the drop-out teachers did not). 12 teachers who
participated throughout the competition and 14 teachers who did not participate at all were
selected for a phone interview:
62% of the participating teachers found the competition good or very good.
65% of the teachers claim that the class found the activity good or very good.
43% of the teachers would like to participate again.
77% of the teachers think that the class has learned something about smoking during the
competition.
• 86% of the teachers think it is a good way to teach children something about smoking.
•
•
•
•
We learned from the evaluation that the marketing of the competition should be better next
year. The rules about smoking - not smoking should be clearer. Too many teachers expected
that the quality of their activity would be part of the winning criteria. At the end of the
competition we should inform every participating class immediately about the winners, and
perhaps give them a gift. The idea of the special activity works very well, and drop-out is
almost always caused by smoking'. During the year 98/99 the competition will be carried out
nationwide at 7th and 8th grade levels.
17
13^
skiviik.
SMOKEFREE CLHSS ) ' ’
smokefreeciA^,
Suonsn S/upaylidist./s Isfve;s r; sosiaaH- a isr*.eysmirister o'
18
Heli Tyrvainen
Finnish Health Association
Jyvaskyla
THE SMOKEFREE CLASS COMPETITION 1997/98 IN FINLAND
The Smokefree Class Competition was arranged in Finland for the ninth time. The organising
team consisted of four non-governmental organisations, whose co-operation worked very
A new poster for the competition is prepared every year. In addition, schools receive two
different contract forms and teaching material. The competition and the material are bilin
gual; Finnish and Swedish. The Finnish competition has cash prizes: 2 x 1650 Ecus, 8 x 825
Ecus and 20 x 170 Ecus (about).
All the grade 7 and grade 8 classes in the country were invited to participate in the competi
tion. About a half of the 7th grade classes and a fourth of the Sth grade pupils accepted the
challenge. Participating classes were to abstain from smoking for six months. Some 35% of
the participating 7th grade classes and 26% of the Sth grade classes reached this goal. In
terms of the number of successful classes, the success rate has remained about the same since
the first year the competition was organised.
The working principle of the competition was to involve popular role models and idols from
film, sports and music as promoters. These celebrities occupied a prominent position in the
competition poster. In conjunction with the competition, a campaign was carried out through
the radio and Internet, where a band that is well-known and a favourite among teenagers
made a public promise to quit smoking. The teenagers had an opportunity to send encourag
ing messages to the band and make jokes about smoking. This campaign was a big. success,
and many young people said in their Internet feedback that they had given up smoking be
cause their idol had done so.
Information was this year’s weak point. Information on the competition was mailed with the
competition poster to all schools. In addition, the competition gained some coverage in the
media, and local papers frequently published bulletins about it. Yet, the information did not
reach all the school teachers who would have been interested: The te^Uefs also needed more
motivation and direct contact with the competition organisers.
Schools are very busy with their work. Only one third of the schools used classroom materi
als related to the competition. During the school year the whole effort may have been forgot
ten by some students and teachers. Schools that were actively involved had also arranged, for
instance, smoking-related special events and contests ivithin the school. Experiences from
those events were very positive.
19
l^°|
According to the feedback, teachers doubted their students’ honesty and felt that maintaining
surveillance over the competition is impossible. Responsibility was not always adequately
shifted to the students themselves. Another problem that was mentioned was that the classes
could not participate if there was a student who smoked regularly, and in those cases that
student may have been blamed or made to feel guilty.
Having learned from these experiences, in the future more attention will be paid to the ways
we could better activate the schools, motivate the teachers and improve the promotional and
informational support. To a large extent the practical arrangements in the schools have be
come routine, so we need new stimuli and fresh ideas to foster the notion of non-smoking and
keep it in the foreground.
20
i
Kamel Abdennbi
Association Coeur et Vaisseaux
Paris
THE SMOKEFREE CLASS COMPETITION 1997/98 IN FRANCE
109 schools from Seine St. Denis, a close suburb of Paris, were invited to participate in the
competition. The target group was the first year (66me) and the second year (5cme) of secondary
school. This represented 1316 classes who should have received the documents inviting them
to enter the competition, but we learned that the information did not work correctly.
Every school received documents inviting them to participate. These documents were sent to
the headmaster, the doctor and the nurse. Even though we dispatched the documents, many
nurses, for example, did not receive them because the headmaster of the school decided not
to enter the competition.
1. Registration
31 schools participated in the competition, 28% of all schools contacted.
A total of 91 classes reached the goal of being a “smokefree class” until May 31, 1998.
36 classes dropped out the competition (39.5%).
2. Duration
The competition was organised from January to May 31 (5 months).
3. Rules of the competition
If none in the class experienced tobacco: Level A
If one to two pupils experienced tobacco: Level B
If three to five pupils experienced tobacco: Level C
If more than 5 pupils smoked: Dropped-out.
4. Sponsors
The competition was encouraged by the artist Barbara Henricks. The poster presented the
Parisian football team Paris Saint Germain, the famous reporter J.M. Larque, the world cham
pion of the 400-meter dash Stephane Diagana, and the artists Smain and Les Inconnus.
Some financial help was received from a pharmaceutical laboratory and from the communal
health services (DASS ). The main financier of the competition was association Institut Coeur
et Vaisseaux.
1^1
2J
U J 4 -d
N G AI - 0
wO
-■-
gAtjMMrC’^ • *'■ '• V'/
SMphww CMtMwno'.jn;?;.‘y
B
-
W B8,
ft’'■-■'■’IfA
"■■ Wi
. ..
1*«-
-..■
V t w]Bl
.A X •-
1 .
5
: 'W
.■
--
-
-<
Bft'WWs
1
/ BOB
■'
v
7
:<■:</..
'
"
7
■-
M^ftcw iiS ig^cr?JSk
TKftj*
ifegba^
J
b-""’ te
B’
<
'
. .- **
?■
r z
S
«
■■
■.
■■-
'■’
4''~\
:a
■
.
’
' ;V
■', V 'W
.
z <
''■
®. p
'.
|R
■ fIf
■®A,
■
ft,
‘*'"' •
■
WS
'
9
g$;■vigp
’.- ■ -■r
■r ';7:-^R^5'- '
5------ "-’-7; |E|
itt
._ ml
-,__•-
ftftfftgW;
"|J|
3•
ftg
-■
. ft 1
.
’-^1
TTZ- 'T'---'
s. "ft. ..ft'.ftJA!.*
B»u.
r- :
1 B MB ^COHCOUBS^
..
W CLASSES wow ran™,
■-P.'..
•Wj, ■ 4 Jca^Mich’d lrwqu&.,ft^r*
'ft"'
. ft«
'
ft ■
■
R si
;;,
^r* 4 i
■
ft
•
ft
SSfeB
s»
..
■■
■
.' ;ft-; ;
ft" 'IB I'-'.?l <Bft.
-'BO
ft.- /7ftJ*-;
/<.f
■'
5?®':
ft
‘
.
; ft'.; ■"""■/
> ~->‘ -rjvy'
-
. .7'...
i"«'
""A . . ft/ . -#-:
••
I
"•
to* Inrx'nn.n.
W.....
'ft.-
''' ''
'
?. ■
_____________
IJ J J;5'
22
Q-AystyiiM ifflwiWz
5. Prizes
Level A: 4 prizes of 20,000 FF
Level B: 3 prizes of 10,000 FF.
No level C was registered.
All the pupils who were present at the prize ceremony received a Smokefree Class T-shirt.
The international prizes were rucksacks from IFT-Nord.
6. Prize ceremony
The prize ceremony was held with the Minister of Health, Bernard Kouchner, in attendance.
The ceremony programme consisted of rap music about tobacco, theatre, poems, a paintings
exposition and similar events.
7. Feedback from teachers
• Teachers suggested that the competition starts earlier next year.
• The web site is not very attractive in its French version, so they would like to see it
improve.
.
• The prizes should go first to a school, then to a winning class; this would prevent one
school from winning too many the prizes. (In fact, three classes from the same school won
prizes.)
8. Materials
The teachers had the possibility to contact all the associations working in the field of tobacco
prevention in the department. They also received a CD-I (interactive CD-ROM) with an
8-hour programme on tobacco. Some classes organised information activities around tobacco.
9. Press reports
The competition was presented three times on TV in national news reports and two times on
in national newspapers and
radio (RTL and BFM). In addition, three articles were published
[
in a specialised medical publication.
10. Congresses
Poster presentation at the 3rd National Congress of Preventive Cardiology (Toulouse Septem
ber 1998).
23
•ti ilOil
is® ^015
'•<■■■
v--'-.
NICHTRAUCHEN '98!
-x-
|Bo
bJ
3
•'XrX''
®SOM
®
f
i
Gudrun Wiborg and Reiner Hanewinkel
Institute for Therapy and Health Research
Kiel
THE SMOKEFREE CLASS COMPETITION 1997/98
“BE SMART - DON’T START” IN GERMANY
1. Numbers and percentages of participating schools and classes
1227 schools were invited to participate in the competition. As can be seen from table 1
below, around T8.5% of all invited schools registered for the competition.
Table 1: Numbers and percentages ofparticipating schools and classes
Retention Rate, %
At Start
At End
Schools
227
154
67.8 ____________
Classes
462
'271
58.6____________
Grade 7
260
161
61.9 ____________
Grade 8
203
110
54.1
2. Workshops for teachers
The competition programme included three workshops for teachers. Two were held prior to
the start of the competition in the two Bundeslander participating in the project. The third
was organised halfway through the competition. Pupils were also invited to participate m the
second workshop. Around 30% of all participating teachers participated in the workshops.
3. Questionnaires for teachers and pupils
At the end of the competition, questionnaires were sent to all teachers and to a representative
sample of 30 classes (regardless of whether the class had remained in the competition or not).
Data was assessed anonymously and prior to the announcement of the winners. A self
addressed, stamped envelope was also enclosed.
Questionnaires were developed to assess the following.
a.
b.
c.
d.
Could the onset of smoking be delayed?
Could smoking be reduced?
Was the target group reached?
How useful were the main rules of the competition?
25
e.
f.
g-
h.
i.
Did pupils lie in the weekly assessment, since they knew that there was no external
control?
Did pupils take the competition seriously?
Did negative group pressure (bullying) occur during the competition?
Were parents interested in the project?
The applicability of the health education material and several other aspects that shall
not be discussed here.
70% of the teachers and 70% of the pupils returned the questionnaires. The main results are
discussed below.
357 pupils returned the questionnaires.
305 teachers-returned the questionnaires.
Results
a. Could the onset of smoking be delayed?
Very encouraging data: 72.3% of the pupils reported that smoking could have been delayed
“very often”. 10.8% said that it could be delayed “often”.
The teachers’ data is nearly as promising: 70.7% reported that smoking had been delayed
“very often” or “often”. There were no meaningful differences between the grades.
b. Could smoking be reduced?
Around 4Q% of pupils and teachers reported that smoking had been reduced “very often ” or
“often”. Around 30% of both said that it could be reduced “sometimes”. A noticeable
difference between the class 8 and class 7 pupils was that only 30.4% of those in class 8
believe that smoking had been reduced, while 48% of those in grade 7 were of that opinion.
This data shows that the competition seems to be more suitable as a primary prevention
project, which means that it might be able to delay smoking onset among non-smokers to a
wider extent than it is able to reduce smoking among smokers — at least on a short-term basis.
c. Could the target group be reached?
61.2% of the pupils and 72.2% of the teachers were of the opinion that the target group was
reached. But: We also asked whether it would make sense to extend the competition to grade
six, and 68.8% of the pupils and 64% of the teachers were convinced that the competition
should start in grade six. When asked for a reason, teachers and pupils mentioned repeatedly
that they regularly come across smokers aged 10-11.
d. How useful were the main rules of the competition (assessed by teachers)
• At least 90% of the class has to decide to participate in the competition. 63.4% considered
this rule as “very usefur’ and 24.8% as “useful”.
• Class contract: 59.1% said it was “very useful” and 27.1% said it was “useful”.
26
• Pupils’ contract: 48.8% judged it as “very useful” and 24.8% as “useful”.
• 10% of the class is allowed to smoke: 55.8% regarded this rule was “very useful” and
23.1% considered it “useful”.
• Weekly assessment of smoking status (based on pupils self-monitoring): 43.6% considered
the rule as “useful” and 20.5% as “very useful”. But: 20.5% of the teachers gave a “mixed”
response. They argued that this rule makes pupils more likely to lie.
' e. Did pupils lie in the weekly assessment, due to a lack of external control?
The results of this question are very interesting: While 89% of the pupils reported that they
themselves told the truth, only 33.5% of the pupils were of the opinion that their classmates
were honest. However, the teachers show more trust in their pupils than the pupils in their
classmates: 87.6% of the teachers regarded their pupils to be honest.
f Did pupils take the competition seriously?
56.6% of the pupils took the competition “seriously” or “very seriously”. 24.4% had mixed
feelings about it, because of the missing control of potential smoking behaviour. Here we
have to look at the grades again: Grade 7 took the competition more seriously than pupils in
grade 8 (39.2% in grade seven vs. 22.8% in grade eight).
g. Did negative group pressure (bullying) occur?
• Around 21 % of the pupils reported that non smokers put pressure on smokers “sometimes
• According to the pupils, smokers only put pressure on non smokers “sometimes” in about
5% of the cases. The percentages for teachers are very similar.
h. Did parents show interest in the project?
Very disappointing results in this case: 60.7% of the parents never or seldom showed any
interest in the project. Only around 30% of the teachers organised a parent evening concerning
the project.
i. Health education material
Health education material was developed and given to interested teachers before and during
the competition. The material was developed to provide the teachers with some inspirations
for various activities dealing with non-smoking that they could carry out in class in different
subjects. For us it was of great importance to make sure that the material could be integrated
into different subjects (like biology, sports, German, French, etc.), since we know that teachers
don’t have so much time to spare for activities besides normal class.
—
63% of the teachers used the materials “a few times” and 10.6% used it “often”.
61% of the teachers considered the material to be “helpful” for activities carried out in class
and 7.6% judged it to be “very helpful”.
27
4. Outlook for the next run
• Extension to the sixth grade
• Involvement of the parents
• Spot-check controls of pupils
5. Preparation for the school year 1999/2000
For the school year 1999/2000 the competition was included in the ENYPAT Framework
Project proposal for the programme “Europe Against Cancer” of the European Union.
Moreover, Iceland will participate as country number 12 in 1999/2000.
I2!?
28
Elizabeth Tamang and Giovanni Pilati
Centro di Educazione alia Salute
Padova
THE SMOKEFREE CLASS COMPETITION 1997/98 IN ITALY
The Italian Smokefree Class Competition was carried out in the Veneto region. Veneto has
4,380,797 inhabitants in a territory of 18.364,28 km2. We have about 670 secondary schools
and 220 high schools. Third-year secondary schools and first-year high school classes
(13-14 year olds) were invited to participate in the competition for the year 1997/98. A total
of 141 classes belongingla 82 schools with 2,938 students joined the competition. The classes
signed a contract to remain smoke-free for a period of 19 weeks monitoring their smoking
behaviour each week.
At the end of the competition the classes who kept their commitment to remain smoke-free
received a non smoking certificate and participated in the national prize draw. The first prize
was a CD player/radio tape recorder for each student of the winning class. The second winning
class participated in the international draw for a trip to one of the other countries and since the
international prize draw was won by a German class, they received the “Be smart don’t start”
rucksacks. Each student who participated at the competition till the end received a colourful
purse with the Smokefree Class Competition (SEC) logo. The prize giving ceremony was
held in the school of the winning class. The school had also organised a concert for the
occasion by students of the participating classes.
1. Materials prepared for the competition
• Leaflet about the SEC
• Student’s contract
• Class Contract
• Monitoring chart
• Participation Certificate
• Purses with SEC logo
• Press conference packs
The Veneto region is divided into 21 loeal Health Units (LHU), each LHU has a Service of
Health Education and Health Promotion which are connected to the Regional Centre for
Health Education. This network was used to present the competition to schools and to distribute
the materials. A press conference was held before and after the competition. In the second
press conference some students from the participating classes and two teachers were also
invited and interviewed by the journalists. There was a lot of press coverage both in TV and
newspapers.
29
centro di educazione alia salute
SERVIZIO REGIONALE DI DOCUMENTAZIONE
K
I
Al ■
competition
____
30
Si
I
2. Results
Participation:
82 Schools; 141 classes and 2,938 students. The drop out rate was 32.6%.
The number of 3rd year secondary school classes participating was 74 and the number of 1st
year high school classes was 67.
Drop-outs:
• 3rd year secondary school classes: 17 (23%)
• 1st year high school classes: 29 (43%)
A poster presentation about the competition was made at the “Working together for better
health” Conference in Cardiff in September 1998.
3. Feedback from teachers and students about problems or difficulties
In one class the teacher discovered some pupils had smoked without the class admitting. In
the beginning, some classes’ students had some difficulties controlling the smoking behaviour
of each other; one class reported teasing from senior students by offering them cigarettes (but
this was done in play and not as bullying).
4. Lessons learned for the next edition
Although participation was not as high as we had hoped, we will continue this project in 98/
99. Enthusiasm for the project has grown among health workers and teachers as the competition
has progressed in the classes during the school year. Next year we will start the competition
earlier, from 1st November 98 to 30th April 99. Presentation of the materials to the Local
Health Unit and to schools will be done earlier. Invitations to schools will also be made
directly with the competition packs. The monitoring chart size will be A4 (much easier to
photocopy for the schools and to send by fax). We intend to prepare six postcards like some
of the other countries to get feedback each month from classes, to use testimonial and have a
special post card enabling classes to choose to write to classes in other participating countries.
Classes will also be invited to prepare a slogan for future edition of the competition.
1^1
31
°f
lx
AM®
3^
B;
JiMi
r^j^z4
s
'.
>
JIHiw
min
I
k
til®
Hi-
fc..
w
■
■■•■•■
IW" fe
1O>
•
■■
■
■,.-
■
'
;^®w
ilili
SS|
<<;fe!j<iiSM
iiSIII
«H
32
I
Manel Nebot
Institut Municipal de la Salut
Barcelona
THE SMOKEFREE CLASS COMPETITION 1997/98 IN SPAIN
1. Preparation phase
In November 1997, once the proposal was approved, the preparation phase was launched
basically consisting of:
■-
Befinition of the rules
----- -—
• Design and development of a graphic “logo”, support materials and flyers for the programme
diffusion.
2. Diffusion phase
In December 1997, programme information was sent to all the secondary schools of the city.
At the same time, the programme was introduced to the district school staff and to the
Educational Authority of Barcelona (Institut Municipal d’Educacio de Barcelona) A panel of
ten experts was used to help the local project co-ordinators both in programme diffusion and
follow-up, and in helping us to choose the appropriate prizes. The programme was also
presented tp the local Cancer League (Associacio Espanyola contra el cancer), which decided
to sponsor the programme.
3. Follow-up phase
The competition was run from January 15,h to May 15th. Overall 88 classes from 25 schools
decided to participate and to become a non-smoking class for this period. 25 classes from 6
schools dropped out very early and 12 classes dropped out later. 51 classes succeeded to stay
non-smoking until the end of the programme (58% of all participants).
In each participant class the teacher monitored the situation and promoted activities related to
smoking prevention. After the competition the contact person sent the follow-up form to the
organisers.
...
..- .......................................
4. Prizes
The competition had four national prizes. The main prize was a day cruise and a Walkman for
each pupil of the class. Second and third prizes consisted of books and tape recordings. A
special prize sponsored by the Cancer League (as CD-player for every pupil of the class) was
given to the best slogan related to tobacco prevention. In addition, all classes that remained
smokefree received a certificate.
33
5. Final assessment
Despite the fact that the information about the programme did not reach schools until the end
of the first term, the programme was well accepted. Most schools that left the programme did
so relatively early This suggests that teachers discovered that pupils were a ready smoking
and not willing to stop. This was confirmed by some teachers in the follow-up forms.
Nevertheless, this indicates that most teachers took it very seriously and preferred leaving the
competition rather than ignoring or hiding the problem.
The prize delivery was an extremely warm and friendly event and we all had a lot of fun
Perhaps we are used to dealing with health topics in a very senous way, so the event was
quite refreshing new approach. The slogan contest was also a success; every school deve oped
a sMgan andXt drewa picture even though it was not in the rules. Teachers said that they
had used this as an occasion to talk about smoking, its dangers, its addictive power
ways to resist social pressure.
In summary we are highly satisfied with the programme. In terms of the future challenges,
™
improve dFffiiion and soda! visibility, and »e need to develop new matenals
(posters, flyers) using the ideas given by pupils through the slogan competition.
34
Sue Bowker and Ceri Breeze
Health Promotion Wales
Cardiff
THE SMOKEFREE CLASS COMPETITION 1997/98 IN WALES
1. INTRODUCTION
The Smokefree Class competition is a pan-European project that aims:
• To encourage pupils to remain smokefree by discouraging experimentation with tobacco
To help experimenters not to become regular smokers
• To show clearly that not smoking is normal
• To encourage discussion about the benefits of remaining smokefree
2. BACKGROUND
Teenage smoking in Wales has increased between 1986 and 1996 so that 23% of boys and
29% of girls aged 15-16 smoke at least weekly1. During this time there has been success in
delaying the onset of smoking, so that in 1996 for those 11-16 year olds who have ever
smoked the average age of first experimentation was 11.32 years.
The Smokefree Class Competition-is based on an idea developed in Finland during 1989-90. ,
It was initially targeted at their 8th grade pupils (our Year 9), and attracted 15,000 entrants in
the first year. The competition has run annually since then, and with an extension to 7th grade
pupils (our Year 8) regularly sees entry levels of 55,000.
An evaluation of the Finnish project demonstrates success in delaying the onset of smoking
amongst young people2.
3. THE COMPETITION
3.1. Consultation phase
A meeting was held at Health Promotion Wales’ offices in July 1997 to discuss the proposed
competition. Twelve representatives of the health and education sectors in Wales attended the
meeting, and eight others discussed the idea by telephone.
The proposal was outlined as below:
• Competition to be aimed at Year 8 pupils as research shows that this is a prime age for
experimentation with smoking
• Competition to run for 5-6 months, from January 1998
• Pupils decide in their registration classes to enter the competition as a whole class
35
1^5
SowS^^W
i Dost
iV.
O^bbc
; /. '-4^• i-vr
•isaiojf
.
Helpwch^i i $daj[ati
(?^^J<i'^'7®^r':‘!fr'f -
M/v
■■
i*.. 'sill
2®
<y r.V-I. > <<SV.1?
ft .
\r'l
f <
*K
ST/
0
w . .j
aO is i
.. .^.—'
J
fl
36
• Individual pupils sign a commitment not to smoke for the competition period
• Pupils reaffirm their commitment monthly
• Classes still in the competition after 3, 4, 5 (and 6) months are entered into a prize draw.
Following the meeting the proposal was refined to take account of some concerns expressed:
• Entry is possible as long as 90% of the class wish to join in, and are not regular smokers
• Classes can stay in the competition as long as 75% of the class wish to do so, and are not
regular smokers
• A regular smoker is defined as someone who smokes one or more cigarettes per week
• Prizes to be for the school rather than for individual classes or pupils
• Wales will not participate in the European prize draw as this offers travel to the winning
class
• Competition materials to make it clear that is acceptable for pupils to encourage others to
enter, but not to force them
• Research to be undertaken to assess the incidence of undue pressure
• Competition materials to make it clear that the competition complements other work on
smoking, but should not replace it
• Individual areas of Wales to opt in to the competition, rather than an all-Wales competition
• Health Promotion Wales to agree with local personnel the mode of contact with schools
• Carbon monoxide testing, as a means of verification, to be decided on locally
• A letter for parents to be included with the competition materials; this to be used at the
discretion of the school.
The revised proposal was sent to all those who attended the meeting, to all District Health
Promotion Managers, appropriate Local Education Authority (LEA) advisory staff and Health
Promotion Commissioners. Subsequently a letter was sent to Directors of Education in those
areas where it was proposed to run the competition.
This consultation period resulted in schools in 15 of the 22 Unitary Authorities being targeted.
In seven of these, this was with the support of both the LEA and Health Authority; and in
eight with the support of the LEA only, although in one case a local NHS Trust also offered
support.
3.2. Planning phase
During Autumn 1997 detailed planning was undertaken, including two videoconferences
with North Wales to clarify local and national roles.
Competition materials were designed:
• Flyers - bilingual, A4 folded into 3. These informed schools about the competition and
invited them to send for the entry pack.
• Entry pack - Bilingual, A4 wallet containing Teachers’ information booklet, two posters,
entry form, five monthly commitment forms, six Freepost envelopes, letter for parents.
• Set of five postcards to be sent to classes monthly to remind them to return their commitment
form.
• Headed notepaper - stating that the competition was being co-ordinated in Wales by Health
37
- --
.. , . . ..... ....
c;.
Promotion Wales with the support of local partners. This has no address on it and could be
used by any of the partners.
• Pin badges saying Smokefree Class or Dosbarth Di-fwg.
A database was set up in Health Promotion Wales which would record the name of the school,
form and form teacher; address; telephone number; number of pupils in the class; number of
pupils entered; and return of commitment forms with number of pupils still participating.
3.3. Recruitment phase
During November 1997, flyers were sent to all schools in the target areas (150 in total). In the
six North Wales Unitary Authorities these letters were sent out by the local Health Promotion
Departments, and in most cases were accompanied, or preceded, by a letter of support from
the LEA. In one Unitary Authority the letter went from an LEA adviser. For all other Unitary
Authorities, Health Promotion Wales mailed direct.
Twelve flyers were sent to each of Headteacher, Head of Year 8 and Head of Personal and
Social Education (PSE). A covering letter informed them who else had received the information.
Classes were asked to return a reply form by l^111 December if they wished'to receive a
competition entry pack.
Competition entry packs were mailed to all classes requesting them during the first week of
the Spring Term (8th - 15th January 1998). A sample pack was also sent to the Head of PSE in
all those schools who had not responded to the flyer. Classes were asked to return their entry
forms to Health Promotion Wales by 26th January 1998.
Over two hundred packs were requested from thirty-seven schools. Classes in thirty-two of
these schools subsequently entered the competition. Classes in eleven schools entered as a
result of receiving the sample entry pack.
The final entry figures were 198 classes from 43 schools, representing 5,066 pupils. This
entry figure equates to one seventh of the Year 8 pupils in Wales, and approximately 22% of
pupils targeted.
3.4. Competition phase
The competition ran from Monday 2nd February 1998 to Friday 26th June 1998. Classes returned
commitment forms on Fridays 27th February, 27th March, 1st May, 29th May and 26th June.
Reminder postcards were sent out one week prior to these dates.
Any class not returning a commitment form within one week of the date was sent a reminder
letter. For the last three months the receipt of the form allowed entry into the prize draw. Any
classes that had not returned forms 3 days prior to the draw received a telephone reminder.
38
I
During February all classes were sent sufficient pin badges for every pupil, in either English
or Welsh.
During March classes were invited to request the name of a Danish school in order to set up
a penpal link. 39 classes responded to this offer.
Prize draws took place on:
2 classes won £500 for their school
2 classes won £750 for their school
2 classes won £1500 for their school
34 classes won £100 for their school
1 class won rucksacks (produced by the German team for one
class in each of the participating countries)
Friday 15th May
Friday 12th June
Friday 10th July
Naomi King of ASH undertook the draws in the presence of at least one independent witness.
to ensure that 75% of the
Prior to the draws the entry figures for each class were ccalculated
-----------------pupils were still participating.
The major prize cheques and rucksacks were presented in school assemblies as soon after the
draw date as could be arranged. The major prize winners were:
£500
£750
£1500
Rucksacks
8C Amman Valley Comprehensive, Ammanford
8B4 Bryn Hafren Comprehensive, Barry
8L Pentrehafod School, Swansea
8Q Olchfa School, Swansea
8YM St Gyres Comprehensive, Penarth
8D1 Caerleon Comprehensive
8A Ysgol Uwchradd Gian Clwyd
3.5. European Comparison
Wales’ performance in the project’s first year of development compares favourably with that
of the other Member States involved. The following table summarises (in ranked order)
participation levels achieved in each country:
Country
No. of participating classes
Finland
2688
46^
Germany
UK- Wales
204
Denmark
145
Italy
141
France
91
Spain
88
39
~
15^
Finland’s performance reflects the fact that the competition was launched there in 1989/90
and has been held each year since that date. It is now an integral part of the school year. Of all
countries participating, Wales achieved the lowest drop-out rate (17%) amongst participants
in the competition. The next lowest drop-out rate was in Italy (33%).
The competition is increasing in profile within other Member States of the European Union
and in the European Commission itself. The Commission’s decision to support the competition
for a further year and to invite more countries to become involved is evidence of this. In
1998/99, Greece, the Netherlands, Austria and Belgium will join the project. Continued
involvement in the project and the role played in developing the project during its first year,
will maintain Wales’ position with the leaders on health promotion programme developments
in Europe.
3.6. Evaluation
Process evaluation was ongoing throughout the competition period, and certain things, e.g.
database and draw preparation, were refined as necessary. Opportunistic discussions were
undertaken with partners and school staff. A meeting was held between Health Promotion
• Wales staff and health promotion officers from North Wales in July 1998 to discuss further
improvements.
More formal evaluation was undertaken by means of pupil and teacher questionnaires and
biochemical validation was carried out in North Wales.
Teacher questionnaire^
Questionnaires were sent to all form teachers whose class had entered the competition, and to
the Head of Year 8 and Head of PSE in all schools that had classes involved. These
questionnaires were sent ten days after the end of the competition, and reminders were sent to
form teachers three day later, with the letter announcing the prize winners.
The questionnaire dealt with teachers perceptions of the competition and their opinion of
pupils involvement, as well as asking for suggestions for improvement.
Results
Responses were received form 91 teachers, of whom 71 were Year 8 form tutors and 18 were
Head of Year 8:
• 83% said the competition encouraged discussion about smoking
• 73% said materials were appealing
• 95% said forms were easy to fill in
• Only 11 % thought it took an undue amount of time
• 87% said Y8 was a good year to target, and only 3% thought it wouldn’t work with Y7
• 90% would encourage classes to enter next year
• 84% thought that most of the pupils were honest
40
1^6
• 77% informed parents about the competition in some way
. 76 teachers noted positive aspects of the competition. Of those, about half mentioned raismg
the profile of non-smoking. Only 12% mentioned the possibility of a prize. Some typical
specific comments were:
The fact that at least once a month the topic of smoking was brought up.
Participation as a group and truthful discussion to help ‘wavering’ smokers.
It highlighted the fact that very few pupils smoke regularly in this age group. It took
away the glamour of smoking.
Raised pupils awareness of smoking. Engendered a ‘team spirit'to avoid it.
Possible improvements centred on the prize structure with a suggestion of more smaller prizes.
11 teachers also mentioned the possibility of providing materials or poster-type competitions
in support of this initiative.
Those who mentioned the CO testing found it positive.
Pupil questionnaires
A random sample of fifty classes was selected from the total number of classes entered in the
week prior to the start of the competition. Eight control classes were randomly selected from
schools in those Unitary Authorities not included in the competition.
. Short, self-completion questionnaires were sent for every pupil in these classes, whether or
not they had entered the competition. The form teacher administered the questionnaires. Al
pupils were supplied with envelopes in which to seal their questionnaire before returning it to
the teacher.
Thirty-five intervention and eight control sets of questionnaires were returned in the first
month of the competition. Those classes that returned the flrs\^est;“meWeTdJutltv)1
further questionnaire in the week following the end of the competition (29 June - 3 July).
Classes who had not replied were contacted by telephone on 15,h-16,h July.
Questionnaires dealt with beliefs and behaviour related to smoking and to bullying. The second
questionnaire also asked about involvement in the competition.
Results
604 pupils returned the second questionnaire:
• 55% of pupils said that the competition helped them to stay smokefree.
. 76% thought the competition was a good idea, with a further 17% having no strong opinion.
Only 6% of pupils agreed with the statement ‘Pupils in the class were less nice to each other
because of the competition’. 65% disagreed or strongly disagreed with this statement.
41
IbI
--- ' -
Biochemical validation
In the North Wales Health Authority area random testing of carbon monoxide levels was
undertaken, using smokelyzers.
Testing occurred in the week immediately following the completion of the March and the
May commitment forms.
s.
Classes were selected randomly by Health Promotion Wales; one class in each school with
less than four classes participating and two classes in schools with a larger entry. Schools
were contacted in the week before the testing to arrange a suitable time.
Testing was carried out by a member of staff from the local health promotion department in
North East Wales; and in North West Wales by a combination of a local health promotion
department staff member and school nurses.
For the March testing, and for the May testing in North Wales, the tester selected six pupils
from the chosen class(es) to be tested. These were one boy and one girl from each of the
front, middle and back of the classroom. For the May test in North Wales, Health Promotion
Wales randomly identified six pupils from each class.
The procedure was explained to the pupils, as was the interpretation of the results. Prior to
testing, pupils were asked to confirm that they were still participating in the competition.
Results
ppm CO
Number of pupils
0
134
1-5
53
6-10
1
>10
2
Total no. tested
190
These results indicate that only two pupils out of 190 were smokers and had therefore not told
the truth on the previous commitment form.
It is the perception of the health promotion officers who undertook the testing that both teachers
and pupils welcomed the testing and valued the verification it provided. Pupils were keen to
volunteer to be tested.
Undertaking the testing was also useful in maintaining contact with the schools and reinforcing
the benefits of involvement in the competition.
42
I 1—
3.7. Recommendations for future competitions in Wales
Subject to amendment on analysis of teacher questionnaires
• Alert schools to the competition earlier in the school year - by a combination of a letter to
the school before the flyers are sent out and local marketing with PSE co-ordinators.
• Send flyers to school nurses in addition to Headteacher, Head of Year 8 and Head of PSE
• Maintain the competition dates as February to March for the coming year, but attempt to
get classes entered by Christmas
• Offer the competition to Year 7 in addition to Year 8
• Keep prizes at 3, 4, and 5 months, but possibly give more lower prizes:
4 x £200 at 3 months; 6 x £300 at 4 months; 4 x £750 and 30 x £100 at 5 months
• Devise a system to ensure a better geographical spread of prize winners
• Keep prizes as school prizes, but encourage the school to spend some of it on the winning
class
• Offer schools the opportunity to participate in the European draw (which will be a trip to
London)
• Provide small momentoes, such as the badges, to all pupils, on more than one occasion
• By means of a box to tick on the entry form, offer schools the opportunity of having their
details on the Internet site so that they may be contacted by other European entrants
• Ask schools at the inquiry stage if they will be willing to participate in research if randomly
• selected
• Leave a clear gap between receipt on entry forms and the start of the competition, so that
more sensitive evaluation can be undertaken
• Make sure that teachers know that the order of names on the commitment form is not
important
• Maintain biochemical validation as a local option
• Ensure that all correspondence sent to schools is copied to local partners
• Ensure that all correspondence sent to form tutors is copied to Head of Year andjlead of
PSE
• Inform schools that commitment form has been received by means of a postcard which
also canies some information about smoking, possibly in a quiz format.
References
1 Young People in Wales: Lifestyle Changes 1986-1996
Health Promotion Wales Technical Report No: 24
2 Vartiainen E., Paavola M., Vertio H. “No Smoking Class” competitions in Finland: their
value in delaying the onset of smoking in adolescence. Health Promotion International,
1996: 3 (11): 189-192.
43
its
APPENDIX
Table 1: Main characteristics of the competition in different countries
Country
Denmark
^inland
France
Germany
Further Remarks
Important Rules_____________ ’rizes_____ ____
Competition was
•Each class has to carry out an • Prizes 1-4: Cash
carried out only in
• Prizes 5-6: T-shirts
activity dealing with tobacco
grade 7(13 year-olds).
and smoking.
• If somebody smokes but promi
ses not to smoke anymore, the
class decides what to do. Regu
lar smoking is not accepted.
Experience in orga
Cash prizes
• Whole class has to remain
nising the competition
smokefree.
since 1989/90
• If a pupil smokes, but promises
not to smoke again, the class
can remain in the competition.
• Regular smoking is not
accepted.
_________
Cash prizes:
• Prizes are graded according to
•No smoker: Prize A
the number of smokers in the
• 1-2 pupils have smoked: •
‘ class.
Prize B
• If more than 5 pupils have
• 3-5 pupils have smoked:
smoked, class drops out.
Prize C_______________
Teachers workshops
Cash prizes
• At least 90% of pupils have to
agree to participate.
• Up to 10% of the pupils are
allowed to smoke.
• Classes are allowed to exceed
the 10% limit once.__________
Italy
Spain
UK
•If.any pupil becomes a regular
smoker, the class drops out.
• In the case of experimental
smoking the class remains in
the competition.
Is' prize: Radio/tape/CDplayer to every pupil
2nd prize: participation in
the international prize draw
• One single episode of smoking •First prize is a day cruise
is acceptable if the class decides • 2nd and 3rd prizes: music
recordings, books
so.
•
Special prize for the
• Regular smoking of any pupil
slogan: CD player______
is noi accepted
• At least 90% of the pupils have • Cash prizes: (rather to
whole school than to indi
to agree to participate.
vidual classes or pupils)
• Class drops out if more than
•
2
third prizes at 3 months
25% of pupils smoke.
• 2 second prizes at 4
• Prizes are graded according to
months
the period of time that the
•
2 first prizes at 6 months
classes participate.
and 30 small cash prizes
• Bullying is grounds for
disqualification.____________
45
Every class had to
make its own “com
petition slogan”. The
best one won an award.
• A consultation exer
cise as a part of the
project development
• Did not take part in
the international
prize draw
• Entry requirements
ensured that no
" bullying appeared
.4
PUBLICATIONS OF MINISTRY OF SOCIAL AFFAIRS AND HEAD rl 1997:22
FINNISH STRATEGY
TO PROMOTE HEALTH
AND NON-SMOKING
AMONG YOUNG PEOPLE
MINISTRY OF SOCIAL AFFAIRS AND HEALTH
Department for Promotion and Prevention
Helsinki 1997
l£s~
PRESENTATION LEAF
Publisher
Ministry of Social Affairs and Health/Finland
Authors (in case of organs: name,
chairman and secretary)
Consensus Development Conference
on Promotion of Non-Smoking Lifestyles
among Young People held 27-28.8.1996
Date
1.7.1997
Art of the publication
Consensus Statement
Principal
Ministry of Social Affairs and Health
Date of appointing the organ
The title of the publication
Finnish Strategy to Promote Health and Non-Smoking among Young People
Parts of the publication
Recommendations
Summary
The Concensus Conference proposed 38 measures to promote healthy and smokefree lifestyles
among young people in Finland. The aim of these measures is to create healthy and smokefree environments for young people, to improve co-operation and communication between
parents, other adults and young people in families, at schools and during their leisure
activities and in this way to promote and to support healthy and non-smoking growth of
young people.
Keywords
Education, health education, health promotion, preventive health policy, schools,
smoking, young people
Other data
Title and number of the series
Total number of pages
Language
ISSN
ISBN
1236-2050
952-000353-3
Price
Confidentiality
English
Distributor
Ministry of Social Affairs
and Health/Finland
Publisher
Ministry of Social Affairs
and Health/Finland
CONTENTS
Introductions
Towards a policy of consensus: reasons and recommendations for actions
Legislative measures
Actions by authorities
Developing professional skills
Actions to support families and parenthood
Actions supporting the work of schools and educational institutions
Actions aimed at leisure time
Other actions
Implementation of the recommendations for action
4
16$
INTRODUCTION
5
8
10
11
13
14
16
18
20
20
Finland is one of the first countries which has
introduced comprehensive legislative and ad
ministrative actions to reduce and prevent smok
ing. In Finland the Tobacco Acts of 1976 and 1995
have been the main elements of the health-ori
ented tobacco policy based on health education,
pricing policy, protection, restrictions and re
search.
The key provisions of the Finnish Tobacco Act
include:
- a total ban on direct and indirect tobacco ad
vertising and sales promotion of tobacco prod
ucts and smoking;
the ban on sales of tobacco to young people
under 18 years;
- a requirement for smokefree air in all public
and business premises, workplaces, child day
care centres and schools, including yards;
- obligatory health warnings and content label
ling on retail packs of tobacco products;
■ the vending machines under continuous supervision, and
the ban to establish smoking rooms in the
buildings in which people under 18 years mainly
stay or which they use.
The proprietors of indoor premises may allow
smoking in a smoking room in so far as no tobac
co smoke can enter those premises where smok
ing is prohibited.
The Finnish smokefree policy has been '
successful. The proportion of daily smokers
been decreasing since the 1960’s. In 1996 22c
Finnish population smoked daily (18% worr
27% men). These figures are the lowest in
rope. However, the situation has not beer
positive among young people. In Finland t
tend to begin smoking earlier than in most Ei
pean countries. In 1995 26% of boys and 24?
girls aged under 18 smoked daily.This is why
need new measures and activities to discour
onset of smoking among young people.
The Finnish Ministry of Social Affairs i
Health initiated the action to prepare a plan
a Finnish strategy to promote health and smo
free lifestyles among young people. In 1996,
expert group was appointed to propose recc
mendations for smokingtfprevention. The m<
bers of the group represented NGOs, child <
care centres, student organizations, medical
perts, schools, communities, the church,
searchers, sports associations, media, and
vertisers. The Ministry of Social Affairs a
Health with co-partners organized a consem
conference in August 1996. Its aim was to ci
cally assess and discuss the 38 recommem
tions prepared and proposed by the consem
group. After a two-day lively discussion by I
500 conference participants the recomment ■
tions were finalized.
Smoking among young people seems to be
related to environmental factors. Smokefree en
vironment and role models play an important role
in onset of smoking. In theirdaily life children and
young people seem to need strong support and
presence of the parents and adults. This may be
one of the most important elements in promot
ing health and smokefree lifestyles among young
people. The active role of the whole society as a
“couch” of smokefree life is also needed.
The recommendations are now in their prac
tical stage. In implementation the actors are
mainly the same which participated in their prep
aration. The idea is to initiate a comprehesive and
interactive process promoting knowledge about
and action for non-smoking at several levels. It
is stressed that the onset of smoking among
young people is in the beginning a psychosocial
problem, not a health problem.
The special network nominated by the Min
istry of Social Affairs and Health will follow and
evaluate the process. In 2000 the network will
organize a follow-up conference on the issue.
Daily smokers (%) aged 14
in 1977-1997 by sex
°/0
30
25
20
15
10
5
0 Lr*
o
vco
o>
co
00
<n
IO
co
o>
00
o>
00
o
▼-
co
0
o>
The Adolescent Health and Lifestyle
Tampere School of Public Health
University of Tampere
Terttu Huttu-Juntunen
Minister of Social Affairs and Health
6
Proportion of daily smokers (%)
aged 15-64 years in 1960-1996 by sex
Consumption of cigarettes
per person aged 15 or over, 1950-1996
/ears
%
60
50
Joys
2000
40' •
>
□ids
30
Males %
1000
■i '
20
Females %
ro
10
0 ■ HI III I HH III H IIIH III III II HHII I I III Hl HH
•o
jy 1997-
H H 5 s s s 8 s H
t-
V-
r-
r-
r-
t-
T-
r-
lllllll IIHII Illi II HU IIIIIIHIIIH
fe S 8 8
oo>o>a>cno>a>c»a>o>oc>o>
»”
1950-94: Wholesale trade purchases and imports.
1995-96: Tobacco products delivered for
taxable consumption.
Statistics Finland.
Tobacco statistics 1996.
0
National Public Health Institute 1996
TOWARDS A POLICY OF CONCENSUS:
REASONSAND RECOMMENDATIONS FOR ACTIONS
Smoking is today the greatest preventable health
problem in Finland and the other industrialized
countries. In Finland, almost all regular smokers
have started smoking before the age of 20, in con
sequence of which the exposure to the detrimen
tal substances of tobacco becomes very high. Two
out of thtee of those who have started smoking at
an early age will catch a tobacco-related disease.
One out of two regular smokers will die premature
ly from a tobacco-related disease. Every fourth of
those who started smoking before the age of 16
will lose his/her capacity for work as a result of a
serious tobacco-related disease priorto the retire
ment age. On a global level, three million people
die every year due to smoking.
If smoking is started before the age of 18, it
will usually result in an addiction continuing into
adulthood. Smoking causes considerable health
problems as early as in childhood and increases
the risk of many serious diseases when grown up.
School-age smokers are more often ill and suf
fer more often from ill health than non-smokers.
At the same time they also suffer more often than
non-smokers from abdominal pains, headaches,
tension, nervousness, insomnia and tiredness.
Smoking among schoolchildren is also associat
ed with other unhealthy lifestyles - early experi
ments with alcohol drinking in order to get drunk
and bad food habits. Almost all young abusers of
medical and narcotic drugs also smoke. Smokers
are on average less successful at school than
non-smokers. Learning how to smoke and how to
roll cigarettes also tends to make it easier to start
8
using cannabis products. The cheapness of rollyour-own tobacco, which is made possible by the
low excise duty, almost tempts people to use it.
Adults, in the same way as young people,
smoke more often the lower their education.
Those with a lower education also smoke in
quantitative terms more than those with a high
er education, and smoking is clearly more usual
among vocational school pupils than among
those attending higher secondary school. As re
gards smokers at vocational schools, they have
usually started smoking at comprehensive
school. Young people’s choices concerning edu
cation often depend on their family background
apart from their success at school.
The differences in smoking among social
groups increased from the end of the 1970’s to
the middle of the 1980’s and have thereafter re
mained unchanged. It can be concluded from the
indirect information concerning social group de
pendence of smoking among young people that
their situation resembles that of the adults.
Therefore it can be assumed that socioeconom
ic differences in morbidity and mortality (e.g. cor
onary diseases and lung cancer) will remain un
changed or even increase in the near future.
Smoking experiments and smoking among
young people increased at the end of the 1980’s,
but in the beginning of the 1990’s their level fell
to that of the beginning of the previous decade.
Young people in Finland start smoking very ear
ly. Here the pattern deviates from the usual West
ern one so that boys usually begin experiment-
ing with smoking at an earlier age than girls. In
1994 52 % of Finnish girls aged 13 and 70 % of
boys of the same age had experimented with
smoking. The corresponding figures for those
aged 15 were 77 % (girls) and 81 % (boys). In Fin
land those aged 15 smoke daily more often than
their peers in the other countries from which sta
tistical data are available.
Smoking among young people is possible be
cause of sufficient pocket money and the re
duced control by the parents: children break
away from the sphere of parental control quite
early. Those young people who start smoking
associate smoking with images of adulthood and
success.
■ Finnish schools are very worried about smok
ing among pupils. Although the statutory restric
tions on smoking have increased since the end
of the 1970’s , there are still problems related to
control. In 1995 every fourth pupil aged 14 and
half of the pupils aged 16 at higher secondary
schools and vocational institutions said that ob• servance of the restrictions on smoking is notsupervised at all in their school. On the other hand,
when pupils said that there is supervision, it was
most often said to be “rather strict” but seldom
“very strict”. In 1995 20 % of Finns aged 14 -16
were daily smokers, and about half of them re
ported to be smoking every day on the school
premises.
ures were agreed upon as a result of the multi
faceted and critical debate at the national discus
sion forum in Jyvaskyla in August 1996. It is a
great challenge to reduce smoking amongyoung
people, and it calls for the contribution of all
parties: homes, schools, non-governmental or
ganizations, business life, media, authorities,
experts and the young themselves. The task is
not an easy one, but we can be hopeful since we
have succeeded in reducing smoking among the
adult population in Finland. It is essential that we
work systematically for several years and initiate
interactive processes promoting knowledge
about and action for non-smoking at several lev
els. The objective of these recommendations is
to make Finnish society understand the problems
relating to smoking among young people, take a
serious attitude towards them and to implement
the proposed action.
These recommendations summarize the pol
icy lines and the means to promote health and
non-smokingamongyoungpeople.These meas
9
LEGISLATIVE MEASURES
Tobacco is a plant containing toxic chemical com
ponents; products made from it would not be
granted a selling licence if they were put on the
market today. Non-smoking is one of the most
significant factors promoting young people’s
health. Support for non-smoking is a means to
prevent many serious illnesses, also abuse of al
cohol and other substances and drugs.
A factor influencing the learning of health
promoting issues, adopting the knowledge,
changes in attitudes and behaviour is the whole
social environment of young people, where the
school plays an important role. Non-smoking
among school staff is a basic factor contributing
to the effect of messages concerning the advan
tages of non-smoking.
Recommendation 1:
........................................................ ...........
■■■"'■
The Ministry of Social Affairs and Health
' should prepare an amendment to the Act on
! Measures to Reduce Smoking according to
; which schools and educational situations
; shall be totally smoke-free.
In spite of the great health hazards involved in
smoking the interest shown by society and poli
ticians in prevention of smoking has not been
sufficient, since smoking among young Finns is
more common compared with the other Europe
an countries. Marketing and sales promotion of
tobacco products is considered as an ordinary
business activity, and the decision-makers are
not willing to interfere in it. Tobacco products,
used as they are meant to, involve a great health
hazard though.
10
Recommendation 2:
The Ministry of Social Affairs .
should prepare an amendment t*
Measures to Reduce Smoking a
which the sanction for a repeate
of the prohibition against sell!
products to young people undei
18 shall be the loss of the right
bacco products.
There is clear and binding evidenc
of the prices of tobacco products ar
power on their consumption: the cc
tobacco products is the more comi
ous the greater amount of cigare
have money to buy. The price is c
affect more children’s and young p<
ing than that of adults. When nicot
is a factor, children and young peo
tain nicotine according to what thf
e.g. by changing over to cheap cig<
arettes which they themselves roll
low taxation of cheap cigarettes <•
tobacco makes it possible for chil(
ments with smoking to develop an a
when their limited purchasing pow
erwise protect them. It is difficult t(
co prices and the tax on tobacco sin«
uct which affects the cost-of-living
Recommendation 3:
The Ministry of Finance should i
ration with the Ministry of Soc
and Health prepare an amendm
Act on Excise Duty on Tobacco i
raise the taxation of tobacco
clearly over the minimum level d
by the European Union and to <
the tax on all tobacco products t
sameamount per consumer unit
factory-made cigarettes.
Recommendation 4:
Health
Acton
lingto
lation
bacco
age of
ell to-
he effect
rebasing
iption of
and serichildren
dered to
’s smokddiction
y to obt afford,
s or cig
present
igarette
; experiion even
uld othe tobac5 a prod-
Tobacco should be excluded from the costof-living index.
The sales and marketing of ten-cigarette packets
have increased remarkably in recent years. Ac
cording to a study, among those aged 14, about
half of those experimenting with their first ciga
rettes and a third of those who had experiment
ed a little more often had last bought a ten-ciga
rette packet. Smoking experiments among young
people are started with the same cigarette
brands as are the most popular among daily
smokers.
Also the easy access to tobacco products is
a factor encouraging young people to initiate and
continue smoking. The mail-order and vending
machine business allowed by the present legis
lation facilitate obtaining tobacco products.
Recommendation 5:
The Ministry of Social Affairs and Health
should prepare an amendment to the Act on
Measures to Reduce Smoking standardiz
ing the size of cigarette packets to 20 ciga
rettes.
Recommendation 6:
laboFfairs
0 the
er to
lucts
lined
mine
if the
tat of
The Ministry of Social Affairs and Health
should prepare an amendment to the Act on
Measures to Reduce Smoking prohibiting
the sales of tobacco products from vending
machines and by mail-order.
Although tobacco advertising is prohibited by
law in Finland, it is conveyed to the country
through foreign media. Finland should not accept
the mixed European practice concerning tobac-
co advertising that reduces the credibility
own legislation. Rescinding the Finnish na
legislation which prohibits tobacco advei
cannot be accepted under any circumstan
Recommendation 7:
For the purpose of protecting young p
pie’s health Finland should impose a t<
ban on tobacco advertising in the EU,«
in particular a ban on tobacco advertis
through sports, culture and other spon<
ing. It must always be possible to hi
stricter legislation at the national le
than that defined in the proposed direct
on ban on tobacco advertising.
ACTIONS BY THE AUTHORIT
The present action to promote young pe<
health is not enough but new resources
ways and a strong commitment to promotf
smoking are needed. The State and the loc
thorities must develop concrete health f
strategies to support non-smoking. Dev
ments in non-smoking among young p«
should be reported in the Public Health R
given by the Council of State to Parliamc
regular intervals.
Adults cannot bring up today’s young p
after the same models as were used in
youth, but adults have to be available
present. A young person shall be acceptec
sensible, conscious and responsible learne
is supported and guided in making choice
solutions concerning his or her own life. 1
grown-ups who are working with young p
must be aware of the significance of theii
example, of the prevailing youth culture ar
health risk involved in smoking. These grow
must also develop their mutual collaborat
promoting health in municipalities and agree on
the general objectives and policies to prevent
smoking among young people.
The bans and restrictions of the Act on Meas
ures to Reduce Smoking are society’s message
that smoking is not considered acceptable. On
the other hand, a weak control of the observance
of the Act can strengthen young people’s idea
that these or other collectively agreed rules of the
game are not meant to be followed.
The present experience indicates that the ban
on the sale of tobacco products to young persons
under 18 has not been implemented as presup
posed in our legislation. .
The enforcement of the ban on sales
products presupposes an active wor
mation between health care, school;
other actors. The municipal health o
inform, support and educate the st<
and kiosks regardingthe enforcemer
on sales and the health criteria of the
The present signs in shops indicatinc
sales and health risks of tobacco proc
up in cooperation with tobacco indi
fulfil the requirements of the legislal
officers should utilize the expertise
governmental organizations working
health in the enforcement of the ban c
in related information.
Recommendation 8:
R^mmendatiopio:
| .}#he Ministry of Social Affairs and Health
! ^^y^S^Haborate with the supervisory
’ autndrities and agencies representing re- !
( tail trade in preparing uniform and clear
I directives on the enforcement apd supervi- j
i sion of the ban on selling tobacco products
I to young persons under 18.
It is widely accepted that carefully planned pur
chase tests directed at all retail sale premises at
regular intervals is the most effective way of su
pervising the observance of the sales ban. The
importance of supervision can be increased by
combiningthe supervision with guidance and in
formation.
—ir“'
—
i glt^Mthdij^fshould supervise tl
■ selling tobacco products furnish th
I premises with signs indicating th
sales of tobacco products to perse
under 18 and the health risks of the
i ucts. Furthermore, the signs shou
young people to be prepared to
! their identity cards.
f The^lftinicipal supervisory authorities
i sfiotiid intensify the observance of the ban
As the restrictions on tobacco adver
increased, the appearance of tobac
has become a more and more impoi
conveying images and arousing ini
package as such advertises the pr
Finnish authorities should prepare
aiming at the sale of tobacco products
packages bearing the same coloi
should also advocate this actively in
Council of the European Union. Visit
, ourful presentation of tobacco produc
I
*
!
:
I
premises, easy access and purchasing
children to buy them. Placing tobacc
clearly on view and demonstration
products weaken the health message
the risks of smoking conveyed by otf
Recomtnendation 9:
..r"
h------ ’
..........
-.... - • ----------
-
on sales of tobacco products to those under 18 by increasing supervision and developing the supervision methods (e.g. test
purchases) in cooperation with the Minis*
try of Social Affairs and Health.
12
)bacco
i inforde and
s must
shops
he ban
ctions.
ban on
drawn
do not
Health
ic nonromote
les and
hose
;ales
n on
, aged
)rodnvite
sent
ig have
rackets
t factor
•st. The
ct. The
!asures
uniform
Finland
Health
md colm sales
:ourage
roducts
f these
cerning
neans.
'• It is possible to increase professional un
standing and skills to reduce smoking am
young people through research and develoi
the action based on it. Research is the basis
point of departure for health promotion, as
as a means to assess the outcome of the m
ures taken. For the time being there is not enc
systematic material to constitute the basis
future research and development.
Recommendation 11:
The Ministry of Social Affairs and Health
and the central organizations of retail trade
should prepare a recommendation with a
view to placing tobacco products on sales
premises out of sight for children.
!
1
Tobacco advertising considerably increases chil
dren’s interest in experiments with smoking. Fur
thermore, some TV programmes show much
smoking. Maybe the most difficult thing to tack
le is the conveyance of tobacco advertising from
abroad e.g. through various sponsored sports
and cultural events. In some cases tobacco in
dustry also tries to influence the illustration of
news and events shown in the media. In spite of
the total ban on tobacco advertising the Finnish
TV channels conveyed in March 1996 about four
hours of tobacco advertising in the context of
sports programmes.
; Tlil^in^g^^IJransport and Communica• tions should start negotiations with representatives of the Finnish mass media in
order to bring about uniform directions and
; policies to prevent the conveyance of ma; terial containing tobacco advertising and
’ promoting smoking. To begin with, the
prevalence of tobacco advertising and
smoking in the media should be studied,
studied.
1
;
;
;
•
j
i
j
Recommendation 13:
i
An expert group appointed by the Ministr
of Social Affairs and Health should asses
the research and development concernin
smoking among young Finns and give
proposal for long-term continued actio
taking into account future needs.
DEVELOPING PROFESSIONA1
SKILLS
In the education of health care personnel srr
ing issues have been outshadowed by the
struction focused on treatment of illnesses. Ii
international study carried out in 42 countrn
was found out that students of medicine v\
astonishingly ignorant of tobacco-related disc
es, and that the curricula lacked informatior
them. In consequence, health care personne
ten neglect to try to persuade people to s
smoking, even though that would be very im]
tant from the point of view of care. This defect
be remedied by means of education. Educais important also in terms of tobacco policy, si
health care personnel’s influence on peop
opinions in health issues is vital.
Recommendation 14:
Recommendation 16:
Institutes of social welfare and health care
studies, polytechnics, faculties of medicine
and other units providing health care edu
cation should develop an education pack
age concerning prevention of smoking, to
bacco-related diseases and withdrawal
methods. The need for such education
should be studied by surveyingthe present
volume of education relating to tobacco.
Employees engaged in social
health care, education, youth v
sports provision should not smolworking hours.
A young person cannot adopt health values in an
environment where health is not valued, where
health messages are in conflict with the prevail
ing patterns of behaviour or where the circum
stances make it difficult to pursue healthy life
habits. Young people observe and adopt health
values from their environment without being con
scious of it and often in such situations that the
grown-ups do not at all understand as being ped
agogic. Non-smoking among child day care work
ers, teachers, social and health care personnel
and their attitude to smoking are significant fac
tors when bringing up children to be non-smok
ers. Therefore non-smoking should be consid
ered as a factor influencingthe appraisal of suit
ability when choosing employees for the abovementioned sectors.
Recommendation 15:
Vocational education for child care, educa
tion, social and health care, youth work and
sports provision should include instruction
in skills and knowledge which promote non
smoking. Those graduated from these insti
tutes should be themselves non-smokers.
14
ACTIONS TO SUPPORT
FAMILIES AND PARENTF
The prerequisites for health-promotir
are created in one’s early childhood. T
tion for a child’s mastery of life, self-€
mental health is laid in the family. Alsc
health habits are determined by the
culture of the family. In connection \
training for parents expecting a chi
should also be trained for parenthood,
child care and upbringing. This so calk
school model shall be followed als
health clinics. At the same time •>
strengthen the parents’ capacity to si
active health-promoting cooperatio
other growth and school environmchild. The public discussion should by
sible means support the parents in
lenging task to bring up their childre
healthy life habits and non-smoking.
The parents function as the first r
of non-smoking for the child, and this rr
be strengthened when people are gr<
parenthood. Maternity and child hea
shall emphasize the idea of a smoke-f
One significant risk factor contributing
ed infections in children is tobacco sm
home. When treating children with re
fections the parents’ attention must b«
this circumstance. The importance 0
own attitude in supporting the child
growth and development, as well as t
tance of mutual interaction as a mee
bringing must be stressed. Health ed
J.
just as important for those who are expecting
ing that will make it possible to help these <
their first child, and smoking parents must be
dren at an early stage.
encouraged to stop smoking. Also parents of the
d
first child starting school need special informa
g
tion and guidance.
Recommendation 21:
Social welfare and health care and the edu
Recommendation 17:
cational system should collaborate i
working up and developing identificatioi
A study of health promotion work done in
ture risk behaviour and exclusion and taki
should be initiated. Its outcome would pro
them into standard use for the purpose 0
vide the basis for an action programme to
prevention.
des
help parents to bring up their children in a
da-
way promoting health.
and
A child always reflects the “health” of its farY
Id’s
ind
and prevention methods to anticipate fu
homes, obstacles to it and its possibilities
growth conditions and living environment,
Recommendation 18:
though the responsibility for bringing up child
shifted to the day care centre, school and oti
ife,
One objective of family training and mater
nity and child health clinics should be to
its’
promote parents’ non-smoking and a
ents always bear the main responsibility. I
Hid
smoke-free home.
nily
nts
and young people has to a greater extent be
tall
Day care centres must give the children the I
Recommendation 19:
:he
sic facilities for adopting non-smoking and o
er health-promoting habits and lifestyles.
os-
Health care centres should provide those
al-
expecting a child and parents of small chil
lue
parents’significance and role is further of cru(
itnportance for the child’s healthy developme
an
:he
groups outside the family, the home and the p
dren an opportunity to take part in with
Recommendation 22:
drawal from tobacco and to get nicotine
del
substitution therapy free of charge.
Within child care non-smoking should be
ust
promoted by means of play and various
Ito
activities. The facilities of the cfey care per
ics
Recommendation 20:
sonnel to promote non-smoking among
Measuring the carbon monoxide expired by
supplementary training.
ne.
at-
families should be increased by means of
:he
parents should be introduced as a tool and
in
as a part of the ordinary health examina
tions at maternity clinics.
to
ts’
A considerable risk factor with a view to ch
dren’s smoking and other development is aft(
hy
or-
Behaviour that preindicates future smoking and
noons spent without grown-up control. Childn
are influenced by circumstances that are beyoi
ip-
other risk behaviour and exclusion can be ob
the parents’ control. In Finland children are e
1 is
served as early as in small children, and detect-
pected to grow functionally independent earli
1
than their psychosocial development would al
low. In cases where the parents are in full-time
employment schoolchildren should have an or
ganized programme during afternoons - in the
same way as in many other countries. The pro
gramme should be planned so as to contain rec
reational and stimulating activities for children
under the care of grown-ups.
its prerequisites, which is supported by the so
cial environment Guided by it young people can
learn how to master health issues and make so
lutions concerning health. Control of social pres
sures undermining health can be promoted in
education and upbringingby givingspecial atten
tion to creating a positive picture of oneself and
to strengthening one’s self-esteem. Instruction in
social skills (communication, expressing oneself,
social intercourse) shall be an integral part of the
education and upbringing.
Recommendation 23:
There should be organized afternoon activi
ties for schoolchildren on school premises
| or elsewhere after school hours. They could
; be organized by e.g. schools, parishes, !
municipal youth and sports services, and •
other hobby organisations.
Recommendation 24:
; ‘‘Ari action pfogrSnrrne for non-smoking )
|
.!
i
i
J
•
ACTIONS SUPPORTING THE
WORK OF SCHOOLS AND
EDUCATIONAL INSTITUTIONS
(
The health behaviour adopted in youth is often
retained throughout the life, and thus health
should be a quality factor in the educational sys
tem at its all levels. Basic knowledge and skills
relating to health shall be integrated into all com
prehensive and vocational education. With the
reformed curricula the share of health education
has been reduced considerably in schools and
educational institutions. Their curricula and
teaching methods shall promote and strengthen
non-smoking, which is integrated into the in
struction even from the lower level of the com
prehensive school.
A young person seeks situations according to
what he or she has learned to value. Health pro
motion does not consist of teaching individual
facts or learning things by heart, but young peo
ple must get a positive overall view of health and
16
should be drawn up for each school and
educational institution in cooperation with
school and student health care. The programme should be a registered strategy
agreed upon jointly - also with the pupils
contributing. It should manifest the attitude towards smoking, measures to prevent from onset of smoking, policies in different situations, continuous monitoring
and evaluation.
;
(
:
j
!
\
j
Recommendation 25:
.... .......................
/ ? Health education in schools and educa-
|
i
!
!
I
tional institution^should be strengthened,
and prevention of smoking should be
linked to young people’s mastery of life and
the school’s teaching of manners. The Na- ■
tional Board of Education should in col- !
I
i
;
1
j
I
laboration with experts develop opera- '
tional models within the curricula of ■
schools and educational institutions. These ■
models should include means of which all ■
young people can be taught matters relat- ’
ing to prevention of smoking
j
Although promotion of non-smoking and health
v
Young people often say that they are interested
concerns the whole school or educational insti- , in stopping smoking and talk about
- - - „
-—
^.t numerous
tution, teachers need many-sided help from pro
attempts to do so, but find the nicotine addiction
fessionals in different fields. In this context rep
problematic. Besides the addiction, also the re
resentatives of school and student health care
warding and strengthening factors related to
play the most central role.
smoking guarantee in the end that experiments
School and student health care are part of the
with smoking often lead to lifelong smoking.
statutory public health work of a municipality.
More research findings are needed concerning
Their goal is to promote a healthy growth and
how to make young people stop smoking, its
development of pupils and students as well as
methods and outcome.
the health of the whole community. Such action
requires from the school health personnel be
sides an active contribution, initiatives and con
Recorhftlendatiofi-27:
stant presence also cooperation with the school
and educational community.
( Hfealth centrq^hould organize activities to j
With the economic recession the resources of
support those pupils/students who want to
school and student health care have decreased,
stop smoking (e.g. withdrawal groups).
since the time spent by public health nurses and
Young people’s knowledge of the risks of !
physicians on it has been reduced in recent
smoking as well as confidential discusyears. The recommendation is that there should
sions about smoking should be promoted
be a maximum of 750 pupils/ students per one
. e.g. by means of measuring expired carbon
public health nurse employed on a full-time bamonoxide as part of ordinary health examisis in school or student health care. If the public
; nations.
health nurse is responsible for several schools or
institutions, the number of pupils/students
should be lower, since time has to be reserved for
According to Finnish studies teachers are in need
contribution according to school or educational
of more information in almost all areas of health
institution.
education: targets, contents, methods and in
general issues relating to young people’s health
behaviour and smoking habits. The professional
Reco^e^tf^:
facilities of teachers shall include the ability to
2^^—-------------- *-------------------- ------ x
discuss health issues with their pupils/students.
Healthcare ceptfe's should guarantee the j
public health nurses and doctors working
in school and student health care enough
Recommendation 28:
. time for taking care of the pupils’/students’
-... --------- ......... —---------------health and for promotion of non-smoking in j
i teachers ahd/schbol and student health I
collaboration with the other school and
personnel should be provided joint suppleeducational community. The facilities of i
- mentary training for the purpose of develI school and student health care should be ■
i oping the content and working methods of
situated in connection with the school or
health promotion, school and student !
educational institution.
i
! health care and curricula for health edu- ;
[ cation.
17
Today’s society poses young people more and
more challenges relating to adulthood. Every
young person matures individually gathering ide
as, advice, influences etc. from various quarters.
Also healthy life habits have different values and
emphases in different individuals’ lives. The
starting point for health education promoting
non-smoking shall be the young person, his or
her life situation and living environment. Studies
have shown that the best results in promoting
non-smoking among young people have been
achieved when a programme at population level
directed to both young people and adults has
been integrated into health education pro
grammes of schools and educational institutions.
Rec^e^ti0n^:
--------------------- —
-th^ed-ucatiohabsystem, social welfare,
health care, temperance work and non-gov
ernmental organizations should collabo
rate in developing and implementing
health education programmes aimed at
non-smoking for young people and adults.
They should take into account expert rec
ommendations, local conditions, young
people’s needs, lifestyles and cultures.
Follow-up is an efficient-means to influence non
smoking and other lifestyles. In addition to the
national follow-up an efficient prevention re
quires intense and well-timed local and school
based monitoring, when the action can be direct
ed according to problems and their impact can be
followed.
Recommendation 30:
■
.....................
Non-smoking among young people should
j be fplfowed by means of a national system
which produces sufficiently quickly and fre
quently information about the prevalence
of smoking per school, educational institu
tion and municipality.
ACTIONS AIMED AT LEISURE TIME
Children remain primarily in the sphere of influ
ence of the parents until the age of ten years.
After that leisure-time activities, friends, idols
and other reference groups become very influen
tial. Young people taking part in organized group
activities use according to studies intoxicating
substances to a minor extent than other young
people.
Being together with other young people, lei
sure time interests, habits and hobbies consid
erably mould the lifestyles of young people and
the culture formed by them. An adult participant
must accept that young people themselves are
the real experts in youth culture. Influential indi
viduals play an important role in youth groups.
It would be important to seek out the local opin
ion-leaders among the young and to motivate
them to maintain health-supporting models of
action.
Information is necessary for making choices
supporting health. However, in particular in pu
berty smoking can be fascinating because it can
be seen as a game with risks and can channel
young people’s defiance towards authority.
Therefore it is important to organize various
kinds of stimulating activities for young people.
Society must offer children and young people
various kinds of leisure time activities. The State
and the local authorities shall increase their fi
nancial support to children’s and young people’s
school clubs and leisure-time activities. Further-
18
{
more, they must seek new flexible solutions to
ensure an efficient use of new and existing
premises for such activities.
In Finland more than 350,000 children and
young people aged 3 -18 participate annually for
three months in organized sports club activities.
It is possible to lay foundation for health-promot
ing choices even in such a short time. Hobby or
ganizations should develop their activities so as
to better promote healthy life habits and under
line non-smoking as one basic principle in their
action.
According to a sports study those children
and young people who are not participating at
the moment are also interested in sports club
activities. If sports and leisure time organizations
working with young people would have enough
resources they could double their number of
members.
Non-smoking shall be extended to all levels
of young people’s leisure-time and to their circle
of friends. Since coaches and hobby instructors
serve as models for children and young people
their non-smoking should be promoted. Itshould
be stressed within the framework of their train
ing that it is not recommended that instructors
and children’s parents smoke in connection with
hobby activities - neither indoors nor outdoors.
The premises and the surrounding area should
be totally smoke-free. The State, local authorities
and parishes should aim at making the premis
es and outdoor facilities owned by them smokefree.
Confirmation classes, in particular camp
classes have become a rite of becoming adult.
Issues relating to smoking have however caused
much trouble in the youth work of parishes and
for instance in confirmation classes. The teach
ers in confirmation classes have not given much
attention to matters that are essential for non
smoking and other health matters for young peo
ple. Parishes and churches should assume more
responsibility for non-smoking and healthy life
styles among young people.
Recommendation 31:
The State and the local authorities should
make it possible for sports and other hobby i
organizations to provide a greater selection 1
of health-promoting leisure-time activities
on children’s and young people’s condi
tions.
Recommendation 32:
:
\
!
One condition for granting financial support by the State and municipalities to
hobby and sports organizations should be
promotion of young people’s health and
non-smoking.
Recommendation^:
------ ------------ --------------- ------
The chibrches an^|arishes should specify j
thgir targets regarding heaith promotion |
j and promotion of non-smoking in confirma- 1
i tion classes and other activities targeted to
young people.
Recommendation 34:
the State, the local authorities and par
ishes should prohibit smoking in outdoor
facilities and sports grounds possessed
and administered by them.
Recommendation 35:
Tobacco products should not be sold in ca
fes or kiosks in connection with hobby fa
cilities.
19
OTHER ACTIONS
As regards those doing their national service the
attitude of foremen towards smoking and group
pressure have traditionally favoured smoking.
The time in military service and its atmosphere
should support non-smoking and good health.
___ _________ -
: The defenc^Fprc^should designate non; smo^fftg and health promotion as one impdrtant educational target.
I
A
IMPLEMENTATION OF
THE RECOMMENDATIONS
FOR ACTION
pi
is
The consensus panel proposes an immediate im
plementation of these recommendations. Fur
thermore, it proposes thatThe Ministry of Social
Affairsand Health appoint, fora minimum of five
years, a steering group for the implementation of
the recommendations to monitor and assess the
action taken.
is
L >
Rec^neiMtri
Z®----------- -------- ,v
‘ The
Action according to the recommendations put
forth above needs to be supported by systemat
ic nation-wide information over several years. It
is known that repeated messages in mass media
can strengthen the health education takingplace
in the field and add to its weight.
[iiiistifcof-Sdaal Affairs and Health
□ see to it that a follow-up meeting
will be organized after three years, as well
i as draw up a report concerning the imple‘ mentation of the proposed action.
;
;
j
'
mendation'37:
' Therj greaSeed for long-term informa-
■
__ __ .. .
.^i^m favoiir of non-smoking
in Ii
.... 9 society’ Finnish society.
>*■
•<
(
16 Smoking Habits
The factors which encourage young persons to start smoking have
been extensively studied in the West. Parents, and older siblings who
smoke, often induce youngsters to imitate them. Peer pressure is one
of the most important reasons for adolescents taking to cigarettes. On
an average, boys in the West begin smoking at twelve or thirteen.
With approaching adolescence, they feel that smoking will make them
appear more mature, tough and sophisticated. Smoking is found to be
more prevalent among the lower socioeconomic classes, poor academic
performers, and traumatised adolescents. About ninety'per cent of
addicts in the West are reported to have begun smoking as teenagers.
The percentage of smokers among college graduates is less than that
of high school graduates, which, in turn, is less than that of dropouts.
Some youngsters start smoking out of sheer curiosity. Thus, social
factors, particularly the environment, play a major role in inducing
• people to smoke.
For a beginner, the first cigarette, causes considerable irritation,
nausea and unease. About thirty per cent feel sick after their first
cigarette; only 20 per cent report to have enjoyed it. Persistent smoking
increases tolerance, causing people to enjoy smoking without feeling
nauseous. They find that smoking exhilarates them. The action of
nicotine is very rapid. Once inhaled, nicotine is absorbed rapidly into
the bloodstream where it moves to the brain and activates the pleasure
centres. However, nicotine is metabolised very rapidly, so that within
twenty to thirty minutes, the levels of nicotine in the brain and tissues
fall. The smoker lights up another cigarette just to maintain high levels
of nicotine in his brain and blood, and extend the feeling of euphoria.
It is in this manner that most people become addicts.
People vary in their attitudes and habits when it comes to smoking.
Confirmed non-smokers, will not smoke even in company. Occasional
smokers, are those who are not addicts, but who smoke once in a
Smoking Habits
81
while just to keep company. Light smokers restrict themselves to five
or six cigarettes a day. Moderate smokers habitually smoke 10-25
cigarettes per day. Finally, there are the heavy smokers or chain
smokers, who smoke anywhere from twenty-five to forty cigarettes a
day; and are addicted to cigarettes. The moderate or heavy smoker is
likely to suffer from withdrawal effects if he quits smoking. People
begin smoking just for pleasure but will later smoke to avoid suffering
from withdrawal symptoms. The factors responsible for a person to
continue smoking are chiefly pharmacological, and are different from
those responsible for inducing a person to smoke. For most drug
addicts, heroin or opiates give only a short period of enjoyment, for a
fortnight or a month at the beginning. The addicts then have to continue
with the drugs, just to stave off the withdrawal effects. The heavy
smoker is only slightly better off than the drug addict.
Smoking becomes a regular habit with many smokers. They
automatically smoke a constant number of cigarettes at particular times
during the day or week. In the West, most people smoke anywhere
between twenty to forty cigarettes a day. In India, however, the average
smoker is limited by his income, and consumes far less than twenty
cigarettes a day.
There are differences in the way men and women smoke. Women
take more frequent puffs of smaller volumes. The amount of nicotine ’
obtained from a cigarette relative to the amount of tar, depends on the
puffing pattern and shape. Women obtain a higher nicotine to tar ratio
from each cigarette, compared to men.
Smokers alter their pattern of smoking and number of cigarettes
according to their needs, and the circumstances under which they
smoke. They subconsciously adjust their nicotine intake to the optimum.
Smoking in company may improve the cohesiveness of social groups.
When in company the smoker is relaxed, and takes in slow but deep
puffs, to achieve tranquillity. When smokers have to concentrate on a
demanding job and stay alert, their nicotine intake is limited to a
stimulatory effect. When the addict is under stress or is agitated, he
smokes many cigarettes in quick succession, taking more frequent
puffs and inhaling the smoke deeply. This increases the tissue levels
of nicotine which now acts as a depressant, suppressing anger, anxiety,
and other such unpleasant feelings. Smoking alters (attenuates) the ,
physiological and psychological response to stress. Thus, by
subconsciously manipulating the puffs and nicotine intake, the addict
is able to use smoking as a psychological tool. It stimulates him, when
he is tired, helps him stay alert and aroused in a challenging task; and
soothes him when he is agitated or stressed.
....... r
. - ..>
g2
Tobacco and Areca Nut
Unfortunately, the pleasures of smoking are short-lived, limited to
the duration of the smoke. The long-term consequences of smoking,
however, are serious and harmful. Habitual smoking leads to respiratory
diseases’, like chronic bronchitis and emphysema, cardiovascular
diseases, as well as cancers at different sites, of which the most
prominent is lung cancer. Addicts are reluctant to stop because while
the rewards of smoking are immediate, the harmful effects of smoking
are slow and appear only after many years. Besides, not all smokers
suffer from the ill-effects of smoking. For example, only about 10-15
per cent of smokers get lung cancer. The fact that smoking related
diseases take a long time to manifest and that not all smokers are
affected, allow addicts to continue smoking, in the fond hope that
they will not be affected. Thanks to the persistent, intense anti-smoking
campaign in the West supported by clear, unequivocal medical evidence,
about 75 per cent of smokers now admit, although half-heartedly that,
cigarette smoking is very injurious to health.
Despite accepting the fact that smoking can lead to various terminal
diseases, people continue smoking for various reasons. For one, they
overestimate their own chances of survival, and underestimate the
risks of smoking. Many of them have misconceptions about the benefits
of smoking, the relative risks of smoking, and of the prognosis of
smoking-related"diseases. Some smokers value the psychological effects
of smoking highly. They are also sceptical of anti-smoking campaings,
and the information on the effects of smoking on one s health. But
there are smokers who genuinely believe that smoking is very bad for
health. Many have tried to quit smoking but only a few succeed, because
of the addictive nature of nicotine. Only one of four smokers trying to
quit, succeeds in doing so.
In course of time, addicts begin experiencing some of the unpleasant
effects of smoking. These include coughs, dyspnea, sore throats,
respiratory infections, symptoms of peptic ulcer, oesophagitis, angina,
dental and gum diseases, and so on. It is then that they realise, that
they are not immune to the long-term effects of smoking, and start
thinking about quitting. When some of these symptoms become severe
they feel the need to quit smoking. Many may attempt to quit but very
few succeed. The craving for cigarettes, and the withdrawal symptoms
following abstinence, compel them to go back to smoking unless they
have good self-control.
Several strategies have been devised to help addicts quit smoking.
These include counselling by the family physician, treatment of
withdrawal effects with drugs, particularly nicotine chewing gum
behaviour therapy hypnosis, and so on. A number of smoking clinics
i*7
J
Smoking Habits
S3
have now opened in the West, to help people quit smoking. Counselling
by physicians helps tremendously. It is enough if the physician spends
three to five minutes with the smoker, patiently explaining to him the
long-term benefits of quitting - better health and greater longevity.
The quitting rate is found to be double when the physician takes a
personal interest in helping an addict quit smoking. The family
physician’s role includes: boosting the smoker’s resolve to quit, helping
the smoker overcome his withdrawal syndrome by prescribing suitable
drugs, particularly nicotine chewing gum, encouraging the smoker to
try again, if he relapses. Counselling by the family physician is also
found to be cost-effective.
Nicotine chewing gum
The main incentive in smoking is the consumption of nicotine, and
the major impediment for quitting is the withdrawal syndrome, brought
about by nicotine deficiency. Hence, it would be logical to attempt
nicotine administration as an alternative to smoking. Initially, nicotine
was administered orally in the form of nicotine tartarate tablets and
found to be completely ineffective, since the blood level was too low.
Nicotine chewing gum has been found to be far more satisfactory and
is widely used now.
Nicotine chewing gum is a resin containing 2 mg of nicotine and a
bicarbonate buffer. A spicy flavour masks the taste and irritating
sensation of nicotine. The bicarbonate buffer provides an alkaline
medium, allowing for greater absorption of nicotine. The gum should
be chewed very slowly, for over twenty to thirty minutes so that the
nicotine is gradually released and completely absorbed through the
buccal mucosa into the bloodstream. The blood level of nicotine
attained is about a third to half of that produced by smoking cigarettes.
The withdrawal symptoms are considerably reduced, though not
completely eliminated. Nicotine gum is particularly useful for those
smokers who had withdrawal symptoms earlier, those who smoke
within thirty minutes of waking up and those who smoke even when
they are sick. There are several reports that nicotine gum helps a
!
person abstain from cigarettes.
Nicotine guru however, has some minor side-effects related to
chewing and to the influence of nicotine on the gastrointestinal system.
It can cause irritation in the mouth, sore jaws, sore throat, heartburn,
dyspepsia and" hiccups. Dental appliances such as bridges and caps
can occasionally loosen or deteriorate. A few patients also experience
palpitations.
84
Tobacco and Areca Nut
Nicotine gum should be used correctly to derive maximum benefit
and minimise potential unpleasant side-effects. Because it is meant
only to relieve withdrawal effects, the gum has to be regularly used,
only after the patient has stopped smoking. It is imperative that the
patient chews the gum slowly, because vigorous chewing will result
in nicotine being released too quickly, and this irritates the mouth.
Excess nicotine is swallowed, as its absorption through the buccal
mucosa is slow. As it passes through the gastrointestinal tract, it causes
hiccups, heartburn, belching, nausea, and dyspepsia. It is primarily
metabolised and inactivated in the liver, and very little reaches the
bloodstream to produce any psychological effect. A smoker trying to
quit,.should use this gum for at least three months and chew it as soon
as she feels a desire to smoke. Many people stop using nicotine gum
as soon as they feel confident that they can do without it. A few
become addicted to it and use it for as long as one year.
The use of nicotine gum is contraindicated during pregnancy and
in cases of recent myocardial infarction, and life-threatening arrhythmias.
Nicotine gum may aggravate coronary disease, peptic ulcers, esophagitis
and peripheral vascular diseases. Hence, care should be exercised in
prescribing it to the patient.
Other drugs: Many other drugs have been tried to relieve withdrawal
effects but have not been of much use. These include lobeline and
tranquillisers like diazepam. The opiate antagonist naloxane is very
effective but the effect does not last long. Chloridine, an anti
hypertensive drug and an alpha-adrenergic antagonist relieves a number
of acute withdrawal effects in heavy smokers. A dosage of 0.15-0.30
mg of chloridine per day has been found to. benefit heavy smokers
receiving behavioural therapy. However, its long-term effects are not
known.
/
Aversion therapy: Two forms of aversion therapy are being practised,
both of which are unpleasant. In one, the addict receives a mild electric
shock, whenever he tries to light or pick up a cigarette, or even when
he expresses a desire to smoke. In the other, the addict is made to
smoke rapidly, about one puff in six seconds, a rate much faster than
what she is accustomed to. Both these forms of treatment induce a
strong dislike for smoking in the addict. The second method is said to
have a success rate of 60 per cent.
Hypnosis: Hypnosis is one of the most popular methods to stop
addicts from smoking. It is also found to be very effective..This method
will be successful only under certain conditions:
□ The patient should be strongly motivated to give up smoking.
/»7
Smoking Habits
□
□
35
The therapy should be individualised, taking into consideration
the particular patient’s mental makeup.
The treatment should involve a number of sessions and regular
follow-up.
Acupuncture: Acupuncture, as a method for quitting smoking, has
not been studied fully. It has been claimed that acupuncture produces
an immediate, strong dislike for the taste and smell of tobacco. This
claim, however, needs confirmation and thorough investigation.
Smoking clinics: A number of smoking clinics exist in the West to
help addicts give up smoking. Besides educating them about the evils
of smoking and techniques to quit the habit, they also offer a wide
range of treatment like counselling (psychiatric treatment), hypnosis,
group therapy and ‘programmed smoking’. They advise addicts on
using nicotine chewing gum correctly. Smokers derive some benefit
from these clinics but the success rates is only a moderate (about 12 to
28 per cent).
Relapse: Most of the cessation methods practised, initially cause a
substantial decrease or even an outright elimination of smoking. But
this success is very short-lived. Relapse is the most important problem
with smoking. There is a steep decline in the number of non-smokers,
so that by the end of three months, only about 35 per cent remain
non-smokers, and at the end of six months, only 25 per cent. After this
period, the number of non-smokers reverting to smoking is less, so
that at the end of one year, about 20 per cent remain non-smokers.
Generally, they continue as non-smokers so that the true, success rate
is about 20 per cent.
Men are more successful in quitting smoking than women. This
may be because men and women smoke for different reasons. While
most men smoke for relaxation, and as a pastime, women smoke
generally start smoking to soothe themselves, to attenuate their anger
or anxiety and decrease their stress. Smoking that is started in order to
provide relief from stress, is more difficult to quit.
Surveys conducted also reveal that people who have not had much
exposure to cigarette smoke, find it easier to quit. These include light
smokers, those who have been smoking only for a short time, and
those who do not inhale smoke from a cigarette. Extroverts and people
with better education, are also found to be more successful in quitting.
Will power and self-control are absolutely necessary for a person to
quit smoking. A majority of those who have successfully quit smoking,
have accomplished it through self-control alone.
17 The Rise and Fall of
the Cigarette in the West
The rise of the cigarette
The cigarette originated in Central or North America during the
nineteenth century. There is no record of who invented it, or whether
it evolved in the course of time. The cigarette is now smoked by all
races in all the countries of the world. Europeans were introduced to
the cigarette during the Crimean War, (1856-1858). The automatic
cigarette making machine which was invented in 1853, made cigarettes
easily available at very low cost. Very soon, it replaced the cigar and
the pipe as the most convenient form of smoking. At about the same
time, many governments enacted legislation prohibiting tobacco
chewers from spitting in public areas. Tobacco addicts took to cigarette
smoking instead. World War I (1914-1918) provided a very great
impetus for the spread of cigarettes. The soldiers took to smoking to
relax, and to break the monotony while waiting at the battlefront.
Smoking among women was socially unacceptable until World War I,
when women’s rights activists began smoking in an attempt to campaign
for equality with men. By 1950, smoking became popular among both
men and women in the West. Cigarette smoking became widespread.
People smoked for various reasons - for relaxation, to stimulate
themselves and remain alert at work, to tone down their anger and to
soothe themselves when depressed.
Discovery of the harmful effects of cigarettes
By the close of the nineteeth century, people became dimly aware
that smoking could cause respiratory disorders. In 1938, Professor
Pearl of the Johns Hopkins Institute provided convincing statistical
evidence that cigarettes could reduce a person’s longevity.
I ct>)
The Rise and Fall of the Cigarette in the West
87
The announcement came as an eye-opener, showing people that
cigarette smoking may not be as beneficial as they thought it was.
This had two important consequences. First, a thorough analysis of
the chemical constituents of cigarette smoke and their biological effects
was undertaken. This revealed that cigarette smoke contains numerous
harmful chemicals - carbon monoxide, which interferes with oxygen
transport and contributes to ischemic heart disease; hydrogen cyanide,
a potent cilia poison leading to bronchitis; nicotine, which increases
pulse rate and heart rate, and contributes to coronary heart disease; a
wide range of carcinogens, cocarcinogens, and tumour promoters
including the volatile N-nitrosamines, non-volatile tobacco-specific
nitrosamines, the potent polycyclic aromatic hydrocarbons, and small
amounts of the radioactive polonium-210. Simultaneously, large-scale
epidemiological investigations on the health effects of smoking were
carried out, involving a number of case-control and prospective studies.
The results revealed that smoking can cause cancers in various parts
of the body such as the lungs, mouth, larynx, pharynx, esophagus,
pancreas, kidney and bladder. Smoking can also give rise to some
non-fatal but very distressing diseases like peripheral vascular disease,
cataract, hip fracture and periodontal disease. Smoking during
pregnancy can harm the fetus. The fetus is also succeptible to
spontaneous abortion, ectopic pregnancy, limb reduction defects, low
birth weight, stillbirth and neonatal death. The first report on Smoking
and Health by the Royal College of Physicians, London in 1962 and
the U.S. Surgeon-General’s Report in 1964, clearly brought out these
harmful effects of smoking. They were confirmed in subsequent reports
of the U.S. -Surgeon-General. Passive smoking, particularly in poorly,
ventilated rooms and confined spaces, was also found to be very
^injurious. These reports concluded that a fifth of all deaths in these
countries were due to smoking alone, an enormous loss of life, which
is strictly preventable.
Restrictions on cigarette smoking
These revealations on the deleterious effects of smoking had a
powerful impact on the public, the media, the government as well as
the cigarette manufacturing companies. As it could not be banned
outright in any free society, governments took a wide range of measures
to curb smoking. Excise duty on tobacco and cigarettes was raised. It
was found that a tax rise of 10 per cent resulted in only a one per cent
decrease in the number of Smokers. Smoking in public places such as
theatres, cinemas, churches and offices was banned. Open advertising
and promotion of cigarettes and other tobacco products were forbidden
V
Ufa.--—.:
88
Tobacco and Areca Nut
on television and restricted in other media. The government also made
it compulsory to mention on every cigaratte packet, the public health
warning "cigarette smoking is very injuries to health’. Smokers were
helped in their attempts to quit smoking by increasing the number of
Smoking withdrawal clinics, and subsidising anti-smoking aids and
anti-smoking campaigns.
Filter cigarettes
Cigarette manufacturing companies responded to the increased
awareness of smoking among the public, by introducing well-ventilated,
filter* cigarettes covered with perforated paper. This helped to reduce
the levels of tar, carbon monoxide, and other toxic constituents of
cigarette smoke. By using suitable blends of tobacco and changing
their manufacturing patterns, the tar and nicotine contents of cigarettes
have been progressively reduced to 10-15 mg tar and 1.3-1.5 mg
nicotine per cigarette. This is found to be the minimum acceptable
level of nicotine, for smokers. Low-tar, low-nicotine cigarettes yielding
just 10 mg tar and 1 mg nicotine, are also available. Some governments
also stipulate that the tar and nicotine yields of cigarettes should also
be displayed on the cigarette packet. Smoking low-tar, low-nicotine
filter cigarettes substantially reduces the incidence of lung cancer.
Compensatory smoking
When low-tar, low-nicotine filter cigarettes were introduced, the smoker
adopted various strategies to compensate for the lower nicotine yield
of cigarettes, and to get the usual amount of nicotines she was
accustomed to. She increased the number of cigarettes smoked, and
the number of puffs taken from each cigarette. In such cigarettes, a
larger volume of smoke is taken from each puff, and inhaled more
deeply. The cigarettes are also smoked to a shorter butt-length. By
adopting all these measures, the smoker was able to compensate for
nearly two-thirds of the nicotine decrease due to low-tar, low-nicotine
cigarettes. A 35 per cent reduction in nicotine resulted in an 18 per
cent increase in the number of cigarettes smoked. Despite this, however,
low-tar, low-nicotine cigarettes helped in substantially lowering the
incidence of lung cancer. But the risk still remains; there is no such
thing as a safe cigarette.
Decline in smoking among men and women
Following the reports in the early 1960s of the Royal College of
Physicians, U.K. and the Surgeon-General, U.S.A, the media in these
countries began carrying out intense anti-smoking campaigns very
The Rise and Fall of the Cigarette in the West
I
i
•I
89
effectively. The proportion of men smoking started declining first.
The percentage of Americans smoking decreased from 64 per cent in
the 1950s to about 31 per cent in 1990. The decrease in the consumption
of cigarettes among men in the U.K. fell from about 98 billion in 1986
to 91 billion pieces in 1992/93. Because of a lag period of twenty to
thirty years between smoking and the onset of lung cancer, the decline
in the incidence of lung cancer among men came much later. The
incidence of lung cancer among men steadily increased for a number
of years, from 20 per 100,000 persons in 1950 to 70 per 100,000 in
1975, stabilised to 75 per 100,000 in 1985, then began decreasing.
Women started smoking later; and the proportion of women smoking
steadily increased, even after men had started quitting. The decline in
smoking among women occurred only recently. The incidence of lung
cancer among women in U.S.A, has been steadily increasing from 5
per 100,000 persons to 25 per 100,000 from I960 to 1985; and has
started stabilising only recently. The second half of the twentieth century
thus witnessed a steady decrease in consumption of cigarettes in
Western Europe and the United States.
According to the latest reports from the U.S.A. (March 1999), smoking
is no longer a socially acceptable practice. Cigarette smoking is
progressively declining and may soon become completely extinct in
the U.S.A.. In Britain, the medical profession gave up smoking first.
Medical students no longer smoke. Some Scandinavian countries are
planning to have a completely smoke-free generation.
Dumping of cigarettes in third world countries
The manufacture and marketing of cigarettes is controlled by about
seven multinational companies, based mainly in the U.S.A, and U.K.
On finding that their markets have shrunk in the developed countries,
these companies have started dumping cigarettes on the third world
countries in Asia, Africa and South America. Through aggressive
marketing tactics, they have already established themselves in most of
the countries and started making huge profits. Though smoking inside
the U.S.A, is actively discouraged, the production of tobacco in the
U.S.A, has actually increased from about 600,000 to 700,000 tons per
year between 1985 and 1994. So also the manufacture of cigarettes.
Cigarette smoking has been on the rise in third world countries even
as it is decreasing in Western Europe and the United States. The opening
decades of the twenty-first century will witness a very rapid increase
in lung cancer, almost to epidemic proportions, in the developing
countries. Hopefully, this may be followed by a decline in the rate of
cigarette consumption and lung cancer.
!•
19^
18 Global Efforts at
Tobacco Control
Medical and economic impact of tobacco use
It is now accepted all over the world that smoking is the srngle major
avoidable cause of disease, debility and death. About three mill on
ry year, out of
people in the world die of tobacco-related diseases every
the eleven million people suffering from them.
Ilsine tobacco products also creates economic losses, tor tne
consumer government and society. The diagnosis and treatment of
these diseases, particularly cancer, are very
-
if
Be
u™8 cigarettes carelessly can cause fires, and cigarette smoke pollutes
the atmosphere.
COMPOSITE PROGRAMME FOR TOBACCO CONTROL
in the early 1960s, the discovery of a close link between cigarette
smoking lung cancer and various other diseases, brought about public
concern The media and the governments, were forced to adopt several
measures to control cigarette smoking, and restrict tobacco use. The
W H O eXd a comprehensive, composite, tobacco control
programme whose major objectives were:
□ To prevent persons from starting to smoke;
□ To help addicts to quit smoking;
^5"
;
.’'7ia
Global Efforts at Tobacco Control
91
□
To reduce the toxic constituents in cigarette smoke, and hence
minimise the damage to smokers who are unable to quit;
□ To protect non-smokers from environmental smoke.
This composite programme has several arms; these are listed below.
Mass health education
This attempts to raise public awareness about the adverse effects of
smoking, chewing tobacco and dipping snuff, by using the mass media.
The ultimate goal of this method is to create a well-informed society,
where non-smoking would be the norm. The publication of the 1962
and 1971 reports of the Royal College of Physicians of London started '
a reversal in the trend and greatly contributed to the 30 per cent
decline in male smoking in the U.K. (1962-1980). Similarly, the
periodical publication of the U.S. Surgeon-General’s Reports from 1964
onwards is a major contributory factor in the decline of smoking
prevalence in the U.S.A. Large-scale health education through the media
helps prevent non-smokers from taking to cigarettes. In a habitual
smoker, it also substantially increases the motivation to quit. Equally
important, it facilitates necessary legislation such as increasing tax
rates, to control smoking.
Educating the public through the mass media on the adverse effects
of smoking, is a prime requisite for any tobacco control programme.
Ban on all forms of tobacco advertisements and promotion
Most children and teenagers are lured by cigarette advertisements,
which depict the smoker possessing mature, tough qualities, which
they themselves would like to emulate. The tobacco industry is
extremely resourceful in designing advertisements to attract specific
groups. For example, it had brought out slim cigarettes to encourage
> smoking among young girls. Once a person becomes a smoker, he or
she finds it extremely difficult to quit. Even with all the cessation
techniques available now, only about 35 per cent of smokers are able
to quit smoking. The saying once a smoker, always a smoker generally
holds true. Hence, we need to prevent the urge to smoke in the first
place. Banning all forms of tobacco advertisement will be of great
help.
Multinational tobacco companies who have money and influence,
also engage themselves in numerous promotional activities, sponsoring
games and entertainment programmes so on. This indirectly serves in
promoting their product. It also creates a circle of people who become
dependent on the tobacco industry for funds.
Realising the serious consequences of tobacco advertising and
1OBACCO AND ARECA NUT
promoting, twenty-seven countries have banned outright all forms of
tobacco advertisements and promotional activities. Eighty-four countries
have imposed severe restrictions on tobacco advertising. All these
countries have prohibited the sale of cigarettes to minors.
Health warnings
Most countries stipulate that every cigarette packet should carry the
health warning ‘cigarette smoking is injurious to health’. This warning
is carried even in those countries where cigarette advertising has not
been banned. In practice, however, this single line advertisement is
barely noticeable. This warning also has no effect on the addict, who
becomes used to seeing it. However, it may influence a young potential
smoker. Lt may also counteract promotional advertisements.
There have been many suggestions to make this health warning
large, and hence effective. A few advanced countries stipulate that the
tar and nicotine yields of the cigarettes should also be printed on the
packets.
Strategies for cessation of smoking
A variety of cessation techniques can be employed to help smokers
quit, depending on their motivation and degree of addiction.
Smokers attempt to quit only after making a conscious decision to
do so. However it has been observed that less than five per cent of
smokers succeed in abstaining from cigarettes at the end of a year. It
is thus necessary to help smokers quit if the success rate is to be
appreciable.
Brief counselling sessions for three to five minutes by the family
physician is found to help light smokers. Apart from'counselling them
on the beneficial health effects of quitting, the physician may also
provide leaflets on the hazards of smoking. The success rate achieved
is limited, only 5-12 per cent. Greater success can be achieved through
longer sessions but this may not be cost-effective. The distribution of
free nicotine gum or a nicotine patch substantially increases the quit
rate, and prevents quitters from relapsing.
Counselling alone is not enough for moderate smokers to quit. Such
smokers use fifteen or more cigarettes a day, and start smoking within
thirty minutes of waking up. More than half of them will experience
withdrawal symptoms, when they try to quit and need nicotine
replacement either in the form of nicotine gum or transdermal nicotine
patches which are now easily available and can be used during the
day, or for 24 hours. With only a few side-effects, they are best for
brief use. The physician should guide the smoker about using nicotine
ITt
Global Efforts at Tobacco Control
93
chewing gum properly. The gum should be chewed very slowly for
twenty to thirty minutes, so that the nicotine is gradually released, and
absorbed through the buccal mucosa into the bloodstream. Nicotine
nasal sprays cause irritation in the nose, and have poor compliance.
They are useful for highly addicted, heavy smokers. Nicotine
replacement therapy has been found to help moderate to heavy smokers
and prevent them from having a relapse. Some moderate smokers,
treated with nicotine patches, can quit smoking within a week. The
nicotine patch treatment is very cost-effective for these patients.
Highly motivated, but addicted heavy smokers, need intensive
therapy in specialised clinics to help them quit smoking. The treatment
is very expensive, involving repeated counselling in many sessions,
nicotine replacements in various forms, and so on. Group therapies
are arranged to save physician’s time, and cost to the smoker. Patients
attending specialised clinics within a particular geographical area, are
grouped together or paired within the group, and made to declare
their commitment to abstinence.They are then offered treatment through
various cessation techniques. They are often made to check upon
each other to ensure that all addicts maintain abstinence. Smoking by
any defaulter can be easily checked through two biochemical
parameters: by measuring the nicotine metabolite cotinine levels in
the saliva (this test is applicable only for those not receiving any nicotine
replacement like nicotine gum) and by measuring carbon monoxide
in the expired air. Expired carbon monoxide is found to be a useful
indicator of smoking in 90 per cent of cases. Portable carbon monoxide
meters are now available. Intensive treatment in ‘specialist smokers
clinic§’ resulted in 35 per cent of abstainers at the end of one year; and
22 per cent at 5 years, compared to 9 per cent and 5 per cent respectively
in the non-intervention group.
Fiscal policy
One of the most effective ways of reducing smoking is to raise the
taxes on tobacco and tobacco products. For every 10 per cent increase
in tax in U.S.A., there is a four per cent decrease of adult smokers and
a 14 per cent decrease of teenage smokers. Governments raise tax on
tobacco and tobacco products for three reasons: to raise their total
revenue, to compensate for medical and health care expenses arising
out of tobacco-related diseases and to curb smoking (sumptuary tax).
In Western countries, smoking is closely linked to the socioeconomic
group. Over half of the people in the lowest socioeconomic group
(unskilled manual workers, and their spouses, smoke). They also suffer
most from tobacco-related diseases such as chronic obstructive lung
■-
94
Tobacco and Areca Nut
disease, ischemic heart disease and lung cancer. The price rise in
tobacco and cigarette has its maximum impact on this group producing
a sharp decline in the number of cigarettes smoked. Smoking in the
upper socioeconomic groups (professional workers, managers, and
their spouses), is not a major problem and any price rise in cigarettes
or tobacco has no effect on their smoking behaviour. Smoking is
moderate in the middle socioeconomic groups (clerical workers, skilled
and semi-skilled manual workers), and they also respond moderately
to price rise in cigarettes and tobacco. It has been reported that the
government revenue increases even though the overall consumption
of cigarettes falls. The increase in tobacco tax is borne more by the
wealthier smokers than the poorer ones sincethey can afford to smoke
at the same level as before.
The prevalence of smoking is highest among the poor, who spend
a disproportionate share of their incomes on smoking. Any reduction
in their smoking due to a price rise in cigarettes, will benefit their own
and their families’ health. However, addicts who continue with their
smoking at the same level as before will be spending a lot more on
cigarettes than earlier. Thus, price rise in cigarettes can damage many
poor families. Governments will have to carefully monitor its taxation
on tobacco and tobacco products, •’out of consideration for socially
disadvantaged groups. A method of progressive taxation on tobacco
and tobacco products is one of the key elements in the Comprehensive
Tobacco Control Programme administered by the World Health
Organization. An efficient fiscal policy on tobacco, coupled with sound
mass health education achieves the maximum results. As the majority
of people are non-smokers, and as the whole society is fully aware of
the harmful effects of smoking, tax on cigarettes for health reasons, is
a popular tax, enthusiastically accepted by most sections of society in
the West.
There are some countries in Europe, where hand-rolled cigarettes
are used. They include the Netherlands (49 per cent of all consumption);
Denmark (27 per cent), Belgium (21 per cent), Germany (10 per cent),
France
(5 per cent) and the U.K. (4 per cent). These cigarettes are
taxed less but have a higher tar yield. All these will adversely affect
tobacco control in these countries.
Product modification
The established correlation between cigarettes and a number of serious
diseases, as well as the knowledge that cigarettes are addictive brought
about various programmes to control and prevent smoking. From early
1970s progressive product modification with less and less toxic yields
/
Global Efforts at Tobacco Control
95
became an integral part of all comprehensive tobacco control
programmes.
Tobacco companies responded by introducing filter cigarettes, with
substantially reduced tar and nicotine yields. Since the reduction in
both these substances were gradual and spread over years, they did
not evoke any consumer resistance. By 1993, the tar yield of cigarettes
in the U.K. had been reduced to 15 mg/cigarette. It was agreed that,
by 1997, the upper limit for tar would be 12 mg/cigarette, and for
nicotine 1 mg/cigarette. This will be followed by all countries of the
European Union (EU).
Deaths due to lung cancer and chronic obstructive lung disease
have been substantially reduced by product modification. The effect
on ischemic heart disease has not yet been clearly established.
Ban on smoking in public places
The majority of people are non-smokers and should be protected
from environmental tobacco smoke. Passive smoking can also cause
respiratory distress, lung cancer and other diseases. Hence, many
countries have banned smoking in public places like schools, churches,
and theaters. Smoking is also either completely banned or largely
restricted in most of the larger companies and other workplaces in
the U.K.
CONTROL OF TOBACCO HABITS IN DEVELOPED COUNTRIES
Among the Western countries, the U.K. and the U.S.A, have made
remarkable progress in controlling smoking among both men and
women, by adopting the comprehensive tobacco control programme
initiated by the W.H.O. Smoking among men declined steadily from
^about 60 per cent in I960 to about 28—30 per cent in 1992 in the U.K.
Smoking among women rose steadily from about 38 per cent in 1950
to 45 per cent in 1966-70, and has steadily decreased since then to
28 per cent in 1992. Though a steady decline in adult smoking has
been achieved in the U.K., the rates of smoking among teenagers are
still high. About one in four teenagers become addicts by the time
they reach sixteen. The U.K. hopes to reduce the rate of adult smoking
from about 30 per cent in 1990 to 20 per cent by 2000, reduce underage
smoking from 8 per cent to less than 6 per cent of 11-15 year-olds,
and smoking during pregnancy, by about a third.
Scotland has one of the highest incidences of smoking and lung
cancer, among both men and women. Anti-smoking measures,
96
Tobacco and Areca Nut
including counselling through telephones, are now being pursued
vigorously.
In the U.S.A., while smoking has been on the decline, there has
been a revival of the use of smokeless tobacco. From the 1970s
teenagers and young adults have been increasingly chewing tobacco
and dipping snuff. These practices are more common among boys
than girls. Smokeless tobacco causes leukoplakia, and oral and
pharyngeal cancers. The five-year survival for oral and pharyngeal
cancers is about 50 per cent in the U.S.A. As such, the morbidity and
mortality associated with smokeless tobacco is considerably less than
that in smoking. Smokeless tobacco is still popular among native
Americans. About a third of them use smokeless tobacco, and. are
consequent victims to oral lesions.
Tobacco control programmes are being pursued very seriously in
some Scandinavian countries like Norway and Sweden. These countries
use rotating health warning on packets of cigarettes and other tobacco
products. In this system of rotating warnings, several different messages
are in use at any one moment, appearing at random on all packages
and oh advertisements. Norway and Sweden each use sixteen warnings
and periodically replaced them with a new set to ensure that the
messages rema’in effective.
Tobacco control programmes in many other European countries
are not as advanced as those in the U.K. or U.S.A. While lung cancer
has been decreasing in the U.K. Since 1988, it has more than doubled
in Yugoslavia, Poland, and Hungary. Lung cancer mortality has increased
by 55 per cent in the former U.S.S.R. between 1970 and 1980. In some
of the European countries, women have begun smoking only recently ’
In many countries in Eastern Europe, which have recently become
free from communist rule, state monopoly trading in tobacco has ended.
Multinational tobacco companies have entered these new markets,
after buying many local companies there. A steady rise in smoking
and lung cancer in these countries can be expected in the coming
decades.
6
CONTROL OF TOBACCO HABITS IN DEVELOPING COUNTRIES
With a population of over one billion, China has the highest number
of cigarette smokers in the world. More than half of the men, but only
6 per cent of women, smoke. The most popular form of smoking is
cigarettes. So China has been the biggest target of all multinational
cigarette companies for decades. Till recently, there was monopolistic
<50/
Global Efforts at Tobacco Control
97
trading by Chinese National Tobacco Corporation, but now the Chinese
market has been thrown open and multinational companies are
reported to have already started advertising there, though China has
passed a comprehensive tobacco control legislation. It would be
interesting to see how this country fares in the next few decades.
There are wide differences among developing countries with regard
to tobacco control. Some countries like Thailand, Singapore, Sudan
and Botswana, have stringent tobacco control programmes, which are
strictly implemented. Even multinational tobacco companies are
punished, if they violate these regulations. However, there are also
many countries, particularly in Africa, where very few men and women
smoke. These countries do not even have a national survey of tobacco
habits, or any programme for tobacco control. They are not fully aware
of all the harmful effects of smoking, or of the various strategies adopted
by multinational cigarette companies to spread this habit.
Tobacco companies spend billions of dollars to advertise their
products, and counteract the growing public awareness of smoking.
Advertising and other promotional techniques used in developing
countries are reported to be different from those used in developed
countries with strict tobacco control programmes. Tobacco companies
are accused of following double standards.
The risk of tobacco-related diseases in developing countries is rising
due to increased consumption of manufactured cigarettes. Between
1970 and 1980, cigarette consumption increased by 62.5 per cent in
Pakistan; by 40 per cent in India; by 32 per cent in Kenya but by only
4 per cent in the U.S.A. In the U.K., cigarette consumption was actually
decreasing. Asia now accounts for more than half of world’s
consumption of cigarettes. Lung cancer is one of the three commonest
forms of cancer in India, Malaysia, and Pakistan, and is common among
both blacks and whites in Zimbabwe. Tobacco-related diseases will
appear in developing countries in a very big way, even before
communicable diseases and malnutrition have been controlled. This
is in sharp contrast to the West, where communicable diseases and
malnutrition are no longer present. Thus, the health problems of the
third world countries will be far more severe, unless remedial measures
are taken immediately.
There are many international organisations, which are concerned
about the health hazards of tobacco habits and the impact of tobacco
control programmes. Some of them are the World Health Organization
(W.H.O.); the International Union against Cancer (U.I.C.C.);
International Union against Tuberculosis and Lung Diseases;
International Agency on Tobacco and Health; Action on Smoking and
VO
1 OBACCO AND ARECA 1NUT
Health; International Organisation of Consumer Unions; International
Network of Women Against Tobacco, and Asia Pacific Association for
the Control of Tobacco (A.S.P.A.C.T.). There are many others, all of
which work towards safeguarding the health and well-being of
humanity.
19 Tobacco Control in India
The developed and developing countries who have realised the harmful *
effects of smoking and. chewing tobacco, are striving Jiard to cohtrol
the rates of tobacco consumption. Though none of them will achieve
the WHO goal of 'Health for all by 2000A.D. \ they would have gone
a long way towards that end. In India however, there have been very
few measures taken to control tobacco consumption. Numerous factors,
economic, social, and others, make it difficult to implement tobacco
control programmes in India.
Firstly, the cultivation and manufacture of tobacco products play an
important role in the Indian economy. India is the third largest producer
of tobacco in the world, after China and U.S.A. It produces 587 million
kg of tobacco annually, in 391,000 hectares of land. The tobacco industry
in India is also very well-established producing a variety of tobacco
products like bidis, cigarettes, hookah paste, zarda, cigars, cheroots
and chuttas. Raw FCV (flue-cured Virginia) tobacco is exported to the
U.K., Russia, Japan, Italy and Iraq. Manufactured tobacco is exported
to countries in the Middle East. All these provide the government
i*of India with an appreciable excise duty (Rs. 3,445.82 crores during
1994-95) and foreign exchange (Rs. 421 crores during 1995-96). The
Indian government is thus reluctant to take steps that would cut down
on these revenues.
Tobacco is a highly remunerative crop, and gives good returns.
However, as most farmers sell their products during harvest season for
want of the storage facilities, the crop is sold at extremely low prices.
The major share of the profits go to merchants and middlemen. Since
other crops are not as remunerative as tobacco, or as rugged and pest
resistant, tobacco cultivators are reluctant to switch to other crops.
People employed in the manufacture, packing, distribution, export,
and sale of tobacco products, reap high profits, and are hence averse
to tobacco control.
100
I
I
Tobacco and Areca Nut
Secondly, the Indian tobacco industry employs five to six million
persons. About 1.2 million people are engaged in the cultivation,
processing, and curing of tobacco, and another 3 million (including
illiterate women in rural areas) in the manufacture of bidi. Thousands
of tribals are employed in the collection of bidi leaves. The cigarette
industry alone provides employment to 25,000 people, while 500,000
people are engaged in the marketing and export of tobacco and tobacco
products. Thus, any attempt at tobacco control will affect millions of
people, including socially disadvantaged groups like women and tribals.
Any elected government, will think twice before creating such social
upheaval. Tobacco control in India must necessarily be gradual.
Society’s attitude towards smoking is an important factor determining
the success of any anti-smoking campaign. Smoking is now an accepted •
practice in India, unlike sixty years ago, when it was a social taboo. A
majority of people, including many educated people, are not aware of
all die serious ill-effects of smoking. Cinema also often depicts smoking.
This is in sharp contrast to the U.S.A, where public figures refuse to
appear with a cigarette in hand. The Indian public has to be educated
about the highly deleterious effects of smoking, the variety of diseases
it can cause, and the fatal nature of many of them if we are to implement
any tobacco control programme.
The government of India exerts some control over the manufacture,
promotion, and sale of tobacco products (primarily cigarettes) but not
very effectively. It has enacted the Cigarette Act, 1975, which stipulates
that all cartons and packets of cigarettes, and advertisements should
carry the statutory warning, ‘Cigarette smoking is injurious to health’.
Cigarettes carry higher tax but any increase in the rate of tax will have
only a marginal effect, as only the affluent smoke cigarettes. Others
may cut down slightly on the number of cigarettes they smoke. Cigarette
packets and advertisements carry the statutory warning, but as the
cigarette companies themselves are fully aware, this warning has
practically no effect on smokers. All cigarettes sold in India including
the so-called filter cigarettes, are reported to have high yield of tar and
nicotine. An average Indian cigarette contains 19-28 mg tar and up to
1.8 mg nicotine as compared to tar and nicotine yields of 12 mg and 1
mg per cigarette in the U.K. It is unfortunate that there is no legislation
or any move to control these levels.
There are absolutely no restrictions on cigarette advertising in India,
except in state-controlled radio and TV. channels. Most small shops
in Tamil Nadu, for example, carry large signboards advertising cigarette
brands. After the economic reforms of the early nineties, foreign brands
have also started making their appearance in the Indian market/
101
Tobacco Control in India
As bidis .are a product of a cottage industry, its employees enjoy
several concessions from the Indian government. While cigarettes are
subject to progressive rises in tax, the excise duty on bidis is still
comparatively low. Packets of bidis and tobacco do not carry any
health warning, despite the fact that bidis contain higher levels of tar
and nicotine than cigarettes. Epidemiological studies reveal that cancers
of the larynx and pharynx are more common in India than in the
West, because of the high rates of bidi consumption. There is practically
no quality control on the tobacco used for chewing and making bidis.
Millions of dollars are spent on promoting cigarettes, which are subject
to some government restriction. On the other hand, there is very little
promotion for bidis or chewing tobacco. Bidis act as cheap alternatives
for cigarettes and in a way, stem the rapid spread of cigarettes, backed
by multinational cigarette companies. Bidi smoking in India is confined ‘
to people of the lower middle-class and the poor.
The use of tobacco preparations as dentifrices is another feature
unique to India. Many popular brands of toothpastes in Bombay and
Goa contain tobacco. Their long-term use will certainly lead to oral
lesions, including cancer.
Smoking.in public places like schools, hospitals, cinemas, religious
places, buses and airlines should be strictly prohibited. Recently, the
government has banned the sale of cigarettes in railway stations.
Smoking inside government offices and institutions has also been
banned.
While the general public are only now waking up to the
consequences of using tobacco, the doctors in India have been aware
of them for a long time, and have also warned the Indian government
that the total cost incurred for the treatment of tobacco-related diseases
exceeds the revenue acquired from the manufacture and sale of tobacco,
by as much as Rs. 685 crores. This is a conservative estimate, and does
take into account the cost of establishing facilities for treatment.
Besides these huge economic losses, tobacco addiction also causes
human suffering, which cannot be translated into monetary terms.
The Ministry of Health has accepted these findings and made a number
of recommendations for effective tobacco control in India, similar to
the Composite Tobacco Control Programme, enunciated by the World
Health Organization. One of the significant provisions is that all tobacco
products put up for sale, including bidis and chewing tobacco, should
carry the health warning in two languages, English and Hindi or the
regional language, and should depict the universally known danger
sign, skull and crossbones, for non-literates.
pis
.p.0)
(J71U5
'
i
' ?A
J
100
i
Tobacco and Areca Nut
Secondly, the Indian tobacco industry employs five to six million
persons. About 1.2 million people are engaged in the cultivation,
processing, and curing of tobacco, and another 3 million (including
illiterate women in rural areas) in the manufacture of bidi. Thousands
of tribals are employed in the collection of bidi leaves. The cigarette
industry alone provides employment to 25,000 people, while 500,000
people are engaged in the marketing and export of tobacco and tobacco
products. Thus, any attempt at tobacco control will affect millions of
people, including socially disadvantaged groups like women and tribals.
Any elected government, will think twice before creating such social
upheaval. Tobacco control in India must necessarily be gradual.
Society’s attitude towards smoking is an important factor determining
the success of any anti-smoking campaign. Smoking is now an accepted •
practice in India, unlike sixty years ago, when it was a social taboo. A
majority of people, including many educated people, are not aware of
all the serious ill-effects of smoking. Cinema also often depicts smoking.
This is in sharp contrast to the U.S.A, where public figures refuse to
appear with a cigarette in hand. The Indian public has to be educated
about the highly deleterious effects of smoking, the variety of diseases
it can cause, and the fatal nature of many of them if we are to implement
any tobacco control programme.
The government of India exerts some control over the manufacture,
promotion, and sale of tobacco products (primarily cigarettes) but not
very effectively. It has enacted the Cigarette Act, 1975, which stipulates
that all cartons and packets of cigarettes, and advertisements should
carry the statutory warning, ‘Cigarette smoking is injurious to health’.
Cigarettes carry higher tax but any increase in the rate of tax will have
only a marginal effect, as only the affluent smoke cigarettes. Others
may cut down slightly on the number of cigarettes they smoke. Cigarette
packets and advertisements carry the statutory warning, but as the
cigarette companies themselves are fully aware, this warning has
practically no effect on smokers. All cigarettes sold in India including
the so-called filter cigarettes, are reported to have high yield of tar and
nicotine. An average Indian cigarette contains 19-28 mg tar and up to _
1.8 mg nicotine as compared to tar and nicotine yields of 12 mg and 1
mg per cigarette in the U.K. It is unfortunate that there is no legislation
or any move to control these levels.
There are absolutely no restrictions on cigarette advertising in India,
except in state-controlled radio and T.V. channels. Most small shops
in Tamil Nadu, for example, carry large signboards advertising cigarette
brands. After the economic reforms of the early nineties, foreign brands
have also started making their appearance in the Indian market.'
Tobacco Control in India
I
1
i
101
As bidis .are a product of a cottage industry, its employees enjoy
several concessions from the Indian government. While cigarettes are
subject to progressive rises in tax, the excise duty on bidis is still
comparatively low. Packets of bidis and tobacco do not carry any
health warning, despite the fact that bidis contain higher levels of tar
and nicotine than cigarettes. Epidemiological studies reveal that cancers
of the larynx and pharynx are more common in India than in the
West, because of the high rates of bidi consumption. There is practically
no quality control on the tobacco used for chewing and making bidis.
Millions of dollars are spent on promoting cigarettes, which are subject
to some government restriction. On the other hand, there is very little
promotion for bidis or chewing tobacco. Bidis act as cheap alternatives
for cigarettes and in a way, stem the rapid spread of cigarettes, backed
by multinational cigarette companies. Bidi smoking in India is confined ‘
to people of the lower middle-class and the poor.
The use of tobacco preparations as dentifrices is another feature
unique to India. Many popular brands of toothpastes in Bombay and
Goa contain tobacco. Their long-term use will certainly lead to oral
lesions, including cancer.
Smoking.in public places like schools, hospitals, cinemas, religious
places, buses and airlines should be strictly prohibited. Recently, the
government has banned the sale of cigarettes in railway stations.
Smoking inside government offices and institutions has also been
banned.
While the general public are only now waking up to the
consequences of using tobacco, the doctors in India have been aware
of them for a long time, and have also warned the Indian government
that the total cost incurred for the treatment of tobacco-related diseases
exceeds the revenue acquired from the manufacture and sale of tobacco,
by as much as Rs. 685 crores. This is a conservative estimate, and does
n#t take into account the cost of establishing facilities for treatment.
Besides these huge economic losses, tobacco addiction also causes
human suffering, which cannot be translated into monetary terms.
The Ministry of Health has accepted these findings and made a number
of recommendations for effective tobacco control in India, similar to
the Composite Tobacco Control Programme, enunciated by the World
Health Organization. One of the significant provisions is that all tobacco
products put up for sale, including bidis and chewing tobacco, should
carry the health warning in two languages, English and Hindi or the
regional language,, and should depict the universally known danger
sign, skull and crossbones, for non-literates.
*
)
102
Tobacco and Areca Nut
The launching of the National Cancer Control Programme (NCCP)
by the Ministry of Health and Family Welfare in 1985 gave an added
impetus to tobacco control programmes in India. It led to the National
Cancer Registry Project, and the establishment of Population-based
and Hospital Cancer Registries. From the data obtained from these
Registries, it was computed that about 48 per cent of cancers in men,
and 20 per cent in women are due to tobacco habits. On an average,
a third of all cancers in India are tobacco-related and entirely avoidable.
Two conferences, both held in Mumbai helped to focus attention
on tobacco habits and tobacco-related diseases in India. The first one
was a workshop ‘Tobacco or Health’, sponsored by the International
Union Against Cancer (UICC) in April, 1987. The workshop brought
together scientists, medical experts, policy makers, people working
for voluntary organisations, and the media. They evaluated the available
scientific evidence on possible hazards associated with various tobacco
habits, and suggested suitable strategies for controlling them. One of
the papers presented in this workshop revealed that Kerala has the
highest number of tobacco addicts in India. About a lakh of foreign
cigarettes flow into the state daily. It has the maximum number of
registered bidi-workers’ cooperatives, in addition to a number of
independent bidi makers. Kerela is also one of the largest consumers
of chewing tobacco. As expected, lung cancer is the most common
cancer among men in Kerala. The worst feature is that lung cancer
occurs in Kerala ten to fifteen years earlier than in developed countries. A
reduction of age is seen in the incidence of coronary heart disease also.
Another conference, an international symposium on ‘Control of
Tobacco-related Cancers and Other Diseases’, was held in January
1990 aspects of tobacco use were discussed.*
Many cancer hospitals and social workers are keenly interested in
tobacco control programmes, and in increasing public awareness about
the dangers of smoking. The Cancer Institute, Chennai, observes a ‘no
tobacco day every year. The Sundaram Medical Foundation in Chennai
has adopted the 'can stop programme, aimed at ending smoking. The
Indian Society on Tobacco and Health, whose members are medical
and social workers, has been fighting tobacco addiction,In Thiruvananthapuram, Kerala, the Regional Cancer Centre launched
a massive programme using the help of college and high school
• The Proceedings of both these meetings have been published as Tobacco and Health: The Indian
Scene, Eds. L.D. Sanghvi and P. Notani, UICC, , Tata Memorial/Centre, Mumbai 1989; Control of
Tobacco-related Cancersand Other Diseases, Eds. P.C. Gupta, J.E. Hamner III and P.R. Mujti, Oxford
University Press, Mumbai, 1992. Both of them together constitute a valuable source of information
on tobacco habits in India, their health effects, and the dilemma faced by the government of Irjdia
in implementing tobacco control measures.
Tobacco Control in India
103
students, health workers, voluntary agencies, social organisations, and
the media, to combat the widespread tobacco addicion in Kerala. Under
the National Service Scheme (N.S.S.), it has trained students from various
colleges to carry out anti-smoking campaigns. High school students
were educated on the evils of using tobacco. The students were
rewarded for selling booklets on the harmful effects of tobacco. Health
workers were trained to detect oral cancer and oral pre-cancers, and
to create awareness among villagers about the harmful effects of
chewing and smoking tobacco. This has enhanced primary prevention,
and ensured early detection of oral cancers. Voluntary agencies and
social organisations participated in all these anti-tobacco campaigns,
carried out through lectures, slides and documentary films.
The Rajasthan Cancer Society has been vigorously campaigning
against smoking in Jaipur and Jodhpur, through public lectures,
distributing leaflets in the local language, slogans and slide shows’
The Goa Cancer Society has been conducting health education camps
for teachers and students in Sindhudurg and Ratnagiri, and has found
that educating children often results in parents giving up smoking.
Some major national dailies have been regularly publishing,articles
on tobacco control and passive smoking. However, some of them also
publish attractive colourful advertisements on cigarettes at'the same
time.
Recently, a lawsuit has been filed against cigarette companies,
demanding that they compensate for the damages caused by smoking.
It may not succeed, but it will succeed in focusing public attention on
the harmful effects of smoking.
Recently, the Kerala High Court allowed two public interest writ
petitions, and gave a judgment, banning smoking in ‘public places in
the state, like educational institutions, hospitals, commercial
establishments, factories, cinema houses, walkways, bus stops and
efen railways stations’. Smoking in these areas will now be punishable
under section 188 of the Indian Penal Code (IPC). A Division Bench of
the High Court has said that, ‘Public smoking is illegal, unconstitutional
and is a violation of article 21 in the Constitution.’ The judiciary has
directed district collectors in the state to promulgate an order under
Section 133(a) of the Criminal Procedure Code, prohibiting public
smoking within a month from the date of the high court ruling. The
office authorities have been asked to take appropriate steps to book
the offenders. According to a Press Trust of India Report, the Hosdurg
Magistrate Court in the Kasargod district, Kerala, has fined five people
Rs. 500 each for smoking in public places. Two people who were
unable to pay the fine, were imprisoned for fifteen days.
104
Tobacco and Areca Nut
ISO
isisifiis
A betel quid preparation (Courtesy: Fali S Mehta, Head, Basic Dental
Research Unit, Tata Institute of Fundamental Research, Mumbai)
- 'C,
®
.
'
■ ■
■.
V
-1^
SlllS
'ts®
... Ifgill ill
In
Reverse chutta smoking: a woman from Goa
(Courtesy: Fali S Mehta, Head, Basic Dental Research Unit,
Tata Institute of Fundamental Research, Mumbai)
5//
Tobacco Control in India
I
I
■ft
Fl
Submucous ■fibrosis. Note the shrunken
tongi
--- —
jue and difficulty in opening
the mouth. (Courtesy:
—t-- >-Faii
- ...............
S Mehta, Head, Basic Dental Research Unit,
Tata Institute of Fundamental Research, Mumbai)
1
i
i
sag
’■‘x xs:»S
1
i
I
Cheek cancer in a betel quid chewer who also smoked
(Courtesy: Pali S Mehta, Head, Basic Dental Research Unit,
Tata Institute of Fundamental Research, Mumbai)
105
20 Tobacco Research and
Interventional Studies
in India
The Government of India set up the Indian Central Tobacco Committee
in 1945, to develop all aspects of tobacco cultivation, processing, and
. marketing. The committee, in turn, established the Central Tobacco
Research Institute at Rajahmundry, Andhra Pradesh, in 1947, to conduct
fundamental research on all varieties of tobacco, and applied research
on cigarette and Lanka tobaccos. It set up Regional Research Stations
at Vedasandur (Tamil Nadu) in 1948 for research work on cigars and
chewing tobacco; at Pusa (Bihar) in 1950, for research on hookah and
chewing tobacco; and at Anand (Gujarat) and Nipani (Karnataka) for
research on bidi tobacco. A cigarette tobacco research station was
already functioning since 1936, at Guntur (Andhra Pradesh). The
Committee also established a wrapper and hookah tobacco research
station at Dinhatta (West Bengal) in 1952. The Central Tobacco Research
Institute and the various Regional Research Stations were brought un er
the control of the Indian Council of Agricultural Research in 1965. The
Bidi Tobacco Research Station at Anand became part of the Gujarat
Agricultural University.
The Central Tobacco Research Institute (CTRI) in Rajahmundry
has three main departments: division of genetics and plant breeding,
division of agronomy and soil science, and division of biochemistry
technology and plant nutrition. There are also various departments of
Entomology, Pathology, Statistics, Seed and Seedlings, Engineering;
Farm Management. Keeping in mind the directive Scientific
Coordination with which it was set up, the CTRI has involved itself
with a variety of research projects, aiming to improve the quality,
production and productivity of tobacco. It also studies factors that
XIM I
£,!'< 11V-/1N/1L JlUUlCd UN 11N1J1A
IV/
influence the quality of tobacco leaves produced, like colour of leaves
(light or dark), texture (thin or heavy-bodied), elasticity, their nitrogen
and nicotine contents, and their aroma and taste. The CTRI has
acclimatised several exogenous varieties of tobacco to grow in India.
Employing mutation, hybridisation and recombination techniques, it
has also evolved new strains of tobacco like ‘Kanakaprabha’ and ‘CTRI
Special’, which are of a better quality, have greater yield, are more
pest-resistant, and so on.
Recently, with world opinion hardening against tobacco and tobacco
addiction, the CTRI has embarked upon three new projects, which
aim, to help tobacco control programmes. They are:
Product modification
This is an attempt to reduce the yield of tar and nicotine from cigarettes
and bidis. It was found that adding potassium citrate to cigarette shreds,
bring the potash level up to about 3 5 per cent, reduce the total
particulate matter by 35 per cent, and bring down the mutagenicity of
cigarette smoke by 80 per cent.
Scientists of the Gujarat Agricultural University at Anand have also
carried out investigations to reduce the tar and nicotine yields of bidis.
They have observed that 1. bidis made from all available, varieties of
tobaccos in India yield nearly the same levels of tar and nicotine, and
2. variations in growth conditions like transplanting dates, fertiliser
nitrogen levels, source of nitrogen, irrigation, plant density, .topping
level and harvest date, do not produce tobacco with lower yields of
nicotine and tar.
After testing three filters for bidis (cotton, cotton scented with amber
and cigarette filters) they recommend the use of cotton scented with
amber filters for bidis. It is effective in reducing the levels of toxic
chemicals in the smoke, and is readily acceptable to consumers. When
tobacco is grown in a carbon dioxide enriched atmosphere, the yield
of leaves increased by 7 per cent. The leaves also contain less protein,
nitrate, alkaloids and other chemicals which give rise to toxic substances
like N-nitrosamines. Scientists at the Bidi Research Station at Anand
are trying various strategies to grow tobacco under carbon dioxide
enriched conditions.
Other uses of tobacco
Tobacco is a rich source of several phytochemicals like nicotine,
solanesol organic acids (malic, citric and oxalic), and pentosans. About
10 per cent of the tobacco goes waste, when used in the manufacture
of tobacco products like cigarettes and bidis. This serves as the material
for manufacturing nicotine, solanesol, organic acids, and pentosans.
a'*
!!
•I
U
108
Tobacco and Areca Nut
There are a few companies in Gujarat which make these chemicals
from the bidi tobacco wastes.
Nicotine is widely used in the form of nicotine sulphate, as a pesticide
also serves as the raw material for the manufacture of the
pharmaceuticals nicotinic acid and nicotinamide (found in the vitamin
B complex), and nikhethamide. Solanesol is used as an intermediate
for manufacturing a cardiac drug, and making vitamin K analogues
Malic and citric acids are used in both food and drug industries'
Pentosans are used for production of the industrial solvent, furfural
Roughly 40-42 per cent of tobacco seed comprises of oil. This is
used as a semi-drying oil in the paint industry. When refined, it may
also be used as edible oil. Proteins in the tobacco leaf can be useful as
a food. Immature tobacco which is ninety days old, should be used to
ensure the maximum extraction of all these chemicals.
Nicotine sulphate is a stomach, contact, and fumigant poison It is
sXhate^and
in Japan' Both nicotinc
sulphate and solanesol are exported to Japan, the U.K the U S A
Canada Switzerland and Germany. There is thus a good export market
for both these chemicals. The possibility of utilising nicotine sulphate
as a pesticide in India itself should be explored. As a natural product
it may have advantages over synthetic pesticides that we use at present’
Substitute crops for tobacco
The feasibility
ic^iuiniy of
oi growing
growing other
other crop;
crops remuneratively instead of tobacco
has been explored. However there are many inherent'difficulties in
arriving at a possible solution. Tobacco is a drought-tolerant rugged
plant, and can grow in semi-arid areas. It is also resistant to many
pests, and is a remunerative cash crop for farmers. Most other plants
do not possess these qualities. Andhra Pradesh and Gujarat tried in
vain to substitute tobacco with cotton and chillies. Cotton is not resistant
to many pests, and gives low yields. Chickpeas, mustard, coriander
and sMflower, can be successfully grown instead of FCV tobacco on
the black soils of Andhra Pradesh but their market prices are subject
to great fluctuation. Hence, farmers prefer to grow only tobacco, which
gives a more steady income.
In Gujarat, castor can be grown more remuneratively, but the demand
for castor oil has not been assessed so far. In West Bengal, crops like
potato, cauliflower and mustard are more remunerative than the cigar
filler and chewing tobacco cultivated there. However, these crops
s°™etlme® fetch verylow prices due to overproduction. In Tamil Nadu
chillies, safflower, groundnut or cotton can easily substitute the chewing
tobacco grown rotationally between bajra, ragi, and sorghum. Farmers
dm"
Tobacco Research and Interven'd nal Studies in India
109
however, still prefer to grow tobacco b* .cause—
of thez erratic monsoon
pattern which will bring varying yields with he o ler crops. Bihar is
the only place, where chewing tobacco is stea Jv giving place to
sugarcane, maize, potatoes, groundnut, an 1 mu .a-d.
The investigations carried <out' at variot ;. tobacco research stations
thus repeal the possibilities and problem, connected with:
Product modification, aimed at reducin g tar and nicotine yields
of cigarettes and bidis;
Alternate uses of tobacco, with the v rrious chemicals that can
be manufactured from it; and
Substituting other crops for ' >bacc j in the tobacco cultivated
areas of India.
Epidemiological investigations and laboratory analysis
Epidemilogical studies on cancer in India are now nearly a century
old. As early as 1902, Niblock observed an appreciable number of oral
cancer patients in the Government General Hospital at Chennai He
correctly ascribed this to the prevailing betel quid and tobacco chewing
habits among the people. A more detailed case-control,study was
carried out f y O.r in 1933 among the people of Travancore (now
known as Kerala), which confirmed Niblock’s observation, and clearly
established betel quid along with tobacco addiction as the cause for
oral cancjr.
Wahi and co-workers have carried out extensive studies on tobacco
habits m the Mainpuri district of Uttar Pradesh in 1965-66. Tobacco is
•mixed, with slaked lime, finely-cut areca nut, camphor,'and cloves.
About 7 per cent of the villagers are addicted to this preparation.
Prolonged chewing is found to lead initially to leukoplakia and oral
submucous fibrosis and later on to oral and oropharyngeal cancers.
Smoking and chewing tobacco, combined with alcohol consumption
is found to increase the risk for these cancers synergistically.
In 1959, Shanta and Krishnamurthi studied the etiological factors
causing oral cancer (squamous cell cancer). A sharp increase in all
tobacco-related cancers in Chennai during the period 1987-91
compared to 1982-86, has been reported by Gajalakshmi, Ravichandran
and Shanta in 1996. The per capita consumption of tobacco has also
increased during this period. A survey of 7,737 households in Chennai,
conducted during 1997-98, revealed that among men, the proportion
of smoking, chewing and drinking alcohol were 31.1 per cent, 7 per
cent and 10 per cent respectively; eight per cent of women chewed
tobacco, but hardly any of them smoked or drank; about 88 per cent
were aware of the harmful effects of smoking and chewing tobacco.
110
Tobacco and Areca Nut
A case-control study carried out by Sanghvi, Rao and Khanolkar in
1955 at the Tata Memorial Centre, Mumbai, revealed that smoking
bidis leads to cancers of the oral cavity, pharynx, larynx, and esophagus,
and contribute largely to cancers at the oropharynx; and chewing
tobacco, besides leading to oral cancer, contributes to cancers of the
larynx, pharynx, and esophagus. These results were later independently
confirmed by Jussawalla and Deshpande.
Bidi smoke was chemically analysed only in 1974 by Hoffmann,
Sanghvi, and Wynder in the U.S.A, laboratory and was found to contain
larger amounts of toxic chemicals like tar, nicotine, carbon monoxide,
and hydrogen cyanide than cigarette smoke. This suggests that smoking
bidis is far more dangerous than smoking cigarettes. An analysis of
smoke from various brands of bidis has been carried out since then in
India, by Pakhale and co-workers at the Cancer Research Institute,
Mumbai. Most of the tobacco used in India contain a higher percentage
of nicotine than tobacco used in the West. Also, the tobacco used for
making bidis is considerably richer in nicotine than the tobacco blend
used in making cigarettes. This explains the higher yield of nicotine
from bidis, though they contain only a fraction of the tobacco used in
cigarettes. The carcinogenicity of bidi smoke was confirmed by Bhide,
who observed that seven out of fifteen BALB/c mice treated with bidi
J smoke, condensate develbped tumours (one gastric carcinoma, one
esophageal cancer, four liver haemangiomas, and one papilloma of
the stomach).
Recent investigations by Bhisey and co-workers suggest that the
vast number of women rolling bidis, constantly inhale tobacco dust
and hence have a high risk of tobacco-related diseases. The urine of
bidi rollers was found to contain cotinine as well as thiqethers, revealing
the cutaneous and lung absorption of nicotine and other toxic
components of tobacco.
Investigation by Nagabhusan and co-workers reveal that betel leaves
by themselves are anti-mutagenic and anti-carcinogenic, and will tend
to counteract the carcinogenicity of tobacco. Catechu has also been
found to be anti-mutagenic.
Interventional studies
Cross-sectional studies carried out by Mehta and co-workers among
4,000 Bombay policemen in 1960-61 revealed that there is an
appreciable incidence of leukoplakia and oral cancer among paan
chewers and bidi smokers. A survey carried out in 1965—66 by Pindborg
and co-workers among 35,000 outpatients in dental clinics in Bangalore,
Lucknow, Bombay and Trivandrum confirmed the high prevalence of
leukoplakia in India.
<5/7
Tobacco Research and Interventional Studies in India
Ill
These studies led to a large scale, marathon project on oral cancer
and pre-cancers, carried out by the Basic Dental Research Unit of the
Tata Institute of Fundamental Research, Mumbai. The project,
supported entirely by funds from the National Institutes of Health,
U.S.A, under the P.L. 480 Indo-American Research Agreement, lasted
for twenty-seven years, and began in 1966. Dr Fali S Mehta of the
Basic Dental Research Unit served as.the Principal Investigator; the
late Dr. Jens J. Pindborg of the Department of Oral Pathology, Royal
Dental College, Copenhagen, Denmark, as the co-principal investigator;
and Dr. James E. Hamer III, from the University of Tennessee, as the
N.I.H. project officer. Some of the other investigators involved in this
project were Drs. P.R. Murti, R.B. Bhonsle, P.N. Senor and D.K. Daftary
(all Dentists); Dr Prakash C. Gupta (Statistics), and Dr. Mira B. Aghi.
A unique feature of the project, was that if was a population-based,
house to house survey in the rural areas, and involved as many as
2,00,000 subjects. In terms of persons involved, money spent, and the
duration, it was one of the largest projects ever carried out in India so
far. Though expensive, and time-consuming, the project yielded rich
dividends and for the first time provided, an integrated picture of the
various tobacco habits in India. It has also given a lot of information ,
on the pathogenesis of the pre-cancers, leukoplakia and oral submucous
fibrosis and palatal lesions, and the subsequent onset of oral and
palatal cancers, mainly from the pre-cancers. Above all, it has
demonstrated the feasibility of intervention through health education,
resulting in a ‘significant and substantial’ decrease in oral pre-cancers
and cancer.
In the first phase of the project, lasting from 1966-69, a survey of
the prevalence of various tobacco habits among villagers in seven
select areas of India was carried out. The areas selected were Ernakulam
in Kerala, Goa, Pune, Bhavnagar in Gujarat, Srikakulam in Andhra
Pefedesh, Singhbhum and Darbhanga in Bihar. The survey revealed
that bidi smoking was most common among men in all these places,
except Srikakulam, where chutta and reverse chutta smoking were
practised. Cigarette smoking was high only in Kerala, among 6 per
cent of the population. In Bhavnagar, Srikakulam, and Goa, most men
smoked. Chewing was more common in Pune and Uttar Pradesh while
in Ernakulam, Singhbhum, Darbhanga and Mainpuri, both smoking
and chewing were widely practised. Women preferred chewing tobacco
to smoking in all the places except Srikaklam, where almost all of
them practised reverse chutta smoking and in Duarbhanga, where
hookah smoking was more common. This study revealed that tobacco
use in one form or other is quite common in rural India, ranging from
61 pef cent (Pune) to 88 per cent (Andhra Pradesh) among men; and
15 per cent (Goa) to 67 per cent (Srikakulam) among women.
A survey of 50,915 villagers in four states revealed twenty-six cases
of oral cancer. The prevalence of leukoplakia ranged from 0.2-4.9
per cent and mainly affected men. Leukoplakia was found to strike at
a younger age than oral cancer. Its starts appearing among people of
the 15”24 age group,- and to a larger extent in the 25-34 age group.
The exact location of the leukoplakia depended very much on the
kind of chewing and smoking practised. Hookli smoking led to
leukoplakia on the labial mucosa, and reverse chutta smoking on the
palate. Epithelial atypia was seen in 8.4 per cent of homogeneous
leukoplakia, but in 59-1 per cent of speckled leukoplakias. Submucous
fibrosis occured exclusively among betel quid and areca nut chewers,
areca nut being the etiological factor. It strikes mainly in the oral
cavity and occasionally, in the pharynx and oropharynx.
A ten-year follow up study of this population revealed that:
Preleukoplakia and leukoplakia occurred only among those
who smoked or chewed tobacco
Oral cancer occurred almost always from the pre-cancers,
leukoplakia, or submucous fibrosis; and
While leukoplakia may regress, after a person stopped
consuming tobacco, submucous fibrosis, once formed, does ■
not regress at all. It is definitely a pre-cancerous state.
In a seventeen-year follow up of sixty-six cases of oral submucous
fibrosis, oral cancer developed in 0.4 per cent of cases at the end of
ten years; in 4.5 per cent at the end of fifteen years, and in 7.6 per cent
at the end of seventeen years. Only if one stops chewing tobacco, can
one prevent its further transformation into pral cancer. Other oral lesions.
like leukedema, leukokeratosis, nicotina palati, palatal erythema, central
papillary atrophy of the tongue, paan ch ewer’s lesion or oral lichen
planus-like lesion do not become malignant. Reverse chutta smoking
led to a variety of palatal changes like keratosis, excrescences, patches,
red areas, ulcerations and non-pigmented areas. Red areas are the
most dangerous, with 52 per cent of them exhibiting epithelial dysplasia.
Over a ten-year follow up period, ten cases of palatai cancers arose,
all from pre-existing red areas or patches. The majority of palatal lesions,
about 75 per cent remained as they were, while a small percentage
(14 per cent) underwent regression. The palatal lesions regressed further
if a person stoped smoking. Thus, the ten-year follow up study revealed
that oral cancer and oral pre-cancers occur only among tobacco addicts,
showing that the abolition of smoking and chewing tobacco should
reduce incidence of oral cancer.
□
□
□
The third phase of the project was the actual ‘intervention’ which
attempted to investigate firstly, whether health education could motivate
tobacco users into giving up tobacco, and secondly, determining
the impact on the oral pre-cancers. A ten-year prospective study
(Ipyy-gg) was conducted in three areas - Ernakulam, Srikakulam and
Bhavnagar. Each place built an ‘intervention cohort’ constituting about
12 000 people, who were periodically trained on how to quit tobacco.
A control cohort of about 10,000 tobacco users was formed from-the
previous ten-year study. These people did not receive any or only
minimal levels of health education. It was seen that most tobacco
users began using tabacco, believing it to have medicinal value, such
as, a curative for toothache, bad breath and gastric disturbances. Some
were vaguely aware that tobacco was harmful but very few knew all
about its deleterious effects. In the Bhavnagar district, only men were
targeted, as very'few women smoked or chewed tobacco.
The intervention team consisted of dentists, trained social workers,
interviewing clerks, and locals. At the beginning of this stage, all the
subjects were examined by dentists. People in the intervention cohort
were then offered medical advice, and educated on the need for, and
method used, to stop tobacco consumption. They were also informed
of the withdrawal symptoms through individual or group interviews.
Personal communication helped clarify doubts and clear individual
problems relating to tobacco use. Confidence and trust were also built
up through these sessions. At each one-year follow up, the subjects
were asked about their tobacco habits, to see if there was any reduction.
They were than examined by the dentists for any possible pre-cancerous
changes. This was followed with encouragement to maintain or intensify
the motivation to quit. Each annual follow up thus assessed the efficacy
of the intervention phase. In addition to personal advice, a variety of
other strategies were employed to make the intervention effective.
Films were found to be effective in bringing about behavioural changes^
particularly as the intervention population included non-literates and
semi-literates. Being a mass media, films had the advantage o
communicating to a large audience at one time. Specially designed
posters, some with written messages, and others with pictures, were
used to remind the target population of the need to quit tobacco
consumption. Slides prepared from these posters, were shown
shown in
in the
the
nearby theatres. Folk dramas which were found to be very popular in
the Srikakulam area, were effective in conveying the message against
tobacco use. Radio programmes in the form of talks, interviews, dramas^
and documentaries, and articles in local newspapers, were also used
to educate the public. Finally, cessation camps were held to help
114
Tobacco and Areca Nut
those who had made previous attempts to quit tobacco consumption
but were unable to do so. Thus, all conceivable methods were employed
to bring about behavioural changes in tobacco users.
The intervention trials were found to be very effective in both
Ernakulam and Srikakulam. In Emakulam, at the end of the intervention,
about 14 per cent of tobacco users have completely stopped usage,’
and many others have significantly reduced their tobacco consumption’
This has brought about a decrease in the leukoplakia rate in Ernakulam,
and palatal changes in Srikakulam, which, in turn, would signify a
decrease in the rampancy of cancers. However, the intervention trials
in Bhavnagar had no significant effect on the tobacco habits of that
population.
Protective agents against smoking and chewing tobacco
Oral cancer is a major health problem in Kerala. An attempt has been
made by the Regional Cancer Centre, Thiruvananthapuram, to elucidate
the risk factors for cancers at specific sites within the oral cavity. It was
observed that chewing betel quid containing tobacco increases the
risk of cancers in the buccal mucosa and the gingivum. This is explained
by the fact that the people in this part of India customarily keep the
bolus of betal quid in between the buccal cavity and gingivum.
Smoking is found to be the major cause of cancer^in the anterior
two-thirds of the tongue.
As there is a high prevalence of oral leukoplakia in Kerala because
of the high betel quid consumption rate, investigations have been
carried out to see whether chemoprevention of leukoplakia is possible.
Chemoprevention is a forfn of primary prevention, by taking in dietary '
or pharmacological inhibitors of carcinogenesis. Investigations were
conducted on fishermen who had oral leukoplakias because of chewing
betel quid. About 65 per cent of these participants also drank, while
30 per cent were bidi smokers. Treatment with oral vitamin A as retinyl
acetate at a level of 300,000 I.U. per week for a ye'ar, causes complete
regression of leukoplakias in 52 per cent of the cases. Beta carotene at
360 mg per week for a year effected a complete regression in a third
of the cases, while only 10 per cent of regression was observed in
placebos. The fishermen continued smoking, chewing and drinking
throughout the treatment period. Homogeneous leukoplakias and
smaller lesions responded more readily than non-homogeneous and
larger lesions. No toxicity was observed but a relapse occurred when
the supplementation with vitamin A or beta carotene was stopped.
Vitamin A was found to be more effective than beta carotene. These
investigations reveal that chemoprevention of the incidence of oral
Tobacco Research and Interventional Studies in India
H5
leukoplakias can be
I achieved through administration of vitamin A or
beta carotene, even when the tobacco habits are being continued.
The success rate however, is not very high.
Other contributions
Both basic and clinical research on various aspects of smoking and
chewing tobacco are continuing in several laboratories in India. Statistics
on the morbidity and mortality due to smoking and chewing tobacco
have been compiled earlier by Gupta of the Tata Institute of
Fundamental Research, Mumbai, and Jayant and Notani of the Tata
Memorial Centre. Information on cancer incidence, morbidity and
mortality are available frpm the reports of the National- Cancer Registry
Project. The use of hand-held computers (electronic diaries) for
numbering tobacco addicts among the general population in big cities
like Mumbai, has recently been reported by Gupta of the Tata Institute
of Fundamental Research.
I
I
I
i
21 Considerations,
Suggestions and
Future Prospects
There are more diverse tobacco consumption habits in India than in
any other country in the world. Bidis and cigarettes are the most
common fornis of smoking in India, while cigars, cheroots, chuttas,
and reverse chuttas, hookahs, hooklis, and chillums are less common.
Besides the cancers caused by cigarettes, smoking bidi leads to a
higher incidence of cancers in the pharynx, larynx, and the base of
the tongue; reverse chutta smoking, causes cancer in the hard palate.
Thus, the resulting cancers are equally varied.
The chewing habits are equally diverse in India. Plain tobacco with
slaked lime, other tobacco preparations (khaini, zarda, kiwam,
Mainpuri), a variety of areca nut preparations (raw areca. nut slices,
fermented areca nut (bura tammool); scented areca nut (supari), mawa,
paan masala, paan masala gutka), and betel quid in various
combinations are chewed. In addition, a variety of tobacco preparations
(mishri, bajjar, gudhaku, and creamy snuff toothpaste) are used as
dentifrices. All these result in very high rates of oral cancer, and cause
pre-cancers, leukoplakia and oral submucous fibrosis.
Chewing also causes cancers of the pharynx, larynx, and esophagus.
In the West, cancers of the mouth, larynx and pharynx together
constitute 5-10 per cent of the total cancers. However, they are all
serious health problems in India, accounting for 30-40 per cent of all
cancers among men in some places.
Bidi
The bidi is now the most common form of smoking and of tobacco
use in the country. It is a tobacco product unique to India, and yields
Considerations, Suggestions and Future Prospects
117
greater amounts of tar and nicotine than cigarette. Epidemiological
investigations show that it also causes cancers of the pharynx, larynx,
and of the posterior third of the tongue. It is undoubtedly responsible,’
at least in part, for the relatively far higher incidence of these cancers
in India.
However, any attempt to reduce bidi consumption must be carefully
planned, since the manufacture and marketing of bidis provides
employment to over three million people. However the government
can make a small beginning by insisting on ‘health warnings’ on all
packets of bidis and chewing tobaccos. It can also insist on bidis
being provided with cotton filters, scented with amber so that the tar
and nicotine yields of bidis are reduced. This may make the bidi
slightly more expensive, but the resulting health benefits will more
than compensate for it.
I
Cigarette
Cigarette smoking is likely to increase rapidly in India in the future.
There is only a limited ban on cigarette advertising so that cigarette
manufacturing companies can use aggressive marketing tactics to
promote th^ir products. Cigarettes are more common among affluent
students especially male students who are low achievers. Very few
girls smoke at present.
While cigarettes in all the developed countries, yield low amounts
of tar and nicotine, their yield from Indian cigarettes is still very high
(19—20 mg of tar, and aboout 2 mg of nicotine per cigarette).
Even, the so-called filter cigarettes in India have high tar and nicotine
yield. Both the Indian government, and the Consumer Council of
India should act against this immediately. In many Western countries,
cigarette companies have to print the tar and nicotine yields on cigarette
ggckets. The ministry of health, of the Indian government should also
consider implementing this.
The large-scale entry of multinational cigarette companies into India
will result in a continuous drain on foreign exchange, besides ruining
the health of the nation. The only factor which prevents a greater use
of cigarettes in India is an availability of the bidi as a cheap substitute.
As India ‘progresses’; the cigarette may replace the bidiz
I
Hookah
Hookah smoking which began during the mughal period, is still
practised in the Middle East. India exports substantial amounts of
hookah paste to countries in this region.
Nicotine
The long-term harmful effects of cigarette smoking have been known
for over forty years now. However, people in all countries still continue
to smoke. This is because of the profound psychological effects exerted
by nicotine, which is reported to improve learning and memory in the
individuals.
The question arises whether nicotine alone can be used safely to
produce the desired psychological effect. At the moment, it is used as
nicotine patches, nicotine chewing gum, or spray, primarily to control
withdrawal effects.
Nicotine’s known adverse effects are on the cardiovascular system.
If we could find a cardioprotective agent which will protect the vascular
system, without interfering with the psychological and other desirable
effects of nicotine, then it could be used for a number of purposes,
including treatment of Parkinson’s and allied diseases. It will also enable
the development of a really ‘safe cigarette’, without any cardiotoxicity.
Areca nut
The areca nut is extremely popular in India and is chewed in a variety
of ways. Unfortunately, some of the preparations are harmful, causing
diseases such as oral submucous fibrosis. This is a serious ailment,
characterised by a strong rigidity of the oral mucosa (loss of elasticity).
In extreme cases, the person may not be able to open her mouth at
all. This condition does not regress, and in some cases can develop
into oral cancer. There is no known cure for oral submucous fibrosis.
A survey revealed that about 10.9 per cent of mawa chewers were
suffering from oral submucous fibrosis. Many of them were young,
well below thirty-five years; they had begun chewing mawa at an
early age. The mechanism of how the areca nut induces submucous
fibrosis should be studied and also, whether it could be prevented by
simultaneously chewing a protective agent.
Paan masala and gutka are well-advertised popular areca nut
preparations chewed in northern India. Gutka also contains tobacco.
Many eipidemiologists and dentists fear that these will lead to high
rates of oral submucous fibrosis and oral cancer in the future.
The areca nut is potentially carcinogenic. It contains alkaloids, which
can undergo nitrosation changes inside the body to give rise
carcinogenic N-nitrosamines. An epidemiological report from Natal in
South Africa, states that habitual chewing of areca nut alone by Indian
women there, has led to oral cancer.
‘Bura tammool’ which is often fungus-infected may or may not have
contributed to the very high incidences of pharyngeal and esophageal
cancers prevalent there.
While tobacco has been extensively studied, there is still scope for
research work on the biological effects of areca nut, and of various
preparations containing areca nut. There are also innumerable imitations
sold as areca nut in small packets in wayside shops in Chennai, and
consumed by the public, without knowing its contents. Both the
Consumer Council of India and the state government should thoroughly
investigate what these packets contain, and their biological effects.
Betel quid (paan)
Epidemiological studies suggest that betel quid without tobacco does
not pose a significant risk of cancer. Among the various components
of paan, the individual ones betel leaves protect against carcinogenesis
areca nut could induce cancer, and chunam (slaked lime), an irritant
could act as a promoter. Hence, habitual chewers would do well to
increase the number of betel leaves, minimise the quantities of areca
nut and slaked lime, and strictly avoid tobacco. The frequency of
chewing should also be restricted.
Nationwide survey
Unfortunately, we do not have a nationwide aurvey of tobacco, betel
quid and areca nut habits in India. A population-based nationwide
survey will be very expensive; but will provide a wealth of baseline
information, on which other studies can be based. Though a nationwide
survey does not exist, considerable information is available from other
sources, which include:
1. The project on oral cancer and pre-cancers, carried out for twenty
seven years by the Basic Dental Research Unit of the Tata Institute
of Fundamental Research, Mumbai, in six districts in India
(Ernakulam; Pune; Srikakulam; Bhavnagar; Singhbhum'; and
Darbhanga) from 1966 to 1993;
2. The population based Cancer Registries at Chennai, Bangalore,
^Mumbai, Ahmedabad, Delhi, Bhopal, and Barshi;
3. The Hospital Cancer Registries at Thiruvanathapuram and Dibrugarh;
and
4. Various research papers published from cancer and other centres at
different times.
All the information thus gathered, makes it possible to build up an
integrated picture of smoking and chewing habits in India.
The role of the government of India
The Government of India should declare unequivocally that complete
tobacco control within India is its ultimate goal. It must work out a
long-term plan to erase tobacco addiction in stages. It should also
take into full consideration its own finances, including its astronomical
foreign debt, and the various economic and social issues involved. A
practical policy at this juncture would be a mixture of both tobacco
promotion and tobacco control.
India earns a substantial amount of foreign exchange by exporting
FCV and other varieties of tobacco, and tobacco products like hookah
paste, zarda, as well as small amounts of cigarettes and bidis. In view
of its foreign debt it is imperative that India increase its exports. It
should be remembered that even the U.K. and U.S.A., which are strictly
and successfully implementing tobacco control programmes at home,
have not cut down on their cigarette manufacture nor have they stopped
dumping them in third world countries. India would do well to export
high quality products which are less harmful.
The Tobacco Board should also increase the manufacture and export
of other tobacco products like the pesticides, nicotine sulphate, vitamins,
nicotinic acid, and nicotinamide, the pharmaceutical intermediate
solanesol, and tobacco seed oil. At present, only one or two factories
in Gujarat are manufacturing these products. The Central Tobacco
Research Institute has suggested the possibility of using tobacco seed
protein as an edible protein. This has to be tested first through animal'
experiments, for toxicity and nutritive value.
In order- to bring about effective tobacco control, the Indian
government should enforce, through appropriate legislation:
1. The maximum permissible values for tar and nicotine yields of
cigarettes, (15 mg tar and 1 mg nicotine per cigarette as adopted by
the European Union). Cigarettes yielding higher amounts should be
taxed heavily. This will automatically make the cigarette companies
conform to the permitted values. Selling filter cigarettes (that are moje
expensive but yield the same or higher amounts of tar and nicotine)
rather than ordinary cigarettes is nothing short of cheating the customers
and should be made a punishable offence.
Chewing tobacco and bidi packets should carry health warnings.
Bidis should also be provided with effective filters.
There should be a strict ban on tobacco and cigarette advertising
throughout the country.
The sale of cigarettes and bidis to minors should be banned.
None of these measures will affect the revenue to .the Government of
India.
It is estimated that about 30 per cent of cigarettes in any country are
smuggled, causing the government to lose that amount of revenue.
The Government of India should safeguard against smuggling.
I
!
Companies allege that the high taxes and consequent high prices of
cigarettes, are reasons why smuggling occurs. It may thus be necessary
to optimise the tax on cigarettes.
Dr. Nigel Gray, an advocate of the anti-smoking campaign in
Australia, repeatedly warns that, ‘Multinational cigarette companies
should never be allowed to enter or establish themselves in any country.
The huge profits made by them will cause a continuous foreign
exchange drain’.
--The state governments should provide more remunerative jobs for
bidi workers as alternatives
It should also seriously consider reports of dentists, that a habitual
consumption of paan masala and gutka leads to oral submucous fibrosis
and other oral lesions.
There should be a radical change in the attitude of Indian society
towards smoking, if any tobacco control programme is to succeed.
Smoking is now an accepted practice in society.
Indians are only vaguely aware that smoking can injure one’s health;
very few know how smoking can actually harm a person. Hence, any
tobacco control programme should begin by educating the public,
about the debilitating effects of smoking. The medical profession and
the media can do this best, doctors can be invited to talk to large
gatherings, or on television, or radio. Anti-smoking messages in cinemas,
could be one of the most powerful means of reaching the masses.
Popular English and regional language dailies should also be inducted
in the campaign for non-smoking. The Hindu, a widely read popular
English daily, is already pioneering a campaign against smoking in
south India. It publishes regular articles on the adverse effects of active
and passive smoking, on the punishments meted out to offenders
who smoke in public places, and so on.
Quitting smoking
Smoking is a difficult habit to quit, once it becomes addictive. An
intensive cessation therapy produced a quit rate of only 35 per cent,
implying that the rest were unable to quit smoking.
Similar results were obtained at the end of the Interventional Trials
by the Basic Dental Research Unit of the Tata Institute of Fundamental
Research, in Ernakulam, Kerala. In spite of administering various
intervention techniques like personal communication, documentary
films, radio talks, folk plays, and cessation camps, for ten years, only
14 per cent of the addicts completely stopped using tobacco, though
some reduced their frequency of tobacco use. These studies lasting
Uli'lt 1
122
Tobacco and Areca Nut
for twenty-seven years have, undoubtedly, produced a wealth of
information on the prevalence of various tobacco and areca nut habits
in this district, and on the pathogenesis of leukoplakia, oral submucous
fibrosis and oral cancer. But, as an intervention, it was not a great
success. Once again, the same conclusion is reached: The tobacco
habit, whether smoking or chewing, is difficult to quit. It is best not to
start the habit.
A strong motivation is absolutely necessary for a person to stop
consuming tobacco. The addict could also use various aids, like nicotine
chewing gum, nicotine patches, and nicotine spray. The Central
Tobacco Research Institute can develop methods for their manufacture
in our own country. A press report published by the WHO claimed
that it would make these products available at subsidised rates. Private
‘smoking cessation clinics’ have started coming up in our country. As
they are likely to be very expensive, often beyond the means of the
average smoker, it may be better, if such clinics are started in
government hospitals. Smokers can also form self-help groups.
Protective agents
Forty years of attempting tobacco control has revealed that, firstly,
tobacco habits will persist, and cannot be eliminated overnight, and
secondly, they can be reduced only marginally, as revealed by
intervention trials. These disappointing findings led to a third approach
as to whether tobacco could be prevented from exerting its harmful
health effects, by simultaneously administering a protective agent. This
is known as chemoprevention, preventing tobacco’s harmful effects,
by counteracting it with a protective agent. Drs. Krishnan Nair, Sankara
Narayanan, and others in the Regional Cancer Centre, Trivandrum,
have investigated the effects of administering vitamin A or beta carotene
to fishermen, who regularly chewed betel quid. As many as 65 per
cent also drank alcohol, and 30 per cent smoked bidis. Vitamin A was
found to prevent the incidence of oral leukoplakia in 52 per cent of
the cases, and beta carotene, in 33 per cent. These investigations reveal
that chemoprevention is at least partially effective.
We have conducted experiments on chemoprevention of cancer in
laboratory animals. We have observed that the induction of gastric
cancer in Swiss mice by the potent carcinogen, 3, 4 benzo(a)pyrene;
and hepatomas in Wistar rats by 3’-methyl 4-dimethylam inoazobenzene,
can be effectively prevented by the simultaneous feeding of cumin
seeds (jeera). Poppy seeds (khuskhus), basil leaves (tulasi) and
Considerations, Suggestions and Future Prospects
123
ponnakanni leaves have also been found to be effective, but to a
lesser extent. Various other scientists have shown that turmeric is also
anti-carcinogenic. As we are not likely to eliminate or reduce smoking
or chewing in the near future, the possibility of preventing their adverse
health effects by consuming these plant products holds great promise.
Further work on these lines with dietary components as protective
agents should be carried out. Investigators in the West have found that
regular consumption of yellow-green fruits and vegetables reduces
significantly the incidence of breast cancer and heart diseases.
Kerala's experience
Kerala has the highest rates of tobacco addiction in India, though it
does not grow any tobacco. It is a major producer of areca nuts and
supplies it in a variety of forms (kotapakku, kalipakku, seeval) to
other states. The detailed surveys, investigations, and interventions
carried out by the Basic Dental Research Unit of the T.I.F.R. in Ernakulam
District for over twenty-§even years show that, Kerala, probably has
the highest incidence of oral cancer in India, among both men and
women. It is also the state, where the first case-control studies
confirming betel quid tobacco chewing as the root cause of oral cancer,
was carried out by Orr in 1933- The Regional Cancer Centre at
Thiruvananthapuram is presently carrying out a wide range of research
projects on oral cancer and leukoplakia and their control, with the
help of international funding. Kerala has taken the initiative in banning
smoking in public places.
The future
r
It is predicted that deaths due to tobacco consumption for the whole
world will increase from the present level of three million to about ten
million by the year 2025, out of which a death rate of seven million
will be from the developing countries. China alone will account for
two million deaths. At present deaths caused by tobacco addiction in
India, is estimated between 630,000 and one million. It is likely to be
higher in the future, because of increasing cigarette consumption, and
increased longevity. India may thus account for another two million
deaths by 2025. Lung cancer, which is a good indicator of smoking
behaviour addiction has been steadily increasing at all places in India,
as reported by Cancer Registries. Some epidemiologists have predicted
a lung cancer epidemic in India, if the present trend continues.
I
..U
urir1
124
Tobacco and Areca Nut
Many countries in Asia are now initiating precautionary measures
against the long-term ill-effects of tobacco consumption China
Malaysia, Hong Kong, Korea and Thailand have established national
coordinating organisations on tobacco control. Singapore and Thailand
have enacted very strict laws on smoking and tobacco control, and are
enforcing them too. The Ministry of Health, Government of India, has
recommended a wide range of measures for tobacco control in India;
but only some of them have been put into practice. On the whole’
India’s approach to tobacco control has been half-hearted so far. Public
opinion against tobacco use in India is yet to gather momentum.
Smoking will continue to decline steadily in the U.K. and U.S.A.,
during the coming years. There will be a progressive decrease in
mortality due to tobacco-related diseases. But, it is very doubtful, if
these countries will be able to completely eradicate smoking. There is
a growing public opinion the world over, particularly among health
lobbyists that, these countries should restrict the multinational cigarette
companies to follow certain definite norms. The U.S. and U.K. tobacco '
companies arjd their subsidiaries should adhere to the same standards '
of product, marketing, promotion and sales in developing countries,
as are required in their own countries. They should also stop
pressurising governments in developing countries to prevent passing
and implementation of anti-tobacco measures. It has been alleged that
some U.S. senators and U.S. consulates help these tobacco companies
in their export and cigarette promotional activities. In the long mn,
the U.S. and U.K. governments will earn the goodwill of the whole
world, if they put an end to the dumping of cigarettes in third world
countries.
The high prevalence of oral cancer in different regions of India has
been reported by several investigators from time to time. In Singapore,
the incidence of oral cancer among Indians is considerably greater
than among Chinese or Malay residents there. Indians in Malaysia
account for 52 per cent of the oral cancer admissions although they
form only 10 per cent of the Malaysian population. Oral cancer and
oral submucous fibrosis are common among the Indian community in
Natal, South Africa. The reason for the high prevalence of oral cancer
is the practice of chewing betel quid with tobacco.
It is well-known that chewing tobacco leads to various oral lesions,
including oral cancer. The advent of paan masala, an areca nut
preparation, has led to a vast increase in oral submucous fibrosis. The
epidemiogical investigations among Indian women in Natal, South
Africa have some common features. About 50 per cent of the women
who chew the areca nut, do so without using tobacco or betel quid.
^3
Considerations, Suggestions and Future Prospects
125
Oral submucous fibrosis occurred in 38 per cent of the people,
especially in those who chewed areca nut without betel quid. Oral
cancer among women occurred mainly in the buccal mucosa and
tongue and 65 per cent of these cancers arose in women who did not
use any tobacco. This South African investigation clearly demonstrates
that chewing areca nut, alone can lead to oral submucous fibrosis and
oral cancer. The messages from all these findings are clear. Chewing
of tobacco should be avoided, as it undoubtedly leads to oral cancer.
Habitual chewing of areca nut and areca nut preparations like paan
masala carry a high risk of oral submucous fibrosis and oral cancer,
and are therefore best avoided. Areca nut is an integral part of betel
quid. Hence, betel quid should contain only a minimum amount of
areca nut and no tobacco. It is safer to use such betel quid, for this
does not carry any significant risk for oral cancer. As an educated
community, we should restrict ourselves only to safe betel quids; our
unenviable reputation of having the highest oral cancer rates, will
then be a thing of the past.
*
Protection from exposure to second-hand tobacco smoke. Policy recomme
Appendix 3
Health effects associated with exposure to Second-hand Tobacco Smok
Summary of findings of the California Environmental Protection Agency, 2005
Effects causally associated with SHS exposure
Developmental effects
• Fetal growth: Low birth weight and decrease in birth weight
• Sudden Infant Death Syndrome (SIDS)
• Pre-term delivery
Respiratory effects
• Acute lower respiratory tract infections in children (e.g. bronchitis and pneumor
• Asthma induction and exacerbation in children and adults
• Chronic respiratory symptoms in children
• Eye and nasal irritation in adults
• Middle-ear infections in children
' Carcinogenic effects
• Lung cancer
• Nasal sinus cancer
• Breast cancer in younger, primarily premenopausal women
Cardiovascular effects
f
• Heart disease mortality
• Acute and chronic coronary heart disease morbidity
• Altered vascular properties
Effects with suggestive evidence of a causal association with SHS exposure
Reproductive and developmental effects
• Spontaneous abortion, intrauterine growth retardation
• Adverse impact on cognition and behaviour
• Allergic sensitization
• Decreased pulmonary function growth
• Adverse effects on fertility or fecundability
Cardiovascular and haematological effects
• Elevated risk of stroke in adults
Respiratory effects
• Exacerbation of cystic fibrosis
• Chronic respiratory symptoms in adults
Carcinogenic effects
• Cervical cancer
• Brain cancer and lymphomas in children
• Nasopharyngeal cancer
• All cancers - adult and child
3
Protection from exposure to second-hand tobacco smoke. Policy recommendations.|
Summary of findings of the United States Surgeon General, 2006
Reproductive and developmental effects from exposure to SHS
Sudden Infant Death Syndrome
The evidence is sufficient to infer a causal relationship between exposure to SHS
and sudden infant death syndrome.
Preterm delivery
The evidence is suggestive but not sufficient to infer a causal relationship between
maternal exposure to SHS during pregnancy and preterm delivery.
Low birth weight
The evidence is sufficient to infer a causal relationship between maternal exposure to SHS
during pregnancy and a small reduction in birth weight.'
Childhood cancer
The evidence is suggestive but not sufficient to infer a causal relationship between
prenatal and postnatal exposure to SHS and childhood cancer.
The evidence is suggestive but not sufficient to infer a causal relationship between
prenatal and postnatal exposure to SHS and childhood leukaemias.
The evidence is suggestive but not sufficient to infer a causal relationship between
prenatal and postnatal exposure to SHS and childhood lymphomas.
The evidence is suggestive but not sufficient to infer a causal relationship between
prenatal and postnatal exposure to SHS and childhood brain tumours.
Respiratory effects in children from exposure to SHS
Lower respiratory illnesses in infancy and early childhood
The evidence is sufficient to infer a causal relationship between SHS exposure from
parental smoking and lower respiratory illnesses in infants and children..
The increased risk for lower respiratory illnesses is greatest from smoking by the mother.
>'•
Middle-ear disease and Adenotons illectomy
The evidence is sufficient to infer a causal relationship between parental smoking and
middle-ear disease in children, including acute and recurrent otitis media and chronic
middle-ear effusion.
The evidence is suggestive but not sufficient to infer a causal relationship between parental
smoking and the natural history of middle-ear effusion.
Respiratory symptoms and prevalent asthma in school-age children
The evidence is sufficient to infer a causal relationship between parental smoking and
cough, phlegm, wheeze and breathlessness among school-age children.
The evidence is sufficient to infer a causal relationship between parental smoking and
ever having asthma among school-age children.
Childhood Asthma Onset
The evidence is sufficientTo infer a causal relationship between SHS exposure from
parental smoking and the onset of wheeze illnesses in early childhood.
!?
Protection from exposure to second-hand tobacco smoke. Policy recommj
The evidence is suggestive but not sufficient to infer a causal relationship betwe<
exposure from parental smoking and the onset of childhood asthma.
Lung growth and pulmonary function
The evidence is sufficient to infer a causal relationship between maternal smokii
pregnancy and persistent adverse effects on lung function across childhood.
The evidence is sufficient to infer a causal relationship between exposure to SHS
and a lower level of lung function during childhood.
Cancer among adults from exposure to SHS
Lung cancer
The evidence is sufficient to infer a causal relationship between SHS exposure ar
cancer among lifetime non-smokers. This conclusion extends to all SHS exposur
regardless of location.
The pooled evidence indicates a 20% to 30% increase in the risk of lung cancer fr
exposure associated with living with a smoker.
Breast cancer
The evidence is suggestive but not sufficient to infer a causal relationship betwee
and breast cancer.
Nasal sinus cavity and nasopharyngeal carcinoma
The evidence is suggestive but not sufficient to infer a causal relationship betwee
exposure and a risk of nasal sinus cancer among non-smokers.
Cardiovascular diseases from exposure to SHS
The evidence is sufficient to infer a causal relationship between exposure to SHS
and increased risks of coronary heart disease morbidity and mortality among bot
men and women.
Pooled relative risks from meta-analyses indicate a 25 to 30% increase in the risl
coronary heart disease from SHS exposure.
The evidence is suggestive but not sufficient to infer a causal relationship betwee
exposure and an increased risk of stroke.
Studies of SHS and subclinical vascular disease, particularly carotid arterial wall
thickening, are suggestive but not sufficient to infer a causal relationship betweei
exposure and atherosclerosis.
Respiratory effects in adults from SHS exposure
/'Odour ahd 'irritation
ftye evidence is sufficient to infer a causal relationship between SHS exposure an
| ^annoyance.
1 • The evidence is sufficient to infer a causal relationship between SHS exposure and na
\\ irritation.
'
' :
The evidence is,suggestive but not sufficient to conclude that people with nasal al
or a history of respiratory illnesses are more susceptible to developing nasal irriti
from SHS exposure. -
S3
r
234
Protection from exposure to second-hand tobacco smoke. Policy recommendations
ions.
Respiratory symptoms
The evidence is suggestive but not sufficient to infer a causal relationship between SHS
exposure and acute respiratory symptoms, including cough, wheeze, chest tightness and
difficulty breathing among people with asthma.
IS
ring
The evidence is suggestive but not sufficient to infer a causal relationship between SHS
exposure and acute respiratory symptoms including cough, wheeze, chest tightness, and
difficulty breathing among healthy people.
' birth
The evidence is suggestive but not sufficient to infer a causal relationship between SHS
exposure and chronic respiratory symptoms.
ig
Lung function
The evidence is suggestive but not sufficient to infer a causal relationship between
short-term SHS exposure and an acute decline in lung function in people with asthma.
■ HS
The evidence is suggestive but not sufficient to infer a causal relationship between chronic
second-hand smoke exposure and a small decrement in lung function in the general
population.
Asthma
The evidence is suggestive but not sufficient to infer a causal relationship between SHS
exposure and adult-onset asthma.
S
The evidence is suggestive but not sufficient to infer a causal relationship between SHS
exposure and a worsening of asthma control.
S
'
S
&
•ur
?s
.......
Chronic obstructive pulmonary disease
The evidence is suggestive but not sufficient to infer a causal relationship between SHS
exposure and risk for chronic obstructive pulmonary disease.
Appendix 4
compared to 36pg/m3 in premi
Countering the opposition
smoking was not observed durinc
toring period.42 This level is more t
While effective smoke-free laws are popular,
policy-makers must be prepared to respond
to many, often-made arguments aimed at dis
suading their passage and implementation.
These arguments generally involve ideological
issues; challenges to science on the health
effects of SHS exposure; proposals for alter
natives to smoke-free laws; the economic and
other negative effects of smoke-free laws as
well as the feasibility of implementation and
enforcement.
Previous sections provide background infor
mation that can be used to refute many of these
arguments. Below are other common argu
ments not found in these sections with their
responses.
The risks of involuntary” smoking are trivial,
particularly compared to other health issues
This claim has often been made respecting lung
cancer. The increase in risk fora never smoker
married to a smoker is about 20% compared to
that for a never smoker married to a never
smoker. As many scientific publications have
shown, a 20% increase in risk is substantial, both
at the individual and population levels for an
exposure that is so widespread. Highly exposed
individuals, such as bar and restaurant’work
ers, may have far higher risks than the popula
tion average. The risks associated with heart
disease are even larger and more immediate
than for lung cancer.
The levels of toxic emissions from cigarettes
are low compared to other air contaminants
On the contrary, they are exceptionally high
compared with most other environmental and
workplace toxins.14 The air pollution emitted
by cigarettes is 10 times greater than diesel
car exhaust.150 Moreover, a recent study of fine
particulate matter PM25° exposure in indoor
smoking and smoke-free settings in 24 countries
found an average level of PM25 of 317 pg/m3in locations were there was tobacco smoking
the WHO general air quality guid
recommend nhaximum 24-hour n
sures of 25 pg/m3. 151 In fact, wor
United States exposed to tobacco !
regular basis during their working
risk of cancer that is between 7 an,
higher than levels established as c
for exposures to contaminants
SHS.138
Epidemiology, the basis for risk ei
exposure to SHS, is “junk science
Use of the pejorative term "junk .•
describe the scientific method of ef
can be traced back to the tobacco ir
other industries, which are fearful c
cations that epidemiological researc
for their products. Tobacco industry
have left an extensive trail showing a
effort to discredit it. A well-establisl
mental science of public health, ep
is the scientific method for directb
information on the health effects ol
as received in natural settings,
approaches employed successfully I
SHS have been used over decade;
tious diseases and for major acute
ic diseases. Epidemiological evid<
foundation for public policy ih many
as infection control and managemer
water pollution.
Smoke-free laws are unconstitu
violate the personal rights and I
smokers.
This argument states that smoking i
al choice for adults and that legislatic
smoke-free environments victimizes;
tizes smokers and sets a dangerous
about the reach of the state. Howev
free legislation does not say that sit
not smoke; it only limits where smokin
sible to prevent smokers from harrr
P S *3
?re
niuld
iat
In addition, there is no Tight to smoke" in any
national constitution or international human
rights law.152 Conversely, the right to life, the
right to the "enjoyment of the highest attainable
•ohe
i a
standard of health," the right to a healthy envi
ronment and other rights relevant to protection
from exposure to tobacco smoke are found in
»a
es
numerous international human rights laws.138
us
Universal application of smoke-free laws is
not realistic or appropriate for developing
countries.
an
to
The goal of universal protection is also equally
valid in high- and low-income jurisdictions,
although the means for achieving it may differ.
There may be a perception that developing
gy
id
countries cannot afford to implement smokefree laws, but in reality modest resources are
li-
needed to implement these laws; costs go down
dramatically following implementation of the
laws and improved public health will reduce
health-care costs.
of
✓e
ts
?d
ig
JS
Comprehensive smoke-free laws are
culturally inappropriate in many places
National, provincial and local governments in
'9
varied cultural and ethnic settings and in devel
oped and developing countries have shown that
e
comprehensive smoke-free laws are feasible
and successful regardless of a country's income
level, language or ethnic background. In Ireland
ie
h
d
it was argued that smoking was an essential
component of the pub atmosphere, yet Ireland
has been smoke-free for more than two years
with overwhelming public support. Spanish-
d
if
and French-speaking countries are often cited
as places that could never become smoke-free
because smoking is such an integral part of
their culture. Yet Uruguay is smoke-free, a
g
majority of the French population supports
t
smoke-free bars and restaurants, and the
French-speaking province of Quebec in Canada
became smoke-free (including in bars and
restaurants) on 31 May 2006.
Universal application can only be achieve
gradually
When smoke-free environments becam
increasingly widespread in North America an
other developed countries throughout the 198C
and 1990s, the pace was incremental, wit
smoke-free environments being introduce
gradually on a sector-by-sector basis. This wa
usually necessary because the public was les
aware of the damage caused by SHS exposur
and because smoke-free environments wer
not a familiar part of the public consciousnes:
An incremental approach may be the only prac
tical initial option for some countries, but
may not be required i.n others. The benchmar
for smoke-free environments is now far highe
than when policies first began to be imple
mented, and this has made rapid change fc
more feasible. The many case studies no1
available show that jurisdictions can go an
have gone from virtually no smoke-free legisle
tion to comprehensive 100% smoke-free legisle
tion in a single step. Scotland and Uruguay ar
just two significant examples of this.
Smoke-free environments cannot be imple
mented unless combined with support to hel
smokers quit
The success of smoke-free laws is not dependei
upon providing cessation programmes in smok(
free.settings. Programmes to help smokers qi
in settings that become smoke-free can send
supportive message to smokers reminding thei
that smoke-free policies are not meant to isola
them but to protect everyone's health. Howeve
experience shows that they are not necessary fc
smooth implementation of smoke-free law
While smoking'cessatiiin programmes can be
useful ancillary intervention to smoke-free env
ronments if resources are available, lack <
resources for smoking cessation programme
should not delay implementation of smoke-fre
environments. Protection of public health is th
primary goal of smoke-free environment
n Also known as passive smoking
o PM2.5 are harmful fine particles that are easily inhaled deep into the lungs and are emitted in large quantities from burning cigarett
E
Protection from exposure to second-hand tobacco smoke. Policy recommen
Studies quoted by opposition groups i
What if they
passed a law
that took away
30% of your
business?
dire economic effects from smokenormally rely on subjective data or do
uate objective data with acceptable
methods. Data may also be reported o
text. For example, opponents of Ireland
free law noted that receipts for beer a
in pubs declined following implemer
the law. What they failed to mention is
trend began before the law came into e
did not worsen as a result of the law.1
Tobacco industry front groups have
iirhit happen* if ynur si ate lefltslaiure
a restaurant that prohibits smoking
W omi/rounrilbaM smoking m
Can you risk closing your door* ro 20
mlauranls?
percent ot yaor customers?
YouH kne busUxns. Maybe as much
The Tciiacco Institute can help you
as M percent rrfyour bustneM. arcording
make sure this never happens.
io restaurant owners who have
Write us and well send you
riprrlenced aueh bans. Before a
information on how other restaurant
smoking ban was repealed InBeaerty
groups have fought smoking ban*. Wen
Hills, rcalau rants were expecting to
into
lose
help you derelop ways to accommodate
198? as
a resuh.
*8 your customers—smokers and nona touto(ai2million In 198?
*•>
reeul..
Here’s the real npn. tliough.
V Ina
In a
smokers alike. AndarcH hdpyou ensure
recent Gallup pon almost 20
40
that your voice Is heard
perrrra W the U.Spopula' I rll Im* a';,'A,;?1-"
when government take* up
Uon said they would not visit
I'll ww—w oc »«>>•
the Issue.
many studies presenting as data the pr
or opinions of a select group of bar
These predictions always turn out to t
as the tobacco industry itself has i
(Figs. 3, 4).
Restaurant Revenues (Millions of Dollars)
$30
Fig-r. 3 The Tobacco Institute ran this ad in California in the late
1980s. The president of the Beverly Hills Restaurant
Association, Barry Fogel, later testified that. "There was
no Beverly Hills Restaurant Association before the smokefree ordinance. H/e were organized by the tobacco indus
try. The tobacco industry repeatedly claimed that Beverly
Hills restaurants suffered a 30% decline in revenues dur
ing the five months that the [original] smoke-free ordi
nance was in effect. Figures from the State Board of
Equalization using sales tax data, however, showed a
slight increase in restaurant sales. ~ Vogel went on to say
that he regretted his participation in opposing the law.
The chart below shows the industry's claim versus actual
sales in Beverly Hills.
Actual Revenues ..
< /
$25
X-
$20
X
Tobacco Industry Claim
$15
$10
$5
$0
1986
1987
1988
Fig. 4 Actual revenues vs tobacco industry claim
Smoke-free laws will reduce business in the
hospitality sector and harm tourism.
The impact of smoke-free legislation on employ
ment and business has been studied in dozens
of jurisdictions. Not a single study using objec
tive data and sound research methodology has
found an overall negative impact of smoke-free
legislation association.451153 The effects are uni
formly neutral or positive, with little short-term
effect on the hospitality business and some pos
itive effects in the long-term as non-smokers
start going to bars and other venues that they
once avoided because of second-hand smoke.
E3
Some places have promoted smoke-fi
ronments in their tourism campaign'
nizing that many visitors will value th
tunity to enjoy entertainment without
smoke (Fig. 5).
I
Protection from exposure to second-hand tobacco smoke. Policy recommendations.
ating
laws
Bval-
Smoke-free workplaces will cause smokers
to smoke more in the home, thus increasing
children’s exposure to SHS.
There is no evidence that smoke-free work
itific
con-
places will increase children’s exposure to
oke-
tobacco smoke at home. Indeed, a growing
body of evidence suggests that legislation ban
ning smoking in public places and workplaces
)irits
in of
this
and
leads to a reduction in smoking in the home.
Smoke-free workplaces encourage smokers
to quit. The reduction in smoking among adults
means that fewer children are likely to be
ised
ions
exposed to smoke at home. Smoke-free work
places are associated with a greater likelihood
ers.
ong,
of workers implementing smoke-free policies
in their homes.155
tted
Fig. 5 Norway's tourist promotions highlight its smoke-free
policies.
100% smoke-free environments are not
enforceable: people will not obey the laws.
The reality is just the opposite. Unclear laws that
designate square footage or percentages for
189
non-smoking and smoking sections; prohibit
smoking only during certain hours in specific
establishments; or set requirements for DSRs
create confusion for institutions implementing
nvi-
the law, and for employees and customers and
inspectors enforcing the law.
og'orcco
On the other hand, if the law simply requires
a certain type of institution (such as schools
or retail establishments) to be 100% smokef
free, building managers and owners know that
they cannot permit any smoking in their build
ing, employees and customers know that they
cannot smoke in the establishment, and
inspectors know immediately if an institution
is complying with the law: either someone is
smoking inside or no one is smoking inside.
SOCIAL
SCIENCE
------- &-------
ELSEVIER
MEDICINE
Social Science & Medicine 66 (2008) 1356 1367
www.elsevier.com/locate/socscimed
Crowding out effect of tobacco expenditure and its implications
on household resource allocation in India*
Rijo M. John*
University of California San Francisco, Center for Tobacco Control Research and Education.
530 Parnassus Avenue, STE 366, San Francisco, CA 94143, USA
Available online 9 January 2008
Abstract
This paper examines whether spending on tobacco crowds out expenditure on basic needs and whether it has implications on
nutrition intake and household resource allocation in India. The paper uses a household sample survey from India for the year
1999—2000. A system of quadratic conditional Engel curves was estimated for a set of 10 broad groups of commodities. The results
suggest that tobacco consuming households had lower consumption of certain commodities such as milk, education, clean fuels and
entertainment which may have more direct bearing on women and children in the household than on men suggesting possible
' ‘gender effects’ and biases in the allocation of goods and services within th'e household. Tobacco spending was also found to
have negative effects on per capita nutrition intake. The nature of crowding out was found to be similar in low- and high-income
households.
© 2007 Elsevier Ltd. All rights reserved.
Keywords: Tobacco; Consumption; Poverty; Crowd out; India; Expenditure; Gender
Introduction
Expenditure on tobacco occupies a significant
portion of household budgets in many developing and
developed countries. It varies from close to 1% in coun
tries such as Mexico and Hong Kong to nearly 10% in
Zimbabwe and China (Selvanathan & Selvanathan,
2005; Wang, Sindelar, & Busch, 2006). In developing
countries, where people in general are relatively
* This work was supported in part by a fellowship award from the
Indira Gandhi Institute of Development Research, Mumbai, India and
in part by a fellowship provided by a grant from the National Cancer
Institute (CA-113710).
♦ Tel.: +1 415 476 3139; fax: +1 415 514 9345.
E-mail addresses: rijo.john@ucsf.edu; rmjohn@gmail.com
0277-9536/$ - see front matter © 2007 Elsevier Ltd. All rights reserved,
doi: 10.1016/j.socsci med.2007.11.020
constrained by money, it is reasonable to expect that
the expenditure on tobacco will have higher opportunity
cost in terms of reduced expenditure on basic goods
such as food, education and energy over and above
the direct health consequences of tobacco consumption.
Most studies on tobacco consumption overlook the
nature of crowding out that occurs due to spending on
tobacco. Internationally, there is a dearth of sufficient
empirical evidence to show whether tobacco spending
actually crowds out the consumption of other goods in
ways affecting the well being of household members.
A few studies, however, address this issue in some
detail. The pioneering work in this area came from Ban
gladesh in a study by Efroymson et al. (2001) which
demonstrated that tobacco expenditures exacerbated
the effects of poverty and caused deterioration in living
R.M. John / Social Science & Medicine 66 (2008) 1356-1367
Standards among the poor. Using data from New Zea
land, Thomson, Wilson, ODea, Reid, and HowdenChapman (2002) found that if second lowest income
decile households with smokers were to be smokerfree this would on average allow an estimated 14% of
the non-housing budgets of those households to be real
located. These studies were early attempts to address
the issue of crowding out due to spending on .tobacco
and are based on descriptive observations of data. Using
data from the US population, Busch, Jofie-Bonet,
Falba, and Sindelar (2004) found evidence indicating
crowding' out of housing expenditures as a result of
spending on smoking. In an attempt to explain whether
spending on tobacco drives out critical expenditures,
Wang et al. (2006) found that in rural China, tobacco
spending leads to a reduction in expenditures on educa
tion, health, insurance and investment in farming. How
ever, since authors have modeled expenditure shaies of
these.items as functions of expenditures on tobacco
there is an issue of endogeneity. This is because given
the total budget there is simultaneity involved in con
sumption decisions. Unless one explicitly accounts for
this endogeneity using certain instrumental variables,
it may have the effect of rendering the estimates biased
and inconsistent.
This paper takes the case of India to closely examine
the issue of crowding out for a variety of reasons. India is
the third largest producer of tobacco (Food and Agricul
tural Organization, 2007) and the second largest cons
umer of unmanufactured tobacco in the world (Reddy
& Gupta, 2004). India is home to nearly 17% of smokers
in the world (Shimkhada & Peabody, 2003), with an
estimated 46.5% of all men and 13.8% of all women con
suming some form of tobacco (Rani, Bonu, Jha, Nguyen,
& Jamjoum, 2003). India has one of the highest rates of
oral cancer, a direct result of tobacco use, in the world
(Shimkhada & Peabody, 2003). Previous studies (Gupta
& Sankar, 2003; John, 2005; Rani et al., 2003; Subrama
nian, Nandy, Kelly, Gordon, & Smith, 2004) have shown
that prevalence of tobacco consumption in India is
higher among the low-income groups. Roughly, a quarter
of India’s population of more than a billion persons live
under the official poverty line. An average individual
spends around Rs. 486 in rural India and Rs. 855 in urban
India on monthly expenses as per the 1999-2000
National Sample Survey (NSSO, 2000). (The exchange
rate for Indian Rupees was roughly Rs. 46.5 per US Dollar
during this period.) Thus, in India, a thriving tobacco
industry coexists with low income and poverty. Hence,
consumption of tobacco in India is a concern not only
due to its consequent high morbidity and mortality but
also due to the opportunity cost of spending on tobacco.
1357
Spending on tobacco may also generate biases in the
household allocation of goods and services due to many
reasons. In India, tobacco use is primarily an adult male
activity with a prevalence of 47% among men and 14%
among women in the age group 15 years and older (Ram
et al., 2003). Moreover, many Indian households, espe
cially in rural areas, are characterized by the age-old
patriarchy, with many household consumption deci
sions being made by the adult male members. MenonSen and Kumar (2001) note that “Indian women are
marginalized in decision making and leadership by a
variety of processes that begin in infancy.” The National
Family Health Survey (UPS, 2000, p. 66) shows that
more than 50% of married rural Indian women play
no role in household decisions regarding purchases.
This figure is 40% in urban India. Children also may
bear the brunt of constrained incomes, and parents
with a strong taste for adult goods are known to discrim
inate against female children (Subramanian & Deaton,
1991). Hence, it*can be suspected that women and chil
dren are affected by the tobacco spending decision of
a few (mostly adult male) members in a household.
Data and preliminary results
Household cross section data from the National
Sample Survey Organization (NSSO) collected during
the period July 1999-June 2000 under the auspices of
the Ministry of Statistics and Programme Implementa
tion, Government of India (NSSO, 2000) was used for
this study, with similar data from a previous period
(July 1993—June 1994) as a check of the robustness
of the findings. The data contain information on con
sumption for a wide variety of goods from 120,309
households spread across 10,140 villages m India.
This nationally representative and official household
consumption survey collected information on consump
tion of over 500 commodities over a 30-day recall
period. Expenditures on 10 distinct categories which
are exhaustive and mutually exclusive, including food,
education, health care, and entertainment were consid
ered for the analysis in this paper, though for certain
groups disaggregated items were examined to address
specific issues.
A categorical variable indicating each household’s
tobacco expenditure status was constructed first. This
categorical variable divided the sample into four
mutually exclusive and exhaustive groups: households
with no-, low-, moderate-, and high-tobacco spending
denoted as NoSpend, LSpend, MSpend and HSpend,
respectively. Conditional on having positive tobacco
expenditures, if the budget share spent on tobacco is
1358
R.M. John I Social Science & Medicine 66 (2008) 1356—1367
in the first 20 percentile of the distribution of budget
shares on tobacco of the positive tobacco spending
households, such households were defined as lowtobacco spending households. Similarly, if they are in
the 20th—80th percentile or 80th—100th percentile,
they are categorized as moderate- and high-tobacco
spending households, respectively. This classification
is purely arbitrary and is done only to see the severity
of crowding out among higher tobacco spenders and
is used only for the descriptive analysis. A dummy vari
able taking values 1 and 0 for positive tobacco spending
and no spending, respectively, was also constructed.
Analyses are carried out separately for both rural and
urban India.
Table 1 presents a summary of expenditure and bud
get shares allocated to tobacco by the tobacco consump
tion status of households for different expenditure
groups in rural and urban India. The middle-income
group represents households between the 30th and
70th percentile of the distribution of monthly per .capita
consumption expenditure of households. Lower and
higher income groups are those below and above this
range. It can be seen that households with positive
tobacco expenditure have higher total monthly average
expenditure versus those without tobacco expenditure
in rural India. This is true for all the income groups in
rural India and low- and middle-income groups in urban
India. However, monthly per capita expenditure is
lower among tobacco consuming households compared
to others, which is due to the fact that the average
household size is higher among tobacco consuming
households (5.4 and 4.92 in rural and urban India)
than non-tobacco consuming households (4.4 and 4.3
in rural and urban India). In addition, within the tobacco
consuming households the average monthly expendi
ture declines as one moves from category LSpend to
HSpend while the average monthly per capita expendi
ture does not decline.
While LSpend households in rural India spent 0.54%
of their budget on tobacco the HSpend category spent as
much as 6.30% of their budget on consuming tobacco in
the all-income groups. These figures are 0.5 and 7.24%
• in urban India. Though prevalence of tobacco use is
higher among the poor, as a share of their total budget
poor households spent slightly less than their richer
counterparts in India. This is in contrast to some previ
ous studies (de Beyer, Lovelace, & Yurekli, 2001;
Nichter & Cartwright, 1991; Shah & Vaite, 2002) which
found that the poor spent more of their income on
tobacco compared to the rich.
Table 2 gives the results of Student’s /-test for the
differences in mean expenditures between the tobacco
Table I
Summary averages
Urban
Rural
NoSpend
TotTob
LSpend
MSpend
HSpend
NoSpend
TotTob
LSpend
MSpend
HSpend
All income
Monthly household expenditure
Monthly per capita expenditure
Expenditure on tobacco
Share on tobacco
2361
534
0
0.00
2498
2919
462
482
15
61
0.54
2.66
2493
455
53
2.15
4086
2090
461
958
132
0
6.30
0.00
3536
719
92
2.93
3480
4331
695
759
78
20
0.50
2.31
2907
755
209
7.24
Low income
Monthly household expenditure
Monthly per capita expenditure
Expenditure on tobacco
Share on tobacco
1482
292
0
0.00
1778
294
43
2.56
1944
295
11
0.57
1784
294
37
2.11
2264
1577
430
295
93
0
6.16
0.00
2455
419
64
2.84
2480
2795
417
425
57
14
2.33
053
2037
421
137
6.84
Middle income
Monthly household expenditure
Monthly per capita expenditure
Expenditure on tobacco
Share on tobacco
2140
486
0
0.00
2535
477
62
2.68
2824
476
14
0.53
2568
477
56
2.19
2160
478
129
6.19
3541
813
0
0.00
3686
785
91
2.81
4389
789
21
0.49
3668
777
81
2.27
2907
810
210
7.32
3549
3824
4944
937
879
94
24
2.82
0.51
3811
858
79
2.13
2800
864
201
6.75
6236
1864
0
0.00
5658
1742
158
3.38
5632
7485
1747
1793
124
32
2.34
0.46
4334
1668
325
7.78
High income
Monthly household expenditure
Monthly per capita expenditure
Expenditure on tobacco
Share on tobacco
937
0
0.00
Notes: expenditure in Rs. and share in percentages. LSpend, MSpend and HSpend represent 0—20, 20—80 and 80—100 percentile, respectively, of
positive tobacco spending households. Similarly, TotTob is for all the tobacco consuming households and NoSpend is for the rest. All figures are
weighted by appropriate sampling weights and hence are representative figures.
1
1359
R.M. John I Social Science & Medicine 66 (2008) 1356 1367
Table 2
T-Tes| for the differences in mean of shares between tobacco users and non-users (55th round: year 1999—2000)
Urban India
Rural India
Categories
Difference
/-stat
Difference
r-stat
Food
Cereals and cereal substitutes
Fruits
Pulses
Milk
Edible oil
Non-veg
Vegetables
Beverages
-0.148
-3.773
‘0.451
0.088
0.975
0.1 ?3
-0.176
-0.068
2.068
-1.65
-41.69
28.63
4.43
15.57
_ 7.87
-5.57
-2.57
29.43
-2.538
-3.997
0.513
-0.267
1.409
-0.256
-0.970
-0.693
2.248
-21.90
-47.06
28.27
-14.59
24.90
-14.76
-26.24
-23.48
20.64
Pan
Alcohol
Fuel and light
Firewood
Dung cake
-0.089
-0.670
0.447
-0.184
-0.333
-7.64
-35.33
13.80
-6.84
-20.82
-0.209
-0.896
-0.269
-0.848
-0.229
-17.12
-34.96
-7.41
-35.23
-24.74
0.070
0.555
0.023
0.130
0.083
0.791
0.025
0.457
0.026
2.57
23.49
0.44
4.36
9.78
26.31
3.41
19.23
e 6.80
0.115
1.359
-0.249
0.034
0.298
1.531
0.053
0.297
0.076
4.31
31.34
-4.63
0.94
19.57
33.90
3.34
10.24
11.28
Clothing
Education
Medical non-institutional
Medical institutional
Entertainment
Conveyance
Railfare
Bus/tram
Schoolbus
3.93
0.191
-0.80
Durables
—0.026
45.46
3.557
_______
36.55
_______________
Other
' A90
Notes: difference shows ‘mean of non-users’ — ‘mean of users’ . The indented items in the first column are subgroups and may or may not sum to the
total of the group above it.
/-Stat shows the Student /-statistics for the Ho: mean (non-users) - mean (users) = 0 for each of the goods.
All differences in columns 2 and 4 with the corresponding absolute value of /-statistics greater than 2 are statistically significant at 5 /o level.
consuming and non-consuming households. Detailed
tables describing actual differences in broad commod
ity-wise expenditures and shares for rural and urban
households by tobacco consumption status are not
reported here but can be made available upon request.
Statistically significant differences in budget shares
are observed between tobacco consumers and non
consumers in all expenditure heads except food, medi
cal non-institutional expenses and durables in rural
India and medical institutional expenses in urban India.
A brief discussion of these patterns for each expenditure
aggregates is given below.
Food
Roughly 62% of the rural and 54% of the urban
household expenditure was spent on food consumption
in India in the year 1999—2000. This reflects the extent
of poverty and low-income levels in this country. How
ever, food expenditure is considerably lower among the
high-tobacco spending category especially in rural
areas. This may have implications for the nutrition
intake of households in this category, a factor which
is examined later. Even though the difference in budget
share on food is not significant between tobacco con
suming and non-consuming households in rural India,
it is observed that tobacco consumers allocate more of
their budget to cereals and cereal substitutes versus
non-tobacco consumers. In contrast, milk and milk
products, an item mostly consumed by children, is
a highly compromised item among tobacco consuming
households. Consumption of fruits and beverages is also
compromised in a similar way. This is supportive of
evidence from elsewhere in the literature (Thomson
et al., 2002) indicating that tobacco spending is likely
to affect the level of food quality and nutrition available
to children.
Alcohol and Pan
In India, average monthly consumer expenditure on
alcohol is roughly half of the expenditure on tobacco
1360
R.M. John I Social Science & Medicine 66 (2008) 1356—1367
according to NSSO data. Budget share spent on alco
holic drinks by the non-tobacco consuming households
is a mere 0.39% in rural India and 0.22% in urban
India. In contrast, the high-tobacco spending category
households have alcohol expenditure 1.46 and 1.56%
of the budget, respectively, in rural and urban India.
Spending on Pan (betel-quid chewing) is also higher
among tobacco consumers. As tobacco consumers
tend to spend more on alcohol it leaves them more
impoverished with less disposable income to spend
on other commodities.
Fuel and light
Overall fuel and light expenditure is lower among
tobacco consumers in rural India and higher in urban
India. But a closer examination of expenditure shares
within the fuel and-light category shows interesting
patterns. Households with tobacco spending systemat
ically allocate more of their budget to unclean fuels
such as firewood and dung cake. This pattern was
also observed from the previous period of data that
was examined. This observation prompts one to ask,
what drives tobacco consuming households to allo
cate significantly more share on unclean fuels than
clean Tuels? A study by World Bank (2002, p. 158)
observes “for the rural poor (in India), the more
dominant economic decision-making power and pref
erences of men play a significant role in fuel use
choices at the household level, while women continue
to bear the burden of collecting fuel wood and use it
for cooking, thus exposing themselves to highest
levels of indoor air pollution.” More detailed studies
are required to explain and establish any potential
links between tobacco consumption and household
fuel choice decisions.
Clothing
Budget share spent on clothing is higher among non
tobacco households compared to tobacco consuming
households in rural and urban areas.
Education and transport
Educational expenditures are significantly lower
among tobacco households. It was also observed that,
expenditures on school buses are significantly lower
among them. This suggests that children may bear the
brunt of tobacco consumption by adult members in
a household by way of less allocation to education
and transportation. However, as noted before, this also
cannot be taken as causal evidence linking tobacco con
sumption and access to education, though it certainly
points to possible biases in resource allocation within
households.
Health care
Medical institutional and non-institutional expenses
are slightly lower among tobacco consuming house
holds. /-Tests reveal that medical non-institutional
expenses are statistically different between tobacco
users and others among urban households but not
among rural households. On the other hand, medical
institutional expenses are significantly different among
rural households but not among urban households.
Entertainment
Entertainment is another expenditure that seems to
have been compromised by tobacco spending house
holds across all groups analyzed. Decreased spending
on entertainment within a family may have implications
on intra-household dynamics, as entertainment is often
an avenue for spending quality time together with fam
ily members.
Durables
Durables are a highly aggregated item consisting of
a variety of durable goods such as furniture, jewelry,
household appliances, residential buildings and land.
Expenditures on durables are lower among tobacco
using households in urban households but not in rural
households.
A similar analysis using an earlier round (50th) of
data from the year 1993—1994 was carried out to ensure
that the findings are not a matter of chance from a single
cross section. The patterns of crowding out from this
data was found to be similar though differing in magni
tudes. The results are not described here but can be
made available on request.
The differences in consumption expenditures ob
served for certain items above do not control for house
hold specific characteristics such as household
demographics and other socioeconomic characteristics
of households. Moreover, there is simultaneity involved
in purchase decisions. One has to control for these other
characteristics to examine the crowding out effects
properly. One must also check whether preferences of
tobacco consuming and non-consuming households
are fundamentally different leading to their differing
consumption choices. This warrants a more robust
... M
R.M. John / Social Science & Medicine 66 (200S) 1356-1367
gives what are called conditional demand functions
which can be written as:
econometric analysis of household consumption pat
terns which is done in the subsequent sections.
A conditional demand model, conditional on the
consumption of tobacco, is estimated to.
a;
1. Test whether tobacco users and non-users have dif
ferent preferences over the other commodities, and
2. Examine statistically the nature of crowding out of
other goods due to tobacco spending controlling
for household specific characteristics.
Conditional demand
Let us say household preferences, given a vector of
characteristics (a), can be represented by a utility
function U = U(xh ..., .r„;a) where xf denotes its con
sumption of ith good. Given the prices of all goods,
(Pl, •••, Pn} household maximizes its utility subject .
to a budget constraint, i.e.,
Max U
^(a'),...,^,^)
n
SA^PiXi
Y
(1)
where Y denotes total expenditure. The solution to this
maximization problem will yield the normal uncondi
tional demand curves for each of the goods as a function
of Y and the vector of all prices denoted by P given the
set of household characteristics, i.e.,
(2)
Xi
Following Pollak (1969), let us say that household’s
consumption of one good has been predetermined. In
this case, let us say household has already decided its
budget on tobacco consumption and a certain amount
has been already “preallocated” for it. This effectively
means that the household now has to maximize its util
ity subject to the expenditure in excess of the preallo
cated expenditure for tobacco. If tobacco is the nth
good, assume that the first n - 1 goods are available
in the market for the prices {pi,
pn-\} over which
the household has no control and the total expenditure
on these goods are given by M (M = Y - prt, where ptt
is the expenditure on tobacco). Now the utility maximi
zation problem for the household will become.
s.t^PiXi
Max U
1361
(3)
i=i
_' additional
i =xn where
xn denotes
with the
constraint
xn
household’s demand for tobacco. The solution for this
maximization problem, solving only for n - 1 goods.
(4)
The function
above is the conditional demand
function for the /th good conditional on the consump
tion of nth good (here tobacco). Thus one gets the de
mand for the other commodities as a function of their
own price, prices of all goods except the conditioning
goods, total expenditures excess of expenditures on
the conditioning goods and the quantities of the condi
tioning goods. It is advantageous to use conditional
demand functions especially when dealing with goods
that are not consumed by many households, e.g.,
tobacco (Browning & Meghir, 1991).
Conditional demand functions can be conveniently
used to test whether zero expenditures on tobacco arise
from comer solutions or sheer abstention. There may be
a large number of households reporting zero consump
tion of tobacco simply because they do not want to con
sume it However, theoretically, when one observes
a large proportion of zeros against the consumption of
tobacco in a cross-sectional consumer expenditure sur
vey, it cannot be concluded that all of them resulted
from pure abstention. Ignoring the possibility of infre
quent purchases, a zero consumption of tobacco can
result either due to comer solutions, resulting from the
budget constraint, or sheer abstention. From the point
of view of demand functions, comer solutions mean
purchases are not made because prices are at unafford
able levels and if the prices actually decrease there may
be positive purchases by the same consumers who had
not purchased previously. But if abstention is the actua
cause of zeros, it typically means tobacco users and non
users have different preferences. Theoretically there is
no a priori reason why one should assume either case
though for all practical purposes one may have reasons
to believe that abstention could well be the predominant
reason behind such zeros. If abstention is the reason
then an estimation of demand functions for tobacco
should only have tobacco consuming households in it.
Hence one needs to statistically test whether such zeros
are due to abstention or comer solutions. A simple test is
developed (Vermeulen, 2003) for this purpose by aug
menting the conditional demand function with a binary
variable indicating the status of tobacco consumption.
A necessary condition for zeros on tobacco to corre
spond to comer solutions is that both tobacco users and
non-users behave according to the demand function as
given in Eq. (4), which would mean that some con
sumers do not preallocate money to tobacco simply
1362
R.M. John I Social Science & Medicine 66 (2008) 1356-1367
because they are constrained by budget. A simple test of
null hypothesis of corner solutions consists of testing
whether the demand function 4 depends on a binary
variable d, which indicates whether positive (d= 1) or
zero (d = 0) expenditures on tobacco are observed. If
this conditioning binary indicator is significant in the
demand for the other commodities for all households,
it would mean that both tobacco users and non-users
behave differently and would reject the null hypothesis
of zeros arising from comer solutions, supporting absti
nence as the cause. On the other hand, if the binary in
dicator d is insignificant it is not sufficient for rejecting
zeros to be derived from abstention. “It is possible that
both smokers and non-smokers have the same (condi
tional) preferences on the rest of the commodity bundle
(so that the null hypothesis would not be rejected), but
that tobacco acts as an argument in a smoker’s full util
ity function, which is not true for non-smokers in the
case of abstention” (Vermeulen, 2003). This test can
also be seen as a test of whether tobacco is weakly sep
arable from the consumption of other commodities.
Separability of X/ from d (i.e., if d is insignificant) im
plies that if a household starts allocating money for to
bacco, this only generates an income effect and no
substitution effect on the rest of the commodity bundle
(apart from the substitution effects if x, is not separable
from tobacco consumption).
The empirical implementation of this model requires
a specific functional form for the U in Eq. (3). The paper
now turns to this issue.
Quadratic almost ideal demand system
Empirically, the objective is to estimate the changes
in budget shares allocated for various goods of interest
due to the changes in expenditure allocated to tobacco.
Since direct price information is not available for all
goods of interest one can only estimate Engel curves
(in this context, conditional Engel curves) instead of de
mand functions as in Eq. (4). The Engel curves from
Quadratic Almost Ideal Demand System (QUAIDS) de
veloped by Banks, Blundell, and Lewbel (1997) were
used here. While being consistent with the utility theory
QUAIDS permits goods to be “luxuries at some income
levels and necessities at others” with the presence of
a quadratic income term on the RHS.
Incorporating household characteristics (a), condi
tioning expenditures on tobacco (p/) and possible het
erogenous preferences of tobacco users and non-users
via a categorical variable J, the following conditional
Engel curves for 10 broad goods of interest were
estimated.
Wj = (alf- + a2id + oc^Ptt + 5'a) 4- (^j,- 4+ (rli + T2,'i)(lnM)2
(5)
where w, = p/ty,/x is the budget share of commodity i in
the remaining budget excess of expenditures on to
bacco, ptt is the expenditure on tobacco and M is the
total expenditure minus the expense on tobacco. The
set of demographic and socioeconomic characteristics
of the household (a), include log of household size, ratio
of number of adults (14 years or older) to household
size, average education (total education received by
all the members in years divided by the household
size) of the household, years of education received by
the most educated member in the household, dummies
for different religious groups, social groups and occupa
tional groups. An indicator variable to control for any
effect of residing in tobacco producing states was also
included. Seven region dummies were introduced to
eliminate broad regional taste differences, if any.
The regressors associated with M and the regressor
ptt are potentially endogenous. The Durbin—
Wu—Hausman test for exogeneity (Davidson & Mac
Kinnon, 1993, pp. 237-240) was carried out for the
set of explanatory variables. This tests the null hypoth
esis Hq. Regressors are exogenous. A rejection of the
null indicates regressors are endogenous and hence in
strumental variables techniques are required. Results
of these tests are not reported here. Both M and ptt
were found to be endogenous in most cases except
a few. Hence, instrumental variable methods were
used, which produce consistent and unbiased estimates.
The groups expenditure M was instrumented by the total
expenditure and pX by the ratio of adult (14 years or
older) males to adult females (adult sex ratio). The de
cision to use the total household expenditure to instru
ment M was guided by Keen (1986) and Vermeulen
(2003) which resort to a similar approach. Adult sex
ratio was thought to be a good instrument for tobacco
expenditure since tobacco consumption in India is con
centrated more among the adult males, and hence this
variable is expected to be positively correlated with
tobacco expenditure while being uncorrelated with the
error term, a condition necessary to qualify as an instru
ment. One may also expect some of the dependent
variables to be correlated with the disturbances of
some other equations (contemporaneous correlation).
Because of this, one should use an estimation method
which is robust to the use of instrumental variables
along with Seemingly Unrelated Regression (SUR).
Hence, the paper estimates the system of Engel curves
using Three-stage Least Squares (3SLS) method which
R.M. John / Social Science & Medicine 66 (2008) 1356—1367
1363
devoted to food, education and entertainment in rural
India while it leads to a rise in share devoted to health
care, clothing and fuels. A similar effect is seen in urban
India, except that fuel expenditure is also decreased.
The 50th round also showed a similar pattern in crowd
ing out suggesting that the crowding out patterns may
not be specific to one particular round. These results
are also not reported here and can be made available
Empirical evidence on crowding out
upon request. A separate analysis was carried out to
see if there is any difference in crowding out between
Table 3 reports the results of tests of null hypothesis
the income groups. The results from the Table 5 show
for corner solutions as discussed above. The null
that the nature of crowding out is similar among both
hypothesis is that the three parameters associated with
low- and high-income households. The effect of spend
the binary variable d in Eq. (5) are jointly not signifi
ing on tobacco on other commodities, wherever signif
cant. i.e., Ho: «2, = fe = Y2z = 0- It turns out that in
icant, is in the same direction for both these groups
both rural and urban India, the null hypothesis of zeros
though with small differences in magnitudes.
arising from corner solutions is rejected, making ab
Commodities are not classified into necessities and
luxuries here based on the sign of the parameters of
stention the likely reason behind zero expenditure on
tobacco. This does not indicate that price has no effects
In M since (i) M does not represent the total expenditure
on initiating tobacco consumption. The empirical evi
here and (ii) the results are conditional on the outlay on
dence so far on the effect of price on smoking initiation
tobacco. As expected the parameters of the quadratic
is mixed (Cawley, Markowitz, & Tauras, 2004). The
term In M2 in table turned out to be significant in
fact that the result here is based on household and not
most cases. It should be noted that the objective is not
on individual consumption decisions may affect these
to analyze the demand for other goods, but rather to
examine the effects of tobacco expenditure on the con
conclusions to some extend.
Table 4 reports the results on the crowding out
sumption of other goods. Hence, the estimated parame
effects of tobacco for households irrespective of their
ters for household demographic and socioeconomic
income levels. Goods are not separable from the con
characteristics are not reported.
sumption of tobacco except alcohol, travel and durables
It was seen earlier that, though the food share is sim
in rural India and clothing, alcohol and durables in ur
ilar for both tobacco users and non-users, certain items
ban India for which d has turned out to be insignificant.
such as milk and milk products were compromised
This means there is both an income effect as well as
while items like cereals were consumed more by the to
substitution effect of consuming tobacco on goods
bacco consuming households. As the above regression
such as food, health care, education, fuel and entertain
results indicate possible crowding out of expenditure
ment in both rural and urban India. An increase in the
on food among the tobacco consuming households it
outlay for tobacco leads to a fall in the budget shares
is of interest to examine if this has any implications
on nutrition intake. NSSO provides information on the
intake of calories, protein and fat for each of the house
holds. Table 6 gives the per capita per diem intake of
Table 3
nutrients by tobacco spending status for both rural and
Test for comer solutions
Urban
urban India. Comparing tobacco consumers and non
Rural
Commodities
consumers, one observes that intake of fat is lower
41.48
121.22
Food
38.15
while calories and protein intake are higher among
65.71
Health
12.85
70.11
the tobacco consuming households in rural India,
Education
14.56
51.02
Clothing
whereas all three are lower among the tobacco consum
34.32
177.46
Fuel and light
ing households in urban India. As one moves to higher
32.34
35.74
Entertainment
tobacco spending categories these nutrients are increas
250.35
589.36
Alcohol
43.80
ingly lacking as compared to the no spending groups.
141.12
Transport
53.48
100.02
Thus, along with the reduction in consumption of
Durables
Notes: values in each column are the %2 statistics from a Wald Test for
various necessities, intake of sources of nutrition also
the joint significance of three parameters (a2n Pn and Y2/) associated
becomes an issue among the households consuming
with the binary variable d in Eq. (3). All statistics are highly signifitobacco as their expenditure on tobacco increases.
is robust to the application of I Vs in SUR. Because the
dependent variables of the 10 equations add up to one
(adding up restriction) one has to arbitrarily drop one
'■ equation from the system of Engel curves before pro
ceeding with the 3SLS estimation. The equation on
“other goods” is dropped here.
cant at p-values less than 0.01.
1364
R.M. John I Social Science & Medicine 66 (2008) 1356—1367
Table 4
Conditional Engel curves — (conditional on tobacco spending)
Rural India
d
PJ
In M
In AY2
d In M
Jin M2
Urban India
d
PJ
In AY
In M2
d In M
Jin M2
Food
Health
Education
Cloths
Fuel
Entertainment
Alcohol
Travel
Durable
3.886*
0.514
-0.038*
0.005
1.437*
0.131
-0.099*
0.008
-1.024*
0.135
0.067*
0.009
-2.422*
0.373
0.021*
0.003
-0.701*
0.095
0.048*
0.006
0.631*
0.098
-0.041*
0.006
0.706*
0.128
-0.006*
. 0.001
0.162*
0.033
-0.010*
0.002
-0.183*
0.034
0.012*
0.002
—0.329**
0.136
0.003**
0.001
-0.054*
0.035
0.003
0.002
0.089*
0.036
-0.006*
0.002
-0.787*
0.181
0.009*
0.002
-0.245*
0.046
0.014*
0.003
0.205*
0.047
-0.013*
0.003
0.304*
0.053
-0.003*
0.000
0.075*
0.013
-0.005*
0.001
—0.080*
0.014
0.005*
0.001
0.008
0.147
0.001
0.001
-0.005
0.037
0.001
0.002
0.000
0.039
0.000
0.003
-0.286
0.161
0.003
0.001
-0.151*
0.041
0.011*
0.003
0.078
0.042
-0.005
0.003
-0.324
0.203
0.003
0.002
-0.307*
0.052
0.022*
0.003
0.091
0.053
-0.006
0.003
4.173*
0.697
‘-0.085*
0.015 .
0.935*
0.135
-0.064*
0.008
-1.076*
0.180
0.070*
0.012
-2.069*
0.478
0.039*
0.010
-0.367*
0.093
0.024*
0.006
0.527*
0.123
-0.034*
0.008
1.012*
0.286
-0.023*
0.006
0.210*
0.055
-0.012*
0.003
-0.261*
0.074
0.017*
0.005
-0.022
0.175
0.003
0.004
0.003
0.034
-0.001
0.002
0.007
0.045
-0.001
0.003
0.585*
0.213
-0.010**
0.005
0.105*
0.041
-0.008*
0.002
-0.149*
0.055
0.010*
0.004
0.290*
0.096
-0.005**
0.002
0.059*
0.019
-0.003*
0.001
-0.075*
0.025
0.005*
0.002
0.358**
0.166
-0.006
0.004
0.091*
0.032
-0.005*
0.002
-0.089**
0.043
0.006**
0.003
-0.822*
0.291
0.020*
0.006
-0.211*
0.056
0.015*
0.003
0.218*
0.075
-0.015*
0.005
-0.783**
0.346
0.010
0.008
-0.315*
0.067
0.022*
0.004
0.202**
0.089
-0.013**
0.006
by 100. J is the tobacco dummy, prt is the expenditure on tobacco and In AY is the log of expenditure in excess
Notes: parameters ofp/ are minltiplied
!
of tobacco consumption. Values below each coefficients are standard errors. * and ** shows levels of significance at 1 and 5%, respectively.
Discussion
Literature from developing countries suggest the
importance of the economic effects of higher spending
on tobacco on household standards of living and expen
diture patterns and these effects may be different in dif
ferent countries (Efroymson et al., 2001; Wang et al.,
2006). No study has examined such issues in the context
of India which is the second largest consumer of to
bacco in the world (Reddy & Gupta, 2004). This study
uses a nationwide representative household survey data
to examine such crowding out effects of tobacco spend
ing separately for the rural and the urban households in
India. This is hence the major contribution of this study.
As the study shows, it is obvious that concerns regard
ing the crowding out potential of tobacco expenditure,
over and above the health consequences of tobacco
use, are well founded.
To recapitulate, using a system of conditional Engel
curves the paper estimated the effect of tobacco spend
ing on broad groups of items. It was found that an
increase in the outlay for tobacco led to a fall in the
budget share devoted to food, education and entertain
ment in rural India while it led to a rise in the shares
devoted to health care, clothing and fuels. A similar in
crease in tobacco expenditure in urban India led to a de
crease in the budget shares for food, education, fuel
and entertainment while leading to a rise in the shares
of health care and conveyance. The effects of spending
on tobacco on the consumption of other goods were
found to be in the same direction for both low- and
high-income households. A further analysis of the im
plications of reduced food expenditure on the nutrition
intake of households revealed that per capita per diem
intake of nutrients such as calorie, protein and fat are
lower among high-tobacco spending households com
pared to households with no tobacco expenditure.
The findings here support the idea that expenditure
on tobacco in India has crowding out effects as observed
in other developing countries such as Bangladesh and
China. Moreover, the effects of higher spending on to
bacco on nutrition intake adds to the findings by
Efroymson et al. (2001) in Bangladesh, who discussed
the implications of tobacco spending on poverty. The
paper thus reiterates, how spending on tobacco affects
smokers and their immediate family members in ways
other than through direct health consequences. The allo
cations of household goods and services in this analysis
1365
R.M. John ! Social Science & Medicine 66 (2008) 1356 1367
. -Table 5
Conditional Engel curves — low- and high-income groups
Entertainment
Alcohol
Travel
Durable
0.290**
0.122
0.818
0.432
0.166
0.371
0.032
0.301
-0.007**
0.003
-0.009
0.011
-0.011
0.010
-0.001
-0.204
0.245
0.310*
0.098
-0.091
-0.336
0.334
-1.214*
0.486
0.001
0.001*
0.000
0.001
0.001
-0.001*
0.000
0.000
0.001
0.002**
0.001
0.004*
0.001
-0.402
0.565
0.413
0.298
-0.419
0.306
-0.252
0.387
0.013
0.119
0.504
0.283
-0.933*
0.329
-0.172
0.237
-0.022
0.012
0.011
0.006
0.006
0.003
0.007
0.002
0.002
-0.009
0.005
0.020*
0.006
0.006
0.018
-0.014**
0.006
0.716
0.403
-0.245
0.201
0.559*
0.206
0.314**
0.623*
0.177
0.079
0.395
-2.508*
0.613
Food
Health
Education
Cloths
Fuel
Rural — low income
d
2.180
1.332
-2.122*
0.831
-0.071
0.226
-0.885
0.479
-1.029
0.585
0.060*
0.022
0.003
0.019
0.006
0.013
-2.799*
0.697
0.871*
0.258
-0.631*
0.194
0.005*
0.002
-0.002*
Urban — low income
d
0.759
0.934
-0.081**
Pd
0.035
Rural — high income
d
5.059*
0.805
Pd
.PJ
-0.013*
0.002
Urban — high income
-2.189*
d
5.363*
0.629
0.720
0.035**
0.015
0.238
0.132
0.008
0.005
0.011
0.001
-0.004
-0.001
0.006
-0.017*
0.017
0.009
0.006
0.003
0.003
0.003
0.006
0.010
on tobacco. Values below each coefficients are
Notes: parameters of pj arej milultiplied by 100. d is the tobacco dummy and ptt is the expenditure
**
shows
levels
of
significance
at
1
and
5%,
respectively.
standard errors. * and
P7
-0.004**
0.002
-0.042*
0.011
were found to be unfavorable to woman and children by
reductions in education, clean cooking fuels, family
entertainment and food, especially milk and milk
products. Reduced expenditure on children’s education
among tobacco consuming households may suggest an
intergenerational effect of tobacco consumption by
adults on the educational opportunities of children.
The ramifications of this are enormous, as investment
forgone in education can have long lasting effects in
terms of adverse implications for human development
and loss of future income earning opportunities.
Such unfavorable allocations are not surprising in
the Indian context where, more often than not, women
and children have less bargaining power versus their
male counterparts. It is possible that male decision
makers in tobacco consuming households may compro
mise mostly those items of expenditures which has
direct bearing on children and women. As Deaton
(1997, p. 223) observes, “since children are not volun
tary members of the families to which they belong,
there can be no general pre-supposition that their inter
ests are fully taken into account.” So is the case with
women in India who are “marginalized in decision
making and leadership” (Menon-Sen & Kumar, 2001)
with more than 50% of married rural Indian women
playing no role in household decision making (UPS,
Table 6
Per capita per diem intake of calorie, fat and protein by tobacco spending status
Category
Urban India
Rural India
Calorie
Fat
Protein
Calorie
Fat
Protein
58.47
49.65
2155.70
59.11
36.14
2148.59
59.03
53.42
2189.95
58.23
38.87
2133.25
NoSpend
57.73
44.66
2110.46
59.54
34.79
2156.14
Total tobacco
62.62
52.55
2307.63
59.96
32.99
2207.96
LSpend
57.23
42.59
2078.66
60.11
35.26
2174.07
MSpend
54.31
42.99
2008.69
57.40
35.19
2050.34
HSpend____________ ________________________
___ _______
are
weighted
by
appropriate
sampling
Notes: units of measurements are Kilo calories (kcal) for calorie and gram (gm) for fat and protein. All figures
All
weights and hence are representative figures.
1366
R.M. John I Social Science & Medicine 66 (2008) 1356—1367
2000, p. 66). These effects on household allocation of
goods and services may have far reaching impacts in
the long run, which need not be confined within the
household alone.
Tobacco Control Conference organized by ACT India
and AFTC at Tata Memorial Hosptial, Mumbai (2729 January 2006). Thanks are also due to all the writing
seminar participants at the University of California San
Francisco.
Limitations
More detailed intra-household analysis of consump
tion expenditures is warranted in order to examine the
full effects of tobacco consumption in terms of the
opportunity cost.. However, unavailability of detailed
consumption data at the individual level does not permit
such analysis, which is a limitation of this study. Hence,
it should be rioted that the unit of analysis in this paper
is household, whereas much of the tobacco consump
tion decisions are made at the individual level. If the
current National Sample Surveys on consumption ex
penditures can be extended to capture information on
intra-household allocation*in some way, it would be of
great benefit in this regard. The data reported in this
survey are based on self-reported information for the
previous 30-day reporting period. It is possible that
the reported consumption suffers from measurement
errors. The readers should also note that the link between
tobacco consumption and consumption of various other
items that are observecLhere cannot be taken as causal
relationships since these relationships are established
using only two different cross-sectional time points.
Policy implications
A major implication of the analysis in this paper is
that, since expenditure on tobacco has crowding out ef
fects, if a policy recommendation leads to an increase in
the expenditure on tobacco, it is likely to have adverse
effects in terms of reduced expenditure on items such as
food, education and entertainment. In contrast, if a tax
policy on tobacco can be devised effecting significant
cut in consumption resulting in net reduction of expen
diture, it can have positive implications not only on the
overall household welfare but also on intra-household
allocation of goods and services. Given that tobacco
products are generally inelastic, it would require sub
stantial increases in taxes to attain a net reduction in
expenditures. Knowledge of price elasticity of tobacco
products is very crucial for any such tax policy.
Acknowledgements
l am indebted to A. Ganesh-Kumar, Kirit Parikh and
Joy de Beyer for their valuable comments and sugges
tions. I also thank participants of the first National
/.n.
L-i-------------------- ---
■ ■■
References
Banks, J., Blundell, R., & Lewbel, A. (1997). Quadratic Engel curves
and consumer demand. The Review of Economics and Statistics,
79(4), 527-539.
de Beyer, J., Lovelace, C., & Yurekli, A. (2001). Poverty and to
bacco. Tobacco Control, 10, 210—211.
Browning, M., & Meghir, C. (1991). The effects of male and female la
borsupply on commodity demands. Econometrica, 59(4), 925—951.
Busch, S. H., Jofre-Bonet, M., Falba, T. A., & Sindelar, J. L. (2004).
Burning a hole in the budget: tobacco spending and its crowd-out
of other goods. Applied Health Economics and Health Policy,
3(4), 263-272.
Cawley, J., Markowitz, S., & Tauras', J. (2004). Lighting up and
slimming down: the effects of body weight and cigarette prices
on adolescent smoking initiation. Journal of Health Economics,
23(2), 293-311.
Davidson, R., & MacKinnon, J. G. (1993). Estimation and inference
in econometrics. New York: Oxford University Press.
Deaton, A. S. (1997), The analysis of household surveys. Baltimore:
Johns Hopkins University Press for the World Bank.
Efroymson, D., Ahmed, S., Townsend, J., Alam, S. M., Dey, A. R., &
Saha, R., et al. (2001). Hungry for tpbacco:: an analysis of the
economic impact of tobacco consumption on the
I poor in Bangladesh. Tobacco Control, 10, 212—217.
Food and Agricultural Organization. (2007). FAOSTAT, Food and
Agricultural Organization of the United Nations. Available
from http://faostat.fao.org/site/567/default.aspx.
Gupta, I., & Sankar, D. (2003). Tobacco consumption in India: a new
look using data from the national sample survey. Journal of
Public Health Policy, 24(3), 233—245.
UPS. (2000). India: National Family Health Survey-II (1998-99).
Mumbai, India: International Institute for Population Sciences.
John, R. M. (2005). Tobacco consumption patterns and its health
implications in India. Health Policy, 71(2), 213—222.
Keen, M. (1986). Zero expenditures and the estimation of Engel
curves. Journal of Applied Econometrics, 1(3), 277—286.
Menon-Sen, K., & Kumar, A. K. S. (2001). Women in India: How
Free? How Equal? Report commissioned by the Office of the
Resident Coordinator in India (UNDP), New Delhi.
Nichter, M., & Cartwright, E. (1991). Saving the children for the
tobacco industry. Medical Anthropology Quarterly, 5(3), 236—256.
NSSO. (2000). Consumption of some important commodities in
India, NSS 55th Round (1999-2000), Ministry of Statistics &
Programme Implementation, Government of India.
Pollak, R. A. (1969). Conditional demand functions and consumption
theory. The Quarterly Journal of Economics, &3(1), 60—78.
Rani, M., Bonu, S., Jha, P., Nguyen, S. N., & Jamjoum, L. (2003).
Tobacco use in India: prevalence and predictors of smoking
and chewing in a national cross sectional household survey.
Tobacco Control, 12(4), E4.
Reddy, K. S., & Gupta, P. C. (Eds.). (2004). Report on tobacco con
trol in India, Ministry of Health and Family Welfare, Government
of India.
R.M. John I Social Science & Medicine 66 (2008) 1356 1367
Selvanathan, S., & Selvanathan. E. A. (2005). Rich versus lhe poor:
consumption of food, tobacco, alcohol and soft drinks: an econo
metric analysis. In B. M. de Silva, & N. Mukhopadhyay (Eds.),
Proceedings ofthe international Sri Lankan statistical conference:
Visions offuturistic methodologies. USA: RMIT, Australia/University of Connecticut.
Shah, S., & Vaite, S. (2002). Choosing tobacco over food: daily
struggles for existence among the street children of Mumbai,
India. In D. Efroymson (Ed.), Tobacco and poverty: Observation
from India and Bangladesh. Canada: PATH.
Shimkhada, R., & Peabody, J. W. (2003). Tobacco control in India.
Bulletin of The World Health Organisation, 81(1), 48—52.
Subramanian, S., & Deaton, A. S. (1991). Gender effects in Indian
consumption patterns. Sarvekshana, 14. J—12.
Subramanian, S. V., Nandy, S., Kelly, M., Gordon, D., & Smith, G. D.
(2004). Patterns and distribution of tobacco consumption in India:
1367
cross sectional multilevel evidence from the 1998-9 national fam
ily health survey. British Medical Journal. 328(7443), 801—806.
Thomson. G. W., Wilson. N. A.. ODea, D„ Reid, P. J., & HowdenChapman, P. (2002). Tobacco spending and children in low
income households. Tobacco Control. 11(4), 372—375.
Vermeulen, F. (2003). Do smokers behave differently? A tale of zero
expenditures and separability concepts. Economics Bulletin, 4(6),
I
i;
Wang, H„ Sindelar, J. L„ & Busch, S. H. (2006). The impact of
tobacco expenditure on household consumption patterns in rural
China. Social Science & Medicine, 62(6), 1414—1426.
World Bank. (2002). India: household energy, indoor air pollution,
and health, joint UNDP/World Bank Energy Sector Manage
ment Assistance Programme (ESMAP). [Report N" 261-021
Available from. <http://wblnOO 1 S.worldbank.ofg/esmap/site.nsf/
pages/South+Asia>.
I
^^3
- Media
 10548.pdf
10548.pdf
Position: 6251 (1 views)