RURAL HEALTH SERVICES AND TRAINING PROGRAMME
Item
- Title
- RURAL HEALTH SERVICES AND TRAINING PROGRAMME
- extracted text
-
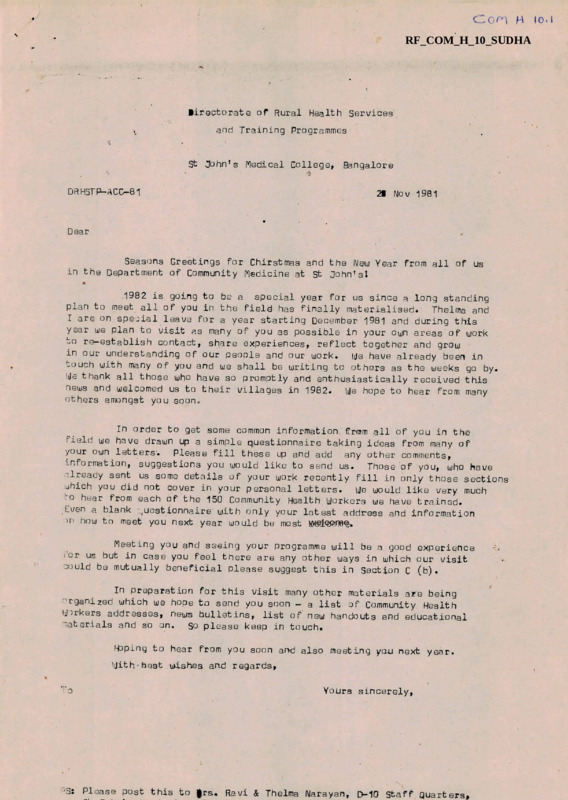
Co^l H IQ. I
RF_COM_H_10_SUDHA
lirectorate of Rural Health Services
and Training Programmes
St 3ohnfs Medical College,
Bangalore
DRHSTP-ACC-81
29 Nov 1981
Dear
Seasons Greetings for Chirstmas and the New Year from all of us
in the Department of Community Medicine at St Johnfsl
.1982 is going to be a special year for us since a long standing
plan to meet all of you in the field has finally materialised.»
Thelma and
I are on special leave for a year starting December 1981 and during this
year we plan to visit as many of you as possible in your own areas of work
->o re-establish contact, share experiences, reflect together and grow
in our understanding of our people and our work,
ije have already been in
touch with many of you and we shall be writing to others as the weeks go by.
We thank all those who have so promptly and enthusiastically received this
news and welcomed us to their villages in 1982.
We hope to hear from many
others amongst you soon.
In order to get some common information frmm all of you in the
field we have drawn up a simple questionnaire taking ideas from many of
Please fill these up and add any other comments,
your own letters.
■'.n format ion, suggestions you would like to send us.
Those of you, who have
already sent us some details of your work recently fill in only those sections
We would like very much
which you did not cover in your personal letters.
to hear from each of the 150 Community Health Workers we have trained.
Lven a blank ,uestionnaire with only your latest address and information
w how to meet you next year would be most welcome.
Meeting you and seeing your programme will be a good experience
i or us but in case you feel there are any other ways in which our visit
could be mutually beneficial please suggest this in Section C (b) •
In preparation for this visit many other materials are being
organized which we hope to send you soon - a list of Community Health
Workers addresses, news bulletins, list of new handouts and educational
Materials and so on.
So please keep in touch.
Hoping to hear from you soon and also meeting you next year.
With'best wishes and regards.
! 0
Yours sincerely.
JS: Please post this to |rs. Ravi & Thelma Narayan,
D-10 Staff Quarters,
- ■ r'
:•
■
i
::■
■■T
i■
■
■
.
i
r
, ...■ ? (
:
■
,
■i-
j
<
i
■ n.
.
■
■
1
. • i'
Directorate of Rural Health Services &
Training Programmes
FQLLOW-UP EVALUATION OF CONNUNITY HEALTH
WORKERS TRAINED IN ST 30HNrS NEDICAL COLLEGE
PROFOWA
Instructions :
Section A and C to be filled in by all Community Health Workers
Section g to be filled in by those who are doing health work
at present.
(please keep us
SECTION - .A
a)
informed regarding change of address)
- GENERAL INFORMATION
Name :
c) CHJ Course No.:
b) Age:
ti) Name of Congregation:
e) •Jiloceses
Permanent Address
(Mot.tjer House/superior)^ :
9) Present Address
(For future correspondence) :
h) Ijhat have you been doing after the course ?
(if you have changed from place to place give us some details of your workin each place).
i) Give us a short description of the present team }
yo-y are working ^ith atd
what each member does (not only health actiuities,)
j)
Have y w attended an> Qo^jrse/me.etings/workshop.
is si>ce you completed the
Course ?
I
?
2 :
k)
Are you in touch with any of the other Community Health Workers?
give us their recdnt address.
1)
Give in a few sentences a description of the poeple you are working
with (rural, urbcxp, tribal, non-tribal, main occupation, other characteristics
etc).
How many villages? Total population, what distances apart ?
If so
SECTION B
a)
Give a short description of the health activities you are involved i|«
b)
How many hours are allotted for this daily/weekly ?
• c) ^re you functioning independently or with a team of workers?
how is the health work shared amongst you ?
If so,
d) Do you get any assistance from the local Primary Health Centre?
If so, specify ?
&
e) Do you get any assistance from a Taluk/flission Hospital?
If so, specify?
f) Do you work with any special groups in the village (young farmers,
youth, mothers, harijans etc.)?
v
...3
:3s
9) Do you participate
in training of local
people ? Grihinis,
worker, mothers etc.
village level
h) Do you have <any
“
of the following programmes?
Food for work.) Health Insurance,
CRS- PICH ^ogramme, any others
i) <Are you part of
any Diocesan Society or Health Team ?
If so. specify.
SECTION C (Regarding 1982 project)
a) Give Us detailed information
on how to reach your village/project/centre?
(By bus and train,
also from station and bus stop)
b) -Are there any forms of support which
a visiting team can give you next
Hat e:
year ?
Signat ure:
Please use the
remaining blank sosce to giveany further details
for which there
was not adequate spaCe in the questionnaire.
*
Ccr^) H
ST. BOHN’S MEDICAL COLLEGE, BANGALORE 560 034
Department of Community Health
Dated s
Dear Sister/F^ther/Brother,
Greetings from St
Bohn’s Medical College, Department of Community Healthl
We have received your present address from the superior of the convent
from which you had come to us ifor_ the Community Health Uorkers Training
course.
We had promised informative material & -Consultatory help.
However, before
that we would like to have a few more details regarding your present work
and address as also some of your view-points on our training. This would
enable us to improve on our training as well as to help you in relevant
aspects•
Enclosed herewith is a questionnaire with most of the answers provided.
Tick or underline the1, answer you find most appropriate.
You may use the
space on the last page for any other details you like us to know.
Kindly fill in the questionnaire and mail it back to us as early as
possible preferably before November 30th 1991.
Thanking you8
Yours sincerely,
f *r
OR REYNOLD WASHINGTON
Countersigned s
DR. DARA S AMAR
prof. & Head
p es, g Please post this to.
Dr. Reynold G. Washington
Dept, of Community Health
St. John’s Medical College
BANGALORE 560 034
io- fX-
«
DEPARTflCNT CF COMMUNITY HEALTH
GENERAL PROFILE; COMFUNITY HEALTH WORKERS
b)
I a) Name?
d)
c) Sex;
Age;
Year Attended CHW Course;
f) Caste; SC/ST
e) Religion;
II $) What was your educational qualification before joining the course?
a) Below S.S.L.C. (Xth Std)
b) S.S.L.C.
c) P.D.C./P.U.C.
d) Higher qualifications Medical
(specify)Degree/Diploma? Non Medical
e) Technical Training
2) Have you improved your educational qualification since then?
Yes/No
3) What is your educational qualification at present?
Below SSLC/SSLC/PDC/Higher Degree/Technical Training/Professional
-3 related to health or Community Development
Ill i) Have you done any other course
after the course? (Please tick or underline)
Laboratory Technician/Auxiliary Nurse Midwife/Nursing/Community Health
& Uevelopment/lntegrated Rural Development/Diploma course for mentally
retarded/ Bachelor of Education/ Teacher(s Trailing/ Theology,
Philosopher/ Multipurpose Worker's Course/Social Awareness Course/
Adult Education/Bachelor in Social Science/Naturopathy, Ayurveda,
Unani, Siddha, Herbo-PUneral, Magnetotherapy Course/Small industry &
Co-operative course/Leprosy Training Course/Any other/ Acupressure &
Acupuncture.
/
of continuing
ii) Have you attended any seminars or workshops as a process
education such as?
- Diocesan meeting on Health Development
- Natural Family Planning
- Maternal & Child Health
— Vocation Seminar
- Youth Seminars
- VHAI Conventions
- Social Work meetings
- Adhoc mission hospital-based training
Com H
ST. JOHN’S fEDICAL COLLEGE, BANGALORE 560 034
Department of Community Health
Dated g
Dear Sister/rather/Brother,
Greetings from St
John’s Pledical College, Department of Community Health!
We have received your present address from the superior of the convent
from which you had come to us for the Community Health Workers Training
course.
We had promised informative material ft -Consultatory help®
However, before
that we would like to have a few more details regarding your present work
and address as also some of your view-points on our training. This would
enable us to improve on our training as well as to help you in relevant
aspects•
Enclosed herewith is a questionnaire with most of the answers provided®
Tick or underline the answer you find most appropriate®
You may use the
space on the last page for any other details you like us to know®
Kindly fill in the questionnaire and mail it back to us as early as
possible preferably before November 30th 1991»
Thanking you,
Yours sincerely.
ft *>•
UR REYNOLD WASHINGTON
Countersigned 2
DFUDARA S ANAR
Prof® & Head
ptS, j Please post this to®
Dr® Reynold G. Washington
Dept® of Community Health
St® John’s Medical College
BANGALORE 560 034
DEPARTHEINT CF COMMUNITY HLALTH
GENERAL PROFILE? COMMUNITY HEALTH WORKERS
c) Sex?
b) Ages
I a) Name?
d)
Year Attended CHbJ Course?
e)
Religion?
f) Caste? SC/ST
II d) What was your educational qualification before joining the course?
a) Below S.S.LeC®
b)
(Xth Std)
S.S.L.C.
c) P.D.C./PeUoC.
d) Higher qualifications Medical
(specify)Degree/Diploma* Non Medical
e) Technical Training
2) Have you improved your educational qualification since then?
Yes/No
3) Ulhat is your educational qualification at present?
Below SSLC/SSLC/PDC/Higher Degree/Technical Training/Professional
-) related to health or Community Development
Ill i) Have you done any other course
after the course? (Please tick or underline)
Laboratory Technician/Auxiliary Nurse Plidwife/Nursing/Community Health
& Development/Integrated Rural Development/Diploma course for mentally
retarded/ Bachelor of Education/ Teacher(s Trail ing/ Theology,
Philosopher/ Multipurpose Worker's Course/Social Awareness Course/
Adult Education/Bachelor in Social Soience/Naturopathy, Ayurveda,
Unani, Siddha, Herbo-PUneral, Magnetotherapy Course/Small industry &
Co-operative courSe/Leprosy Training Course/Any other/ Acupressure &
Acupuncture <»
ii) Have you attended any seminars or
education such as?
workshops as a process of continuing
- Diocesan meeting on Health development
- Natural Family Planning
- Maternal & Child Health
- Vocation Seminar
- Youth Seminars
- VHAI Conventions
- Social Work meetings
- Adhoc mission hospital-based training
2
IV i) What area do you stay in ?
Rural
Urban
Tribal
Others
T ribal
Others
ii) What type of people do you serve?
Rural
Urban
V)i) Specify the year in which you
type of works
were involved in any one of the following
yes /no
- Dispensary
- Mobile Clinic
- C.R.S* Programme
- Maternal & Child Health
- Creche/Balwadi
Immunization
- Health Education
- Natural Family Plamning
- Adult & Non-formal education
Malaria Surveillance
- Leprosy work
School Health work
- Nutrition Education
- Home for the Aged
- Major hospitals
- Village level worker’s training
Mahila Mandal
- Youth club
- Grihini Course
- Agricultural Extension
- Animal Husbandry
- Vegetable gardens
- Environmental Sanitation
- Community Organisation
- Conscientisation
r
Year
Duration of Experience
in years
3
ii) Did you at any time work as any one of the following? Specify the yeafcs
Teacher in a school
Parish Priest
Rehabilitation Centre/
Hostel
Superior
Parish
parish work
Manager of Estate
Informafcisn/Mat ron
VI) Did you integrate Community Health Work in these roles?
yes /no
VII) Has the Community Health Workers Training helped in your work?
(i)
YE5/N0
(ii) What aspects of field training/visits do you find relevant?
- Family studies
- Chlorination of well
- Immunization sessions
- Natural Family Planning
- Health Education
- MCH Services
- School Health
- Training of TBA’s
- Training of 1eachers
- Mobile Clinic
- Leprosy Survey
- Nutrition Demonstration
- Child to Child
- Family Role in Illness
- Spastic Society/Physically Handicapped
- Visit to the Blind
- Child guidance clinic/
Speech & Hearing/
Food preservation & Canning
iii) VJhat teaching methods helped you the most?
LectureLecture with Audic-Visual Aids
- Discussion
- Demons!rations/practicals
- Supervised field work
- Simulation games
(Monsoons,Chikkanahalli)
- Learning by doing (Nutrition demonstration, child to child)
iv) Did you h ve difficulty in learning any of these areas during the course?
YES/NC
- Content?
- languages
- durations
- Method of teaching used s
- timing of sessions^
- sequence of sessionss
Last
minute changing of time-tables
v) Was any action taken to help you learn better? YES/MO
vi)
so what action?
Extra classes/withdrawal from course/report to supervisor/
personalised attention Ly trainer/others«
vii) With respect to your objectives in joining the course, were you
satisfied immediately after the course?
YES/NO
viii) Do you think refresher course are necessary? YES/NO
On what aspects ?
- Control of Communicable diseases
- MCH
- Nutrition
- Immunization
- First Aid
- Health Education
- Environmental Sanitation
- Planning, Management
- Evaluation of Health Status
- Curative care for minor ailments
- Community Development Activity
- Vital event registration
- Ruferral
- Other systems of medicine
(Ay u r v ed a/ H o me o p at h y/bn an i )
J
5
VIII) What problems do you encounter in your work at present?
- Lack of self-confidence
- Lack of technical guidance
- Lack of support - personnel/mcncy/material
- Restriction imposed by superior
- Lack of interG'St
- Lack of community participation
- Lack of co-operation with other groups(Govt
- Lack of cooperation with other groups (Private)
- Lack of continuing education from St
John’s o
- Any others
\
%
COMMUNITY HEALTH UORKLRo uUESTIONNmIRE
WORK OF THE COMMUNITY HEALTH WORKERS
I
CONTROL OF COMMUNICABLE DISEASES?
1.a) Do you screen patients for common communicable disease?
Yes/No
b) How often do you screen patients for disease?
once/6 months
Once/year
once/3 months
once/month
c) What common communicable diseases have you screened patients for?
TB/Leprosy/Malaria/skin diseases/Vitamin’A’ deficiency/others(specify)
Yes/No
d) Do you screen any particular age group more often?
Under 5/ 5-15 school going/ 15-45/ 46-60/more than 60 yrs
2.a) Do you impart health education concerning common communicable diseases
Yes/No
in your area?
b) How often?
Once/year
oiice/6 mths
once/month
□nce/3 months
once/week every opportunity
c ) What diseases have you taught or informed people about?
T .B ./Leprosy/Malaria/V .D ./Skin diseasts/AIDb/Diarrhoea/Acute Respiratory
Infections/Worm Infestations/others(specify)
Y es/No
3oa) Do you perform any laboratory tests
b)
If you do so, What?
Malaria slide/Stool examination/Sputum for AFB/Urine Sugar and
Albumin/Hbo / Leprosy smear.
Yes/No
4oa) Do you treat patients with communicable diseases?
b) What communicable diseases do you commonly encounter?
Measles/polio/Oaundice/Malaria/TB/Leprosy/Diarrhoea/Uysentry/
Others(Specify)
c) What do you use to treat them?
Home remedies/Allopathic Drugs/Other systems
(eg?
Ayurveda, Homeopathy)
specify
d) Do you follow-up patients with chronic communicable diseases?
lijhat is your level of involvement in the following programmes?
a) Diarrhoeal Disease Control Program
b) ARI Control Program
c) Tuberculosis Control Program
Yes/No
2
6. What is your level of
7. How will ycu manage;
a) An infant
with ARI
b) A young adult with malaria
c) A child with diarrhoea
IMTERNAL AND CHILD HEALTH
II
1.
in
Do you identify pregnant women from with/the community?
Yes/No
2.a)
Do you identify high risk cases?
Yes/No
Are the high risk cases referred for appropriate care?
Yes/No
3
Do you arrange for T .T. Vaccination for Pregnant women?
Y^s /Nq
4O
Do you educate them on general care, nutrition an
b)
immunization during pregnancy?
Yes/No
5.
Do you assess weight gain regularly in pregnant women?
Yes/No
6 • a)
Do you conduct laboratory investigations for pregnant women?
Y es/ Np
b)
What? Hb/urine/Blood group and type/VDRL
7o
Do you distribute Iron and Folic Acid tablets to pregnant women?
Yes/No
8 .a)
Have you assisted delivery at any time?
Yes/No
b)
At Home/hospital
Have you trained Traditional Birth Attendants(TBA)
^egi Dais) at any time?
9.
ID.a)
b)
Do you inform and
What methods?
motivate pregnant women: for family planning?
NFp/others
Yes/No
Yes/No
(specify)
11 .a) Do you visit the newly delivered mother at heme?
Ycs/No
b) How many visits usually?
Dne/two/three/more than three
12.
Is the weight of the new born child recorded?
Yes/No
13)
Do you advise on child care?
Yes/No
14)
Are you involved in any pre-school (Balwadi/Crecho)activity
Yes/No
15)
Do you distribute Vitamin-’A’ drops/capsules for children
16)
who need it?
Yes/No
Have you organised any MCH programs (Mahila flandal/Non—formal
functional literacy groups for girls etc)
Yes/No.
taken ?
5) What preventive steps in communicable disease control have you
a
3
17„
Do you maintain registers?
Yes/No
a) Birth Register
b) Pregnant Women Register
c)
Family Planning Register
Local NCH ^ridicators
18.
a) No. of expectant mothers who received ante-natal care in the
last year.
b) No
of mothers identified as high risk
c) No. of deliveries terminated as abortions or still births
d) No. of deliveries conducted at home/at hospital
e) No
of post-natal check-ups
f) No. of infants attending immunization clinic
III. imUNIZATION
1.a)
Oo you educate groups on vaccine Preventable Diseases?
b)
To whom? Mothers/School-going children/AWto/others(specify)
2.a)
Do you motivate mothers and children to utilise immunization
sei vices?
b)
3.a)
Yes/No
Yes/Nc
How?
Have you assisted at giving immunization?
b)
Where?
c)
What vaccines? Polio/Measles/DPT/BCG
Yes/No
4.
Have you organised any out-reach programmes for immunization?
Yes/No
5.
Do you evaluate your immunization programmes?
Yes/No
6
Can you do a survey to assess immunization coverage in your
area?
Yes/No
7.
Do you maintain an immunization register?
Yes/No
8
Do you hand over immunization cards to the recipients?
Yes/No
9.
What facilities for the maintenance of ‘cold Chain’ do
you have?
4
10oa) O.P .T . is given s
Or’ally/Sub-cutaneously/ int ra-dermal/
intra-muscular
b) Measles Vaccibe is givens
Orally/Sub-cutaneously/intra-dermal/
intra-muscular
IVo NUTRITION
1.a) Do you support promotion of breast feeding m your area?
Yes/No
b) If breast feeding is insufficient, do you suggest
bottle feeding/pallida feeding/spoon & glass/othcrs (specify)
buffalo’s milk/tinned milk/ cow’s milk
introduce weaning foods?
2.a) When do you advise mothers to
b) What type of weaning food do you advise?
3.a) Do you conduct sessions on nutrition
education/nutrition demonstration?
Yes/No
b) For whom?
Yes/No
4o
Do you promote kitchen gardens?
5o
Do you maintain growth charts of children in your
6.
render them special care
Do you identify the malnourished and
7.a)
Are you involved in any
b)
.
supplementary feeding programs?
Name them
8.
What are your
a)
In pregnancy
b)
In infancy
area?
local findings on diet practices?
/
Yes/No
Yes/No
Yes/No
9
5
V. FIRST AID
1. Have you come across cases of
Burns/Wounds/Fractures/Bitcs/Accidents/Poisoning
2. What have y>u done for such cases ?
Nothing/First-Aid and Referral/First-Aid and Curative Care/
Referral straight away/pirst-Aid only
3. What is the first step you take.s
a)
In a case of dog bite
i) give rabies vaccine
•
ii) stitch the wound
iii) Wash the wound with soap and-water
iv) dress the wound
b)
In a case of burns
i) Pour cold water
ii) apply oi 1
iii) apply burnol
iv) dress the wound
VI. ENVIRONMENT
1.a) Do you educate the community ons
- Safe water supply
- Sanitary latrines 2 construction and use
- Waste disposal
- Food protection & food hygiene
- vector control (insects)
- personal hygiene
b) Who do you educates
- School children
- Mothers
- families
r»
6
2,
Do you motivate the community to use
- Safe drinking water
- Sanitary latrines
- Soakage pits
- protect ecl food
vector control measures (ego DDT spraying)
•- smokeless chullas
3O
Have you arranged for Chlorination of water source
~ DDT spraying
Construction of - soakage pits
- smokeless chullas
- sanitary latrines
4.
How has the community involved itself in these areas
Good/Fair/^oor
- Maintenance of water supply
- use of sanitary latrines
- waste disposal
- food protection
- vector control
□o
What are the diseases transmitted by mosquitoes?
a)
Diarrhoea
(b) Malaria
(c) Filaria
(d) Pneumonia
7
VII. IDENTIFICATION OF COHNUNITY HEALTH PROBLEMS L'ITH A VIEUJ TO SOLVE THEMg
1.
Have you identified any Community Health problems in your community?
VJhat type of problems have you,
2.
come across?
Yes/No/sometimes
3) Do you take steps to solve them?
VIII. MEASUREMENT OF HEALTH STATUS OF
1
2.
COMMUNITY^
Have you measured the ’health status’ of your community?
Commonly used Indicators of Health ares
- Infant Mortality Rate
- Life expectancy at birth
- Disease - specific mortality
- All the above
- None of the above
Yes/No
/
8
COPING UITH COI’IHCN HEALTH PROBLEMSg
IX.
1)
(Treating/Referring -when necessary)
What type of cases do you commonly come across?
Pains/Worm infestations/eye diseases/ear diseases/skin diseases/
Dental problems/Venereal disease/Mental disease/fits/others(specify)
2) Have you treated them?
Yes/No
3)a) Have you referred any cases?
b) What type of cases have you
referred?
‘
c) To whom do
youi refer?
Private Hos pital/Govt .Hospital/ovt .Doctor/Gove •Doctor/-AlMlV
Others(Specify)
d) How far is the referral centre?
- i5 km/
Less than 5 Km/6 — 10 Km/ 11
16-20 Km/ More than 20 Km
mode of transport for such patients?
e ) What is the common
- Pvt. Vehicle
- Motorised vehicle - -• Ambulance
- Public Transport Service
- Bullock Cart
— Walk
4)
Do' you
follow-up referred patients?
Yes/No
9
X.
HEALTH EULICATION
Yes/No
1) What aspects have you dealt with?
- Nutrition
Immunization
- Communicable disease Control
First Aid
Environmental Sanitation
- Family Planning
- Others (specify)
2) What methods have you used?
Very Often
Oft c
Rare
Not at all
Lectures
Lectures with Audio-Visual
Aids
’Professional’ Talks
Group Discussions
Demonst rations
Simulaticn Games
Chi Id-to-ChiId/Youth-to-ChiId
3) What Audio-Visual Aids do you use?
Very Often
Often
Rare
Not at all
(ocas ion ally)
- Nonp
- Charts/Flannel graph
- Chalk/Black-board
- Slides
- Overhead Projector
Films
- Tape-recorder
Video films
4) Have you used folk-media?
Very Often
Song
- Dance
skits
O.f t en
Not at all
10
Do you use the Mass-media ?
5)
Very Often
Often
Rare
Not at all
Rad io
f. \/
- Newspapers
- Magazines
6)
Do yo’1 organise mother-groups for health education?
7)
Do you utilise school-children/contact mothers for conveying
health education messages?
~ ? youth/childrun/women/
Have you organised training camps for
men/others (specify) or :involved yourself in them to teach
Health?
S)
Have you organised any health exhibitions/baby shows?
9)
10)
Do you utilise the opportunity of home-visits for inter
1l)a)
Do you evaluate your Health Education Programs?
personal communication on health?
b)
12)
Yes/No
Yes/No
Yes/No
Yes/No
Yes/No
Yes/No
How?
Do you document the program & its evaluation?
Yes/No
r
11
COWUNITY DEULLOPHENT ACTIVITY
XI.
1)
Have you been involved in training for any Community Development Activity?
Animal Husbandry/Horticulture/Piggery/Poultry/Tailoring/Arts & Crafcs/
Weaving/Sericulture/Agriculture/Formal Bit In-formal education/
Others(specify)
2) Do you motivate the Community to involve tnumselves in any of these
Yes/No
activit ies ?
3)
Is health & Community development related?
Y es/ No/Don 11 Icno w
4) Does the Community participate in these activities?
a) - in perceiving the need
b) - in decision making
c) - in planning
d) - in implementation
Yes/No
Yes/No
Yes/No
Yes/PJio
Yes/No
e) - in evaluation
Yes/No
f) - in bringing about changes
Yes/No
5) What steps have you taken to improve community participation?
5
12
XII.
HAINTEN-ANCE OF VITAL STATIST ICS
1)
What are Vital Statistics?
2)
Do you collect & convey information regarding Births, Deaths & Marriages
in your area?
XIII .
PROVIDING FOR COIMTINUIh G EDUCAT I ON
1) What steps have you taken to increase your knowledge & skills in your
work?
2)Who do you approach in case of?
- lack of ’technical'
for
guidance in you community health work
increasing your kno-wledge and skills in you community health work
13
XIV
PRACTICE OF OTHER SYSTEMS OF MEDICINE
1)
bJhat other systems of medicine do you practice?
2) Have you received formal training in them?
3)
Where did you receive such training?
SYSTEMS
PRACTICE
Yes/No
TRAINING
Yes/No
PLACE OF
TRAINING
DURATION OF
TRAINING
- Ayurveda
- Homeopathy
- Accupressure &
Accupuncture
- Herbo-Mineral
- Herbal Therapy
- Home Remedies
- Magnetotherapy
Siddha
Unani
- Naturopathy
- Others (specif y)
4) What percentage of
your patients are treated with these other systems only?
loss then 25’/,/ 26 - 50^ /
5.1 - 75 %
/ more than 75 %
5)a) Do you combine allopathy with these systems in any one given patients? Yes/No
b) What combinations do you commonly use?
6) Do you document such treatment?
Ycs/No
7)a) Have you. evaluated the efficacy of such treatment?
Yes/No
b) How?
c)What are your findings'7
r
u ULst ionnairl
r.nmuNity
CONTROL OF COMMUNICABLE DISEASE s
I
for disease
Is is necessary to screen patients
for disease ?
How often should one screen patients
once/mon th
once/3 mths
once/year
once/6 mths
1) a)
b)
Yes/No
What common diseases require frequent screening?
c)
2) a)
Is
Health education regarding Common
b) How often?
Once/yr once/b months
Communicable diseases necessary
once/3 moths
Yes/No
once/mt h
once/week
every opportunity
c) Uhat diseases do people
need to be taught about?
TB/Leprosy/r'Ialaria/ VD/Skii,n
3)
Is it necessary to do blood,
communicable diseases ?
Grade by degree of importance,
Diseases/AlOS/Diarrhoea/ARl/Uorm Infestation
Urine,
Sputum or stool tests for
the relevance of the following tests
in your areas
- Malaria slide
V. rale vent
Relevent
not re lev ent
- Malaria
Worm infestation/
- Stook examination
- Sputum for AFB
Urine - Sugar
Hb
Yes/No
Arnot biasis
- TB
- Diabetes
Anemia
4) Importance of the
oilowing programmes in your areas s
V,relevent
- Diarrhocl disease control program
- ARI Control Program
- National Tuberculosis Control
Program
- National Lperosy Lrauication
program
- Malaria Control program
^elevent
not releven t
2
II
IWLRNAL & CHILD HULTHs
1.
Is is necessary to identify pregnant women in the community?
20 Is it important to identify ’risk’ cases & refer them ?
Yes/No
Yes/ No
3.
Is T >T • vaccination essential for pregnant women*7
Yes/No
4.
I® education of women on general care, nutrition & immunization
during pregnancy rclevc-nt?
Yes/No
Is regular assessment of weight gain of a pregnant women
essential?
Yes/No
6o Arc blood and urine examination needed for a pregnant mother?
Yes/No
5.
7:,
Are Iron and Folic Acid supplements necessary for prt gnant
women?
Yes/No
8. Do women in the community need assistance of a trained person
during delivery?
Yes/No
9. Is it necessary to train ’Dais’ (TB^s) in Safe delivery
Yes/No
practices ?
10. Is family planning information & motivation relevant for
pregnant mothers?
11
Is it necessary for a newly delivered mother to be visited
and advised by a health worker?
Is it important for the Community Health Workers to advice on
child care ?
14. Do children in Ralvadis/crcches need health care
15
Are Vit ’A’ drops/capsules needed for small children?
16. Dots the Community Health Worker have to integrate his/her
work with other programmes of women & children ?
17
Yes/No
Yes/No
12o Is it necessary to weigh the new born child?
13»
Yes/No
Y es/ No
Yes/No
Yes/No
Yes/No
Is it necessary to. maintain
- Birth Register
~ Y es/ N o
- Pregnant Women(Antenatal) Register
- Yes/No
- Family Planning register
- Yes/No
../3
3
III.
imUNl Z/-,T ION
1
Is there a need for people in your area to be educared & made aware
of V.P.D.(s)?
Yes/Np
- Who needs this education most ?
2.
Is it necessary for mothers & children (in your area) to be
motivated to utilise immunization services?
Hou can they be motivated?
t,
Yc-s/ No
3. Are immunization sessions by a Community Health Worker
necessary?
Yes/No
4. Are ’outreach’ programs for immunization required?
Y es/No
5,,
Is monitoring & evaluation of immunization programs essential?
Yes/No
6. Has immunization cove rage survey been undertaken in your
area?
Yes/No
7O
Is it necessary to maintain immunization registers?
Yes/No
8.
Is it necessary to hand over immunization cards to the
recipients?
Yes/No
VI. NUTRITION
1. Is it advantageous to promote breast feeding?
Yes/No
2. Do mothers need to be cucated on "weaning foods " ?
Yes/No
3. Are sessions on .Nutrition Education & Nutrition Demonstration
important & useful?
Yes/No
Uho should be the recipients at such sessions?
4.
Are kitchen gardens useful?
5
Is it necessary to monitor a child’s growth?
6. Should the Malnourished be identied & rendered special carec
Yes/No
Yes/No
Yes/No
4
V.
FIRST AID
1) Is it necessary for a person to be trained to administer First Aid in
your area for8
V, Relevent
Relevant
not relevant
Relevant
not relevant
Good
not good?
Relevant
not relevant
Burns
Fractures
- Wounds
Bites
Accidents
others
VI.
ENVIRONMENT
1)a) Does the community need to be educated on g
\J, Relevant
- Safe Water supply
- Sanitary Latrines
- Waste disposal
- food protection & hygiene
- Vector control
- personal hygiene
b) Who should this education be targeted at?
J. Good
- School going children
Mothers
Families
- Patients in hospital
- others
)
Should the community be motivated to use?
relevant
- Safe drinking water
- sanitary latrines
- soakage pits
- protected food
vector control measures
- smokeless chullab
../5
5
3) Does the community need a facilitator for 2
- Chlorination of water
- DDT spraying
- Construction of soakage pits
Smokeless chullas
- Sanitary latrines
4)
Grade Community participation in g
Fair
Good
Pc o r
- Maintenance of water supply
- use of sanitary latrine
- waste disposal
- food protection
- Vector control
U11 o
IDENTIFICATION OF COMI'IUN IT Y HEALTH PROBLEMS WITH A VIEbJ TO SOLVE THLM s
- should the community*health worker play a role to?
Yes/No
- identify - health problems g
solue
VIII
Yes/No
- health problems
Yes/No
Measure the health status of the communitys
IX. COPING WITH COMMON HEALTH PROBLLMSs
- Tresting them
- Referring them (when necessary)
1 o
What are the common ailments seen in this area?
Pains/worm infestation/eye diseases/ear diseases/skin diseases/
Dental caries/Venereal disease/Mental disease/Fit/Diarrhoea/ARI
2. Who can treat these common ailments?
Self/Witch doctor/pharmacist/ANM/CHW/Nurses/Doctors
3. Do difficult cases need referral?
To whom? Hospital
Put/Gout
A.
Doctor
Put o
ANlVNurse
Is follow-up of referrai patients important?
Others
Yes/No
r
6
f
X. HEALTH EDUCATION
1. Are health messages on
the following useful or not?
Very useful
Useful
Not useful
Useful
Not useful
- Nutrition
Immunization
Malaria
- Diarrhoea
ARI
- Environmental Sanitation
- Family Planning
AIDS
2.
What methods of health education are useful?
Vo useful
Lectures
’Professions1 Talks
- Discussions (Group)
- Demonstration
- Simulation Games
- Child to Child/
Youth to child
3o
Is it beneficial to use the following for conveying health messages $
- Yes/No
- AUdio-visual Aids
V. Good
Good
Not useful
Good
Not useful
Chestsg Flannel-graph
ChalR - Black Board
Slides
- Over Head Projector
Film reels
- Tape recorder
Folk media
- Yes/No
V. Good
Song
Dance
Drama
Story telling
proverbs
7
5. Electronic Media?
Yes/No
Vo Good
Good
not useful
Radio
T.V.
• Video
Films
6O Mother groups
7. School children/contact mothers
8. Training camps?
Men/Youth/Women/ Child ren
9. Health Exhibitions/Baby shows
10
Home visits
XI. Community Development Activity:
1. What types of Community uevelopment Activity could be incorporated
or advanced in your area?
- animal
husbahdry/horticulture/piggery/poultry/tailoring/arts & crafts/
weaving/sericulture/agriculture/others»
2. Is ’motivation1 of the community necessary for involvement in such
3
activity?
Yes/No
Is health and community development related?
Yes/No
8
4.
Grade Community participation in these endeavours in generals
Good
Fair
Poor
5. Should steps be taken to increase the level of Community participation?
Yes/Nc
What steps?
XII. MAINTENANCE OF VITAL STATISTICS
Is it necessary for the CHW to
1) - Know
2) - Maintain
Yes/No
Yes/No
Vital statistics related,to his/her area of 'Jork?
XIII- Continuing Educationg
9
XIV. PRACTICE OF OTHER SYSTEMS OF MEDICINE
1. What other systems of medicine <o people (of your area) believe in
and
are th«3f useful?
2)
Is training of practitioners in these systems important?
Vo useful
useful
not useful
T raining
Yes/No
- Ayurveda
- Homeopathy
- Accupressure& Accupuncture
- Hebro-mincral
- Home remedies
- Magnetotherapy
- Siddha
Unani
- Naturopathy
Others
3)
Should allopathy be combined with other systems of medicine in
patient?
a given
Com h
10.3
A PROJECT PROPOSAL
to consolidate some of the past efforts
of
Ross Institute Unit of Occupational Health, in the Plantations
in
A short term consultancy,
the
South India, in the areas of continuing Education and Research.
Duration: 6 months in 1988
Venue
: Coonoor/Bangalore
Background
In
the
college based
as
since
its
the
inception
continuing education programmes for plantation
an adjunct to the Comprehensive Labour Welfare
by the United Planters Association of Southern
organised
Unit of
Ross
Health evolved a series of plantation-based and medical
Occupational
staff,
years
ten
f i rst
health
Programme
India.
In addition it also undertook a pilot study on the Health Status
of Tea
Plantation workers with
collaboration with
in
occupation,
special
the
reference to
Regional
their
Occupational
Health Centre, Bangalore (ICMR Unit).
Since 1984 the unit's activities have been somewhat restricted, with a
slowing
down
of
multiple factors
the
initial momentum of
its
development
outlined in the discussion document
due
to
circulated by
Professor Bradley in May 1986 entitled "The Future policy for the Ross
Institute"
and
the
paper "The Ross Institute Unit
Health 1974-84 - an Overview,
of Occupational
and assessment and some thoughts about
the future", by Dr Ravi Narayan in April 1987.
The
short term
suggested to
continuing
some
consolidate
Education
of the
mentioned
consultancy outlined in this
note
some of the past efforts of
a
is
process,
the
Unit
in
and Research and to explore the feasibility of
ideas and future possibilities outlined
in
above
the
associated with
the
Compilation of a Reference manual on Plantation Heal th
from
documents with all the institutions
Unit in the past.
Objectives
A - Definitive
a)
the
reports/hand outs/teaching materials/studies
by the
generated
UPASI-CLWS and the Ross Unit continuing education
programmes.
b)
Organisation
of
3-4
District
level
workshops
in
the
Plantations on "Occupational Health and Research in the
Plantations".
These workshops will be an occasion to share the findings of
the
other
ROHC/RIUOH Tea plantation pilot study as well as
studies
identified by the recent assignment on "Health
Agriculture - Inter-relationships".
Plantation
medical
officers
and
Apart from keeping the
informed
about
recent
developments in Plantation Health around the world it would
also be an opportunity to ascertain the interests of medical
officers in research.
B - Explorative
c)
The
Feasibility of a comprehensive evaluation and
of
trends
in
Health
Status from the
analysis
collected on
data
estates participating in the CLWS Scheme from 1971-86.
d)
The feasibility of the evolution of a Plantation Study group
(consisting
of researchers from the different
institutions
and research units in India who were in touch with the Ross
which would
Unit),
organise and
support col 1aborative
research programmes with plantation medical officers.
Dynamics of Consultancy
i)
The consultancy will be undertaken over a period of six months in
1988
in
close collaboration with UPASI and
St
John1s Medical
Col 1ege.
ii)
The
consultant will be assisted by a full-time research
assistant
for the duration of the consultancy.
staff member
project
In addition one
each from the Medical Unit of UPASI and
from the
Department of Community Medicine at St Johns would be involved in
the
project,
and
would
contribute
to
specific tasks
and
participate in continuity of efforts beyond the consultancy.
iii) The
consultant and research project assistant will both base
in
Bangalore and Coonoor alternatively depending on the plan of the
up in the initial week of
consultancy drawn
Apart from
Coonoor the consultant and research
to
travel
also
the
plantation district
other
consultancy.
assistant will
headquarters
for
workshops and discussions with plantation medical staff.
iv)
the
of
One
purposes
of this consultancy
is
explore the
to
a broad-based support to Plantation Health work
feasibility of
to
from all institutions in touch with or initially linked
have
institutes will
to be made to CMC,
in
to
be
its
to
different
component of
important
an
Apart from centres in Bangalore,
consultancy.
Unit
2-3 weeks of visits
Hence
Unit project.
Ross
the
the
visits will have
Vellore (especially the Epidemiology Resource
Community Health
and Development
Department),
Institute
of Research in Medical Statistics and Regional
labour
Institute
in Madras,
National Institute of Occupational
Health
Ahnedebad
and the ICMR and other units in New Delhi.
worthwhile
to
establish links with
the Regional
It may be
Occupational
health Centre at All India Institute of Hygiene and Public Health
in
Calcutta and
contact some of the Ross
Units
(pre
-1972)
contacts in Assan and West Bengal Tea Gardens as well.
v)
The
consultancy is an adhoc step meant to consolidate
the
past efforts and explore future
provision
Ross
of
The
budget
for it will therefore have to be adhoc as well
From
sources with some inputs supported
locally
by
UPASI could provide for travel
and
Institute
UPASI and or St Johns.
1 ocal
some
eg.
alternatives.
hospitality for consultant and research assistant while in
Coonoor or travel 1ing/visiting in the plantation
st
districts.
Johns may help provide secretarial assistance for compilation of
reference manual including xeroxing and audiovisual facilities.
vi)
The research project assistant will need to be well versed in the
use
a word
of
processor and will
editorial
assistance
consultancy
in
For
and
other
necessary
undertake the
supportive
a participatory way along with
actions
for
the
consultant.
the
the preparation of the manual particularly the use of a word
processor is crucial,
especially to cut on the time of
repeated
typing of drafts.
A presents an approximate budget estimate for the short
vii) Appendix
term consultancy,
subject to further modification after general
consultancy is approved and any suggestions
format of
received
for modification incorporated.
on the consultancy may be circulated to the
vi i i)The note
UPASI;
Director,
Medicine
at
Secretary
Principal and Head of Department of Community
St Johns Medical College,
elsoe whose
and anyone
suggestions may be considered valuable.
ix)
A detailed
time
schedule of the Consultancy in terms
schedule,
consultancy
tasks
and deadlines will be
of
programme,
planned once
is accepted in principle and finalised in the
two weeks of the consultancy.
outlined in Appendix B.
the
first
Some broad components are however
x)
The consultancy will result in three documents.
a)
The manuscript of a Reference Manual on Plantation Health.
b)
A
report of 3-4 district level workshops on
"Occupational
Health and Research" in the plantations.
c)
xi)
A feasibility report on the Plantation Health Study Group.
1987
These documents can be discussed at an extended meeting in
all
between
the
units/institutions
concerned and
a
more
meaningful
fol 1ow up action on the future of the links
can
be
explored.
Publication
will
be
an
of the
Reference Manual
important matter on the agenda.
xii) The
consultancy project proposal is planned in such a way that
certain
definitive
workshops)
outputs (the reference manual
would justify the project
investment.
and
district
Additionally
the explorative objectives may help to make a breakthrough in the
quo situations of the three
present
status
(Ross
London-UPASI-St
Johns)
alternatives for the future.
with
institutional
evolution
of
link
feasible
APPENDIX B
Component Steps of Definitive objectives
I.
Reference Manual on "Plantation Health"
a)
Col 1ation
of documents/reports/handouts from archives which
will include:
Assam and Bangalore Ross Units
UPASIS-CLWS
Papers of Dr Donald Mackay
Papers presented at District level plantation medical
officers meetings
Reports/studies on plantations identified during
background reference work undertaken for "ICMR Tea
study" and " Health and Agriculture relationships"
assignments
i)
ii)
iii)
iv)
v)
b)
An
outline plan of object!ves/contents/formats/visuals for
the manual.
c)
An editorial review and selection.
d)
Compi1ati on
and
fi nali sati on
of
chapters
and
draft
manuscript.
e)
of draft manuscript to an editorial
Ci rculation
collective
and some key advisers.
f)
Incorporation
of
comments/changes
and
finalisation
of
manuscript for publication.
Note
i)
Items (a) to (d) will be attempted during the project period
while
(e)
and (f) will be followed up beyond
the
project
be
formed
schedule of 6 months.
ii)
It
is
suggested that an editorial
specifically
for the manual.
col 1ective
The manuscript could be sent
'• *
to
Dr
C
M Francis,
Professor David Bradley and
Dr
C
R
Ramachandran (ICMR) for additional comments.
II
District Workshops
a)
An
outli ne
workshops
of
on
the
scope and
"Occupational
dynami cs
Health
and
of
the
district
Research
in
the
Plantations" to be drawn up.
b)
An
with
exploratory questionnaire and some
initial
discussions
plantation medical officers to be undertaken to evolve
the workshop programme in a participatory process.
c)
Identification
of resource persons in addition
to
project
consultant.
d)
Handouts and reading lists to be prepared for the sessions.
e)
Organisation of workshops
f)
Compilation of workshop reports
g)
Compilation
of
an
Overview from the
3-4
district
based
or
col 1ected
from
surveys
and
i-
workshop reports.
Ill
Study of UPASI - CLWS Data base 1971-86
a)
Perusal
available
of
data
generated
participating estates through CLWS-86.
b)
Documenting
nature,
phasing, components
of
routinely monitored data.
c)
Outlining the possible methods of analysis of data.
d)
Outlining
a
more
detailed research protocol if a)
to
c)
establish feasibility of study.
■
j
ST SOHN'S MEDICAL COLLEGE,
BANGALORE 560034
COMMUNITY HEALTH mi
Directorate of Rural Health Services and^/1,(Fjrst
vt=L^
Training Program e
NEWSLETTER 3
NAY
1982
Dear Friends,
Greetings from Bangalore! -bJe' ret urned home after over hundred
days of travel covering approximately 10,600 kilometres in the
States of Karnataka, Tamilnadu, Haryana, Delhi, Rajasthan, Gujarat
and Maharashtrao It was an eventful journey and the modes of
transport included train, bus, jeep, rickshaw, jutka and cycle.
It was a wonderful experience of observing work at the grass-root
level. Rural India is so diverse in scenery, development, life
style and culture!
During the tour we met twelve CHWs, fourteen alumni doctors
of St John’s, staff from three departments of Community Medicine
and members of U.H.A.I., C.H.A. and the Medico Friends Circle. We
also visited centres and projects like Social Work Research Centre
(Tillonia), Centre for Science and the Environment (New Delhi),
Sewa Mandir (Udaipur), VIKAS, ASAG, Safai Vidyalaya and Behavioural
Science Centre in Ahmedabad, Prayas (Mangrol), Tapovan (Amravati)
and so on. The learning experience was much richer than we had
imagined!
NEWS OF CHills
It would be impossible to share with you all the details of
the work of those we met among the CHlils but here are a few salient
points?
(a) Sunanda Project
(KGF)
The name means ’The Bringer of Joy’ and the team which includes
two* of our CHUIs—Sr Jude (BC5) and Sr Nalini (BC8) are dedicated
to bringing joy and liberation through programmes which include
a temporary relief home for children, schools of tailoring and typing,
savings scheme, health and nutrition programme,9 non-formal education
through trained animators , resource farm and community organisation
in the-villages near KGF«
Two striking features of this team were
the gradual acceptance of a simple ’ashram’
life style and the
use of street theatre medium in non-formal rural education involving
animators who also belonged to the Dalit movement.
(b) Deepti Bhavan, Vimalalaya and Qyotirvikasa (Mandya)
These centres are run by the Missionary Society of St Thomas
with the assistance of the Sisters of the Sacred Heart Congregation.
The team includes three of our CHWs—Fr Joseph Purayidom (BC6),
n Oo
Sr Elsy (BC7) and Sr Francilia (BC7). The work includes living
among the people of the village, survey, dispensary, nursery
school and classes for non-school going children and extension
clinics. The project is in the formative years but the team has
a holistic plan and is committed to sharing, simplicity, manual
labour and team work. One of their dispensaries has been designated
a Fever Treatment Depot by the Government under the National F&laria
Eradication Programme and is acknowledged as the best one in the areai
(c) Kamagere Health Centre (Mysore Diocese)
Sr Artcilia
who works at this centre was away on leave
but we visited the centre and its two outreach sub-centres at
Hannur and Prakashpalayam along with Dr Ravindran, a St John’s
Doctor who works in the main hospital. In addition to the MCH
programme based on the CRS plan, the community health team also does
home visiting, clinics for leprosy and TB patients and runs a
savings scheme for local people.
(d)
Kalathipura Mission (Chickmagalur Diocese)
This little mission station and dispensary nestled amidst
coffee and cardamom plantations is run by Franciscan brothers.
Br tlency (BC8) came here after his course in December 1981, to
join a senior Brother who is well known through his dispensary
for miles around. The t_eam/§ocs survey work, home visiting,
catechism anc night classes for non-school going children and
adultSo After getting quite a comprehensive picture of the life
and problems of plantation workers through home visiting 9
Br Ulency is gradually beginning to work 'among anc. 'witti them rather
than only'for them. He also has good contacts with the local
government PHC.
(e) Tamil Nadu V HA Meeting (Macros)
On 19th Februray, we both attended this mooting on the theme
’Health through People’,
In addition to meeting many members
keenly interested in Community Health Work wo got the opportunity
to have a short group discussion with three of our CHiiJs—
Sr Justina (BC3) working with a team involved with MCH programme,
non-formal education and dispensary in Devikapuram (North Arcot),
Br Xavier Amal (BC3), now a warden of a boy’s hostel in Trichy?
..o.3
Co^' H
Aufrust 17, 1982.
Secretariat for ^bdical Education
St. John’s’Medical College
Bangalore - 560 034.
To: The heads of the departments, teaching and non-teaching and others
c once med.
<n
Dear friends,
Already a few months ago the former Bean and Secretary of the
Evaluation Committee f Br. C.h. Francis had sent you a circular regarding
the proposed Evaluation of our College. In this connection Br. Ashok
Sahhi> Birector of Indian Institute of T-hnagement and Prof. Krishnayya.
of Systems Research Institute, Pune have prepared their respective
questionnaires with a view to collecting the necessary data for the
process of the Evaluation. Br. Sahni has already sent'his questionnaires
out but the response so-far has not been adequate.
I request all of . you therefore to fill up the questionnaires supplied
to you and place it in the boxes kept with the Receptionist in the Hosnital
and the Bean’s Secretary in the College office. In soliciting this
co-operation from you, I feel confident that your contribution to this
Evaluation is going to be of immense value and will enable the Evaluation
Team and the authorities concerned to arrive at satisfactory conclusions.
In case any one wishes to meet Br. Ashok Sahni and discuss matters
with him, ho will be available in our College in Room No. 101 E,
(next to the Administrative Officer’s chambers) on Thursday and Friday
the 19th and 20th instant .between 2.00 and 5.00 P.M,
Once againI earnestly request you to fill up your questionnaire
and deposit it in the box meant for this' purpose by the 23rd instant
at the latest.
' Thanlang you,
Yours sincerely,
A
(Er. Ignatius Pinto)
Secretary
C.B.C.I. Society for Rbdical Education
Qi -
/Wjcca.
A/o.
10-if
I
INDIAN SOCIETY OF HEALTH ADMINISTRATORS
136/20, 7th Cross, Wilson Garden, Bangalore - 560 027
Cable: "HEALTHADMN"
Phone: 226237
August 16, 1982
To:
a) All faculty
b) Academic Departmental Heads
c) Key administrative officials
d) Senior administrative staff.
Dear Sirs:
Sub: Evaluation Study of St.John's Medical College
1. Kindly refer to our letter of July 15, 1982 enclosing
four questionnaires (five questionnaires for categories b,c,
and d above) requesting you to kindly fill out the same and
return to Mrs.Ryan by August 1, 1982.
2. We are sorry to note that we have received very low
resoonse so far. Your candid reactions and suggestions are
extremely important in establishing the goals, programmes
and organizational systems as well as nosition responsibilities
and corresponding authorities and powers.
3. Please do not write your name oil any part of the ques
tionnaire. All information will be statistically analyzed as a
group and not presented on an individual basis. Conies of the
report will be available for your reference. Should you like
me to meet you personally, I shall be gald to do so.
,4. Please fill out the questionnaires and return to us
by August 23, 1982.
Thank you very‘much and with kind regards,
Cordially yours,
Ashok Sahni, Ph.D.
Executive Director
C.B*.CH. Secretariat for bfedical Education
St^ ^hn1 s "Msdical College
Bang <Lore - 56O“O34August 20, 19S2.
To: The ^fembers of the faculty and others concerned.
Dear friends,
In connection with the Evaluation of our College, Mr. S.K. Sharma
of Systems Research Institute, Pune has' come to St. JohnTs and will be
available in Room No :101E, next to the Administrative Officerrs chambers
between 10.00 A.M. and 1.00P.M. and 2.00P.M. and 5.00P.M. on all working
days from today upto 3.9.19^2. You are requested to furnish him any
necressary information he asks for orally or through a questionnaire. If
during the hours mentioned above you are unable to meet him you can contact
him at our Guest House in the campus and meet him there. Tel.No:52349•
Mr. Sharma will be going round and having a look at the departments
in the College and Hospital whenever he is free;
Please extend jrour full co-operation to Mr. Sharma.
Thank you,
Yours since rely,
(Fr. Ignatius Pinto)
Secretary
C.B.C.I. Society for Pbdical Education.
I
I
I
i-
‘VOL
I
< -s
H /o-S"
ST JOHN’S MEDICAL COLLEGE,
BANGALORE 560034
-T-fJ
Directorate of Rural Health Services and^/1 #(Firsi
V'
Training Proar^g---------------------------------------------------BANGALOaV-R<>a<<
NEWSLETTER 3
MAY
1982
Dear Friends,
Greetings from BangaloreJ 'We'returned home after over hundred
days of travel covering approximately 10,600 kilometres in the
States of Karnataka, Tamilnadu, Haryana, Delhi, Rajasthan, Gujarat
and Maharashtra o It was an eventful journey and the modes of
transport included train, bus,, jeep, rickshaw, jutka and cycle.
It was a wonderful experience of observing work at the grass-root
levelo Rural India is so diverse in scenery, development, life
style and cultures
During the tour we met twelve CHWs, fourteen alumni doctors
of St John’s, staff from three departments of Community Medicine
and members of V.H.A.I., CoH.A. and the Medico Friends Circle. We
also visited centres and projects like Social Work Research Centre
(Tillonia), Centre for Science and the Environment (New Delhi),
Sewa Mandir (Udaipur), VIKAS, ASAG, Safai Vidyalaya and Behavioural
Science Centre in Ahmedabad, Prayas (Mangrol), Tapovan (Amravati)
and so on. The learning experience was much richer than we had
imagined!
NEUS OF CHWs
It would be impossible to share with you all the details of
the work of those we met among the CHWs but here are a few salient
points:
(a)
Sunanda Project
(KGF)
The name means ’The Bringer of Joy’ and the team which includes
two-of our CHWs—Sr Jude (BC5) and Sr Nalini (BC8) are dedicated
to bringing joy and liberation through programmes which include
a temporary relief home for children, schools of tailoring and typing,
savings scheme,
health and nutrition programme, non-formal education
through trained animators, resource farm and community organisation
in the-villages near KGFo Two striking features of this team were
the gradual acceptance of a simple ’ashram’
life style and the
use of street theatre medium in non-formal rural education involving
animators who also belonged to the Dalit movement.
(b) Deepti Bhavan, Vimalalaya and Oyotiruikasa (Flandya)
These centres are run by the Missionary Society of St Thomas
with the assistance of the Sisters of the Sacred Heart Congregation.
The team includes three of our CHWs—Fr Joseph Purayidom (BC6) ,
i 2s
Sr Elsy (BC7) and Sr Francilia (BC7). The work includes living
among the people of the village, survey, dispensary, nursery
school and classes for non-school going children and extension
clinics. The project is in the formative years but the team has
a holistic plan and is committed to sharing, simplicity, manual
labour and team work.
One of their dispensaries has been designated
a Fever Treatment Depot by the Government unoer the National F.alaria
Eradication Programme and is acknowledged as the best one in the areaJ
(c)
Kamagere Health Centre (Mysore Diocese)
Sr An-cilla «(B£6} who works at this centre was away on leave
but we visited the centre and its two outreach sub-centres at
Hannur and Prakashpalayam along with Dr Ravindrany a St John’s
Doctor who works in the main hospital. In addition to the MCH
programme based on the CRS plan, the community health team also does
home visiting, clinics for leprosy and TB patients and runs a
savings scheme for local people.
(d)
Kalathipura Mission (Chickmagalur Diocese)
This little mission station and dispensary nestled amidst
coffee and cardamom plantations is run by Franciscan brothers.
Br Uency (BC8) came here after his course in December 1981, to
join a senior Brother who is well known through his dispensary
for miles around. The t_eam/§ocs survey work,
home, visiting,
catechism anc night classes for non-school going children and
adults. After/getting quite a comprehensive picture of the life
and problems of plantation workers through home visiting,
Br Wency is gradually beginning to work 'among anc 'witti them rather
than only’for them.
He also has good contacts with the local
government PHC.
(e) Tamil Nadu VHA Meeting (Macras)
On 19th Februray, we both attended this meeting on the theme
’Health through People’.
In addition to meeting many members
keenly interested in Community Health Work we got the opportunity
to have a short group discussion with three of our CHlils—
Sr Oustina (BC3) working with a team involved with MCH programme,
non-formal education and dispensary in Devikapuram (North Arcot) 9
Br Xavier Amal (BC3), now a warden of a boy’s hostel in Trichy?
o
O . o O 3
A
-<
.
and Sr Constance (BC2) working in Vikravandi (South Arcot) with
the MCH programme of Pondicherry Diocesan Society.
(f) Qagadhri (Haryana)
It was quite a change to see the agricultural development
of the Haryana- villages when ujc
visited the project run by
Sr Co.rcena (BC4) of the Sacred Heart Convent in Oagajihri. The
team of sistqrs run a balvadi,
dispensary ano tailoring centre
in the nearby village. Their primary involvement in the area is
English Medium Convent, from which they have started this extension
work.
(g) Kalambi-Vihar (shilonda,
Maharashtra)
Br Tommy Kuruvilla (BC8) who was completing his regency in this
tribal area of Maharashtra, shared with us the experience of living
out among the people,
home visiting, conducting adult education
classes and health work.
A weekly clinic is run at this centre by
a St Bohn’s doctor—Sr Vilma Nazareth—who is in-charge of the
Mission Hospital at Talasari.
(h) Shanti Satan (Borsar? Maharashtra)
After a one-day Seminar on ’Community Health’
organised by the
Bishop for priests, sisters, teachers and parish workers of the
diocese in Aurangabad,
we visited the mission stations of Borsar,
Vaijapur and Ghogergaon along with Swami Sevanand
(BC8)
who is
himself the parish priest of Borsar and is involved with a very
holistic health effort of counselling and spiritual healing. We
also visited St Luke’s Hospital in Srirampur but were unable to
meet Sr Tresa Dose (BCl) who is a Nursing student.
It was encouraging to see CHWs Tliving among the people, learning
from them and serving them’ .
CJ
ct
cc
I—
(J
z:
CL
Ld
Ld
Catholic Hospital Association (refer address Newsletter 2) has drawn
up Diocesan Level Health Plans. Contact the Delhi office for names of
your regional animators and for more information about the programme.
Safai Vidyalaya, Harijan Ashram, Mahatma Gandhi Ashram Marg,
Ahmedabad 380027. Write to them if you have any questions or problems
regarding rural sanitation programmes. They have done pioneering work
in this field and have also produced health education materials. They
also run short practical courses for field workers.
With best
wishes and regards,
RAUI AND THELMA NARAYAN
ST. JCHNhS MEDICAL COLLEGE # BANG A LCR E
9 Aug 1982
Dear Doctor,
I am enclosing a questionnaire planned by the Systems
Research Institute o^ Pune.' The Review Commission set up by
us ,t° go into the question o^ whether the objectives for which
this College was instituted are being achieved in order that the
agencies that have helped us in the past may continue to do so,
have asked for certain expert analysis to be made. Systems
Research Institute is one of the expert organisations that has
agreed to undertake this work.
I shall be grateful if you would kind.iy fill in the
questionnaire and if you are not in the campus, kindly send it
directly to^Prof. J.G. Krishnayya, Systems Research Institute,
17-A Gultekdi, Pune 411 0C9, India, at an early date so as to
reach him before the end of August 1982.
If you are in the campus, you may either hand it over
personally to the Systems Research Institute people when they
come here in the third week of this month or deposit it in the
boxes placed for this purpose in Mrs. Ryan’s office in the College
or at the Reception of'the Hospital.
Thanking you.
Sincerely yours.
(Fr. Percival Fernandez)
Administrative Officer
: 5
DRUGS
USE MD MISUSE:
From this issue we a.
are Publishing a series of articles on
improper use of drugs for' a country like In^ia. The material has
been from the Medico Friends Circle. We start with an article nutting
the problems in persoective
HOW TO COMBAT MISUSE OF DRUGS ?
The greatest danger to Health in Ipdia is the over medicalising of
our Health Care System. Eternal vigilance is required that the
Doctor-drug producer axis does not exploit the people and that the
‘ abundance’
abundance of drugs does not become a vested interest in health*.
-ICMR/ICSSR study on ’’Health for .■'ll"
- an alternative strategy.
(1) 1500 branded drugs are on sale in Ipdia but a Government
Committee believes that Health needs would bej met by only 116
drugs.
costly)
There is now an overproduction
ot drugs (often very costly)
overproduction of
meant for the rich and well to do, while the drugs needed by the poor
people (and these must be cheap)
---) are not adequately available 1
The real purpose of an essential drug list must be seen as taking
drugs to those who need them most, not as reducing the drugs bill.2
Could we accept an essential drug- list- for cur-oractiee-in which
cosji__would be an important-criteria in selection in addition to
efficacy, safety and -quality?
(2) All UN agencies and governments involved in preparing a list
of essential drugs are convinced that prescriptions should be
through the generic names of drugs only.6
Generic name is not chemical name but official, international,
non-proprietary name e.g. , not Acetylsalicylic acid but Aspirin.2
Branded named products cost higher bec-4w.se they include
promotional costs and cost of claims of additional ingredients in
tormulation e.g. Librium by Roche is available for Rs.J16/-.ner 100
tablets but generic equivalents are available for Rs.1.50.
^AaS^UdY °? UNGTAD has shown that bio-availability argument ^or
anded drugs ie.,, therapeutic
on formulation
difference based
formulation is
therapeutig difference
based on
is
not very valid for most drugs.
>
- - - accept
Could _we
Generic Prescribing ? i.e.. By Aspirin not
Plusorin, B Disprin?, etc.
(3) ICMR/ICSSR and the Hathi Commission have recommended that
the small . scale sector, <cooperative sector should be encouraged,
Hospital and dispensary based formulations should be promoted. 1,3
r
Ian we prescribe drugs which are Indian ratheg.-fchan- t^reig^Government rather than-private-industry
industry.-.' small scale and
coocoratiye^ectpr rather than large sector ?---- ------------- —
-: 6
(4) Multiple drug combinations often containing drugs in amounts
far m.excess of what is required are presently marketed in In^ia.
here is a collPsal national wastage of drugs because of such
combinations.J
Packaging increases the cost of drugs very greatly becuase the
is to ™ake it attractive and highly elegant and to add cosmetic
embellishments to promote sales :?B 1
The^drugs Consultative Committee examined 34 categories ot fixed
doee combinations and concludedJ that in the case ot 23 categories of
these formulations, there was no therapeutic rationale for their
marketing.
Could we
values are -
drugs whose on
r-gleqant packing
• Irrational-combination
iniitatm .druqs Inadequate evidence of greater value ?
(5) An TCMR/ICSSR <study
1
observed that production of INH
and
and
Dapsone
are
third
a
.
,
--la quarter respectively,, of the minimal
r^guyeraents of the country. On the other hand, tonics and vitamins
which are mostly alcoholic preparation and soln money are produced
• 1
in wasteful abundance’
A study by Kamala Jaya Rao on tonics has shown that most of the
high potency or’4 7orte' preparations of multirvitamins are a sheer
economic waste.
,
T12ese . are not only a drain on the patients 'nurse'
e also help only to vitaminise our sewage systems.
Can we step this . rtonir’
practice ?
study by WHO has revealed that Doctors misuse •’drugs in : :
Hrugg. Drugs are nrescribecl in
75 ways. The commonest
corrmonest is overuse of ^rugs.
lone durations and too many drugs at the
for too lono
o?mA~timl
S CLiTie
,»
O
Drug: are prescribed when none are needed to retain the
patient's good will
Most patients believe (and many doctors would
like’ them to do so) that a good doctor prescribes large number of
costly medicines. 6
Drugs are prescribed to proVe that one is up to-date.6
rational drug therapy which- is-XaX necessary
—-———i£ic.nt—^I-c)
low cost and
(d) easy to administer ?
r=nrZsentM??wf!P°f
SS thaV dru9 advertising and contacts with
representatives of pharmaceutical firms are often the main sources of
-information for a physician on drugs and sometimes the only one.
uch information is -largely influenced by commercial interest.6
al?e °£Pen being ascribes by many doctors not because
-hev thin,< a particular nn<= is boet
^,,+.
because the company which produced it gives the maximum monetary and
material advantages and inducements to them. These range from free
samples (often sold in practice), pens, calendars, diaries, teas,
lunches, travel and conference attendance costs. 1,6
ContM. ./7.
-: 7
+-r> • Medical training in Colleges does-not train future Physicians
nor does it include
to judge a.preparation critically
conscious immunization against the half truth of persuasive
industrial advertising. 6
we stop accepting physicians
, ,
inducements from Medical Comp an i e
samples anc^ other forms of
(8) Many medicinal herbs and roots that are used by grandmothers,
- local dais and village medicine
*
•' ■ - - ~~ men ’ 1-------have been scientifically
tested
and research and known to have therapeutic value. Their descriptions
in journals collect dust in reference
---- j libraries <» 2.6
Herbal medicines and home remedies are not only low cost and easily
available but their popularisation will help in breaking the doctordrug producer axis for over 80% of the common minor ailments which
are
now being over-treated.
4_lnC1?ina has . integrated over 50 herbal medicines and home remedies
in their armamentariums not only as a drug policy but as an expression
of local participation in health care. 2,6.
we propagete s imple--heme-remedi es—and locally
herbal medicines after studying their efficacy ?
available
large number of technioues o^ healing are being
researched tiday in which diseases are tackled and cured without
drugs. Non-drugs therapies include Yoga, Pranayama, Meditation,
Accuouncture, Acupressure and Chiropractice among others. Traditional
systems of Medicine such as Ayurveda, Unani, Homeopathy which use
orugs but of a different sort are being resea£ched in various
places and the therapeutic effectiveness of many of their products are
being discovered and documented.
,. Can we adopt a more opeR-policy of enquiry and use of traditional
medicine and non-drug therapies ?
(10) Health Care is becoming increasingly a.quest for priorities.
Clean water before antibiotics, food before vitamin pills,
vaccination before kidney machined. , mG^ers milk before
.
powdered baby foods mixed with dirty water, health for villagers and
slums before more hospitals for the affluent suburbs of capital cities"?
"
Inspite_ of our preoccupation with- -Brug-P-reseribing—nelicy—eeu-ld
we commit outselves to other more important Health Care ‘Priorities ?
References:
1• Health for All - as alternative strategy
ICMR/ICSSR Report (1980^
2* Drugs and the Third World, Anil Aggerwal
Earthscan publication, 10 Percy Street,
London WIPODR (1978)
3• HaLhi Committee; Report of the Committee- on-Dru-q^s
and Pharmaceutical Industry, Ministry of Petroleum
and Chemicals, Govt, of India 11975;
Conf d.. ./8.
8
4e
5-
f£- 5
MFC ?^ok -containing .
Selection of Essential DrmQs, WHO Expert Committee<>
WHO TRS No,615 (1977) and 641 (1979)
6. Medicines as if people mattered - Health for the Millions
(MI bimonthly) Vol.VII Bo. 2 & 3, April-June 1981.
News & CorrespbddencQ
1
.
Polishing below a long letter by Dr. G.D. Ravindran.
The
tirst paragraph refers to a short course he attended in SJMCH,’ in
MN°MS Sheep' 3 an<3 1? hiS attenTOt3 to register anfl study for the
MNAMS & FCGP general practice examinations.
Dear Sir,
received your letters dated 11th Dec and 7th Jan.
4=
tor the greetings which you sent.
I thimk yor
I.reported to Sr. Chanthal on 30th of January, Since the.staff
was.going for a blood donation r
camp organised by the youth Congress,
I did not spend much time in the
The next day Sr. Chanthal taught
a lab.
lab.
me teverything about grouping,
cross matching, about blood collection
and about preparation of packed cells.
I rspent a fruitful day
learning everything about blood transfusion.- The. next ^ay ia'eo,,
January 1st, 1982 I spent revising all that I learnt,. Thank you very
much for the excellent arrangements. that you made.
• Our jnew hospital
’
at Prakashpalayam was ooene^ on 3rd of January.
The hosoital has 24 beds,
I yisist the hospital1 .every Saturday.
. »
I
have to see about 60 - 70 patients between 3 - 6 p.m.
”I "have to take
care .. \ of in-patient' also.
If they have a serious case I visit the
hospital. These days I am extremely
/
r"1!- bu’sy.
. ’ Only, this Sunday I arn
getting some free time,
I hone vou
Hence I. um writing to youc.
will excuse me for the delay,
I Vote another letter to Dr. B.C, RciO
reguesting him to enroll my name for the coaching classes being
organised for MNAMS & FCGP exams, So far I have not heard anything
from.him., • .
The sisters reguested me to stay for few more years here.
I have
tln December 1933.
By the end of 1W3' I- will be '
Moreover I enjoy workina here and
exarts"
I derive lot nfP 1
I derive lot of joy and personal satisfaction. I think it is beister
JSOC?mJg
becomin g frustrated and bitter trying for ^G.
to stay for one more year.
I hone that I will
04-,-Tl
Liaison6^!fi|e 6 rural newsletter arid also help from you and the
^fhen I was i__
in Bangalore I. could not meet you.
I met Dr, Ravi.’
He is coming here thistriday?
.* • 1 will be coming to Bangalore in the
month of April,
—*
3-m attending a weeks course on Psychiatry organised
by NIMHANS.
I hope that I will be able to meet you then.
Regarding the newsletter I have a few suggestion to make z
1. Please ask the Dean
-: 9
2. You Publish only the success stories in the newsletter,
I am sure
there are many of us who have failures and frustration,
I am sure
that they write to you about it. oiease try to publish some of it.
While I was in Bangalore few of the seniors whom I met commented
that the newsletter was a means of propaganda by the college. If
you Publish some stories of failure our students will realise
that the newsletter is meant for sharing rather than an instrument
of propaganda.
3. Working in the villages we
to forget laboratory medicine,
Please try to publish small articles on laboratory medicine
especially the pro^ecures involved.
f.
(G.D. R WIND RAN')
NAMES & AD''>res
c ES
OP
ottd
ditto
-DOCTORS:
10
NAMES& DATE OF PEOPLE FINISHIMC SOON*
rd ;1
/Ssd 0'■
1. Dr. Donald F^rhari^es
'-■'irtrrfjO r—' I r;.
> .F I ’7
: ~i/ ;f Fims^d -is Rural
IPBE.'
•2O Dr.
Maries Jose
r
” f i '>
F * *< j**!' r
s'*
. jd
J K
'
tO oj-:.
....'
J
•*'•
r
”
“ ?*”
,Wtll ;.be finishing on
OO /J
;5 3. Dr. Anthony FernAann!eK•r T'il «?. finishing
J
, itno"’ 'r{tr>''r
4. Dr. Jose
^• finishinc' on;Xst'June, '1Q82. ’ I M?
. ~r
5. Dr. G.D. Ravindran
xendd-riX LsocD oa<J
w-i i i >> p- • -u •
ill be finish i ng^ pij., 1s ^j J^?z ? 11Q82; epocn tin X
♦
-r
, - ... J-....:
£21“2^3«®L2®’2:
'
'
'
.h:„
,.■,. gf...g.
u,ivjS4^“h.?fU;X X7”
<
■/
owr««. e«a=t. ais „I1} h„v, on :^Sh :
......
»t -toKther, ports' i ,«mor
Th.Q .event wont off
'
7 ’.
11
We are proud when we hear that one of our students completed two
years of rural service. The name of students serving in rural areas
is made known every where, (e.g. it appears in the journal of C.H.A.)
so much propaganda is made about the people who oo to rural areas.
In this process we are forgetting the majority of our students.
Fr. Ignatius Pinto writes, "reports have also reached us that quite
a few, chiefly our religious sisters, have so adapted themselves to the
life style of the villagers that they feel like spending their whole
life time in the service of the poor, helpless rural folk. This is
because of the training imparted to them in their houses of formation
APART FROM THE EMPHASIS LAID BY THE COLLEGE ON RURAL ORIENTATION AND
DEDICATED SERVICE"e If this statement is really being implemented .
then why is there so much apathy and indifference amonq our students
to serve in rural areas?
Reflecting on the time I spent at S.JM.C. I feel that I did not
get any orientation towards rural health care. All of us were made
to feel that the only salvation for us was to become specialists and
It was a degrading thing to be a basic doctor.
super specialists.
Very few people have emphasised'’that we were to be basic doctors.
Most of the teachers have forgotten that they are basic doctors •
first, only then super specialists, and that they have to train
basic doctors and not super specialists.
I remember how our medicine clinics used to end up in neur© ophthalmology (the person who took these clinics was a neurologist)
some how every patient whether suffering from GIT, CVSZ or R.S.
disorders used to end up having a neurologicfel abnormality. So
much so that we used to look for a neurological abnormality in every
patient (somehow cook up a finding to
please him) we examined.
to.nlease
This disease of soecialisation is not limited to clinical
I remember how we mugged larynx for anatomy
departments alone,
exams, when we heard that one of the examiners had done some research
work on larynx (unfortunately not a single Question was asked on the
larynx).
I am mentioning these instances to show how much the idea of
specialisation is prevalent in SJMC. Any number of instances can be
given when we are exposed throughout to the idea of specialisation •
How can we all of a sudden think of becoming basic doctors?
We are exposed to rural health through the 'Departuient of
Most of us have an impression that the rural
Community Medicine,
health care is a complete monopoly of the Community Medicine Heot.
There is not much glamour attached to Community Medicine, The same
thing is added on to rural’ health.
After working for one and a half year in rural areas I have come
to the conclusion that we cannot practice any preventive medicine
It is no use speaking to
unless we have a good educative base.
the villagers about sanitary latrines if you cannot treat his
diarrhoea. Clinical staff should get actively involved in rural
health. Present day involvement of the clinical staff in rural work
It does not serve
is by conducting one day camps in the villages.
:
12; t _ ■
1
- ' ’
-
.
'
■:
J. .7'1
3 i. ;J
' ' '
; :
'
' ■■ ~
. • .'
,
' '
•
’
. '
J
B
to fa maiprWbsnitaf
and a^.-king. them to -borne' for
thatf''fnetoK cfeicirP sensei tb cobie^tp'a
J
Most ot the Vi i 2 acorn
major hoscitMf'^rf Wy arc tsaldWWciy UWis ohly 'their! economic
PV
. ...
conditions' whAWWrbteW'th^h f boWibmfnd.7 ' ? :
■ ■ ■r
P 0VI by fl 1
'■ '
' t
' .
•; 1
5 '
.
o . borhg a i: .b
dr - Tnbtetad gE these bhei ffle.^ oigbibs/Wdabbbtgyh^'W^W tai tn <:''
■o Sx
spend-atEe-ast a gibntfi inctunad'areab ^Ver^^at.' WHs-lynn of
programs wltl; wake
ruta'l^brihbtatlnhWo' their teaching ‘
and also will make them realise that they ar,e basic doctors, first.
r egarding
internship
■
:n niSeven ofrus-were-Posted at Mallur.
Since it wa‘s a big droub " ' ;
there was' not-enough trbtk'tor1 al 1 (Doct&fs: betibhth1 ratio l-Wf i : h
It was our first .costing as-interns. The medical-.Officer was bn
leave, we used to run the clinic. Each one of us choose a rpiriorspeciality anflttuaied<ii .In ;htflil1-1if
1^ Sd matifeht’'babe
nstient came? ' with."”
n C n
T 4 -i-lh ifeNm
skin complaint, he wastref epe’dn£o somebody, ■-'if!
he'c'smekwitb;r
corpnlaint'' tbr Someone else' This ' way bvef?
even’ ip
our rufa 1 ' Bost inn ?>re
in bhhwnirarftpsEind
we ’ 'vt';'
i fij- ‘ re r.s
.
< ■'
: cj;- e to.. if
i ■ 6 '--w .ns:?
becaome minbr? specialist. 1 -<‘ a- ' ' '--..g' ’ •
1/
L
G
t
How Is the-vassesSment
WiseWy Whe^ tt 'i9 • n^rasfesseej-
by ther.service bender»<S; to •EHi bormiunity; SWis' assey^grVWy thS' ?
project -feoorti This ; efribWasis'-Sn'oroj bc't rgoortt^akes the stGdPnts
concentrate op projects and neglect the neonle.
Reflecting on all the above, mentioned instances, I wonder
whether any of us had jany rural orientation in S.J.M.C. It is a
wonder that INSPITE of
-- St. John’s, our
<
venture to work in
students
rural areas.
I hone that their tribe increases.
Dr., Ravi Narayan has written that the Dept, of Community Medicine
has organised a rural camo .for the 1st year students. At last some
change is seen in SJMC.
It is not enough if a 1 month camo is held
1st year is
uring the 1st year.
Most of the studetits are immature.
tne transition period from a regular college to a professional one.
Hence these 'camps are bound, to become like N.S.S. Canos. The college
should post students for a month in rural areas every year.
I am
sure that if our students get in contact with the rural masses during. : ’
clinical year most of them will go to rural areas.
. Instead of costing interns for one month in their chosen
speciality, post them for . 15 days, each in all the minor specialities.
This way our students will have a working knowledge of all the
specialities.
I hope a Say will corne when most of the students of S.J.M?. will
go willingly to serve in rural areas.
G.D.
RAVINE) RAN.
'
SYSTEMS
RES ’E ARCH
J.G.Krishnayya
Executive Director
President
J.S.Lail
INST ITUT'E
Vice Presidents
C. Rangarajan
- L.G.Rajwade
17-A Gultekdi
Pune 411 009
(India)
Te.l_...s 470323 '
Dear Alumnus,
F_
We would like to introduce ourselves as Prof.
JG Krishnayya
and Mr. SK Sharma of Systems Research Institute, Pune. oxxx
SRI is
a non-profit centre of policy & management research involved in
study of public services including rural medical services,
In 1979-80 we worked clcs ely wi th the CMCH
hcs pitals, etc.
Vellore in the development of their forward plan. We have now
been asked by the St. John’s Evaluation Team to assist in their
study of the college•
St. John’s has several unique features which m&ke this
study a very interesting one. We plan to meet individual
members of the faculty very soon, but before that we thought it
would be useful to send you this questionnaire which identifies
the questions we have. We would greatly appreciate your filling
it out carefully, making your own comments wherever necessary.
Kindly post it back to us in the envelope provided, The
individual questionnaires will be treated as confidential, ux
of
course, but we hope the Evaluation Team will find our Analysis
useful.
Thank you.
J.G. Krishnayya
S.K. Sharma
SYSTEMS RESEARCH INSTITUTE
SRI/SJMC/July 1982
QUESTIONNAIRE FOR ALUMNI DOCTORS
Note : Please answer the questions as freely and fully as you
can. The answers to these questionnaires will be kept at SRI,
nnd only the analysis supplied to the Evaluation Team,
Some of these questions are factual a nd some ask for
your opinion or impression; they are equally impottant
for the success of this Survey.
4
1. Name (optional)
3. Place of birth & Age
4. Father’s Occupation &
Education
5. Grandfathers* Occupation: 1 (Maternal)
& Education
(Paternal)
6. Religion
Approximate annual income
:
today
2. Sex:
2
8. Educational background (High School and abcve) :
(Please give names of the institutions/ places/ and dates)
Name of the Institution
and Place
Degree etc•
Date
Work Experience (Please give names of the Institutions/ places
& dates) :
Dates
Designation
Nature of
Name of the Institution
duties .
and Place .
‘1
10*. How marly years were yon. at St.John’s and in what capacities?
Please g ive de ta i1s•
Nature of Duties
•Designation
Dates
■■ V?.
11. Other •family members at St.John's (Past and Present) :
Please mention relation/ role at St. John's/ and approx.dates•
?[
■..I,.
12. How did you: first hear of SJMG?
From parent s/frlends/relatives/
Others ••• (please specify)
3
13. Why did you decide to join Medicine?
a) Parents * encouragement
b) All friends were also joining Medicine
c) Other reasons (please specify)
*-
1
14. Your current place of work is
Rural/Small town/City/Abroa d : Third World Country /Developed
Country
15. Did you go in for higher studies after St. John's?
/Wh ich
Yes 7 No
‘ ' dVis c ip 1 ine?
Where?
4.'”’
16. You are working in:
[Government[Private [How many beds?
Private [Mission-[Mission
Practice [Hospital [ Management [Hospital
[Hospital [
it
i
✓
«
«
17. In which of the following activities (one or more) are you .
involved? Please give a percentage breakdown, if possible
(in terms of the time spent)
a)
Curative medicine :
b)
Preventive/Community Health Care : /
c) Teaching
d)
: Medical/"^"? Nursing/
/
7 Paramedical.
Research
e) ? Rural Development
f) Administration
18.
(DO NOT ANSWER this question if you are a full-time salaried
.
employee)
What percentage of your work,? in terms of time,
is charity, Ke. without getting any monetary reward?
19* Does St.John's Medical College have the following major
objectives?
(Your impression please)
A)
ti
Training Doctors for Rural Health Service1’.
Yes / No
VJhat has S JMC done to ach ieve this objective?
(List actions you know atout)
How well have they succeeded?
Very well/So-so/Not at all
What could they do to improve in this area?
4
B)
"Inculcate ’Catholic' values in Doctors".
Yes / No
What has SJMC clone to achieve- this objective?
How well have they succeeded?
Very well/So-so/Not at all
What could, they do to improve in th is area?
C)
"Train ing for Medical excellence",.
Yes. / No
What has SJMC done to achieve this objective?
How well have they succeeded?
Very well/So-so/Not at all
What could they do to improve in this area?
D)
ii
Provide professionals for Catholic Health-care
Yes / No
institutions".
What has SJMC done to achieve this objective?
How well have they .succeeded ?
Very well/^o-so/Not at all
lAThat could they do to improve in this area?
2 0* In which fields do you think St.John's should strive to
400-1-beds
become a professional leader?
leader*^
(The hospital has 400+beds
now and is going to grow - in which departments or in which
direction, do you think this grovrth should take place.)
5
5
21. St. John's has tried to be innovative in the following areas.
Kindly indicate the success of these innovations. Please
also make explanatory comments indicating whether the
innovation is desirable and■suggesting improvements.
Innovation
Hesult
a)
Selection process
(including attitudinal
tests etc.)
i) Totally successful
ii) Partially
do
iii) Failed
b)
Integration and
semiencing of courses
(e.g. clinical and
non-clinical)
li)
ii)
iii)
c) Orienting students to •
rural practice
i)
ii)
iii)
d) Teachino Medical Ethics
i)
ii)
iii)
e) Teaching First aid and
Nursing procedures
i)
ii)
iii)
f) Teaching Bio-statistics
i)
ii)
iii)
g)
Comments.
Internship with 6 months' i)
community health inclu- ii)
iii)
ding 3 months in
villages
h) Tutors (Guides) for
i)
small groups of students ii)
iii)
i) Electives and Research
for students
i)
ii)
iii)
j) Curriculum Planning
i)
Committees -with student ii)
representatives
iii)
k) Full-time and non
practising facu Ity
i)
ii)
iii)
1) Bond to serve at a
place designated by
the college
i)
ii)
iii)
22.
i* the average social stratum of your own patients?
(Please also give a rough percentage breakdown ifpossible)
6
-very rich
- rich
- upper middle class
- lower middle class
- poor
- destitute
23. St. John’s graduates are. by and large (please tick one) :
1. The best in the country
2. As good as the best in the country
3. Not as good as the best in the country
24. If 2 3(3) why?
25. St. John’s graduates command (please tick one)
great respect in your field
2. average :respect in your field
3. poor respect in your field
26. If 25(3), please give reasons why?
*
27. St. John’s radical education is
1. the best in the country
2. as good as the best in the country
3. not as good as the best in the country
28. If 27(3), where are the gaps?
29. What are the research outputs of St.John’s that you
have heard of?
30. St. John’s research is
31. If 30 (3), please give reasons why?
32. Do you find your present place of work as good as St.
John1s ?
Better
As good
Not as good
33. Please st^te why?
34. Would you like to go back to and work at St. John’s?
so, under what conditions?
If
35. Please list 3 major shortcomings of St. John ’ s «
1.
2.
3.
36. How relevant is the St. John’s training to the Indian
’health* environment? Please tick all the statements you
agree with.
- is as relevant as any other medical college in the. country
- trains doctors suitable only to work in large hospitals
- produces graduates who go out and work in the rural areas
- St.John’s education tends to orient students towards
specialisation rather than in a General Practitioner’s
role
- producer graduates who want to work with the most
sophisticated eouipment
- produces graduates who believe in humbly serving the
people
- produces doctors who are urban-oriented and want to
work as consultants
- produces doctors with driving ambition to do well
- produces doctors who can work in any environment
8
37. Having been trained at St. <John's has helped you (please
tick those that you agree with)
- in just getting a job
- in getting a professionally satisfying job
- in getting good remuneration
- to gain resoect from professional colleagues
- in treating very complicated leases
- to develop a good rapport with your patients
- to help the poor •
- in charting a lifetime career
- in selecting a field of specialisation
38. Have you faced any disadvantages because of your training
at St. John's? Please explain:
39.
In your professional capacity, which International/National/
Regional Organizations/ Committees, Panels etc. do you
belong to?
40.
If you are practising now or have practised, in a rural
area (if not, please go to Question 41) - Did the St.John's
training ecruip you well for this field? Yes / No
What gaps in your training do you no7 perceive?
Personal aspects:
a.) What are thedeprivations you experienced/are experiencing
while living in the village?
9
b) Wat is the
minimum level of amenities a doctor in your
™
position would expect to have in the village?
c) Do/Did * *
tW
abOUt lwrovin 9 the general conditions
in the village
ge through your personal initiative?
d) How important was/is it for
you to have the cs.
company of people
with similar status and int ellectual capaci ty?
-> Very
impo rta nt/D ome wh a t irfiportant/Not impcr tant
e)
How serious were the problems
family (if any7 in
—i the village
No problems
(Please give some examples)
T----- --- _
.4
adjustment faced- by your
Very seriouS/Somewhat serious/
J Do ■you think ■Doing able to s
the■ disadvantages of villageserve the people overcomes all
a life?
Yes / No
fe22L§^s_ipn^^^]D_ecus.
g) VJhat. suggestions do
you have for overcoming the problems
faced by doctors in the villages?
h)
How does the work in fural
areas affect your career prospects?
!
■I
10
deficiencies which
in the~ vPlages the
preventive medicine?
m both
---.I curative and
J) What yparticular
• *
eftorts d<Ld you make to
deficiencies?
remedy these
now successful
were these efforts?
41)
WLa+- kjnti of
U in. Ing
courses would you like to
attend new ?
What
tei°'
Sys
in India,: Of other
in India,
eopathy. Ayurvedic, Unani etc.?
So-X
medicine
43)
44)
Did
you sign the
st St. John’s?
Xf
/1fcer’1Oe b°"a
yon, did you fulfil the
bond or
taking admission
repay the bond amount ?
45) What ; l._.
?oo^, oo^ooo/f
S
Smaller/10,
46) To what extent
ytent would you be WiUlng to __
weaknesses in a
little/Not
^ dev°ut person?
little/Not at
at aliel:LglOU!3
all
■?£Sessional
Quite a bit/A
47) Do
^inb that ]being a doctor is
a Professional
1ii
------ calling/like
any other
occupation for earn ing
48) ln r
comparison with an IAS (
1 ike
officer of your cwn age
I
»' *
11
50. What would be the' special advantages to St. John's(and the
disadvantages) of university recognition for PG courses’?
51. Do you agree with the 'No Private Practice' policy for
faculty? What are its advantages and disadvantages?
52 .X^Jiich are the 3 major strengths of St. John’s?
5 3. In your opinion should St. John’s future efforts be
directed towards training doctors in
a) Modern high-technology medicine
or
b) Community heal th/Rural medicine
Com h »o- C
♦
ST. JOHN'S MEDICAL COLLEGE,BANGALORE-5600^4
RURAL HEALTH SCHEME ~ NEWS LETTER
January-March 1982
VoL 2 No ? 1
EDITORIAL:
Dear Friends ,
In the first issue of this newsletter (Jan-March 1982) I had
written that I honed that all <of you would use the newsletter to air
your views and that we would soon have a vigorous
.. 3 .ebate conducted
through our correspondence column,
It has taken a little over a
year to set the ball rolling, In this issue you will see a
a letter
by G.D. Ravindran and also an article by him.
I will say no more
about either of them except on a few points
O —
1. Dr. Ravindran is one of our success stories.
stories. He is
happy where he is and in fact intends to stay on at
his hospital even after his bond period expires.
Hence his views need special attention.
2. He has asked the Dean to write a column regularly.
The Dean has promised to do so.
3. He writes that there is a feeling that the newsletter is
a means of oropoganda by the College" as only success
stories are Published. Here I must disagree with him
strongly. Firstly, the college authorities have
never tried to influence what is nublished in the
newsletter. That is solely my responsibility. In
fact a cony is sent to Jne Dean & Fr. Pinto after it
is posted to all 6? you, and that is the first they
I must ask you to believe me when I say
see of it.
that I have no interest in "Propoganda". On the
other hand,.I cannot publish the darker side of the
oicture unless you write and tell me your comnlaints
of the system.
So please, ffeel free to write what you feel and you
can be sure
that your views will be aired.
PREM PAIS.
FROM THE DEA^S DESK
Greetings to all from St. John’si
The problems and issues of St. Jf,
John’s Medical College with
Bangalore University remain unresolved. A time has now come when
action is called for
Conf d. ./2.
*
: 2 :
We have been waiting oatiently for long for the Bangalore University
and the Government of Karnataka to bring a solution to these issues.
Everyoneagrees as .to the excellence of our institution whether it
be in the field of training or oatient care or research. ^he
^hievements of the students at the various examinations sneak for
the excellence in teaching and learning. In the recently announced
list of Rank-Holders for the first ten ranks, 8 out of ifl- (l was
bracketted) were from St. John’s, including the First and Second.
The.hospital in the campus has been doing very well in. giving good
patient care and in expanding its services. nuring the year, the
sanctioned bed strength has gone up from 250 to 401. The institution
is carrying out quality eesearch in the fields of Malaria, Diahorrea,
Cytogenetics in Mental Retardation and other areas. Insoite of all
hhese achievements the University has not given Affiliation for the
institution from 1981-82 onwards'. Sanction for starting nost-graduate
Course of study has not been given even though this matter has been
pending from 1971 and the college has all the necessary facilities for •
Post-graduate studies’. 1 The St. John’s Medical College Hospital
built, equipped and staffed at great expense to be a model teaching
hospital has not been recognised by the Bangalore University tor
teaching purposesL I ’.
Hopes of a solution for these problems came when the Chief
Secretary to the Government of Karnataka called a meeting on December
17, 1981 at which the Government Secretaries for Education, Health and
Law, the Secretary to the Governor, the Vide-Chancellor of Bangalore
University and the Director of Medical Education, Karnataka State
were present. The college was represented by Bishop Patrick D'Souza,
Chairman of the Executive Committee, Archbishop Henry D1Souza,
Secretary General CBCI, Bishop Alphonsus Mathias, Bishon of
Chickmagalur, Fr. Ignatius Pinto, Administrative Officer and the Dean.
At this meeting it was resolved that early steps will be taken by
the University and all formalities completed with resnect to all these
3 pending issues, such that Government Orders could be Passed before
28th February 1982. This date has now come and gone away but the
University has not even moved to appoint a local insepction committee
which according to them had to be appointed as the first steo.
The Government has failed to keen its Promise.
Two members of the Minorities Commission, Mr.Giani Sujan Singh
1/ /“
and Mr. Dorai Sebastian along with Mr. G.S. Sial, IAS, the
Secretary
visited Bangalore from the 15th to ,17th February 1P8 2 to oo into the
Complaints of the college with respect to the harassment by
Bangalore .University. The Commission was very much impressed by
the facilities provided in the College and the' osnital. They met
all the concerned authorities of the University and the Government
including the Governor and the Chief Minister. All •-<?. of them
promised that action will be taken soon but nothing has happened.
The strategy would appear to be to go along with the arguments and
to praise the institution but do nothing about it Pushing the
institution to a situation where they will be forced to agree to the
unjust demands. The Commission has issued a press release in which
our. College but it had no desired effect.
they
-- ± have praised vzuij
Meanwhile the Institution is going on doing its very best combining
concern.
it
and social
excellence
We need your he Id.
Wishing you all the best.
Yours sincerely,
(C. Mt FRANCIS, MBBS,Ph.D)
:3 :
MEDICAL CORNER
HEART DISEASE & PREGNANCY
Pregnancy can effect the heart in 3 ways:
1. Diagnosis of heart disease where none exists.
2. Aggravation of pre-existing heart disease.
3. Pregnancy per se, as a cause of heart disease.
Circulatory Adjustments in Pregnancy:
1. Cardiac out-out increases by 40% mainly due to increase in
blood volume.
2. During labour, each uterine contraction is associated with
increased cardiac outout and increase in blood oressure.
3. Soon after delivery, there is a dramatic increase in blood
volume as uterus involutes.
All changes regress by 2-3 weeks after delivery
Signs which do not necessarily mean heart disease in a oregn^nt women:
1. Pedal oedema
2. False sense of cardiomegaly due to elevated diaphragm.
3. Ejection systolic flow murmer at the base of the heart, ^his
flow murmer usually appears around 12th week and disappears by
1 week after delivery.
4. Mammary Souffle - a continuous soft murmer at sternal border
It appears late in 2nd
due to dilated mammary vessels.
trimester and is easily obliterated by oressure.
Supine hypotensive sundrome:- eoisodes of syncope and dizziness if
patient lies supine. It is due to uterus compressing IVC and is
treated by telling the patient to lie on her side.
Rheumatic heart disease and Pregnancy:- In India RHD is the
Commonest form of heart disease associated with pregnancy.
Mitral
stenosis is the commonest non obstretric cause of death in nregnancy.
Heart disease must be suspected where there is
a) History of pre existing heart disease sr murmer.
b) Systolic murmer associated with a thrill.
c) Any diastolic murmer.
cO Atrial fibrillation.
e) True cardiomegaly.
Effects of pregnancy on RHP:
a) Murmers of MS and. AS increase becuase of large blood volume
murmers of AR and MR decrease because of low oerinheral
resistance.
Conf d,.,/4.
old ni
'
-•n OiV I-
Ph Vs
pm m., ,r
piilbupy (^.
-Pc’S,
4tTiW (b '
.ylspomoiboso scnT (p
mfoow i- -- s Vd j-zpeoppA eeroano ’ IA
‘ dd>L ['£ J-pg
i*d:LpC?-
............ OB- SH
Physiological tachycardia of nregnancy.'-;...-;;.,^\
•;
. mgc'i rfon m .• i;'Odrvel s mJ- Ptrf / F sp#;;m-.f
3v- ptsnoS' sa.tr ?4 ..2
a J ri‘T , c-) Pulmonary oedema-• is6especially; liable • toe occur at':•orsoon
^^labour.
It- must be: treatedlwith intravenous morphine
\4'-5-mgm) lasix
. Janoxint (0.5 ^mgm:k- and in sever severe
...■•.vo.r ;:„^ases by.vOiesection of.-1. pint pf bloody
■
Antenatal care of patient: ■
’ ■’
R '
-.A
A2H
..
f m'• g f 1.
t.-a)- Pr eriodiemi monthly')' evaluation, y.
.£■.
.?i ktoi offSet -2rhours
in aftepiaop©; ^4- fcho^rsc^
r. sc. \ ,ev ear
require^-. . <■> j-isoff ";O
fl .f.
pl tCo^rgct .aggrava-ting.-ana^mia.-rPresjodratoryixnf_eetlons
1 soliM
.Ybyp^rtensdoti. (PET^iorecurrent:-.theumatic feyer>.<ir.dY\P^
.
- placental ihsuff iciency .may result.
.
,rr
e) If rpu 1 monar^-o^tematdevelops r -advice- -h-bshita4i-S-atioh--feifl 1
term.
te
rm *
’
f) Admit Patient a few days' prior to due date.
:
Management of labour:
s
Vaginal delivery with forceps to shorten 2nd stage. Keep patient1s
shoulders and head elevated. Additional 'd-u-iretics- ahd- digoxin may
be given to cover stress of labour.
Prophylaxis' against SB1S - Pfochine penicillin 6 lakhs i.m.
BD + streptomycin .1 gm l.m. OD from onset of labour to 3 days after
.
..
delivery.
. On;discharge• advise delay or prevention of next pregnancy and
surgical correction if possible.
Role of Cardiac Surgery :
Very rarely required. An occasional.natient with MS and
refractory pulmonary oedema may need\early surgery*
Termination of Pregnancy:
Also very rarely required,
Indicated if oatient ‘develops
pulmonary■ oedema in 1st trime.stpf.. Thereafter, it. is better - to.
'. - //■’X.cC' 0
7':'
carry the'patient through to term.
L
-.v'd ’./fc-hWi
Sign of poor prognosis; ,
- Maternal age over 35 years.
- history of heart failure in the Past.
- episode of acute rheumatic fever in previous 6 months
- atrial fibrillation.
PREM PAIS.
F
Co/n H Fo.3-
■'-rswoa*
t JOHN'S MEDICAL COLLEGE, BANGALORE 560034
Directorate of Rural Health Services and
Training Programmes
0-0-0 —oo-n-o-o-0-0-0—0-0-0-0-0-n-o-o-o
Ne u q
LETTER-2
FEBRUARY 1982
Dear Friends:
We have been planning out our travels in response to your
letters* The prospects are becoming more interesting day bv day.
It now includes a 35 km trek in Orissa, a meeting on Health
in Aurangabad,, a Health Education Seminar in Mizoram, a
sojourn through the' North East and the tribal regions of
Andhra, Bihar and Madhya Pradesh and so on. We arc also
visiting some alumni doctors of St Johnrs working in rural
areas and some health and development projects run by
other groups. It will not be possible, therefore, to visit
all the CHWs in their place of work, as we have- less than
300 days for our travels. We hope that we will be able to
meet some of you in small groups at Central places for a day
eg., Mangalore, Goa, Karwar region, Mananthavady, Calcutta,
Hazaribagh* Varanasi etc. You will soon get letters from the
organizers* The first phase of our travel starting from last
week of January till end of April will include Kolar, Salem,
Mandya, Kollegal, Chickmagalur, Madras, North Arcot. Then to
Delhi, Rohtak, Jagadhrij Chandigarh, Ludhiana, Tillonia,
Udaipur, Ahmedabad, Vadodara, Rajpipla, Zankhvar, Talasri,
Thane, Talegaon, Pune., "Jamkhed, Nasik, Aurangabad, Amaravati,
Wardha, Nagpur and back. We shall be writing letters to
individuals giving further details.
In Madras, on 19/20 February, the Tamilnadu Voluntary
Health Association have arranged a meeting and we hope to
meet many of our CHWs there. Do keep in touch with us
particularly if you change your address or your work. Our
contact address will be D-10, Staff Quarters, St John’s
Medical College, Bangalore 560034 till June. You will have
to excuse us for delays in replying since we shall be. on wheels
most of the time. If the matter is very urgent, please mark
’urgent ’ and ’redir ect ’ on the cover of the letter; otherwise
they will await our arrival.
’’Many problems can be resolved when people work
together and give each other help and support”
r+
g
ft
ff
) Keeping contact with the Department
While we arc away on our travels, if you are interested
in the following T . ■'
■
r
<
a. List of latest addresses of CHWs of your batch
and those working in your area;
contd...from pre-page
:2:
b. Letter to your PHC doctor or DM0 (Dist Med Officer)
introducing you and r co nesting them to encourage
you ond include, you in their programmes (send name
and address of doctor/s);
c. Details of next Basic Course or "Refre sher Course;
d. Any other information
•
please write to Professor SV %ma Tteo, Head of the Department of
Community Medicine, St John’s Medical College, Bangalore 560034.
) Keeping track
We have ho hews recently from the following, If you are in
touch, please'send us their latest addresses and news about
what they arc doing.
BC6 .
- Sr Paula, Sr Stella Mary, Sr Bctcy
BC5
- Sr Annette, Sr Genevive, Sr Nirmala, Sr ./Inna Joseph,
Br Sebastian Dung Dung, Br Francis Tiru
BC4
- Sr Anastasia, Sr Egidia, Sr Evangeline, Sr Setvia,
Sr Josetta, Br George MM
BC3
BC2
Br G Victor
- Sr Shuba Minj and Br Nirmal
News of any of your other colleagues will also be always
welcome.
(4) Contacts with VHZil/CHA
Hope you are in touch with VHVI (Voluntary Health Association
of India, C-14 Community Centre, Safdarjung Development Area,
New Delhi 110016) and CHA (Catholic Hospital Association of.Ihdia,
CBCI Centre, Goldakkhana, New Delhi 110001). They will keep you in
touch with new concepts in health, audio-visual education materials
and contacts with others working in the field in your States.
(5) Newsletter
We would like you to share some of your experiences with the
others through short articles on your work. Please write and we
shall put them in. If you’have not written to us’or to the
Department after November 1981, please acknowledge receipt of the
newsletter giving latest address to continue getting further issues.
With best wishes and regards,
RAVI & THELMA NARIYAN
l”Primary Health Care is not just medicine. It means ditches,
I water pipes, nutrition, latrines, family welfare. Health
| is development”. — Earthscan
|
Com H io g
ST JOHN’S MEDICAL COLLEGE,
BANGALORE 560034
Directorate of Rural Health Services and
Training Program e
NEWSLETTER 3
NAY
■ 1982
Dear Friends,
Greetings from Bangalore^ We returned home after over hundred
days of travel covering approximately 10,600 kilometres in the
States of Karnataka, Tamilnadu, Haryana, Delhi,‘Rajasthan,•Gujarat
and Maharashtrao It was an eventful journey and the .modes of
transport included train, bus, jeep, rickshaw, jutka and cycle.
It was a wonderful experience bf observing work at the grass-root
level. Rural India is so diverse in scenery, development, life
style and culture!
During the tour we met twelve CHUs, fourteen alumni doctors
of St John’s, staff from three departments of Community Medicine'
and members of V.H.A.I., C.H.A. and the Medico Friends Circle.' We
also visited centres and projects like Social Work Research Centre
(Tillonia), Centre for Science and the Environment (New Delhi),
Sewa Mandir (Udaipur), VIKAS, ASAG, Safai Vidyalaya and Behavioural
Science Centre in Ahmedabad, Prayas (iMangrol), Tapovan (Amravati)
and so on. The learning experience was much richer than we had
imagined!
NEU1S OF CHUs
It would be impossible to share with you all the details of •
the work of those we met among the CHUs but here are a few salient
points;
(a) Sunanda Project
(KGF)
The name means ’The Bringer of Joy’ and the team which includes
two of our CHWs—Sr Jude (BC5) and Sr Nalini (BC8) are dedicated
to bringing joy and liberation through programmes which include
a temporary relief home for children,
children,, schools of tailoring and typing,
savings scheme, health and nutrition programme, non-formal education
through trained animators, resource farm and community organisation
in the villages near KGFo Two striking features of this team were
the gradual acceptance of a simple ’ashram’
life style and the
use of street theatre medium in non-formal rural education involving
animators who also belonged to the Dalit movement.
(b) Deepti Bhauan, Vimalalaya and Qyotiruikasa (Nandya)
These centres are run by the Missionary Society of St Thomas
with the assistance of the Sisters of the Sacred Heart Congregation.
The team includes three of our CHWs—Fr Joseph Purayidom (BC6) 9
)
2s
Sr Elsy (BC7) and Sr Franc-ilia (BC7). The work includes living
among the people of the village, survey, dispensary, nursery
school and classes for non-school going children and extension
i
clinicso The project is in the formative years but the team has
a holistic plan and is committed to sharing, simplicity,
ma n ua 1
labour and team work. One of their dispensaries has been designated
a Fever Treatment Depot by the Government under the National f.alaria
Eradication Programme and is acknowledged as the best one in the areal
j
(c)
Kamagere Health Centre (Mysore Diocese)
Sr Aneilla (BCfi) who works at this sentre wta® &w&y on U»vir
but we visited the centre and its two outreach sub-centres at
Hannur and Prakashpalayam along with Dr Ravindran, a St Sohn’s
Doctor who works in the main hospital.
In addition to the MCH
programme based on the CRS plan, the community health team also does
home visiting, clinics for leprosy and TB patients and runs a
savings scheme for local people.
(d)
Kalathipura Mission (Chickmagalur Diocese)
This little mission station and dispensary nestled amidst
coffee and cardamom plantations is run by Franciscan brothers.Br lilency (BC8) came here after his course in December 1981, to
join a senior Brother who is well known through his dispensary
for miles around. The Leam/^oes survey work,
home visiting,
catechism and night classes for non-school going children and
adults. After getting quite a comprehensive picture of the life
and problems of plantation workers through home visiting,
Br Money is gradually beginning to work’among anr ’with them rather
than only’for them. He also has good contacts with the local
government PHC«
(e) Tamil Nadu VHA Meeting (Madras)
On 19th Februray, we both attended this meeting on the theme
In addition to meeting many members
keenly interested in Community Health Work wo got the opportunity
’Health through. People’0
to have a short group discussion with three of .our Chills
(BC3) working with a team involved with MCH programme,
non-formal education and dispensary in Devikapuram (North Arcot),
Sr ZJustina
Br Xavier Amal (BC3), now a warden of a boy’s hostel in Trichy>
3
and Sr Constance (BC2) working in Vikravandi (South Arnot) with
the MCH programme of Pondicherry Diocesan Society.
(f) Jagadhri (Haryana)
It was quite a change to see the agricultural development
of the Haryana villages when wo visited the project run by
Sr Corccna (BC4) of the Sacred Heart Convent in Oagadhri. The
team of sisters run a balvadi,
dispensary and tailoring centre
in the nearby village. Their primary involvement in the area is
English Medium Convent^ from which they have started this extension
work.
(g)
Kalambi-Vihar (Shilonda, Maharasht ra)
Br Tommy Kuruvilla (BC8) who was completing his regency in this
tribal area of Maharashtra, shared with us the experience of living
out among the people,
home visiting, conducting adult education
classes and health work.
A weekly clinic is run at this centre by
a St John’s doctor—Sr Vilma Nazareth—who is in-charge of the
Mission Hospital at Talasari.
(h) Shanti Sadan (Borsar,
Maharashtra)
After a onc-day Seminar on ’Community Health’
organised by the
Bishop for priests, sisters, teachers and parish workers of the
diocese in Aurangabad,
we visited the mission stations of Borsar,
Vaijapur and Ghogergaon along with Swami Sevanand (BC8) who is
himself the parish priest of Borsar and is involved with a very
holistic health effort of counselling and spiritual healing. We
also visited St Luke’s Hospital in Srirampur but were unable to
meet Sr Tresa Jose (BC1) who is ,a Nursing student.
It was enccuraging to see CHWs * living among tlie ppo£l£± learning
from them and serving them’.
cj
cr
i—
o
Q.
UJ
LxJ
Catholic Hospital Association (refer address Newsletter 2) has drawn
up Diocesan Level Health PlansrTontact the Delhi office for names of
your regional animators and for more information about the programme.
Safai Vidyalaya, Harijan Ashram, Mahatma Gandhi Ashram Marg,
Ahmedabad 380027. Write to them if you have any questions or problems
regarding rural sanitation programmes. They have done pioneering work
in this field and have also produced health education materials. They
also run short practical courses for
With best
wishes and regards,
RAVI AND THELMA NARAYAN
com f-|
io- s
ST JOHN’S MEDICAL COLLEGE, BANGALORE 560034
Directorate of Rural Health Services and
Trainino Programmes
NEWSLETTER 4
JUNE ” 1982
Dear Friends,
With great sorrow we inform you of the passing
away of Major General B Mahadevan, Ex-Director
of Rural Health Services and Training P.rogramm
on 7th June 1982, after a heart attack. ’Papa’
- T’
#
Tl^O
TSO
as he was affectionately called by all of you,
was responsible for the development of the CHW
course and we all remember with great gratitude
the interest and enthusiasm with which he planned
each course and guided each group of participants.
Among the many contributions he made to the college
during the six years that he was associated with it,
as Professor of Community Medicine and Director,
he will be remembered particularly for his commitment
to re-orienting the college to Rural Health Work.
May his soul rest in peacel
”Yes, all men are dust, but some are gold dust”
- John A. Shedd
For those of you, who would like to communicate with
his family, the address is?
MRS C. MAHADEVAN
187 Defence Colony
Indira Nagar, Bangalore 560038
(2)
NEWS FROM THE COLLEGE
The college has finally been granted
(a) Affiliation ?
affiliation for two years by the Karnataka Government.
We thank you for your prayers!
We are continuing
the dialogue to get permission to start post-graduate
courses, which has still not been given.
(b) Dr C M Francis, Dean left the college in May to take
up his new assignment as the Director of Salgaocar
Medical Research Centre in Goa.
(c) Dr G M Mascarenhas, Professor of Cardio Thoracic
Surgery at St John’s Medical College Hospital has
taken over as the new Dean.,
'
(3)
NEWS FROM THE DEPARTMENT
(a) Professor SV Rama Rao will complete his term as
Professor of Community Medicine on 30th June 1982
and will take over as the new Director of Rural
Health Services and Training Programmes from
1 July 1982. So please keep in touch with him
regarding your work.
&
.UH
: 2s
(b) The next Basic Course for Community Health
Workers (CHW BC9) will commence on 30 Aug 82.
The last date for applications is 30.7.82.
(c) The next Refresher Course for Community Health
Workers (CHW RC-4) will commence on 22 Nov 82.
The last date for receipt of applications is t
10 Oct 82.
4, OUR PROJECT PLANS
As planned earlier, we shall be spending the summer
and monsoon months - MAY-3 UL - writing out our experiences
of the CHW courses and analysing all the letters and questionnaires
that you have sent to us since 1979. We also hope .to complete other
writing commitments.
Our extensive travel undertaken in Banuary—April made us
realise that it would be unrealistic to try and cover the.
whole country in a year. Many of our friends and CHUJs are working
-----in interior areas and getting to each of them takes a lot of time
and travelling.
We feel that such a field contact can be undertaken by us
over a longer period of time anc need not be completed by December
1982. Also other faculty could be involved as Well. We also feel
that getting CHWs together at a central place for a one-day meeting
would not only cut down travel time but also give opportunities
for them to meet each other. The TNVHA meeting (NEWSLETTER 3)
was one such opportunity. Places where this seems possible are
the Nilgiris, Mangalore region, Karwar region, Goa and Wynad.
We have decided now to give the Southern States lower priority
since we can continue to keep in touch with them in later years
_______
___ 1 __
from
St__John.
So The next trip will -probably cover the Eastern regicn
since this is a much neglected area. We are awaiting letters before
we finalise details,.
With best wishes and regards,
RAVI & THELMA NARAYAN
”If everyone of us could drink pure clean water, keep.our
surroundings free from flies and dirt, and make the best
use of the food we grow and buy, we could protect ourselves
against diseases and many of our health problems will
disappear. For pure water, good sanitation and adeguate
nutrition are the world’s best medicine”
V
4--
H IO.ro
ST. JCW^ S, MEDICAL COLLEGE, BANGALORE
RURAL HEALTH SCHEME - NE^S LETTER
April - June 1982
Vol:2 No;2.
EDITORIAL:
My Dear Friend/.
This issue of the newsletter, comes at a time of changes,
for the college. First the good news. The Karnataka Government
has granted affiliation to St. John's Medical College for the
years 1981 to 1982 and 1982 to 1983. At last the college
appears to be getting justice and our stand has been vindicated.
One can now hope that recognition for post graduate courses will
not be far behind.
Secondly we have to inform all of you, that Dr.C.M. Francis
is no longer the Dean. The Government Body regretfully accepted
his resignation in April. All of you know "C.M." and it will
not be necessary for me to sing his praises. His interest in
rural medicine and especially in all of you out there in the
villages is also well known-®- We hope he will continue to take
an interest in our affairs. The new Dean, is not new to the
college, and is a person of eminence.
I am sure most of you know
him - Dr. Gerry Mascarenhas. With all his experience in
administration both in Government service and as Medical
Superintendent of S.J.M.C.H. , I am sure he will make an
excellent Dean, For the first time we have a clinician at the
top. You will shortly be getting your copies of the Alumnus
bulletin which tells more of the matter.
Finally on a personal note, this will be the last issue of
the newsletter that I am editing. From the 1st of July I will be
O5*i the staff of St. Martha’s Hospital. Let me assure you that
although I may not have official connections with the college and
with all of yoUj I remain a Johnite always,
always. Anytime I can' be of
don't hesitate.
any help, in any way, please don4t
I will look forward
to meeting any
you when you come to Bangalore.
PREM PAIS
A change from the old guard to the new - taken from the Alumnus
Bulletin*
It is on a Sad note that we bid farewell to Dr. C.M. Francis.
After much procrastination and with great reluctance the Bishops
of India have finally accepted the resignation of Dr. Francis as
Dean of St. John’s Medical College and Hospital.
A Physiologist with specialisation in Neuroendocrinology in
Cambridge, Dr. Francis became Dean of the St* John's Medical
College in July 1974.
ContM_,72.
I
: 2
He was selected to this important post mainly becuase of his
experience and widely acclaimed ability as an academician cum
administrator. Previous to joining St. John's, Dr. Francis had
been Principal of the Trivandrum Medical College and later
Principal of the Kottayan/Calicut Medical College. He was
Executive Director of the Sree Chitra Thirunal Medical Centre
for advanced studies in specialities when he was approached for
Deanship at St. John's. The Kerala Government released him on
But, able that he was,
deputation for a three year period.
Dr. Francis soon became indispensable and had to continue in
St. John*
John's.
His stay here could have been longer but for his
So
decision to call it a day, and being firm in his request, the
Governing body regretfully accepted his resignation.
St. John's owes a lot to Dr. Francis. When one thinks of
his approach to a problem one cannot but comment on his immense
knowledge of the subject, his honesty in dealings, his hard work,
his concern for details. The campus hospital is what it is
today in large measure due to the untiring efforts of Dr.Francis
who also ensured that the hospital would be able to afford a
great deal of free and concessional care to the poor and needy.
With his personal commitment, rural orientation of medical
education became ’the' feature of training at St. John's. The
institution continued to claim laurels in the field of
academics, research, sports. Fruits of his labour are evident
in various spheres and one can truthfully say that his efforts
have not been in vain.
We, alumni, will miss our dear Dr. Francis, He has been
a friend, philosopher and mentor to many of us. Though he leaves
St. John's we do hope that our association with him will continue
for many many years to come.
On this occasion we wish Dr, and Mrs. Francis continued
success and happiness in their every endeavour.
Good Bye Sir and God Blessi
The Chairman and members of the Executive Committee of the
Alumni Association congradulate Dr. Gerard Margin Mascarenhas on
his apoointment as Dean of the St. John’s Medical College and take
this opportunity to wish him a long and effective term in Office.
Dr. Gerry (as be is amiably known) graduated from the Madras
Medical College in 1948 and joined the Hyderabad Medical Services.
With the States reorganisation, he was allotted to the Mysore
Medical Services. Dr. Mascarenhas worked as a Registrar in
Thoracic Surgery, University of Edinburgh and obtained his
F.R.C.S. in 1955. As an US AID Fellow, he underwent training
in open heart surgery at the University of Kentucky
and in
1968 he became a Fellow of the American College of Surgeons.
Dr. G.M. Mascarenhas is well known in Government Service
for his pioneering work in Thoracic Surgery. He was responsible
for setting up the Department of Cardio-Thoracic Surgery in
Karnataka State in January 1968. Closely associated with SDS
Sanatorium for T.B. and chest diseases since 1957, he was the
medical Superintendent of that institution till 1976.
Cont’d. . . ./3.
I
: 3 :
In July 1976 Dr. Gerry retired voluntarily from the Karnataka
Government Service after 26 years of service.
St. John's Medical College Hospital, then a newly opened
and
budding hospital, was fortunate to have the services d>f
Dr. Gerry. He joined the institution in December 1976 as
Professor and Head of the Depattment of Thoracic Surgery.
Because of-him, the unit at St. John’s has become a leading
referral centre for Heart Surgery and Thoracic Surgery, So
much confidence did the Management repose in Dr. Gerry that in
January 1977 he was appointed the Medical Superientendent of
the campus hospital.
As alumni, we extend our warm welcome to our new President.
We are confident that Dr. Gerry will take our Alma Mater many
steps forward in the realisation of her objectives.
Medical Comer:- Recently Dr. A.R.A. Fernandez from & Chickmagalur
has written asking for clarification on a number of medical
questions. We can tackle the first this time. He wishes to know
something obout the interpretation of blood counts in a rural
setting.
Normal value of Hb is 13 - 15 gms. A low haemoglobin
Anaemia
(i.e. anaemia) can be due to excessive destruction of blood or
Tridkfc
reduced formation. The next step in the investigation is to
tt peripheral smear examination and a total and differential W.B.C.
count.
a) In excessive destruction (haemolytic anaemia) peripheral
smear will show RBC of abnormal shapes such as spherocytes
(RBCs which are smaller than usual and lack the central
pallor) or fragmented pieces. There is usually a
leucocytosis. Urine will show urobilinogen in excess.
Further work up requires tests like reticulocyte count,
fragility test and haemoglobin electrophoresis which are
usually not available in small hospitals.
b) Reduced production could be due to
i) Defficiency disorders - Iron deficiency. Peripheral
picture shows the well known microcytic hypochromic picture.
WBC count is usually normal. Peripheral signs of iron
dificiency are usually present. A cause must be looked for
- B12 and Folate deficiency produce' a macrocytic
anaemia with large oval RBC. WDCT count is on the low
side and the polymorphs show a ’’hyper segmentation" i.e.
the number of lobes of the nucleus are five or six instead
deficiency can be caused by
of the usual 3 or 4. B
pernicious anaemia. Folate deficiency is caused by
malabsorbtion and malnutrition.
- Dimorphic anaemia - seen in states of poor
nutrition when there is deficiency of both folate arid iron.
There is a mixed picture of large cells with a hypochromic
apnearance.
Cont1 d, . o/4<»
I
I
: 4 :
ii) Reduced production due to infiltration of the bone marrow.
- Leukaemias can be diagnosed from the WBC count and
peripheral smear.
- infiltration by secondary deposits of cancers or
lymphomas in the marrow. Peripheral picture is one
of general reduction of cells like an aplastic
marrow. A bone marrow aspiration, if possible will
show the cancer cells.
iii) Aplastic Anaemia : There is reduction in all the elements
of the marrow. Thus besides anaemia, the WBC especially
polymorphs are markedly reduced and the platelets are also
On a peripheral smear there should be 8 - 10
reduced.
e The number of
platelets per oil immersion field.*
platelets per oil field X 10,000 gives the approximate
platelet count. Aplastic anaemia may follow infections
especially viral infections, drugs(chloramphenical,
phenyl butazone, anti-cancer drugs) irradiation or may
be idiopathic.
W.B.Co Count in infection:- If a patient has an infection
whose aetiology is not clear, a WBC count is often of great
use. Combine it with a differential count and study the
morphology of the WBC.
a)
Viral infections:- Generally §ive a low or normal WBC count
with relatl- • lymphocytosis. An excepticmis infectious
mononucleosis where the WBC count is elevated upto 50,000
to 50,000 oer cubic mm, most of the cells being lymphocytes
of an abnormal type - large cells with large folded nucleiThe picture may resemble a lymphoblastic leukemia.
b)
Bacterial infections - Most acute bacterial infections give
rise to a polymorphonuclear leucocytosis. The more acute
the infection the higher the count. The WBC are young they have few lobes and band forms are seen. These are
young cells where the nucleus has not yet divided into
lobes. Very severe, overwhelming infection, when the
patient is in shock, may be associated with a suppressed
WBC count but the polymorphs will show increased band forms
and their granules will be coarse and prominent - toxic
granulation.
Qiid
Sub acute infection with gram negative bacilli especially
especially typhoid fever have a suppressant effect on the
marrow and may be associated with a decreased or normal
WBC count.
PREM PAIS
Treatment of Diarrhoea:
Diarrhoea is defined as frequent passage of unformed stoods.
It is one of the most common diseases and certainly the commonestalimentary’ disorders in our Country. The underlying cause may
be very simple and benign or a serious disorder. Most episodes of
acute diarhoea are infective in nature, are self limiting and
easy to manage.
: 5 s
Occassionally however, etiological diagnosis may not be easy.
Recent researches have facilitated clearer understanding
of the pathophysiology. It has been shown that approximately
7-9 litres of fluid are poured as secretions into the alimentary
system everyday; 100-200 ml of this is excreted, the reminder being
reabsorbed. Normal stools result from a .balance between the
process of secretion and reabsorption.
Excessive secretion or d
diminished reabsorption may result in diarrhobis.
Etiology - Bacterial infection account for the majority of
cases. Shigella and Escherichiae are common organisms which infect
the gut. They invade the epithelial cells of the ileum and colon
and cause out pouring of large volume of fluid into the bowel. The
Vibrio Cholerae produces an enterotoxin which binds to the
epithelial cells. Stimulate adenylcyclase and cyclic AMP activity
leading to secretion of protein free isotonic fluid into the gut.
Protozoa and flagellates or other helminths may be responsible for
an episode of acute diarrhoea.
Enteroviruses are frequently cited as cause of epidemic or
sporadic gastroenteritis and diarrhoea.,
Several studies have
revealed that enteroviral infection is common
>
in children but
less as compared to E. Coli infection. (Cecil 1979).
From treatment point of view, it is advisable to find out
the underlying cause and treat it. Spicy fatty food should not
be allowed.
Oral rehydration is the most effective therapy,
. .. Oral
rehydration agents containing Sodium, Pottassium, Bicarbonates,
and sugar have been increasingly used with good results, They are
of particular value in infants and young children. Their use may
be life saving in rural setting. The fluid can be prepared at home
by disolving 3-r5 grams of sodium Bicarbonate, 1.5 grams of
Potassium chlodide, 2.5 grams of socium Bicarbonate and 20 grams
^1 condition of the patient,
of glucose in a litre of water.* General
his skin and tongue give evidence indicatingf the State of
hydration. Fluids should be given to ensure a urinary out-put
of 1200 - 1500
—
ml. in 24 hours.
Coming to the role of antibiotics,, they may be required
only in selected cases. 7Ampicillin
‘ ‘‘ 500
-- mgms orally QDS x 7 days
for adults (100 img per kg in 4 divided dues in children),
Cotrimexazole tablets
------ 2 BDS for 7 days tetracycline ^00 mg four
times a day for seven days or Sulfaguanidine 250 mg CDS for 7 days
can be used. Tetracycline should be avoided in children.
COMMERCIAL. PREPRATIO^S :Let us come to the role of commonly available antidiarrhoeal
mixtures which are frequently used in general practice.
chart gives the name of the preparation, contents
and their cost.
Conf do o./6.
: 6 :
Antidiarrheal Preparations
NAME
CONTENT
COSTIM Rs.
1. Kaltin c Neomycin
(Abbott)
Each 30 ml contains
Kaolin 6 gmz Pectin-130mgR)
Neomycin -300 mg.
Sodium lactate-500 mg,
Tinct. Belladona -0.3 ml.
Pot Chloride -330 mg.
Sodium chloride -470 mg.
60 ml cost
5-20
2. Pekolin
(Cadila)
Each 15 ml contains 0.225
grams of Pectin Kaolin-3 gms.
150 ml. cost
11-68.
3. Kaopectin c
Vellafonaa
(Pharma Lab)
Each 5 ml contains
Kaolin 1.25 gm.Pectin 0.0625 gm, Belladona 0.125 ml.
450 ml. cost
11.00
4. Pectocin
(Pharma Lab)
Each 30 ml contains
Kaolin - 6 gm. Pot Chloride
0.32 gm. Pectin -0.13 gm
Neomycin -0.3gm, Sodium
acetate-0.1 gm.
60 ml cost
6.00
5. Bismopep
(Anakem)
Each 5 ml contains.Sodium
Bismuth tartarate -100 mg
Pepsin-2.5 mg, Nux Vomica
0.05 ml. Glycerin 0.05 ml
Alcohol -13%
6. Eukopect
(Eupharma)
Each 5 ml. contains
1 gm - Kaolin
0.05 gm-Pectin
1OO ml cost
4.00
7. Pectilin SG
(Wockhardt)
Each 30 ml contains
Sulfa guanidine -1.380gm
Pectin -150 mg Homatropine
Kaolin -6 gm.
450 ml cost
14-76
8. Streptomagma
(John wyeth)
Each 15 ml contains
streptomagma -0.15 gm
Kaolin -1.5 gm
Pectin - 0.135 gm
Aluminium gel -70mg
90 ml cost
6-10
110 ml cost
5 fe = 0
If one sees the contents of the different proprietory
It is evident that most of them are shot
preperations carefully,
them contain Kaolin alone or in
of
gun preparations. Most
Tte
role of Kaolin in diarrhea is
combination with pectin.
Conf do ##7.
: 7 :
highly controversial. Some workers have found it to be of some help
whereas others observed, no significant benefit from its administration.
In the symptomatic treatment of diarrhea, it has been recommended by
Martindale (1972) to be given in the dose of 15-75 gram per day.
The 2 gram dose generally used in the antidiarrheal mixture has little
effect. Adecuately controlled clinical studies that demonstrate the
efficacy of these popular preparations are lacking. They may have
minimal effective antidiarrheal action. The general opinion is that
even if it does not reduce the number of stools their consistency
changes for the better. Some of the proprietory preparations.
contain Neomycin. Neomycin can act as an intestinal antiseptic in the
dose of 2 - 8 gm per day. It is poorly absorbed from GIT and helps
in suppression of bacterial growth in intestinal tract. In infantile
diarrhea it has to be given in the dose of 3O-5Omg/kg body weight.
When given by mouth, Neomycin sometines can produce laxation and may
interfere with intestinal absorption of food. Prolonged oral therapy
may result in overgrowth of non-susceotible organisonal such as
Candida in intestines. To avoid this it has been advocated that
Neomycin should not be given for more than 3 days.
Reports regarding the use of codeine, Bismuth Salts and opiates
Generally they should be avoided in infective
are conflicting.
diarrhea. Their use, it is feared, may prolong damaging.effect on the
bowel mucosa and absorption of toxing preparations containing Atropine
are definitely Contra indicated in cases showing Pyrexia a sign of
toxemia.
'The cost of treatment with most of the ineffective proprietory
antidiarrheal mixtures is exorbitant and certainly so in.a country like
ours* So while prescribing the above mixtures one should think twice
regarding their efficacy, their usefulness and their cost.
R E F E R S N C E S
£)= The Pharmacological basis of therapeutics (1980)
Goodman & Gilman.,
2) Journal of applied Medicine (April 1981)
Vol -7, No. 4.
3) Drug - May (1980)
4) Cecil's Text Book of Medicine 15th Edition (1979)
5) Martindale's Extra Pharmacopoeia.
(1975).
DR. P.S. PATKI, Pune.
M.D.(Pharmacology ).
(MFC Annual Meet-1982)
: 8
Lomotil in young children:
Is it useful?
or
It is dangerous?
The latest WHO pronouncement on the treatment of diarrhea says
"Lomotil is one of nine treatments not recommended" (1)
Lomotil is being used widely bv majority of physicians,,
Let us analyse scientifically its effectiveness & dangers.
Ife it useful?
a. Against dehydration:
Ths cause of death in diarrhea is dehydration.
Lomotil may appear to help by reducing the frequency of motions
but it does not reduce the loss of fluid into the intestinal
lumen. This internal loss of fluid is difficult to assess
clinically, Therefore, Lomotil is in fact dangerous, as it can
mask dehydration. (2)
bo Against infections :
Acute diarrhea in children is usually infective t but
antibiotics and antidiarrheal drugs rarely help O'.
Lomotil prevents the children from getting rid of the
infective agent and may prolong the period of infection. ((4)
Febrile volunteers receiving lomotil alone experienced over
a day more fever than those in other treatment groups suggesting
that drugs that retard gut motility facilitate intestinal
infection (5) .
Id Lomotil dangerous?
Lomotil ingestion is a cause of serious poisoning in young
children, especially those aged under five. (6)
Lomotil poisoning in children can include atropinism,
respiratory depression,#:com^.
even with therapeutic dosage.
There is no correlation between the severity of symptoms and the
dose ingested.
Manufacturer's warning:
In the U.S#, Lomotil is contraindicated for children under
two years.
This warning by the manufacturer is not because there has
been inadequate pediatric testing of the drug but rather because
severe life threatening reactions (which are not rare) occurs in
this age group (7) P.R., Sureka, Bombay-64.
(MFC Annual Meet-1982)
Conf d. . ./9.
: 9 :
References:
1. World Health Organisation - Treatment and prevention of
dehydration in diarrheal diseases (Geneva :WHO-1976)
2. Lomotil for diarrhea in children The Medical letters, 25, 104, 1975.
3. Diarrhea in Children - Drugs and Ther Bulletin
(d’an 6, 1978) p. 2.
4, Pittman F.E.,
"Adverse effects of lomotil, Gastroenterology,
67, 4O8-9> 1974.
5. Dupont HoLo & Hormich R.B. - Adverse effect of Lomotil therapy
in Shigellosis,
6O Penfold Do
Overdose from Lomotil,
(Nov. 26, 1977, pp 1401 -02.
& Volan G.No,
British Med,J.
7
A. MA. Dec. 24 -31, 1973, 1925 -8.
Wasserman GOSO "Lomotil Ingestions H Am. Fam.
Physicians Oct 1976, pp 27 - 8.
(Based on the leaflet on lomotil - published by Social Audit
Limited, 9 Poland street. London WIV 3 DG.)
Correspondence s- In the last newsletter we published a long article
by Dr. G.D. Ravindran. Here are some replies. First comments by
Dr. A.R.A. Fernandez from Chickmagalur.
- Dr. G.D. Ravindran’s view that only success stories are
published in this newsletter are totally incorrect.
- I agree with Dr. G.D. Ravindran J.n doubting whether the
S.JoM.C. M.B.B.S. course has any relevance to rural health care.
- All’I could say is rural service is not too easy for anybody.
There are various reasons for them. This could be discussed at a
later date.
Dr. Dara Amar was asked for his comments as the Community
Medicine Department plays a large role in rural orientation, He
has given a detailed reply
Orientation of Medical Graduates of St. John* s, to serve in rural
areas - An Introspective View, by Dr. Dara S. Amar.
I write this with special reference to the letter written by
It was a nice experience to read this letter
Dr. G.D. Ravindran.
and know that some of us are truly perturbed about the situation
of Rural Orientation among our graduates. His letter shows a lot
of insight into the real problem and I appreciate him for having
brought it to light. However, there are a few points which I would
like to clarify and also to bring upto date the fresh efforts made
in this orientation endeavour.
Conf d. ./10.
I 1© I
At the outset I my confidently state that orienting a medieal
graduate, or anybody for that matter, to accept a changed manner of
thinking is not as simple as is often made out to be nor is it the
sole responsibility of any individual, department or for that matter the
the institution itself. Orienting a medical graduate to serve in the
rural areas must be viewed in the context of how this graduate's
mind and thinking as been influended by his social and family
background, his parental aspirations for his future, the economic
returns and the most important of all is thn peer group pressure
brought on the fresh medical graduate.
A lot of water has flowed under the bridge since Ravindran’s postinc
posting at our institution and I shall attempt to bring untodate some of
of our new programmes. The credit for the new changes brought in,
especially by the Department of Community Medicine in their field
programmes, goes largely to the recommendations made by innumerable
interns like Dr, Ravindran. But it has taken time for implements
ation due to several administrative, financial and other
constraints.
Nevertheless each of their recommendations are and will be
implemented over the course of time.
One of the major recommendations
which repeatedly was voiced by several earlier interns was the fact
that when they were posted to a rural centre where a Medical Officer
was stationed, -they had very little to gain in terms of independent
patient management and confidence in handling cases. ^t was with
this view and partly due to the successful grant, of finances from
the State Bank of India that we were able to launch into a new
scheme o£ rural centres deep in the interiors of Dammasandra Block.
Four such centres are functioning and two more are envisaged. The
uniqueness of these four Sub-centres is that the interns themselves
(two boys) have to manage the entire centre which includes not only
patient-care but financial management and organisation etc., under
the realistic constraints of administration and monitary factors.
Thus the emphasis is on the interns being able to manage a General
Practitioners Clinic in the rural area with limited fundspi limited
medicine, limited diagnostic facilities and the usual constraint of
rural life. Thus • the emphasis has broadened out from mere preventive
and promotive methods to curative services as well, as we have
realised that the entry to any health care system is through
curative services. The old system of compulsory projects, programme
components etc., have been done away with inorder to give the interns
a lot more time to devote their skills as a General Practitioner
in a rural area. This is not to say that the other programmes of
training in preventive and promotive care have come to a halt
but under the new circumstances, curative services have been
given greeter importance than in the past. One could say that at the
the end of the three months posting as independent doctors in
the rural centres, the graduates will now be armed with
sufficient experience to manage a general practitioners clincc even
if it is in a rural village. So far this newer system of independent
posting of intern has been extended to the
’ . male interns only.
However, we propose to very soon broaden it out to include lady
interns as well, the only constraint being one of security. The
old centres like Mallur are now not being used for internship
posting unless there is an excessive number of interns coming in
to the department.
But this problem seldom arises as the interns
postings have been streamlined for the entire year and an advance
planning can now be undertaken.
Incidentally Dr. Ravindran's^
suggestion for short term 15 days postings in small specialities
has now become a reality. I do agree that even under this new
system of independent interns posting there are a number of lacunae.
: 11 :
But any change is bound to throw up newer- challenges and it is
only a matter of time before these are streamlined.”
Apart from the above, f
'
at orientation are being
attempts
made also at the undergraduate level. Dr. Ravi Narayan, in an
. earlier newsletter has already written about the rural
orientation programme for the 1st MBBS students and therefore
I shall not go into its details. However, again certain points
need clarification .
^n the first instance, the Rural Orientation
Camp is not merely meant to increase the knowledge in terms
of health care or medical problems of a village. The main
intention is to impart an EXPERIENCE to the students, of village
life. To this end the camp emphasizes that the students find
out for themselves about other social factors like transport,
communications, trade, religion, politics etc., of the village.
The idea being that without a knowledge of these factors of
rural life, ther? is no point in giving a tubular vision of only
health, to the students.
In fact the r-isponse of the last three
camps has been one of overwhelming enthusiasm on the part of the
students. During these camps it is the senior faculty of the
department who reside with the students and this I believe is
very important. This camp is meant to be repeated in the third
and final years.
I hasten to add at this juncture, that having
learnt a lot of lessons from the old (and now given up) Mallur
posting of interns, we have realised what it means to overstay
our training programmes in one village only. Therefore, the
Rural Orientation Programmes are conducted in different sets of .
villages each year, thus not exhausting the patience of the
villagers either. As these camps' are conducted mostly in the
drainage areas (in terms of patients) of the College Hospital,
these students are in a much better position to understand the
village milleau of the patients coming to the hospital. This
indeed is a great step forward considering the fact that these student
graduates will now think in practical terms before advising or
recommending any followup measures to their patients in the
hospital.
The third major facet of rural orientation
attempts by
the department is directed towards the staff of other departments.
Even in this sphere I can confidently say that a lot of progress has
been made considering the fact that originally it was believed
that clinical staff would never go to rural areas. There could
be no greater falsehood that saying the clinical people are
not interested in going to the rural areas. What is necessary
is to create an opportunity for them to go to the village and
this is being done by the department in terms of organising
monthly Multi-disciplinary Camps in each of these village
centres (using theomnipresent white elephant, officially
termed the Mobile Clinic). The interns posted at the
subcentres carry out an intensive publicity campaigns. This
has resulted in an attendance of over 300 to 400 patients
at each camp. Being a multi-disciplinary camp the
disciplines involved are at present the socalled minor
specialities like dental, ENT, Ophthalmology, Skin and one
major department, the Surgery Department. I assure
Dr. Ravindran that these Multi-disciplinary Camps (based
on a regular programme schedule and not "ipsofacto") are
no more the old types of "picnic" trips to the village and this
Conf d. . e/12.
I
: 12 ?
staff.
could be corroborated by the actual clinical
Infact at the last such camp the patient turnover crossed 500.
This amply disproves the fact that these camps are mere picnics
jaunts’
. Most importantly, the followup of the patients at these
camps are carried out by the residential interns and the
departmental social worker an^ behavioural scientist.
I do not §ay that following all the above new changes at
orientation, I expect the entire lot of graduates of St. John’s
to rush to the villages and it would indeed be absurd to dream of
such a proposition at this juncture, at least. However, we
must remember that the interns of St. John's Medical College are
the only interns who continue to reside in the new sub-centres
supervision, unlike the scenes witnessed at other
without any
Medical Colleges.
^t is unfair to pat our own backs for this
comparitive analogy and I do understand that we must try for
the absolute ideal. However it is at least a step in the right
direction.
Indidentally other medical college staff and Govt,
officials have visited the institution, after having heard of the
newer projects to orient our students and their verdict is that
we are ahead of others on this path, but I do agree with
Dr. Ravindran that we have a very long way to go*. It is only a
^natter of time before the changes become evident.
I assure Dr. Ravindran that we shall continue to try and
improve methods of orienting the graduates to rural health and I
hope that he shall continue to f avour us with- his recommendations
and suggestions which are most welcome.
Cor<i H 10• II
Directorate of Rural Health Services
and Training Programmes
St John’s Medical College,
HC/MTH CJ2LL
47/1,(First Hoor)Sfc. Marks Roac
BANGALOBE-560 001
Bangalore
dt Nov 1901
DRHSTP-ACC-81
Dear
Seasons Greetings for Chirstmas and the New Year from all of us
in the Department of Community Medicine at St John’si
1982 is going to be a special year for us since a long standing
plan to meet all of you in the field has finally materialised.
Thelma and
I are on special leave for a year starting December 1981 and during this
year we plan to visit as many of you as possible in your own areas of work
to re-establish contact, share experiences, reflect together and grow
in our understanding of our people and our work.
We have already been in
touch with many of you and we shall be writing to others as the weeks go by.
We thank all those who have so promptly and enthusiastically received this
news and welcomed us to their villages in 1982.
We hope to -hear from many
others amongst you soon.
In order to get some common information frrom all of you in the
field we have drawn up a simple questionnaire taking ideas from many of
Please fill these up and add any other comments,
your own letters.
information, suggestions you would like to send us.
Those of you, who have
already sent us some details of your work recently fill in only those sections
which you did not cover in your personal letters.
We would like very much
to hear from each of the 150 Community Health Workers we have trained.
Even a blank
uestionnaire with only your latest address and information
on how to meet you next year would be most welcome.
Meeting you and seeing your programme will be a good experience
for us but in case you feel there are any other ways in which our visit
could be mutually beneficial please suggest this in Section C (b).
In preparation for this visit many other materials are being
organized which we hope to send you soon - a list of Community Health
Workers addresses, news bulletins, list of new handouts and educational
materials and so on.
So please keep in touch.
Hoping to hear from you soon and also meeting you next year.
Ijith best wishes and regards,
To
PS: Please post this to Drs.
Yours sincerely,
Ravi & Thelma Narayan, D-10 Staff Quarters,
Directorate of Rural Health Services &
Training Programmes
FDLEOUJ-UP EVALUATION OF COmUNITY HEALTH
WORKERS TRAINED IN ST SOHN'S Fl ED ICA L. COLLEGE
PROFORMA
Instructions :
Section A and C to be filled in by all Community Health Workers
Section 0 to be filled in by those who’are doing health work
at present.
(please keep us informed regarding change of .Addressl
SECTION - fA
GENERAL IN FORMAT I 0 N
a)
Name :
b) /Age:
c)
CHJ Course No.:
d)
Name of Congregation:
e) Biocese:
f)
Permanent /Address
(Nother House/superior) :
g) Present /Address
(For future correspondence)
:
h) What have you been doing after the course ?
(if you have changed from place to place give us some details of your work
in each place).
i) Give us a short description of the present team you are working with and
what each member does (not only health activities)
J) Have you attended any course/meetings/workshops since you completed the
Course ?
s 2 i
k) Are you in touch with any of the other Community Health ijorkers? If
SO
give us their recent address.
1) Give in a few sentences a description of the poeple you are. working^
with (rural, urban, tribal, non-tribal, main occupation, other characteristics
etc).
How many villages? Total population, what distances apart ?
i':
h:
SECTION B
a)
Give a short description of the health activities you are involved in.
b)
How many hours are allotted for this daily/weekly ?
c) Are you functioning independently or with a team of workers?
how is the health work shared amongst you ?
If so,
d) Do you get any assistance from the local Primary Health Centre?
If so, specify ?
i) Do you get any assistance from a Taluk/Mission Hospital?
e
If so, specify?
f) Do you work with any special groups in the village (young farmers.
youth, mothers, harijans etc.)?
. ..3
S3;
g)
Do you parti ci pat e in training of local people ? Grihinis,
worker, mothers etc.
village level
h) Do you have any of the following programmes?
Food for work, Health Insurance, CRS- MCH Programme, any others
i) (Are you part of any Diocesan Society or Health Team ?
If so, specify.
SECTION 0 (Regarding 1982 project)
a)
Give us detailed information on how to L^~,i
reach your village/project/centre?
(By bus and train, also from station and bus stop)
b) $re there any forms of support which
late:
a visiting team can give you next year ?
Signatute:
Please use the remaining blank space to giveany further details for which there
was not adequate space in the questionnaire.
H I 0*4
Oo
4 O'
'’7^2X9
ok
-
SUWffiY
VII,i
health worker training
C^iomn-iLinity
1977.
The
community health worker was to
community, who
fc tthese
y-^ese wr©
fell
•’jere
would undergo a short
the community'
spread over 3 mon this.
wor kers arid not government servants.
extension of health
October 3"id
te a person of the
training course for a period of 200 hours
to promote the
India on
r.,.
grTKdating
•? i he F?valu*t
and serve them.
—.
They
would live with
be voluntary
began in
They were to
The concept was therefore
services to rural
areas by involving
or
increasing community participation.
St. John's Medical College in its effort to promote rural service's
to under ' served areas, following
eispecial ly
ccxnmittee report,
the guidelines of the
its cjwn experience
projects, began
trainees
the? biddings
CECI conmission arid co
in ‘the use of village health wc^rkesrs
a cc<r«n.inity heal th workers
were mostly
"religious”
of the Srivastava
sisters
the basis of
in some of its micro
basic course in April
wino
ca/ne? from
all
1978.
The
over
India,
has teen going
on for
especially rural areas.
The community health
more than 13 years now.
was
conducted, no
decade after
Fhcugh
workers basic course
informal and formal evaluation of each course
forma1 eva1uation
the institution
of
the training
of this
course.
of
studies
was conducted
eva1uation was
even a
thus felt
necessary.
A
provided
literature
guidelines
insuff iclent.
evaluation.
on
review
formulating
the
on
comrnunity
evaluation
but
health
these
workers
were
felt
It was tferefore decided to adopt an innovative approach to the
As a first step in evaluation it was decided to evaluate only "tte?
of
relevance"
the training prog ranine
1981 - 1990.
ctossf^was
study.
TTie . objective
methodology,of training of
community.
to
hea 1 if i
From
of
>.s.
of the
study
to
.identify . areas that
tfe community
required
training,
or* vthe
. ■ ■?-tn>•?’• j :■? 1 "•
a15 r n
was to
study the
s t reng t hien ing
tfe content and
determine
the community health worker,.
worker and
training emd
fboetech, apipracx: h
to study the work of
local
an anal ysis of the above men timed
recom/nendations for
of
- A multi
9?* (
tie corm unity
the local health
It was decided to evaluate a decade of
needs of the ccninunity.
decade
relevance to
- the
arid
health needs
of
the
components the study was
to
offer
appropriate
As a background to the study,a general profile
tea1th workers provid.ing
not only
genera1
characteristic
such as age and sex but also otter information regarding their work status and
the. feed back cn training, was also elicited.
I he community health workers trained during the decade were
traced through reply paid post
health workers traced
of states or
cards sent to their superiors.
;.X<. -
first
The conirunity
:
through post card replyies were stratified on the tests
regions ,within the country
and arranged in serial
order of the
year in which they had attended the course end the ni-unter on tbie nominal role.
All .of thiese were sent, a
genera1 prof i1e.
107;
constraints
sampling.
structured closed postal questienpaire to elicit the
A response rate of 67.94X was received.
of
tbie sampling
f rame
of tine and finance and
v^as
considered feasib1e
given
the
this was chosen by systematic stratified
I tie work of tte ccwnunity health workers and the local
health need
of thic?' comcfiuni ty
using
was studied
served by >’ the community i health worker
interview schedule and personal •observations. '
Trainers
sampling5
of community
workers were
health
cbiosen by
purposive
a trained, being defined as.on^ wtio tiave teen involved in training of
coiTMTM-inity health workers for 3 or more? years and
trainers
23
decade.
prescnally in ter viewed
were thus > identified
on the
opinion
ti «e
arid of.
on. specific
years fallincj within the
wticzm
21 ■ (91.307.)
aspects on
specified fields of interest to determine whethen the training
were
training
in
was knowledge,
attitude or skill oriented.
Training was also studied for its course
contents end methodology
<•
f rom a records review of files in the department.
Thedata collected
presented
using ■ ■ descriptive
by ’the
above
statistics
in
method was
the
form
is
of
percentages
or
'!
proportions in four chapters namely,
i) <General profile of the CHW
and
compiled
1
ii)
The training of tte O-W
iii)
The work of the Cl 14
iv)
The local health need of tf)e community.
■ Analysis was then made by simple comparison
>
of the thra? angles of
l eal th need of the community and
tlie study namely the training, work and local
this was viewed in the background of the general profile.
Areas in training tJiat required strengthening were thus identified
in 10 specified fields of interest and one additional aspect narnely
i)
Q:xrfl*_inicable disease control
ii)
Maternal and child health*
iii)
htrtrition
iv)
ImffiLinization
v)
First Aid and Care in Minor ai Intents
vi) ■
Enyi ronmenta1 sanitation
vii)
Health Education
viii)
Comnunity development activity
ix)
Health plctnning and managewient
x)
Other systems of medicine
*
(..ton tinuing education
In ’conclusion certain
programme
as
whole
reconrnendations are
as
it
st reng this and
existed
for a
ttien proposed for ttie
specifically through tte modified schedule
weaknesses of
decade
are
the training
highlighted.
training programme as a
The
V'frtole and
for ccDmnonity health workers basic
course.
VII.2, CONCLUSIONS
t)
In conclusionj, the
worker
training
at
St.
evaluation of the
John's
Medical
strengtbis and weaknesses of the programme.
decade of ccxnmunity
Co 11ege
brings
to
health
light certain
These
-^aknps^s4,(
. the.. , program are categorized
under the following leadings:
i. Content of Training.
.. I
•4
r 1., e.’D
Kc
‘
ii. Methodglogy pf, Jrainjpg. ■;
r) >
Ap. Training, Prggrain,
no
1 •. f ’ >
> Training. t ( ,.,
’■ 1 e!gr-» iY,’
,-y-
fiPHTWh.^in,. Train,ing.
IJ
•• I ...
•,..1 I
.-.I
' .HWn?
vii. Trainers characteristics., ii •
•;:h 1
1
i '.;i. •
viii. Selection criteria.
ix. Student characteristics.
X
■ T!
h ^i'-'atW‘'.Wfllng.,.,
'iH
■
! j i r ■■ > ' •: 'I
.
:I
i
. ■ i
I-':
xi. Follow-up of Trainees.
.. JTb.. ^tftnuing...KlMRatipn.,,,,,,
L. '
hl
’ J
•h-> 1
i•Ij .i 1 1 1
’ i. f hh
rrrv-q / > ■» -1
'• .1 C :-4 L ’■
:• h j
I. I l<’
J .111) • 1
.. I I !• i
i J
11 k ? i r
, -•.bl.)
: t : -.' ■’ I
I1!)'
h M 1 • 1 r th 1 fe 1
i, h I
•■•I . .: ■ -h •. | •
I!?
■ ’!«: .•..
11
■’
hI• >
11
i. • •
1•
!: I ’
ib
1
» I )
Ij
•
I
■
'
■ :* i
hhr 4
O’ L» • ! ? ’
• I
-
VI1.2.1.STRENGTHS CF TTE FROGFWTE
< i
VI 1.2.1.1. Con tent of Training.
A k:d.c!e ^coverage of topics and a firm foundation
on basic concepts
which contributes to the trainees developing1 a conceptual approach
tJn an
average about 12.527. of the total training time is’ spent on
basic concepts in Health and Developmmt.The total duration of the
rentained
the same as that recommended by
course fias
the Government of India, though thee
total numter of teaching Txxtrs is much more/
VII.2.1.ii. Methodology of Training.
ITiere
are
a wide
variety of methods
used
in
training- These
include s
classroom
based
lectures.
group ' discussions,
demonstrations
practicals, learning by doing, simulation games-, role plays, field
,
visits and
studies, project work; and visits to various institutions.
VII.2.1.iii. Flexibility in Training Program.
the course schedule bias not been rigid, but, flexible
arid c tianges
have been made from time to time even during the course as is obvious from the
ink correction cn tfe printed schedules cn different dates.
VII.2.1.iv. Field—based Training.
there is a proportion of training
which is totally field based in
all courses and this usually about 35.357. of the total duration of tlie course.
VII.2.1.V. Approach in Training.
’T’l’iere is
trainers.
.t^.^ted.apprc)ach in
Training has included visits to
especially for
training
and
type?
of
various institutions and projects
development aspects, rellabilitaticn care of speczial groups and
to intensify training in these specific "health” issues.
VII.2.1.vi. training Resources.
I raining resource
in tte
form
material , library facility, class room
o-f-materifSl.resource -
reading
facility, availability of audio visual
aids, facilities for residence, food ar id transport have all been provided
seem
adequate from
feeed back
reports.
Wl’rerever poin ted
cut
and
by trainees,
necessary changes have teen irmediately imple<ientec:l.
VII.2.1.vii. Trainers characteristics.
Irdiners c fraracteristies
training.
All
cand number have also
the faculty directly involved in the
There
medical faculty for most
is
a 2
: 1
emtributed to tfe
train ing are teact'jers of
proportion
years of the training.
of medical:
The staff student ratio
Non
in
any given course during the decade lias not exceeded 1 : 3.
VII.2.1.viii. Selection criteria.
Basic
"Selection
criteria"
I"iave teen
laid
down
and
this licis
resulted in more or" less hanoqencus group of students.
VII.2.1.ix. Student characteristics.
Students are
mainly '^reliciious" and this has
tfe homogeneity among students.
also contributed to
VII.2.1.x. Evaluation of Training.
Formal_^^atieDsi
.
• , i' i I •’
t ’
iJ
valuations conducted
informal
'
■
cour&e
cind
faculty
with faculty
and
the
and after
dur ing
before,
"i- ;> •
group discussions
through
through project presentations regularly, during tie course,have corrtriLuted to
I .
.
! ■.
'
•
< . •
.
-•
f h
a continuous evolution of
■
i
. I ! I < ■ 1
i
!
-
.
:
1 ! l-J
• I I »-, •
! 11
„ ■
»
i ■
I
I
J
the course.
j... J i) .•
!
- *•
■i 1
? 1
•
‘in* h i
. ,• I !
I ' I
>!
• i ■ < J
i
if ? >•' !’ |
I I I’
I :
I •
r
f
I••• ;
. = i'
■ U
!• . >
I
'
>■ i J
VI1.2.2. UEAFJMESSES OF 1HE FWORAM
VI1.2.2.i. Content of Training.
I here are
with evolution of
too.. ffianY..topics
and list.
been growing
thie course, whereas the course duration as a whole, or tine
spent cn training has not altered much.
for
of topics fiave
experiential 1earning
This could only result in lesser tine
and practice of skills
and
necessary.
'’!^tent_too
were among ttie niost coninon problem encountered
by trainees during thie training.
>>
VII.2.2.ii. Methodology of Training.
While a variety of
niethods tiave been used in training, class room
basetd lectures is still the most conynonly used and in the ‘recent year has even
exceeded
all other methods combined
together.
This
not only compromi.ses on
skill based learning tut also is not suitable for adult learners (VHA1 1978)„
i ,
VII.2.2.iii. Flexibility in Training Program.
1 he over
learning.
flexibility in course schedule has
’’F'reciuent chianges in time table1 ’
been a constraint in
was the third mc:«st ccjmmon pr oblem
in learning for■the trainees.
VII.2.2.iv. Field—based Training.
I tie? proportion
dependent on the
centre and
of field training in the
availability of dormitory
this has
restalted in
training in certain course’s.
various courses has been
facilities in the
compromising
the duration
primary hea1th
of field
based
VII.2.2.v. Approach in Training.
While tiie
was found useful to
multi faceted approach to training
less tbian 25%; of ti e trainees.
may, be unique!, this
T hi s especia11y inc1uded
visits-to., various physically or mentally handicapped rehabilitation centre's. >
‘ * > 1
' i
I.
•I
VII.2-2.vi. Trainers characteristics.
Most of-(the Trainers were Medical personnel .English was tbie n»edium
of
instruction
trainees was
for al1
courses.The
mc^st common- d ifficu1ty. experienced by
"language". Thie use of medical
jargon and technical terminolcxjy
is probable.
:r
• I ft •
VII.2.2.vii. Selection criteria.
While tfie fact
• ,/ Selection • criteria biave not been strictly applied.
that, an under
inc 1 tiding
qualification may be
nurses 5 have
over looked j,
also joined the
many health professionals!,
commi..ri i ty biea 1 th
this has to be paid attention to.
workers course and
> . H -■ h ■
I
VII .2.2.viii. Follow-up of Trainees.
There is no formed system of follow up of trainees after training.
Oily about
657. o f
trainees could fc)e
addresses that were available.
traced in
the decade
on tlie? basis
of
Apart from tfe? present study tfere is no data
available co what trainees are presently engaged in, in the field of community
health or other wise.; >
VII.2.2.ix. Continuing education-
Continuing
i’1
■
education programme's are strikingly deficient.
about 687. ccmnunity tea 1th wor kers
liad had some form of
Though
cot itinning education
mainly
tiircxigti
ref resher ecu rse.
in fornia 1 processes
(Diagram),
88.73% felt
the
need
for a
Only 4.237. did not feel this need.
VI1.2.2.x. Evaluation of Training.
I i •:
Here is no system hy which impact
the cornrro-jity can be studied.
tfie commt..inity health
the course.
never been
traced
No conditions have
been laid down regarding
worhers continuing in coamunity
health activities after
10.42% of those
decade (1990) are
of the corrnunity health worker
traced in tfie courses
not yet involved
in commui rity
involved in activities before
in the decade liave never been
either before nor after the course,
of tte last year
in the
heal th activities and
tiave
the course either.
7.65% of those
involved in community health activities
(diagrams).
VI11,1,GENERAL RECCFrOOATIONS
Vlll-l-i. Content of Training.
Comiroiity health workers need to he taught
lQr__thg]L„Jn_th^
, ye
ar id are
"Topics
. u- . ,y : ■
not necessary even
conceptual background,
tte human biology dealing
especia11y on
!••*•.,{
may be deleted.
they have no relevance
).
?
may be excluded where
• r:«rk£»r» E-- _
for a
j^jega^ary
Tteis many
mar«y
Thus
with the endocrine system
topics
c<nd so on
...
Tte number of topics n taught” must thus be reduced.
VUI.l.ii. Methodology of Training.
Training must
be strengttiened in the development
use of more participatory methods of learning.
learning by
doing, project
work, simu1ation
field work, group discussions must be
of skill by tie
Thus use of practice sessicxiSj,
role plays,
games,
used irore often.
supervised
Fartici pator y mettads
metbiods such as social or
of situation analysis of a commLnity through use of
ccmniunity mapping and body mapping must te included. (Chambers R.,1990 & Rifkin
S. et al,1988) Participatory methods of
training and use of audio visual aids
were preferred by many cornrriunity tea 1th workers.
Vlll.l.iii. Flexibility in Training ProgramWhile a cer’tain degree of
flexibility in sctedule is
recofTMTcnded
it must be emphasized that frequent changes in time table must not be re-sorted
to.
Vlll.l.iv. Field—based Training.
Wl O recawiended that a proportion of training n*ust te conducted in
tte f ie 1 d»(WTU,
1979: T ec tn ic a 1 Repor t Ser ies,
.
It did not specified tte
propor“tion -
However it wae elicited
from trainees and trainers
and i t tf ius
recornmended that an ideal training programme must be_totanxjield.
the absence of
facilities for field
based training for
based..
In
Field—based vjorkers,
such endeavours should not be•undertaken.
VIII-l.v. Trainers characteristics.
Trainers
social- : scientist,
of coi/ino’iity ■ health workers
social
workers.
!■
is
recowncanded
as trainers too.(WHO
Sa>affiitY...health_..warkgrs be? used
Series9 780)
It
tjave bees i
most1y doc tors,
tfet„_e^Qsiced
1987; I ec: fm i c a 1 Repor t
.
''Language'1 was the most common difficulty experiencec:! in learning,
by ■the community
health workers.lt is
language and avoid the use of complex.
recommended that
scientific,
Trainers use.simple
tec;: hn ic a 1, medic a 1, j argcjn
(during training.
'.'fersona.lised__ attentipn.
activity that enabled learners to
SL_th&
lEained! ’^as-
the
n«ost
conrnon
overcome their difficulty.lt is recomniended
hliat this be continued.
Vlll.l.vi. Approach in Training.
Visits
rehabi1itaticn
to
various
institutions
must be reduced to a bare
espazial ly
in
the
field
of
minimum and even here the visit may
t:e left as an "elective" for the trainee.
VIII-1-vii- Selection criteria.
Se 1 ec t ion c r i ter- i a
as willingness
to hard work,
oust inclu^^ttltudirTal.._characteristics sueh
ability to
commLUi ic a te, a bi 1 i ty
to work
with
others in a health team. since tbiese are some of the attributes most difficult
to develop during training.
(see append i x >; i. 7).
Lkider selection criteria
must be laid
itself a stipulation
down
tfiat the cowwanity health worker_fflust_teJnyolyial_.in_ccwLM
Ia.C
« nunirnyffi.
I.^Y_ii.._years.)....ai:ter -CanBletig-j. of
training.
U te o f
Lite
common J. y
furtherance of education
ex pr ess-ed
for
reasons
or religious formation.
was
tlx?
therefore be
1 aid
non~viork
I t may
down that a!.ly_thg§e..who..Itave.. cgnBleted_.their_religigus.Jarmatign .. may.■
Pnotfer common reascri for non involvement in community heal th work
was tlx? holding of otter responsibilities for example superior.
may
also be selectively excluded in certain
the
added
reaper isi bi 1 i ti.es wou 1 d
prevent
I his category
situations wlx?re it is sure that
active
invo 1 vefro'it in
commur ii ty
hea1th activi ties.
VIII. 1.viii. > Student characteristics.
Ito' advantage
of I omogeriei ty
arid diversity
within tlx?
learners must be capitalised on during the training programme by
s^SiQns
efid...jgrggje.
inc 1 uding I x?a.1. thy
dY[2am.ics
competition.
group of
Use_ef__Qraug
This
makes
learning experience more satisfying.
Vlll.l.ix. Follow-up of Trainees.
A
system of
follow up
must to?
built up.
directory of the ccxfimunity health workers is a necessity.
contain not
only tlx? address
of tlx?
tlx? or gau iisers aware
trainees
tut wouId
but also
give
to/sto is involved in.
This would
not
of tlx?
also t3'.iable_ti^
Ito directory nust
community health worker
brief details of the type of activity
only keep:*
regularly updated
A
wl-jereabcuts and
activities of
their
fa'"
continuing educatim. _feregnnel, Resg^^. for- technical guidance on
could
al‘so te
iden t.i. f ied iEtnd
intiffjated to tfe
corrjniurj i ty fiea 1 th
Uie field
workers as
necessary if tte directory was maintained.
VIII.1.x. Continuing education.
A
system
of continuing
educaticn must
be built
up.
This
could be
’; I
achieved by --
<:■<» specific relevant topics as requested by tie
participants.
I t e refreshier course nust be of
a short duration so that the work
of the ccrnniuriity heal th worker in the field is not interfered with.
Tte refresher
course could
te organised at....a regional level if a
directory of cowriunity heal th workers is developed and maintained.
b)
Circulation of ^s.tlar.bulwould also
be a means of ccntinuincj education.
■
c)
Distance education
developed
education.
and
!
modules for:learning
these' would
Moreover
•'
perhaps
be the
cn specific topics
most 1 cost-
the comniunity health would not have
can also te
effective
means of
to leave ter place
of work.
Recommendatioiis (ix. and x.) would necessitate the mobijization of
adequate resources for the sajre.
t
VIII.2,
SPECIFIC RECLTrO&ATIONS
•i
rec:c:<ririendatici“i j|q , the. trailing progr anr<»e
. Pis • a
details itself n"A
dram up
c«f the com.inity health; workers course lias been
(See appendix)
and is presented.
» . i
i v.'
IFe modifiedi,scheduled envisages
• I
M ,|.
■
|
.»! ■. • •
a total duration, of 12
weeks.
>! • • f
All topics to tie taught tiave been converted into problems ttiat are
coninon ly
expressed , by |(comniiL.f)ity
health
Thus , a^prgtxlem„solving
workers.
approach must,be adopted in tbiese sessipns. .,
)
i:!<
A , systems approach
tjeen
integrated
with first
aid
and care
minor
in
disease, jCogtrol with JIab diagnosis for the, same-
Within
adoptedwith
TFius p ie
ttie
and tl ius
has been adopted
systems
approac hi
a
tonan biology bias
aiIments, ccmnunicable
,
M.fezcYcl^.^arDach
begins with cmception . and a. pregnant
L-jeen
mottier tlien deals
infantgrowing j child,. an
.adolescent, an
adu11.and f ina11y
lea 1 th orier> tied
approach rattier
than,a
This enables a
t"ias
the aged.
disease’s or
problem
based approac 11 -
, |Xir:.ation
of each
sessions, has not
departs from tie routine of teurly sessions and
teen .specif ie-d.
However., it
is restricted to a mininon of.
only 3 sessions or less per day. 11 is pr oposed that these thiree ssssj.ons be of
Three?, two, and one hot.tr duration respectively on each day.Thus
an average
of abcxit six hours of training each
there? will be
day except on Saturdays where
only one ’session will te;conducted’and airidaywhere there will be no session.
• • I 1
' this cables r nfcire
..
i.
11
i < •. i
g roup discussicns,
'• ! !• • •.• I
years-
which are
■ i < ■
1
! U
• f
'
p^rficipatorv' learning
not’1 ‘feasible !in
b .» c I
y i.-'H
tojrly sessions
of
fjas a’ dual "! benefit ’for both
.. i ■
regldred ’ for a1 days
laciAlty and
Trainees
trainers ’and ‘ ‘ trainees;
over from’ one* topic
rapid1y changed
previous
» < 11- •>»
in addition it decreases the frequmcy
this1
is also
are not
number of trainers
to another1 and total
teaching sessions
or-
through ’ exercises
only one1' or’ two
recduced
trainers are hecessary for the 'entire days ses^ioi-'
b!-
.-h i;.. I .)
i.> I i.hsn
would not
This
:
ji * " i
>
to the trainer
be burdensome
as tt ie
trainer is<
expected to facilitate a process of learning and not "to teach" .
i ■
i
■: I I
• I •••.!
blexibility Inas
| • ' IH
■ • ' ‘
‘
of sessions ’on' any
’■ )! i !
»>
cnly by granting
been allowed not
by ’ permi LtIng1 inter1 f cl iknge
but also
I t has
i k-‘;! IU
open sessions
given specified day.
teen the experience tliat rural folk are usually unavailable during tte
mid ;norrdngv ,tajr‘s. ’’ 'F-ifeld ’’visits inay! 1 "thus' tie shifted
’ to 'afternoon or
dusk
sessions and the number of hours modified accordingly.
introduced
for1 f»ave ’ tjeen
farmsespecially
j2)f.Jjjr^nih^’
including diarrhoea and WI.
topics related’to maternal and child health
I ‘
1 ■
With
Qtt^r
i!
Ii >.«
'.I ’•d.'-r'
1*' ) ’' -' '
;
‘ • I: .
'
regard to ttie content of training .itself:
systems of
medicine have
been res trie ted
systercis wliere skill develdpthent is feasible.
to formal
ar«d informal
More emphasis
bias
been
given on
I'lea .1 th
p 1 ctnn inq
and n^iagefiien t
and
especially the use of participatory fnethods in the same.
lack of
community participation»was a commonly
work*Participatory methods
expressed (22.53X) problem in
in Planning and Management
especially through use(
of techniques such as “community mapping" may enable ccmmunity
tea1th workers
to overcome this difficulty.
! L<’ : I
formulation of -<L^£twn^
t he >, 1 ater. weeks in tbe; f ie id
by mid course „ tcnbe implemented in
has also been included in
order- to develop the
skillsof -.the community health worker in planning and managemen t. 35.217- of the
community tealth workers expressed, “lack of. SLtppprtn in
and
ma ter ic< 1 s. TI ii s train ing compionen t
vxjuld pert iaps enable
resources, that are necessary. . >
hi
the form of
tten to mobilise
)
hi'
finance
I ! I
t ' •
Ite need of urtjan areas and especially ttejarb^^lun^ has tjeen included.
I < ‘
~
More. time. has been devoted < tp,
i .i i•
I nuL.u • ff.
. i ij <
. I >
tormwication.
_}
I r^ihirig • in ta.£ijQMnicable: Disease < 1Contrpl has not only been integrated with
lab diagnosis of the same but tiipe. tes also been given for practice sessions.
■ I raining, in epidemiology....in , teal th care lias, teen included.
ltds incr eases
the value and credibility.;of.;tte community tea 1th
worker within the community
by enabling the corrmtuiity health worker to explain
tte ''how'’ and "why" of any
given situation. (See appendix).,
i
i
ca.re<2f^te..aged tes also txseri included into tte curriculum.
fissM^stimalJhealihJhaggr^
hiave been included instead
of topics irrelevant, in rural areas (example;ESI Act).
“
f^aiiaaiton especially informal evaluation almost every week
i">.’ ''?» »« I < Vf’
5 /f
a substantial proportion of 'time! ’
■-
• j > ,
>
*4
• ■
j;
’
- r-
$
' ! *I
t
.• A\Xv ■
V
k
; 7
1 ; *<
V
■
i
•-7 1
1 •’ ■' /
' >1 • •'
■■■
.
r-,-. x !k }v ’ .iv■A,.''.
w t /
•'
r:.
■
i'
i • ■
. H fc • !
ij
:
>!
■
>1
!
.
t
'
has been given
■ Ihe pr-oportion of time spent on the various teaching ffjetliode. used
in the year 1990 and in the modified schedule is represented in the diagram
belo»/n
I
I
<
T-
'
■
■ ■ :
'
'
•
I•
Vlll.a. METHOLOGY IN TRAINING
1990-COURSE VS MODIFIED SCHEDULE
INST- VISIT
5.26%
DEMCNSTRATIO
17-41%
CT
INST. VISITS
13 23%
DEMONSTRATION
FI^L^/ISITS
068%
FIELD VISIT
21.11$
PRAQT- EXER.
16.77%
PRAD. EXER.
30.06%
LECTURES
54.19$
LECTURES
2612%
1990 COURSE
3E
MODIFIED SCHEDULE
26-1:-z of L1"e to te sper,t m
eAL^btAt^6,Df,ly
inttnods or learning such as Practical exercises
PERCENTAS
leccures..utner participatory
Demonstrat ions (21.117.), Supervised
(30.887.),
Institutional visits!5.28%), are given emphasis<
Field
vi si ts (17.41 %) j,
and
sessions,
group
include;
practice
Practical
Exercises
assign!nen ts, ro 1 eor group)
dynamics/exercises,simulation games,individual
plays,and use of modules for learning.
include; demcostraticn of
tercostratims
and
i.ca11 demcnetrations „ and
ini.ca
and cc11in
procedures 51 aboratory
training prcxjrains(TBA training)»
of
demonstrati co
Field.. visits include; Family studies, Mobile clinics, Field surveys,
Ekzhool tealth and Balawadi visits and activity ,Field-based education programs
and visits to Field based projects.
Institution visits include^ visits to various Retabi1itation centres.
The Format of the Training is presented in the diagrams and
table. I he details of the modified schedule are given in the appendix.
ttie
WDIFIEp SCFEDLLE FOR COMMUNITY HEALTH NQRKER BASIC CIXRSE
SYSIB^" ^FROACH TO FROBtEM ""BASED ”LEAmi^... .... ..
r
r
L
r
1. :(F<fFOT._CTICjlM
(1 - 5)
T
(
2. FO'WJ BODY, FIRST AID
CAFE IN MINOR AILFENFS
(1 - 25)
L
r
i
i
T
I
3. ENVIRONTENr AND HEALTH
(1 - 7)
L
i
i
L
4. BASIC NUTRITICN AND FEALnH I
(1-6)
I
J
T
1
I--------------------
|_________ |
______________ 1________________
|| 5.1.CARE OF MOTHER |'
|j
(1-13)
| L
| 5.2.CARE OF' INFANT
(1 ~ 5)
I
LIFE CYCLE AA-RfJACH
IS
j
I
L
I
FFmjEM EASED LEAKNINS
I
| (____________ 1___________________
______________ I__________
| | 5.4.D=fiE OF YOUNG ADULT]
| 5.3.CAFE OF CHILD
(1 - 12)
||
rI
(1 " 23)
f
j
T
I
6. CARE OF THE AGED
I
(1 - 3 )
I
j
T
____________ 1_____________
j 7. CARE OF THE SICK
I
(1 “ 6)
L
1
1
J
T
____________________ I____________________
| 8. OTHER SYSTEMS OF MEDICINE
I
t
(1-9)
I
f
I.
L
i
9. CARE OF TEE ravH...NITY
|
(1 - 29)
I--------------------4 EVALLATI ON
l
J
(
) :
"Child":
Indicates No. of sessions
Refers to pre school and sc:Fool going.
I
1I
II
.1
I
1. IN1RODUCTION
(1 - 5)
j)
I 2.
2. HUMAN
HUMAN BODY,
BODY, FIRST
FIRST AID
AID
f=Jj
|
CARE IN MINOR AILMENTS f
(1 - 25)
84. BASIC NUTRITION
J) AND HEALTH
d-6)
I
- Housing
- Safe water
- Sanitation
- Role of vectors)
- Huaan biology
- First Aid
- Care in sinor ailsents
- Self introductions)
- Experience sharing)
- Role of CHWs
5
3. ENVIRONMENT
& HEALTH
(1 - 7)
- Digestive systes
- Basic foods
Ii - Malnutrition
- Food safety
- Food toxins
- Food adulteration
- Anesia
- Basic concepts in |
Health/Developsent)
i
i
i
L
5.1. CARE OF MOTHER
ADULT (1-23)
|
(1 - 13)
7. CARE OF THE SICK
(1 - 6)
6. CARE OF THE AGED
(1 - 3)
5.4. CARE OF YOUNG
7.1. Hose Nursing |
7.2. Essential drugs)
- Social probleis
- Medical probless
)
- Easily Welfare
- Fertility awareness)
- STD/AIDS
)
- Occupational Health)
- Rheuiatic fever
- Social probless
- COMMUNICABLE
DISEASES
I
J
l
L
I
j
9. CARE OF THE
COMMUNITY
(1 - 29)
| - Acupressure (2) |
| - Herbal Medicine(4)|
j - Ho.e reBedies (3) |
9.1. Health Education |
It Cofiiunication (6) )
j- A R I
|- Hors infestation
|- lasun. coverage
|- Nutrition assessaent)
j- School health
j- Health education
I___________
i
E
V
A
L
U
A
T
I
o
T
j
5.2. CARE OF INFANT
(1 - 5)
')- Diarrhoea
9.2. Health care
s
delivery (5)
j
9.3. Rehabilitation^) j
9.4. Health Planning |
St sanagesent (12)
L____
LIFE-CYCLE APPROACH
5.3. CARE OF CHILD
I
(1 ' 12)
8, OTHER SYSTEMS OF
8 MEDICINE (1 - 9)
- Care in pregnancy j
- Care in delivery )
- Care of newly
|
I
delivered
|
- TBA training
j
N
- Neonatal care
i
- Infant feeding
{
j - Growth monitoring |
| - Issunisation
|
j
s
f
MODIFIED CTXR3E SCl-EDLLE FOR WUU Tr HEALTH UEEKERS
Sl._.
NO.
T O P I 0
LECT
ORES
(g )
Ff¥^CT.
EXER.
(P)
3.17
5
7
CC'7.
FIELD
VISIT
(F)
IFxIST.
VISIT
(I)
DSTOIM.
(D)
1.
In troduc t ion
2
Human body. First aid
c£ire in minor ailments
14.78
24
9
3.
Environcnent & Flea 1th
3.69
5
3
4.
Nutrition & Health
3.69
5
3
6
5.1. Care of mother
7.39
7
5
3
13
5.2
4.
8
5
8.97
3
17
10
23
5
11
3
Care of Inf an t
5.3. Care of child
16
2
4
3
2
2
5.4
Care of young adult
13.72
6.
Care of Aged
1.58
1
7.
Care of Sick
2.90
3
8
8.
□tFier systems of
Medicine
6.33
11
11
9.
Care of community
9.1. Health education
3.96
3
9
3
9.2. Health care delivery’
5.28
2
6
12
9.3. Rehabi1itation
4.75
2
9.4. Health planning .?<
management
8.18
3
12
Evaluation
7.39
5
23
100.00
100.00
99
26.12
111
10.
TOTAL
%age
13
16
Foot note: The percentage is calculated on the basis of
versus the total number of tiours for supervised training.
12
69
18.21
4
20
5.28
number of teaching
80
21.10
flours
Total No. of teaching hours = 379j, which is about 31.58 hours per week or 5.26 hours
per day for six days a week.
C(^)T"0T:i N0IJ.U™A3 A"T€BM
( »..jo peypssnsaj
Aueuoujxnd OTpuea
J„O LIOT.pi?..4^Si..>Z)».Ua(J)
^uosuad pajo Cut
ue ^radsueuq aw op ivk ^i
-l.eaq
o-.| st rej. ^jeaq aqq. j .t
doq.s burq^eauq uno ueQ
«I)9-Z
(tua^sAs Auoqej xdsay
pue Ajo^eT^O-riTD 4-0
uoTTj-oury. pue a.jnq.3n_44S)
aqq^auq aw Aqw pue moh
3.eaq qjeaq
atp. seop Aqw pue mc ^{
Aa ?PT.jj
(o)v’Z
(asyojaxa
tenpTATpux)
syuTyds pue sButts
Afdde aw op mom
(d)£*Z
AOP
op
:p?qf4
Aq^ ssaun^Dejj
ip.TM ^uom aw sai^snw
^-fjowatuej^ T^4aT^>f^ -J'X)
((DZ-Z
ubTs/iuo^dwAs e st
^bupieq AuoqsTH
st
pry 3.sjtj
qeq^
(o)T’Z
Aejd axon
(d)-£"T"6
saTTP^J- (sasTouaxa uoTyeopjnwuJoC))
MaiAjayuT aw ueo Mcy.;
uaqyoue auo qyrM
s t T t ys uory^opdnwujo^
ayeoTtjnunuoo aw ysrvu moh
(o)-3-T"6
(buTtpeaq. sAep
aqri uo s^ueip
j..o UDpejedajj)
•4Lja»jju&Tssy
(d)S-T
(tssauxTT yosAaud aw ueQ
AT IT TW aw op Amm
^uai -1’4 a toy yuaw
-doyaAap >j Ln-ieaq Ajm
(□)£'!
ur 6uTxq.7|as
TH - N0ISS35
(aujeg uoTyepMUTS)
--------SNCXBrJCW —
(d)fr'i
(SMH3 aqi J.o aioy)
°P
SMH3
ysnu.1 yeqft
aqy. 40 ue [c|)
(bbjito
{[tm yeqw
uueaT
(ysaq auj)
Mou >f sm op qonui moh
(o) £-T
U - N0ISS39
asuroo ujouj . uoTqeyoadx-g
buxj^qs aoMBTjadxg
(uoTyonpojquT dmj&
/uot :|□npouy.MT 4. t ^js )
UMOinjun 0-4 ur^ou>j ujoj j
ixjTyejnbiieui •- ^eAejj
(d)T'T
I - NOISSBS
-paM
Aepsanj..
XepuoiAi
AW
SHEMHDM HTWH A1INFW403 HDd HTIOB-OS 3SHnOT
ero l H u/o^
WEEK - I J.
SESSIQM
I
Mon«
2.7(D)
Why and tow does
b1eeding occur
Cuts ? Bruises,wounds
what do we do.
Tues.
How does our skin
protect us?
Conrixrjn skin diseases
2.10(c)
Wed.
Hurs.
Fri.
Sat.
2.13(c)
A persons
Unconscious
With stroke
With fits
Why
What do we do
2.16(c)
How do
see
(structure and function
of the eye)
What are sore eyes
If eye gets injiAred
9.3.1(1)
What is blindness?
Can it be prevented?
(v i si t to b1 ind sc: boo 1)
SESSION - III
SESSION -• II
2.8(D)
What is blood
transfusion
(Demonstration of
blood grouping and
typing)
2.9(p)
Dressings and
Bandages
(Individual
supervised
exercise)
2.11(c)
Bum/scald what will
we do?
2.12(c)
Poisoning
Wtiat do we do'?
2.14(D)
Headaches,
if tiie head is injured
Why and What do we do'?
2»15(p)
Head bandages
(Individual
super visaed
exercise)
2.17(D)
Why do we wear
spectacles?
How do we test
for vision?
2.18(c)
Foreign body in the ear
Ari infected ear
If the nose bleeds
Sore throat
Why and what do we? do?
9.3.2(1)
Can we prevent deafness
Visit to Institute of
speech and hearing.
2.20(c)
Diseases we get from
An ima 1 s. Dog bi. te, snake bite
What do we do?
WEEKLY EVALUATION [10.2.(c)]
2.19(c)
What does our
Kidney do?
Common urinary
problems
WEEK - m
DAY
SESSION - I
SESSION - II
SESSION -III
3.1(F)
Field study / Mobile/
MCH CLINIC
3.2(c)
Housings Wliat role
dees it play on Health
3.3(c)
Do insects transmit
disease - How can we
prevent and control?
Fues.
3.4(D)
3.5(1)
How can we dispose of
Visit to station health
so1id/1iquid wastes?
organisation or
(Soakage pit / compost
demonstration of envir
pit)
onmental models.
Wed>
3.6(c)
Field study / Mobile/
What diseases can we
Dispensary (2.22 (p) }
get from drinking
impure water - How can
we prevent them?
Thurs.
4.1(F)
Field study on nutrition
(Food habits, infant
feeding practices, foods
grown and consumed.....)
Fri.
4.3(D)
Consequences of eating
less
Sat.
Wiiat is anemia - How can
we prevent it?
3.7(D)
How do we purify water?
Demonstration of chlor—
ination of well
4.2(c)
Fate of the food we? eat
(Digestive system)
What foods should we eat
why?
4.4(D)
How do we keep food
safe? (Food hygiene,
food preservation).
4.5(D)
Can certain foods be
harmful? (Food toxins)
What is food adultera
tion?
4.6(c)
WEEKLY EQUATION [10.3. (c)]
(Field study/ mobile clinic/ dispensary/ MCH clinic small batches in rotation.
WEEK -- IV
DAY
Mon.
SESSION -- I
5.2.3.(p)
Nutrition Demonstration
(How should an
infant be fed)
SESSION - II
SESSION -III
5.2.4.(c)
How do we know if one
is eating well.
5.2.5.(D)
Road to health card
5.3.3.(p)
Module on diarrhoea
Tues.
5.3.4.(p)
Module on WI
W&xJ.
Thurs.
Fri.
Sat.
5.2.6.(P)
Preventing specific
disease by immunisation
(Domm. PHO)
5.2.7.(c)
Six killer diseases in
children
5.3.1. (F)
Immunization coverage - Field study
10.5.(p)
PROJECT PF^ESENTATTON
5.2.8.(D)
Video film
5.3.2.(p)
Evaluation of
Immunization programme
WEEK V
DAY
SESSION - I
SESSION - II
SESSION - III
Tues.
5.1.1.(p)
Care during pregnancy
5.1.2.(D)
Lab. tests in pregnancy
Weed.
5.1.4.(D)
MCH c1inic ZDispensary
(Mallur)
5.1.5.(c)
How a child is bom?
Care during delivery
5.1.7.(c)& 5.2.1.(c)
Thurs.
2.24(p)
MCH c 1 in ic /Mobi 1 e
(Domntasandr a) c 1 inic.
Fri.
MCH clinic/Mobile
(Ka 1 km ta ag rahara)
10.4.(p)
Sat.
Weekly evaluation
PR11ECT FFESENTAIION
Care of newly delivered
fnother
Car e of the newborn baby
5.1.10.(D)
IDA contact training
program
5.1.3.(p)
Practice of tests
5.1.6.(D)
Video film
5.1.8.(D)
Video film
5.1.11(c)
Discussion
WEEK - VI
DAY
SESSKJM - II
SESSION - I
JK
Non.
9ESSIC1N - III
MCH CLINIC (MUBALUR)
Tues.
5.3.5.(p)
Nutri t.ion demonstration II
5.3.6.(0)
Child passing worms
Common stool tests
5.3.7.(p)
Practice of stool tests
Wed.
5.3.8.(F)
Nutritian assessment:
How & Why? (Balwadi)
Thurs.
5.3.10 (F)
Schoo1 hea1th
program
5.3.11(c)
Common diseases among
children? What do we do'?
9.1.4.(p)
Child to child program
(preparation)
Fri.
9.1.4.(p)
Child to Child programme
(Conduct)
9.1.5.(c)
Child to Child programme
(Evaluation)
5.1.12(c)
Registers for MCH
Preparation of MCH
SAT.
9.4.1.(p)
Action plan format
5.3.9.(C)
Caring for
school children
uor:|.e.ji»dajd i.3aroja
UOTSSHDSTCI
(^■zvtr’e
uoTTdaae-JTUos
j.o spcxRaw uaqw
(a)'0T’fr-s
(Saiv/OISJ'XBS UT
pauTTdr^TpijT st buo
O)‘6-Ve
NDIlWlhBSJHJ lOJrajJ
(d)•9-01
""4*S
X^TmuwjDD jeuru e j.o
spuezeq [eiJOTiedra^Q
(J)’TT"fr’Q
" MJ
PiaTa-aJSU-TSM ZT Tu»d
ur uoTieanpg qip?an
(d) ‘8"t--g
seuK>.u euTTSoBny -ug
- - ssauaueMe ATTTTTuaj
(Qj'Z'tr’fi
sewam euTTsaBny -jg
----- ssaua-iewe XTTfTq.jaj
---------------- _ _
^/j -Tu Bts it saop ^epw
•jQTSoxdxa uoT^^xncioj
III - NDISS3S
'san.i
(a)‘S‘fr'5
(=>)"V’t7"S
UOTSSnDBTQ
Aprqs pja-rj
- aje^taw A-[rtire?.-|
(2)"z;-tr"s
(JJ'T'fr'S
II - NDISS3S
I - NDISS3S
" inow
AWG
IIA - XHJM
WEEK - Mill
DAY
Men.
Tues.
Wed.
SESSION - I
5.4.14.(F)
Social problems in
young adults
5.4.16.(F)
Leprosy survey -field
5.4.IS.(D)
Lab Tests
(skin smear for- Leprosy)
Thurs.
5.4.21.(D)
Lab Tests
(Smear for MF7MF)
Fri.
6.1.(F)
tore of the aged.
(field study)
10.7.(p)
Sat,
F-ROJEC1 FFESEHTATION
SESSION - II
5.4.13.(c)
RFieufitatic fever
Who does it effect?
How can we prevent?
SESSIUM —III
5.4.15.(C)
What is leprosy
Now can we prevent
arid control
5.4.17(c)
What, is Tuberculosis?
How can we prevent «t
control?
5.4.19.(D)
Lab tests
(Sputum for AFB)
5.4.22.(c)
Fevers j, what to do?
Malaria, Filaria:
What to do?
6.2.(c)
Diseases of lifestyle
5.4.20. (p)
Practice
5.4.23.(p)
Practice of
Tests
continue
theory session.
6.3.(p)
Discussion
WEEK -IX
DAY
SESSION - I
8.1.(D)
Mon.
SESSION - II
SESSION - III
8.2.(p)
Acupressure and Health
Dr. Shi rdi Prasad
8.3.(c)
Tues.
8.4.(D)
- - Flome remedies--
8.5.(p)
Dr. Shirdi Prasad
Wed.
Thurs.
Fri.
27/11/93
Sat.
9.3.3.(I)
Rehabilitation of physically handicapped
(visit to AFH and visit to Spastic society)
9.3.4.(c)
Discussion
9.2.1.(F)
Visit to CdmmLinity
development centre
(ASTm)
Role of ttie Church
in delivery of Health
care
Fr. Sebastian
9.3.5.(I)
9.3.5.(c)
Rehabilitation of mentally handicapped
Mental health
(visit to NIMHANS/Child guidance clinic/Sakalawara)
health care.
10.8.(c)
WEEKLY EVALUATION
printary
WEEK - X
DAY
Men
Tues
SESSION - II
SESSION - I
SESSION - III
7.1.2.(p)
7.1.1.(D)
Home nursing:
Measurement of temperature, pulse , respiratory rate, blood pressure
Administration of medicines: Ora 1 tablets/syrup/drops
Injections IM/ID/SC/IV
Cold compress, steam inhalation, hot formentation,
Mouth wash, garg1ing,
application of eye and ear drops
cleaning and dressing of wounds and ulcers
(Demonstration and individual supervised exercise)
7.1.3.(D)
7.1.4.(p)
8.7.(p)
Herbal Medicine and Health
8.6.(D)
Wed.
8.9. (p)
8.8.(D)
- - Herbal Medicine and Health
Thurs.
Fri.
4/12/93
Sat.
7.2.1.(D)
Village Kit box
(Demonstraticn)
10.9.(p)
Role of indigenous
systems of medicines
(DEWTE)
7.2.2.(D)
Allopathy' commcr, drugs used -
b<:)IlVlN3B3dd OdfOHd
(d)“0T-0T
*
(sua3.srba.ui pue spucoau jxj aaueuaqup?^)
auea q^fean ur AtofOTuiapTdg
A^.t »..«"wjijuo 3 e jj.0 sn^e^s
Mlieaq jo :p..ojjajnseew
(□)-0T-tr-6
7|.uawssasse paau tunf-s ueqjn
(d)-8"tr"6
(au«?b uorqexnuJTS)
- » SNIW3
---------(d) "Z.’l7-6
(seHTA exTqew)
miea^ ur ijawotf j.o afo^------(d)-9-tr"6
------quawdofaAaa
(aweb uorqex^TS)
- oITltWhRTC’IOIHO „
(d)-l7-t7-6
buxddeuj Apofl
(G)"£’i7"6
suapeax
j.o uorqeDT^TqLiapi
-sanj.
(d)-£-i7"6
(ftuyddeui xexoog)
saDunosau/paau/swa tqoud .Apn^^-i A.} tunwmco
(a) -s-17-6
IH - NDISS3S
"T-ld
(d) "6"fz’6
II - NDISS3S
(d)"T"i7"6
I - NDIS83S
Atti
IX - MHSM
i
WEEK - XII
DAY
Mon.
Tues.
Wed -
Il-Mrs.
Fri.
Sat.
ROW
SESSION - I
SESSION - II
9.2.1.(c)
Health care delivery
in India.
i
SESSION - III
9.2.2.(p)
Study of PHC : Structure, •fLinctim j, organisation
staffing
9.2.3.(F)
Working with field staff of PHC
9.2.5.(I)
Working through cooperatives
(Visit to Mallur Health (Cooperative)
9.2.4. (p)
Na tiona1 Hea1th
programme at PHC
Community participation in
Health care and planning.
9.4.11.(c)
9.4.10.(c)
— Planning, Management and Evaluation of a health programme ” -
10.11.(0) Sj 10.12. (p)
How much do we know?
Final evaluation
Evaluation of the Course
i
Ac:tian plan for
the year
-- VALEDICTORY FUNCTION - -
Dr Dara S .
Amar
) o.
REFRESHER COURSE FOR F
COMMUNITY I-HEALTH WORKERS report
(16th TO
J 29th AUGUST
--- ‘
1993)
~ Dr REYNOLD WASHINGTON
A f t o r a 1 rn q s ■£•
decade. a REFRESHER COURSE
for COMMUNITY
HEALTH WORKERS t r a i n e d f:< e t w e e n
1991
and 1991, was
conducted in
our COMMUNITY HEALTH
training CENTRE, at MUGALUR,
i r c<rn
the 16th
to the 28th of
August 1993„ This
is envisaged to
be the first
step towards a
CONTINUING EDUCATION PROGR AM for
the community
hea 1 th workers ,
a g1 arin g lac una
i n the T raining
program thus
Tar, as evident
from the Evaluation study done
on training during
the decade 1981 •••-1990 .
A total number of
the course.
The response of
unexpectedly poor ,
.17 c o m m u n j. t y heal t h
workers attended
the "re 1i gi ous sis ters"
was
and "religiOLlB«« made up less
total numher of participants for
the course.
however
than 257. of the
The participants had
c o m e f r o m d i f f e r e n t regions in the
country, i n c 1 u d i n g M a d h y a
Pradesh, De1 hi, Karnataka,
Kera1 a and
Tamil Nadu , representing a 1 umn.1
from 1982, 1985, 1989,
1990 and
?1- All of
them were actively
involved in different forms of
c o i n m u n i t y h e a 11 f •j and
deve1 opment activity
in their respective
areas of work «
The
diseases,
course content
including
inc 1 tided s Control
-d raided-
of co/nniunicable
AIDS,
Heal th planning and
Mai i ag ement i nc1u d i ng t: e c h n i g u e s o f
Participatory Rural Appraisal ,
H e a 11 h E d u c a t i c.< n Materials
and Methods, Herha 1
Medicines and an
update on the use of
c ommon drugs, an
integrated approach to the
problems of Mother and Child
through an overview
of the Child
Survival and 8 a f e M o t h e r h o o d
Program, N u t r i t i o n I r j t e r v e n t i o n
and
N u, t r ;i. t. i c::< n E c:l li c a t. i o n 3
Muc h
t i me
wae
C o mm u n i t y
devoted
d ev e 1
s pec ifi c a 11 y
c ou r s e w a s c on d u c te d
d e p a r t m e n t o f C o m m li n i t y h e a 11 h 5
C h i t o o r f o r H e r b a 1 Med ic ines -
Doctor :
Lab.
coneurrently
d la i" i n q
b y t h ee
f a c u 11 y
of
the
e x c 1 Lt s J. o n o t F r . J q <s e p h
wsisLH the
All
Doc tor
resource personnel
and
among the par tic i pan ts ,
sessions to ” e x pe r i en c e s ha r i n g "
The whole
p m e n t. a n d F:‘ r a j e c:: t F' 1 a n n i n g «
topics were taught by a team of
Soc i a 1 Sc i en t i s t / wor k er
or
technician,
Doctor
:
D o ctor co nj bi na t i on s
as
.elevan t.
The methods adopted
use of
Modu les j,
c 1 a s s r oftw a n d
level?
Ro1e—p1ays ?
field—based?
based
Case —
studies j,
an d
tra i n ing
Demon s t r a t i on s
G r o u p e x e r c i s e s,
1 ec t u r e-d i s c u s s i o n s „
i n c 1 ud ed ?
both
F am i1y and c ommun i ty
Field studies at
G r o u p d i s c u s s i on s
c1 assroom
.tCtW dA'XA d u r i n g
The
in addition
was
course
to
total 1y
residential in t h e T r a i n i n g c e n t r e .
A feedback eva1nation
from the
17 participants,
both
i n the form of a formal semi—struetured questionnaire and through
classroom discussion which
n informal
eac h
s e s s i cj n w i t h
to
regard
s p e c j. f i <::: a 11 y deal t
t h e c c.:« n t g n t ?
m e t hod o 1 o g y a d o p ted ,
t r a i n i n g a n d t he c 1 a r i ty o f
time spent j.
place of
condue ted.
T h e f o r m e r g a v e a b r o a d o v e? r v i e w o f
its content;,
re1evance ?
the
the
staff
tot a 1
was
course;
and
the 1 a 11 e r
t o p i c a n d s t a f f d e v e 1 o p m e n t.
The course
d u r at i on and organ i sa t ion?
f o r ind ividua1
was usefu1
wi th
c o n c 1 u d e d w i t h a short and entertaining Valedictory session■
A
g r a p h i c a 11 y .
brie f re po rt
The
of
In forma 1
i n d .1 v i d u all y t o e a c h s t a f f -
the Formal
Feedback
f eed bac k
has
been
is
presen ted
c om mu n i c a ted
ST. JOFFtS MEDICO- CJ1E(£, BAhX^LCF£ 560 034
Cownunity Health Workers (16 — 28 August, 1993)
D^te/Day
I
II & III
16.8.93
Monday
fcttlirjg in and
Course expectations -RB*J/RMC
Control of Diarrhoeal diseases
Modular Training -RGW/RMC
17.8.93
Tuesday
Cc::<ffrfnunic: ab 1 e Di sease Con tro 1
How do we prevent •?< control
AIDS? - RGW/FMC
How do we prevent •?< control?
TB/Leprosy/Ma1aria (inc1udes 1ab. demonstration)
- PM/JM
18.8.93
Wednesday
Cot Tirol of ARI
Modu1ar Training
-PM/JM
Hc:w do we prevent
control?
TB/Leprosy/Ma1aria ~
a.9.8.93
Tl’iursday
Haalth Planning •?< Management
Evaluation of Idea 1th status
of a community -• FM/MIQ/MG
FRA Tec I r i i ques s
—Socia1 Mapping/Focussed
intervievjs/Body mapping/
demon s t ra t i on MG/MI
20.8.93
Ccnduc t of Chi 1 d-to-Chi 1 d
prog rafwixa a t sc Fioo J. /
conwro",i ty -MG/MIQ
Mu tri tion temcnstration in
tte Community - practicals
- MIQ/MG
21.8.93
Saturday
Ex per ience storing
-DSA/MG/MIG/AK
I-fer ba 1 Medic ine
22.8.93
Sunday
Pierba 1 Heel i <::: i ne?
23.8.93
Monday
Ftea1th Education
Materials .?< Media
(exercise)
24.8.93
Tuesday
CSSM Programme Modu1ar Training
Interventions for tlie Child
- BJ/DM
25.8.93
Wednesday
Participation in Maternal
.?< Child Health clinic
ac t i v i t i es — KFMT/CS
(Ma11ur MCH c1in io)
Conrncn problems among women
(Medical)
26.8.93
Thursday
C3BSM F'rograjwe Modular Training
Irrterveritions for tie Mother
- KFMT/CS
Mi.vtriticn assessment of a
ccfrimuTfity — KFlTr/CS
27.8.93
Friday
Cc*n imun i ty Deve 1 cp<nen t
I n terven tions— LB/Ftt?-/FS^
Pro.j ec t p 1 ann ing for
individua1 partic ipanis
2B-8.93
Saturday
Evaluation & Valedictory
.I..A..5 n .■
m
x inc:: 1 udes 1 ab« demonstration)
- PM/JM
-AK/Fr. J. Chitoor
Fr. Joseph Chxtoor/AK
-BJ/DM/TS’C
Update on Co^rtcn Drugs
- BJ/DM
- KRMT/CS
- LB/RGW
All Faculty
/ •...'
RGW/as
DR. DARA S AMPR
Head
Professor
SATIS FACTION OF CITWs
(CONTENT OF COURSE)
FT.FJ..X
JSS
imi ■
?D. 59^
12
w
ff&Maisfesgigig81'1' w™
IBSiW..
M'WWWW
............................ r ■
\\\\\\\\\\%
'\\\\\\\\\\
Fj LHITl U.LT HLTISIFIED 5
2&.41&
--«--J»- '■... VJ».--,"~
DISISATISFAC-TIO N: CONTENT INADEQUATE >
TACK OF PFA-CTICAES, MATERIALS:, EXAMPLES
TDTAIr--.1.7
SATISFACTION OF CIHVs
(RELEVANCE TO WORK)
FULLY 3A3I3FIED 13
igfcfthu..
71149'S
.■niisgjgaiiig
ISaaawMjiw
JSEg
ifB
a
s
H
/
-■
I; i iBL..........
—.^....J®3"
u
.x\
1
^Bil'iiil
■:
X\ \ \ X \ X X X X \
x\\\\\\C\
•^-xx. \
Fjuni4.i;i;iir S4TC3FIBD 4
23.53^
'T
SATISFACTION OF CWs
(ORGANISATION OF COURSE)
«_....
FULLY Sbm^Fmi’ 12
VD.59^
B
40
SHF ■ 1
iaai
TL-rrtW
1; f
VA\\\\\\\X
wir
%Wx\
PAHTULLT SATISFTSII
TED 5
20.41^
Mk
sipF
\ \, \ \ \ vr”
DISSATISFACTION: FIELD VISITS TOO FAR
GROUP DYNAMICS NOT USED .APPROPRIATELY
SATIS FACTION OF CHVLs
(LODGING FACILITIES)
.FULLY S.1T23FIED 15
El El. 1X4.^
J®
gMgg^e
! * ■ ;:8ftsS
"Cllllffriti
•«
....... ............
..
." < ", < --■■'<ihMMF
J"....
r WlitiasW
W - 111 '-^7: ’
WaHH \\ r..\\A'r
. V,VW's
L
’.
I\\
I
*.
\
\
*.>••
P^ILtlLLrii'- amiEIFIED 2
11.^0%
DIS SATISFACTION:
FOOD, WATER & IWECTRICT'TY SUPPLY.
rDTAIr-.-lT
TOPICS OF IMPORTANCE COVERED DURING
COMMUNITY HEALTH 1YORKER -REFRESHER COURSE
LEAST I WORTANT
GEE&TESTIMPOETANCE
itninuiiMwiiBw»iniiuiniiu>iHiiwniiiiiiittiiiiwiiiim«—iiHwnnwniniiitwniiiniin
1) Maternal and Child Health
2) Child te Child
3) Co m.mim icable Di see a sc control
4) CSSM Program
5) Nutrition.
6-) H e al th E d u c a. ti o n
1} P u Ft A. T e c h.n i q ue 3
2) Herbal medicines
3) (Malaria)
4) Health status eval/
Update on drugs/
P r oj e c t p r op o s al
TOTALS 17 (IN ORDER OF COMMONALITY OF RESPONSE)
OPINION OF
(DURATION OF COURSE)
ADEQUATE IE
:-:-X
/
L
•
’
.
■/
■?
*’
TOO SHORT 3
17.
\ x«
i
\ \ \\
\ \ H
MSifiF. \ X X X t
^/x, X, X, X, X «.
TOT DMO E
i - ’. •. •
t ’• ’• ‘
’i • ■>>
i1
TOPICS INADEQ UATELY COVERED DUE ING
REFRESHER COURSE FOR CWs
NOT AT ALL COVEEEP
INADEQUATELY COVERED
i) Women and. Development
1) F roj e c t p r q p cis a 1
2) C o rjom im i ty d cts 1 o p me n t
3} Maternal & Child Health
4) Child to Child/ PHA
5) ARI/ CSSM/Herbal Medicine
TQTAL^l.7 (IN ORDER OF CiyKO/GNALTTY QF
CHANGES IN REFRESHER COURSE RECOMMENDED
BY TRAINEES TO MAKE IT MORE USEFUL
i
I
I
i
I
1) Traiidiig to include more practical exercises
and to allow more practical experience.
2) iuu Fw demonstrations to uo iixuliidau..
3) Field visits to be more practical oriented and
not to be too distant from centre.
4) Games to be organised during free time.
/) More songs to liven up sessions.
0) Group aotivitiea/reaponHibilltlea to be alloted.
(classroom cleaning/ washing/ etc.)
7) Participants to arrive one day before the course.
B) Group diaousaiona using homogenous groups and
heterogenous groups depending on the issue discussed,
(homogeinity with regard to type of work involved in)
9) More time to be given for experience sharing and
this to be done at the beginning of the course.
10) Hand—outa in simple language to be given
for all topics.
TOTAL = 17
C.C) rY)
REPORT 0=- gyMJNlTY
BASIC enJ^E.^
F£D3^vB,-gy>TICiNS BASED ON FEEDBACK FRCM D-^
gjn-^_OTl:j^^g
prevent can fusion as to to/j
to transport
2) Cotirse trust be more structured. A lot of tine wasted waiting
arrive? betvMeen sessions., and during the evenings.
•for staff to
1) Course to begin on a luesday to
the CHWs to the Training Centre.
more seif“-learning. In
3) A Library is an essential pre1—requisite to enable
'-.he absence of relevant reading
material, assignments that could have been
given are impossible to complete satisfactorily.
4) There must be more facility for recreation and relaxing. Provision of more
facilities for indoor games and light informative reading material would be
suitable for the OHW age group.
5) Adequate sitting arrangements must be provide-?d for in the classroom. Whi 1 e
mats may be culturally
appropriate, it is
cn mats
sitting on tbs
floor- cn
mcntfiS. especially for the
uncanf ortable wbien the duration extends to three months,
more elderly.
must be coordinated tetter. There were so many vehicles
ffKuving up and down everyday, yet no vehicle available when actually meeded.
6) Vehic 1 e novenei"j ts
7) Staff movements (change
ai: ten un pred ic ta b 1 e«
fronj one to
another) f«ave teen
tc:o frequent and
is necessary* to ensure
that
8) A single co-ordinator for the entire course?
the course is proceeding according to plan. A fecalty resident for at least a
or a learning block ‘would al ternately suit the fWizsosse.
was very approachable and helpful at any given moment. Hc*\uaver tlit-j
9) The
sa/iie could not te said of the interns who were riot only unapproachable tut
also very' cc:nde~cending in their attitude.
Language has been a barrier to learning. Staff must te urged to use more
simple" language. Besides
as far as
Besidrsa since the group itself was heterogenous
lanquage is ccricern^J,ccfrrrtinicatico through "sharing sessions” did not really
make headway»
2) During the field sessions:
-- supervision was grossly inadequate. Very often briefing itself Wci£> riot
adequate and CHUJs were at a loss as to what exactly they were expected to
learn from the field situation.
- language was a barrier , since only three? were ven/ ccoversant with Kannada.
visits to far off plates may te reconsidered as the benefit derivea from
these visits were not as much as the effort, and time expended, leave alone the
cost.,
/OU^.
I
3) 11 is necessary that individual and group written assignments
throughout tte course. A Library is a necessary pre-requisite.
fe give=ri
to individual care for minor
4) Practical exercises especially with regard
was dealing with such
Muga
1
ur
ceritre
a i 1 men ts were inadequate. though the
various
>
sec:tions in the
cases, unless the CHls are formally posted to the un1ikely to uti1ise the
are
centre (Lab., Injections, Dressing) tl’iey
opportunity provided.
"modules” as teaching aids. The module on
diarrhoea was well appreciated tut tl'e module cn PEI requires that more copiesbe produced
distribution.. Appropriate
be developed, or
for distribution
modules may t::e
produced for
Appropriate modules
acquired if already available, for otter important topics.
■ ■be more? sessions using
5) There must
Of Audio visual aids was restricted to tte use’ of the blackboard arid
video films
occasional use of the slide projector. Tho use of otter aids as
that wi11 be
simple
audio-visual
of
aids
cuId be useful.. Preparation and use <
in must be
available and useful within the community that tte □•M works
taughit..
■ • Ltee
•• ,
6)
7) Lectures
must te macle shorter and more assignments may be given.
8) Simulation games must txe conducted more
to participate more fully.
slowly to enable every individual
ccctradictory opinicns frem different teachers on tte same topic
This resulted in confusion. This could be avoided if tte
clarify
these issues.
staf f 11" emse 1 ves
9) Thiere were
a few instances.
in
10) It would be preferable if one entire learning block is conducted by
single staff or a single team of staff. This would reduce frequency of change,
vehicle mvement and would prevent contradictory messages on topics.
1.1) Reduce the actual number of faculty
ensure continuity with a g.iverj block.
directly responsible for teaching to
r-’i Topics must l:::e done saqumtially as planned irrespective of change in
staff'"to’’suit individual cmvenimce. Staff wanting
that tfere is no
with regard to their res-idaatial posting must ensure
.c...::
change in the schedule of teaching.
.13) The total duration of tie course could be rediAced to aboi.it 10
cover every thing that is being taught at the moron t.
f^HSt^Wluatico during the
oral questioning.
course must te
weeks to
through both written and
It must te done at tte end of every "subject block .
were c.endue.ted only twice. Thiese must
=i_(.on Saturdays
L—
2) Weekly evaluations^
must
also be tetter structured.
and
Ji-.t
conducted with more <
te
tfe '’Project presentations" it would be more useful and ericcM..iraging
if more faculty attended. The presei"ice of the faculty responsible for teaching
3) During
1
a p p Pec i a t ecrMjn±--44-<e ._modtoloori ART"Tequ i res t ha t more c opi es
foi^hlTrn
be pr oduc ed
. Ai? p.*'" ° p r a
c:) u ie’15 m a y
d r
■erT'ed
be
i f a :•
M e conaernEed topic .to inard^tory u
SPECIFIC SESSIONS:
1) Tte exposure to tO! clinics arid tte FHC were very cccnpretjensive and useful.
Only tte visit to Mallur was a little too distant and tiring.
.2) L..ahora'tor"y tests require nx::)re demonstration and practice. It is advisable
that they be conducted by a team of Doctor and Lab. technician to ensure
greater applicability of the tests.
3) The time alloted to tie "Other systems of Medicine" must be increased to
allow more time for practice. The session cn "Preparation of Mixtures and
Ointments" rmay be either- conducted by dept, staff themselves or totally left
cut .
4) Tie visit to NlTlW-fcj was not useful. The session was
at a level too high for comprehension of the CHWs.
tie "Station Health
5) Tte visit to the
rural situation at all.
tcc theoretical„ and
Drgariisaticri" was not
relevant to
tie
6) The session on "Poultry Training" was a waste of time as only a few could
understand Kannada. To make matters worse the session was repeated. Tte
training could be conducted by the dept, staff itself in a language understood
by all.
7) The See-ion oci "TOA Training " was very useful both in
reinforcing appropriate methods of training.
its content and in
8) More tine to t::e alloted to tte "UpiatE? on CoiTrio"i Drugs"„
9) More time to be spent in explaining anatomy. While very beautiful charts
were used it was difficult to visualise
Tie visit to the Prjatcmy
rea1ity, Tie?
visua1i se reality.
luseum may therefore be reintroduced. Appropriate models rray also be? used.
10) Tte session cn "Natural Family Planning” was very useful tut requires more
tiine.
11) "Role of tie CPurch" was totally irrevelant in tte mixed group of CH-to.
12) "Itopulaticn Explosion” was no I. urrt/ not understood H h».to also irn^veTmt in
the? gi'.'ui --■--■■■■■‘■ ■m-i. A social analysis of the country would be more appropriate.
13) Ttere must be more time for practice
accomodated during tte night sessions..
14) "Health Education
of "Home Nursing”.
This could be
Materials and Media” was not conducted at all.
$15) A session on "Drug-abuse" to be included in tte next schedule.
deve
Com P
G8
cri/)t
cf>l%l
'QhfMUNITY HEALTH WORKERS COURSE
A’'
ST, JOHN’S MEPICAL COLLEGE, QANGAI.QRE
vX' HISTORICAL BACKGROUND AND EVOLUTION OF THE COURSE
In the years 1973 to 1976, the Dept, of Community
Medicine had gained some experience in training and utilization of
village workers in health care in two of their micro-level health
care projects in the villages of Mallur and Silvepura.
1975: Srivastav report on medical education and support
Community
manpower
training
of
recommended
Based,
Semiprofessional, part time workers to provide a whole range of Basic
Health Services.
1977: A perspective report to the Catholic Bishops
Conference of India on St. John’s Medical College in its subsection
Looking to the future (31.4) an idea was mooted that the college
should undertake the training of the seminarians as village health
workers, in response to the Government of India proposal.
an
out
Organization
brought
Health
1977:
World
Organizat ion
experimental edition of a book called Primary Health Worker, which
outlined various guidelines for training of personnel to intervene
1 eve 1 after
in health care at the most peripheral practicable level
simple training.
1977: Prof. S.V. Rama Rao of the Dept, of Community
Medicine, outlined the broad and specific objectives of the course
for primary level health workers.
1978: A cor /Lnum publication from Vatican on The new
orientation of health services with respect to primary health care
work helped in clarifing the Christian approach.
1978: Major Gen. Mahadevan, the newly appointed Director
of Rural Health Services and Training Programmes, further outlined
the Learning objectives of the course.
1978: St, John’s Medical College involvement in Primary
Health care work was given certain policy guidelines by the^Dean
and the Director of Rural Health Services, Dr. C.M. Francis, Dean,
outlined further ten areas of expertise of participants o these
courses to be organised in St. John’s.
April 1978: The first pilot course for Community Health
was
held at St. John’s Medical College and Hospital and
workers
Rura 1 Centres for a duration of three months.
The course
training methodology.
subscquont1y
©vo1vod
bo t h
in
con ton t
and
G9
In 1988 an attempt was made to integrate related topics.
Thus a system was dealt with as a whole beginning with the Anatomy
and Physiology, continuing with common ailments and minor injuries
and their management or first aid respectively, and followed by
pathology and preventive and promotive and curative measures for
the same.
The
1991:
All topics were converted into problems.
teaching schedule was now altered to include two three hour session
per day in college and three sessions in the field. This did away
with the hourly changes of staff and topic which was not conducive
This problem based teaching was also more
to student learning.
ince
they
raised
issues that had been brought to light
practical s
scientific approach problem based
the
past.
The
by CUWs in
of the staff in training
required
a
re-orientation
teaching also
methodo1ogy.
TO DATE
Total No. of courses conducted = 27
Total No. trained
= 526
Usual intake per course
“ 18 to 25
SELECTION CRITERIA
Basic Qualification :
S.S.L.C. or Equivalent
Those already engaged in Social Developmental and Health fields in
peripheral areas.
sponsored by the
Religious Sisters,
Priest
Seminarians,
,
congregation or Bishop.
Lay people sponsored by voluntary agencies engaged in developmental
work.
Bishop or
Lay people in health team sponsored by congregation,
inst i tut ion
Working Knowledge of English
Exclusion criteria
Previous medical or nursing training
Inclusion criteria
Person from the same congregration or diocese
Person recommended by previous CHW trainee.
of
ORIGIN OF 27-batches
COMMUNITY HEALTH WORKERS (1978 -1992)
of
address
zw
/■
Z*-.
\
a. i
\(
V*
</ -V
(39)
®
<
V/(l55) /zT^x z
G
%
o0
0 ?O*
(U
I
p—4
/
O
V.
w
c
/
/
TOTAL No. TRAINED - 526
I
GOAL
71
The Community Health Worker mustia) Determine the needs, problems and potentials in the community
in the field of heal th.
b) Accord priority to community participation in Health services.
c) Provide primary health care when and where it is most needed.
OBJECTIVES
To enable the Community Health Workers to help their community in:
a) Control of communicable diseases by:
” preventing the spread of epidemics and notifying such
diseases
- undertaking vaccinations as approved
-identifying, treating, advising and when necessary referring
patients with communicable diseases.
b) Provision of Maternal Care by:
- identifying the pregnant women in the community, advising
thorn and referring high-risk oases to the health centre
.
or hospi tai.
- preparing for delivery, assistance at child birth, giving
first care to the mother and the baby, calling for
assistance or referring cases when necessary
- giving post-natal care, advice and family planning
informat ion
c) Providing child care for both well and badly fed children and
promoting nutrition education.
d) Giving first aid in cases of“ ’burns,, wounds, fractures,
accidents
and i—
~ —---- — and referring them when necessary.
bites,
sanitation, health
e) Concerning himself with environmental
supply,
water
excreta and
problems by advising the community on
waste disposal and food protection.
a view to solve some
f) Identifying community health problems with
of them.
standard
u) Measurement of health status of a communi ty us ing
indicators of health
h) Care in minor ailments and referral for cases such as pains,
intestinal worms, skin diseases, eye diseases, diseases of mouth
and teeth, mental diseases, venereal diseases and head-aches.
' A’-
-Ci
i) Promoting health education trying t-qr make each person ana
family, an agent for change for better health and health practices.
■
of’ various types including
J) Community Development activities
animal husbandry» agriculture,
avui w.. w , horticulture, .poultry, piggery and
*‘h local leaders
and
on,
by
dlHousAing
oommunity problems with
ho
the
the
of
life
of
quality
working out solutions for improving t
popu1 a I ion.
cases and problems outside
k) Referring to appropriate centres all
or above his competence.
vital events (Births and
1) Maintaining basic medical records of
deaths in the Community.
COURSE CONTENT
1 . Human Biology
First Aid and care in minor ailments
2.
3. Nutr i t ion
Immunization
4.
Maternal
and Child health
5.
Family
Natural
Planning
6.
FrivirorifnontcilIIottltli
.
7
Control of Communicable and Non-communicable diseases
8.
Health Education methods
9.
10. Medical Records
11. Health planning and management
12. Stat i st ics
13. Home Nursing
14. Simple laboratory procedures
15. Mental health
16. Occupational health
17. Traditional systems of medicine
18. Essential drugs
the Church
in health care
1 of’ I-.19. Role
--20. Conversational Kannada
Field level:
1.
Primary Health Centre: Organisation, structure, funct i ons
staffing pattern and functions of star .
2.
Village family life. Community diagnosis, Commun 1 ty^<
organisation, environmental sanitation,
3.
4.
Maternal and child health oare services, school health,
nutrition assessment.
Mob i1e
Health education methods, organisational matters,
clinic
73
METHODOLOGY
Didactic sessions
Lectures with audio-visual aids
Group discussions
Demonstrations and practicals
Simulation games
Role play
Learning by doing
Supervised field visits/field work
Visits to institutions
i-- col
-- lege departments
Visits to hospital and
Work on the Mobile clinic.
Use of modules
(Audio-visual aids used commonly i nc1ude, slides,
board, over head projector, models and video films)
1.
2.
3.
4.
5.
6.
7.
8.
9.
10
11,
12.
cha 1 k
FACULTY AND INSTITUTIONS INVOLVED IN TRAINING
1
Faculty of Dept, of Community Health
2' Faculty of Dept, of Fertility and Family Welfare
ENT)
3. Faculty of Clinical Departments (Dermatology, Eye,
F.
(Visit to Anatomy Museum, and Blood Bank, SJMC)
Rehabilitation contros
1. Association for the physica11y handicapped
2. Spastic Society
3. Institute of Speech and Hearing
centre
6. Child Guidance clinic (NIMHANS)
Deve1opment
1 . Visit to Astra
Mallur Health Cooperative
2. Visit to 1---Individual faculty
1.
2.
3.
4.
Dr .
Er .
Dr .
Mr .
----- and Homeopathy
Shirdi Prasad: Accupressure
1 Medic ino
Rorba
Joseph Chittoor:
Medicine
Ida : Ayurvedic
AK Roy: Heal th Caro Admin istrat ion
b 1 ack
67
DURATION OF COURSE
T„o oo-rso 1S or t-.rvo weeks dr.11 oTM,
This <?|~nduoted twice a
is of
weeks 8
and October,
year comonolnS every July
.u y an
rura| basad
institution based and four i—
weeks are 1
Is of two I vo weeks durat ion
Nolo: From 1093 onwards the course centre in Mugalur.
Only one
totally rural1 based in our training
in the month of October.
course will be
L held every year
those who
A two week Refresher course will bo hold for
involved
in
_ are aolively
have completed the basic course and
areas.
i____
This
Community Health and Development work in peripheral
be conducted in the month
— based and wi 1 1
course will also be rural
i
of July.
9
EVALUATION
Evaluation is conducted both
concurrently and terminally
evaluation through feedback sess ions
p-tauon.
and practical examination in First aid.
Terminal: Written, oral
the end of the course.
written examination at
---i in Eng Ii sh
writing their exam
The trainees who have difficulty in
__i
1 conducted
Evaluation is
^oaXWuegh ^e iTanTpa1;Uc" pVnTVva 1 uat ion af ter giving them the
expected answers.
1.
Wide
coverage of topics
with a
firm foundation
on basic concepts,thus
strengthening conceptual thinking.
2.
Problem based approach both during teaching and in.evaluation.
3.
Flexibility in schedule.
4.
Balance between field based and institutional based learning.
5.
Cordiality between staff and students very good.
6.
Trainers
are teachers
of
community health.
Most of
them
have had
experience in working in rural and backward areas.
7.
Involvement
of outside faculty
and other institutions
- especially for
developmental processes and Other systems of Medicine,provides for wider
coverage.
8.
Firm selection criteria.
9.
Relatively homogenous group of students, mostly religious.
10.
Evaluations during and after the course have been conducted and necessary
changes are
made after each course.
100
WEAKNESSES OF THE PROGRAMHE
1.
Too
2.
Not all trainers have been trained or exposed to problem based teaching
3.
Frequent changes in the time
learners.
4.
Field training has been
centre.
5.
Selection criteria has been relaxed in certain instances.
6.
Institutional visits have not been found useful to many.
7.
A chasm tends
8.
No system of follow up after training.
9.
No organised system of continuing education has been built up
many topics and hence skill based
knowledge oriented training.
training giving way
table has been
to
more
an expressed difficulty
dependent on availability of
of
the primary health
to divide the religious from, the lay leading to unhealthy
groupism within the class
10. No system of evaluation or indicators specified
to assess impact of the
community health workers services on the health status of the
community training.
No conditions have
(The community
what
health worker is
been laid down
as to the
often unsure where
she will go
type of work she will be involved in after training.)
1.
2.
WAYS IN_WHICH ATTITUDES ARE WigSEED
Providing information
Providing role models
3.
4.
Providing experience
Providing discussions following an event
5.
Role playing exercises.
status after
to or
Training of Auxiliary HeaLth_Worker
COURSE
FOR WHOM
IXJItATION
FREQUENCY
PLACE
12 weeks
twice a
year
8 weeks
Institution
4 weeks field
Field based
a) Community Health
Workers
X std Pass (basic
qualificat ion)
b) Anganwadi Workers
Training Program
(Karnataka State
Council for Child
Welfare)
Anganwadi workers
pre-placement &
in-service
twice a
month
c) Traditional Birth
Attendants (TBAs)
TBAs of our field
practice areas &
of NGO(s)
ongoifng
i) Contact Training
Programme
One day
field based
5 days
ii) Regular Training
Field based
d) Health Animators
Trg. Programme
Voluntary Workers
from Community
(NGOs)
ongoing
e) Health cum deve
lopment workers
training
Mahila vikas
on going
Field and
Institution
f) Training of Change
Agents
Mahila Vikas
ongoing
Field
/
Health Related Training Programs
COURSE
1) Health Management
Trg. Workshop
2)
Food Hygiene
Course
H)R WHOM
DURATION
HWIJUENCY
PLACE
Field based
(Plantations)
Managers in the
Plantations under UPASI
1) Hotel Managers &
&, Supervisors
10 days
on request
Institution
based
ii) Cooks & Servers
5 days
on request
Field based
(hotels)
Once a
Field based
3)
Teacher’s Trg.
Program
Rural School Teachers
One day
4‘
Trg. Program on
1) Deacons,Sem1nar i ans
First Aid,Personal 2) (NGOs)
Hygiene,Home
3) Plantation Staff
Nursing,Managemen t
of Common ailments
one week
On request
Institution
based
1 day
twice a
Field based
(factory)
5 days
ongoing
Institution/
field based
5) Trg. in Occupational 1) Small Scale
Industries
Health (detection of
occupational hazards
their prevention &
control)
month
6) Natural Family
Planning Courses
- Medical .& Nursing
students
- Community Health
Workers
- Health Animators
7) ChiId-to-chiId
ealth Education
Programs
students/school teachers/
NGO
ongoing
field based
8) Group Motivation
Programme for
Parents of Spastic
Parents of Spastics
chiIdren
ongoing
Field based
Training in Public
Health Laboratory
Techniques
Plantation Nurses/
Compounders
ongoing
Plantations
chiIdren
9)
Co m
DEPT. OF PREVENTIVE & -SOCIAL MEDICINE
ST.JOHN’S MEDICAL COLLEGE?BANGALORE-34
Inst ruct ions..AQ.. An^-ST-D-S
1. Consumption of alcoholic beverages while the interns are posted
for training to field health centres, is ^^ctJyj^hAbiLed3
2. The interns should not leave the health centre before 4.00 P.P1on .Friday to attend Interns’ Meeting on Saturdays, and they
will be back at their post (Rural Health Centre) On Sunda \
night latest.
3.
It is reported by the medical officer that the ante-*natal cards,
under—five clinic cards which are supplied at considerable cost
and difficulty are being misused and wasted. The interns are
requested not to indulge in such-.wasteful activitias.
COMPULSORY ROTATING INTERNSHIP IN PREV & SOC MEDs OBJECTIVES 2
1. To give practical training to medical graduates in the administrative,
preventive, promotive and clinical aspects of integrated health service in
rural/urban areas.
2. To orient an intern to the social effects of- illness; on an individual
and family, and the lrole
----- of
-------socio-economic factors in the causation of
health and disease.
3.
orient an i*teir in the social dynamics of a community including
dynamics of load01%hip, the motivation of a ^WTmunity and the vaiiuu*.
important factors of influencing loadeif. in the promotion/acceptance
of health programmes.
4. To orient an intern in the organisation and management of a comprehensive
health service for a community including environmental sanitation,
immunization, health education and specific care of vulnerable groups.
5. To orient an intern to the concept of team work with para medical health
workers.
6. To orient an intern to the working of the national health programmes at
the primary health centro/village levels.
7. To expose the students to the role of voluntary agencies and other
Government agencies in the promotion of health and welfare of the people.
PHOGR.WIE COMPONENTS
1. Participation in the preventive, promotivc and curative services of a
rural/urban health centre.
2. Participation in the activities of all categories of field staff in
primary health centre
3. Planning and undertaking of a community survey or an epidemiological
project in the community
4. Planning and participation in an immunization and health education
p rogramme.
ALLOCATION
a
h
/ C -1 E
s 2 s
Urban posting — 4 weeks — National Tuberculosis Institute
1 week
- City Family Planning Bureau
2 weeks
- Action Gpoup/Student Health Service - 1 week
Optional - Plantation Health Service - 4r6 weeks
REPORTS
A
- from medical officer of health centre
i.attendance report
ii.Confidential report on conduct, attitude, mot ivation
special aptitudes and quality of work done.
0 - from intern
i* report of service responsibilities
ii. report of community survey/epidemiological project
iii# diary of weeks posting in primary health centre
<
"pEPAP.TxMENT OF PREVENTIVE AMD SOCIAL MEDICINE
I
St. John1s Medical College
Internship objectives expressed as specific knowledge,
skulls and attitudes to be learnt by each intern during 3 months
posting in Rural Urban areas#
Knowledge
1. Knowledge about community, environment and
diseases with health problems. Role of individual
members in the community.
2. Knowledge about political structure and community
^ealth set ups at local, block, district,
state, national and international levels#
Orientation of administrative set up for all
National Health Programmes.
3 • Knowledge about community development and
welfare agencies and their respective roles in
relation to agriculture and health programmes#
4. Knowledge about functions of Primary Health
Centres and national health programmes, keeping
adequate statistical records and interpretations
of Health Indices.
5# Knowledge about Social dynamics of the community,
socio economic, literacy, culture 1, geographical
and communication aspects of rural areas
especially in his region of work - Dynamics
of leadership, motivation of community in health
activities.
6. Knowledge about diagnosis and management of
c.ommunicable, nutritional and other common
diseases.
7< Concept of team work and knowledge of roles
of various paramedical workers.
8. Basic knowledge of health administration including
management techniques like cost/effectiveness,
personnel management, etc.
9. Administrative aspects of running the Primary
Health Centre - Purcahse of drugs, basic equipments,
■ cost of diet - utilisation of allotted budget
to the best advantage.
10. Meet villagers, participate in village committee
meetings (atleast health committee) and
participation# Role of village teacher and
village level workers and getting familiar’ with
other village development activities#
- 2 i)
ii)
iii)
iv)
v)
vl)
Case detection
notification
Surveillance
Contact tracing
Immunization
Concurrent and terminal disinfection.
2. -Practical measures for environmental sanitation
i)
ii)
iii)
iv)
Chlorination of drinking well Waiter
Construction of sanitary latrines
Soakago pits
Other simple methods of wastes and sulla-.e disposal.
3. Participation in the implementation of National
Programmes at the Village Level.
i)
ii)
iii)
'iv)
v)
vi)
Small pox eradication programme
Malaria eradication programme
Applied Nutrition programme
T.B. Control
Family Planning
0ther programmes.
4. Participation and organisation of health education
programme.
i) Health talks to groups of villages with aid of
flash curds, flip charts, flannel graph, slides;
films.
5. Participation in Maternal Child Health and school health
services.
i)
ii)
iii)
iv)
v)
Antenatal check ups
Domiciliary midwifery
Post hatai
Under 5 clinics
School Health Examinations.
6. Participation in organisation and impl^ment^xo^mass campaigns.
i) Mars immunization
Sterilisation camps
iii) Eye camps
iv) Sp . cialist' camps
ii‘
7. Compilation, analysis and interpretation of health and
disease data.
S. Particij^ation in adiriinistrrtivo activities of s. health centre.
i) Planning of work
ii) Analysis of Records
iii Meetings of health team (Weekly and monthly meetings of
Staff at Primary Health Centres and at College)
3
^QtTrpQaeptsj.- (action oriented)
A. Participation in community health programmes 6f centre
4•
1. ^munazation:- administration and foiled up of
a) Small pox — at least 5 vaccinations
b) Triple antigen - at least 15 imnrunizations
c) Tetanus toxoid - 10 doses
d) BCG, TAB, Cholera, as many as possible during mass programmes.
2. Maternal Child Health;a) .. Antenatal check'up (at least 10 cases
b) Domiciliary deliveries (at least . 3)
it
c) post natal check up of (b)
d) Under 9 clinic - (at least 100 children with complete follow
up of 11nd and 111rd degree malnutrition *ases)
e) Health examination of school children. "
3- Environmental Sanita4'ion:a) Chlorination of wells (at least 5)
b) Supervision of construction of sanitary .latrines and
Soakage pits (at least one each) •
4- Curative work
a) Attending out patient clinic
b) Stool examination of at least 5 cases
c) Urine examination of at least 5 cases
d) Blood/sputum investigations whenever indicated.
5• Social case history tsking
At least
Medico Social cas" histories may be obtained
6* Health Education
a) At least one health talk wi^h Audio Visual Aids.
b) Organisation of 1 film show/mass media programme.
(y) Family Planning Work:z
zra) Motivation and follow up of atl ast 2 couples in the use of
contraceptives.
<
- 4B. Parti»ipation in the activities of the following categories
•f health linkers (at least 1 day each).
a) Medical officers of health centre
b) Public Health Nurse/Health Visitor
c) Auxiliary Nurse lidwife
«i) Extension educator
e) Basic Health Workers
c. Planning Organisation, Execution and reportisfc of at least
x.++•+ j
*n® C0Bnnunity s^vey/epidemiological investiyitiorArowledfo,
attitude & Practice .stu^y and reporti.ng of the same dji the accepted scientific
paper.format. (Summary, Introduction, objectives,
materials and methods, observations and results, conclusions
discussions suggestions or recommend'tions acknowledgements
’references)
J , ZvkVWvWlA'■
/
2
Wl
^Vv'v'VvOVv SAA/l/vt’/-'
4■$.
V'Otrk.
CvW WvSfo-(?/■
7
Pu^vwvwj
:4:
4.
COMPULSORY ROTATING TNTEPJ\iSHTP-qiJRAT. TWINING
\
Im is essential to outline the objectives that are
to be achieved, during the 3 months rural stay during internship
period. An outline of the objectives to be achieved ip suggested.
a ) Administrative aspects
b<, Preventive aspects
c) Clinical aspect’s
a)
:
1) Under administrative aspects, rural internship should
serve to orient the student in the political1
structure and acirninistration of a rural areas,
and in the actual working of those organisations
concerned with local self government namely,
zila parishaos, ths panchsyat samities and"other
facts of community development work.
2) It should serve to orient the intern with the'
concept of team work with para medical health workers
namely, the health visitor, the vaccinator, the
sanitary inspector, the social scientist and the
health educator, especially in connection with
national health programmes.
J
3) It should orient the intern in the socldl._-d^rnaiiiXc^.._oi
a community. This has an important bearing in '
health work. This should include the dynamics of
of a community and the
leadership, the motivation
’’-..-fa
various important factors of inf luencing ' leac.ers
in the oromotion of health programmes. This is an
integral part of the application of health eduction ■
principles in the promotion of development vj^rk.
4) It should serve to orient the doctors on the
administrative aspects of various national health.. programmes
whic ■;; are ani integral part of work at primary health c^nt're^^^
such
These should primarily be
.
-g programmes as:
■ x
/
a) the malaria eradication programme
b) small pox eradiation programme
c ) tuberculosis
' ’
"
control_
d ) family planning
e ) certain specific communicable o is eases,' sjch as
filaria, leprosy, trachoma, V.D. etc.
r
-
— — — -w— —
A. SZ s J 4.
i
5) It would serve to put the health proqramm.9s
in the
perspective of the overall national develooment programmes,
namely, agriculture, education, social welfare etc.
B) PREVENTIVE ASPECTS:
1) It should serve- to orient the intern in the organisation'
and.management of a comprehensive health service for a
community. This programme should invariably include the
environment of the community.
2) It should se-ve bo orient the intern in the'Nrole of
individual members of the health team and o f impoqru a nt
community.
leaders in
i♦
:5:
4) It would serve to orient the doctor 'towards the effective
utilisation of all resources in the community for promotion of
health programmes,
5)
It would serve to indicate that .'illness is an episode in
total frame work of an individual’s health. The need for
adequate contact tracing and follow up of sick patients after
therapeutic treatment should be demonstrated to the maximum in
a rural community.
■’ -
it-..
6) It should^give an indication of the priority needed of various
facts, of health prgrammes, such as’the importance of
immunization of nutritional education, care of’ the pre-school
child etc.
7} The social effects of illness on an individual and family,
and the result of socio-economic factors in causing illness
should be demonstrated.
‘
8) The planning and evaluation of a community health service.
c) CLlfliCAL, ASPECTS
1
1) It should
sharpen an individual!
----v
f s diagnostic capacity, so that'
he may be able to make use of his individual senses'"witlicLU'L/ ’
dependence on expensive aids,
=>4 z-j? such as laboratox^’^ X-ray etc.
2) It should permit of an :individual taking responsibilityz for
minor illnesses and surgical complications
3) It should serve to indicate his limitations and realization
of when to call for consultative services or a referral. /
The methods by which this could be achieved
i
1) A planned programme in order that all students should
have an opportunity to meet with village representatives
•and to participate in village meetings“ especially rhose
of the health committee. In order to effectiveLv demonstrate
the role of community leaders in a health programme,
it should be the duty and responsibility of the staff of the
rural field centre to form a health committee in every
rural field training area.
2) The role of other officials in the village, namely the
teacher, the village level worker etc, should also be
demonstrated and the students should be given ar.
opportunity to meet with the block development officers
and his staff, and to become familiar with the ether
development programmes in the village.
3) Every effort be made to ensure that the hostels and
the houses of the staff of the health centre, as well as
well as the surroundings of the centre itself should be
such that minimum facilities, such as protected and
safe water latrine etc, are provided. Wherever possible
the students should be made to live in the village^ but
under hygienic conditions which are capable of reproduction
by the villager.
I
:6:
5) It should be ensured, that the q?rimary~hea-lth ce'ntre"'is '
supplied with adequate vaccines and sera and- modern drugs.’"’
6) The administrative aspects of running a primary health
centre should be demonstrated to the students, and they may
be allowed to make sujiestions in such matters, as the
purchase.of drugs, the type of basic equipment, the cost
of the diet etc, and how the Centre funds could best be
utilised.
7) The students should have every dnportunity of working with*
the health centre staff ano visiting the homes. The
principles of.health education ano the approach to a community,
and of an individual should also be effectively demonstrated
to them and the students be required to practise this under
skilled supervision.
8) To effectively implement the above requirements the staff
of the field training area be adequate in number, be
properly trained, and have the facilities to undertake the
teaching andtraining that are required.
(A true extract from the Medical Council of India letter
No. MCI«-9(5)/7O-Med/583-xiated 1<4.71)
com H fo n
4
CURRICULUM ON SOCIAL 8. PREVENTIVE MEDICINE FOR UNDERGRADUATE
TRAINING
■■ . r
------r
_
_
„ - -
SUMMARY
W I 1—.W1 rw TM ■ ■
—-n
a ) The teaching of Social & Preventive Medicine shot Id take
place throughout the teaching period.
b) During the pre-clinical period, a minimum of 50 hours be
devoted to the teaching of social & Preventive Medicine.
period, about 250 hours be devoted to the
c) In the clinical period
teaching of the subject. The detailes are included in the
report.
d) During the students attendance at various departments, which
is now required under medicine and surgery, such as infect
ious diseases, T.B.? Leprosy, V.D. etc., emphasis should be
laid as mbch on the preventive as on the clinical ano therapeu
tic aspects of these diseases.
e) In addition to the teaching undertaken by the departments
of Social & Preventive Medicine, a joint programme with
other departments is essential in orcer to give the students a
comprehensive picture of man, his health and illness.
f) Stress be laid on national programmes, inc.ludinq those of
control of communicable diseases and family planning and
he 1th education.
g) A separate examination in Social & Preventive Medicine may
be undertaken in the 2nd professional examination. Questions
on the preventive and social aspects of diseases should also be
included in the examination in clinical subjects at the final
M.B.B.S.
h) An epidemiological unit as an integral part of every hosoital
in order to achieve a (comprehensive study of disease by the
students shouldbe established.
i) The objectives of the internship should be clearly defined
and that a proper training programme be oriented for this P
period. Objectives, and the methods by which the internship
could be made into a much more satisfying and fruitful
experience than at present have been laid. down. This is one of
the weakest links of the teaching programme and there is an
urgent need for sharpening and for planning in this phase of
education.
j) As regards the qualifications of the teachers, it is highly
1 important that all teachers in Social & Preventive Afedicine
should have as far as possible had adequate administrative
experience in addition to the teaching experience.
The following are the recommendations of the Council:
UNDERGRADUATE OR M.B.B.S. COURSE
CURRICULUM
1.
PRE-CLIMICAL
a. The present educational system requires those students
intending to undertake medical studies to chose the science
group of subjects. In order to prepare the student for
A
•y •
Medicine^th™ SeSunical
deV°ted fo? S^^l & Preventive
f1 Penod- The following subjects
should form a. part oj-. ^2
.he teaching in this discipline:
Personal Hygiene
iP
Bio-statistics and vital statistics
iii j
Human Ecology
iv) Elementary psychology
v) Elementary social science
vi) Normal growth and development
vii) Nutrition and dietetics.
A number of these items could be undertaken in collaboration with
the departments of physiology/ and bio-chemistry, and should
form integral part of their teaching.
c) The teaching of Social 8. Preventive Medicine should be
undertaken by the department of Social 8. Preventive Medicine in
coordination with other departments.
2. CLINICAL
a) A ccourse of systematic
i
instructions iin.the principles and
practices
of
social
4-i—
i
, ,,
--- & r-preventive
-1- v ■-11 vc? medicine which should pyionH
throughout the whole period of study.
a + +obThere ?h?ulx be aminimum of 250 hours in total
for
nhridv"«®+Of lectures> demonstrations, seminars, conferences
’
field visits and practicals durinc the clinical period!
The following subjects should be included in the teaching programme
M!dil!nt-tf^iS'ti^Syin-1Uding collection, tabulation,
ES oftsta + ?J1?d ^he i^^P^ation of data-, and the
use oi statistics! methods
EocJEoati^al and1 — ”
raan and his environment,
occupational and industrial hygiene, village and
foo™ hygxvn^0"'
-K, “od a„d
iii) Parasitology, helminthology and entomology in relation
to communicable diseases, their prevention and control.
iv) Principles of epidemiology
v) Communicable diseases , their prevention and control
Vi) Public Health Administration ,including the requirements of
international health, social security, public health law,
•and the role international
oral ,ano other health, organisations.
vii) Advanced courses on nutritional deficiencies.
vin) Community Medicine Teaching should include clinico
sociopathologica! conferences with other departments, maternal
and chile, health the care of mothers and infants including
anTvisits1'11'11”9 3nd Sch°o1 heaitK,.supervised field study
Lh -
c ?)■ In order
luhat the discipline of Social & Pr^Vfrtive
Order that
:3:
d) To study disease in a comprehensive manner,
manner, it is
essential that an epidemiological unit be set up in the out
patient department of the teaching hospital. Such an epidemiological
unit will enable the students to understand the social, economic
and,environmental factors in relation to illness during his
training period.
e) During the,students attendance at the specialist
departments, instruction in the preventive aspects should be
emphasised during the study.
i) Acute infectious diseases anc other local endemic
diseases, for example, trachoma goitre, filariasis etc.
iiJ Tuberculosis
iii) Preventive a specie of psychological medicine and
psychiatry
iv) Preventive aspects of leprosy
v)
/
V.D. Control
Vi) Preventive aspects of dietetics and Nutrition
information on all national health programmes and the
role of international health corganization should be
given in order that the medical^graduate*
participate in the successful implementation of these
schemes during his career after graduation.
4.
?n 0]rcier to make the students practise what is beinq
L+
caught, it is absolutely necessary that the hospital where he works
and the hostel he resides should be ga. model of sanitation. To
uhis extent, he should be involved along with the professors
- > of
the various diciplines of the hos i cal, ' and
aild uoh^.L
authorities
other duuio
concerned, to take a keen interest in the environmental
- — ■ —*. sanitation.
g) Principles of health educ tion including the education
(of hospital and health staff,
patients and their relatives within
the hospitals.
h) The medical students should be given demo stration of
family planning at a family planning centre attach to the medical
college or at a recognised health centre during the regular course
for,undergraouate training either under the department of
obstetrics and gynaecology or Social & Preventive Medicine, The
concept of family planning and population control should be
emphasised by all disciplines.
Every student should be required to submit one
sa .is-i actory writeen history of a community health survey undertaxten.unoer the guidance of staff of the Social & Preventive
Medicine^in a rural are , and o e written case history of a
patient rollowed up with the assistance of the epidemiological
unit,,m coordination with the department of social and preventive
o o. zl c i o >
3.
EXAMINAT'IONS :
be a separate university examination
a) There should
.
:4:
4.
COMPULSORY ROTATING IMTERNSfflIP-RURAL TWINING
It is essential to outline the objectives that areto be achieved, during the 3 months rural stay during internship
period. An outline of the objectives to be achieved i.s suggested.
a) Administrative aspects
b) Preventive aspects
c) Clinical aspects
a) A^gNISTJ^TJV^
:
1) Under administrative aspects, rural internship should
serve to orient the student in the political
structure and administration of a rural areas,
and in the actual working of those organisations
concerned with local self government namely,
zila parisha,:• s , the panchayat sanities and other
facts of community development work.
2) It should serve to orient the intern with the'
concept of team work with para medical health workers
namely, the health visitor, the vaccinator, the
sanitary inspector, the social scientist and the
health educator, especially in connection with
national health programmes.
3) It should orient the intern in the sociaJ-d^/T^mj_Gs_of
/
a community. This has an important bearing, in
health work. This should include the dynamics of/
leadership, the motivation of a community and t/ie
V
various important factors of influencing leaders
in the promotion of health programmes. This is an
integral part of the application of health education
principles in the promotion of development work.
4) It should serve to orient the doctors on the
administrative aspects of various national health programmes
whic ; are an integral part of work at primary health cent'res^^
These should primarily be such programmes as:
/
a) the malaria eradication programme
b) small pox eradication programme
c> tuberculosis control
d f a mi1y p1a nni ng
e certain specific communicable diseases, such as
filaria, leprosy, trachoma, V.D. etc.
/
5) It would serve to put the health programmes in the
perspective of the overall national development programmes,
namely, agriculture, education, social welfare etc.
B>
YEHLTXA...ASPKQZS1
1) It should serve- to orient the intern in the organisation
and management of a comprehensive health service for a
community. This programme should invariably include the
environment of the community.
\
I
:5:
4) It would serve to orient the doctor -bvards the effective
utilisation of all resources in the community for promotion of
health programmes.
It would serve to indicate that/illness is an episode in
total frame work of an individual’s health. The need for
adequate contact tracing and follow up of sick patients after
therapeutic treatment should be demonstrated to the maximum in
a rural community.
5)
6) It should give an indication of the priority needed of various
facts of health prorammes,. such as the importance of
immunization of nutritional education, care of the pre-school
child etc. •
7) The social effects of illness on an individual and family,
and the result of socio-economic factors in causing illness
should, be demonstrated.
8) The jianning and evaluation of a community health service.
: • IT: .
1
C) CLBvICAL ASPECTS
1) It should sharpen an individual’s diagnostic capacity, so that
he may be able to make use of his individual senses "wittion'L.^ ‘
dependence on. expensive aids, such as laboratory-. X-ray etc.
2) It should permit of■ an individual taking responsibility for
minor illnesses and surgical complications
3) It should serve to indicate his limitations and realizatiop
of when to call for consultative services or a referral. !
The methods by which this could be achieved
1) A planned programme in order that all students should
have an opportunity to meet with village representatives
and to participate in village meetings, especially those
of the health committee. In order to effectively demonstrate
the role of community leaders in a health programing,
it should be the duty and responsibility of the styaff of the
rural field centre to form a health committee in ^very
rural field training area.
/
2) The role of other officials in the village, namely the
teacher, the village level v^orker etc, should, also be
demonstrated and the students should be given an
opportunity to meet with the block development Officers
and his staff, and to become familiar with the b.ther
development programmes in the village.
n
3) Every effort be made to ensure that the hostels and
the houses of the staff of the health centre, aS well as
well as the surroundings of the centre itself should be
such that minimum facilities, such as protected and
safe water latrine etc, are provided. Wherever possible
the students should be made to live in the village^ but '
under hygienic conditions which are capable of reproduction
by the villager.
:6:
f
*5) It should be ensured, that the primary-health centre*''!s
• supplied with adequate vaccines and sera and- modern drugs.
6) The administrative aspects of running a primary health
centre should be demonstrated to the students, and they may
be allowed to make suggestions in such matters, as.the
purchase of drugs, the type of basic equipment, the cost
of the diet etc, and how the Centre funds could best be
utilised.
7) The students should have every opportunity of working with
the health centre staff and visiting the homes. The
principles of health education and the approach to a community,
and of an individual should also be effectively demonstrated
tothem and the students be required to practise this under
skilled supervision.
8) To effectively implement the above requirements the staff
of the field training area be adequate in number, be
properly trained, and have the facilities to undertake the
teaching andtraining that are required.
(A true extract from the Medical Council of India letter
No. MCI-9(5)/70-Med/583-<jated 1.4.71)
H
•--l
.a— ii ■ »i-i« nnr— in—mt>t
rural i nt er ns hip'
Health Cent re
Tn. order to help you understand the working of a Government
Primary Health Centre, a work—sheet has been designed to be
used during your posting. The questions and comments are to
ne used as guidelines.
1.
ORGANISATION
FUNCTIONS
DIRECTOR OF HEALTH & FP SERVICSS
t
Policy, Administration
and control
DIST HEALTH 8. FP
OFFICER
....Administration, Supervision
and control
I
f
r
...I
5
MEDICAL OFFICER
OF HEALTH
!
L.M.O.-
j -----M.O»H
Administrative head, super
vision A control responsible
for all tne work turned out
in the PHC area
(Trng)
Health Inspector-------- Health Visitor—Extn. Educator-J-Clerical stafT
!
1
Basic Health
Workers
1
'
[
/) ------A.N.M.
i
!
J
F.P. Health Assist. (■<
’ 2- SSSiS^Health^Service^rendgrod^in^the^Primary^Heclth Centre
2. MCH and FP
3. Control of
1. Medical Care
Communicable Disease. 4. Vital Statistics, 5. Environmental
sanitation, 6. Health Eoucc.tion, 7. School Health Service,
d. Na t i o n a 1 H e a 11 h P ro g ra m m o s
Duties and Responsibilities:
Write down the responsibilities and activities of each staff
!*
bv talking to them: .
1. /Medical Officer of Health
2. Medical Officer of Health (Training)
3. Lady Medical Officer
4. Health Visitor
IO- r2_Q
1
-26. Extention Educator
7. Family Planning Hejlth Assistant
•<
8. Aux . Nurse Mid-wife ’
9. Basic Health Worker
4. LIST THE REPORTS THAT ARE SENT EVER- ’MONTH FROM TH.”
PHC TO THS
DHO.
1.
2.
3.
4.
5. List the Registers maintained in th
they serve.
P.H.C; and what purpose
6. * NAT TONAL HEALTH PROCRai MME : (outline the work done in the PHC
in each of the following )■-
1. N g E P:
2. N S E P:
Apolied Nutritional Programme
4. Tuberculosis Control Programme
5, Leprosy: Control Programme
6. Family Planning Programme
7. Give suggestions to improve the quantity and quality of
nealtn work taking into account the difficulties and problems
encountered m the villages.
DEPT. OF PREVENTIVE & SOCIAL MEDICINE
ST. SOHN’S MEDICAL COLLEGE, BANGALORE
Date*
PSIVIPR/76
To®
At the end of your rural posting at
Mallur/ Sil.Pura/uttarahally
you are required to submit a report on the work/survey done
during your posting.
The report should be prepared on rhe
following lines*
1. Short Summary of Project. 2.
Introduction;
3. Material
(subjects, patients) and methods; 4. Results/Observation
5. Discussion;
6. Conclusion;
7; Acknowledgement; &
8. Reference.
The report should, at first, be submitted to the Medical
Officer concerned and after perusal by him/her, with
his/her
signature on the report, the report should reach the Dept, of
Preventive and Social Medicine, within one week after the
date of relief at the Centre, fai'lin'gwhich the confidential report of
tho
; concerned intern, will not only be withheld but is
likely to be forwarded with remarks that the intern s
work
was . not up to the mark.
,NPH- J
(DR.S.V.RANA RAO^BBS'.'
for Prof. & Head of the Dept, of
Preventive & Social Medicine
WARTMBNT OF PREVENT ITO & SOCIAL MEDICINE
ST. JOHN'S MEDICAL- COLLEGE, BANGALORE - 34
Intern1s Attendance Form
Name of Centre
posted:
i
Name of Sister-in-charge/Medical Officer:
1. Name of intern:
Day
2. Date of commencement of posting:
Month
Year
3* Last date of posting:
1.
2
17
3
IS
4
19
5
20
6.
21
7
22
8-
23
9
24
10.
25
11
26
12
27
13
28
14
29
15
30
16 •
31
Signature
Medical Officer/Sister-in-charge
(Please return in a sealed cover on completion of posting addressed
to the Professor, Dept, of Preventive & Social Medicine, St. John's
Medical College, Bangalore.560034j
,
APPLICATION..!
1
PART I:
Date:
Unit:
Reasons
.
Name of Intern:
Department:
Period of leave: From. ♦•••••••
(Total no. of days:
Sundays & Holidays, if any,
$
proposed to he prefixed/suffixed 0
to leave (with dates)
2
)
Prefixed
Suffixed
Unit/pepartment.. >
Remarks?, fro .
2. Internship Coordinator....
5. Dean for sanction
Signature
_
INTERN
Pate:
MO
P;\RT II
4
is
Shri/Smt .
casual leave requested for from
is sanctioned subject to the following:-
hereby informed that special
-fco
....(inclusive)
■wr
h
c
duty.
internship co-ordinator
PART III
(Applicant may please detach this joinigto the office on the expiry of leave).
To:
report for completion and return
The Dean,
Through the Head of the Department of
Dear Sir,
After the expiry of my leave from
I have rejoined duty this day the.
to
Yours faithfully,
Si^xnature
To
The Internship Coordinator,
The above mentioned intern may rejoin his duties.
Oo <v) H / $ • 7-V
. Titles
COmUNITY HEALTH AND ST. JOHN’S.
The Department of C»mmunity Medicine at St. John's has always
played the pivotal role in fulfilling the most important objectives
5
•f the college.
Serving the under privileged and more importantly
training others to serve the underprivileged has been the main focus
■f the Department.
The enabling process of identifying and attempt-
ing to meet the felt needs of the community 9 is done by the Dep^artment •
The training and service components are provided to all-.members
• f the health tea..! (from the grass-root level workers to t.eriiary
i^ar e specialists).
TRAINING FOR COMMUNITY HEALTH CARE?
Being a Medical College1? St
John’s is in a unique position tn;4
provide all the training ctmponents in the formation of a Health
tear.
Thi*, creates a better understanding of each member’s role
in Community Health Care rather than a isolated form of training t»
separate Health Team Members in separate institutions.
The various
Training programmes in Community Health are as follows:r
1.
Frtr Medical Students:-
a) Rural Orientation Programmes- Conducted every year 9 during the
months of January - February? the main objective of the camp is to
expose the medical studeats to the various facets of rural liFe
through a residential progiamme at Dommasandra Primary Health Centre.
The students visit all the rural subcentres and are guided in deter■nining the various factors which govern rural life such as
Agr iculture 9 Animal Husbandary? Snail Scale Industries^ Fairs 9
Festivals 9 Customs and traditions, Commerce and trade, Transport 9
Traditional systems of Health 9 Housing and environment, Role of
women in society? Maternal care practices 9 Child Care practices and
Food practices.
These are presented in the form of field projects
by groups of students.
In addition 9 the students also organise many
r
2
b) Clinico Sicial Case uork for HBBS Students;-
This is conducted
every month, by posting them in batdhes to the health centres.
Their
training involves case work in the field, working up the social aspects
nf a number «f communicable diseases as well as antenatal cases.
The
©bjective is to train the students to cons'ider a case as a holistic
health care problem rather than a mere clinical entity.
The socio
economic causes, contributing factors and consequences of major diseases are highlighted in this training programme in addition to the
usual clinical features of the disease.
c) National Secial Services in rural villages: -
Under this scheme,
the medical stuoents carry out community health
and developmental
projects at
various villages in batches once a week.
t« the generally known NSS activities,.
In contrast
the NSS programme of this
institutian aims at highlighting community health and community development, as the main features of this service •
Education for school
i
*
children, adult education, school health education, improving environmental health etc., are some ^f the main components of this programme.
d) Child to Child health1 education programme:
Evolved as a novel
approach tR health education, this programme has proved to be an
immense success at D^mmasandra, Anekal and Bidadi health centres.
The basic objectives is to teach groups of children.
various aspects
of health, using innovative teaching materials, live demonstrations
and ’’health sings’1
Later the children are allowed to share their
knowledge with each other atid each ch’ild is encouraged to tell* the
•ther what he er she saw in her/his group teaching.
This way the
factor of curiosity and natural thirst for knowledge and sharing the
same, are invoked in each of the children.
This greatly contributes
to strengthening the health education in a natural cumulative manner
from child to child.
At each rural centre, the major middle and high
s c hbo1 are covered under this programme.
The positive aspect t)f this
:
3
:
Motivation Programmes Groups of rural mothers are invited
e
to the rural subcentres and they are made aware of various facets of
nutrition 9 maternal care 9 child care
9 immunization etc.. The Programme
is conducted in the form of
1
practical nutrition demonstration 9 immunization procedures} infant feeding techniques
, preparation of weaning
diets etc.
Emphasis is laid on the fact that all' the components of
this programme must be dnne through practical demonstrations
9
using
locally available resources only
anly,9 with the mothers themselves actually
executing the work. Lmphasis is also stressed
on the cost factor during
these demonstrations.
e
f) Field uprk in urban siums:-
Senior clinical students visit families
and maintain family health records, 'enumerate eligibles for immunisation
^immunization coverage, refer to the St. John's Hospital those in '
also ccarry
4 nNutriti^n,
.
need of medical services and also
.. x /V* •
a r r v nn+- FioiH
out field surveys in
child health etc.
■' r
g) Seminars, discussions and Lectures;-
*
Over. 4 00 hours are spqrit in
teaching community Health tn medical students during their entire
HBBS training period.
All the subjects from concepts in Health care,
to Nutrition 9 Maternal and Child
9 Occupational diseases, sta
tistics , sociology 9 Behavioural sciences H
ealth Management and
s
Planning, control of CRmmunicable and
non-communicable diseases etc.
n
are. taught to the medical students.
h)Study tours to
ther Health related I nstitutionsS — In an effort to
expose our students to real life situations 9 they are taken to various
health institutes 9 field projects and institutions of public health
importance.
^er e they get a chance to interact with other Health
agencies and their staff and actual field problems in health care. n
I
«
4
c
2* F*r Nursing Students:
a) Rural Orientation Programme for Nursing Students:- Conducted every
year during the month of May, the main objective of this camp remains
t^e same as that for medical students.
The camp is conducted at
Bidadi Primary Health Centre and the rural Mobile Clinic stationed
therein is used extensively during the programme,
In addition to
theactivities^refered to in the medical students camp, the Nursing
students are given extra assignments in the field of Maternal and
child care ,
•
etc.
□ miciliary deliveries
n
r!-'
3. For Community Health Workers:■Rural Training programme for Community Health Workers 2 - This course
3-3 3 three monthsprogramme,9 conducted twice a year, during which on
©anth^A.s spent,..ae/a rural residential camp.
The ..emphasis during this
cource is on various field, cl in ical, Lab and institutional training
e*
!■ the various aspects of community health. Additional training in
first aid, home nursing, natural family planning, Herbal medicine,
counselling, community development and human biology are also conducted.
The rural posting comprises mainly of various field projects
on the dynamics of rural life, rural Mobile clinic work, domiciliary
deliveries, maternal and child health, school health etc.
Rural
projects planning and management of health centres is also taught
to the community health workers.
As of the current 20th basic course
for Community Health Workers, a total of 355 community health workers
from every state in India and also from Nepal have been successfully
trained.
Interns:
4.
rr
Rural Internship training programme:-
All Interns in hatches 9 are
posted to the six rural subcentres for a period of three months dura
tion each.
Apart from managing the rural clinic, these interns are
also involved in epidemiological surveys, domiciliary visits, domici
liary deliveries?immunization and school health.
Bes ides, they parti
5
They have successfully participated in field evaluation surveys for
immunization coverage, in remote villages in a number of districts
in Karnataka.
5 • Training programmes for Deaco n s y Seminar ians and others;;»
Being basically a training institute 9 a large number of small organ!Nations are constantly availing the facilities for training their
•wn health workers.
This programme is arranged on individual request
basis with the theme of the training being highly specific to the
■eed of that organisation.
Many of these programmes are j_in the form
of work experience in our ongoing rural programmes.
Some of the
programmes, however, are formal month long structured training programme s•
The Deacons and Seminarians from St. Peter’s Seminaty, Suvidya
Colleg e, Deena Seva Ashram, Workers from Association of Physically
handicapped and several other Government and Non-governmental agencies 9
undergo these coursesin Community Health Bcmducted by the Department.
6• food Hygiene Training Programme:-
Keeping in view the importance
of Food Hygiene in Public Eating Places 9 this training programme aims
at providing appropriate knowledg e and methodology of safe food keeping ti Hotel Managers 9 cooks and Servers,
This ’.s a monthly programme
conducted at the Hotel premises itself in the local language so that
the programme is highly effectiva.
The topics of food hygiene are
especially selected to reflect Indian foods and indigenous techniques
of food preparations.
7 • Plantation Health Services:-
Under the aegis of the United Planters
Association of South India and the Department of Community 1Viedic ink,
a series of training programmes, collaboration research and service
Programmes are undertaken throughout the year for the plantation
workers 9 Doctors, Managers and Lab Technicians of the Tea, Rubber,
Coffee plantation of South India.
Elective clinical training for
2
6
o
training of plantation creche attandants are some of the major areas
of involvement of our institution.
The main objective is to provide
adequate community Health care to the workers of the plantation nommunity in South India.
8 • Rnral School Health Programme2 -
Under this programme ail the rural
middle and high school teachers of Anekal Taluk are trained in the
various facets of school health.
is to train rural
The main objectives .3f this training
school teachers in basic health care, early detection
ion of illness in children 9 immunization and health education.
Follbu
up of this! programme has revealed that ths school teachefs have succfessfolly organised regular teaching programmes in health (for their school
children.
In addition. some of the senior school children have been7
trained to supervise healthy practices, environmental cleanliness etc.
Thus the responsibility for health is transferred to the school child.
Periodical school health surveys and health camps in the specialised
areas of ENT, Ophthalmology, Dentistry and Surgery are carried out by
the clinical faculty of the concerned departments of the Hospital.
Thase clinical faculty participate in these rural programme regularly.
• For the students of Diploma in Hospital Administration:- Apart from
severals hours of didactic teaching in Community Health, these students
are posted to our rural health training centres and other field health
programmes of the department.
They also carry out Health Management
projects with the guidance of the departmental faculty.
10• Colloquim for doctors and Commnnity Health Workers working in
rural areas:-
In addition to basic training in health care to various
categories of health workers, it is important that a follow up is done
on the utilisation of the knowledge gained.
methods are followed.
For this purpose, several
At the professional level 9 doctors can seek
elective posting in selected specialities for skill development.
Reg.io
nal colloquim are organised for sharing professional experiences among
s
Alumni doctors,
7
permanently working in rural areas, attended this
two-day colloquim wherein they shared their experiences in management
of clinical emergencies with limited resources, motivation of villagers
on health awareness,
communicable disease control. use of herbal medi-
c in 9, management of social problem9 cultural taboos, etc.
The follou-
ing recommendations were forthcoming as a result of this charing
experienres2 - To arrange a one year training programme in family medicine covering
all major clinical subjects including behavioural sciences, counsellimg, community development etc.
This could enhance the knowledge
and skill level of the rural-based doctors.
Several of the partici-
gating rural doctors have offered to participate in this course by
offering their own centres for specific training sessions under rural
conditions•
A short in-service,
skill oriented training for all
they take up their rural postings.
interns, before
This training should essentially
cover maternal and child health.
- To coordinate a national network of our rural graduate doctors’
with
nur college newsletter acting as the mode of communication between
the members of the rural doctors network.
- Conducting regional colloquia of a similar nature in various parts
of our country on a regular basis.
The present teachers of our coll
ege should participate in these regional colloquia in order to discover the actual needs of our rural graduate doctors, so that their
teaching methodologies and syllabi caA be restructured to suit
rural realities.
11 • 1 nteqrated child Development Scbeipc Anganwadi Train inc. Programme: Under this programme, the Anganwadi workers in the Anekal and Attibele
circles are trained in various health programmes with greater emphasis
:
:
8
12. Extension training in agriculture? water resources and Veterniary
care for village youth:- This programme has been organised in the
Dommasandra ? Anekal areas.
The programme consists of imparting field
training and guidance on improvisation of existing methods and provi
sion of expert assistance to extension workers.
The stress is laid
on youth motivation and training in these areas since it has been found
this scheme provides useful outlet for youthful energies and enthusiasm
especially among these who are unemployed and sufficiently educated.
This scheme is seen as a method of providing entry into the^field of
agriculture and veterinary care for fresh workers rather than merely
intensify and promote already established rich farmers etc.
13. Integrated Health Care Training:to indigenous s.ystems of medicine
Villagers in India often
The training at St. Sohn’s
resoi
for the
various categories of health workers including its own medical students
comp-rise training in Herbal Medicine 9 Herbo-mineral Medicine
ssure, Homeopathy and Yoga
Accupr e-
Many of its graduate doctors working in
remote rural areas have substantiated the fact that there is this need
to integrate allopathic Mec|icine with the other systems of Medicine.
14. Training of Govt. Medical Officers:-
At the request of the State
G□ver nment ? our departmental staff conduct training programmes in
Universal Immunization Programme methodologies for Govt. Medical~0fficers in various parts of the State.
15.Training of foreign Elective Posting ^'edical Students: Under this
scheme, on an average, 10 - 15 Medical students per year from U.K.?
U o S.A . ? France, Italy are given experiential learning in Community
Medicine for 4' - 6 weeks each at our rural health centres.
SERVICE PROGRAMMES IN COWUNITY HLmLTH CARE:
Meternel and Child Health ClinicsS-
Conducted fortnightly at all
the six subcentres by the faculty op the Department these clinics
provide an apportunity ■or the women and children to avail themselves
J
f
10
o
5• Universa'l Immunization Programme: Organised in collaboration with
the UNICEF , this programme is a major service programme whose main
objective is to achieve rearly 100 percent of coverage with immunization against Diphtheria, Pertusis, Tetanus, Poliq TEr
Measles for
children below 1 year of age in Anekal, Dommasandra and Bidadi. Primary
Health Centres plus a five lakh population in the urban areas as well.
ft. Rural Mobile Clinics:- As part of the Re-Orientation of Medical
Education Programme, three rural Mobile Clinics operate in 18 remote
villages of the Anekal, Dommasandra and Bidadi Primary Health Centres.
On an average, 80 to 100 patients attend these clinics per day.
The
Mobile Clinics provide an ideal opportunity to conduct not only routine
clinical care at the remote villages, but they also provide an opportunity to carry out specialists care such as ENT, Ophthalmology,
Dentistry, surgery and Dermatology.
diseases can be taught
Basic clinical features of common
especia11y to para-medical workers at these
Nobile Clinics, since the rural patients are not constrained by the awe
inspiring presincts of a large hospital•
This aids in butter inerac-
tion between the patients and health worker which is not possible in
the sophisticated hospitals.
7Serving the Urban under-privileged:- Urban slums in and around
Bangalore, are also served by St. Oohn^.
Health programme such as
immunisation coverage against the major killer diseases for children 9
maternal and child health clinics for expectant mothers, school health
programmes are some of the urban-based health activities of St. 3ohn’s•
In addition, the medico-social unit provides councelling in alcoholism
drug addiction,
juvenile delinquency etc.
The trainees learn to
serve the under privileged in all aspects of health care.
8. Referal Services:- Village patients are refered to the Hospital for
tertiary care.
The referal is done by the resident intern at the rural
health centres and followed up by the social workers of the department.
9
s
This particular service is all the more important since large number
of f emale^ .3 pat lent s often hesitate to be attended by our male residential interns.
During these clinics, the opportunity to educate the
mothers on ante-natal, natal, post-natal and child care services are
also availed of•
&
2* Rural Specialists camps?- As mentioned earlier, the rural Mobile
clinics are amply provided with facilities which are made use of to
organise rural surgical camps in the field of Ophthalmology 9 ENJ,
and Dental surgery.
This has been a novel programme.
Through these
rural specialists camps, it has been proved that it is possible to
conduct surgical procedures such as Tonsillectomies, Antral wash,
Cataract extraction. Dental extraction, Denta-1 fillings, and other
surgical procedures, even under Leneral Anaesthesia.
It has been
heartening to note that there has been no post operative complications
or infections reported so far although each camp has on an average
of 30 to 40 operative Cases.
^he local Youth Clubs are involved in
the management of the organisation and publicity etc. 9 of these camps.
Follow up care is provided by the residential interns.
Natural Family Planning Services:-
The family Welfare °ervices .
section of the Department of Ob & Gynae of the Hospital accampany the
Maternal and child health service teams and conduct awareness progra
mme in Natural Family Planning among the villagers of the Six rural
subcentres 9
An average of 4 to 6 couples accept the Natural Family
Planning each wee<.
4a Factory Workers Health Services:- Under the occupational Health
Services provided for small factory workers, the department is involved actively
ir the provision of pre-placement,
factory safety ’education ^Occupational
periodic examinat io r j1
hazards survey and executive
:
11
:
The ENT, Skin, Dental and Ophthalmology departments participate in
these specialist camps.
9« Food Hygiene Inspection*-
The Hospital Canteen and other Hesses. ‘
ih the institution, are subject to regular food hygiene inspections*
carried ont by the Department faajity.
This is done in collaboration'
with the concerned administrative.chiefs for effective and prompt
iriplementation of the recommended control measures.
10. Immunization Coverage Evaluation Surveys:-
In collaboratiqn with
the State Government directorate of Health Services, teams of staff
from the department conduct specialized immunization coverage ^valua—
tion surveys in various districts of the state such as Kolar ftis^trict,*
z
Hysore District, Coorg District etc.
i
11. Preparation of Health Education Haterials:-
With a regular artist
as part of the Department staff. several posters, charts, etc., on !
Wealth Education has been prepared and used in health exhibitions.
These materials are also borrowed for use by various other inst itoit io ns
The same is true of audio cassettes prepared in local languages to
depict songs and drama about important issues in health of the
Community.
12) Participatory process:- The main objective of the various health
participatory process, wherein the
programmes of St. Cohn’s aims at a oarticipatory
the villagers themselves participate in financing health care, supply
of materials and manpower, etc •
the
This is particularly exemplified by
Hallur Health Cooperative Centre, which now has its own hospital
building and other facilities provided through a cooperative movement
which the college initiated in 1973.
Village Health Committees ^have
been formed at each of the Rural Health Centres, and all decisions are
participatory in nature.
A largepart of the organization of surgical
and other speciality Rural Camps is also under taken by village youth
%
A
12
RESEARCH PROGRACTE IN COmUNITY HEALTH
The fact that a large number interns are posted to our rural
health
Centres each year, has enabled the formulation-Hidexecution
pf several research studies, by the staff (j.f the Department.
Some
of the impoFtant-research projects covered oyer the years are deteclar region, health hazards of sreiculture
tiQB of goitre in the Muftiar region,
Prevalence
workers, house dust mites and allergy in rural areas,
Polio lameness surveys
surveys of Leprosy, TB and other Major diseases,
Leprosy health education methodologies, helminthic surveys, Knowledge
attitude practice survey's,
school health surveys, environmnntal
‘health factors surveys,anaemia and productivity among tea pluckers
Paperss have been published by the staff in
Paper
al
var ious ' Bat ional and internatior/ health journals.
IB
the plantation etc.
Publications in food hygiene and immunization methodologies
Ifcave been written by the staff in English and the local language
ol Kannada as well •
Using appropriate technology, practical methods of solar cooking
vegetable storage devices, smokeless chullas, kitchen nutrition
gardes etc,, have also been evolved by the staff of the Department.
LOOKING BEYOND:
All the programmes outlined, so far
are dynamic in nature since
they are updated constantly depending on the feedback received of
their effectiveness and efficiency.
The emphasis is thus on training
and health education rather than merely the provision of multiple
services.
This ensures that whatever may have been the programme
inputs, the results will be long lasting, self perpetuating and
effective.
*
Go^l H lO.'l-/
Titles
COmUNITY HEALTH AND ST. JOHN’S
r.
The Department of Community Medicine at St. Sohn’s has always
played the pivotal role in fulfilling the mnst important objectives
•f the college.
Serving the under privileged and more importantly
training others to serve the underprivileged has been the main focus
•f the Department.
The enabling process of identifying and attempt-
ing to meet the felt needs of the community 9 is done by the Department •
The training and service components are provided to all members
• f the health tea.a (from the grass-root level workers to tertiary
rare specialists).
TRAINING FOR COmUNITY HEALTH CARES
Being a Medical College , St. Dohn’s is in a unique position tn
provide all the training, components in the formation of a Health
tear.
n
This creates a better understanding of each member’s role
□
in Community Health Care rather than a isolated form of training to
separate’ Health Team Members in separate institutions.
The various
Training programmes in Community Health are as follows:-
1.
For Medical Students:-
a) Rural Orientation Programme:- Conducted every year, -•during the
months of January - February, the main objective of the camp is to
expose the medical students ;to the various facets of rural lite
through a residential progiamme at Dimmasandra Primary Health Centre.
The students visit all the rural subcentres and are guided in deter—
lining the various factors which govern rural life such as
Agr iculture 9 Animal Husbandary? Snail Scale Industries, Fairs 9
Festivals 9 Customs and traditions. Commerce and trade, Transport 9
Traditional systems of Health, Housing and environment, Role of
women in society. Maternal care practices, Child Care practices and
Food practices.
These are presented in the form of field projects
by groups of studencs.
In addition 9 the students also organise many
2
b) Clinico Social Case uork for HBBS Students:-
This is conducted
every month, by posting them in batdhes to the.health centres.
Their
training involves rase work in thVfield, working up the social aspects
nf a number Rf communicable diseases as well as antenatal cases.
The
•bjective is to train the students to consider a case as a holistic
health care problem rather than a mere clinical entity.
The social
economic cams, contributing factors and consequences of major*^iseases are highlighted in this training programme in addition to the
usual clinical features of the disease.
CNational Swcial Services in rural villages:-
Under this scheme,
the medical students carry out community health
and developmental
projects at
various villages in batches once a week.
to the generally known NSS activities,
In contrast
the NSS programme of this
iistitution aims at highlighting community health and community devey,
lopme nt, as the main features of this service .
*A
Education for school
children, adult education, school health education, improving ejnvironw
mental health etc., are some nf the main components of this programme•
b) jEh_iId to Chi 1 d health education programme:- Evolved as a novel
approach to health education, this programme has proved to be an
immense success at Dimmasandra, Anekai and Bidadi health centres.
The basic objectives is to teach groups of children, various aspects
of health, using innovative teaching materials, li\>e demonstratinns
and ’’health songs’*.
Later the children are allowed to share their
knowledge with each other and each child is ’encouraged to tell the
•ther what he er she saw in her/his group teaching.
This way thp
!■
factor of curiosity and natural thirst for knowledge and sharing the
same, are invoked in each of the children.
This greatly contributes
to strengthening the health education in a natural cumulative manner
from child to child
At each rural centre, the major.middle and high
school are covered under this programme.
The positive aspect of this
programme is the school teacher’s involvement and their willingness to
t
S
3
s
e) ElQLtb-g-TS1 Motivation Programme? Groups of
rural mothers are invited
to th~e rural subcentres and they are made aware of various facets of
nutrition, maternal care, child care, immunization etc* The” Programme
is conducted in the form of practical nutrition demonstration
A
immu-
nization procedures, infant feeding techniques 9 preparation of weaning
diets etc.
Emphasis is laid on the fact that all the components of
this programme must be d*ne through practical demonstrations 9 using
lecally available resources iinly, with the mothers themselves actually
-executing the work. ^mphasis is also stressed on the cest factor during
these demonstrations.
n
f) Field work in urban slums:-
Senior clinical students visit families
and maintain family health records, penumerate
n i i m □ t' o •!- □ <-> 1 i r. i H. 1
/U. x?
M
/
for fri-mmunisation,
eligible^
Mb immunization coverage, refer to the St. Sohn's Hospital
Hospital those
tfribse In
in
need nf medical services and also carry out field surveys ir* lMutr i ti«n,
child health etc.
g) Seminars ? discussions and Lectures?~
Over 400 hours are spent in
-1~
, a
teaching 6cmnyunity Health to medical students during their entire
FIBB5 training period.
All the subjects from concepts in Health care 9
to Nutrition, Maternal and Child Heaith, Occupational diseases, s ta
tistics , sociology, Behavioural sciences 9 H ealth Management and
Planning, control of communicable and non-communicable diseases etc.
are. taught to the medical students.
h)Study tours to other Health related Institutions;- In an effort ti
expose our students tn real life situations, they are taken to various
health institutes , field projects and institutions of public health
importance.
Here they get a chance to interact with ather Health
agencies and trheir staff and actual field problems in health care,
z
4
2
2
2* F*r Nursing Students:
a) Rural Orientation Programme for Nursing Studehts: - Conducted every
year during the month of Nay, the main objective of this camp remains
the same as that for medical students.
The.camp is conducted at
Bidadi Primary Health Centre and the rural Nobile Clinic stationed
therein is used extensively during the programme.
In addition to
theactivities refered to in the medical students camp, the Nursing
students are given extra assignments in the field of Naternal and
child care, ^omiitiliary deliveries etc.
3• Fur Community Health Uorkers:- '
fl
Aural Training programme for Community Health Workers:j.s a
This course
three mo ntfe programme, conducted twice -a year,
year , during which on
©■nth.is spentas . a rural residential camp.
The emphasis during-this
rource is on various field, clinical, Lab and institutional training
io the various aspects of community health,
Additional training^in
first aid, home nursing, natural family planning, Herbal medicine,
counselling, community development and human biology are also conducted.
The rural posting comprises mainly of various field projects
on the dynamics of rural life, rural Nobile clinic work, domiciliary
deliveries, maternal and child health," school health- etc.
Rural
projects planning and management of health centres is also taught ’
to the community health workers.
As of the current 20th basic course
for Community Health Workers, a tfital of 355 community health workers
from every state in India and also from Nepal have been successfully
trained.
c
4. Interns:
Rural Internship training programme:-
All Interns in hatches 9 are
posted to the six rural subcentres for a period nf three months duratian each.
ft.part from managing the rural clinic, these interns are
also involved in epidemiological surveys, domiciliary visits, domici
5
They have successfully participated in field evaluation surveys for
immunization coverage, in remote villages in a number of districts
in Karnataka.
5. Training programmes for Deacons, Seminarians and nthers;Being basically a training institute
a large number of small organ!-
-Nations are constantly availing the facilities for training their
*
•wn health warkers.
This programme is arranged on individual request
basis with the theme of the training being highly specific to the
■eed of that organisation.
Many of these programmes are tin the form
of work experience in our ongoing rural programmes.
Some of the
programmes, however, are formal month long structured training programmes•
The Deacons and Seminarians from St. Peter’s Seminary, Suvidya
Colleg e, Deena Seva Ashram, Workers from Association of Physically
V.
handicapped and several other Government and Non-governmental agencies 9
undergo these coursesin Community Health •emducted by the Department,
n
6• Food Hygiene Training Programmes -
Keeping in view the importance
of Food Hygiene in Public Eating Places 9 this training programme aims
at providing appropriate knouledg e and methodology of safe food keeping tfc Hotel Managers 9 cooks and Servers.
This is a monthly programme
Conducted at the Hotel premises itself in the local language so that
the programme is highly effective.
The topics of food hygiene are
especially selected to reflect Indian foods and indigenous techniques
of food preparations.
Plantation Health Services:-
Under the aegis of the United Planters
Association of South India and the Department of Community |Viedic infe,
a series of training programmes, collaboration research and service
Programmes are undertaken throughout the year for the plantation
workers, Doctors, Managers and Lab Technicians of the Tea, Rubber 9
Coffee plantation of South India.
Elective clinical training for
6
training of plantation creche attandants are some of the major areas
of involvement of our institution.
The main objective is to provide
adequate community Health care to the workers of the plantation tommu- *
nity in South India,
8• Rnral School Health Programmed -
Under this programme ail the rural
middle and high school teachers of Anekal Taluk are trained, in the
various facets of school health.
is to train rural
The main objectives of this training
school teachers in basic health care, early detect^n
ion of illness in children 9 immunization and health education.
F ollot*
up of this programme has revealed that the school teachers have success
folly organised^regular teaching programmes in health dor their school
children•
In addition, some of the senior school children have been
trained to supervise healthy practices, environmental cleanliness etc.
Thus the responsibility for health is transferred to the school child.
Periodical school health surveys and health camps in the’ specialised
areas of ENT, Ophthalmology, Dentistry and Surgery are carried out by
the clinical faculty of the concerned departments of the Hospital.
These clinical faculty participate in these rural programme regularly.
9. For the students of Diploma in Hospital Admini -1ration:- Apart Prom
severals hours of didactic teaching in Community Health, these students
are posted to our rural health training centres and other field heal th
programmes’of the
department.
They also carry out Health Management'
projects with the guidance of the departmental faculty.
10 • Colloquim for doctors and Community Health Workers working in
rural areas:-
In addition to basic training in health care to various
categories of health workers, it is important that a follow up is .done
on the utilisation of the knowledge gained.
methods are followed
For this purpose, several
At the professional level 9 doctors can seek
elective posting in selected specialities for skill development.
R eg.io-
7
Alumni doctors, permanently working in rural areas. attended this
two-day cqJloquim wherein they shared their experiences in management
of clinical emergencies with limited resources? motivation of villagers
on health awareness, communicable disease control^ use of herbal medic in^ 9 management of social problem? cultural taboos9 etc.
The follou-
ing recommendations were forthcoming as a result of this charing
exper ientfes2 - To arrange a one year training programme in family medicine covering
all major clinical subjects including behavioural sciences, co unsellimg, community development etc.
This could enhance the knowledge
and skill level of the rural-based doctors
Seneral of the partici
pating rural doctors have offered to participate ir. this course by
offering th^ir own centres for specific training sessions under rural
Gonditions•
4
A short inservice. skill oriented training for all
they take up their rural postings.
interns, bef or e
This training should essentially
cover maternal and child health.
- To coordinate a national network of our rural graduate doctors1
with
^ur college newsletter acting as the mode of communication between
the members of the rural doctors network.
- Conducting regional colloquia of a similar nature in various parts
of our country on a regular basis.
The present teachers of our coll
ege should participate in these regional colloquia in order to dis
cover the actual needs of our rural graduate doctors
so that their
teaching methodologies and syllabi can be restructured to suit
rural realities.
11 « Integrate d c hi 1 d Q^e ye 1 opme n t S c he m u A n g a n w a di T r a in in c Prog r am m e: Under this programme, the Anganwadl workers in the Anekal and Attibele
circles are trained in various health programmes with greater emphasis
:
8
2
12. F.x t ens io n train i ng in ag r jeu 1 tu r e
Water resources and Veterniary
care_ for village youths- This programme has been organised in the
Dommasandra9 Anekal areas.
The programme consists of imparting field
training and guidance on improvisation of existing methods and provi
sion of expert assistance to extension workers#
The stress i^ laid
on youth motivation and training in these areas s.'nce it has been found
this scheme provides useful cutlet for youthful
nergies and enthusiasm
especially among these who are unemployed and sufficiently educated.
This scheme is seen as a method of providing entry into the field of
agriculture and veterinary care for fresh workers rather than merely
intensify and promote already established rich farmers etc.
13. Integrated Hoalth Care Training:to indigenous systems of medicine
Villagers in India often
resort
The training at St. John’s
for th
various categories of health workers including its own medical students
comp-rise training in Herbal Medicine 9 Hurbo-mineral Medicine 9 A c c u p r e s s u r e ? Homeopathy and Yoga#
M any of its graduate doctors working in
remote rural areas have substantiated the fact that .tnere is this need
to integrate allopathic ^'sdicine with the other systems of Medicine.
14• Training of Govt. Medical Officers:-
At the request of the State
Government 9 our departmental staff conduct training programmes in
Universal Immunization programme metnodologies for Govt. Mecjicai Officars in various parts of the State.
5•Training of foreign Elective Posting Medical Students: Under this
averages. 10 - 15 Majaqstudents per year from U.K.j
scheme, on an average^
U.S.A . ,F r a n c e, Italy aru given experiential learning in Community
Medicine for 4' - 6 weeks each at our rural health centres.
SERVICE PROGRAflMfS IN > OMMUfi
1• Maternal and Child Hualth Clinics:-
Jonducted fortnightly at all
the six subcentres by the faculty o* the Department these clinics
provide an apportunity ~or the women and children to avail themselves
of medical care by senior doctors.
10
0
5. Universal Immunization Programme: Crganised in collaboration with
the UNICEF , this programme is a major service programme whose main
objective is to achieve rearly 100 percent of coverage with immunization against Diphtheria, Pertusis, Tetanus, Policy TErNeasles for
children below 1 year of age in Anekal, Dommasandra and Bidadi Primary
Health Centres plus a five lakh population in the urban areas as well.
<5. Rural Nobile Clinics: - As part of the Re-Orientation of Nedical
Education Programme, three rural Nobile Clinics operate in 18 remote.
villages of the Anekal, Dommasandra and Bidadi Primary health Centres.
On an average, 80 to 100 patients attend these clinics per day.
The
Nobile Clinics provide an ideal opportunity to conduct not ondiy routine
clinical care at the remote villages, but they also provide an opportunity to carry out specialists care such as ENT, Ophthalmology,
Dentistry, surgery and Dermatology.
diseases can be taught
Basic clinical features of common
especially to para-medical workers at these
Mobile Clinics since the rural patients are not constrained by the aue
inspiring presincts of a large hospital.
This aids in better inerac-
tion between the patients and health worker which is not possible in
the sophisticated hospitals.
7• Serving the Urban under-privileged*- Urban slums in and around
Bangalore, are also served by St. John’s.
Health programme such as
immunisation coverage against the major killer diseases for children,
maternal and child health clinics for expectant mothers, school health
programmes are some of the urban-based health activities of St. Sohn’s.
In addition, the medico—social unit provides councelling in alcoholism
drug addiction, juvenile delinquency etc.
The trainees learn to
serve the under privileged in all aspects of health care.
8. Referal Services:- Village patients are refered to the Hospital for
tertiary care.
The referal is done by the resident intern at the rural
health centres and followed up by the social workers of the department,
K
9
s
This particular service is all the more important since large number
of f omalespatient s often hesitate to be attended by our male res.idential interns.
During these clinics, the opportunity to educate the
mothers on ante-natal, natal, post-natal and child care services ai?e
also availed of.
2. Rural Specialists camps:- As mentioned earlier, the rural Mobile
clinics are amply provided with facilities which ar.e made use of to
organise rural surgical camps in-the field of Ophthalmology 9 ENT,
and Dental surgery.
This has been a novel programme.
Through these
rural specialists camps. it has been proved that it is possible to
conduct surgical procedures such as Tonsillectomies., Antral wash,
Cataract extraction, Dental extraction, Dental fillings, and other
surgical procedures, even under General Anaesthesia.
It has been
heartening to note that there has been no post operative compileat ions
or infections reported so far although each camp has on an average
of 30 to 40 operative cases.
The local Youth Clubs are involved in
the management of the organisation and publicity etc. 9 of these camps.
Follow up care is provided by the residential interns.
3. Natural family Planning Services: -
The family Welfare Services .
section of the Department of Ob & Gynae of the Hospital accampany the
Maternal and child health service teams and conduct awareness programme in Natural Family Planning among the villagers of the Six rural
subcentr es,
An average of 4 to 6 couples accept the Natural Family
Planning each wee<.
4. Factory Workers Health Services:- Under the occupational Health
■Services provided for small factory workers. the department is involved actively ir the provision of pre-placement, periodic examination/1
factory safety education^Occupational
health .
hazards survey and executive
<
11
:
2
The ENT, Skin, Dental and Ophthalmology departments participate ink
these specialist camps.
9. Food Hygiene Inspection*-
The Hospital Canteen and other Plesses
1
ia the institution, are subject to regular food hygiene inspections
carried oct by the Department faculty.
This is done in collaboration
m a
•c k
with the concerned administrative.chiefs for effective and prompt
iraplementation of the recommended control measures.
101 Immunization Coverage Evaluation Surveys?-
In collaboration with
the State Government Directorate of Health Services, teams of staff
y.
from the department conduct specialized immunization coverage efcalua*
tio* surveys in various districts of the state such as Kolar District,
Mysore District, Coorg District etc.
11e nreperation of Health Education Materials.—
With a regular artist
as part of the Department staff, several posters, charts, etc •, on . u
Wealth Education has been prepared and used in health exhibitions^
These materials are also borrowed for use by var ious other inst ittiit io ns
The same is true of audio cassettes prepared in local languages to
depict songs and drama about important issues in health of the
Community •
12) Participatory process:- The main objective of the various health
programmes of St. John’s aims at a participatory process, wherein the
supply
the villagers themselves participate in financing health care,
of materials and manpower, etc •
the
This is particularly exemplified by
flallur Health Cooperative Centre, which now has its own hospital
building and other facilities provided through a cooperative movement
which the college initiated in 1973.
Village Health Committees hawe
been formed at each of the Rural Health Centres, and all decisions are
participatory in nature. A largepart of the organization of surgical
and other speciality Rural Camps is also under taken by village youth
1'
2
12
RESEARCH PROGRAWE IN COmUNITY HEALTH
The fact that a large number interns are posted to our rural
lealth
centres each year? has enabled the formulation-£ndexecution
pf several research studies, by the staff of the Department.
Some
□ f the important)-research projects covered over the years are detect*
tioiiof goitre in the Muiiiar region, health hazards of sreicu’lture
workers, house dust mites and allergy in rural areas, Prevalence
surveys of Leprosy, TB and other Major diseases. Polio lameness surveys
Leprosy health education methodologies? helminthic surveys, Knowledge
attitude practice surveys,
school health surveys? environmental
||©altli factors surveys, anaemia and productivity among tea pluckers
Papers have been published by the staff in
a!
r
various •■ational and internatior/ health journals.
it •;tha plantation etc.
Publications in food hygiene and immunization methodologies„
lave beeft written by the staff
in English and the local language
of K-annada as well.
Using appropriate technology, practical methods of solar cooking
vegetable storage devices. smokeless chullas 9 kitchen nutrition
gardes etc., have also been evolved by the staff of the Department.
LOOKING BEYOND:
All the programmes outlined, so far 9 are dynamic in nature since
they are updated constantly depending on the. feedback received of
their effectiveness and efficiency.
The emphasis is thus on training
and health education rather than merely the provision of multiple
services.
This ensures that whatever may have been the programme
inputs, the results will bo long lasting, self perpetuating and
effective•
<ZCrY\ H I 0 O
Title:
COmUNITY HEALTH AND ST. JOHN'S.
The Department of Community Medicine at St. Dchn’s has always
played the pivotal role in fulfilling the most important objectives
of the college.' Serving the under privileged and more importantly
training others to serve the underprivileged has been the main focus
The enabling process .f identifying and attempt-
•f the Department.
ing to meet the felt needs of the community, is done by the-’ Department.
The training and service components are provided to all members
the health tea..i (from the grass-root level workers to tertiary
^are specialists).
•'M
TRAINING FOR COMMUNITY HEALTH CARE:
Being a Medical College, St
.Cohn’s is in a unique position tn
provide all the training components in the formation of a Health
tear.
This Creates a better understanding of each member soole
1
in Community Health Care rather than a isolated form of training t«
separate Health Team Members in separate institutions.
The various
7
Training programmes in Community Health are as follows s-
1*
Fat Medical Students:-
a) Rural Orientation Programme:- Conducted every year, during the
months of Oanuary - February, the main objective of the camp is to
expose the medical studeots to the various, facets of rural life
through a residential programme at Dommasandra Primary Health Centre.
The students visit all the rural subcentres and are guided in deterlining the various factors which govern rural life such as
■?<
Agriculture, Animal Husbandary, Small Scale Industries, Fairs,
*
Festivals , Customs and traditions, Commerce and trade. T ransport,
Traditional systems of Health, Housing and environment9 Role of
women in society, Maternal care practices, Child Care practices and
Food practices.
These are presented in the form of field projects
by groups of studencs.
In addition 9 the students also organise many
2 s
:
:
b) ClinicQ1 Social Case work for fIBBS Students: -
This is conducted
every month, by posting them in batdhes to the health centres.
Their
training involves rase work in the field, working up the social aspects
r
of a number Rf communicable diseases as well as antenatal cases.
The
*
•bjective is to train the students.to consider a case as a holistic
health care problem rather than a mere clinical entity.
The socio
economic cauneis5 contributing factors and consequences'oT major diseases are highlighted in this training programme in addition to the
usual clinical features of the disease.
c) National Social Services in rural villages:-
Under this scheme,
the medical students carry out community health
and developmental
project's at
*
various villages in batches once a week. tIn contrast
t« the generally known NSS activities,
the NSS programme of this
itstitutihn aims at highlighting community health and community developme nt, as the main features of this service •
Educatifin for school
children, adult education. school health education. improving environmental health etc.. are some rtf the main components of this programme.
d) Child to Child health ec‘ducatibn programme’s - Evolved as a novel
rr—inij, ne—-ii iiri
n
rn 1 'WTr-ryiT
approach ta health education, this programme has proved to be an
immense success at Q^mmasandra, Afiekal and Bidadi health centres.
The basic objectives is^ to teach 'groups of children, various aspects
of health, using innovative teaching materials, live demonstrations
and ’’health songs’’.
Later the children are allowed to share their
knowledge with each other and each child is encouraged to tell the
•ther what he or she saw in her/his group teaching.
This way the
factor of curiosity and natural thirst for know&edg e and sharing the
same, are invoked in each of the children.
This greatly contributes
to strengthening the health education in a natural cumulative manner
from child to child.
At each rural centre, the major middle and high
school are covered under this programme.
The positive aspect of this
programme is the school teacher’s involvement and their willingness to
3
2
■--Itlg.Ll1 Motivation Programme; .Groups of rural mnthers are invited
to the rural subcentres and they are made aware of -various facets of
nutrition, maternal care, child care. immunization etc* The Programme
is conducted in the form of practical nutrition demonstration immu9
nization procedures, infant feeding techniqu es 9 preparation of weaning
diets etc.
Emphasis is laid on the fact that all the components of
n .1
this programme must be d*ne through practical demonstrations
using
9
locally available resources only, with the mothers themselves actually
executing the work.
mphasis is also stressed on the cast factor during
these demonstrations.
f) Field uork in urban slums;-
Senior clinical students visit families
■? r-« -L R 1 r-. «
-•
— . . — iL. jj •*’.
and maintain family health records, pniimoroi-a
enumerate al
eligibles’’f’or
immunisation
immunization coverage, refer to the St. Bohn's Hnspit'hl those in
need of medical services and also carry nut field survey^ in ^utriti*nf
child health etc.
~g) Seminars ? discussions and Lectures;-
B
Over 400 hours are spent in
teaching community Health to medical students duringI their entire
MBBS training period.
All the subjects from concepts in Health care,
to Nutrition, Maternal and Child
Occupational diseases, s ta
tistics, sociology, Behavioural sciences 9 H ealth Management and
Planning, control of communicable and non—communicable diseases etc.
are taught to the medical students.
....
h)Study tours to other Health related Institutions;- In an effort t«
expose our students to real life situations, they are taken to various
health institutes , field projects and institutions of’ public health
importance.
%re they get a chance to interact with other Health
agencies and their staff and actual field problems in health care,
es
a
e
■i
4
2
2• F*r Nursing Students2
a) Rural Orientation Programme for Nursing Students:- Conducted every
year during the month of May,9 the main objective of this camp remains
the same as that for medical students.
The camp is conducted at
Bidadi Primary Health Centre and the rural Mobile Clinic stationed
therein is used extensively during the programme.
in additien to
theact ivities-, ref ered to in the medical students camp, the Nursing
students are given extra assignments in the field of Maternal and
child care, ^omidiliary deliveries etc.
,4
3• F»r Community Health Uorkers;-
Hural Training
J-3 3
programme for
- «t
Community Health WorkersS-
This course
three months programme,9 conducted twice a year, dur ing- which onr
■
1
i ii ■ m i u .
!■■■<■ 1^,1, . .Tn-iwaii'i.r.irf j ii i-
■ i
©rtnth^is spent ,ae,a rural residential camp
.
■
■ ,
,
The emphasis during this
rtource is on various field, clinical, Lab and institutional training
in the various aspects of community health,
Additional training in
first aid, home nursing, natural family planning, Herbal medicine,
counselling, community deveinpment and human biology are also conducted•
The rural posting comprises mainly of various field projects
on the dynamics of rural life 9 rural Mobile clinic work, domiciliary
deliveries, maternal and child health, school health etc.
Rural
projects planning and management of health centres is also taught
to the community health workers.
As of the current 20th basic course
for Community Health Workers, a thtal of 3,55 community health workers
from every state in India and... also from Nepal have been successfully
trained.
Interns:
Rural Internship training programmes -
All Inte^iis .in hatches 9 are
posted to the six rural subcentres for a period ®f three months dura
tion each.
Apart from managing the rural clinic, these interns a.pe
also involved in epidemiological surveys, domiciliary visits, domici
f!
5
They have successfully participated in field evaluation surveys for
immunization coverage 9 in remote villages in a number of districts
in Karnataka.
5. Training prugrammus for Deacons 9 Seminarians and others;Being basically a training institute, a large number of small organi
-Nations are constantly availing the facilities for training their r
•wn health workers.
This programme is arranged on individual request
basis with the theme of the training being highly specific to the
■eed of that organisation.
Many of these programmes are
of work experience in our ongoing rural programmes.
in the form
Some of the
programmes9 however, are formal month long structured training programmes.
a
The Deacons and Seminarians from St. Pster’s Seminatys Suvidya
Colleg e, Deena Seva Ashram, Workers from Association of Physically
handicapped and several other Government and Non-governmental agencies,
undergo these course3 in Community Health ao-nducted by the Department.
6 • Food Hygiene Training Programmes -
Keeping in view the importance
of Food Hygiene in Public Eating Places 9 this training programme aims
at providing appropriate knowledge and methodology of safe food keep
ing to Hotel Managers $> cooks and Servers.
This is a monthly programme
ronducted at the Hotel premises itself in the local language so that
the programme is highly effective.
The topics of food hygiene are
especially selected to reflect Indian foods and indigenous techniques
of food preparations.
7 • Plantation Health Services:-
Under the aegis of the United Planters
Association of South India and the Department of Community se die in ,
a series of training programmes,
collaboration research and service
Programmes are undertaken throughout the year for the plantation
workers, Doctors, Managers and Lab Technicians of the Tea, Rubber 9
Coffee plantation of South India.
Elective clinical training for
s
6
training of plantation crbche attandants are some of the major areas
of involvement of our institution.
Tha main objective is to provide
adequate community Health care to the workers of the plantation oommunity in South India.
8 • Rnral School. Health Programme»-
Under this programme all the rural
middle and high school teachers of Anekal Taluk are trained in the
various facets of school health.
is to train rural
The main objectives of this training
school teachers in basic health c^re, early detection
ion of illness in children 9 immunization and health education.
FTollou
up of this programme has revealed that the school teachers have Successfolly organised regular teaching programmes in health <6or their school
children•
In addition, some of the senior school children have been
trained to supervise healthy practices, environmental cleanliness etc.
Thus the responsibility for health is transferred to the school child.
Periodical school health surveys and health camps in the specialised
areas of ENT, Ophthalmology} Dentistry and Surgery are carried out toy
the clinical faculty of the concerned departments of the Hospital.
Thes-e clinical faculty participate in these rural programme regularly.
9 • For the students of Diploma in Hospital Admini>trations- Apart from
severals hours of didactic teaching in Community Health, these students
are posted to our rural health training centres and other field health
programmes of the d'epartrrfent.
They also carry out Health Management
projects with the guidance of the departmental faculty.
10• Colloquim for doctors and CommHnity Health Workers working in
rural areas:-
In addition to basic training in health care "to various
categories of health workers, it is important that a follow up is done
on the utilisation of the knowledge gained.
methods are followed.
For this purpose, several
At the professional level 9 doctors can seek
elective posting in selected specialities for skill development.
R egio
nal colloquim are organised for sharing professional experiences among
o
7
Alumni doctors, permanently working in rural areas, attended this
two—day colloquim uherein they shared their experiences in management
of clinical emergencies with limited resources, motivation of villagers
on health awareness,
communicable disease control, use of herbal medi-
cin^, management of social problem, cultural taboos, etc.
The follou-
ing recommendations were forthcoming as e result of this charing
exper ieneesS — To arrange a one year training programme in fanfily medicine covering
all major clinical subjects including behavioural sciences, counsellimg> community development etc.
This could enhance the knowledge
and skill level of the rural-based doctors.
Several of the partici-
gating rural doctors have offered to participate ir. this course by
offering thair own centres for specific training sessions under rural
oonditionse
A short in-eeruice> skill oriented training for all
they take up their rural postings.
interns,
before
This training should essentially
cover maternal and child health.
- To coordinate a national network of our rural graduate doctors’ with
nur college newsletter acting as the mode of communication between
the members of the rural doctors network.
- Conducting regional colloquia pf a similar nature in various parts
of our country on a regular basis.
The present teachers of our coll
ege sho-uld participate in these regional colloquia in order to discover the actual weeds of our rural graduate doctors, so that their
teaching methodologies and syllabi can be restructured to suit
rural realities.
11• Integrated child pevelqpment Scheme Anganwadi Traininc Programme:Under this programme, the Anganwadi workers in the Anekal and Attibele
circles are trained in various health programmes with greater emphasis
:
0
12. Extension training in agriculture; w at er resources a nd V et e r ni a r y
care for village youth:- This programme has been organised in the
Dommasandra 9 Anekal areas.
The programme consists of imparting field
training and guidance on improvisation of existing methods and provi
sion of expert assistance to extension workers*
The stress is laid
on youth motivation and training in these areas snee it has been found
this scheme provides useful outlet for youthful energies and enthusiasm
especially among these who are unemployed and sufficiently educated.
This scheme is seen as a method of providing entry into the field of
agriculture and veterinary care for fresh workers rather than merely
intensify and promote already established rich farmers etc.
13. Integrated Health Care Training;
to indigenous systems of medicine o
Villagers in India often
resort
The training at St. Sohn’s
for the
various categories of health workers including its own medical students
comp-rise training in Herbal Medicine p Herbo-mineral Medicine
s s u r e ? Homeopathy and Yoga.
Accupre-
fl any of its graduate doctors working in
remote rural areas have substantiated the fact that there is this need
to integrate allopathic ^'edicine with the other systems of Medicine.
14. Training of Govt. Medical Officers;-
At the request of the State
Government, our departmental staff conduct training programmes in
Universal Immunization Programme methodologies for Govt. Medical Officers in various parts of the State
15.Training of for sign E1e ct ive Post 1ng '
‘’’u die al Students: Under this
scheme9 on an average, 10 - 15 MbCjical students per year from U.K.,
U.S.A. 9France, Italy aru given experiential learning in Community
Medicine for 4" - 6 weeks each at our rural health centres.
SERVICE PROCjRAflflES IN CuMPWNITy HtaLTH CARE:
1- Meternal and Child Hua 1th Clinics:-
Conducted fortnightly at all
the six subcentres by the faculty o- the Department these clinics
provide an apportunity -or the women and children to avail themselves
of medical care by senior doctors.
10
0
5. Universal Immunization Programmes Organised in collaboration with
the UNICEF , this programme is a major service programme whose main‘
objective is to achieve rearly 100 percent of coverage with immunization against Diphtheria, Per tusis, Tetanus, Policy Tfr
Measles for
children below 1 year of age in Anekal, Dommasandra and Bidadi Primary
Health Centres plus a five lakh population in the urban areas as well.
ft. Rural Mobile Clinics:- As part of the Re-Orientation of Medical
Education Programme, three rural Mobile Clinics operate in 18 remote
villages of the Anekal, Dommasandra and Bidadi Primary health Centres.
On an average, 80 to 100 patients attend these clinics per day.* The
Mobile Clinics provide an ideal opportunity to conduct not onihy, routine
clinical care at the remote villages, but they also provide an opportunity to carry out specialists care such as ENT, Ophthalmology 9
Dentistry, surgery and Dermatology.
diseases can be taught
Basic clinical features of common
especia11y to para-medical workers at these
Mobile Clinics since the rural patients are not constrained by the awe
inspiring presincts of a large hospital.
This aids in butter inerac-
tion between the patients and health worker which is not possible in
the sophisticated hospitals.
7. Serving the Urban under-privileged:- Urban slums in and around
Bangalore, are also served by St. Oohn * s.
Health programme such as
immunisation coverage against the major killer diseases for children 9
maternal and child health clinics for expectant mothers. school health
programmes are some of the urban-based health activities of St. John1s•
In addition. the medico-social unit provides councelling in alcoholism
drug addiction, juvenile delinquency etc.
The trainees learn to
serve the under privileged in all aspects of health care.
8. Referal Services:- Village patients are refered to the Hospital for
terkiary care.
The refural is done by the resident intern at the rural
health centres and followed up bv the social workers of the department.
»
9
This particular service is all the more important since large number
of femalesspatients often hesitate to be attended by our male residential interns.
During these clinics, the opportunity to educate the
mothers on ante-natal, natal, post-natal and child care services are
also availed of.
2. Rural Specialists camps:- As mentioned earlier, the rural Nobile
V
clinics are amply provided with facilities which are made use of to
organise rural surgical camps in the field of Ophthalmology 9 ENT,
and Dental surgery.
This has been a novel programme.
Thrdiugh these
rural specialists camps, it has been proved that it is possible to
*
conduct surgical procedures such as Tonsillectomies, Antral wash,
Cataract extraction, Dental extraction. Dental fillings, and other
surgical procedures, even under General Anaesthesia.
It has been
heartening to note that there has been no post operative complications
or infections reported so far although each camp has on an average
of 30 to 40 operative cases.
^he local Youth Clubs are involved in
the management of the organisation and publicity etc. 9 of these camps.
Follow up care is provided by the residential interns.
3• Natural Family Planning Sec vices: -
The family Welfare Services .
section of the Department of Ob & Gynae of the Hospital accampany the
Maternal and child health service teams and conduct awareness programme in Natural Family Planning among the villagers of the Six rural
subcentres,
An average of 4 to 6 couples accept the Natural Family
Planning each wee<.
4. Factory Workers Health Services:- Under the occupational Health
Services provided for small factory workers, the department is involved actively ir the provision of pre-placement, periodic examinationf
factory safety ©ducation,Occupational
hazards survey and executive
:
11
:
The EMT, Skin, Dental and Ophthalmology departments participate in.H
these specialist camps.
9• Food Hygiene Inspection*-
i £
The Hospital Canteen and other Hesses-,
ii the institution, are subject to regular food hygiene inspections^
• u
carried oat by the Department faculty.
Th^s is done in collaboration
with the concerned administrative.chiefs for effective and prompt
iriplementation of the recommended control measures.
i
10• Immunization Coverage Evaluation Surveys?-
In collaboration with
the State Government Directorate of Health Services, teams of staff
from the department conduct specialized immunization roverage<evalf’ation surveys in various districts of the state such as Kolar District,
x
Hysore District, Coorg District etc.
11• ftreperation of Health Education Haterials:-
With a regular artist
as part of the Department staff. several posters, charts, etc., orj
Wealth Education has been prepared and used in health exhibitions.
These materials are also borrowed for use by various other institditions
The same is true of audio cassettes prepared in local languages to
depict songs and drama about important issues in Heaith of the
Community.
12) Participatory process:- The main objective of the various health
programmes of St. John’s aims at a participatory process, wherein the
the villagers themselves participate in financing health care, supply
of materials and manpower, etc.
the
This is particularly exemplified by
Hallur Health Cooperative Centre, which now has its own»hospital
building and other facilities provided through a cooperative movement
which the college initiated in 1973.
Village Health Committees^have
been formed at each of the Rural Health Centres, and all decisions are
participatory in nature.
A largepart of the organization of surgical
and other speciality Rural Camps is also under taken by village youth
t
r
12
RESEARCH PROGRAMME IN COMMUNITY HEALTH
The fact that a large number interns are posted to our rural
health
centres each year, has enabled the formulation-andexecution
pf several research studies, by the staff of the Department.
Some
ot the impoFtanfa resear ch projects covered over the years, are detec
tioi of goitre in the Muaiar region, health hazards of sreiculture
workers, house dust mites and allergy in rural areas, Prevalence
surveys of Leprosy, TB and other Major diseases. Polio lameness surveys
Leprosy health education methodologies. helminthic surveys, Knowledge
attitude practice surveys,
school health surveys, environmantal
^ealtb factors surveys, anaemia and productivity among tea pluckers
r
Papers have been published by the staff in
al
various lational and internatior/ health journals.
ig the plantation etc.
Publications in food hygiene and immunization methodologies
||ave beeh written by the staff in English and the local language
of Kannada as well.
Using appropriate technolo.gy, practical methods of solar cooking
vegetable storage devices, smokeless chullas, kitchen nutrition
gardes etc., have also been evolved by the stafp of the Department.
LOOKING BLYONDs
All the programmes outlined, so far, are dynamic in nature since
they are updated constantly depending on the feedback received of
their effectiveness and efficiency.
The emphasis is thus on training
and health education rather than merely the provision of multiple
services.
This ensures that whatever may have been the programme
inputs, the results will bo long lasting, self perpetuating and
effective •
y
f
C CAT H
Title:
CO.mUNITY HEALTH AND ST. JOHN’S
The Department of Community Medicine at St. Dnhn’s has always
i
played the pivotal role in fulfilling the most important objectives
of the college.
Serving the under privileged and more 'impottantly
training others to serve the underprivileged has been the main focus
!
of the Department.
The enabling process of identifying and attempt-
ing to meet the felt needs of the community,9 is done by the Depart—
ment •
The training and service components are provided to all members
of the health team (from the grass-root level workers to tertiary
rare specialists).
’
'K-. •
,
'
’
-
TRAINING FOR COMMUNITY HEALTH CARE:
Being a Medical College 9 St. John’s is in a unique position to
provide all the training components in the formation of a Health
team.
This creates a better understanding of each member’s role
in Community Health Care rather than a; isolated form pf training to
separate Health Team Members in separate institutions.
The various
Training programmes in Community Health are as follows:9
Fhr Medical Students:.a) Rural Orientation Programme:- Conducted every year, during the
to
months of January- - February 9 the main objective of the camp is to
the
medical, students to the
various facets of rural life
expp.se
1
•
f-iff
■
through a residential programme at Dommasandra Primary Health Centre.
The students visit all the rural sub.centres and are guided in determining the various factors which govern rural life such as
Agriculture, Animal Husbandary, Small Scale Industries, Fairs 5
Festivals 9 Customs and traditions. Commerce and trade. Transport 9
, ;; 1
Traditional systems of Health, Housing and environment. Rnle of
*
women in society. Maternal care practices. Child Care practices and
Food practices.
These are presented in the form of field projects
by groups of studehcs.
In addition,
addition the student's also organise md'ny
2
.L
b) Clinico Social Case work for HBBS Students;-
This is conducted
l'-
,
every month, by posting them in batdhes to the health centres.
Their
training involves case work in the field, working up the social aspects
■
•of a number of communicable diseases as well as antenatal cases.
The
•bjective is £o train the students to consider a case as a holistic
health care problem rdther than a mere clinical entity.
The socio
economic cams, contributing factors and consequences of major disea
ses are highlighted in this training programme in addition to the
usual clinical features of the disease.
e) National Social Services in rural villages?-
Under this scheme,
the medical students carry out community health
and developmental
projects at
various villages in batches once a week.
to the generally known NSS activities'^
•In contrast
the NSS programme of this
institution aims at highlighting community health and community deve'lopme nt, as the main features of this service .
s
Education for school
childr en,* adult education, school health education, improving environmental health etc., •are some of the main components of this programme.
■
•
•
?
d) Child to Child health education programme?- Evolved as a novel
approach to health education, this programme has proved to be an
immense success at Dommasandra 9 Anekal and Bidadi health centres*
The basic objectives iszto teach groups of children, various aspects
of health, using innovative teaching materials, live demons t rat'll ns
and ’’health songs’*.
Later the children are allowed to share their
knowledge with each other and each child is encouraged to tell the
^ther what he tr she saw in her/his group teaching,
This way the
factor of curiosity and natural thirst for knowiedg e and sharing the
same, are invoked in each of the children,
This greatly contributes
to strengthening the health education in a natural cumulative m^hner
from child to child.
At each rural centre, the major middle and high
school are covered under this programme.
The positive aspect of this
programme is the school teacher’s ..involvement and their willingness to
r>...
0
3
e
Groups of rural mothers are invited
e) Mothers' Motivation Ptogramme? I
made aware of various facets of
to the rural subcentres and they are
immunization etc. The Programme
nutrition, maternal care, child care,
nutrition demonstration, immuis conducted in the form of practical
nizatlon prooedurea,' infant feeding techniques, prepeeetlcn of weaning
<
H ■■■■■ ■
■
—
diets etc.
aphasia is laid on the fait that =11 the components of
this programme
"must be dine through practical demonstrations, using
with the mothers themselves actually
locally available resources *nly,
the cost factor during
executing the work. ^mphasis is also stressed on
these demonstration^
visit families
S e n io r clinical students
enumerate eligibles for immunisation,
family
health
records,
and maintain
John's Hospital those in
do immunization coverage, refer to the St.
nut field surveys in Nutritinn,
also
medical
services
and
carry
need of
p
f jeld uork in urban slums? -
1n
child health etc.
g) Seminars,
discussions and Lectures:-
Over 400 hours are spent in
dommunity Health t. medical students during their entire
concepts in Health care,
MOBS training period. All the subjects from
sta and Child health. Occupational diseases,
Maternal
to Nutrition,
Behavioural sciences, Health Management and
tistics, sociology,
non-communicable diseases etc.
communicable and
Planning, control of
teaching
are taught to the medical students.
hjStudy tours to' other Health related InstitjAj^nsi - In an effort t®
expose our students tn real life situations, they are taken to varrous
health institutes,
importance•
field projects and institutions of public health
Here they get
a-chance to interact with other Health
in health care.
agencies and their staff and actual field problems
4
2. For Nursing Students^
a) Rural Orientation Programme for Nursing Students•- Conducted every
year during the month of May, the main objective of this camp remains
the same as that for medical students.
The camp is conducted at
Bidadi Primary Health Centre and the rural Mobile Clinic stationed
therein is used extensively during the programme.
In addition to
theactivities refered to in the medical students camp, the Nursing
students are given extra assignments in the field of Maternal and
child care, uomitciliary deliveries etc.
3. Fcr Community Health Workers:Rural Training programme for Community Health Workers:- This course
i.s a three mcwnths programme, conducted twice a year, during which one
©onth^is spent,jaa a rural residential camp.
The emphasis during this
course is on various field, clinical, Lab and institutional training
in the various aspects of community health.
Additional training in
first aid, home nursing, natural family planning, Herbal medicine,
counselling, community development and human biology are also conducted.
The rural posting comprises mainly of various field projects
on the dynamics of rural life, rural Mobile clinic work, domiciliary
deliveries, maternal and child health, school health etc.
Rural
projects planning and management of health centres is also taught
to the community health workers.
As of the current 20th basic course
for Community Health Workers, a total of 355 community health workers
from every state in India and also from Nepal have been successfully
trained.
4. Internsi
Rural Internship training pro r ammes-
All Interns in batches, are
posted to the six rural subcentres for a period- of three msnths duration each.
Apart from managing the rural clinic, these interns are
also involved in epidemiological surveys, domiciliary visits, domici—
liary deliveries>immunization and school health.
Bes ides, they parti
cipate in all the other rural service programmes .conducted by the
5
They have successfully participated in field evaluation surveys for
immunization coverage, in remote villages in a number of districts
a
in Karnataka,.
5.
Train!no programmes for Deacons y
Seminarians and other#:-*
-■■■
rascM---------------!-■
j- - bi m
th
->•»mwBH
■■
ii ■■b ..r*ew.■t—"
Being basically a training institute ? a large number of smafl organidations are constantly availing the facilities for training their
own health workers.
■j ?•:
This programme is arranged on individual request
basis with the theme of the training being highly specific to the
need of that organisation^
Many of these programmes are •in the form
of work experience in our ongoing rural programmes.
Some of
the
programmes, however, are formal month long structured training prog^ranimes ♦
The Deacons and Seminarians from St
Peter’s Seminahy, Suvidya
Colleg e 9 Deena Seva Ashram , Workers from Association of Physically
r.
handicapped and several other Government and Non-governmental agencies 9
undergo these coursesm Community Health conducted by ths Department.
6• Food Hygiene Training Programme?-
Keeping in view the importance
of Food Hygiene in Public Eating Places, this training programme aims
at providing appropriate knowledge and methodology of safe food' keep
ing tn Hotel Managers
cooks and Servers
This is a monthly programme
conducted at the Hotel premises itself in the local language so that
•the programme is highly effectiva.
The topics of food hygiene are
especially selected to reilect Indian foods and indigenous techniques
of food preparations.
7.- Plantation Health Serv.‘*ces:•
ii I
■< n i ■
i
. ■ ua -n .-amn.
: lair.T.,.
Under the aegis of the United Planters
Association o? Sc;uth India and the Department of Community 1V| e d i c i n fe,
■'
■
■
a series'of training programmes, collaboration research and service
Programmes are undertaken throughout the year for the plantation
workers ? Doctors, Managers and Lab Technicians of the Tea, Rubber 9
Coffee plantation of South India,
Elective clinical training for
Plantation Medical Officers, training in. Public Health laboratory
6
training of plantation creche attandants are some of the major areas
of involvement of our institution.
The main objective is to provide-
adequate community Health care to the workers of the plantation wommunity in South India,
8• RTal School Health Pro r ammo.-
Under this programme ail the rural
middle and high school teachers of Anekal Taluk are trained in the
various facets of school health.
is to train rural
The main objectives of this training
school teachers in basic health care, early detection
ion of illness in children , immunization and health education.
F ollou
Up of this programme has revealed that the school teachers have
success
fully organised regular teaching programmes in health 6or their school
children•
In addition, some of the senior school children have been
trained to supervise healthy practices, environmental cleanliness etc.
Thus the responsibility for health is transferred to the school child.
Periodical school health surveys and health camps in the specialised
areas of ENT, Ophthalmology, Dentistry and Surgery are carried out by
the clinical faculty of the concerned departments of the Hospital.
These clinical faculty participate in these rural programme regularly.
9. Fjpr the students of Diploma in Hospital Administration;- ftpart from
severals hours of didactic teaching in Community Health, these students
are posted to our rural health training centres and other field heal th
programmes of the department.
ihey also carry out Health Management
projects with the guidance of the departmental faculty.
10* Colloquim for doctors- and
-n_d-._Commcnity Health Workers working in
rural areas;-
In addition to basic training in health cate to various
categories of health workers , it is important that
a follow up is done
o n the utilisation of the knowledge gained.
For this purpose, several
methods are followed. At the professional level,
doctors can seek
elective posting in selected specialities for skill development.
R eg.ional colloquim are organised for sharing professional
experiences among
2
7
Alumni doctors, permanently working in rural areas, attended this
two-day colloquim wherein they shared their experiences in management
of clinical emergencies with limited resources, motivation of villagers
on health awareness, communicable disease control, use of herbal medic in^ 9 management of social problem, cultural taboos, eto.
The follow-
ing recommendations were forthcoming as a result of this charing
experienfresS- To arrange a one year training programme in family medicine covering
all major clinical subjects including behavioural sciences, counsell-
img 9 community development etc.
This could enhance the knowledge
and skill level of the rural-based doctors.
Several of the partici-
pating rural doctors have offered to participate in this course by
offering their own centres for specific training sessions under rural
conditions•
- A short in-service, skill oriented training for all
they take up their rural postings.
interns, before
This training should essentially
cover maternal and child health.
- To coordinate a national network of our rural graduate doctors’ with
nur college newsletter acting as the mode of communication between
the members of the rural doc tors'network.
— -Conducting regional colloquia of a similar nature in
of our country on a regular basis.
various parts
The present teachers of our coll
ege should participate in these regional colloquia in order to dis
cover the actual needs of our rural graduate -doctors , so that their
teaching methodologies and syllabi can be restructured to suit
rural realities.
11. Integrated child Developmunt Scheme Anganwadi Training Programme;Under this programme, the Anganwadi workers in the Anekal and Attibele
circles are trained in various health programmes with greater emphasis
on health education, nutrition demonstration to mothers and child care
:
J
8
12. Extension training in agriculture 3 water resources and Veterniary
care for village youths- This programme has been organised in the
Dommasa ndr a, Anekal areas.
The programme consists of imparting field
training and guidance o n improvisation of existing methods and provi
sion of expert assistance to extension workers.
The stress is laid
on youth motivation and training in these areas since it has been found
this scheme provides useful outlet for youthful energies and enthusiasm
especially among those who are unemployed and sufficiently educated.
«
This scheme is seen as a method of providing entry into the field of
agriculture and veterinary care for fresh workers rather than merely
intensify and promote already established rich farmers etc.
13. Integrated Health Care Training;to indigenous systems of medicine.
Villagers in India often
rcsoT'4’
The training at St. John’s
for the
various categories of health workers including its own medical students
comp-rise training in Herbal Medicine 9 Herbo-mineral Medicine 9 Accupr essure, Homeopathy and Yoga.
M any of its graduate doctors working in
remote rural areas have substantiated, the fact that there is this need
to integrate allopathic Mgbicine with the other systems of Medicine.
14
Training of Govt, Medical Officers:-
At the request of the State
Government, our departmental staff conduct training programmes in
Universal Immunization Programme methodologies for Govt. Medical Offi
cers in various parts of the State.
15 •» Training of foreign Elective Posting ‘’'edical Students: Under this
scheme, on an average, 10 - 15
e dical students per year from U.K.,
U.S.A.,France, Italy are given experiential learning in Community
Medicine for 4-6 weeks each at our rural health centres.
sJj_lLCE PROGRAMMES IN COMMUNITY HEALTH CARE;
1 o
Maternal and Child Health Clinicss-
Conducted fortnightly at all
the six .subcentres by the. faculty of. the Department these clinics
provide an apportunity for the women and children to avail themselves
9
This particular service is all the more important since large number
of femalesspatients often hesitate to be attended by our male resid
ential interns.
During these clinics, the opportunity to educate the
jp
mothers on ante-natal, natal, post-natal and child care services are
also availed of.
2. Rural Specialists camps:- As mentioned earlier, the rural Mobile
rlinics are amply provided with facilities which are made use of to
organise rural surgical camps in the field of Ophthalmology 9 ENT,
and Dental surgery.
Through these
This has been a novel programme.
rural specialists camps, it has been proved that it is possible to
conduct surgical procedures such as Tonsillectomies
Antral wash,
Cataract extraction, Dental extraction, Dental fillings, and other
surgical procedures, even under General Anaesthesia.
It has been
heartening to note that there has been no post operative complications
or infections reported so far although each camp has on an average
of 30 to 40 operative cases.
The local Youth Clubs are involved in
the management of the organisation and publicity etc., of these camps.
Follow up care is provided by the residential interns.
3. Natural Family Planning Services:-
■t
The family Uelfare °ervices
section of the Department of Ob & Gynae of the Hospital accampany the
Maternal and child health service teams and conduct awareness progra- -1
villagers
in
Natural
among
of
Family
the
the
rural
Planning
Six
mine
subcentres,
An average of A to 6 couplas accept the Natural Family
Planning each week*
4 a factory Workers Health Services? - Under the occupational Health
Services provided for small factory workers, the department is involved actively in the provision of pre-placement, periodic examination i1
factory safety education,Occupational
health •
hazards survey and executive
10
0
5. Universal Immunization Programme: Upganised in collaboration with
whose main
the UNICEF , this programme is a major service programme
with immunive is to achieve rearly 100 percent of coverage
Policy TEr Measles for
zation against Diphtheria, Pertusis, Tetanus,
children below 1 year of age in Anekal, Dommasandra and Bidadi Primary
as well.
Health Centres plus a five lakh population in the urban areas
6. Rural Mobile Clinics:
- As part of the Re-Orientation of Medical
operate—-in 18 remote
Education Programme, three rural Mobile Clinics
I
villages of the Anekal, Dommasandra and Bidadi Primary Heaith Centre^.. < :
I
The
attend
clinics
per
day.
these
100
patients
80
to
On an average,
Mobile Clinics provide an ideal opportunity to conduct not on(hy:: routine
clinical care at the remote villages, but they also provide an opportunity to carry out specialists care such as ENT, Ophthalmology,
Dentistry, surgery and Dermatology.
diseases can be taught
Basic clinical features of common
especially to para-medical workers at these
Mobile Clinics since the rural patients are not constrained by the awe
This aids in better imerac-
inspiring presincts of a large hospital.
tion between the patients and health worker which is not possible in
'
;
J. .
the sophisticated hospitals.
7. Serving the Urban under-privileged*- Urban slums in and around
Bangalore, are also served by St. Sohn’s.”" Health -program^ s.UQhz asr
i
immunisation coverage against the major killer diseases for c-h.ildre.n9
maternal and child health clinics for expectant mothers, school health
programmes are some of the urban-based health activities of St. Sohn’s.
In addition, the medico—social unit provides councelling' in alcoholism
drug addiction, juvenile delinquency etc.
The trainees leafri t,o
serve the under privileged in all aspects of health care.
8. Referal Services:- Village patients are refered to., the Hospital for
tertiary care.
The referal is done by the resident intern at the rural
health centres and followed up by the social workers of the department.
:
11
:
The ENT, Skin, Dental and Ophthalmology departments participate in
these specialist camps.
• ^ood H-ygiene Inspection* -
The Hospital Canteen and other Messes
in the institution, are subject to regular food hygiene inspections
carried oat by the Department faojlty0
This is done in collaboration
with the concerned administrative chiefs for effective and prompt
implementation of the recommended control measures.
10• •Immunization Coverage Evaluation Surveys;-
In collaboration with
the State Government directorate of Health Services, teams of staff
from the department conduct specialized immunization coverage evaloa
tion surveys in various districts of the state such as Kolar District,
Mysore District, Coorg District etc
11. ?reperation of Health Education Materials;-
With a regular artist
as part of the Department staff, several posters, charts, etc •, on
Health Education has been prepared and used in health exhibitions.
These materials are also -borrowed for use by various other inst itoit io ns
The same is true of audio cassettes prepared in local languages to
depict songs and drama about important issues in dGaith of the
Community •
12) Participatory process;- The main objective of the various health
programmes of St. John’s aims at a participatory process, wherein the
the villagers themselves participate in financing health care, supply
of materials and manpower. etc.
the
This is particularly exemplified by
nallur Health Cooperative Centre, which now has its own hospital
building and other facilities provided through a cooperative movement
which the college initiated in 1973.
Village Health Committees have
been formed at each of the Rural Health Centres, and all decisions are
participatory in nature.
A largepart of the organization of surgical
and other speciality Rural Camps is also under taken by village youth
12
RESEARCH PROGR/WE
IN COmUNITY HEALTH
The fact that a large number interns are posted to our rural
health
centres each year, has enabled the formulation-£ndexecution
of several research studies, by the staff of the Department.
Some
of the important^research projects covered over the years are detection of goitre in the flunnar region, health hazards of sreiculture
worker s, house dust mites and allergy in rural areas, Prevalence
surveys of Leprosy, TB and other. Major diseases, Polio lameness surveys
Leprosy health education methodologies, helminthic surveys, Knowledge
attitude practice surveys,
school health surveys, environmental
health factors surveys, anaemia and productivity among tea pluckers
in the plantation etc.
Papers
Papers have been published by the staff in
various national and internatior/ health journals.
Publications in food hygiene and immunization methodologies
have been written by the staff in English and the local language
of Kannada as well.
Using appropriate technology, practical methods of solar cooking
vegetable storage devices, smokeless chullas, kitchen nutrition
gardens etc4, have also been evolved by the staff of the Department.
LOOKING BEYONDs
All the programmes outlined, so far 9 are dynamic in nature since
they are updated constantly depending on the feedback received of
their effectiveness and efficiency.
The emphasis is thus on training
and health education rather than merely the. provision of multiple
services•
This ensures that whatever may have been the programme
inputs, the results will bo long lasting, self perpetuating and
effective.
*
. Titles
GO
H * 0 ■ '■>-!
COmUNITY HEALTH AND ST. SOHN’S,
The Department of Community Medicine at St. Oehn’s has always
*
played the pivotal role in fulfilling the mast important objectives
if the college.
Serving the under privileged and more importantly
training others to serve the underprivileged has been the main focus
•f the Department.
The enabling process «f identifying and attempt-
ing to meet the felt needs of the community, is done by the Department.
The training and service components are provided to all members
of the health tea.a (from the grass-root level workers to tertiary
rare specialists) •
.. r
TRAINING FOR COMMUNITY HEAL’TH €AREs
Being a Medical College, St. John’s is in a unique position to
provide all the training components in the formation of a Health
tear.
This creates a better understanding of each member s role
in Community Health Care rather than a isolated form of training to
separate Health Team Members in separate institutions.
the various
Training programmes in Community Health are as follows:1.
FAr Medical StudentsS-
a) Rural Orientation Programmes- Conducted every year? during the
months of Oanuary - February, the’ main objective of-the camp is to
expose the medical studeots to the various facets of rural liF©
through a residential programme at Dammasandra Primary Ffealth Centre.
The students visit all the rural subcentres and are guided in deterlining the various factors which govern rural life such as
Agr iculture 9 Animal Husbandary, Snail Scale Industries, Fairs 9
Festivals , Customs and traditions. Commerce and trade, Transport,
Traditional systems of Health, Housing and environment, Rele of
women in society. Maternal care practices, Child Care 'practices and
Food practices.
These are presented in the form of field projects
by groups of studencs.
In addition 9 the students also organise many
2
b) Clinico Secial Case uork for MBBS Students:-
This is conducted
every month, by posting them in batdhes to the health centres.
Their
training involves rase work in thfe field, working up the social aspects
nf a number «f communicable, diseases as well as antenatal cases.
•
‘ 3
The
•bjective is to train the students to consider a case as a holistic
..
health care problem rather than a mere clinical entity.
The socio
A
econamic causes, contributing factors and consequences of rn^jor diseases are- highlighted in this training programme in addition to the
>
usual clinical features of the disease.
cNational Social Services in rural villages
a
the medical students carry out community health
projects at
Under this scheme,
and developmental
varirus villages in batches once a week.
t® the generally known NSS activities,.
In contrast
the NSS programme of this
iostitutinn aims at highlighting community health and community development, as the main features of this service .
Education for schnol
children, adult education, school health education, improving environmental « health etc.,* are some nf the main components of this programme •i
) Qhild to Childhealth education jdrogrammes- Evolved as a novel
approach to health education, this programme has proved to be an
immense success at D^mmasandra 9 Anekal and Bidadi health centres.
The basic objectives is to teach groups of children, various aspects
of health, using innovative teaching materials, live demonstrations
and ’’health songs’*.
Later the children are allowed, to share their
knowledge with each other and eatfh child is encouraged to tell the
•ther what he or she saw in her/hisngroup teaching.
This way the
K
factor of c uriosity and natural thirst for knowledge and sharing the
same, are invoked in each of the children.
This greatly contributes
to strengthening the health education in a natural cumulative manner
from child to child.
At each rural centre, the major middle and high
school are covered under this programme.
The positive aspect of this
programme is the school teacher’s involvement and their willingness to
3
e) Mothers 1 Motivation Pro rammes Groups of rural mothers are invited
to the rural^subcentres and they are made auare. of various’facets of
nutrition, maternal care, child care , immunization etc.. The Programme
is conducted in the form of practical nutrition demonstration, immuimmunization procedures, infant feeding techniques, preparation of ueaning
diets etiC,.
Emphasis is laid on the fact that all the components of
this programme must be dsne through practical demonstrations, us ing
locally available resources unly , uith the mothers themselves actually
-executing the uork. ^mphasis is also stressed on the cost factor during
these demonstrations.
t*
?) Fifrld uork in urban s1urns:-
Senior clinical students visit families
and maintain family health records, enumerate eligibles for immunisation,
A
d® immunization coverage, refer to the St. 3ohn!s Hospital those in
o
i* a
«
■
need of medical services and also carry out field surveys in Nutriti®nt
child health etc.
g) Seminars
discussions and Lecturess-
flver 400 hours are spent iff'
teaching comnxunity Health to me dical students during their entir‘e
N0BS training period.
All the subjects from concepts in Health care,
to Nutrition, Maternal and Child Heaith, Occupational diseases, s ta
tist ics, sociology, Behavioural sciences s h ealth Management and
Planning, control of communicable and non-communicable diseases etc.
are. taught to th-e medical students.
h)Study tours to other Health related InstitutiohsS- In an effort t®
expose our students to real life situations, they are taken to various
health institutes , field projects and institutions of public health •
importance.
^er e they get a chance to interact uith other Health
agencies antj their st%ff and actual field problems in health care.
I
S
4
s
2• F*r Nursing Students:
Q^i^ntation Programme for Nursing Studentss — Conducted every
a)
year during the month of Nay, the main objective of this camp remains
the same as that for medical students.
The camp is conducted at
Bidadi Primary Health Centre and the rural Nobile Clinic stationed
therein is used extensively during the programme,
in addition to
theactivities refered to in the medical students camp , the Nursing
students are giv^en extra assignments in the field of Natejnal and
child care,
omibiliary deliveries etc.
Far Community Health Workers^- ’
r.’1
r
Aural Training programme for Community Health Uorkerss-
3-3 ,a
This course
three monthsprogramme, conducted twice a year, during which on
©inth^ftS spent,as
rural residential camp
The emphasis during this
rource is on various field, cl in ical, Lab a'hd institutional training
i» the various aspects of community health.
Additional training in
first aid, home nursing, natural family planning, Herbal medicine,
counselling, community develnpment and human biology are also con9*
r.
ducted
The rural posting comprises mainly of various field projects
on the dynamics of rural life, rural Nobile clinic work, domiciliary
deliveries , maternal and child health, school health etc.
Rural
projects planning and management of health centres is also taught
to the community health workers.
As of the current 20th basic course
for Community Health Workers, a total of 355 community health workers
from every state in India and also from Nepal have been successfully
trained.
4. Interns.
Rural Internship training programmed -
All
Interns
.in
hatclies 9
are
posted to the six rural subcentres for a period ®f. three, months duratian each.
Apart from managing the rural''clinic, these interns are
also involved in epidemiological surveys, domiciliary visits, domici
liary deliveries9immunization and school health.
Bes ides , they parti
5
6
They have successfully participated in field evaluation surveys for
immunization coverage, in remote villages in a number of districts
n
in Karnataka.
5. Training prwgrammus for Deacons
Seminarians and others; -
Being basically a training institute, a large number of small organ!-Nations are constantly availing the facilities for training their
tun health workers.
This programme is arranged on individual request
basis with the theme of the training being highly specific to the
■eed of that organisation.
Many of these programmes are tin the form
of work experience in our ongoing rural programmes.
Same of the-
programmes, however, are formal month long structured training programmes.
The Deacons and Seminarians from St. Pster’s Seminaty 9 Suvidya
College, Deena Seva Ashram, Workers from Association of Physically
handicapped and several other Government and Non-governmental agencies
undergo these course3in Community Health •onductsd by the Department.
6• Food Hygiene Training Programme;-
Keeping in view the importance
of Food Hygiene in Public Eating Places
this training programme aims
at providing appropriate knowledge and methodology of safe food keep
ing to Hotel Managers 9 cooks and Servers.
This is a monthly programme
conducted at the Hotel premises itself in the local language so that
the programme is highly effective
The topics cf food hygiene are
especially selected to reflect Indian foods and indigenous techniques
of food preparations.
7• Plantation Health Services:-
Under the aegis of the United Planters
Association of South India and the Department of Community |V|edicinfe,
a series of training programmes, collaboration research and service
Programmes are undertaken throughout the year for the plantation
workers, Doctors, Managers and Lab Technicians of the Tea, Rubber,
Coffee plantation of South India.
Elective clinical training for
s
6.
o
training of plantation creche attandants are some of the major areas
of involvement of our institution.
The main objective is to provide
adequate community Health care to the workers of the plantation Bommunity in South India,
8 • Raral School Health Programme<-
Under this pr gramme ail the rural
middle and high school teachers of Anekal Taluk are trained in the
various facets of school health.
is to train rural
The main objectives of this training
t
schodl teachers in basic health care, early detection
ion of illness in children 9 immunization and health education.
F ollou
t
up of this programme has revealed 'that the school teachers have successfolly organised regular teaching programmes in health (for tiieir school
children•
In addition, some of the senior school children have been
trained to supervise healthy practices, environmental cleanliness etc.
Thus the responsibility for health is transferred to the School child.
Periodical school health surveys and health camps in the specialised
areas of ENT, Ophthalmology ? Dentistry and Surgery are carried out by
the clinical faculty of the concerned departments of the Hospital.
Thes-e clinical faculty participate in these rural programme regulerly.
9 • For the students of Diploma in Hospital Administration;- Apart from
severals hours of didactic‘teaching in Community Health, these students
are posted to our rural health training centres and other field health
programmes of the department.
They also carry out Health Management
projects with the guidance of the departmental faculty.
10 • Colloquim for doctors and Community Health Workers working in
rural areas;-
In addition to basic training in health care to various
categories of health workers, it is important that a follow up is done
on the utilisation of the knowledge gained.
methods are followed.
For this purpose, several
At the professional level 9 doctors can seek
elective posting in selected specialities for skill development.
nal colloquim are
Reg.io-
o
7
a
Alumni doctors, permanently working in rural areas, attended this
two—da^ aollaquim uherein they shared their experiences in management
of clinical emergencies with limited resources, motivation of villagers
on health awareness, communicable disease control. use of herbal medicin^, management of social problem, cultural taboos, etc.
The follouj-
ing recommendations were forthcoming as a result of this charing
exper ieneesS- To arrange a one year training programme in family medicine covering
all major el j r i cal, subjects including behavioural sciences, counsellimg, community development etc. | This could enhance the knowledge
and skill level of the rural—based doctors.
Several of the part inl
gating rural doctors have offered to participate ir. this course by
offering thejj? own centres for specific training sessions under rural
conditions.
A shori in—service, skill oriented training for all
they take up their rural postings.
interns, before
This training should essentially
cover maternal and child health.
- To coordinate a national network of our rural graduate doctors1 uith
nur college newsletter acting as the mode of communication between
the members of the rural doctors network.
- Conducting regional colloquia of a similar nature in various parts
of our country on a regular basis.
The present teachers of our coll
ege should participate in these regional colloquia in order to dis—
cover the actual needs of our rural graduate doctors, so that their
teaching methodologies and syllabi can be restructured to suit
rural realities.
11. Integrated child Oevelopment Scheme Anganwadi Traininc Programme:Under this programme, the Anganwadi workers in the Anekal and Attibele
circles are trained in various health programmes uith greater emphasis
8
2
• Extension training in agriculture, water resources and Veterniary
car^ for village youth;- This programme has been organised in the
Dommasandr a, Anekal areas.
The programme consists of imparting field
training and guidance on improvisation of existing methods and provi
sion of expert assistance to extension workers.
The stress is laid
on youth motivation and training in these areas since it has been found
this scheme provides useful outlet for youthful energies and enthusiasm
especially among those who are unemployed and sufficiently educated.
This scheme is seen as a method of providing entry into the field of
agriculture and veterinary care for fresh workers rather than merely
intensify and promote already established rich farmers etc.
Villagers in India often
resort
The training at St. John’s
for th-
13. Integrated Health Care Training;
to indigenous systems of medicine.
various categories of health workers including its own medical students
comp-r Ise training in Herbal Medicine
s s u r e , Homeopathy and Yoga.
Ivi any of
Herbo-minera1 Medicine, Accupreits graduate doctors working in
remote rural areas have substantiated the fact that there is this need
to integrate allopathic Medicine with the other systems of Medicine.
14. Training of Govt, Medical Officers;-
At the request of the State
Government, our departmental staff conduct training programmes in
Universal Immunization Programme methodologies for Govt. ,V|edical Officars in various parts of the State
15.Training of foreign Elective Post/nq ’"edieal Students; Under this
scheme, on an average, 10 — 15 Mgica1 students per year from U.K. $
U.S.A.,Franee, Italy are given experiential learning in Community
Medicine for 4‘ - 6 weeks each at our rural health centres.
SERVICE PROGRAMMES IN COMMUNITY HlhLTH CARE;
1• Me ter no 1 and Child Health Clinics;-
Conducted fortnightly at all
the six subcentres by the faculty o~ the Department these clinics
provide an apportunity "or the women and children to avail themselves
of medical care
by senior
doctors.
The faculty concerned, carryout
10
0
5. Universal Immunization Programme; Ur ganised in collaboration with
whose main
the UNICEF , this programme is a major service programme
objeotive is to achieve rearly 100 percent of coverage with immunization against Diphtheria, Per tusis, T etanus, Policy TEr
Measles for
children below 1 year of age in Anekal, Dommasandra and Bidadi Primary
Health Centres plus a five lakh population in the urban areas as well.
ft. Rural Mobile Clinics;- As part of the Re-Orientation of Medical
Education Programme, three rural Mobile Clinics operate in 18 remote
villages of the Anekal, Dommasandra and Bidadi Primary d^gith Centres.
On an average,
80 to 100 patients attend these clinics per day.
The
Mobile Clinics provide an ideal opportunity to conduct not on.ihy routine
clinical care at the remote villages^ but they also provide an opportunity to carry out specialists care such as ENT, Ophthalmology,
Dentistry, surgery and Dermatology.
diseases can be taught
Basic clinical features of common
especially to para-medical workers at these
Mobile Clinics since the rural patients are not constrained by the awe
inspiring presincts of a large hospital.
This aids in better inerac-
tion between the patients and health worker which is not possible in
the sophisticated hospitals.
7. Serving the Urban under-privileged;- Urban slums in and a'rb'und
Bangalore, are also served by St. 3ohn1s•
Health programme such as
immunisation coverage against the major killer diseases for children 9
maternal and child health clinics for expectant mothers, school health
programmes are some of the urban-based health activities of St. John1s.
In addition, the medico-social unit provides councelling in alcoholism
drug addiction, juvenile delinquency etc.
The trainees learn to
serve the under privileged in all aspects of health care.
8. Referal Services;- Village patients are refered to the Hospital for
tertiary care.
The referal is done by the resident intern at the rural
health centres and followed up by the social workers of the department.
I
»
fl
9
This particular service is all the more important since large number
•of f emales .spatients often hesitate to be attended by our male re'sidential interns.
During these clinics, the opportunity to educate the
mothers on ante-natal, natal, post-natal and child care services are
also availed of.
2. Rural Specialists camps?- As mentioned earlier, the rural Mobile
clinics are amply provided with facilities which are made use of to
organise rural surgical camps in the field of Ophthalmology 9 ENT,
and Dental surgery.
This has been a novel programme.
Through these
rural specialists camps, it has been proved that it is possible to
conduct surgical procedures such as Tonsillectomies, Antral wash,
Cataract extraction, Dental extraction, Dental fillings, and other
surgical procedures, even under General Anaesthesia.
It has been
heartening to note that there has been no post operative complications
or infections reported so far although each camp has on an average
of 30 to 40 operative oases.
The local Youth Clubs are involved in
the management of the organisation and publicity etc.
of these camps.
Follow up care is provided by the residential interns.
3. Natural Family. Planning Services?-
The family Welfare Services .
section of the Depart^^nt of Ob & Gynae of the Hospital accampany the
Maternal and child health service teams and conduct awareness progra
mme in Natural Family Planning among the villagers of the Six rural
subcentres y
An average of 4 to 6 couples accept the Natural Family
Planning each wee<.
4. Factory Workers Health Services?- Under the occupational Health
Services provided for small factory workers, the department is invol
ved actively ir the provision of pre-placement9
factory safety $ducat ion,0ccupational
periodic exarninat ion f
hazards survey and executive
:
:
11
The ENT, ‘Skin, Dental and Ophthalmology departments participate in..”
these specialist camps.
9. Food Hygiene Inspection*-
The Hospital Canteen and other Hesses
in the institution, are subject to regular fgftd hygiene inspections^
This is cone in collaboration
carried ont by the Department fanjlty.
\.T,
A
with the concerned administrative. chief s for eff^tive and prompt
implementation of the recommended control measures.
si
10< Immunization Coverage Evaluation Surveys:-
In collaboration with
■x-
*
the State Government directorate of Health Services, teams of staff
'f 9
from the department conduct specialized immunization coverage evalua>
*
'•
tion surveys in various districtsof the state such as Kolar Disttict.,
Mysore District, Coorg District etc,
11. Freperation of Health Education Materials.-
With a regular artist
as part of the Department staff, several posters, charts, etc., on
Wealth Education has been prepared and used in health exhibitions.
These materials are also borrowed for use by various other institutions
The same is true of audio cassettes prepared in local languages to
depict songs and drama about important issues in Heaith of the
Community.
*
•
•
12) Participatory process^- The main obtjective of the various health
programmes of St. John’s aims at a participatory process, wherein the
the villagers themselves participate in financing health care, supply
of materials and manpower, etc.
the
This is particularly exemplified Sy
Mallur Health Cooperative Centre, which now has its own hospital
JR
building and other facilities provided through a cooperative movement.
which the college initiated in 1973.
Village Health Committees have
been formed at each of the Rural Health Centres, and all decisions are
participatory in nature.
A largepart of the organization of surgical
and other speciality Rural Camps is also under taken by village youth
• <,
a
i
0
12
RESEARCH PROGRAWE IN COMMUNITY HEALTH
The fact that a large number interns are posted to our rural
health
centres each year, has enabled the formulation^ndexecution
pf several research studies, by the staff of the Department.
Some
of the impoFtanfa research projects covered over the years are detefc*tioB of goitre in the Muihar r'egion, health hazards of srd'iculture
workers, house dust mites and allergy in rural areas, Prevalence
surveys of Leprosy, TB and other Major diseases, Polio lameness sdrveys
i
Leprosy health education methodologies, helminthic surveys, Knowledge
attitude practice surveys,
school health surveys, environmnntal
jjealth factors surveys, anaemia and productivity among tea pluckers
Papers have been published by the staff in
al
various lational and internatior/ health journals.
!■ the plantation etc.
Publications in food hygiene and immunization methodologies
have bee.^ written by the staff io English and the local language
ol Kannada as well.
Using appropriate technology, practical methods of solar cooking
vegetable storage devices, smokeless chullas, kitchen nutrition
gardgas etc., have also been evolved by the staff of the Department.
LOOKING BEYONDs
All the programmes outlined, so far 9 are dynamic in nature since
they are updated Constantly depending on the feedback received of
their effectiveness and efficiency.
The emphasis is thus on training
and health education rather than merely the provision of multiple
services.
This ensures that whatever may have been the programme
inputs, the results will bo long lasting, self perpetuating and
effective.
Go m h
EVALUATION - THE NEED, ITS VALUE AND
A4ETHOD
By Dr. Dara S Amar.
J- What is Evaluation?
Evaluation, in lay language, would
mean the separation of the
most valuable from the less valuable and the value-less.
Evaluation measures
1.1 The degree to which objectives <anc1 targets are fulfilled
1.2 The quality of the results obtained
1.3 The productivity of available resources in achieving
objectives
1.4 The cost effectiveness achieved.
Evaluation makes possible the reallocation of
priorities and
of priorities
and
resources on the basis, of changing, health needs.
2. Types of Evaluation:
2.1. Pre-evaluation: It is necessary to establish a baseline at
the beginning of a programme against which to measure the
results.
2*2 Concurrent evaluation: Evaluation should not be left to the
end but should be made from time to time, so that if the
programme is not progressing successfully, modifications can
be made. The programme moves thus:>—
ACTIVITIES
pVAEUATIOrj
/ REVISION )(ACTIVITIES
VALUATION
2»3 Terminal evaluation; The evaluation of the ultimate achievement
of the programme in terms of objectives and sub-objectives
fulfilled and the extent of planned activities carried out.
Evaluation may be approached from the- following angle too
2.4 Evaluation of structure and organisation.
2.5. Evaluation of the Process
2.6. Evaluation of the results.
. . .2
4-
"t1
2
3. Tools usee3 for Evaluation
3.1 Observation schedules
3.2 Records and registers
3.3.Work diaries
3.4 Personal interviews
. 3.5 Health Examination
3.6 Discussions
3.7 Questionnaires.
4. Provision for Evaluation in your progxamme.
The following provisions must be made at the stage of
planning itself.
4.1 Person responsible for evaluation should be specified.
4.2 Amount of time, the personnel can ejive for rv'j'lu~tion work.*
4.3 The funds available for evaluation
4.4.Stages of the programme at whichevaluation will be cone
4.5 Is there a provision in the planning, for making either
major or minor modifications in the programme, depending on
the MfeGd-backn from the evaluation.
5. The process of Evaluationl
A systematic procedure should be- followed in evaluating any
programme. The
The theoretical concept of evaluation is relatively
simple but its practical application can be very difficult,
difficulties have been used as excuses for not
too often, these
starting, but the right approach • is to begin; for onee begun,
experience, techniques, and data grow rapicly. It is better
to start even if only with the evaluation of a few aspects of ,
some activities of a programme, than never to have started at all.
as follows: .
The basic steps in evaluation are
Measuring effectiveness
vi)
vi
i) Statement of objectives
t
of programme
ii) Establishment of Baseline Data
vii) Measuring efficiency ofJT
• programme.
iii) Measuring coverage and Uti
lization of services
viii) Collection of.Tata
iv) Evaluating utilization of
ix) Analysis of Data
Resources
x) Presentation of Results
‘‘ j Activities and Atti
anc3 Recommendation.
v ) Evaluating
tudes of the programme
staff and public
. . . .3
%
3
5•1 Statement of objectives:
■ ■-_• n i
Since evaluation is related to and dependant
on objectives,
the statement of objectives must be sufficiently specific to be
measured.
In fact, the more specific the objectives,
the better
the evaluation.
Two levels of objectives are distinguished.
a) General objective (or aims) which n'ay or may not be
measurable.
b) Specific objective which are measurable.
General objectives only set out the main intentions but not the
details.
e^: To provide preventive, promotive
services to the community.
nc curative health
Specific objectives set out measurable details,
The folloi^ing
are the criteria for making specific objectives.
/*’’primery vaccination” of all child-F
5.11
, A clear definition os what is to re attained; for example /
'
before they are six months-of age.
’z
5.1.2. . A clear statement of the amount or degree of intended
attainment; for example
example-, 100% of the children must
have primary vaccination before ..ca.oh child is six
months old.
5.1.3
A clear statement of the time- in which this degree of
expecfer; for example, ’’between I July
attainment; is expected;
and I September 1963”.
5.1.4 A clear specification-of the geographic location of the
programme; for example
•5.1.5
Bata. Village .
A-clear specification of the particular people, or the
portion of the environment, in which the objective is
to be attained; for example, the parents- of all children
under six months of age should have these children vacci
nated.
The objective might read, ”To persuade parents of children'
under six months of age in Bata village to have all these
children (100%) vaccinated between I July and -I September 1968”.
Sub-ohljectivc-s might include- the’ following:
1) ”To tarry out a house-to-house survey of the village
in order to list the names of all the infants under
six months,”
2) ”To identify leaders especially among the women who can
assist with this survey.”
The programme fs success depends on accomplishment of the
___ , Sometimes a sub-objective may not be
sub-objectives.
direct v related to health. If the objective were ”To get
50% of rhe restaurants in a given locality to reach a speci
fied level of cleanliness in one year”, one sub-objective
might be ”To have restaurant owners buy new uniforms for the
■b
4
5.2 Establishment of Baseline- Fata :
Often termed as "pre-evaluation", it measures the current
Health Status and neec^s of the community sc that these may be
compared again at the end of the programme in order to measure
the changes in health status and
c... fulfillment of the needs of thccommunity.
The Health Status of thc- communi'ty is usually stucied by
collecting data on:i) Age/Sex distribution of population
ii) Mobility of population
iii) Socio-economic levels and factors .prevalent
iv) Birth Rate
V) Bc-ath Rate
vi) Morbidity Rates
vii) K.A.P. Surveys.
FERCEIVEr needs(i.e.
The needs of the community may be
.
the people themselves perceive the need for the programme) and
PROFESSIONAL needs (i.e. what the medical professionals believe
are the needs of the community). Most often both the needs
are beyond the capacity of the resources available for the
programme. Whereas the change in the Health Status
Community at the end of the programme, can be measured guantit Lively,
the measurement of the "fulfillment" of the needs is often quali
tative and therefore subjective. Nevertheless, an effort must
be made, since without the Baseline rata, evaluation cannot begin.
the programme.
The three components measured here are:
i) Geographical coverage •
- ii) Population coverage
iii) utilization rate of the programme services.
5 3 1 Geographical coverage: This refers to the geographical
’
distribution of .thepeople who make use of the programme
services e.g. C^te^rea of a-hospital. If the ■
geographical.area of coverage is large, it cou c mce
.5
IvuT'/V,./
2.)
■
C-ti .
.. •
;
■■
.••
W-’
Az,
5
. 7- -
i) Your programme is popular
ii) Your programme is more of a specialized nature which is
is
generally not available.
5.3.2 Population coverage: This refers to proportion of the
whole population, who are eligible for your programme services.
If your programme is specialized, the coverage is low (eg. only
maternity services) but if your programme is of a general nature
(e.g. Community development projects) the coverage is often 100%.
5.3.3 Utilization Rate: Not everyone eligible for your programme
service, will necessarily use your services, therefore it is
necessary to measure the proportion of the eligible population
who make use of your services.
5.4 Evaluating•utilization of Resources:
Resources are men, material, money and time. These
form the .inputs that is consumed or utilized to produce the
output of .the-programme. Merely because resources are consumed
rapidly, does not signifiy that your programmes is progressing
equally rapidly. What needs to be evaluated or measured, are
the following criteria.
5.4;!
/ 5.4.2
5.4.3
Quantity of Resources available/used.
Quality of Resources available/used.
Rate of utilization of resources in relation to
programme phases/duration.
5.4.4
Eistribution of Resources
(The use.of resources in measuring the EFFECIENCY of a programme
. is denoted later)
its optimization
Evaluation of resource utilization anH
can be. carried out using techniques., in the realm of operations
Research, cost effectiveness■studies etc," which’ are beyond the
scojbe of this present paper.
*
5.5
Evaluating Activities and Attitudes of
staff and Public;
5.5.1. Activities: • These are the number of items of work (eg.
^vaccinating children, making- home-visits, ■registering births etc1)
6
that may be used is the 0 and M technique or the organization
and methods evaluation which measures such matters as division
of work, delegation of authority, co-ordination, etc. Another
type of activity analysis which is increasing/u^ed
the
P.E.R.T./C.P.M. or programme evaluation Review Technique;'
Critical path method in Operations Research. Detailed
reviews of the above techniques are available in specialized texts.
5.5.2 Attitudes: This is most often ignored in any evaluation,
mainly because of its difficult and subjective nature. The
techhiques employed are usually in the form of questionnaires
that arc framed to provide unambiguous replies and the method
of filling the qucstionaircs is through direct personal
interviews and discussions. However, unless the people are
well informed and sufficiently knowledgable on the matter, most
of the responses are guarded, generalized and do not reflect
true attitudes of the people. Though very difficult and subjective,
the technique of direct observation combined with the above
technique, aids in arriving at a fair diagnoses of the changes
or otherwise of the attitudes of the people towards the
progress of your programme:
Measuring Effectiveness of the programme;
Very often, due to constraints on resources and often
due to faulty management, many of the objectives planned
at all or only partially so. Measurement of the EFFECTIVENESS
.
using the following proportion formula, often serves as a
^JogJamSe^a^eHgftJn^t
rough guie’e toyjur achievement.
accomplished
Effectiveness = No. of objectives actually achieved
No. of objectives originally planned.
To have an idea of the extent of individual objectives achieved,
the percentage coverage of each objective may also be calculated.
5.6
Measuring efficiency of the Programme:
This constitutes the most important factor for evaluation
of your programme, as far as your funding agency is concerned.
It relates your programme output to the money spent forthe
programme. However, since money is not the only important
consumable resource, the following proportion formula must be
5.^
t
i
7
Efficiency £ No. of objectives actually achieved.
Total cost (direct & indirect)
actually expended.
5.8
Collection of fata: So far, we discussed WH/vT data to collect
for evaluation of a programme. The following points constitute the
main criteria in the actual methodology of collecting the data:i) How should the- date be collects?
ii) When should the data be collected?
iii) From whom should the data be collected?
iv) By whom should the data be collected?
5.8.1. How----- —?: This is usually in the form of a health
survey for which th’efe are 4 approaches:
i) Using exhisting records/registers for gathering data.
ii) Using Questionaires containing unambiguous .and well
structured questions..••• ■:
.r
iii) Personal interviews and discussions
iv) Health examination of individuals.
When------ ?: Two points to be remembered are
i) Season of the year: eg. If the baseline data ia collected
during an .epidemic of chole-ra, the morbidity rate will be un
usually. high.,
ii) Evaluation procedure: Is the data gathering a continuous
procedure throughout the year or is it episodic?
It is preferable to collect basic data continuously (to overcome
problem(i)) but a more detailed data collection must be carried
out at predetermined intervals. Thus the workload, of the data
collecter is not continuously overburdened.
5.8.®.
5.8.3 From whom.---- ?: Obviously, larger the number of sources
and people from whom data is collected, better would be the
evaluation. However, practical constraints in resources may
..
necessiate the employment of SAMPLING TECHNIQUES. Thus
’’populations at risk” may be measured first due to the economy
achieved. If, however, your programme is a unique and
innovative type, then a group of matched CONTROL population
must be simultaneously studied in order to claim the unique
benefits of your.programme.
8
5.8.4: By whom---- ?; This is entirely dependant on the
resources available for your programme. A lot of project
leaders feel that an independant group of staff, not involved
with the programme, must do the evaluation in order to avoid
any biassed opinions. Though this method may be theoritically
sound, its practical implication can be often futile and
useless. The reason being that many of the project workers
’’feel” that an "outsider” knows little about the actual
conditions of work and so his evaluation and recommendations
In order to avoid such "discontent”
are not always right.
in the organization, a PATT of the evaluation team must
consist of the project workers (actual field- workers and
NOT project leaders/consultantsJ) .so that a balanced opinion
and analysis is made.
5.9: Analysis of Data: Before analysis, the data must be
"collated" ie : checking of completeness of data and sequencing
and tabulation of the data collected. The work of collation
can go on simultaneously with data collection and not be left
to the end.
The amount and type of analysis required will depend on the
problem and complexity of the programme and can vary from simple
tabulation to complex analysis of multiple variants. The
services of a statistician is often required.
6*
Presentation of Pesults and Recommendations:
The presentation of the evaluation report depends upon for
whom it is sent. If it is to the project agency, then it must
contain all details but if it is for publication then a lot of
summarization is required! The report should, however, generally
follow the criteria stated below;
6.1 Be brief as possible
6.2 Pesults.must be tabulated simply
6.3 Emphasize practical implications
rather than theoritical discussions
c/
6.4 Emphasize improvisations e s pe c i a 1 ly |
for field workers.
6.5 Make clear, practical recommendations.
6.6 Illustrations in the form of graphs etc.
should be used.
.. .
BI
t
9
6.7 Figures in tables must not be repeated in the text.
6.8 The FORM/iT of the report should bo as follows:
- Summary of Report
- Aim of Evaluation
- Methods used for Evaluation
- Results in the form of tables/graphs etc.
- Eiscussion of results of evaluation
- Recommendations.
7. Common c1 ifficultic-s in Evaluation:
7.1 Demands and needs often exceed resources and so evaluation
results are often discouraging.
7.2 Inadequate planning, especially for evaluation, beforestart of programme.
7.3 Lack of expertise. Evaluation requires expertise in such
fields as social medicine, statistics, sociology, social
psychology, economics, administration, computer science etc.
Qualified people are thus scarce.
7.4 Techniques and terminologies in evaluation procedures are
strange to programme/projc-ct staff and so they are often
distrusting and uncooperative. Some terminologies have
forbidding names but are basically simple dg. cost-benefit
analysis, network analysis, simulation, management audit,
resource allocation model etc.
7.5 Methodological difficulties.
For example, many health
programmes cannot be measured in quantifiable terms and
their benefit to the people are often subjective, general
rather than specific; and have subtle effects that cannot
be measured.
7.6 Due to the pressure of day-to-day work of the programme,
the ’’demands" to analyse, record ,■ compile, measure activities
etc. "seem" to be an additional burden.
HOWEVER IT MUST BE PEMEWEERED THAT THE OBJECTIVE OF
EVALUATION IS NOT TO CONDEMN OR PRAISE, BUT TO SIMPLY STATE
FACTS SO THAT THE PROGRAMME KV\Y BE
SUITABLY MODIFIED TO
GIVE ITS BEST TO THE PEOPLE FOR ^OM IT SERVES
• I £.C c’w >v» t vt
-/r0
t
"
!■'
,
I
)
(
(\^
ida.
•
<.7 4
• vy/o\j
nv
•
•
"
—.
<?'’^/V ■' I
0
V • (/
<-
85^^^7 ^ y>PV
- J—
z- .■
V
Q'
'fyj
a
r-JM
p 2/ j
Tvv
RURAL HEALTH EVALUATION REPORT
Cem K
(O
The following pages contain a number of incomplete stories.
We want you to read and complete them giving your imaginative
best as to what happened from the point where it was left off.
There are no right or wrong conclusions to those stories.
Please do not try to read all of them first anc1 then go
back over them towrite the conclusions.
+uY°U-haYu °nZY 5 minutes for each. In order to finish all
thZ-aP?ttGS! tlme y°u wil1 havG fo write your spontaneo”reaction immediately after reading each story.
—
•’
*3
J - - .
KVJ i
1Z135
1
1‘
hou?enn?4bacr?Uri<?
finished a year's surgical
(J°(rtor h?0
officership in his medical
house^
mec'ical college
''
tn rhnne
\offroership
hospital. He has
2 yea?s! between two assignments each for a period of approximate!
The first is a government primary health centre only 5
that i+r?s pa ! myical,Folle9e with 9°od roah connections so
fo?th to the Xf°r
h Parents and the doctor to go back and
o^^i^
is L^X^y^fs^wn^i^t^f
It is in an area of
weather and bad roads.
What choice bid he make and why ?
2.
*
Dr. Banerji is ca successful
practitioner who had never been
out of Calcutta.■ 11V
He
has
just
returned from his first visit
to a viPa9? where he hac’
with
--.gone
in talking wj
Er Chatterji,> a young colleague who a wedding party.
was born and brought up in
disjust9at thoTTT/" Strong language
.
a,
—his
revulsion and
c isgust at the lack of- lateri
dps -in
laterines
m the village. He vows, that
he will never go back toa a village again because he can’t bear
the thought of going out to the fields morning and night.
Er Chatterji responds
3.
Er Viswanathan had been surprised to find that his 5 years in
primary health centre hae'. passed as a rapid and pleasant
interlude, His wife and two children
1 ay^.
aged 4-^ and 2^ enjoyed the
life in
+K
• the village and the children played
... ■'-7-d happily with some of
„
the village children.
C._
;
One. spring
day the doctor saw 5 cases of
severe vomitting and diarrhoea in the <’
was^ll^XxVoor^-fou^'
■V^SJC?ller’
next r’o°r and found 7;
the 4i
4 ^?S:g-frand9Ooi?9blSa"L„
child dying of cholera.
- --- - Dr Viswanathan immcbiatcly
4.
On graduation from the r
alt^rnative choices. He could college Dr Gupta had three
Dr-Primary Health Centre where he could accept a job in a government
per mont.
,,
.
start earning Rs.550/iiviW L9m ton±nWKL'/Vc^PriVate
practitioner in
was.private Pract^ioner
in aa big city
junior at 200
-------- : as a Wrk°inat
200 rupees a month •
He was selected to do post-graduate
subject for vhich he
had
^^n2+P3rt“^ar+Prefc-rence. After careful a consid^aV
The following pages contain a number of incomplete stories.
We want you to read and complete them giving your imaginative
best as to what happened from the point where it was left off.
There are no right or wrong conclusions to those stories.
Please do not try to read all of them first and then go
back over them to write the conclusions.
You have only 5 minutes for each. In order to finish all
of them in the allotted time you will have to write your spontaneous
reaction immediately after reading each story.
1.
Dr Singh is a young doctor who has finished a year's surgical
°fficGrship in.his medical college hospital. He has
to choose between two assignments each for' a period of approximate!'
2 years.
The first is a government primary health centre only 5
miles.from the medical college with good road connections so
GasY for both patients and the doctor to go back and
forth to the city. The second is a health centre in an isolated
valley m.the Himalayas, which is supported by his own religious
organization. It is in an arsj.
area of great medical' need where
communications with the outside
--- J are frequently out off by
— world
weather anc1 bad roads.
What choice did he make and why ?
2.
never been
Dr Banerji is a successful practitioner who had never
been
He has just returned from his first visit
Wf °f Calcutta.
to1 a illage where- he had gone with a wedding party. In talking with
Dr Chatterji, a young colleague who was born and brought up in
'
a village
, he
+hreiPrvSS?Sii2 sirong languages his revulsion and
disoustWt
disgust at the lack of latennes m the village. He vows, that
4-u Wxi
nevCr 9° back to a village again because he can't bear
thought.of going out to the fields morning and night.
Dr Chatterji responds
3.
Er Viswanathan had been surprised to find that his 5 years in
One spring day the doctor saw 5 cases of
On going home
o LTh -1 eCneL/oOr
found the 4 year 01d friend of his own
child
chile dying
eying of cholera.
Dr Viswanathan immediately
the village children.
severe vomitting
anC diarrhoe
Vng 4and
diarrh0Ga in the dispensary.
4.
On graduation from the- medical college- Dr Gupta had three
alternative choices. IL
He could ^accept a job in a government
Primary Health Centre where he could
' ’ ' earning
1
-d jstart
Rs.550/- per month
His maternal uncle who was private practitioner
.
‘---- 2.)in a big city
*
invited him to join his clinic as aa junior
at 200 rupees a month.
t0
P°st-graduate ■ work
hn/'L
in a subject for which he
work in
nac no particular preference. After careful corner
The following pages contain a number of incomplete stories.
We want you to read and complete them giving your imaginative
best as to what happened from the point where it was left off.
There are no right or wrong conclusions to those stories.
Please do not try to read all of them first and then go
back over them to write the conclusions.
You have only 5 minutes for each. In order to finish all
of- them in the allotted time you will have to write your spontaneous
reaction immediately after reading each story.
Dr
bmgn is a young doctor who has finished a year fs surgical
ur Singh^is
house^ officership inhis medical college hospital* He has
to choose between two assignments each for' a period of approximate.
1.
The first is government
. .....^1
a g
?
health centre only 5
primary
miles from the medical college with
_J connections so
” good’ -road
that it is <easy^for both
' patients and the doctor to go back and
forth to thef city.
se?:9nc^
a health centre in an isolated
valley in the Himalayas, which is supported by his own relioious
organization.
It is in an area of great medical need where"
wpT+h2iCatl10CS^Wlth .the outsicle world are frequently out off by
y
weather anc bad roads.
What choice- c1id he make anc1 why ?
2.
Dr. Banerji is a successful practitioner who had never been
out of Calcutta,
He has just returned from his first visit
where he
village Wnere
ne hac1
har’ gone
’’ talking
' "
9°nG with a wedding party.
rZ
..^J
wiIn
young-colleague who was
s v TTl; fa young'colleague
and brought,
born and
brought up
was born
un in
in "
«soi?9at Jhe expresses
SV?
strong languages Ihis revulsion and
in s?ro"9.
cisgust at the lack of latennes
village, He vows, that
-s m the village.
1
’ to a village
*
he will never go back
.111^
again
because he can't bear
the
ongoing
out
to
thought
the
fields
r- ru + + " . •
■<
- ---- — s morning and night.
Dr Chatterji responds
3.
Er Viswanathan had been surprised to find that his 5 years in
in+rrWoarVu-cal-» centre had passed as a rapid and pleasant
interlude.
His wife and two children aged 4^ and 2^ enjoyed the
anr thG ch?ldren Piayc-d happily with some of
thf
sJvPrr1in9-+?1WrCj'd-Onc1.Sprin9 day the doctor saw 5 cases of
he
T"9 fT dlarrhoea in the dispensary. On going home
V T
found the 4 YGar 01d fric-nd of his own
Z6? /0037
lie eying of cholera. Dr Viswanathan immediately
4.
On graduation from the medical college Dr Gupta had three
Primarv HrV +hVr<~C+01CGG* Hg could accept a job in a government
Bh Ci tru where hG could start earning Rs.550/- per montl
invited himbo^v W£° waG.PFlvate Practitioner in a big city
He v/as selected tn dTn c^lnic ,as+a junior at 200 rupees a month,
hnd nn nb+iib 1 d0 ,P°st"Pracuatc work in a subject for which he
?narticular( preference. After careful cons id —-it ’-n
THE RAJHARA HMLTH PROGRAMME
A YEARTS EXPERIENCE
.
Since June’1981, Kishor Bharati has sponsored me
to work in a programme, initiated and organised by
the Chattisgarh Mukti Morcha, to build up a health
movement in and around Dalli-Rajhara. This sponsor
ship was an outcome of the belief,held at that time
by many in Kishor Bharati, that reform programmes,
such as health programmes, could not have any signifi
cant and lasting .social impact,unless they were linked
to,end formed part of, ongoing people’s movements. My
own academic and field experience of Public Health work,
and my interaction with experience with the Medico
friend circle, led me to '
broadly share this view..
I was also at that time, looking for a socially sig
nificant and useful role for myself,as a h e a .~I t h prof
essional. It was therefore considered that my being
sponsored by Kishor Bharati for his work would be to
our mut ual adv an t ag e.
The objects of this sponsorship were two-fold vi z ;
L
He althprogramme,
(1 ) To enable me to expbre the feasibility and scope
of CMSS,/and of my own participation in it,
(2)By sharing and discussing my experiences at
Rajhara with others at Kishore Bharati,to enable
the people at Kishor Bharati to enlarge their
general understanding about the role of, and pro
cess of implementing a health programme within
the context of a people ’s movement.
Soon after arriving at Rajhara, I made myself at
home in the Union Office,where I also used to stay.
I was quickly absorbed,although to a limited extent
only, in the day to day life and work of the Union.
Personally for me this was a very stimulating exper
ience, as I had never been involved with any political
work before. However, the lack of any concrete task
to perform was very trying to my patience, particularly
as I had to overcome a lifetime’s conditioning of adhe
rence to the work ethic, and of feeling an obligation
to employ myself"Usefully ”. Nevertheless, I was deter
mined not to rush precipitately into any particular
course of action. I therefore bided my time.
On investigating what ideas the Union leadership had
about the future shape of the health programme, I fon
nd that a decision had already been taken t
to build a
’’PRASUTI GRIH A" (Maternity Hospi tai) near thej
Union Office.The plans were already at an advanced stage,and
the money had been set aside,architectural blueprints
drawn up etc. I also discovered that tie Union Leaders
very clearly expected me to devote a large part of my
energies to clinical curative work. Their ideas on the
actual content of a health programme consisted largely
of what seemed to me to be fairly conventional ideXs,
such as performing Health Surveys, organising clean-up
compaigns, etc. These discoveries
dismayed me greatly.
I was extremely cynical about the effectiveness of curative clinical work; I c ertainly had no ideas of work—
ing in a hospital, and a maternity hospital as that. I
had aleo ]plenty
"
of experiences of how activities such
as health Surveys could degenerat;e into time-filling
Page-2
This was difficult for me to digest, as I was to a political”sanctity’of hea
accustomed
lth work. However,at this time I took a very crucial
decision that determined in a very large measure, the
nature and extent of my future involvement in the health
programme and the Union. This was; that,while maintain
ing and constantly developing my own theoretical under
standing,! would give first priority to the existing
perceptionsand priorities of thepeople, as articulated
in the direction of the Union Leadership. This may seem
like a very conventional decision to a Government Bueaucrat;however,
none of the numerous friends I had ,work
ing in health programmes all over the country,had ever
voluntarily put themselves in such a position. The toplevel health professional is almost always in a position
to determine his own programme priorities and to set his
own goals. I also did not have any well worked out theo
retical arguement for making such a decis ion,it was made
mainly because I found the CMSS atmosphere very exhilerating,and had made up my mind to work with them at any
cost. As it was turned out to be a fateful decision; and
ultimately
led to a totally new theoretical understand
ing of the role of health and other reform programmes in
a people’s movement. This understanding is outlined later
on in tiis paper.
2111®. inaguration of tie programme :The prograr me was inaug
urated on 15th August ’ 1 981 ,during "the Independence BayCelebrations . We had by then articulated an Eight Point
Pro gramme,which was outlined in a pamphlet distributed
at t he inauguration. In t he pamphlet, the basic philo sprogramme-that it was an attempt to direct
phy of the
the energies of Union to goals larger than economic one’s
and designed to set the foundation for a new society-was
outlined . The Eight Point were drawn up on more or less
theoretical considerations; they were:1 . A Tuberculosis Programme,
2. Sanitation and Water Supply,
3. Building a Hospital,
4. Running a dispensary,
5. Carrying out health surveys,
6. Training health cadres,
7. Maternal and child health programmes,
8. Health education.
"3AFAI..ANDO LAN”
The programme was called-*STRUGGLE FOR HEALTH COMPAIGI8;,
("SWASHTHYA KE LITE SANGHASHA KARO ANDOLAN) .
The first major campaign we
carried out was designed to
force the BSP to take its Public Health, ard in particular
its scavanging duties seriously. Thewihole of Dalli-Rajhara
township is under the administrative control of the BS P
Management. The sanitary arrangements throughout the^area
where the Contract Labourers lived were woefully inade
quate, a nd large piles of rubbish could be seen at freq
uent intervals*
The Union organised a massive clean—up
campaign. About 2000 workers together with students and
small businessmen from the town spent an entire morning
loading trucks with rubbish. A number of these trucks
were BSP Trucks commandeered off the road. The sting of
the compaign was in its tail • At the end of the morning,
all the trucks loaded with rubbish were parked infant of
the Mines Office,and a huge procession shouting health
Fa,ge-3
if we had to repeat this Clean-up campand told that
aihgn, the rubbish would be dumped on his lawn. The re
sult was that the BSP has deployed special trucks in
Rajhara specifically designed for cleaning away rubbish,
andall rubbish piles are cleaned every d ay.
Health_Commi11ee:In November ,1981 ,a Health Committee
was chosen to oversee the Health pfogramme . Representat
ives were chosen from each mohalla,by the people living
in the mohalla. At a very big meeting at which all these
representatives
and the Union Executive were present
together, people were asked to volunteer their names for
Health Committee. 107 out of all those who had been
the
chosen volunteered- From among these 107 people,the
and these 107 people together selected
Union Executive
an Executive Committee of 27 men and women.
The Participation of the Health committee members and
ths executive,in the day to day running of the health
programme, and in the hospital construction effort has
been extremely disappointing. Right from the first meet
failed to attend .
ing more than half the members £simjbly
*
ingsattendance
We arranged weekly meet ings;
at tendance al
at these meetings
quickly dwindled, and less than 10 people attended
--------- 1 regularly. However, a few people have takemi a very active
and responsible role both in running the Health Programme and in building the hospital.
The hospital is a large cement
-HQ.SRi±aI,. Const ruct ion
and Steel, building which will house an outpatient depart
ment together with minor surgery and labour rooms,and
wards to accommodate twenty beds. Of two floors, one has
been constructed. The task of constructing the building
has been a truly Herculean one,carried out in the face of
constant Government non-cooperation
and interference.
ere again, while a few of the workers have contributed
a great deal oftieir time and energy in managing the con
struction, reqisitioning materials, etc,the majority of
the health committee as
well as
as the
ordinary mazdoors
the ordinary
mazdoors
as well
ave shown little active
in
interest
work. However
□ interest in the
the work.
However,
■
9
whenever the Union has r*“
requested
volunteers for specific
tasks(loading trucks with bricks,or
getting sand from
the river bed, or the magnif i ciunt <
occasion on which
relays of 200 workers worked all day to panr the
roof
the ground level)such volunteers have always been
°
avai_Lable •
DisKgnsax^sDr.Ashish Kundu.and I had been
— a ttending
Office on
to patients in the
Ugion
Uqion Office
on an adhOc basis for
a very long time, It was decided in January’82 to
improve the physical
arrangements
for seeing -patients
. .
---------------- and
to regularise the working hours for the dispensary. A
temporary shed was built to house tie
o dispensary in the
garage adjoining the Union Office. 7
Initially we had both
men and twomen
-------- colunteers working with
--a us in the dispensary helping to keep
j accounts, dispensing medicines and
generally helping
us to attend to the patient s •
Two men, Takshlal, iand Eval Singh developed into very
good ,skilful and committed
------------ J workers- It is a great tribute to t heir tenecity that t hey
are present in the d ispensary every day, after working
The
dispensary
was inaugurated on 26th January'82.
Page-4
(Women- J
workers /-
But because family responsibilities weighed more hea
vily upon tiem ,Z_t hey w er© unable to attend the clinic as
regularly. However, here as elsewhere, the familiar
pat tern Presented itself. Thus ,while there were a few
gen-uinly excellent workers, most of the people took
little interest in tie actual running of the dispensary,
although from the point of view of the patient load,
we were quite successful.
Working in the. Mohallas: Along with our work in the
clinic, we had decided that, instead of trying to imp
lement our programme diffusely throughout the organis
ation, that we would initially concentrate oh small
areas and work intensively. Accordingly I started liv
ing and working in an area called Pandridalli, and Asshish
Kundu concentrated in an area called Kachhe Dafai.
My work at Pandridalli was not successful. I held num
erous meetings and spent a lot of time trying to explain
pur programme to the people there. We had a large number
of Mohalla meetings, and finally w e w e re able to agree
on a programme to establish a clinic where I would give
part of my time. This seemed logical as this Mohalla was
a considerable distance from the Union Clinic.
Clinic, However,
this clinic never actually started work, as there was no
concerted support for it in the Mohalla.
Dr. Ashish Kundu was much more suffessful in the KachheDafai. He was able to organise the people of the Kachhe
Bafai to set up a small c reche for pre-school children
of working mothers. This doubled as a library for the
Schoolgoing boys in the evening, The schoolgoing boys of
t he area organised themselves into an
ithusiastic group;
they frequently initiated and carried out new ideas, One o f
the reasons for the success of this Mohalla was that al most all the people in this mohalla also worked together
in one co-operative mining society. The discipline and
organisation of the work place reflected on t heir work in
the mohalla as well.
Conclusion ; Looking back a t the end of one year’s
exciting and exhilerating experience ,what general lesson
can we learn from our work?
One of the featuers that puzzled us a great deal, was
the tremendous contrast between the enthusaistic,commi
tted and immesely creative contributions of a few peop
le and one or two small groups, and the overall apathy
towards the health movement of the general mass of the
people. This was particularly puzzling because we were
able to see,every day fresh evidence of the fact that
the people were genuin, ly organised into a militant trade
union movement, for which(even in non-economic issues)
people were willing to work and sacrifice. Our puzzle
ment led us to question one of the b sic assumptions
with which we started the programme; that people org
anised for one issue(Trade Union) will be easy to org
anise for a different issue(Health Movement).
Then what is the advantage of working is a set up
like the CMSS/Chattisgarh Mukti Morcha, inst ead of’ any
Page-5
correctly directed process of social change , and not
simply tinkerring around with a few social institutions
of peripheral importance. The second difference is that
one has ready access to a large number of highly comm
itted political and health cadres- a much larger number
than one could find in a ny ordinary community. The third
difference is that one possesses an indigenous resource
base ' that can sustain the programme.
Whitt can
can a politically conscious health professional
contribute to such a programme? Apart from the obvious
answer—technical skill—these are a number of other poss—
programme is born out of a
ibilties. No revolutionary
vacifflum,but out of the womb of bourgeois traditions* The
revolutionary health professional needs to possess a.
critical awareness of the entire health service tradi
tion, which he can bring to the work at hand.
The other contribution is a more general one-the
ability to
abstract from the life experience
of the
people in the working class,and on t he basis of these
a bs trat i ons , to concretise their aspirations. This pro
cess is known aphoristically as ’’from the people, to the
people” and forms an important part of the work of any
intellectual, working in a Peoples Movement.
In fiajhara , an organised people’s movement has
taken a conscious decision to build and run a hospital
and develops a health programme* While other srnilar org
anisations have in the past, built hospitals or have
attempted to develop decentralised primary health care
services, it is probably the first time that this prog
ramme of social reform, along with other reform programmes
such as the 'anti-liquor campaign ’, have been incorpora
ted into the Central Political programme of the organi
sation.
What isthe object of this programme, a nd why is it
given so much prominence? In order to understand this,
it is necessary to articulate our objedtives in terms
of the general differences between bourgeois reformism
and revolutionary social reform programmes- The first
difference, is that burgeois reformism is directed pri
marily at suppressing the emerging class antagonisms
and contradictions between State Power and people ’s
Power. Revolutionary social reform, on the other hand,
by the very f’act that it is based on a militant recog
nition of class antagonisms and of the oppressive natHire of the State Power, is directed towards precisely
the opposite goal. Consequently, the most important
goal of a revolutionary reform programme is not the ach
I
9
Page-6
The second difference is that revolutionary reform
does not derive its strength from any exogenous group
of "Reformers" standing outside the mainstream oft he pe
ople's movement. .Instead, its primary resources are a
the political consciousness, organised strength and
creative nower of the working class and peasantry. Cons
equently, we cannot take a single step in this programme
without considering the direction inwhich the people want
it to proceed. Any attempt to work out new ideas has to be
preceded by an effort to explain these to the people,and
to establish them in the popular consciousness.
This also means that at any given, moment, the direction of the programme cannot be governed by ”a priori”
considerations of the appropriateness of the measures taken.
The existing direction is always limited by the existing
perception of the people,of thej issues around which the
programme is formed, based on their collective past exper ience. Nevertheless, it is necessary for those leading
p r og ramme s t o hav e a deep and concrete historical knowledge
of similar programmes 9 and of the issues as they exist
.(In the case of health, this^
(---concretely in the community
j~
~ 5 a knowledge of epi dem
possess
would mean that we should
history of technology and
knowledge
of
the
io logy and a I---- —
.’.tealth service programmes-)* This knowledge is necessary
so"that it may be posed ina constant dynamic tension to
existing perceptions, so that the two may come close to
each other in a dialect ical process of successive approximat ion.
The third difference is that revolutionary reform is
vitally conscious of the inevitability of its own failure.
That is, we believe that the ills which owe their exist
ence to an oppressive social order cannot, except marginally,be cured except by a radical restructuring of that
order-that i s-revol ut ion. Consequently, we do not hope
nor expect that our programme will succeed in effecting
more than marginal improvements in the health of the peo
ple or even in the availability of curative care. However,
our attempt is to direct the energies of the people into
the establishment of an institution and a programme which
reflects their aspirations, and in this process presents
to them a redically new vision of an alternative
social
o rde r.
We also hope to create
. within the internal organis
ation of the programme, e,n image of what the social org
anisation of such a programme in a socialistic society
might be. Through the working- of the programme and through
raise,
its internal organisation, we also hope to
questions in the minds of the people about the way in
the
which the .existing social and political structure
existing
e
xisting health s’ervices exxpropriat e rather than add to
the health of the people, and thereby articulate a living
existing social order.
ciritique of one part of the
i
Gt? m H
Re: [mfri^ndcirclp] INTERNET AND HEALTH: is there a doctor?
SuEbjjeciis R<Bo [mmiTirneMdciirde] UNTIERN1ET AND HEALTH: ns Ulhieir© a doctoir?
Date: Wed, 23 May 2001 10:04:36 +0530
Firomm: ’’tapasvi73” <tapasvi73@yahoo.com>
RejpDy-T®: mfriendcircle@yahoogroups. com
T©: <mfriendcircle@yahoogroups.com >
hello sir,
telemedicine seems to be doing well in Mozambique, but certain issues are there which must be
answered.
if some one refer to a doctor via telemedicine, now suppose that perticular doctor is not practising
ethically & only interested in moneymaking then how to rely upon the advice. As for example one
doctor at village refers a ECG to cardiologist via telemedicine, now if that doctor is not a rationlist may
advice for angiography for it. which might be not required at all. many doctors will find it suitable to
increase their practice via telemedicine with finding a base in rural/remote area too.MAny big private
hospitals may take advantage & may find telemedicine for their profit making by unneccesary advices
for referal via telemedicine.
Some one has also raised the medicolegal issues relating to the telemedicine. So before we may go for
it in our country we must think on these issues. ISRO has started its pilot project for telemedicine in
gujarat for three months. Let’s hope for the best.
-----Original Message----From: DOLKE
To: MFC eForum
Sent: Tuesday, May 22, 2001 9:56 AM
Subject: [mfriendcircle] INTERNET AND HEALTH: is there a doctor?
http://www.itu.int/newsroom/wtd/2001/FeatureHealth .html
INTERNET AND HEALTH: is there a doctor?
Picture this. A young child in a poor, rural town, playing football by
the
' side of a busy road, runs out on the street to chase the ball and is
hit by
a car. The frightened parents take the unconscious child to the nearest
medical centre for emergency aid. The doctor, a young, eager but
inexperienced practitioner fresh out of medical school, takes an X-ray
of
the child’s skull to determine the extent of the injuries. Although the
child is stable, the doctor faces the difficult dilemma of either
providing
treatment locally, based on his or her own diagnosis or sending the
child on
a long, arduous and perhaps dangerous journey to the capital for
treatment
at the country's better-equipped hospital. It is a choice which could
have
life or death consequences.
Now picture the same scenario, but with a different ending. The injured
child is brought to the rural doctor. The doctor takes an X-ray of the
skull, but instead of making the diagnosis, he or she sends the image
via
the Internet to the hospital in the capital so that more experienced
doctors
can make the call, The image is sent via low-cost teleradiology
equipment,
which not only allows X-rays to be sent in a digital format clear
enough for
experts to identify the extent of injury, but also allows the experts
to
send advice back to the doctor for treatment. The doctor successfully
treats
1 of 6
<2-3 )6
5/24/01 3:04 PM
Re: [mfri^ndcircle] INTERNET AND HEALTH: is there a doctor?
the child, who soon returns home and continues to play football with
friends, well away from the busy road.
o
A vision of the future? No! A snapshot of reality in countries such as
Mozambique shows that ’’telemedicine ’’ is making a real impact on the
availability of health care and health care information in the
developing
world. Telemedicine is a term which has emerged to describe the
provision of
medical services and health care via telecommunications-based systems
such
as the Internet, either by terrestrial, wireless or satellite links,
Mozambique is being viewed as perhaps one of the most successful
examples of
telemedicine in action. In cooperation with the International
Telecommunication Union, through its Telecommunication Development
Bureau
(BDT), the government of Mozambique has established a telemedicine link
between the central hospitals of Maputo, the capital, and Beira, the
country
’s second largest city some 1000 km away from the capital. The link
allows
the hospitals to exchange messages regarding laboratory results and
treatments as well as radiographs.
As a result, doctors in Beira can refer cases to the central hospital
in
Maputo for primary or secondary opinions and to send medical records to
the
capital so that experts there can determine whether patients facing
more
serious problems can be treated locally or transferred to Maputo, The
project was especially important for the hospital in Beira since it had
no
radiologist when the telemedicine link was established, ’’They were
handling
roughly ten thousand X-ray films per year, ’’ noted Leonid Androuchko, a
Geneva-based professor of telecommunications who formerly headed an ITU
telemedicine programme. ’’On simpler cases it was easy to interpret the
image
locally, but for more complex cases they had to refer to the capital.
That
was not only frustrating but very costly.
For developing countries, such telemedicine projects tend to be
relatively
inexpensive to implement. Mr Androuchko said the approximate cost in
hooking
up Maputo and Beira was around USD 50 000, with the main cost being the
digitalization of the X-ray images. Mozambique's Government is so
satisfied
with the results that its Prime Minister has written to the ITU to ask
for
its help in establishing additional telemedicine links with a hospital
in
Nampula, the country's third-largest city, with part of the cost to be
covered by the government.
A similar project is being implemented in Senegal, where a telemedicine
link
will be established between the country’s main hospital in Dakar Fann
and
regional hospitals in the towns of St Louis, Djourbel and beyond. The
link
will not only allow for the transmission of medical images and medical
information, but will also allow doctors to discuss cases in detail via
videoconferencing. As in Mozambique, the telemedicine connection is
especially important for the regional hospitals in interpreting X-ray
images
2 of 6
5/24/01 3:04 PM
Re: [mfriendcirclp] INTERNET AND HEALTH: is there a doctor?
since neither hospital has a staff radiologist
Additional telemedicine projects have been set up with ITU assistance
in
countries such as Bhutan, Georgia, Malta, Uganda and Ukraine. In
Georgia,
the project is relatively simple and involves trans-telephonic
electro-cardiogram (ECG) monitoring systems. With this simple system, a
cardiovascular patient holds a small, box-shaped ECG device that
transmits
information to a hospital-based cardiologist, The remote monitoring
allows
cardiologists to monitor their patients' progress after they are
discharged
from the hospital without the time and expense of frequent return
visits.
Petko Kantchev the coordinator of ITU’s telemedicine projects, says
the
benefits of telemedicine are not only the ability to bring rural areas
into
the net of the national health care service at relatively low cost, but
also
the ability to better utilize the intellectual resources within a
country.
"The typical rule in a developing country is the concentration of the
most-able intellectuals and professionals in the capital," he noted.
"These
people, who tend to be very few in number have extremely important
know-how
and experience which is pertinent to the local environment. They are
more
familiar with the diseases and illnesses which can be handled locally
rather
than consulting with doctors in Canada, Russia, Germany or the United
States."
Dermatological diseases are an example, of a type of illness which is
prevalent in developing countries and where telemedicine can facilitate
treatment. A telemedicine project, now being considered in Ethiopia,
would
allow digital and video images of patients in rural areas suffering
from
skin disorders to be sent, via the Internet, to doctors in the capital..
These doctors would then consult among themselves and forward advice on
treatment. The project has become more feasible thanks to the
widespread
availability of digital cameras, "There are a lot of skin disorders in
these
countries which rural medical staff don’t know how to deal with,"
Kantchev
noted.
An area in which the Internet can instead make a difference is in the
support of medical research and the training of health professionals.
After
all, the Internet was until recently a purely academic/research network
- a
function which still holds a strong and solid presence among academics
and
researchers in developing countries.
The possibility of accessing a vast source of medical information and
professionals on a global scale provides unique learning opportunities
for
medical students and other health professionals. Distance-education
opportunities are not new, but the Internet and its unique
communication
features provide a new and unprecedented medium for accessing education
3 of 6
5/24/01 3:04 PM
Re: [mfripndcirclp] INTERNET AND HEALTH: is there a doctor?
services worldwide. Distance education in the health sciences was
hampered as .in other disciplines - by some of the traditional problems which all
non
face-to-face education suffered: poor interaction with tutors and no
rate a sense of
interaction with other students, a slow response rate,
isolation
and lack of incentives to continue, therefore, a high drop out rate.
Furthermore, in the medical sciences there were considerable problems
in
sharing images and explaining hands-on procedures.
With the Internet, most of these problems are gone. Even with a slow
Internet connection, the educational experience can be dramatically
different .
Another way in which the Internet is making a difference is in the
easy,
fast, and almost free distribution of high-quality educational material
to
support the activities of health workers working on the ground at the
community level. An example of this is the launch of the Tools for Life
Kit,
a versatile health communication kit that includes Activity Cards and
Information Cards designed to enhance community health workers'
education
and counselling skills. The Tools for Life Activity Cards can assist in
engaging communities in relevant health issues, such as safe
motherhood,
nutrition and infant health, diarrhoea, prevention of common illnesses
and
reproductive health, The Tool Kit has been posted on the Web for
comments
and improvement, The open and collaborative nature of the Internet has
in
the first three months of the pre-test, attracted more than 5000
visitors
from 29 countries to the 'Tools for Life’ website many of whom
haveprovided
valuable comments and contributions to the design of the material
Advocates of telemedicine are quick to note that it is not a panacea
for a
nation’s health care woes. In fact, a number of telemedicine projects
introduced in the late 1960s and early 1970s failed for reasons such as
inadequate medical regulations in force, the high cost of equipment,
lack of
suitably trained staff and administration and, in the case of
tele radiology,
poor image quality, "To make it work, you need a good telephone line. a
good
ISDN connection or a VSAT (very small aperture terminal) link," noted
Kantchev. "You also need good local leadership to ensure proper
implementation and follow-up." Many developing, countries are setting up
national committees or task forces comprising representatives from both
the
telecommunication and health care sectors. These groups play a very
important role in enlisting support from all stakeholders in the
country and
in formulating viable telemedicine projects.
Most telemedicine projects call upon a mix of delivery paths.
High-precision
remote surgical interventions, for example, or remote access to very
complex
imagery such as brain scans, dictate the use of high-speed broadband
telecommunication links. However, in many cases, the public Internet
offers
huge possibilities. It provides fast access to medical data and
4 of 6
5/24/01 3:04 PM
Re: [mfri^ndcircte] INTERNET AND HEALTH: is there a doctor?
expertise
nationally, regionally or globally, thus bringing medical care to
patients,
who would have been otherwise unattended. Whether for seeking advice on
standardized symptoms or real physiological data, including a patient’s
vital signs from on-line doctors that can be anywhere on the planet,
the
Internet is increasingly being exploited. The increasing quality of
videoconferencing and audio tools on the Internet are also providing a
valuable resource for live, remote consultation and diagnosis.
The continuing decline in the cost of telecommunications and
information
technology, as well as great leaps in digital imaging and compression
techniques have spurred a new wave of enthusiasm for telemedicine,
particularly in developing countries. It is in these countries where
telemedicine’s greatest asset - allowing specialist medical expertise
to be
delivered to regions and locations where doctors are few on the ground
shows the best prospects for success. For governments struggling with
limited health care budgets, a shortage of doctors and other health
care
professionals, dispersed rural hospitals and poor transportation
infrastructure, telemedicine may help them overcome some of these
difficult
challenges in meeting the health care needs of their citizens,.
When opinions count
The Research Institute of Radiology and Interventional Diagnostics in
Tbilisi, Georgia, provides a number of sophisticated medical services
using
modern technology, From time to time, however, doctors at the Institute
seek
to verify some difficult cases with colleagues from other medical
centres
within Georgia and abroad. The telecommunications link connecting the
Institute with other medical centres allows them to obtain a second
opinion
quickly and efficiently but it also provides enhanced access to medical
information within the nation and abroad.
In September 1998 the first medical file including the X-ray film was
sent
over the Internet to Switzerland for a second opinion. Specialists from
the
Centre of Imaging Diagnostic in Lausanne studied the case, and within
48
hours the Institute of Radiology in Georgia received an opinion with
recommendations for the treatment. During September and October of
1998,
more than 10 cases coming from Georgia were analyzed by high-level
medical
professionals in Switzerland-several of the cases under consideration
were
of professional interest to doctors at both ends of the line.
To unsubscribe from this group, send an email to:
mfriendcircle-unsubscribe@egroups.com
Your use of Yahoo! Groups is subject to the Yahoo■ Terms of Service
5 of 6
5/24/01 3:04 PM
Re: [mfri^ndcinc’e] INTERNET AND HEALTH: is there a doctor?
Yahoo! Growps Sponsor
Website Semees
Yahoo! Website Services- Click Here!
To unsubscribe from this group, send an email to:
mfriendcircle-unsubscribe@egroups .com
Your use of Yahoo!
6 of 6
Groups is subject to the Yahoo! Terms of Service.
5/24/01 3:04 PM
- Media
 RF_COM_H_10_SUDHA.pdf
RF_COM_H_10_SUDHA.pdf
Position: 3117 (3 views)