MFC 5TH ANOTHOLGY HEALTH IN THE 1980'S ISSUES AND PERSPECTIVES
Item
- Title
- MFC 5TH ANOTHOLGY HEALTH IN THE 1980'S ISSUES AND PERSPECTIVES
- extracted text
-
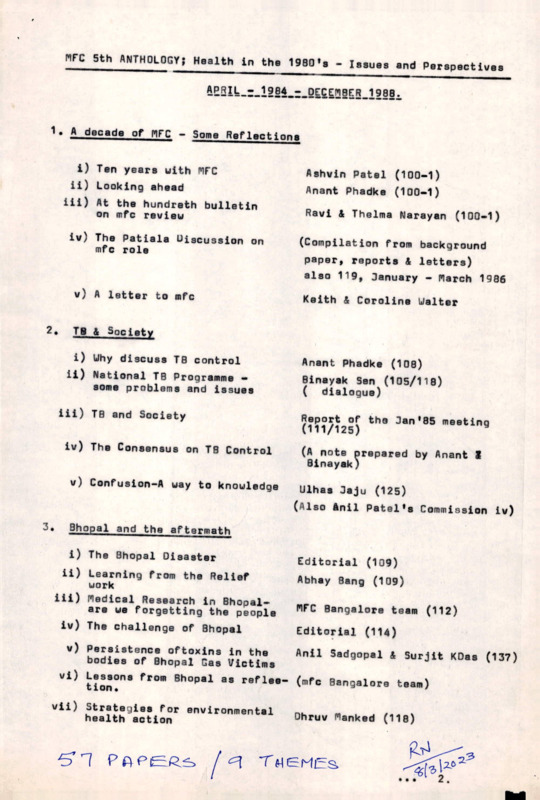
MFC Sth ANTHOLOGY; Health in the 1980'3 • Issues and Perspectives
APRIU-r-lEeA^^DECEriiBER^iges^
1• A decade of MFC • Some Reflections
i) Ten years with MFC
ii) Looking ahead
iii) At the hundreth bulletin
on mfc review
Ashvin Patel (100-1)
Anant Phadke (100-1)
Ravi & Thelma Narayan (100-1)
iv) The Patiala Uigcussion on
mfc role
v) A letter to mfc
2e
(Compilation from background
paper, reports 4 letters)
also 119, January - March 1986
Keith & Coroline Walter
TB & Society
i) Why discuss TB control
ii) National TB Programme —
some problems and issues
Anant Phadke (108)
Binayak Sen (105/118)
( dialogue)
iii) T0 and Society
Report of the Jan'SB meeting
(111/125)
iv) The Consensus on T0 Control
v) Confusion-A way to knowledge
(A note prepared by Anant I
Binayak)
Ulhas Jaju (125)
(Also Anil Patel's Commission iv)
3.
Bhopal and the aftermath
i) The Bhopal Disaster
Editorial (109)
ii) Learning from the Relief
work
iii) Redical Research in Bhopalare we forgetting the people
iv) The challenge of Bhopal
Abhay Sang (109)
MFC Bangalore team (112)
Editorial (114)
v) Persistence oftoxins in the
Anil Sadgopal & Surjit KDas (137)
bodies of Bhopal Gas Victims
vi) Lessons from Bhopal as reflee (mfc Bangalore team)
tion.
vii) Strategies for environmental
health action
Dhruv flanked (118)
TMGMiEs.
>
2.
• £
Family Planning controception and Women1a Health Issues
i) Family Planning in India:
Theoretical assumptions,
implementation and alternatives
Leela Visaria
ii) Editorial
Sathyamala (129)
iii) Two decades of sterilization
Modernization and Population
growth in a rural context
Stanley A freed(129)
and Ruth S freed
iv) A femanist understanding of
contraception
v) Injectable contraceptives
Manisha Gupte (121)
vi) The E.P. Case
Mira Shiva (143-144)
vii) Use and abuse of Bio-Medical
T echnology
Amar Jesani (124)
viii )Sex determination and female
f oeticide
Garbha Parikshan
Virodhi Maech (146)
ix) Dialogue
Abortion
Victim blaming is not the
solution
Arun Gadra (146)
One Daughter Family: Fact or
F ancjj
5.
(MFC Annual meet rejbort
mfcb131)
Padma Prakash (113)
Amar Jesani (146)
Ulhas Jujoo/S.P. Kalantri
(146)
Child Health Issues:
i) Child health in India what is our commitment.
ii) Child health in India
Ravi Narayan (106)
Editorial (133-134)
iii) Child health in India
Report of XIV Annual Fleet
(138)
iv) Paralytic Poliomgetitis A tragedy on the rise
Gloria Surrett (130)
v) Universal child immunization
and child survival: A positive
view.
Ashok Bhargaea (133-134)
Anil Patel
vi) Sex differentials in Nutritional
status in Rural Area of Gujarat
State - An Interim Report.
Leela Visaria
vii) Child care and the prosperity
of Punjab - A reflection.
Sameer Chaduhuri (106)
viii) Blened are the small in sizeif they are Indians.
Kamala S. Jaya Rao (115)
xx£
3
6• Rational Drug Policy 13sues:
i) Doctors role in the RDP Movement
ii) A letter to the Drug Controller
iii) Drug awareness and Action
iv) Fighting for a peoples Drug Policy
— the KSSP experience
Editorial(l03)
Anant Phadke (107)
Editorial (107)
B Ekhal (Dec 85)
v) Scientific medicine
(112)
7. Technology and Health Care.
8.
i) Medical Technology:neither glitter/
nor gold.
Ulhas Oajoo/S.PeKalantri
(145)
ii) Emerging Medical Culture
Ulhas Sajoo (115)
iii) Clinical perspective: Chest
Radiography
S.P. Kalantri (145)
iv) Beware of X rays
S.G. Kabra (145)
v) Transtechugue aspects of Disease
& Death
M<La Kothari &
Lopa A. Mehta.
Primary Health care issuess
i) Towards an appropriate strategy
Eood is the Hands of Big Industry
iii) Logistic support and facilities
for primary health care
iv) Pricing the medical care in
Government hospitals-problem and
alternative solution
v) The Indo V vaccine Action Programme
- A recipe for Disaster
vi) Choloroquin, Cholera and mfc
vii) Media as a tool in Health Action
9.
A
Ulhas Oajoo (102)
Kamala S. Jayaroa 014^
Ashish Bose (137)
Abhay 4 Rani Bang (39)
Proful Bidwan
(148)
Editorial (148)
V imal Balasubramanian
(127)
Politics of Medical Work
i) Conventional medical work
ii) Radical Medical work
iii) Myths perpetucted by the
Voluntary Health Sector
Anant R.S. (141)
Anant R.S. (142-143)
Sathyamala (142-143)
I
4
9. iv.
v.
Narmada Project and Retribals
The HARD Strike - A view Point
10. when Rome is Burning: A Dialogue
'
!\
-*-*-*-*-*-
'I
ARCH, Mangral (104)
Sanjay Nagral (108)
Arun Cadre &
Jyothi Cadre (124)
Dileep Havalankar (126)
Kamala
Oaya Rao (126)
Mukund Uplekar (126)
Sujit K. Das (128)
Marie D* Souza (129)
Dhruv Mankad (130)
Rita Priya (130)
POTENTIAL ARTICLES FOR S’th ANTHOLOGY
Subject
Author
A Feminist Understanding of
Contraception
Manisha Gupte
124
Use and Abuse of Bio-Medical
Technology (Amniocentesis A Case Study)
Amar Jesani
124
When Rome Is Burning
Arun & Jyothi Gadre
Confusion - A Way to Knowledge
U.K. Jajoo
Tuberculosis and Paramedical
Workers
Marie D’Souza
mfc bulletin
No,_____
^21
125
125
\
\
126
When Rome is Burning (response) Dileep Mavalankar
127
Media as a Tool in Health
Action
Vimal Balasubrahman
127
hen Rome is Burning
responses)
Kamala Jaya Rao
Mukund Uplekar
128
Integration of Medical
Systems (A theoretical
Perspective and Practical
Blue Print)
S.K. Kelkar
128
When Rome is Burning
(response)
Sujit K. Das
129
When Rome is Burning
(response)
Marie D*Souza
130
When Rome is Burning
(responses)
Rita Priya
Dhruv Mankad
131
Family Planning in IndiaX:
Theoretical Assumptions,
Implementations and
Alternatives
(XIII mfc Annual Meet, Kaya)
Leela Visaria
131
Integration of Medical Systems
(response)
B.K-w Sinha
131
A Letter to mfc
Keith and Caroline
Walker
• •2
:2s
Author
mfc bulletin
No.
Subject
132
The Epidemiological Approach :
Its Elements and its Scope
Ritu Priya
132
Injury Prevention and Basic
Preventive Strategies
Dinesh Mohan
133 &
134
Universal Child Immunization
and Child Survival x A
Positive View
Ashok Bhargava &
Anil Patel
133 &
134
The New Drug Price Control
Order - A mockery of rational
planning
Anant
135
Persistence of Toxins in the
Bodies of Bhopal Gas Victims
Anil Sadgopal 6c
Sujit K. Das
136
Sex Differentials in Nutritional Leela Visaria
Status in a Rural Area of Guja
rat State : An Interim Report
- Part - I
137
Sex Differentials in Nutritional Leela Visaria
Status in a Rural Area of
Gujarat State - Part II
137
Logistic Support and Facilities Ashish Bose
for Primary Health Care (Crucial
Role of Physical Accessibility)
138
Child Health (XIV Annual Meet
of mfCf Jaipur)
Sathyamala
139
Pricing the Medical Care in
Government Hospitals :
Problem and Alternative
Solution
Abhay and
Rani Bang
141
Politics of Medical Work
Part I : Conventional Medical
Work
Anant
R.S
142
143
Politics of Medical Work
Part II : Radical Medical Work
Anant
R.S.
142
143
Politics of Medical Work - III
Myths Perpetuated by the
Voluntary Health Sector
Sathyamala
142
Issues for Debate on Peoples
Science in Health Care
C.R. Bijoy
R.S.
• •3
3
mfc bulletin
No.
4
Subject
Author
143
144
The E.P. Case
Mira Shiva
145
The Trans-Technique Aspects
of Disease and Death
M.L. Kothari and
Lopa A. Mehta
145
Beware of X-Rays
S.G. Kabra
145
Clinical Perspective : Chest
Radiography
S.P. Kalantri
145
Medical Technology : neither
glitter, nor gold
U.N* Jajoo &
S.P. Kalantri
146
Patient*s Right
Anil Pilgaonkar
146
Sex Determination and Female
Foeticide in Baroda
Garbha Parikshan
Virodhi Manch
146
Victim Blamin Is Not The
Solution
Amar Jesani
146
Dialogue : Abortion
Arun Cadre
146
One Daughter Family : Fact
or Fancy?
U*Ne Jajoo &
S.P. Kalantri
I Block, Koramangala,
Bangalore - 560 034.
3rd August 1992
PHONE ? 53 15 18
k Dear Friends,
Greetings from Community Health Forum!
We had a very interesting meeting on 11th July 1992, when the CHC
Team presented an report of its activities and concerns mostly
through visuals and we got an enthusiastic and stimulating
response from 48 of our Forum members and associates. Many ideas
and suggestions were shared and CHC got a lot of stimulus to work
upon in the months ahead, A detailed proceeding of the meeting
will be sent to all of you, shortly, A short summary is given
overleaf for the benefit of those who could not attend.
This is just to keep you informed that the next two Community Health
Forum Meetings have been arranged.
1o Date
; 14th August 1992 (Friday)
Tine
: 2.30p.m. - 4.30 p.m.
Venue
: Ashirvad,
30, St.Mark’s Road,
Bangalore
560 001.> (Phone 2 21 01 54)
Dr. Vanaja Ramprasad will report on the RIO Conference issues and concerns that should be of relevance to us as
Community Health action initiators.
2. Date
z 5th September 1992 (Saturday)
Time
: 10.30 a.m. - 12.30 p.in.
Venue
s Ashirvad,
30, St. Mark’s Road,
Bangalore ~ 560 001 (Phone; 21 01 54)
Prof. Ravi Kapur, Deputy Director, National Institute of Advanced
Studies (better known to all of us as one of the key pioneers
of the Community Mental Health work of NIMHANS) will share his
perspectives onllYoga and Mental Health’’ deriving inspiration
from his own experiments in this area.
Shirdi Prasad, the facilitater of our Forum has gone .to Sri Lanka
on a special assignment to review Community Health needs of
refugees from the troubled zone..He
He will give us an additional
first hand report on <one of these occasions,. depending on when he
returns.
We look forward to your participation with the same enthusiasm and
numbers witnessed on 11th July 1992.
A pamphlet and newsletter released on 11th July 92 is enclosed for
all those who could not make it to that meeting.
With best wishes from the CHC Team.
See you on 14th August and 5th September.
1
_si ncerelv.
18 percent response. The latter was prompted by
a crisis situation which arose when the then editor
perceived a lack of participation and support and
serious discussion regarding continuation of the
bulletin ensued.
The survey showed an overall
support for the bulletin, which then got a fresh
lease.
1978
1979
Readership surveys
Critique :
Abstract analysis
Too much criticism
Too little constructive suggestions
Increasing formality
Suggestions :
— More experience reports
— Recent advances and appropriate
health care techniques
— More editorials
— More organisational news
— More variety in authors
Responder characteristics :
Medicos — 68%
Non-medicos — 32%
Members — 65%
Field Workers — 10%
Medical College teachers — 35%
Response :
Most popular — title articles and
materials
Bulletin useful — 90%
Existing system irrelevant — 90%
Alternative possible — 90%.
fb)
Availability of articles : Though the Bulletin
appears to have appeared regularly, editors
have had their range of reading and article
extracting ability stretched to the extreme,
resulting in frequent crisis. Typically in
1980, there was an appeal in June as fol
lows : "If this state continues the last issue
will appear in July”.
The crisis was most
often got over by reprint of suitable articles
from other sources. Many were very good
and added an important dimension to the
bulletin. However, lack of original articles
can be not only a health hazard to the editor,
but it also question the creativity and dyna
mism of our membership 1
(d)
Printers' devil : This has not been as much
of a problem as it could have been in a small
bulletin of this nature because of a series of
meticulous proof readers. On occasion, how
ever, it has caused some degree of embarrass
ment and often comic relief. Recently, in
the front page of the bulletin, 'health' our
main preoccupation was wrongly spelt and
'mgc' not 'mfc' was committed to achieving
it by 200 A.D.
With the increasing diversity in membership,
MFC may have to consider producing bulletins/
newsletters directed to stimulating 'thought cur
rents' at different levels.
A bulletin with this perspective and supported
by subscriptions and donations only, is bound to
have many problems. The three most important
often reported in the bulletin were :
Focus : With the diversity of readership and
their expectations 'selection on material for
the bulletin is a gymnastic more difficult than
walking on a tight rope'. (31).
Finances : This has been a chronic problem
throughout, but the remarkable ability of con
sequent publishers to continue against all
odds deserve real kudos. MFC has fiercely
guarded its independence by committing itself
to a policy of financial support by subscrip
tions and personal donations only. It was felt
that external project funding would result in
some inevitable institutionalisation, possible
loss of independence and very likely decrease
in the personal support of committed mem
bers. The increasing deficit has constantly
challenged this stand and the discussion in
1983 finally resulted in a more open policy of
funding with certain restrictions to maintain
our value stand (87).
The future
Some problems
(a)
(c)
The 'demystification of medicine' and 'the
evolution of a style within reach of the common
man' are two important but neglected dimensions
in the bulletin. The fact that many of our member
writers also write for the popular press in the
regional language is some cause for satisfaction
though this needs to be promoted much more
through MFC in the future.
In conclusion the hundredth milestone of our
bulletin has been reached through an exciting and
exacting collective endeavour. What has been the
contribution of this effort to health related thinking
in India in the last decade- only the future will tell.
Ivan lllich, when interviewed in 1978 is reported
to have said that "the bulletin was the best periodi
cal in the third world which analyses health struc
ture and its problems”. Two readers in the 1979
survey on the other interestingly felt that the
the health care system in India was relevant and
that the bulletin had been responsible for their
opinion! Only our readers can decide where we
stand between these two extremes.
9
I
IpC
K
-iv11
I
prescribing. Certain unusual problems like Lathy
rism, discrimination against women in health,
disaster medicine etc., have also been presented.
By and large, however, tne range has been within
ihe traditional boundaries of medicine — both
clinical and community with a strong preoccupa
tion with nutrition, health service policy and drug
issues.
may be representative of the fact that many
of the analysts of yester years are deeply
immersed in action today. In turn these rea
listic issues may be instrumental in stimulat
ing further activism: in MFC circles.
Here
again we are vulnerable to the criticism that
the emphasis on drug issues represents
medical bias but this is inevitable in our pre
sent doctor oriented predicament.
Non-medical issues which are vital to health
care have been covered peripherally with stray
articles on green revolution, dairying, soya bean
and low energy economics.
Vocal Figures
Feature
Three areas stressed in the MFC manifesto
have been particularly neglected.
These being
demystification and popularisation of medical
science, humanisation of medical/health practice
and the open-minded enquiry into non-allopathic
systems of medicine and non-drug therapies.
Does this reflect the existing professional/
medical bias of the group?
Even within the traditional boundaries of
medicine certain issues like ecology and environ
mental health, health problems of tribal regions
and urban slums, workers health, the clinical
investigation, business, unnecessary surgery, malpraxis, the nuclear epidemic and the relevance of
existing research in the country have hardly been
considered. Emerging issues important in a wider
context but relevant to the health movement like
pedagogy, communications, participatory manage
ment and humanistic psychology among others
need also to be included.
1.
2.
3.
4.
Book reviews
32
26
24
17
64
14
1
13
8
8
2
4
2
8
2
8
Activity reports
a. mfc groups 8
b. health
projects
1
(c)
Activity/Project reports : Reports by small
groups all over India with an MFC perspec
tive have been featured on and off. Reports
on projects like Jamkhed, Gonoshasthaya
Kendra and CINI have also appeared. Consi
dering the wealth of field experience gained
in India in the last decade this is an area
I
7
26
19
Discussions/dialogue : The thought current
nature of MFC should have made these a dis
tinctive feature of the bulletin. The experience
has been different. The first phase saw a
very active response from members. Even
though these were often the same inveterate
discussants, they set a healthy precedent. The
second phase saw a very active response from
members. The second phase saw an increase
in this phenomena with a much wider cross
section of readers participating in columns
such as Hyde Park/Dialogue and contributing
letters to the editor. In the last four years
this phenomena has begun to wane and should
be a cause of concern. Are bulletin readers
so busy with their own local preoccupations
that they do not find time to participate in
discussion or is the Bulletin not adequately
thought provoking? Are there many other
factors?
Only a readership survey could
probably throw light on this.
The format of the bulletin has shown much
variation but certain basic features have remained
constant.
These have been the key
L^ad articles :
feature of the bulletin. They have included
original articles written by members and con
tacts as well as reprints from other journals
and sources. These articles have been very
responsible for the reputation of the bulletin.
The selection has been surprisingly consis
tent in terms of relevance and analysis in
spite of the fact that there has never been a
very clear cut editorial policy — our mani
festo reworded from time to time being the
only guiding principle.
Of late the articles
have moved from a more abstract analysis of
issues like health policy to more concrete
like drug misuse, community health worker
and health education.
This concretisation
Articles
a. original
32
10
b. reprints
Letters to
Editors/readers
dialogue
49
(b)
Features
(a)
Phase of bulletin
1-25 26-50 51-75 76-100
I
CHC / ?1EP /
Research Project
Strategies for Social Relevance and'Community
Orientation in Medical Education
:
Buildina.
on the Indian Experience
A
PROCESS
REPORT
Community lldalth CeM ,
Jyune
e
Bangalore#
1992 \
Sponsored by f Christian Medical AssociaVion of India (CMAI).
Catholic Hospital Association of India (CNaI), Christian
Medical College, Ludhiana ( 3MC-L ) .
\
* Society for Coniiiuni ty HealtH Awareness, Research and Action
No. 326, V Main, I Block, Koranian^’ala, Bangalore - p60 034.
/
I ( i i i)
needing much more attention.
Reports of
well-known projects are not as important as
sharing by friends of the little lessons in their
field experience, the new perspectives gained
and the small but appropriate innovations
made. The Sevagram group has been parti
cularly remarkable in such little inputs.
MFC organisational reports have been a con
sistent and welcome feature. The informal
nature of these reports have been typical of
MFC. Reports of the lively group discus
sions at the meets have helped those who
cannot attend the meet to get a feel of the
frank and open style of MFC group work.
(d)
(e)
(f)
(s)
Surprisingly in a hundred issues less than
twenty books have been reviewed. These
have included the classics by lllich, Maurice
King, Mendelsohn and Morley and the ICMR
and WHO compilations of alternative approa
ches. In the light of the recent explosion in
health care literature this is a serious lacunae
in our efforts. Not that all the material avail
able is necessarily relevant to the MFC search
but there is an urgent need to keep members
and readers upto date and well informed, if
this quest for an alternative people oriented
health system is to be built on a scientific
(h)
base.
*- ::
In recent
Government policy documents
significant
output of
years there has been a i \
and
related
government policy documents
reports taking a new look at the Indian situa
tion and supporting/professing alternative
approaches. By and large the MFC bulletin
has carried active response to each of these
— the Srivastava Report, the Janata Health
Policy, the Medical Education Policy and the
Health for all Report. The lack of response
to the new Health Policy of 1983 is a serious
omisssion. This active analysis and feedback
is particularly crucial because the reports of
late feature very radical statements and pro
grammes that create myths and some confu
sion.
These reports seldom mention the
process by which these radical changes can
be actually introduced into the existing exploi
tative and irrelevant systems. MFC members
have a definite role to bring out these contra
dictions and also apply themselves to issues
of process ignored by these reports. At the
same time we need to emphasise those
elements which are helpful to the evalction of
literature m health, job opportunities and other
available resources. In 1978-79, a column
of news clippings to keep readers informed
about issues raised in the popular press was
attempted. In the absence of a documenta
tion centre to back the efforts of the editors,
this has been a low key feature.
Editorials : Like the lead articles these have
been a distinctive feature of the bulletin
though the style has varied greatly. The
first phaes saw annual editorials setting
measurable objectives for the bulletin but
remaining a silent catalyst in between. The
second phase saw a more regular feature
which not only galvanised the group work but
also put the contents of the bulletin in the
MFC perspective. The last four years has
seen the evolution of a more analytical and
technical editorship which has put the bulletin'
on very scholarly foundations.
Miscellany: Bulletins 1-29 had the Chinese
slogan "Go to the people, live among
them........ " at the bottom of every page
expressing the beginnings of the MFC quest.
Bulletin 30-35 saw the introduction of five
additional features — these being Hindi
articles, health related poetry, cartoons and
line drawings, a contents list and provocative
gimmickry to enhance readers participation.
JR was the only personality to be honoured1
in the front page being a sort of chief
inspirator of the group (46). He displaced
the red disc from top right to right down. In
cidentally the red disc was not selected to
depict the rising sun of revolution but was a
practical attempt to balance the numbers and
break the printed monotony of the first page.
Coincidentally this gave the bulletin its
popular and recognisable symbol.
Anthologies
Twice in recent years, anthologies of the best
original articals were published by MFC. The first
(In Search of a Diagnosis) covering issues 1-24
and the second (Health Care — Which Way to Go)
covering issues 25-50, have both seen a pheno
menal popularity. The first one is now out of print
while the second one is on its way out. The third
anthology is a scheduled to be released later this
year.
Readership surveys
To enable mid-course corrections and get a
feel for the readers views, readership surveys have
been undertaken. Twice, these have been reported
in the bulletin. The 1978 survey elicited only a
nine percent response while the 1979 survey an
a more humane and just system.
Information : Most bulletins have featured
snippets of information on recent events and
8
I
I
1
AT THE HUNDREDTH MILESTONE
Ravi and Thelma Narayan
mfc is as of today, mainly a thought current and the monthly medico friend circle bulletin........
is the medium through which members communicate their ideas and experiences to each other.
Running the bulletin in our chief common activity........
MFC
manifesto 1983
have evolved as time went by — being modified,
re-emohasised and added unto (see Index). Against
the background of these wide objectives the evo
lution and performance of the bulletin has shown
an interesting variety and a rich diversity. Atleast
once during this eight year period a situation of
crisis (45) called into serious question continuation
of the bulletin but the heated discussion threw up
three reasons of organisational significance which
made the bulletin necessary in addition to its
wider relevance. These being that the bulletin was
the only means — to be heard at national/international forums; to involve the new members; and
to prevent degeneration into a federation of local
scattered groups. All these objectives taken to
gether gave the bulletin a new lease of life at
every crisis.
In this centenary issue, as we reflect on the
past, consider rhe present and look into the future,
w'e review the preceding ninty-nine issues of the
bulletin, to discover the strengths and weaknesses,
the opportunities and threats that have been part
of its eight years history.
The Beginnings
The MFC bulletin began as a cyclostyled
note that was circulated regularly to members of
the initial nucleus group, many of whom had links
with the Tarun Shanti Sena in 1974-75. Our re
cords show that there were atleast fifteen such
notes. The style was informal — a sort of 'dear
friends' newsletter keeping members about meettings and discussions, field opportunities and
thought provoking articles on various relevant
health issues.
Founder members will probably
recall with nostalgia the series on the present
health system, 'alternative approaches' and 'radical
medicine', the column entitled 'vocal figures' pre
senting telling statistics of the health situation in
India and the proclamation of Maurice King's book
as the ''bible for every doctor"! The characteris
tic feature of this embryonic phase of the bulletin
was its youthful idealism and infective enthusiasm.
Rallying slogans such as "If China can do it why
can't we?" and 'let's coordinate our efforts to fight
the situation instead of blaming western culture
and criticising brain drain' were typical examples.
Outreach
The bulletin subscription has ranged from
250-700 over the years. Presently it is a little
over 400. The readership includes rural health
project workers, medical students, medical college
teachers, academicians, research workers and non
medicos interested in health.
These are spread
out all over the country but more particularly in
the Western region — Gujarat and Maharashtra —
the traditional home of MFC. A detailed break
up of the subscription list is not yet ready but a
cursory perusal indicates that the readership among
medical students and non-medicos is still far from
significant.
The MFC bulletin as we know it today took
shape at the second annual meet at Sevagram in
December 1975. The first editorial committee
was formed and a plan of issues outlined for the
whole of 1976. The first bulletin was printed in
January-February 1976. Since then the bulletin
has travelled a long way — 93 months of regular
printing, seven double issues, three editors and
seven printing press — to reach this hundredth
milestone.
Scope
The articles featured in the bulletin have
represented a very varied range of topics related
to medicine and health. An index of the hundred
issues which is featured as a supplement to this
bulletin shows twenty eight sections in the classi
fication.
These include health services, medical
education, maternal and child
Objectives
Though the initial objectives were outlined in
the first issue — as many things in MFC, these
control,
communicable
sanitation, mental health,
6
health, population
diseases,
drug
environmental
policy and drug
'5
M•
fy.
r
I
For the last eight years, we have been involved
in health and development work in villages. We
feel it was very fortunate that one of the first books
we read on arrival was 'In Search of Diagnosis': it
helped orient us along the right lines and led us to
become members of mfc, which has always seemed
like a lone voice of sanity crying in the wilderness
of India's health care scene. Now, as we prepare
to leave India, we want to offer our congratulations
for keeping up the critical analysis, and our grati
tude for all we have learned from you over the
years. Reading through the latest anthology re
minds, us that it was on your advice that we threw
out the Terramycin 2cc injections, the Novalgin,
the tonics and all other rubbish, and promoted
ORS in the clinic; and after the TB meet in
Bangalore, our TB programme was revised and
improved.
7
c
The dreadful state of health care in India is
well known to readers of mfc bulletin. The back
ground papers of the Family Planning Meet make
particularly saddening and infuriating reading. We
used to look on this work as a challenge: but after
eight years of close contact with-the health prob
lems of the rural poor, we have to say that we feel
sickened and depressed by the
amount of
ignorance, greed and exploitation which permeates
every level of what passes for 'medical care' for
the majority, of people. Our solution has to be
that there can be no solutions without political
solutions; and that in that movement, we as foreig
ners, have little role to play. It has to be upto you
all then in what looks like a long hard and bitter
struggle.
Keith and Caroline Walker, Valiparai
medico friend
circle
bulletin
APRIL-MAY 1984
TEN YEARS WITH MFC : MY PERSONAL VIEW
ASHVIN J. PATEL
When I was told to give my reflections upon
ten years of MFC, I accepted it reluctantly. Firstly,
because1 I did not have many things to say and
secondly it was not spontaneous for me. However,
I give some stray thoughts that occurred to me.
An Overview
>
'v'
Many of the readers may not know that MFC
was not a planned efforts but a spontaneous one.
It orginated from a socio-political movement Tarim
Shanti Sena which was inspired and ignited by zeal
for total revolution.
Naturally MFC carried
legacy and hang-over of this perspective, values,
culture etc. Many of the founder membersi were
considered radical and unorthodox Gandhians.
Within a year it could attract friends who rang
ed from academicians to field activists; not suprisingly it also included various shades' of opinions from
light to left. I do remember that some friends
clearly denied then, that the doctor has any other
responsible role than treating patients coming to
the dispensary. While others, on the other hand,
felt that health sendees are just an entry point
into the community.
Real health work iis to
struggle for socio-economic-political revolution.
This latter viewpoint was shared by both, the
Gandhians and the Marxists alike.
MFC criticised the present health system and
its approach so eloquently and vociferously that it
could attract attention of many young doctors and
non-doctors. The “prophetic vision” and enthu
siasm of old members proved to be too much for
some. A few resented the indoctrination and the
aggressive way of discussion. A proportion of
them felt that MFC could not give a relevant pro
gramme according to their aptitude and abilities.
There was a feeling that MFC wanted everybody
to agree with its analysis, and then left them alone
to face the frustrating situation.
In the first four years, study-cum-work camps
were organised for medical students and others
which generated lots of enthusiasm. Some medical
colleges could evolve health care programmes for
slums and nearby villages. Many of them are still
continuing. But/perhaps, except for a few, there is
no continuous follow-up and dialogue. They have
become just like any philanthropic dispensary
without having a wider perspective of community
health and development.
How would one measure the progress of such
an organisation? By the number of its members?
It’s impact on societjy? The growth of its 'members
as a collective to understand, analyse and respond
to a situation?
As experience showed the annual meets of
MFC served a purpose as a major point of contact.
However, new participants felt isolated, the target
of indoctrination and threatened by the level and
nature oft discussions. The objective of increasing
the number was not to be realised effectively. Old
members felt that the preoccupation with new
members kept the level of discussion at a preliminaiy level. There was no scope for learning and
mutual growth. Robust, impersonal and objective
arguments were appreciated and welcomed by old
members, while many of the new members perceiv
ed in the same exchange of views, aggressiveness
that tended to be personal. I feel that in the ten
years, MFC members have shown a lot of maturity
to take the arguments and criticism as that of the
thought and not of person. No one ever doubted
another's genuineness, honesty of purpose and
concern for the poor. Even after a session of hot
and involved exchanges there has been no tyace of
bitterness and the feeling of friendship and soli
darity has always grown. To an onlooker sometime
it may seem that we are simply splitting hairs and
are involved in mere polemics, But this seeming
polemics represents deeply held differing view
points, perspectives, social & political ideologies
and backgrounds.
In the first few years, the number of MFC
contacts increased very fast. It might, have been
due to the long felt need for such .a forum, the
unconventional and critical views appearing in
MFC bulletins, the annual meet deliberations or
the regional camps, Then its growth in number
Not only the numbers stag
rached a plateau.
nated, but also the core group, which evolved
spontaneously due to continuous interaction and
concern for the MFC organisation, developed a
kind of disinterest in the organisation. What was
the origin of this disinterest?
lions, concepts, valines and models like bare foot
doctors — C.H.W.; underfive clinic; campaigns
against bottle feeding, commercial foods and irra
tional therepeutics, attacking drug industry, alter
native simplistic curriculum for medical schools;
people’s participation; demystification and de
institutionalisation of health care; self-sufficient
health care programmes; self help; promotion of
other sysetms of health care: etc., etc.,” (to be refe
rred hereafter for sake of brevity as ‘health care
mix’). And even proponents of the first trend,
though grudgingly endorsed this ‘health care mix'
without providing overall framework or model
linking it with the process of socio-economic
change. This led to a lot of confusion in some
and smugness in others.
An interesting current was emerging intertwined
with the other trends, now and then. How as a
group were we going to evolve methods and a pro
cess of self learning conducive to personal as well
as collective growth? This perceived need was not
adequately responded to, which led some to dis
continue their interaction with MFC in despair.
However, a sizeable number of members continued
tenaciously to struggle to find the way tout. This
struggle was not born out of merely .'emotional
attachment to the organisation, but because the
needs and tasks were demanding so. Moreover,
MFC may be small in terms of resources, infra
structure and manpower, but perhaps it is the only
organisation struggling collectively to search for a
socially mjeaningful and durable alternative. It has
evolved and practised certain norms in public life
consistent with its objectives and concern for the
poor.
Various Trends
There were three discernable trends within
MFC
First trend wanted MFC to be a body to
provide deeper analysis of the health situation and
its relation to socio-economic-political factors.
Second one wanted it to experiment in alternative
health approaches at micro level informed with
critical analysis of present health system. Third
trend wanted it to promote philanthropic health
services. The last trend got disillusioned immedia
tely. They thought MFC with such a thorough
critique of present health affair would now come
out with new sefs of concrete alternative program
mes. This was not to be. Although attempts
were made, through regional camps and some
health care programmes involving a few medical
colleges, to introduce this 'analytical process to new
comers; a number of constraints (prevailed.
A
questioning process could be initiated, but the
view-point that not only socio-economic changes
were precondition for improvement of health, but
also that “real activity” to be taken up had to logi
cally aim/ed at socio-economic change, had a para
lysing effect on many.
Not surprisingly, the second trend also consi
dered a socio-economic change to be precondition
and also aim of their health activities. They could
go upto a point in analysing alternative health
approaches in India and elsewhere. They agreed,
in their eagereness for action, ot “certain intewen-
A lone but (emphatic voice was raised which
was appreciated by many about a rush for alterna
tive and much ado about ‘health care mix'. No
efforts were put beyond refuting certain historical
events and pointing out some limitations and defi
ciencies in various work. A point of saturation of
thinking and imagination seemed to have arrived.
I remember how one strong protagonist of
community health got alarmed when government
agreed to implement CHW scheme at national
level. His instant reaction was, “Now government
has agreed to implement CHW scheme, what role
and functions are left for us!” This 'was an indi
cation of poverty of understanding and arrest of
growth at a given time point. But experiences in
the field had shown that the ‘health care mix’ was
2
r
4
H Fc
i
I kF1
Wo
FOO' I O I
I-
'world. If yes, how can we go about it? It may
need broadening of our focus to include those from
academic institutions who have knowledge, compe
tence and aptitude to contribute to such efforts.
Simultaneously, we have to learn and develop our
abilities to understand not only social sciences but
natural sciences too. We may have| to work out
overall plans Of action informed with this perspec
tive and ipersuade ourselves and other groups to take
up some of these commonly agreed upon activities
over a period of time so as to improve our insight
as a collective.
far from adequate. It was misleading and tended to
breed rituals; it gave a false sense of achievement
and even complacency that one was doing everything
one had to do in community health . Wide gaps
in knowledge, information and strategies were there
waiting to be discovered. These were the growth
points one had to look for very carefully. This
realisation underlines the need to develop experi
ences, tin sights and knowledge which is relevant
and pertinent to Indian situation. Both social
sciences as they relate to health problems and natu
ral sciences have to develop further so that com
munity health ceases to be underdeveloped and
primitive. More painful and frustrating is that
even some proponents of the second trend are also
equally unattentive to this perception.
Tire
wateright compartmentalisation
into
political activists and health activists can
help. Competence in health sciences
no longer help.
1
is essential, but
assimilation of egalitarian
values and understanding of political reality are
crucial to undertake such “field research” condu
cive for the health of the masses. ’Most of (the
MFC members have internalised the latter; ques
tion is to fill up the deficiency in the former1 one.
But MFC members are small in number.
Most of them are already engaged in traditional
project work, political activities, campaigns for
educating masses, teaching and research in establi
shed institutions, etc. according to their aptitudes
and priorities. Would such a shift: impinge: upon
personal freedom and preferences?
Possible Tasks
■f
t
MFC lias realised the simplistic nature and
sloganism of various technological and social
interventions in vogue. It is not only not enough
to speak about shift from individual to community
diagnosis, but to understand and decipher intricate
webwork of the individual as a member of a family,
of much larger social groups to which he belongs
through kinship, residence, occupation, religion,
beliefs, etc. and conditions of his life, his work,
his economic and social placement and culture, his
physical and biological environment. Furthermore
refinement and differentiation in relation tjo each
disease process. Thus the real problem does not lie
in actual activities but lies in the theoretical under
standing of the complexly of the disease process in
the community that inform these activities. It( is
through continuing analysis and actions of various
groups on at least some of these1 problems in simi
lar perspective! that relevant, durable and realistic
pieces of knowledge are going tio be built.
We have been busy struggling with ourselves
and for various other factors, we could not interact
with medical students, socially concerned non
medical friends and consumers of health care
adequately. If we refer to the deliberations of the
second annual meet at Hoshangahad it dileneated
guidelines for action programmes quite well. Why
could we not persue it? Can we learn from positive
experiences from KSSP and negative experiences of
other organizations? Is it just a lack of infrastructure
and full time worker or adhocism responsible for
our failures?
Is there a critical mass of socially concerned
physicians! today who are competent enough to
build tip this knowledge: Does the ‘health care
mix’ aped by voluntary groups have rigour and
strength to stand the “scientific scrutiny”? Can
voluntary groups face, with their own observation
and evidences, a tough and thorough-going “objec
tive” criticism made by sympathetic academicians?
Could our priority be to evolve a (collective voice
known not only for its honesty and commitment
to tre cause of the poor; but also respected for its
ability and scientific rigour; not only among like
minded people but also among the professional
Conclusion
I have not tried to reflect on all the aspects of
MFC.( M|any things (have been left out; jljikje i^s
commendable achievements, its democratic and
egalitarian ways of working, place and role of MFC
bullentin, interaction with various groups and
individuals, details of various projects, campaign
and workshops, managing on low budgets function(Continued on page 10)
3
Looking Ahead...
Anant Phadke
would be — it does not show the process through
which the solution it offers can be brought into
practice. MFC can claim that it can show the
process of change which MFC wants to bring
about and that MFC itself constitutes a part of the
process/ Whatever may be our position, we can't
ignore this report. To be sure, there are many
aspects of this report with which MFC agrees.
This report has thus raised the level of debate,
If we are to find out how MFC can develop
further in the future, we should try to understand
the factors that affect the growth and develop
ment of MFC. These factors lie both within MFC
and outside it.
Let us start with the social fac
tors outside MFC.
The socio-economic condition in India is
turning from bad to worse. The plight of the
ordinary people is increasing, so is their opposi
tion to their oppressors. A section of the white
collar intellectuals, students, are bound to be
affected by this and some of them are'bound to
seek alternatives.
This sensitive, .humanitarian,
democratic layer from within the intelligentsia
constitutes a potential for MFC. All of us con
tinue to meet many sensitive, socially-conscious
medicos for whom a group like MFC offers a plat
form which they are happy to know about and
which they would like to join. MFC would grow
if it can approach, such individuals. If there is
a social movement amongst the intelligentsia on
any issue concerning human values, justice, we
can even hope to get a large influx of newcomers.
The original group of MFC was a product of the
Jay Prakashwadi movement. There is no such
movement on the horizon now, but to be sure it
is/ound to emerge, perhaps in a different form.
The social conditions that gave rise to it still con
tinue to dominate our lives. Today the intelli
gentsia seems to have resigned to whatever is
happening. This cynical aloofness is a counter
acting force which affects the growth of groups
like MFC. Nevertheless, on the whole, the situa
tion contains a lot of potential for the growth of
groups like MFC. But along with the growth of
general dissatisfaction amongst the people, the
challenges in front of a group like MFC have also
grown. What are these challenges?
and has set a reference point for discussion and
action. It is no more sufficient for groups like MFC
to discuss and act at the same level as was done
before the publication of this strategic report.
In the non-Government sector, the achieve
ments of some of the pathbreaking voluntary
Health Projects are now well known. What do
groups like MFC have to ^ay about these projects,
their achievements and /limitation, their relation
ship with the goal that we want to achieve? A
number of international agencies are fostering the
methodology as being attempted by these projects
and this adds to their importance.
Thirdly within the medical field, a number
of oppositional movements have grown in last
10 years of Junior Doctors, paramedics and Govt.
Medical Officers for better pay and better work
ing conditions; of consumers against misuse of
drugs .................
How groups like MFC should
relate to these movements
Groups like MFC cannot grow and develop
to any substantial extent unless such new deve
lopments are analysed properly and a standpoint
taken in theory and in practice. Does Medico
Friend Circle have the Resources-theoretical and
practical — to successfully deal with the new
challenges and hence grow into a trend which can
make a dent on the national scene? To answer
this question, let us locate the strengths and weak
nesses of MFC. MFC has been able to survive
and grow against all odds. (Compare MFC with
similar groups.) MFC has not survived by degene
rating into a lifeless institution. (Such institutions
continue only because some funding source is
re,ady to "keep” them.) MFC has also not degene
rated into a political sect with no basis in social
movements. To survive as a lively group is an
achievement for group of medicos which is funda
mentally opposed to the existing medical profes
sion and the existing system of medical care.
Secondly MFC is unique in that though most of
The publication of the report — "Health for
All : An alternative strategy” has posed a concrete
problem. After the publication of this prestigious
report (prepared by the collaboration of ICMR —
ICSSR with the help of a number of renowned
persons in the field of health-care) groups like
MFC have to take/ concrete position about what
is in our view, wrong with the existing system of
medical care and what is the alternative. Is oqr
analysis and solution any different from what Mas
been described in this report? If yes, in what way
and why? One of the criticisms of this/7report
4
4
4
MFC
A/P J90- Ici
(Continued from page 3)
ing without paid full time personnel, tetc. Inspite
of all its limitations and failures, MFC has ’created
a lot of hopes and expectations from varied quar
ters. Pertinent question is whether MFC can
collectively show resilience and 'tenacity to meet
the challenge of examining the process and progress
of its functioning continuously in the light of fresh
experiences and knowledge without slipping into
high profile global fashions, slogans and cliches.
MFC could show a change in emphasis after
a long debate on ‘MFC which way to go' from
achieving socio-economic change to evloving a
pattern of medical education and methodology of
health care relevant to Indian needs and conditions
as a part of broader efforts to improve all aspecst of
society for a better life, more humane and just in
contents and purposes. MFC bulletin could also
show a shift from merely paralysing critiqufe of
micro level issues to examination of various micro
level alternatives and interventions. Annual meets
also tried to respond to issues- like women land
health, medical education, etc. MFC also respon
ded to live and emergent issues like reservation for
sieats in medical colleges for the scheduled tribes
and castes.
These experiences make one feel
confident that MFC has the potential to respond to
relevant issues in a mature and courageous way.
i
COMMOi'^ITY HEALTH FORUM
No. 367, ‘Srinivasa Nilaya*, Jakkasandra, I Main Road,
I Block, Koramangala, Bangalore - 560 034.
30th June, 1992.
Dear
Greetings from Community Health Forum 1
This is to inform you of the next CQHO Forum meeting ?
Date
11th July 1992 (Saturday)
Time
2«00 p.m.
Venue
Topic
s
s
to
4.30 p.m.
Ashirvad,
30, St. Mark’s Road,
Bangalore - 560 001„
iPhone - Ashirvad
C.H^Forum
- 210154
- 531518)
•‘COMMITY HEALTH GET J,.11
You are aware that it is a year since the C.H.C. has registered
as " Seciety for Community Health Awareness, Research and Action”.
Members of C.H.C. will be briefly reviewing the past activities,
sharing with you its concerns and initiatives, while putting up
plans for the future.
As members of the COH. Forum and friends of C.H.C. we EARNESTLY
request your participation, ideas and viewpoints to enable a common
initiative towards Community Health.
Do mark this date/time in your schedules and looking forward to
our meeting.
With regards and Best Wishes,
Yours sincerely,
for CCPMJNITY. HEALTH FORUM,
>
Mf' £ l<
Looking Ahead...
Anant Phadke
would be — it does not show the process through
which the solution it offers can be brought into
practice. MFC can claim that it can show the
process of change which MFC wants to bring
about and that MFC itself constitutes a part of the
process. Whatever may be our position, we can't
ignore this report. To be sure, there are many
aspects of this report with which MFC agrees.
This report has thus raised the level of debate,
and has set a reference point for discussion and
action. It is no more sufficient for groups like MFC
to discuss and act at the same level as was done
before the publication of this strategic report.
If we are to find out how MFC can develop
further in the future, we should try to understand
the factors that affect the growth and develop
ment of MFC. These factors lie both within MFC
and outside it.
Let us start with the social fac
tors outside MFC.
The socio economic condition in India is
turning from bad to worse. The plight of the
ordinary people is increasing, so is their opposi
tion to their oppressors. A section of the white
collar intellectuals, students, are bound to be
affected by this and some of them are bound to
seek alternatives. This sensitive, humanitarian,
democratic layer from within the intelligentsia
constitutes a potential for MFC. All of us con
tinue to meet many sensitive, socially-conscious
medicos for whom a group like MFC offers a plat
form which they are happy to know about and
which they would like to join. MFC would grow
if it can approach such individuals. If there is
a social movement amongst the intelligentsia on
any issue concerning human values, justice, we
can even hope to get a large influx of newcomers.
The original group of MFC was a product of the
Jay Prakashwadi movement. There is no such
movement on the horizon now, but to be sure it
is bound to emerge, perhaps in a different form.
The social conditions that gave rise to it still con
tinue to dominate our lives. Today the intelli
gentsia seems to have resigned to whatever is
happening. This cynical aloofness is a counter
acting force which affects the growth of groups
like MFC. Nevertheless, on the whole, the situa
tion contains a lot of potential for the growth of
groups like MFC. But along with the growth of
general dissatisfaction amongst the people, the
challenges in front of a group like MFC have also
grown. What are these challenges?
In the non-Government sector, the achieve
ments of some of the pathbreaking voluntary
Health Projects are now well known. What do
groups like MFC have to say about these projects,
their achievements and limitation, their relation
ship with the goal that we want to achieve? A
number of international agencies are fostering the
methodology as being attempted by these projects
and this adds to their importance.
Thirdly within the medical field, a number
of oppositional movements have grown in last
10 years of Junior Doctors, paramedics and Govt.
Medical Officers for better pay and better work
ing conditions; of consumers against misuse of
drugs .................. How groups like MFC should
relate to these movements
Groups like MFC cannot grow and develop
to any substantial extent unless such new deve
lopments are analysed properly and a standpoint
taken in theory and in practice. Does Medico
Friend Circle have the resources-theoretical and
practical — to successfully deal with the new
challenges and hence grow into a trend which can
make a dent on the national scene? To answer
this question, let us locate the strengths and weak
nesses of MFC. MFC has been able to survive
and grow against all odds. (Compare MFC with
similar groups.) MFC has not survived by degene
rating into a lifeless institution. (Such institutions
continue only because some funding source is
ready to "keep" them.) MFC has also not degene
rated into a political sect with no basis in social
movements. To survive as a lively group is an
achievement for group of medicos which is funda
mentally opposed to the existing medical profes
sion and the existing system of medical care.
Secondly MFC is unique in that though most of
The publication of the report — "Health for
All : An alternative strategy" has posed a concrete
problem. After the publication of this prestigious
report (prepared by the collaboration of ICMR —
1CSSR with the help of a number of renowned
persons in the field of health-care) groups like
MFC have to take a concrete position about what
is in our view, wrong with the existing system of
medical care and what is the alternative. Is our
analysis and solution any different from what has
been described in this report? If yes, in what way
and why? One of the criticisms of this report
4
f\Jv
f - Wv
lDD-1 Cl,
1^4-
I (i 0
the leading members of MFC are politically cons
cious, they have enough of healthy, non-sectarian,
democratic approach to allow medicos from diffe
rent political leanings to come together, debate,
criticise each other, learn from each other and
develop into a tolerant, mature group. It must,
however, be noted that the "friendly" atmosphere
in MFC is partly because there is not much at
stake. If MFC squarely faces the problems men
tioned above, starts growing as a formidable cur
rent on the national plane, the friendly atmos
phere is bound to be affected atleast to a certain
extent. But the tradition, we have set up will help
us in challenging times. The tradition of respect
ing other's viewpoint, of mutual trust, openmindedness has been our asset. To be sure some
sectarian mistakes have been made of because of
which some people got alienated. But many have
come back and on the whole very few have drop
ped out with sharp discontent. (The core-group
of MFC sometimes gives an impression of an arro
gant, radical, intellectual clique involved within
itself. But this is only a cursory impression — even
that should changes and it is not at all the true
nature of this group.)
The third positive asset of MFC is the ten
dency in MFC to examine things in a critical the
oretical perspective, on a principled basis yet in
a way that would be relevant to the problems in
the actual field. Since most of the leading mem
bers are actually working at the grass-root level,
this critical questioning outlook acquires a special
down-to-earth practical connotation.
This has
earned MFC seme good name (as well as bad
name amongst those who don't like such ques
tioning.)
But the theoretical development in MFC has
been quite slow. It is only recently that things
have really begun to move. The tendency in MFC
to be self-complacent and self-congratulating has
more or less been replaced by a serious concern
to study, work upon and develop our understand
ing.
But still it would take a lot more effort to
systematically develop position on the problems
mentioned earlier. There does not seem to be
adequate realisation in most of us that MFC must
answer these and such problems if it has to make a
dent on the national level. A sense of urgency, requ
ired in view of MFC's lagging ebhind as of today,
is by and large absent. There is a concern for
developing our understanding; but not in relation
to the challenge posed by the events happening
around but as a general concern for theoretical
development.
Things are bad when we come to the ques
tion of making a co-ordinated effort to make an
impact on a national level by forging, propagating
an alternative viewpoint. Most leading members
of MFC are quite involved in their local work.
Most of us have not been able to devote much
time and energy for MFC's organizational work.
Unless the leading members of MFC replan their
local work in such a way that they spend much
more time for MFC's organizational work, unless
more fresh blood comes in, MFC will not be able
to face at all the challenge posed to her by the
developments in last few years. Unfortunately not
Some are even
many MFC members see this.
content with the running of the Bulletin and the
Annual Meet. We must realize that even mere
continuation at the existing level is financially
becoming more and more difficult due to price-rise.
The financial deficit is increasing very fast. Unless
we have atleast 1,000 subscribers (compared to
about 400 to-day) the deficit would become
unmanageable next year (even this year.) There
are more than 2 lacs MBBS doctors in India, (to
take one yardstick of assessing the potential for
MFC to grow) and even one per cent of this
becomes more than two thousand.
MFC is
unknown to many of those who would readily
become its members. We should have reached at
least this section. But that involves a change in
the attitude of many leading MFC members
towards MFC and hence a re-planning of their
priorities in practice. Are we really serious about
forging an alternative, making a dent on current
opinion in India about medical care? Shall we
critically study, try to develop and practice communty medicine much more seriously? Shall we
study and understand in a much more concerned
manner the history, development of social move
ments, social changes in India and abroad? In one
word, shall we get rid of amateurism in us? The
answer to these questions will decide whether MFC
can play its role in the "fundamental socio-econo
mic change'' that MFC wants to align with.
□’
I
5
108
medico friend
circle
bulletin
DECEMBER
1984
Discussing Tuberculosis Control-Why?
— Anant Phadke, Pune
(In the coming Xlth Annual Meet of the Medico
Friend Circle at Bangalore, we would be discussing
various issues concerning tuberculosis control in
India. The question is so vast that it is impossible
to have any useful discussion unless we define the
focus of the discussion. In my view, the purpose of
discussing any issue in mfc needs to be clearly
thought of and agreed upon. In this note, I would
argue what in my view would be the appropriate
purpose of the discussion at the mfc annual meet.
This note would inevitably involve a discussion on
the role of mfc.)
Role of discussion at the annual meet
Let me first quickly put forth a consensus that
we had reached about the general role of the dis
cussion at the annual1 meet. It was thought that
there is a definite section within medicos and non
medicos in India who already have a perspective
similar to that of mfc or who could come to mfc, if
there is adequate contact and dialogue. Different
individuals in this section are more interested in
specific aspects of the health system in India. If mfc
takes up various issues in different meetings, then
those individuals with
specific interdsts in these
subjects would come closer to mfc and may join us.
Secondly such discussions would help us, the mfc
members, to enrich our knowledge and perspective
of the health problems in India through well planned
discussions with the help of resource persons out
side mfc; and mfc in turn would hopefully make some
impact on the new participants during the course of
these discussions. Fine enought But all this does not
specify what specific kind of knowledge we want to
gain and generate through these discussions; whether
and in what way would the discussions be different
from the discussions in the academic or established
circles of community health.
Specificity of mfc
To answer this question, let us go back to the
origins of mfc, the kind of discussions we have had so
far and the debate on ‘mfc — which way to go’
carried through the pages of the bulletin and reprinted
in our anthology — HEALTH CARE WHICH WAY
TO GO? I would also like to remind readers of the
Centenary issue of the mfc bulletin No. 100-101
(May-June 1984) where the contributors had taken
a somewhat critical overview of what the mfc has
achieved, not achieved and what challenges we face
today. It is not possible to go through the history
of mfc in this note. I would only point out two specific
characteristics of mfc which are reflected in all these
writings. One, its concern for Social Revolution. At
least the core members of mfc have been very con
cerned about this and hence the articles in mfc bulle
tin have been quite critical about the existing health
system and the debate ‘mfc which way to go?” was
centered around how mfc could contribute to funda
mental socio-economic-political
(S-E-P as Abhay
Bang had put it then) change. The second characte
ristic has been the critical and questioning attitude
of mfc members:
critical of new ‘solutions’/strategies put for
ward by the establishment and the community
health enthusiasts (this critical outlook partly
reflects the grass root village level at which
many mfc members work)
critical (admittedly to a lesser extent) about
mfc’s achievement and
of late, critical about the existing prescrip
tions of community medicine.
*
False and genuine limitations
are genuine ones is something that needs to
be worked out concretely and is in a way a matter
of judgement also, but to be sure, there is such a
difference. Secondly the established value system
does not completely disappear in such project work
and the problem of poverty, social and educational
backwardness, bureaucracy etc., etc., would continue
to affect health work in such a project, though in a
mitigated and different form. But the direction of
where we want to go would be clear.
My plea is, let us be more conscious about our
' specific character and. shape our discussions in the
coming annual meet accordingly. What does this
mean concretely? For example, let us look critically
at the argument that ‘since India is a poor country
Inj. streptomycin should be reserved only for sputum
positive cases and only the two drug regimen of
Isonex plus thiacetazone be given to sputrum nega
tive cases.’ We shout’d question this argument and
ask ‘Is Indian economy so backward today that it
cannot really afford to give streptomycin to all the
cases of tuberculosis?’ Today, the existing system
squanders resources on useless activities and keeps
a smaller share than what is possible and necessary
for health work. Even within health, resource utilisa
tion is in favour of the medical establishment and the
well-to-do. In the case of drug production, for exam
ple, out of a total of about Rs. 1200 crores of drugs
used annually in India, it is estimated that only about
Rs. 350 crores of drugs are essential and rational.
The rest, though they yield higher profits for drug
companies, are useless and irrational. If these re
sources are utilised properly why can’t all those who
need antitubercular treatment get proper treatment?
Is Indian economy really so backward that radio
graphic facilities cannot be extended more to help the
diagnosis of tuberculosis and other conditions? Why
should mfc accept the false limitations imposed by
the existing system and try to work out solutions
within these false limitations?
A question may be posed: What is the point in
trying to create ideal islands of project work when
tney are going to remain islands, when the strategy
is not going to be generalized?’ Firstly I am not
talking about ‘ideal’’ situations which have no basis
in today’s reality. One is talking about rejecting only
false limitations. Now it is true that even this cannot
be generalised within this system (obviously!) and
our alternative can only flower in a different, better
social system. That is why mfc members should work
within the context of and with the cooperation of
social movements; forces which are really aiming at
a different and better society. This is how we as
medicos can help the social revolution which was the
original and is the specific inspiration of mfc. Instead
of working within the existing system and hence help
ing it, legitimising it, why not work outside or on the
system and help those social' movements which are
aiming at changing the system itself?
There is a practical advantage in working with
such social movements. If a project work is under
taken in an area where such a broad movement to
wards fundamental social change is taking place,
people’s participation, one of the most important
requirements of good community health work (and
which is generally lacking in many projects run
mainly on the basis of funds) can become a reality
and the entire atmosphere is quite different from the
usual one of apathy, lack of faith, lack of commit
ment and too much bureaucracy. In such places, one
can concentrate on the real problems of health work
and also obtain people’s cooperation and participa
tion, required to solve them. I have deliberately used
the general terms social revolution and social move
ments, because concretely which are such movements
is something which individual members have to decide
on their own. Ideologically and politically mfc is not
very homogenous and different individuals have diffe
rent opinions. But one thing is certain, all of us want
a fundamental socio-economic change even if the exact
character of this change is a matter of debate.
My plea is that when we discuss the problem
of tuberculosis or any other problem, let us discuss
it with a view to the social revolution that alone would
be able to create conditions for a healthy society and
a healthy medical system.
We all know very well that India is both econo
mically and socially backward and even after a social
revolution resources are not going to develop at such
a rate as to make all desirable facilities available in
the immediate future. We would, therefore, have to
work out solutions within the constraints of limited
resources. But over and above these real constraints,
the existing system has imposed its own constraints
like — malutilisation of resources for the benefit of
a few; bureaucratic callousness of doctors and other
health personnel; curative oriented training; corrup
tion and commercialization in medical practice;
political interference by vested interests etc., etc. All
these together make it almost impossible for a scienti
fic strategy to be successfully implemented. In
these circumstances should we try to suggest methods
of improving the existing state of affairs a little more
by accepting all the false limitations of this system?
Towards a better medical and social system
Instead of falling into their trap under the name
of ‘Practical difficulties’, and suggesting improve
ments to those who are neither particularly
willing nor capable of improving the existing state of
affairs (remember what happened to the reports of
numerous expert committees) why not expose them?
Why not concentrate on evolving a people oriented
scientific strategy in our own projects and other
activities? Such an approach would reject false limita
tions and try to work within genuine limitations.
Firstly which are false limitations and which
Tall talk?
It may be thought all this is high flown, tall talk'
there is no point in planning for a future society today
when we do not know when and whether it would
come about.’ Yes, in a way, it is tall talk. Was not
2
*
7
aiming at freedom from British rule tall talk in the
1930’s? Were not Mao and his comrades utopian
when they were aiming at a new society in the 1930’s?
The Freedom Movement in India was aiming at
total political independence on the one hand but at
the same time demanded certain reforms within the
system. Likewise we can and should ask for certain
changes in the existing medical! system to partly
alleviate the sufferings of the people. Our discussion
should also be geared to find out such points of
action. This is quite different from allowing our dis
cussions to be limited by the framework/problems
created by the existing system.
Innovations, ideas, created, practised by such
radical health work may allso be used in a diluted,
distorted form by the existing system (for example,
the concept of community health worker). But it is
a different matter to aim at, limit oneself (consciously
or otherwise), to changes in the existing system. If
somebody says that you are evolving strategies which
cannot be generalised and hence your work is useless,
we should stand up boldly and say that yes, our work,
ideas are useless for the existing system but as the
movement for social revolution grows the success and
influence of our ideas would also grow.
There may be an objection that ‘all this tall talk
leaves no scope for those who cannot devote them
selves to such project work’. There is a misunder
standing involved in this argument about project
work. Project work does not necessarily mean village
level project work. Alternatives are to be planned
and tried out at all levels, wherever possible. A move
ment geared to analyse and expose the existing medi
cal system, alternative experiments in production and
distribution of rational, low cost drugs, in medical/
health education . . . etc., are all project work in this
sense. Concretely, in the case of tuberculosis control,
it is not necessary that everybody from the group has
to devote themselves to a rural project in order for the
group to analyse the existing strategy of the tuber
culosis control programme and to try to evolve an
alternative. There are a number of other small and
big tasks involved in this work: for example, gather
ing information, analysing it, disseminating informa
tion, organization . . . etc., in which different indi
viduals can contribute differently. Independence was
“We already possess all the necessary weapons
to wipe out TB. All we need to defeat the disease,
now and forever, are the financial resources and the
political will.”
World Health — 1982
not won by full time political activists alone, it was
the product of the collective efforts of millions of
ordinary people contributing their individual, small
mite.
The coming annual meet
Concretely speaking, in the discussion on tuber
culosis during the coming annual meet, my sugges
tion is that we should concentrate on: (a) forging an
outline of a fundamental critique of ^he existing state
of affairs in tuberculosis control in India; (b) identi
fying measures which should be demanded from the
government to alleviate some acute problems; (c)
evolving an outline of an alternative strategy of
tuberculosis control. This would involve:
1.
Understanding the theoretical basis and the
evolution of the National Tuberculosis Pro
gramme . Finding out whether the strategy
has accepted and internalised the false
limitations imposed by the system;
2.
Sharing our knowledge and experience of
how this programme works in the field and
why;
3.
Identifying and analysing the genuine tech
nical and social problems involved in the
control of tuberculosis in a backward coun
try like India;
4.
Learning from the experiences of other
countries and formulating an outline of an
alternative and the role of mfc in it.
(We are awaiting comments before we finalise
the session by session plan of the meet. These must
reach us by the 31st of December. The final plan will
appear is January 1985 issue — Editor/convenor).
/
*
« *
il05
medico friend
circle
bulletin
I
1984
SEPTEMBER
ft
NATIONAL TUBERCULOSIS PROGRAMME
: some problems and issues :
Binayak Sen**
ft
ft
ft
ft
ft
ft
ft
ft
ft
ft
ft
r
£
c
ft
. ft
ft
- ft
, ft
ft
ft
ft
ft
ft
ft
ft
ft
ft
€
““ ‘
1. Conceptual Problems
In their seminal 1962 paper on
ft
H
c
c
is in operation in the
are still being turned
tta. ev„ « Ue
3
tuberculosis programmes.
The credibility of this system rests on the ade-
with wbSX S.%
”
would, ttootau, * m
ripvelooment of an integrated and well-defined system
for mckling the entire range of tuberculosis sympto
matology.
Instead, the National Tuberculosis Programme has
set its sights on a Mirage— the mterruption of bac
terial transmission. To this end, it Refines a case of
tuberculosis as a person excreting tubercle baoll
his'sputum. This approach is unscientific because it
is onN at a much later stage along the exponential
curve of falling prevalence that the interruption of
transmission becomes even a remote P055115111^ _ “
also ignores the fact that never in the history of human
tuberculosis has a reduction in transmission been
brought about by a specifically medical intervention.
BPW. 22
>«
As a result of my four years experience of work
ing in voluntary institutions participating in district
tuberculosis control programmes — in Hoshangabad
and in Burg — I am familiar with the way in which
this approach works in practice. A person who pre
sents himself at a Public Health Institution with symp
toms suggestive of tuberculosis is not regarded as a
person suffering from disability and consequently in
need of help, but simply as an entity to be categorised,
i e TB or not TB. After a cursory physical examina
tion he is sent for a sputum test. K he obliges by
producing a positive sputum, that is the end of the
matter. He can then be placed on a standard treat
ment regime (generally INH and Thiaeetazone dady)
and forgotten about. Once in a way his sputum may
be checked but the treatment regime is not affected
thereby. I have documented evidence of P^'^s,
sputum positive after a year’s treatment with INH
and thiaeetazone, being continued on the same drug.
When challenged, the government doctor has explained,
“that is the only regime available”. In point of fact, m
practice this is often true.
But. we will come to problems of chemotherapy
to make is, that £from
later. The point I am <trying
/
I
I
I
I
M 'Fc |2>
IP5~. ^j-uvyku
__ 2Jj22
«r
fl
apparent primary tuberculosis can safely be treated by
a short course of INH alone. This is a notion that
goes against ail bacteriological logic. One.only crea
tes a population of INH resistant bacteria, strategi
cally situated to subsequently produce reactivation
disease.
the point of view of a desperately sick man, frightened
by a dreaded diagnosis, it is cold comfort to t?e given
30 tablets and told to come back aeain after a month’s
treatment, and assured that he will get well in 18
months time. This is particularly so since there are doc
tors at every street comer assuring patients (with con
siderable honesty) that they will get well with some
private treatment in six months or less.
b. Extra Pulmonary Tuberculosis
The chapter on Epidemiology in the Text Book
■ of Tuberculosis (by the Tuberculosis Association of
India) has nothing to say about extra pulmonary
disease. In my experience this forms a significant
proportion of cases of tuberculosis. In particular,
‘scrofula’ (burnt out tuberculous cervical lympha
denitis) ..is still a common finding in backward areas
of the country.
Let us now come to the case of those who were
sputum negative. The cost of a ‘free MMR X-ray
from Durg to a person in Rajhara, is well over Rs.
50.00. The cost of a local private X-rav is Rs. 35.00.
Which should the patient choose?
It should be noted that I have been talking all
along of the ideal case. We have not taken any account
of the government doctor nudging the patient towards
his private clinic; the laboratory technician asking
for his ‘fee’; the X-ray technician’s rudeness, or the
irregularity in drug- supply.
3. Staff Problems
Cases of ignorance among people working in
the field of tuberculosis are not rare. This is because
almost the entire field level medical staff of the
tuberculosis programme are ‘dead-beats’ — people
___ promoted
___
who have been
to an administrative posi
tion because their seniority has become an adminis
trative embrassment.
In a Government District Hospital, despite all
the other problems, one can atleast meet doctors who
are interested in their work in the medical, surgical,
gynaecological and other specialist departments. Not
so in tuberculosis. The department which should, by
all epidemiological logic, claim the most brilliant and
dedicated of our technical manpower, is invariably
academically dead. In Hoshangabad, the District
Tuberculosis Officer was simply absent for a long
period of time.
The para-medical staff, on the other hand, are
often exceptionally dedicated and able. They often
run the programme practically independently. How
ever, they have to pay the price for their competence.
In Durg, the statistical assistant — a key person,
and in this case extremely competent and dedicated
__ has been on full time deputation to the Civil
Surgeon’s office, helping to administer the hospital.
The patient of tuberculosis is basically a suiiering person. It is the least of his concern that he is
excreting M tuberculosis in his sputum. What he is
much more worried about is the fact that he has
cough, chest pain, fever, body ache and nausea. He
cannot work. He feels weak. He loses his sexual
potency. His children starve and often fall ill in
their turn. A physically distant and emotionally re
mote health centre can offer him nothing. It is well
to remember that the Madras Chemotherapy Centre
study on domiciliary treatment had weekly home
visits as part of their protocol. It is a great pity that
this investigation has formed the basis for a programme
that thinks it sufficient to throw some tablets once a
month at a desperately sick man.
2. Primary TB and Extra-pulmonary TB
Treating the problem of tuberculosis as a pro
blem of suffering people, rather than as a problem
of successfully eliminated parasitic myco-bacteria,
brings us to two sets of illnesses often neglected in
the current programmes, viz..
a. Primary Tuberculosis
I
I
I
t
e II
e I
€ I
e I
e II
e
e I
I
e I
e I
I
e
e
e- I
e i :
c i ?
i i
i'
i
c i :
c I .
c I .
c
:
c i
i G
in
I .
I
I
4. Chemotherapy
Between 10 & 20 percent of Indian children are
tuberculin sensitive by the time they are five years
old, though some surveys (Raj Narayan) yield a lower
estimate. The popular (medical) conception of pri
mary tuberculosis is of a mild intercurrent illness that
is only incidentally detected in a chest X-ray and
attains clinical significance only in the ‘progressive’
form. This is not true In malnourished children not
only is infection itself accompanied by significant mor
bidity, but it is the ‘interaction’ between infection and
nutrition — that is the factor that needs to be con
sidered. Whpn we consider that, according to 1CMR,
65% of Indian children are malnourished, the dimen
sion of the problem becomes a little more plain.
a. Existing patterns
In theory, the National Tuberculosis programme
provides a wide choice among several alternative
regimes. These include, daily INH and thiacetazone
with or without an initial period of intensive treatment
with daily streptomycin and/or PAS. The bi-weekly
supervised regimes consisting of INH/SM and INH/
PAS, have been designed specially to ensure patient
compliance.
Even according to the treatment manual supplied
to the district Tuberculosis Officers, only sputum
positive patients are eligible for all these reetmes.
X-ray positive, sputum negative patients often just
It is a common misconception (even, as I have
discovered, among TB ‘Specialists’), that clinically
\
c I
(Continued
I
c 1I
G
G
C
I
I
e II
c
on page 8)
R | (
2
1 .
g L.
11 €-^ M b£?
b > FC
I
-do
l
1
as sick as their ‘positive’ brethren and about 5 times
X'm"’lNH/THblregimely Ksumably"1 compli:"ot a Serationwhere they are concerned.
»
r
»
»
R
antnal nractice, the only regime available
In actu P
’
inh/TH. (Incidentally,
with any
necessary to counteract INH indut
r
!» I •
■ I »
(3)
Patients are told to eat lots of peanuts!) PAS I have
one year. Streptomycin
nott «en
seen in
m the
tne past
p
ients areis consoften
.
■* I
* I »
M |
,
* I
’ I
* I
? I
** I
,
«
«
Coming to the INH TH regime, TH is by no
*
e i •
C I 55
I
<* I
I
<* I
e i
following incidence of side effects.
Cutaneous hypersensitivity reactions ~ 7%:
Jaundice — 3%;
Intractable vomiting — 3%
Apart from these, there are minor side effects
such as anorexia, nausea, vomiting and head ache.
Weight gain and rise in haemoglobin level are less in
natients on TH as compared with those on PAS. Th
effect of such minor side effects on patient compliance,
especially in the absence of adequate medical super
vision and reassurance, can only be imagined.
i
«* ■
e I
e ■
e I 5
e! ’
s: >
■
<
<
>
3
*
3
3
3
3
3
3
3
3
3
3,
3
3
3
3
>
>
We will consider possible alternative regimes in
the next section. For the moment let us stick to
the first line/second line chemotherapy model We
have already noted, some of the prob ems with the
bi weekly INH/SM regime not available for sputum
The lone patient I managed to get referred to a
Sanatorium in Bhopal emerged after two months
tooking much better and clutching a prescnption for
rifampicin and ethambutol.
c. Possible Alternatives
It is well known that there now exists a wide
variety of alternative drug regimes for the treatment
of tuberculosis, many of which result in cure of a
higher proportion of patients in a much shorter penod
of8timePthan existing standard regimes. The conven
tional wisdom is that these alternative regimes com
prise a ‘second line’ of treatment for patients rests
tant to the standard regimes.
The fact that the government itself does not take
this argument seriously is shown by the free availa
bility of the so called ‘second line’ drugs in the open
Of W tb« price «
of the ordinary tuberculosis patient. As a resurt,, w
have in India the ironic situat’oi^where the District
Tuberculosis Officer and the PHC Medical Officers
are the only medical
practitioners who (m their
official capacity) have no access to the newer drugs
for the treatment of tuberculosis.
In effect there are today, in tuberculosis, as in
every other field of medical and indeed of public
■■_ —- one for the
life, two sets of policies m operation
Kt for those who can (even if only with
poor and one L----difficulty) pay.
live within about 5 kms of a PHC.
b. Drug resistance
Coming now toj the problem of resistant tuber
culosis, there are a inumber of problems in the existing framework.
; a rare
(D Drug resistance^
show that the
phenomenon.‘''Eristffig'studies
- ------- o
• a---------A-j
prevalence of primary drug resistance^ to
prevalence
both INH and SM in Indiai are (individually)
of the order of 5 to 10 percent. The pre
valence of acquired drug resistance is not
known to me. But the success rate of the
standard first line treatment regime is of the
order of 80 to 85 percent, under ideal
conditions.
(2) There is evidence to show that pre-treattnent drug sensitivity tests do not affect the
outcome of treatment, provided standard two
<11
MAVA *—■ —
—-
phase regimes are used, with an initial
intensive phase using three drugs. However
in my experience, such regimes are available
only to a very small proportion of patients
even in the district centres, and to practi
cally none in the peripheral centres. Most
patients go on a standard two drug regime
(generally INH-TH).
When a patient fails to respond clinically to
a particular regime, there are no facilities
for drug sensitivity testing even in these
selected cases. Theoretically, in tne exis
ting model, they can be referred to Tuber
culosis Sanatoria for treatment with 2nd line
drugs. In practice, however, (a) practically
none of these patients do get referred to
Sanatoria; and (b) even among those who
are started on second line drugs at such
centres, there are no facilities to continue
drugs after the patient is discharged.
The argument against the newer regimes can now
be seen plaffily for what it is - a question of co •
It is worth going into this question m some details.
>
5. The question of cost
a. How much?
humIvU course of treatment with
The cost of a complete
the newer drugs at current
<-------- market prices is of the
3
I
<
i
I -)
MPc
IPS’,
*1
(Continued (rom page 3)
J
order of Rs. 500.00 to Rs. 1000.00. Regimes con
taining Streptomycin are liable to cost more, because
of the administrative cost of giving the injection.
1
We are not talking of enormous sums of money.
The cost of bi-weeklly INH/SM with an initial inten
sive phase is not much less. Neither is the cost of
1NH/PAS regimes. The logic of the exclusive depen
dence on INH/TH now becomes clear.
Put another way, the cost of treating a case of
tuberculosis with the newer drugs and the cost of
treatins a case of intestinal obstruction or pyogenic
meninsttis is about the same. The cost of treating a
case of ischaemic heart disease or lung cancer or
brain tumor or diabetes mellitus or chronic renal
failure is several times higher. The comparison ^comes
ridiculous when one carries the contrast 5° fidds
outside medicine — say, to defence or CHOGM.
b. Cost to whom ?
The second aspect of the cost equation — what
is the ‘cost’ of a twenty percent relapse rate which is
the best result obtainable with the standard 'first line
regime? What is the ‘cost’ of a case of thiacetazone
induced agranulocytosis or Stevens-Johnson Syndome.
What is the ‘cost’ of travelling up and down from
village to PHC, village to District centre, village to
wherever, for 18 months as against the six months
with newer regimes? What is the ‘cost’ in bus fare?
What is the ‘cost’ in lost income? What is the cost
in the suffering of a poor man? This is a question which
the policy makers of tuberculosis must answer.
1
?
J
3
0
3
■
&
a
3
3
wI
&
I
I
i :
1
*
*
«
III
medico friend
circle
bulletin
MARCH
1985
TB AND SOCIETY
Preamble
It is the first time in the last eleven years since
our inception that mfc has taken up a single dise
ase entity for discussion at the annual meet.
The disease selected—Tuberculosis'—was particu
larly relevant because of many reasons:
i. To begin with there is greater understanding
today of the multifactorial aetiology of the disease
where social factors more than biological are known
to have a significant impact on incidence, preva
lence, spread, diagnosis, management and control;
ii. Secondly unlike most of the national pro
grammes in India the NTP has developed on crucial
sociological perspectives derived from1 relevant
field studies;
iii. In its approach in terms of integration with
general health services, choice of appropriate investi
gative technology, alternatives in chemotherapy and
other aspects it has shown a greater people/patient
sensitivity than most other programmes and a signi
ficant shift from the dependence on the industrial
aspects of medical care;
iv. Inspite of these salient features the case
finding and case holding performance is far from
satisfactory and these have become a matter of great
concern for TB programme organisers and decision
makers;
v. The 1CMR/ICSSR Report while analysing
the drug situation in the country has highlighted the
shocking state of availability of anti-tuberculosis
drugs (‘one third of minimal requirement’) when
vitamins, tonics, health restoratives and digestives
are being produced in “wasteful abundance”;
vi. By its inclusion in the 20 point programme
the government has endorsed its relative importance
in the health scene of the country though whether
this step is part of a 'populist rhetoric’ or a nati
onal commitment towards control of the problem,
only time will tell.
It is in this context that the mfc decision to
relook at the whole situation of the TB problem and
its control in India as an exercise for 1984-85 is
significant.
Scope and Focus
The meet of over 110 friends from various
diverse backgrounds (ref mfcb 110 Feb 1985) with
♦
its intensive small and large group discussions
highlighted that the subject was too large and too
important to be tackled in 16 hours of discussion
and that rather than expecting a meaningful criti
que of NTP to emerge from sq diverse a group —
what would really be more realistic would be to
accept the annual meet discussions as the initiating
of a process of critical analysis. This would be
followed up by further study, small group work and
field evaluation through 1985 from which would
hopefully emerge an mfc perspective on the problem.
This sense of realism was forced on the group after
the first session on “Expectations of the Meet” in
which participants were asked to raise issues and
questions for discussion.
Expectations of the Meet
The exercise identified a phenomenal range of
problems far beyond the scope of the meet:
1. Need to understand the organisational
structure and implementation of NTP and the devi
ations from ideal in the actual field situations.
2. Need to identify issues on which we should
put pressure on policy makers.
3. Need to discuss the range of non-pulmonary
tuberculosis and how it is viewed by the NTP.
4. Need to discuss childhood TB and how it is
viewed by NTP.
5. Need t0 study how NTP actually operates
at the PHC level and what are the components of
the services actually available at the community
(village) level.
6. How do non-allopathic systems view TB as
a problem?
Q
I
O
involve other non health sectors like the education
7. How far can TB be considered an occupa
department etc.?
tional health problem because greater susceptibi
30. Why is awareness building given such low
lity to it after certain types of occupational ex
priority? Why is there no definite, researched and
posure are well known?
evaluated communication strategy integrated into
8. Knowledge of cost factors in the range of
NTP?
alternative regimens of chemotherapy.
During the "discussions at the meet some of
9. Data on drug production, distribution and
the
above
expectations were debated in greater detail
availability in relation to total estimate of patients
and
some
were not, either due to inadequacy oi in
and in the context of recommended drug regimes.
formation or time constraint. We report some oi
10. Identify genuine constraints in NTP
the key areas of discussion. Decisions for follow
and false limitations accepted by programme plan
up study or action are given at the relevant places
in brackets. Wherever participants have commit
ners.
ted themselves to specific action this is indicated.
11. Identify genuine constraints and false limi
Where it is not indicated it means that volunteers
tations in TB programmes of voluntary agencies.
from
members/subscribers'/readers are welcome to
12. How far is TB actually integrated with
c-et involved. We also welcome any information,
general health services? Is there need for greater
perspectives, opinions on any of the questions
integration or greater identity?
listed (get in touch with mfc office immediately).
13. To develop guidelines for patients who
TB—a socio-economic-political strategy
have already received treatment before — be it
inadequate or inefficient.
From the discussions, it evolved that TB con
14. Role of voluntary agencies in NTP.
trol must be discussed in the context of
oi aa radical
radical
reorganisation of society towards a more equitable
15. Role of private practitioners in NTP. Why
and just system- where the smallest and most vulner
are they excluded from the plan?
able person is central and only this can secure some
16 Understanding of the social stigma associ
stability t0 the health and welfare of the people.
ated with the disease and its effect on case finding
In the strategy to achieve this society, all
or holding and the measures to combat it.
interventions particularly those at the grass roots
17. The effects of the over emphasis and pres
must be through people’s movements and organisa
PHC
sures of the family planning programme on TIIC
tions so that demands and decisions are the peo
functioning as well as NTP at PHC level.
ple’s free choice. In this strategy the process oi
on
18. What is the 7th plan policy decisions
reflection and conscious action
(ie., education)
TB programme?
i« on all fronts: social, economic, political, cultural,
relation to other
respiratory
19. TB and its ---------.
- . health and countering myths and superstitions; and
occuring
in
certain
occupational
environseeks to make the person/group/society self reliant
diseases
ment.
and confident.
20. How can NGOs support/complement/supMicro level action is primary but also sharply
plement NTP of government?
limited. It must be linked to the wider reality.
21. What is the method of collection, analysis,
Critical collaboration is necessary with peoples
feed back of statistics of NTP from field level?
movements and wider political action. However,
there needs to be a high critical awareness of he
What is the method of feed back from the centralis
danger of ‘over politicisation’ and a danger of the
ing agency to the peripheral delivery system?
sabotage of the people’s freedom by political con22. Role of para medicals and community health
flicts.
workers in NTP.
Within the context of the above perspective
23. What are the legal rights of industrial
we as a group endorse the following thought curworkers vis a vis TB?
rents, action and demands on the SEP front
24. What are the differences between NTP
1 A demand for the reallocation of resources
performance in different states and regions and
in the Union Budget. There should be more money
the causes for such difference?
allocated for health and within the health sector
25. What are the present.t efforts in public
the rural-urban bias should be eliminated (There is
the available media?
awareness building? What are t..~
need to study the funding of NTP, the cost alloca
In what way can this be further promoted?
tion, for detection, drugs and personnel as well as
26. What is happening about drug resistance
the rural—urban bias.)
2 Each block and PHC should make it public
in NTP?
27 In spite of the more holistic epidemiologi
tn the’ people as to what are the available and allo
/
cated resources for that area. All these resources
cal understanding accepted today, why is NTPs
.
should be channelised for the benefit of all people
perspective severely clinical and curative.
in a just manner.
28. Why/how can TB be seen as a social pro
3 Occupational (farming, wood gathering,
blem to be tackled by society not as a medical pro
wage labour) and seasonal constraints do not allow
blem to be tackled by the health services only?
in the working
the patient (most often an adult
t-------------- age
29. Why has NTP in its planning not cared to
2
♦
M Fa
U
> (\ \ t Iv
2- C n ‘9
sations. People should be the axis when considering
the TB problem. There should not be an undue em
phasis on extraneous agencies such as doctors or
policy makers. Experts should be made answerable
to the people and crucial decisions should be made
by people. Conscious peoples organisations would
lead to socio-economic changes without
which
general health status or even TB situation would
not improve.
11. mfc members have to emphasise that the
socio economic factor is the most important aspect
in TB and for that matter in other communicable
diseases as well. As an organization we should work
to explode the fallacies accompanying the concept
of TB eg. TB Association of India pamphlet on
‘What should you know about Tuberculosis’ lists
poverty, over crowding, unhygienic living conditions
as legends about TB). mfc members who are already
involved in organising people should develop a net
work for communication.
12. Nutrition, housing, environment at the
working place and amount of leisure determine resi
stance or susceptibility to TB. This means that only
a fundamental change in the socio economic struc
ture of society will help in the control of TB.
13. Whilst demanding a basic structural change,
we should also demand that existing peripheral
services are more effective. Voluntary agencies
should as far as possible not duplicate the effort of
the government.
In fact the government should be made respon
sible for delivering basic public health services
Whilst doing reformist work at grass roots
we
should
work towards basic
change
and contribute towards this change ideologically
and organisationally. Alternatives such as low cost
drug production should also be a simultaneous acti
vity.
14. Land reforms, the minimum wages act
and the right to work should be implemented
strictly. In Kerala these measures have greatly help
ed to reduce incidence of TB
15. To bring about the above mentioned socio
economic changes, a political change aimed towards
>socialist society is inevitable.
Marie Tobin, Jansaut
Manish?. Gupte, Bombay
group) to go long distances for treatment regularly.
This reduces access to and availability of TB
treatment. Health services especially those for the
detection and treatment of TB should be handled
by para medicals and should reach the villages if
not the door steps of the people.
4. There should be the least dependence on
International agencies for funding and powerful
individuals in the first world who influence develop
ing countries— India is strongly so influenced.
5. Multinational corporations symbolise the
most centralised economic power and therefore they
should not be encouraged particularly in the drug
industry. However the local government interests
are always linked with that of the MNCs and there
fore just removal of MNCs will not eradicate
inequalities.
6. The profit motives of the drug industry
should be strictly monitored and kept in check by
a relevant drug pricing policy.
7. Doctors should correct their own miscon
ceptions about TB. They should realise that the
germ? theory is inadequate to eradicate TB. They
should also get rid of the stigma that they harbour
about TB itself. When doctors harbour such stigma
they perpetuate and legitimise it. The stigma that
the doctor harbours reflects the value system that
most of us inculcate during our education which has
a certain bias. This stigma is particularly com
mon in our attitudes to the poor, caste problem,
leprosy and TB and we need to fight against it.
8. Health problems cannot be solved by doctors
or government health departments. Th6y can be
solved only by creating people’s organisations.
Health is an indicator of the quality of life and
TB should be seen in this perspective. Enhance
ment of health would therefore be much more
guaranteed if health issues are taken up as a part
of wider people’s movements, ie., trade unions,
rural organisations of the oppressed, feminist
groups etc
9. Health education should be aimed at infor
ming people on their right to be healthy and their
right to prom.pt, effective, inexpensive and safe
treatment when ill. Health education should also
highlight myths related to TB or illness in general
and show how many of them’ are used by the elite
classes to perpetuate ignorance.
10. A conscious effort at the grass roots level
is necessary to build decentralised people's organi-
Towards a relevant TB Control Programme
Many of our members are involved at field
level in community health projects organised by
various non-governmental agencies in which TB con
trol is an itegral part. Based on their own field ex
periences and the discussion on the wider social
issues highlighted in the earlier report certain guide
lines were drawn up at the meet for all who are so
involved. These would help to ensure that their
involvement in the field of TB control would be
based on a clearer focus of the social reality in
which the problem dxists. It is also an attempt to
internalise the ideas and positive experiences from;
various case studies and projects discussed at the
meet.
3
I
2. The time period of each phgse and the spac
ing of the drugs depend on factors such as — a.
accessibility to clinic and health centre;
b. infrastructure available; c. cost? d. availabi
lity of drugs; e. stage of disease—serious and nonserious patients; and f. knowledge of patient com
pliance.
Many regimes taking these factors into account
are already recommended from which a selection can
be made.
3. While the regime is being dispensed it is
essential to ensure: a. psychological reassurance of
the patient; b. maintenance of a satisfactory doctor
patient relationship; and c. tactful information to
the patient to increase his ability to identify toxic
effects.
4. The use of supportive therapy such as cough
mixtures etc., should be done in a rational way
taking care not to overuse/misuse supplementary
medication.
1. Broadly speaking TB control programmes
should ensure the following three crucial features:
(a) A link with socio-economic and developmental
activity
(b) A stress on health education and awareness
building at all levels
(c) A commitment to community participation in the
decision making process and project evaluation.
It was felt that many of us who are working in
the field have already a sufficient rapport with the
community and the above could be integrated pri
marily by sensitising oursdlves to these issues.
Ensuring the above principles, certain specific
recommendations were made for practical imple
mentation during: A. Case Finding/Case Holding;
B. Drug Regimes; C. Training of Workers.
A. Case Finding/Case Holding
1. There is need to have a rough estimate of
how many TB patients ought to be in the area and
work towards identifying at least that number.
2. Involve health personnel at all levels in the
programme and also all the cadres of the govern
mental health service be they MPWs, CHWs and
Dais. Local indigenous practitioners and traditional
healers should als0 be involved.
3. School health check ups could be done as
an additional focus for case finding as in leprosy.
School teachers and high school students should be
involved in general awareness building.
4. People’s organisations like organisations of
the rural poor, workers, trade unions and other formal
and informal groups in the community should be
sensitised to the problem and involved.
5. Malnutrition surveys and m'antoux testing
could be adjuncts to case finding specially for
childhood. TB.
6. Patients who are on regular treatment or
have been cured should be actively involved.
7. The family of patients should be involved
in a positive way in the programe. Once they are
sensitised to the problem' in a positive way (rather
than feeling a fear or social stigma) they can be
helpful in making the community aware and also
bringing patients from other neighbouring families
for treatment.
8. The socio economic difficulties of patients
should be assessed and transportation fare and other
small compensation for wage loss etc., should be
provided.
C. Training of Workers
1. First the present knowledge/myths/perceptions existing in the particular area should be
studied;
2. The people should be taken into confidence
about the programme envisaged by the team! and
their participation in decision making ensured.
3. Grass-root workers at village level to be
involved in the programme should be selected by
the community. The selection should be based
among other things on personal motivation and
stamina.
4. The training of grass root workers or CHVs
should be undertaken in appropriate size of the
group (10-15).
5. The content of the training should include
cause of disease; symptomsi; case holding; side
effects of drugs and their management; and motiva
tion of patients.
6. The training should be theoretical along with
practical field training. The methodology should
include.
a. use of available aids, modifying them to make
them more relevant and meaningful to the local
area; b. involve the patient and get him' to talk
about his symptoms/difficulties etc., c. reinforce
the learning by continous on-the-job training; d.
older CHVs to be involved in training newer ones;
e. use simple laymen language and avoid technical
jargon; f. concentrate on training to communicate
effectively with patients and the community.
7. Periodic evaluations of the training pro
gramme should be undertaken eliciting feedback
from the CHVs.
8. Similarly an effective supportive supervision
plan and a system of continuing education in which
problems faced in the field are constantly identi
fied and discussed, should be included.
9. The CHVs should be trained to increase
community awareness of the existing NTP and the
availability of effective treatment as a right so that
B. Drug Regimes
There are several regimes which have been re
commended and are available in the existing litera
ture and also promoted by the NTI. Certain basic
principles to be followed before selecting the ap
propriate regimen are:
1. Technical — an intensive phase of two
bacteriocidal drugs and one bacteriostatic drug
followed by a maintenance phase of a bacteriocidal
and a bacteriostatic drug.
4
ND Hl,
200?
problem but as effective educators of their patients
in the preventive/promotive aspects of TB.
CHW training: There was a general feeling that
the existing governmental CHW training programmes
gave low priority and emphasis to TB control. The
lesson plans were limited and not integrated with
the rest of the training but given separately at DTCs
and PHCs.
From the experience of participants who were
involved in health projects in whiohf training of
CHWs was being undertaken there emerged the
need to include certain innovative methods of train
ing to make the CHWs more effective in the field:
These included:— (i) participation of senior CHWs
in training; (ii) learning through doing;, (iii) decent
ralised and localised training; (iV) participatory
methods; (v) use of locally developed or regionally
adapted AV aids and Sq on.
The group suggested that we in the mfc should
undertake to:
A. Review all available educational materials
and AV aids on Tuberculosis available from govern
mental and non-governmental sources and check
whether the points included in (1) above are present
and whether the social focus as identified in discus
sions exist.
(Anant Phadke agreed to study the TB Associ
ation Pamphlets for a start).
demands for more regular drug supply and more
effective government health centre services can be
generated. In the absence of such a commitment
the programme of NG’Os will become ends by
themselves duplicating the efforts of government
and supporting their inefficiency. In the long run
since voluntary agencies cannot build up parallel
structures to government health services, the catalyst
nature and the 'awareness of rights’ generation
nature of non-governmental voluntary effort should
be promoted.
Mona Daswani, Bombay
Sub-group Report
Para-professional training and community
awareness in TB
1. The objectives of health education of the
community should be to promote an understanding of
the medico-technological aspects of TB, the socio
economic-political aspects, the rights and responsi
bilities of the patients and people, the common
beliefs and superstitions and demystification of all
aspects of the TB control programme.
2. The responsibility of providing this educa
tion and awareness is the joint responsibility of
government and non-governmental agencies. However,
it seems that one of the main reasons why health
education has not been given top priority in the
NTP is because of the field reality that the existing
services (even if they are geared up) cannot cope
with the increased demands of TB patients, if
awareness becomes widespread. There seems to be
no other reason why even after decades of NTP,
there is still no rationally formulated and researched
communication strategy. TB Associations have play
ed their role but their efforts seem to lack continuity,
technical competence or creativity and are predomi
nantly urban based.
3. Health education efforts should creatively
and competently involve all sections of the commu
nity not only as recipients of awareness building
efforts but also as promotors of further awareness.
While focussing on all sections particular interest
should be taken of policy makers, politicians and
community leaders including the functionaries of the
gram panchayat.
4. Improving the communication skills of all
categories of health workers from doctors all the
way to the community health workers should be an
important part of the strategy. At present this is one
of the most neglected areas in the existing curricula.
5. The science syllabus of schools does not
equip children with practical knowledge of common
diseases in India or for that matter for healthy
living. There is considerable scope for incorporating
knowledge about TB in the science teaching of
schools. Schools could also become a focus
of creative involvement of school teachers and
children in health promotion.
6. There are a sizeable section of private
practitioners of non-allopathic systems who should
be involved in awareness building. They should be
involved not only in management of TB as a clinical
B. Review all available training manuals of
health workers (CHWs, MPWs, HAs) for the im
portance given, content, and focus of teaching of
tuberculosis.
(Marie D’Souza and Minaxi Shukla agreed to
undertake this exercise).
Based on the above two studies recommendations
can be made to policy makers, programme organi
sers and health educationists in the country.
Narendra Gupta,
Prayas.
Sub-group Report
Tuberculosis in Medical Education
The group focussed upon the problem' of produ
cing a socially useful doctor in connection
with
tuberculosis, and the hurdles in the present medi
cal education system that have to be overcome in
this direction. The group itself was a smiall one and
represented five medical colleges only.
Preamble
1. The basic structure of present day medical
colleges and medical curriculum, propagates a
certain value system, which is predominantly* exploitatory in nature;
2. We believe that propagating the attitudes
currently plaguing the medical system is a general
process, which involves the attitudes and practices
of faculty members, the expectations of our families
and society, and the 'traditional’ role of a doctor
3. That medical education is incomplete in
itself, unless the social dimension of disease is^stres5
system into the teaching that unless one’s clinical
judgement is backed up by labs, one is practising
'poor medicine’.
In fact, making a confident clinical diagnosis
with limited facilities available, is ‘good medicine’.
7. Emphasis is once again laid out on one
therapeutic regimen (ie., SM/INH/TA) for all TB
patients. The concept of suiting TB treatment to a
particular patient's background is not even
touched upon, eg., A labourer who can at
tend a TB clinic twice a week may be offered a
different treatmJent regimen compared to another
who can attend daily for SM injections. It is sur
prising that in spite of the fact that much of the
research work on alternative regimens of chemo
therapy emanate from India most of these well ac
cepted findings hardly find a place in medical edu
cation in the country.
Limitations of the discussion
We in our group were not able to touch upon
the following topics as regards medical education in
tuberculosis.
1. Research in tuberculosis and research prio
rity identification. Whether research and intervention
of a purely technological nature as is currently
practised by the NTI should be pursued or other
issues regarding socio-economic-political factors be
raised as well. Lack of research in communication
and education strategies which is a major lacunae,
also could not be discussed.
2. Continuing education of doctors about tuber
culosis; whose responsibility it is; and the form of
the continuing education programme. The group sug
gest that in light of the discussion a comprehensive
integrated model of teaching of tuberculosis should
be drawn up which can be tried out within the exis
ting constraints of the medical curriculum* in India.
As a preliminary process to this effort a much wider
feed back from) members in or of different medical
colleges should be obtained on their own experiences
of TB training in their education. This exercise would
establish a continuing link with the annual meet
theme of 1984 and probably could also be
featured in the Anthology of medical education under
preparatibn.
(Ravi Narayan, Vineet Nayyar, and Srinivas Kashalikar agreed to follow up on this along withf other
♦members).
Vineet Nayyar,
Vellore
fsed upon. It is for this reason, that many of our
senior colleagues (even those from NTI) believe in
purely technical or medical intervention for TB
control.
4. Priority of medical education as it stands
today, is directed towards the question of where is
the lesion? or what is the lesion? rather than how
was it caused and why? Our medical education does
not stimulate an average student to ask and seek
answers to social questions.
5. That trying to produce primary care doctors
in tertiary care centres is a major drawback in
itself.
Specific issues
1. We felt that the topic of TB as a disease is
dealt with in a fragmented way, and is dealt with by
several departments in a medical college. It is for
this reason that the dynamic nature of TB as a
disease is ill understood, and problems in TB con
trol not even perceived. Some of us even passed
MBBS with the notion that TB meningitis is a dif
ferent disease from pulmonary TB and so on.
2. Specialised departments involved in TB
education cater to their own fields (perhaps a part
of the bigger problem of medical education in a
large set up). Attitudes of the faculty mJembers are
built along the same plane. It is for this reason,
that physicians in the medicine departments absolve
themselves of the responsibility to teach about the
social aspects of TB.
3. Clinical medicine is glorified, while preven
tive aspects are looked down upon. Our system is
disease oriented and not health oriented. We look
at cavities and not at patients!
4. “Germ theory” of causati-on of disease is
propagated and medical intervention only is stressed
during undergraduate teaching. Even PSM depart
ments which undertake instructions in sociological
aspects of disease, have a narrow view of the dise
ase process. Most recommend medical interventions
as a solution quite like their own colleagues in clini
cal departments. Those that go a step further, preach
'better housing, more ventilation apd more food’
without understanding the deeper social aspect of TB.
Social action is almost never undertaken. Even
development projects which encourage incbme
generation schemes and other such social schemes
suppress a more basic question of unemployment in
society and so on.
5. Clinical teaching overemphasiises
that
tuberculosis is a common problem and only classi
cal cases are shown to an undergraduate. This propa
gates the myth that being a common disease, it is
eaiy to diagnose and manage TB. Realities of TB con
trol are never dealt with or discussed so that an
average medical student at the end of his final year
[never recognizes any problems concerning tuber
culosis.
6. There are dictums laid down by clinicians
who teach that investigations are essential to make
a diagnosis. While this is largely true in places
where facilities are available, it introduces a value
6
f
rXhlFc ShMm /vt>\ \ E
—
——
National Tuborcnlosis Programme —A dialogue. . ..
author’s information I am quoting only one exam
ple of Eskimo population around the Arctic circle
in whom the annual rate of infection was 25%
(highest ever known) but after the introduction of
a very intensive programme of diagnosis and treat
ment among the Eskimos, the rate of new cases
diminished to the levels observed in some Euro
pean countries eg. France. Thus the rate of inci
dence of disease and the risk of infection decreas
ed by 20% per year. Mass BCG campaigns were
not used (Rouillon et al Tubercle (1976), 57, 275299).
It is not possible to discuss the entire article,
published in mfc bulletin No. 105., as it would mean
discussing rationale of the programme in great
detail. However, we would like to point out a few
inconsistencies. The rationale of the programme is
for
already adequately
documented
and
additional reading the author may resort to K.
Toman^s book “Tuberculosis Case finding and
Chemotherapy; Questions & Answers'’ — a WHO
Publication.
a) Intercepting Transmission is not a mirage
The only sure diagnostic tool lor tuberculosis is
bacteriological examination, which has high degree
of sensitivity and specificity. Other tools like
x-ray or tuberculin are less specific and variable
from place to place depending on the users experi
ence and training. It is generally known and adequa
tely documented that about 50% to 60% of the
x-ray positi. e bacteriologically negative patients
ar.e not having active TB. It is, therefore' unethical
to close the diagnostic process on the basis of x-ray
reading and treat a patient as TB when he could
be suffering from a serious non-TB condition. As
regards use of tuberculin testing as a diagnostic
tool, w-e may not need to comment much.
1.
Thus it could be seen that when one wants to
treat ‘Tuberculosis,’ he has to be reasonably certain
of the diagnosis which the doctor can only be with
the help of bacteriology. So we feel the best servi
ces to the chest symptomatics, that has been provi
ded to these people is the extension of sputum diag
nostic services throughout the length and breadth
of this country. To us it appears almost revolutionary
extension oi scientific finding.
The quote of the article picked up from Dr.
D. Bancrji’s article does not find any place in the
article but rather contradicts his statement. What
is ailing the programme is the fact that even today
80% of felt need patients are turned away without
subjecting to the most scientific way of case-finding.
Indeed it is tuberculosis patients who themselves
showed the way to integration of services to General
Health Services. There is, in addition, sound admini
strative justification for dealing with all the health
problems of a community as an integrated whole,
demanding an integrated approach. Even as early
as I960' it was foreseen that extension of TB ser
vices to the community will be furthered with deve
lopment of infrastructure of general health servi
ces eg. through multipurpose worker or community
health guide. So today atleast fortnightly or month
ly visit to the patient’s home can be made through
this extension.
1
“Never in the hi4ory of human TB, a reduc
tion in transmission has been brought by a
specific medical intervention.’’
Medical literature is full of instances where it
has been achieved by medicab intervention. For
b)
2
Author's personal experience
While we do not disagree with the author that
his experiences in two DTCs must have been unfor
tunate, we feel that if he keeps the overall
perspective of the health programmes in view,
he will choose to change his opinion even with the
same experiences On DTP. The solutions thus does
not lie in attempting to remove inadequacies in
NTP alone but rather in the entire health services
system.
3.
Chemotherapy
The author wants costly effective drug regimens
to be made available in the DTP. There is no dis
agreement on this. But the system which delivers
these regimens must be adequately strong for the
regimens to be effective and regimens must have
higher acceptability. Researches are still being
carried out to find out what could be the problems
of delivery to be encountered. However, an opera- ■
tional study conducted by Dr, Baily showed that
Isoniazid -J-Thioadetazone regimen (82% Trial
efficacy) achieved 60% sputum conversion by 56%
drug regularity while Biweekly Streptomycin +
Isoniazid (94% Trial efficacy) achieved 68% sputum
conversion due to poor regularity of 31%. Short
course Chemotherapy regimens with 100% trial
efficacy have an intensive phase of 21 months with
4 drugs to be given preferably under supervision.
So acceptability of short course drug regimen is a
big question mark. Besides this, the author must
remember that under a “vertical malaria programme” even a five days radical treatment cannot
be effectively delivered to the population. A six or
a nine monthly regimen is a very different matter
altogether. The point is — do the people conform
more with a six monthly regimen compared to a
12 monthly or 18 monthly regimen. This is a cru
cial question, cost comes later. There are other
questions as well eg. availability of drugs, adverse
reactions due to drugs, their management. Hence
before unleashing this treatment measure on a
wide scale over the entire country, it requires to
be studied. On a pilot basis the new Short-course
drug regimens are being tried. We hope our pro
blems are solved soon and we are able to extend
the benefit of our findings for general use.
4
MFc
i
otj-
aJo ii$
NTP alone. However, it is only by analysing the
short comings of the NTP that we can move forward
towards a more rational and humane policy for
tuberculosis. And certainly the present lamentable '
condition of the DTC’s is not accidental, but a pro
duct of the entire strategy for tuberculosis, which
is in turn part of our health policy.
3. With regard to the question of chemother
apy, we can deal with the question of efficacy and
compliance later. Before that, we must answer two
questions.
a) To the safety of thiacetazone adequately
demonstrated, expecially considering that other
alternatives are available.
In Dr. Sen's presentation, cost has been made
out to be the only reason. But the reason is some
thing else. It is the ability to deliver the measure
which requires more emphasis.
Dr. (Mrs) P. Jagota Senior Medical Officer
NTI, Bangalore - 3.
The reply
Dr. Jagota’s reply to my article is a disappoint
ment. 1 do not claim to be an expert on tuberculosis
and I would have been happy to have been proved
wrong in the points I had made, through scientific
reasoning. However, her whole accent is on defend
ing the system at all costs.
To take her points one by one:
1. a. Relative
merits of sputum
smear and
X-ray as diagnostic tools: It has never been our
contention that patients should indiscriminately
be started on tuberculosis treatment on the basis
of an X-ray shadow alone. The contradiction exists
within the NTP. Examination of the records of any
District Tuberculosis Centre (DTC) will show that
a large proportion of cases under treatment are
‘sputum negative X-ray positive’ and their entire
treatment consists simply in a monthly doling out
Or TNHz TH. Does the NTP seriously believe That
these patients have tuberculosis or does it not? If
it does, then they should receive safer and more
effective treatment. It it does not, then these pati
ents should come off treatment.
Please refer to Toman—page 103.
“Thiacetazone in doses of 150 mg. daily given in
a single dose has about the same toxicity as PAS
(other drugs have less-B.S) its side effects includ
ing rashes, jaundice and bone-marrow depression.
Gastrointestinal upsets seem to be somewhat more
frequent with thiacetazon’e, especially in Asians.
Moreover, cutaneous reactions appear to be more
serious than with other drugs. Thus
exfoliative
dermatitis or Stevensf—Johnson syndrome may
occur if the drug is not stopped.’’
See also Toman page 120', where a detailed
study on thiacetazone toxicity is reported. “The
investigation suggested that thiacetazone might be
too toxic for large scale use in the population
of Singapore, whether Chinese, Malay, or Indian”.
May we know what the NTI has done to moni
tor drug toxicity in the field?
b) Why has the Government released second'—
line TB drugs in the open market and at the same
time prohibited their use in the NTP (upto district
level)?
Although these questions have been raised in
the article Dr. Jagota does not address them.
As for the problem, of acceptability of regimes,
it is my view that all questions of patient compli
ance are answerable in terms of the effort that has
been made to fit programme design and implemen
tation to the social milieu in which the programmes
are executed. In other words, the customer is always
right. Today
‘patient compliance’ views the
patient as a passive consumer and measures the
extent to which he is able to adopt the norms of an
extraneous system. A truer view of patient compli
ance would look at the dynamic interaction that
takes place at field level between the pati
ent and the treatment system. To say that a pro
gramme has ‘low acceptability’ is simply to beg
the question.
Dr. Jagota says that ‘researches are still be
ing carried out to find out what could be the pro
blem of delivery to be encountered’. The efficiency
of ethambutol against human tuberculosis has been
known since 1961, of rifampicin since 1968. What
has been done all these years?
Binayak Sen, Dalli Rajhara
If fact no physicians of any integrity would
treat patients on the basis of X-ray findings alone
Sputum negative X-ray positive patients are (pro
perly) diagnosed to have tuberculosis on the basis
of a series of clipical observations and therapeutic
trials to exclude non-tuberculosis disease. Perhaps
it is only a vertically oriented Government pro
gramme like the NTP that can afford to be so care
less with its clients.
Incidentally, it is interesting to find Dr Jagota
talking' about horizontal integration. She could
not have read the second paragraph of the article
too closely. However, as long as integration remains
merely an administrative concept, devoid of social
and political content, it will be ineffective.
1 .b) Dr. Jagota claims that medical literature
is full of instances where reduction in transmis
sion has been achieved by medical intervention.
This is a revolutionary claim, and will interest
well known, epidemiologists like Mckeown and
Navarro greatly. However, to back it up, she should
try to produce some-what more solid evidence than,
her example about ‘Eskimos around the arctic
circle’. It is perhaps a measure of the futility of
the NTI that they should think that this kind of an
example could be extrapolated to the Indian situa
tion.
Coming now to ‘author’s personal experience’
we a ree whole heartedly that the solution does
not lie in attempting to remove inadequacies in the
5
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent tos
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark's Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team,
Yours sincerely,
for DAF-Karnataka.
Gopal Dabade
To
( < 1? t
Ml C
i's of course asking for too much. Nowhere is an
understanding of the medico-technological aspects of
TB attempted with any grade of health workers.
‘Theirs is not to reason why ’ seems to be the general
attitude. In their training, viewing the bacillus under
a microscope is not even suggested.
The ‘Manual for Health Workers’ is available only
in English, at least in Maharashtra. An enterprising
Health Instructor in Dhule District translated it into
Marathi and got it cyclostyled. HWs in training
eagerly bought copies and it is now out of stock.
The manual does have several lessons on tuberculosis
(3). However in the training programme for Health
Assistants and Health Workers lasting 6 weeks, (6-day
weeks), 26 hours are for Family Planning, while only
4 hours are for TB (7). This is of course somewhat
better than that allotted for CHVs.
The HWs are expected to carry out the preventive
measures for TB control i.e., case-holding, BCG
vaccination, and health education. The storage
preparation, administration and the results of BCG
vaccination is explained in great detail (2). As regards
to health education, except for a film on TB no aids
are available. But the Health Assistants are asked to
check on the educational programmes on TB organized
by the HWs whether talks, group meetings, exhibi
tions etc. And in their training, while the HWs have
guidelines in plenty for educating the community on
Family Planning, there arc none on TB (7).
The focus of all the teaching and instructions on
TB in the Health Manuals is the services offered to the
community in the line of diagnosis, treatment, and
prevention through BCG. As mentioned earlier, no
stress is laid on health education of the community,
for which purpose the CHVs should be trained and
aids provided. In the preparation of aids it will be
useful to keep in mind what is mentioned in their
own manuals (5). Aids should be simple with em
phasis on one idea. Therefore, EITHER treatment
is free OR treatment must be taken for 18 to 24 mon
ths OR the result of indiscriminate spitting etc., must
form the single messages. The health education
material available so far have either too many mess
ages incorporated into one presentation (eg. film by
the TB Association, the slide show by Janscva Mandal), or only one message prepared by different or
ganizations—“TB is curable” (eg, CMC, VHAI,
CHETNA). VHAI does have two other sets on
‘childhood TB’ and ‘BCG vaccination’ which I have
not been able to review.
In the Health Manuals, the following are some of
the lacunae which needs to be filled in while preparing
health education aids.
1. Relatives of TB patients to be checked for TB.
2. Patient to cover the mouth while coughing and to
spit into a receptacle; sputum to be later disposed
off.
3. Study made of local diet habits in order to suggest
improvements on what foods the patient should
take more of. (The Manuals only say there is no
need for expensive or extra nutritious food.)
4. The bacilli find fertile soil in a malnourished indi
vidual.
5. Taking irregular and haphazard treatment builds
resistant strains of bacilli with the resultant resis
tance to drugs.
6. As a result, responsibility of the community to see
to that the patients avail of the treatment available
at the Govt, health institutions.
7. This requires awareness on the part of the co
mmunity about the TB Control programme, the
funds available for TB Control in the District
and the drugs available at the PHC so that if drugs
run short as often happens with streptomycin
injections demands be made for allocation of the
required amount of drugs.
Lately, in Nandurbar Taluka of Dhule District,
people diagnosed as having TB, receive their tablets at
home, every month, delivered to them by the HW.
Presumably this is one activity now included in the
NTP all over India. Surely case-holding will have
improved since previously patients had to cover long
distances to reach their PHCs losing their wages etc.
Hopefully the NT1, who had decided at their
Silver Jublee Proceedings that one of their future
efforts will be health education, will take note of the
above recommendations.
Materials reviewed:
1. Manual for Community Health Workers.
2. Manual for Health Worker (Female), Vol. I.
3. Manual for Health Worker (Male), Vol. II.
4. Manual for Health Assistants (Male and Female).
5. Primary Health Centre Training Guide, Part I,
Training Methodology.
6. Primary Health Centre Training Guide, Part II,
Training of Community Health Volunteers.
':
7. Primary Health Centre Training Guide Part IV,
Training of Health Assistants (Male and Female)
and Health Workers (Male and Female).
(All are published by the Ministry of Health and
Family Welfare, GOI).
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent tos
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark’s Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team,
Yours sincerely,
for DAF-Karnataka,
Gopal Dabade
To
M r c- r<
r
-e ln f
7 -1
/
Tuberculosis and Paramedical Workers
(Review of Training Manuals of Health Workers)
at least the minimum possible about TB. They are
taught—that it is caused by germs, affects the lungs, is
diagnosed by sputum examination and x-ray, is curable,
treatment should last for at least 12 months and that
the diagnostic and treatment facilities can be obtained
free from the government health institutions. CHVs
are advised to refer persons with cough and fever of
more than 15 days, and are informed that infants are
to be vaccinated with BCG.
.—Marie D’souza.
From the review of the training manuals prepared
by the Ministry of Health and Family Welfare listed
at the end of the article certain facts emerge clearly.
(I was not able to get hold of the ‘Manual for Health
Workers, Female, Vol. IF and the ‘Manual for Health
Workers, Male Vol. I).
The CHVs who are closest to the people infact
one of the community, arc not taught, much less
motivated towards the preventive aspects of TB. Nor
are they expected to give any health education to the
people.
Common beliefs and superstitions regard
ing TB are not discussed with the CHVs. Their tasks
seem to be to report suspect cases to the Health
Worker (HW) and advise patients to continue treat
ment.
Family Planning is the programme to work for.
Tuberculosis is not given any extra attention as com
pared to other diseases, though malaria holds prece
dence over tuberculosis in importance.
In a suggested schedule for a training programme
for Community Health Volunteers (CHV) lasting ten
weeks (4-day weeks), the time table is detailed.
Family Planning is allotted 9 hours, malaria 7 hours,
smallpox 5 hours, while tuberculosis is not even men
tioned. J suppose it is included in the one hour allo
tted for immunization (6) (Why 5 hours for smallpox ?)
However, the ‘Manual for Community Health Workers
does have a chapter on tuberculosis from which it
can be concluded that the CHVs are expected to know
All the training manuals emphasise only the germ
theory of tuberculosis. HWs are informed that
crowded and dirty living conditions help spread the
disease (3).
x z. That the germ finds fertile soil in under
nourished individuals is not even mentioned. To
expect that the manuals will discuss causes of under
nutrition (poverty, unemployment, unjust society)
6
I
I
109
*
medico friend
circle
bulletin
A/yw
_____ =#=
JANUARY
1985
3C9
Editorial
The Bhopal Disaster
world in which violence, waste and
( m
and those who manipulate our behaviour,
.................
"'«■
»/
M
—Anwar Fazal
International Organisation of Consumer Unions
The world’s worst ever man made industrial and
100R4g,tCnKtra8?dLtO°k pace On ,he 3rd of December
84 at Bhopal. 30 tonnes of stored methyl iso cyanate
escaped into the atmosphere killing over three thou
sand people and over 3000 cattle and affectine over a
People (oftcial estimates!). Even these shocking
statistics hide the actual enormity of the human
tragedy — of the hves lost, the families affected the
people blinded and ill and the thousands impoveri-
licity has led to the spontaneous formation of citizens
groups and collectives to look into not only the
deeper issues of this event but also to prevent such
renv /2?he, future’ Zahreeli Gas Kand Sangarsh
Samit, (Bhopal), PARISARA - Movement lor Envi
ronmental Protection (Bangalore), Movement for a
e Environment (Bombay) and Movement for Envi-
Notwithstanding the phenomenal huirjan tragedy
un-TT1118 Ca^Sed by this event wh’:ch need relief
rehabilitation and compensation efforts, all concerned
citizens should not miss the opportunity to analyse/
understand the deeper socio-political and techno^
gical crisis of which this disaster is only a symptom.
This is the time to question
Hheki01e x°f IJluItin?tional corporations and the
ouble standards in their functioning in the
developing world;
6
—
the governments role and complicity in impro
per siting continued licensing, improper moni
toring of dangerous industries and in the
tfons1111
°f itS °Wn ruIeS and r^u,a-
the national industrial and d^
v.
developirjent
policy
in the light of people’s health and ecological
issues;
—
the political exploitation of the poor especially
the slum dwellers and workers;
~
2n„n<Ck °f awareness amoas people, citizens
groups, consumer groups, workers unions
heSarsyafeOtrganiHati°nS and aCti0n gr0l,Ps on’
nealth, safety and environment issues;
—
the whole question of the right to information
at all levels and the existing control/monopoly
of information at multinational and govern^
ment and professional levels;
—
the basic question of the relevance of pesti
cides to our agricultural economy in the light
of available scientific and social knowledge
regarding the disruption of eco-systems and the
ong term effects on land and agriculture
This bulletin issue is a start in that direction and
mcludes a memorandum from Bombay of which mfc
merrbeX th"’
r6port from
°ur
meir.bers of the dynamics of relief work in Bhopal
and an overview of the efforts of unions and workS
m occupatmnal health action in the US
WOrKers
rn c
J
I 0
wva
H
b
A report From Bhopal
Learning from the Relief Work
abhay bang*
An article in mfc bulletin on the Bhopal disaster
is expected, by tradition, to focus on the political
and economic reasons behind the tragedy. For such
analysis the readers are recommended to read two
excellent papers by Barry Castleman**. T shall also not
attempt to investigate and describe the chronology
of events. Newspapers have published a lot of infor
mation on that and 1 am* no wiser than the journalists.
As the title suggests I shall restrict myself to the relief
aspect, that too mostly in relation to public health,
for there were ample things to learn from that alone
of people with respiratory symptoms. Many also had
vomiting. The medical personnel were in the dark
about the harmful effects of methyl iso cyanate
(MIC). They were not even certain whether it was
MIC or phosgene gas: so the fear of the coming
unknown effects was looming on everybody. 19 cases
of CNS involvement were reported in the Hamidiya
Hospital. This gives credit to the rumour that on
autospy, cerebral oedema and haemorrhage were often
found.
When the Gas Struck
When we reached Bhopal on the morning of 5th
December, the administration had overcome the
initial shock and relief operations had begun. Hospi
tal staff, interns, and medical students; various social
and religious organisations had responded quickly.
Food and blankets were being distributed freely.
Dead bodies were being removed.
The Ongoing Relief and its Criticism
When the gas struck at about 1.00 a.m. on 3rd
December, people woke up with a severe sense of
suffocation, cough and irritation in the eyes. Most
of the deaths were instant due to suffocation or pul
monary edema. The worst hit were children, many
of whom died in bed. The result of this cruel pre
ference of the gas was that very few children remai- ,
ned orphan, because usually children died before their
parents.
The first instinct of the medical profession
naturally was to offer symptomatic relief to the
sufferers. As the hospital was full with the dead or
very serious, most of the relief work was done from
temporary tents. About 100 such medical relief clinics
were opened in the premises of the hospital or on the
roads near the affected areas. Doctors were treating
long queues of patients. The method was typically
uniform everywhere, with some obvious shortcomings.
It is almost a universal law that the poorest live
in dangerous areas. When a flood strikes, the people
who live on low land and are the most affected are
always the poor. Bhopal was no exception. People
living in the immediate vicinity of this chemical vol
cano, were mostly slum dwellers. But besides this
fact, two other disturbing pieces of information
explain the very striking class distribution of the
victims.
No case papers were made. Hence the identity
of the patients, physical signs and the treatment
given — nothing was being recorded. The reason
offered was that the doctors were too busy treating
people and records were not the priority in such a
situation. The result of course was that medicines
were distributed like toffees. One of us saw a child
taking an injection and then running to his friends to
boast that it was his sixth shot that day.
The residents of Jayaprakash Nagar slum which
is the closest and the worst affected area, categori
cally state that at about 12 O’Clock midnight, all the
workers in the union Carbide plant fled away in the
factory buses but no siren was blown. It means
factory staff came to know about the impending
danger at 12 and safely escaped without warning
people or the police. This may explain the strange
fact that only one worker of the factory was injured
by the gas when hundreds were working in the night
shift.
People were the first to recognise this deficiency
and started losing faith in such totally adhoc and
symptomatic treatment.
Interns and doctors running these clinics were
not given any guidelines for treatment by the senior
doctors. Hence they were using medicines in the
most bizarre way.
Similarly, it is alleged that on coming to know
■ of the danger, most of the police and other govern
ment officers and the ministers escaped out of Bhopal
by the government vehicles at their disposal, instead
of trying to warn or help the people. Rich also fled
in their private vehicles. Those who did not have
any vehicles, obviously the poor, had to face the gas.
No attempt was made to train or involve non
medical volunteers or family members. Thus for con
junctivitis, even eye drops were put in the eyes by
the doctors alone.
This resulted in an unending
burden on the doctors; and the patients were able to
The immediate effect of the gas on the survivors
was irritation of the mucus membranes of eyes and
the respiratory tract, leading to severe and widespread
conjunctivitis, sometimes keratitis, and a large number
* Gopuri post, wardha dist Maharashtra-442112
* • International Journal of Health Services Vol. 9, No 4 (1979)
and Vol. 13, No 1 (1983)
3
get eye drops in their eyes once a day whenever they
could reach the doctor through the long queue.
3.
No certificates of death or disease were being
issued. There did not even exist a reliable method of
recording and counting deaths, which resulted in
widely varying estimates of death from 2000 to 6000.
This neglect may become a tremendous handicap to
the poor to get compensation whenever that comes.
4.
5.
Besides the sheer magnitude of the problem,
another reason for such erratic medical relief was
■ that it was put in the hands of clinicians. When
200,000 people were affected, it was absurd to control
the medical relief operation from the hospital by the
medical superintendent. Though a very decent man,
he thought that respirators were the most important
need of the hour. The whole operation was carried
out from the clinician’s point of view. This resulted
in such decisions as offering treatment in clinics
expecting victims to come there. Clinicians can only
see those who come to them and never know about
those who don’t come. This deprives them of the
total view of the situation. We found that a large
number of victims were not going to the clinics due
to reasons like despondency, inability to walk because
of severe eye problem or loss of faith in the quality
of the relief offered.
(B)
A quick and crude survey of the remaining
residents of JP colony showed us that about 50%
had eye problems and about 25% had respiratory
symptoms. Surprisingly a large number of people,
even those with minimum respiratory symptoms, had
rhonchi and coarsQ crepitations in the chest. It
seems that the irritation by the gas had produced
chemical bronchitis and bronchopneumonia on a large
scale. As many of such ‘mild cases’ were not being
examined, clinicians in the OPD could fail to appre
ciate the widespread nature of the respiratory involve
ment. Unfortunately all these facts were not docu
mented and hence, it seems, the real epidemiology of
morbidity may never be known.
The experience
The experience of the next 10 days work, as
reported by the social worker in charge of the opera
tion was as follows:
—
Alternative Plan
We planned a relief program to be run by
SEWA, a local Women’s organisation for a small but
defined population. The main features were:
(A)
—
Fem'ale social workers from SEWA visiting all
the houses in a slum of 1000 families for
1.
population enumeration
2.
identifying dead, lost or moved out persons
for compensation and economic rehabilita
tion of the family
Doctor visiting all the houses, examining those
with respiratory symptoms and suspected kerati
tis (identified by social worker), recording phy
sical signs and treatment given. We thought
that all the persons with rhonchi and/or crepi
tations should be given an antibiotic cover
(preferably inj. benzathene penicillin) as they
carried a great risk of catching secondary infec
tion, similar to one after an attack of measles
or influenza .
We thought that the treatment should be
provided at home so that all the population
will be identified, examined and treated, which
can not happen in an OPD set up. This was
specialty important for the documentation of
morbidity as many victims did not go to OPD.
(Cj All the population to be followed up for coming
few weeks to provide continuous care and recor
ding complete impact of the tragedy.
Two doctors, three interns, four nurses
and about ten fem'ale social workers could be
mobilized and were explained the deficiencies
of the ongoing relief operations; and the con
cepts and methods involved in the one planned
by us. Forms for population enumeration and
case records, and guidelines for survey and
treatment were prepared and explained. Un
fortunately I could not stay longer but felt that
the plan was well explained and agreed upon
by the team.
This also meant that the real number of the
people affected would never be known. The estimates
of the number of patients treated varied from 65000 to
1,50,000 and each estimate may have counted the
same patient many times and totally missed those
who did not attend the clinics.
'
screening of all persons for the presence
of symptoms which started with the gas
exposure and recording these
uncomplicated conjunctivitis and gastritis
to be treated by the social workers, involing and training the family members in eye
care and handing over a tube of eye oint
ment to them
identifying patients with suspected kerati
tis and patients with respiratory symptoms
to be examined by doctor
—
—
4
On the first day when the team went to the
slum and started home visiting, doctors pro
tested that it was not their job and they set up
an OPD. At least half of the doctors could be '
pursued to continue home visiting
Doctors could not accept the idea of social
workers treating conjunctivitis and kept all
the clinical work to themselves
The doctors in OPD refused to write physical
signs and diagnosis in the case papers on the
ground that it would take time and the fact
that the diagnosis could be guessed from!
their treatment
The typical treatment given was:
I
MR
Lessons
: eye drops put once in a day by doctor oi
nurse;
: cap tetracycline one TDS tor one day;
: tab B Complex;
: tab multivitamin;
: corticosteroid injection
—
1.
2.
All the time saving devices in the plan like
training and delegating easy tasks to social
workers; using eye ointment which has longer
duration of action than eye drops; using benzat.hene* penicillin to ensure week long antibiotic
cover, were stubbornly refused by the doctors.
It was not possible for the social worker to
over rule the medical supremacy.
3.
4.
5.
The physical signs recorded by the doctors by
home visiting were usually of poor quality. Some
examples are:
—
•—
—
chest clear, crepts present
mild crepts found (there is nothing like ‘mild
crepts’)
slight coarse crepts + ve
6.
Each doctor used his pet expression and the
recorded signs were monotonously the same in all the
patients examined by the same doctor. Obviously the
doctors did not examine sincerely or they were not
at all sure of their findings of physical examination.
In spite of these short comings, this relief
approach gained instant popularity mainly because it
was the only place in Bhopal where case papers were
being prepared and records maintained. People quickly
realized its importance and even asked for records
to be given to them'. The relief authorities in the
city brought foreigners to proudly show this operation.
7.
Surprisingly and fortunately the tide of secondary
infection did not occur anywhere and hence the
death toll did not continue to rise after the first 3-4
days. The reasons for this reluctance on the part of
micro organisms to invade damaged respiratory tracts
are not understood.
Antibiotic cover was either
not given or was very inadequate for most of the
affected persons; and hence, cannot explain the
phenomenon.
After 10 days of working when the operation
neutralization of the stored MIC started most of the
relief work was wound up as the people fled away.
At that time, eye problems had considerably reduced
but the respiratory ones had continued, though at a
reduced level.
I recently learnt that the ICMR has declared a
decision to develop a plan of long term surveillance to
find out the effects of gas exposure. That would be a
stupendous but very valuable task, specially because
industrial toxicologists in the West are predicting
that 5 to 10 percent of the affected will have chronic
respiratory diseases.
1
The compensation for death and disease may not
be fully available to all due to lack of records or
evidence.
5
Organising mass medical relief in a disaster
situation should be done not with a clinical
approach
but
a
poputation/comm'unity
approach;
Persons in responsible positions should be
trained for disaster management in anticipa
tion;
There should be continuity in the planning
and implementation of any program, the lack
of which was responsible for improper imple
mentation of our plan;
Record keeping and documentation is vital in
all such operations;
Besides their well known bias against delega
tion, even the clinical performance of the
doctors was a sad comrrjentary on the outcome
of medical education and the standard of the
profession. One tends to question the right
of objection by the medical profession to the
use of auxiliaries or village health workers on
the ground of the lack of professional training
to them.
The Bhopal tragedy acts as a warning signal
to all socially conscious persons that industrial
hazards and pollution are no longer a remote
problem restricted to the developed countries.
As Barry Castleman points out in his earlier
mentioned papers, developed countries are
rapidly exporting their technology, production
processes and products to the third world
without proper safety measures or information
and education to the people.
The Bhopal tragedy can be a powerful tool in
the hands of environmentalists and consumer
and citizens rights groups. A careful documen
tation of the ill effects — medical, social, eco
nomic and ecological —- will go a long way
to support the efforts of such groups.
112
medico friend
circle
bulletin
A?RIL
1985
Medical Research In Bhopal
—Are we forgetting the people?
Concern for man himself and his safety must
always form the chief interest of all technical endea
vours. Never forget this in the midst of your diagrams
and equations.
—Albert Einstein
Preamble
In a tribute to the medical relief workers
involved in service to the Bhopal disaster victims the
ICMR has noted (1) that a disaster of such magni
tude of such suddenness and caused by the please
of a highly toxic chemical methyl isocyanate (MIC)
into a densely populated habitat is unparallelled in
human history. The doctors, medical students, civil
servants, governmental, public sector and voluntary
bodies and the people themselves rose to the occasion
in a human gesture equally unparallelled’. . .
In the absence of authoritative information on
the released gas; the unwillingness of the company to
part with authentic information; the unpreparedness
of the local bodies and the government health autho
rities to understand the consequences of the disaster;
and the absence of technical or toxicological exper
tise on MIC among our scientific community, it was
imperative that a national body like the Indian
Council of Medical Research through its own initia
tive would have to harness the scientific medical
expertise in the country including the local medical
college community to meet this challenge. Conside
ring that the affected population was over 2 lakhs
and that the dead were over 6000 (though official
estimates are 2000!) this research initiative had to be
equally unparallelled in meeting the phenomenal
challenges of the world’s worst'recorded ecological
disaster. Do the records of events in the past four
months since the disaster bear this out?
The Plan
A report on the first nine days of the Bhopal
disaster identified (1) three objectives for the ICMR’s
research programme:
1. To establish a clinical and patho-physiological profile of the hazard which would
also provide clues for improved patient
management and clinical outcome
2. To study the long term sequelae of toxin
exposure to lung, tissues, foetus, genes and
cancer induction
3. To obtain a basic understanding of the
biological alterations associated with MIC
exposure.
Strangely enough there is no mention in this
report of a strategy by which conclusive research
data as and when available would be transmitted to
the relief and rehabilitation effort in Bhopal, ie., to
the treating doctors and through a health education
effort to the affected public.
A report of projectization of ICMR supported
research effort (2) lists out 17 study projects which
covers acute and long term health effects, lung func
tions, follow up of children aged 5-15 years, ocular
changes, pulmonary and neurological changes,
growth and development of new borns, clinical and
forensic toxicological studies, pathological and
microbiological investigations, radiological studies,
biochemical and immunological studies, carcino
genicity, mutagenicity, teratogenicity and chromo
somal changes, data management information system,
hospital based cancer register, cytofluorometric
hi,
Issues of concern
studies and blood gas analysis. The studies ranging
from a time span of 6 months to 5 years would incur
a total financial outlay of 1.07 crore rupees.
-X
!•
An mfc fact finding team which visited Bhopal
in mid February at the request of various non govern
mental agencies and action groups published a report
on the realities of medical research and relief which
has been widely circulated and is now well known(9).
In mid March an mfc team of 16 members camped
in Bhopal and undertook an epidemiological survey
which included detailed history taking, physical exa
mination, lung function tests, haemoglobin estimation
of a 10 percent sample of a severely affected area and
a control area(lO).
■-
Some surprising on! jssions in the list were the
assessment of psychologic stress and its manifestations in the affected families, studies on health of
women (not obstetrical outcome but gynaecological
effects) and the assessment of medico social effects
like reduced earning capacity and functional disabi
lity which would affect rehabilitation efforts. Though
there were references, to an epidemiological and
community based outlook the research endeavour atleast as on paper did not seem to be a coordinated
holistic effort in understanding the total problem
but basically a series of vertical research programmes
initiated and funded according to the interests of the
professors involved in the exercise.
The team also met decision makers, relief and
service providers, medical teams of voluntary agencies
and others, apart from undertaking a survey of the
people’s perceptions of relief services and an overview
of the services itself. The findings of the team are
being analysed and will be reported shortly (a press
release is published in this issue) but the experience
of the third week of March in Bhopal strengthened
the findings of the earlier fact finding team and
identified a whole series of issues of concern in the
ways in which research efforts were becoming
exploitation of peoples’ suffering rather than expres
sions of support to programmes of human welfare.
Results
It is four months since the tragedy and about
three months since many of the research programmes
got underway.
As far as a communication strategy goes three
press releases and two lectures by the director
generals and a minutes of the meeting on the thio
sulphate controversy are the only freely available
literature on the research (3-8) efforts. From these
all that any member of the scientific community or
the general public can gather are:-
i.
that there is no evidence of irreversible
eye damage or blindness
ii.
that the autopsy findings are indicative
of severe respiratory damage caused by
pulmonary odema and asphyxia
iii.
that studies of exposed persons with lung
symptoms/signs have shown obstructive
and or restrictive abnormalities
iv
that a double blind clinical study under
taken using sodium thiosulphate and
a placebo has established that sodium
thiosulphate administration results in
symptomatic improvement and in increa
sed excretion of thiocyanates in the
urine. On the basis of clear cut results,
the State government has been advised
to administer sodium thiosulphate to the
exposed population and detailed guide
lines have been drawn up and circulated.
1
1.
Lack of dissemination of technical guidelines
The medical relief services continue to be
starved of authentic and authoritative scientific
medical information to support clinical judgment and
patient management. In the absence of clear cut
guidelines from the seniors in the profession treat
ment continues to be adhoc, symptomatic and
unstandardised. Findings of autopsies, lab investi
gations and x-rays and other tests are not available to
the treating doctors. Doctors have not been alerted
to the fact that a wide range of symptomatology like
fatigability, weakness, memory problems are all part
of the MIC syndrome. In the absence of such
information peoples’ sufferings have often been passed
off as malingering or compensation neurosis.
2.
Pill distribution
The treatment basically consists of a whole
series of pills which are efficiently and actively
prescribed to the people in a sort of conditioned
reflex. In the absence of proper record linkages each
patient is collecting large amounts of pills and not
feeling the better for it, apart from the dangers ot
over drugging. Other forms of care, counselling and
non-drug therapies have not been thought of.
that two visiting psychiatrists have
found that 10—12% of the affected indi
viduals attending the medical clinics in
Bhopal are presenting with psychiatric
manifestations — symptoms of anxiety
and depression are foremost.
3.
The Thiosulphate controversy:
Even after the ICMR studies establishing the
validity of thiosulphate administration and the pre
paration of clear cut guidelines for its administration,
(6,8) this specific antidote is not being used as
effectively as it should be. It has become a casualty
in a medical controversy between cyanogen and
carbon monoxide lobbies and the victims rather than
being informed and helped are being confused and
neglected.
Why this secrecy? or is it administrative over caution?
A more updated report prepared in mid March
collating all data as of that date has again become a
casualty in the commitment to secrecy (caution!) and
no press release has followed.
2
xxx rih/w x n r okofi
No. 367, ‘Srinivasa Nilaya*, Jakkasandra, I Main Road,
I Block, Koramangala, Bangalore - 560 034.
30th June, 1992.
Dear
Greetings from Community Health Forum L
This is to inform you of the next CcHo Forum meeting s
Date
s
11th July 1992 (Saturday)
Time
s
2^ 00 p.m.
Venue
3
Ashirvad,
30, St. Mark’s Road,
Bangalore - 560 001.
(Phone - Ashirvad
C.HL Forum
Topic
3
to
4.30 p.m.
- 210154
- 531518)
"COHlfflNITY HEALTH CELL"
You are aware that it is a year since the C.H.C. has registered
as " S®ci£ty for Community Health Awareness, Research and Action”.
Members of C.H.C. will be briefly reviewing the past activities,
sharing with you its concerns and initiatives, while putting up
plans for the future.
As members of the C.H. Forum and friends of C.H.C. we EARNESTLY
request your participation, ideas and viewpoints to enable a common
initiative towards Community Health.
Do mark this date/time in your schedules and looking forward to
our meeting.
With regards and Best Wishes,
Yours sincerely,
for CC?liiyNITX.AHEALTH FORUM,
—T
-
SHlRrXI
eIrASAD
. y- /
TEKURL'
nt r
A)(c
4.
IMA, voluntary agencies, action groups that there
are urgent needs to be actively met :
Women’s health
The mfc fact finding team had highlighted the
problems of women who have suffered abortions, still
births, diminished foetal movements, suppression of
lactation, abnormal vaginal discharges and menstrual
disturbances. The studies undertaken by two doctors
of mfc reported in this bulletin (11) establish the mag
nitude and severity of the problem. It, however,
continues to be neglected by the concerned authorities.
5.
* Need to evolve a bold, imaginative and open
communication strategy to all the doctors and health
workers (treating the disaster victims) who are present
ly starved of authentic technical/medical information
hampering clinical judgment.
* Need to evolve a creative, relevant health
education and awareness building public education
strategy to meet the expectations of the disaster
victims and to help and reassure them through the
crisis and prepare them for the eventualities.
Absence of Health Education efforts
Whatever the other validity of the research efforts,
in the ultimate analysis it should get translated into a
strategy of health education and awareness building
of the affected people. As of date there are no
official guidelines or efforts in this direction. The
range of areas is phenomenal—advice to mothers of
the risk to the foetus and preparation for conse
quences including options for MTP, advice to couples
on contraception till detoxification is over, breathing
exercises and antismoking advice to those with
fibrosis of lungs, avoidance of overdrugging of
pregnant mothers, advice to mothers regarding feeding
of infants/children as lactation suppression has taken
place, availability of thiosulphate and other medical
relief measures. None of this has even been recogni
sed as being necessary.
6.
* Need to ensure that research efforts are geared
to supporting relief and rehabilitation efforts and
not become esoteric exercises for institutional deve
lopment and career advancement.
* Need to make the commitment to patient care
and human welfare primary and to ensure that it does
not get bogged down by professional rivalries, inter
departmental incoordination, procedural constraints
and administrative protocols.
♦ Need for closer coordination between voluntary
agencies, action groups, citizen committees, medical
and health workers and the people oriented and
socially sensitive sections of the medical profession
and government authorities to ensure that the peoples’
suffering are not exploited and made pawns in the
games played by politicians, multinational compa
nies, and misinformed professionals—all symptomatic
of an exploitative social system.
Poor epidemiological and medico social orien
tation of problem assessment
The general impression is that research and
relief efforts are suffering from an acute clinical and
institution based orientation rather than a community
based epidemiological orientation.
An authoritative Lancet editorial (12) had
mentioned that Tn a year’s time we will have learned
a lot more about methylisocyanate at an appalling
price’. With the prevalent medical anarchy in Bhopal
in relief and research, this price may be immeasurable.
—mfc team. Bangalore
Only if all data is field based and is related to
known available morbidity patterns (or comparison
with controls) can early problems and special trends
be identified and urgently acted upon. The danger
of getting into the pursuit of a very neat and fool
proof epidemiological planning exercise can be equally
counter productive.
7.
References
Lack of informed consent
1. ICMR, The Bhopal disaster — current status (the first nine
days) and programme of research
2. ICMR. Projectization of ICMR supported Research
3. ICMR, Medical Research problems in Bhopal (V Ramalingaswami)
4. ICMR, Pathology and clinical toxicology of the Bhopal
disaster (S Sriramachari)
5. ICMR, Medical research on Bhopal Gas Tragedy — press
release 31st Jan 1985
6. ICMR, ibid, press release, 12 Feb 1985
7. ICMR, ibid, press release, 27th Feb 1985
8. ICMR, Thiosulphate therapy in MIC exposed — minutes of
meeting at ICMR, 14 Feb 1985
9, mfc. Medical Relief and Research in Bhopal —the realities
and recommendations.
10. mfc. Approach document of a project to evolve a strategy
of medical relief and rehabilitation which best meets the
peoples’ medico social needs and expectations
11. Rani Bang, Effects of the Bhopal disaster on the women’s
health — an epidemic of gynaecological disease: reports
I & II
12. Lancet editorial, Calamity at Bhopal, 15 Dec 1984
The people are not being informed about the
tests being done. Nor is consent being taken for
being included in the studies or for procedures to
which many of them are being subjected to. This is
a minimum medical ethic.
8.
Lack of coordination
This is a universal problem and the ultimate
sufferer’s are the disaster victims themselves. This
incoordination is occuring between goverment
services and research efforts in the medical college,
between the different research workers themselves,
between government and non-government relief
efforts, between voluntary agencies involved in action,
relief, rehabilitation and of all these groups with the
disaster victims themselves.
While a more detailed report is awaited, we in
the mfc appeal to government decision makers in
Bhopal, medical college professors, ICMR scientists.
3
114
medico friend
circle
bulletin
JUNE
EDITORIAL
1985
—
THE
CHALLENGE
OF
BHOPAL
"The growing multinational culture must be destroyed because it leads to economic chaos, increased
social disparities, mass poverty andfilthy affluence in coexistence, environmental degradation, and ultimately
civil strife and war.
To get a balanced, rational development and to preserve the environment, a new development process is
needed. The biggest intellectual and political challenge of our times is to articulate and demonstrate this
new kind of development."
— A statement of shared concern
Citizens report on state of India’s Environment, 1982.
Its six months since the worst industrial and
environmental disaster in recorded history. Bhopal
has not only been a nightmare for those who were
there on the night of 2/3 December, 1984. It is
also a portent of events to come.
World Environment Day (5th June) has
come and gone. There have been the usual meetings,
seminars and lectures, the usual lip-service to eco
logical sensitivity, the usual narrations of the
health and social hazards of environmental pollu
tion and the usual pious recommendations of what
dan and should be done.
How many more Bhopals will we need in this
country before we are shaken from our apathy?
—from our callousness to our disadvantaged
'and exploited fellow human beings who are
always the worst hit in such disasters.
•—from our insensitivity to nature, our forests,
our rivers and our land.
—from our insensate rush for chemicalising and
technologising our lifestyles.
—.from our race for profits even ’at the cost of
the health of our workers, our people.
The medical community in India will be
increasingly called upon to respond to the medical
and health problems caused by more ecological
disasters. What will our response be?
Will we see every disaster as a chance to
refine our clinidal skills, satisfy our charity and
welfare urges, exploit the research poten'ti'al for
career development and use the opportunity to ask
for more and more sophisticated gadgetry for our
institutions?
Or will we be challenged by these disasters
to rlaise our voice collectively to oppose the unheal
thy trends in our society to use our knowledge
and social potential to support the growing aware
ness for a healthier and more egalitarian social
system; to use our research skills to strengthen and
concientise our fellow human beings to an increas
ing health 'and ecological awareness.
The dilemma of a man who enters a room
to find a tap running and a wash basin overflowing,
faces us today. Will we choose 'to be floor moppers
or tap turners off?
Overpowered, compromised and hypnotised
by ‘the products and high pressure slales tactics of
the multinational pharmaceutical industry, our sen
sitivities have been so dullened that we are quite
content to be merely ‘floor moppet®-’. Can we ever
be tap-turners off? The International movement of
physicians for prevention of Nuclear war is a thou
ght provoking example showing that if we
to, we can.
want
Bhopal too is a challenge? So are many other
more insidous developments in our country.
country The
growing investment in nuclear -dis
— energy now discredited as an energy resource in the West, or the
gradual take over of the cottage industry in food
by big business, — tfach of
this
though
though
different from
from . th©
the other has a growing similarity
representing either a subservience to the profit
u
motive or an insensitivity to health hazardsJ or
bullhetinW W^r6 fS°TC °f. theSe
in this
bulletin. We also feature investigations in Bhonal
which raise some of these issues for our readership,
distantS.eveso’ Long isIan<i were too'
andn w .®ake
™pact. Amlai, Chembtir, Handigodu, Hanhar Zuan, Nagda, Mavoor, Silent vally
Bhopal do To?
DOt StimuIated us ei*er. Will
medico friend
circle
I
bulletin
OCTOBER
1985
STRATEGIES FOR ENVIRONMENTAL
HEALTH ACTION
Dhruv-Mankad*
A)
INTRODUCTION
The term environmental health has a wide
scope, encompassing the relationship between health
and habitat, air, water, work place and so on.
Although the theme has been discussed since
long, the Bhopal tragedy has brought it into sharp
focus. Milder versions of Bhopal have been occuring
frequently but the actions taken have been in the
form of spontaneous protests by local people in the
’ affected area. Many times, investigative journa
lists- have brought such issues to light e. g. plight
° of villagers around the ACC cement factory at
Sevaliya in Gujarat or the Grasim episode. Later,
after some local action, interest has died down. It
is only after Bhopal that planned action at an all
India level is taking place.
There was a time when capitalistic indus
trial development encroached upon the lives of the
workers only — both at the workplace and in the
homes which were not very far away from the fac
tories. But the ever expanding, blind industrial
development process during the present phase of
capitalism,' has spread its tentacles over the
lives of all but the highly privileged few, both in
urban as well as rural areas. Thus Occupational
Health has been
subsumed by Environmental
Health and the effects of the nature of industrial
development on health is no longer a concern
of the workers only. Though, the analysis of the pro
blem and the solutions offered, would differ from
class to class. But, any such movement would cer
tainly pose certain basic questions regarding the
rate and the nature of present industrial growth.
B) STRATEGIES ADOPTED BY THE PEOPLE
People have always reacted spontaneously
against encroachments
by alien elements on
* A note for discussion at the MFC-annual Meet, Patiala 25-29
July 1985.
their ways*of life. A brief overview of strategies
used may help in formulating future strategies.
1) The working class, looked upon as merely
a tool in the production process, has always been
the first one to bear the brunt of the effects of a
new technology.
i) One of the most successful health movements
of workers was the Black Lung Movement of coal
miners of' the USA. Loy Rego, writing in The Socia
list Health Review 1:3 puts down the reasons for
its success as1—
a) the workers strength vis-a-vis the mine
owners, for coal is a key item.
b) public sympathy.
c) capacity of the workers to shut down mines.
All this was possible because of the mass
nature of the movement as reflected by the fact
that many folk Songs were written on the work
lines.
ii) Even when the position of the working
class was weak, partially successful actions
have
been initiated. For instance, a newspaper report
in a local daily in Gujarat regarding the plight of
workers in the slate-pencil industry, spurred a social
worker to file a writ petition in the Gujarat High
Court. The report filed by the Committee appoint
ed by the HC forced the State Labour Department
to make surprise checks which controlled some of
the problems of lime dust.
INSIDE
N.T.P — a dialogue
4
Banned Pesticides
6
News from Bhopal
7
From the Editors Desk
8
ill) Citizens of Ward 12 in Ratlam had moved
a local trial court to direct the Municipal Council
to construct proper drainage for the locality. The
State High Court affirmed the trial court’s order.
The Municipal Council approached the Supreme
Court, who turned down the plea and directed the
Council to carry out the work. In his judgement.
Justice V. R. Krishna Iyer observed that the citi
zens could “use the law and oall the bluff of the
municipal body’s bovine indifference to its basic
obligations.”
2) Growth of industries in the rural areas
under the guise of decentralization has meant a
direct threat to the rural people as well as to agri
culture. Farmers too, have successfully fought this
encroachment.
i) In Sevaliya in Gujarat, around 14,000 far
mers were affected by cement dust from the ACC
cement factory. After several years of memorandagiving and lobbying, they adopted a strategy of
no-tax campaign and gheraoed the management of
the factory. As a result, a precipitator was immedi
ately installed. The workers of the factory were
sympathetic to the farmer’s demands but were afr
aid that they would lose their jobs if they joined
the struggle and therefore kept out of it.
C)
1) Mass actions are almost always (Successful,
even when only partially. They also have the ad
vantage of the heightened environmental health
concern being passed down the generations and
across geographical areas as evinced by the Black
Lung Movement and the Chipko Movement.
ii) The famous case of the Chipko movement
of Garhwal is well known. The women of Chamoli
and other villagers in Garhwal, in a unique fashion,
protested against the senseless destruction of
forests by contractors by embracing the trees. In
lesser known incidents, women have adopted
novel ways to protest against cutting of. trees. In
1978, women of Bhuyander villages in the Chamoli
region, stole the .axes of men from nearby villages
who had come to cut the trees and refused to ret
urn them till they agreed to go back.
2) Actions against industries by the citizens
are more likely to succeed if the workers of the
industry concerned -as well as other allied indust
ries are directly involved. This is shown in the
case of Zuari Agro Chemicals. On the other hand,
workers are more likely to succeed in their struggle
tor better work environment if they acquire the
sympathetic participation of all the affected people
as is seen in the Black Lung Movement.
3) As pointed out earlier, the anarchic capita
list development of industries now threaten to dest
roy the lives of ordinary citizens mainly of those
living in and around cities.
Citizens too, have adopted various
to combat this menace:
ALL THESE INSTANCES SHOW CERTAIN
COMMON PATTERNS :
3) While dealing with Government bureaucracy
and Industry executives, mere rhetoric and agita
tion is not adequate. Sometimes information made
public wields power. For this it becomes important
that scientists are involved.
strategies
i) A Citizens Anti Pollution Committee was
formed in 1975 in Goa against the air and water
pollution by the Zuari Agro Chemical Industries.
It took out a morcha in protest, but to no avail.
Later, three political parties supported the Com
mittee and a threat was given by the All India Port
and Dock Workers’ Federation to boycott un
loading of raw materials for the Birla factories at
various ports. The company had to bow down and it
paid compensation to farmers and provided clean
drinking water facilities to the affected villages. A
water treatment plant Was also installed.
ii) At Mavoor in Kerala, Gwalior Rayon dis
charged effluents into the once clear Chaliyar
River, beginning from 1948. Fish died, skin infec
tions spread. In 1963 people protested but pro
mises given were forgotten. The protests persisted
during 1965, 1967, 1968, and 1973. Finally in
1978-79, Kerala Shastriya Sahitya Parishad brou
ght out a report which concluded that the problem
persisted because of the callousness of the factory
management to employ the available know how of
effluent treatment. In 1979, in a massive agitation,
people broke down a company erected bund to pro
tect its own water intake. Thus, it was forced to
lay a pipe line to dump the effluent in a far away
brackish water-stretch.
4) An educated population having the support of
scientific information might be able to carry out a
sustained struggle for better environment as is seen
in the case of Gwalior Rayon, Mavoor. In contrast
to this in another Birla owned factory at Amlai the
movement of local villagers only petered out after
the management gave some flimsy promises. In the
former case, the people admit that support of KSSP
was vital for the movement.
5) Women have a direct stake in the protection
of forests. They are more easily mobilised for such
actions than men, who sometimes are in favour of
contractors in order to protect their jobs. Chipko
and other movements in the Chamoli region point
to such a situation.
D)
STRATEGIES FOR ACTION
From the on going account,, it is clear that it is
possible to select one or more from several strate
gies used, to make Environmental Health Action
sustainable and successful.
1)
Information Gathering and Disseminating :
Done in a planned,
conscious
manner or
in an unplanned, unconscious and (experiential
manner, this is the first and vital step in the right
2
ii>
ND
f
either disinterested or actively against such move
ments for the fear of losing jobs, in case the indu
stry is forced to close down.
2) Lobbying etc : First, lobbying could also
serve the above purpose. The existing democratic
institutions should be utilised for this. Lobbying
among legislators and political parties is a useful
strategy for gaining support from ‘within’. Although
there is always the possibility of opportunist politics
entering the movement in this way, if one guards
against it consciously and if the decision making is
democratic enough, it could be combated.
In such a case, it is imperative on the part of
the aggrieved party to explain to the workers their
problems and also to include in their demands, the
demands of compensation and alternative employ
ment for the workers in case the industry is closed
down partially or wholly. This may ensure also the
involvement of workers.
3)
2‘) it is a common belief that lack of safety
measures, non-implementation of safety rules and
compensation laws in case of accidents or occupati
onal health hazards are highly prevalent in the un
organised industries. Under the guise of decentra
lization this sector has mushroomed during the
past few years.
Publicity and public opinion building :
Due to widespread experience of environ
mental piracy by various industries, people are be
coming sensitive to environmental issues as also
are the government bodies, bureaucracy and the
executive. Wide publicity In the existing media
newspapers and magazines has its impact. With the
tradition of public interest litigation picking up
in our judicial process, even newspaper reports are
now being converted into writ petitions by various
High Counts and the Supreme Court.
5
2> C v i >)
direction. It helps to make people concerned con
scious of the problem and breaks the ice for the
people to speak out.
But, given its nature, the workers have little
strength to fight it. They can do so only at the risk
of unemployment or even losing their lives. While
the stron er, more organised workers enjoy a better
work environment.
i)
4) Legal Action: Action can be initiated aga
inst environmental offenders under the Prevention
of Pollution Acts, Factories Acts and other Acts
governing the worker management relationships,
Municipalities Acts (as in the Ratlam case) and
finally as writ petitions in the State High Courts
Court
invoking
the
and
the
Supreme
and
the
Directive
Fundamental
Rights
Principles enshrined in our Constitution. Though
the efficacy of such actions is limited if nothing
else, they serve the purpose of highlighting the
issue. Tins strategy is particularly useful for citi
zen’s actions and the unorganised section of work
ers who have little strength vis-a-vis the industry
and the state.
First, one needs to examine this belief.
a) Mine workers would be considered as orga
nised workers. A survey of 11 coal mines totalling
9643 workers showed the prevalence rate of all cate
gories of
pneumoconiosis
as
10.8%.
A
survey of 7,653 underground miners with 5 or
more years of service in the Kolar Gold fields re
vealed the incidence of silicosis to be as high as
43 8%.
b) The accident rate in coal mines during 1977
was 0.47 fatal accidents and 4.33 seriously injured
persons per 1000 persons employed. Textile work
ers are also an organised section of the working
class. Injuries reported for 1978 in textile factories
were 54.32,% of total reported injuries in the
industries during the year. While it employs on an
average 26.62% of total number of workers emplo
yed.
5) Direct Actions: Whether the aggrieved are
workers, farmers or ordinary citizens, men or women; this form of protest works best if properly
organised and properly carried out. The success de
pends upon the strength and ability of the aggriev
ed to be able to hit the concerned at the place
where it hurts most. It could take the form of a
strike action in a key industry (as in the Black
Lung Movement), prevention of movement of key
raw materials and finished products (as in the
Gwalior Rayon Case), no tax campaigns (as in ACC
Sevaliya case), or simply creating a bad image of
the offending industry’s high selling product.
This shows that the quality of work environ
ment for the organised working class is also not
good. That for the unorganised working class would
certainly be deplorable
ii) Even then, it is true that unorganised work
ers have very low strength Vis-a-vis their manage
ments and the State. Therefore, they are unable to
initiate actions on their own. They need greater
outside support and help than does the organised
working class.
6) Certain prnblem areas :
While surveying
environmental ‘ill health’ and actions against it,
one comes up against certain tangles defying pat
solutions:
iii) Now, the question arises, as to whether in
the existing situation in India where the environ
mental health movement is in its infancy, it is bet
ter to support a stronger section where chances
of success are high or to take up the cause of those
1) It is commonly observed that if aggrieved
citizens
plan
action against an offending
industry, the workers and their Trade Unions are
(Contmoed on
3
page 8)
K
nc
0
JI
(Continued from page 3)
workers whose needs are greater but chances of total
' success are low.
The answer could be in affirmative to both in
part. It would be prudent to aim for total success
by supporting the organised and enlightened sec
tions of workers possessing some leverage. On the
other hand low key actions like publicity, lobbying
and legal actions would ensure partial successes
for the weaker unorganised section of the working
class.
F) ROLE OF GROUPS LIKE MFC : Being
what it is, MFC can be looked upon chiefly as a
resource group. It could provide technical help on
its own or by referring people to experts/resource
(centres known to it.
1) Carrying out Studies : Any movement strong
or weak, spontaneous or planned would need a
solid information base if it is to have a lasting im
pact. MFC could undertake studies in the field of
the impact of environmental degradation on health.
2) Publicising the issue : MFC members
could write m the popular press, in medical journals
etc. about environmental health issues thus publici
sing it and lending it credibility.
3) Direct medical intervention : As in Bhopal
under extraordinary circumstances in case of an
. environmental disaster, MFC could intervene
mtdu,allyx-by Provi#ng medical relief and long term
rehabhtation as a ’part of an ongoing people’s
movement.
*
*
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You ’may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection/ I, on behalf of DAF-KZ had a
discussion with the Community Health Cell team (CHC team)
in Bangalorez and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. Howeverz the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis andz therefore/ we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent to?
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1/ St Mark's Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your teamz
Yours sincerelyz
for DAF-Karnataka/
Gopal Dabade
To
135
medico friend
circle
bulletin
?fv)
DECEMBER 1987
Persistence of Toxins in the Bodies of Bhopal Gas Victims *
Anil Sadgopal & Sujit K Das
Soon after the gas leak, the Indian Council of
Medical Research (ICMR) announced that the gas
victims were afflicted with systemic and Persistent
cyanide poisoning and recommended detoxification of
symptomatic gas-exposed population by sodium
thiosulphate. The Govemment of Madhya Pradesh,
however, dragged its feet with icspect to this iecom
mendation. The State administration went to the
extent of stopping Dr. Nisi th Vohra of Jana Swasthya
Kendra from pursuing this therapy. In July 1985,
two gas victims and their physician Dr. Nisith
Vohra approached the Supreme Court claiming the
right of the gas victims for detoxification.
In the course of hearings, the Supreme Court
appointed a seven-member expert committee on
November 4, 1985 with the following terms of refer
ence :
(i) Carrying out fair distribution of sodium
thiosulphate;
(ii) Carrying out proper epidemiological survey
and also house to house survey of the gas
aflected victims for the purpose of determining
the compensation payable to the gas affected
victims and their families; draw up a scheme
for carrying out survey;
(iii) Ensuring proper medical facilities to the gas
affected victims; give directions from time
to time for carrying out survey and providing
medical relief;
(iv) Draw up a scheme for provision of medical
relief and for monitoring the implementation
of the scheme for medical relief;
(v) Give direction to produce the results of the
surveys which have already been done.
The Committee, in its last held meeting on Decem
ber 13-14, 1986 decided to submit two separate in
terim reports to the Supreme Court—one by the
majority constituted by five official members, and
the other by the two undersigned non-official mem
bers constituting the minority. Besides its lackadai
sical functioning, the Committee could take up work
only on the first term of reference, i.e. carrying
out fair distribution of sodium thiosulphate. Ig
noring the proposal submitted by the Minority
Members, the Majority Members decided not to lake
up the remaining tasks specified in the Supreme
Court order.
Even on the issue of sodium thiosulphate therapy,
the Majority Members declined to pursue oi analyse
all relevant scientific data. As a consequence of this
enigmatic attitude towards the work of the Supreme
Court Committee, the Majority Interim Report only
perfunctorily went through the motions of recom
mending sodium thiosulphate therapy to unidentified
subjects and failed to come to grips with the central
questions viz. persistence of toxins, role of antidotal
therapy and magnitude of the task. We, therefore,
undertook it upon ourselves to collect and analyse
*Excerpts from a preliminary report submitted to the Supreme Court on October 26, 1987 by the minority group.
all available scientific information in order to fulfil
the task entrusted by the Supreme Court.
(f) detection of carbamylated haemoglobin (hae
moglobin linked with MIC) in the blood of
gas victims;
Our Minority Interim Report is almost ready and
will be submitted in about a month’s time. Despite
refusal by various official research bodies and indivi
dual scientists engaged in research on Bhopal victims
to provide us with essential information, we have
been able to collect significant evidence pointing
towards systemic and continuing presence of toxins
in the bodies of the gas victims. Yet we were frust
rated all along this work because the data on this
issue as presented before the Committee as well as
those released in ICMR publications could not
stand the test of objective scrutiny in scientific forums.
It is in this light that the evidence obtained by us in
August 1987 and analysed during the past few weeks,
assumes special significance.
(g) finding
of cherry-red colour of venous
blood in the autopsy studies;
(h) evidence for the presence of anti-MIC anti
body in blood samples drawn from gas
victims;
0)
observation of disturbance in several immune
parameters and adverse impact on the responsiveness of lymphocytes; and
(j)
evidence of MlC’s ability to cross air-blood
barrier in animal studies conducted by
DRDE, Gwalioi.
All the above-mentioned pointers towards syste
mic and persistent poisoning of gas victims have
been discussed in detail in the Minority Interim
Report to be submitted later to the Supreme Court.
What is of special concern presently is the pointers
relating to elevated levels of urine thiocyanate and
the ameliorative role of sodium thiosulphate. The
early reports of increased excretion of thiocyanate
in the urine of gas victims led ICMR to conclude
that the gas victims could be suffering from toxic
effects of persistent cyanide poisoning. This inference
was based on the well-known cellular reaction for
transforming cyanide into thiocyanate in the presence
of an enzyme called rhodanase. Under normal
conditions, the cyanide radicals, entering human body
through certain foodstuffs or through consumption of
tobacco, get converted into thiocyanate as a result
of donation of sulphur by intrinsically present sul
phur-containing compounds, constituting the ‘sulphane pool’. In the case of acute cyanide poisoning,
the victim dies unless a large extraneous source of
sulphur is quickly made available. The antidotal
role of sodium thiosulphate has its basis in this simple
biochemical mechanism. Since there was no known
record in medical literature of chronic persistence
of cyanide after single exposure, the ICMR found it
necessary to invoke the concept of an ‘enlarged cy
anogen pool’ in the bodies of the gas victims, which
would become a continuing source of cyanide-like
compounds through the chronic phase.
The Medical Context
At quite an early stage, the Indian investigators
detected significant pointers towards the possibility
of systemic and persistent toxicity of the poisonous
emission, These pointers are briefly enumerated
below :
(a) presence of multisystemic ailments in a
significant percentage of victims and a high
frequency of symptoms relating to nonrespiratory systems in patients not reporting
respiratory complaints, as revealed by Medico
Friend Circle’s epdiemological sutdy;
(b) presence of a large percentage of patients
who suffered from respiratory symptoms but
were free from any evidence of organic
damage to lungs, as reported by ICMR;
(c) evidence of significantly increased rate of
spontaneous abortion among women who
conceived upto 10 months after the toxic
exposure, compared to the rate prevailing
before the exposure, as reported in Medico
Friend Circle’s Pregnancy Outcome study;
(d) early reports of the presence of two to three
fold higher levels of thiocyanate in the urine
of gas victims than the levels found in un
exposed subjects;
Scientific Evidence
(e) observation of symptomatic relief and further
elevation of urine thiocyanate levels on ad
ministration of sodium thiosulphate injec
tion, even several months after the toxic
exposure;
What is being presented here is a part of an ICMRfunded research project (No. 5/7/28E/84-RB) dealing
with analysis of urine thiocyanate levels in child
(0-15 yrs.) and adult (15 yrs. and above) population
2
NC I
11
4
samples collected' from control and gas-exposed
areas of Bhopal. The study, led by Dr. M.G. Karmarkar of the Department of Endocrinology and
Metabolism, All India Institute of Medical Sciences,
New Delhi, was undertaken with the objective of
finding out “whether thyroid function is affected in
population which was exposed to MIC’. The urine
thiocyanate level was determined in this study in view
of the well-known antithyroid property of this chemi
cal and in the wake of reports from Bhopal that
the gas victims were excreting two to three-fold
higher levels of this chemical compared to the sub
jects from Delhi. These investigations were conducted
in two distinct phases.
, f)(. c -e vx-Ux-v
i T'
selected from both the control and exposed areas of
Bhopal, that were coded by ICMR. The sampling
was conducted according to a randomised block
design prepared by ICMR’s Senior Statistical Officer
associated with the Bhopal Gas Disaster Research
Centre at Bhopal. The size of each sample was
found to be adequate for applying statistical tests of
significance for assessing the validity of observed
differences, if any, in urine thiocyanate levels of the
ssamples being compared. It may be worthwhile to
note here that the control areas coded by ICMR
may not be taken as equivalent of unexposed areas
since Medico Friend Circle’s epidemiological study in
March, 1985 showed that Anna Nagar, one of ICMR’s
‘control’ areas and also included in the present
AIIM Sstudy, was actually a mildly exposed colony,
though il was 8 kilometeis from the Union Carbide
plant.
In the first phase, from July to November 1985,
urine samples from 326 gas-exposed women admitted
in Sultania Zenana Hospital in Bhopal for delivery,
were analysed for thiocyanate levels. An estimate
of the ‘normal range’ (baseline) of urine thiocyanate
levels was obtained by studying a group of 35 Delhi
residents from six different socio-economic categories
in order to have a representative sample. Care was
taken to ensure that the sample was composed of
roughly equal number of individuals with respect
to sex and age groups (i.e. children and adults).
The report presented to ICMR in December, 1985
reveals that the control sample from Delhi had a
sample mean value of 0.399 mg% of urine thiocyanate
with a standard deviation of 0.06. Compared to
this mean value of the control sample, the group of
326 ‘exposed mothers’ had a sample mean value of
0.45 mg%, with a standard deviation of 0.27. It was
found that 88 individuals out of 326 ‘exposed mothers’,
i.e. about 27% of the sample, had urine thiocyanate
levels which were above ‘mean plus 2 standard de
viation units' of the control sample, a fact reported
to an ICMR Project Advisory Committee meeting
held on May 1, 1986. This implied that a significant
percentage of women in the sample were excreting a
noticeably high level of thiocyanate in urine. The
investigators further noted that 40 out of these 88
women had urine thiocyanate values in the ‘smokers
range’ (i.e. 0.55-0.70 mg%)*. It may, therefore, be
concluded that about 14.7% of women in this sample
could be unambiguously categorised as ‘high
excretors’ of urine thiocyanate.
An important feature of this study was a follow
up 6 months later in March, 1987, of the samples ini
tially investigated in September, 1986. It is reported
that the follow-up study investigated the change in
urine thiocyanate output of exactly the same indivi
duals who constituted the original sample.
Table I compares the mean urine thiccyanale
levels of children and adults from control and .ex
posed areas in both September, 1986 and March,
1987. These data were subjected to a detailed sta
tistical analysis by applying the Test Statistic, standard
normal deviate, foi testing the statistical significance
of observed differences.** This exercise revealed that
the differences observed in the mean urine thiocyanate
values of exposed and conti ol samples are statistically
significant, and not due to chance fluctuations. In
other words, it means that the toxic exposure is most
likely responsible for an increase in the excretion of
thiocyanate in the uiine of gas victims on a population
basis. It is fuither evident that the raised levels of
urine th'ocyanate persisted in the gas-exposed
population until at least March, 1987.
The data shows that the gas-exposed samples,
irrespective of the age group and time of
testing, have a larger proportion of high-excretors
than the control samples. These ob^eived differ
ences in the proportions of high-excretois of ui ine
thiocyanate in various samples were subjected to a
rigorous statistical analysis. It turns out that the
above-mentioned differences between various exposed
In the second phase of this study, conducted in
collaboration with the Department of Medical Bio
chemistry, Gandhi Medical College (Bhopal), popu
lation-based samples of children and adults were
♦Consumption of tobacco, whether through chewing or smoking, is reported to approximately double the output of urine
thiocyanate.
♦♦The statistical analysis, referred to in Table I, was conducted by Shri Subhash Ganguly, a professional statistician and
an activist of Calcutta’s Scientific Workers Forum, at the request of the authors of this report.
3
and control samples being compared are statistically
significant, implying thereby that the toxic exposure
could reasonably be taken as the cause of the observ
ed increase in the proportion of high excretors of
thiocyanate.
Analysis and Interference
The results presented above have established
beyond doubt that exposure to toxic emission from
the Union Carbide plant led to an increase in excre
tion of urine thiocyanate in gas victims and this in
crease persisted until at least March, 1987, if not
even later. This indicates the possibility of a sys
temic and continuing presence of certain toxic chemi
cals in the bodies of the gas victims, which are bio
chemically transformed into thiocyanate. This find
ing obviously cannot be attributed to earlier reports
of a rise in thiocyanate content of the water of Bhopal
lakes because (a) the increased rise was temporary
and the elevated levels returned to normal by August,
1985, and (b) intake of thiocyanate from water would
have equally affected populations amples from control
and exposed areas.
1987 in both children and adults alike (see Table 1).
However, the statistical significance of this obser
vation cannot be ascertained on the basis of compari
son of mean values alone. For this, it would be neces
sary to compare individual thiocyanate values at both
points of time, which unfortunately was not possible
because the original data, lying in possession of the
Head, Department of Medical Biochemistry, Gandhi
Medical College, Bhopal, were not accessible to us.
The importance of stdying the declining trend may
not be overemphasized, since it is only through its
detailed analysis that meaningful predictions can be
made about the duration for which the toxis would
persist. This information is required for making a
reliable assessment of the current and future toxicolo
gical risks faced by the gas victims. Clearly, no de
toxification programme can be planned wihout such
an assessment.
An assessment of the current toxicological status
of the gas victims would have been possible even with
out statistical analysis of the declining trend suggested
above, had the direct monitoring of urine thiocyanate
levies been continued beyond March, 1987. This,
however, did not happen since ICMR, for inexplicable
reasons, could not see the significance of the findings
by the AIIMS team and decided to terminate the
project. It is peculiar that ICMR has not even
thought it fit to list this research project in its list of
studies on Bhopal, published in ICMR research
update of December, 1985. The ICMR research
update of December, 1986 makes a mere four-line
reference to this study, without even mentioning its
findings concerning urine thiocyanate levels.
Elevated urine thiocyanate levels do not necessarily
imply cyanide poisoning alone, as has been assumed
so far because of the well-known enzyme-catalysed
transformation of cyanide into thiocyanate. The
Minority Interim Report to be submitted later, would
present evidence pointing towards the possiblity of
MIC itself being the cause of systemic and persistent
toxicity in gas victims. Attention has been drawn to
animal studies conducted by DRDE (Gwalior)
showing that sodium thiosulphate may have anti
dotal role in animals exposed to pure MIC. In
The above-mentioned decision of ICMR to termi
light of this, it would be pertinent to explore hitherto nate the project is baffling, to say the least. This
unknown biochemical basis of persistence of MIC or study, when compared to the pioneering and much
its metabolites and pathways for their removal (ie. bigger study conducted by the Medico-Legal Institute,
detoxification) from human body. In this context, Bhopal, is distinguished by its scientific appioach
antidotes other than sodium thiosulphate may also which involved the following features :—
need to be investigated.
(i) use of a more reliable and specific method of
estimation of urine thiocyanate,
The systemic and continuing presence of toxins,
be they cyanide or MIC or any other chemical, in the
(ii) use of a statistically valid method of sampling
bodies of the gas victims points towards the possible
population; in contrast, the Medico-Legal
long-term risks to themselves and to their progeny, as
Institute’s study had investigated only hospi
indicated earlier. This clearly calls for much larger
tal-bound patients, that too without taking
allocations for medical relief, rehabilitation, surveys,
a
random sample, and thus it has never been
monitoring and research, covering the entire gas-exable
to present a representative picture of the
posed population for much longer duration than what
toxicological
status of Bhopal’s gas-exposed
have been so far anticipated on the basis of informa
population.
tion furnished by Union Carbide.
(iii) use of comparable controls whose only limita
Tfyere is a visible declining trend in the urine
tion was due to ambiguity in ICMR’s coding
thiocyanate levels from September 1986 to March
of areas with respect to degree of exposure.
4
M P-C
I U Pn
wt 1^ v
NV>
(iv) taking into account the effect of tobacco
(v) doing a follow-up analyisis six months later
on the same individuals, which makes it the
consumption on the output of urine thiocya
only
study on Bhopal victims known to us
nate by (a) random sampling which ensured
that has yielded information on the trend of
that probability of including or excluding a
toxicological status as a function of time.
tobacco-consumer in the selected sample was
equal for both control and exposed areas,
Another distinguishing characteristic of the AIIMS
and (b) including a sample of children in team of investigators engaged in this study has been
the study who for all practical purposes can its willingness to share and subject its data to open
be considered as non-consumers of tobacco, scientific scrutiny.
Table I
MEAN URINE THIOCYANATE LEVELS OF CONTROL AND GAS-EXPOSED POPULATION
SAMPLES FROM BHOPAL*
Age Group
Children
Time of
Testing
Status of
Exposure
Sept. 1986
Exposed
67
0.52±0.145
Control
113
0.41 ±0.109
Exposed
67
0.44 ±0.134
Control
113
0.37±0.105
Exposed
83
0.54±0.159
Control
111
0.41 ±0.135
Exposed
83
0.48 ±0.154
Control
112
0.37±0.113
(0-15 yrs.)
March 1987
Adults.
Sept. 1986
(15 yrs & above)
March 1987
Size of
Sample*
Mean
Urine Thiocyanate
level
(in mg %)
Whether Mean (ex
posed) turns out to
be significantly grea
ter than Mean (Con
trol) on the basis of
statistical test ?**
Yes
Yes
Yes
Yes
* Basic data taken from the report of ICMR Research Project No. 5/7/28E/84-RB (see Annexure 6).
* Indicates the number of individuals tested in each sample. The sampling was done on the basis of a ran
domised block design from gas-exposed and control areas as coded by ICMR. The size of each sample
was determined on the basis of statistical principles and found to be adequate for applying statistical tests
significance.
** The Test Statistic, standard normal deviate, was used for testing the statistical significance of observed
differences in the mean urine thiocyanate levels (see Annexure 8 for details). The statistical analysis was
conducted by Shri Subhash Ganguly, a stastician and an activist of Calcutta’s Scientific Workers Forum,
at the request of the authors of this report.
5
medico friend
125 circle
bulletin
2i>)
FEBRUARY 1987
Confusion—A Way to Knowledge
U.N. Jajoo
The Annual MFC meet at Bangalore on tuberculo ed, previously untreated residents of Bangalore City,
sis (1985) has provoked much critical thinking to the judged as active by two miniature X-ray film readers.
extent that a consensus on the ertique of NTP is yet Half of these were randomly allocated to treatment
to emeige. Anant and Binayak tried to prepare a regimen of INH and TCZ and the other half were on
note which Anil Patel found uncompromising. I add placebo. 31% of those who were initially sputum
to the confusion here by placing some facts and figures negative by one smear examination were found to be
with the hope that it will pave the way to knowledge. sputum positive on second examination. 10.7% by
smear and 20.8 % by culture alone. Even those
Question I: What is the fate of radiologically posi patients who were not read as active by any of the
tive and sputum AFB negative patients, two readers, 2.8% proved to be sputum positive on
if untreated?
second examination. A few more became sputum
positive or showed radiological progress of the disease
Let me quote an editorial from the Indian Journal
during the course of follow-up with no treatment.
of Tuberculosis (1). “For many years there has been
Thus about 40% out of initially sputum negative
an increasing awareness of a need to study the fate
continued to be sputum negative, while 60% of them
of sputum negative patients who seek treatment at
proved definitely to be active tuberculous at some
various centres for symptoms suggestive of chest
stage or the other, more often within first four months
diseases. Some workers have recommended that
following detection. Among sputum negative treated
such patients should be kept under observation while
group, regression of lesions was more frequent than
many clinicians prefer to put them on prolonged
in the untreated.
intensive anti TB drug therapy. In July 1974, this
problem was discussed in the pages of this journal.
In rural areas where follow-up for observation is
The National Conference at Hyderabad in 1975 de
not easily possible and is hardly ever done, patients with
voted a full session to this important problem. A
highly suspicious X-ray shadows should be offered
study based on a long term follow-up by the New
anti TB drug therapy if clinical picture is also sugges
Delhi TB Centre showed most of such patient to be
tive since tuberculosis continues to be the most co
definitely active and tuberculous.
mmon pathology. Mistakes in diagnosis though few,
will
continue to occur even in the best of hands, the
A study carried out in Hong Kong recently with
question
is which is less risky and likely to be more
the collaboration of the British Medical Research
profitable
generally—to treat or not to treat.”
Council has shown that 34% of the patients whose five
sputum specimens were negative by direct smear be
The conclusions drawn are;
came sputum positive during the course of one year
when left untreated.
—The radiological reading of active tuberculosis in
suspect cases must be considered fairly sensitive
A controlled study of such patients was undertaken
recently by the National TB Institute, Bangalore also.
(more/than 2/3 at least) and if coupled with clinical
judgement should be regarded as reliable tool.
The patients included in this study were freshly detect-
3
6. What do you expect will emerge from such a Workshop?
7. Any other relevant/related issues?
Please fill in this form and return it to
The Co-ordinator
Drug Workshop
Community Health Cell
47/1 St Mark’s Road
Bangalore 560 001
by 5th February 1989.
Hr,
ar,
—The epidemiological surveys done till date are based
on the evidence of ‘active pulmonary TB lesion'
in X-ray, and therefore stand as fairly reliable
evidence of quantum of pulmonary tuberculosis in
the community.
NTP banks on those patients who themselves re
port to medical opinion for relief of sufferings and
presupposes that all who take action will come to these
centres for their expertise. The erdibility ‘enjoyed’ by
these centres is obvious from the fact that, “out of
those registered at the DTC, only 27% have not rece
ived treatment earlier” (7). It is not only the dis
tance of the diagnostic centre but the behaviour, the
care, the concern shown towards human sufferings
that attracts the poor ill person, the absence of which
is obvious from the figure that only 23% seek relief
from the nearest health centre. The inefficiency of
case detection, the non-availability of drugs/detectors
erode the credibility of these peripheral units. It is
this faith in the healer that matters for the patient and
not merely a free technical expertise. At the time
NTP was conceptualised this important sociological
dimension of patient care was forgotten.
—In a clinic situation (PHC or DTC), it is fairly logi
cal to treat suspect cases i.e., radiologically positive
but smear negative.
Under NTP, a person with tuberculosis who mat
ters is one who brings out AFB in sputum smear.
The efficacy of case detection by microscopy in the
present situation is as follows: (2,3)
—Total number of sputum positive cases in average
district (infectious cases only)
= 5,000
—Potential of case detection by meti
culous sputum examination (passive
case detection in clinic setting)
= 2,000 (40%)
Question 2:
—Number of cases detected in actual
field situations
=776*
Let us not confuse between active case finding and
passive case detection in a clinic situation. The above
statement is true only for active case finding. To
quote verbatim, “For sputum positive cases, large
majority of patients could not be found even if ser
vices were provided close to their villages. The
number of patients found under such conditions was
considerably short of estimated total prevalence. It
was not possible to diagnose even about 50% of the
existing cases in the community i.e. number that was
already reporting to the PHC for examination because
of their chest symptoms by any of the currently avai
lable methods (community development approach—
active detection of symptomatics and referral to micro
scopy centres or mass campaign with X-ray available
at few miles distance) (9).
Thus, those who do not bring out AFB in sputum
smear (thanks to our inefficiency), are very graciously
shown the way to DTC for MMR which in practice is
out of the reach of the majority. It has been found that
only 20% report to DTC (4) and much less turn up to
collect the report, since patients are not prepared to
travel more than 5 kms (5) unless symptoms are very
pressing. The wage loss implicit in such action is
never taken care of. In reality what it boils down to
is, if you have faith enough to take pains to reach the
peripheral microscopy centre, and bring out AFB in
smear detectable by our microscopists, only then you
matter us enough for inclusion under NTP. We
(the NTP) full of sympathy for your sufferings, will
send you back with tonics and cough mixtures and will
consider it your fault if you fail to turn up again for
unrelenting symptoms. NTP merely looks at the
impact of the strategy on the prevalence of TB and
forgets the agony of the sufferers.
Flowever a situation in an accessible clinic where
static MMR facility is available will be entirely diff
erent. The purpose of installing an MMR machine
in these peripheral clinics is not to mop up the ‘non
action’ taking cases of the community but to detect
precisely the action taking group (52% smear posi
tive). The moot question is whether we expect bonus
of this radiological support or not. It is a known
fact that 70% of the registered cases every year are
AFB negative (radiologically diagnosed) in DTC.
This is a clear indication that the concept of case
detection by microscopy has not even been conceived
by the district centre and that radiological support
The reliance of microscopic examination alone for
the diagnosis of TB must be weighed against the foll
owing considerations, (i) microscopic detection of
AFB is a tool which requires- sincerity of human ele
ment involved—something which cannot be legislated
in our setting, (ii) There is a phenomena of ‘intermit
tent positivity’ (6) which further reduces the reliability
of one sputum examination, a general practice in
PHCs.
♦
Isn’t it true that Indian and WHO
documents say that MMR does not help
in detecting more cases than is possible
by microscopy alone ?
20 to 30% of expected potential or 15% of the total infectious pool.
2
3
6. What do you expect will emerge from such a Workshop?
7. Any other relevant/related issues?
Please fill in this form and return it to
The Co-ordinator
Drug Workshop
Community Health Cell
47/1 St Mark’s Road
Bangalore 560 001
by 5th February 1989.
I
has considerable potential of dividends to be paid in
our existing inefficency.
Question 3:
The radiological facility at PHC (accessi
ble clinic) is a costly proposition and
should its appropriateness not be judg
ed before it is pleaded for?
The logic that recurring cost of MMR static unit
will be too much is negated by the following observa
tions: (10)
The radiological facility at the PHC has an added
spin-off benefit in the early diagnosis of bronchopneu
monia in children—the number one killer in under
fives. While limitations of financial stringency to
wards non-recurring cost is put, at least principally a
need of radiological back-up support must be accepted
and its feasability must be tested in field situations.
I suggest the strategy given below.
Question 4:
Can culture facility at PHC add signifi
cantly to case detection at PHC?
The cost in US$ of diagnosing one case by different
methods
Not much really, clue to the following reasons—
Approximate
cost per exa
mination
Approximate
cost of diagno
sing a case
Direct microscopy
0.21
3.4
(i) Out of 20 cases/1000 population, 2.5/1000 are
smear positive and 1.6/1000 are only culture positive.
Tn passive case detection at PHC where around 52%
of infectious pool is expected to turn up, the bonus of
‘only culture positive’ will be reduced further.
Culture exam
70 mm x-ray
film (static unit)
passive detection
0.49
12.1
0.26
3.5
(ii) -Culture report takes-at least 6 weeks—a time
lag which will shift the ailing patient elsewhere in pur
suit of relief.
73.0
(iii) The cost involved in detecting a case is 4 times
higher than that by smear examination or static MMR
(10).
Examination
70mm x-ray film
(mobile unit) ac
tive detection)
0.50
Symptomatic patient
| one sputum smear
I
AFB positive
AFB negative
confirm by MMR
and treat
subject to MMR
normal
non tubercular
I
tubercular
repeat AFB
I
I
negative
positive, treat
I
put on broad spectrum
antibiotics for 10 days
repeat MMR after 3 weeks
along with smear exam.
Radiological
resolution
Not resolved
or increased
or AFB positive
Treat for TB
3
r
3
6. What do you expect will emerge from such a Workshop?
7. Any other relevant/related issues?
Please fill in this form and return it to
The Co-ordinator
Drug Workshop
Community Health Cell
47/1 St Mark’s Road
Bangalore 560 001
by 5th February 1989.
1
A/
>V0 /AT
Question 5:
Can tuberculosis prevalence be brought
down by medical intervention? Should i
the aim of NTP be only alleviation of
human suffering?
Socio-economic factors being important in causa
tion of tuberculosis, we are tempted to argue that any
amount of medical intervention alone cannot reduce ;
the prevalence of tuberculosis. However, the figures
drawn up after careful analysis do not favour this
hypothesis. If the full potential of microscopic detec
tion is tapped and all geographical area is covered by
NTP, estimated probable reduction in prevalence of
TB is 6.4% per year. With the present case detection
rate (30% of the expected), 4.8% reduction can still be
achieved (3). NTP is epidemiologically a sound
proposition but has failed to make a dent due to opera
tional failure in case detection/case holding.
References:
i
i
I
4
1. Editorial ‘Sputum negative patients’, Indian Jour
nal of tuberculosis: 26,173, Oct 1979.
2. ‘Potential yield of pulmonary tuberculosis cases by !
direct microscopy of sputum in a district of South !
India’, GVJ RBaily etal, Bull. Wld. IJlfh. Org :
1967, 37, 875-892.
j
3. ‘Tuberculosis in India-A perspective’, D.R. Nag
paul, J. of Ind. Med. Assn: 71,44-48, 1978.
4. ‘District TB Control Programme in concept and i
outline’, D.R. Nagpaul: Ind. J. of Tub. XIV, i
196-198.
5. ‘Prevalence of symptoms in a South Indian rural
Community and utilization of area health centre’,
Ind. J. Med. Res.: 1977, 66, 635.
6. Some aspects ot sputum examination in tubercu
losis case finding’, D.R. Nagpaul, et al, Ind. J.
of Tub.: 26, 11, 1979.
?
7. Socio-Cultural Context of TB treatment’, Ind J ■
Tub.: 1982.
8. ‘Symptom awareness and action taking of person !
with pulmonary TB in rural community surveyed
repeatedly to determine epidemiology of the
disease, Radha Narayan & H. Shrikantaram;
Ind. J. of Tub.: 28, 1261, 1981.
9. An operational study of alternative methods of
case finding for tuberculosis control, National
Institute of Tuberculosis, Bangalore, Ind. J. of
Tub.: XXVI, 26, 1979;
10. A Case finding by microscopy’, D.R. Nagpaul,
et al, WHO/TBITech. information: 68, 63.
3
6. What do you expect will emerge from such a Workshop?
7. Any other relevant/related issues?
Please fill in this form and return it to
The Co-ordinator
Drug Workshop
Community Health Cell
47/1 St Mark’s Road
Bangalore 560 001
by Sth February 1989.
? (v'9
medico friend
145 circle
bulletin
November 1988
The Trans-Technique Aspects of Disease and Death
M. L. KOTHARI AND LOPA A. MEHTA
f
!
The technological triumphs of this century
outweigh and outclass the aggregate achievements
of the entire human past; yet modern man has been
denied the elixir of cure for his disease and death.
A logical survey of medicine's failures reveals that
it is not that the technology per se is ineffective but
that what technology has solved is trivial, and what
it just can't touch is crucial, being beyond any techniqe. Most of human disease and death is trans
technique. Technique in medicine is whatever a diag
nostician, therapist or researcher does to a patient.
Trans-technique aspects of disease and death are
those innate, ordinary, day-to-day features of human
living and dying that le technique can in no way
modify to a patient's advantage.
Seemingly, technology has reached its apo
gee, its Ultima Thule; the march is unimpeded, for
the would-be-obsolete CT scan is likely to be repla
ced by the could-be-obsolete NMR imaging. How
ever, a dispassionate, epistemologic evaluation of
medicine's gains reveals them to be imagery, accessive3 analytic associatiue, and amplificatory. The more
the physicistic science and the physicianly art inter
act, the greater is the variety in which medical
imagery can be obtained. Yet, to take but an exa
mple. roentgenography, xerography, CT scan, ultra
sonography and NMR imaging have left a cancer
where it was—diagnosed always a little too late.
The ability to cannulate the pancreatic duct/artery
towards the diagnosis/treatment
of pancreatic
cancer is an access-ive advance that leaves the can
cer's autonomy untouched. Increasingly refined
biochemical techniques allow many a substance to
be measured with pico- precision, thus analytically
telling us a lot about heart attack diabetes mellitus
or rheumatoid arthritis, but without the liberty to
predictably/and/or favourable alter the course of
the disease. Epidemiology connects the husband's
cigar to the wife's cancer, coffee to cardiovascular
disease, and HLA-antigen to a host of maladies
—an associative exercise that makes more anxiety
than sense. The E/M amplifies the size of a T-lym
phocyte n-tuple times only to amplify our ignorance
on the cell to the same magnitude. In the modern
medical setting, technology glitters, but is, often
not gold.
A quartet of diverse medical men, (10,17,
19, 27) in its recent generalization, is not far from
the truth that 90% of the bad things that happen to
man are beyond the ken of modern medicine.
Armed with technical might, the doctor can, with
vis medicatrix naturae providentially at the patient's
beck and call, revert to ew-states acute physio
logic crises, set fractures, fix retinae, deliver babies
facing dystocia, remove lumps and cataracts,
replace a valve or a joint, correct mechanical
defects such as cleft lip or hernia, all this com
prising the 10 per cent of man's maladies that
medicine can manage, The rest is trans-technique.
Let us see how, and why.
Four biomedical factors account for the
trans-technique scenario that we are witnessing.
These are Cellularity, Systemicity, Uniqueness and Herdity. An integrated appreciation of these factors
will help us understand medicine's limits, no
matter what its technical might.
Cellularity : Celldom Unconquered
There are features of a mammalian cell that
make disease and death trans-technique in more
ways than one. It is a fitting paradox that what
advanced cytologic techniques have revealed ab
out the cell has snowballed to drive home the
truth that a cell's behavior, in health or disease,
can hardly be trifled with.
The microsize of a cell accounts for the
fact that before a scan discovers a cancerous
lump measuring one cubic mm and weighing one
mg.,—the smallest tumor mass that one could
ever hope to detect clinically—the cancer is al
ready a million cells strong and several years
old; early diagnosis of cancer is only a myth.
(13) The same considerations apply to an athero
matous plaque, held by some as mitotic in ori
gin. 21 Even if we end up with a scanner that
can spot a single wayward cell, the latter could
mislead by exhibiting the Shakespearean repertoire
of looking benign despite malignant intentions
and vice versa. Any attempt at flooding the body
with antiabnormal-cell-agents (radiation, chemicals)
fails because of the selfsameness of all body
cells, rendering selective destruction of undesired
cells impossible, Supposing that a highly speci
fic drug is developed and administered, the target
cell can recall its microbial past to readjust its
genetic machinery—mutate—to KO the drug, the
mutative repertoire of a human cell bordering
close to 256 followed by 2.4 billion zeros. Tra
nsplanted, the guest cells refuse to merge their
identity, their unique self-ishness as much as
the host cells, and all hell is let loose. Each of
our body cells carries in its bosom a decision in
advance of performance. (6) The thousand inner sho
cks that the flesh is heir to are indelibly pro
grammed into it ab initio; all that we see is an
unfolding of a built-in story with the flow of time.
Systemicity
2
The human body is a holon that starts as
a single cell, and sui generis, builds up a cytogalaxy that behaves as a single, concerted unit
whose seemingly disparate parts form, grow, and
decay in unison.
Acknowledgedly, cancer is a disease of the
whole organismm.{22) In the brain, where-from can
cers usually do not spread, it is a disease of
the whole brain. A cancer thus does not lend
itself to complete destruction by surgery, radia
tion, chemotherapy or immunotherapy. Even if
we were to nab the last cancer cell, (26) the next
normal cell would foil the attempts by turning
cancerous, through a process named neocanceration or recruitment. (13) The sole curative triumph
against gestational choriocarcinoma is due enti
rely to the fact that such an eventua.ity of neocanceration is ruled out by the absence of the
normal progenitor cells that comprise the dis
carded fetal part of the placenta. The appellation,
a disease of the whole organism, is no less appli
cable to any form of blood vessel disease, be
it the coronaries or the cerebrals. A bypass ta
kes care of the block that the operator seess
or has access to, but what of the vessels be
yond, or before, or elsewhere. This explains why
a patient of angina shows normal coronary arte
riogram and the patient having normal coronary
arteriogram can die a sudden coronary death. (25)
As for diabetes, euglycemic agents touch the
proverbial tip of the metabolic iceberg, affecting
in no way the generalized, accelerated vaso
occlusion that is now an accepted part of the
diabetic process.
Uniqueness
Variability, it's said, is the only invariable
law of biology, a natural propensity that unfai
lingly varies one cancer from another, one heart
attack from the next. If the uniqueness of every
individual is an unsolved problem of biology, (20)
than uniqueness of every disease is the unsolved/
unsolvable problem of medicine: "There are," Ca
rrel axiomatized "as many different diseases as
patients." (2) The presumed identicality of the geno
type in homozygous twins is unable to circum
vent the Carrelian code, a nosologic non-concordance that is well-known but as yet poorly
accounted for.
*
Cancer, indisputably traceable to precisely
pinpointable/culturable culprit cancer cells, provi
des a remarkable example of what Dubos (5) would
call the unprecedented, unparalleled, and unrepea
table nature of a disease. Writing / on the 'Uni-
quenes of malignant tumours/ Spriggs and co
workers (25) concluded that naturally occurring ca
ncers are extremely diverse even when they carry
the same diagnostic label. No two cases of co
ronary artery disease/stroke/diabetes/arthritis/auto
immune disease are identical either in their pre
sentation or in their progress. The behavioral
uniqueness of a disease, with its unpredictability,
forms the basis of unexpected successes and the
equally unexpected failures, given the same treat,
ment. Cancers have been classified into good and
bad, the good ones curable by any treatment, the
bad ones by none—a retroactive judgment (13)
applicable to any other disease and fully justi
fying the Chinese proverb that a therapy works
in a patient destined to survive.
Vis-a-vis the celebrated and honored ppractice of prognosing, what the doctors know
■J are
group statistics but when it comes to a disease
in an individual, the physician has to contend
with unknowns stacked upon unknowns, a si
tuation that merits the title of a book by Fran
cisco Sanchez, published in 1581 : Quod Nihit
Scitur Nothing Can Be Known. In a recent study
in Bombay, of 535 sudden coronary deaths, 66%
of the cases did not show coronary occlusion
and 78% failed to show any myocardial infarct,
in many of these, the heart was too good to'
die. (23) And what of diabetes with the SMA-12
at the behest of the clinician I It is true in dia
betes mellitus as in other chronic diseases that
the prognosis for the patient is extraordinarily
individual. (15)
The unique reality of medical practice is that
be it Paul Dudley White and his patient Chales
Thierry, on James Herriot and the dog Jock, it
is a one-to-one encounter where the uniqueness
of the individual, his disease, his very biologic
trajectory is unpredictable, unalterable, and over
whelmingly important. For modern medicine, the
most chastizing part of an individual's biologic
trajectory is its refusal to provide any quantita
tive correlationship between the earliness/lateness
of a disease on the one hand, and the proba
bility of the disease/death it may beget, on the
other. The healthy do not necessarily survive; the
diseased do not necessarily die.
Herdity
Herdity could well be described, at the very
outset, as a corporate programme subserved by
individual performance. Cellularity, systemicity and
uniqueness are features innate to an individual;
herdity is a force that the human herd exerts
on the individual. The individual-herd relationship
is a remarkable biologic feature that more than
vindicates John Donne's intuitive generalization
that no man is an island of itself; every man is a part
of the main.
As Dobzhansky (4) put it, mankind was and
is, a single inclusive Mendelian population and
is endowed with a single corporate genotype, a
single gene pool. Apposite to this is Carrel'S
description (2) of an individual as one who ex
tends, in time as in space, beyond the frontiers
of his body, and who is linked to the past and
to the future, regardless of the ephemerality of
his present. Add to this, the conceptual frame
work of quantum physics that reveals a basic
oneness of the universe wherein at a deep and
fundamental level, the seemingly separate parts
of the universe are connected in an intimate and
immediate way, in a complicated web of rela
tions between the various parts of the whole.
(1, 28) We are now poised to view an indivi
dual's body, his disease, his cancer—each un
failingly unique—as a spatiotemporal manifestation
of a cosmic order. I am what I am, and allowed
to be so, for I know who all others were, are,
and will be so as not to duplicate them, and
they in turn know of me so as not to make a
duplicate of me or of my disease at any time.
Climbing down from cosmic considerations
to clinical reality allows us to appreciate the role
herdity plays in the distribution of disease in any
given group. As the general statistics go, the
incidence of, say, acute lymphatic leukemia is 1
in 33,000, of cleft palate/neural tube defect is 1
in less than 1,000, of cancer 1 in 5, of blood
vessel disease 1 in 2, at random, country after
country, year after year. "Anybody who spends
a little time brooding over the statistics of can
cer must be struck by their unexpected cons
tancy. From year to year the figures for eac^
J
The evolution of the concept of polygenic
inheritance has brought a shift in genetic thin
king, from heredity to herdity, for polygenic in
heritance is necessarily a statistical concept that
concerns not the individual but Mendelien po
pulations or population aggregates. (4, 7) Polygenic
inheritance has been invokd to explain a wide
variety of diseases, ranging from congenital mal
formations to cancer, porphyria to peptic ulcer.
This means that most diseases do not have a
cause. Cause^ss diseases cannot be prevented;
they are an integral part of man'a growing; ca
use-wise and course-wise they are transtechnique*
Herdity is trans-technique.
AN ILLUSION
^orm'of cancer shxyw remarkably- little variation."
"having so -generalized,-Olemser (8y citers* figures;
^Here there are 5,3^5 cases of cancer of the
/pancreas ope
^427 cases? of tha cancer of
the pancreas two years later—almost
the same
number. Or in another country, there are. 218 ca
The noumenon of herdity governs all the
phenomena in relation to disease and death in
a herd. The herd determines who will get what
and when, in whom the disease will be slow,
•in whom fast, and so on. This would explain
why the commonness of prostatic cancer beyond
the age of 50 is paradoxically matched by the
uncommohness of its malignant behaviour and
how persons with bad coronary angiograms out
live those with good ones.
ses of cancer of pancreas one year, 221 cases
of pancreas the following year." These regional
constancies and interregional variations merge in
to a constant, global,
human character when it
is realized that although the anatomic
distribu
tion of cancer in different parts of the world is
extremely varied, the overall death-rate from can
cers at all sites is remarkably constant for humans
the world over. (24) The age-specific mortality
Tates from cerebrovascular disease, year after year,
rdecade after decade, and country after country
"fit quite closely the same line (10)" There is
something fundatnentally human in the global
impartiality with which disease and death treat
mankind. The prevalence of diabetes mellitus(l8)
is more or less constant for all countries. Can
cer, stroke, diabetes, hypertension, heart attack
and so on are an integral part of humanity, of
human herdity. This remarkable herd-certainty and
individual-probability of pathologic events is a
function of a corporate herd programme that
finds expression at the level of an individual who
has crossed a critical genetic threshold. (3) He
rdity, thus, is a reciprocal relationship between
an individual and his herd, what geneticistshave
been describing as polygenic inheritance.
4
The most compelling evidence in favour of
herdity is, in general, the programmed herd mor
tality that, as a physiologic function, (14) is
seen in man, in animals, in drosophila. Gompertz
(9) saw this as a constant increment in mortality
beyond the fifth quinquernium of human life,
doubling every 8 years, a phenomenon no me
dical advance has been able to stem. John
Knowles, as President of The Rockefeller Foun
dation, wrote in 1977 on "The responsibility of
an individual" (12) charging the latter's "perso
nal misbehaviour and environmental conditions"
for over 99% of illnesses. Knowles' faith in rea
soned behavior did not prevent the pancreatic
cancer that killed him in 1979. He was but one
of the 19,000 that develop pancreatic cancer and
die from it in USA, every year. Knowles died at
52. some do at an earlier age, others at a later
age, all a part of herd distribution, of herdity.
That human herdity has been exercising such in
fluences from times immemorial may be realized
from the fact that King Herod of Judea, died
of pancreatic cancer, in 73 B. C., at the age of
69. Cancer as a trans-technique problem has been
curing itself of research and researchers, and may
one day eliminate them altogether.
|0 r
_
v\l U
H
' 1
Conclusions
2] Carrel, A. : "Man, the Unknown". MacFadden
Publications, New York, 1961.
Systemicity, Uniqueness, Cellularity and Herdity of diseasing and dying can be read as the
latter's SUCH-ness, a Kantian ding-an-sich or as
the Zennist A’an Wats summed up, This is it.
The evolution of the tr< ns-technique concept,
based on SUCH-ness, explains technology's failu
res and limits, exercises restraints on this age of
inflated expectations, encourages us to be radical
enough to abjure straight-line solutions and many
a technologic trap—to wit, the tyranny of mass
screening, debilitating therapies, or killjoy preventionism. Jacob-Bigelow lamented, in the last
century, that most
men have
an exaggerated
opinion of the powers of medicine.
3] Carter, C. 0. : Genetics of common single mal-
A recent editorial (11) title "The toss-up"
bears eloquent testimony to the rationale of the
foregoing. It is common experience that, on a
given case, the proposed diagnostic/therapeutic
thrust ranges from medical conservatism to sur
gical ultraradicalism. After attributing such diverg
ence in medical thinking to the idiosyncracies of
the physicians, the authors propose: "Perhaps all
these factors are involved in clinical controver
sies, but we propose that one explanation has
not been sufficiently recognized; that it simply
makes no difference which choice is made. We
suggest that some dramatic controversies represent
/toss-ups'—clinical situations in which the conse
quences of divergent choices are, on the average,
virtually identical." The identicality of the conse
quences, no matter zvhat the investigations and the
therapy, is a function of the basic fact that the
problem be ng tackled is beyond the limits of
9] Compertz, B. . On the nature of the functions
expressive of the human mortallity and on a
new mode of determining life contingencies.
Phil. Trans. Roy. Soc. (London), Ser. A., 115: 513,
1825. Quoted by Kothari, M. L. and Mehta, L.
A.: Treatment of Cancer. In, "The Nature of
Cancer". Kothari Medical Publications, Bombay,
India, 1973, pp. 515-837.
technology.
Scientia est potentia: knowledge is power. The
knowledge that a lot in medical practice is beyond
medical technique can, as a concept, propel us
towards not doing in medicine. Munsif, an eminent
Bombay surgeon, was fond of aphorizing that a
good surgeon is one who knows when not to operate.
What a medical man needs to learn, in today's
technicalized scene is when not to act, an intelle
ctual and a therapeutic revolution that can safely
rest on the concept of trans-technique.
REFERENCES
‘“Capra, F.: "The Tao of Physics". Bantom Books,
' w York, 1977, p. 57.
formations. Brit. Med. Bull., 32: 21-26, 1976.
4] Dobzhansky, T. : "Mankind Evolving". Yale
University Press, New Haven & London, 1967.
5] Dubos, R. : Foreword. In, "So Human an Ani
mal." Charles Scribner's Sons, New York 1968,
p, 7.
6] Foulds, L. : "Neoplastic Development''. Vol. I,
Academic Press, London & New York, 1969.
7] Gardner, E. J.: "Principles of Genetics". Wiley
Eastern Private Ltd,, 1968.
8] Glemser, B.: "Man Against Cancer". Funk and
Wagnails, New York, 1969.
10] In gelfinger, F. J.: Arrogance. New Engl. J. Med.,
303: 1507-1511, 1980.
11] Kassirer, J. P. and Pauker, S. G.: The toss-up*
NewEngl.J. Med., 305:1467-1469, 1981.
12] Knowles, J. H.: The responsiblity of the indi
vidual. In, ‘ Doing Better and Feeling Worse:
Health in the United States." Editor: J. H. Knoweles, W. W. Norton and Company, New York/
1977, pp. 5780.
13] Kothari, M. L. and Mehta, L. A.: Cancer; Myths
and Realities of Cause and Cure". Marion Boy
ars, London, 1979.
14] Kothari, M. L. and Mehta, L. A.: The trans-science aspects of disease and death. Perspect. Biol.
Med., 24:658-666, 1981.
15] Krall, L. P.: Clinical evaluation of prognosis. In,
"Joslie's Diabetes Mellitus". Editors: A. Merble,
P. White, R. F. Bradley and L. P. Krall., Lea &
Febiger, Philadelphia, 1971, pp. 211-216.
16] Kurtzke, J. F : "Epidemiology of Cerebrovascu
lar Disease". Springer-Verlag, Berlin, 1969.
17] Lipkin, M : "The Care of Patients—Concepts
and Tactics ''. Oxford Univ. Press, New Yorf
and London, 1974.
5
REFERENCES: Continued
18] Malins, J.: "Clinical Diabetes Mellitus," ELBS
and Chapnan & Hall, London, 1975, p. 47.
19] Malleson, A.: "Need Your Doctor Be So Use
less ?" George Allen and Unwin, London, 1973.
20] Medawar,. P. B. : "The Uniqueness of the Indi
viduals". Methuen, London 1957.
21 [ Peto, R. : Epidemiology, multi-stage models &
short term mutagenicity tests. In, "Origins of
Human Cancer". Editors: H. H. Hiatt, J. D. Wa
tson, and J. A. Winsten. Cold Harboi Labora
tory, U.S.A., 1977, pp. 1403-1328.
22] Roe, F. J. C. : Cancer as a disease of the whole
organism. In, "The Biology of Cancer." Editors
E. J. Ambrose and F. J. C. Roe., D. Van Nos_
trand, 1 966, pp. 1 -32.
23] Shah, S. J. : "Layer Concept of Coronary Heart
Disease". States' People Press, Bombay, 1980.
6
I
24] Smithers, D. W. : "Clinical Prospects of The
Cancer Problem". F. & S. Livingstone, Edinburgh
and London, 1960.
25] Spriggs, A. I., Boddington, M. M. and Halley,
.
W.: Uniqueness of malignant tumours. Lancet,
1: 211, 1967.
26] Wiicox, W. S.: Ti e last surviving cancer cell;
The chances of killing it. Cancer Chemotherap.
Rep., 50: 541-542, 1966.
27] Wildavsky, A.: Doing better and feeling worse;
The political pathology of health policy. In,
"Doing Better and Feeling Worse: Health in the
United States". Editor: J. H. Knowles, W. W.
Norton and Co., New York, 1977. pp. 105-123.
28] Zukav, G.: "The Dancing Wu Li Masters:
Overview of the New Physics". Bantam P
New York, 1979, p. 82.
102
medico friend
circle
bulletin
JUNE
1984
^0)
TOWARDS AIM APPROPRIATE STRATEGY
Ulhas Jaju, Sewagram
However much one may speak of an egalitarian
society, there will always exist stratification and the
differences between strata can at the most be mini
mised. Those who are better placed are in the mino
rity and utilise the available health services to the
maximum, while the vast majority who are poor crave
for them. If the health services are to be utilised
equally by all, the system should be so moulded that
it remains accessible equally to both groups of the
population.
How can one achieve this goal? The proper
distribution of available resources calls for restraining
those who over-utilise them and facilitating the use
by others who under-utilise the health services.
The distinction becomes very difficult when a sick
person (whether rich or poor) comes to the hospital.
Human considerations justify all earnest attempts to
save one life, whatever it may cost. On the other
hand, with limited resources at our disposal, cost
bdnefit rationale demands sacrificing one life for
the sake of saving a hundred others.
The lack of this logic in the administrative set
up of almost all medical institutions is responsible for
the diversion of 80% of the health budget to few
urban hospitals which have intensive coronary care
units, dialysis centres, sophisticated cardiac surgery
units, cancer institutes and so many other facilities
while the majority of the population lives without
even primary health care.
I
Even if one agrees in principle to use this logic
in health service administration, suitable alternative
approaches need to be tried in the field. Many
philanthropic institutions, out of compassion towards
suffering humanity, have extended their services to
the ‘Have Nots’ These are charitable hospitals or
dispensaries which provide free services to the needy.
However, charity corrupts people and makes them
dependent on welfare services. The health needs of
this group of population is so enormous, that these
institutions perpetually depend heavily on outside
finances.
A few institutions have tried to raise resources
locally. Some such attempts have been made in the
organised labour sector also. In the unorganised
sector, no attempt has been made till now. The
description which follows discusses in detail how a
health insurance scheme was evolved for the villagers
near Sevagram Medical College, over the last five
years.
When the search began :
It started with village Nagapur. A decision to
start a weekly OPD was taken in a village meeting.
The school building was offered to us for running
the dispensary. An initial contribution of Rs. 4-00
per family was collected by the village leaders towards
the drug bank. Commonly needed drugs were pur
chased on our advice. A village health worker was
selected who was assigned the job of drug purchase,
drug dispensing and record keeping. The drugs were
dispensed at cost price.
One day a mother carried her sick child to the
dispensary. The child had bronchopneumonia. The
total cost of drugs prescribed, including anti-biotics
was around Rs. 15-00. The mother had no money.
She requested drugs on loan and promised to pay
the bill the next week. Human considerations prevai
led. The next week never came in spite of repeated
reminders. The story was repeated for many others.
Our drug bank went bankrupt. A meeting was held
with the villagers and it was unanimously decided that
drugs will not be issued to the defaulters in future
until the old loan was paid.
Although the decision sounded fair, we could
envisage a sick child in a poor family, lying at home
INSIDE
Dear Friends
3
The Final Epidemic
4
Anti-Nuclear War appeal
6
Keeping Track
7
From the New Office
7
Editorial
8
The total contribution collected fell short of
our drug bank’s demand. We had to depend on free
drug samples to run the OPD, for the next one year.
At the end of the year, analysis of illness treated in
the village dispensary revealed that 95% were com
mon, self-limiting diseases (upper respiratory infec
tion, viral fever, gastrointestinal infections etc.)
which a village health worker could treat. Other
patients needed costly drugs (mostly anti-biotics)
which put a heavy burden on the drug bank and
invariably these patients needed hospitalization.
with high fever but the mother not coming to us as
she fears we would demand clearance of the old
debt. Analysis of a year’s OPD data revealed that
the village dispensary was utilised preferentially by
the rich section of the community.
It was time for us to evaluate. Why do we go
all the way to a village to run a dispensary? Is it to
treat minor illnesses of those who can afford to visit
Sevagram hospital 5 kilometers away or to provide
medical help to a needy child from a poor family.
We again sat with the villagers. The conclusions
emerged that for the health facility to be accessible
to the needy, it must be provided free at least for
acute unforeseen illnesses; and to help those who
cannot afford the cost of the medical treatment, a
village fund should be collected every year when the
iowar crop is harvested. Villagers found it easier
to contribute in kind. The sense of brotherhood still
prevailed in our village community and the idea ot
contributing according to capacity and services being
given according to need was accepted. Contribu
tions were decided on the basis of land-ownership.
A wage earner’s family would contribute 4 Payah or
jowar while a farmer would contribute 2 Payah per
It was at this juncture that we learnt that health
services among the poor cannot be totally self-reliant.
We also realised the need for a central hospital to
cater for acute illnesses and emergencies.
From the third year on, the village dispensary
was linked with the Sevagram hospital for referral
and for admission of the sick. We learnt new lessons!
A pregnant lady was admitted a month before the due
date on the pretext of getting recurrent abdominal
pain and her husband expected us to keep up our
promise of treating and feeding her free in the hos
pital till she delivered. Another wanted hospital
TABLE
COST ANALYSIS YEAR
1982
Village: 4
Population covered: 3973
INCOME
Contribution toward health insurance
Rs.
EXPENDITURE
4,959.50
VHW Honorarium at the rate of
Rs. 35.00 per month x 4
Village drug kit at the rate of
Rs. 15.00 per month x 4
Fuel charges for monthly visit at the rate
of Re. 1.00 per km for an average of
15 km run per visit per village
Salary of ANM at the rate of
Rs. 700.00 per month for
coverage of 12 villages
Recovery from indoor admissions —
non-insured bill
— with 25% hospital bill
5,490.00
630.00
11,079.50
Balance with the hospital
Rs. 16.67 per indoor admission
5,159.50
(total 307 admissions)
Rs.
1,680.00
720.00
720.00
2,800.00
5,920.00
admission to by-pass court summons. A paraplegic
was dumped by the relatives in the hospital.
acre of land holding. Where there is additional source
of income, the family should contribute 4 Payah
more. As a code of discipline, non-contributors would
not be offered beinefits of the dispensary.
We went from house to house to collect jowar.
To our surprise, active enthusiastic village leaders
were conspicuous by their absence. When their turn
came, they evaded us under some excuse or other.
•After four visits to the village for collection we had
to digest the hard fact that the rich section had pre
ferred to keep away from the scheme. The calcula
tion of cost-benefit revealed to them that even though
their contribution would be more, the services offered
to them would be on par with others.
Since theta we had to modify our criteria for
free indoor service. For all acute and emergency
patients, hospital services were offered free while for
chronic illnesses like cataract, hydrocele, hernia, old
polio etc. and normal delivery the patient was charged
25% of the hospital bill.
The village dispensary is now run by the village
health worker, who is provided with a drug kit. An
arrangement is made to ensure proper referral to the
hospital. A mobile health team consisting of a doctor
and an ANM visits once a month when maternal and
2
y)
jl | r C
A>vx 1 hhl-i.
NV
»
'SmKSSBS
been extended to eight villages.
Evaluation
We evaluated accessibility of medical services
to the poor from the percentage of coverage of health
insurance scheme
3 ^ears
farmers. It rose from 46.5% to 71.5 /0 in 3' y
in the total population and from 36% to 78 /o
labourers and marginal farmers. That the village
folk took some years to trust us, is obvious from the
rising figures in successive years.
The total number of hospital admissions increa
sed over successive years in parallel to increasing
health insurance coverage, a sign that the hospital
is utilised more and more by the people if it is within
their reach. There was one hospital admission tor
every 13 people and this figure has remained constant
over the successive three years. Average hospial stay
was 5 days.
Cost Analysis
It is difficult to calculate the money the hospital
spends on admissions. The existing hospital charges
are not worked out in accordance with what the hos
pital spends on a particular item. Sevagram hospital
(01;
f
01®
to what a service oriented hospital would have. Being
a post-graduate teaching hospital and research orien
ted institute, it is not possible to restrict admissions
to emergencies and common medical problems. Seve
ral specialities exist and thus lead to extra-expen
diture than what one would expect from a hospital
equipped only to deal with common emergency
situations.
The cost analysis tor the year 1982 reveals that
83.7% of the money spent on the village health
worker’s remuneration, his drug kit, travelling charges
and salary of ANM could be recovered from the
village contribution. If income of the hospital from
indoor patients of the covered villages is taken into
account, the hospital could get Rs. 16.75 per hospital
admission. Obviously hospital had to spend much
more on indoor admissions (see Table) .
Hospital indoor expenditure apart, we spent
Rs. 1.50 per capita over peripheral health service.
The State gives Rs. 8.85 per capita health budget
in Maharashtra, which includes all services. It is our
belief that even with existing resources, proper distri
bution of available funds can provide qualitatively
much better services if an appropriate strategy is
employed.
ri *
I C'V)
Drug Action Focus
(’Dear friend. . .
4.
Annual Meet 1985 — Some reflections
This was the first mfc meet I attended. 1 am
very happy to have come. I am impressed and
encouraged to meet such a variety of people
who are committed to people especially the op
pressed and who are concerned about a change
in values — <a change of society.
The meet was interesting, but a little too
packed; there was not enough time to meet
people individually (But in only 2 dlays it is
almost impossible)
Hilda Sima, Vagamon, Kerala.
2. First let us say that the qualities, backgrounds,
achievements, activities, and aspirations of the
group in general were varied and exciting It
is good that such different people can come to
gether with some hopes and interests in com
mon, and share and develop their ideas. The
‘old’ group did not dominate the ‘new’ nor did
they show impatience nor intolerance with
the ‘new’. Even the long term mfc members
did not criticise each other in harsh terms
and showed1 mutual respect even in disagree
ment. This is amazing and highly commend
able.
Everyone seemed welcome to attend and parti
cipate. The attitude seemed to be that we
could all learn from each other.
Small group discussion followed by plenary
sessions were very good. A little more time
for informal meetings would have been nice .
It would have been nice to have all the back
ground! papers before the meet because read
ing time was short once we arrived..
The meet served its main purpose for us in
meeting like minded medicos and non-medicos
alike from various parts of India.
Penny Dawson, Jamie Uhrig,
Mitraniketan, Kerala.
I got to know quite a number of people with
3.
whom I would never have come in contact otherwise.
It was quite informative except where people were
getting into unavoidable technicalities, which of
course were difficult to follow.
The time limitation was an inhibiting factor.
We had to skip quite a lot of things.
I was in the group discussing how to raise publie awareness about TB. The ways that were dis
cussed were the ones that we had already discussed
in our SPACE meetings. Participants were trying
to express with their experiences why they came to
such conclusions. They were not allowed to tell their
experiences but what they had inferred from it—
of course due to lack of time.
Then some participants had a set of opinions
formed and they refused to come out their circle.
This led to heated arguments now and then.
On the whole it was nice.
—Malarvizhi, Madras.
1.
Instead of choosing new topics each time can
we have a meet where we reanalyse some oast
issues and topics. There is a general feeling
amongst people that after discussions we do
not follow up on the topics anymore. Drugs
topic for example.
I think although the Drug Ac'ion Network is
working full time some of us in mfc feel side
lined now and find little or nothing to con
tribute Raising the issue in an annual meet
may turn out newer aspects of the problem.
I think that DAN is directing its efforts in the
wrong direction. Instead of pressing the drug
controller of India for action all of us should
conscientize undergraduates' and upcoming do
ctors. Our fight should be at a lower level
rather than at the level of government policy.
This is my disillusionment with the DAN and
I hope we can correct its course by another
discussion on the topic of drugs.
Vineet Nayar, Vellore.
Whither Company Doctor?
5.
5
The purpose of this letter is to motivate a
social scientist or a researcher to conduct a
study on the interaction between a worker and
the so called “company Doctor” I am sure that
the findings of such a study will be revealing.
Both public and private sector Industries em
ploy doctors on parttime or full time basis to
man their first aid centres, ambulance rooms,
dispensaries and hospitals, and these doctors
’are called “company Doctors”.
An observation made by mfc (over a period of
three decades) is that the workers look at the
company doctor wiKh askance. He is consider
ed as a “management Agent” having no sym
pathy for the workers. The workers attribute
the following characteristics to the company
doctor.
1) He lacks human touch. He thinks that
workers FEIGN sickness.
2) His medical opinion and diagnosis are de
pendant on the instruction of the company/management .
c) At the behest of the mlan'agement, he goes
to the extent of certifying as “medically
unfit” even physically fit persons.
4) He asserts that working environment and
sanitation are the best available any
where.
In most cases where his opinion is contested
and referred to outside doctors and specialisl' S,
he is proved wrong. In most of the court
cases, he is disbelieved and held to be biased.
, I wish that there is a healthy debate and any
company doctor comes forward to assuage these
feelings of workers. It is observed that public
sector employees have better opinion about
their company doctors.
Yours
Bangalore
U.S. Venkatraman,
IM
' C -v;
is not possible to come to a consensus in our under
standing of how to proceed in action — atleast
not
always.
The direction
is similar but
mode
of
action
will
differ
according
to our perspectives. We have now to choose bet
ween two options:—
i) Do we insist on common action and in the
process either split up (each group may claim to be
mfc) or let the group wither away in what appears
to be a natural aging process. OR
ii) We regard each other as important and
necessary and express concern towards each other,
try to understand how the other person is thinking
and acting, try to spell out the direction in which
we should progress and leave the action at an indi
vidual level.
Vear Jriend
mfc role
mfc has been trying to define it’s role (refer
minutes of Patiala meeting mfeb 116-7). The expec
tation of individual members are so varying that it
has been difficult to come to a common conclusion
In the process the decision is being kept open.
Most of us wish to see mfc in action, be it
drug action forum or Bhopal disaster. In their bub
bling enthusiasm (I am all for it), the individual
members sometimes ‘try to project their action
(action which they feel correct) as mfe’s action.
All the members might not support the way in which
action is taken. In the process, I see some members
withdrawing from mfc—a sign that mfc will wither
away if the same process continues.
What I mean is that we be non-possessive
for a ^roup-action and be more committed to mak
ing friends and understanding each other.
I am trying to limit the role of mfc to a body
of friends with a common concern and regard for
each other, interested in trying to spell out a com
mon direction. The action is left to the members
individually. Which means, there will be nothing
like mfc activity but activity
performed by the
members of mfc. In the process if a group of mfc
members
find
< they can go ahead
k
r.
. a common
action,
with it in a group capacity and1 not in mfe’s
capacity.
We are so possessed by the obsession that
mfc should plunge into collective action, that we
have started neglecting the group’s linking thread
i.e. the friendship. There was a time when we used
to come together to share our field experience and
our dilemmas in day to day life. We tried to overcome
our loneliness by coming to mfc where we found
some thing to fall back upon.
Look at the mfc meetirgs in the recent past!
We are so ’‘action oriented” that we come together
only for a specific business. The agenda is packed
and exhausting. The poor convenor is hard pressed
in trying to sort out all the matters in a specific
time. In the process there is hardly any time
to
strengthen the bonds of friendship. Infact they often
get burnt during heated aggressive discussions—a
characteristic of mfc. After all we are all conscientised individuals! We see the need for intellectual,
partnership, the tender linkages between hearts in
a common search is forgotten. The vociferous few
dominate the group meetings and succeed in gett
ing mute consensus. The mute members, do not
dare oppose the vociferous few, and in the process
prefer to keep away from action and sadly from the
medico-friends circle itself.
The task ahead is tremendous. Our numbers
at present are quite inadequate. In the process of
our individual searches our egos are also nurtured
making us feel that our way^is the only way. Let
this 'ego’ not clash-I see it happening. In turn let
us nurture friendship, a friendship that can appre
ciate another’s views however different from ours.
For a group like mfc, to grow in a spirit of dialogue
and evolve, however slowly, a common perspective,
this attitude must remain primary.
Ulhas Jajoo
MGIMS
Sevagram, Wardha.
AIDAN role
Saw Vineet’s note in the mfc bulletin of May
1985 (No.
(No^ 113) 1I was quite amazed at his assessment of Drug Action Network’s (DAN) direction
of efforts.
I am not against action. A committed indi
vidual is always involved in action at his own level
The real issue is whether mfc as a group is coher
ent enough to take-up common action.
If there is anything we all feel good about the
Network, it’s the total liberty of members to choose
the level of action and mode of action related to
drug issues — as long as they are in keeping with
the major objectives.
We come from various backgrounds. Wc
have a common goal. . . We have commitment. The
•road that will take us to the desired goal differs
considerably depending on which shade of ideology
we owe our motivation. Though we do no:
doubt the bonafides of each other’s commitment
towards the goal, we agree to disagree on the stra
tegy of action. The means adopted to reach the goal
is important to most of us.
The Drug Controller of India happens to be
merely one person in a massive bureaucracy dealing
with Drug Policy issues. With the National Drug
Policy in the offing, pressure has to be applied at
various levels on various individuals involved in
the making of the drug policy from the members
of Parliamentary Drue Consultative Committee
What 1 am trying to drive at. is that due to
the heterogenous nature of membership in mfc, it
7
struggling
to
get
are
countries,
which
out of the clutches
of
the
pharmaceutical
giants. If a handful of health activists have to
intervene, it can only be at the most strategic
points. I am afraid, for effectively motivating thou
sands of undergraduates coming out of the 106
medical colleges, we will have to depend upon the
socially conscious members of mfc. DAN has never
made any promises of changin the world over
night. It is an emerging force no doubt, depend
ing on long term commitment and contribution of
a host of persons like you and me to the drug and
health scene of the country. Most of the organiza
tions involved in AIDAN are extremely clear about
their choice of their workipg strategy and details
of their action plans- Fighting for a Rational Drug
Policy is the priority of the Network, as decided
by the Coordinating Committee; it being the need
of the hour.
to the Department of Chemicals and Fertilizers,
Ministry of Health to Social Action groups, faculty
members of medical colleges, consumers etc.
The DAN expects pooling in off efforts, so
while some networkers contribute by protest mar
ches, signature campaigns, public and consumer edu
cation: others contribute by alerting key social
action groups and monitoring policy changes. Our
contribution depends upon our initiative, our
understanding ot the problem and our area of fun
ctioning. For those based in medical colleges, the
expectation is that they contribute In screening
medical literature, reaching out to medical gradua
tes and providing back up support.
The entire DAN cannot and should not put
its efforts in medical colleges. Why don’t we en
quire from others in mfc what their experience has
been in terms of impact with such efforts? These
efforts were not related to the issue of drugs but
dealt with the much more fundamental concept of
‘health’
>—mira shiva
Coordinator , (AIDAN);
New Delhi
(We request reactions to both these letteirs so
that the dialogue can be continued — Editor.)
You must be aware that the National Drug Policy
.is coming up in the parliament in the monsoon ses
sion and if you have been following up the trends,
you would be as distressed as many of us are. The
discussion on these matters should not be merely
at the consumer and medical graduate level, but
also at the level of faculty and top brass of teach
ing institutions.
You may not be aware that when we were try
ing to muster support for the courageous Bangladesh
Drug Policy, when pressure from vested interests
was mounting, the support came much more from
IITs
(Indian
Institute of Technology) than
medical colleges.
What can those who want to work primarily
with medical students do? Here are some suggetions:
1. Review medical literature regarding fixed
dose combinations of steroids and other to prove
their irrationailty;
2. Review whatever sources we can about the
various drug utilization studies in India and
identify areas of interest for conducting special
studies on drug utilization patterns, eg TB care or
diarrhoea care.
3. Prepare guidelines of what young doctors
ought to know about Rational Drug Policy.
4. Follow up Pharmaceutical policy issues in
Economic Times, Eastern Pharmacist, Financial
Express; Business Week etc., to follow the trends
and communicate these to the doctors and under
graduates.
The Bangladesh Policy itself may not be able
to survive, if India formulates the kind of drug
policy it seems to be formulating. This would put
an end not mdrely to our own efforts towards a
Rational drug policy, but also of other third world
8
►
/Y<c
I
Food in the Hands of Big Industry
Iodine — deficiency goitre is one of the
nutritional prolems that can be ver^ easily con
trolled and prevented. This has been successfully
done in many European countries. In India, the
entire Sub-Himalayan belt comprising of Jammu
& Kashmir, Punjab, Haryana, H P; northern parts
of UP, Bihar and Bengal, the far-eastern States
and isolated pockets in Maharashtra and M P. are
endemic for goitre. In 1959, the government with
UNICEF aid set up 12 iodisation plants to produce
iodised
salt
(Potassium
iodate
added
to
common
salt).
The salt
produced
was to
meet about 50% of the estimated needs and also
some of the needs of Nepal. However, and not sur
prisingly, even this simple programme of manufa
cture and distribution of the salt, suffered from
various defects. These were reviewed by Dr. Gopalian
under the title ‘The National mitre Control Pro
gramme — A sad story’ (NFI Bull. July 1981).
About four years ago, at a seminar at the
NIN, we were informed that the government
was
contemplating handing over the iodisation pro
gramme to the Tatas. In this matter, obviously the
govt, did not drag its feet and on my recent visit
to Delhi, 1 saw iodised salt in the market. Whether
handing over the production to the Tatas will solve
the goitre problem, is an entirely different maitter.
I do not know whether Tatas will also handle the
distribution- One of the reasons for the failure of
the National Programme was nonavailability of the
required number of railway wagons for the trans
portation of salt, and that the railways did not
provide covered wagons duriny the rains. How
will the Tatas solve this problem, and if distribu
tion is still in the hands of the government, then
what matters who produces the salt?
The Control Programme involved manufacture and distribution of the iodised salt. Plants
for iodisation were set up with UNICEF aid and
■we had all the technical know-how. Since it was
fortified common salt, the house wife would use it
in cooking and there was not much nutrition educa^tion involved. The salt was to be sold in place of
ordinary cooking salt, therefore sale of ordinary
salt was to be banned The extra cost of iodisation
was not to be borne by the people but by the govt.
There the salt was to be sold at subsidised
cost. Perhaps. Tatas are now receiving the subsidy.
Whether administrative inefficiency alone was
responsible for handing over the production to the
Tatas or whether other factors weighed equally or
more, one will never know.
As Dr. Gopalan said
“administrative incompetence, lack of co-ordina
tion between various agencies involved, and Com
mercial and vested interests (emphasis mine) have
apparently combined to wreck the Programme.”
Although termed a National Programme it was natu
rally restricted to certain contiguous geographical
areas. Of couse, in a country of India’s dimensions,
even this area is sufficiently large. Nevertheless,
the Programme was a comparatively simple one.
But it failed and that too, in the'hands of a govern-
ment which claims to improve the health and nutri
tion of millions of children through a nation-wide
network of ICDS Programmes.
I do not know whether the Tatas are using
the national iodisation plants or whether their salt
production is in addition to that produced by the
public sector or whether those plants are now let to
lie idle. The point is, that a health programme, not
dependent on ‘drugs’, has passed into the private
sector.
That, however is not the end of my story.
Of the total common salt, or sodium, chloride manu
factured, only a small amount goes for human
consumption. Much of it is used for industrial
purposes. The Tata chemicals were perhaps already
manufacturing common salt, and production of
iodised salt will be a very small part of this ven
ture. However, for producing edible salt for iodisa
tion, they apparantly produce more salt than
needed for fortification. This Tatas are therefore
now marketing table salt, at least in the cities
where table salt (powdered common salt) is mostly
used.
Hitherto, table salt was marketed by small
entrepreneurs. It w*as
mostly pulverised crude
salt. Tatas salt may be more refined. However, the
small industries will never be able to compete with
a big industrial house. By taking the lead from the
Tatas, if other chemical manufacturers also market
table salt, the small or cottage industries will have
to close their business. A year or two ago, Brooke
Bond, the famous Tea and Coffee House Started
marketing powdered spices like chilli, turmeric,
dhania etc. Once again, entry of a big industrial
house into the domain of cottage industries. Very
recently, in the South, another big company has
started marketing vadams (badis) and papads, in
fancy shapes and under very fancy names
This then is a slow but steady entry of big
industry into that part of the processed food market,
which uptil now was entirely under cottage indus
tries. Although such cottage industries were in the
hands of middle classes, driving them out of busi-
(Continued from page 7)
ness in this manner, will not help the poor but only
expand the ranks of the poor. I am not an econo
mist. I do not understand the full implications
and the reasons for big industry entering into the
small-chain food market, but to me the consequen
ces appear alarming.
— K. S. Jayarao, Hyderabad
7
4
mfc bulletin: JUNE 1985
RN.27565/76
Effects on Mental Health
(Continued from page 5)
supportive follow up for mental health problems in
adults, adolescents and children (2).
A team of psychiatrists from NIMHANS,
Bangalore have conducted training programmes in
mental health for the medical officers of the state
health services, posted in the gas affected areas.
Tht training provides the necessary skill to diag
nose and manage the common mental problems seen
in the victims of the gas exposure (2).
A mental health care manual has also been
prepared by the Bangalore team (3).
The mental helalth dimension is a much
neglected dimension of health inspite of the much
publicised WHO definition of health. Doctors in
Bhopal werei disregarding or misinterpreting the
symptoms of
stress
and
passing
it off
as malin ering or compensation, neurosis, Thi's
mis-dia,gnosis was sadly reflective of our medical
training which plays only lip service to mental
he’alth inspite of its grave importance in health
care and the doctor patient relation-ship.
We salute our community oriented Psychia
tric colleagues for bringing to the fore this much
neglected dimension through practical interventions
in supportive care, communication and training in
Bhopal and not exploiting the situation only for
its research potential.
1. Kinston, W and Rosser, R. (1974)
Disaster: Effects on Mental and Physical state, Journal of
Psychosom. Research 18, 4'i'l
2. Directorate of Information and Publicity, M.P. Govt (1985)
Review meeting of ICMR Projects at Bhopal, Khabar,
5th May 1985.
3. Mental Health Care Manual for Medical Officers.
by R. Srinivas Murthy et al., National Institute of Mental
Health and Neuro Sciences, P.O. Box. 2900, Bangalore 560 029. (For copies of the manual write to Dr. R. Srinivas
Murth} at the above address)
4. Also available with mfc office a list of references on mental
health aspects of disasters.
The Challenge of Bhopal
(Continued from page 1)
ghf provoking example showing that if we want
to, we can.
Bhopal too is a challenge? So are many other
more insidous developments in our country. The
growing investment in nuclear -— energy now dis
credited as an energy resource in the West, or the
gradual take over of the cottage industry in food
by big business, — Cach of
this
though
different from th© other has a growing similarity
representing either a subservience to the profit
motive or an insensitivity to health hazards or
Editorial Committee :
kamala jayarao
anant phadke
padma prakash
ulhas jaju
dhruv mankad
abhay bang
editor : ravi narayan
Regd. No. L/NP/KRNU/202
both. We feature some of these aspects in this
bulletin. We also feature investigations in Bhopal
which raise some of these issues for our readership.
Minim ata, Seveso, Long i sland were too1
distant to make any impact. Amlai, Chembur, Handigodu, Harihar, Zuari, Nagda, Mavoor, Silent vally,
Thai vaishet hare not stimulated us either. Will
Bhopal dp so?
Nuclear Hazards
(Continued from page 6)
true, is truly shocking.
7) Functioning of the health physics unit: The
health physics unit that monitors radioactivity and
oher environmental pollution in the NFC should be
under an independent agency not answerable to NFC
or the BARC. The alleged victimisation of a scien
tist of the health physics unit who did try to raise
his voice about some of th© environmental issues,
(if correct) is a matter of deep concern.
In conclusion we suggest that an independent
panel of experts and concerned ctizens be invited
to make an indepth, impartial inquiry, and review
the situation in its totality (rather than isola
ted accidents) and suggest immediate remedial
measures. In this regard our Forum will be willing
to offer Whatever help it can.”
(Some action towards improvement has taken
place in response to this letter. For instance the
Nuclear Fuel Complex has been brought under the
Pollution
Control
Board
and
they
have
to
obtain
consent
from
the
Pollution
Control Board before discharge of the efflu
ents. They have built a compound
wall to
improve security. Their sedimentation ponds have
been lined with some kind of plastic material to
prevent seepage. Several shortcomings still need to
be reexamined.)
Will citizen’s groups keep up the pressure
please! This is particularly urgent since a recent
government decision will promote their installation
all over the country in our attempt to prepare our
selves for the ‘quantum
jump’
into the
21s Century. The movement against the prevention
of Nuclear War is not enough!!
(see mfcb 102)
(Continued from page 7)
ness in this manner, will not help the poor but only
expand the ranks of the poor. I am not an econo
mist. I do not understand the full implications
and the reasons for big industry entering into the
small-chain food market, but to me the consequen
ces appear alarming.
— K. S. Jayarao, Hyderabad
Views and opinions expressed in the bulletin are those of the authors and not necessarily
of the organisation.
Annual subscription — Inland Rs. 15-00
Foreign ; Sea Mail — US $ 4 for all countries
Air Mail : Asia — US $ 6; Africa & Europe — US$9; Canada & USA — US $ 11
Edited by Ravi Narayan, 326, Vth Main, 1st Block, Koramangala, Bangalore-560034
Printed by Thelma Narayan at Pauline Printing Press, 44, Ulsoor Road, Bangalore-560042
Published by Thelma Narayan for medico friend circle, 326, Vth Main, 1st Block,
Koramangala, Bangalore-560 034
l (
a;. I vl
47/1. (First Floor) St. Marks Road,
Rancmlore - 5SO CO If
E
F
137
^“9
a7
E2
Sb
4 ?
15
3b
Ip
lb
1112
-
3
b
j
:
j
j .
■J
■
iZ
K.
\
i .; b
medico friend I bils
circle
biiiletiri
■
;
()i9
|!
FEBRUARY 1988
ii
.'nA
Logistic Support and Facilities for Primary Health Care
(Crucial Role of Physical Accessibility)
Ashish
In the rhetorical discussions on the Alma Ata
Declaration of Health For AH By 2000, not enough
attention has been paid to the crucial roie ot
physical accessibility. The Alma Ata Declaration
(1978) does show awareness of the fact that "the
success of primary health care depends on ade
quate, appropriate and sustained logistic support.."
and recommends that "government ensures that
efficient administrative delivery and maintenance
services be established reaching out to all primary
health care activities at the community level....
That the government ensures that transport and
physical facilities for primary health care be func
tionally efficient.."
"The global strategy for health for all by 2000"
adopted by the World Health Assembly in 1979
indicates that "the main thrusts of the strategy are
the development of the health system infrastructure
starting with primary health care for the delivery
of country wide programmes that reach the whole
population." (WHO, 1981 : 12).
In the international literature much is made of
the Kerala model. Several Sophisticated statis
tical exercises have also been made on the impact
of literacy, education, status of women, higher
age at marriage and related factors on the fertility
pattern. However, there is no evidence that
these exercises have taken adequate note of the
human settlement pattern and the access to
health and education which the state of Kerala
has, by virtue of its unique settlement pattern
where one can hardly distinguish a rural area from
an urban area. This is partly a function of density
■ i io
Bose
of population. But a number of historical, geo
graphical, political, economic and other consi
derations have influenced the settlement pattern
of Kerala. For example, according to the 1981
Census, in Kerala, 90.3 per cent of the rural popu
lation was enumerated in villages with population
of 10,000 and over. The comparable figure for
Bihar was 4.2 per cent; Madhya Pradesh 0.1
per cent; Rajasthan 0.9 per cent; and U P 0.7
per cent. In terms of the number of villages (in
Kerala)^74.3 per cent of the total number of rural
settlements belong to villages -with population of
10,000 and over.
The comparable figure for
Bihar is 0.3 per cent; Madhya Pradesh negligible;
Rajasthan 0.1 per cent and U.P. 0.1 per cent.
These figures bring out the sharp contrast between
Kerala on the one hand and large states like,
Bihar, Madhya Pradesh, Rajasthan and U P (which
will be referred to subsequently as BIMARU
states), on the other.
As is well-known, in our strategy for primary
health care, we have more or less adopted a
blanket approach throughout the country (though
there are some minor modifications in tribal and
hill areas) by laying down norms for the establish
ment of primary health centres, sub-centres, etc.
lj
H
iI I
The computational work in connection with
this project was done at the Computer Unit of the
Institute of Economic Growth. The author ac
knowledges the assistance given by K. Lal, Pro
grammer and Jatinder Bajaj, Senior Research
Analyst, Population Research Centre.
§
»
a
M pc
Inherent in our primary health policy is the weigh
tage given to population. In other words, if the
majority of the villages in Kerala have a population
of over 5,000, it is obvious that there will be sub
centres located in these villages and the access
of the people to primary health care will be greater
in Kerala than in U P because of the combined
effect of the settlement pattern and the weightage
given to population in our health policy. When
we consider the physical accessibility on the basis
of data on transportation, the contrasts are even
sharper. For example, in Kerala, for every 100
sq kms, the length of roads was 275 kms. The
comparable figure for Bihar is 48; for Madhya
Pradesh 24; for Rajasthan 21 ; and for UP 52.
Another index of road transportation is the length
of roads per one lakh population. In Kerala, for
every one lakh population, the length of roads
is 421 kms. The comparable figure for Bihar is
120; for Madhya Pradesh 204; for Rajasthan 213;
and for UP 129.
!
I
'd■ I
'-J
li
I
iI I'
i i
a
I
bi
■1
Ik
!
..
I
I
"’4
■J
I
I
i
T
I
11
11
11
11 ■
Mo
I
o’L
H
Next we cerne to high /higher secondary
schools. In Kerala, the figure was 76.5 per cent
while in Bihar it was 4.8 per cent; in Madhya
Pradesh 1.8 per cent; in Rajasthan 3.6 per cent
and in UP 3.5 per cent.
-A
These figures speak for themselves.; Both in
terms of health and education, the settlement
pattern favours Kerala. If the literacy rate is high
for Kerala, one could ask why is it high ? It is
obvious that the settlement pattern in Kerala makes
access to schools and primary health centres
easy, compared to the situation in BIMARU states.
Before we look into the so-called cultural and
other factors while explaining the diversity in
India, we feel that we should have a good look
at the human settlement pattern, transport linkages,
and the communication network.
The 1981 Census (and also earlier censuses)
classified rural settlement into the following seven
categories (Table 1).
Another question one may ask in the context
of physical accessibility is, how many villages are
linked with roads ? the road statistics give such
data for only two categories of villages namely
(a) villages with population 1000-1500 and (b)
villages with population 1500 and above. In
Kerala, 100 per cent of villages are linked with
roads in category (a). The comparable figure
for Bihar is 39 per cent; and for Madhya Pradesh
40 per cent; for Rajasthan 40 per cent; and for
UP 25 per cent. For category (b) villages, the
figures are as follows : Kerala 100 per cent; Bihar
52 per cent; Madhya Pradesh 65 per cent;
Rajasthan 56 per cent and U.P. 52 per cent.
Thus, the human settlement pattern, the size fof
villages, the distribution of villages, and the road
transportation system all favour Kerala in terms
of the delivery of health services. What is true
of health is also true of education.
G
G"
G
G'
C
c
c
c
G
C
6"
G
&■
C
&
V,
e
e
Aa
TABLE-1
Category
e
Population
I
less than 200
II
200-499
III
500-999
IV
1000-1999
e
e
e
e
e
e
V
2000-4999
(S.1
VI
5000-9999
e
VII
10,000 and above
In our statistical exercise, we have worked out
the settlement pattern with reference to villages
as well as population in all the districts of all the
states in India. We have defined a small village
as a village with population of less than 1000.
Our hypothesis is that these small settlements,
barring a few exceptions, are by and large, inacces
sible. We have calculated two indices : (1
Population Accessibility Index (PAI); (2) Village
Accessibility Index (VAI).
According to the 1977 Economic Census, in
Kerala 96,3 per cent of the villages had a primary
School right in the village. The comparable
figure for Bihar was 60.0 per cent; for Madhya
Pradesh 65.5 per cent; for Rajasthan 55.8 per
cent; and for UP 45.5 per cent.
If, in a district, the population of villages in
categrories I to III (i.e. less than 1000) is more
than 50 per cent of the total population of the
district, the district will be designated as a low
population accessibility district. Similarly, if in a
district more than 50 per cent of the villages are
In the case of middle schools, the position was
as follows: in Kerala 92.3 per cent of the villages
had a middle school located in the village. The
comparable figure for Bihar was 14.5 per cent;
for Madhya Pradesh 10.5 per cent; for Rajasthan
14.6 per cent and for UP 9.3 per cent.
2
e
e
e
e
e
e
e
c
c
c
V
c
GJ
G
Ci
€■
C
C
V
* •
-J
j4
J
. J
in the categories I to III (i.e. less than 1 000 popula
tion) then the district will be designated as a
low village accessibility district.
TABLE 2 : Jhunjhunun District
Population
range
1981
We shall present a few figures here. In India
as a whole, our Population accessibility Index
(PAI) was 60. In Kerala it was 98; in Bihar 59;
in Madhya Pradesh 47; in Rajasthan 55; and in
UP 55.
As regards the village accessibility index (VAI),
the figure was 38 for India. It was 95 for Kerala,
38 for Bihar, 34 for Madhya Pradesh, 37 for
Rajasthan, and 38 for UP.
■■
■
Mt? ^3-?,
4 O
■■ 3
■' 15
13
g
a
J5
J2?
14
J,
4 e
The average size of a village in India in 1981
was 911. It was 16,967 in Kerala; 966 in Bihar;
583 in Madhya Pradesh, 774 in Rajasthan; and
808 in Uttar Pradesh. In India as a whole, 29.8
per cent of the population was in LAP districts
(i.e. low accessibility in terms of population).
In Kerala, the figure for LAP districts was 0; in
Bihar 19.4; in Madhya Pradesh 80.0; in Rajasthan
23.1 ; and in UP 16.1,
7.5
500-1999
28.8
2000-4999
82.2
5000— and above
90.9
All rural settlements
34.1
(Contd. on p. 6)
Before we conclude, we would like to mention
that in our initial exercise ,we had assumed that
the size of the settlement had a direct relationship
with the accessibility to health services. In other
words, smaller the village, lower the accessibility
and vice-versa.
Subsequently, we found enough
support for our assumption in the District Census
Handbooks. Unfortunately, all the 1981 district
census handbooks are yet to published. How
ever, we shall quote the data from the Jhun
jhunun District of Rajasthan in support of our
contention (census of India
1981, series 18,
DCH Jhunjhunun ixiv Table 2).
An Opportunity with a Difference
Low Cost Standard Therapeutics (LOCOST),
an organization aimed at encouraging the practice
of rational therapeutics among the member: of
its large drug network requires :
1. A person to meet the drug net rk members
personally and act as a change
lent for correct
medical and pharmaceutical pjzfctices.
2. A person who likes working with scl>ool
children and is interested in promoting awafeness
about health practices among childremzdonnmuni-
We hope to do this analysis for all the districts
of India, as and when all the district census hand
books are available.
cation and writing ability in Gujarati is essential.
You could be a graduate of pharmacy, science,
medicine orarts. Those who enjoy travelling will
find this work interesting. Write to LOCOST,
Premananda Sahitya Sabha (1st Floor), opp.
Lakadi Pool, Dandya Bazar, Baroda-390001
We. shall conclude by pointing out that our
preliminary analysis shows that our primary health
care policy has not taken note of problems of
physical accessibility and logistic support which
4
Upto 499
are absolutely crucial for any strategy for health
for all by the year 2000. We would recommend
that the states should be asked to prepare district
health plans on the basis of available data and
each state should have the flexibility to devise
alternative strategies to meet the local and sub
regional requirements, keeping in mind physical
accessibility as a crucial factor. In fact, our
analysis raises serious doubts about the strategy
of multiplying sub-centres only on the basis of
population size, as spelt out in all our five year
plans.
In terms of the low accessiblity districts in
terms of villages, (LAV districts)
the overall
position was as follows: In India, 75.3 per cent
of the districts were LAV districts: The figure
for Bihar was 74.2 per cent; for Madhya Pradesh
100 per cent; for Rajasthan 92.3 per cent; and
for UP 91.1 per cent. In Kerala, the value was
zero.
-It;
j ~
3
___
Percentage of
villages with
some medical
✓ facilities available
in the village,
1981
T"'
w MO' )
? Ci'<9
1
!
(Contd. from p. 3)
It is unlikely that this strategy would succeed
in delivering health care services to rural people,
particularly in the small villages of the large states
of Bihar, Madhya Pradesh, Rajasthan and Uttar
Pradesh. Alternative models based on increasing
mobiiity rather than multiplying sub-centres should
be seriously considered, along with other criteria
for logistic support and facilities for primary health
care.
Paradoxically enough, a large population has
helped and not hindered individual rural settlements
in having access to health services because our
health policy has an inbuilt bias in favour of
population size.
Our plea is for the fullest consi
deration of physical accessibility as an important
factor in planning for primary health care. This
is an obvious point. Nevertheless, our planners
have innocently ignored it.
(The paper was presented at the seminar on
"Health for all : concept and reality" in November,
1986 organised by "The Foundation for Research
in Community Health, Bombay)
y
T
I
i
■
‘.''T
i
Form IV
(See rule 8)
I
1.
Place of Publication
New Delhi 110029
i
2.
Periodicity of its publi
cation
Monthly
■ f
3.
Printer's Name
(Whether citizen of India?)
Address
Publisher’s Name
(Whether citizen of India ?)
Address
Sathyamala
5. Editor’s Name
(Whether citizen of India ?)
Sathyamala
Yes
as above.
6. Name and address of indi
viduals who own the news
paper and partners orshare
holders holding more than
one percent of the total
Medico Friend Circle Bulletin
Trust 50 LIC Quarters
University Road, Pune-
4.
capital.
6
Sathyamala
Yes
B-7/88/1, Safdarjung Enclave
New Delhi-110029
Yes
as above.
411016
■''F
s
f'<
I
1/I
1
■
STEP BY STEP
Towards An Appropriate Medical Education
»
“1 'Strategies
The CHC/CMAI/CHAI/CMC-L Project on
Community
Orientation
for Social Relevance and
Building
on
the Indian
in Medical Education
involvement
based
on
a
long
Experience’
was
how
researchers
in
exploring
of the primary
be
made
more
relevant
COUld
medical education
many
to the needs of society, These included
CHC,
formation
of
initiatives before the
during
CHC
’
s
formative
years.
followed by some
This report therefore brings together the key
researchers
initiatives/reflections of the
which
preceded the study and helped to give
the project greater focus.
CONTENT LIST
INTRODUCTION
A.
TOWARDS AN APPROPRIATE MEDICAL EDUCATION - STEP BY STEP
B.
REFLECTIONS OF AN INTERN (1972)
C.
TRAINING DOCTORS FOR COMMUNITY HEALTH SERVICES (1973)
D.
LESSONS FROM A YEAR OF TRAVEL AND REFLECTION (1982)
E. MOVING BEYOND THE TEACHING HOSPITAL (1988)
F. MEDICAL EDUCATION
TOWARDS GREATER SOCIAL RELEVANCE (1989)
G. AN ALTERNATIVE VISION OF EDUCATION FOR
CARE (1990)
DECENTRALISED
HEALTH
APPENDICES
I
FEEDBACK FROM PIONEERS OF A RURAL BOND SCHEME (198U)
II
MEMORANDUM ON A HEALTH UNIVERSITY TO GOVERNMENT OF KARNATAKA
(1988)
III
'PROS* AND 'CONS’ FOR AN ALTERNATIVE MEDICAL COLLEGE (1989)
IV
MFC ANTHOLOGY HANDOUT.
COMMUNITY HEALTH CELL.
Society For Community Health Awareness. Research And Action,
326, V Main. I Block,
Koramangala,
BANGALORE 560 034.
(J s
JU
0
0
'J
3
0
-3
0
Ji
23
JI
JI
2
43
4 o
4 0
4 0
.3 v
3 0
1 0
1 0
J o
1 o
J o
j
0
J o
J c
J 0
0
J
J Q
J Zi
J o
3
J o
J
J
J A
J
J
J
J
J ,
J
J
i
i
I
/A
Pricing the Medical Care in Government Hospitals:
Problem and Alternative Solution
Abhay Bang and Rani Bang
The government of Maharashtra has intro
duced fee for medical care in all district hospi
tals and medical colleges hospitals from Feb
ruary 88. The patients have to pay Rs 2 for
outdoor card, Rs. 10 for urine, blood or sputum
examination, Rs. 20 for X'ray, Rs. 30 for ECG,
Rs. 5 per day as the bed charges for indoor
admission and Rs. 150 for a major operation.
This is not simple 'fee rise' as stated by the government because earlier there were no charges
to most of the patients for any service in these
institutions except 10 paise for ORD card. Hence
all other charges are a new category of tax and
the outdoor card fee is raised by 2000 percent.
What is the effect ?
As we see
<
from the small district town of
Gadchiroli, the patient
*
•
-attendance
in the district hospital has suddenly decreased.
• The middie class is turning to private practitione
. --------- ..ors while
the poor patients are avoiding to go to the hos
pital or are refusing to get admitted or treated
even when they are found to be suffering from
serious diseases. "We can't pay for the treat
ment" is their plea. Government has announced
that 40% of the patients shall be treated free,
but this is left to the discretio
n of hospital authorities. Can a Civil C
Surgeon every day decide who
should be treated free from the daily crowd of
300 to 500 patients? The (
experience of anti
poverty programmes suggests
■ that the benefits
selectively meant to be- for the
r~- usually don't
...o poor
reach them. So most of the poor
' are not likely
to receive the benefit of free service.
This decision of the government of Maharashtra in principle means that the State is no
longer willing to shoulder the responsibility
of free medical care to the needy as public
service. If this sets up a trend, people especially
the poor, may increasingly lose the
- »..J benefits
of free medical care, education or even police
protection as their rights. Our country is committed to 'Health for All by the yea r 2000/ This
is something beyond the ability of the govern
ment to deliver because health depends on food,
income, education, housing, water supply and
health care—basic amenities which the govern
ment can not provide to the poor people in the
near future. But the government can at least
meet the goal of 'Health care for all." Mahara
shtra was nearing this commendable goal when
this decision suddenly came from the blue and
deprived the State of the honour. The public
feeling can be judged from the fact that on our
appeal 1500 persons from 70 villages of this
tribal district came to sign a memorandum and
two MLAs agreed to take this to the state government.
The Prime Minister is repeatedly expressing
his expectation that the public sector units
should generate profit. Everybody thought that
this applied to the public sector companies in
volved in production or economic endeavours.
But the state government seems to be apply
ing this to the public services like health care
as well. Is it necessary?
The two arguments often
put forward in
justifying the introduction of this fee structure
are:
1
|l
I
1
■— These hospitals ?•
are meant to be referral
hospitals, but they/ are unnecessarily
i--------- ---------- ■■
crowded by patients with minor problems
------ j who
come mainly to get injections.
- The cost of medical care is increasing very
fast so the government must try to meet
the two ends.
11
While there is some truth in both these points
the solution of charging a fee creates a still
bigger problem. By charging the patients, the
government has succeeded in reducing the num
ber of patients, but not the 'unnecessary' ones.
The poor anyway don't attend the hospital for
minor problems because they can't afford to
lose the wages. The new criterion of elimina
tion is not the seriousness of need for medical
help but ability to pay. This means that now the
government medical care is selectively for those
who can pay and not for those who are in
need. This is essentially same as the private sec
tor medical care. To crown the similarity, the
proportion of 40% free service offered by the
government is the same as one proposed by the
Director of Apollo hospital in his proposal for
new commercial hospital in New Delhi.
■ »•
'•
1
5
i. 1
to
I
lyp
Let us suggest some ways of meeting the '
above mentioned problems of unnecessary pa
tients coming for free injections and of increas
ing costs of medical care.
W
ll
■f
■4
•i
i
Ij u!
i
4
I
I II i
r;
Gadchiroli has a small Government district
hospital of 30 beds. A study of the outdoor pa
tient attendance in the district hospital done by
our institution SEARCH, showed that 36%
of the outdoor patients were getting one or
other injections. Out of these injections, 60%
were unnecessary just going by the categories
of medicines injected. These werei njections
Terramycin, B' complex, Bj B6 Bi2 Chloroquin,
Wymesone, Diazepam etc. All these medicines
are equally well absorbed when given by mouth.
Actually Terramycin is difficult to give in thera
peutic dose of 250 mg every 6 hourly in ORD.
The usual dose of 2 ml (100 mg) once a day
is ineffective.
Injection Bj B6 B12 can some
times lead to fatal reaction. Thus it is unneces
sary and undesirable to give these medicines
in injection forms in outdoor. These injections
are justified only when the patient is uncon
scious or too ill that S/he can not take medi
cines orally—situations when patient should be
admitted and not treated in outdoor.
After discussing these findings with the Di. rector of health services. Civil Surgeon, and the
doctors in the hospital, it was decided by all
that the 8 unnecessary categories of medicines
in injection forms will not be kept in outdoor
and the doctors shall not prescribe unnecessary
injections. These medicines in oral forms and
other necessary injections supply was ensured.
The effect of these measures was as follows.
f
(2)
Saved time of the patiems, doctors and
nurses spent in giving injections
(3)
Saved medicines
(4)
Reduced outdoor attendance by 11%
by eliminating those who were unneces
sarily coming to hospital only for injec
tions.
After
Redu
ction
307
273
11 %
(2) Daily number of injec
111
tions
54
51 %
(3) Proportion of patients
receiving injections
36 %
20 %
45%
(4) Proportion of unneces
sary injections
60 %
2 %
■.J
I
(1) Daily
number of
patients in ORD
1
c B
Another study done by search showed the fol
lowing pattern of use of antibiotics and antiparasitic agents in the patients admitted in the
wards.
Out of all admitted patients 16%
were given no antibiotic antiparasitic medicines,
20% were given these medicines for sound rea
sons and 64% were given these medicines un
necessarily or excessively or wrong, for which
many reasons could be found. Urgency of the
situation or lack of bacteriology facilities were
responsible for such use in some cases but in
majority (two third) of such instances the cause
was lack of knowledge or wrong prescription
habits of doctors. Again let us emphasise that this
problem is everywhere and not specific to Gad-
El
This suggests that if retraining is provided to
doctors to upgrade their knowledge about ratio
nal use of antibiotics or change their prescription
habits, a tremendous cut can be made in the un
necessary use of costly medicines, besides sa
ving patients from side effects and nurses from
work load. Lot of hospital costs can be thus re
I
’■
r
e E
c
Ee
e . . IE
;; -
eI
e..J
e -1
e-E
duced.
The purpose in describing these studies here
is to show that some of the factors responsible
for increasing cost of medical care in the govern
ments hospitals can be corrected. In order to
make two ends meet, the government should
introduce retraining of doctors in rational therapy
and prescription audit. Charging the patients for
medical care and thereby depriving the poor and
needy is neither necessary nor desirable.
96%
This one single measure and the self discipline
by the doctors had the following results
(D
G^'
Daily 56 injections meaning 17000 injections
in an year could be avoided. If the cost of one
injection is considered to be Rs. 3 (medicine,
syringes, needles, boiling, doctor's and nurse's
time) net 50,000 Rs. could be saved per year in
a small 30 beded hospital. Moreover, patients
were reduced by 11% which further saved time
and money of the hospital and of the patients.
Anybody who knows the prescription pattern in
the medical colleges or district hospitals else
where would agree that this pattern of unneces
sary injections is similar everywhere.
chiroli.
Before
G
G-iS
r
Saved patients from the side effects of
unnecessary medicines
6
e
c ;
c:
eI
e ■
eJ
e®
cI
■-
medico friend
148 circle
bulletin
I
<
i
February 1989
v)
The Indo-US Vaccine Action Programme :
A Recipe For Disaster
PRAFIjL BIDWAI
Following public criticism, the Government
of India has appointed a high-powered committee
to scrutinize the trials of vaccines to be produced
and imported under the Indo-US Vaccine Action
Programme (VAP). Dr. AS Paintai, director-general
of the Indian Council of Medical Research, who
heads the committee, has meanwhile been quoted
as saying that he will not allow any vaccines to be
tested in India which have not already undergone
trials on human subjects in the United States of
America.
It this assurance is rigorously translated in to
practice, then the VAP will lose its relevance at least
for one of the two parties which signed the agree
ment, namely the USA. There is little doubt that
under the VAP India is to be used as a vest, cheap,
and poorly regulated laboratory in which to con
duct trials of new vaccines on Indians. It is difficult
to imagine that any other considerations, including
benevolent charity and philanthropy, which may
have guided the American government in sponsoring
the VAP will subsist if vaccine trials are indeed tig
htly regulated in India.
This is exactly as it should be. For, without
doubt the VAP is one of the most ill-conceived,
potentially hazardous and environmentally malign
projects ever signed and underwritten by the Go
vernment of India.
The VAP agreement is open to question on
numerous grounds, including the perverted view it
takes of the health priorities of the majority of the
Indian population. To put it simply, the VAP emp
phasizes vaccines as miraculous substances—,
magic wand with which to do away with an amazing
range of diseases and ailments, from malaria to
dysentery. Vaccines do have a place in any compre
hensive health plan. Butthat place is necessarily
limited largely because of problems of distributionfrequent breaks in the cold chain, inadequate cover
age of susceptible populations, loss of effectiveness
of vaccines against specific pathogens and the ada
ptability of and mutation among such pathogens
leading to resistance.
The only successful example of effective
large-scale inoculation that the world, and in par
ticular India, knows of is the smallpox vaccine. Its
success is attributed to a number of features that
are unique to the disease and its pathogen. The
ease with which the disease can be identified by
ordinary people, the mode of transmission of the
virus (solely through physical contact, as distinct
I
water or through air), the possibility of sealing off
susceptible pockets from the rest of the population,
the handsome incentives offered for reporting a sma
llpox case, and the vigour with which the WHO
launched its campaign against the disease, all contri
buted to the success. It would be pure arrogance to
assume that such conditions can be replicated in
respect of most other diseases included in the VAP
list.
The VAP, then, is part of a search for 'techno
logy fixes'for health problems that are mo.-e app
ropriately tackled through better sanitation, improved
nutrition and the supply of clean drinking water. Like
all such 'technology fixes' imported from the affluent
West, the VAP too will be an artificial transplant that
is likely to undermine indigenous efforts at develo
ping solutions to the health problems of the Indian
people. Little wonder, then, that the programme has
only been supported by those who have a stake in
perpetuating a relationship of dependence on the
West.
The following are some serious objections
that can be levelled against the VAP agreement :
First, the agreement is 'intended to develop
vaccines to expand the range of diseases that can be
prevented by immunization and to develop accurate,
inexpensive diagnostic techniques for use in the he
alth care system
This contradicts the claims of the
Department of Biotechnology (DBT) that 'no R and
D work would be undertaken on any communicable
diseases other than those which are already prevalant in the country as major diseases'. Under the
agreement, it would become possible to develop
vaccines even for new diseases, for example AIDS.
Secondly, the VAP is an unequal agreement
insofar as the effective formulation control and exe
cution of the project is concerned The USA has
pledged dollar 7.6 million dollar 6 million through
the Agency for International Development (AID) and
the rest through the U. S. public health service. The
Government of India is committed to spending dollar
2 million to take care of the domestic costs. The
fine-print clauses of the project agreement are riddled
with conditions and convenants that favour the USA.
For instance, all documents, plan specification, con
tracts, schedules, other arrangements,' 'with any
modifications therein' must be approved by AID.
(Sec. B. 2 of Annexure 2 to the Project Grant Agree
ment) And 'goods and services financed under the
grant...will not be used to promote or assist a for
eign AID project and activity associated with or
financed by a country not included in code 935 of
the AID geographic code' (B.4).
AID officials will have the right and oppor
tunity to inspect the project and all the books and
records pertaining to it (B.5). Further, all goods to
be transported to India must be shipped by AIDapproved air or ocean carriers to qualify for grant
finance; carriers of a country not included in Code
935 are debarred. Besides, at least 50 per cent of all
shipments must be carried under the U. S. flag. Many
such restrictions occur.
Thirdly, the project provides for a wide range
of vaccine trials—'bench, clinical and field research
to develop new and improved vaccines' (Annexure
1, P. 2) This makes it explicit that the primary pur
pose of the project is to allow an extended range of
trials on numerous subjects, from laboratory animals
to human subjects in the field. Although the priority
areas have been identified as 'cholera, typhoid fever,
rotavirus, hepatitis, dysentery, rabies, pertussis, pne
umonia and malaria,' these 'could change in succ
eeding years of the project as other areas of research
opportunity are identified.'
Fourthly, the project provides for a joint
working group and an environmental review commi
ttee consisting of equal numbers of 'experts
jointly selected' by the DBT and the U. S. govern
ment, through AID and the U. S. public health ser
vice. This will look into the environmental impactpotentially risky
or
dangerous—of
particular
research proposals. Thus, Indian scientist will not
be able to implement research programmes without
American approval. The review of research and tes
ting programmes in respect of particular vaccines
will also be subject to U. S. approval. Even in case
of adverse environmental impact, there is no guara
nty that Indian opinion will prevail.
Fifthly, the project agreement emphasizes the
involvement of both the public and private sectors
in India and the U. S. Given the great disparity bet
ween these in the two countries—most biotechno
logy research and production in the U. S. is in the
private corporate sector, while such activity in India
is mostly in the public sector-the emphasis opens
the way for U. S. private companies' entry into the
arena of field trials. This is indeed the critical
part of the VAP, as will be detailed below.
2
i
Sixthly, the Memorandum of Understanding
(MOU) explicitly states that 'both governments
acknowledge the importance of the protection of
the human subjects in any medical programme'
(Article V) and that 'some of the medical research
will involve recombinant DNA technology', i. e.
methods of gene-splicing or genetic engineering.
The emphasis is thus clearly on developing bioen
gineered vaccines for human iseases
This is a high-risk area where vaccines may
have unpredictably harmful consequences. Indeedit is precisely because the risk has been acknowle
dged that many countries in the West, including the
USA, have had to evolve regulations on recombi
nant DMA research through prolonged debates and
public hearings lasting years.
I
Article VII of the MOU states boldly: Both
countries have similar regulations governing the
conduct of recombinant DNA research', This is sim
ply untrue. The USA does have such regulations.
India does not. A DBT official confirms that 'only
environmental laws of a general nature exist as of
now, although a high powered committee has been
set up to evolve a code'. Thus, the assurance that
all genetic engineering research ‘will be carried
out in accordance with the laws and regulations of
the country in which the research is conducted' is
meaningless.
t
And finally, the VAP accomplishes in one full
swoop what the pro-Paris Convention lobby has not
been able to do to the Indian patent protection
system despite years of efforts. Article VII of the
MOU says: 'It is recognized that the work carried
out under the VAP may produce patentable result
and in the publication of the scientific findings. In
order to assure that the rights of both countries are
protected, an accord on intellectual property, copy
rights, and patent provisions will be developed and
agreed upon within ninety days of signing of this
MOU, and will be appended as Annexure 2/
What it implies is not only that the protection
provided by the Indian Patents Act of 1970 will be
destroyed and replaced by a strong U. S. style sys
tem of patent protection which is heavily biased in
favour of the developed countries, but also that
organisms and life-forms engineered with the use
of biotechnology will possibly be allowed to be
patented. Incidentally, a recent move in the USA to
allow such patenting has opened up a Pandora's
3
box. The e’hical problems involved in the patenting
of life are too obvious to need comment.
The Indian government's assurance that the
Patents Act will not be ettisoned or bypassed is at
variance with Article VI of the MOU. This represents
a major policy shift in the Government of India's
position. The official Indian position has been that
only processes and not products should be patented
and those too for a limited length of time and con
ditionally. By allowing patents to be taken out on
bio-engineered life-forms, it will make nonsense of
the notion of limited protection of intellectual pro
perty..
If India signs a special 'accord' under Article
VII on patent protection for vaccines or bio-engi
neered products, its entire opposition to the Paris
Convention as an unequal, anachronistic and dis
criminatory treaty and the very basis of its resista
nce to Western pressures to accede to it, will be
seriously undermined. That this should be a pro
minent article in the MOU speaks for itself.
The confidence with which the DBT commi
tted itself to such an 'accord' within three months—
when the revision and repeal of the old colonial
patent law took several years—is equally remarkable.
It is far from clear, however, if it had the Union
Cabinet's sanction for bringing about a major policy
change to the detriment of the country.
Equally significant Article V of the MOU sti
pulates the appending of'Annexure 1' containing
a joint 'Assurance of Protection of the Rights and
Welfare of Human Subjects of Research in the IndoU. S. Vaccine Action Programme.' This annexure is
to be mutually agreed upon within ninety days of
the signing of this MOU'. Until it is signed and
appended, no research activities involving human
subjects can be conducted. As matters stand today,
neither annexure has been signed although the dea
dline is long past.
All this sounds innocuous, as does the assu
rance that laws and regulations in force in both the
countries would be taken into account while draf
ting Annexure i. However, the article seriously
compromises India's exclusive and sovereign right
to decide on the norms for the protection of human
subjects in this country and to draw up a code or
protocols for vaccine tests on them. For the article
says that Annexure 1 will be 'negotiated and sig
ned' by India and the USA.
The very existence of the term 'negotiate' in
field trials on vaccines in other countries, so as to
respect of what cannot be open to negotiation is a
bypass the U. S. regulatory system altogether. They
serious assault on India's sovereignty in respect of
her o/vn citizens'safety. The article grants an alien
have decided, to quote Dr Alan R. Goldhammer, a
director of the Industrial Biotechnology Association
country and government, that of the USA, a role in
of the USA, a representative industry body, that the
negotiating what constitutes adequate 'protection
pathway may be clearer in foreign nations to gett
of the rights and welfare of human subjects' in
ing approval’ (New York times, 13 Nov. 1986).
India.
Officials of the U. S. National Science Foun
It seems that the objective is to open India
dation concur: 'We may be overregulating and pu
to U. S. biotechnology corporations and institutes
shing companies to test their products overseas'.
and turn it into one vast laboratory where all man
While most U. S environmentalists disagree on the
ner of vaccines can be tested without regulation,
first part of the proposition and argue for stricter
let or hindrance.
regulation, no one questions that U. S
I
companies
are increasingly going abroad, or planning to do so.
That objective has a significant history. In
1986 the Wistar Institute of Philadelphia, a private
firm, tested a bio-engineered rabies vaccine on Ar
After the Argentinian furore over Wistar, it
was probably thought wiser to enter into formal
gentine cattle without even bothering to let that
agreements with Third World governments which
country's authorities know that it was doing so.
Wistar was patently unethical in doing what it did.
have weak or no regulation on bio-engmeered pro
It failed to isolate the inoculated animals, to place
ducts and their testing. The MOU signed with India
is evidently one such agreement.
warning signals at the research station, to vaccinate
four animal handlers against possible diseases from
The Wistar case has not been forgotten. In
the cattle under the trials, and to prevent them
deed, in a 59 page 'project paper' prepared last year
from drinking milk from the latter.
by the U. S. government, which was the starting
point for the VAP agreement with India, Wistar is
The Wistar case, about which disclosures we
re made in September 1986, three months after the
trial, evoked a strong protest not only from Buenos
specifically mentioned as an outstanding example
(p,20): ‘Rotavirus is the most common cause of
Aires but also from American scientists. So did an
diarrhoea in infants, and is the mo^t common cause
of death among the diarrhoeal diseases in this most
other instance, that of Oregon State University re
vulnerable age-group. Immunization offers the only
searchers testing a gene altered animal vaccine in
New Zealand, also in 1986, although in this case
the trial had been approved by Auckland. Yet ano
prospect for prevention of this disease, and several
vaccines developed at the NIH and a less attenuated
bovine vaccine developed at the Wistar Institute.
ther controversy has involved the iceminus bacteria,
Field trials and other research related to rotavirus
or Pseudomonas syringae, genetically engineered by
vaccines will be eligible under the project.' The
Advanced Genetic Sciences, Inc., which was illega
singular, indeed unique, treatment accorded to Wis
lly field-tested on strawberries.
tar speaks for itself.
The debate that;has followed the Wistar sca
ndal reveals that several U. S. biotechnology cor
porations and laboratories, now under economic
pressure to put their products on the market and
earn an income, have drawn up plans to conduct
But what does India stand to lose if USAmade bioengineered vaccines are field-tested here?
It is impossible to predict the biological and envi
ronmental consequences of a vaccine trial: it might
4
i
not produce immunization and yet its release could
visit devastation upon life-forms and life-support
systems, indeed the whole environment.
To quote Jack Doyle of the Environmenta1
i
*
Policy Institute in the USA: 'The ability to predict
what might happen with genetically engineered
organisms will have to build on what's known ab
out the ecology of existing organisms. But that is
not much In today's agricultural environment, there
are at least 1 60 species of bacteria; 250 kinds of
viruses; 8000 species of insects; and 2000 species
of weeds. But some scientists estimate that as many
as 80 per cent of our soil microbes have yet to be
cultured, and perhaps as many as 90 percent do
not have names. [These numbers are probably se
veral times higher in India—PB.] Of those that are
named, we do not know much about their relation
ship to other microbes. How organisms such as
these establish themselves, why some species mul
tiply in nature and others do not is still largely a
mystery . .
...Once a recombinant population is establi
shed, it can be expected to evolve in ways benefi
cial to its own survival. And that could increase its
undesirable effects as well, if it turns out it has
those along the way. Remember that there is no
recall of living organisms'.
<
Dr Martin Alexander of Cornell, who acted
as a consultant to the U. S. Environmental Protec
tion Agency on a major risk assessment project, has
testified: 'Alien organisms that are inadvertently or
deliberately introduced in natural environments may
survive, may grow, may find a susceptible host or
other environment, and may do harm I believe the
probability of all these events accurring is small,
but I feel it is likely that the consequences would
be enormous.
I
It is Jhe enormity of such consequences
that should be the basic criterion for deciding
whether to go in for a project like VAP. The ethi
cal considerations involved are too weighty to
be brushed aside. Enlightened opinion in the USA
on the issue was best summed up in a New York
Times editorial apropos the Wistar case: 'It is at the
very least a poor way to do science, let alone win
friends.'
But such opinions do not seem to have in
fluenced the Reagan administration in formulating
what the MOU terms the 'Reagan-Gandhi science
and technology initiative'. What has influenced the
Indian department of biotechnology into signing
the VAP agreement remains a mystery. It is clear
that the project should be scrapped forthwith.
Courtsey : The National Medical Journal oj IndiaVolume i3 Number i3 1988.
® ®
Dear Friend,
For the past six months we have been cons
tantly telling people that there is research going on
in North Arcot District regarding KPV (Killed polio
vaccine), a product of two companies: INSTITUT
MERIEUX (which produces an improved salk vac
cine) and CONNAUGHT LABORATORIES (Canada).
We have been drawing attention to the fact
that most of the Measles vaccine and distilled wa
ter supplied under the POLIO PLUS programme of
Rotary International have been made by the same
CONNAUGHT
LABORATORIES
and INSTITUT
MERIEUX.
Now comes the startling revealation that INSTITUT MERIUEX is one of the four partners in the
Rs. 100 crore project to be set up under the IndiaFrance agreement. This pact will be signed in the
first week of February. 75 crore rupees will be in
vested by Indian sources (Public, Government and
IPCL).
Does the medical & scientific community at
large have any idea whether we are buying OPV or
KPV technology : let alone other details of the agree
ment? Why not? OPV technology is available free
from WHO.
Is the cold chain of OPV a problem that we
can surmount by producing KPV ? What about the
cold chain requirements of Rabies vaccine, of Anti
snake venom and even of the Merieux Measles vac
cine ? Shouldn't we spend the same money develo
ping solar powered refrigeration instead?
And can measles deaths be prevented by the
vaccine only ? Wellnourished children do not die
of measles. Malnourished children die without mea
sles I
PRABIR
5
-
k
t •
■ike
7 TV vw
____
V\
\
Chloroquin, Cholera And MFC'v’
Some of the health-strategies of the Govt of
India were criticized at the 15th annua; meet of the
Medico-Friend Circle at Alwaye. The MFC meet
concluded that the strategy of giving four tablets of
chloroquin to every case of fever is a wrong stra
tegy. It was a part of the strategy of the National
Malaria Eradication Programme, where in it was
necessary that every case of fever had to be taken
as that of malaria and had to be presumptively treated with chloroquin to help stop the transmission of
malaria. But now, the eradication strategy has been
given up; the aim has been lowered to that of mala
ria control. In such a situation there is no need to
suppress each and every case of Malaria by blindly
adminitering chlonoquin.
Secondly, now the cadre of the village health
guides has been created and one VHG is available
per thousand population. These VHG's can distin
guish between fever due to upper respiratary tract
infection from malaria fever. There is therefore no
need to blindly administer chloroquin to all cases
of fever.
The current strategy not only necessarily was
tes tonnes of choloroquin but also helps to create
resistant strains of malarial parasites, because in
practice, most cases of falciparum malaria get inade
quate treatment with only 4 tablets of chloroquin.
The MFC meeting also concluded that cho
lera vaccine should no longer be used either in
epidemic situations or for routine immunization
programmes.
This recommendation is based on the follow
ing conclusions: a) the cholera vaccine that is pre
sently in use is not efficacious in preventing the
spread of cholera epidemics. Transmission of patho
genic organisms is not reduced, b) The number of
attacks of clinical cholera occuring in young child
ren is not reduced as a consequence of cholera
vaccine inoculation. While the number of attacks of
Editorial Commitree :
Anil Patel
Abhay Bang
Dhruv Mankad
Kamala S. Jayarao
Padma Prakash
Vimal Balasubrahmanyan
Sathyamala, Editor
R.N. 27565/76
• /-i
k
v onolera
O occuring in adults is reduced between 3050%, their severity is not reduced, c) Even above
results are obtained only with good quality vac
cine. However it is well known that cholera vaccine
produced in India and available in Government stock
is generally of poor quality and is poorly maintained.
Moreover this level of protection lasts only for app
roximately 3 to 6 months, d) In the field situationa
it is our regular experience that ordinary standards
of asepsis and sterilization are rot maintained. The
risk of spreading diseases such as hepatitis, AIDS
and syphlilis through needle is indeed real, as is
the risk of local abscesses.
1
*
Keeping in mind the grossly unrewarding
cost-benefit ratio of performing large scale inocu
lation under such condition, we feel cholera in
oculation is not worth while; moreover it exposes
those being vaccinated to unacceptable harzards*
In this context it may be noted that similar recom
mendations have been made by WHO, DGHS and
ICMR. Alternative measures are available for inter
national travel.
Existing stocks of currently availab'e vaccine
should be destroyed and the production of such a
useless vaccine should be discontinued. Briefly fo
llowing measures are recommended by the MFC to
prevent and control cholera/gastro enteritis: a)
Longterm: Wide spread availability of safe and po
table drinking water supply. Popularisation of scien
tific and appropriate measures for sanitation and
excreta disposal, b) Short term and During Epide
mics—Hyperchlorination of water supply up to 6-7
ppm.
of chlorine at source. Where
these
measures are not possible or feasible people
should be advised to boil their drinking water.
However it should be noted that practically it is
difficult for people to do this regularly. It is only a
measure of last resort. And lastly the efficacy of ORT
should be widely popularised and every effort made
to give it currency. People should be convinced that
ORT is the first and best treatment for the gastroentritis/cholera complex.
Views and opinions expressed in the bulletin are those of .the authors and not necessarily of the organization.
Annual Subscription—Inland Rs. 20.00
Foreign: Sea Mail US 4 dollars for all countries.
Air Mai': Asia—US 6 dollars Africa & Europe Canada & USA—US 11 dollars
Edited by Sathyamala, B-7/88/1, Safdarjung Enclave, New Delhi 110029
Published by Ulhas Jajoo & S. P. Kalantri for Medico Friend Circle Bulletin Trust, 50 LIC quarter
Unive.sity Road, Pune 411016
Printed at Samyayog Mudranalaya, Wardha
Conespondence and Subscriptions to be sent to UN Jajoo, Bajajwadi, Wardha. 442001
>
1
a
I
A
127
medico friend
circle
bulletin
APRIL 1987
Media as a Tool in Health Action
Vimal Balasubrahmanyan
Can the general mass media be used by the rational
health movement to influence people’s attitude, under
standing and behaviour on health matters ? As one
who has been writing on health issues in various
newspapers and journals, I feel this is a topic which
needs to be thought about seriously by activists in the
movement. People at large can understand the
deeper aspects of the politics of health only if they
have exposure to adequate information and analysis
on the subject—the sort of information confined
at present within the ‘alternative media’ of health
activists and progressive social scientists, and circula
ting therefore mainly among the ‘already converted’.
4>
4
Although in recent years there has been more
coverage in the mass media on specific health issues,
like harmful drugs, there has been little enlightenment
of the public on what health-for-all really means,
what people must do to change their own outlook
and lifestyle, or what kind of economic and social
measures are needed to be implemented as part of
health policy. The public sill equates health-for-all
with sophisticated medical-care-for-all. which in
turn is equated with costly diagnostic facilities,
surgical procedures and ‘technologised’ medicine.
In the public mind, the low health status of the people
is a result of inadequate medical facilities and hence
the clamour for more doctors, more hospitals and
more CAT-Scan units.
The serious progressive journals which comment
on these issues have an extremely limited, intellectual
and academic readership. So, the question facing the
health movement is: can a sustained consciousness
raising campaign be directed towards the lay public,
using the mass media as one of the tools?
One must begin by acknowledging that this kind
of health education must necessarily explode a lot of
myths and this will inevitably mean that powerful
vested interests are not going to like it one bit. To be
credible and convincing to the public, this task should
not therefore be left to journalists alone, for two rea
sons.
(a) General articles on health issues (as opposed to
reportage on, say, harmful drugs, which has both
news value and sensation value) carry greater convic
tion when the information and advice comes from
qualified health personnel. Readers are far more
receptive to health advice from a column whose by
line is a ‘Doctor Somebody’.
(b) The medical profession is itself hostile when a
non-medical person exposes malpractices in the area
of health care. Health columns which seek to en
lighten the public on the politics of health will nece
ssarily tread on Establishment’s toes. And when
such articles are attacked by qualified and senior
medical personnel, often with fancy designations, the
public doesn’t know whom to believe, the doctor or
the journalist.
On the basis of some of my experiences while
writing on health issues, I would like to offer some
ideas on how the mass media can be used by the health
movement and those sympathetic to it, to further the
cause:
1. Health activists, especially those with medi
cal degrees and designations, must acquire media
skills, establish contact with editors, and introduce
regular health columns in the print media. The help
and guidance of sympathetic media people can be
*
enlisted to ensure that these columns are written in
appropriate language and style (Dr P.K. Sarkar’s
column on Harmful Drugs in the Calcutta Telegra;h,
and LOCOST’s Education Service published in the
Sunday Express magazine are examples of the kind of
initiative needed).
2. Constant and tactical use of letters-to-theeditor columns should be made to: initiate debates;
get across information on crucial issues; and refute
distorted information planted in the media by vested
interests. (See example of ORT narrated later in
this article).
3. Qualified medical people, especially those iin
high positions, who may not be ‘activists’ but are
progressive in outlook, should come out on vocal
support of any campaign launched by activist groups.
This could be in the form of a formal statement issued
as a press release or just a letter to the
editor. Such endorsement greatly enhances the
credibility of the campaign in public eyes. For
example, media coverage on the rational drug policy
campaign helped in creating some public awareness
and even succeeded in getting government’s pro
industry proposals stalled for several months. But
the movement would have been more successful if
the ‘eminent’ members of the various government
appointed committees, which have in the past called
for an essential drugs policy, had realised the need to
issue statements supporting the demands of the All
India Drug Action Network.
people. For example, a critique of cholera vaccina
tion programmes should be timed to coincide with
the drought or flood situation when such pi ogrammes
are usually conducted.
7. If an issue needs coverage in the press, a suitable
and timely write-up should be released to the media
and this statment should be short, straightaway men
tioning the highlights in the first two paragraphs.
A long research type report, often polemical in langu
age, may be all right for publishing in the alternative
media, but very difficult for use in the general media.
It is my impression that health activists do not fully
realise this and are often disappointed when reports
they send to the press don’t get published.
8. The media has to be consciously used by the
movement in as dynamic a manner as it is currently
being used by the Establishment and Industry. The
PR departments of the drug firms work overtime to
present a favourable picture of the industry and its
products and the public swallows it all. When a
harmful drug gets a great deal of adverse publicity,
the industry manages to get spokesmen from the
medical profession to defend its product and such
statements are reported prominently with big head
ings—leaving the public thoroughly confused as
to who is right. Unless these statments are swiftly
challenged and refuted, the public will only get dis
torted information. And this kind of counteraction
can only be effective if the health movement main
tains the same kind of contact with the media which
4. Health activists must feed information more the industry does, and demands the same kind of
effectively to committed journalists so that timely coverage and space which the industry is at present
coverage of important issues is ensured. The health getting.
movement should actively seek out and identify sym
pathetic media people and keep up a steady flow of
9. The potential of radio and television in serving
information to these contracts so that consistent the cause of the health movement remains almost
media coverage on health matters is maintained.
totally untapped. Some recent programmes on
television indicate that immense possibilities exist.
We are so obsessed with the notion that radio and
television, being government controlled, are not
‘free’ that we have overlooked the fact that it is preci
sely because they are government controlled that they
have a good potential to serve our purpose. The
government, at least on paper, is committed to all
kinds of radical ideals, and so it should be possible
for the health movement to demand time on these
media for health education of the public. Talks,
interviews, features, even serials could be planned,
with the help of sympathetic and progressive producers
on these media to get across information and messages.
Since the initiative to do all this won’t come from the
government, it is up to the health movement to lobby
for effective use of the government media to achieve
5. It is sometimes more useful to feed information
to a news agency rather than to a staffer or a free
lancer whose report can appear in only one paper or
journal. An agency report on the other hand has the
potential to appear in a large number of papers all
over the country. For example, when the MFC
critique on painkillers was published, I realised that
any article I might write on it would only appear in
one of the weekly journals to which I contribute. So
I passed it on to a friend in PTI, persuaded him to do a
short item on it, and this subsequently appeared in
several newspapers in different parts of the country.
6. Specific health actions should be planned
and published with an eye on factors like news value
and topicality—the two holy criteria for the media
2
»•
f c vy
MR.
at least those radical goals which have been accepted
in official policy.
diate response from a Madras doctor, asserting that
doctors know best’, and defending some of the
commonly consumed irrational preparations (which
one assumes he was in the habit of prescribing). This
was immediately followed by a letter from an eminent
Madias doctor, who is well known to the readers of
the Hindu, defending the statement of his younger
colleague, and condemning the misinformed sensa
tionalism indulged in by ‘journalists and politicians’.
The fact is that the different fonns of media have
been generally thought of as areas of expertise beyond
the purview of those not specifically trained to handle
them. But activists in progressive movements must
realise that it is not difficult to learn to use the media
to serve their cuase, and for this they have to begin by
going to the media instead of waiting for the media
people to come to them.
I now stood thoroughly discredited in the eyes of
the Hindu readership, and all because I had tried to
share with them the information I had regularly been
receiving from health action groups and from no less
a source than the WHO-supported journal. Diarrhoea
Dialogue, published from London!
The ORT Example : Some points raised in this
paper may be illustrated by a recent experience.
Since the early 80s, there has been a lot of UNI
CEF-inspired coverage on ORT, which has acquired
the image of a miracle solution to Third World diarr
hoeal deaths. ORT as a phrase has become associat
ed with ‘poverty’ and ‘children’. Nowhere does the
ORT message clarify that this is a therapy for all
rich and poor, adults as well as children. Nor is the
ORT slogan accompanied by a statement to the effect
that most of the commonly used anti-diarrhoeals are
irrational and harmful. In the eyes of the middle
class newspaper reading public, even today after a
veritable media blitz on ORT, the salt-and-sugar
remedy is seen as something meant for the very poorthose who can’t afford to buy antidiarrhoeal drugs.
I realised that my own rejoinder would not carry
enough conviction unless my stand was also support
ed by doctors. I therefore sent photocopies of my
original item and of the responses of the Madras
doctors to doctors in health groups all over the
country and requested them to respond to the Hindu.
Of the 16 letters sent by the health activists, the Hindu
published about eight—all deploring the attitude of
the Madras doctors, welcoming the critique which I
had offered, quoting texts to support it, and endorsing
my statement on irrational antidiarrhoeals. Some
of the letters also used this as an occasion to explain
why a rational drugs policy alone can pievent the
consumption of harmful and unnecessary drugs, and
why it is necessary for socially conscious journalists
to inform the public on such issues. There was
absolutely no answer to any of this from the Madras
doctors, and one assumes that as far as the Hindu
readership was concerned, the point about ORT had
been adequately made in fact, more effectively pro
bably than if my original item had not raised the ire
of the Madras doctors. Because, as a result of their
intemperate response, the issue was kept alive in the
Hindu's columns for almost two months afterwards.
Although I have written about this aspect of the
OR! mystique in various serious progressive forums,
I fell it’s important to focus on it in a typical Estab
lishment paper whose readers are unlikely to have
been exposed to this understanding of the ORT issue
and who are also likely to be the kind to consume
irrational antidiarrhoeals, either self-prescribed or
prescribed by doctors who are themselves unconvinced
about ORT.
It has been my experience that both editors and
readers are suspicious of controversial health infor
mation coming from non-medical writers. So, instead
of an ‘advice’ piece, I did a short ‘news report’
based on Health Action International’s Diarrhoea
File, and this I sent to the Open Forum of the Hindu,
which declined to use my item on that page (probably
because I am not a doctor and therefore not compe
tent to write on matters medical 1) and placed it instead
in the Letters-lo-the-Edilor column. Anyway, my
purpose was served.
This little episode shows that: 1) ft is not easy to
gel radical health information into the Establishment
media; 2) Even when one ‘smuggles’ it in, there is
opposition from the medical profession itself; 3) When
a doctor contradicts a journalist on a health issue, it
is the former’s words which carry weight, regaidless
of how well-informed and scientifically sound the
latter’s argument may be: 4) In spite of these handi
caps it is still possible to save the situation and turn
it to the advantage of the movement by mounting an
oi chestrated attack on the views being propagated
by the vested interests; 5) In such a strategy, the
role oj qualified medical people is cr>
• 6) The
letters pages of the Establishment p?
>
ideal
My piece specially mentioned that many doctors
themselves do not promote ORT but prescribe irra
tional drugs. Not surprisingly, there was an imme-
•rtho1
3
forum to introduce information which may not be
readily accepted in the news columns or the features’
pages. This fact should be more consistently ex
ploited by the movement; 7) The letters pages also
need to be used swiftly to refute every kind of dis
torted information which may be aimed at misleading
the public. For example, when a sophisticated and
elitist diagnostic service displays a full page advertise
ment, using the slogan Health-For-All, and announces
that the Health minister will inaugurate the building,
a strongly worded letter-to-the editor from activist
doctors should set right the picture in public eyes:
that Health-For-All does not mean costly medical
services for the affluent, and that it is scandalous for
the Health minister to be a party to this perpetuation
of falsehood.
However, this type of alert action has so far not
come naturally to the health movement, because they
haven’t really thought about it seriously. Taking
the ORT episode for instance, many progressives
who read the Hindu may have silently criticised the
Madras doctors’ statements but did not realise that
in public interest they must sit down and write re
joinders. The activists who did write had to be
contacted and briefed, and their subsequent use of
the media to put across the viewpoint of the move
ment was part of an organised strategy. For, this
issue of using the media more actively was something
we had discussed earlier, during a conference in
December 1985 on ‘Pharmaceuticals and the Poor’.
And so, when the Hindu incident cropped up, every
one was alive to the need for swinging into action.
to
(Adapted and condensed from a background
paper. The Media, The Message and Health For All
prepared for a seminar on ‘Health for All: Concept
and Reality’, organised by the Foundation for Re
search in Community Health, Bombay, on November
15 and 16, 1986)
4
i. (» ii si • iuui; oi. u/arks Bead,
Banqalore - 560 001.
I
■!
I
1
I
medico friend
*
!
I!
I!
a
Politics of Medical Work
a?
a)
'o
o
b)
"~O
o
•"“'O
—
-o
■1’
'>0
1
11 fc
ANANT R S
To begin with, it is to be noted that any
medical work simultaneously involves and results
in three types of activities, changes.
-O
I
Part I! Radical Medical work
sa
■
9 d')
July- August 1988
c?
Economic : production, distribution and use of
medical technologies, (eg. drugs, equipments,
skills and knowledge of medical personnel in
the form of therapies).
Biotechnical changes: a tubercular lung being
converted into a non-tubercular lung; an infec
ted wound into a non-infected wound etc.
c) Cultural, ideological, political change: though
most people are not aware of it, medical work
cutomatically, inevitably breeds cultural, ideologi
cal relations
between
doctors,
paramedics,
patients and the rest of the 'healthy' populations.
For example, the concept sickness involves some
cultural
assumptions
A couple of
hundred
years ago, persons affected by schizophrenia,
(madness), were not considered to be sick but
were supposed to be possessed by evil spirits. They
were tortured and burnt alive. In India, even today
in many areas the disease of madness. Has not
acquired legitimacy i. e.f the status of sickness.
In the 19th century, the use of contraceptives was
considered immoral, worthy of prostitutes, now
no such controversy exists because of a change
in social values. A number of such examples can
be found to illustrate the value-relations that are
established between a diseased person and the rest
of the ’health' society. Here we are more concerned III 4
about the value-relations that are estabtished
during the interaction between a patient and a
medical professional such as a doctor. Conventional
type of medical work reinforces the dominant,
cultural, and ideological values in our society like :
,
J
III ;
— money determines your status;
— patients are bound to be ignorant, medical; /;
knowledge is always very complicated and
■
b> yond the scope of a lay person :
• !lGI
— intellectual work as that of a doctor's is
inherently superior to that of manual work
of a labourer, etc. etc.
It |
Besides these values which legitimize the
domination of the upper class, upper caste, male,
technical elite, doctors exercise authority over | ill! |
patients Doctors have the authority to decide
whether a worker is sick or not. Doctors employed
by the management of a company tend to refuse | b I
to call workers sick. Authority can be established
|
by punitive measures like refusing to issue a nece- >
?
ssary certificate or by co-optive methods by
treating a patient
at a concessional rate or by
k
issuing an unjustified certificate. In any society/
■
doctors would be necessary (though not the sole !(
agency) to decide whether continuing work would
jeopardise the health of a person or not. But in
today's society, based on the antagonistic relations
’ III!
IJ
11
- —--------------------------- -, k
J
>AFc ^vxlk^vi NO
of employer and employee, doctors acquire autho
rity ( which however can be bought). Doctors have
also a disciplinary role to play. Medical care is
expensive and sometimes tiresome, ( long queues)
so that nobody would like to be called sick unless
the suffering is too great to be tolerated.
—
Radical Medical Work
Medical work done with a radical perspective
should be done in such a manner that it transcends
the limitations imposed on all the three aspects
mentioned above by the requirements of the
existing dominant social relations. Thus a medical
project done by a radical group would create a
model, an island where the laws of the existing
medical system are flouted and medical work is
organized by a newer, higher set of norms. Briefly
speaking, radical medical work would demonstrate
in practice :
I
II
i
a) How medical resources (drugs, personnel
equipment) available in a backward country like
ours can be used rationally. This involves analy
sing medical problems from a pro-people epidemio
logical approach and planning a strategy of medical
interventions on that basis. This is in contrast to
the chaotic, irrational intervention of the existing
medical profession which suits the requirements
of the drug industry, the elite doctors and the
existing social hierarchy.
b) How radical Medical work generates
values which are contrary to the values bred by
work.
This
conventional type
of medical
deprofessionalizing,
of
involves demystifying.
medical technology. One example will concretely
demonstrate as to how new values can
be
generated
Let us imagine that a village health worker
manages a case of diarrhoea in such a medical
project. In this interaction, the. following things
happen :
a)
a non-profit oriented economic activity takes
place based on rational utilization of resources
(the economic change),
b)
the diarrhoeal disease
biotechnical change).
c)
a set of socio-cultural-ideological values are
created due to the peculiar practice and the
perspective behind the practice by the VHW.
is
controlled
(the
technical health education about diarrhoea; the
hows and whys of the causative, curative,
preventive aspects of diarrhoea.
explaining the social aspects of diarrhoea; how
it is a disease of the poor and backward areas
with improper water supply and how resources
are not being utilized for the benefit of the
poor; how the solution to the problem of
diarrhoea is proper water supply and not
drugs; how today's elite doctors and the drug
industry are not interested in this rational
solution.
—
explaining and proving that a doctor is not
generally needed to treat a disease like
common diarrhoea; how medical work is not
always complicated and that certain aspects
can be manged by lay people if properly
trained.
....... __ _
—
explaining that the commercialized, private
medical system is against such type of work.
—
explaining that the government's medical work
is not really committed to this approach.
—-
showing in practice that the medical work is
being done by a team in which the doctor is
also bound by the democratic decision making
process.
—
explaining that such a medical work is being
done because people have taken initiative,
shown enthusiasm in trying to solve their
problem, have organized themselves.
This last point is very important and needs
a little elaboration. Health problems are not consi
dered a priority by the poor people in our country
because more pressing problems are yet to be
solved. People will get attracted to good curative
services offered to them. But the kind of democratic
enthusiastic participation indispensible for such a
project cannot be generated by medical work alone.
Poor people are apathetic, dependent because
their day to day life of
poverty,
oppression
and dependence
smothers
their
inspiration
and enthusiasm. Unless their confidence and
aspirations are rekindled, one cannot hope to do
medical work In a different way. A nomhealth
input such as a properly implemented develop
mental work or
of a radical medical work,
In the absence of such a non-health input, it would
become a mere charity or curative work, and all the
talk about people's
participation, democratic
decision making etc. would be shorn of its content.
Many health projects in India are accompanied
by developmental activity "also". But this "also"
type of marginal, decorative developmental activity
reinforces the dependent, servile mentality of the
e-.w
3
(-?■—8>-
e-K
e-t:
e r
?
2
&
■
e
> - g.
1,^
a;
- .
- 3
: 0 ■
i-5
:-0
:-^
;-0
: -O
-o
' 'O
*"3
'C3
^3
'3
w
a vj
* 0
•\?
4
o
'G
:~o
R O
ra
G>
"O
~o
4 O
■~o ’
"O
"0
■ o
--0
"-O
I
people. Mere pouring of huge financial, material
resources has the same effect. Unles developmental
work has a conscientizing element in it, unless it is
primarily geared to the building of self-confident
self-reliant attitude of the people, it would not be
conducive to radical medical work. Any work based
on the enthusiasm and the people's participationn,
dispenses with the "motivation-problem" and
with it, also the need to build up elaborate arrange
ment to keep watch on who works and who does
not.] need not dwell here on all the advantages
of genuine people's participation but would only
reiterate that it is essential for any radical medical
work
The Role of Radical Medical Work
The perspective outlined above does not look
upon medical work merely as an "entry point". A
conventional type of medical work can act as a
stepping stone But that's all. Moreover its method
of work and hence the consciousness that it
generates contradicts the social perspective of the
radical group Radical medical project is also not
to be seen as mere stepping stone towards a
general radical, social, political work though both
are conducive to each o’hor. Radical med:cal work
has a subsidiary but nevertheless a definitive auto
nomous role to play as one of the channels of
communicative self education in a broad movement
towards revolutionary change It has an ideological
political aspect and can become a part of a revolu
tionary movement if one does not equate revolutio
nary change with a mere economic and political
change.
What is political about such a medical work ?
To clarify this, we must be clear as to what is
’politics. Politics is an activity of establishing, exer
cising the will to power in order to enhance
particular interests of a class, social group, indi
vidual etc. Our society Is divided into particular
social groups wiih particular (specific) interests
which are many times antagonistic to each other.
For example, the interests of the industrial capita
list are different from those of middle - peasants a
industrial workers, Our society is not based on
general interest of the society as a whole.
The particular interests are not confined to
only economic field. They naturally pervade all
spheres of life. The conventional, dominant medical
system serves the interests of the drug companies,
elite medical profession and indirectly the ruling
power. A radical medical work on the other hand
serves the interests of the people. It has therefore
an ideological-political aspect. According to our
constitution and laws, the drug companies have the
right to produce and sell any medical product and
the right to acquire profits. A doctor has the right
to refuse medical treatment to a person who does
not pay his/her charges and what charges are
legitimate is determined by the doctor on the basis
of what standards of living and wealth a doctor is
considered legitimate by the existing society. A
radical medical project flouts these rights in its
own work This is a political act. Any action which
relates to the domain of rights or authority is a
political action.
Radical medical project does not obey some
of the existing laws of medical practice. Its scope
however does not go beyond the field of medical
care. It leaves the main domain of existing system
of power relations (in the economic field) untou
ched Hence this medical work has a subsidiary
role to play in the struggle to challenge the
existing myriad of rights.
A fundamental socio-economic change does
not mean only economic change. This fundamental
change must take place in all spheres of life. A
movement for a fundamental change in the medical
system must start from today eventhough political
and economic change is a precondition for a
fundamental change inthe medical system itself.lf an
embryonic, prototype, movement, experimentation
does not start from now, such a change may never
come-the desirable transformation may remain only
at economic and political level.
A radical medical project is only a part of a
broader health-movement which aims at a funda
mental tranformation of all the aspecs of medical
system like the prodction and use of drugs, pattern
of medical education in medical colleges, a ystematic, community based research on non-allopathic
methods of therapies, etc. etc. Such a project has
in the main, a demonstrative and experimental value
apart from its significance for the local grass-root
root work/movement which it is a part of It
embodies a critique of the present pattern of
medical work and simultaneously represents the
embryo of the future pattern. This embryonic
current will grow only with the growth of revolu
tionary social political movement.
In short, even though a medical team
working with a radical perspective has fundamental
limitations in improving qualitatively the health
status of the population in an area (becausa it
cannot provide food, water etc, to the people), its
medical work can become part of and thereby
help a broader movement for fundamental change
provided, the medical work is done with the
perspechve outlined above.
(concluded)
______
5
l’\l
'
-
—
>
il,
I!
1! II
■
1I 1p
I
1 h
i
0
I
I
jlj I
1 I
H
$|r I1
11
hi;
nl j
f
47/1, (First Hear) St. faarks Reset
a;."
KSs •
a
medico friend
circle
bulletin
i/.<^
il
1.
14!
,.4)
i;
S '
,1
x"'"'
Bangalore - 560 001.
.
gsas»
owsg
JUNE 1988
a -3
i
Politics of Medical Work
-
Part I : Conventional Medical Work
s 3
a«
Ih
Anant R S
H
3 v
A number of new activists groups, hailing from different backgrounds have been working in increasingj numbore rrtr\c'+l\/
i r»
I
1!_
r _ . .i
•
bers mostly in the rural areas of India, for the last 10-15
-a years. Many of them are not associated with any
political party but some have leanings towards a sov
1
I?
r-\
r-v-. - -*
A
TL
3 *
cialist
or /-»/-»
communist
view-point.
. Ihese groups comp-
I
sv
.
. ,
h
_ _______
f w
J * rise of developmental groups of different shades;
_; milif * tant groups with varying perspectives of organising
g * struggles of the toiling people; charitable, welfare‘ or
* religious groups. . . . etc. Of the groups that have
3 C been active in the field of health or are interested in
an activity, those who believe that the |pressing
3 ■3. such
problems of the poor people cannot be solved in the
existing social-political system face a dilemma about
J a taking up medical work, These
___ radical y
,
groups
differ
@
with each other in their understanding of
f the social
systems,
of the fundamental change they want to bring
.........................
<
about,’, or of the methods to achieve their goal. But
* * they
'
all face the same problem of how to link their medical
work
t_to their J...
—
aim of fundamental, radical change in
;
the whole
social
-----------L." set up. In what follows, I will briefly
■*try to outline a perspective of how this linkage could
1 ^possibly be achieved.
^Marginal role of Curative Services
All medical problems are 0:1 the one hand biomedi^cal problems; at the same time, they are also social
^problems—i.e., they have non-biotechnical, social as•pects. For example, tuberculosis is, on the one hand
-a biotechnical problem—tubercle bacilli overwhelming
-the body's defence mechanisms and thus producing a
^Jisease complex. On the other hand, it is a social
problem caused by social factors like poverty, exploita
tion, and ignorance. This much is clear. ' The real
difficulties lie ahead—to see the relation between these
two aspects. Most medicos especially doctors are not
aware that the history of last 100 years tells us that
their technical curative work has’ contributed only mar
ginally to the improvement in the health status of the
population in Europe, America as well as in India.
The health of a population depends primarily on food,
water, housing, sanitation, ecological, occupational,
cultural environment and health education. In last
100 years, there has been a tremendous improvement
in the health-status of the American and European
population primarily because of the vast improvement in
these prerequisites of health. The science of medicine
has contributed to a certain extent in designing imp
rovements in the above-mentioned factors, especially
sanitation and water supply.
. .
But the fantastic, dazzling invention of antibiotics and other drugs has contributed very little to the fantastic decrease in the morbidity and mortality due to infections diseases, for example. Pulmonary Tuberculosis in England and Wales.
During the last 100 years, the death rate in England and
Wales has reduced by 75%; out of which, reduction
in deaths due to tuberculosis ranks first by contribut
ing 18/c to this fall. But most of it was achieved be
fore the inversion of Streptomycin and ocher drugs
and the B.C.G. vaccination. The death rate per thoussand was 3.8 in 1838. It came down to 1.8 in 1882
when the tubercular bacillus was discovered by Robert
Koch. It dropped down to 1 in 1910, before the TBSanitoriums had become fashionable; to 0.6 in 1940
before Streptomycin was invented and to 0.5 in late
I>
!i I
: i
I
N
HI
I ft I
I
111
1 II1
COMMURHTY HEALTH CELL
-
(First FloorlSt. .Marks Koad
BAWGAlORE - 500 001
*
r
~
-
---^T
)
/V)pc,
■j
I
A/p
'
’. Simiforties before B.C.G. vaccination was ■introduced,
drop
has
been
documented
for
New
York
city in
lar ( .
In
fact
in
Europe,
the
scourge
of
most
of
the US.
the infectious diseases was almost over before the era
of antibiotics. Vaccines is the only complicated modern
technological product which has contributed to any
measure to the substantial fall in the morbidity and mor
tality due to infectious diseases—for example diphtheria
and whooping cough. Antibiotics have taken care
of only the residual problem of endemic cases. Thus
the credit of the fall in infectious diseases goes not to
doctors but to research scientists, sanitary engineers
and workers, and above all to the general improvement
in the standard of living of the people in Europe. This
is not to say that the bio-technological miracles like
antibiotics and other modern drugs were irrelevant.
They have saved the lives of lakhs of people, reduced
pain and suffering, made modern surgery possible etc.
But on a ;social, historical landscape the contribution
of these drugs and of curative medicine should not be
Most of the deaths, and they number
overestimated.
in millions and millions, have been saved by non
medical factors.
The situation in India today
In India also, whatever improvement has occurred
during the last 50 years in the health status of our po
pulation is not mainly due to the brilliance, scholarship
and clinical acumen of top-ranking doctors. The dis
appearance of plague, small pox, the fantastic drop
(until recently) in the prevalence of malaria, the subs
tantial reduction in the incidence or cholera, are the
chief of the achievements in the field of health in the
last 50 years. These are due to the work done by
people on the Oasis of science of preventive and social
medicine—health planners, malaria workers, vaccina
tors, water and sanitary inspectors etc. etc. The highly
trained doctors doing (good or bad) clinical practice
have contributed virtually nothing to these achievements.
The symptomatic, case-to-case treatment given by
doctors has its role to play in the amelioration of pain,
suffering and also to a certain extent in the decrease
in the death rate. But most of the achievements are
not due to clinical practitioners.
I !
I
;S!
:
After 1966-67, i.e., after the third five years plan
period, the Indian economy is sinking year after year.
Technical, economic, human resources are more and
more mal-utilized or even non-utilized. There is dege
neration in the social ethos. Under such conditions
what is critical for improving the health status of our
population is a change in social conditions.
If this
happens, there will be a qualitative improvement in the
.7—-
again, the ex- C’j?
health status of ouf population./ Here
I
ampic ui luuc.vuIvuL
a pointer—the prevalence c*®
ample of tuberculosis is a
(10 million cases) and the death-rate (1 million per
year) due to tuberculosis has not decreased in the last
C,
35 years even though all the technical prerequisites
C'
like technical knowhow, personnel, drugs, etc. can be
easily made available in India today. The critical in
• lacking
•
~ is the
’
conditions. The
put that is
properr social
s—
is
the
case
of
the
problem
of
malnourishment. C
same L — ----- The per capita availability of food is even today enough
to eliminate malnourishment in children to a substantial extent. It is unequal access to the food produced^that is critical in determining the extent of malnourishment today. It is thus social conditions and not biotechnical inputs that are primary in determining the
tempo and extent of improvement in the health status
u
c
g
E
El
of a population.
i
Health work and medical work
-I
We begin to face the crux of the problem only after ” f
the above position is accepted; because now the ques c 6
tion arises as to why one needs to do medical work ai C
all until a social revolution takes place? How would C~
medical work help to achieve the aim of social revolution without which health problems cannot be solved
’
to a substantial extent? I would argue that within
the context of the perspective outlined so far, it is quite
meaningful to do medical work if it is done in a certain
way. Before we proceed further, I would like to make
clear the distinction between health-work and medicalwork.
eee-
In some quarters, medical-work is looked down C“"
upon and a lot of talk is made of promotive, preventive
health-work. Instead of the term medical-service or o
medical-work, the term health-service or health-work
is used, denoting a broader orientation. But in pracre-
tice, by and large, the work by a 'health team' re
mains essentially medical. By medical-work, I mean
the work in which knowledge of the science of medi
cine becomes an important, indispensable element
and medical technology in the form of medicines, spe
cial rays, surgery. .etc. used for curative, preventive^-'
or rehabilitative purpose is the key instrument of inter-C
vention. (Medical work is not tantamount to only eq
curative work. Vaccination, a preventive intervention,
is also medical-work). Compare such medical work^...
with that of organising the rural labourers for higher^
wages. This work may have a very good, positive
impact on their health, but this work of organizing ^e^
rural poor is not medical-work. Somewhere in bet
ween these two extremes lies health-work in which *
the science of medicine is only one of important fac-^
tors guiding the work. For example, building under-C •*
e-
e
ee
■
w
u
2
e-<
e
' xl
■
T'
j;’
j:
J
.. .g
-W
J '
a5
^"‘5
R’
•
M FC '
N 0V
I (4-1
ground drainage system to avoid breeding of mospicked up this terminology but also the ideology be
- quitos and flies thereby helping to control malaria and
hind it; namely that health can be improved with health
gastrointestinal infections is not medical-work but is
work. Let doctors and other medicos working in such
health-work because the science3 of medicine is only
projects realize or admit that their specific contribution
one of the important elements guiding this intervencan only be primarily medical and that medicalwork is
tion. The result of such an intervention is not only in
not going to improve the overall health-status of a
terms of health but is also in terms of achievement
population. Some health-projects have reduced In
sense of cleanliness. {Similarly, a daily bath is a good
fant Mortality Rates by their medical work involving
health practice, but is> more of an aesthetic, cultural
better antenatal care, safer delivery, better medical
necessity. The same is true with building latrines,
care
to mothers and children, immunization and
or well-ventilated houses or sinking tube-wells,, .etc.
extensive
propagation of Oral Rehydration. Therapy.
In all these interventions, science of medicine helps to
ut no medical work has improved the overall
improve the quality of the intervention in terms of the
health status of the population as indicated by more
impact of this intervention on health. But here, medi
sensitive health-indicators like substantial reduction in
cal knowledge is not indispensable and the result of
t e incidence of all grades of malnourishment in child
the intervention is as much to do with ease, aesthetics,
ren When anything beyond a reduction in IMR or
convenience as with health.
m Maternal Mortality Rate is achieved, there is always
some non-medical input like supplementary feeding or
rise m income..etc.
J
Misleading slogans
1 V-
Acceptance of the secondary role of medical work
The above distinction between health-work and medi
in
the process of improving the health status of the
cal work is not sterile semantics. I would argue that
people
does not mean that socially conscious medicos
the role of doctors and other medical people ( bearers
do
not
have
a worthwhile role to play in the process of
of knowledge of medicine) is primarily medical. Even
social
revolution
or fundamental socio-economic change
1 0 when medical people are participating in health-workexcept by engaging in non-medical activities. Socially
I
water and sanitation programme for example, their
conscious or radical medicos can undertake broadly
specific contribution remains medical. By and large,
three types of medical activities.
most 'health-schemes' are primarily medical schemes
and
most 'health-workers' are primarily medical wor
j
(1) We can make use of our medical knowledge to
kers. But since many policy-makers, national and inter
expose
to the public, various irrational practices in medi
national, for various reasons, are not satisfied with'
I
cine-overuse of diagnostic investigations; overuse
mere dispensing of pills," everybody in the develop
of drugs, use of irrational, hazardous drugs; misleading
ment field talks about medical people doing 'health
claims, advertisements by drug—companies, .etc. Medi
work.^ The real problem with this mistaken use of the
cal work does not necessarily mean treating patients
term health-work' starts when international and hence
with drugs. Any activity which uses medical know
national policy-makers start talking about improving
”■'0
ledge as an indispensable, chief tool is an authentic
the health of the people through 'health-work.' There
'0 are several National Health Programmes which create medical activity. This medical-work contributes to
t e process of Social revolution by educating the people
an illusion that they would make the people healthy
about
the current rotten state of affairs in the field of
Health for All by 2000 A.D." becomes the program
Medicine.
matic aim of the health ministry.
This slogan is being
brandished about, in the context of increasing infla
(2) There are many unsolved or half-solved prob
tion, unemployment, poverty, squalor, drought. What
lems in the field of development of appropriate 'model'
the health ministry can and should aim at is medical
of delivery of health-c~
“- "to our poor people.
care
For
care and health education for all by 2000 A.D. But
example, to what extent can paramedics handle cases
that would look too narrow an aim I Hence the health
competently? How to |prepare
----appropriate teaching
ministry has the nice slogan of health for all by 2000
material including good manuals? Why' the standard
A.D. I Even the name of this ministry is now "Ministry
recommended approach of community medicine does
. of health and family welfare;" Family welfare being the
not succeed in practice as regards many of the aspects
■
euphemism for population-control.
of community medicine ? How to maintain the cold5
chain for polio-vaccine? How to achieve
The role and hence intentions of the international
------- * a high degree
of compliance in completion of the c_..
and national agencies pushing this terminology of
complete course of
immunization of the various vaccines
health-work is suspect. But unfortunately, many well—?’ What are the
meaning people in the 'voluntary' sector have not only
(Contd. on p. 5)
1J?
i
i
a
D
i?
3
I
I 1
I il
I I 3
i
I
1 II
I 1
I1
tu I
I
3
... jjy
•M
M Fc
1^6^)
Nt>
1
(Contd. from p. 3)
specific health—educational messages that need to "be
given to the people, and how? What are the changes
required in the content and method of education of
doctors so as to make the competent clinicians as well
as competent in community medicine at the level of
Primary Health Centres, and at the level of general
practitioner in urban areas? How to develop democra
tic working relations between doctors and paramedics?
Such questions need further theoretical and practical
work for their satisfactory solution. Socially cons
cious medicos can take up any of such questions and
work upon it in a project. This experimental work
helps to make our criticism of the existing health
services concrete, mature, instead of it being general
and superficial. If there is a new political-economic
situation which allows building of a really pro-people
structure of health care; we should have concrete
examples of how things can be done differently. This
sort of medical-work requires understanding of not
only clinical medicine but of medical sociology, eco
nomics, pedagogy.. etc. Such a project is better done
as part of a broader development project aimed at ex
perimenting with an alternative strategy of develop
ment and use of resources. This would make avail
able other, non-medical inputs, which are so impor
tant for the success of any medical-work.
(3) If this medical work is undertaken in the con
text of an economico-political movement of the down
trodden people, it would directly contribute to the pro
cess of fundamental social revolution. But even if it
is not possible to do so, a health project can be a radi
cal one, and can indirectly contribute to the overall
march towards fundamental social revolution, if this
medical work is done in a radical way. Let me clarify
here, as to what I mean by radical medical-work.
The beginning however requires an understanding of
the ideology and politics of medical work.
J
■ p-'
I I
i I
I
i' I
I H
i ^5-
I
&
!
l„
II
I fc-'
If.
•I
L'
;i
(To be concluded)
5
C
4J.ni I Y HZA.rHCELL
^7/1. \Pirst F loor) St. Murks Roadfl
Bangalore - 530 001.
'/■
■.
<
5.
health, disease, and healing. Studying and addressing root causes
of illness and despair should be a priority, Ways must be found to
renew a badly damaged environment.
Learning and practicing behaviour that redefines persons as God's
children rather than as economic or political objects generates
hope and is one step toward renewal. Patient community building
and making ourselves available to each other elicits hope.
Diaconal action in witness and service are expressions of hope,, and
engender new hope.
The development of positive relationships between the North and the
South - penetrating institutions and peoples-is a indication of
hope. Movements created and sustained by people from below and
breaking through structures of injustice are signs of hope.
The dimensions of agape love and justice in health challenge
churches, locally, nationally, and globally to be healing
communities"•
/
* * ★** * * *
*
* *
* * * *
■k
★ it
* *
★
i
Aug
3
Politics of Medical Work
Myths
Perpetuated by
f ’ ip
Saha
tha Voulntary Health Sector.
SATHYAA4ALA
n
I
■
3 I
I
i
it
’
Anant in his article (mfc No. 141-2) has
taken great pains to explain the distinction he
sees between health work and medical work'
and then goes on to outline how medical work
with a radical perspective has the possibility of
helping a broader movement for fundamental
change. Part I of his article conveys the impre
ssion that conventional medical werk apart from
;ts marginal role played by curative services is
harmless enough and groups running
health
projects may justifiably feel why quibble over
terms like 'medical' and 'health' work if the
activity is aimed at improving the health of a
population. I would like to show that it is not
as simple as that and the voluntary health sector
by not critically evaluating its activities has
created a set of myths about what has come to
be termed 'Community Healh work' and in the
process has played and continues to play an antipeople role. To illustrate this, I would like to take
the example of the greatest contribution, if one
can call it that, that the voluntary heal'h sector
has made in the last twenty years —demonstra
tion of the possibility of training semi literate-or
illiterate persons from villages to provide minimal
medical relief at the village level : The Village
Health Worker (VHW).
Myth No. 1 : Health is neutral :
"By demonstrating the Acid Fast Bacilli
under the microscope, the VHW is
convinced
that leprosy is not divine curse" ( R. S. Arole,
Jamkhed). From the time that the 'germ' was
discovered, the germ theory of disease has effe
ctively helped to divert attention from the root
cause of disease : the fundamentally exploitative
nature of society. An outcome of this has been
the victim-blaming attitude of most of the health
education messages. The attitude of blaming the
victim is further strengthened by creating the
myth that every one has equal chances of falling
sick. For instance, in answer to the question,
'who gets TB', one health message states :
Anybody can get TB
Rich people and poor people can get TB
Young children and old can get TB
4
People in the villages and people in the cities
can get TB
Good and Bad people can get TB
,-w
Men, Women and Children can get TB (1)
U.:
According to such messages, there is abso
lutely no relationship between poverty and ill
health. Health education messages in most flash
cards and posters encourage people to uncritically
develop certain attitudes and beliefs; they basi
cally persuade people to develop an unquestioning
faith in doctors and the modern system of medicine.
If prevously people believed disease was due to
fate or divine curse, which struck them for some
fault of their own, they are now encouraged to
believe that disease is due to germs which also
affect them because of their own fault either
because they have not kept clean, eaten well or
accepted hazardous contraceptives (2).
It is repeatedly stated that the primary role
of the VHW is to impart healh education with
particular reference to the priorities of the health
programme. And when the VHW repeats the neutral
'health' messages, she becomes the tool of the
establishment, albeit unwittingly. It may be too
much to expect the government to train a cadre
of health workers with the aim of questioning
the exploitative practices in the village and in
the medical system, but even the groups in the
voluntary sector, with their relatively autonomous
existence, fear to do so. The reality is, if the
project wishs to servive, it cannot afford to
alienate the rural elite which is bound to occur
if the VHW begins to encourage people to
question the exploitative practices I Infact, the
popularity that a health project enjoys with the
local elite, is a good index of how effective
the programme is. Yet, instead of accepting their
sitting-on-the-fence attitude, these projects tend
to cover themselves with all the choicest, radical
sounding terminology. What is even more shock
ing is that "there even appears to be an understan
ding among the local power group, the police,
and these organizations that each will leave the
other alone. The status quo remains and basic
change fails to occur. There is an example of
a coordinator at CROSS ( Comprehensive Rural
w
■
e
p
r
eft
-
ft
1
k
I
-
•
aa 'I< .
j
J
■4
3
3
3
M H-
v\l Lc-M v\
Operations Service Society) who, with the ble
ssings of the director, employs unpaid bonded
labour in his farm, while he gets a salary from
the organization for the
upliftment
of the
poor" (3).
Some, acknowledging the stratification in
the village, have actually recommended that health
a
aZ?
a
* 3
^3
o
o
d
•G)
Q
G)
■a
■‘O
.. 3
GS
Q
o
o
o
o
“CO
“O
“O
o
o
ZO
o
co
0
programme can be organized to mobilize all the
people in the village, irrespective of their caste
creed and class towards a common goal, there
by helping in creating a 'community' where none
exists. This kind of suggestion is at best a
reflection of naivete and at worst a deliberate
attempt to allay suspicion. It may be possible
to mobilize financial support from the rich land
owners for an immunization programme just the
way big business houses are willing to donate
large sums of money for 'charitable' purposes,
but this in no way alters the exploitative interact
ions that constatly take place in the villages
between the land owners and
the
landless
labourers. In that sence, it is a misnomer to call a
Village a community and health programme formu
lated in this way, a community bassed programme.
Myth No. 2 : First meet the felt needs of a
community and once rapport is built, meet
the real needs.
Here a false dichotomy is being created
between what is considered felt needs and what is
considered real needs. The felt need by virtue of its
nature, is considered to be subjective, not rooted
in reality but only in the mind of the subject. The
real need on the other hand is considered to be
objective, for it is what is perceived by the health
group. This myth is also stated in another way:
Create a balance between curative and preventive
services; curative to meet the felt needs and preven
tive to meet the real needs.
How do the poor view their needs ? When a
medical team visits a village, it is true that it comes
up with the need for curative services, and although
almost everyone in the village has a medical com
plaint, most of these complaints seem to be minor
aches and pains in specified and unspecified parts
of the body: If one cares to listen and observe, one
finds that the high level of morbidity is generally
the unspecific symptoms of under nutrition, over
work and the constant stress of making the two
ends meet. The people express it as illness and the
medical team tries to diagnose it as a disease. There
in lies the mistake. The expression on the part of
the people is the expression to feel healthy. Since
Jpv
1^14-
the role of a medical team is perceived to be that
of alleviatim of illness, tfie need gets expressed to
the team as the need for curative services. More
specifically, the need is expressed as a demand for
injections, tonics,—a demand created by the pro
motional efforts of pharmaceutical companies and
the private medical sector. If, instead of a medica*
team, a non-medical person were to visit the village
she would come up with the need for employment,
food, drinking water-all 'felt' needs of the poorAnd if real needs are being stated as 'preventive
services' by the medical team, the above stated felt
needs for employment, food, and drinking water are
in reality real needs as well. In any case,- preven
tive services in medical terms mean immunization,
personal hygiene and health education, all very
innocuous and comparatively ineffective as com
pared to real preventive measures of providing
adequate nutritious food and water. It is clear that
in providing the traditional preventive services, the
medical team is meeting its own need for statistical
measurment of its performance. (It is easier to
measure performance, if 'the target' to be achieved
is in numbers of children to be immunized, pregnant
women contacted etc.)
Thus, it is on the basis of what is considered
real need as perceived by the medical team that
priorities are set. Although much has been made of
" start from where the people are... ", the medical
team approaches the village with Its pre determined
objectives, well-defind and time bound and with
the help of the VHW imposes these on the people
in a subtle way than before. In doing this, the
* community ' based programme often becomes the
means for ideological brain washing and the VHW
the effective vehicle. For instance, in 'community
health ' programmes, there is a great emphasis on
antenatal care. Infact, this is the other major pre
ventive programme aimed at women in the repro
ductive age group apart from the oppressive
population control programme. Justification for
this comes in the from of " scientifc " facts which
quote the high maternal mortality rate in India,
compared to developed countries, as the most
important cause of death among the women
population. Statistics however show a differnt
picture. In 1980, deaths due to child birth and
pregnancy accounted for only 1.2% of the deaths
due to all major causes in India. Further, deaths
due to maternal causes accounted for only 11 % of
the total deaths among the women population. In
other words, 89% of deaths among women were
due to causes other than maternal mortality (4)
I
I
i
i
■
I I
I
I
, I
:
■
;
|
i
i1
/
II
£
!
’ 1
’ .T I
J
i
'f’f i I p
/w
MH: - &V\IU-Kv NO
Similarly, it is a popular medical belief that one of
the major causes of infant mortality and maternal
morbidity is births with out proper spacing, It is
with this understanding that several hazardous
spacing methods are being promoted through the
VHW. Again, if one takes the trouble to observe the
rural situation, one would find that in any commu
nity where the practice of prolonged breast feeding
exists, the spacing between two births is on an
average from 22-26.5 months, the recommended
spacing interval (5).
i
In reality, the myth operates in a rephrased
manner : meet the ' meetable ' needs, and after
allaying suspicions, impose your own needs. Since
the VHW is " one among the people ", people will
not be too suspicious and soon enough will come
to believe in the propaganda of the ruling classesThis strategy of ' using ' health programmes to get
what YOU want is not new. the missionaries did it,
the colonizers did it, and now the so-called comm
unity health programmes are doing it.
Myth No 3 ; Majority of the health problems in
rural areas are simple.
t
It is stated that " what is needed at the com. munity level is not professions expertise, so much
as nearness to the community
its confidence,
emotional rapport with the people, willingness to
assist, low cost and capacity to spare the needed
time" (6). And further, " Once simple criteria have
been developed for diagnosis treatment and after
care, it is not essential to deploy professional persd;
or implementation " (7).
Here, the word simple is being confused with
the word common, and it is implied that people do
not seek early treatment because of ignorance or
due to cultural alienation. Let us take the example
of tuberculosis and let us also assume that it is the
VHW who has identified a ‘ suspect
The VHW is
neither in a position to confirm diagnosis nor in a
position to initiate treatment and the patient has to
therefore depend upon the next tier of the delivery
system - the Primary Health Centre, for both these
services. What are his/her chances that s/he will get
cured of the disease ? Mira Sadgopal from Bankheri
has identified 39 obstacles which prevent a patient
from being diag nosed and treated for tuberculosis.
(8). Except for 6 of the obslactes, which come
under the category of 'failure of communication to
patient by doctor',( intention or lack of intention
of doctor to inform; patient's fears; contradictions
in the belief system, in the society about disease;
doctor's impatience; mystification of doctor's role'
poor relations/faulty communication between PHC
staff) the VHW is not in a position to tackle any
of the problems that the patient faces. It may be
true to an extent that professional expertise in the
form of a qualified doctor too will not be able to do
anything much apart from those factors under his/
her control. But to project a VHW trained in con
ventional medical work (Anant's definition), as an
effective measure to tackle these problems is equally
unrealistic. I have purposely not taken the example
of diarrhoea in an under-five child as an example
because it may seem easier to diagnose and treat
with ORT. In a poor household whose very survival
depends upon the adult earning member, the
illheath of a small child with diarrhoea may be rela
tively unimportant as compared to that of an adult
with tuberculosis.
Before I conclude, I would like to comment
on the selection criteria used in the conventional
med cal projects for choosing a VHW. The conventi
onal medical projects have a long list of the qualities
a VHW should possess. Among the visible qualities,
the recommended ones are " the VHW should pre
ferably be a married middle aged woman with life
experiences such as bearing children and raising
them " (9). This is in keeping with the traditional
approach in which women and children are the
targets of any health programme. However, if the
intention is to train a health activist along the line
suggested by Anant, activist defined as a person
engaged in sustained participation in struggles
and social actions; w o is active in the everyday
struggles in the life of others and struggles related
specifically to her as a woman and a worker then
the criteria for selection changes. The VHW is then
not only integrated with the people in order to
work but also that she is first of all a person alienated
in some crucial way from the normal society, alienated
enough to want to change, its oppressive character. In
the given context, activism is seen in its develop
mental process, with its beginnings in nascent
activigy, leading to participation in social action
backed by an evolving personal and political con
sciousness (10).
How is this translated into practice ? A study
carried out among the health workers in a resettle
ment colonies in Delhi showed that a large majority
of the health worker considered themselves active
prior to becoming members of their sanghs. They
had either taken part in struggles within the kinship
network and immediate neighbourhood wh>ch in
0
.....
-
$
4
I;
XX
X
i
...
e.-'
r
■
§
V-
si
'»
eX.
X'
f ii
M pC ‘ SwllrHn AJdi
.j ..
■J ?
E
■
H°
E5
E0
R
T’O
4-3 -Ci
1
<5
J.-9
J.o
1 -A
J..Q
J A
3-A
J A
J A
3 n.
eluded cases of violence against women (domestic,
rape and sexual harassment) or had struggled aga
inst their own and other women's oppression within
their families like fighting against purdah, seclusion
on reaching puberty, struggling against extreme
forms of domestic violence and even going in for
inter-caste marriage, as illustrated by the life of
two health workers. “ Virmati, 28 years old, a resi
dent of Jehangirpuri, married earlier then widowed
and remarried, faced extremes of violence including
two occasions when her husband attempted to
murder her by setting fire to her. He also attempted
to force her into prostitution. Virmati recalls not
having accepted her husband's views as final. She
refused to keep purdah, and finally decided to end
his tyranny by leaving him, along with her daughter
and has started earning to support herself and her
daughter ".
" Sumitra, 36 years old, a resident of Sundar
nagari has led a life of continuous struggle. Illtreated by her in-laws for not having had a child
■ immediately after marriage, she underwent extreme
forms of violence. At one time she was forced to be
fully in purdah and was escorted even to the public
latrines. Her giving up purdah, sitting on a bed in
front of her men folks, drew a vicious attack on her
but she continued to struggle, gradually getting in
touch with other women, almost desperate to free
herself from the confines of the four walls of her
house" (11). What is clear is, if such a criteria were
to be employed in selecting the health workers, the
' community' may not be interested but infact be
antagonistic. These women would probably have a
*bad' name for not having been socially condi
tioned enough to be 'good' house wives and
mothers. The fact is that at least in this health
programme in the resettlement colonies of Delhi
the health workers have been active for the last
four years and have consistently raised issues millitantly and have been successful enough to mobilize
the women from the slums dispite thein non-con
forming life. The VHW concept was a known con
cept even at the time the Shore committee sat down
to make its recommendations for a health system
in the independant India. (The USSR had already
demonstrated that a health delivery system cou.d be
based on workers at the local level) But it was
only after twenty years, that International organiza
tions as well asgroupsin the voluntary health sector
decided to pick this up as a result of international
coverage that the 'bare-foot doctors' from China
received. By accepting modern medicine uncritically
and by promoting it more effectively through the
VHWs, the voluntary health sector ( and their
VHWs ) has acted as the extension of the ideolo
gical arm of the medical establishment in the
process deliberately depoliticising health. In their
turn, the International organizations like the WHO,
have orchestrated the
achievements ' of the
voluntary health sector, especially in promoting the
VHW s concept, because it suited them to 'prove*
on mere anecdotal discriptions of these project that
health can be improved without any fundamental
changes in the society. This is the greatest disser
vice that the groups in the voluntary health sector
have done to the poor of our country.
i
References :
1.
"Better Care in Tuberculosis " George
A, Health for the Millions, Vol X, April,84.
2.
" Taking Sides : The Choices before the
health worker ", Sathyamala, Nirmala,
Nalini, Anitra Trust, 1986, p190.
3.
" Community Health Projects : At the
cross roads ?", Sumati Nair, Socialist
Health Review, Vol II, No 2, p84.
• - j • f n ..'T' I- •
n Health Statistics of India ", CBHI,
GOI, 1983, p197, 214-15.
4.
5.
" The Chance of Conception during lac
tation ", Jeron KVG, J Biosoc. Sci„
Supp., 4, 1977, p41-54.
6,
Report of the group on medical educa
tion and support manpower health servi
ces and medical education: a programme
for immediate action, GOI, April 1975.
7.
" Auxilaries in Health Care : Programme
in Developing Countries", Fendall, John
Hopkins Press, 1979, p4.
8.
" Health Care vs Struggle for Life ''
Mirais, Under the leus, Health and medi
cine, mfc, 1986.
li
■i
i
d
I
1’1
9. " Comprehensive Rural Health Project ",
R S Arole, mfc-b (49).
10 a 11. " Emerging Grass Roots - Level women
Activists : A selective study in the rese
ttlement colonies in Delhi ", Mallika V,
M Phil dissertation, Oct. 1986, p19.
J A
J A
J A
J A
•I
is
7
/.
104
medico friend
circle
bulletin
AUGUST
1984
^(ivl
NARMADA PROJECT AND THE TRIBALS *
— don’t let them drown in despair
Preamble
We are three voluntary groups, working since
1980 amongst the tribals who have been ousted from
their traditional homelands by the Sardar Sarovar
Project on the Narmada river undertaken by the
the Government of Gujarat. Our experience regard
ing the problems of these tribal rehabilitees has raised
many questions and issues in our minds which we
would like to share with you.
When ambitious developmental projects like the
Narmada Project are undertaken, a large number of
families are asked to leave their lands, houses, familiar
surroundings and settle elsewhere. This is justified
on the basis of ‘public purpose’ which is essentially
that much larger benefits accrue to much larger popu
lations who would otherwise live at a low standard
of living. This, of course, must imply that those who
give up everything so that the project can become a
reality, must also not suffer a drop in their standard
of living. In fact it is necessary that they too improve
their lot commensurate with similar improvements
in the standard of living of the beneficiaries of the
project. Our concern is focussed on the social and
economic suffering that these oustees are going to
face if the governments rehabilitation policy on paper
does not match with the actual programme in the
field. We have reason to believe that certain ambi
guities in policy and trends in implementation seen
in that area are going to seriously affect the health,
life and future of these people.
Background
About 220 villages in the three States of Gujarat,
Maharashtra and Madhya Pradesh are going to be
affected by the inundation of large tracts in this
area. Among them we have worked with the illite
rate tribals of 19 villages in Gujarat and most of the
facts and issues discussed derive out of this experience.
The main occupation of tribals in this area is agri
culture. The income from agriculture is supplemented
through collection of forest produce, hunting and
other forms of labour.
Due to cultural reasons and administrative hur
dles at local levels, the overwhelming majority of
tribals have had joint holdings for generations toge
ther. Thus a seemingly large land holding (more
than 5 acres) in the name of one person, in reality
may mean that two or more families are actually
earning their livelihood from it.
There are a few landless labourers. Even these
earn their livelihood by cultivating government owned,
fallow forest land or other waste land. It is not pos
sible to estimate the amount of land brought under
such cultivation since this is treated as unauthorised
cultivation. Whatever -the technicality of such a
situation, it is an established fact that they have been
living and cultivating such lands for many years and
they are entitled to compensation for the loss of this
only source of living.
Water Dispute Tribunal
A tribunal was set up to study the problems
arising out of the project implementation. Its award
took into account the factors of total dependence on
land of these tribals as well as the responsibility of
the rehabilitation programme in removing the poverty
of the ‘oustees’. It, therefore, provided land for land
compensation (ie., if more than 25 percent of land
owned by any family was acquired for the project
they were to be given an equal amount of irrigable
land). It also made a specific provision of a minimum
of 5 acres of irrigable land to all those whose land
holding was less than 5 acres of land. It also stated
that first preference would be given for rehabilitation
within the command area of the project. However,
if the ‘oustees’ did not want to settle there, they were
to be settled in their respective states on a similar
basis. In addition, it #as decided that the agricul
tural lands were not to be provided free of cost, but
the occupancy price should be recovered from them
in 20 yearly interest free instalments; the first instal
ment being half the compensation received by the
‘oustees’. The tribunal has also made the proviso
that if an individual is losing atleast 75 percent of
his land he should have the option of surrendering
the rest of his land as well. This award on the face
of it seemed a relatively fair policy and it was hoped
that with proper implementation it would tackle all
the grievances of the tribals.
ment will have to be made by the govern
ment.
4
J
The usual analysis of land records do not
show the reality of land holdings in a tribal
region where joint holdings are significant.
We reanalysed the land holdings not by
the units as they are officially recorded but
by the number of families who are actually
dependent on the land. We found that
there were 624 land holdings in the 18
villages surveyed, whereas the number of
families actually dependent on them are
2109, since most are joint holdings. Also if
holding is taken as the unit only 41.8%
of the total holdings are less than 5 acres
whereas if family is taken as the unit we
found 94% of the families with a holding
less than 5 acres!
Some ambiguities
1.
2
3.
Damming the tribals
The Narmada Tribunal being an inter-state
water dispute tribunal took into account the
rehabilitation of oustees from Madhya
Pradesh and Maharashtra. No reference
was made to those from Gujarat! Clearly
what applies to Maharashtra and Madhya
Pradesh should apply to oustees of Gujarat
as well; but the government of Gujarat has
not earmarked any land in the command
area of the project for this rehabilitation.
Even though these tribals will be the first
to be affected, they are expected to buy their
own land and only after they do so other
basic amenities like wells, schools and roads
are to be provided.
‘The construction of dams has effectively resulted
in a direct assault on the country’s tribal population.
Dams are usually constructed in remote, forest areas
where most of the tribal groups also live. The sudden
influx of the modern system, destruction of the sur
rounding nature on which their lives are dependent,
and ultimately displacement and resettlement, leaves
a tradition-bound tribal family totally bewildered,
powerless and on the verge of total social, cultural
and economic collapse.’
— State of Environment Report, 1982, CSE.
Project implementation and its problems
There is a government resolution CG. R.)
of June 1979 of the Irrigation Department
of the Government of Gujarat which states
that a minimum of 5 acres of land should
be provided for each oustee family for their
rehabilitation. There is, of course, no pro
vision to provide
irrigable land in the
command area of the project in this
resolution.
Some problems have arisen due to the half hear
ted implementation of a watered down and modified
government resolution. These are:
i. The ‘oustees’ have been shown lands which
are so poor in quality and so far away from
their traditional homeland (about 150 kms
away) that their economic situation inse
cure as it was, would worsen further and
their whole social and cultural life disrup
ted. Naturally they rejected such outrage
ous propositions.
ii. When the oustees refused the land the
government asked them to purchase land
from private land owners from their com
pensation money. The consequences of
this were: (a) the oustees with less than
5 acres of land could not buy 5 acres of
land which they were entitled to; (b) some
could not even buy the land equal to what
they had been originally cultivating; (c) the
amenities that they were entitled to could
not be had as per the law because of the
wide scattering.
iii. It has not been possible for the illiterate
tribals to deal on an equal footing with the
In the cost estimates in the project report
prepared in 1980, the Government has made
no provision for the cost of acquiring the
total of 40000 acres of land that it would
have to acquire to rehabilitate all the
oustees. It has instead provided for only
1310 acres of land which is clearly meant
for roads and house sites only. In fact the
agricultural land to be acquired should be
clearly more than the actual amount sub
merged, specially because a significant
proportion of oustees who own less than 5
acres of land are to be provided at least
5 acres as per the directive of the tribunal.
The argument that the land is not to be
given free of cost, and hence the cost of
acquisition need not be mentioned is not
tenable, since clearly some initial invest2
PtaaVLcA1 I'V
I\} o Id y , Ava^ mi l^(|.
high caste land owners in these land deals
thrust upon them by the governments in
action. They have been cheated and ex
ploited. In the beginning the Additional
Collector gave active help and the deals
were made relatively easily. However, even
now these deals are not yet completely
registered and the ownership of lands still
rests with the original land owners. The
whole matter depends on the goodwill of
the concerned government official and m
our experience there has been a general
aloofness and reluctance on their part to
get too involved.
iv)
The Government of Gujarat has been plea
ding from the very beginning, that it is vir
tually impossible to give agricultural land
to the oustees as no surplus land is availa
ble. Forest lands cannot be given, as only
a few forests are left and other waste lands
are scarce. However the government could
instead purchase or acquire private lands in
large tracts so that proper rehabilitation,
can be carried out, and rehabilitation of the
oustees itself could be proclaimed to be a
‘public purpose’ in this respect.
v)
In some villages the situation has arisen
wherte 80% of the village land has been
acquired. The land acquisition authority is
refusing to acquire the remaining 20% of
the land. This land is owned by 20-30
families; of these families, 4-5 of them
happen to retain practically all their lands.
If these lands are not to be acquired the
isolation of these families will be near total.
They will be cut off physically, socially and
culturally. They will be deprived of other
amenities like school,
shops and health
services. The land acquisition authority is
taking a very rigid view of the land acquisi
tion procedure which states that only land
under submergence can be acquired.
vi)
»9
of Rs. 2000 per acre. This is totally unsatis
factory . This computed average compensaton is so low that most of the villagers will
be deprived of their land in exchange for a
paltry sum, insufficient to buy adequate
alternative land to survive . The consequence
of such myopic action of the government
can only be that the ‘oustees’ will become
poorer.
To summarise the situation as it exists today —the government has abandoned its primary responsi
bility of providing land for land as directed by the
tribunal, it has offered a totally inadequate sum of
compensation; it has shown no aptitude or willing
ness to keep down the prices of the surrounding
private lands wiiich may have to be acquired by the
putstees; it has used ‘holding’ as the unit and not
‘family’, in its computation, thus hiding a concrete
reality of the tribal regions; and its grave lack of
responsibility has resulted in the ousted
tribals
becoming a prey to high caste land owners and
their brokers. In brief, with a policy implementation
that is insensitive to the human problem of these
tribals it has made the tribunals recommendation of
the objective of ‘abolition of poverty of the oustees’
a myth.
The ‘Cost’ Facade
Among others, the main claim for this inade
quate implementation of the tribunals recommenda
tion has been the cost factor. The government has
claimed that land acquisition of the type recommended
will push up the cost of the project. The following
facts about the governments lop-sided sense of pro
portions in cost provisions for certain other aspects
of the project is not only disturbing but also show
how hollow the claim is in the first place.
The project report shows that the cost estimate
of the whole rehabilitation programme including com
pensation for lands, houses etc., in all the 220 villages
in the three States is Rs. 19.83 crores, while the cost
estimates of the construction of the staff buildings at
Kevadia Project Colony alone will be Rs. 23.45
crores. Add to this cost the miscellaneous and estab
lishment costs of the same magnitude and we begin
to sense how distorted is the government’s sense of
proportion. The scales which the government holds in
its hand give more than twice the weightage to the
temporary needs of providing houses only to a few
hundred families of the project in one colony alone.
In comparison to this, the entire rehabilitation cost
of 10 to 12 thousand families scattered over 220
villages of the three States, which can make or mar
thek entire lives, gets less than half the weightage.
What is more surprising is that the staff quarters, the
water lines, the electricity lines, guest homes, the
roads in the Kevadia Colony have already been built
while the staff are yet to arrive. In contrast the
notices to acquire lands from the people to be ousted
All the tribals in the affected villages of
Gujarat have so far voluntarily surrendered
their lands, and other villages are ready to
follow suit. There is, however, still wide
spread uncertainty about the amount of
compensation they would be paid. Since
all the villages are losing their land under
the same project, it is only fair that they
should get a uniform and generous com
pensation. The State Government has not
yet made up its mind and is vascillating
on the issue. The traditional way of com
puting the amount of compensation by
taking current market values for the land
is clearly not applicable to tribal land since
for many years no sale deeds have been
concluded in this area. In its cost estimates
the government has put an estimate of
average cost of land acquisition at a rate
(Continued on page 6)
3
10th February, 1992
MEDICAL
01.
02.
03.
04.
05.
06.
07.
08.
09.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
EDUCATORS
REVIEW
MEETING
TENTATIVE
LIST
PARTICIPANTS
OF
JUNE
1992
Dr. Abraham Joseph, CMC-Vellore
Dr. Prem Pais, SJMC, Bangalore
Dr. Alex Zachariah, CMC-Ludhiana
Dr. Cherian Thomas, CMC-Miraj
Dr. D.K. Srinivasa, NTTC, JIPMER, Pondicherry.
Dr. Asha, JIPMER, Pondicherry
Dr. Kartikeya Nanavathi, NHLMC, Ahmedabad
CMET, AIIMS, New Delhi (Representative)
Dr. B. Ekbal, Medical College, Calicut
Dr. Ulhas Jajoo, MGIMS, Sevagram
Dr. Siddarth Das, KGMC, Lucknow
Dr. M.K. Vasundhra, BMC, Bangalore
Dr. N.H. Antia, FRCH, Bombay (Special Invitee)
Dr. Palitha Abeykoon, WHO-SEARO, New Delhi (Special Invitee)
Dr. C.M. Francis, Bangalore
Dr. P. Zachariah, Vellore
- Advisers, Medical Education Project
Dr. V. Benjamin, Bangalore
Dr. George Joseph, Madras
Dr. Ravi Narayan, Bangalore
Dr. Thelma Narayan, Bangalore
Dr. Shirdi Prasad Tekur, Bangalore
CHC Team
Dr. Mohan K. Isaac, Bangalore
Dr. M.J. Thomas, Bangalore
IN ADDITION
One additional participant each from the 4 CMC's to be
nominated by the Director/Principal (a faculty member who
is involved in Medical Education Reform) and whose costs
may be met by Institutional fund.
One nominee each from CHAI, CMAI and VHAI whose costs may
be met by the associations themselves.
★ ★ * *
* * *
* *
★
*rn/mk
MR.
MO
l©q..
Q(
has already been served but the vital issue of com
pensation for imminent land loss is still unresolved.
Suggested Changes in Policy
iv.
Having worked with the tribals in the 19 villages
of Gujarat since 1980, we as a group have just begun
to understand the problems from the perspectives of
the tribals. We suggest the following changes in the
policy of rehabilitation to make it sensitive and rele
vant to the socio-economic, cultural, psychological
and ecological needs of these oustees who are as
much the ‘public’ as any other.
v.
The poverty of “development”
The forest issue
‘In a country like India, with a high population
density and high level of poverty, virtually every
ecological niche is occupied by some occupational or
cultural human group for its sustenance. Each time
an ecological niche is degraded or its resources appro
priated by the more powerful in society, the deprived,
weaker sections become further impoverished. For
instance, the steady destruction of our natural forests,
pasture lands and coastal water bodies has not only
meant increased economic poverty for millions of
tribals, nomads and traditional fisherfolk, but also
a slow cultural and social death: a dismal change from
rugged self-sufficient human beings to abjectly
dependent landless labourers and squalor-stricken
urban migrants. Current development can in fact be
described as the process by which the rich and more
powerful reallocate the nation’s natural resources in
their favour and modern technology is the tool that
subserves this process.’
— The State of India's Environment, 1982, CSE
i.
ii
iii
the amount of forest land and/or other
waste lands they are actually cultivating
and provide them with alternate land in
appropriate amounts.
Not only must individuals (whose land
acquired is more than 75%) be given the
option of surrendering the rest but this rule
must be extended to the villages as a whole
as well if they are going to loose atleast
75% of their total agricultural land.
The compensation for land acquired must
be adequate and sufficient to buy new land
of atleast equivalent size keeping the basic
objective of rehabilitation i.e., abolition of
poverty of the oustees in mind.
Following our recent contacts in the interior
villages of Gujarat and Maharashtra, we have come
to understand another important dimension of this
problem. The tribals, especially Dungari Bhils who,
have lived in these forests for centuries cannot imagine
how they will survive outside the forests. The forest is
so much a part of their life. Even outsiders like us who
are quite sympathetic cannot fully appreciate or
understand their attachment to the forests, let alone
the aloof and faceless bureaucracy of the Narmada
Project.
For these tribals, the forests are not only the
fountain of their material needs, but also an integral
part of their social, cultural and religious life. You
have to be with them to understand what forests
mean to them. No wonder that the inhabitants of
these villages are refusing to move outside the forest
area. Even those oustees who agree to resettle on
non-forest lands, would opt for forest land, if the
option is offered to them.
The ambiguities in the rehabilitation propo
sals must be clarified immediately
— the rehabilitation of displaced people in
all three States is of equal importance;
— the land for land compensation with the
minimum provision of 5 acres should
be implemented efficiently;
— the land offered should be irrigable,
agricultural and as far as possible within
the command area of the project and
preferably in their respective States.
The government should either buy or acquire
private lands in large tracts if it does not
have any surplus within its own possession.
Under no circumstances should the oustees
be asked to purchase their own lands.
The government should take a family as a
unit (and not ‘holding’) and provide mini
mum of 5 acres of irrigable land to each
oustee family irrespective of the fact whe
ther they legally own their land or not.
If necessary, the government can conduct
a detailed survey in the villages to find out
Why is the Government so adamantly refusing
to release forest land for resettlement? The reevaluation of the government’s blanket policy with
regard to forest land is urgently called for. The
Govemment’s argument is based on the laudable
objective of ‘conservation of forests4’ The plausibility
of this argument is only superficial. It is clear now
that the Government itself is destroying large tracts
of forest in the name of ‘development’. It also sanc
tions felling of the forest in the name of ‘satisfac
tion of market needs’. Only when it comes to giving
forest lands to tribals, the Government raises the
bogey of ‘Conservation of forests’. Hidden in this
argument is the unfounded charge against the tribals
that they are the culprits behind the massive defore
station. The facts if examined closely would reveal
exactly the opposite story. The tribals have in fact
protected the forests and their needs of forest wood
is so small in comparison to the unsalable hunger of
the urban centres for timber that it is sheer perver
sion to say that they are destroying the forests.
We therefore make a demand that these tribals
must be resettled only in Forest land, so that they
6
10th February, 1992
MEDICAL
01.
02.
03.
04.
05.
06.
07.
08.
09.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
EDUCATORS
REVIEW
MEETING
TENTATIVE
LIST
PARTICIPANTS
OF
JUNE
1992
Dr. Abraham Joseph, CMC-Vellore
Dr. Prem Pals, SJMC, Bangalore
Dr. Alex Zachariah, CMC-Ludhiana
Dr. Cherian Thomas, CMC-Miraj
Dr. D.K. Srinivasa, NTTC, JIPMER, Pondicherry.
Dr. Asha, JIPMER, Pondicherry
Dr. Kartikeya Nanavathi, NHLMC, Ahmedabad
CMET, AIIMS, New Delhi (Representative)
Dr. B. Ekbal, Medical College, Calicut
Dr. Ulhas Jajoo, MGIMS, Sevagraro
Dr. Slddarth Das, KGMC, Lucknow
Dr. M.K. Vasundhra, BMC, Bangalore
Dr. N.H. Antia, FRCH, Bombay (Special Invitee)
Dr. Palitha Abeykoon, WHO-SEARO, New Delhi (Special Invitee)
Dr. C.M. Francis, Bangalore
Dr. P. Zachariah, Vellore
- Advisers, Medical Education Project
Dr. V. Benjamin, Bangalore
Dr. George Joseph, Madras
Dr. Ravi Narayan, Bangalore
Dr. Thelma Narayan, Bangalore
Dr. Shirdi Prasad Tekur, Bangalore
CHC Team
Dr. Mohan K. Isaac, Bangalore
Dr. M.J. Thomas, Bangalore
IN ADDITION
One additional participant each from the 4 CMC’s to be
nominated by the Director/Principal (a faculty member who
is involved in Medical Education Reform) and whose costs
may be met by Institutional fund.
One nominee each from CHAI, CMAI and VHAI whose costs may
be met by the associations themselves.
* * ★ *
* ★
* ★
★
*rn/mk
(Continued from page 6)
can preserve their forest bound culture and way of
life. In raising this demand we are not at all pitting
ourselves against the ‘conservation of forest’ objective.
If forests are in danger, the tribals living in
forests are not basically responsible for it. The ob
jective of ‘conservation of forests’ and that of reset
tling the tribals in forests are not incompatible.
Indeed they could with imagination become comple
mentary objectives. We, however, challenge these
so-called developmental schemes which are destroying
both the forests and the defenceless tribals.
Conclusion
Through this report we have tried to bring to
your notice the plight of these oustees of the Narmada
project and the ambiguities and insensitivity of the
government rehabilitation policy. Our attempts to
bring about appropriate changes in the policy have
made very little progress. We need your help to tackle
this problem. We must act and act decisively if we do
not want to let the tribals drown in despair!
Further reading
Dams. Forests, Tribals and Health
1. The State of India’s Environment 1982
A Citizens Report from Centre for Science and Environ
ment, 807 Vishal Bhavan, 95 Nehru Place, New Delhi
110019 (1982).
2.
3.
Major Dams - a second look
LT Sharma and Ravi Sharma (Eds)
Environmental Cell, Gandhi Peace Foundation, 223 Deen
Dayal Upadhyaya Marg, New Delhi 110002 (1981)
Report of the Committee on Forests and Tribals in India,
Government of India, Ministry of Home Affairs, Tribal
Development Division, New Delhi 1982.
Hills, dams and Forests.
Some field observations from the western ghats by Madhav
Gadgil. Available from Centre for Theoretical Studies,
Indian Institute of Science, Bangalore 560012.
5. Forest, environment and People: Ecological values and social
costs Water Fernandes (Ed), 1983. Rs. 15-00
6. Peo pie and Forests: the Forest bill and a new forest policy
Desmond D’Abreo, 1982. Rs. 7-50
7. Towards a new Forest Policy— People’s rights and
environmental needs.
Walter Fernandes and Sharad Kulkarni (Ed), 1983. Rs. 25-00
4.
8.
Social Action
, ■
I S I Quarterly, April-June 1983 and .Ju1y-SePrte®berC4^
issues. (Nos 5 to 8 are available with the Indian .Social
Institute, Lodi Road, New Delhi 110003.)
I
/!/
10^
F) C C •€ kv
Of V)
The 'WARD' Strike-A View Point
— Sanjay Nagral, Bombay
the government would revoke the decision (which
meant displeasing people with the clout and money)
in response to the protest of a small section of the
medical community they were hoping for too much.
The twenty-eight day long strike by resident
doctors, interns and medical students all over Maha
rashtra to protest against the opening of three capita
tion fee based medical colleges ended a few months
ago. The withdrawal of the strike on just a no-victimi
sation assurance was regarded by many as total sur
render. Two of the capitation fee medical colleges
have already opened since then and plans have been
announced for many more. In that sense the strike
was a failure. It was, however, unique in many
senses. For example, it was the first time that the
MARD (Maharashtra Association of Resident
Doctors) was going on an indefinite strike for an
issue other than pay rise. It is important to analyse
the various aspects of the strike not just Because
there is a lot of ground for criticism but more im
portantly to make us better equipped to react to
such struggles in the future. As the interns’ represen
tative on the central committee of MARD and on the
negotiating team, I had the opportunity to have a close
look at the events during the strike, and in this article,
I shall try to analyse some of them in the light of its
failure.
Political moves have to be fought politically and
‘ ’i the present strength
" by political forces. And with
of the ruling classes and their
F
parties and their
total grip over the various state agencies,
^agitations many a times are likely to end
up wresting concessions of varying degrees
rather than changing decisions. It was with this undesstanding that some of us from. K.E.M. MARD
were proposing the idea of negotiating with the
government over the percentage of seats to be kept
on genuine open merit basis. In fact at one stage,
the government was ready to do so. What was dis
missed as a ‘compromise’ was in fact a tactical
move keeping the reality of the situation in mind.
A protest against capitation fees means a
protest against the right of the government to make
education a privilege of the rich and the moneyed.
But when a government is a puppet in the hands of
the capitalists, landlords and merchant class, it ulti
mately implies a clash with the strength of the rul
ing classes. This will necessarily have to involve
large sections of the masses, for whom even simple
medical education is a dream, for it to succeed. It
was these political realities that the MARD leader
ship failed to grasp. Although the strike did teach
quite a few lessons in cunning, ruling class poli
tics, by and large the attitude of the leadership re
mained immature and at times even opportunist.
And not in a few instances was this not due to inno
cence but a genuine desire for fast popularity and
personal gains.
First of all a few facts about the strike. On the
twenty second of June a one day token strike was
observed by resident doctors, interns and medical
students all over Maharashtra as a mark of protest
against the government’s decision to permit the
opening of three capitation based colleges at Karhad,
Satara and Pravaianagar in the State. A delegation of
the MARD was literally dismissed by the Chief
Minister who refused even to discuss the issue. A
decision was then taken to launch an indefinite strike
from the tenth of July, the call for which was given
by the MARD. The strike action by around 4500
residents was joined right from the start by around
1500 internees and later by around 8000 medical
students. It lasted for 28 days and was withdrawn
on the 6th of August with just a no-victimisation
assurance from the government.
To begin with, was the total lack of prepara
tion and ground work for such a big struggle. Many
assumed that just residents striking work and
paralysing public hospitals would bring the govern
ment down to its knees. That in the past, the demand
was always a small pay rise, was totally forgotten.
Then, there was the total lack of effort (except by
some sections) to involve the medical fraternity as
well as other sections in the struggle. It was not
surprising that many senior doctors and their organi
sations although generously offering a lot of sympathy
refused to join the strike. Most of them are so well
entrenched in the profession and have so readily
accepted to be a part of a corrupt and wretched
medical system that to take such a step would be to
invite the wrath of the very government to whose
tune they dance. The classical example was of the
IMA many of whose office bearers although openly
supporting the strike refused to criticise the health
minister or take action against her as a president elect
The origin of many of the drawbacks of the
strike and of its eventual failure lay in the fact that the
leadership of the MARD never understood or analy
sed the politics behind the opening of capitation
colleges. The government’s arguments in favour are
too nonsensical and ridiculous to merit discussion.
The fact remains that this was and is a political
move by the government to satisfy the powerful sugar
barons (and their children), earn quick cash and
at the same time build a pseudo ‘pro-rural poor’
image. The desperate haste with which some of
these colleges were started, flouting all routine
norms, the panic on the government’s part after the
court case was filed, showed that the government
had a lot at stake in these institutions. The crude
effort to break the strike by offering personal bri
bes and favours to some of the leaders, proved this
even more. And if the MARD leadership hoped that
(Continued on page 8)
6
n
MpC k/V'. I k'tm NV
(Continued from page 6)
of the IMA. There is no doubt, however, that if the
senior doctors had joined the strike, the impact
would have been much greater because of the total
paralysis of even the skeleton emergency services
that would have ensued.
Excessive faith and hope was placed by many
in the legal system to give a favourable decision.
The counsel for MARD bared it all very early when
he bluntly told us that the case against capitation
colleges was strong only as far as the ‘standard of
education’ part was concerned. That this legal system
does not consider ‘capitation’ as illegal and unconsti
tutional was apparent in the court’s verdict also. In
fact this ‘standard of education’ ploy was used time
• and again by the government during the negotiations
to trap us into discussing something irrelevant. The
minister would go to extreme lengths to point out
how the standards were being maintained and some
of the MARD leaders would very obligingly deviate
from the issue of capitation.
Mention must be made here of the role of the
KEM unit of MARD, for here a definite attempt
was made to broaden the base of the struggle. The
mass contact programme, street plays, public meet
ings and parallel out patient departments, were all
efforts to take the issue to the public Meetings of
trade unions and student organisations were held to
chalk out a more broad plan of action. It would be
appropriate to mention that very few trade unions
responded to the invitation and those, who attended
showed extreme lethargy to take any concrete action.
Thus, what was an excellent opportunity for the
working class movement to fight for a genuine issue
was lost. The gherao of an ENT Surgeon from
Bombay was deliberately planned to prove that mem-
Wz
bers of the profession who associated themselves with
these colleges should be exposed and attacked.
Two of the colleges have since then opened with
a lot of fan fare. Many more are being proposed.
These will start sprouting up with regular fre
quency, closely competing with engineering institu
tions . The fight therefore will have to be a prolonged
one. Organizations like the MARD cannot and
should not fight such struggles alone. This is the
work of mass organisations; trade unions and working
class parties. Science movements and organisations
like the medico friend circle must take up such issues.
Always keeping in mind however that it is the symp
toms of a wretched and rotting economic structure
that are being manifest, time and again. It should
also be borne in mind that non-capitation ‘open merit’
education although apparently giving equality of
opportunity is heavily loaded in favour of the rich
and the moneyed. This is especially true of higher
education. This is not very surprising since it is the
moneyed who rule. Capitation fees is just a more
vulgar and crude form of a degrading but crumbling
system. The only way to put a permanent stop to
such terrible obscenity is to strike at the roots of the
disease. Such struggles however have to be fought
and if fought with the right perspective can contri
bute a lot in this direction.
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Ceil team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent tos
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark's Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team.
Yours sincerely,
for DAF-Karnataka,
Gopal Dabade
To
10
This is shocking. If looked at from one angle it is
a great hypocrisy, on the other side, it is a great self
deception, an escape from reality, a coward attitude to
run away from the war front.
and can convince the patient about uselessness of
injections, He cures the severely dehydrated child
and is in a position to teach ORT. We may convince
the poor illiterate person about the ORT by our Health
guide, but unfortunately there is not a single doctor
to back this up on clinical front. He will even suggest
NBM* till Vomiting & Diarrhoea stops, if not, he will
laugh at the idea and since he is the person who is
going to give medicines to the same poor person, the
whole funds, time, efforts invested in ORT training
would be evaporated. This will happen and this is
happening. Direction of Health education is just
never from patient to doctor. It must be from Doctor
to patient. Unfortunately we neglect our Cure front
which is never in tune with Community Health as only
the money oriented doctors, quacks are ruling this
empire and our motivated doctors are running away.
What we object to is the basic character of the new
religion of community Health as it gives a so-called
rational basis to a running, frustrated, hypocritic
individual.
So we urge to face reality.
Prevention and Education, though sugar coaled,
are bitter capsules. We feel that though all the basic
principles of community health are to be accepted in
totality, the direction of its application is wrong. The
spread of community health principles will be visible
only if the cure system is changed. The person who
cures, and relieves patients from pain and death;
though not god, is the best person to educate people.
So whoever is concerned must enter this pond of mud
to fight the present dirty status.
The list is unending.
To start with Clinical Practice, to educate along
with Clinical Practice, to give patients correct and
cheap medicines to establish a rapport through cure
and to stimulate all patients to think is the basis for all
the community health activities in future. We can
not build up this future without a strong base. The
present situation on clinical front is just horrible and at
this moment the person who wants to serve the poor
must never leave ‘cure side’. The doctors shedding
this basic responsibility in order to serve the poor
through seminars, research, bulletins, ANCs, Balwadies, departments of PSM are Neros playing fiddle
when ROME is burning and sadly with the belief that
this playing fiddle is the ‘cure’ for the burning ROME.
One Doctor friend of mine sarcastically commented.
“Doctor cannot do much. It is your totally baseless
assumption.
He is just a policeman directing the
Journey of a patient from birth to death and above all,
taking, bribe for the same!”
It is basic commonsense that those who want to
bring something new must provide first, an alternative
to old & bad and that is what we are missing.
But it is not an easy joo to enter this ‘Cure Market’
with determination to serve ethically, academically
and with principles of community health in mind.
There is no thrill in it. The person who enters is an odd
one. Neither is he an exploiter nor a revolutionary.
As the funding agencies are now in pseudo euphoria of
community health, there are no funds available. To
open an operation theatre, a doctor has to invest up to
Rs 1 lakh. Banks charge him 15% interest irrespective
of where he opens. So he has to charge not just to
fulfil his own living requirement but to repay loans, to
pay servants. So in the eves of the poordie is just like
any other quack. Due to insistence that there are no
injections for energy, no tonics for weakness, no inj.
(I.M.) to accelerate labour, no cheap 5 rupees treatment
for chronic suppurative bronchitis, he loses patients.
So he has to live with fear in the mind, he has to live
in isolation. He has to spend empty hours. He has to
fight the frustration. In one sentence he has to wait
and wait endlessly. He has to take all the risk in the
world to go ahead and perform Ceaserian section on
a very serious patient, he has to adjust with available
help.
But there are opportunities to grab. He saves the
life of a patient by successful Caeserian section and now
can teach the whole village about ANC. He cures
fever persisting for two months with antimalarial drug
5
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent tos
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark’s Road
Bangalore 560 001.
by Sth February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team.
Yours sincerely,
for DAF-Kamataka,
Gopal Dabade
Tn
■
IC k
‘When Rome Is Burning’
"T
)0
DR. ARUN GADRE
DR. JYOTI GADRE
’ j a Private Nursing
(Now running
Home in Kinwat, Dist. Nanded)
rate pharmaceuticals with fourth rate combinations
with the help of quacks, half doctors, ruthless ex
ploiters rule the health of the poor person. The
poor landless labourer spends half of his income on
Bplex injections when actually he is suffering from
Pulmonary Tuberculosis. Later on takes some 15-20
inj of streptomycin with rifampicin for 15-20 days as a
starting treatment. Later he receives LV. Glucose as
a sure medicine to get cured. Lastly only death can
cure him of his extensive pulmonary T.B. A patient
with cold receives dexamethasone. Parents spend
money to buy tonics for their child suffering from
PCM. Old man receives five good bottles ol LV.
Glucose when suffering from congestive cardiac failure.
The woman in desperation spends hundreds of rupees
for 3 consecutive injections of E.P. Forte in order to get
an abortion done and finally ends up in 16 wks pi egnancy. She dies of obstructed labour in a remote rural
But still, this new religion of Community Health area where she has no access to an operation theatre.
is fast becoming an escape route for ideologically moti The market oriented specialist is not a fool to invest in
vated fresh graduates who do not want to enter the that area. The Govt. Hospitals are run by incompe
pond of mud of clinical practice. This is what we are tent corrupt doctors. And the social organisations are
worried about. On th'? one hand the majority of not nowadays interested in this routine clinical service.
trained clinicians are entering this golden rush with So the woman with obstructed labour must die. May
out a second thought. They give cut, take cut, from be she is well oriented to ORT, immunisation theoiies
rackets, join hands with Pharmaceutical industry and thanks to this new religion of Community Health, but
exploit ruthlessly.
Naturally we cannot expect she must die of obstructed labour. So the quacks do
these doctors to go into the rural, remote areas where MTPs. They give a 100 rupees worth magic spectacles
maigin of profit is negligible. And our young moti to ‘cure’ dataract as not a single motivated opthalvated doctor who is a potential candidate is leaving mologist is available to educate, to operate. (There
‘Clinical Practice’ to join Community Health Projects, might be somebody with a degree but now doing a
that too with a belief that he/she is really doing some- revolutionary work of finding out the Statistics of
Vit A Deficiency blindness). So the rural landless
thing for the poor.
labourer has to spend 2000 rupees in two years to get
cured of bronchial asthma as not a single doctor takes
This is a great paradox.
her Blood pressure in these two years so as to diagnose
The net result is, the internal brain drain. The her condition as c.c.f. due to severe hypertension.
person in whom society has made investment so as Thanks to our M.D. Physicians busy in debates about
to get him trained to ‘cure’ in return is leaving his ‘what is the ideal caloric diet for poor?’ in a seminar
specialised field to the very non-specialised Community at some posh resthouse in a Hill station resort support
Health sphere. The doctor acting thus does not under ed by a Foreign funding agency. So the poor person
stand the simple fact hat all the Community Health loses his confidence in existent rural Health Care
projects are just non-specialised simple jobs. So it is a system where he has nobody to go with expectation to
form of brain drain and this leaves the poor masses in get cured even for a simple ailment. And to serve him
rural are in the hands of quacks. The most horrified our potential doctors are going door to door urging
line of treatment is followed here, some out of igno him not to go to open air defecation as it will prevent
rance, some to exploit. The medical shops, the third him from getting all those illnesses.
Along with MFC, many organisations, institutes
and individuals are working to spread awareness
about Preventive, Educative and Social facets of
Health care which are neglected for long. The priority
of social service through Health is now shifted to
wards‘community health’. There is glamour attach
ed to it. All funding agencies are funding these
projects and there is a Pseudo euphoria for the same in
all the intellectuals. Fortunately or unfortunately the
methods of application of the principles of com
munity health are not rigid.
On one hand it calls for
innovation and on the other hand this leads to sheer
confusion and frustration. There are now doubts
expressed about its basic role and some even proclaim
that unless the basic socio-economic system is changed
through political action there is no use trying to
change the health care system.
4
----------- m**
I
*
^7
d
e
y
s
y
i
c
C
fc
J
&
The Cadres’ belief that society expects doctors to
‘cure’ is a very limited view of the field of medicine
and is perhaps the outcome of the curative orientation
of the present medical services and medical education.
The doctor is there to promote health, prevent diseases
and ix required cure and rehabilitate. So those who
practice community medicine instead of curative
services are not betraying the society; on the contrary,
they are serving the society much more efficiently.
1
>
•
The Cadres’ belief that community medicine
projects are “just non-specialized, simple jobs” seems
to be naive. If that were so, no one would have ever
known or honoured Aroles and Amte and many
more who carried out such projects. I would not
consider the organization of an immunization pro
gramme or teaching village people about ORT less
specialized or simpler than doing caesarean section
or operating a cataract. Only those who have done
both can tell us better which one is difficult.
‘When Rome is Burning’ by Arun and Jyoti Cadre
(MFC, 124), was a surprise. Their observations on
the ‘dirty’ state of the present clinical medicine in
India seems to be true and their contention that some
one needs to clean up the “pond of mud” is also the
need of the hour. But their views on the “new religion of Community Medicine” are not supported by
logical arguments or statistics.
The Cadres’ argument that most of the funds are
now put in community medicine is also not true, if
you take into account the local donations besides the
foreign agencies’ funds. Many more people still
donate money for hospitals, wards, or sophisticated
equipments than for community medicine. Their
prescription that one has to cure before prevention is
like putting the cart before the horse. It totally ig
nores the age old saying that ‘prevention is better
than cure’. Cure will be infrequently required if
prevention and promotional activities are very strong.
A woman may not have to die because of obstructed
labour if a well trained dai or an ANM is available for
proper antenatal care, and of course with clinical
back up. A child may not reach the stage of severe
dehydration if sanitationisgood and ORT is available,
In both theory and practice no community medicine
person worth the salt neglects curative services. On
the other hand hardly any clinician remembers to
practice community medicine,
t
?
I do not agree that community medicine has become an escape route for the ‘ideologically motivated,
frustrated and hypocritic individuals’. Community
medicine is as yet the most unexplored and difficult
branch of medicine. There are no set patterns of
progress in the field of community medicine; each one
has to find his/her own path. And that is where the
challenge lies. Such a field cannot be an escape route
for anyone. The idea of the ‘internal brain drain’
put forward by the Cadres is not supported by any
quantification. For instance, in Gujarat for the year
1981 (the latest figures available), 432 post graduate
degrees/diplomas were awarded; none of which were
in Preventive Medicine (1). The picture has not
changed very much since then. My guess is that not
more than 1 to 2 percent of doctors go in for commu
nity medicine. This miniscule proportion can hardly
affect the doctors available for clinical services; and
this would hardly qualify to be called brain drain.
Finally I do agree completely with the Cadres’
that the “clinical front is just horrible” and it does
need to be changed. But trying to do it at the expense
of community medicine will be like adding fuel to the
already burning Rome!
— Dileep Mavalankar,
Ahmedabad.
(Ref. 1, Health statistics of Gujarat, 1984, State
Bureau of Health Intelligence, Directorate of Health,
Medical services and Medical education, Ahmedabad.)
7
MFc B~
DEAR FRIEND,
The pressure of attempting to ethically practice
clinical medicine, and that too in a small town, is
such that one can appreciate the Cadres frustration
(MFCB, 124). Generally, the denunciation of co
mmunity health arises from the fact that people tend
to confuse it with the type that is taught and practised
by the PSM departments of our medical colleges. It
is also true that philosophical discussions can be highly
irritating to one who is struggling to perform an
emergency caesarian operation with meagre resources,
in a near hopeless situation.
I wish to assure the Cadres that the HealthWallahs who attend seminars, gather statistics on
Vitamin A deficiency blindness and run bulletins
(how neatly I fit into this) are too small a number to
be bothered about. (They can take a lesson from
the govt, as to how to ignore us!) We are in this
either because we want to earn name and fame instead
of money, vthey are not the ignored lot) or because we
are social drop-outs: Bless us, but without us where
else could the Cadres find a forum to express their
genuine frustration. If there is no religion of co
mmunity health, we will find or invent some other
creed, but would never enter the portals of the estab
lished church of clinical Medicine. Neither clinical
medicine nor community health either gain or lose
anything, by our presence (or absence).
^cn~)(L
C y.^on/^')
to
)!>'-
f 7' s
latter is the real internal brain drain, and hence we
feel that today whether a doctor is in clinical medicine
or out of it, is immaterial. There is no genuine clini
cal medicine. What we are forced to practice today
is a non-specialised simple job, and have no scope for
the “very specialised field”.
Yes, Rome is burning, but the Neros are in Delhi.
Their fiddle screeching is so loud and atrocious, the
people’s wails are drowned in it. If doctors really
want to practice good clinical medicine, they should
join us with kettle drums and trumpets, so that the
Neros in Delhi can no more ignore us, and more
important cannot ignore the people.
Kamala Jaya Rao
(A social Dropout)
Hyderabad.
*
*
*
“How many of the existing public or private
community health projects are engaged in pure re
search or community health activities without provid
ing curative care?”... “What proportion of the
thousands of doctors passing out of medical colleges
opt for working with such projects rather than entering
into medical (mal) practice?”... “And what propor
tion amongst those clinicians interested in community
health research are researching into areas absolutely
unrelated to their training in clinical medicine?”...
However, a word about community health in its
correct perspective. It is not preventive medicine.
It is wrong to think there is no ‘cure medicine’ in the
practice of community health. As long as there are
diseases in the community, they need to be treated.
There are many who are doing this successfully, the
most well-known example being the Aroles of Jamkhed. The role of clinical medicine in community
health is neither denied nor denounced.
The answer to all the above questions is common
and that is ‘Negligible’. The reasons are obvious.
Of the small minority that wishes to be away from
the muddy ditch of private practice, a few resort to
working in community health projects not always
because they have tried and failed to settle down in
practice but chiefly because most of the community
health projects are located in or around urban areas
and also provide curative service to the people. A
common problem faced by community health agencies
wherever they are working has always been a dearth
of devoted and motivated doctors. The Cadres’
fears about internal brain drain are, therefore un
founded.
However what is it that organisations like the
MFC are crying about? The Cadres have, for
instance, mentioned malaria and ORT for diarrhoeajust two examples; the list does not end there. The
question is not whether to treat diarrhoea, with ORT
or antibiotics, (he issue is not about which are the first
line drugs for tuberculosis. Our main question is,
why are these diseases allowed to exist, the degree
that they exist, in this age of super-computers ? In
short we are asking for community health and not
community medicine. We would like a situation
where we can apply our brains and our skills to treat
diseases that really need treatment, and not dispense
vitamin A drops, teach how to prepare ORT etc. The
Comparing a handful of research organisations
and the preventive and social medicine departments
to Nero playing the fiddle when Rome was burning
is grossly underscoring the importance of research in
community health. What research is being conducted
at these places and whether it could be made more
meaningful and applicable could be a point of debate
and it is for doctors like the Cadres to raise their
7
f To
_______________
voice against wasteful research and pin-point areas
where it is needed most. The answer is certainly not
in the packing up of these institutions or leaving them
completely in the hands of the non-medicos, driving
the clinicians working with them out to remote areas
for practising curative medicine. A clinician’s close
association with the researcher is a must to identify
areas of research that would prove relevant and useful
and to see that the outcome of the research is appli
cable to tackle the problems in the field. The right
place for the best of our motivated brains should
always be with the researchers. Unfortunately,
this is not the case. The fault probably lies in the
system that discourages and fails to attract these
brains away from the lucrative business of private
practice. One would call it a welcome change if
more clinicians than there are now, opt to join co
mmunity health service and/or research.
R.N. 27565/76
amount of inputs into curative care is going to help
us solve our problems for good. The state of health
of the vast slums of Bombay is a living example, Coordinating with a community health agency to spend
and manage safe drinking water supply to an area
would be far more advantageous in the present cir
cumstances than coercing a handful of clinicians to
give up research to treat diarrhoeas, dysentries,
dehydration and worm infestations.
The research in community health, if relevant and
useful must continue on a priority basis.
—Mukund Uplekar
FRCH Bombay
I
The burning problem of poverty of curative care
amidst plenty of medical hands may be solved not by
individual doctors to set-up their practices in the rural
areas just because they claim to be motivated or that
they believe in ethical practice, but by:
(a) Strengthening the infrastructure in remote
rural areas by the public sector/government
policies.
ro
(b) making doctors, after they get the qualifica
tion, work in remote rural areas for a stipulat
ed period of not less than a year, before
allowing them to make their choice.
(c) making the voluntary agencies work more in
the areas where they are needed most.
It would be unwise to compartmentalise curative
medicine and community health. With the over
saturation of urban centres with medical practitioners
and saturation even in the semi-urban areas, doctors
will be forced to go to villages to earn a living but no
i
I
HFc flDear Friend,
When Rome is Burning:
^-'0
<
A“~O
1.^3
* g
;._w
<
v)
■~s
““G
I"0
“^D
“~G)
“7?
-
-r3
~rJ
Gd
7Mcm/ /9 S7 C
z)
)C)
waste a moment to seek curative medicine when they
are in need themselves. It is common experience
that the teachers of Self-Helt immediately rush to
wards a modern hospital or a nursing home when
their own dear ones are in trouble. As the Indian
sage once said, to a hungry person God must approach
in the form of food, health activists should realise
that to moribund patients, preventive medicine or
community health carries no meaning at all except
ridicule.
Dr Arun and Jyoti Gadre’s article (mfcb-124)
has brought in a whiff of clean air of realism in the
prevaling intellectual and eruedite atmosphere of
the mfc bulletin. The article makes its entry as if
like a bull in a china shop and pierces holes — I lost
count how many, — in the padded framework of
progressive health debate. I appreciate it for the
simple reason that we, in West Bengal, have been
Cadres assert that the doctors who are engaged
working.so long with the same view in mind. Health
in curative practice are the best persons to educate
activists (for want of a better term), who have been
people in Health matters. I am hesistant to make
crying for a people oriented health care service, have
such a bold declaration. But I can guess at what
somehow been shunted into a world of their own,
they want to imply. A health care system cannot
isolated from the real health scene. That is why
be run without a sound medical care service. Even
they did not find it necessary to identify the real
in a heavenly world where all preventive techniques
actors in the health drama being daily enacted in
have been exhaustively implemented, diseases will
real life, before prescribing roles and revising scripts.
still occur and medical care be needed. In a country
Gadres’ article, though a little bit strident and some
like ours, basic determinants of health like food,
what emotive does just that by focussing the attention
clothing, shelter, employment, education, women’s
on the real priorities. It is time for even the elitist
lib etc., cannot be realised without a fundamental
and snob section of the health activists to realise
political and economic change. It cannot be achiev
that as a slogan ‘prevention is better than cure’ is
ed by parallel social efforts, (termed grass root actions)
no longer the in-thing in fashion. The sincere and
keeping the State apparatuses in the hands of the
serious health activists, particularly those with left
exploiting classes. People must win power in order
orientation, should stop to give a second look to the
to realise the basic health determinants for them
political, social, economic and cultural realities of
selves. And, one must admit that peoples’ struggle
the attractive populist formulations. True, that
in that direction will continue in spite of the health
curative medicine can never be the answer to the
activists. But one cannot allow the premature deaths
problem of ill health, but preventive and social cannot
and avoidable disabilities-till the end. What the
be delivered without a political vehicle. Health
health activists, at present, are required to do is to
planners may imagine that they are offering a novel
join the people in their demand for medical care and
path of salvation to the people by raising the slogans
force the ruling classes to concede the demand.
of Community Health, Self Care, People’s Health
in People's Hands, Demystified Medicine, Integrated
It is sad that the health activists overlook the
Medicine and what not. But these have not been
emerging phenomena that the ruling classes have
able to attract people’s attention. People, who
borrowed a leaf out of the progressives’ manifesto
struggle to earn their daily bread just cannot afford
and lent their voices in chanting the glory of preven
the luxury of shunning life-saving modern medical
tive medicine, community health, self-care, indigenous
care in their own desperate situation. Rakku’s
medicine etc. and that is how they proceed to arm
story (Sheila Zurbrigg) dramatically exposes the
their slogan ‘Health for AH’. Prevention is. the
options before the people. People’s need of the
answer — so stop offering medical care to the poor.
hour is medical care and that is what they demand.
The recalcitrant poor however, refuse to digest the
There is no real contradiction between their need
brilliant proven theory of preventive medicine and
and demand as the specialists would have us believe.
community health, and had already tasted the fruits
It may be true that there are matters where people
of modern medicare which they continue to demand.
do not understand what is right as the specialists
. But you cannot provide the poor with costly medicare
do. But it is not universally true. There are sub
and maintain the profit rate too. So give them a
jects where people can very well realise what is right,
cheaper alternative and here comes the allocation
in spite of the specialists’ efforts to confuse the issue.
of 1/3 rd of health budget to indigenous medicine
Health, I guess, is one of the latter subjects. Here,
in the 7th Plan. Take care — that the people do not
direct observations and real life experiences are
look upon indigenous medicine as a pseudo. On
eminently helpful. People have observed that
the one hand, invoke the glory of Indian tradition
vociferous protogonists of preventive medicine never
and precious people’s culture, and on the other,
7 expose the heinous exploitation of the modern medical
practitioners. This will do the trick. The trick is
perhaps succeeding and the Government appears
to be getting away with it. But why the health
activists should turn a blind eye to the people’s urgent
need of life-saving medicare? The Editor however
asks a pertinent question. “Can one really practice
ethical, quality curative medicine in the present
socio-economic set up without the crutches of tonics,
injections and other magic remedies? How often
does it end as a conflict between survival and service?”
O.K. then, — let us put the blame on the socio
economic system and not expect the doctors to act
as noble men and women. But how come commu
nity health appears as an alternative?
Sujit K Das
Calcutta
il
ID
I
r?
Dear Friend,
When Rome is burning:
A man lives by his stomach. When his diet is
balanced and his environment sound, he remains
healthy. But are many of our countrymen able to
have a balanced diet? Eating to subsist is their
first priority
keeping healthy their next.
The conclusion is that well-equipped curative
centres can only cater to the middle class and better
off citizens. Fn the above mentioned case, the really
poor did not attend the curative centre because they
could not afford the fees however low. They went
to a Government Hospital or died at home.
45 to 50% of India’s population is below the
poverty line. (A landless labourer who can spend
Rs 2000/- ie. Rs 80/- p.m. on medicines over a period
of 2 years is probably above the line). It is not
surprising that “ideologically motivated fresh graduat
es”
and not so fresh too, should opt for Community
Health. Of course, this can be questioned if they
just limit themselves to seminars, research, etc.
So the poor have no choice besides Govt. Hospi
tals. F do not agree with Arun and Jyoti Cadre’s
sweeping statement that Govt. Hospitals are run by
incomPetent and corrupt doctors.. Some might be
incompetent and many corrupt. Nothing can be
done about the incompetent unless they are caught in
flagrant incompetency
Remember they have been
trained in the same institutions as those in the rest of
the country including the Gadres and the ideologically
motivated doctors.
The majoi focus of Community Health appears
to be Prevention. But prevention alone is not the
answer, I agree. Curative services are important.
But Community Health includes above all EDUCA
TION.
As regards corruption, it exists not in Govt
Hospitals alone. It also exists in Private Practice.
And corruption can be tackled if there truly exists a
COMMUNITY Health Program which includes
‘Education’.
In a rural town in Maharashtra curative services
were offered by a non-governmental organisa
tion. To be of greater service to the poor commu
nity, the doctor trained in general surgery and set up
an operation theatre. Maintenance required raising
of fees
though they were kept low. However in
the 5 years after setting up the operation theatre just
2 Caesarean Sections were performed and those too
on women who could afford going to better equipped
places.
Education to what?
— To how the PHC is administered and one's rights
in obtaining services whether free or in certain
cases fairly low fee.
— To the use and abuse of injections, prescriptions,
diagnostic procedures by GPs, Specialists, and
Govt. Doctors.
— To the Pharmaceutical Fndustries, including the
MNCs, aim of making profits through means
fair or foul.
And finally, an idelogically
motivated doctor who forms part of the
community he/she is working with,
will not rest satisfied unless the
socio-economic conditions of the
community is improved.... for only
then can she hope to achieve
COMMUNITY HEALTH.
Marie D1Souza
Nandurba
3
6. What do you expect will emerge from such a Workshop?
7. Any other relevant/related issues?
I
Please fill in this form and return it to
The Co-ordinator
Drug Workshop
Community Health Cell
47/1 St Mark’s Road
Bangalore 560 001
by 5th February 1989.
i
V
M.FC
Jc
/
/
10
I Dh^u>v
bVHAt
bu-r) I VI/*'
U
’
-JUl/
The debate on 'medical care vs community
health', which started with the Cadres high pitched
cry of "Down with Community Health" has
reached a stage when, all parties concerned, need
to pause and clarify a number of issues. First,
neither Cadres nor Kamla Jayarao, Uplekar------ and
now Das, have clarified what they mean by the
term 'Community Health'. Though, Kamla Jayarao
has given us some glimpses of what she has in
mind by implication, she has still responded only
tangentially to Cadres' attack on community
health.
Cadres' main complaint is (1) it is almost
'criminal' for doctors trained to deliver medical
care to go into community health; (2) such a
'capitulation' is indeed glorified by the health
establishment including the funding agencies.
What we are not told very clearly is, whether they
are against community health as such or, against
community health by doctors alone.
Das has now
joined this debate by enlightening the "elitist and
snob sections of the health activists" that the slogan
"prevention is better than cure is no longer an
in-thing in fashion" and also that "to a moribund
patient .. community health carries no meaning
i—
except ridicule."
Cadres seem to have completely misunder
stood what community health really is and there
fore their attack is, in fact, a 'non-attack', attacking
what at present goes in the name of community
health (with some notable exceptions though).
Das, too, confuses the issue further by flocking
together community health with other equally
unclear terms like self-help.
Therefore, let me try to clarify what, accord
ing to me, is meant by community health.
"Community Health is .... a way of looking
at the problem of dealing with ill health in inchvi-^
duals in their social, biological, and physical
setting? Community Health has at its focus both
individual and environment. Community Health
is .... about the health of all the individuals in
the community", (emphasis mine) (1).
The
specific tool of Community Health approach is
Epidemiology besides the conventional tool of
clinical medicine.
Community Health is about asking the ques
tion 'why did this child suffer from pneumonia in
the first place' after treating the moribund child
with bronchopneumonia following
measles—a
5
ro
child whom Das is so anxious to save.
Further
it is about asking, the question—why do so many
children suffer and/or die from pneumonia follow
ing measles in the locality where a doctor practices.
It is also about asking the question 'why does
tuberculosis persist in the community despite 20
years of the National Tuberculosis Control Pro
gramme and with extremely potent anti-tubercular
drugs like Rifampicin available. In no way does
it preclude treating an individual suffering from
tuberculosis but it certainly prevents a doctor
getting the wrong idea that by modern, medical
care alone—and thus by modern medical doctors
alone, tuberculosis can be controlled. Community
health approach by placing the illness that pre
sents itself at the clinic—which is often the tail
end of the disease process—in the community, it
places medical intervention in its proper place:
amongst many other types of interventions namely,
socio-economic, political and cultural, all of which
i
I
exercise in ideological rationalisation of the profitoriented, often irrational and incompetent, as well
as the over-glorified practices in clinical medicine.
Does he really believe that the thousands of doc
tors who flock every city/town in the country are
really busy saving people's lives, all or even most
of the time? What about cough and cold prac
tice, and un-necessary medications, injections as
well as surgery? What about cut-practice? What
about the activities favouring pharmaceutical com
panies wittingly or unwittingly?
Or should we
not diagnose and treat the deep rooted disease
that afflicts the 'noble' profession because every
body else is also suffering from the same disease?
Like the omnipresent 'foreign hand', Das invokes
the ruling class's attempt to push forward indigen
ous medicine and self-help and its attempt to
denigrate modern medicine in order to, destabi
are needed to do away with a disease.
ill
I
■ihJ
lize' it There is some truth in this theory, no
doubt. But is it not also true that it is the very
nature of modern medical practice at present that
has provided the ruling class the ground for crticising it and utilising the criticism to deny modern
Secondly, contrary to what the Cadres and
medicine to the people?
Das seem to imply, community health is not (and
should not be) a separate discipline. Though a
Dhruv Mankad, Nipani
doctor can (and should) obtain special skills in
epidemiology, there need not be community health
References
doctors as there need be surgeons, physicians, and
gynaecologists. It is possible and it is imperative
1. Ashvin Patel and Anil Patel; A note on
to impart a community health orientation to clinical
teaching of community health—A Critique ;
medicine. For instance, a doctor who is able to
Background paper presented at the X
see that a TB patient is unable to come to a Dis
Annual Meet of MFC, 1 983.
trict TB Centre for his/her daily stretptomycin
injections because it is WKms from his/her village
and s/he is too poor to afford the bus fare, has the
community health perspective. Or a doctor who
perceives a pattern in several patients of infective
*
*
*
*
hepatitis coming to his/her clinic from a particular
locality and demands that the water supply of the
locality be tested is practicing community health.
Today, an epidemiological outlook in clinical prac
tice is'becoming all the more important to a clini
cian because of the appearance of iatrogenic diseas
es. Side effects and toxic manifestations of a
a drug do not become obvious unless the treating
doctor carefully looks for unusual symptoms in a
number of patients consuming the drug in ques
tion. Forming of even such impressions on the
basis of observation is community health, in the
broadest
sense
of
the
term.
Finally, Das' attempt, to defend the existing
status of medical practice by absolutizing an impor
tant but only one of its aspects namely, the "much
needed life saving medicare" is nothing but an
6
0
(
C.,
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kittur*
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent to?
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark’s Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team.
Yours sincerely,
for DAF-Karnataka.
Gopal Dabade
Tn
n pc
•V •
{
w iQtvx .c
Dear Friend,
'0
Inspite of being one of the 'cowards' myself I
share the basic point that the Cadres have made in
their article 'When Rome is Burning' (mfcb-124).
In fact it is from the point of view of community
health itself, defined in its broadest and most
political sense, that I see the need for more attempts
at and experiments in clinical medical practice.
The process of evolving an alternative health system(s) has to include alternative ways of clinical
practice. Community health theory has to in
clude an analysis of existing clinical practice
(which it has to a large extent) as well as evolve a
system of curative health activity conducive to
our notion of an egalitarian, human, health system.
But any theory evolving in a vaccum is meaning
less. Theory and practice together can be the
only way of working out any socially meaningful
alternative.
Of course, clinical practice alone has its limita
tions. But don't community health activities alone
have their own limitations as well ? Curative
medicine always ends up forming an important
part of any such programme and most of us fall
back upon the conventional form of clinical prac
tice. However, our major impact in terms of the
message carried to the people is often through
the curative services rendered because they are the
ones felt to be the most needed and relevant by
the 'people' themselves. It is the most important
contact point and a major need. But as yet, I feel,
that we have failed to evolve modes of clinical
practice in accordance with our understanding of
the existing and of the desirable health system:
the doctor-patient relationship, technology to be
used, the approach
towards 'treatment' and
'healing', the holistic vs partial view of a patient/
person, the balance to be struck between treatment
as human intervention and allowing nature to do
its own work in the healing process etc. etc... Not
that all these issues have been theoretically resolved
as yet but neither can they be without trying out
various options in practice and testing their vali
dity in the social reality rather than as we think it
to be.
All I'm trying to point out is that it isn't a ques
tion of clinical practice vs, community health work.
They are both a part of and complementary to each
other. Both are socially relevant from a radical
progressive view point if undertaken with certain
4
Rttsr?- i
value positions and with attempts at fresh thinking
and innovative action in response to the social
reality around us. One can understand the reac
tion of the 'community health wallas' to curative
medicine because of the overriding emphasis on it
with neglect of the social aspects and because of
the nature of curative medicine in the established
health system. Unfortunately it has also resulted
in our acquiring a 'holier than thou' attitude border
ing on the contemptuous towards clinical practi
tioners, even those trying to practice honestly,
ethically and creatively. This is what the Gadres
are reacting against, and therefore the extreme
positions and strong language that they have
used.
And this kind of clinical practice is in many
ways a much more difficult task than that of keeping
one's hands clean and staying out, engaging either
in safe, 'clean' work such as a community health
project doing preventive, educative and social
activities or engaging in 'research'. To be able to
hold one's own and work amidst others who are
corrupt, within a system which can easily elimi
nate, amidst a clientele which demands a certain
kind of services which it has been habituated/
addicted to is an extremely intimidating task,
full of frustration, helplessness and the fear of
getting carried along with the tide. It requires
much greater strength of conviction and an inner
strength to be able to Fiold out. It also requires
the ability to innovate and creatively use available
resources in accordance with one's critique of
prevalent medicine and clinical practice, Mutual
support and exchange of experiences could be
most helpful in such a situation.
Therefore if we see the two (clinical practice
and community health work) as parts of a whole I
would consider it important to support and en
courage clinical practice of the kind referred to.
I wonder if mfc can become, besides a group of
doctors and others focussing on community health,
also a forum for discussion and debate on ethical,
innovative clinical practice. The mfc bulletin can
probably be used to initiate the dialogue among
such clinical practitioners and between them and
those focussing on community health. Later a
separate cell could be made for this if the need
arises making the mfc, as I see it, more 'wholistic'.
Or may be a separate organisation becomes neces
sary, but that is yet far in the future.
Ritu Priya, New Delhi
vC
fvi C " 5> 6vvxA
medico friend
circle
bulletin
106
OCTOBER
1984
Special Issue : Child Health
“
CHILD
HEALTH
IN
INDIA
What is our commitment?
“Real and lasting improvement in the condition of our children can be brought about only through
successful
attack on the basic problems of poverty and social injustice and not through adhoc palliative
a
programmes
if we have to successfully attack these problems, the concept that human resources
represent a most valuable national asset must become the central theme of our national developmental
strategy
— C. Gopalan, Jawaharlal Memorial Lecture, 1979.
The selection of the theme — “Children’s Health
— Tomorrow’s Wealth” by the World Health Organi
zation for the year 1984 has once again focussed
attention on the urgent need for action on behalf of
the world’s children, many of whom continue to die,
get diseased and disabled in numbers and in condi
tions that are scientifically and socially unacceptable
today. Five years ago the International Year of the
Child (1979) generated enthusiasm and awareness
on the needs and rights of children on an unprece
dented scale. Action programmes were initiated and
expanded and long term plans were drawn up.
Mounting evidence in recent years has, however, shown
that the ability of nations to transform this enthu
siasm into action has been limited.
even wider than the immediate results of poverty
like lack of food”. This is a strong indictment of the
lack of governmental, professional and social/public
commitment to the National Policy for Children
adopted a decade ago (1974) which stated that the
‘nations children are a supremely important asset
and their nurture and solicitude are our responsibi
lity’ .
A UNICEF (1984 b) study has shown that the
world economy in the 198O’s has been in the deepest
and most sustained recession since the Great Dep
ression of 193O’s. Due to falling family incomes and
cutbacks in government investment in welfare and
education, there has been great deterioration in the
lives of children, who are most affected by these events.
The study reports that India (also China) has been
least affected because of past economic progress and
relative self-sufficiency. However, the situation of
children in India is not vastly different from the rest
of the developing world. The year 1984 could well
become the starting point for an analytical review of
the situation and a commitment to concerted action.
Is this happening?
First there is a wide disparity between States in
the magnitude of these indicators., eg. IMR in
Kerala is 40 while in UP it is 159. Uttar Pradesh,
Madhya Pradesh, Bihar, Gujarat, Rajasthan, Assam,
Orissa and Haryana form a critical infant mortality
belt (all above 100).
Situation of children in India
A UNICEF report (1984 c) published recently
has found that “of the more than 270 million children
of India, the number who have access to an essen
tial minimum of nutrition, health care a^id learning
opportunities may be less than half. Indeed the
effects of ignorance and ill-health seem to have spread
The important findings of this report are sum
marised in Box I. The demographic, health, nutri
tional and social indicators available on the situation
of children in India present a grim picture. Hidden
in these very numbers are further important aspects
of our social reality.
Secondly, there are wide variations between
rural and urban areas, and within each of these situa
tions, between the well-to-do and the disadvantaged
INSIDE
Book Reviews
Children’s Health Tomorrow’s Wealth
— progress or platitudes
Child Care and Punjab
Reccomendations on Breast Feeding
Dear Friend
Keeping Track
5
6
9
10
11
12
I — SITUATION OF CHILDREN IN INDIA
(some indicators)
A.
DEMOGRAPHIC
Population below 15 = 255 million
Rural = 204 m.
Urban = 51 m.
Children below subsistence level
Rural = 55%
Urban =45%
Infant Mortality Rate. = 114
Rural =124
Urban = 65
Infant Mortality:
Almost half (47 per cent) the total number of
deaths occur in the age group 0-4 years. About a
third of all deaths occur in the first year of life.
Nearly a fifth of all deaths occur in the first month
and about a tenth of all deaths occur in the first
week.
Female Mortality: Higher in 1-4 & 5-14 age
groups. Life expectancy at birth: Male = 55.1
Female =54.3
B HEALTH
Malnutrition = 23% of under fives
Anaemia = Under 3 = 63%, 3-5 = 45%
Vit. A Def. = 30000 blind/year
Tuberculosis =1% per year
Leprosy = 0.64 million
Measles =14 million per year
Diarrhoea = 1.5 million deaths per year
Poliomyelitis = 0.2 million per year
Immunization coverage: DPT = 38.2%
Polio = 17.7%
BCG = 8.8%
C.
SOCIAL
Pre-school education: 5% of 3-6 group covered
School education: 75% are enrolled in primary
and middle school age group
Water supply: 163 million have no access
Child labour: 16.3 million are working
Disabled children (in thousands)
Blind = 250
Deaf = 250
Orthopaedic = 500
Orphans = 18000
Mentally retarded = 2300
— An analysis of the situation of Children in India,
UNICEF, 1984.
sections of the community eg., in 1978 the IMR in
rural and urban India was 136 and 70 respectively
but for scheduled castes as a separate group in the
same situations it was 159 and 90 respectively.
almost no national multi-sectoral studies that have
established a wide data base as well as an indepth
analytical framework”.4
Interventions in Child Health and Welfare
Thirdly, when these indicators are separated out
on a sex basis, the situation of the female child is
found to be uniformly poor reflecting the social discri
mination against females in health care and nutrition,
which is an all too common factor in our social life.
The history of interventions in child health and
welfare in India may be broadly divided into three
phases.
I — Pre-iDdepeadence :
Fourthly, the reliability of these indicators is
itself open to question. Many of these indicators are
extrapolated to national levels from micro-level data
collections which often have an urban bias. In re
cent years the sample registration scheme, the model
registration scheme and the national nutrition moni
toring bureau are helping to make available some
reliable data for purposes of planning. However,
anyone who has had occasion to witness the dynamics
of record-keeping and record ‘cooking’ in our health
centres will realise that for a long time to come
statistical indicators based on records of questionable
quality kept in our health centres, hospitals and dis
pensaries are bound to be misleading. The reality will
always be much worse.
This phase was marked by little or no involve
ment of the State in child welfare. Many pioneering
child welfare agencies of the voluntary sector were
established during this period. Balkanji Bari and
Children’s Aid Society (Bombay) and the Guild of
Service (Madras) are the best examples.4 However,
all of them were urban based and institutional in their
approach.
II — Post-independence (till the seventies)
The constitution of India pledged support to the
needs and welfare of the child but the first two five
year plans saw not even a mention of the child.
However the establishment of the Indian Council of
Child Welfare (ICCW) in 1952 and the Central
Social Welfare Board (CSWB) in 1953 helped to
mobilise voluntary activity in all the States on behalf
of children’s needs and welfare. Through grants-in-aid
to voluntary organisations, both these organisations
supported balwadis, nursery schools, creches, orphan
ages and rehabilitation centres. However, the stress
was on the charity and welfare dimensions streng
thened through the institutional framework of the
services. As in previous years, the focus was on ur
ban areas though the balwadi programme (fid reach
An Asian Conference on Children and Youth
held in Bangkok in 1966 observed that “one of the
serious problems affecting the preparation of deve
lopment plans for children is the prevailing lack of
sufficient data on the nature and extent of children’s
problems.”4 Eighteen years later the quality of data
available on children in India is definitely not a tri
bute to the large number of research personnel, insti
tutions and statistical services that we have in the
country. The Central Statistical Organization have
themselves bemoaned the fact that “there has been
2
pG-
I t c-H kv
"The National Policy Statement on Children
(1974) was the next major event. It sought to pro
vide adequate services for children both before and
after their birth conducive to their physical, mental
and social development. It was envisaged that the
National Children’s Board and two national institu
tes — the National Institute for Public Cooperation
and Child Development (NIPCCD) and National
Institute for Social Defence (NISD) established for
this special policy would plan and coordinate a series of
programmes organised through the Ministry of Social
Welfare. These programmes would offer health and
nutrition services; free and compulsory education upto
14; pre-school education and non-formal education
for school drop outs; physical education and recrea
tional, scientific and cultural activities; programmes
for disadvantaged and disabled children, protection
•against neglect, cruelty and exploitation; control of
child labour; relief in times of natural disasters; child
welfare legislation and attempts to strengthen family
ties through the organised services.4
some of the rural areas through the organisation of
• supportive mahila mandals. In the third plan at the
instance of ICCW a Child Welfare Plan was contem
plated but beyond a few integrated child health pro
grammes like the Indo-Dutch project at Chevella
Block (Andhra Pradesh) and some balsevika training
programmes nothing much materialised.4
in — 1970 onwa
In the last fifteen years the child in India has
for the first time found a separate niche in our plan
ning exercises. Children are beginning to be consi
dered as an economic asset in whose health, welfare
and education the country should invest.
In the early seventies, special nutrition pro
grammes trying to integrate health care, nutrition and
health/nutrition education were launched. These were
the special nutrition programme (SNP), applied nut
rition programme (ANP), mid-day meal programme
for school children (MDMP) and more recently the
world bank supported Tamil Nadu Nutrition Pro
gramme (TNP). These programmes helped in creat
ing a general awareness and some organisational base
for future programmes in terms of centres and field
workers. However, there were major weaknesses which
prevented them from making much impact. Limited
financial resources, poor project formulation, inade
quate monitoring and feed back systems and lack of
community participation were the most important
among these.6
The Integrated Child Development Services, a
package plan for 0-6 year olds in urban slums, rural
and tribal areas launched in 1975 was the foremost
of these proposed programmes. Starting with 33 ex
perimental blocks, it was increased to cover 620
blocks in 1982-83 and is expected to cover 1000 blocks
by 1985. (See Box II and III for overview and evalu
ation) . This programme which in its magnitude is
probably the largest one of its kind in the world is
II — INTEGRATED CHILD DEVELOPMENT SERVICES (an overview)
Objectives
Package of services
1.
Reduce malnutrition, morbidity and mortality
in 0-6 years
— supplementary feeding;
2.
Improve health/nutritional status
— immunization and health check up
3.
Provide environment for social, physical, psycho
logical development
— referral services
— nutrition and health education
— pre-school education
4.
Enhance child care ability of mothers.
— non-formal education for women
Coverage
Organizational set up
1975-76 — 33 blocks (experimental)
1982-83 — 620 blocks
1985
— 1000 blocks
(Total no. of blocks in the country = 5011)
Ministry of Social Welfare at Centre/State level
Block : BDO coordinates with Child Develop
ment Project Officer (CDPO)
Village : Anganwadi for every 1000 popula
tion with anganwadi worker offering
services.
Financial outlay
(1982-83) per project in rupees
Rural =1.5 million
Tribal = 0.95 million
Urban =1.68 million
(costs include costs of staff, strengthening PHC,
recurring cost of medicine and POL, supplemen
tary nutrition and non-recurring costs).
— ICDS — An Assessment
UNICEF, May 1983
Beneficiaries (by 1985)
Immunization and Health Care = 10.3 million
Supplementary Nutrition:
Children =6.1 million
Women =1.1 million
Mothers with non-formal education =3.4 million
3
HI—INTEGRATED CHILD DEVELOP
MENT SERVICE (An assessment)
Positive Points
* 60% of 0-6 age group covered in areas of
operation
* 62% of children from poor families were
covered
* More children received immunization/nutrition services in ICDS areas as compared to
non-ICDS areas depending on regular PHC
services
* Immunization coverage was beyond 50%
* Cost of Anganwadi is Rs. 12 per year per
beneficiary over and above the cost of health
services infrastructure
Negative Points
* High drop out rate in serial immunizations
* Vaccines not available regularly
* Poor arrangement for referral services
* Important drugs not generally available espe
cially in rural/tribal blocks
* Visits by medical/para medical staff irregular.
Busy with family planning and other campaigns
* Personal hygiene of children poor
* Severely malnourished children detected but
no special diet developed. Food supplement
merely doubled
* Community contribution and participation
poor and adhoc
Problem areas
* Quality and applicability of training
* Magnitude of community involvement
* Regularity of delivery of supplementary food
* Social/cultural barriers which limit participa
tion by certain castes
* Weak link between the grass-root level worker
and the block.
— Krishnamurthi & Nadkami (1983)5
B. N. Tandon et al (1983)5
the symbol of this new and definite commitment to
comprehensive child health and development in the
country. How far this change of focus and effort will
be sustained and supported only the future will show.
ponents that will make major impacts on child health
and development if they become even partial realities.
The question, however, is whether our present socio
political situation and the imagination of our health
professionals can sustain such a commitment.
The Challenges ahead
After decades of rhetoric we have now moved
into a phase of realism (or is it populism?) where in
quantitative and qualitative terms the commitment
to child survival, protection and development issues
have begun to receive more than casual attention.
However, even though the outlay on social welfare
has shown a fifty times increase from the first to the
sixth plan, it is still important to remember that this
is still 0.2% of the total plan outlay (the highest
percentage was in the second and fourth plans =
0.6%) and represents an actual decrease from pre
vious plans.4 From this fact itself it is obvions that
in spite of policy statements we have yet to realise
the value of children as potential human resource for
the future of the nation.
The ICDS is an important milestone in keeping
with the growing realisation that “whether judged by
hard-headed economic calculation or by the elemen
tary tenets of human welfare, protection of the
physical and mental capacities of a nation’s people
and a nation’s future (children) is the most funda
mental of all investments’4 Recent' evaluations and
assessments (see Box) show that we have a long way
to go to make the scheme reach the umeached mil
lions. Even where it has reached, the status-quo fac
tors in our social, cultural, political and professional
milieu are preventing the services from being effec
tive. Is that surprising?
The challenges ahead are multiple. Firstly, a
challenge to our professional and technical manpower
and in reality to Indian Science itself. As Dr. Ramalingaswami has recently said “the tragedy of Indian
science is that while we have demonstrated the ability
to put a geostationery satellite in orbit and set up
nuclear power stations, we are still faltering in national
immunization programmes in which at best no more
than a third to one half of the eligible child popula
tion are getting immunised now”.
Secondly, a challenge to health workers in parti
cular who need to ‘lend their expertise to much more
far reaching campaigns involving people, institutions
and channels of communication which go far beyond
the present scope of health services themselves’!
Thirdly, a challenge to our socio-political system
for it is well-known that ‘greater social justice is of
fundamental relevance to the well-being of children’.
— An Editorial Review
The 1980’s have seen the development of a ple
thora of National Policies and Perspective Plans: eg.,
National Population Policy, National Health Policy
(1983), Projections and targets for Health for All by
the year 2000 with a 20 year perspective, Targets for
Water and Sanitation Decade (1981-1990), Objec
tives and Targets of the Sixth Plan (1980-85), Appro
ach to the 7th Plan (1985-89). All these have com
References
UNICEF (1984 a)
The State of the world’s Children—1984.
2. UNICEF (1984 b)
The Impact of World Recession on Children.
3. UNICEF (1984 c)
An Analysis of the Situation of Children in India.
4. Ministry of Social Welfare (1981): Profile of the Child in
India—Policies and Programmes, GOI-NIPCCD-UNICEF
publication.
5. Krishnamurthi KG & Nadkami MV (1983). Integrated
Child Development Services—An Assessment, UNICEF
Regional Office for South Central Asia, New Delhi.
6. Tandon, B N et al (1983). A Coordinated approach to
Children’s Health in India. The Lancet, January 15, 1983
(Abridged copies of 1 & 2 and copies 3, 4 & 5 available on reuqest form UNICEF, 73 Lodi Estate, New Delhi 11003)
1.
4
(Contd. fromp. 12)
the number of ORS packets per 100 children un
der five in 1984 was only 34 in 1984 (State of
World's Children UNICEF, 1987).
If neither within nations nor between nations,
structural changes are going to take place even
if they are moved by the plight of the dying children
what makes UNICEF confident that nations will
want to adopt the UIP ? "Assignment Children",
61/62 UNICEF states"... .the decision maker
must either see the problem as a felt need, as a
poltically attractive issue, or be willing to make it
one. Small pox eradication was not initially a high
priority in a number of endemic areas. Threats
of economic sanctions and international qua
rantine helped these reticent nations to develop a
cammitment to the programme. Offers to pay for
a programme, such as US funding of the global
malaria campiagn of the 1960s can often create
political will. As unpleasant as it sounds, such
coercion is not uncommon and can serve useful
ends". (Haven't we heard this before ?)
"Assignment Children", 69/72 UNICEF further
states "There are perhpas two main reasons why
the governments of the industrilized world might
wish to consider a much greater support in order
to realize the greater potential for UIP ? The first,
and most important, is that the immunization of
all children remains one of the greatest humani
tarian goals. The second is that it would also
result in very signifcant economic gains for the
industrialized nations themselves. Evidence for this
can be found in the annals of the international
campaign to eradicate smallpox. In 1967, small
pox killed an estimated 2 million people. In 1977,
the last case of small pox was recorded in Somalia.
The cost of the eradication campaign was approxi
mately US $ 24 million a year, of which about one
third came from the developing countries them
selves. For the duration of the programme, the
USA contributed a total of US $ 32 million (in
1970 dollars). Since then, the Government of
the United States of America has been able to
discontinue small pox vaccination and dismantle its
elaborate quarantine and surveillance systems—
which were costing approximately US $ 120 mil
lion a year in today's terms. In other words, the
eradication of a major disease has meant that the
USA is now saving every few months more than the
total amount it invested in the eradication program
me itself (emphasis theirs). As we have already
stated, the USA is today spending approximately
US $ 50 million a year on vaccination and routine
surveillance against measles and will contine to
do so for as long as measles is at large in the world.
A successful eradication programme would there
fore save the USA, US .$ 50 million a year—every
year from now on".
A child Survival Revolution strategy could either
mean that we go round and round in circles, spinning
on one's axis or overthrow, or change the explotitave system, the major deterrant to survivals.
It is not because of some quirk in one's character
that one keeps harping on the socio-economicpolitical roots of both illhealth and the strategies
that are popularised/imposed (and it certainly does
not improve one's temper I), I too feel the need to
think positively, but give us some evidence please.
Sathyamala
Jkc
'j/7'.
From the Editor's Desk
The theme for the next annual meet is Child
Health in India. Unlike the general trend in mfc to
critique a new policy/strategy, the moment it is
announced, this time we will have the experiences
of five years of GOBI (Growth monitoring, oral
rehydration, breast feeding, immunization) and the
three years of UIP (Universal
Immunization
Programme) of the UNICEF.
So, instead of
sounding like prophets of doom, we have the possi
bility of looking at these programmes in the light of
the 'Indian' experience. But this exercisse will
probably be hampered by a major constraint.
There are no authentic studies to show the
general pattern of illnesses in the under-five
population. Most of the quoted figures are from
sample surveys localized to specific areas and hence
cannot be generalized. What everyone does seem
to agree is that infant mortality rate in India is high
(again estimates vary from 105-220/1000 live
births). By putting together the little data we
have, one can come to a common agreement that
the major cause of mortality in the under-five
children is diarrhoea followed by respiratory in
fections and measles/tetanus with polio cau
sing a high level of disability and pertussis, per
haps, a high level of morbidity (but there are no
community based surveys to show the extent).
According to the only large community based
study that we seem to have, (Narangwal, 1971 /73),
of the 135 deaths per 1000 in the age group of 0-3
years, 39 was due to diarrhoea/enteritis, 19 due
to pneumonia/respiratory, 5 due to malnutrition
(starvation ?) including low birth weight, 2 due to
tetanus, 1 due to measles and 34 due to other causes.
Both diarrhoea and respiratory infections al
though the most common causes of death, are
muti-factorial in etiology and are not preventable
by vaccines available today. With measles, it is
a well known fact that mortality increases by 400
times in under-nourished children.
Tetanus is probably the only one in which the
relationship between nutrition and mortality/mor-
r
p
I
i
R.N. 27565/76
bidity has not been established (but nevertheless
it is a reflection of poverty and disparities). Yet
we are going to be spending approximately Rs. 161
crores, 70% of which will
be supposedly
contributed by the GOI, on the vertical UIP to
prevent immunizable diseases. If the intention:
was to reduce childhood mortality, surely the vacci
nation technology provides a second best alter
native. Why then this emphasis ? UNICEF's
"State of the World's Children, 1987" provides a
clue. "Poverty is the basic cause of early deaths,,
ill health and poor growth among so many of the
world's children. In the 1980s, programmes against
that poverty has been slowed, and in many nations
thrown into reverse, by the effects of a longrunning world
recession... .structural change
within nations—including land reforms, the redi
stribution of income-earning opportunities, and
economic policies designed to increase the parti
cipation and productivity of the poor are funda
mental to the reacceleration of the progress. Simi
larly, structural change between nations.. (yes,
this is from the UNICEF's report)... .is also
fundamental to the restoration of growth world
wide and to the creation of the conditions in
which the vast majority of the world's families
can earn enough, through their own efforts, to
improve the quality of life for themselves and their
families.... UNICEF which devotes the bulk of its
own resources to the development of basic living
conditions in the developing world, is now drawing
on its own experience, and that of the many govern
ments it has worked with over the last forty years, to
try and to find new ways and means of main
taining progress for the world's children even
in the absence of significant increases in the re
sources available".
So the key phrase is "in the absence of signi
ficant increases in the resources".
Attacks on
diarrhoea is not possible without an attack on
poverty. Even in diarrhoea, a half-hearted attempt
was made at introducing the 'appropriate' tech
nology of ORS which met with a very low success;
(Contd. on p. 77)
1J
,■ 7
■J
■ J
medico friend
circle
bulletin
130
j ■
■J 3
■
frfr
JULY 1987
Paralytic Poliomyelitis : A Tragedy on the Rise
ifr
al
J
■ 3
■3
-/•-j
S
A*
. a aO
] r
J-
J 3
j.i;
j,
a...d
j
J... .A
..
- jl;
J ;
J..;
i
4. *
Gloria Burrett
The Spastic Society of Northern India is a
voluntary organisation which runs the Centre for
Special Education. This is a special school for
children with cerebral palsy. Here problems such
as stubborn self willed limbs, specific learning
difficulties, hearing problems and unintelligible
speech are handled by a group of professionals
working closely with the parents of the affected
children. This article traces our increasing inter
vention in the area of polio, both in management
and prevention. This is significant in that, cerebral
palsy was intended to be our main area of speciali
sation. We also hope to project through this the
enormity of the problem in that—epidemics of
polio are occurring in an area well connected to
hospitals; despite the OPV (oral polio vaccine)
children are being affected by polio; and general
practitioners are aggravating the problem by the
indiscriminate use of injections.
Kms from the main civil hospital at Faridabad. One
could say that the area we chose had access to
primary health care as well to other referral services.
Soon after the rural centre was opened, we
realised that there were several problems in starting
a centre of this kind in villages. The whole area
of "handicap" is not a priority. Children with
severe cerebral palsy die or are starved to death.
In poorer families like those of the daily wage
earners where the work load on parents is greater,
each day's wage is precious; and where it is diffi
cult to feed one's normal children, the handicapped
child is a problem that is best forgotten. So,
often we had to create a problem in the minds of
parents and make the child's handicap appear
more serious than it seemed to them at that time.
In our minds we could imagine these disabled
children growing into handicapped adults.
Our rural centre :
Shift of Priorities:
Two years after starting our centre at Delhi and
following our brief experiment with the children
from Madangir (an urban slum development area
of Delhi), we felt it was necessary to reach out to
the many children affected by cerebral palsy in the
villages. Our centre would have to be sufficiently
distant from Delhi for it to be viewed as a necessity
and yet close enough for our regular visits. This
October will have made it six years since the incep
tion of our rural centre at Dayalpur village (Faridabad District). The centre is situated within the
Primary Health Centre campus, 10 kms from the
district hospital at Ballabgarh which is also the
training centre for interns from the All India Insti
tute of Medical Sciences, and approximately 20
Of the seven students we started with, only one,
a severely handicapped, immobile, intelligent, eight
year old with cerebral palsy was brought in by
parents who were desperate for our services. The
others we admitted were either mildly affected
physically and/or had speech problems. One was
a child with polio whom we wanted to integrate
into a normal school as quickly as possible. There
was always the feeling that with our limited staff
and our initial intention of rehabilitating children
with cerebral palsy, the condition of polio could
never take precedence. We believed that the
severely affected spastic children in the course of
rime would make up our numbers and take up our
full attention.
i
77/^ QlAllt-fa, iVV-
However, within six months, and increasingly
so today, the great number of polio referrals and
to a lesser extent those with hearing problems
have made us think otherwise. The following
facts are indicative of our growing involvement
with polio.
I
f'i
I L
J
€-;
merit by way of time,
energy and manpower
than we had bargained for and yet there is no
choice for us.
What would happen if we referred all such cases
to the nearest hospital? The Civil Hospital at
Faridabad has two orthopaedic surgeons but our
operation
cases were turned away with the state
our
children
is
as
follows:
Today the breakup of
ment that "this operation is not done here". The
District hospital at Ballabgarh does not have .an
—52
Polio
orthopaedic consultant. Four years ago, during
—24
an ICMR project on polio, a team from the Rehabili
Hard of hearing
tation department of the All India Institute of Medi
—17
Cerebral palsy
cal Sciences visited the hospital regularly twice a
week. Since then all cases requiring rehabilitation
—13
Others
are referred to Delhi where the department provides
us maximum support by way of diagnosis and
These figures are not a complete index of
provision of aids. A word about the ICMR project
cases existing in this area, but only those who
is in order here as an example of Government's
attend our centre. There are many mildly affected
intervention in the area of polio. The project
polio cases who see no need for our services and
covered the greater part of Faridabad district. The
some severely affected cerebral palsy children who
ICMR team conducted an impressive survey of
are unable to attend our centre. But we are aware
the number of handicapped children of all catego
that the number of polio children who are not
ries in all the villages. Measurements for calipers
being catered to by the centre at present far
for all polio children were taken at one go and the
exceeds the latter.
families were promised delivery of free calipers at
their homes. Although some children did receive
To cater to the growing number of cases other
the calipers immediately, we know that these were
than cerebral palsy, a home management program
still being delivered as much as two years later. Apart
me was introduced for children needing specific
from the obvious outcome of ill-fitting calipers
help in one or two areas and needing to attend the
and disappointed parents, even those with well
centre only once a week, fortnight or a month.
fitting calipers
discarded them in a couple of
We held a six-months training course for local men
months due to a lack of follow-up. Many homes
and women to enable them to detect, diagnose and
in the ICMR project area display calipers hung up
treat polio. Right now there are six fully trained
on the walls as an 'object de art'!
rural rehabilitators who are instrumental in increas
ing the number of polio referrals. Their closeness
Coming back to the question of referral services
with the community aids detection. They also
for the handicapped children, the chances are that
have a special ability to motivate parents as three
they would be sent onto the hospitals in Delhi of
of them have children affected by polio.—
which, Kalavati Saran Children's hospital, the All
India Institute of Medical Sciences, and the
Our medical follow-ups include regulation of
Safdarjung hospitals are the most frequented.
drug doses for epilepsy, diagnosis of neurological
Generally in these hospitals, even if they boast of
conditions, audiograms,
applying for free aids
superspecialities, the rehabilitation units tell a sad
available in hospitals and operations. Of these,
tale. I recollect how an intelligent and a very
the most running around is involved in the case of
confident parent of one of our polio children had
operations. Upto five visits are necessary before a
to intervene in his son's treatment. He realised
child is admitted and another four during admission
that the fixed contracture would need more than
to get feed-back from doctors. Of the 25 cases
the wax treatment his son was being given. The
we have referred so far, 23 are cases of polio.
Consultant was, fortunately, honest enough to
Following surgery, and also in most polio cases not
admit the misktake—a costly one for the father,
requiring surgery, calipers and crutches are essen
who had to travel the long distance from Haryana
tial. This requires another round of hospital visits,
to Delhi, but the father was allowed to meet the
to ensure that the recommendations we forward
consultant only on his third try when accompanied
are heeded by the doctors. Getting into the area
by me. We also have had parents tell how
of polio sometimes forces from us a greater involve-
■
!
S(
,
2
€
* V.,!,,
1
«>■
*I
■
'■
a 3* *
at
E
iO
■ •
[
p
E
E
3. i
J
a.;
j
E
jA
M Fc
a/p-
/2of
futile they felt the daily sessions to be and even
after a-year of treatment at one of these hospitals
many parents have no real knowledge of the
problem. Over 50% of our cases are drop-outs
from such hospitals because of the problems of
distance, time and money. They now have child
ren needing operations for unattended fixed joints
because of parental frustration in the face of the
uncaring medical profession.
All this has forced us to get into this area of
polio in greater depth. We have had to follow-up
old hospital cases, accompany parents to hospitals,
be actively involved at every stage of the operation
procedure, and motivate parents and children into
doing therapy so that mobility and integration may
follow.
This management of polio has made a difference
in that it has helped us gain more credibility.
While earlier, a high percentage of acute cases
relied on the local village 'phalwan', who claim
to have the ability to activate flail limbs through
vigorous massage (even within the very vulnerable
first month following the onset of polio), today, we
are being referred acute cases as compared to
the initial referral pattern of cases of plus-five
years of duration.
i56^)
nset waSaetected by us
isolated case of six-days onset
in Tigaon. In all 10 acute cases were enrolled
in the month of April 1987.
There were three disturbing facts about this
epidemic. (1) A recent survey carried out by the
Dayaipur primary health centre showed that out of
the 36 cases who had received three doses of
OPV, 18 had contacted polio; (2) why with two
hospitals within half an hour away, should there be
such an epidemic? Both these hospitals run
primary health centres attached to them, and
immunisation is meant to be a priority area for the
staff; (3) It is a known fact that 90% of the polio
cases follow injections given during the early
symptomatic stage of fever/cold. Why then were
the doctors indiscriminately using injections for
fever cases in children? The urgency of the situa
tion however, demanded that we take immediate
action.-Our action included working at four
levels:
1. Private doctors— A meeting was held where
all the private doctors from the nearby villages
were invited to find out their routine 'treatment' of
polio as well as their awareness to the link between
intra-muscular injections and polio. The meeting
was most revealing in that none of the doctors
present knew that an IM injection could aggravate
paralysis. They felt that as long as there was no
reaction to the injection and as long as it was
properly given, no problem could result. They
surmised that only when the child was injected
wrongly, 'injection palsy' could result, and the
fault therefore lay with the technique and not with
From Rehabilitation to Prevention
The next step was apparently to go beyond the
acute cases and evolve measures to prevent or
lessen the incidence of polio. However, after
giving it much thought, we felt ill-equipped to
get involved with such measures. It would have
meant involving ourselves with too many priority
problems, a situation where we would be spreading
ourselves too thin. We already had on our priority
list the following priority areas: training courses,
sheltered workshop, employment opportunities in
factories, educational programming, integration,
daily management of cases, following-up govern
ment facilities for the handicapped and completing
the medical follow-up. But two issues forced us
into the area of prevention sooner than we thought.
The first was a recent case of polio following an
injection administered by a private practitioner
for low grade fever. The second an epidemic of
six cases of polio at Madalpur village. This epide
mic would have gone unnoticed save for the
referral by a Physical Training instructor in the
regular school who had been approached by
parents to strengthen their daughter's lifeless
limbs (she had been a normal two years old till
two days before the paralysis). Since then an
the practice.
We did manage to convince them of otherwise
with our practical experience, medical data, and
explanations. They were also made aware of our
seriousness in following up each such case with
the doctor concerned. Even those who did not
attend our meeting were sent a summary of the
proceedings. Appreciating the doctor's problem
of giving into persistent parents to whom an injec
tion is a magic remedy, we arrived at the following
compromise. The doctors could continue using
injections as before except in children under five
years of age suffering from fever and chills and
especially during the months of May to September.
As a follow-up to our meeting, a private doctor
ready to inject a child put the syringe away and
persuaded the mother to rely on tablets, on sighting
two of our staff who chose that moment to call on
him I
3
-li.
(Contd. from p. 4)
2. Affected Families— A
day after hearing
about the epidemic, our local team went-round
Madalpur with their charts and songs on polio.
As people who had gone through similar experienc
es, the members of the team supported and advised
the parents of the affected children. Stress was
■ placed on 'what not to do' in the first month follow
ing the attack. A report was lodged with the
Sarpanch, and details regarding our centre was left
with the parents. A month later as none of them
had visited us, another visit was made to explain
the change in treatment and to look into the matter.
i
3. Community— An all out effort was made to
inform all our old and new parents as well as their
neighbours about the epidemic, the need for
immunization and the role of injections.
Many
who had not been given the OPV in Tigaon were
referred immediately to Ballabgarh hospital.
4. Government Health Authorities— Madalpur
village is under the jurisdiction of the Chief Medi
cal Officer, BK Hospital, Faridabad.
Through a
letter personally delivered to him, we appraised
• him of the situation and the need for follow-up
‘action. We also offered our help. However,
there was further feed back only when our local
team made a second visit to the area a month later
and found out that children had been given their
first round of OPV. Following the GMO's delay
in getting back to us, we approached a doctor at
Ballabgarh district hospital who felt that it was not
possible for one
government organisation to
interfere with the area that lies within the jurisdic
tion of another government organisation. He also
felt that we, as a voluntary organisation, should
not have delayed in buying vaccines and administer
ing them in the village when we came to know ofthe ’
epidemic. It was obvious thatthe problem was back
in our court. But the question remains as to why a
voluntary organisation be asked to take on a major
responsibility when there were well-equipped and
well-staffed
government
hospitals that were
supposed to
provide
comprehensive health
care to the population it covered. We still have to
meet the GMO, the Health Workers, and Super
visors at the two sub-centres (Madalpur and
Tigaon) to find out details pertaining to the immuni
sation programme.
T-.
I
I’il
1
There is no way of knowing how effective all
this will be. Our credibility in this area has certainly
(Contd. on p. 7)
gone up. Following repeated requests from the
parents of polio children and the village leaders,
a new centre has been opened at Tigaon. A
recent survey done by the local society (Jan
Kalyan Samiti) gave us the names of 50 polio
children. This did not include the 8 already being
treated by us, and those detected more recently.
It is interesting to note that the list has 3 deaf
children and one child with cerebral palsy. It
does seem that we will have to change our priority
from providing services for spastic children to
helping children handicapped with polio. It is
not so much the change in priority that is causing
us concern, as much as the question—When the
simple technology of immunization is available
why should a situation of increasing incidence of
paralytic poliomyelitis come up?
Could this
tragedy not have been averted ?
ii) Our efforts should be focussed on supporting existing
system to prompte HFA 2000.
iii) Our efforts should—be health oriented and should balance
knowledge, attitude and practice dimensions.
iv) Need to train people as role models.
v) Should foster team work not individualism or isolationist
approach.
vi) Should utilize all existing resources in the community.
vii) Should promote a flexibility in human resource development
responding to different needs in different communities.
viii) 'We. should prioritise the categories of people who need to
be trained. The present system is top heavy, disoriented
and too expensive for the community and the government.
We need to balance the categories.
ix) Human resource developments should be related to needs
and based on decentralised planning.
x) While determining the optimum mix we should make conscious
decisions to allocate finances for different categories as
well as use existing resources optimally.
xi) The policy must stress continuing education and constant
updating of knowledge and attitudes at all levels.
The broad principles that emerged in tne groups deliberations
were that our new policy emphasis should be
i) On humanpower development training at the peripheral level
a) Full time government and other workers, rural development,
extension workers, panchayat workers.
b) Quasi government - Anganwadi, Community health volunteers
guides etc.
c) Volunteers - TBA’s, traditional medical practitioners
d) Religious groupst social activists and NGO's.
ii) We should work together and support each other.
iii) We should be accountable to the community and focus on
educating and empowering people to their own roles and
responsibilities in health.
iv) We should also identify people at higher levels of the
system - doctors and administrators and try and foster
the right attitudes, values and practices in them.
^1
medico friend
circle
bulletin
138
Hl 3
bJ!
iis
S'3
r ‘!'n
’
■
■
MARCH 1988
■
■■■3 c
3 s'
■IF
Report of the XIV Annual Meet of the MFC
on Child Health
‘d ..’ins
oot esw
? -oi!: on
«’■
.yr if
20-21 January 1988, Jaipur, Rajasthan
'3
The theme for the annual meet had been chosen
keeping in mind the current emphasis on child
survival as the most revolutionary concept in
child health. As several participants had not
received the background papers in time, the ses
sions started with the summarizing of the back
ground papers. The discussions that followed
in the small groups was facilitated by the listing
out of questions that arose in the context of the
information that was presented. The four major
areas that were identified for discussions were :
1. Acute respiratory infections;
J
2. Immunization;
3. Survival of the girl child;
4. Nutrition and child health.
Following is a brief report of the discussions
that took place in the It- days of the mfc meet.
The afternoon session of the second day was
spent on discussing the changing emphasis
from child health to child survival, The meet
ended with the evaluation by the participants.
j...;
j....
aiF'
Acute Respiratory Infections
(ARI) :
Among childhood diseases, ARI forms the second
most common cause of deaths in children, Estimates of mortality range from 15% to 25%
of the total childhood deaths. Studies have
shown that 20-40% of out patient and 12-35%
of childhood hospital admissions are due to
ARI. The background paper prepared by Abhay
Bang highlighted the problem and the strategies
that are being proposed to deal with them?
Studies have shown that the frequency of attacks
of ARI per child per year is similar in the deve
loped and developing countries.
Within deve
loping countries, frequency is more in urban areas
as compared to rural areas. This would suggest
that socio-economic improvement may not be a
major determinant of the frequency of ARIs but
overcrowding is certainly an important factor as
the organisms cannot survive in the absence of
a large population in constant interaction with
each other.
However, the severity of the infec
tion and the resultant mortality are significantly,
high in the under-nourished children. For insr
tance, in a study carried out in Manilla, the case
fatality ratio in well-nourished children was 6/1000
episodes whereas in the severely under-nourished
children it was 77/1000. Smoke (fuel and,
tobacco), vitamin A deficiency are other factors,
influencing incidence and mortality rates.
The control of ARI through a single vaccine is
not possible because of the large variety of causa
tive organisms involved although it is estimated
that 25% of the total mortality due to ARI can be
prevented through the vaccines available today
(against diphtheria,
whooping cough, tuber-J
culosis and measles). Based on the fact that
majority of the acute lower respiratory infections
are caused by bacteria and hence amenable to
treatment with
antibiotics, .:and based on the
Narangwal experience that showed a dramatic
‘
I
■
e
;
reduction in mortality when these children were
treated with injection penicillin by Family Health
Workers, a secondary prevention approach—
Case Management Approach has been formulated.
According to the guidelines, a respiratory rate of
50/minute is the criterion chosen for identifying
children who need antibiotics. Currently pilot
studies are being carried out in 4 centres in India
to assess the feasibility of launching a nation
wide programme of ARI control through the case
management approach.
ones. In developed countries, viruses and my
coplasma were the major organisms whereas in
the developing countries 60% of the cases were
bacterial. It was suggested that climatic condi
tions could be an additional factor but it was
pointed out that the native American Indians living
in Arizona in a relatively lower temperature, also
showed organisms similar to that in developing
countries. I.t is possible that even in developing
countries ARI may be of viral in origin with super
imposed bacterial infections.
Question was raised about the sensitivity of the
indicator recommended i.e., respiratory rate of
50/minute. According to the background paper,
this rate was likely to give the lowest number of
false positive and false negatives. Some partici
pants however felt that the 72% (true positive)
was too low a figure to justify its use as a diag
nostic criterion. It was also noted that if one
increases the sensitivity of a test, its specificity
may not remain and therefore a balance has to be
achieved and the recommended criterion of the
respiratory rate along with history given bythe
mother (difficulty in breathing) should be suffi
ciently sensitive. A suggestion that field workers
be given a stethoscope did not find favour as it
would not improve diagnostic possibilities.
No consesus was reached about the ARI
control programme on a nation wide basis. If
this programme was to be launched, it will be yet
another vertical programme to add to the other
existing vertical programmes with all the atten
dant problems. At present adequate data is not
available within India as the pilot studies are still
underway. There may be opposition from the
medical establishment if paramedical workers are
allowed to handle antibiotics. Finally, a pro
gramme such as this might succeed in decreasing
mortality but the attack rate and morbidity will
continue to remain high.
Immunization : The article entitled “Universal
Immunization Programme: A Positive view” by
Ashok Bhargav and Anil Patel (mfcb 133-34)
formed the background paper for discussion.
(Since it has already appeared in the bulletin, it
will not be summarized here). Despite the non
achievement of targets in the Extended Programme
of Immunization, our country launched the Uni
versal Immunization Programme in Nov 1985.
(The EPI had only 14% coverage for DPT and
5% for polio). Given this experience is UIP a
desirable strategy? The group felt that there
are many 'dark' areas in the figures available
regarding the prevalence of communicable diseases
in our country, the coverage by immunization
programme, the cost-effectivity of such program
mes etc. It was felt certain parts of the country
do not have as high an incidence of a particular
disease as other areas. It is perhaps necessary
to substantiate the prevalence of the six vaccine
preventable diseases in -the various parts of the
country with data. It is essential to do this prior
to planning the strategy. At the present moment
it is not possible to work out the cost-effectivity
of the programme. Statistics necessary for such
an effort do not appear to be available. Secondly,
in the current socio-political set up, it is extremely
difficult, if not impossible to say that a particular
programme has resulted in a particular effect. It
is quite possible that an improvement in drinking
The case management approach raised two
major areas of concern. One was related to the
development of high levels of antibiotic resistance
in the community and the other, the possibility
of hypersensitivity reactions to the antibiotic
recommended (penicillin). It was agreed that
antibiotic resistance would definitely emerge as
an outcome of its widespread use, but it was
contended that in any case resistance is going
to occur in about 10-20 years because of the
widespread misuse of antibiotics by private prac
titioners, so at least till then why not let all sections
of the society get its benefit I To the question
of sensitivity reactions it was stated that in children
anaphylactic reaction to penicillin is very rare
and since some felt that intra-dermal test was
quite useless it was well within limits to accept
the risk of 1 in 2.5 lakh without the test dose.
This question was not resolved to everyone's
satisfaction. The question of referral was then
considered. It was suggested that in the case
of recurrent symptoms and wheezing, referrals
may be required and that there was a need for
an x-ray unit at the referral level. There was
some dissent on this.
The etiological picture in ARI is different bet
ween the developed countries and the developing
2
I”
G6
€ L
■'y ri
i
€' r - .•
.>■
AA—
3
e-
e-t
B
■
AlTc
1
-
I-
g
A
‘9
■4
.Li
•9
■9
r*
. ...
A/P-
)
■)))
children. Although at the macro level it is well
established that in India females at ages from 0
to well into reproductive period suffer from higher
risks of mortality as compared to males, efforts to
understand exactly how discrimination takes place
seem to pinpoint that medical intervention at the
time of illness could be the crucial factor in deter
mining mortality rates. From her own experience
and on the basis of other studies carried out in
India, it appears that there is no hard evidence to
indicate any discrimination on a regular basis,
discrimination exists only in terms of special foods
such as butter, sweets, ghee etc. Kamala Jayarao
had analysed the data of the National Nutrition
Monitoring Bureau (NNMB) which showed that
adult females have less calorie deficit than adult
males i.e., the food intake of women is better
than that in men or that the energy intakes are
similar. Further, in the underfive age group
there were no sex difierences although the under
five girls had a greater body deficit. This diffe
rence was lost when girls grew up and body
deficit in women was less- than in men. The
conclusion reached was that women were not as
underweight as men. Her paper also presented
evidence from an NIN study which followed up a
large number of children
whose weights and
heights were recorded when they were 1-5 years
of age and later. The results showed that sur
prisingly in girls with severe malnutrition there was
an attempt to catch up (the increase in height of
girls who suffered from severe grades of malnutri
tion, the increase was much greater than not only
those who were in mild and moderate grades but
even than in American girls.) However the in
crements were not sufficient to allow them to
attain a normal height. The reasons for the better
performance of girls in late childhood and adoles
cence was not clear.
water supply, sanitation etc. may be equally costeffective. The manner in which UIP is being
promoted, as an approach
in isolation, as a
panacea for childhood morbidity is not acceptable.
UIP cannot be a substitute for socio-economic
improvement. Individual experiences shared in
the group highlighted the fact that UIP is accep
table only as an integral part of primary health
care programmes. It is not true that vested in
terests are not involved in the planning and pro
motion of UIP. There could be international
and national political influence in the planning
and selection of strategies
such as the UIP.
Planning for an immunization
programme is
more likely to be effective if it is location specific
rather than uniform nation wide. Several expe
riences were shared regarding the different stra
tegies each had adopted. The strength of the
measles immunization programme implemented
in the city of Jaipur was the large number of
private practitioners that were enrolled for the
effort.
A single day was declared immunization
day and prior publicity was given through the
media. About 30,000 children were vaccinated
that day in the age group of 0-5 years. The
immunization programme carried out in the 20
villages around Wardha as part of the primary
. health care programme being carried out by the
medical college had 90-95% coverage with measles,
70-75% with DPT and polio. The dropout rate
between the doses was minimal and most of it
occurred because the services could not be ren
dered at a particular time. In the subsequent
years, the drop out rates diminished and for the
past three years, there is not a single case of
measles\or polio. If planning and execution is
done in an efficient manner, targets can be reached
effectively.
Consensus could not be reached on these
questions : can 2 live vaccines be given at the
same time and whether 3 or 5 doses be given in
polio immunization. Since the UIP is already
amongst us, what should be our reaction to it
could not be discussed due to paucity of time.
All this naturally led to a very energetic dis
cussion. In neither of the papers there was ade
quate evidence that no discrimination exists in
terms of food intake. Yet the impression that was
created by both the papers was that no nutritional
discrimination exists. Can one really quantify in
statistical terms the differences in nutritional intake
within a family? The very fact that an outsider
(the researcher) is measuring food allocated to the
different members within a family would surely
introduce a bias. Does a lack of substantiative
data mean that discrimination does not exist ?
The NNMB data came under attack and was
questioned for its statistical validity. The data
had been obtained for purposes other than estab
lishing discrimination and it was agreed that the
Survival of the girl child : Leela Visaria's
paper "Gender bias in survival and Nutritional
status of Children : Review of available Evidence"
brought out clearly the paucity of substantiative
data to support that girls are discriminated against
in terms of food allocation. According to her,
the only study that had attempted to measure in
detail the quantity of food intake of children was
carried out in Matlab (Bangla Desh) which indi
cated food intake was biased in favour of male
3
■1
he QvxlLc'bm /yr
.1 cf'-g-g
data should be checked for its biases. It was also
pointed out that earlier when .-Harvard standards
were used, which is a combination for girls and
boys, girls tended to be more under-nourished
whereas when different standards were used for
boys and girls boys appear more under-nourished.
The 1960-70 studies from ICMR, NIN had shown
nutritional deficits in girls based on anthropometric
indices. Therefore, it seemed unlikely that the
situation had changed so much since the ICMR's
findings that there was no longer a major nutri
tional deficit experienced by girls. The only
conclusion that the group could come to was that
there were no adequate studies to substantiate
the forms that discrimination takes although they
are observed as widespread phenomenon.
I
I
!L i
1
h
r
r
■
I <■ ;
5 ()}
growth monitoring is no more than a diagnostic
and (possibly) educational - tool...... Growth moni
toring by itself, however efficiently executed,
cannot bring about nutritional improvement; it
must always be followed by action on the part
of the health worker and the mother—the action
consisting of appropriate and necessary improve
ments in child-feeding and child-rearing practices.
Thus, growth monitoring is not even a means to
an end; it is only a means to the means" was
the central point in C Gopalan's paper "Growth
monitoring : Some basic issues".
The ICDS
(Integrated Child Development Services) with
its emphasis on supplementary feeding programme
is using growth monitoring (age to weight) to
screen children for its feeding programme. The
use of the 'under-five' growth cards is no longer
concerned with the detection of growth faltering,
rather it is to identify children who have become
sufficiently undernourished
for
rehabilitation
through the feeding programme.
This shift
has been on the authority of various Western
scientists who contend that mild and moderate
under-nutrition in a third world population is
acceptable as these children in any case adapt as
they grow up by stunting their height and a popu
lation of stunted adults is normal and healthy
given the 'environmental and economical condi
tions'. The
field level experiences of many of
the participants showed that ICDS is failing to
achieve even this limited objective, in that the
under-three and the grade III children are not
reached through the ICDS as the programme
expects the children to either walk upto the
Anganwadi or be brought there by someone
else. Further, feeding programmes are ''offset by
the perennial problems of substitutes, pilferage etc.
Manipulation of records is the usual practice and
in some instances it was seen that the wejght of
2 or 3 children were marked on the same card.
Integration with the health services is poor and
the training institutions work in isolation and
continue to emphasise 'high protein' foods.
Despite these, the official evaluation have always
been laudatory and independent evaluation con
sistently bring out failures.
The group also contended that caution needs
to be exercised in accepting 'access to health
services' as the determinant factor in mortality
rates among the girls. Firstly, until recently hardly
any rural population had access to health services
and this would have affected children of both
sexes more or less uniformly. Secondly, we need
to define what we mean by access to health
services. There may be a PHC, subcentre, private
practitioner or local healer easily 'accessible' to the
population, but this in no way means access to
effective health services. The mere act of taking
a child to any of these services in itself doesnot
indicate that they are effective enough to prevent
mortality. It was also pointed out that the higher
mortality rates in girls may be due to an interaction
of several factors rather than the result of a single
factor and that we may not be aware of these
factors at this point of time because of the inade
quate attention paid to the subject. The discussion
then veered off into the question of how important
is it to understand the factors responsible for the
higher mortality and morbidity rates in the female
population in order to intervene positively? Are
we all not aware of the fact that women are dying
and suffering as a result of the patriarchal attitudes
and values in the society? In that case the posi
tive intervention would be to attempt to change
these attitudes and values and for this purpose the
understanding of the forms of discrimination is
largely irrelevant. This brought us to the same
(old I) debate that has continued (and one hopes
will continue) since the inception of MFC : To
reduce a
disease' of socio-economic-political
origin what is the 'level' at which a socially cons
cious medico intervene ?
C'
C:
e.
c;
vn
♦ ;
V-
y.'-"
1
.3
^7
ejj
-
In terms of intervention, to improve the nutri
tional status of children using growth monitoring
to identify early stages of growth faltering, Gopa
lan's paper had quoted the study from Ludhiana
which showed that marginal changes in child
feeding and rearing practices which are feasible
and within the means and resources of poor
families might suffice to arrest growth retardation.
This was greeted with some amount of scepticism.
Nutrition and Child health : "At the risk
of stating the obvious, it must be emphasised that
4
■.......... ...............
j;.%
.....
I
..
•2 ■ JI -
.4
■ 4
o
fl
•E
0
fc
J?
j.£.
B
Can mere health education improve
the nutritional status in a situation wheie access to ressources is extremely restricted because of poverty.
The group also crticised
---------- d the recent trends in
harnessing' the adolescent girls
for child rearing
since they themselves are in need of
opportunities for better growth.
Low birthweight continues
to .be a major
problem. There seems to be a direct
relationship
between stunting of the mothers and the
occurrence of low birth weights in
the offspring.
Studies have found that the pre-pregnancy nutripre-pregnancy nutritional status of mothers an important determinant
of low biith weights, Medical and
nutiitional
intervention during the time
.... e of pregnancy seems
to have little impact in reducing*the
incidence of
low birth weights.
St -
eh M
.Tl7refore Pregrammes
that aim at
child survival by 'fire-fighting' strategies should
not be carried out in isolation but need to be
implemented in the context
of the improved possibility of improved child
nutrition irrespective of
their degrees of under-nutrition.
The c.
current fixation for mortality indicators like
the IMR have
arisen out of the fact that these
parameters can be managed and manipulated
without attempting to change theTo^cio
'
. ______ j -economicpolitical situation, f
Since the time of Bhore committee we have shifted from
- - ---- ) a near-comprehensive
commitment to improved quality of life
...j to narrower and narrower
concepts like child survival.
Gopalan's paper "IHeights of populations
An
index of their nutrition
----- 1 and socio-economic development" pointed
out that infant mortality rates,
increase in life
expectancy do provide a measure
of the overall improvement
i
in health status but
do not tell ius much about the state of health,
nutrition and well being of
the survivors.
survivors. He
of the
suggests that height measurements and quantifi■t) On .°X ^e|9bt deficits through comparison
with an international or national standard and the
The major issue that faced the
group was the
difference in the c
—Cept• °f c^l,d health and child
C?2
survival. Only 2-4% of the under-five children
suffer from r
----severe
grades of under-nutrition and
some of them succeed in surviving.
About
60% of children
are mildly or moderately
affected by under-nutiition,
and most of them
survive to reach adult hood, What is the 'quality
of life' of these survivors ? Kamala Jayarao's paper
"Malnutrition and child survival" attempted to
answer the question. Studies have shown that
even severe under-nutrition does not damage the
app ication of the procedure of Z scores will help
capacity of the body to grow during adolescence
US to Identify differences in nutritional status as
particularly the linear growth, but the children
and
,d ,ferent regi0ns' Populations, groups
cannot make up the handicap suffered during
ocial classes in the country and to monitor
early childhood, A small body size results in a
changes over a period of time.
decreased work capacity, and hence the earning
capacity, Studies have also shown
that physical
labour during late childhood in under-nourished
children may adversely affect subsequent growth.
Kamala Jayarao in another paper entitled
Health and Nutrition" had compared the IMR and
nutritional status of children in Punjab and
Kerala. Punjab has a higher IMR as compared
to Kerala, However, in the under five age group
the incidence of under nutrition among 1-5 year
olds is much lower than that in Kerala The
It must also be remembered that the concept of
child survival —
was postulated on the basis that a
policy of population control will not be successful
as long as there is no substantial reduction in
infant and child rmortality. The national and the
International planners are not
are not interested in
improving the quality of life for th
.ne children in the
third world countries and attempt to do
so
is considered a luxury that
a poor country can ill
afford and is therefore discouraged. This dan-
gerous trend must be reversed and’the propaganda
be exposed for what it is.~~
reason could be that the availability of better
health services, better road facilities and the high
female literacy in Kerala, enables mothers to seek
early treatment for their children thereby reducing
IMR, child mortality but because of poverty (per-
Sathyamala
(Background papers of this meet are available
from the convenor's office for Rs. 10/ - per set).
|. ’
Sc*
about'ATo/ be'°W the P°Ver,y line in Kera,a' is
about 47/0 as compared to the 15% in Punjab)
food intakes continue to be low and hence the
mcdence of under-nutrition is higher in Kerala.
hi d survival cannot be ec/uated with good child
5
I.
*
133
134
medico friend
circle
bulletin
OCTOBER—NOVEMBER 1987
Universal Child Immunization and Child Survival :
A Positive View
Ashok Bhargava & Anil Patel
The Universal Child Immunization (UCI) as a
goal to be achieved by the year 1990 through a
strategy of Extended Programme of Immunization
(EPI) is very much in vogue now a days. Health
authorities in India, for a change, are also nowtalking about the EPI-UCI. However, many questions
are being raised regarding EPI. How serious is the
Government about the EPI ? Is EPI feasible ?
Can it help bring down infant and child mortality
as claimed ? Or is it a facade, deception or a
diversion ? Is EPI yet another ad hoc vertical
programme at cross purpose with primary health
care ? Is it flight of unrealistic ideas through and
through ? Or is it within the reach of the art
of possible ? This article attempts to address
these and other related questions.
When one views the Government propaganda
and take a somewhat cursory look at the published
material by the Government, depending on the
degree of one's gullibility or scepticism, s/he will
either accept or reject out of hand Government's
claim. We believe that neither will do. For a
group like ours which is actively involved in
evolving different aspects of women and child
health care programme including immunization
programme, it is not enough to just brush off
Government's claims. We need an in-depth ana
lysis of the EPI strategy as conceived and im
plemented by the Government. It is only by doing
so we will be able to clearly identify the levels at
which the Government's EPI strategy suffers from
shortcomings. For, it is not enough just to point
out dismally low levels of immunization attained
and reject the claims.
Even a correctly conceived and implemented
strategy of EPI is bound to have low rates of im
munization in country like ours in the initial
phase.
Therefore, demonstrably low rates of
achievement can hardly clinch an issue and help us
decide our stand Vis-a-Vis UCI. It is only by taking
the Government's claim
seriously and studying
the strategy more thoroughly we can assess the
level of seriousness, commitment and likelyhood
of success.
We therefore, begin from the beginning i.e.
setting of target.
Target : The yardstick of performance
A close examination of the exercise of target
setting is necessary to understand and assess the
Government's intention and willingness to achieve
the target requisite levels of immunization in the
children population by the year 1990.
Surveys done in India have shown that at least
in the year in which the EPI was officially launched
(1978), the coverage of DPT and Polio vaccines
was around 14% and 5% respectively (Table 2).
These figures did not materially change during
the years 1980-81, 1981-82 and 1982-83 (table
1). The final target of 85% of DPT, Polio and
measles vaccines is to be achieved by the year
1990. The whole exercise of target setting at a
theoretical level has been accomplished already
(Figure 1 : John J. 1985). One would expect
that the Government should set up systematically
and progressively increasing targets to achieve
<
the final target in time. There is no evidence
however to show that the Government is proceeding
to set the targets in such a fashion. What one
observes instead is the mystically arrived at magic
figures handed down to the hierarchical order of
the health bureaucracy. Since no rationale is
given, one can only conclude that this is an arbitrary
exercise in tune with typical bureaucratic flair for
target chasing for its own sake. On the other hand,
published evidence indicate that the authority has
no appreciation for such increamental target set
ting. Thus in the handbook for medical officers
(Sokhey et. al 1983) published by the Ministry of
Health and Family Welfare, Government of India,
the crucial question of setting target is discussed
vaguely (1). This ensures that no precise annual
targets will be set against which the performance
can be judged. The first link in the chain of
successful achievement of UCI is thus missing.
Table-1
DPT and Polio Vaccine Coverage of Under-1
Population
in
Year
Under1 Popu
lation
DPT
millions
Per Polio Percent
cent
1980-81
48.7
6.0
12.3
1.4
2.9
1981-82
50.9
7.2
14.1
2.3
4.5
1982-83
53.2
8.3
15.6
3.7
6.9
Source :
Don't miss any opportunity
The World Health Organisation (WHO) re
commends and the Government of India accepts
the following : a child's visit to any health centre,
clinic, hospital for any reason should be viewed
as an opportunity to immunize the child and such
opportunity should be seized.
This part of the
strategy is hardly more than a decorative piece,
because
overwhelming majority of the target
population is in the rural area and number of health
centres which have semblance of working are far
and few. Even if the opportunities are not
missed, which in fact they always do (in a study
done at the out patient department of Christian
Medical College, Vellore Steinhoff et. al 1985
it was found that as large as 57% of children of
who could be safely immunized went back with
out it), the impact on the coverage would be in
significant.
Vast number of
Primary Health
Centres are oddly placed so that accessibility
through public transport is greatly hampered (See
Table 3). Whereas, the WHO boldly recommends
that even for a single child a new vial should be
opened and that not to do so is a false economy
(WHO 1987), the Health Ministry blithely instructs
the Medical officers that a minimum of 10 children
EPI FULL COVERAGE OF UNDER-ONES AND
PREGNANT WOMEN 1978-1990
///
Health Statistics of India 1985, Central
Bureau of Health Intelligence, Ministry of
Health and Family Welfare, New Delhi.
65
60
55
50
45
40
35
30
25
20
15
10
5 —~"6pv<i
0
1978
START
Performance
As shown in Table 1, the DPT vaccination
coverage for India is stagnating at dismally low
level of 15.5% and that for Polio at around 7%
even after the five years of EPI implementation.
If we break down these figures for rural and
urban areas the hopelessness of the situation is
glaring (See Table 2).
What is the strategy adopted by the health
authorities to achieve the EPI targets of 85%
coverage by the year 1990 ? Does it inspire any
confidence ? Unfortunately the answer is in the
negative I
' //! I
/
1
// I
l/7 / ‘
W
/
■/
/
X-/ //
// /
///
27,
1984
MID-POINT
//
/
/
1990
TARGET DATE
hitute 17 vlnter 198S-86
2
f
M Pc -
I 3^
A\ i
per immunization session are necessary to make
the exercise economically viable (Sokhey et al
1983).
to the VHWs. There is little doubt that the pre
paration of the Handbook is a futile exercise in
isolation and most probably is an attempt to play
to the gallery. Disastrous gaps at the heart of this
strategy as revealed in the Handbook is yet another
hard evidence of missing link in the strategy of the
EPI. Clearly the Government does not mean busi
ness.
Out reach Operations and Campaigns
•1
t
f
For the population beyond 5 Kms. of the health
centre, the para medical staff has to go and im
munize en mass the children in villages. The popu
lation which cannot be covered through centre
based routine immunization, and out reach opera
tions, should be covered through campaigns
(Sokhey et al 1983). Both these parts of the
strategy as outlined in the Handbook are fine.
But it slurs over a crucial part of the problem which
is—are these teams of paramedics going to go
round all the villages beyond 5 Kms all round the
year continually immunizing the child population,
including those who are being added in the list
continually ? It does not also say much about
another curcial problem—who is going to regu
larly update the list of eligible children and bring
to the notice of the paramedics teams.
The infrastructure
Having played havoc with the village level
infrastructure in a most cavalier manner, the
Government can do precious little at the moment
to push for the coverage of the target population.
The EPI is suffering from grievous injury—self in
flicted no doubt ! The Handbook says that one
third of the refrigerators at PHCs are not working.
One is sorely tempted to speculate that the Centres
at which the 'fridges are not working, the electricity
is available and vice-versa I And there goes the
maintenance of the cold chain I If the para
medics have continuously to visit the villages
to immunize, who will look after the family planning
programme—the sacred cow of the Government I
(Iyengar and Bhargava 1987) Those who are
knowledgeable and realist do not need to be told
as to what will be sacrificed at the altar of the
Development!
Having thoughtlessly and whimsically got rid
of the vast net work of Village Health Workers
(VHWs) in the beginning of 1986 (in the middle
of the EPI campaign) and having failed to replace
them, the Government is faced with infrasturctural
vacuum at the village level, The Handbook which
was prepared in 1983 when VHW net work was
presumably intact and in place, does not even
assign and acknowledge these crucial functions
Ordinarily this should suffice as a critique of
the EPI as it is conceived and sought to be opera
tionalized here. However, we should add one more
point to it for the sake of record—what about the
supply of syringes and needles and their effective
sterilization. Injection borne hapatitis B virus is
TABLE-2
children
Percent distribution of under-1
found immunized in 1978
TABLE-3
Percent Distribution of Rural Population
covered by Transport and Medical Facility
DPT
POLIO
RURAL
8.70
2.20
URBAN
34.04
15.58
14.20
5.00
TOTAL*
^Totals are calculated on the basis of Rural-Urban
Percentage.
Source :
Survey of Infant and Child Mortality,
Office of the Registrar General, India,
New Delhi-1979.
Distance
Bus stand
Medical
facility
Within 2 kms.
44.7
34.9
2—5 Kms.
26.2
25.0
5—10 Kms.
18.6
24.1
10Kms and above
10.3
16.0
Source:
3
Survey on Infant and Child Mortality
Office of the Registrar General, India,
New Delhi-1979.
spreading like wild fire thanks to insanitary practices
(we must refrain from joining the AIDS mania).
How does the health authorities propose to cotain this menace, we have no clue.
eluding health services which asserts that most
of the dangerous infectious diseases in Europe
came under control, before such medical inter
ventions became available, due largely to profound
socio-economic reforms. In view of this his
torical experience it is held that medical inter
ventions are by and large irrelevant, if not useless
for improving the health status of the society.
Another variant of basically the same theory argues
that all types of medical interventions, including
the UCI, are not necessarily ineffective or useless
but given the socio-economic structure and forces,
being what they are, these interventions have no
chances whatever to succeed. They are merely
techniques and unless the socio-economic struc
ture is changed in certain ways, these techniques
in fact will remain ineffective and useless. The
logical outcome of this argument, although not
always explicitly stated, is to bring about socio
economic changes of certain kind before the tech
nics—health intervention measures—are implemented
to achieve the desired effects.
Control versus Eradication
We would certainly like to eradicate as many
infectious diseases as possible, which kill and
maim.
The considerations which should pre
vent us from going for eradication, when it is
possible, are those of costs and even more im
portantly distortions in the even development of
primary health care that may result. There is no
inherent tendency in the UCI to drift towards
eradication. No doubt, there are enthusiasts who
would like to give a push in this direction but
this has been soundly and wisely resisted by those
who are for healthy evolution of primary health
care (Hopkins et. al 1982, Henderson 1982)
Nor does that mean that at no stage of develop
ment of health care we should not push for
eradication. The only point is, that at this junc
ture it is premature and even quixotic to aim at
eradication.
There is no doubt some truth in the above
argument. The health measure technologies have
to be effectively integrated into the socio-econo
mic situation. It is also true that varying degrees
of changes in the socio-economic setup and even
health measures will have to be brought about.
But to fashion the multi-pronged strategy to alter
the health status of the community is a practical
question to be worked out patiently and dili
gently in practice in the real life situation. What
is possible and what is not possible, in this con
text, is not purely a theoretical question. To
insist a priority that since socio-economic changes
of certain types are not affected, the health inter
vention measures of this type or other cannot
succeed, is to mistake a practical question for a
theoretical one, a serious mistake indeed. Besides,
even if we do not challenge the analysis of histori
cal trend as a fact, which is open to serious
doubts, it does not necessarily follow that all the
societies at different time and places have to pass
through the same pattern of experiences, as though
driven by the force of the law of nature.
The UCI and Primary Health Care
As it is, the UCI has all the markings of a
vertical programme, that is, it appears to be out
side and independent of primary health care, con
ceived and imposed from above where the commu
nity by and large is a passive receipent. There
is a legitimate fear that the UCI might by-pass
and scuttle the fragile primary health care set-up
(This is discussed above in the section of strategy).
However, this is not inevitable. In the existing
situation, the viable strategy of the UCI must
make a judicious combination of elements of a
vertical programme and those of primary health
care. The target setting, the supply of vaccines,
maintenance of the cold chain and supply of
trained health workers, at least in the first phase
of the programme, when a huge back log of unim
munized children has to be taken care of—they
all have the hall marks of vertical programme.
Gradually as the UCI takes roots and becomes more
acceptable to the community, more and more
tasks will be taken over by the primary health
workers with an increasing involvement of the
community.
Such radical critiques have consequence, if
unintended, of rejecting one and all forms of inter
ventions strategies out of hand. Any modification
in the proposed strategy or even proposing a new
one is completely out of question by definition.
The government, as a result gets away with most
shoddy pieces of strategy without facing even a
token opposition let alone a serious opposition.
Reflections on some critiques of the UCi :
The UCI is open to a potential attack from yet
another angle. There exists a deeply radical cri
tique of health interventions of various sorts in
4
j
A few suggestions
5C9
From our critique of the Government's strategy
of the UCI above, it is clear that the Government
lacks the will and intention to carry out the pro
gramme of UCI efficiently and successfully in the
first place. If it were not so, the Government was
bound to take into consideration the critical features
of problem analysis which are established and well
known.
Problem of art of possible is not even properly
posed by the Government, where is the question
of its Solution.
Since 1978, when the UCI was first announced,
there have been several useful developments which
allow a degree of optimism that a progress towards
universal immunization is within the realm of pos
sibility even for a country like India whose socio
economic order is believed to be inimical to achieve
ment of such goals. This is so, for a simple reason
that many other countries whose socio-economic
order is not so much different from ours have done
much better than we have. In India also, in small
pockets where the will for immuization is found
the comparable high rates of immunization have
been achieved without unduly high investment of
resources. (Balraj, V. & T. J. John, 1986; Dyal
Chand, A. 1987).
The Art of Possible
A successful programme of immunization de
pends on logistics of vaccine supply at right tem
perature (2), at right time, at right age, at right
place and in right quantity in the most interior
villages of India and the resources in terms of
equipments and personnel that would be required
to carry out this exacting task (3).
coverage and made the whole process of immuniza
tion extremely cumbersome. This is yet another
boon in simplifying the immunization procedures
facilitating the involvement of VHWs and attaining
high coverage to provide protection to practically
all the children.
Let us now have a look at the problems of cover
age of various vaccines at village level. They are
problems of
different types. Most important
problem is that the Village Health Workers net
work is demolished without any replacement. The
VHWs, when they were there, and other primary
health workers were totally geared to the family
planning targets so the orientation and training
needed to identify and solve the problems of im
munization at various stages of the UCI at village
level were not imparted to them.
Therefore,
these vital gaps must be immediately made good.
The most important vaccine is measles vaccine
which is still to be incorporated in the EPI in India.
It must be immediately included in the EPI.
There are problems arising from the characteristics
of vaccines and popular response to various types
of vaccines. The polio vaccine since it is to be
given orally and measles vaccine since it is only
one
time affair, are largely acceptable to the
community. But they both require maintenance of
cold chain and measles vaccination in addtion
suffers from constraint that it cannot be given
before 9 months of age and must be given before
15 months of age if the children have to be pro
vided maximum protection against measles. (4).
These factors effectively rule out the policy of
routine immunization all round the year at village
level by even the well trained VHWs.
The main problem with the DPT is the post
vaccination reaction of transient fever and muscle
pain, especially among the children who can walk
and run. Because of this, parental reaction to
this vaccine is the most formidable block. Ac
ceptance of polio and measles vaccines also often
get adversely affected because of this. Happily
DPT vaccine is relatively stable at room tempera
ture (5) and DPT vaccine unlike measles vaccina
tion can be initiated at an early age of 6 weeks.
Through out the year DPT can be given. This
probably will have an effect of drastically reducing
the frequency and intensity of reactions, helping
to bring down parental resistance.
Happily there have been positive developments
in the last few years which pertain to improvment
in vaccine, improved storage and transport of
vaccine and simplified and more effective moni
toring of the 'Cold Chain' (Handerson 1984a).
They also include the epidemiological insight into
the efficiency of immunization. As a result it is
now known that immunization of children can
begin at 6 weeks for DPT and even earlier for
Polio (Halsey &
Galazka 1985). This small
looking insight has tremendous implications for
acceptance and high coverage of the most diffi
cult vaccine DPT, as we shall see. Large number
of epidemiological studies have been responsible
in knocking down one after another contraindica
tion (Galazka 1984) and unnecessary precuations
which created countless barriers on path of wide
This will have an additional and probably a
beneficial effect of dissociating two types of im
munizations e.g. polio and measles vaccination
on the one hand and DPT on the other.
5
Pulse Vaccination Versus Routine Vaccination
Notes :
Utility, effectiveness and feasibility of pulse
vaccination has been well established at Vellore
by the pioneering work of Dr. Jacob John and his
colleagues. In the context of the problem analysis
we have presented, it is obvious that there is no
opposition between the two approaches. They
both complement each other in accomplishing the
UCI and both support and strengthen primary
health care. The UCI can succeed and attain its
objective of child survival only if it is squarely
embedded in the primary health care.
1. To set the target for immunization programme
according to the Handbook (Sokhey et. al 1983)
first the population of Children under 2 years
should be calculated by the formula. Total
population X Birth Rate X (1-IMR)X2. From
this figure number of children immunized last
year should be deducted and the target should
be fixed at 85% of the outcome. But when
one looks at official figures one finds that not
only the targets fixed are much lower than that
can be arrived at by the above formula but
also the increase in the child population every
year is not taken care of; the target figures for
immunization remained same year after year.
(Health Statistics of Gujarat, 1984, State Bureau
of Health Intelligence, Directorate of Health,
Medical Services and Medical Education, Ahmedabad. Gujarat).
The DPT vaccination, thanks to relative heat
stability and effectiveness, even in infants as young
as 6 weeks can be carried out routinely and conti
nually at the village level by well trained and
supervised VHWs covering the young children
of 6-14 weeks. Since the total number of im
munization will be spread over 12 months, the
mind boggling problem of supply of large number
of needles and syringes and their steam steriliza
tion, as is the case when pulse vaccination is
carried out, is effectively minimised, Only a small
number of syringes and needles will do.
They
can be easily and efficiently steam sterilised to
kill viruses of hapatitis
B & AIDS. (World
Health Forum 1987).
Pulse immunization is useful in clearing out
the huge backlog and also for polio and measles
vaccination in the semi-annual cycles. (Sabin
1980). Problems of maintenance of cold chain
upto the village level are thereby practically
removed.
Concluding Observations
The Government of India although having
adopted the programme of the UCI by 1990. has
clearly no heart in it. It is totally preoccupied and
obsessed with family planning programme. The
child survival is yet to command the necessary
attention. The UCI is merely a decorative piece.
The Government of India in its single mindedness
could not care less about what happens to the
primary health care or so it appears.
Our case is that the UCI is basically a sound
programme—sound on theoretical and empirical
grounds. It has potential to improve the child
survival, it is an ally of primary health care, and
given the will and correct strategy it is within the
reach of possible.
The Government must be forced to adopt the
UCI with the sincerity and honesty of purpose it
deserves.
6
2.
In tropical climate vaccines are more difficult
to keep at the appropriate temperature. Even
highly heat stable tetanus toxide can be des
troyed within minutes when exposed to tem
peratures of 60 C, easily obtained inside of a
closed jeep parked in the sun (Handerson
1984).
3.
In a typical village of about 2000 population
there would be 100 children to be vaccinated.
If each child takes about 4 minutes, about 7
hours working day for that village will be
required.
4.
Target age group for different vaccine coverage
Polio
Antibodies to all 3 types of viruses
are
present
by
school
age.
Most paralytic disease occure be
fore age three (Beneson, A.S. ed.
Control of Communicable Diseases
in Man, APHA. Washington 1985).
Hence all the children from birth
to 36 months should be immunized.
DPT
Highest
incidence of whooping
cough and Diphtheria is found under
five years of age in India (Park J.E.
The Text book of PSM, Banarasidas
Bhanot, Jabalpur 1983).
There
fore all children between 6 week
and 60 months should be protected.
Measles
Most of the children will have an
attack before 3 years. Every child
between 9 months and 36 months
should be immunized.
(Park, J.E.
ibid).
’ Nv •
A)
5.
5(y)
WHO (1987) Expanded Programme on Immuniza
tion World Health Day: Immunization a Chance
for Every Child, Geneva, Switzerland.
Vaccine Stability at 37°C
Measles (unconstituted)
Approximately 1
week
DPT
Approximately 1
week
OPV
Approximately 1
day
IYENGAR, S. AND
BHARGAVA, A
(1987)
Primary Health Care and Family Welfare Pro
gramme in Rural Gujarat, EPW XXII No 27
July 4, 1987.
(Upto 3 weeks at 18°C
—22°C).
World Health Forum (1987) How to choose injec
tion equipment Vol. 8 No. 1 p. 116.
REFERENCES
Balraj, V&T.J. John (1986). Evaluation of a Polio
myelitis Immunization Campaign in Madras City,
Bull of WHO, 64(6): 861-865.
Dyal Chand, A. (1987). Community Financing for
Primary Care: Report of a Study. EPW XXII
(24) June 13, 1987: 951-956.
Galazka, A.M. et al (1984). Indication and Contrain
dications for Vaccines used in the Expanded Pro
gramme on Immunization, Bull of WHO 62:357366.
Halsey, N & A. Galazka (1985). The Efficacy of
DPT and Oral Poliomyelitis Immunization Sche
dules Initiated from Birth to 12 weeks of age.
Bull of WHO, 63(6): 1151 -1169.
Manderson, R.H. (1984a). Providing Immunization:
The State of the Art. Working Paper, Bellagio
Conference on to Protect the World's Children.
Manderson, D.A. Letter to the Editor; The Lancet
July 24, 1982 (Also in MFC Bull 126, March
1987)
Manderson, R.H. (1984b).
Contact 82: 10-14.
Immunization
Update
Hopkins, D. et al (1982). The Case for Global
Measles Eradication; The Lancet, June 19, (Also
in MFC Bull 126, March, 1987)
John, J. (1985).
17: 39-42.
Issues in Immunization, Future
Sokhey, J., Indra Bhargava and R.N. Basu (1983).
The Immunization Programme India: A Hand
book of Medical Officer Govt, of India, Ministry
of Health and Family Welfare, New Delhi.
Steinhoff et al (1985). Evaluation of the Oppor
tunities for and Contraindications to Immuniza
tion in a Tropical Pediatric Clinic Bull of the
WHO 63(5) 915-918.
Sabin, A.B. (1980). Vaccination against Poliom
yelitis in Economically under Developed Coun
tries—Bull of WHO 58(1): 141-157.
7
The New Drug Price Control Order
—A mockery of rational planning.
Anant R S
categorisation would lead to a sudden jump in
the prices of most of the life-saving drugs by
more than 40%. Critics have pointed out that this
increase in the mark-up is based on a study funded
by the OPPI (which represents the interests of
MNCs) though conducted by the National Coun
cil of Applied Economic Research.
Unless the
cost-data supplied by the drug-companies
are
available for independent scrutiny, such studies
cannot be taken as representing the true state of
affairs. That is why this increase in mark-up has
been criticized by many analysts. Secondly, the
idea of removing the life-saving drugs from cate
gory-l shows that the government cares little for
the life of the people and is 'bold' enough to take
such a shameless step.
So finally the crunch has come !
Something
which some of us who have been lobbying for a
pro-people rational drug policy, were hoping would
not happen. But with the declaration of the New
Drug Policy in December, 1986, the writing was
there on the wall for everybody to see—two things
were definite after the declaration of the NDP—
the basket of price-control was to be drastically
reduced and the mark-up on the price-controlled
drug was also to be substantially jacked up
almost doubled. What remained to be seen was
the precise extent of this price-decontrol and the
precise list of the drugs to be under price-control.
These two details have now been announced on
26th August. In analysing this new Drug Price
Control Order, one finds that the list of drugs
included in this new DPCO is not based on any
consistent principle or a set of criteria. Secondly,
there is no mention of implementing other re
commendations of the Kelkar Committee's report
on whose recommendations this new DPCO has
supposedly taken a final shape. Thirdly, there is
no sign of any mechanism to eliminate irrational
and hazardous drugs, contrary to the promise
made in the policy-announcement on 18th De
cember, 1986. The result is that the drug-industry
has got the best of all the worlds—comparatively
very few price-controlled drugs; almost doubling
in the mark-up on price-controlled drugs and no
obstacles to the production of irrational and
hazardous drugs or their combinations.
It reflects on the efficiency of "the Government
that works faster," that it took eight months to
decide as to which drugs belong to this new
category-l. There are about a dozen National
Health Programmes, atleast on paper, and it has
been reported that the officials of the Health
ministry prepared a list of 150 drugs to be included
in this category. But it is not the Health-ministry
which has a major say in the drug-policy, but it is
the Ministry of Chemicals and Petrochemicals
which holds the reins. These gentlemen quietly
kept aside this list, and instead, a list of a mere
27 drugs was included in Category-l.
This list has many shocking omissions. The
most glaring omissions from category-l are the
vaccines. This happens in a period when so much
is being talked about "the biggest ever vaccination
programme" to be executed in India as a part of
the strategy of 'Health for All by 2000 A.D.'
Drugs used for prevention of diseases should be
given top priority in Health-planning and hence
their prices should be kept as low as possible;
but since the drug policy is not seen primarily as a
part of health-policy, this elementary consideration
has not been taken into account. Exclusion of
Vitamin-A from Category-l occurs when 40,000
children go blind every year due to vitamin A
deficiency and when the Government has declared
a war on this national shame, with the help of a
National Programme for the prevention of blind
ness. Other National programmes have been for
mulated because they seek to prevent millions of
Shameless omissions :
The NDP of 18th December, 1986 had said
that the drugs under
price-control would now
be in two new categories—Category-l
would
consist of drugs required for the National Health
Programmes. The Maximum
Allowable
Post
manufacturing Expenses (MAPE, a new name for
mark-up)—for this category is to be 75%, as
compared to 40% allowed for the erstwhile cate
gory-l consisting of life-saving drugs—of the
DPCO of 1970.
To begin with, it is highly questionable as to
why life-saving drugs have now been shifted from
the old Category-1 (40% mark-up allowed) to the
new Category-ll (100% mark-up allowed). The
Government could have atleast retained them in
the new category-l (75% mark-up). This new
8
M H *9^1 Lt'Hw.
illnesses and deaths.
But the list declared on
26th August takes care of only Tuberculosis, Lep
rosy, Trachoma, Malaria, Filaria and includes oral
Rehydration salt for 'prevention of dehydration.'
It does not include even the oral contracetive
pill which is used in the Government's pet pro
gramme of family-planning. In the drugs for
malaria, Primaquin-the second-most important drug
is missing whereas
paracetamol
(available
under the brand-names like: Crocin, Metcacin..
etc.) a drug used in ordinary fevers, and which is
not used for treatment of malaria finds a place !
Such queer selection can only be called hair
brained ; and such gross omission of a whole
set of drugs required for many National Programmes
can only be called shameless.
CategoryI Drugs :
The Category-11 drugs are supposed to contain
'other-essential drugs.' It appears that this list of
139 drugs as announced by the government is a
truncated version of the Kelkar-committee's list
of 154 drugs. If we compare this list with the
guideline list of essential drugs recommended by
the WHO, we find many glaring omissions in the
government's list. Except lignocaine, which is
used for local anaesthesia, none of the drugs used
for anaesthesia-ether, halothane. Nitrous oxide,
oxygen, thiopental, scoline, neostigmine, atropine.,
etc. have been included. These drugs were not
included in the Kelkar-committee's recommenda
tions under the imbecile,
bureaucratic pretext
that these drugs are not "directly consumed by
human users." Morphine and pethidine, routinely
used in surgery are also missing. The secondimportant class of drugs not included in Category-11
are Anti Rabies vaccine. Polyvalent antisnake
venom serum (for treatment of snake-bite), di
phtheria and tetanus anti-toxin, all of which are
classical life-saving drugs; and are required in large
quantities in our country. Thirdly, many of the
skin-preparations
(neither Benzoic plus salicylic
acid-the classical ointment for fungal infection
of skin, nor the new antifungal agents like mico
nazole, nystatin) find a place in this list even
though fungal infections are quite rampant in our
country. What is most surprising is the exclusion
of the lotions used for the treatment of scabies—
Benzyl Benzoate and gamma benzene hexachloride
(BHC or lindane) even though scabies is typically
a very common skin-infestation in the poorer
communities and when the current prices of these
drugs are already beyond the reach of poor people.
Mebendazole, the drug of first choice for treat
ment of worms, is also missing. Ferrous sulfate
which is being distributed to millions and millions
of pregnant anaemic women and anaemic children,
is missing in this list, so is the case with calcium
gluconate, which is required in hundreds of tons
to be given to poor pregnant women whose bones
get depleted with repeated pregnancies.
It has been argued that drugs whose annual
total consumption in India is less than Rs. 50 lac
have been excluded; otherwise the practical work
of controlling prices of all and sundry becomes too
much to handle. It is difficult to take this argument
seriously in the world of computerization. But
even if one accepts this argument, the omission
of these common drugs which are required on a
huge scale cannot be defended. ANOTHER cri
teria that has been put forward is that of 'encourag
ing the indigenous producers.' Obviously minerals
like ferrous sulfate and calcium gluconate do not
require sophisticated technology, so is the case
with many skin-preparations. Production of Sera
is also not a new technology at all in India. What
is so peculiar about the technology for the pro
duction of morphine, pethidine, codein for them
to be exempted for price-control, when so many
drugs produced by the Indian sector by using com
plicated technology have been included in cate
gory II ?
One has to conclude that in making this list,
none of the criteria have been consistently adhered
to. The most important consideration that seems to
have been applied is to make this list as small as
possible and to please the big-shots in the industry.
The strangest thing that defies any logic is the
inclusion of a few drugs which are not in the
WHO essential drug-list and which are therapeuti
cally not important in the Indian context either
or are even obsolete.
These are : Baralgan,
Ketone, Bephenium,
Cyproheptadine, (healthgroups have asked for a ban on this drug !)
Levamisole, Piroxicam (a dangerous drug) Tetramisole and fifteen more such drugs. Instead of
these drugs, the really essential drugs mentioned
above could have been included without lengthen
ing the list, (if that is to be accepted as a cons
traint).
To offset the sharp price-rise in these essential
drugs due to this new DPCO, the Kelkar committee
had recommended the abolition of all taxes on
them. If the Government accepts this recommen
dation, there would not be a steep rise in drug
prices but the Government's income would come
down to that extent; to be made good by fresh
taxes on other items or higher budgetary deficit
9
in the next budget : Ultimately, the consumer
will have to pay in one way or the other for the
increased profitability of the drug-industry.
up was really less compared to other industries and
hence in need of an increase, such increase in
mark-up should be accompanied by a ban on all
irrational drugs and irrational combinations. Let
the drug-industry get an adequate rate of profit
without cheating the people. Then increased pro
fits can be coupled with decreased prices of drugs :
But even this simple demand is not being granted.
Apparently, for the power that be, moderniza
tion and march towards the
TWENTYFIRST
CENTURY does not mean adopting modern, scienti
fic planning 11
The ultimate result of this new DPCO is that
instead of 347 drugs under price-control as of now,
there will be only 156 drugs underprice control
and even in this category, the mark-up has been
almost doubled from 40 and 55 per cent to 75 and
100 per cent for category-1 and II respectively.
The result of this mockery of the concept of rational
planning will be experienced by all of us in a few
days.
The production of certain essential drugs currently
under short supply is likely to increase because the
Government has now almost doubled the mark-up
on these drugs. Now that the Government has
responded to the drug-industry's black-mail by
conceding a much higher rate of profit, the com
panies will now utilize the capacities kept idle as
part of their black-mailing strategy. But so long
as there is no ban on irrational drugs nor any
control on their profitability, the drug industry
would continue to focus on these production of
these non-essential but highly profitable drugs.
There is only one slender hope of forcing the
issue of controlling the prices of many drugcombiration. This can be done by putting a finger
on the definiton of Category I and Category II
formulations as given in this new DPCO. These
definitions specify category I and II formulations
as containing any bulk-drug either individually
or in combination, specified for either category-1
or Category-11 formulations. If we strictly follow
this definition, it would mean that any combination
containing any of the drugs in Category-1 and II
would be under price-control. For example if
a company manufactures a combination containing
say theophylline (a Category-ll drug) and 2-3
non-essential or useless drugs, this combination
would come under Category-ll and would be
under price-control. In this manner, hundreds
of drug-combinations would be under price-con
trol. The Drug industry would, of course resist
such interpretation but it is possible to force the
government to take its own declaration seriously.
There is a way out :
The text of the New Drug Policy released on
the 18th December, 1986, had said that A Na
tional Drug and Pharmaceutical Authority will be
created and Among other things, it would go into
the question of rationalization of existing formula
tions in the market including the banning of for
mulations of harmful nature." But since then,
there has not been any effective action in this
regard. Banning irrational drug-combinations is
important from purely price-aspect also. If only
rational drugs and their rational combinations are
allowed, the drug-bill of the consumer would be
more than halved I For example, most of the antidiarrhoeal mixtures contain one rational antimi
crobial agent and three to five useless or otherwise
irrational ingredients. In cough-mixtures, it is
difficult to find even a single really useful ingredient
recommended by standard medical
textbooks.
So called tonics, as is wellknown, abound in ir
rationalities and overdosages of water-soluble vita
mins whose only function is to enrich the sewerage
and the drug companies. If only rational combi
nations are allowed, the drug-prices would come
down drastically due to the deletion of unnecessary
ingredients.
If it is proved by independent study open to
public scrutiny, that the earlier 40% and 55% mark-
But the above is only to extract something out
of a hopeless situation. The real scientific way to
get out of the present muddle is to allow only
those drugs and their combinations which have
been recommended by medical text books and
by National Medical Authorities; to disallow all
other products and to give a uniform, adequate
rate of profit to all such essential drugs. There is
no need to make different categories within the
category of rational drugs and to allow differential
rate of profit for different categories. (The only
exception would be research-products.) If this
simple scientific demand is conceded, instead of
40-60 thousand formulations,
to be controlled,
or monitored, there would be at the most a thou
sand rational formulations made out of all the 250
essential drugs and say a hundred more secondline drugs. Let the drug-industry accept this simple
demand of making a good business without cheat
ing the people I
10
* W
t?
h -
5 'j
h
h
i.?3
■3
|
medico friend
a rcle
bulletin
S' C vV
1 '.J v
A
i
JANUARY 1988
V
Sex Differentials in Nutritional Status in a Rural Area of
Gujarat State : An Interim Report
a
PART—I
B
Leela Visaria
R
I 3
I
■<... ?
■2
a ;
^3 "
..... fl
E
E
p
E
“i
4
I;
|L;
< *
Women are regarded as both biologically
stronger and physiologically superior to men.
Biologically, the presence of a pair of X chromo
some protects women against chromosome linked
recessive disorders and makes them less suscep
tible to infectious diseases (1). Physiologically,
women are reported to be more efficient than men ;
for a.given quantum of work, they require some
what less protein and energy than men(2). Other
things being equal, these innate differences would
result in lower female mortality compared to that
of men; this situation is observed in most parts
of the world today. In the developed countries,
the sex differences in mortality has been widening.
By 1983, a difference of 7 to 8 years in the life
expectancy at birth between males and females
was not at all uncommon and was reported by
USA, France, Finland and Australia (3). The once
common maternal deaths have been virtually
eliminated. At the same time, the biological disad
vantage of men is aggravated by a stressful life
style and accidents, which account for a significant
proportion of deaths. The observed high male
differences in mortality at ages 35-75 in countries
such as Finland, France, USA and USSR are attri
butable to the higher incidence of cardiovascular
and respiratory diseases (including lung cancer)
and accidents among mon (4). In sharp contrast
to this general pattern is the situation reported by
the populations of the Indian subcontinent where
males enjoy lower mortality than females almost
from birth until about the end of the reproductive
period of the latter. This has been an important
factor contributing to the anomalous excess of
males in the population reported by the censuses
for nearly a century now. The age specific death
rates based on the recent large data sets such as
the Sample Registration System in India have
confirmed the excess female mortality suggested
by the earlier estimates of life expectancy at birth
and other ages, based on the census age data.
This paper is a preliminary examination of the
data on birth weight and on nutritional status or
weight gain among children under the five years
of age available from a research-cum-action project
in a rural area of Kachchh district of Gujarat state,
to see whether and how far these support the
widely held hypotheses about differentials in treat
ment between young boys and girls in terms of
food allocation and health care, being a major
cause of higher female mortality.
4
I
1
mJ
’ll
The Study Area
The study area was selected because of the
scope for collaboration withan NGO (non-govern
mental organisation) based in Ratadia village in
Mundra Taluka in Kachchh district. The NGO,
named Shri Sangh, is led by two health professio
nals, actively involved in multi-faceted develop
mental work while employed by the Panchayat
hospital with an attached maternity home. The
project area, spread over 25 villages, covers about
3400 households with a population of 17,000.
! I
Following a pretest in April 1985, a benchmark
survey of all the households was carried out during
June-July 1985. The region is very heterogenous
in caste composition and also has a long tradition
of outmigration to Bombay and other urban centres
and even abroad, to East Africa in earlier decades
and recently to the Gulf countries. This is reflected
in the sex ratio of population in rural areas of
Kachchh district, 975 males per 1000 females in
1981, was lowest in the State, compared to 1043
for Rural Gujarat.1
The action programme involves a careful re
cording of all the pregnancies, births and deaths
as well as monthly monitoring of the weight of
all the children below five years (or sixty months)
of age. (Measurement of height began in October,
1986). The growth monitoring activity began on
October 2, 1985 in five villages (total population,
2490; number of under-five children, 374). It
was expanded to four more villages in May 1986
(total population 3509, number of under-five
children, 414). The tenth village was added in
August 1986. In addition, we have data on births
that occurred in the maternity home since 1980.
5(y\)
boys and 28 percent*of girls, born in ourproject
area during 1980-85, had a birth weight of less
than 2500 grams. The intercaste variations in this
percentage are very small except that more than
50 percent of the Harijan children (45 percent of
boys and 56 percent of girls) had birth weight of
less than 2500 grams. Such babies are considered
"high risk" according to the WHO standards.
However, the Indian pediatricians report that
"full-term" babies weighing between 2000 and
2500 grams can survive with minimum inputs.
As noted above, the data do not include any in
formation on the duration of gestation, but about
5 percent of all children (4 and 6 percent of boys
and girls, respectively), and 15 percent of the
Harijan children (8 percent of boys and 23 percent
of girls) had a birthweight of less than 2000 grams
and were "at risk" according to the Indian "stan
dards" as well.5
The observed sex difference in birthweights
in our project area was similar to that in the data
for the reference population of the National Center
for Health Statistics (NCHS). On an average,
girls weighed about 200 grams less than boys
at birth but the difference was not statistically
significant. The intercaste differences also do not
seem to be significant. The limited number of
observed births might be the likely explanatory
variable. Yet, surprisingly, among the Barot babies,
the average birthweight of girls exceeded that of
boys by 110 grams. Unlike other women in this
region, the Barot women tend to be tall and betterbuilt, but the observed difference is certainly not
statistically significant6.
Sex Differences in BirthWeights
Out of about 200-225 deliveries occuring in
the Ratadia maternity home each year, between
60 and 70 percent are to the mothers who come
from the project area.2
The hospital maintains
records of all the deliveries with details about
the caste, education, occupation of the parents
along with the sex, parity and the birthweight of
each baby.3 Over the six years 1980-85, recorded
birthweights are available for almost 800 babies
from the project area villages.
On the whole, boys do not begin life with any
marked advantage over girls in our project area.
We shall next examine whether and when in the
course of next five years, clearly identifiable dis
advantages emerge which adversely affect the girls.
Admittedly, the information on the gestational
age of the fetus is net accurate. Most of the
women come to the hospital for the first time
at the time of delivery or register their names just
a couple of weeks before the date of delivery.
Therefore, the information on the time elapsed
since last menstruation, given by the women or
their relatives, is accepted at its face value. The
hospital did not until recently ascertain the gesta
tional age of the fetus independently through
measurement of the fundus height.
Dynamics of the
Observation
Child
Population
2
■ani
................................................................ ■■
c
c
r .
■j
i >I
- '•
■
-,
-:
Under
In our programme of monthly weighing of
children, the base population changes every month.
Apart from the loss of some children because of
deaths, some children cross the stipulated age
limit; some migrate from the region permanently
with their families or are temporarily away; they
are not weighed. Some children may not be
brought for weighing because of illness or because
parents are busy or for any other reason. The
changes in the denominator as well as the numera
tor need to be monitored every month to assess
the proportion of children weighed and the reasons
Interestingly, the percentage distribution of
children of various caste groups according to their
birth weight Shows that both the mean and the
distribution are similar to those observed in many
other Indian Studies (cited in Visaria, 1985)4.
About 25 per cent of the children (22 percent of
a..':
-
%
-
't
c
i
J A vi v A >
-J
-'J
"•'J
-J
J
■ for the non-weighing of others. A summary of
our data on the subject in Table 1 below indicates
that close to 90 percent of the children eligible
for weighing have been weighed at least twice.
In a given month, however, this proportion may
be somewhat less, partly because of temporary
migration.
vention period. If ages of certain children could
not still be ascertained, reference was made to the
other children in the family and occasionally
even to the weight of the child. In the latter cases,
judgement of the health workers might have in
fluenced the recorded age, although we had to
resort to this approach only in very few cases.
Further, prima facie, the sex composition of the
under five children, who were weighed, shows a
preponderance of boys
(52.7 percent) over
girls (a sex ratio of 1113) but its underlying factors
remain to be explored. An analysis of data by
village also will have to be done in order to under
stand the sex composition of the young children.
Children are weighed on a Salter spring balance
scale which is calibrated for 100 grams. The scale
has to be suspended from a beam. The health
workers have been trained in the procedures of
weighing the children, reading the weight accura
tely, managing the child who is fidgety or crying
and recording the weight in a register as well as
on the growth chart, which is kept with the mother
and which she brings during the weighing ses
sions. The mother is shown the plotted graph and
is told how her child is faring in relation to the
previous month's weight and in relation to the
reference curves.
Table
3
J)
1
Dynamics of the Under-five Child Population in
Nine Villages of Kachchh District
““5
Boys
■*75
''0
-'C
... 0
'"0
1. Total number of underfive children listed in the
Baseline survey plus new
births.
2. Number who completed
five years or permanently
migrated or died before
weighing began in 5 and
4 villages in
October
1985 and May 1986, res
pectively.
3. Number
weighing
eligible
4. Number
once
weighed
414
Girls
374
I if
i|
il
Ii
I
I
All
788
34
37
71
380
337
717
40
37
79
336
88.6
302
89.6
638
89.0
I
Subsequently, the weights of these children
are plotted on large graphs separately for boys
and girls so that both the weight distribution of
all children and the weight increment status of
each child over time are readily comprehensible at
a glance.
HO
1 ’la
I
The nutritional status of the project area children
is assessed by using the data gathered by the
National Centre for Health Statistics of the United
States of America (NCHS) as the reference popu
lation. These data are based on a sample of Ameri
can children which contains between 300 and
1600 children in each yearly age group. In addition
to height and weight, other anthropometric mea
surements are also available such as arm and head
circumference, skinfold thickness etc. The Indian
standards prepared by the National Institute of
Nutrition are not based on anthropometric measure
ments for a sufficiently large sample. The NCHS
data are increasingly considered as most suitable
for use as an international reference. One of the
advantages of NCHS reference is that the measure
ments are available separately for boys and girls.7
for
only
5. Number for whom pairs
of weight measurements
are available and whose
weight data are analysed
5 as % of 3
I
: P1
So far, we have been able to collect data on
weight only. (Measurement of heights of the
children has begun in October 1986. It is expected
that the height of the children will be measured
once in every three or four months, because the
increments in height are very small). The median
or the mean curve of the NCHS reference data is
taken as the standard. Cross-sectionally, very few
Indian children fall above the mean curve. The"
other three reference curves on the growth card
Distribution of the Children by their Nutri
tional Status and Age
A list of under-five children was prepared for
each village on the basis of the baseline survey
data. The list was again checked and updated and
ages were verified at the time of weighing of
children which began in five villages in October
1985. Updating was done for births, deaths, mig
ration and completion of 5 years during the inter-■5
3
HI
hl1
5 I
I
'1
iI
I
;
ih E
•
;
i.
show the two standard deviations below the mean,
three standard deviations below the mean and 60
percent of the mean, for each age. The area bet
ween the three standard deviations curve and 60
percent of the mean curve is shaded and warns
. the health workers and the mothers that the child
falling in this region is a high risk child and should
be watched carefully. Those children who fall
below the 60 percent of the mean curve are clearly
in the very high risk category and would need
nutritional supplementation under careful super
vision. A single episode of illness in such children
can be hazardous.
i'
i i!
i I;
il
I
I
*
11
Table 2 examines all available pairs of weight
measurements in terms of weight gain, constant
weight and weight loss. The salient findings are :
1. While 3 percent of all girls (majority of them
were in the age group 0-5 months) were above
the NCHS median, and 35 percent above the two
standard deviations from the mean curves, the
corresponding percentages for boys were less
than one and 34, respectively.
2. A higher proportion of girls (23.6 percent)
fell below the three standard deviations from the
mean curve than boys (20.8 percent). Thus, the
proportion of girls at the two extremes of nutri
tional status was higher than that of boys.
On the whole, after the age of six months, the
nutritional status of each child that prevailed during
a major part of the period shows a remarkable
stability in the weight increment status of children
in the sense that they rarely "Cross over" to the
adjoining reference curves.
3. As might be expected, during the initial
six months after birth, 90 percent of the children
fared well in terms of their nutritional status mea-
Table 2
Number
of
children
Total
Pairs of
Observa
tions
-
■
-
€
J
t1: ■
Distribution of Pairs of Observations of Weights of Children in Project Area According to
Their Nutritional Status, Direction of Change and Sex
Nutritional Status
c
Percent of Children Showing
Weight
gain
Weight
unchanged
Total
,
■
t
e-N
Weight
loss
e,
HiI
‘1
I
I j!
-i
II I ’
Boys
Above the Mean
2
5
100.0
bet. mean & 2 SD
114
481
71.3
10.2
18.5
100.0
bet. 2 SE & 3 SD
150
762
60.5
11.4
28.1
100.0
bet. 3 SD & 60% of mean
59
270
62.6
11.9
25.5
100.0
60% of mean
11
41
61.0
7.3
31.7
100.0
Total
336
1559
64.3
11.0
24.7
100.0
100.0
cf
O-
€ l:
£
Girls
Above the mean
9
33
72.7
9.1
18.2
100.0
bet. mean a 2 SD
108
456
67.8
11.8
20.4
100.0
bet. 2 SD a 3 SD
115
575
67.7
10.6
21.7
100.0
bet. 3 SD a 60% of mean
58
343
61.z
12.5
26.3
100.0
60% of mean
12
61
54.1
18.0
27.9
100.0
Total
302
1468
65.7
11.7
22.6
100.0
4
G
G|
e'.As
•
ih
Bl
j
■3
O
9
j
9
9
9
9
9
9
■4 9
9
<9
' J3 9
B
'3 9
■ ' J 1'9*
'.'■3 G
->
3 9
S3 9
9
J 9
j
J ?
as
■J
I
9
..
J F
JI
J
■ J «
J
A
J A
•J
J 5
J
J 0
J
■
J «
j ;
j-
J ’
I-/?
MFc FhILchn Mo
sured by weight; but a higher proportion of girls
(12.3) than of boys (4.7 percent) fell in the "at
risk" category. The birth weight of a large majority
of children puts them between the mean and the
three standard deviations curves, and their growth
pattern broadly follows the standard curves.
4. After the age of six months, however, falter
ing of growth begins among both boys and girls.
The percentage of children below the three stan
dard deviations curve rises to 20-25 percent or
more from about six months upto four years of
age, with a relatively small sex difference. A proper
feeding of the children during the post-weaning
period as well as managing the weight loss or
lack of gain due to infectious diseases seem to
pose a problem.
5. After the age of 3 years, a markedly higher
percentage of girls, than of boys falls below the
three standard deviations from the mean curve.
However, given the small number of children, the
sampling error is large and the observed sex
differences are not statistically significant.
6. As indicated in Table 2, on an average, we
have 4.7 pairs of observations of weight per child.
About 65 per cent of the observed cases of both
boys and girls relate to weight gain. About 23-25
percent of weight observations indicated loss of
weight between two successive months. The extent
of seasonality in weight gain or loss, is yet to be
explored.
Another way of looking at the serial weight
measurements (discussed by Jelliffe 1966) brings
some of the above observations in a sharper focus.
Ideally one needs a minimum of one year's weight
observations in order to calculate the average
monthly weight gain by age. However, to obtain a
larger number of observations in each group,
weight data for five villages (where the programme
was launched in October 1985) and those for four
villages (where it was launched in May 1986) are
pooled. The data for five villages based on 11
months' observations show a sex and age pattern
very similar to that evident from the pooled in
formation as for nine villages. The data indicate
that the total weight gain of the project children
upto five years of age was 68 percent and 77
percent of the mean standard of the NCHS for
boys and girls, respectively. Interestingly, girls
faired better than boys in relation to the standard
from the age of 6 months onwards. At every age,
the difference in the weight of boys and girls in
the projects area is smaller than observed in the
NCHS reference data.
The data also indicate that the weight gain of
the project area children was short of the NCHS
standard more during the first year of life than
during the next four years. Within the first year of
age, the growth shortfall was somewhat more
during the second half or the
post-weaning
period; the difference was particularly marked in
the case of girls.
Notes :
(refers to numbers in small print)
I
1. Besides rural Kachchh, an excess of females in
the population was reported by only one other
area-rural Valsad district (Sex ratio of 993
males per 1000 females) according to the 1981
census.
2. According to our baseline survey, nearly 30
percent of the births of the previous one year
in the project area took place either at Ratadia
hospital or at a similar institution elsewhere.
This figure is quite high for a rural area of
Gujarat. In rural area of Gujarat State as a whole,
the Sample Registration System has reported
less than 13 percent of the births to be occurring
in an institutional setting during 1982 and 1983
(SRS 1982, 1983).
i!'
3. The hospital nurse generally weighs the new
born on a spring baby weighing scale which
is calibrated for 50 gms.
i
4. Prima facie, the implied sex ratio at birth of
1154 boys per 1000 girls appears implausible
and needs to be investigated.
5. An effort is under way to trace each of these
children to find out how they have fared later
in terms of their weight and survival.
6. Barots in Kachchh are largely engaged in animal
husbandry and maintain large herds of goats
and sheep. They also own some milch cattle
as well as land which is generally unirrigated.
The Barot women are quite active in tending
the cattle and also appear to enjoy decision
making power in household matters including
marriage.
7. For a discussion of the NCHS data, and their
advantages over other similar large data sets,
see : (Waterlow, 1977).
(Contd. in the next issue')
5
J
4 ,
fl ~ 11V
pdo
Sex Differentials in Nutritional Status in a
Rural area of Gujarat State
.
.
‘
.
(r'o.b'
.'■V ■Tav
PART II
1
Leela Visaria
I
‘
.
i,
r
]|
I' lr
I
Il I
1
Medical Intervention in the Event of Fatal
Illness
A review of studies and our own data on nutri
tional status provides little clear evidence of a
discriminatory behaviour towards girls.
The
question then arises; are there differentials in the
prevalence as well as the incidence of infant and
childhood illnesses ? Unfortunately, the relevant
information on morbidity patterns in our field area
is not yet analysed. However, what is available
is the information on infant and child mortality,
from our efforts at continuous recording of vital
events. We have tried to ascertain from the
parents of each deceased child, the symptoms
preceding the death of the child, the medical help
sought (if any) along with the names of the
practitioners and v/herever possible the actual
treatment. One of the doctors attached to the
project in Ratadia has examined these records to
indicate further whether and to what extent the
cause of death can be diagnosed from the reported
symptoms.
I-1
young girls were also taken to the "doctors"
outside the village, when there was no "health
medical practitioner" within the village. (Out of
nine villages for which data on death are presented,
six had no "doctor" within the village, their resi
dents had to travel about 5 to 7 kms. to reach a
village with a medical practitioner. Each village
is connected with Ratadia by bus communica
tion, with at least one service per day.) In the
case of four girls, parents even went to the district
head quarters (Bhuj) and to another town (Anjar)
to consult qualified trained doctors. Perhaps,
our study region is a typical relative to other parts
of the country. The contacts with urban areas
as well as outside world have perhaps influenced
the perceptions of parents about seeking help in
the event of illness. Yet, given the wide sex
differentials in mortality, one cannot help wonder
whether parents
seek
medical help for their
daughters when it may be too late to do much
to save their life.
■
■
■■
.V
c- ■
Discussion
I fl
lu ;
1
II!
fl
I
The data relating to the infant and child deaths
during the 15 months since our benchmark survey
conducted during June-July 1985—upto Septem
ber 30, 1986 are summarized in Table 3. The
number of female infant deaths was two and a
half times that of male infants. But, yet, because
of the small number of events, it is difficult to
generalize about the sex-bias in the incidence of
fatal illnesses or in the utilization of medical help
prior to death. However, diarrhoea, infections
of respiratory tract and post-measles complications
account for close to 80 percent of all deaths.
The remainder were due to congenital problems,
prematurity or sheer "wasting away", presumed
to be due to chronic infection.
Interestingly, the sex bias, which is believed
to exist in the seeking of medical help, does not
seem to be extensive here. In the case of three
female child deaths, and one male child death the
family had relied on home remedies only; the
percentages of these deaths to total child deaths
were 17.6 and 14.3, respectively. Yet, overall.
4
I.
On the whole, we cannot identify any clear
sex-bias in health care or food allocation in our
project area in Kachchh. Yet, the difference in
the number of boys and girls succumbing to death
appears quite so that one has a feeling that some
where something goes against girls in the process
of growing up. The one dark area to which we
referred earlier is the timely recourse to medical
help provided to girls. Is it sought too late ?
In the instance of two girls (both belonging to the
Rajput caste) we were told plainly that only home
remedies were tried because they were girls.
Strangely enough, one of the girls was a second
parity child; the earlier daughter born to the
mother also had died in infancy, The other girl
was a tenth parity child, with two surviving
sisters and six surviving brothers.
(Another
daughter had died earlier). In the case of a third
child (fifth parity, with two surviving brothers and
one surviving sister) belonging to a scheduled
caste, poverty was apparently the reason for not
seeking help from a private practitioner in the
nearby village. While help at Ratadia is free.
c
e
■' '■
A
'
L
■
I ■
J
if
E
:
rvc>- /?7Z
MFc -
Related to the Antecedents
Infant and Child Deaths
-
Males Females
1. Population of nine villages *
2617
(July 1, 1985)
■
S'-
SiS
-p
.■'I
3^
_5_
12
17
3. Child deaths (July 85Sept. 86)
2
5
7
•4. Total deaths under age 5
7
17
24
1
8
9
3
4
7
1
2
3
1
1
(July 85-
5. Symptoms preceding death :
(ii) respiratory
fections
tract in-
(iii) Measles and post
measles complications
(iv) congenital problems
(v) premature birth
2
3
3
6
2
2
(iii) in another village
2
5
7
(iv) in the neighbouring
urban area
1
4
5
(v) used home remedy
only
J
2
6. Medical help Sought :
(ii) within the village
'2...
2
2
(vi) 'Wasting away'
(i) at Ratadia
J
Another issue, noted during our field visits
but not yet investigated in any depth, is the posi
tion of Rajput women in the community. The
available anecdotal information indicates that at
the time of marriage of a Rajput daughter, her
parents bid her farewell for good and give her,
among other things, even a shroud to cover her
dead body. The parents apparently do not hope
to see the married daughter again. Quite pro
bably, this practice is a relic of bygone era, when
the transport facilities were limited and maternal
mortality high, so that these women rarely had a
chance to visit their natal homes. The transport
facility is important because the Rajputs of Kachchh,
called 'Jadejas', had to marry non-Jadeja Rajputs,
of whom there are none in Kachchh.
(The
Jadejas of Kachchh claim themselves to be the
direct descendants of the ruling family of erstwhile
princely state of Kutch. Although today most
of them are small cultivators with their women
folk supplementing the limited family income by
spinning yarn at home, their behaviour and temper
resemble that of a feudal ruling caste. According
to our baseline survey, the Jadejas formed a little
over 20 percent of the total population of 10
villages). Therefore, spouses for marriageable
children had to be found in other parts of Gujarat
as well as Rajasthan. Even today, many daughtersin-law, brought from some districts of Rajasthan,
have come to Kachchh from more than 500 Kilo
meters away and have not visited their parental
homes even once in several years. Also, unlike
in other areas, the Rajput marriages were tradi
tionally performed in the village of the bridegroom,
with the bride brought there with only four escorts.
All
5150
(i) diarrohea
V
of
2533
2. Infant deaths
Sept. 86)
o
was a labourer engaged in stone-quarrying (consi
dered so arduous that apparently the workers need
to rest for a day after every three or four days of
work).
TABLE 3
Statistics
1
3
Further, the married Rajput women observe
'purdah', stay indoors and do not take up work
outside their homes even when their family is
poor. They do not even fetch water from the
village well or collect fuelwood; these tasks are
done by the men; or those who can afford, employ
servants for the work. During their conversation
with us, the Rajput men often cite these facts
to argue that their women enjoy a high status in
the family and are spared the arduous chores that
women of other communities have to perform.
However, Jadeja
women,
especially young
daughters-in-law, narrate very different grim tales.
They recognize their low status and feel that they
are a burden on the family.
4
* It has not been possible to register vital events
in one of the villages due to internal conflicts;
our health workers have not been able to carry
out their tasks, except for monthly visits to
weigh the children.
-d
J. ’
.7.
K -
r3
’/-clrrM-A
money needed for busfare and the loss of a day's
wage can be a problem. The mother of this
unfortunate girl primarily collected fuelwood for
sale to the Rajput households, while her father
5
AJo '2 7,
Mli-
2n^
Another point reported during our interaction
with some of the women was that girls are not
sent to school so that after marriage they may not
narrate their woes to parents through letters;
And yet, some informal channels presumbably
operate to facilitate exchange of Rajput news
about daughters between Kachchh and other
areas.
In recent years a small percentage of-Jadeja
women have become literate or educated and
young girls have started going to school in large
numbers. The educated men are taking
up
salaried jobs in urban areas;
they take their
spouses with them. When they visit their native
village, their urban culture presumably has some
demonstration effect on others. In the short run,
each caste group functions virtually as an auto
nomous entity, hardly subject to influence by
other castes. Over time, however, pressures do
build up to alter the traditional behaviour.
s p;
' >•
I!!
'I
i'
!il
i
r |
i2
Jadejas form a small minority in our project
villages as a group but in some villages they are
a dominant group. There are indications, how
ever, that the position of Jadeja women and
indeed of other women has begun to improve;
the question is one of accelerating the frustratingly
slow pace of change. The social scientists must
cling to the fond hope that their efforts at under- ■
standing the prevalent situation will facilitate
the social engineering necessary to loosen the
foundations of
centuries-old
prejudices and
behaviour. To serve this purpose, the social
science research on such issues will have to
assume a multi-disciplinary character to unravel
the complex web of intra-family relationships.
We shall attempt to pursue these issues over the
next two years.
I
I
REFERENCES
1. Waldron I (1983). “The Role of Genetic and Biological
factors in sex differences in Mortality", in Lopez AD and LT
Ruzicka (eds) “Sex Differentials in Mortality; Trends, Determinants
and Consequences', Australian National University, Canberra,
pp141-164.
2. Rivers JPW (1982). “Women and Children Last : An
Essay on sex Discrimination in Disasters" Vol. 6, No. 4, pp 256-
267.
3.
United Nations, Demographic Year Book, 1984.
4. Lopez AD (1983). “The sex Mortality Differential in
Developed Countries" in AD Lopez and LT Ruzicka(eds) 'Sex
Differentials in Mortality : Trends, Determinants and Conse
quences', Australian University, Canberra, pp 141-164.
STEP BY STEP
Towards An Appropriate Medical Education
The CHC/CMAI/CHAI/CMC-L Project on 'Strategies
for Social Relevance and Community Orientation
in Medical Education - Building on the Indian
Experience’
was based on a long involvement
of the primary researchers in exploring how
medical education could be made more relevant
many
to the needs of society. These included
CHC,
initiatives
before the formation of
followed by some during CHC’s formative years.
This report therefore ’Orings
wrings together the key
initiatives/reflections of the
researchers
which
preceded the study and helped to £ive
the project greater focus.
CONTENT LIST
INTRODUCTION
STEP BY STEP
A* TOWARDS AN APPROPRIATE MEDICAL EDUCATION
B.
REFLECTIONS OF AN INTERN (1972)
C.
TRAINING DOCTORS FOR COMMUNITY HEALTH SERVICES (1973)
D.
LESSONS FROM A YEAR OF TRAVEL AND REFLECTION (1982)
E. MOVING BEYOND THE TEACHING HOSPITAL (1988)
F. MEDICAL EDUCATION
G.
TOWARDS GREATER SOCIAL RELEVANCE (1989)
AN ALTERNATIVE VISION OF EDUCATION FOR
CARE (1990)
DECENTRALISED
HEALTH
appendices
FEEDBACK FROM PIONEERS GF A RURAL BOND SCHEME (198a)
TO GOVERNMENT OF KARNATAKA
MEMORANDUM ON A HEALTH UNIVERSITY
(1988)
III
MEDICAL COLLEGE (1989)
'PROS’ AND 'CONS’ FOR AN ALTERNATIVE
*** Tyr
MFC ANTHOLOGY HANDOUT.
CCi4MUNlTY HEALTH CELL,
Zommunity
Health Awareness, Research And Action,
Society For
325, V Mam. 1 Block,
Koramansala.
3ANGALORE 560 031*
■ HP/
[^6
Child Care and the Prosperity of Punjab
S. N. CHAUDHURI*
not able to give adequate attention to their
children especially those who were ill
this
resulted in some not reaching the health
centre when they should.
I had visited Punjab once in 1968 and again in
1983 The change 1 noticed over the years was re
markable The people looked prosperous Entering
Ludhiana city the sight of thousands of television
antennas on the roofs was really impressive. Coming
tom Bengal where one is used to the crowded city of
Calcutta and of rural areas Wlth thatched or tiled
roofs mud walled houses, unpaved roads, the con
trasting signs of prosperity as evidenced by a profu
sion of scooters and well paved roads was very
significant.
In the villages around Ludhiana, the fields were
under intensive cultivation, with bullocks as well as
tractors. In many places Punjabi farmers had parked
£r scooters next to the field while superv.smg the
labourers or giving directions about farming and g
culture. The village houses were all of brick and
cement and neatly whitewashed. In many ot the
yards there were tractors, motor cycles, scooters as
well as agricultural machinery for cutting fodder an
other chores.
Most of the farmers own atleast 15-20 buffaloes
and the houses have furniture and television sets.
Even in the houses of scheduled castes there were
buffaloes as also goats reared for meat . Most of the
roads were paved.
During visits to the houses of some of the farmers
including those of the scheduled caste we however
discovered certain aspects of child health not in con
sonance with the overall prosperity.
milk was not
*
Immunization — second and third doses
were not always possible because the mothers
were working on the field.
*
Mothers who had to cook for large numbers
of farm labourers and family members were
diluted
*
The mothers were aware of ill effects of bottle
feeding, repeat doses of immunization, family
planning operations and facilities available at
the health centre. This awareness could not
always. be
be translated into practice because of
work
and other pre-occupations.
their
• Director, Child in Need Institute, Vill: Daulatpur, PO Amgachi Via Joka, 24 Parganas, West Bengal:
It is logical to think that the level of child care
would be high in the presence of such prosperity.
Milk is in abundant supply and the normal Punjabi diet
based on wheat, dal, vegetables and milk products is
naturally a balanced one. Most of the children looked
apparently healthy.
Bottle feeding with
uncommon.
mostly to the male
Attention was given
t
’ > was often
children rather than the female who
neglected and ill.
These observations once again brought into
focus the socio-cultural factors of discrimination bet
ween sexes,, the wilful neglect of the female child,
the status of women and their bearing on mother
and child health. Though these were simihar to other
parts of India, the evident prosperity of Punjab did
not seem to have made any dent on these issues. In
the face of this social reality will improvement in the
health of mother and children remain a distant
mirage!
Many of the primary and subsidiary health centres
did not have the usual crowd of patients.
MBBS doctors were posted to the subsidiary health
centres which were adequately stocked with medicines
needed for day to day care. Primary health centre
workers move around in well organized beats to covei
every house, enquiring after everyone’s health and
referring patients to the centres if necessary.
*
*
9
medico friend
circle
bulletin
JULY
1985
v'ii'9
Blessed are the smaii in size — if they ere Indians
Kamala S. Jaya Rao
(A debate has been going on over the past 4—5
years regarding the meanin ; of malnutrition and
the significance of small body size. The debate is
published mainly in Economic and Political Weekly,
land to some extent, elsewhere alsoi. The debate was
sparked off by a study by V. M. Dandekar and N.
Rath on the measurement of poverty in India. Since
the whole debate is of topical interest land concern
to mfc, Anil Patel has been coaxing me to write
about it in the Bulletin. I have been hesitating
because,
being
a debate
mainly
between
economists and statisticians, I felt I cannot do am
ple justice to it. However, I agree with Anil about
the importance of the subject to mfc and Abhay
Biang assured me it is not too late even now to
write about it. I have, for obvious reasons, kept
absolutely clear of all complicated statistical
definitions and 'arguments. Yet, I hope, I have bro
ught out the essence of the debate, and more import
antly, the implications of it.)
In 1971, Dandekar and Rath published the
results of their study on measurement of poverty
in Indila. The definition of poverty is relative, and
varies from place to place and, from time to time.
Any criterion chosen to measure the incidence of
poverty has, therefore, to be necessarily arbitrary.
However, there has to be strong logic in using thlat
particular criterion. Dandekar and Rath used the
mean per capita energy requirement of la household
as the cut-off point: percentage of households con
suming less energy than this value should be con
sidered a percentage of population thlat is poor.
The argument being that the income of the house
hold was so low that it did not permit them to buy
adequate food to meet the specified energy. There
fore households with such low energy intakes may
be considered poor and therefore income levels of
such households be considered as being below the
poverty line. This argument sounds logical It js
well-known that in countries where malnutrition is
a sizeable problem, the major cause is poverty. It
is also known that in poor households, a major part
— 80% or more — of the total income is spent on
purchase of food. Dandekar and Rath therefore
considered income levels which did not meet with
the mean per capita energy intake of a house
hold, as being below the poverty line. Thus esti
mated, the incidence of poverty, in the seventies,
was 40%. It is necessary to point out one thing
here: this does not mean thlat a household with low
energy consumption (less than 2A250 Kcals) is
necessarily poor or that one consuming more than
2,250 Kcals is necessarily not poor. The figure
only indicates that by the chosen ykrd-stick the
incidence of poverty in India was 40%.
Dr. Sukhatme objected to the use of the mean
energy intake as the cut-off point. Perhaps Dr.
Sukhatme would not Have objected if the figure was
higher, but strangely
and unfortunately the
figure was 40%. Let me explain this. In a large
population, if the values follow a normal distribu
tion (statistical normal) the mean and the median
values will be similar-, so, Half the population
will have values above the mean, and half below the
mean. Dr. Sukhatme largued that if nearly half the
population is to- be considered undernourished, the
other half must be overnourished. Hence, there will
be no one with normal nutrition! Therefore, the
use of the mean figure as a cut-off point was wrong.
If you notice, the focus took a strtange turn. While
Dandekar and Rath said that about 40% of the
households were poor, Sukhlatme said that 40% of
the population was not undemjpnrished
Dandekar (EPW 16 (30) 1241, 1981) pointed
out this anomaly. He said, ‘I wish to emphasise
that, all through our little study on Poverty in
anci-
Indih, Rath and myself have been discussing pover
ty and not undcrnutrition,.
control of body weight is exercised through
llary co-factors’.
When a population is classified on the basis
of a certain income or expenditure, howsoever deter
mined, .... we are defining poverty
on the
the other hand, if we classify la population by its
energy intake, we are trying to identify undernutri
tion
The two are related,
But the
two are not identical’.
‘The only inference I dan draw is that energy
intake is used with variable efficiency by means of
some homeostatic mechanism working for the good
of the whole body and controlling body weight in
the process
The real controlling variable of
the homeostatic process is not energy balance,
but fluxes, pressures, electric potentials, concentraand body
temperature,
environment,
tions
etc.’
‘However, 'a point is reached in the
intake; below which the body is not able to
maintain body temperature and is forced to part
with its fat to maintain weight. That is the point
of undernutrition, also alternatively called the
lower threshold value of the homeostatic fatage,
for maintaining nutrition state, of the body. In ?. .
Kerala, external temperatures are close to body
tempera;ture, heat dissipation is negligible
and
body weight can be maintained at relatively low
intakes’.
1 will explain in a little more detail why
Sukhatme is not willing to accept the mean figure
as the cut-off point. However, it is necessary to point
out that while Dandekar wlas considering energy
intake of households, Sukhatr c was talking of
energy intake of individuals.
The riange of values for any parameter indicates
that the value for that parameter is not the same
for every individual studied. Different indivi
duals have different values, and the whole forms
the range. Thus there are variations in values of
individuals, that is, there is inter-individual Varia
tion. Apart from this, there is an intra-individual
variation. For example, if my pasting blood sugar
is 80 mg% one day, it may be 75 on another day
85 on another day—but all within the normial range.
I will not comment on Sukhfatme’s knowledge
of human physiology. Perhaps, he should have stuck
to his own field of statistics and not strayed into
nutrition and physiology. He calls the ‘-2 S.D
level’, a threshold value. Thus, wittingly or unwit
tingly, he Was invested this statistical cut-off point
with physiological significance. It is important to
remember thht this so-called ‘threshold’ is a stati
stically derived value for a set of energy intiakes. If
nutritionists were to discover at any later date,
that what they hitherto considered the meah energy
requirement w|as an error, and that the mean Is
actually higher or lower than the presently consi
dered value, the 2 S.D. value may also change.
1 hen, will the body also change the level kit which
it is ‘able to maintain body temperature’?
According to Sukhatme, the inter- and intraSndividu'al variation in energy intake of individuals
of a given physiological group, are similar. Thus,
if the energy intakes of females of my lage and body
size were to range from 1900-2500 Kcals, my
energy intake on different days may also vary from
1900-2500 Kdals. Sukhatme derived this by analy
sing data published by other workers. His conten
tion may be true, or may not be true. The reason
for my doubt is not on statistical grounds; but
from a purely common sense point of view, it seems
incredible that the variation can be so large.
Nevertheless, we shall accept it in the absence of
any contrary data. This being the case, Sukhatme
slays that one should consider only values below—2
S.D. of Mean as low intakes. Thus estimated, and
according to Sukhatme, the incidence of under
nutrition in the country is only about 2,0%, or half
of the figure derived by Dandekar. Dandekar, in
turn, analysed data published by the NNMB, using
the criterion suggested by Sukhatme and found
that 40 — 45 % of the households had energy inade
quacy. Dr. Sukhatme prompty rejected this on
grounds that NNMB data were not reliable.
Now Sukhatme’s argument Was that since in a
healthy, active population half of them are expected
to have energy intakes less than the mean, if we
accept Dandekar’s figure of 40%; it shows that the
population is healthy, active and normal! We
must remember that energy intakes of half a nor
mal population will indeed be below the mean but
but if their requirements were higher, they dan af
ford to buy the extra food Dandekar was saying
that 40% of the households had incomes which did
not permit expenditure on food to meet the mean
requirement. He therefore Sarcastically asked whe
ther in a healthy, active population half of them
should have such low incomes too! He said Suk
hatme Was unable to clearly see the distinction bet
ween poverty and undernutrition■ the two are re
lated; but not identical, phenomena. He then said,
‘Sukhatme is confused’. I do not 'agree with Dande
kar. Sukhatme was not confused. Sukhatme sim
ply tried and succeeded in confusing nutritionists as
well as ’administrators, by neatly^ exploiting the
fact that Dandekar used energy requirement as a
yard-stick to meiasure poverty. Sukhatme’s argu
ment that undernutrition is far less than 40%, and
his use of terms like ‘threshold value’ — have come
in handy in many quarters. Dr. Gopalan put it mild-
Two questions arise here. If a nornial indivi
dual’s energy were to vary between — 21 S. D. to
4- 2 S. D. of mean, why can it not on occasion fall
below — 2 S.D. too. Why should he be classified
as undernourished if on one day his value is this
low; in the n'ext few days he may go back to the
above—2 S.D. level, since his intake is highly vari
able. Secoridly, how does the body deal with such
large variation in energy intake? Sukhatme gave
his answer (EPW 17 (50) 2000, 1982): Tf the con
trol system in the body were to tolerate energy
balance of this order and yet maintain body weight
within narrow limits
(it) means that the
2
M vc
i
ly when he said that this has ‘generated the unfortu
nate impression among policy-makers that under
nutrition is not a serious problem in the country
any more’ (EPW 18 (15) 591, 1983). Sukhatme
himself proudly proclaimed (EPW 16 (32.) 1318,
1981): ‘Already the term mild malnutrition has
disappeared. . the principle that an individual eating
below the recommended intake is at risk and that as
the intake decreases the risk of deficiency increases,
is being reformulated’. Whoever has helped Sukhatme
in performing this hat trick, I am certain it is not
the sensible among the nutritionists.
J
1^5“
5(V) )0
eager to know what this wonderful biochemical
measure is, but would have been immensely grate
ful to Sukhatme had he declared its nature.
Whether it is warranted or unwarranted to
label them as. undernourished, the fact remains that
a large number have a small body size. In Nepal
and Sri. Lanka which are our neighbouring coun
tries, and whose data Sukhatme Was published
(EPW 17 (50) 2000, 1982), ignoring India, only
40—60% have normal body size. So at le'ast 40%
have small size (height or low body weight or both).
Strange, but we have come back to the figure of
40% I What about this? Tell them, tell the policy
makers and planners they are ‘small but heialthy’
says Sukhatme. They can work hard, they do not
die; in other words, they Wave ‘adapted’ to this
and they are in no^ danger.
In assessing nutritional status, energy intake
cannot be the sole me’asure. In fact, a single ass
essment by itself is not a reliable indicator. It has
to be taken in conjunction with anthropometric
measurements, at least, height and weight. Irres
pective of whether values below mean energy require
ment or below—2 S.D. of mean, should be consi
dered as undernutrition, if 'a large portion of the
population is underweight or underheight or both,
this needs to be taken note of. Since undernutrition
is a major cause of growth retardation in a country
like ours, this should also indicate the incidence
of undernutrition in a population. If Sukhatme’s
argument w'as correct, then a large proportion of
the population should have normal body size, which
we know is not true. Sukhatme was quick to rea
lize that
this
argument
would
crop up.
In fact, he was quicker than the nutritioni
sts, who for some reason kept quiet for a long time.
Either we were overwhelmed by the statistical lan
guage, or the whole debate was considered to per
tain only to statistics. Or, Sukhatme succeeded and
he totally confused the nutritionists. It w’as an
opportunity lost for the nutritionists and a tacti
cal gain for Sukhatme. To forestall the above argu
ment, Sukhatme advanced two more hypotheses
leading the issue into 'a very disturbing and dang er
ous situation.
c
It is indeed true that the small body size is an
end-result of
adaptation.
But what is this
adaptation? A growing child cannot grow normally
if the building material, namely nutrients, are lack
ing . That is, there is growth retardation. The orga
nism in order to survive physically, has cut down
its growth rate to conform to the energy available.
Here,, instead of food being sufficient for normal
growth, growth has suffered due to 1'ack of food.
This
‘adaptation’
cannot be
considered
a
normal
state
but
as a
compromised
state, and at what physiological cost it has occured
we do not know Gopalan said (EPW 18 (15) 591
1983): ‘Adaptation, in the current context, repre
sents not a stage of normalcy but one of ‘ strategic
metabolic and functional retreat”
‘The assumption that these stunted children are tperfectly
healthy and functionally as effective and productive
as children with normal growth and development,
is a sweeping one
The new low levels pro
posed as the limits of calorie adequacy (mean —2
S.D.) may be a good prescription for a “survivial
ration” which will permit mere existence. Those
interested in building a strong vigorous nation, of
healthy productive adults, and of 'active children
who can run, play and bounce about.... may how
ever not be prepared to buy such a prescription’.
However, it is not hard to see that there are many
who actively welcome such prescriptions.
First, was the postulate of a threshold value
He said (EPW 13:1373 1978) “fortunately for most
of us, unless the intake is too low5 the efficiency
of utilisation of energy is improved. Therefore, ar
intake lower than the average may not cause an>
hardship unless this was so low that the power of
regulatory mechanism is diminished’. Although he
argues that Values above 2 S.D. are all normal
(which may be true), implicit in the words ‘too
row’ and ‘so low’ in the above passage, is the ack
nowledgement that values below the mean may be
low. Then he acknowledges that in their ‘own sur
veys in Uruli — Kanchan and in villages around
Pune....the body build of children living on in
takes, smaller than the Average was certain!v
small’, and adds 'a strange comment that ‘the infer
ence that they were
undernourished . . . .was
found to be unwarranted on biochemical examina
tion of blood ! And, I was under the impression that
nutritionists were yet to find a biochemical index
more sensitive th'an body size to assess undernutri
tion. If food intake and body size are not good indi
cators of undernutrition, not only would one be
Sukhatme’s argument is two-fold. Since the
mild and moderate degrees of malnutrition can take
care of themselves we need to bother only about
the severe cases and their number is small. Even if
this be true, Gopalan pointed out a fallacy (NF1
1983 and Apr. 1984). The so-called
mild, moderate and severe forms of malnutrition is
an arbitrary classification. More importantly, they
are not static conditions. The mild and moderate
cases can and do slide into severe degrees of mal
nutrition. Therefore to think of extending help only
to severe dases is extremely unwise. This would in
effect mean that we wait till a mild case becomes
severe and then extend help to it. This is like the
Sanskrit saying that one starts digging a well after
the house has caught fire.
3
ough looking small in stature for their age, c'annot
be considered to be under risk of developing mal
nutrition5’.
This argument about small individuals being
‘adapted’ individuals who are at no risk unless they
go below a ‘threshold’ level is a very harmful
theory. This is relegating a large part of the popula
tion not merely to remain small in size but to suffer
all ills of which the small size is a consequence.
Therefore Asok Mitra, formerly of the Planning
Commission, said, “the turn the controversy has
taken in recent years has not helped in reducing
malnutrition. . . . (but) has sought to bring about
what 1 once called instant revolution .... Intellec
tuals and scientists responsible for introducing
this line, must be held cle’arly accountable. I would
not hesitate to call it harmful, witting or un
witting
sophistry because in
other forums
of debate, we
grade the progress
of people
and countries for instance ... ^. by the • average
national weight and height. . . . For our own child
ren we do not consider small bones, low height,
small weight, low physical perform'ance and low
energy level “beautiful” or “good nourishment'’
& all’. (Future 11:12).
If you have not read' the above passage carefully,
please do so. We are told we have a problem of
poverty. As 'a consequence our children are small
in size. But that will improve, when economic
conditions improve. However, do not be anxious
about the economic conditions. They take a very,
very long time to improve. But even otherwise, the
children have adapted to the low food intake 'and
will continue to survive. God bless them.
In case you are the type who will not believe
what an Indian tells you and want to hear it from
a white-skinned ‘expert’, here is David Seckler
endorsing the Indian’s view (Seckier in Newer
Concepts in Nutrition — Maharashtra Assn.. for
Cultivation of Science, Pune. ED. P.V. Sukhatme
pp 127-137). Seckier says there are two types of
smallness, one ‘due to poverty, to poor physical and
socio-economic environment’. Second is due to
malnutrition. He says in the first instance the envi
ronment should be improved; and, Sukhatme has
already told us that this is a slow process, but the
children though small in size arc under no risk.
Now, any ‘sensible’ person would ask sooner or
later, th'at if the population is not under risk, if it
is ‘small but healthy’, why should even the environ
ment be improved? That will automatically solve
so many other problems, will it not?
Sukhatme’s second argument is that the small
body size is not a consequence of undernutrition
but is due to poor environmental sanitation and
diarrhoeas. That these two have a role to play, no
one would deny. But to say, undernutrition has no
role to play whatsoever, without supporting evi
dence, is most unscientific. On the other hand,
there are any number of animal experiments, where
environment has been maintained evenly and the
anim’als showed growth retardation when food was
restricted.
Regarding the second one. Seckier s'ays inter
vention should be addressed towards individuals.
What soirt of intervention? In Seckier’s own words,
‘The great challenge to nutritional science is
to
devise anthropometric indexes based on safe mini
mum standards rather than maximum genetic
potential’.
When Dandekar and Rath spoke of the incidence of poverty, Sukhatme diverted it towards
undernutrition, and says undernutritiOn is no big
problem in the country. The statistical jargon and
formulae were enough to totally confuse the nutri
tionists. Then he talked of “adaptation to low
energy intakes” and made many off the cuff state
ments regarding energy balance, BMR, genetics etc.
Thfe message is clear. Sukhatme says we need
not eat as much as the nutritionists ask us tot eat,
and which the Americans, Europeans and many
others are eating. We do not die even if we cat less.
We are doing all the necessary work. Yonr pro
blem is you are shorter 'and lighter than the
Americans. So what, but you are ‘healthy’.
The papers were published in the EPW which
most biologists do not read anyway. The arguments,
on the other hand, being outside the field of econo
mics, the economists kept quiet. Having however
acknowledged that body size is small, he has ad
vanced the ’‘small but be'autiful” hypothesis. And
now, ultimately this body size restriction is said
not be due to undernutrition but poverty. But, what
is the extent of poverty he does not mention. He
says (EPW 17: 2000, 1982) : ‘The second problem
we are confronted with is the problem of poverty,
small stature in
children
is
the
direct
result of this poverty ’and low socio-economic sta
tus, expressing itself in miserable conditions of
living. Intervention to deal with this problem need
not be focused on food and water ............................
As overall economic growth increases environmen
tal conditions may be expected to improve. This
will necessarily be ’a slow process, but this aspect
need not disturb us unduly because these people
will normally be in energy homeostasis and alth-
Seckier says, who told you, you are small. You
are aiming too high. Why should you be so tall and
so heavy. What if your own nutritionists have
shown that when nutrition, environment and health
care are good, your children grow up like the
Americans. You need not reach the Standard. Bring
down your Standards. So, eat food bare enough to
keep you living and bring down your anthropome
tric standards. See, there is no problem of either
undernutrition or small body size.
By equating sheer ability to survive, with
health, Sukhatme and Seckier have declared that
there is no problem of under nutrition. The exis
tence of poverty is acknowledged but implied is
the meaning that we need not be much exercised
(Continued on
4
page 6)
•
»
• 1
(Continued from page 4)
labout it, since the people are ‘healthy’ and survi
ving. It is obvious that this will be most welcome
to a government, which hitherto did not know how
to1 deal with this problem of poverty and under
nutrition. We can now, not make even a show
of socialism' and can, as is being done nbw, talk
more openly of computers, colour TVs, delux cars
and what not. It is, therefore, important that
this issue is again taken
up freshly — the
issue of poverty and under nutrition. Previously
we were told we were small in size because of
racial and genetic factors. When this was disproved,
we are now told being small is no handicap. Suk'hatme’s arguments have led the country into a
dangerous situation, and created a happy situation
for those who want to see us always small, poor
land undernourished. We must realise that the three
go together and cannot be artifically separated, as
Seckier has tried to do. It is time some economists
nutritionists and other scientists write strong y
land clearly about this issue. This is not
statistical exercise, as the nutritionists hitherto
thought. Nor is it a question of mere
nhvsiology as perhaps the economists are tmnk
kins It Ts a very importlant issue of whether the
See will s^vive7 as fstrong, independent natron
or not.
I
'' ‘ f
-
rv- JvavU
Mi-U (J J
PRESENT medical education IN
Q TTOP1
op
THE RELEVANCE OF
RURAL INDIA.
making doctorsfok ---------- "
Th.,. 1=
quarters.of all doctors mmam m
where only 20 /. o bur p
<
reflect the effortsof a
| espoused by our leadc's ,
d
I ficance when it is rem
I doctors are trained at
exp a
I expense of the comm m m^m
I"."
(1)
it
o{ dcvelopment
is of greater sigmthe vast majority of
the s(„te j. e at the
,
<
why hos
g
.n appr0.
-
I
■ to answer them.
B
Let's clarify at the ou c-e
y
doctors in rural
improvement-
| As economy shall hv.P.ove uv* ^dj3eases in general.
an upper class and caste
education and over t
carry their urban bias through their
their professional life.
almost total cultural and ecoThese factors lead to ..... frOm village life. Their
nomic
doctors ^ntiv i ban education
nomic alienation
aiienanun of the
v.<
r in a modern, predominantly
participation in a modern, pre omi
comes from
leadsrto
to a^^^^Xofional
a change in perspective
process leads
and ecomic
having an
"having made it ’I" haung
than manua|
on a
security which is based o
pride (we al-e
elitist
position
creates
labour, i his elitist position c
d.ssociatja(, from rural life,
the cream of our country )
3greed, developed
The medical education sy
«
when
in a colonial way in the pre-lnidepen en
[npdjc31 educ.
independence came, ms ead of adaP^
sore„
|inrm<.my with other cogs in
■ Doctors, again have
1
cc0!ld clarification tnat
■ the health care system Uem
determ es
■ the type of health c.
m m the country,
is
■ the type of medical educethj3 sy;.Aenl
e
ation system to our needs, w
diffusion of a cultural
of medical sciences (am
-certa;n cultural
innovation fr°m the western world^
definitely
political and social
COuntry
in ind□gainct the Wider mtcres^^fpducat.on.s,n g translation
ustrialized
fr°m '"tB
Ixxssv'Z
■ Z. BMP'.
medical education
■
The question now, is tne presen
rural India? No it
H system relevant in mak'”g d'X'Tngmined assumptions
isn,t- Let\bXrXX> which are detrimental to this aim.
in our medical p-
Fi,„. b.M IM*'
,
M
d skilled piofessional g.oup.
£«, h..» n..p.
social responsiwill defend its .
91 billty La., y.
s|<i|ls in a private as opposed to a
S assumed right to use its s c Is >
;;ssuniptions. we
K social contact havmg J
irit0 the medical
E go onto the raw mntem I
(
tha; 8S /• of doctors
g colleges. A^|®nScSanie ftlm urban families and 697. of
K working at
eqp education. Moreover. 96 /. of do■ their fathers had coileg ., .°
■ ctors were either io
D or land ownmg
■ vile9e Of PI?Xot a
W institution, but not a
bu;jnesSi go,.t. Gervice
ell;cycd the very special pnA11W|S may be the most elits
'
earl siXties to the "commuThe need for reorientalion in India was much
T^nSw^"
■l”’m“’
in our present
^paratVthe "core” of natrual
scienceTnom the -ciocultural
•b7“
“'"Z”
■'enVelo^e'X
,“c,'in9 “
s'“"d'“SZsZ“ -—
which a doctor in a
9
medicine faster. Third,
devising of
of inexpensive
inexpensive
doctor is much
the disease load
10ad per u.
umt
in an infectious
ou. dlseas3S
diseases ar
higher.. Qualitatively, oui
era . Medical education
to be and child mortality etc.
educa!on. had
htdJ°,J|
he.m problem.. «l
me.em.l
Medical'education has
This regrettably didnt come about.
Incorporated oui ur- bias and hence
zxzzzszzz
‘ , different picture is seen in other
students in seven medi-
■
m » 7ZX0, «>• »"'» 36''
I zzz
•■.1
,tei' “■
STI
_ Yogesh Jain
AllMS Study also revealed
hers had college education. The
Brahmin or higher non
that 887. of doctors were from er taring the medical prote
Brahmin castes. Clearly, peoplean urban background with
ssion tend to come from education and generally from
predominantly public school
. These students would natural y
I lrf
. m. 'I” •ZZXZ.Z
U«
Much mo>e important is t.
I
and malnutn8 lion shall decrease a
______
live, highly technical
‘ZXeZ: ’Z—.
ogyT-----•
fields and aspire to use
(5)
- iq
|M i£t
to make a doctor relevant for rural India.
Fourth, as per recommendations of Bhore Committee
and Mudaliar Committee, Govt, agencies had taken the
major responsibility for dealing-with health problems of
India. An enormous network of services was established &
the medical education should have been influenced by this,
i. e. it should have geared itself to train doctors to man
these services and not for private clinical practice.
Any analysis of the medical education would be
Incomplete without a discussion of preventive and social
medicine. These courses were started in medical colleges
to serve as a catalytic agent to bring about social orientatj ion of medical education. It was a challenging task but
| the experience of adecade and a half showed that the
i impact of these departments so far does not appear to be.
i as distinctive and enduring as one would have hoped (8).
i On the other hand with creation of PSM, teachers of me
| dicine, surgery etc. have in many instances stopped teachii ng the preventive aspects of their subjects (9). This has
i out at the very root of teaching of comprehensive integrated
I medical care.
To conclude, the present medical education alone
can't be accused for the present dearth of quality and qu
antity of doctors in rural India, simply because the content
of medical education alone is not very important in making
doctors for villages. What is of prime importance is our
values due to our predominantly urban background. Lack
of adaptation in the medical education system handed over
to us by the British is also responsible, we ought to learn
i from the success of the China barefoot doctor in managing
’ the health problems of an equally populous country.
h
; REFERENCES:
1] Pocket book of Health Statistics: 1980, GOl, P70.
2] Ramalingaswamy, P and Neki, K (1971): student s pre
ference of specialities in an Indian Medical College,
British Journal of Medical Education, V : 204-209.
-• 1: Doctors and Society: Three Asian case
3] T. -N. -Madan
studies Vikas
Publ. House 1980: P82.
...........
’ 4] C. E. Taylor, Doctors for the villages, Asia Publ. House
i|
1976. PP
PP 48-9.
48-9.
.
...
hjj 5] 1976,
D. Banerji (1966) social change and Scientific advance.
Their relation to medical education: Journal. Ind. Med.
|l
47 : 429-33.
I 6] Association,
Prywes, Moshe (1971) : The balance of research, teac
hing and service in medical
education :
education:
Mlnervat
!
IX: 451-71.
7] See '5' above
' 8] National Institute of Heal. ' Administration and Education
(1966): Report
of the conference
Ronnrt &
ft recommendations
recom
on teaching of PSM in relation to health needs of the
country. New Delhi.
91 ’bid.
9J
.4»y“ -
(6)
j
■
J -A
a
8
J J
K
a '
medico friend
circle
bulletin
MAY 1987
i '
j.--
Integration of Medical Systems
i ■’
i?
(A theoretical Perspective and Practical Blue Print)
■i0
S.K. Kelkar*
Broadly speaking. Eastern people are known for a
synthetic mind and for having a wholistic vision.
Occidentals are highly analytical but tend to be
fragmentary in their approach. With very well
developed communication channels and the
.w cultural
fluxes to which the world today (India in particular),
is subjected to, it is inevitable that the two have to
meet at many points and possibly head for a common
culture.
■>2
E
Tn
X-fA
j;,
x;
/
identical. The other common ground is that of
patient welfare of which cure is one part albeit an
important one.
’
there is certainly scope for
---- 7Here
exchange. We would have to discover
---------- fo/c'/cry
every
disease its most effective pathy. The identity loss is
only partial and it will be in the areas where knowledge
’
’been proved to be incorrect or obsolete or both,
has
in either pathies. To that extent no one needs to
grudge the identity loss. The words homogenous
and not-uniform are important. When the dis
tinctive features come to stay side by side they do not
assume the characteristics of other pathy and still
do not clash or turn antagonistic. It can be further
stated that we are for Unity and not for Uniformity.
Medical systems also cannot escape it. T../,
people
in India have voiced various opinions about the
...e
existingmedicalsystemsin the world. These opinions
border from almost fanaticism to fragmented isolated
thoughts. But the broad principle which appears
to be surfacing frequently in all these currents is that
Desirability: I think the question of whether it is
there should be integration of medical systems es
desirable to integrate is superfluous. The necessity
pecially the Indian Ayurvedic system with the Western
appears to be a foregone conclusion., Certain
Allopathy. While we think of integration several
aspects of this need elucidation. Allopathy as it
aspects must be understood, first. What exactly do exists is a very effective proven science in disease
we mean by integration; the desirability or other alleviation in many areas and has shown enormous
wise of integration; and the attitudes-involved-as potential-for growth due to its research orientation.
regards this word and process on both allopathic and The statistics of disease mortality ratio reduction,
ayurvedic sides.
proven remedies on statistical basis etc., is not so well
developed in Ayurvedic sciences. Yet Allopathy
Integration can be considered as bringing two
is not a complete science. Its approach is on the
dissimilar entities together on certain common grounds
basis of structural changes preceded by functional
of utmost importance, taking something from and
changes on tissue level. Allopathy has developed
giving something to each other without losing special
identifying features of noble virtues, with the inten tremendously as regards elucidation of structural
tion of developing later into a homogenous new changes even chemical changes which are also struc
but not an uniform new. That Ayurveda and Allo tural. That knowledge needs to be utilized by others.
pathy are dissimilar there is no doubt. Yet there are
broad areas like anatomy, surgery, which are almost
I
a_____
-VI
r
♦With help from P.N. Kulkarni BAMS, Ashvini Hospital,
Nadikeri
i •
I
1
’
1
Mi-C
MR
Although there is an attempt to discover the forces
of mind, intellect, subconscious, unconscious existenc
es, soul etc., they are by no means weU found out
The Ayurvedic orientation is substantia y i.i
realms of existence. This can be used for developing
more mature attitudes in people towards disease
entities and to life itself. Again these two have to
meet somewhere. Whether spirtualism, however we
developed could keep a disease state away is; sti
debatable. Ramakrishna Paramahamsa s and Vi
kananda’s diabetes can be give as examples,
comment upon this,
area of research.
Causal Cures?
This could be an important
Symptomatic Cures?
Suppressed
illnesses?
o£
Ift
' above
.1.
There is an alWe have discussed faith
’ ; Indian
most universal belief in the
1------- mind that Ayurvedic cures are delayed but permanent. So w tn
HoXSy: O„ .bo
i. is bold .h.. AlldP^c
On the re1----------cures are symptomatic and not causal.
causal, They sup—■‘■"'j dormant
press the illness but the disease remains
subscribe to both. In most
this needs to be studied.
in the body. I do not
i are only controls to be achieved
places for both there
by continuous medication in the form of medicines
There
is
an
attempt,
logical,
for
arrangement
of
or certain other practices, dietary, yogic massage,
There is
data in older sciences, arrangement of citing past change of environment etc.
v ■
It
is
needed
experiences
and
to
learn
and
to
teach.
L
experiences
that everybody knows about these ways, Definite
This belief has come about due to a lack of under
havVbeen demarcated in Allopathy where the standing about allopathic thinking. Allopathy ha
areas J---causology and treatment of diseases is highly un established the physical basis of illness on the structui
satisfactory. it
It is worth its while to discover their side by demonstrating the structural change/devia
solutions in other pathies for the benefit of human tion from the normal. There is a spectrum of nor
malcy of structures which is not uniform, thou h p
kind.
arl normal. The immune system as.we understand
if
are n
• concept of why disease
Faith: People have an uncanny faith in the powers is ]argely the basis of our
occurs. There are demonstrated alterations on the
of pathies other than Allopathy,. Allopathy has 0CCurs. There are
uuuy cells
vuho and
—d i:immune cells, ims
V
Indian mind, physical plane ofi body
failed to generate it especially in the
t
hasnotbeenaccepted by the laity and Ayurvedachans
This faith takes to a level of their being a panacea to
alike. The possible reason is that it does n
all forms of illhealth. It is worth its while to prove with the Tridosha theory for which physical basis s
If
we
do
so
we
will
have
a
that this faith is correct.
lacking as having not been demonstrated Th
gold mine uncovered. Strictly speaking, it is equally
essential to say that if we cannot prove it by methodo- jin itself is due to the fact that all body mechanisms,
io0gkai7e's'ear”c]Jthat the faith is wrongly formed and say;
iowing have not
say, swal
swallowing
not been
been btoken
that as a science it is either worthless or will have to structural
structural elements,
elements.
These st™ctu
The
state its limits and potentialities once for all. This cons
titute a unit
functioning o i P
constitute
u...... —
i
been ascribed a
means that the whole of Ayurveda will have to be indiv
idual structural units have not
individual
restated about where it fails, where its applications particular unique function which^noi other dissimilai
in a demust be recognized and tissue can carry out. This has been done etmrtural
are limited, where its powers
monstrable
fashion
on
the
basis
of
the
structur
where it can supplant or supplement Allopathy.
The subsequent
deviations from normal in Allopathy,
of functions resulting in disease is the
derangement c.---its
higher
forms
is
costly,
Cost: Allopathy in
basis of allopathic concept of disease.
comparatively
distant
and
The Tridosha theory lacks it.
hospital oriented and
somewhat beyond the reach of the common people.
Still in more manageable disease states the answers
This has resulted in the2 non-acceptance of the
Allopathy has, is more effective than the other pathies. cause or disease anu
led to the
of disease and has consequently
c
One cannot dismiss it on this bias alone, as long as non-acceptance of the permanency of cure regarding
other less expensive alternatives are not found out.
A further problem related to
Ayurvedacharis are afraid that they
Cost wise Homeopathy is definitely cheaper although th^fs^that^he
is that the Ayurvedacharis
it is time consuming in its process of diagnosis and will have to replace their basis of understanding :h
■■
‘ -» replace their basis
can be practised (truly that is) at a consultant level
causation of diseases..........
if they accept Uns whmh v-o^
-y"
:
if this school
accepted ? It is a
of thought of disease causation
■
fe
'I:'
1
II
I
J
!
.“beM, .0 or rhooih. or or-. »«»•'«” '■
2
..
A/
.
ii
.,z-A
E
■J
a'"3
■ J-3
T'3
iZ*
. i.«
J V
•J
i.e., of reawakening the vital force or the immune
system, are only truths stated differently and not two
different theories. I will clarify this point by anti
cipating the next question: Do we consider the
immune system to be the vital force? The answer is
probably that the immune system is one manifestation
of the vital force on physical level and there are
probably others about which not much is known.
Scientific function abounds with speculation of it
but it has not become science yet.
very complicated question and I do not have the
answer. One way out is to watch the more discrete
disease labels in Allopathy, say, pulmonary tubercu
losis or pneumonia by a similar disease label from
the Tridosha theory disease differentiation.
Historically in Allopathy the syndromic represen
tation of similar diseases was comparatively greater.
When structural studies progressed the syndromes
were broken down into disease entities. This was
also done by finding out the variations of one symp
tom common to all these diseases grouped into a
syndrome and by delineating the associated
symptoms which are found in some but never in
others. This was further substantiated by marking
the association of prior occurrences with the deve
lopment of more severe illness. For example, the
diagnosis of acute glomerulonephritis and rheumatic
fever are almost always associated with a minor
throat infections which pass oft' even without any
treatment. It forms the basis of diagnosis and has
considerable importance.
Defining cures and the criteria of cure:
Since there are difficulties in understanding the
theory of causation of diseases the question of defining
what is cure becomes almost impossible. The varia
tion of symptoms especially in time is the one that is
clearly understood by Allopathy. I do not think it is
indistinct in Ayurveda. Defining cure is essential in
clinical settings if the treatment has to be evaluated.
Probably the definition of cure for each evaluation
of disease is the greatest difficulty when it comes to
double blind clinical trials and that too involving
two systems and not two drugs from one.
J}
As far as I can see the grouping of diseases in
large syndromes with comparatively less differentia
tion into individual labelled disease is very much
present in Ayurveda. For historical reasons the
minute differentiation of this into more discrete entity
has not reached the scale as in Allopathy. (It is also
true that even in Allopathy, some diseases remain at
the syndromic level in the present state of know
ledge.)
J
J
j z
J 2;
k
J
J
J
■
feu
'■'"1
■'
.
i
For instance, in the case of jaundice, people tend
to take ‘native’ medicines of which several are known.
Generally the time duration of jaundice is from 3
days to 3 months and according to Allopathy most
patients will recover between 20-28 days provided it
is Type A. It does not have any serious complications
and the body is left intact. By the initial blood
testing we can always get a fair estimate that this
Whatever it may be, the fact remains that the jaundice is likely to last for so many days and that
crux is the theory of causation and the concept of it is Type A and not B. Whether it is treated or not
cure. To either cover it up, or to avoid confronta it will have spontaneous cure. How do we prove
tion, certain theories have been taken advantage of by that the native medicine has acted? That can be if
both Ayurveda and Homeopathy. It is the theory the duration of the problem is shortened to say 5
of vital forces being deranged thereby causing disease. days or so in almost 100% of the cases. When
Allopathy does not talk about this functional non remedies are claimed to be effective they do not
tangible side of causation of disease and this is the mention the time elapse before the medicine was
argument put forward to silence allopaths. Now started. Neither is the alteration in bilirubin esti
if I say that in an infection We identify the derange mated nor its return to normal. According to Allo
ment in vital force as the failure of tlie immune sys pathy anyway there is going to be spontaneous
tem, we may be accused of and perhaps ridiculed of cure. Further the treatment of jaundice as given is
having finally subscribed to the functional theory symptomatic and does not take into consideration
of Ayurveda. At the same time we will not be patted the cause. It can be of Type A, Type B, due to
on the back for giving a physical basis to the theory malignancy, obstruction of bile passage or drug
of vital force. Today Allopathy is poised for a induced. What is it that the native medicines are
break through by devising simple chemical means curing when they have not established what they are
by which the powers of immune system are sought treating. This is what we mean by defining cure.
to be awakened to simply gobble up even diseases A definition of cure in jaundice could be that the
like cancer. If it is so, actual success apart, the drug should substantially reduce jaundice or elimi
claims made by both the Ayurveds and the Allopaths nate it in a defined short period of time.
3
i
C2)
1^0
,*
■Alongwith ‘cure criteria", importance of the
parameters developed for testing in blood etc and the
way they change in disease states must be accepted
as a reproducible method for establishing cure.
Parameters alter in disease state and come back to
normal with cure. A hypertensive/diabetic conti
nues to feel okay with elevated levels does not mean
that these levels have been reduced to acceptable
levels. And again the acceptable levels are the ones
known to be desirable from the patient’s point of
view because it leaves a safety block or range before
it can turn abnormal and consequently dangerous.
In elevated levels this safety range is markedly reduced.
All in all there is need to put all sciences on firm
footings so that we know the weaknesses, the
strengths, limitations etc. through a specified re
search model. Let us supplement, supplant or
complement each other where necessary for the
alleviation of human suffering.
Criterion for cure is similarly confused in diabe
tes. Allopathy is considedred to control diabetes
and Ayurveda to cure it. The criterion for cure
could be that after a period of time, no medication
is necessary and after another specified time no die
Ji Hi;:..'.'1
tary restriction. Allopathy confesses that in rare
(Dear reader, this is only a part of the article
instances temporary diabetes may appear and get
written by the author. We are keen to know if such
cured for years with no drugs or restrictions. Medi
articles are useful. Only if we have a positive res
cine given for such a patient can claim cure but it is
ponse from you will we print the other part-Editor)
purely coincidental. If the cure is real all diabetics
must be given a cure. There are stress states like
pregnancy, in which diabetes disappears once the
stress is over. These variations of diabetes can be
distinguished normally also. A medicine claiming
cure in this second state also has to clarify the role
of this stress in the so called cure. I know hundreds
of cases when people claim that they are undergoing
Ayurvedic treatment and that their diabetes is cured.
On closer enquiry it is found that they continue
to take the tablets ar times 6-10 per day, continue to
observe dietary restrictions etc., etc. The claim is
cure. In what way is it different from Allopathy?
Allopathy too believes that when dietary control,
adequate exercises, rest, tranquility, reduction in
obesity, etc are achieved, and sugar does not come
within normal limits, the person would require drugs
or insulin but there is no cure.
is
■'
Similarly in the case of, say, systemic lupus erythe
matosus or rheumatoid arthritis the criterion for
cure could be that the drug alleviates pain, swelling
and dysfunction early and that it stops further erup
tion of the disease once the drug is stopped. Accord
ing to Allopathy, these diseases can only be controlled
Kxr
by nnntiniious
continuous medication which have considera e
side effects and in the case of SLE, the disease pro
gressively involves more and more systems despite
medication. Let SLE be simultaneously defined
as a wata or some tridosha disease and be treated by
Ayurveda but the criterion should be the halting
or reversal of disease preferably without medication
after a particular time period.
'I
■
j I
i
!
■J
So is the case with every disease state. Its natural
course has been outlined. While evaluating ayurve
dic therapies, the criteria and definition of cure will
have to be outlined and the drug trial undertaken.
Then only the Ayurvedic methods will gain precision.
It will be possible to evaluate the claims and assess
success & failure rates. In our terms, when these
methods do not exist in a science it is an empirical
science and the propositions become debatable. It
has to be reduced to the level of non empirical re
producible science.
I
bJ
"•
v-
.
-I
g
■■ ?
•:
I
■
N
‘/A
- '31
& r
^<x
h\ MR - /2
Nr ■
This refers to the article "Integration of
Medical Systems" (mfcb No. 128). Yes, publica
tion of such articles is useful but it is just one step
forward in a long march to evolve a system of
treatment capable of meeting human's need
and aspiration of freedom from illness and suffer
ings.
The starting point, therefore, of such an
endeavour becomes to look critically at treatments
recommended by different systems, not merely to
identify what is common between them to bring
two systems like ayurveda and allopathy on one
common ground which Kelkar describes as integra
tion of two systems, but to provide the ground from
which to proceed further to study what is consi
dered to be cure in different systems and situations
and how it is accomplished in different systems.
It would seem to be possible to abstract laws that
regulate cure in specific situations and cases.
Side by side these, laws have to be integrated with
the knowledge of life, mechanisms and processses
affecting human life, body's own curative power in
specific situations and in terms of specific disorders,
types and the course of diseases in different situa
tions, different ways of affecting cures and costs
involved in treatment not only in terms of drugs
and other necessities, but also in terms of human
day£ lost and dangers to other health. Such a
data base could give us a clue to work out a system
of cure which is most acceptable to the individual
sufferers as well as the societies in which the
sufferings take place. Knowledge embodied in
different systems of treatment then would be
integrated to become a whole. But then it will
not be an integration of ayurveda and allopathy,
or allopathy and
homeopathy (which is not
central to the need); it would be the integration
of human's knowldedge geared to meet human
need.
Besides, integration does not mean, as
Kelkar maintains, '/bringing two "dissimilar entities
together on common ground of utmost importance
... taking something from and giving something to
other, .. with an intention of developing later into
a homogenous new but not an uniform new".
Integration of two dissimilar entities might result
in their transformation into qualitatively different
entities as chemical combination so appropriately
demonstrates. Human's quest to understand nature
has given birth to different branches of science with
specific problems and specific laws. These laws
may look even contradictory as the indivisibility
of atoms in chemistry and physics. Yet, both these
branches of science are true and are integrated in
the great scheme of science. Similar can be the
situation in terms of disease, treatment and medi
cine in the integrated system of medicine. Hope, it
will find hospitality in your bulletin.
, B.K. Sinha, Bembta.
I
K* ....
-
E
J.’
J
p
■ T
J v
. jZ?
Eiedico friend
circle
bulletin
Mire (??
/
MAY 1987
H 3
■'
J
1
’T
iTO
J J
1Z
zz
yZ
d-Z
xZ
J4... ".
za
J
-z
•K
• <A
E
.4^
■ . :? *■
ir
1
■'C
Integration of Medical Systems
(A theoretical Perspective and Practical Blue Print)
S.K. Kelkar*
Broadly speaking, Eastern people are known for a
synthetic mind and for having a wholistic vision.
Occidentals are highly analytical but tend to be
fragmentary in their approach. With very well
developed
communication channels and the cultural
•
vunuial
fluxes to which the world today (India in particular),
is subjected to, it is inevitable that the two have to
meet at many points and possibly head for a common
culture.
identical. The other common ground is that of
patient welfare of which cure is one part albeit an
important
x
t one. Here there is certainly scope for
exchange. We would have to discover
c’/rr"
---------- for every
disease its most effective pathy. The identity loss is
only partial and it will be in the areas where knowledge
has been proved to be incorrect or obsolete or both,
in either pathies. To that extent no one needs to
grudge the identity loss. The words homogenous
and not-uniform are important. When the dis
tinctive features come to stay side by side they do not
assume the characteristics of other pathy and still
do not clash or turn antagonistic. It can be further
stated that W'e are for Unity and not for Uniformity.
Medical systems also cannot escape it. people
in India have voiced various opinions about the
existing medical systems in the world. These opinions
border from almost fanaticism to fragmented isolated
thoughts. But the broad principle which appears
to be surfacing frequently in all these currents is that
Desirability: I think the question of whether it is
there should be integration of medical systems es desirable to integrate is superfluous. The necessity
pecially the Indian Ayurvedic system with the Western
appears to be a foregone conclusion., Certain
Allopathy. While we think of integration several
aspects of this need elucidation. Allopathy as it
aspects must be understood first. What exactly do exists is a very effective proven science in disease
we mean by integration; the desirability or other alleviation in many areas and has shown enormous
wise of integration; and the attitudes -involved~as potential for growth due to its research orientation.
regaids this word and process on both allopathic and The statistics of disease mortality ratio reduction,
ayurvedic sides.
proven remedies on statistical basis etc., is not so well
developed in Ayurvedic sciences. Yet Allopathy
Integration can be considered <as bringing two is not a complete science. Its approach is on the
dissimilar entities together on certain common grounds
basis of structural changes preceded by functional
of utmost importance, taking something from and
changes on tissue level. Allopathy has developed
giving something to each other without losing special
identifying features of noble virtues, with the inten tremendously as regards elucidation of structural
changes even chemical changes which are also struc
tion of developing later into a homogenous new
tural. That knowledge needs to be utilized by others.
but not an uniform new. That Ayurveda and Allo
pathy are dissimilar there is no doubt. Yet there are
*With help from P.N. Kulkarni BAMS, Ashvini Hospital,
broad areas like anatomy, surgery, which are almost Nadikeri
HR ^vxllUV-n
f i
-I
comment upon this, This could be an important
Although there is an attempt to discover the forces
area of research.
V
of mind, intellect, subconscious, unconscious existenc
es soul etc., they are by no means well found out. Causal Cures? Symptomatic Cures? Suppressed
The Ayurvedic orientation is substantially in t icse
realms of existence. This can be used for developing illnesses?
We have discussed faith above. There is an al
more mature attitudes in people towards disease
most
universal belief in the Indian mind that Ayurentities and to life itself. Again these two have to
vedic cures are delayed but permanent. So w tn
meet somewhere. Whether spirtualism, however we
developed could keep a disease state away is still
•he
“ “hA 7 “
debatable. Ramakrishna Paramahamsa s an
tve- cures are symptomatic and not causal. They~sup
kananda’s diabetes can be give as examples, All press the illness but the disease remains dorman
in the body. I do not subscribe to both. In m
this needs to be studied.
places for both there are only controls to be achieve
by continuous medication in the form of medicines
There is an attempt, logical, for arrangement of
dietary, yogic massage,
or certain other practices,
j
data in older sciences, arrangement of citing past
of environment etc.
experiences; and to learn and to teach. It is needed change
that everybody knows about these ways. Definite
This belief has come about due to a lack of under
areas
have
been
demarcated
in
Allopathy
where
the
Allopathy has
areas 1
standing about allopathic thinking,
causology and treatment of diseases is highly un
is of illness on the structural
satisfactory. It is worth its while to discover their established the physical basis
2.2 structural change/deviaside by demonstrating the
solutions in other pathies for the benefit of humanThere is a spectrum of nortion from the normal. ---malcy of structures which is not uniform, though all
kind.
s
are normal. The immune system as we ^ndemtm^
Faith: People have an uncanny faith in the powers is largely the basis of our concept of w ly
of pathies other than Allopathy. Allopathy has occurs. There are demonstrated alterations 1
failed to generate it especially in the Indian mind. physical plane of body cells and immune cells, m
Lsnot been accepted by the laity and Ayurve achans
This faith takes to a level of their being a panacea to
The possible reason is that it does n
all forms of illhealth. It is worth its while to prove alike
Sth the Tridosha theory for which physical basi
that this faith is correct. If we do so we will have a
h>
gold mine uncovered. Strictly speaking, it is equally lacking as having not been demonstrated.
‘
to
the
fact
that
all
body
mechanisms,
essential to say that if we cannot prove it by methodo- in itseif is due
logical research, that the faith is wrongly formed and sav, swallowing have not been broken down^into, its
structural elements.
These structural element
that as a science it is either worthless or will have to
constitute
a
unit
functioning
of that process We
state its limits and potentialities once for all. This
individual structural units have not been ^cnbc
means that the whole of Ayurveda will have to be indivlduai structural umu> a.— ~
' ‘ T no other dissimilar
restated about where it fails, where its applications particular unique function which
This has been done in a deare limited, where its powers must be recognized and tissue can carry out.
of the structural
where it can supplant or supplement Allopathy. mOnstrable fashion on the basis
The subsequent
deviations from normal in Allopathy.
disease is the
functions resulting
derangement of
c.----_ _ in
Cost: Allopathy in its higher forms is costly, basis of :allopathic concept of disease.
a
hospital oriented and comparatively distant and The Tri dosha theory lacks it.
somewhat beyond the reach of the common people.
----Still in more manageable disease states the answers
This has resulted in the non-acceptance
Allopathy has, is more effective than the other pathies.
led to the
cause of disease and has consequently
cOne cannot dismiss it on this bias alone, as long as non-acceptance of the permanency of cure regarding
’ i related to
other less expensive alternatives are not found out. allopathic science. A further problem
Cost wise Homeopathy is definitely cheaper although this is that the Ayurvedacharis
__
afraid
are
i----that they
theh" basis of understanding the
it is time consuming in its process of diagnosis and
will have to replace
-----can be practised (truly that is) at a consultant level
causation of diseases if they accept this which woul
"ably lead to a total loss of identity of Ayurve ;
I am not sure that costwise and that includes loss 0
human-days from work, that Ayurveda is in any way Could Ayurveda still be practiced even f th s schoo
cheaper than Allopathic general out-patient practice. of thought of disease causation is accepted > It is
Unless more data is available it will not be fair o
3
3
••
I
8
r
fe
ll
I
2
S '73 ' •
I
'^15
1^,
i.e., of reawakening the vital force or the immune
system, are only truths stated differently and not two
different theories. I will clarify this point by anti
cipating the next question: Do we consider the
immune system to be the vital force? The answer is
probably that the immune system is one manifestation
of the vital force on physical level and there are
probably others about which not much is known.
Scientific function abounds with speculation of it
but it has not become science yet.
very complicated question and I do not have the
answer. One way out is to watch the more discrete
disease labels in Allopathy, say, pulmonary tubercu
losis or pneumonia by a similar disease label from
the Tridosha theory disease differentiation.
--"i
K
■2?
JL?
j
V
j v
1-3
g?
.'
■
■
J
I7'
J -
Historically in Allopathy the syndromic represen
tation of similar diseases was comparatively greater.
When structural studies progressed the syndromes
were broken down into disease entities. This was
also done by finding out the variations of one symp
tom common to all these diseases grouped into a
syndrome and by delineating the associated
symptoms which are found in some but never in
others. This was further substantiated by marking
the association of prior occurrences with the deve
lopment of more severe illness. For example, the
diagnosis of acute glomerulonephritis and rheumatic
fever are almost always associated with a minor
throat infections which pass off even without any
treatment. It forms the basis of diagnosis and has
considerable importance.
Defining cures and the criteria of cure:
Since there are difficulties in understanding the
theory of causation of diseases the question of defining
what is cure becomes almost impossible. The varia
tion of symptoms especially in time is the one that is
clearly understood by Allopathy. I do not think it is
indistinct in Ayurveda. Defining cure is essential in
clinical settings if the treatment has to be evaluated.
Probably the definition of cure for each evaluation
of disease is the greatest difficulty when it comes to
double blind clinical trials and that too involving
two systems and not two drugs from one.
As far as I can see the grouping of diseases in
large syndromes with comparatively less differentia
tion into individual labelled disease is very much
present in Ayurveda. For historical reasons the
minute differentiation of this into more discrete entity
has not reached the scale as in Allopathy. (It is also
true that even in Allopathy, some diseases remain at
the syndromic level in the present state of know
ledge.)
For instance, in the case of jaundice, people tend
to take ‘native’ medicines of which several are known.
Generally the time duration of jaundice is from 3
days to 3 months and according to Allopathy most
patients will recover between 20-28 days provided it
is Type A. It does not have any serious complications
and the body is left intact. By the initial blood
testing we can always get a fair estimate that this
Whatever it may be, the fact remains that the jaundice is likely to last for so many days and that
crux is the theory of causation and the concept of it is Type A and not B. Whether it is treated or not
cure. To either cover it up, or to avoid confronta it will have spontaneous cure. How do we prove
tion, certain theories have been taken advantage of by that the native medicine has acted? That can be if
both Ayurveda and Homeopathy. It is the theory the duration of the problem is shortened to say 5
of vital forces being deranged thereby causing disease. days or so in almost 100% of the cases. When
Allopathy does not talk about this functional non remedies are claimed to be effective they do not
tangible side of causation of disease and this is the mention the time elapse before the medicine was
argument put forward to silence allopaths. Now started. Neither is the alteration in bilirubin esti
if I say that in an infection We identify the derange mated nor its return to normal. According to Allo
ment in vital force as the failure of the immune sys pathy anyway there is going to be spontaneous
tem, we may be accused of and perhaps ridiculed of cure. Further the treatment of jaundice as given is
having finally subscribed to the functional theory symptomatic and does not take into consideration
of Ayurveda. At the same time we will not be patted the cause. It can be of Type A, Type B, due to
on the back for giving a physical basis to the theory malignancy, obstruction of bile passage or drug
of vital force. Today Allopathy is poised for a induced. What is it that the native medicines are
break through by devising simple chemical means curing when they have not established what they are
by which the powers of immune system are sought treating. This is what we mean by defining cure.
to be awakened to simply gobble up even diseases A definition of cure in jaundice could be that the
like cancer. If it is so, actual success apart, the drug should substantially reduce jaundice or elimi
claims made by both the Ayurveds and the Allopaths nate it in a defined short period of time.
3
..
i
^^7-
AJc
Similarly in the case of, say, systemic lupus erythe
matosus or rheumatoid arthritis the criterion for
cure could be that the drug alleviates pain, swelling
and dysfunction early and that it stops further erup
tion of the disease once the drug is stopped. Accord
ing to Allopathy, these diseases can only be controlled
by continuous medication which have considerable
side effects and in the case of SLE, the disease pro
gressively involves more and more systems despite
medication. Let SLE be simultaneously defined
as a wata or some tridosha disease and be treated by
Ayurveda but the criterion should be the halting
or reversal of disease preferably without medication
after a particular time period.
B
Mkc (2)
•Alongwith ‘cure criteria’, importance of the
parameters developed for testing in blood etc and the
way they change in disease states must be accepted
as a reproducible method for establishing cure.
Parameters alter in disease state and come back to
normal with cure. A hypertensive/diabetic conti
nues to feel okay with elevated levels does not mean
that these levels have been reduced to acceptable
levels. And again the acceptable levels are the ones
known to be desirable from the patient’s point of
view because it leaves a safety block or range before
it can turn abnormal and consequently dangerous.
In elevated levels this safety range is markedly reduced.
I
!
i
.
c
c
e-r
All in all there is need to put all sciences on firm
footings so that we know the weaknesses, the
strengths, limitations etc. through a specified re
search model. Let us supplement, supplant or
complement each other where necessary for the
alleviation of human suffering.
Criterion for cure is similarly confused in diabe
tes. Allopathy is considedred to control diabetes
and Ayurveda to cure it. The criterion for cure
could be that after a period of time, no medication
is necessary and after another specified time no die
.I'1
tary restriction. Allopathy confesses that in rare
(Dear reader, this is only a part of the article
instances temporary diabetes may appear and get
written by the author. We are keen to know if such
cured for years with no drugs or restrictions. Medi
articles are useful. Only if we have a positive res
cine given for such a patient can claim cure but it is
ponse from you will we print the other part-Editor)
purely coincidental. If the cure is real all diabetics
must be given a cure. There are stress states like
pregnancy, in which diabetes disappears once the .
stress is over. These variations of diabetes can be
distinguished normally also. A medicine claiming
cure in this second state also has to clarify the role
of this stress in the so called cure. I know hundreds
of cases when people claim that they are undergoing
Ayurvedic treatment and that their diabetes is cured.
On closer enquiry it is found that they continue
to take the tablets ar times 6-10 per day, continue to |
observe dietary restrictions etc., etc. The claim is :
cure. In what way is it different from Allopathy?
Allopathy too believes that when dietary control,
adequate exercises, rest, tranquility, reduction in
obesity, etc are achieved, and sugar does not come
within normal limits, the person would require drugs
or insulin but there is no cure.
>3
Il
So is the case with every disease state. Its natural
course has been outlined. While evaluating ayurve- |
die therapies, the criteria and definition of cure will
have to be outlined and the drug trial undertaken.
Then only the Ayurvedic methods will gain precision.
It will be possible to evaluate the claims and assess
success & failure rates. In our terms, when these
methods do not exist in a science it is an empirical
science and the propositions become debatable. It
has to be reduced to the level of non empirical re
producible science.
I
CO
'■
t
cj
1
c
01
£ r ■£u£yA'(
M
-131
•C
f
L
by MFc- /? Nv- 12^^.
This refers to the article "Integration of
Medical Systems" (mfcb No. 128). Yes, publica
tion of such articles is useful but it is just one step
forward in a long march to evolve a system of
treatment capable of meeting human's need
and aspiration of freedom from illness and suffer
ings.
The starting point, therefore, of such an
endeavour becomes to look critically at treatments
recommended by different systems, not merely to
identify what is common between them to bring
two systems like ayurveda and allopathy on one
common ground which Kelkar describes as integra
tion of two systems, but to provide the ground from
which to proceed further to study what is consi
dered to be cure in different systems and situations
and how it is accomolished in different systems.
• It would seem to be possible to abstract laws that
regulate cure in specific situations and cases.
Side by side these, laws have to be integrated with
the knowledge of life, mechanisms and processses
affecting human life, body's own curative power in
specific situations and in terms of specific disorders,
types and the course of diseases in different situa
tions, different ways of affecting cures and costs
involved in treatment not only in terms of drugs
r «■■■■■■■
.
and other necessities, but also in terms of human
day£ lost and dangers to other health. Such a
data base could give us a clue to work out a system
of cure which is most acceptable to the individual
sufferers as well as the societies in which the
sufferings take place. Knowledge embodied in
different systems of treatment then would be
integrated to become a whole. But then it will
not be an integration of ayurveda and allopathy,
or allopathy and
homeopathy (which is not
central to the need); it would be the integration
of human's knowldedge geared to meet human
need.
Besides, integration does not mean, as
Kelkar maintains, '/bringing two "dissimilar entities
together on common ground of utmost importance
... taking something from and giving something to
other, .. with an intention of developing later into
a homogenous new but not an uniform new".
Integration of two dissimilar entities might result
in their transformation into qualitatively different
entities as chemical combination so appropriately
demonstrates. Human's quest to understand nature
has given birth to different branches of science with
specific problems and specific laws. These laws
may look even contradictory as the indivisibility
of atoms in chemistry and physics. Yet, both these
branches of science are true and are integrated in
the great scheme of science. Similar can be the
situation in terms of disease, treatment and medi
cine in the integrated system of medicine. Hope, it
will find hospitality in your bulletin.
, B.K. Sinha, Bembia.
I
medico friend
circle
bulletin
132
SEPTEMBER 1987
The Epidemiological Approach : Its Elements and its Scope
Ritu Priya
Epidemiology is defined as the study of the dis
tribution and determinants of disease frequency in
man(l). This invovles study of its distribution in
time and place, in terms of its quantity, in terms of
the persons affected, their age and sex distribution
etc. The determinants of disease are the causal
factors—factors involving the agent, the host and the
environment and their inter-linkages in the ‘web of
causation’.
The Approach
Epidemiology is basically an approach to studying
any health problem of a population, commonly applied
to studying the causality of disease. The approach
primarily involves studying the problem as it exists
in the population, in all its various aspects, and then
using this information as the basis for understanding
the causation of the problem; very often with the
additional perspective of trying to identify means to
prevent or control or otherwise effectively deal with
the problem.
Piinciples underlying the approach are
(1) It is a comprehensive, holistic approach;
taking into account the various dimensions of the
problem—physiological, pathological, demographic,
environmental. Based on the undeistanding that
human disease is related to man’s environment, it
involves study of the population’s physical, chemical,
biological, social, economic and cultural environment.
It thus deals with both medical and social sciences
and uses the tools of both. Its field of enquiry will
extend “from the molecule to the social group, from
the prevalence of sickle cell trait to the conditions of
industrial morale,”(2).
(2) It deals with large populations and not with
individuals. Thus, for example, the difference in deal
ing with the natural history of a disease. In an in
dividual, natural history of a disease connotes the
process of pathogenesis of the disease—from prepathogenic phase, to incubation period, to early
discernible lesions, to advanced disease. Epidemio
logy studies this in order to explain the behaviour of
the disease in society, its distribution over time, its
seasonal variations, its geographical distribution,
the characteristics of persons affected, the conditions
for variations in natural history in individuals etc.
It is interested in “community diagnosis' just as
clinical medicine is interested in diagnosing the health
problems of the individual. It is a‘ reconstructive
science in contrast to the laboratory approach of
studying minute components of the whole.
(3) It depends upon the quantifications of pheno
mena using statistical concepts and tools. This
helps in a systematic and ‘objective’ collection and
representation of data, in drawing inferences and
establishing associations, in generalizing from partial
data, and in knowing the possible degree of error in
one’s deductions.
The health status of a population is measured
in terms of morbidity and mortality rates. Causal
relationship between events is established by proving
a statistically significant, statistically determined
association between them and then substantiating
this association with other evidence like time sequence,
strength of association, existing knowledge about
the mechanisms involved, or by direct experiments.
(4) It tests its hypotheses by experiments, even
on human populations, in addition to using the
various tools used by other disciplines. The ‘epide
miological experiments’ involve comparisons between
a study and a control group or between two groups
subject to conditions differing only in the one factor
under study. These groups may be created by natural
conditions or by direct, planned intervention.
reaching standards and in improving health ought to
be appraised. All this has to be related to other
social policies and to resources.
(4) Furthering the knowledge of individual di
seases and of medicine as a whole by completing
the clinical picture of diseases and describing their
natural history on the basis of study of a large number
of cases of all kinds, and by following the course
of remission and relapse, adjustment and disability
(by detecting early sub-clinical disease and relating
this to the clinical and by discovering precursor ab
normalities during the pathogenesis) ; identifying
syndromes by describing the distribution, association
and dissociation of clinical phenomena in the popu
lation; estimating individual risks and chances, on
average, of disease, accident and defect; testing hy
potheses and techniques emerging from laboratories
and clinics about causality, about risk factors, about
effectiveness and side effects of new drugs etc.
(5) It deals with dynamic processes and therefore
has to keep a constant track of changes in disease
patterns, in health status, and in the various factors
influencing them. To be able to do this it has also to
keep testing and altering its specific tools, evolving
new tools, and seeking out new indices of health and
disease.
Epidemiology can help in :
(1) Understanding disease processes in popula
tions—the history of the rise and fall of diseases in
specific societies and changes in their character.
This will help in understanding present health prob
lems and in making useful projections into the future.
For example, McDermott (3) uses the morbidity rates
of various infectious diseases in the USA at the begin
ning of this century to show that these diseases had
begun to decline even before specific therapeutic
and preventive measures for them had been discovered.
He explains this trend by the general improvement
in socio-economic conditions and thereby rise in the
standard of living. This understanding should help
in building our overall perspective towards preven
tive measures, emphasising the importance of socio
economic measures over medical technology based
solutions.
Some Potentials and Limitations in the Scope of the
Epidemiological Approach
(1) All ‘Disease' and no ‘Health' : Having
started as the study of epidemics per se, epidemiology
has extended to the study of disease in non-epidemic
times and to chronic diseases; and from the study
of infectious disease to those non-infectious in na
ture. Having thus been concerned primarily with
disease, a fuither advance in its scope is study of the
positive components of health and its determinants.
This also involves redefining ‘health’. There are
some who think otherwise. While ready to concede
the application of epidemiology to ‘ other biological
processes, including growth, multiple pregnancy,
sex determination, intelligence, and fertility”, they
do not think it important enough to study ‘health.’
(2) Identifying causes of a disease and establsihing their relative importance (multiple-cause theory)
by studying the incidence in different groups, defined
in terms of their composition, their inheritance and
experience, their behaviour and environment. This
knowledge will help in evolving means of treatment
and of undertaking the various levels of prevention.
It is sometimes suggested that epidemiology should
also be concerned with the positive components of
health implicit in the definition used by the World
Health Organisation. According to this definition,
“Health is a state of complete physical, mental and
social well-being and not merely the absence of
disease or infirmity”.
However, the number of
widespread and sei io us diseases of which the etiology
is unknown is more than sufficient to occupy epide
miologists for many years to come. Concentration
of effort on these diseases appears to be indicated by
the urgent need for knowledge leading to their
prevention, as well as by the practical difficulties in
quantitative investigation of concepts that have
not been defined in clinical, pathologic, or other
operational terms.
(3) Planning, organising and monitoring health
services by diagnosing the health of the communtiy
in terms of incidence, prevalence and mortality; to
define health problems for community action, and
their relative importance and priority; to identify
vulnerable groups needing special protection.
Studying the working of health services with a
view to their improvement.
Operational research
translates knowledge of community health in terms
of needs and demand. The supply of services is des
cribed and how they are utilised, their success in
I
2
AI Pc Even a ‘progressive’ book like Morris ‘Uses of
Epidemiology' (2) does not think of positive health
as worth mentioning. Besides the above view, epi
demiology appears to have an inherent limitation in
studying ‘health’, because of its basic reliance on sta
tistical measurements. Disease and death are easier
phenomena to quantify than health. Health remains
more qualitative than quantitative. May be it is
possible to evolve indices of ‘positive health' and
attempts should be made in that direction.
bility of self-help, since the sick person could treat
himself or herself by following a certain diet. Nine
teenth century medicine, by contrast, with its empha
sis on the normal functioning of an organic structure,
required a knowledge of physiology for its practice.
It was on this view, the life sciences in the nineteenth
century were built, not on the comprehensive and
transferable nature of biological concepts, but on
the opposition of health and illness.
Social and preventive medicine extended the
clinical model in the direction of health, expanding
its application from the individual to his 01 her family
and immediate environment. Environmental sani
tation refllects a further extension to the wider phy
sical milieu : environmental sanitation is the study
of disease based on bourgeois epidemiology, i.e.,
the classical triad—host, disease agent, and environ
ment. It is in no sense a study of collectivities.
Insofar as these disciplines remained dominated by
the clinical model, none seems to grasp the notion
of collectivity, without which there can be no ade
quate difinition of health.
Turshen(3) shows how the clinical picture of
health dominates disease and the individual is placed
at the centre, and health suffers. He argues that this
has come about as a result of development of the
capitalistic mode of production in the industrialized
countries.
He explores the limits of the clinical paradigm
that has defined disease and health for centuries.
This paradigm takes individual physiology as the
norm for pathology (as contrasted with broader
social conditions) and locates sickness in the in
dividual’s body. A typical nineteenth century va
riant held that every illness was the disturbance,
exaggeration, dimunition or cessation of a corres
ponding normal function. In this veiw treatment
readjusted the body until its physiological norm was
restored, a mechanistic approach that reduced the
body to a machine whose organs could be discretely
examined and regulated. Implicit in this notion was
the concept of health as the absence of disease.No
positive concept of health was advanced.
A medical paradigm that is not holistic and col
lective produces only an inexact and inadequate body
of medical knowledge.
This suggests an additional proposition—that
medicine’s failure to develop a positive definition of
health results from the individualistic and ideological
bias that pervades medical research and medical
practice, structural relations between practitioners
and patients, shapes the approaches selected for
treatment (eg. chemical or surgical intervention) and
the technology employed, and rejects the initiation
of collective social action by communities.
The clinical perception of disease could not have
emerged in the nineteenth century if the science of
quantification had not been developed earlier, since
it depended on operational verification by measure
ment, clinical study and experiment, and evaluation
according to engineering norms.
The medical
quantifiers of the nineteenth century placed sickness
in the center of a medical system that was a mecha
nised framework for the investigation of the mecha
nical troubles of the human body.
The closest 1 have ever come to finding a positive
definition of health is the following formulation :
Marx regarded as the aim of the socialist movement
“a society, in which menliberated from the ‘alienations’
and ‘mediations’ of capitalist society, would be the
masters of their own destiny, through their under
standing and control of both Nature and their own
Social relationships.”
Foucault, in his study of the origins of modern
medicine, makes the interesting observation that,
until the end of the eighteenth century medicine was
more concerned with health, with qualities of vigor,
suppleness and fluidity that were lost in illness and
had to be restored, than with normality, an analysis
of regularity, the search for functional deviation, and
the return to an equilibrium,. Foucault suggests
that from this early concern for health there followed
not only an interest in nutrition but also the possi-
Thus while one may or may not agree with all
his propositions, one cannot deny the need for a change
in the basic perspective of medical science today,
specially in the light of even the ‘establishments’
professions of emphasis on community participation
and the attempts by ‘non-establishmenf to initiate
community action in health.
3
I
I
(2) ‘Holistic', but no ^Political Environment' :
Epidemiology has from the beginning had the
basic understanding that human disease is related
to the human environment. The environment has
from the earliest (even Hippocrates) been taken to
include the physical and geographical, the biological
and the socio-cultural (food habits, addictions, phy
sical exercise and labor). It still remains primarily
restricted to these (and in fact even the socio-cultural
aspect is taken in a very limited sense). But with
its holistic approach it can, and must, cover more
and more the varied and complex social economic
and political dimensions of the human environment.
projections of the club of Rome) fail to consider the
complexity of relations between people and their en
vironment. He traces this failure to the use of narrow
biological methods in the analysis of problems that
are broadly social. “For in the case of man, the
mediation between the whole and the part, between
subsystem and global system, cannot be explained
by the tools of biology. This mediation is social,
and its explication requires an elaborated social
theory and at the very least some basic assumptions
about the historical process.”
Little attention has been paid to this social aspect
of hygiene, especially since the scientific advances of
the nineteenth century gave the practice of medicine
a solid though theoretically narrow foundation.
Attempts are being made in recent times to add
to the dimensions under purview of epidemiology
by naming new aspects like ‘medical ecology’ (the
study of human disease in relation to physical, bio
logical and social environment) and studying the
‘political economy of health’ and the ‘political ecology
of disease.’
Turshen asserts that the one branch of biology
that has taken it up is medical ecology. He goes
on to describe the conception of environmental
factors according to medical ecology, but I would
contend that they be considered a part of epidemio
logy and his description can be freely applied to
epidemiology as a whole.
One can start with the understanai ng, as Tui shen(3)
does, that, “the theoretical assumptions on which
medicince is based are subjective....... ” Both scienti
Medical ecology thus asserts a relation between
fic and medical knowledge depend on material
production and reflect the social organisation of that environment disease, and man, but selects only bio
It
production, not on historical objectivity”. It fol logical and socio-cultural factors as relevant.
looks
at
the
convex
gence
of
environmental
and
com
lows then “that contemporaiy medical definitions of
munity
factors
only
within
the
person
of
the
patient.
health and disease are inadequate because they are
abstraction derived, for specific historical reasons, At no point is it concerned with the collectivity as
from the clinical study of the individual”. The such. By dismissing political and economic factors
study of these social, economic and political reasons as irrelevent, it suffers from a failure to consider the
thus becomes necessary for understanding the existing relation of people to their environment in all its com
medical perspective and for evolving the ‘new’ per plexity. As with ecology and biology, the methodo
logy of medical ecology is too limited to solve the
spective.
problems of public health. It is constrained by the
The definitions are inadequate expressions of the individualistic and ideological bias of the clinical
relation of medical states (illness) to reality since paradigm which medical ecology reflects.
individuals are not clinical entities. In reality the hu
These points can be illustrated with a brief example
man essence is the product of an example of social
from
Vietnam. In discussing the influence of culture
relations. The clinical model does not encompass
on
human
disease occurrence in northern Vietnam,
the social relations of the individuals it studies, even
J.M.
May,
a prominent medical ecologist, wrote
at its most progressive limits (3).
in 1953 : ‘‘From the water the people get their food,
The idea that the human environment is a complex also their cholera, their dysenteries, their tyhpoid
interacting web has been accepted in the biological fevers, their malaria; from the earth they get their
and social sciences since the time of Darwin. Use hookworm; from the crowded villages they get their
of the concept entails analysing natural pheomena plague and typhus; and from the food their protein
in the context of their total environment. This deficiencies, their beriberi.”
theory of holism rarely directs studies of human eco
logy, because many hidden assumptions preclude
May, who worked as a surgeon in the French
the consideration of cardinal social and political colonial service, recognized the direct influence of
factors. Enzensberger, in his critique of ecology, scarcity and starvation on the pathology he described
points out how recent studies (eg., the hasty global but dismissed any examination of their causes: “We
4
I
will not discuss here the fantastic edifice of mortgages
and debts which rises above the fraction of an acre
of land on which family life is built. Nor shall we
describe the land tenure laws and customs that have
resulted in the reduction of the size of property through
the years to insignificant proportions.” To discuss
and describe in these circumstances was dangerous,
for no intelligent observer could escape the conclu
sion that the origins of indebtedness and land tenure
laws were the key to the ecology of disease in Vietnam.
The etiology was no ‘cultural maladjustment’; it was
the dislocation of the Vietnamese political economy
by French colonialism, which imposed a system of land
classification and taxation that impoverished the
peasantry. Medical ecology could not take political
and economic factors into consideration without
challenging the legitimacy of colonial rule.
As the above example clearly shows study of so
cio-economic and political factors is important for
understanding the existing conditions of health of
people and the condition of medical science and
health services. And this understanding is an impera
tive for future developments in these fields.
Conclusion
If we accept the two propositions stated above,
that of incorporating ‘health’ within the purview uf
epidemiology and that of incorporating socio-eco
nomic and political conditions as part of ‘human
environment’, we can easily substitute the word
‘problems’ for ‘diseases’ in the five uses of epidemio
logy stated above. The epidemiological approach
can then be applied to all dimensions of the health
field. In fact the basic elements of the approach can
be applied to study the various aspects of society at
various levels. It all depends on what parameters
one defines for ‘health’. Inherent limitations to this
application of the epidemiological approach will
definitely emerge and it cannot be the only means of
understanding the complexities of society but it can
definitely be one of the many tools in an attempt to
do so.
References
Other fields studying society too seem to share
the ‘clinical’ concept and its impact is seen in other
modern social institutions and organisations as well.
As Morris (2) says “One of the urgent needs of society
is to identify ways of healthy living, the wisdom of
body and mind and the principles of social organisa
tion that will reduce the burden of disease and improve
the quality of life. The quest for this knowledge is
the main use of epidemiology”.
5
1.
MacMahon, D. and Pugh, T.F. (1970) : Epi
demiology : Principles and Methods, Boston,
Little Brown.
2.
Morris, J.N. (1964) : Uses of Epidemiology,
Williams.
3.
Turshen, M. (1981) : The Political Ecology of
Diseases, Health Bulletin, No. 1, pp. 1—38.
4.
McDermott, Walsh : Demography, Culture and
Economics and the Evolutionary stages of Medi
cine in Human Ecology and Public Health.
Kilbourne E.D. and S.
Dear Friend,
in one's clinical practice, a theme I touched upon ear
lier in this column (mfcb 130).
Prashant’s question put to Amar Jesani (mfc 130)
provides an appiopdate clinical situation wherein
the difference between a purely clinical approach and
a community health approach can be demonstrated.
I therefore, take the liberty of responding to it.
Dhruv Mankad, Nipani.
Apropos Gloria Burret’s article “Paralytic Polio
myelitis” (mfcb 130) I would like to have the following
information :
Prashant s question contains within itself an ans
wer from a purely clinical view point. A patient (the
woman facing oppression) presents hereself with a
malady (pregnancy, may be having a female fetus)
to the clinic. What should a Doctor do ? Prashant’s
clinician genuinely moved by her misery, advises Sex
Determination test and if she finds a female fetus,
does an abortion, feeling satisfied at having successfully
relieved the patient of her malady through medical
intervention. Instead, a socially sensitive clinician
adopting a community Health approach would ask
“Has the woman really been relieved of her misery
by this medical intervention ? How long would I
go on advising SD/aboition, every time she come
with a pregnancy ? What is the guarantee that she
wid not be harassed for having borne a female fetus
in the first place, abortion or no abortion? Proceed
ing on these lines s/he will come to realise that the
harassment of the woman due to bearing of daughters
only, is a Social problem and not a Medical one at
all, wherein medical intervention can only be partially
effective or as in this case, may even be a dangerous
short cut. It would perpetuate her misery without
giving her any advice on the ways and means vf ob
taining freedom from her oppression. This is because
a purely clinical approach sees getting nd of her female
fetus as hei ‘need’ while a community health approach
perceives it as the need to be relieved of harassment.
Therefore, neither advocating SD/abortion (in case
of a female fetus) or giving her a long lecture on medi
cal ethics can be the appropriate way of intervening
here. Her need can only be met by referring her to
a iwomen’s group able and willing to share her misery
.2 to
i-----Lc a collective
collective effort to help her struggle
and
make
against oppression.
1. The exact data to suggest that paralytic polio
has rising incidence (fresh new cases/1000 popula
tion) in India. The data should include incidence
10, 20, 30 years ago and the present incidence to
show that there is rise over a period of time per
thousand susceptible population. Data naturally
have to be community based rather than hospital
based.
2. There has been a plea raised from various
quarters that the number of polio vaccine doses should
be increased from three to five or mo.e because the
efficacy of the vaccine is low in our country. I
would like to know whether the accepted formula
attack rate in the unimmunized—
attack rate in the immunized x 100
vaccine efficacy
attack rate in the unimmunized
has been applied by those who are advocating the raise
on an all India basis.
3. The author has quoted Jacob John's article
say that partial coverage through vaccine causes
jncreas,n£ incidence,. This is, according to John,
because of retardation in the virus circulating and
that retardation is due to (a) improvement in hygiene
(b) because immune individuals are poor transmitters
of the virus. Improvement of hygiene has not ap
parently occurred in this country. No data suggests
this conclusion. As regards immunity gained through
vacc, nalion> less than 6.1% of the population had been
immunized in
~ the
’ year John’s article was published.
It may be presumed that this 6.1% population belonged
mostly to the largei urban areas. Would such a small
number residing in specifically located areas be res
ponsible for retardation of virus circulation in a
country as vast and as far flung as India? If it in
deed did retard circulation of the virus, would such
an eventuality reduce the incidence or increase it?
During epidemics, administration of vaccine is ad
vocated to reduce the incidence of polio why ?
Medical intervention while being useful as a pal
liative measure in other such ‘medico-social’ problems,
can turn out to be counter productive in this parti
cular situation as it may even perpetuate her harass
ment of undergoing multiple abortions till a male
fetus is born.
This instance illustrates the need and the possi
bility of adopting a Community Health approach
Warerkar, Solapur
6
f-|pC C -
H jf p
Injury Prevention and Basic Preventive Strategies
Dinesh Mohan
The injury problem in developing countries looks
so complex that many tend to throw up their hands
in helplessness. It is often recognised that problems
exist and they need attention. But the most that is
done is to put up posters and billboards exhorting
their readers to behave more responsibly. The pro
blem remains unsloved. This is partly because there
are many myths prevalent regarding the control of
injuries. Most people think that injuries are mainly
the problem of rich countries. This is not so. The
data available from developing countries suggest
that in every sphere of activity the proportion of
persons killed or injured is similar to or higher than
that in industrialized countries. Another myth is that
education, propaganda, and law enforcement can
be the most effective tools in injury control. This
also does not seem to be borne out by many studies
around the world. The whole problem can be best
understood if we are reasonably clear about the
concepts which follow.
“Accidents" and injuries are not "Acts of God"
It is vital first step to realize that the occurrence
and outcome of events which may cause injury
are predictable and subject in many cases to human
control. Often an injury can be prevented even where
an accident cannot. In a motorcycle crash, the occu
rrence and severity of head injury depend on whetther a helmet was used and on the quality of helmet
used. Fires and explosions in the kitchen are redu
ced drastically when safer cooking methods are
used. Children do not fall out of windows which
have proper screens.
Similarly, even the so called natural disasters are
not really 'natural' If they were, then the effects of
floods would be the same in the rich and poor
countries. It is rare to see thousands made home
less in the US, but it is a yearly ritual in India. Even
in India, it is the poor who seem to be more adver
sely affected by floods, and storms than the rich.
Therefore, how a physical event influences human
beings is largely influenced by the human
beings themselves. Even the occurrence of the
physical event itself is very often a result of man's
activity. For example, floods may be caused by
deforestation, faulty designs of dams, blocking up
of drainage in cities, etc. Therefore man has a
great deal to do with whether or not accidents and
disasters take place and how these events affect
us. We can design our environment and products
such that the incidence and
and disasters are minimised.
effects of accidents
There is no difference between injury and disease
Injury is a disease that results from acute exposure
of the body to physical and chemical agents. There
are no basic scientific distinctions between injury
and disease. When one drowns, one may die because
of fluid in the lungs which prevent exchange of
oxygen between air and blood. The cause of death
in pneumonia is the same. Any infectious disease
may cause fever, pain, disability, or death. Injuries
do the same. Therefore, the concept of injury is
coextensive with the concept of disease as illustra
ted by the following table.
Comparative epidemiology of Malaria and Skull
Fracture
Pathological Host
condition
Agent
Vector/
Vehicle
Interac
tion
Mosquito
Bite
Malaria
Man
Plasmo
dium
Skull
fracture
Man
Mechani- Motorcal
cycle
energy
Crash
Further if injuries are viewed as diseases, the com
munity may stop viewing them as events resulting
primarily by carelessness. Long ago we learned
that it does little good to blame the victim of a
disease for being sick. For example, when a patient
goes to a doctor with malaria, the doctor does not
blame the victim for not killing the mosquito
before it bit him. The most effective disease
control measures often consists of modifying the
environment, not the behaviour of the individuals,
to make contracting the disease less likely.
Up to now, our efforts at injury control have often
been retarded by a preoccupation with fixation of
blame. This has led to repeated attempts to prevent
injuries by changing the behaviour of their potential
victims. Such attempts are usually costly, not often
successful, and have added to the public's sense
that injuries are an unavoidable evil. In general,
the same principles used in disease control may
successfully be applied to injuries.
AH Injuries cannot be prevented
Most efforts to reduce injuries are termed "accident
prevention" campaigns. We should be clear that
7
_________ ______________ _____ __________ R.N. 27565/76
accident prevention is just one aspect—and not
often the most rewarding one—of a much longer
range of countermeasures used in effective injury
control programme. This is because, making mis
takes is very 'normal' and not 'abnormal'.
It
is normal for professional drivers to be distracted
during some periods of their long driving hours; it
is normal for cooks to be day dreaming at some point
in the kitchen; it is normal for a factory worker to
make a mistake when he thinks of the hundred
problems at home; and it is normal for children to
do the unexpected and hurt themselves.
In short, we will never eliminate carelessness,
absentmindedness and even neglect in day to day
activity. However, by designing our products and
environment to be more tolerant of these normal
variations in human performance, we can minimise
the number of resulting accidents and injuries.
Accidents result from a temporary imbalance bet
ween an individual's performance and the demands
of the system in which he is functioning. They can
be prevented by an alteration in either but most
effectively by focusing on the system and not on the
user, the user.
In many areas of public health we understand this
very well. We know that drinking water should be
purified at its source; it is unreasonable to expect
everyone to boil water before drinking it. Ironically,
it is quite common to create a product or environ
ment which is likely to cause injury, warn the user
to be careful, and blame the user if a mishap occurs.
We would never tolerate a person who introduced
cholera germs into a city water supply and then
asked every citizen to boil water before drinking
it. But this we do all the time to as far as injuries
are concerned.
Injury Control measures can be developed system
atically
Even if one considers injuries to be a health pro
blem, very often it remains difficult to think of all
the possible counter measures because the problem
appears to be too large and un-wieldy. It is always
easier to work in a step-by-step manner. One useful
approach is to consider each injury problem as
resulting from an interection between several disc
rete factors occurring over distinct phases in time.
This can be done if we divide all time into three
categories: before the injury producing event,
during the event, and after the event. The physical
universe can be divided into these factors: man,
the device under consideration, and the environ
ment which consists of everything else. These can
be used to create a 3 x 3 matrix as shown in the
table.
Injury Matrix
Factors
Phases
Pre-event
Event
Post-event
Human
Vehicles &
equipment
Physical, &
socio-econo
mic environ.
1
2
5
8
3
6
9
4
7
(From: "To prevent Harm", Insurance Institute of
Highway Safety, Washington D C )
In developing a program for injury control measures
for a particular injury problem we can go systema
tically through each cell of the matrix and think of
all possible counter measures applicable to that
cell. (In classifying an intervention according to
time, it is the point at which an intervention exerts
its effect, not the time at which it is undertaken,
which is considered). The usefulness of the matrix
is as a tool for generating ideas. At this stage, every
possible strategy should be documented and noth
ing held back because of political or financial consi
derations. After all the possible countermeasures
have been listed, injury control experts and policy
makers can select those which are most feasible,
effective and acceptable politically.
I
.
flvj
>1
IIE
•LJ
■£XB*vvv-\ a/Ia t
^-0^,
3.^27565/76 S 0 B
/ ■'
From the Editor's Desk
I5
II
I
Although the nursing education is somewhat diffe-*
Last year in September, the media splashed, some
what sensationally, the news that 18 unmarried nurses/ rSnt today, the necessity for being 'good' women
-------- i’ is^
recruits to the government DK Hospital in Jaipur, MP,
stilb enrjphasised. The introductory pages of the Text
were forced to undergo pervaginal (P/V) examination
Book for Auxiliary Nurse-Midwives states.
''In order^ I
to maintain respect for the nursing profession, and in^ I
to determine their virginity. The pressure was that the
order that there should be no hindrance in her practi-</j
nurses salaries would be withheld if they refused the
P/V examination. It was only when the nurses struck
cal work, the nurse should always be, clean and neat^ I
work and the Junior doctors and Class 3 employees anctethe uniform complete and correct in every detail.^. ■
No jewellery is to be worn and no perfume used. She^ j
threatened to join the stir, that a magisterial inquiry
was ordered and the Medical Superintendent sent on
should wear a suitable hair style with the hair kept clear1
of,^’’ neck and forehead.. The material and; style of^.’ |
long leave. A small opinion poll conducted by Chattisgarh Mahila Jagruti Sangatan following this incident
her uniform should be plain. If a sari is worn, it must ' ]
not be loose at,the shoulderand there must be no gap*;z 5
showed that approximately 56% men and 65% wo
worn and*M
men surveyed felt that nursing as a profession was
is at the waist. Shoes or sandals must be
looked down upon and the nurses were considered;
< ... .
_ they should not be fancy
, in style
,
or colour.4 And a ^••••3
objects of pity or sexual objects by society.
Th^ little less blatantly, "there will be great demands on her
CAHP-TNAI
(1975)
CAMP-TNAI Nursing Survey in India
1^;. MQ
-7Kv has also strength and endurance, and she must always be in
shown that the necessity of attending to males and deal
control of her emotions if she is to inspire confidence ^3
ing with male colleaguesand having to do night duty and give needed support to patients and their relatives"J
(Chaikey, 1974).
!
' I
accounted for the largest proportion of negative feelr
ypr
.
j
ings about nurses.
..4
The victimised nurses' viewpoint about the Raipur
|
Nursing as an acceptable profession for women
indident was also on similar lines. "Our virginity has
emerged in the late 19th century out of a desire to
come under question; Madam please do not perform
j
the P/V on my daughter., it is a question of, her life £ J
open up non-industria! occupations for women from
the upper classes. Earlier to that, the few women emp
(a nurse's mother); this has not only led to the degradaJ
loyed in the hospitals to look after the dying were
tion of a few victims but has denigrated all woman’
generally drunken and indulged in prostituton and thie
hood; if such practices continue people would not q "
very. Since the upper class women were moving out want to send their daughters to work; the entire nursIT;’?
of the protection and the sanctity of their homes for ing community that draws its inspiration from Florence / "
the first time, it was essential to elevate nursing from
Nightingale has been degraded" (Awaz Aurat Ki, * I
its lowly position. Thus, Florence Nightingale fre
March 88).
•>,
,
'' |
quently reiterated in her writings the equation good
women equals good nurse. Nightingale insisted on
The incident at Raipur is not an isolated freak oc- ** |
the existence of a close link between nursing and femi
currence as it may seem. It is merely a logical exten»
nity, the latter being defined by a combination of moral sion of the society's desire to maintain the 'morality' £ «
qualities which differentiate men from women. The
and control the sexuality of women in general, the
!
success of nursing reforms depended primarily, accord
other side of the coin being the licence given to men to
§
ing to her, on cultivating the femimne character rather
than on training and education (Gamarinikow, 1978).
(Contd. on p. 5)
■
|
...................................................
- e-'i
j
’.^..
'•
•
Editorial Committee.
Anil Patel
Abhay Bang
Dhruv Mankadi
Kamala S. jayanur
Padma Prakash
Vimal Balaaubrahmaoyan
-
Sathyamala, Editor
-
.
-
■
•.
-
■•
•.’
'
'
'
*
-
•
Views and opinions expressed in the bulletin are those of the authors
and not necessarily oif the organization.
. J
Annual Subscription —’ Inland Rs. 20.00
Foreign: Sea Mail US 14 for all countries
Air Mail: Asia— US I £ Africa &Europe Canada & USA— US $ 11
Edited by Sathyamala, B-7/88/1, Safdarjung Enclave, New Delhi 110029
Published by Sathyamala for Medico Friend Circle Bulletin Trust,
50 LIC quarter University Road, Pune 411016
Printed by Sathyamala at Kalpana Printing House, L-4, Green Park Extn., N. Delhi 16
Correspondence and subscriptions to be sent to—The Editor, F-20 (GF),
Jungpura Extn., New Delhi-110014.
■
K
:--A
' •
1
? -1
1
1
il
ss
M F-r. 6 ./^
Y
M >CC t
(Contd. from p. 6)
sexually exploit women. The situation gets aggravat
ed since nurses come from a lower strata of the society
as compared to, for instance, women doctors who are
not subjected to large scale abuse in the work place.
Unless the issue is fought at this level, the profession
of nursing will continue to be denigrated and the nur
ses treated as available sex objects by all their male
colleagues and patients.
—Sathyamala
r/rc-B
/
VI
J
2-
Ik2
w
(b)
Issues For Debate On Peoples Science In Health Care
(C. R. BIJOY, Pathanjalipuri - P. 0., Thadagam, Coimbatore - 641108 )
I
The dominant health care system of our
country is essentialy based on the modern Allopa
thic system. The state and the market have organised
health care to promote the development of this
dominant health care system. A well established
institutional network consisting of educational
institutions, pharmaceutical companies, medical
equipment manufacturers, marketing network, me
dical
establishments - hospitals,
nursinghomes,
clinics and private practice, huge monolith of a
health care structure established by the state with
its hospitals, primary health
centres and sub
centres have penetrated into the most remote areas.
Yet this dominant health care system is not accessi
ble nor affordable to most of our people. It is highly
exclusivist, expensive, generates overuse of unne
cessary drugs, creates dependancy upon a class of
medical/health care practitioner through the media
tion of scientific mystification. It does not reach
the majority of our people and oppresses the majo
rity of those who approach it. The dominant pers
pective sees the modern health care system as a
legitimate and logical conclusion to meeting the
health needs of the people. It persists by further
establishment of an even more elaborate system
with an even more efficient network of infrastruc
tural facilities, developing even more informations,
programmes, manpower and services that bulldozes
amongst our people to provide them with "benefits"
of the modern world in the manner they choose and
under the assumption that they are desirable, bene
ficial, apolitical and inevitable.
The reactions to such a state of health care
system are efforts to reform within the present sys>
tern of health care using modern medicine through
stress on primary health care, extension of health
care facilities to the rural and tribal areas, protec
tion of consumer rights, opposition to continued
marketing of banned and bannable drugs, pressure
against the continued hospital • doctor - disease drug approach to health care, a more rational
drug and
health policy,
increase in
profe
ssional and managerial abilities of the health per
sonnel and efforts at promotion of people's parti
cipation and their self reliance where promotion of
traditional systems of medicine, folk, herbal and
home remedies and local health practices have an
important role.
8
: .< c ■ hnn eqci
, c i .o vlt*;
One stream of thinking is that the existing
socio-economic and political system is responsible
for the evils of the present health and medical sys
tem. The problem is seen as arising out of an elite,
urban bias in the prio ities of policy makers, comm
ercialisation of medical profession, the capitilist
distortion of modern medical science and techno
logy and its mystification. The counter stream
looks critically at the ideological and conceptual
basis of modern society. The societies In which
modern health S & T evolved are imperialistic and
the propogation of this S & T itself is part of colo
nisation of third world, both intellectually and
materially. The sickness and limitations of the
industrial culture, of which this science is a part, in
the countries of origin is too evident now. Alterna
tive life style and culture is seen as a way out*
Indigenous science and technologies, including that
of health and disease, in the context of indigenous
life styles and practices is to be the basis for evol
ving a truly appropriate need based democratic and
participative (health care) system.
:
,/l' ‘'r
This alternative and counter stream is to be
seen in the following context
:i?.
—
extremely limited access of modern health
system and the escalating loss of whatever
benefits from traditional systems;
minority enjoying access to all types of he
alth and medical care including grudging and
condescending incorporation of traditional
systems of medicine;
.
.11
the failure of the western ethno-centric app
roach to meet the needs and aspirations of
the people even after four decades of inde
pendance;
—
the development process that increases dis
parities in the control and use of resources;
I
the social process where market forces deter*
mine what constitutes knowledge and prac
tice;
., ' . !•■
1
*
the cooption of the state by the market;
the health of an individual or ^community
e
e
c.
t
c
*
M pc
w
Kf o
defined in terms of the political state implies
the power of individual and community to
control decisions that affect their physical,
mental and environmental state.
Mitt (h)
2.
3.
4.
Different communities perceive different re
sources in the same environment. The same
resources are more over perceived and put to
use differently by different communities. The
evolution of knowledge and practice, of sci
ence and technology is a cultural construct
and is based on the specific social formation
and the mode of production of that particular
community at that point of time. The exiestence of heirarchy of cultures is founded on
the ideology of the oppressive classes and is
also used as a tool against the oppressive
classes by the oppressed in a liberative pro
cess.
Culture is built upon complex interactions
involving physical environmental, Ideological, political and economic dimensions. The
relations of production, exchange and, con
sumption find expression in cultural and social
responses. Traditions is the vestiges of earlier
cultural trends ideologically influencing the
present and future.
Traditional science and technologies are the
emperical results of socio-cultural and envi.
ronmental demands rather than mere econo
mic imperatives. It is characterised by its
localised expressions suited to locally avai
lable resources evolving local skills, are
ecologically sound, suited to renewable forms
of energy, low capital outlays and high la
bour content The ensuing products are
' Unsophisticated ‘ and geared to serve limi
ted and specific markets and are based on
agrarian economies.
Modern science and technologies are based
on the ecnomic imperatives of industrial eco
nomies rather than the socio-cultural and
environmental demands. It is characterized by
centralised production requiring newer skills
utilising non-renewable sources of energy,
with high capital outlays and low labour con
tent and are generally ecological disasters.
The ensuing products are sophisticated and
geared to serve a broad market through the
■
creation of homogeneous consdmption be
haviour
rsei
The health care system is always articulated
in a given social formation and the mode of
production of that social formation gives
rise to its corresponding health care ’ system.
The present social formation is that of domi
nance and control exercised totmaintain the
exploitative relations of production.^,,
6.
The aspects of mystification and professiona
lism is rooted in the economic base, and has
nothing to do with the systems of medicine,
and is the expression of these systems in the
given social formation.
;
7.
1
?
5.
Some basic notions :
1.
1
^^4 ^2
p
—
d ' • • •’ ->
ffrynjc
' r<.■->
•
-r
,
1 I
The traditional systems of medicine is closer ■ ;
to the indigenous socio-cultural pattern, i
peoples consciousness of health and disease, I
local skills and resources.
' ;rn lo
On a peoples science movement in health care :
The traditional systems of medicine has a
comprehensive body of knowledge in health science
with a well developed theoretical foundation based
on emperical data, scientific methodology and a
materialist philosophy. It developed in its practice
in heterogenous forms catering to the needs of
people according to the then social formation of
specific communities. But with the advent^of the
market with its modern science and technology and
the state as a mechanism to create conditions for
the development of the market, the common proper
ties, resources and rights of communities to it are
being expropriated from the people. Consequently,
the knowledge base, practices, the science and tec
hnology and skills are pushed out of the control the
accessibility, affordability and suitability of the co
mmunities. The state delegitimises the right of
communities to t iis knowledge and practices of
communities by the development of the process of
institutionalisation.'
^idw rbtov:
•
• '’hcorn
The inability of modern health care system of
the state and the market to satisfy the health needs
and aspirations of the people and the r inability of
the modern medicine to exclusively provide a safe
and satisfactory solution to all health problems has
led to the increasing respectability of the traditional
systems of medicine by the state and the market.
The Chopra committee of 1948, the WHO report in-
‘0 > p •
i |
■ I
j
j
I'
I
i
,
;
I
I
/W
. common properties^ndifincre^e the space for
■■
i
qvstems
of
medicine,
National
Health
ICSSR - ICMR
p0,icv
1982
etc, provides sanctity to this process. The state now
sets itself to increase the patronage
to traditi
o< medlelna ae^opiog
n
L
n
3
WtIil Ii
' ’I
i
i
11
w I1 I
1
■' k! i i
1i
'■
-i "People's
(Paper presented at the seminar on
, Tamilnadu, 26-27
Science Movement", Coimbatore
I
»< l.»-
base of traditional
of medicine, the resource L-*3 base of commuof medicine, the resources
systems
•t,is further expropriatednities and their rights over it,
knowledge, practice and
The crisis in the forms of hr.,
people health care
organisation of indigenous
terns
-
s
■
the mode of
rning skills and production su.ted to
of the day. Incorproduction and social formation
health care system on the
poration in the modern
with modern medibasis of testing done primarily
of folk knowledge,
cine rather than the framework
and logic of that
keeping with the assumption
science is the trend considered to be valid. As the
market incorporates the products of traditional sys-
■■1
•■■■■
of their
■
December, 1987).
’i
5
. - individualsand communities to take care
health with available resources and skills. •
|
deepens further.
A peoples science
should seek to legitimise
movement in health care
to
the rights of people
raw
-- -At-r-.-ri
b)
Pre - Pi^of egsional Course :
The
present pre-professional course is to a large
extent
unnecessary repetition of the higher secondary or pntuniverg
medical
course.
All the Subjects taught are not adequate!.,y
oriented :
s
i)
I
-iI
)
I
iii)
Zool/ogy
the
should
be
In
B.o t any
or
stress
unde, standing
the basic principles of hum a n anatomy
fi
ph 'slology
by a study of similar strjX ture and
f unc t i
11
plants and an. mals.
In
Physics efnd Chemistry - various aspects of
Biophysics, and Biochemistry should be stressed.
so-calJ
in
socle
The
student should <rbe prepared for his role
of
socioloscertain
aspects
through
lectures
in
statistics
&
of
economics.
element s
an jmropology,
tyi o m a t h ema 11 c s even at t hi i s s t age.
c)
1.
of
our
medic
Physiology
form the
basis
Anatomy
and
courses
cannot
education
and
Xhe
content of
these
le
rad i cally
al t ^red except that the teaching should be
The stude
c ad av e r - o r i e t ed and more clinically oriented.
must be exposed to clinical material to help him understa
individu
better
the normal anatomy and physiology of an
/
and the changes in them which constitute disease.
LA-vs D _ Att-vA/V
i
’'family’s income is spent on bottled for
mula (of families with a six-month old
batw).
most poor families cannot really
affora baby food of this kind, 82% pf the
mothers in Barbados were dilutingine for
mula. They were making a 4-day can last
from 5 days to 3 weeks.
As the Protein Advisory zGroup of the
UN says "in many instances, placing an
infant on a bottle istantamount to signing
the death certificatyif the child".
Nevertheless this drive to modernisa
tion fuelled by agribusinesses (and com
pounded by high female illiteracy) goes on
unchecked. The UN Yearbook on Interna
tional Trade Statistics states that baby
food export to the impoverished Sahelian
state-'of Niger increased by 88% in one
year I It has been estimated that under
-developed countries using baby formula
l/pl
A/P i
____ 'rt')
imports have suffered economic losses in spiles of infant formula. And this method
of feeding which seems to the mother to
Dillions of dollars.
This situation shows the willingness of be' .easy, free and recommended by the
firmk to exploit the most vulnerable of hospital becomes a nightmare outside,
where she has to pay for it and try to find
populations for monetary gain. Greater
and greater control of food supplies in the clean w^er and sanitary conditions in
order to ptapare it.
Third World are controlled by fewer and
Dumping\upplies, especially in under
fewer corporations. It also means lower
quality higher priced food because that is resourced Third World hospitals, puts
health care workers into the position of
where profits are. Most importantly,
agribusinesses in their qu^st for moder being de-facto sales'people for the for
mula companies. In my experience as a
nisation and profit maximisation give us
paediatrician working in Africa, Asia and
distorted land use - land is used not for
what people need economically but for Latin America, I have seen thousands of
what is needed economically by the cor cases of severe infant malnutrition and
diarrhoea among infantsiwhose mothers
porations.
have been-^ersuaded by company promo
From a Statement to the Press
tion that formula is superior to breastfeed
by Dr. Roy Brown
ing but who have neither the ihpney nor
...There is absolutely nothing that imthe hygienic conditions to prepare the
pedes/more a maternity ward nurse’s
formula safely to feed their children. This
ability to help mothers of newborns to
\
breastfeed, than the ready availability of is the Bottle Baby Disease.
$
Overuse of Unnecessary Investiga
TECHNOLOGY AND HEALTH CARE tions
and Surgery: As elsewhere in the
world and particularly in countries where
there is a well developed private sector in
AN APPROACH PAPER
by Dr. Ravi Narayan ‘ medical care, there is a growing concern
that unnecessary investigations and often
[This is a background paper written to model of health care is inappropriate, this unnecessary surgery are taking place to
support profit margins of hospitals,
appraisal becomes very important.
serve as a basis for discussion at the
laboratories and medical practitioners.
Technology
Missions:
In
recent
years
medico-friends circle (mfc) annual meet
Doctor-Medical Technology Axis: The
ing. It is not exhaustive nor comprehen the concept of ‘Technology Missions’ has
ICMR-ICSSR
Health for Al report warns
grown
and
some
options
have
been
made
sive but attempts to list out some points
that
‘
eternal
vigilance
’ is required against
and
are
being
actively
promoted.
Aljleast
that would help participants to under
the growing Doctor- Drug Producer axis.
two of the present missions are directly
stand the basis for some of the concerns
and issues related to the theme. related to health care - immunisations and Little is documented about the growing
links between practitioners and diagnostic
Those with access to earlier issues of mfc drinking water.
centres. The kick-back available for or
Urban-Rural Disparity in Medical
bulletins would find additional informa
Technology: In keeping with our inequi- dering a CAT scan is a glaring example.
tion in bulletin numbers 57, 60, 62, 65,
Misuse of Medical Technology: The
tous social structure and planning
88,115,121,143-44 and 145.J
priorities, there has been a greater advan growth of amniocentesis/sex determina
WHY DISCUSS TECHNOLOGY cement of the technological status of tion centres highlighted by health activists
medical/health centres in the urban area in in recent years is one among many such
AND HEALTH CARE?
examples which need further investiga
" Therb are many reasons why the both the governmental/non-governmental
tion.
‘technological’ dimensions of medi sectors and a stagnation in the Rural
Medical/Health Care Is Not Only
cal/health care in India need to be critical Primary Health Centres.
Proliferation of Diagnostic Centres: In Drugs: In recent years, drugs and conse
ly examined and assessed. Some of these
quently Rational Drug Policy and Ration
recent years due to various aspects of a
are:liberalised industrial policy, there has al Therapeutics have received much
Health For All by 2000 A.D.: India’s
been a massive growth of diagnostic tech attention from health and development ac
commitment to this lofty goal demands a
critical appraisal of all aspects of the ex nology centres in the urban areas, all over tivists, consumer groups, professional as
isting health care service and an evalua the country. Most of these centres sociations and policy researchers. Groups
promote sophisticated technologies like
like mfc and others have also looked at
tion of alternative approaches and options.
CAT scan, Ultrasound, Echo etc., and^are medical education and policies like TB
With the increasing awareness that the
western high technology institutional • , all in the private sector. What are its im- ■ control, Family Planning, Child survival
plications?
ISSUES AND PERSPECTIVES
8
fc
<Vt 'C/a/k". Ac H/*/v Aj
•
‘’I't'/V'! ~j<sivi- P-e4 l^o
T h)____
».<s
and so on. But.the technological dimen
a) common investigations at Primary
c) therapeutic technologies like injec
sion of medical/health care particularly
Health Centres and general practice
tions and many forms of surgery
diagnostic technology, surgery and re
b) more sophisticated investigations in
d) technologies for community
lated aspects have never been scrutinized hospitals and consultant practice
health/community level interventions
critically. Considering that these form .
quite a major part of the cost of medical
Appropriate Technology: What it is and What it is not?:
care, they need immediate assessment.
‘Appropriateness’ of a technology is for a particular need, a particular situation, a
TECHNOLOGY AND HEALTH particular level. At the ICMR National Workshop on ‘Appropriate Technology for
CARE
Primary Health Care’ two experts tried to define what ‘Appropriate Technology’ ‘was’
The theme can be explored in many and ‘was not’. Between them they explore all the important dimensions as well as the
ways.
misconceptions.
Technology and Health Status: A
major area of exploration can be the
relationship between advances in health
Appropriate Technology :: What it is
care technology and the health of people To be appropriate for the circumstances in which it will be used, a technology must be
their longevity, morbidity, alleviation
from pain etc. McKeown in his book "The
1. scientifically effective (it works)
Role of Medicine" distinguishes five
...... ....... (it
.............
2. culturally acceptable
fits into the hands and minds of the people and does not
groups of measures while assessing the endanger a social fabric that may already be fragile)
impact of science and technology in health
3. economically feasible (they can afford it within the resources available)
status.
4 have an evolutionary capacity (it can be extended and built upon and is likely to lead
i. Measures which are scientific but : to other changes)
owe little to professional science - manur
5.should be environmentally harmless or atleast, minimally harmfur.
ing of land by farmers and limitation of
- Katherine Elliott/
family size by parents.
Nicolas Jequier
ii. Measures leading to environmental
Appropriate Technology : : What it is not
improvements derived from observations
Appropriate technology is not against industrialisation or against modern technol
on the relationship of living conditions to ogy. It does not represent a return to traditional technology.
health.
It is not restricted to production, hardware and industry but it also involves products
iii. Non-medical science and technol in all sectors such as agriculture, health, communication and others.
ogy - chemical fertilizers, insecticides,
It is not primitive or low technology and does not imply undermining basic research.
herbicides in agriculture and engineering : In fact it emphasises an even greater stress on basic research because in the absence of
technology which contribute to control of the beaten Western path in conventional technology, there is no alternative but falling
the environment.
back on fundamental research and new insights,
insights.
iv. Bio-medical research which ex ■ It is not a substitute for the socio-economic changes required for real development.
tended non-personal measures like food
frame
„ It is not pointless within the 4present f
ft^ork,ofsociety because it becomes the key
tn fhr?
nt-i,
and water hygiene.
to
the transformation of society
f
v. Bio-medical research which resulted
AVK Reddy
in immunization and treatment.
He concludes that at least in the West
false positives and false negatives, ie.,
items iv. & v. have had less contribution
CLINICAL INVESTIGATIONS normal findings in ill health and abnormal
to change in health status while i. to iii. AND DANGEROUS DIAGNOSIS
findings in health. Since most biological
have had more impact.
Recognising Limitations of Lab Tests:
parameters follow normal distribution and
This is not an easy hypothesis to discuss The pathological, micro biological and
the ranges for assessment are narrow,
here but some issues could be considered. bio-chemical investigations of ill health as
there will always be a few healthy subjects
Has development of preventive/promo- well as the study of internal anatomy of with levels at the lower end or higher end
tive measures been neglected? If so,
the diseased body have revolutionized not of normality or just outside the range. All
why?
only the understanding of disease, but,
tests need to be done by specific, wellIs health status improvement to be ex today they are the sheet anchor of medical
defined procedures and routines. In the
pected by technological interventions or treatment, aiding diagnosis, assessing
absence of quality control and when
by socio-economic-cultural changes/in- cure and predicting prognosis. However,
corners are cut due to haste, poor training,
terventions?
there are some basic facts about the meas over work or disinterest by laboratory per
How has the growth of medical/health
urement of biological parameters and/or sonnel the reliability of the tests decrease.
technology affected social values, medi the visualization of internal anatomy that
cal ethics and so on?
is commonly forgotten. All laboratory I
In addition, when the test is given a
In this paper it has been decided to focus tests have their own limitations. They are
significance out of context of patient his
on a few areas:
sensitive and specific to different extents.
tory or. is substituted for clinical judge
In simpler terms, it means that there are
ment based on good physical examination
9
Ac p
7 t /V K'
1
-
/'V
vol
\
The situation in India would definitely
be worse. It is time consumer groups and
professional authorities recognised this
danger.
SURGICAL TECHNOLOGY AND
RITUAL MUTILATIONS
Assessing Surgery: The technology for
surgery has made great advances in keep
ing with the development of more compli
cated and sometimes more intricate forms
of surgery. However, it is true that surgi
cal technique has also begun to be
misused, overused and routinised for a
variety of motives- to playsafe, for greater
profits or due to impatience of the patient
or doctor with medical treatment or for
other such questionable reasons.
What is not commonly known is that
many surgical techniques now in common
application have not been adequately
Dangerous Diagnosis
tested for effectiveness or for providing
ECG: "A survey revealed that the reports of expert ECG interpreters varied by twenty
better prognosis. As more controlled
percent among individuals and by another twenty percent when the same individuals
studies are being done and costs measured
re-read the same tracing at another time.
against relative benefits, many surgical
In one test the ECG delivered a positive finding in only twenty five percent of cases of
techniques are coming under critical as
proven myocardial infarction an equivocal finding in half and a totally negative finding
sessment and are proving to be unneces
in the rest.
sary or of ‘unproven efficacy’ or
In one test, more than half of the readings taken of healthy people were grossly
‘effectiveness’. Episiotomy, tonsillec
abnormal".
tomy, adenoidectomy, some forms of
gastric surgery, radical mastectomy and so
EEG: "About twenty percent ofpeople with clinically established convulsive disorders
on are now under increasing suspicion.
never have an abnormal EEG. Y.et fifteen to twenty percent ofperfectly normal people
In a country like ours, in the absence of
have abnormal EEGs!"
good clinical records, record linkage and
efficient professional quality control, this
X-RAYS: "Conservative estimates peg the number of deaths each year directly
problem is very difficult to assess, but
attributable to medical and dental radiation at 4000.
many surgeons are concerned .about the
A survey showed that as many as twenty four percent of radiologists differed with each
other in interpreting the same chest film even in cases of extensive disease. Thirty one problem.
"Ritual Mutilations": Mendelsohn in
percent of them even disagreed with themselves when re- reading the same films.
the book mentioned earlier lists out some
interesting surveys done again on the
LABORATORY TESTS
In 1975, the Centre for Disease Control (CDC) reported that its surveys of labs across American scene. He uses the terminology
"Ritual Mutilations" to indicate how like
the country demonstrated that ten to forty percent of their work in bacteriologic testing
branding, circumcision and other forms of
was unsatisfactory, thirty to fifty percent failed various simple clinical chemistry tests,
ritual surgery linked to socio-cultural
twelve to eighteen percent flubbed blood grouping and typing, and twenty to thirty
beliefs, we continue to accept, promote
percent botched haemoglobin and serum electrolyte tests. Overall, erroneous results
and inflict forms of surgery which should
were obtained in more than a quarter of all tests.
have been discarded based on informed
In a nation wide survey, fifty percent of "high standard" labs licensed for Medicare
and critical professional opinion.
work failed to pass.
:___________ _____ ____------------------For $12 billion worth of lab tests each year, thirty o^e percent of a group of labs tested
RITUAL MUTILATIONS
by CDC could not identify sickle-cell anemia. From ten to twenty percent of the tested
"Conservative
estimates by a congres
groups incorrectly identified specimens as indicating leukemia. And from five to twelve
sional
sub-committee
say that about 2.4
percent could be counted on to find something wrong with specimens which were
'million operations performed every year
healthy,
are unnecessary and that these operations
In one study 197 out of 200 people were "cured" of their abnormalities simply by
cost $4 billion and 12000 lives or five
repeating their lab tests."
percent of the quarter million deaths fol
lowing or during surgery each year.
then the reliability and ‘hazard’ potential
increase. In measurements that use tech
nology requiring electricity, changes in
voltage can affect readings. With more
complex technologies repair and regular
Maintenance become crucial. It is sig
nificant that many of these limitations are
not known to the medical personnel as
well and even less to the patient or con
sumer public. With the proliferation of
diagnostic centres and the absence of any
quality controlling authority, the situation
of ‘dangerous’ or ‘wrong’ diagnosis can
become ‘epidemic’ in proportion in
10
countries like ours and it is time we recog
nise this. When investigations get ordered
for profit motive and get routinised this
problem will increase phenomenally.
Dangerous Diagnosis: Mendelsohn in
his now famous book "Confessions of a
Medical Heretic" records a series of very
reliable surveys done on the situation of
diagnosis in the U.S. Using the term
Dangerous Diagnosis he quotes from
studies of monitoring/regulating by the
Centre for Disease Control on less than ten
percent of the best labs in the country.
Some of his findings are revealing:
^7^'ue
ha i\) '< n
*-■.________________ >(9
, ~ The liiclepciideiit Health Research
Group says the number of unnecessary
operations is more than 3 million.
Various studies have put the number of
useless operations between eleven and
thirty percent.
One study closely reviewed people who
were recommended for surgery. Not only
did they find that most of them needed no
surgery but fully half of them needed no
medical treatment at all.
In six New York Hospitals, forty three
percent of the hysterectomies reviewed
were found to be unjustified.
A seven year study by the Veterans Ad
ministration of more than 1000 people
found that except for high risk patients
with rare left main artery disease, the
coronary bypass provided no benefit.
Mortality rates for surgery patients were
not significantly different from those
medically treated. Among the low risk
patients, the mortality rates after four
years were slightly higher among those
receiving the operation.
The rate of Caesarean deliveries in US
Hospitals is around twenty five percent.
In some hospitals, it is reaching fifty per
cent: Studies of comparable deliveries
show that Caesarean deliveries occur
three to four times more often in births
attended by electronic foetal monitoring
than in those monitored with a stethescope." .
<&
Why does this happen? To what extent
could this be a problem in a country like1
ours?
TECHNOLOGY
FOR
COMMUNITY HEALTH:: DIFFICULT
CHOICES
Critical assessment of options in the
choice of technology becomes particular
ly crucial when one is planning for com
munity needs - be they local, regional or
national. Mass health care and national
programmes require more careful plan
ning and the choices, because of cost, ac
cessibility and availability of services,
logistics, etc., are rather difficult. This
paper will, however, not explore this
dimension in detail. Choices like sputum
AFB vs. X-ray or MMR; ORT vs. IV
fluids and antidiarrhoeals; which vaccines
to include in immunization programmes;
oral polio vaccine vs. injectable polio vac
cine; cholera vaccine vs. safe water
t
VO’ <>>
programmes; iodised salt or iodised oil
injections; choice of contraceptives etc.
all exemplify the technical, epidemiologi
cal, social, economic and managerial fac
tors that need to be considered in making
such decisions. Very often, the choice is
not really based on a detailed analysis of
all the factors and is based on more ad hoc
or empirical decisions and these need to
be constantly scrutinised and critically
debated.
SOCIAL ISSUES AND HEALTH
CARE TECHNOLOGY
From Micro to Macro Analysis: While
reviewing literature one constantly comes
across
social,
.economic,:
cul
tural, political, ecological, historical and
ethical factors which determine the
growth and development as well as the
transfer, adoption and promotion of tech
nologies. This is applicable to all tech-
nological development not only to those
in health care.
It needs to be recognised and em
phasised that macro-factors in society
have often a greater impact on technologi
cal choice than micro factors - be they
professional, technical or managerial.
In our deliberations, therefore, we need
to constantly look at a macro analysis as
well as a micro analysis; a social analysis
as well as a technico-clinical or technicoepidemiological analysis.
A Social Critique: Professor Banerji in
his recent book - HEALTH AND FAMI
LY PLANNING SERVICES IN INDIA outlines some of the factors critical to a
social choice of technology, emphasising
particularly the effect of market forces and
industrial development on the growth of
medical/health technology as well as the
concomitant glorification of ‘technologi
cal fixes’ to solve societal problems.
MEDICAL TECHNOLOGY
One of the features of the development of the Western system of medicine is the
phenomenal growth and development of medical technology. This technology is often
projected as a liberator of human beings from many dreaded diseases. Treatment of a
disease is considered to need some sort of ‘technological fix’. In the flush of major
medical breakthroughs it was earlier believed that what one needed, for alleviation of
suffering caused by diseases, was a clever, well equipped medical technologist, .who
would ‘fix' most of the diseases.
As is the case with other products in rapidly industrialising societies, market pressures
have been a powerful motive force in the spectacular advance in medical science and
technology. They have played a critical role in projecting problems of sickness, not
simply as technological problems, as problems requiring a ‘technological fix’, but also
as problems that are amenable to the particular brand of technology marketed by them.
Thus, apart from having elements, that are undoubtedly rational and scientific and
instrumental in alleviating suffering, the Western system of medicine also has many
elements which are patently extraneous, imposed on it by market forces. Unnecessary
hospitalisation, excessive or even totally unwarranted use of drugs, tonics, vitamins and
baby foods, excessive use of diagnostic tests and performance of unnecessary surgical
operations are some examples of the undesirable consequences of this. Probably even
more than being an instrument for alleviation of suffering of the sick, the entire system
of medicine in Western countries has taken the form of an industry in which human
suffering becomes an object of profit and market forces ‘create’ demands for the \
products of the industry among the potential consumers."
Exploring Social Links in Technology
Choice and Application: Apart from the
factors mentioned in the earlier critique
there are many other important ones as
well:
a. Privatization: The transfer of
provision of health care from the public
sector to the private sector has major ef
fects on accessibility and availability of
health services, and on costs as well.The
latter is more likely to respond to the profit
motive and market pressures. The social-
ly disadvantaged would be. less likely to
be covered by adequate health care.
b. Gender Discrimination: The social
ethos which favours gender discrimina
tion may affect technological choice, eg.,
female contraceptives being researched
more than male contraceptives. Also the
promotion of female sterilization surgery
when male sterilization (vasectomy) is
easier, less costly, safer and logistically
more relevant is a case in point.
11
AC
Z) /V
Q i\j it', VV)
/\JD 'lt
. fO/'/p
./
_______________ _
APPROPRIATE TECHNOLOGIES
c. Dumping of Technology: Third world suring against avoidable duplication of
In the existing health system, there is an
countries have become a ‘dumping such acquisitions. It is also necessary to
emphasis on over sophistication which
ground’ for obsolete and often hazardous device effective mechanisms for the
repair, maintenance and proper upkeep of necessarily influences research. In the
technologies. This may be equally true
all bio-medical equipments to secure their alternative model we have proposed, the
for medical technology transfer in the
emphasis is shifted to the utilization of
maximum utilization’.
country at present.
paramedical
personnel and the develop
In the section on MEDICAL IN
d. Class differences: In an inequitous
ment
of
alternative,
simple easy-to-use
social set up where the upper classes con DUSTRY, it notes interestingly that ‘the
technologies.
The
research
programmes
practitioners
of
the
modern
medical
sys
trol decision making and choices, various
and
policies
should
be
suitably
modified
tem
rely
heavily
on
diagnostic
aids
involv
coercive tactics, disincentives and other
to
meet
this
need.
This
does
not
imply a
ing
extensive
use
of
costly,
sophisticated
organisational procedures may be thrust
swing
to
the
other
extreme
of
under
bio-medical
equipment.
Effective
into planning affecting the lower income
sophistication.
What
is
needed
is
a
proper
mechanisms
should
be
established
to
and socially disadvantaged groups.
identify essential equipments required for balance between the two approaches to
Programmes of compulsory sterilization
extensive
use and to promote and enlarge meet real social needs.
during emergency symbolised this best
Health for All - An Alternative
indigenous
manufactures, for such
though a subtle element of coercion con
Strategy
devices
being
readily
available
at
tinues even today.
ICMRHCSSR Study Group
This is not an extensive list and par reasonable prices for use at the health care
centres.
ticipants may like to identify more factors
On the whole the pronouncements are
and add to the same.
It is apparent that while science and
POLICY STATEMENTS: INADE vague and do not reflect a comprehensive
technology
policy statements are the order
analysis of the issues of technological
QUATE ASSESSMENT
of
the
day
in the country, Health
National Health Policy 1983: The Na choice, use, misuse or policy.
Care/Medical
Care
policy statements still
In the section on PROBLEMS RE
tional Health Policy Statement of 1983
suffer
from
an
inadequate
analysis and
refers to the issue of Technology in Health QUIRING URGENT ATTENTION, it
require
greater
clarity
and
commitment
to
does mention nutrition, prevention of food
Care in somewhat ambiguous terms. In
the
difficult
choices
that
need
to
be
made.
adulteration, water supply and sanitation,
the section on PROGRESS ACHIEVED,
CONCLUSION
it notes that ‘significant indigenous environmental protection, immunization,
The topic ‘Technology in Health Care’
maternal and child health, school health
capacity has been established for the
is
a complex matrix of issues and
and occupational health as priority issues
production of drugs and pharmaceuticals,
problems,
which cannot all be covered in
but in all these, the issues of technological
vaccines, sera and hospital equipment’.
one meeting. The MFC meeting could,
choice
and
development
are
vague
and
In the section on THE EXISTING PIC
however,become the focal point for a
TURE, it concludes that ‘the estab lost in generalities.
beginning of a process of technological
ICMR/ICSSR
Health
for
All
Report:
lishment of curative centres based on the
assessment.
Issues and perspectives
Western models are inappropriate and ir This document, which is meant to be an
could
be
clarified
and an approach to as
relevant to the real needs of our people and important policy guideline for national
sessment can begin to be explored.
the socio-economic conditions in the health planning, has also not tackled this
In the present social ethos,
issue
adequately.
While
drugs
and
phar
country’.
‘
Technology
’ is subject to glorification,
In the section on NEED FOR PROVID maceuticals are given much importance,
high
pressure
sell, and inequitous invest
ING PRIMARY HEALTH CARE, it other aspects of medical/health technol
ment.
Its
impact
on Medical/Health Care
ogy are not adequately researched.
plans to ‘provide specialist services as
is
bound
to
affect
the nature of Health Care
The concept of Appropriate Tech
near to the beneficiaries as possible,
development
in
India.
It is time, for a
within a well planned network’ and sug nologies is, however, mentioned and a
‘
.critical
’
and
‘
informed'
assessment of
gests that ‘expenditure should be reduced somewhat ambiguous plea is made for a
choices.
Could
we
make
a
beginning?
... by economical investment in the pur balance between ‘over sophistication’ and
‘under-sophistication ’.
chase of machineries and equipment, en-
z
LIFE-THREATENING TECHNOLOGIES - Scenes from Malaysia
(Malaysia
(Malaysia in
in so
so many
many ways
ways God
God’’ss own country - the green canopy of the rainforest blanketing the country as far as the eye can
see, (in fact over 50% of the landmass) enormous natural resources -.rubber, petroleum, tin - endless beaches of surpassing beauty,
easy agriculture that produces crops with surprising ease, a multi-racial society that enjoys a fair degree of what one can term as
"democracy" and a rapidly emerging industrial base.
12
ft ’
■ V
medico fend
146 circle
bulletin
Decenr 1988
PATIEPS RIGHT
I
ANIL .GAONKAR
Everybody, including Indian Medical Count,
agrees that medical ethics, as an entity in the pract
of Medicine is of great importance. Yet, neither it
taught in Medical Colleges, nor is it seriously consider
in clinical practice. What is worse is that there is
evidence of any debate on ethical issues. It is wi
this background that this paper on patient’s rights
being presented here. We hope that it will at least provo
readers to think afresh about medical ethics. (Editor
It is said that "medicine has had its ov
scheme of ethics for at least 2500 years, and e
though the moral rules of the Hippocratic Oa
have undergone considerable development ar
modification, much of modern medical practice
atleast
officially inspired
by
Internation
medical fraternity i. e. the World Medical Associ.
tion s declaration of Geneva, London, Helsink
Lisbon, Sidney, Oslo, Tokyo, Hawaii and Venice."
The scrutiny of these codes reveals that thei
is progressively increasing awareness,. recognition an
respect for ‘autonomy' of the patient in medic,
care. The importance of the ineed for recognitio
of autonomy of patient becomes
—3 apparent whe
one realizes that:
a)
the very nature of medical persuit leads t
intervention into a person or personality,
bj
C)
the specialization and superspecialization in
medicine has 'lured' the practitioners to be
more concerned with 'parts of a person ra
ther than the whole person and
the religion and medicine have always been
associated in the past. History of medicine
has references to priest medicine man or witch
doctor trying to employ special 'power' in
cluding communication with 'God' to effect
healing. The erroneous self-perception of the
healers had led them to take on a 'superior
breed' position.
The phrase 'Patient's Rights' might conjure
in the minds of some medical practitioners an
alarming picture of someone trying to snatch away
from them something exclusive their domain. It
might provoke a confrontist response stemming
from a sub-conscious feeling of vulnerability that
plagues human minds. On the other hand 'duties
towards patients' is something that is more amena
ble to doctor's frame of mind, for he/she is con
sciously or sub-consciously aware of the ethical
requirements of profession. The doctor’s duties
towards his patients and their rights are in fa
ct, two sides of the same coin, and the two
are completely compatible with each other. Dr
George Jacoby, who was the first to differentiate
medical ethics from medical etiquettes puts it
•»
a her succintly,
pa^ienl06^
they deal with the question < country endorses the codes. The Indian Medica'
att'tUde °f the phVsician towards th Council must see to it that
ethics are properly
implemented. The ethics have been described in
r a
- .
detail in "Principles of Bio-medical Ethics” edited
Tra
JCa x ssociatlon Declarations (Coc by Beauchamp and Childress, and are also avaio? patients0"
/dut,es of doctors to'right* |ab|e in the American Hospital Association's Bill
of patient's rights.
The spirit of the various declarations c
World Medical Association, made from time t
time demonstrates a noticeable shift from doctor'
duties in earlier codes to patient's rights in late
codes;
The patient has a right .
1
to considerate and respectful care.
2
to obtain from his physician complete current
information concerning his diagnosis, treat
ment and prognosis in terms that he can be
reasonably expected to understand, unless
it is not medically advisable to give such
information to him (in which case such in
formation should be made available to an
appropriate person on his behalf)
3
except in case of emergencies, to receive
from his physician information prior to the
start of any procedure i. e. informed consent
and/or treatment.
4
to refuse treatment to the extent permitted
by law and to be informed of the medical
consequences of his action.
5
to every consideration of his privacy con
cerning his own medical care program.
6
to expect that within its capacity a hos
pital will comply to the request of a patient
The Geneva Declaration (1948, modified
in 1961
and 1983)
Dedicate your life to the service of humanity,
Let health of your
consideration.
patient
be your
first
The London Declaration (1949)
—
The physician shall owe to his patients
comp
lete loyalty.
He shall provide absolute
confidentiality on
all he knows about his patient even after
the patient has died.
The Lisbon Delcaration (1981)
—
A patient
physician.
has
full
right
to choose
I reproduce them briefly here:
his
He has right to be cared by a physician whose
ethical judgements are free from outside
interference.
for services.
7
to obtain information as regards relation
ship of his hospital to other health care
and educational institutions in so far asj
his care is concerned.
8
to be advised if the hospital proposes to
undertake human experimentation affecting
his care or treatment.
9
to examine and receive explanation of his
bill regardless of the source of payment.
10
to have reasonable continuity of care.
11
to know what hospital rules and regula
tions apply to his conduct as a patient.
A patient may refuse treatment after receiving
edequate information.
A patient has right to die with dignity.
A patient has right to i
receive or call for
spiritual and moral comfort.
Adherence to the Declarations:
Moral binding
on Indian counterpart
India, a member of the World Medical Association, is <a signatory to these declarations and
therefore in spirit the
■
J medical fraternity of the
2
'J'
V
medico friend
146 circle
bulletin
December 1988
PATIENT'S RIGHT
I
ANIL
PILGAONKAR
Everybody, including Indian Medical Council,
agrees that medical ethics, as an entity in the practice
of Medicine is of great importance. Yet, neither it is
taught in Medical Colleges, nor is it seriously considered
in clinical practice. What is worse is that there is no
evidence of any debate on ethical issues. It is with
this background that this paper on patient3s rights is
being presented here. We hope that it will at least provoke
readers to think afresh about medical ethics. (Editor)
It is said that "medicine has had its own
scheme of ethics for at least 2500 years, and al
though the moral rules of the Hippocratic Oath
have undergone considerable development and
modification, much of modern medical practice is
atleast
officially inspired
by
International
medical fraternity i. e. the World Medical Associa
tion's declaration of Geneva, London, Helsinki,
Lisbon, Sidney, Oslo, Tokyo, Hawaii and Venice."
The scrutiny of these codes reveals that there
is progressively increasing awareness, recognition and
respect for fautonomy( of the patient in medical
care. The importance of the need for recognition
of autonomy of patient becomes apparent when
one realizes that:
a)
the very nature of medical persuit leads to
intervention into a person or personality,
bj
the specialization and superspecialization in
medicine has 'lured' the practitioners to be
more concerned with 'parts' of a person ra
ther than the whole person and
c)
the religion and medicine have always been
associated in the past. History of medicine
has references to priest medicine man or witch
doctor trying to employ special 'power' in
cluding communication with 'God' to effect
healing. The erroneous self-perception of the
healers had led them to take on a 'superior
breed' position.
The phrase 'Patient's Rights' might conjure
in the minds of some medical practitioners an
alarming picture of someone trying to snatch away
from them something exclusive their domain. It
might provoke a confrontist response stemming
from a sub-conscious feeling of vulnerability that
plagues human minds. On the other hand 'duties
towards patients' is something that is more amena
ble to doctor's frame of mind, for he/she is con
sciously or sub-consciously aware of the ethical
requirements of profession. The doctor's duties
towards his patients and their rights are in fa
ct, two sides of the same coin, and the two
are completely compatible with each other. Dr
George Jacoby, who was the first to differentiate
medical ethics from medical etiquettes puts it
11
»“ 4>
rather succintly, 'they deal with the question of
the general attitude of the physician towards the
patient.
World Medical Association Declarations (Cod
es): Transition from 'duties of doctors to 'rights*
of patients
The spirit of the various declarations of
World Medical Association, made from time to
time demonstrates a noticeable shift from doctor's
duties in earlier codes to patient's rights in late**
codes :
country endorses the codes. The Indian Medica'
Council must see to it that ethics are properly
implemented. The ethics have been described in
detail in "Principles of Bio-medical Ethics" edited
by Beauchamp and Childress, and are also avai
lable in the American Hospital Association's Bill
of patient's rights. I reproduce them briefly here:
The patient has a right .
1
to considerate and respectful care.
2
to obtain from his physician complete current
information concerning his diagnosis, treat
ment and prognosis in terms that he can be
reasonably expected to understand, unless
it is not medically advisable to give such
information to him (in which case such in
formation should be made available to an
appropriate person on his behalf.)
3
except in case of emergencies, to receive
from his physician information prior to the
start of any procedure i. e. informed consent
and/or treatment.
4
to refuse treatment to the extent permitted
by law and to be informed of the medical
consequences of his action.
5
to every consideration of his privacy con
cerning his own medical care program.
6
to expect that within its capacity a hos
pital will comply to the request of a patient
for services.
7
to obtain information as regards relation
ship of his hospital to other health care
and educational institutions in so far as;
his care is concerned.
<
8
to be advised if the hospital proposes to
undertake human experimentation affecting
his care or treatment.
9
to examine and receive explanation of his
bill regardless of the source of payment.
10
to have reasonable continuity of care.
11
to know what hospital rules and regula
tions apply to his conduct as a patient.
The Geneva Declaration (1948, modified in 1968
and 1983)
Dedicate your life to the service of humanity.
Let health of your
consideration.
patient
be your
first
The London Declaration (1949)
The physician shall owe to his patients comp
lete loyalty.
He shall provide absolute confidentiality on
all he knows about his patient even after
the patient has died.
The Lisbon Delcaration (1981)
A patient
physician.
has
full
right
to choose
his
He has right to be cared by a physician whose
ethical judgements are free from outside
interference.
A patient may refuse treatment after receiving
adequate information.
A patient has right to die with dignity.
A patient has right to receive or call for
spiritual and moral comfort.
Adherence to the Declarations: Moral binding
on Indian counterpart
India, a member of the World Medical Asso
ciation, is a signatory to these declarations and
therefore in spirit the medical fraternity of the
I
2
M
v
Lt I 11
f./c
’((.t, Dei <e
Mire n)
No catalogue of rights can guarantee the pa
tient the kind of treatment he has the right to
expect. A hospital has many functions to perform,
including the prevention and treatment of disease,
the education of both health professional and pati
ents, and the conduct of clinical research. All these
activities must be conducted with an overriding con
cern for dignity of the patient.
reconcile with this situation ? I 'should appreciate
reader's response on this issue.
Right of Informed Consent:
In recent years virtually all medical and rese
arch codes of ethics have held, and it is legally
binding, that physicians must obtain informed con
sent of patients before undertaking significant
Since few issues in medical ethics receive
therapeutic or research procedures. Though these
more attention than right of information and infor
consent measures have been designed largely to
med consent I plan to discuss them at length.
protect the autonomy of patients and subjects, they
are observed more in breach than in adherence.
Right of Information about diagnosis, treatment
Often the consent papers merely serve as legal pa
& Prognosis :
ssport for the treating physician to get away with
anything; obtaining informed consent being just an
Three arguments are often put forth for l/mi-*^*-t‘eff^y^ ritual."
ted disclosure in practice :
4
___ _ ______ _
(i)
4
Fear of alarming the patient, a sort of bene
volent deception. It must be however remem
bered that such acts violate the principle of
respect for persons and fidelity, as well as
pose threat to the relationship of trust bet
ween physicians and paTients.
(ii)
Health care professionals cannot even kP°w,
let alone communicate, the "whole truth."
(iii)
Some patients particularly the very sick ones,
do not want to know the truth about their
condition. Should a patient desire so, his/her
wish ought to be respected.
/
Now I shalMake a hypothetical cas'>:
v
The declaration of Oslo (1970, revised 1983)
on abortion has modified "the human li/e from con
ception" to "human life from its beginning." The
declaration gives a green signal to the therapeutic
abortion. The Maharashtra State Ac* dealing with
amniocentesis and prevention of Female Foeticide,
forbids a doctor from disclosing the results of am
niocentesis to the patient. The Declaration of Ge
neva implores the doctor "not to use his medical
knowledge contrary to the laws of humanity even
under threat." Since revealing the results of amnio
centesis tests might, and have been found to, lead
to discrimination against female foetus, a doctor
should keep his lips sealed when asked about the
sex of the foetus. But then does this contravene
with the spirit of the codes ? How should a doctor
3
Since miscoriceptiohs regarding informed
consent are common, it is worthwhile examining
what important functions does informed consent
serve. Alexander Capron has identified these func
tions :
1.
The promotion of individual autonomy
2.
The protection of patients and subjects
3.
The avoidance of fraud and duress.
4.
The encouragement of self-scrutiny by medical
professionals.
5.
The promotion of rational decisions.
6
The involvement of the public in promoting
autonomy & in controlling biomedical research.
Beachamp and Childress have pointed that
the act of consent must be genuinely voluntary and
that there must be adequate disclosure of informa
tion. They note that there are two elements of in
formed consent, each presenting distinct issue. The
information component refers to adequate disclousre of information and adequate comprehension by
patients of what is disclosed, while the consent
component refers to a voluntary decision on the
part of a competent person. They question, "but
how much and what types of information must be
imparted, how well must it be understood ? Is con
sent valid if it is given under conditions of social,
institutional, or family pressure or if the consent is
irresponsible ?"
Informed Consent
The voluntary consent of the human sub
ject is absolutely essential.
— The Nuremberg Code (1947)
•Cancel in 1987 published a study designed
to determine why physicians have misgivings about
the need for informed consent. The study showed
that doctors see a loss of decision making power,
feel uncomfortable because of increase in profe
ssional accountability, and are concerned that it
might affect the ongoing relationship with the
patient.
a
Informed Consent: Consent to surgery by
a patient or the participation in a medical
experiment by a subject after achieving an
understanding of what is involved.
— The Webster's Medical Desk Dictionary
It is too naive to assume that doctors are not
following medical ethics simply because most of
them are not aware of ethical issues. Doctors are
becoming more money-conscious, they are more
callous to the patient's needs than they were before,
no longer are they 'Friend-Philosopher-Guide to
tteir patients. Such excuses as 'work pressure and
outside influences' are lame.
a
Patient has a right-to“seFTdetermination
and that he (she) is entitled to know and
approve of his (her) treatment.
— The American College of Physicians
Ethics Manual
a
Willing and uncoerced acceptance of a
medical intervention by a patient after
adequate disclosure by the physician of
the nature of the interventions, its risks,
and benefits as well as of alternatives with
their risks and benefits.
— Jonson et al.
Since patient is always at the receiving end,
it is necessary that he must be conscious of his
rights Benevolent paternalism from doctors; 'let me
think for you,' and patient's blind faith in his doc
tor : "Afterall he is the best judge of my problems,
I would do what my doctor says anyway'', will be
harmful in the long run. Every consultation must
bring these questions to the patient's mind: What
is n^y doctor doing ? Why he is doing so ? Will it
harn^ me ? Do I have suitable alternatives ?
REFERENCES :
1
Gil^n R. Medical oaths, declarations and codes.
Er Med J 1985; 290:1194-95
2
And this leads us to the main issue at stake :
Why medical ethics are observed more in br
each than in adherence ? The issue is complex and
doctors and patients are both responsible for this
situation. It is indeed a paradox that no medical
student is ever taugth medical ethics during under
graduate training. Medical Journals in India also
seldom seem to discuss ethical problems. Journal
of Medical ethics, which deals exclusively with
ethics, has carved a niche for itself in very few me
dical libraries. Given this continued negligence of
the subject, medical students are hardly interested
in knowing medical ethics, let alone imp.ement them
in future practice.
4
3
Fletcher J. Morals and Medicine, New Jessey
Princeton University Press, 1979:5-6
Beavcham TL, Childress JF, eds. Principles of
biomedical ethics. 2nd ed. Oxford : Oxford.University Press, 1983:336-338.
4
Taylor KM, Shapiro M, Soskolne CL, et al : Phy
sician response to informed consent regulations
for randomized clinical trials. Cancer 1987; 60:
1415-1422.
5
Capron A: Informed consent in catastrophic
disease and treatment Univ. Pa Law Rev 1974;
123:364-376.
aa
m
i
a
s l
131
medico friend
circle
bulletin
Ii'l
II
-
'I
■
-
/
AUGUST 1987
.1
J
S3 3
a
E*
n
a
O
■5
j
j i
J ...
■
j. :
■ -'0
1.^
I
Family Planning in India : Theoretical Assumptions,
Implementations and Alternatives
if
II1
(Report of the Thirteenth MFC Annual Meet)
As is the tradition of the MFC meet, the 13th
meet, held at Kaya, Rajasthan during January 26-27,
1987 also invited a few individuals to prepare background
papers on the theme: Family Plaiming well in advance
and aimed to distribute them to the participants
much before the meet. Thus, rather than the authors
presenting the individual papers, time can be well
spent in discussing the issues which emerge, resolving
the inconsistencies and arriving at some common
platform. However, as happens often, not all the
14 papers were prepared in advance. Although by
the time the meet went into business, all the papers
were available to the participants, their non-availabi
lity before the Meet did somewhat adversely affect
the flow of the discussion.
In any event, this note endeavours to summarize
the major thrust of the deliberations which lasted
for nearly two days, among nearly 75 persons from all
walks of life ranging from medicos, activists, social
scientists and government or semi-government officials.
The issue of family planning was considered from
three broad perspectives: Theoretical framework
keeping in mind the debate on resource constraint
versus population problem (Is there really a resource
constraint and is population control an answer,
even if partial, to it. The second perspective related
to the Indian family planning programme and its
actual implementation as well as underlying medical
and social implications. In light of this reality, the
third perspective aimed to consider workable alter
natives such as natural family planning methods.
Anant Phadke’s paper “Population Versus Re
sources: An Apparent Problem” and Ilina Sen’s
paper “Population Policy in China: Theory and Prac-
01 0
tice”, set the discussion of the first day’s meet. The
group of nearly 75 participants were divided into
four subgroups to deliberate on the theoretical assump
tions underlying the oft-debated issue of population
control versus resource constraints. A set of issues
which appear pertinent were listed before hand, by
some of the members, to be used as a guide. The
four groups, after spending nearly four hours each
discussing the issues on the theme, met together in a
plenary session the same evening, where the four
reporters presented the gist of the discussion in their
respective groups.
The setting for the discussion was the fundamen
tal question: whether there is a resource constraint
or not. According to one school of thought, resourc
es are finite and cannot easily be replenished. In a
situation of growing population, the available stock
of resources will not last long. Hence, the need to
curb the growth of population. According to the
second school of thought, with the advancement in
technology and explorations of alternative sources
of energy and other resources, the scope is unlimited.
In this context, the question of population control
becomes baseless. What is at issue is not limits on
potential availability of resources but their distribu
tion which is highly skewed, with the majority of the
population having access to a small proportion of
the resources and the few rich nations (and few weal
thy individuals within all nations) cornering and
using up a lion’s share of the resources. In this
context, it has been suggested that the development
model or the pattern of development, needs to be
carefully re-examined and suitably altered ormodified.
After great deliberations it was, however, re
cognized that the whole area of alternative sources
COMMUNITY HTALTH CZLL
47/1, (First Floor)Sc. .Marks rioad
BANGALORE-5GO 001
•ill
d
Ml
I■I
111
i
!
I
3
'll
C) Fc
3
of energy is yet an unchartered area. Although
theoretically it offers immense possibilities, one would
have to weigh the pros and cons of each of such possi
bilities, and safeguard against another Bhopal or
Chernobyl like disasters. Thus, one would have
to, for the time being, accept the premises that re
sources are finite.
■I
>
■
l!
MO
I
I
Id i.
11
J ;
/a>,
gramme which receive foreign funding. This may be
;
true even with regard to foreign funds received by
some of the activists or radical elements. In fact,
the elite interests in the country may themselves be
sometimes in tandem with the foreign agencies. Ft
must, however, be recognized that this issue is highly
emotionally charged. What, is needed is objectivity
and willingness to examine the facts with calmness
and maturity.
I
-■
c.
'
It was further agreed upon that even in a situation
of far more egalitarian distribution than what pre
€/■
Regarding the question of China’s population
vails today, we have to have a population policy as
distinct from population control, and disseminate in policy and the recent changes in that policy, a view
formation on various birth control methods, so that was expressed that the great strides that China has
individuals can exercise their free choice. (The made in material development has not been without
various concepts—birth control, population control, a heavy price. Also a question was raised whether
the active pursuation of family planning policy by
population policy, family planning denote very diffe
the Chinese government was a felt need or a created
rent meanings and should not be confused). It was
generally felt that questioning the justification ot need (resulting from the desire to accumulate capital).
population control does not mean that we deny the In light of such doubts and in view of the changes
need for information on birth control as a human that the Chinese themselves are moving towards, do
right. The group as a whole was against population we emulate the Chinese model? Or does it ofier
control, especially because in the Indian context, any lessons? It was, however, agreed upon that we
?7
it implied coercion and interference with personal1 do not know enough about China’s population policy,
except through the impressions of the visitors, and the
lives.
d>.
official statments of its political leaders, and there
Also, the group expressed a view that it is necessary fore. the need is to learn more, historically, about
to gain better understanding of what determines the Chinese population policy.
&
family size and fertility rather than examining the issue
(u
On the issue of integration of maternal and child
in a narrow context, of population versus resources.
In this context questions were iraised about an absence health with family planning, the group, nearly everyone
of well-defined policy on resource utilization, al unanimously agreed that this has resulted in allocating
though there is a national policy on population. and spending a lion’s share on family planning at the
It was fell that we cannot really have one without cost of the MCH programme. Even the Community
Health Volunteer (CHV) scheme has financial alloca
having the other.
tion under the family planning head. Theoretically
(There was a group within the MFC which felt it is difficult to find fault with this integration because
rather strongly that those who work to make ic- family planning should naturally follow a good MCH
A
sources usable are not the ones who consume them programme. However, in the target oriented set-up,
and yet it is their reproduction which is sought to be detailed targets are laid for family planning perfor
curbed in the guise of population policy or family mance (and not for the MCH performance), and the
planning. Further, there ought to be a policy regard emphasis and priorities become lop-sided and are in
ing those who consume the resources to revitalize and
fact reversed.
regenerate those resources).
On the second day the larger group was divided
The context and the content of the family planning into three sub-groups, each having a specific theme to
programme in India were discussed with reference to discuss and deliberate upon. A few papers formed a
three major questions, (i) Is the Indian programme, backdrop to guide the discussion. The three themes
wittingly or unwittingly influenced by the developed that emerged from the background papers were:
countries and their vested interests? (ii) Does the Contraceptives, targetting of family planning towards
population policy of China and the recent shifts in women; and financial resources and parameters
I
that policy offer any lessons tor us? and (iii) should
s
which affect family
1
, . planning, including the spread
the family planning programme be integrated with of family planning among the tribal population.
maternal and child health?
t
Papers by Sathyamala entitled “Contraceptive
The role of developed countries in influencing
!■
Choice: Safety Vs. Efficacy and by Leela Visarta,
our population policy created a lot of heat, A feel“Relative Risk of Pregnancy Vs. Risk of Contracep $
ing was expressed by some of the participants that
tion” and by Mira Sadgopal and Sadhna Saxena on
there often are hidden agenda in the population pro■
e
t
e
3
i
ii!
e
e
e
i
e
(■
2
I
»
H^-0. 131
^c>)
“Fertility Awareness and Natural Birth Control:
Beyond Family Planning ” raised a lot of enthusiasm
among the participants. Overall, it was observed
that as far as the risk of contraception is concerned,
most of the studies and the data pertain to the deve
loped world, which may or may not apply to a deve
loping country like ours. Therefore, there is a need
for systematic, long-term studies within our country.
For example, individuals who have undergone tubec
tomy and/or laparoscopy (these being the most widely
used family limitation methods in India today) should
be followed for an extended period of time to study
morbidity, or what is often described as post-tubec
tomy syndrome, as well as mortality in a systematic
manner.
It was further felt that the camp approach to
prpmote family planning contributes to an increase
in morbidity and mortality among its users, This
is because some of the essential preconditions are
overlooked. For example, aseptic conditions are not
maintained properly in the camps and the doctors are
not always well trained. Also, follow-up of the indi
viduals undergoing surgery is minimal at best. All
these must be giving rise to morbidity among the
sterlized patients. A through study not only of the
camps but also of individuals participating in this
endeavour is in order.
The group as a whole also felt that all available
information indicated that vasectomy as a method of
family limitation was the safest as well as the most
simple. For the couple who has completed family
size, the group recommended vasectomy as a method.
It was also recommended that condom was the safest
method for spacing compared to most other methods
currently in use. However., in the event of a failure
or pregnancy, it should be backed up by safe and early
abortion facilities.
As far as natural family planning is concerned,
it was agreed upon that among the various natural
methods, the cervical mucus method was the easiest
and the simplest and even the illiterate women in
rural areas can learn it and use it effectively. A
general feeling was expressed that the natural methods
should also be promoted by the family planning
programme.
However, one of the major drawbacks
of natural methods is that they demand full support
and co-operation of the husbands. However, this
is an area, where a lot of ground has to be cleared
before we can hope for any results. There ought to
be a systematic teaching of fertility awareness, which
can give self-confidence to the participants. Funds
ought to be earmarked for teaching the rural as well
as urban couples about fertility awareness, (heir own
selves and population related issues.
I31
Padma Prakash's note on “’Family Planning Pro
gramme: Women as Targets” was addressed to the
issue that women have been the focus of family
planning programme since its inception. This, on
the one hand means that contraception becomes
available to women, but on the other hand, it places
heavy burden on women in terms of having to bear
heavy load of morbidity associated with contracep
tives which interfere with hormonal balance. The
group strongly felt that along with female methods,
male methods should also be made popular again,
and while a couple should have freedom to choose
the method best suited to them, the burden of limiting
family size cannot be entirely that of women.
Two papers; one by Sudarshan Iyengar and
Ashok Bhgrgava, entitled “Primary Health Care and
Family Planning Programme in Rural Gujarat:
Some Issues” and the other by Ravi Duggal, entitled
“Financing Family Planning”, formed the background
material for discussion on financial resources and
parameters which affect the financial allocation to the
family planning programme.
The issue of financial allocation was viewed in the
context of the larger health issue and it was shown
that in the target oriented programme, health pro
grammes get neglected and family planning achieve
ments or fulfilment of targets receive priority. It
was further noted that the performance of the PHC
workers is judged on the basis of the family planning
performance. Health related activities are relegated
to the lower place in the order of priorities.
Leela Visaria
3
i'^
n-z
}\)
From the Editor’s Desk
The National Family Planning Programme rests
on several assumptions which are based more on
wishful thinking than on actual facts. One such
assumption is — if it is consistently and continuously
dinned into everyone’s head ‘A small family. Happy
family’, ‘We two, ours two’, ‘Delay the first, Space the
second, Stop the third' etc., through all the avaiable
communication channels, the people will soon enough
come to accept the desirability of acting on the
message. Looking at Kerala with its low infant
mortality rate, high female literacy rate and low birth
rate, it is assumed that there is a direct correlation and
that if these factors are manipulated in a population
showing high birth rates, there will be an automatic
decline in the fertility levels. The article reproduced
in this issue of the bulletin challenges these very
assumptions; a large proportion of the population may
adopt sterilization to limit their family size but this
in no way indicates that they have adopted the twochild family norm as well; a village may be innundated with modern facilities but this in no way inidcates
that the way of life for the majority has changed in
such a way as to make it advantageous to have fewer
children.
Apart from such indirect strategies, there are also
two essential differences in the coercive tactics used
by the government in the past and today. During
the Emergency, the pressure was on the ‘targets’ and
the targets were men. Today, the pressure is on the
Health Workers and the targets are women. In
Uttar Pradesh, 500 Multi purpose workers were
sacked for their failure to achieve individual targets
fixed for a six month period (Indian Express, 16th Oct.
1985).
The Supreme Court is clear about what all this
amounts to; it is not the object of State action (how
ever laudable or desirable such action may be) but the
direct effect of such action on the citizen and his
fundamental rights that must be seen. Thus, accord
ing to two lawyers in the supreme Court (Mr Ganesh
and Venkatramani), “if a given administrative act
contravenes or infringes or even constitutes an immi
nent threat to the citizen’s guarenteed rights, such
acts would be unconstitutional notwithstanding the
fact that it was done pursuant to a laudable policy or
for the intended benefit of the citizen”.
Sathyamala
If people do not behave the way the government
wants them to, the only option then seems to be to
force them into submission. Learning from its past
mistakes, of the Emergency days, the government no
longer considers direct force as a feasible option.
Instead, it merely links EPP to poverty alleviation and
drought relief programmes. Rajasthan for instance,
has experienced severe drought for the last three
years. One of the prerequisite for an ‘eligible’ couple
to get work in the food-for work programme is to
show that one of them is sterilized (if not, they are
‘advised’ to undergo sterilization).
And when
attempts are made on the part of the activists to ex
pose such ‘excesses’, they are immediately arrested
for disturbing the peace of the country, (last month
two activists from the Rajasthan Kisan Sanghathan
were arrested for demonstrating against such mea
sures).
J
lil
medico friend
circle
bulletin
•
■Sa
oo
I
.'Z., .■
■'
JUNE 1987
3^
Two Decades of Sterilization, Modernisation and Population
Growth in a Rural Context*
Stanely A Freed and Ruth S. Freed
Despite a popular reaction against the alleged
coercive aspects of the sterilization programme
during the Emergency from June 25, 1975 to March
21, 1977, the Government of India did succeed, much
faster than might otherwise have happened, in estab
lishing sterilization as a routine and acceptable option
for. couples wishing to, terminate childbearing. In
India, as in the United States, sterilization is now the
principal birth control technique for couples who
want to end childbearing rather than just to control
the timing of pregnancies. This development has
led to a certain journalistic optimism during the last
two or three years at least in New York, concerning
the possibility of controlling India’s population
growth. But caution has also been expressed and the
reason could be found in a photograph accompany
ing one of the report: a sterilized mother, presumbly
more or.less typical, was shown sitting on a cot with
four of her five living children, rather than the two
children that the government would prefer.
.
fc
. v. .J •
' ■ ■■-2
. i
a
Sr
’J
.
w.
.
EE
_
.
•JS J \ 0
fl
to introduce birth control, the growing use of con
traception, most especially sterilization, a declining
birth rate, and the modernisation of education,
communications, and the economy. Although the
growth rate only rose from 2.20 to 2.23 percent, it
nonetheless did not decrease as had been expected.
The apparent paradox of a stable or slightly increasing
rate of population growth in the face of increasing
modernisation, rising sterilization, and falling fertility
has been something of a surprise. The usual ex
planation, that mortality has declined as fast or faster
than fertility, while mathematically sound, offers
little insight into a complex social phenomenon.
This essay concerns the relationships among
sterilization, modernisation and survivorship in the
north Indian village of Shanti Nagar (a pseudonym)
based on the studies made in 1958-59, 1977-78, and
1983. The 25 year period of research is especially
noteworthy because it includes the end of the 1950s,
when very few people were sterilized, and the 1970s
If a significant number of people who undergo just after the Emergency when sterilization was well
sterilization do so only after having had five children, established. Studies carried out in a single village
it seems clear that survivorship, that is, the average may fairly represent a limited region, but one must be
number of surviving children of mothers at the end very careful about extending the conclusions to the
of the childbearing span, will merit more attention greater part of India or even to the north-western
than it has received until now. The fertility rate and. quadrant of the country where Shanti Nagar is locat
the number of persons who “accept family planning”, ed. However village studies have the important
more often invoked than survivorship in discussions advantage of intensity and are a valuable complement
of population growth, are important, but to mini to broad surveys.
mise the significance of the size of the completed
Studies of change in the rate of population growth
families can lead to surprises ’ when the decennial
in India often concentrate on today on two principal
census results are published. Thus the most note
determinants: modernisation and contraception.
worthy feature of the 1981 census of India is perhaps
Modernisation is generally defined as a combination
the slight increase in the rate of population growth
* Condensed from the original in ‘Economic & Political
during the 1970s in comparison to growth during the
weekly’, 20:49, 2171-75, Dec. 1985
1960s, despite an energetic governmental campaign
_
M®1
I
I
II
■’
i
nunicatiorrs revolu
of some or all of the following processes: industrialisa- /economic, educational, and communicati
The village acquired electricity, brick houses
tion, urbanisation, enhanced communications, spread tion.
t
replaced
mud huts, and streets were paved. Farm
of education, improved health and nutrition, female i
machinery
have largely displaced bullock power and
employment outside the home, erosion of traditional i
hand
labour.
Frequent bus service has increased the
customs, and an increase in specific attitudinal and 1
ease of commuting to urban areas where many of
psychological processes such as ‘rational’ as opposed '
to ‘traditional’ thinking. Sometimes several attitudes the men have urban jobs. Radios are now common,
and there are some television sets, and newspapers
or values are conceptually combined and designated
are delivered daily. The educational level has risen
as “modernity values” or a “modernity syndrome”.
dramatically for both men and women. Modern
Fertility is generally assumed, with qualifications to
health facilities are more easily accessible. A nurse
have an inverse linear relationship with most aspects
midwife regularly visits the village to discuss, among
of modernisation. In India, effective contraception,
other matters, family planning and sterilization.
the second important determinant of population
Many villagers have been sterilized. The village has
growth, is chiefly sterilization. The widespread
become much more modern, more prosperous, and
recourse to sterilization suggests that India s persis
better informed about governmental programmes
tently high rate of population growth might be better
including the Family Planning Programme. Moder
understood if attention were to some extent shifted
nisation has had relatively little effect on the family,
from birth and death rates to survivorship because which generally maintains its traditional form and
survivorship, sterilization, and the kind of fertility
functions. There were 110 families in the 1950s and
limitation means that is called ‘parity specific are
176 in the 1970s with an average of more than seven
all related. Parity-specific fertility limitation means
that couples begin to limit their families only after members in both decades.
IL
‘X'WM
1
l!
I
j_
li'
W& 41
I
1
111
-.1
1
I
s
'■''a
I
1
• , fl .
wi
I I
f
■I
I
■W* " !
w
"r II,'
I
p
i!
''
c
c
c
c
V
Xi
I
having had the number of children that they want.
Sterilization and survivorship are closely related
because a couple’s decision to undergo sterilization
is based principally on the number of their suiviving
children especially sons.
Parity-specific fertility
limitation is influenced by the sex of children, for
sons are preferred to daughters. There are many
reasons for this preference, most of them widely
recognised. Few couples are satisfied with just one
son, for the rate of infant mortality is still high enough
to make parents with only one son very anxious.
■
I
A>
During the intercensal period of 19.5 years, the
population increased by 525 persons (65.7%), tanta
mount to an average annual rate of population growth
of 2.59 percent, rather higher than the all India figure
of about 2.21 percent for two decades from 1961 to
1981. When we include in the calculation individuals
currently living away from Shanti Nagar who are
members of the village families (for example, sons
living away from home for the purposes of employ
ment) while excluding married daughters visiting their
parents because they are no longer permanent resi
dents of the village, the average annual rate of popu
One might think that, for sterilized couples, family lation increase was 2.77 percent. The crude birth
size depends on sterilization, for sterilization puts rate during the intercensal period was estimated at
an end to childbearing. In fact, the relationship is
38.5. It should be borne in mind that both the rate
the reverse; sterilization depends on the number of of population growth and the estimated crude birth
couple's living children, especially sons, because couples rates are averages over a period of years and could be
practice gender-influenced parity-specific fertility limita expected to have changed, perhaps significantly,
tion. They do not have a sterilization operation during the period. The proportion of males in the
until they have all the children that they think are population increased from 51 % in the 1950s to 52.5 %
necessary. The
_ __ fertility rate has rather a peripheral Fin the 1970s. The population increase has been
role in such a perspective on family size and the late much less for young children than for old persons.
of population growth. Husbands and wives do not For example, the percent increase from the 1950s
base their sterilization decision on the number of live to the 1970s for children two years of age and less
births, the basis of the fertility rate, but rather on the has been only 23 percent as compared to 66 percent
number and sex of the surviving children.
for the whole village. Although Indian censuses
may tend to undernumerate children four years o
age and younger, we think that the principal reason
Population Growth
that the increase in the number of young children is
Shanti Nagar, located in the north of the Union relatively modest is due to intense birth control pro
Territory of Delhi, is in general demographically and
gramme that the Government of India pursued during
economically similar to many of the villages in the
the Emergency. We began to take our 1977 census
adjacent parts of Haryana and Uttar Pradesh. From only about 6.5 months after the end of this 21 month
the 1950s to the 1970s, Shanti Nagar experienced an
I
2
v
' '■ •. .f**..,*
BL
K!
'
V
a
J
Ip L' > 0
period. Therefore, the relatively small number of
infants upto about 2.5 to 3 years of age partly reflects
the effectiveness of the sterilization programme during
the Emergency.
makes the situation more permanent, provided that
there are no untimely deaths of sons. The usual
explanation for the greater number of males than
females in north India is the preference of males and
the suspected mistreatment of female children.
It is also possible that female children are under
numerated in censuses. One explanation does not
preclude the other and both may be involved. The
motive for most respondents for not being sterilized
was too few sons. On the other hand the expenses
of raising children was overwhelmingly the main
motive for undergoing sterilization. Couples also
frequently
cited the governmental
sterilization
campaign, principally its coercive aspects as reason
for the operation, and some people said that the
sterilization was needed in their cases because of
specific female health problems.
Sterilization
We knew of only one sterilized person in Shanti
Nagar before 1968, but from then on at least one
person was sterilized every year. When we took our
census in 1977-78, there were 68 sterilized persons,
both men and women, equivalent to 26% of the
women of childbearing age (15-45 years). Bv late
1983, there were 93 individuals. Sterilization has
run an uneven course. From 1968-74, 3.4 individuals
on the average were sterilized annually. Then came
the 21 months of the Emergency, and the average
number of persons who underwent sterilization
increased to about 20 per year. After the Emergency,
the figure returned to almost to the pre-Emergency
norm; from 1977 to late 1983, 4.7 persons were steri
lized per year. The big jump in sterilizations during
the Emergency was due to the strong campaign
mounted by the government, which was especially
effective with men holding government jobs. Most
of the men sterilized during the Emergency were in
governmental service.
T3
1
'J
9 "
fc
Wb'*^
..i] "
fl-
That parents seem to be especially concerned with
the expenses of childbearing calls attention to the value
of child labour in the rural areas where children work
on the family farm from an early age. Although
the value of their labour remains considerable, the
modernization of agriculture has generally reduced
the amount of child labour needed. Moreover
there has been an increase in employment opportuni
ties that require an educational qualifications. Under
these conditions, the maximum economic return
from a child involves an investment that most parents
cannot afford for a large family which combined with
the declining value of child labour puts pressure on
parents to terminate childbearing after fewer children
than would have been the case a decade or two earlier.
However, the cost of childbearing and the value of
child labour of children are not the only factors that
parents need to take into account when considering
sterilization. There is also the question of the econo
mic security that children provide and this one consi
deration may outweigh all the low-fertility motives
in the thinking of many parents.
Before 1977, men had 53 percent of the steriliza
tion operations. After the Emergency, this figure
dropped to 15%. This noteworthy change in the
proportion of men to women who undergo steriliza
tion is probably related principally to the introduction
of the surgical technique of laparoscopy, which has
become popular and has made female sterilization
easier, but there are probably other reasons as well.
An important post-Emergency development is the
lower age at which people are sterilized. Before the
end of the Emergency, the mean age of a woman
either at her own sterilization or that of her husband
was 33.2 years; after the Emergency, it was 29.1 years.
Correlated with the decline in the average age at
sterilization is a reduction in the average number of
children per sterilized couple. Couples sterilized
before or during Emergency had families of five living
children; people sterilized after the Emergency had
an average of 4.25 children.
The average sterilized
couple had about three sons and daughters, a sexual
disparity that appears to be. increasing. Until the
end of Emergency, sterilized couples had an average
of 1.4 sons to each daughter, but afterwards, they
averaged twice as many sons as daughters. It is
important to note that sterilization by itself cannot
influence the sex of children. However if either by
random chance or the mistreatment of female children,
a couple has more sons than daughters, sterilization
Respondents regarded all contraceptive measures
(condom, Copper T, loop or foam) except steriliza
tion as unreliable and/or dangerous. The majority
of sterilization took place within 10 months of the
couple’s last childbirth, that is, just before the end ’
of what one respondent called the “safe period”,
which is approximately 11-month post-partum amenorrhoeic period that accompanies breastfeeding
when there is no supplementary feeding of the infant.
Living children, Sterilization and Modernisation
The relationship of the number of living children,
sterilization and aspects of modernisation are investi
gated by multiple regression analysis, a commonly
3
-'.
'■■
■
w
I1 J;
-
docs not extend to family heads, another example
used statistical technique to establish a linear relation of the apparently inconsistent effects of the moderni
ship between a dependent variable and several inde
sation variables. There is also the possibility that
pendent variables. The dependent variables are the
the education of family heads may be positively
number of living children and sterilization. The
associated with sterilization although the connection
independent variables form two groups: the moderni is weak. The apparent lack of any significant rela
sation variables, namely urbanisation (defined as an tionship of either the woman’s education or that of
individual’s having lived and/or worked m a city her husband with sterilization would weaken the
some time during his/her life) and education as they
general inference of a general association of education
affect women, family heads and husbands; and the
and sterilization.
biological and traditional variables namely a woman s
age, caste rank, family land-ownership, and when
sterilization is the dependent variable, number of Size of compieted families and Childbearing span
1 '
j!
I ■
I
1
■3't
U drawnfrom tl^ analvsis^s that womens age and
0II
sterilization are the only two variables strongly related
!
.-.I i
I
I
■I
i-
E
gE j
I
I 1i
JHi
y
■
t
I
i
: •
p
Ii
Hl.
I
I
i
■i •
II
! I
■
c'’i
The average number of living children per mother
The average
of completed fertility, both sterilized and unstenl z
related is basically a truism; therefore, the strong
the children for all sterilized mothers and to 4.3 children
probabilities of a significant relationship in
i both
’
Tn
1950s and the 1970s are no surprise. Sterilization for mothers sterilized after the Emergency,
general, all mothers of completed fertility had a
and the number of surviving children are also positi
' ; 1970s than in the
vely related; when all other variables are held constant, fraction more living children in the
achieved
despite
a reduction of the
a sterilized couple has 1.28 more children than an 1950s, an increase
of about 2.9 years for all mothers:
JiMV ~a contraceptive
_____ x
unsterilized couple. That
measure childbearing span
,
the
number
of
living
children
f
rom
17.1
years
in
the 1950sjo ‘14.2~ years; in the 1970s.
is positively related to t,._ The
reduction
was
only 0.8 years for unsterilized
would appear to be a paradox weier it not for the fact
sterilized after having had a mothers but a substantial five years for unsterilized
that people decide to Ibe
--------certain number of children, especially sons. There mothers (from 17.1 to 12.1 years). Yet this impres
fore, a sterilized woman has more children than her sive lessening of the childbearing span resulted in
unsterilized counterpart when variables such as age only a slight decrease in the number of living children
per mother, a development which reflects in all likeli
are controlled.
hood a decline in the rate of infant and child morta
lity. That mothers appear able to squeeze four or
None of the modernisation variables has a signifi
five living children into a relatively brief childbearing
cant relationship with the number of living children. span would seem to suggest that to postpone the
The probabilities in the case of both women s ui anisa
marriage of women until the age of 19 or 20 years a
tion and the urbanisation of family heads are low
biit the effects of the two prospect that often arouses high hopes for popu a
^^01, might not significantly reduce the average
enough to attract
an.xi*'--*- attention,
------- —, but the effects .o .
variables are not consistent; the relationship is posi number of surviving children by the end of a woman s
tive for women’s urbanisation and negative foi the
urbanisation of family heads. The inconsistent childbearing span.
effect of the urbanisation illustrates a noteworthy
feature, aside from the insignificant probabilities of Remarks
the modernisation variables: they do not always show
At the present time, sterilization is the only method
consistent effects where one would expect to find them.
acceptable to the people of Shanti Nagar that can
check a rapid population increase. However in th
When sterilization is taken as the dependent nost-Emergency period, only about five persons per
variable, we find a strong positive association between year chose to be sterilized and sterilized couples
it and the number of a mother’s living children. continued to have an average of between four and five
There is also a significant positive relationship between children, a number necessary for the protection and
sterilization and the urbanisation of husbands a support of parents in their old age. Couples general y
connection that is probably valid because men classified look to their own interests when deoding whether to
as urbanised almost always held city employment, be sterilized and how many children to have before
frequently in government, and were therefore especially doing so. Their self-interest may sometmte conflict
vulnerable to the sterilization campaign. However, with the best interests of the society, a conflict that is
the relationship of urbanisation and sterilization
■
1
gjlllh
4
_____
----------------------------
________ __
■
<^g
C3
i
::
■S
<r
I
!•
I
□
^3
J
&
S3
Is
Bo
'j
^ften termed the ‘isolation paradox’ or the ‘tragedy
of the commons’, the point of which is that sometimes
what is good for the individual is bad for the society.
In the case of sterilization, a vasectomy or a tubectomy
after four or five children, which from society’s point
of view is belter than no operation at all, will still
allow a rate of population growth that will be tolerable
only in the near term. The discrepancy between
governmental family planning programme, which
urges that families be limited to no more than two or
three children, and individual family planning, which
often requires four or five children, is sometimes
overlooked in evaluating the potential effects on
population growth of increasing number of people
who “accept family planning”.
,a 1
* J
□ ..
5
3.
Sis
SOI
1^3
4- c>' 9
NO 17.^, I CM
On the basis of the Shanti Nagar data, one may
cautiously suggest that indirect effects to control
population through aspects of modernisation such
as enhanced education and urbanisation cannot be
expected to contribute significantly to fertility control,
at least in the short term. The modernisation vari
ables used in this analysis do not seem to be correlated
consistently with reduced fertility. The education
of females is perhaps an exception, but its effects is
relatively weak until women reach a rather high
educational. standard, generally the college level,
and a college education is currently beyond the reach
of most rural women. The urbanisation and educa• tion of husbands and family heads are in general
positively related to sterilization but this relationship
largely derives from Government of India policies
during the Emergency and may not characterise the
post-Emergency period of entirely voluntary steriliza
tion to the same extent.
Needed—A Transfusion
Dear Reader,
Last month, while posting the bulletins, I made
the shocking discovery’ that we have barely 350
subscribers! With growing suspicion, I opened the
account book, and had anothep^hock! No money
to pay the printers for the/next issues. A quick
calculation revealed that we need a minimum of 1000
subscribers to cover the basic expenses; each issue
costs Rs 1.60 to print and there is the added expense
of postage. This^.works out to be more than the
annual subscriptron. Apart from the finacial ^prob
lem, I am sure you will agree that it is a question of
the good (^Fd ‘honour’ — no self-respectipg bulletin .
would like to admit that it has sor few subscribers.4
/
So kindly put on your chappals or whatever and
go forth into the wide world/(or at least up to the
medical college, or hospita/in your area) and collect
a minimum of FIVE subscriptions each (I am not
being greedy, just bein^ practical). This, I am sure,
will not be too difil^flt because in India we produce
something like 12,000 doctors and 8000 nurses per.
year; and of the. NGOs, one has lost count. (Where
are they?) I Expect to be flooded with money orders
in the coming months, otherwise we will have to sink
without a*gurgle.
You]/(clutching at the last straw),
Editor/Publisher
Despite the declining birth rate and the increase
in contraception, it is unlikely that the problem of
population growth has been solved. Many rural
couples feel insecure with fewer than two sons, which
means that the ultimate governmental goal of the
two child family makes no sense to most rural people.
Even if there were a national comprehensive system
of old age social security, many, if not most, rural
people would still not believe that anyone but their
sons would take care of them when they grow old.
Their experience has been that government and poli
cies change too frequently to be trusted in the long
term. Families of four or five children may be larger
than many people want but these same people may
nonetheless believe that they are necessary in view of
existing circumstances. Thus, the number of children
left alive at the end of the average women’s childbear-
■’■S'
&
=0®
ing span will in all probability provide greater insight
into India’s demographic future, than the drop of a
few points in the birth rate or a slight increase in the
number of people who are said to accept family
planning. If parity at completed childbearing were
to stabilise, at between four and five children, India
would continue to live up to its reputation as a
demographic juggernaut.
(For Notes and References see original article in the
Economic and Political Weekly).
JI
w
’f? k;';‘''v
aj>! j'
Bl*
I
II''
‘'I
1
li!i
5
<©
I
III
’’: ’
■
1
121
medico friend
circle
bulletin
OCTOBER 1986
A Feminist Understanding of Contraception
(Manisha Gupte)
Few topics related to the women’s health movement
are as controversial as is contraception. Liberating
heterosexual women at one end by giving them the
choice to control their own reproduction, it snatches
away the same control when contraceptives, many of
them invasive and harmful, come as a package deal
with population control programmes that select,
motivate and whenever necessary coerce helpless
targets. Male hegemony exists in medicine, in policy
and decision making and in research. Do women end
up having lesser choice and lesser control over their
bodies through the usage of existing contraceptives?
what designs operate to keep control of women’s
bodies out of the latter’s hands? And is there a solu
tion?
To understand the above, it becomes necessary to
clarify our own position regarding contraception.
It is particularly important to do so when we are faced
with the possibility that injectable contraceptives may
be officially introduced into the Indian government’s
family planning programme. Whereas our light
should be directed against all contraceptives that arc
invasive, harmful and which have systemic effects,
• at this moment it is necessary to concentrate our
efforts to examine injectable contraceptives vis a vis
the personal choice of a woman regarding contracep
tion.
The present paper, based largely on existing in
formation, attempts to bring forward some views re
garding contraception, the choice that women are
able or unable to exercise when confronted with unsafe
contraceptives within a target oriented, coercive popu
lation control programme.
Feminism and Contraception :
As regards contraception, one argument put
forward is that while it does help a woman to avoid
conception the availability of contraceptives has made
women ‘sexually available’ for men. The argument
has been especially true in the context of our Western
sisters and the recent works of Germaine Greer and
Betty Friedan bear testimony to the fact that the sexual
revolution of the West, did infact oppress women
themselves. The same argument is put forward in
India by well meaning persons about the abortion
issue. What they want to stress upon and to warn is
that once contraceptives are available, men become
more irresponsible in their sexual relation with wo
men, since then a woman’s sexual availability can be
separated from unwanted conception and the accompa
nying guilt and responsibilities. In the event that con
ceptions do occur, the woman then is made to go
through repeated abortions, much against her will
and her physical well being. The position of these
protagonists is in principle quite different from that
of the moralists who see sexuality without conception
as evil, especially if it occurs outside marriage, and who
consider accidental pregnancy ensuing out of such a
relation as a well deserved punishment.
Let us examine this position and its consequences.
In fact, one might raise a counter question in argument.
Are we trying to say that if contraceptives were not
made available, women too would no longer be
‘available’ for sexual purposes? In such a situation,
what would be our analysis? The fact is that partri
archy is powerful and all pervading. It adapts itself
to almost every situation with incredible ease. Infact
it has the power to mould situations, even progressive
i
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
I
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form. The
filled in form may please be sent tos
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark's Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team.
Yours sincerely,
for DAF-Karnataka.
Gopal Dabade
Tn
'
and radical, for newer forms of oppression. It existed
in feudal society, it functions hand in hand with
capitalism; what is even more depressing is that it
has also not been driven out of post revolutionary
societies, nor from left movements. It should not
surprise anybody therclore if it exploited the sexual
revolution of the West or the availability of contracep
tives in general.
Our fight therefore has to be directed against the
real enemy. Patriarchy that oppresses us, degrades
us to being sexual objects, that refuses to accept
responsibility of conception and child rearing and
which overtakes any move by us to gain control of our
own bodies. Withdrawal of legalised abortion or of
contraception would in result be no different from what
rightist moralists would desire in complacent glee: a
further punishment for women. If we accept the fact
• that a woman is not free sexually, then to take away
her defence mechanisms would amount to victim
blaming.
Within marriage, the "availability’ of the wife for
sexual gratification in elation to the contraception
issue raises delicate questions. Similar to the argu
ment raised earlier, does a wife become a sexual slave
only when the couple practices contraception? The
reality of the sexual righ ts of a husband is more deep
than is contraception. Restitution of conjugal rights
is one such issue that encroaches on to the human
rights of the wife. In the Hindu family, the wife
cannot raise the issue of rape within marriage, because
according to the law she has given her consent once
and for all during the marriage ceremony, itself.
Legal cases have been filed by husbands when the wife
has refused to bear children. Where does contracep
tion figure in these cases?
have the freedom to control their own reproduction,
within or without marriage.
From this point, emerges another hotly debated
issue: is contraception solely the responsibility of the
woman? It is clearly not so, and we have to constant
ly question as to why there is more research into
contraceptives for women as compared to those for
men, why women are the more favoured target group
in population control programmes and why unsafe
and invasive contraceptives are being dumped onto
women. Ideally, contraception should be shared
equally by the couple and significantly, the natural
family planning method which is the safest method of
contraception demands such mutual cooperation and
understanding. The man respects the women’s de
mand against conception and actively cooperates.
Here, however, we are referring to the man who hand
les an intimate relationship with some amount of
responsibility. He may well be exception to the rule.
In Bombay city alone the officially registered MTPs
in a single year were around 50,000 besides many
more that go unregistered, (Karkal, 1985) proving
that there were atleast so many unwanted pregnancie|^
in one city in one year.
The point one is trying to make is that while wM
are aware that contraception is shared responsibilitjB
in the absence of a pro-women milieu, avoiding uuH
wanted conceptions through contraception bccomeB
the woman’s last line of defence.
B
Is
there
a
choice?
I
If contraception is liberating because it allows I
woman to control her own fertility, existing contracepl
tives tell a sad tale. Contraceptive choice today i|
not determined so much.by the woman in questionl
The woman’s choice and control over her own but by designs that are beyond her control. Thesl
designs work at national and international levelsl
sexuality would more often be much reduced within
marriage. Each time she goes through an unwanted namely the government’s policy regarding population
control and the interests of multinational companies!
sexual experience, she may not be actually ‘raped’,
The interests of the latter become clear when onl
often, the consequences of not sleeping with her hus
realises the tremendous potential market that they havl
band may far outweigh the consequences of having
in healthy women all over the world. Three to fivl
slept with him. She may be threatened with insecu
rity, with the accusation of not fulfilling her conjugal million women in seventy countries were on depi
provera alone, in 1978 (Corfman, 1978). Accordinl
duties, of frigidity and in dire circumstances with
to the 1981 Census of India, 43.4% of all women arl
desertion. In such a situation, infact contraception
comes to the rescue of a woman: she can at least hold in the reproductive age group and of these 80.48
are married. That makes for 11.6 crores of married
on to one end of the rope, however feebly.
women in the reproductive age group only on thd
One is definitely not making a case that wives and Indian subcontinent. Since injectables are to bd
women in general are sexless and that everytime they used as a spacing method, all of these women becomd
undergo a heterosexual experience, they are doing potential targets at least once in their lifetimes.
I
it against their own will, only to gratify the man.
It is therefore easy to understand the direct anc
Of course not. Women can and should express their
indirect
involvement of drug manufacturers in research
sexuality in their own right. And yet, they should
2
^1
related to long acting contraceptives and the implicit
biasP underlying all these research studies. Even
‘prestigious’ international bodies such as the Inter
national Planned Parenthood Federation (IPPF)
describes all injectable contraceptives as a ‘most
dependable and useful method of family planning
(IPPF, 1978). Contraceptive technology is more
under the control of multinationals than it is with
women. Delivery of contraceptives may lie with
women, as it does in Britain oi in India, but this in
itself does not mean that decision making or the power
to decide on a particular contraceptive on a macro
level lies with women. Miale hegemony exists and
contraception therefore remains an area where all
heterosexual women are disadvantaged by a limited
choice. (Roberts, 1981). Moreover, the medical
establishment is male dominated and much worse,
women are made to fit into male defined categories.
It is with this preconceived bias that the medical esta
blishment sees our menstrual problems. Since our
gynaecological disorders arc termed as ‘psychosoma
tic’ there is little understanding for menstrual chaos,
pain or other psychological disorders that invasive
contraceptives induce inside our bodies.
shot of DP without her knowledge when she was
under general anaesthesia for abortion (Rakasen,
■
'
■’
a
1981). Social workers from Scotland
report that
young girl was giveni a shot of DP, disguised as a
glucose injection. In Britain, Asian women in their
__ rpartum
_____ are
routinely given a DP shot along
post
period
with^the rubella vaccine, without any consideration
for the child that would absorb the hormonal drug
whilst breastfeeding.
The above examples are only the tip of the iceberg.
They are vivid because one can clearly see how choice
is snatched from us, throughabuse of the injectable,
but the general picture would be more subtle. Th
roughout the world, especially in the developing
countries, injectables would be pushed for the sake of
convenience’. The question is: whose convenience?
When the woman in question cannot decide which
contraceptive she must use, ‘informed consent is
actually telling half-truths and when she cannot cont
rol the long term sequelae of the systemic and hormo
nal effects on her body, it is inhuman to speak of
‘convenience’. Infact, it is the convenience of the
drug companies and the dons of population control
that is being considered, so that this dangerous hoi mo
The findings of many of the reasearch studies are nal preparation can be administered to ‘ignorant and
questionable. In field trial studies, the necessary irresponsible’ women.
physical examination is not always performed on
women because it would discourage a woman to
continue to participate in the study and would References:
give FP a bad name at the village level (Balasubrah
manyan, 1981). No long term follow up is also
_ •
* ’
, Vi mat ‘After the Pill’
1. Balasubrahmanyan,
conducted. On what basis theh are claims of safety
Maintream, Vol. XX No. 13, Nov. 1981
made? Hormones can cause long term havoc, there
fore women taking hormonal contraceptives have to
2. Corfman, P.A., Evidence to US Select Com
be monitored for years. Not only they but in the
mittee Hearings on Population, US. House of
event that they used these drugs in the post partum
Representative, 1978 (quoted by Jill Rakusen,
period, their children too have to be watched
1981)
until the latter reach puberty. In this context, our
fight has also to be directed against the Pill and all
3. International Planned Parenthood Federation
contraceptive preparations that cause hormonal and
‘Factsheets’ on Depo-provera.
systemic effects. Our concentrated effort against the
introduction of injectables, however is more because
4. Karkal Malini, Science Age, 1985 (Informa
least control over our own bodies is possible with
tion Collected through personal communica
long acting contraceptives, the dangerous effects of
tion).
which we cannot remedy by immediate withdrawal and
the higher potential of abuse that is related with
5. Rakusen, Jill, Dcpo-provera: thee xtent of the
injectables.
problem. A case study in the politics of birth
control (in) Women, Health and Reproduction
Ed. Helen Roberts, Routledge and Kegan
Paul, 1981.
Long acting contraceptives, especially injectables
?re very important where the question of choice is
concerned. The ‘value’ ol injectables, as the pioponents of PC see, lies exactly in the fact that it steals
choice from women into the hands of male hegemony.
A fourteen year old black girl from London was given
6. Roberts, Helen, Male hegemony in family plan
ning (in above book)
3
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent tos
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark's Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team.
Yours sincerely,
for DAF-Karnataka,
Gopal Dabade
To
113
medico friend
circle
bulletin
<»
MAY
INJECTABLE
1985
<4 (V)
CONTRACEPTIVES
Injectable contraceptives (ICs) have been on
the pharmaceutical map of the world since the ear
ly ‘sixties. Ever since then they have been at the
storm centre of a controversy that may well be the
longest ever on a medical issue. Two countries,
USA and UK have appointed public enquiry com
mittees on the matter.
In India, the ICs controversy was of largely
academic debate until about six mlonths ago when
the government issued a directive permitting the
import of NET-EN, one of the ICs. Around the
same time it was also decided to introduce the IC
as one of the cafeteria methods offered in the govern
ment Family Planning Clinics.
The ICs controversy has raised some fundamen
tal issues — the manner in which decisions which
affect thousands of people are taken; the ethics of
medical research and control and the more funda
mental problem of appropriate animal models for
the testing of drugs. It also brings into focus once
again, the role of the multinational drug companies
in pushing potentially harmful drugs in the third
world with the active participation of the con
cerned governments.
ICs are hormonal contraceptives which may be
administered in the form of once in 60 or 84 day
injections. They are synthetic progestogens. The
two currently available ICs are Depot medroxyprogestogen acetate (brand name Depo) Provera)
and Norethisterone enanthate or NET-EN (brand)
name Norigest) While they are both synthetic pro
gestogens they belong to
different
groups
of
steriods.
These synthetic progestagens
inhibit the production of gonadotropin which
in turn prevents ovulation. The endometrium
and the fallopian tubes are also perhaps affected
contributing to a reduction in fertility.
Depo Provera has currently been approved for
use in 84 countries whilst NET-EN is ‘-registered’
for use in 25 countries but approved for use in 40.
It is neither registered nor used in UK or the US
(War on Want, 1984).
The Depo Provera Board of Inquiry in the US
has strongly recommended to the FDA that the
drug sould not be licensed as a contraceptive. In
UK however, the Board of Inquiry has cautiously
permitted the use of ICs in cases where other
methods are unsuitable. In India Depo Provera is
not allowed to be imported. However, it is not
banned dither.
Since Depo Provera has been in use much
longer, much more research material is available
on this than on NET-EN. Although they are diff
erent steriods, it is possible to examine some of
these findings with reference to
NET-EN.
Toxicological
studies
have been
carried
out in accordance with the requirements of
the US FDA. These results have been monitored by
the WHO Toxicological Review Panel periodically.
The drugs have been tested on rodents, beagle
dogs and rhesus monkeys. The Depo Provera ani
mal studies have come in for a lot of criticism. Ste
phen Minkin a former Nutrition Chief of the UNI
CEF project in Bangladesh
first
revealed
that Upjohn, Depo Provera’s manufacturer had not
in fact reported all the findings of their trial on
beagle dogs. The 7-year studies on beagle dogs had
shown that mammary gland nodules developed in
ad those .animals which survived beyond the first
few years and some of these were malignant.
Another finding was acromegaly
or an abnormal
growth process. Ten-year monkey studies have also
been conducted using DP. Again mammary nodules
developed in the low-dose groups.
Endometrial
carcinoma was also observed in some of the mon
keys. (WHO, 1982). Minkin further reports that
curvature of th© spine was also found in experi
mental animals, which is a possible indicator that
Depo Provera inhibits growth hormones.
Depo Provera has been tried out in India, by
the ICMR, but reports have never been available.
There are two major NET-EN studies — both coordi
nated by the WHO. The first was a two-year multi
national comparative trial of three regimens of DP
given at 90 days interval, NET-EN at 60 day inter
vals, and 84 days interval. Over 3000 women parti
cipated in the trials which began with recruitments
in 1977 and the final follow-up in 1982 (WHO^
1983). The other multicentre trial was conducted
in India by the ICMR in 16 Human Reproduction
Research Centres. This study compared two regi
mens of NET-EN of one 200 mg injection at 60
days and 90 days. Over 2000 women participated in
this study which ended its first phase in October
1983. (ICMR, undated).
The NET-EN studies have not however shown
the same results. The beagle dog studies have
shown that the drug may be inhibiting or affecting
carbohydrate metabolism. One case of endometrial
cancer was reported in the monkey studies. The
WHO Toxicology Review Panel, after a thorough ex
amination of the results came to the following
conclusions — (i) that beagle dogs were considered
an unsuitable toxicological moder for the study of
progestogens; (ii) that the tumours in DP admini
stered monkeys arose from a cell type not found in
women and so could not be considered to indicate
increased risk for cancer. (WHO, 1982).
A common feature of both the studies is the
very high drop out rates, most of which were due to
menstrual irregulaities. In the 1977 WHO trial the
drop out rate per 100 women ranges from 59 to 89
and in the Indian study about 50 per 100. Menstrual
irregularities included amenorrhoea, excessive bleed
ing, and spotting. In the WHO study 40 percent of
the women suffered from amenorrhoea of more than
90 days.
Late last year the USFDA’s Board of Inquiry
has categorically countered both these contentions
of the WHO Panel. It has stated that “Data from
th© studies on the rhesus monkey and -beagle dogs
cannot be dismissed as irrelevant to the hum^n with
out conclusive evidence to the contrary. Such evi
dence is not available at this time. Therefore, the
fact that malignant neoplasias developed in two
species in target organs of sex steriods must be con
sidered as an indication of the potential of progestojgens, including DMPA, to promote the develop
ment of malignancies in target organs.” (Report of
Public Board of Inquiry, (1984) .
Th© 1982 WHO document has specifically
noted that menstrual irregularities are not likely
to be a major health problem'. There is really no
'scientific evidence to back this up! Very little is
known about the mechanism of bleeding disturbance
especially those related to steroid contraceptives
(WHO 1982). This being so, it is rather curious
(that the Indian decision to introduce the IC into
the family planning programme should have come
after the study results were known. One apparently
facetious argument that is being used is that since
Indian women are in any case anaemic, amenorr
hoea would in fact help them in the long run. A
similar argument is forwarded for another of the
side effects, weight gain. In the light of how
little is known about menstrual irregularities, such
If one were to accept the WHO conclusions on
the unsuitability of beagle dogs as toxicological
models for progestogens, then obviously the animal
studies data becomes invalid. If this is so, on what
basis are human trials, which can only follow upon
animal trials, being conducted?.
Huniian Trials
There
are
volumes of
literature
on
the Depo Provera human trials. One of the ‘pio
neers’ jn the use of Depo Provera was E. MacDaniel
who tried out the drug on thousands of Thai women.
These studies have come in for a lot of criticism.
The US Board, of Inquiry has stated that the data
on humans is insufficient and inadequate to either
confirm or refute the animal study results (Report
of Board of Inquiry. 1984.) It has pointed out that
in a majority of the studies there were no controls,
nor is there sufficient background infcrmiation on
which one may decide on the possible carcinogenic
risk. Moreover the Thai trials have also been critici
sed on ethical grounds—‘informed consent’ was no
where practiced.
2
M 0 112 ,
IC’s become part of the ‘cafeteria’ approach, in
formation will be at a greater premium because then
there will be no need to ‘persuade’ the subject so
as to get a adequate sample for research. The
manner in which ICs have been introduced smacks
of indecent haste. For one thing, although the ICMR study was completed by October ‘83, no report
was forthcoming until recently. In fact the first
published article seems to have appeared not in an
ICMR publication but as an article in a specialised
journal to which few non-research oriented institu
tions have access—Contraception. It may of course
be argued that since there has never been a tradi
tion of debate on scientific and medical issues in
the country, why should ICMR have acted any
differently. And that is in fact the major issue
here. — that people have a right to decide whether
or not they would like to take the risks that are
today being thrust upon them.
arguments coming from ‘experts’ in the field must
be roundly condemned as being thoroughly unscienti
fic.
It is also rather disturbing to note that a 24month study should be deemed sufficient to prove
the drug’s safety when it is known to be a possible
carcinogen. Another area which has been ignored is
the possible teratogenic effects of ICs. The child
may be exposed to the drug if the mother’s pregn
ancy is undiagnosed when the contraceptive is adiministered.
Experts have stated that there is a positive
and significant association between progestins and
birth defects (War on Want, 1984). There have
been hardly any well-designed follow-up
of
children who might have been exposed to the drug.
Contraception failure may also lead to exposure of
the foetus to progestogens. In the two studies cit
ed contraception failure occured in 0.4 to 1.4 wo
men per 100 women (WHO, 1983). While this
seems like a small proportion, the total numbers are
likely to be large when ICs are being given through
the family planning clinics. Another factor to be
considered here is the effect of progestogen’s on
breast fed infants. According to file WHO report
a breast fed infant of a mother on NET-EN would
receive about 0.05 per cent of the maternal dose
over a two-month interval. (WHO, 1982). It has
been reported that even this small amount may
prove harmful because (i) the bfaan is not fully
developed and is sensitive to hormones and (ii) the
immature liver and the consequent slower elimina
tion may lead to a high accumulation of the hor
mone in the blood. (War on Want, 1984). When
so Tittle is known in this area, is it ethical to
introduce this contraceptive in the national family
planning programme.
Padma Prakash, Bombay.
REFERENCES:
The I'CMR has outlined a set of guidelines for
family planning clinics regarding the use of ICs
(GOI, undated). These are very similar to the WHO
guidelines and include criteria for selection, pre
examinations to exclude cancer of the breasts and
genital cancers, undiagnosed abnormal uterine bleed
ing and so on. Given the overcrowded understaffed
family planning clinics how much time would the
doctor be able to devote to the potential IC user.?
As reported earlier the government has now
allowed the import of NET-EN by private practi
tioners, nursing 'homes etc. And yet there is no
mechanismi to ensure that the guidelines are follo
wed. Moreover, ICs have a great potential for
misuse. For instance, in UK, women in some hos
pitals were refused rubella vaccine unless they ac
cepted DP (Campaign against Depo Provera).
Closer home in Bhopal, women are not being allow
ed to have MTPs unless they accept copper T’s.
This perhaps is the most frightening aspect of the
whole situation. Women will loose whatever
little control they had over contraception. There
is plenty of evidence that even during the trial
phase, ‘informled consent’ was only a myth. When
1.
War on Want, Norethisterone enanthate, Dec.
1984. UK.
2.
WHO, Multinational comparative clinical Tri
als on Long-Acting Injectable Contraceptives:
NET-EN given in two dosage regimens and
Depot MedroXy Progesterone Acetate. Final
Report Contraception, July 1983.
3.
WHO, Facts about Injectable Contraceptives,
Memorandum from a WHO meeting, Bulletin
of the WHO 60 (2; : 199-210 (1982).
4.
GOI, Guidelines for use of NET-EN, an Inje
ctable contraceptive for its use in Govt and non
Govt FP. Clinics, Undated 1984.
5.
Report of the Public Board of Enquiry on Depo
Provera, Weisz Chairperson, Ross GT and
Stolley PD. 1984 Oct.
6.
ICMR, Comparative Evaluation of contracep
tive efficacy of NET-EN (200 mg) injectable
contraceptive given every two or three months.
Mimeo, undated.
7.
Campaign against Depo Provera UK, 1984.
I
3
- -
IM
i
HibrJ
't. hH; ->
I
The E P Case
T’
j -
F
i-
High dose combination of Oestrogen and
Progesterone has finally been banned. It is tragic
that the public had to fight for 6 long years for
getting a hazardous drug combination banned, that
Questions were raised in the Parliament,
repeated requests were made to the Health Ministry
and Chemical Ministry to make attempts at getting
too against all odds.
In the words of Supreme Court Justice
probably the government never Wished to vacate the
stay; this became obvious because the subsequent
events are pointers to scheming.
It was the socially conscious health activists
and consumers bodies that had initially raised the
issue in the first place, when the EP campaign was
launched way back in 1982 on Women’s Day on 8th
March. Due credit goes to the press for keeping
the issue alive all these years and supporting the
JI
Sa
J
stand of the people.
fc-
It was the drug health and consumer groups
who protested when on 21st July 1982, the ban order
for manufacture was given as December 1982 and
ban for sales as June 1983.
How could a drug
recognized as hazardous be allowed to be manufact
ured and then sold for almost another one year ?
It was not surprising v/hen this was misused by the
manufacturers to challenge the hazardous nature
of the drug, saying that if the drug was hazardous
wouldn’t it have been banned immediately by the
DC authorities and since it wasn‘t - it was obvi
-a
ously non hazardous !
.j
3
J ’
J
|
-5
J.’’
The Legal Battle
' A*
i 2
T
1
1
I
i 7
i i
■i 7?
Tv
T 7^
I
;|
•V
Mira Shiva
The drug companies were quick enough to
find the legal loopholes and the stay order against
the ban order was obtained from the Calcutta and
Bombay High Courts on
legal technicalities.
The fact that it involved a hazardous drug which
could maim and cripple the unborn foetus when
consumed by ignorant pregnant women, —did not
appear
to be a matter worth considering,
Even making an attempt to find out the number of
women put at risk, with annual sales of Rs. 7 crore
worth of drugs (majority of them are consu
med for pregnancy tests and for induction of
abortion though on paper the indications permitted
had been only for secondary amenoorrhea) was
not done.
the stay vacated.
• r
I
■
Again it was due to a writ petition that
Supreme Court took up the issue again. Justice
Ranganath Mishra‘s comments on banning of
drugs is a telling commentry .
“This court as early as 11.4.1983
directed issue of notice to the Medical Council
of India, The Indian Medical Association,
The Drugs Medical Council of India, The In
dian Medical Association & The Drugs Control
Authorities of the States except that of Kerala,
Ii
as it was already made a respondent to the
writ petition. Obviously such notice was given
as in the opinion of the Court, the matter was
one of great importance and the Court looked
for participation of these authorities in the
debate with a view to assisting. the Court in
the disposal of the matter. ,We are surprised
that the notice from the Court has not evoked
response excepting the State of Karnataka,.
Statutory bodies when called upon by a Court,
in particular the apex Court of the Country, are
duty-bound to respond and join the proceedings
before the Court. These bodies are not litig
ants and do not have the choice of keeping
away from the Court like private parties in
ordinary litigations opting to go ex-partc. The
present matter is certainly one which is suffici
ently important and the stake of the entire
nation is high; when the Court SUO moto
extended the opportunity of being heard and
invited the named statutory or other authori
ties to come forward and place their view
7
j
points cn relevant aspects, an attitude of
,--r’'C>allous indifference cannot be appreciated.
We hope and trust that there would be no
repetition of such a situation'.
The Public Hearings
(’
It was unfortunate for public that the
public litigation case was referred back to the Drug
Controller of India. In its Court Order of Novem
ber 1986 Supreme Court gave direction to hold
public hearings to seek the views of consumers and
health groups and decision be taken by end of July
1987. The drug companies were shrewed enough to
use the professional bodies like FOGSI (Federation
of Obstetrics Gynaecology Society of India) to be
their spokesman . FOGSI till the very end continued
to support the stand of the Drug manufacturers
stating that the drug was essential and absolutely
safe. Luminaries such as Dr. C. L. Jhaveri, Dr. C.
S. Dawn, Dr. B. N. Purandare did their utmost to
tilt the balance in favour of the manufacturers. The
role of the WHO expert and the Deputy Drug
Controller who chaired the Calcutta hearing was
not very creditable.
The silence of professional and academic
bodies such as IMA, IMC. at such a time was
unforgivable. It was only the Indian Academy of
Paediatrics that had expressed its deep concern
against the continued sales of high dose E. P. drugs.
The public hearing in Bombay ably proved that
when called upon, the women's organisations can
give a bitter fight fora cause. Even the public
notices for the public hearings were inserted inconspiciously in the papers, the hearings were stated
to be for “formulations of oestrogens and progest
erone”, in the first public notice and “combination
of oestrogen and progesterone” for the second one.
The failure to clearly state that the public hearings
were being held to decide whether or not to ban
combination of high dose Estrogen-Progesterone, was
too significant to be overlooked as an unintended
errors. The way the 4 public hearings in Madras,
Delhi, Calcutta and Bombay were held on Sth Feb.f
10th April, 10th July and 14th July 1987 respectively
is a story in itself. Even when the Drug Technical
Advisory Board met in May 1988, the minutes of
the 4 public hearings were not made available, nor
the summary of the arguments for and against the
drug ban was sent to Boards members for prior in
formation. The fact that it took 6 long years to issue
a Gazette Notification to ban a drug - shows the
forces working on it. A drug, which is known to be
hazardous — which has been mainly used in pre
gnancy - a drug which was banned by the Drug
Controller of India himself in 1982 - a drug which
ICMR strongly recommended to be banned in 1982
as well as in 1987 - a drug which was not allowed
to be registered or sold in the parent country
Netherlands by Organon Infar. was strongly con
tested by drug manufacturers and they had the aud
acity to challenge the DCTs ban order in India.
Enforce the ban immeditely
The EP case involved a drug which the con
temporary Gynaecological medical literature does not
even mention, as it has no role-and as it is not us
ed by any gynaecologist or a doctor, as safer alter
natives exist. Not merely bad several drug regulatory
authorities banned the drug, but several companies
bad withdrawn the product themselves. It was due
to sheer gist and perseverance of the drug activists,
health and consumer groups that the ban order has
come now. Should this be counted as success ?
We have learnt from past experience that
unenforced drug bans are as bad as no bans. The
Gazette Notification was issued on 15th July 1988.
Government media of AIR and Doordarshan should
have been used to inform the chemists, medical pro
fessionals and the ignorant consumers about the drug
clearly stating the brands and their manufacturers !
The Drug Control Authorities owe this to the nation.
The stocks from the manufacturers and the market
should be withdrawn and destroyed.
The Health Ministry has had 6 long years to
make available to the medical professionals the reco
mmended alternatives. Safe, low cost simple pregna
ncy tests, which basic health workers can use, should
be easily available as part of Mother and Child He
alth Programme. Permitting at this stage the manu
facturer and sales of high dose EP drugs as single
ingredients in the same dose would be ridiculing and
sabotaging the ban. The ban h^s come 6 years too
late; now the implementation of the ban muit be
immediate. The Drug Control Authorities and the
manufacturers must be held responsible if these
drugs continue to be sold. If this could happen for
a drug like high dose EP which the consumers and
health groups considered a watertight case-what wo
uld be the fate of other many hazardous drugs ?
Let the government and Drug Controller of India
announce how they are going to make the ban effec
tive.
® ®
8
■'
medico 'friend
124 circle
bulletin vi'9
" . X
■ ■
■
■■
..
JANUARY 1987
Use and Abuse of Bio-Medical Technology
(Amniocentesis-A Case Study)—Amar Jessani
Prenatal testing to determine sex of foetus has
recently created a big uproar in India. Two Bombay
based organisations-the Forum Against Sex Deter
mination and Sex Preselection and the Doctors Against
Sex Determination and Sex Preselection-with the
support of other like-minded women’s and health
organisations all over India are spearheading the
campaign against this nefarious medical service to the
extreme patriarchal practice of selecting the male
offsprings and eliminating the female ones. In a
short time span these organisations have fairly succee
ded in creating a sizeable informed public opinion by
organising a scries of demonstrations, dharanas,
meetings, workshops etc. and by writing and giving
interviews in the English as well as the vernacular
press. Many of the members and sympathisers
of the Medico Friend Circle in Bombay are
actively participating in these efforts. The pressure
created by this campaign has started having its effect
even at government level. A private members’ bill,
sponsored by the opposition as well as the ruling party
MLAs has been introduced in the Maharashtra
Assembly.
The bill is for enacting a new law to
comprehensively ban sex determination at the prenatal
stage using any medical technique. It does not ask
for the ban on the prena-.al medical techniques as such
but demands that the use of such techniques should be
restricted to the detection of medically recognised
foetal abnormalities, and even in such use, the sex of
the foetus should not be communicated to anybody
either directly or indirectly. The Union Govt, has
also issued statements saying that it does not approve
of female foeticide. And lastly, in response to all
such pressures, the Maharashtra Govt, has appointed
a committee under the chairpersonship of the State
Health Minister to make recommendations to the
Government in this matter. Significantly, several
members of the Forum and the Doctors are appointed
on this committee providing an opportunity to these
organisations for proposing comprehensive measures
to ban the use of medical technology for prenatal sex
determination.
Response of established medical profession:
The established professional. bodies of doctors
initially pretended to be totally unconcerned about the
debate on the doctors’ collusion in female foeticide.
But the campaign soon made inroads into their do
main as it started gathering support of socially con
scious doctors. Further, the campaigners, instead of
going for sensationalism, came out with well research
ed information on the extensive use of these techni
ques not only in the big cities like Bombay, but also in
the smaller towns all over Maharashtra and other
states. Thus, the spokespersons of these professional
bodies were driven into open debate. The points they
raised in support of the practices of sex-preselection
and sex determination require serious examination as
the ideological basis of such arguments, has wider
ramifications.
First let us enumerate some of their points: (1)
Many doctors feel that it is none of their concern and
at best, it is a social issue (2) The techniques employed
for sex-determination are less dangerous or hazardous
than the danger involved in crossing roads in urban
centres. (3) They are catering to the psycho-social
needs of people by making known the sex of the child
and allowing the people to make their own choice
(4) Main culprits; are people who go for abortion of the
female foetus. That is, society is at fault, not the
doctors. (5) Social activists should direct their fire
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K, had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent to?
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark's Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team,
Yours sincerely,
for DAF-Kamataka.
Gopal Dabade
Tr>
medical angle.
at the ,society, its traditions, customs and values, and
not on the medical profession which is making an
effort to cater to the needs of the people as cheaply and
as safely as possible. (6) Well, it may be a bad thing to
do, but people are justified in desiring a son after 3 or
4 daughters. (7) Some crude spokesperson justify it
in the name of helping population control progra
mmes of the government. (8) As such women are
maltreated, deprived of nourishment, suffer more
from diseases and burnt alive for dowry and so on.
Not allowing them to come in this world to suffer
such indignities is a human service to the women.
(9) Lastly, this is more vociferous, the govt, has al
ready legalised foetal killing by liberalising abortions.
If such foetal killing is ethical, why not female foeti
cide? Thus, if sex determination is to be banned,
then abortion should be banned, too.
Yet, they danot seern^o recognise it
precisely because as professionals they directly or
indirectly regard themselves quite apart from the
society in general. Thus they say that it is society
which is at fault and not they. If society allows one
practice (here abortion) another will follow (s,ex
determination). Such arguments can, at best, be
considered apology for their own mal-practices or at
worst, their criminal collusion in supporting the evil
practices in society. When taken together, however,
it indicates not only simple apology and collusion
on their part but a definite self-submission to the
ideology of patriarchy. This only adds to the fact
that the values of the medical profession, when exa
mined in the context of their practice and not merely in
their code of ethics, are the values of the society at
that point of time. And therefore, the medical pro
fession is neither apart from the society nor their
codes of practice is given once for all. This view, I
know will not be palatable to even many progressive
doctors, however. But this is only a generalisation to
underline the need to struggle for the better and human
code of ethics, a struggle which goes hand-in-hand with
the struggle for human liberation in the society at
large. In this sense, the success of the campaign
against prenatal sex determination will be a gain for
the larger struggle^.
What is interesting to note about these arguments
of the established section of medical profession is that
all of them, barring one about the hazards of the
technique, are socio-political-economic arguments and
not medical ones. By medical I mean the rational
justification for the use of a therapy or diagnostic
procedure based on the medical indications found in
the patient concerned. Thus, it is clear from the above
that we are not dealing with any controversy surround
ing what is called ‘medical treatment’ and all that goes
into determining rational medical treatment for the
concerned patient (that includes clinical examination,
laboratory investigations, etc.) But we are dealing
with another aspect of the medical practice, what is
considered the provision of ‘medical service’; That
is, medical profession providing service to a normal
human being in response to his/her need or demand
which may not be a medical need or demand.
Now elaborating our earlier points further, the
medical professions’, attitude of considering itself
separate and above society has many implications. In
doctor-patient relationship its reflection is simple—
the doctor knows better and the patient must ulti
mately accept the line of treatment prescribed. In
many countries this type of paternalism is being
challenged and patients have even dragged doctors to
court. But in India, the patients are almost absolu
tely vulnerable to doctors’ paternalism. There is no
Patients’ Bill of Rights in India.
. Readers should recognise here that I am using
these terms ‘medical treatment’ and ‘medical service’
in a very narrow sense. In doing so I have no inten
tion of granting unlimited paternalistic privilege to
the physicians for taking arbitrary decisions in the
‘medical treatment’ aspects of their practice. Much is
written about ideology in the ‘medical treatment’
itself and about its commercialisation as well as the
question of human rights in it. Therefore, we will not
elaborate it here, on the other hand, the ‘medical
service’ which, as we have defined it in the narrow
sense, is purely ideological and socio-political.
At societal level, this paternalism of medical pro
fession takes oppressive and idelological shape. The
professional bodies take care that any critical opinion
on the practice of medicine coming from a non
medical person is adequately discredited and suppress
ed. The professional organisation(s) of doctors are
indeed the most powerful organisations almost every
where in the world. Another aspect of their paterna-.
lism is to consider themselves fit to give their opinion
on all “non-medical” problems of society. Not only
to give opinions, but give a “solution” to the problem
being discussed. Therefore, for many of them the
pre-natal sex testing is a “medical solution” to the
social problem of women’s oppression. Thus they
put Virchow’s famous statement “Politics is nothing
more than medicine on a grand scale” upside down. .
Ideology of medical paternalism:
As I pointed out earlier, given the type of medical
practice involved in sex-determination and sex pre
selection, the established medical profession is hardly
able to produce a single argument strictly from the
2
3
6. What do you expect will emerge from such a Workshop?
7. Any other relevant/related issues?
Please fill in this form and return it to
The Co-ordinator
Drug Workshop
Community Health Cell
47/1 St Mark’s Road
Bangalore 560 001
by 5th February 1989
U(v''V
Meaning thereby that for our established medical
profession, the long lasting solutions of health prob■ lems of people does not rest on the need for deeper
political change (as Virchow postulated), but the
professionals being part of the established oppressive
political nexus, they bring the oppressive communal,
casteist, sexist and capitalist politics at smaller scale
in their day-to-day medical practice.
Jn this context one must recall the role physicians
played during the Nazi holocaust. It has been firmly
established after the famous Nuremberg Trials of the
physicians, and the extensive documentation done on
the role of physicians, that the German medical profes
sion at that time could no longer escape from its respon
sibility by saying that it was coerced by the fascist state
apparatus to medicalise slaughter of certain races of
humanbeings. The fact is that a large section of German
physicians willingly accepted the Aryan Supremacy
doctrine of fascism and it devised medical means to
attain racial health by eliminating the non-Aryans.
It was indeed the self-submission of German
medicine to fascism that shocked the liberal opinion
of the medical world.
medical practice. To all working in the field of health,
these dangerous aspects of the ideology of medical
paternalism must be made clear so that while making
health care available to people they are better equipped
to fight against it.
Can the existing code of medical ethics of the Medi
cal Council of India help socially conscious doctors to
initiate such a struggle? Or is it too inadequate to help
us in bringing some sanity in the medical practice?
Or is the “medical service” aspect totally beyond the
framework of this or any code of medical ethics?
Even if some progressive clauses are there in the code,
is it possible to use them for the benefit of the victims
of medical profession when the regulatory body (the
Medical Council) itself is dominated by the established
medical and political interests? Should organisa
tions like the MFC make the existing medical pro
fessional bodies also a terrain for their struggles? On
this question of pre-natal sex-determination and
numerous such other practices how can debates, edu
cation campaigns, agitations etc be initiated?
When I thought of writing this article at the time
of mid-annual meet, I wanted to give partial answer
to these questions, for I believed and still do believe,
that the question of pre-natal sex-determination can
not be summed up in a for-or-against position, nor
it is as simple as to say that it is just a misuse. On
the face of it, it is indeed a misuse of medical techno
logy. But this ‘misuse’ is deeply rooted in the society
and the ideology-and that also concerns the medicos.
That is to say that medical ethics are rooted in the
social reality. And hence, when I started writing
this article, I realised that it is difficult to evaluate
medical ethics and the question of human rights in
health in one article. While discussing pre-natal sex
testing, this article only poses the issue. I hope to
continue this discussion and request others to also
.contribute.
Without being unduly pessimistic, what I am trying
to point out is that there exists a dangerous trait in the
arguments of the established medical profession.
These arguments, along-with the actual practice of
eliminating female foetuses, seem to be just a beginn
ing of another self-submission of the medical profe
ssion, but of generalisation of the sexist, communal
•and casteist oppression throughout the country. In
this generalisation, the lives of “undesired” commu
nity, caste or sex seem to have no human value. It
is only a matter of lime that this dangerous trait, re
flected in the killing of minority community persons
in the hospital compound, refusal or reluctance to
treat minority community caste or community victims
of riots, doctors and police collusion in the bride
burning cases, doctors’ collusion in torture of political
and criminal prisoners, doctors' participation in forced
sterilisation and so on, become a medical justification,
a “medical” solution to society’s problems. Fascism
made doctors to translate (he fascist genocidal theory
into the terminology of hygienics (racial hygiene);
communalism, casteism, sexism and capitalism have
similar potential.
Thus, the fight against sex-determination and
female foeticide practices in the medical profession has
wider ramification. It should indeed be regarded as
the beginning of wider struggles that progressive doc
tors, women, dalits, minority communities, political
activists etc. will have to undertake to fight against
oppression at every level, including at the level of
3
DRUG ACTION FORUM-KARNATAKA
Kittur 591 115
Bailhongal Taluk
Belgaum District
18 January 1989
Dear
Greetings from Kitturl
You may remember my mentioning to some of you
earlier of the need for drug issue to be taken up at the
grass root level as an awareness building process as
part of the community health and development programme
being undertaken by you and your team.
In this connection, I, on behalf of DAF-K> had a
discussion with the Community Health Cell team (CHC team)
in Bangalore, and I am happy to inform you that they have
agreed to give us the necessary technical support to
hold a Workshop on Drug Issues in the month of April
1989 in Bangalore.
The CHC team are of the opinion that an effective
awareness building process can be initiated only if all
those involved are themselves well informed about all
aspects of Drugs and Drug Policy Issues and are in touch
with the ongoing efforts all over the country. They are
willing to put together all the information/resources
and facilitate the workshop. However, the CHC team has
indicated that it wishes to plan this workshop on a
participatory basis and, therefore, we would request you
to start the process by filling in the enclosed form, The
filled in form may please be sent to?
The Co-ordinator
Drug Workshop
Community Health Cell
No 47/1, St Mark's Road
Bangalore 560 001.
by 5th February 1989.
The venue, duration and the dates of the workshop
will be fixed on hearing from you.
With best wishes to you and to your team.
Yours sincerely,
for DAF-Kamataka.
Gopal Dabade
To
M PC. fl _
Dear Friend.
As you are probably aware, a writ petition against
the injectable contraceptive, Norethisterone enan
thate (NET-EN) was filed in the Supreme Court in
April 1986. One of our main contentions is that,
given the state of the health care facilities in the
country especially in the rural areas, the drug should
not be introduced into the mass family planning
programme, as it requires, careful screening, moni
toring, and follow-up of the acceptors. 1'n order to
strengthen the case against NET-EN, we need to pro
vide evidence that the health services are indeed
inadequate to handle this drug. We request you to
send us information on the availability of primary
health care in your area. This would mean the area
and population covered by the Primary Health Cen
tre, staffing, equipment available, immunization *
coverage and the frequency and the regularity with
which the ANMs visit the villages. If you know of
any published studies on PHCs and sub centres, and
on the abuses of the family planning programme
send us a copy or the reference.
(on behalf of the petitioners)
Saheli, Above shop No 105-108,
Under Defence Colony Flyover,
New Delhi-110024.
Z-
v:
affect their income as much of it depended upon.the
deliveries conducted by them; neither
number of u-----‘The Women’s Health Movement: Feminist Alter- were they in a position to earn money by performing
natives to Medical Control’, Sheryl Burt Ruzek; abortions as they had taken the hippocratic oath
distinction) which specifically
(as another mark of
1979, Praeger Publishers, New York.
rnrnHuc
In
their crusade against aborforbade abortions.
in
the
late
,
lars
,
cited
evjdence of the declining
of
feminism
i
With the resurgence
5
redlsC
°y
er
'
bil
th
’
rates
as
an
example
of
what would happen if a
1960s and early 1970s, female culture: was
in
large
and
small
groups,
they
future
was
|
eft
in
the
hands of women. They,
ed. As women met in
iv
common
concerns
over
their
‘
fear
that
the
decfine in birth rates
soon discovered many common --health and reproductive lives. Along with their among the ‘better’ classes coupled with the ‘prolifera
growing criticism of women’s subordinate role in tion’ of the working classes would lead to a reduction
every social institution, feminists voiced particub
in the ‘White, native born, American Protestant stock
dissatisfaction with the medical care they received
and eventually result in America bemg swamped y
They were outraged at the demeaning manner in inferior categories of human beings. Thus the an which they were treated and critical of the quality o
abortion law that was finally passed was class st
care available regardless of how much they paid. racist and sexist and basically in the interests of the
Above all else, they rebelled at the control men had ‘regular’ doctors. But despite the legislation, women
over their bodies and reproductive functions. From continued to get their pregnancies terminated thrpug
the Supreme Court to the examinmg room men were ■illegal’ means. The abortion debate came up fo
public debate in the early 1960s following the. hahdo:
making fateful decisions about women s bodies
thalidpmide tragedy when a woman who had taken thau
their reproductive lives". (Ruzek, 19 ).
—
’
r
was
refused
aboition
strategic for women’s mide during pregnancy
a 01 1
The medical system was seen
us and later terminated, her pregnancy in Sweden
liberation as it held the key to reproductive freedom The issue resurfaced once again, after anePlde®^
in the form of birth control, abortion te=hnolog.e
German measles resulted in the btrth of ove, 20 0 0
and the means for safe childbirth. Yet, the medical
deformed children, many to,mothers who
system was also strategic to women’s oppression seriously
would’ve had abortions if it had been legal.
P1™®’1
because, justifications for sexual discrimmation in polls taken during this time (1962-1969) were mteres educati^m in jobs, in public life, ultimately rested on L on two accounts: firstly, abortion was most
the one thing that differentiated women from men.
• • ■ to the non-catholic, well-educated, estab
tleir bodies. Theories of male superiority ult.mate y acceptable
lishment-oriented men: and the group that found
rested on biology (Ehrenreich & English). Thus the
abortion most unacceptable was the countei pat
question of who should ‘control’ women s bodies of these men., that is the upper class women, lhese
became central to the feminists’ struggle for attaining men had much to gain and little to lose by reg"g
equal rights within the family, in employment, ed
abortion because “they were satisfied with smal
‘families and were particularly vulnerable to. fmanc a
cation and politics.
and social responsibility for accidental
The abortion campaigni which aroused mass in or outside marriage. In addition, i ( ‘ }
concretized the issue ol j
participation in the US
women who underwent the procedure (Ruzek).
reproductive freedom into a clear specific demand.
considered deviant, illegal yjie Upper class women were most oppose
en
^.Tb^heXncan society. Deliberate ing abortion because it was seen to deprive women
termination of pregnancy was made a criminal offence of a source of income, social status and sens
only around the middle of the nineteenth centuiy achievement that comes out of fulfilling their pnncipa
Review Article
j!
Ii
hh
I
I.
It k.
i]'
I''
III
i
I: <
'I I
■1
’hr'
!‘
di '
li
and was largely due to the efforts of the White, Middle career of motherhood.
class ‘Regulars’ (these were the University Hamed
The feminists entered the debate in 1967 ‘llld
male’ physicians who, inorder to distinguish themselves were against the mere liberalisation °f abo tions^
from the other medical practitioners liked to call Instead their uncompromising stand was
hemselves regulars). It is also significant that the
eg slation was passed at a time when a growing numbe of women from the middle and upper classes laws governing abortion be repealed .
were resorting to abortion as a means of reproduct.ve „r««d .o
ro.™ «t
••«J’
control. Foi the ‘regulars’, such a high rate of induced final decision in the hands of men. In addit.o
abortion (approximately, one abortion was being pci- accepting reform meant compromising the under
formed per five live births), especially in the economic lying feminist goal—the right to limit reproduction.
class that could afford the doctor’s fees, threatened to
...
_
,
. ---------------- --
-
••• ------------ --
■'
” ..........
'
■^4
di
13
f
W
Ip
\-
I
f
g
¥
•1
i
|
il
;
J 3
'.-3 .
Kz?
I
5
' ..4
-.4 5
,J8
o
3
"a
. a
.. j
i 5
H
J
•J *
j4
i’
j
j,,
■ ,.J
J .0
J 3
j ,:.z
1
Strategies adopted by the Women’s movement in
the US included lobbying through established legisla
tive channels to organising under-ground abortion
services. What followed was illustrative of the State’s
interest and power in retaining control over women’s
reproduction. The State was joined by the Church
and Medical Profession • in its opposition to repeal
of the abortion law. According to Ruzek^They
recognized the revolutionary impact of fertility con
trol. They fear that if women are free to end un
wanted pregnancies, they might choose not to have
children at all, to remain un-married, or even to love
women rather than men. In fact, all traditional role
expectations that subordinate women for the con
venience of men might be destroyed.”
men in their legal battles against the Medical
establishment, consciousness raising programmes to
educate and mobilise women were all the necessary
outcome of the movement. The 1970s saw a prolife
ration of nonsexist medical literature in easy to under
stand, demystified language .along with the . develop
ment of theoretical perspectives on the women’s
health issues.
Theoretical perspective not withstanding, the
movement has not been without its contradictions.
For instance, as opposed to biological determinism,
radical feminists have tried to minimize • or totally
disregard biological differences between the sexes.
This disregard has been carried to an extreme,at
times, by denying nearly all differences | between
men and women. To them childbirth is degrading
and they argue that women can be and, should be
totally freed of all reproductive functions by resort
ing to Test-tube’ babies. While, for .the others in
the movement, pregnancy, and childbirth are the
peak experiences in a woman’s life. Some feminists
have argued that menstrual cramps, nausea during
pregnancy, post-partum depression and menstrual
problems are culturally induced, best treated by
consciousness raising while others have disagreed.
But as Ehrenreich and English point out, ‘’The real
trouble is that whatever women say about their bodily
events will be used against them. If women argue
menstruation is painful and distressing, women will
be barred from certain occupations. If it is believed
to be unnoticeable, women may be required to work
the same hours and lift the same weights as men,
regardless of discomfort. If pregnancy is viewed as
an illness, women may be fired early; if defined as a
perfectly ‘healthy’ state, women may be held to overly
rigorous work schedules”.
In the US, women’s experience following the
liberalisation of abortion laws (July 1970) were pro
foundly radicalising. “Women faced humiliating
encounters with the medical personnel. Women were
forced to sign Toetal death certifictes’, had machines
to record foetal heart beats set next to them, were
given bags with a picture of a foetus to be returned
to the hospital after aborting at home or were abort
ed in the same ward as women giving birth. Con
cern over quality of care quickly became as serious
a matter as access to abortion. The situation was
shocking to middle and upper class women who us
ually believed they fared well in the health care sys
tem, but found themselves subjected to these condi
tions. Even after abortion law repeal, women were
pitted against an un-responsive health system (Ruzek).
The abortion campaign brought women face to
face and in direct conflict with the sexist bias in medi
cal and legal establishments. The effect was to add
further to the growing conviction among the feminists
that it was time that women took back into their own
hands what was initially theirs—the care of ‘our
selves’ and ‘our bodies’. The rediscovery of female
culture gave ample proof of how the male physicians
had usurped the place of the female healers, and in
the process had destroyed what was probably a more
rational and humane part of healing. History also
showed the role that medicine had played as an insti
tution of social control. Documentation of personal
experiences (which had till then been considered sub
jective and therefore ‘un-scientific’) delving into long
forgotten medical literature unearthed sufficient evi
dence to challenge the myth of the neutrality of science.
Criticisms have been levelled at the, self-help
groups and women’s clinics for concentrating largely
on the reproductive functions of . women. This is
seen to reinforce rather than question the. role of
women as a reproducer. But feminists assert.that it
is not really a contradiction but that such a focus on
health and body issues is a strategy to subvert the
ideology of sexism at its base. The social inter
pretation of sex differences is crucial to attack, for,
traditionally biological differences have been used to
denigrate women and justify their subjugation and
oppression. To counter biological determinism, the
feminists argue that their subservient position is
socially conditioned and therefore can be redefined.
From this perspective, it is only necessary to alter
the social value of women’s biological characteristics
in order to alter their overall social position; there is
indeed no need to apologise for female anatomy.
Thus, the redefinition of the health and body issues
ft was not sufficient to challenge, gather evidence
and spell out what sexism actually meant, rather, it
was necessary to build up support systems along
with an alternative to the existing health care
system. The women’s self-help groups and cli
nics, the Medical Rights Committees to help wo-
5
i
%
from a feminist viewpoint requires the putting aside
of preconceived notions of the value, eau y,
‘importance’ of the female body for much of these
notions are inextricably part of the patriarchal culture
and value systems.
One of the most important and fundamental
contradiction within the movement is the race and
class composition which conflicts with its egahtanan
ideology. There has been little involvement from the
voXg class and the minority commumt.es This
I! ih
Li
I
€
Women’s Health Movement—Feminist
“The
alternative to Medical Control” by Ruzek describes
‘the evolution of the women’s health movement m
the VS and its impact on the medical pio essi .
The
book is interesting and written in a simple nonhas been largely due to the fact that the health issues
that
nave been taken
— up
- bY the movement are not jargonish manner but the author confines herself to a
that have
directlv relevant to the women from the working class. description rather thani an analysis of the movement.
—i regard
many of the issues Wherever an analysis is attempted, it is sketchy and
For instance, black women
j
with the more serious health at times faulty. She classifies this movement with
as trivial compared \.-~ns tney
- under-nutrition inade- the other consumer movements that aie becomi g
problems
they lace
face suvh
such as
health care, sickle-cell anaemia Although powerful force in the West today. By making such
quate 1
feminists believe that sisterhood will unite a statement and that too in the first chapter
many 1
author misses the fundamental difference between
womeni of all backgrounds, “the reality is a sis
‘the two: consumer movements attempt to reverse the
, be powerful, but so arc race, class and
power structure with the clients on the top, while Ae
hood may
in'shaping perceptions of what constitute as
as an effoit
status i_ as well as possible solutions
(Sounds women’s movement views the struggle
problems
ia the content and the social
their dismay have also to bring about change in
The title is also misleading
familiar?). Feminists to
.gdl1iZation of medicine.
as the need for more Of
realized that a demand such
-^Ihe
description
is
mostly
confined
Jo Jhe
US,
eptives could result in the as the
-- ,
of contraceptives
rigorous> testing
t—
•Id countries having to bear although it is suggestive of something broact .
women from
1----- the Third worh
for the haps an indication of the author’s ethnocentrism!
the greater burden of becom ing guinea pigs
Since the book was published, several
Multinationals.
changes have taken place which has thrown up more
also been problems related to the
There have
organizational structure of the womens
internal The idealistic organizational principles fedora .hroupb th. --“'I E'—.
logy which was envisaged by th mfi
groups.
based on self-realization, equality, anti-elitism, sister- is creating a situation which could
J
A
Xd “nd ««
«< P‘’m‘ “P“r” procreation from the home to the fac J •
feminist nightmare seems to be unto Id o
up of spetra bunk, .Od th. M.m. dvra « d
sciousness raising gioups. Accoiau c
ments for surrogate mothers. As had ‘
d„,rag th. luduttrial K.voluhou
‘the function of • MiUtor rather than »s “““
QtriDoed of all its economic function, it to y
. gofe to be stripped of their raproduohve . u«“o„” eh, th. onl, role left to them —
!
’p
llll
t
Ir
1
i Ij
'
i
been powerful enough to generate academic nte
and research which has forced the medical establ‘s^
ment to change some of its concepts about women :
Secondly, the movement has been saccessf“
demonstrating that radical alternatives based
more egalitarian principles are possible.
CS
-
■
i
1
I
SXu. Tbf pelt®., of <«>•> XX!
I
it ■
k1
■/r
g
S'd^K »
•I '’I
1
“«Xi
■
B
I
to function as sex objects for the sole p easu
As a reaction to this there is a revival of J0",
■
Finally, although the sen neip z
»
love’, ‘romantic motherhood,
Xo supported b, th. radi.t
roman
as the desirable feminist goal.
Hav
“ra. “
H
'■
““apowerful ST1 reckoned with.
full circle?
-3 published
Although the book under review w
in
the
book
are relej h(.
s age> several chapters 1-----J j movement
vvant
;nt t0
to what
what appears
appeals to be the emerging
l.i 1India.
Initially
on
wora
en
and
health
today in
—
on women and L
—
L borrowed from the
“• on“
concepts and stands were
(Contd. on page 8)
Wealth movement in the West is
The Women s
g effectively
important on two accounts
of Medicine
challenged the scient fi
d unassai|able.
’
I
“^ZXnt.Tta.
»h«h rratd «■'
'Ji
has become invalid.
As a
y
6
__ : L
.....
-7—^
'
1
II
•‘j
I
c
■
■ t
’ ■ ‘
. •
■ ■■
R.N. 27565/76
■
(Contd. from page 6)
Western feminist thinking, but over the years, it hass
become clear that the issues are very different and at
times even appear contradictory. For instance, in
the current campaign against the sex determination
tests, .one of the demands has been to make the abor
tion law (which was ‘granted’ to us without a blowi
being exchanged, as it were!) more ‘rigid’, so that
women and their families do not take recourse to the
loopholes in the law. There has also been an ‘appeal’
to the doctors that withholding of such facilities,
even if the demand comes from the woman herself,
would amount to the practice of medical ethics.
These two strategies seem to be in direct contrast to
the earlier Western feminist stand that neither the
court, nor the State, or the medical profession have
the right to withhold such technologies and that
the doctor is merely a technician with no right of his
own to deny such skills to women who demand
111 11 Cl 1 i y
VI
1 11VIO1U
1has
i CIO
L/Wll
Ik/YVllV
VI
Cl
Cl IV
them. Similarly
criticism
been
levelled
atU the
women’s ggroups for their stand against the supposedly
easier to administer contraceptives such as the anti
fertility vaccine and Sub-dermaeimplants. The con
tradiction that is pointed out is women’s groups
comprising mainly of middle and upper class women
and who are certainly not the target of the popula
tion control programme, are making the ‘choice’
that these contraceptives should not be available in
the Indian market on behalf of the women from the
lower classes who are the targets. My point is only
this: In the heat of strategising and getting things
done and expressing one’s millitancy, we neither have
the time to look at the issues critically nor the honesty
to state contradictions openly for, haven’t we all
experienced the way these are used against us?
Sathyamalal
References:
Ehrenreich and English, Comlaints and disorders:
The sexual politics of sickness.
■
II
J
.
'
e
— • -—
. ■ i.
MFC-B
131
August 1987
1 !JI i
II
I I
fII
I
!
ij
n
..
Recently, while discussing 'body politics' with
a few women's organizations, I came to know that
as a strategy to counter taboos imposed on women
during menstruation, intercourse during menstrua
tion was being advocated. This was considered
perfectly alright and some felt that it should infact
be encouraged because this was the relatively
infertile period of the menstrual cycle. While I
do agree that menstrual taboo generally demean
women's sexuality, I feel concerned about advo
cating such a strategy. Despite the fact that the
menstrual blood contains a large number of
WBCs, in the case of menorrhagia the blood clots
formed are potentially a’ good medium for bacterial
growth. I am not a gynaecologist and can only
speculate that intercourse during menstruation
could possibly lead to something like the toxic
shock syndrome (its association with the use of
tampons is well documented). This together
\Contd on page 3)
fi
II
with the fact that pelvic inflammatory disease and
sexually transmitted disease are very common in
slum communities . raises questions in my mind
about indiscriminately encouraging women to
have sex during menstruation. I feel that as
feminists we need to be careful that the information
we give is also scientifically accurate.
Will some gynaecologist please comment on
the points I have raised
Bharati Patel, Ahmedabad*
rW '
VlZv^V
Sex Determination and Female Foeticide
In Baroda
incorrect. We found couples going for test at
first conception. We also found couplesa alrea
dy having one son (the only child) going for
the test as they wanted son second time too.
(A Report by Garbha Parikshan Virodhi Manch)
Following the passage of the bill banning the
use of prenatal diagnostic techniques for sex deter
mination in the Maharashtra Assembly in March this
year. The Garbh Parikshan Virodhi Manch, a front for
med by the progressive organisations, doctors and
other concerned citizens in Baroda (Gujarat), decided
to conduct a survey to find out the misuse of such
techniques in Baroda city and to roughly estimate
the extent of their misuse for female foeticide. The
Manch interviewed 1)30 doctors 2) some patholo
gists 3) some women who have undergone the test
4) some women who are against such test and re
fusing to undergo despite having one or more dau
ghters and under social pressure 5) individuals from
various economic, social and cultural stratas.
FINDINGS
v
B.
The extent of Misuse :
1
According to one information, a well known
laboratory in Baroda has tested 20,000 samples
of amniotic fluid in last 10 years.
2
In 1987, in Baroda city alone estimated 2400
tests.
3
We came to know that a sizeable number of
women go to Anand city to undergo the test*
the real number of women undergoing this test
must be much higher than estimated by us.
C.
Some other findings :
Following are some qualitative findings based
A. Prevalence of Pre-natal Diagnostic Techinques,
on case studies and observations.
1
In Baroda mainly two pre-natal diagnostic tec
hniques are used for sex-determination, viz.
Amniocentesis and Chorion-villi-biopsy (CVB).
Of these two, the Amniocentesis is much more
prevalent as it is comparatively cheap.
1
2
Except very few gynaecologists in Baroda, al
most all do amniocentesis.
2
Some doctors said that sex-determination and
the female foeticide should be encouraged as
a part of family planning programme.
3
Of those who are doing the test, except one
all said that personally they do not favour the
test.
3
Many doctors said that they will stop doing
this test if government bans it. But till then can
not say no as other doctors continue to do this
test and that will adversely affect their income.
4
Some doctors said that they are new in the
business, they have just started their practice
"let us earn a lot for while; After sometime, we
will stop doing this test."
5
Only one doctor believed that this test should
be offered to all couples with two daughters.
According to that doctor, as long as daughters
are unwanted in the world they have no right
to take birth.
6
Only three doctors condemned the test and said
that it violates medical ethics and the medical
profession should take initiative to banish it.
4
5
More than 70% of them admitted that the am
niocentesis could be harmful to the mother and
the foetus. Sometimes it leads to spontaneous
abortion and sterility.
The Manch also came to know that some doc
tors were doing amniocentesis with inadequate
precaution and facility and thus endangering
the lives of the mother and the child.
6
Women from all castes, religion and economic
classes go for this test. Many of them have ta.
ken loan to pay for the test.
7
A common view that parents with two or more
daughters go for such test was proved to be
5
Although doctors did admit the possible harm
ful effect of amniocentesis on mother and child,
and risk of abortion, sterility etc, none of them
maintain any record about the harmful effect
observed by them.
7
Except these three doctors, the others, though
did not favour the test at personal level, bla
med the society for its spread. They believed
that doctors give what the customers demand.
They completely absolved doctors from any
responsibility regarding the test and the female
foeticide.
8
People believe that banning prenatal sex deter
mination tests will not radically change the si
tuation. After such ban, the test will become
constlier.
(Translators' note for the MFC Bulletin : These
findings are taken from a mimeographed report of
the Manch in Gujarati. The presentation is changed
for stylistic reasons. Oh reading the Maneb's report
it was clear to me that the Mahch has done more
of an investigative report rather than a scientific
survey. However, this does not minimise the seriou
sness of the problem they have painfully highligh
ted. The findings are startling. The hypocracy of
the commercialised medical profession is fully expo
sed. We hope that some more systematic research
will be conducted on this subject so that an effort
can be made at national level to banish such inhuman medical practice).
DIALOGUE
Abortion
Arun Gadre
It was a great battle everybody fought to le
galise abortion in India. It was considered as a pro
gressive step in the liberation of women. By legali
sing abortion, it was thought that, i) unwanted
pregnancies would no longer be hindrance in the
progress of a woman's life, ii) MTP would offer a
permanent solution to the problem of unmarried
pregnancies; and iii) abortion could be taken out of
province of quacks into the safer hands of an expertNone of these objectives, I am afraid, have
been fully realised. I identify four main problems:
Firstly quacks are still having a field day and
are openly practicing abortion in rural areas, slums
and even in cities. With Legal control over medica
practice being what it is, quacks continue to enjoy
scot-free status and are fully exploiting the situa
tion. It is a pity that qualifieid specialists in Gynae-
logy are not permitted to offer facilities for MTP
rural centres on the ground that their clinics are
staffed and do not have adequate blood bank
cilities. It is different matter that with the same
nd of set-up they can do, and indeed they do,
iesarean section.
Secondly, I strongly object to abortion being
msidered an extended form of contraception,
’ith the sword of unwanted pregnancy no longer
inging over their head, young weds have become
sry casual in their overall aporoach to family pla
ning. Thus the husband discards barrier contracepves and the wife conveniently forgets pills. Since
oortion is no longer a taboo in the modern society,
yen if pregancy is discovered in the first year of
orried life, 'wiser councel prevails' and abortion is
onsidered a practical solution to the 'unwanted
nd unforeseen' problem.
Thirdly, abortion in the minds of naive coules is 'just another procedure.' They attach no more
nportance to abortion than the procedure of say,
raining an abscess. But than it is not a simple proedure and carries with it all the risks and complicaons of surgery. Women are not aware that abortion
an lead to infection, bleeding and rupture of uterus
nd can also leave behind the legacy of blocked
ubes. One can easily imagine the plight of a woman
etting her first pregnancy terminated, only to deelop intractable sterility for the rest of her life.
Fourthly and lastly carnal pleasures and human
omforts have started taking precedence over the
•aditional mother child relationship. Since a couple
^ants to enjoy the marital bliss and a baby is con’
idered as an unwanted intruder, it no longer hesi-
ates in getting an unborn off. May be our sensiivity to this issue has become blunted, may be an
bortion no longer kindles subtle emotions in such
:ouples, but the fact remains that an abortion has
»ecome an in-thing in the first year of married life.
We must fight the misue of abortion. It will
oe a difficult battle. Abortion is destructive, dehu
manizing and disturbing. The earlier we take up this
issue, the better.
® a
6
v 11 Lt^'N n
6?- ^6.
Victim Blaming Is Not The Solution
Amar Jesani
One important negative off-shoot of the anti
sex-determination campaign is the stirring of anti—
abortionists. I remember that during the campaign
the members of the Forum Against Sex Determination
had to argue vociferously to distance their campaign
from the supporters of right-to-1ife, certain religious
organizations and the doctors who saw problem of
ethics in the MTP and the female foeticide (MTPJ
following amniocentesis as identical. The latter ar
guments might appeal to those who take a kind of
moralist standpoint against the misuse and overuse
of any technology. This note is to examine the pro
blem of misuse and overuse of MTP from different
angle and to point out certain lacunae in these
arguments.
Let us start with the enactment of the MTP
Act. It is wrong to say that the MTP Act was for
mulated in response to the woman's movement's
demand. If it was, it should have been called, say.
Woman's Right to Abortion Act and there wouldn't
have been any need to keep so-called medical indi
cations for performing the MTP. It is know that the
feminists stand for the unconditional right to
abortion.
The
MTP
Act
does
not
give
any such unconditional right. And what was the
strength of feminist movement in the early 1970s ?
Thus, we have to look for elsewhere to find out
real reasons for government to pass this Act.
I submit that MTP Act is not an act for str
engthening women's right (although as a by-pro
duct women do get some facilities for less restric
tive abortion) but it is an act to regulate medical
profession. It was brought in to strengthen domi
nance of allopathic doctors in the Medical profe
ssion. It was passed to confer near monopoly to
perform MTP to the allopathic doctors. It is imma
terial that quacks were and are bad. What is impor
tant is the net effect. Can anybody argue that the
MTP Act did not help modern doctors to get the
most benefit from it ? Most of the doctors doing
MTP are more concerned about the government's
inability to stringently apply it so that the competi
tion from the quack is eliminated. But this is true in
all aspects of medicine practice, why to single out
abortion only ?
It is dangerous to link up lack of health edu
cation in the MTP seeker woman with the 'misuse'
I
4
7
of the MTP. There is nothing like misuse of the
MTP because I believe that woman should have
unconditional right to have it. One can punish a
pregnant woman (by forcing her to take baby full
term) because she is less educated, or husband is
less educated about contraception, or they are lazy
or, woman has no authority in the sexual relation
ship and in the family in general. Pregnancy is a
fact, a physical reality and to deny her right to abort
is to compound one oppression with another. And
medical profession is well known for victim blaming*
Nobody wili dispute concern for the plight of
the women who has no option but to undergo
MTP as she is a powerless person in the family, But
the solution is not in denying her even this escape.
Nobody will disagree with the plea for providing
sex education and education on contraception to
the woman and the man; and also plea to empower
women in the society. But this has to be done by
expanding the frontiers of women's right and
power and not by restricting whatever right she has
(for example that of abortion under the MTP Act).
Firstly, can woman say 'no' to husband when
she understands that she will conceive ? Is there
any law empowering woman to do so ? Is marital
rape considered a criminal offence ? It is not suffi
cient to give sermon to the woman that she should
not allow a sexual relationship which makes her
conceive at a time when she does not want pregna
ncy. What is important is to make right to say no to
unsafe sex a fundamental right under law for wo
men and to create social support system all over the
country to implement such a law. The latter is more
important than the former because we do not want
an empty law like untouchability and many many
others. Are doctors who are so concerned about the
misuse of MTP ready to be part of such an effort ?
Let me assume that doctors would like to
contribute in such an effort. However, for such con
tribution they will have to first break their mental
barrier and prejudice against women's movement
however painful they might feel as a man in doing
so. For whatever effort that is being made in this
country to empower women is being done by the
women's organisations only. Such docotrs will have
to establish links with them rather than blaming
them for the ills within the medical profession.
This brings me to my last point, what does
doctor do when he or she notices a women under
going repeated MTPs ? Denying her the MTP would
R.N. 27565^^^
----------------------------------------------------- ----------be, I believe, not only in human but also unethical.
The only way the doctor can help to 'cure' this pro
blem is by patiently finding out the problem and
then "to step out of medical confines” and "enter
the socio-political field.” This has to be done beca
use there is no "medical solution” to such problemOne has to follow up such cases in the social fieldsby taking support of women's and health organi
zations, and by breaking the complacency of medi
cal or doctor's organisations. The acid test is how
many such doctors will be ready to demonstrate in
support of such women ? To make such a move
ment strong may take sometime, but that is the real
solution, or that has some possibility of taking us
nearer to the solution.
® ®
One Daughter Family : Fact or Fancy ?
To promote the concept of 'One Daughter *
Family' the Government of Maharashtra has intro
duced a novel award of Rs. 10,000 for couples un
dergoing permanent sterilization after one daughter
but without a son. (sic) The award christened as Pt
Jawaharlal Nehru Balkalyan Award was annouced
on 14 November 1988 to coincide with birth cen
tenary celebrations of Pt Nehru.
wife at home. Even a population expert agree&eh
rely: 'People are fanatical about having twq|$y
sons. It is as sacred as religion to them.'
That our first Prime Minister was endeared
children all over the world as Chacha Nehru, that
he loved children as much as the rose on his jacket,
that he had only one daughter and no son and that
this award should therefore be named after him to
ensure equal rights to women a la Nehru ervisagedall these things are admittedly true and might appeal
to the reason. But what surprises one most is the
Government's naive assumption that a carrot worth
Rs. 10000 will lure many a couple to stop after one
daughter. This approach takes no cognizance of the
stark social realities. One can not help feeling pity
at this logic-or rather lack of it. How many couples
will accept this idea and stop after first daughter
voluntarily ? And will 'X' or 'Y' really make no diffe
rence to the hoi polloi 7
J S^>'
L
These are indeed Ten Thousand Rupees Os I
UN Jajoo & SP Kalantri
Publishers
® 0
Strange as it may seem, this announcement
comes close on the heels of Raj Chengappa's article
in India Today (October 31) in which the author has
exposed the limitations and hollow claims of the
Government's family planning programmes in a thr
eadbare analysis. He denounced these programmesas
a big hoax and dismissed the popular slogan, eBeti
ho ya Bete. Bacche do hi acchhe. as a worn-out cliche.
That the Government has paid no attention to this
article is obvious. For consider these reactions which
Chengappa has chosen as representative of people's
general out look at family planning. These explain
why people-atleast from rural background-still long
for a male child. A farmer, for instance said 'I need
two sons. Otherwise who will light my pyre, who
will carry on the family name, who will help me on
the.fields, who will look after me in my old age ?
Another farmer from Rajasthan spelled out reasons
for aspiring for as many as five children : 'One to
look after my cows. Another to tend to my sheep.
One to help me on the field. One to help my
I
r/ Fc
6('')
ICQ
controller
■
A letter to the Drug Banning
of the irrational, unscientific prep^-M
Sir,
We would like to draw your attention to certain
measures which you can take up to curb misuse of
drugs in diarrhoea and foster oral rehydration m
diarrhoea.
As you may be aware, it is estimated that between
1 to 4 million children die every year in India due to
diarrhoea. Recent research has created possibilities
of saving these lives since it has definitively establi
shed that:
• ‘ off cases of diarrhoea, use of anti
(a) in majority
biotics plays no positive role;
(b) mosrofthe deaths due to diarrhoea are not
due to toxaemia but due to dehydration,
(c) most of the cases of dehydration can be very
well treated with oral rehydration;
(d) out of a plethora of antibiotics available, in
vigorous scientific studies, only six have been
proved to be definitively useful and safe.
Dr. Shirish Datar of the medico friend circle has
in a earlier paper summarized the scientific evidence
about treatment in diarrhoea and has also shown that
out of 48 antidiarrhoeal preparations listed m the
January 1983 issue of the MIMS, only four are fully
scientifically justified.
We feel that the production, promotion and
marketing of anti-diarrhoeal agents should be brought
in line with these recent developments. We suggest
that your office can take the following steps to help
to achieve this aim:
1.
rations sold as antidiarrhoeal agents. ToM
start with, banning of preparations contam-^H
ing a combination of Chloramphenicol andM
Streptomycin, since this unscientific combi-™
nation is the most frequently used ‘antidiarr-«
hoeal’ agent.
M
Making it mandatory for all producers olM
2.
antimicrobials used in diarrhoea to print uM
a prominent way the following statutory^B
recommendation on the covering package^®
‘‘Medicine, even when useful, is not enougf^R
in treating diarrhoea. Drinking oral rehydra^^
tion solution is atleast equally important /'M
all diarrhoeas.”
and to print and insert inside the package S
detailed pictorial instruction sheet explain™
ing how to prepare and consume oral rehyM
dration solution at home by using ordinal-™
sugar, salt and baking soda. The printin^B
should be done in Hindi and English- and^M
regional language as is done in the case qM
preparations like Licel, Diazone, Fleet et£.
On our part, we have launched an educational
campaign on diarrhoea, misuse of drugs in diarrhoea
and the importance of oral rehydration in diarrhoea.
If vour office takes up initiative and takes definitive
steps as suggested above, such steps would go a long
way in promoting a rational approach to the manage
ment of diarrhoea; save millions of rupees of the P0°r
people now being spent on unnecessary drugs and«
save lakhs of poor children who would otherwise di«
due to dehydration in diarrhoea. We hope you woulcM
give due consideration to our appeal.
M
Thanking youe
H
Yours faithfully,
A. R. PHADKE
Convenor
Oct. 1983
National Executive Committee, mfl
P S.: This letter was sent almost a year back, but th\
Drug Controller’s office did not bather to re.
pond to it as yet.
(The latest position about antidiarrhoeals
highlighted in the same issue. Refer lead article-Ed^
i !* .
10th February^ 1992
MEDICAL
01.
02.
°04.3*
05.
06.
07.
08.
09.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
EDUCATORS
REVIEW
MEETING
TENTATIVE
LIST
PARTICIPANTS
OF
JUNE
1992
Dr. Abraham Joseph, CMC-Vellore
Dr. Prem Pals, SJMC, Bangalore
Dr. Alex Zachariah, CMC-Ludhiana
Dr. Cherian Thomas, CMC-Miraj
Dr. D.K. Srinivasa, NTTC, JIPMER, Pondicherry.
Dr. Asha, JIPMER, Pondicherry
Dr. Kartikeya Nanavathi, NHLMC, Ahmedabad
CMET, AIIMS, New Delhi (Representative)
Dr. B. Ekbal, Medical College, Calicut
Dr. Ulhas Jajoo, MGIMS, Sevagram
Dr. Siddarth Das, KGMC, Lucknow
Dr. M.K. Vasundhra, BMC, Bangalore
Dr. N.H. Antia, FRCH, Bombay (Special Invitee)
Dr. Palltha A^eykoon, WHO-SEARO, New Delhi (Special Invitee)
Dr. C.M. Francis, Bangalore
Dr. P. Zachariah, Vellore
- Advisers, Medical Education Project
Dr. V. Benjamin, Bangalore
Dr. George Joseph, Madras
Dr. Ravi Narayan, Bangalore
Dr. Thelma Narayan, Bangalore
Dr. Shirdl Prasad Tekur, Bangalore
CMC Team
Dr. Mohan K. Isaac, Bangalore
Dr. M.J. Thomas, Bangalore
IN ADDITION
One additional participant each from the 4 CMC’s to be
nominated by the Director/Principal (a faculty member who
is involved in Medical Education Reform) and whose costs
may be met by Institutional fund.
One nominee each from CHAI, CMAI and VHAI whose costs may
be met by the associations themselves.
★ * ★ *
* * *
* *
★
*rn/mk
>2/ ;
103
RN. 27565/76
MFc
J
lie 'K*'! /Vc
mic bulletin: JULY 1984
Editorial
THE ICMR/ICSSR report on ‘Health for All’
has warned that “eternal vigilance is required to
ensure that the health care system does not get medicalised, that the doctor-drug producer axis does not
exploit the people and that the abundance of drugs
does not become a vested interest in ill-health1”. The
Drug Action Network which has come together in the
last two years is symbolic of this vigilance, which is
growing in India. The memorandum drawn up by
the participating organisations, which is featured in
this issue highlights the diverse aspects of drug policy
towards which this vigilance has to be directed.
THE banning of a wide range of commonly used
drugs for arthritis in U.K., in recent weeks (article
on Drugs alert) raises questions about the complexi
ties of this vigilance. In countries like U. K. and
U.S.A, in spite of drug safety committees, compre
hensive drug laws, efficient drug control authorities,
active consumer groups and socially sensitive elements
in the profession — drugs continue to slip through and
get used for years before their dangers get known and
bans are instituted.2 How much more difficult will it
be in our country where all these elements of ‘vigi
lance’ are still only in the process of evolving?
William Osier’s exhortation that one of the
first duties of the physician is to educate the
masses not to take medicine3 is particulaly
relevant in today’s drug situation.
The role
of doctors in acting as watchdogs is primary
Rcgd. No. L/NP/KRNU/202
— laws, controls and authorities notwithstanding .
Are doctors prepared adequately for this role in India?
Medical education stresses the minutiae in pharma
cology and medicine without stressing the factors of
cost, safety and social relevance. It also does not
consciously immunize the doctors against the half
truths of persuasive medical advertising4.
In the
absence of programmes of continuing education in
the country, practicing doctors continue to be infor
med only by the profit oriented pharmaceutical indus
try, thus worsening the situation.
UNLESS there is a growing realisation among
medical students, young doctors, teachers, health
workers, professional associations, consumer educa
tion groups and science movements that this problem
needs to be tackled in the form of an organized
movement very little change can be expected in the
present situation. Satchidanandan’s critique presents
an analytical framework and background against
which such a movement would have to evolve. His
suggestions for a multi-dimensional campaign of
demystification, conscientization, study, curriculum
change and deprofessionalization could well be initia
ted taking drug issues as the focal point. It would,
however, be important to keep in mind that over
seventy five percent of the people in India have little
or no access to health care. Hence an action pro
gramme only on drug matters would be cut off from
the needs and aspirations of the majority5. However,
if this became part of a wider people’s movement for
socio-political change, the drugs problem would be
tackled at its very roots.
References
1.
HEALTH FOR ALL — AN ALTERNATIVE STRATEGY:
ICMR REPORT, 1981.
2.
NON-STEROIDAL ANTI-INFLAMMATORY DRUGS:
Lancet Editorial, 21st January, 1984.
3.
FEED BACK ONiFRESCRIBING: Lancet Editorial, 11th
February 1984.
4.
WHAT IS RATIONAL DRUG THERAPY?: Health for
the Millions, April-June 1981.
5.
CONSUMER ALERT—CONSUMER ACTION : Bulletin
of Sciences, Vol. 1, No. 2, December 1983.
107
medico friend
circle
bulletin
NOVEMBER
1984
EDITORIAL
Drugs _ Awareness and Action
ftOne of the most distressing aspects of the pre
sent health situation in India is the habit of doctors
to over prescribe or to prescribe glamourous and costly
drugs with limited medical potential. It is also un
fortunate that the drug producers always try to push
doctors into using their products by all means — fair
or foul......... If the medical profession could be made
to be more discriminating in its prescribing habits,
there would he no markdt for irrational and unneces
sary medicines.”
In this special issue one of our members presents
his recent study of antidiarrhoeals. We also
feature a summary of the study done by the Interna
tional Organization of Consumer Unions on Anabolic
ir^S/ Jhe j°,nt study on druS utilization pattern
by NIN/CERC highlight the problem of self-prescri•
* ie e^ers from the People’s Science Movement
in Maharashtra and the mfc Rational Drug Policy
Cell, are symbolic of what we can do to initiate
a discriminating prescribing practice’.
— ICMR/ICSSR, Health for All Report
Among the many challenges that face the All
India Drug Action Network in its campaigns in the
future, one of the key issues will be to make the doc
tors in India more ‘discriminating’ in their prescription
practices. Any pressure on policy makers to evolve a
rational drug policy will fail if the medical profession
does not support it and accept self-imposed controls.
This is possible only through relevant professional
education, continuous dialogue and discussion in our
professional meetings and associations and a meaning
ful continuing education. Who will initiate this?
The All India Drug Action Network at its Wardha meeting decided to take a dozen drugs
in their initial campaign against ‘irrational and un
necessary medicines’. These broadly divide into two
groups:
The first is up for banning. These include Analgin
(singly or in combination); EP Forte drugs, Chloromy
cetin and Streptomycin combinations; Lomotil in
children and fixed dose combinations of steroids.
Enough is known about them and only action is
awaited.
The second group is up for a concerted consumer
doctor alert. These include Anabolic steroids, Antidiarrhoeals, Analgesic combinations, Clioquinols, Oxy
phenbutazone and phenylbutazone, Haematinics,
Tonics and Streptomycin-Penicillin combinations.
Here the dangers and irrationality are known but
there is lack of awareness in the professional ahd lay
public. Awareness must precede action.
The challenge is a four-fold attack on the pre
sent situation — Rational Drug Policy, Public inte
rest legislation, Consumer awareness and Rational
therapeutics. Strange as it may seem, the need
tor regulating the prescribing practices of doctors
is not neW. Centuries ago the Koutilya Arthashastra
had this to say —
The physician who sets about to treat a disease
without knowing anything about it is to be
punished even if he is a qualified physician; if he
does not give proper treatment, he is to be
punished more severely; and if by his treatment
the vital functions of the patient are impaired,
he must be punished most severely.”
Is the medical profession in India today waiting
for such corrective action?
0
Fighting for A People's
Drug Policy
— The KSSP Experience
Dr. B. Ekbal *
The Kerala Sastra Sahitya Parishad, the People’s
Science Movement in Kerala intervenes in areas
like Health, Education, Ecology and Problems of
War and Peace. In the field of health, KSSP is very
strongly questioning the relevance of the present
day health delivery system which is curative orient
ed, individualised^ institutionalised and highly cost
ly and catering to. the needs of only a wealthy mino
rity. KSSP feels that a People’s Health Movement
alone can change the health delivery system in fav
our of the rural poor. KSSP has been striving for
the last few years by various means to initiate such
a movement in our country. With this purpose KSSP
is at present organising health camps, health educa
tion classes, people’s theatre forms and audiovisual
campaigns and field studies on an extensive scale
Although granting that drugs and hospitals have
only a minimal role to play in achieving a healthy
living for the poor, we felt that exposing and fighting
the anti-people and exploitative tactics of the drug
companies should play a major role in the campaign
for a People’s Health Policy for our country. The
aim is twofold, on the one hand we should demystify
pharmaceutical products as far as the people at large
are concerned and on the other hand this can be
used as an entry point into the medical profession
so as to conscientise the doctors and medical stu
dents on the wider health issues.
KSSP started its campaign for a Peoples Drug
Policy from the World Health Day, April 7th, 1984.
With W2 years intense campaign we could make
the drug issue a subject of public debate, make peo
ple aware of the unethical marketing practices of
drug companies and also could identify and organise
a number of doctors and medical students who are
socially conscious and are ready to wage a fight for
a People’s Drug Policy.
We started the campaign with a few major de
mands. These are demands for the production and
distribution of essential drugs, banning of non ess
ential, irrational and dangerous drugs, better qua
lity control of drugs and implementation of the
Hathi Committee Recommendations like, nationali
sation of the drug industry, strengthening of the
public sector, introduction of generic names and
updating of the national formulary. Through the
campaign these demands are explained in detail to
I
the people with the help of documented facts, figures
and authentic governmental and non govern
mental resource materials.
c.-utical sector could be focussed during the Bhopal
campaign.
The campaign started by conducting seminars
simultaneously in all the 14 districts of Kerala on
the World Health Day. The theme paper was pre
sented by a KSSP activist doctor. Representatives
of doctors organisations, medical representatives and
pharmacist organisations and eminent personalities
took part in the discussion. Later 45 zonal conferen
ces were organised taking the campaign still further
forwards. By the end of the year, most of the 600
units of KSSP evenly distributed throughout Kerala
organised seminars attended by hundreds of doctors
and thousands of people.
We are at present organising an All India
Seminar on ‘Drug Industry: A decade after Hathi
Committee, to mark the occasion of the 10th Anni
versary of the publication of Hathi Committee Re
commendations. Since we have a public sector
pharmaceutical company in Kerala (Kerala State
Drugs and Pharmaceutical Industry) supplying
about 45% drugs to the Kerala Health Service a
call to strengthen KSDP is already made so as to
make it capable of producing all the essential drugs
for the Health Services. With this end in view a
seminar on ‘A Drug Policy for Kerala’ will be orga
nised in January 1986.
Apart from lectures and seminars a number of
articles on the various aspects of the drug issue
were published both in KSSP journals and in other
popular magazines. Two books were published and
the studies done by Medico Friends Circle on Anal
gesics and Antidiarrhoeals were reprinted and popu
larised among doctors. We are at present summari
sing the Hathi Committee Report which will be
published by the end of December 1985. Through
the Rural Science Forums of KSSP, about 2000,
wall news papers explaining the various aspects
of the drug issue were displayed in the rural areas.
Thus the message was communicated to the rural
people.
What are the concrete results of the KSSP camp
aign so far?
1 .. The drug issue has been already developed into
a subject of public debate.
The Science Cultural Programme organised by
KSSP is a powerful medium for the popularisation
of ideas on various issues-. Every year Science Cult
ural March will be organised from one end of Kerala
to the other end taking the message of science to the
people in a big way. A few items on health
issues including drugs were included in the last two
jathas which attracted the attention of tihe people.
KSSP units are at present functioning in the
Medical Colleges also. With the help of these units
seminars and discussions are regularly conducted in
the medical colleges. A number of articles have al
ready appeared on the drug issue in the medical
college magazines. Recently the Trivandrum Medi
cal College students opened Dr. Olle Hanson cor
ner to sell books on drug issues at the All India
Paediatric Conference conducted in the Medical
College campus. KSSP activist doctors who are
also members of professional bodies like Indian
Medical Association and Kerala Government Medi
cal College Teachers Association and Kerala Gov
ernment Medical Officers Association and Medical
Students Organisation have made the drug issue a
live subject of discussion in these bodies and could
make their professional bodies take a positive stand
on this issue on many occasions.
2.
People from all walks of life are now aware of
the various issues involved, like essential ver
sus irrational and dangerous dru'S, exploitative
tactics of the MNCs and the indifference on the
part .of the Government in implementing the
Hathi Committee recommendations .
3.
A number of doctors and medical students sympathetic with our views are identified and
orcanised.
4.
The prescription habits
but definitely changing.
5.
The sale of irrational and dangerous drugs
coming down.
of doctors are slowly
• President, Kerala Sastra Sahitya Parishad
We coupled our campaign on the Bhopal Geno
cide with the Drug campaign effectively. Bhopal as
the inevitable out-come of the multinational exploi
tation of the MNCs including that in the pharma-
2
is
lit
|\J q
MpC
1
The New Drug Price Control Order
I'
_ A mockery of rational planning.
Anant R S
>
f
F - ‘
So finally the crunch has come I
Something
which some of us who have been lobbying for a
pro-people rational drug policy, were hoping would
not happen. But with the declaration of the New
Drug Policy in December, 1986, the writing was
there on the wall for everybody to see—two things
were definite after the declaration of the NDP—
the basket of price-control was to be drastically
reduced and the mark-up on the price-controlled
'is A
drug was also to be substantially jacked up
almost doubled. What remained to be seen was
the precise extent of this price-decontrol and the
precise list of the drugs to be under price-control.
These two details have now been announced on
26th August. In analysing this new Drug Price
Control Order, one finds that the list of drugs
included in this new DPCO is not based on any
consistent principle or a set of criteria. Secondly,
there is no mention of implementing other re
commendations of the Kelkar Committee s report
on whose recommendations this new DPCO has
supposedly taken a final shape. Thirdly, there is
no sign of any mechanism to eliminate irrational
and hazardous drugs, contrary to the promise
made in the policy-announcement on 18th De
cember, 1986. The result is that the drug-industry
has got the best of all the worlds—comparatively
very few price-controlled drugs; almost doubling
in the mark-up on price-controlled drugs and no
obstacles to the production of irrational and
II
H
r
i i
i
categorisation would lead to a sudden jump in
the prices of most of the life-saving drugs by
more than 40%. Critics have pointed out that this
increase in the mark-up is based on a study funded
by the OPPI (which represents the interests of
MNCs) though conducted by the National Coun
cil of Applied Economic Research.
Unless the
cost-data supplied by the drug-companies
are
available for independent scrutiny, such studies
cannot be taken as representing the true state of
affairs. That is why this increase in mark-up has
been criticized by many analysts. Secondly, the
idea of removing the life-saving drugs from cate
gory-1 shows that the government cares little for
the life of the people and is 'bold' enough to take
hazardous drugs or their combinations.
Mi!
Shameless omissions :
The NDP of 18th December, 1986 had said
price-control would now
that the drugs under
would
be in two new categories—Category-l
consist of drugs required for the National Health
Post
Allowable
Programmes. The Maximum
name
for
a
new
manufacturing Expenses (MAPE,
be
75%,
as
mark-up)—for this category is to
1
|!
i
I
I
compared to 40% allowed for the erstwhile^catelife-saving
drugs—of the
gory-l consisting of I...
.
DPCO
of 1970.
To begin with, it is highly questionable? as to
shifted from
why life-saving drugs have now been
L_
allowed)
to the
the old Category-l (40% mark-up
allowed).
The
new Category-ll (100% mark-up
have
Government could 1.
— atleast
-------- retained them in
the new category-1 (75% mark-up). This new
u
■<s
■'
such a shameless step.
It reflects on the efficiency of "the Government
that works faster," that it took eight months to
decide as to which drugs belong to this new
category-l. There are about a dozen National
Health Programmes, atleast on paper, and it has
been reported that the
’ j officials of the HealthHealth
a
list
of
150
drugs
to
be
included
ministry prepared
..........
y
But it is not the Health-ministry
in......
this
category.
which has a major say in the drug-policy, but it is
the Ministry of Chemicals and Petrochemicals
which holds the reins. These gentlemen quietly
kept aside this list, and instead, a list of a mere
27 drugs was included in Category-1.
This list has many shocking omissions. The
most glaring omissions from category-l are the
vaccines. This happens in a period when so much
is being talked about "the biggest ever vaccination
programme" to be executed in India as a part of
the strategy of 'Health for All by 2000 A.D.'
prevention of diseases should be
Drugs used
i----- for
priority
in- ‘Health-planning and hence
given top [
........................
lowasas possible;
their prices should be kept
but since the drug policy is not seen primarily as a
part of health-policy, this elementary consideration
has not been taken into account. Exclusion of
Vitamin-A from Category-1 occurs when 40,000
r due to vitamin A
children go blind■ every —
year
and
when
the
Government
has declared
deficiency
this
national
shame,
with
the
help of a
a war on
for
the
prevention
of blindNational Programme
have
been
forness. Other National programmes
mulated because they seek to prevent millions of
I
to
8
.
fo
'■■I
mJ
illnesses and deaths.
But the list declared on
26th August takes care of only Tuberculosis, Lep
rosy, Trachoma, Malaria, Filaria and includes oral
Rehydration salt for 'prevention of dehydration.'
It does not include even the oral contracetive
pill which is used in the Government's pet pro
gramme of family-planning. In the drugs for
malaria, Primaquin-the second-most important drug
is missing whereas
paracetamol
(available
under the brand-names like: Crocin, Metcacin..
etc.) a drug used in ordinary fevers, and which is
not used for treatment of malaria finds a place I
Such queer selection can only be called hair
brained ; and such gross omission of a whole
set of drugs required for many National Programmes
can only be called shameless.
which is being distributed to millions and millions
of pregnant anaemic women and anaemic children,
is missing in this list, so is the case with calcium
gluconate, which is required in hundreds of tons
to be given to poor pregnant women whose bones
get depleted with repeated pregnancies.
It has been argued that drugs whose annual
total consumption in India is less than Rs. 50 lac
have been excluded; otherwise the practical work
of controlling prices of all and sundry becomes too
much to handle. It is difficult to take this argument
seriously in the world of computerization. But
even if one accepts this argument, the omission
of these common drugs which are required on a
huge scale cannot be defended. ANOTHER cri
teria that has been put forward is that of 'encourag
ing the indigenous producers.' Obviously minerals
like ferrous sulfate and calcium gluconate do not
require sophisticated technology, so is the case
with many skin-preparations. Production of Sera
is also not a new technology at all in India. What
is so peculiar about the technology for the pro- ■
duction of morphine, pethidine, codein for them
to be exempted for price-control, when so many
drugs produced by the Indian sector by using com
plicated technology have been included in cate
gory II ?
Category-!! Drugs :
-
<3 -
■*)
■®
t
a4
a
.3
.A
4
KZ
.a
h 'J
1 'OO
The Category-ll drugs are supposed to contain
'other-essential drugs.' It appears that this list of
139 drugs as announced by the government is a
truncated version of the Kelkar-committee's list
of 154 drugs. If we compare this list with the
guideline list of essential drugs recommended by
the WHO, we find many glaring omissions in the
government's list. Except lignocaine, which is
used for local anaesthesia, none of the drugs used
for anaesthesia-ether, halothane. Nitrous oxide,
oxygen, thiopental, scoline, neostigmine, atropine..
etc. have been included. These drugs were not
included in the Kelkar-committee's recommenda
tions under the imbecile,
bureaucratic pretext
that these drugs are not "directly consumed by
human users." Morphine and pethidine, routinely
used in surgery are also missing. The secondimportant class of drugs not included in Category-ll
are Anti Rabies vaccine. Polyvalent antisnake
venom serum (for treatment of snake-bite), di
phtheria and tetanus anti-toxin, all of which are
classical life-saving drugs; and are required in large
quantities in our country. Thirdly, many of the
skin-preparations
(neither Benzoic plus salicylic
acid-the classical ointment for fungal infection
of skin, nor the new antifungal agents like mico
nazole, nystatin) find a place in this list even
though fungal infections are quite rampant in our
country. What is most surprising is the exclusion
of the lotions used for the treatment of scabies—
Benzyl Benzoate and gamma benzene hexachloride
(BHC or lindane) even though scabies is typically
a very common skin-infestation in the poorer
communities and when the current prices of these
drugs are already beyond the. reach of poor people.
Mebendazole, the drug of first choice for treat
ment of worms, is also missing. Ferrous sulfate
One has to conclude that in making this list,
none of the criteria have been consistently adhered
to. The most important consideration that seems to
have been applied is to make this list as small as
possible and to please the big-shots in the industry.
The strangest thing that defies any logic is the
inclusion of a few drugs which are not in the
WHO essential drug-list and which are therapeuti
cally not important in the Indian context either
or are even obsolete.
These are : Baralgan,
Ketone, Bephenium,
Cyproheptadine, (healthgroups have asked for a ban on this drug I)
Levamisole, Piroxicam (a dangerous drug) Tetramisole and fifteen more such drugs. Instead of
these drugs, the really essential drugs mentioned
above could have been included without lengthen
ing the list, (if that is to’be accepted as a cons
traint).
To offset the sharp price-rise in these essential
drugs due to this new DPCO, the Kelkar committee
had recommended the abolition of all taxes on
them. If the Government accepts this recommen
dation, there would not be a steep rise in drug
prices but the Government's income would come
down to that extent; to be made good by fresh
taxes on other items or higher budgetary deficit
9
Mi
I
1
I
I■
i
t
I
■®
8
I
I
I
I
‘MI
■
fl
■I
I
8
I
I
I
i
2
ft rWi
hF< A vxU^ii>
in the next budget : Ultimately, the consumer
will have to pay in one way or the other for the
increased profitability of the drug-industry.
i
The ultimate result of this new DPCO is that
instead of 347 drugs under price-control as of now,
there will be only 156 drugs underprice control
and even in this category, the mark-up has been
almost doubled from 40 and 55 per cent to 75 and
100 per cent for category-1 and II respectively.
It of this mockery of the concept of rational
The resu
planning will be experienced by all of us in a few
■
I ■;
I
Ml
ar
days.
Jb
4;'
I
I R i i
11
S'
■
IIi!1
I
II;
Id
lie I
Hi
!
I
The production of certain essential drugs currently
under short supply is likely to increase because the
Government has now almost doubled the mark-up
on these drugs. Now that the Government has
responded to the drug-industry's black-mail by
conceding a much higher rate of profit, the com
panies will now utilize the capacities kept idle as
part of their black-mailing strategy. But so long
as there is no ban on irrational drugs nor any
control on their profitability, the drug industry
would continue to focus on these production of
these non-essential but highly profitable drugs.
There is a way out :
V
up was really less compared to other industries and
hence in need of an increase, such increase in
mark-up should be accompanied by a ban on all
irrational drugs and irrational combinations. Let
the drug-industry get an adequate rate of profit
without cheating the people. Then increased pro
fits can be coupled with decreased prices of drugs .
But even this simple demand is not being granted.
Apparently, for the power that be, moderniza
tion and march towards the
TWENTYFIRST
CENTURY does not mean adopting modern, scientifIC
planning
11
There is only one slender hope of forcing the
issue of controlling the prices of many drug
combination. This can be done by putting a finger
on the definiton of Category■ | and Category II
formulations as given in this new DPCO. These
definitions specify category I and II formulations
as containing any bulk-drugj either individually
combination, specified for either category-1
Category-lT
formulations. If we strictly follow
or
' 1 mean that any combination
this definition, it would
of
the
drugs in Category-1 and II
containing any c.
be
under
price-control.
For exampl,e if
would
company manufactures a combination containing
a
say theophylline (a Category-ll drug) and 2-3
non-essential or useless drugs, this combination
would come under Category-ll and would be
under price-control, In this manner, -hundreds
of drug-ccombinations would be under price-control. The Drug industry would, of course resist
such interpretationi but it is possible to force the
its own declaration seriously.
governmentto take
—•
a
I
a
I
I
I
i
f
.aB
I
The text of the New Drug Policy released on
the 18th December, 1986, had said that A Na
tional Drug and Pharmaceutical Authority will be
T;
created and "Among other things, it would go into
■
the question of rationalization of existing formula
tions in the market including the banning of for
mulations of harmful nature." But since then,
there has not been any effective action in this
But the above is only to extract something out
regard. Banning irrational drug-combinations is
of a hopeless situation. The real scientific way to
important from purely price-aspect also. If only
get out of the present muddle is to allow only
rational drugs and their rational combinations are
those drugs and their combinations which have
allowed, the drug-bill of the consumer would be
been recommended by medical text books and
more than halved I For example, most of the antiby National Medical Authorities; to disallow all
diarrhoeal mixtures contain one rational antimi
other products and to give a uniform, adequate
crobial agent and three to five useless or otherwise
rate of profit to all such essential drugs. There is
irrational ingredients. In cough-mixtures, it is
no need to make different categories within the
difficult to find even a single really useful ingredient
category of rational drugs and to allow differential
recommended by standard medical
textbooks.
rate of profit for different categories. (The only
So called tonics, as is wellknown, abound in ir
exception would be research-products.) If this
rationalities and overdosages of water-soluble vita
simple scientific demand is conceded, instead of
mins whose only function is to enrich the sewerage
40-60 thousand formulations,
to be controlled,
and the drug companies. If only rational combi
or monitored, there would be at the most a thou
t of all the 250 ||
nations are allowed, the drug-prices would come
sand rational formulations made out c. -....
down drastically due to the deletion of unnecessary
essential drugs and say a hundred more secondingredients.
line drugs, Let the drug-industry accept this simple g
demand of making a good business without cheatIf it is proved by independent study open to
ing the people I
public scrutiny, that the earlier 40% and 55% mark<■!
I
•f
10
I
‘
■■
'
r/ / c
Hv)
/V)
JkJD 111
Scientific Medicine
Whenever there is a discussion on the diff
erent pathies, I am confused by the profusion of
terms to describe the system of medicine that I use
in my practice. Allopathy, western medicine, mod
ern medicine, and scientific medicine are all terms
used to distinguish our system of medicine from
the others — ayurveda, siddha, unam, shamanism
and homeopathy. Perhaps this confusion and pro
fusion of terms comes from muddled thinking.
The word ‘allopathy’ is outdated and should
never be used by us; we should not define our system
of medicine in terms of someone else’s incorrect
perception of our system. Several mfc members
have pointed out that allopathy is a misnomer. Ine
aim of most of our treatments is not to produce an
opposite effect to the disease at all. If homeopaths
want to continue to use the word to distinguish their
svstem from ours, let them' do so.
Western medicine is another popular term1,
but it is a bit limiting. It fails to distinguish our
medicine from the 19th century pseudoscience
homeopathy. The practice of unam also originated
in the west. Besides lending an unnecessary foreign
name to our medical system-, it no longer describes
the practice as it exists in India.
The term modem medicine is also used.
Although most of the knowledge used by us is new,
it is not the distinguishing characteristic of this
knowledge. Two hundred years have passed since
digitalis was first used for dropsy. Modem is a
better emotive term* than a descriptive one.
The best term to use is scientific medicine.
This contrasts our practice with the traditiona. sys
tems of ayurveda, siddha, unani, shamanism; and
even homeopathy.
Scientific medicine includes all aspects of
healing that are proven (by scientific method) to
do more good than harm. This scientific method in
cludes the powerful experimental tool of the clinical
t -aThe use of steamed, sterile banana leaves
as dressings for bums is not western, modern nor
allopathic. It is scientific medicine employing th
scientific principle of antisepsis and proven by clini
cal trial to do more good than harm. The use
Rauwd'fia serpentina for high blood pressure
also describedin ayurvedic practice, but has become
part of our present practice of scientific medicine
only as reserpine has been proven to lower blood
pressure, and treating high blood pressure has been
shown to do more good than harm. . °P?lra'nd!°
practitiopers of scientific medicine wHl have no
diffculty integrating proven methods from the tradi
tional system's into scientific practice.
If we think clearly, perhaps we will begin to
talk more clearly. We will begin to hear less o1 the
other pathies and will begin to hear more of the most
important pathy in the healing arts — empathy.
Jamie Uhrig — Mitraniketan
AZ C
I
Medical Technology : neither glitter, nor gold
What happens if you rely on robtos ? You lose
the use of faculties that you need for their mainte
nance and replacement, so you can't rely on them, (i)
'Good servants but bad masters !' Maurice
King has chosen only five words to show what
modern technology is upto. If one goes through
the recent ads appearing in our national newspa
pers, one can not help feel ng that modern tech
nology—its razzle dazz'e and all that—has hit the
third world countries as well. And so we have
lithotripsy machines which 'leave no stone untur
ned,' MRI Scans which 'can see almost anything',
annual health check-up programmes which 'discover
disease even before it has started' and so on...
With our doctors also deciding to play with exotic
and expensive toys—our euphemism for advanced
technology—the threat that medical technology is
now posing is not de minimis— small enough to be
ignored. Maurice king's warning could .not have
come at a more appropriate time :
'Should we allow ourselves to be seduced,by
the irrestible technological imperative, the seductive
non Sequitar that because some expensive and so
phisticated procedure is done in Detroit or San
Diego, it must also be done in Dacca, Delhi.or Dares-Salaam, then not only is frustration likely to
follow, but there will be less money to spend in
Tubvan and the millions of villages like it, all over
the developing world, (2)
While the idee fixe of the general public that
technology can offer infinite solutions to . the pa
tient's problems can be understood, what is alar
ming is the abysmal ignorance and blind faith of
medical community in technology. Worse still, as
Gajanan Ambulkar shows so well in his cartoon
(page 4), even the traditional patient—physician
relationship has undergone
painful mechanical
metamarphosis. 5
,
Manu Kothari and Lopa Mehta in their characterstic iconoclastic approach attack the myth
perpetuated by medical industry and show that mo
dern medicine is a farce. Many of us may not share
their views on modern medicine, but the sheer logic
behind their trans-technique approach ard \the evi
dence they have so painstakingly gathered to su
pport the hypothesis, is indeed thought-provoking.
i
.
■...
i
|
..
■
■
.
Kabra's article possesses the punch of an eye
opener. The diagnostic X-ray units, the way they
are operating without safety measures, the way they
are proliferating —putting even that wild weed
Parthenium (gajarghas) to shame—is indeed a matter
of great concern. With some 160 million Indians
undergoing radiography each year, and considering
the miserable state most of our X-ray Clinics are
in, the number of reported—and unreported—cases
of X-ray associated cancer must indeed be stagge
ring one. In fact Evans et al (3) have recently sho
wn that 267 cases of blood cancer (1 per cent) and
788 cases of breast cancer (0.7 per cent) that occur
annually In US may be attributable to diagnostic
radiology. Kabra was, and still is, concerned, rather
angry, about the indiscriminate way in which X-ray
is being exploited to day. His plea to check this
hazard in his own state—Rajasthan—fell on deaf
ears of the health authorities. Kabra then went a
step ahead, and filed a writ In the high court requ
esting, among other things, a state-wise checkup of
X-ray clinics. More power to his muscles 1
That brings us to the last article. We do not
deny that radiography has not benefited the society.
Far from it. We owe a lot of debt to Roentgen. But
unless this technology is properly used, the mass
popularity of Roentgen's rays will suceed only in
creating its own Frankenstein's monster. It is in
this regard that the WHO expert committee's report
(4) on rational use of radiology needs in-depth
study. It has shown that rational radiography can
be productive and cost-effective without in any way
compromising the quality of medical care.
Which is what precisely should medical tech
nology be all about !
UN JAJOO & SP KALANTRI
Publishers
REFERENCES
1 Anonymous. Br Med J 1 986; 292 :1261.
2 Maurice King. Medical care in Developing Coun
try. Oxford Text-book of medicine 1984, p- 3.8
3 Evans etal. New Eng J Med 1986; 315: 828-30
4 WHO Tech rep ser; 1983; 689
;
J5
4Ft tLtr,
Clinical Perspective : Chest Radiography
SP KALANTRI
A modern medical student, born and brought
up in era of increasing radiological sophistication
has started turning a Nelson's eye to the traditional
bedside methods of making a diagnosis Perhaps he
should not be blamed. The current culture in the
academic institutions and private practice is steadily
reducing his confidence on the utility of bedside
signs. Even quite a few postgraduate teachers have
seriously been toying with an idea of providing
chest X-rays to the examinees in their long and
short cases. Patients are also sharing the belief that
short of being radiographed,
their examina
tion is highly incomplete. This overuse of diagno
stic radiology, almost global now, the undue
popularity of the Roentgen's rays and a gradual
erosion of faith on the Laennec's tubes should
call for concern.
I made an attempt to go through the avai
lable literature and to put the chest X-ray in its
proper perspective so far as chest diagnosis is con
cerned. In this task I have greatly been helped by
a technical report series published by WHO in 1983;
(1) its basic theme centres on the rational use of
radiology in all disciplines of medicine.. In the
preparation of this article, this report has extensi
vely been referred to. The questions to which I
sought answers were :
(i)
Is routine CXR helpful in screening asympto
matic subjects ?
(ii) What is the utility of CXR in the overall asse
ssment of respiratory diseases?
(iii) Why chest X-rays are being overutilized ?
2.
Routine chest X-ray in pregnant women :
The WHO Expert Committee thinks that un
less there is high incidence of clinically silent
chest disease, routine CXR has no role whatso
ever in pregnant women. In support, it quotes
a massive study of 12000 women by Bone
brake, (3) in which not one patient with clini
cally unsuspected disease could be detected.
J.
Preoperative chest X-ray :
Do preoperative chest X-rays, as is comnv
only believed, affect the decision to operate,
change the type of anaesthesia, and provide a
useful baseline film before operation ? Yes, says
Sane, (4) who studied a series of children and
found that in 3.8% the results ,of preoperative
chest radiography changed either the anaesthesia
or the type of treatment. Milne also considers
them essential for comparison with a postopera
tive film if a patient develops a postoperative
complication. There are, however, some large stu
dies, which do not share this belief. The Royal
College of Radiologists, (6) in a survey carried
out in England, Wales and Scotland concluded
that CXR should be used as an adjuvant to ca
reful clinical evaluation of the patient and should
only be done when it is thought that they will
provide additional useful information.
Lloyd Rucker recently did a study (7) where
patients were drawn from almost all major sur
gical specialities. He proposed that certain risk
factors would increase the likelihood that a patient s
The criticisms that appear in parenthesis after
some of the recommendation of WHO Egbert Co
mmittee are my own.
Contributors
Routine Chest X-ray in asymptomatic population
MANU KOTHARI and LOPA MEHTA are
Professors of Anatomy at GS Medical College,
I.
Routine chest X-ray on admission to the hospital:
Feingold (2) surveyed 39000 hospital admi
ssions,'the majority of patients were elderly, chro
nically ill, poor and came from a population with a
high incidence of tuberculosis. He concluded that
if were no symptoms referable to chest and no fe
ver, no tuberculosis was found. TherS were few
other significant abnormalities that could have been
Bombay.
SG KABRA is a director (Research), Santokba Durabhji Memorial Hospital, Jaipur.
SP KALANTRI is a physician at Mahatma
Gandhi Institute of Medical Sciences, Seva-
gram, Wardha.
detected by clinical examination.
11
/■
preppef^tiv^jp^R wpyld demonstrate a serious
abnormality. Thes'e were: history of cardiac or lung
r•
orb ni olo:!
(What about Bhopal population then? Should
every subject with respiratory symptom be radio
graphed there, or will pulmonary function testing
be a sujtpblp alfprngtive ? And ?hou|d every sub
ject from pndpmic jzjpnes of tuberculosis be radio
graphed,^kre?pective of physical signs ?)
disease, cancer at any site, smoking, asbestos expo
sure,, fumes,, crusts, sprioys systemic disease, recent
tftoraxri?
abnor^ physical findings in
the chest, heart, abdomen and age older than 60
years.
‘
Chest X-ray in disease
(Unfortunately these recommendations are so
comprehensive and cover so many aspects that
virtually every patient needing surgery might end
up with a chest X-ray. Though a number of other
studies have failed to find usefulness of preope
rative chest X-ray independent of complete clinical
evaluation, the more recent and widely read sur
gical texts have avoided the issue entirely, making
no specific recommendation.)
I.
'*'*
1
Tuberculosis :
■
-
/
*
'
‘
.
...
•
The WHO Expert Committee suggested three
criteria for doing CXR in patients of tuberculosis:
■
(i)
During chemotherapy. Periodic CXR at
intervals that should be dependant on the
clinical condition and diagnostic assess
ment.
(ii)
Treatment completed. Periodic CXR only
if clinically indicated.
(iii)
Defaulter. Further CXR if patient has failed
to complete drug therapy.
Mass Chest X-ray survey of unselected population:
The following are the recommendations from
the WHO Expert Committee on Tuberculosis (1974)
-
"Mass miniature radiography is very expen
sive screening procedure for tuberculosis^
even when the prevalence is high. Other dis
advantages of MMR are as follows: (1) it
contributes only to a small proportion of cas
es found; (2) it has no significant effect on
the occurrence of subsequent smear positive
c^ses, as they usually develop so rapidly that
they arise between the rounds of mass radio
graphy examinations ; (3) it requires the
services of highly qualified technicians and
medical staff, who could be better used in the
other health service disciplines; (4) the app
y ?•
aratus and the vehicle used to transport it*
are often out of service the committee con
cluded that the policy of indiscriminate tub
erculosis case finding should now be aban
doned "
f1
•
•
■
(These guidelines are rather vague and it is
difficult to interprets them exactly. Our
criticisms are: (i) How precisely do we de
fine clinical condition: based on symptoms
or appearance of new signs; either or nei
ther ? (ii) if structural damage caused by
tuberculosis can be picked up by physical
examination, be it cavity or fibrosis, effusi
on or pneumothorax, how will CXR help in
the ultimate management? (iii) In defaulters,
CXR is useless in differentiating an active
from a healed lesion, (iv) In defaulters the
rational approach should be to stop the
previously used drugs and start fresh che
motherapy with atleast three new drugs.
Won't further CXRs add to the cost of chemotherapy^?)
Chronic obstructive pulmonary disease :
Routine Chest X-rciy survey of selected population:
2.
The Expert Committee opined that the chest
X-ray is only justified in :
The Expert Committee considers clinical eva
luation better than CXR in periodic assessment of
COPD. In childhood asthma, however, it sounds a
note of caution and tells us that severe asthma and
repeated attacks, may be an indication for chest ra
diography, even in the absence of other clinical ffrK
dings. A recent study published in 1987 (9) also
confirms that routine spirogram and chest films ha.
(i)
Subjects occupationally exposed to respira
tory hazards.
(ii>
Countries or areas where there is high preva
lence of tuberculosis and similar infections.
12
r^viici-h
-
I
N'V ■
I The Physicians role :
tile role in the management of clinically stable
ents.
1I
Lack of knowledge: ’Every patient with che>st
pain needs a CXR’.
22
Undue dependance: How else can I follow tiiy
my
patient of pneumonia, tuberculosis or lung can-
VVTs '-?•'
Lung Canar:
)
A number of studies havej proved that CXft is
useless in picking up <asymptomatic lung cahin early detection of
cer and offers no benefit
I----lung cancer.
cer
3
Powerless Radiologist: ’How can I stop a Phy
sician getting his patient's chest X-ray ?
4
Striving for perfection: 'The medical record sho
uld look complete.' 'I should not miss anything.
5
CXR as a gold standard: *1 know it's pneumonia,
but am I right ?
' v®
6
Busy OPD; No time to think: ‘I had better buy
time. CXR first, physical examination can Wait.
Routine follow up CXR for patients with lung
(ii) cancer should only be dictated by clinical eva
luation and natural history of cancer.
Systemic Disease :
4-
!
The Expert Committee suggests that if there
is no fever and clinical evidence of chest disease,
CXR ofters no benefit in the clinical evaluation
(Two situations, we feel, defy this generahsation,
In patients with miliary tuberculosis and
where fever could be absent due to low immunity
and the chest signs are minimum, CXR is an.'"1P“r‘
tant diagnostic tool. Similarly in patients with per
sistent weight loss without fever and chest symptoms/signs. CXR often uncovers an hitherto unsuspeeled tuberculosis).
5-
Repeated chest
Peer pressure:'If they corner me in hospital
7
death meeting..*
I'-'V 3f'!"
Il
The patienfs contribution :
i
Undue demands: 'I ought to have a CXR for my
annual check up.'
2.
Reimbursement policies: 'But I am not paying
from my pockets . '
3
Reassurance: 'There is something deep within
my chest, why not rule it out ?'
■
radiography for acute pneumonia :
no point in'doingTeri^CXRrto know whether the
Irrational Hope: 'I need CXR to^get cured’.
4
only inpication tor further CXRs in pneumoma.
in
(How about this idea : If history and bedside
physical signs strongly suggest community acquired
pneumonia why not do away even with an mit a^
TXR? More cost-effective approach should be to
ueat the patient with penicillin, reserving CXR only
1
if the patient does not respond).
3
SocialIEconomic ILegal factors :
institutional requirement: 'Every patient admi
tted in medical service must be radiographed.
Defensive Medicine : 'If someone pulls me up in
2
the court Of taw?'
Money matters : ’I scratch your back, you scra
tch mine'; reminiscent of the link-Ci(cn-cu
Overutilisation of chest X-rays
Overutilization of X-rays has been defined as
excessive radiation per film, excessive films. pelex
posure and excessive examinations per patient. (10)
Since the first two. factors depend basically on the
over use of radiology, I decided to find out why
X-rays are being overused. The reasons could be
grouped under three broad categories: physjcian s
?ole patient’s contribution and social/economical/
legal factors.
X;'
'■ ' '
>
'
■■
■
practice.'
Cultoral influence: 'When everybody arduhd -is
doing the same thing, why shouldn t I ? ?
4
Down to earth logic: I invested 5 lacs in this
machine, how else can I recover its cost?
5.
.
.
■
..
;
.■
-
•
■
■
•-
REFERENCES: next page.
•
'
■
Jtearf W*
twlj Ww «ai® ™
'
1
REFERENCES:
1
2
3
_
,1.r
Keport of a WHO expert committeet. A rational
approach to radiodiagnostic investigations:
WHO scientific group on the indications for and
limitations of major X-ray diagnostic investiga
tions. WHO tech rep ser 1983; 689.
Feingold AO. Routine chest roentgenograms on
hospital admissions do not discover tuberculo
sis. South Med J 1977;70:579-80.
4
Bonebrake CR et al. Routine chest radiography
in pregnancy. J Am Med Asso 1978;240:2747-48
Sane SM et al. Value of pre-operative chest Xray examinations in children. Paediatrizs 1977*
60:669-672
5
Milne RA. Surg Clin North Am 1979;2:83-86
6 Royal College of Radiologists National Studyon
pre-operative chest radiography. Lancet 19792:83-86.
7
Rucker L et al. Usefulness of screening chest
roentgenograms in preoperative patients. J Am
Med Asso 1983;250:3209-11.
8
Report of a WHO expert committee. Tubercu
losis. WHO Tech Rep Ser 1974;552.
9
Owens M et al. Influence of spirometry and ch
est X-ray on the management of pulmonary out
patients. Arch Int Med 1987; 147:1966-70.
10
0 Abrams HL et al. The overutilization of Xrays. New Eng J Med 1979;300:1213-16.
w*
\for various reasons (age, etc) are not exjid to have children are not considered to
part of the genetic pool, and their radiation
jsure iis neglected as a component of genetic
ation exposure" (WHO manual on Radiation
tection).
Gene mutations, because of their serious
eterious effects on the next and subsequent
nerations are, therefore, the matter of "highest
iblic concern".
o Dose is Safe
X-rays, as they pass through living cells,
jroduce radicals that act as strong oxidising or
1
. "Thus even small doses of
educing substances.
disturb
the
radiation <---------- --- delicate biochemical equiiibrium of living tissues and must be considered
damaging".
The conclusions here are plain and una"3 of knowledge
mbiguous. "In the present state
mutations
it must be assumed that the point
|
linear
dose/effect
produced by radiation have a
'ationship,' without threshold, recovery, or'tolere1----------rance dose',
accumulation
dose', and
and with unrestricted
----of all doses, even very small ones, received by
the genetic pool".
The severity of X-ray damage, viz. carcino
genesis and gene mutation, is not dose depen
dent. Even very low doses carry the same risk.
However, the magnitude of the risk increases with
the dose, and the effect of every subsequent
dose is cumulative.
The benefits of diagnostic X-rays are un
disputed. The potential for harm from ionising
radiation and the serious consequences of their
improper use are equally well established. Health
authorities neglect the latter to the peril of the
general public. The state governments are expected
and required to appoint appropriate Radiation Pro
tection Committees to monitor and supervise the
functioning of diagnostic X-ray units in the state.
There has to be a Radiation Safety Officer (RSO)
for every diagnostic X-ray unit under the mandatory pro
visions of the Radiation Protection Rules (I971)- The AE"
RB Safety Code lays down the qualifications, certi
fications, duties and responsibilities of the RSO.
At an informal gathering of press persons and
interested members of the public in Jaipur recently
the problem of X-ray units operating in an uncon
trolled manner was discussed. The response was
varied- from curiosity to outright horror. Neverthe
less, this meeting did help to publicise, to some ex
tent, the magnitude of the problem. The consumer,
as it were, can be excused for not immediately sen
sing the gravity of the situation and his ignorance
of his right to safe medical diagnosis and treatment. After
all, X-rays cannot be seen and there are never any
immediate side effects; the chances of tissue damage
are small so that, in all probability, he will never be
affected. This is a most unfortunate and incorrect
attitude. Damage occurs years later, when the me
mory of an earlier X-ray examination is lost so that
the X-ray itself is unlikely to be incriminated as the
culprit. Going even further, it would be a difficult
task, indeed, for congenital defects in future gene
rations to be ascribed to "that X-ray that my great
great grandfather had". The villain in the Bhopal
tragedy was easy to pin down and the Indian public
still smells blood because methyl isocyanate s awe
some effects were there for all to see. X-rays may
be silent but they are no less lethal.
What can you, the public, do ?
1.
2.
3.
Do not suggest an X-ray to your doctor. Let him decide.
for the same. Ask for
Whenever you are asked to have an X-ray carried out yourself, ask your doctor the reason
much or sometimes even more
as
a safer alternative. An ultrasound of the kidneys, for example, often provides
information than an intravenous pyelogram.
....
grounds for it. If your
If you are pregnant, do not allow yourself to be X-rayed unless there are very, very strong
within 10 days of your period so that
t:._L an early pregnancy is not
abdomen is to be X-rayed, then have this done
external genitals when
inadvertantly jeopardised. Males should insist that a lead shield be provided to cover their
their abdomen is being X-rayed.
4.
radiographer
or radiologist does
’ » careful for his safety, much less yours,
the total amount of r-----------that personnel who are v._
r™
—
.... -
i...... x-..,....... a. x.„,....»........•»'<
5.
small child who is obviously
the patient, though on occasions it does become necessary for a parent to accompany a
scared stiff. Under no circumstances should you enter if you are pregnant, even to help ouh Let someone else do so. If
cubicle,
insist upon
being provided a lead apron to wear.
you have to be present with the patient in the X-ray c
-------- ------------.
6.
7.
Do not loiter outside X-ray units, Scattered
bcatterea rays can also kill^
kill.
under the Atomic Eneray
Find out if the X-ray unit has a Radiation Safety Officer (RSO)
Acu^'k^^o RSO covering the unit a complaint can be made in this regard to the health authorities and the
State Government.
_
1'
M R - R ' L( -p1 vt N D
A)<DVtuvJrl/v
T-C-v)
The report says: "in short, the unawareness
of radiation hazards, inadequate plan of installa
tion, poor performance standards of the equip
ment, lack of necessary protective devices, and
above all a commercialization of the use of X-rays
for medical diagnosis and consequent indiscri
minate use" are some of the major factors leading
to unwanted exposures.
The RESULTS of the prevalent improper use
of diagncstic X-rays are :—
1.
Excessive radiation
to be X-rayed.
dose to the individual
2.
Radiation of parts of the body other than
those required to be exposed to X-rays.
3.
Radiation to persons other than the patient.
The "WHO Manual of Radiation Protection
m Hospitals and General Practice" prescribes clear
cut guidelines for X-ray personnel (appendix) and
these norms have also been prescribed by the
AER5 in its safety booklet for diagnostic X-ray
units (AERB Code No : SC/MED-2. Safety Code for
Medical Diagnostic X-ray Equipment and Installa
tions) .
These safety measures are almost universally
ignored in India. Though the flouting of these
basic safety norms is so open and obvious, it
is most unfortunate that it does not attract the
attention of the health authorities.
Scattered X-ray Hazards to the General Public
When an individual is being X-rayed, a sig
nificant part of the beam is scattered in all direc
tions. These scattered rays affect not only every
individual inside the room but pass out of the
room because of their great penetrating power
and affect every individual outside and in the
vicinity of the unit, unless the scattered X-rays
are prevented from escaping the room by thick
masonary walls and lead-lined closed doors and
windows. Under the prevalent conditions and work
culture in the X-ray units of the country, many
more individuals than the patients X-rayed are expo
sed to ionising radiation escaping from these units.
Every one who accompanies the patient receives
small doses of radiation many times during their
stay inside or in the vicinity of the X-ray room.
Because of scattered radiation, for, 9
crore patients X-rayed every year in the ctry
there would be, at least, 18 crore others w^e
exposed to radiation unnecessarily. The riot
cancers and congenital anomalies to the ecessarily exposed health people are similito
that of the patients. The continuing prolifer^n
of "X-ray shops" in busy markets and pc
places are highly hazardous to say the l-t
Their potential danger and resulting harm shtj
not be underestimated or, worse still, overlook
Fantastic Risk from Bad Units
The genetic risk from an improperly operate
X-ray unit when compared to a properly manage
one is colossal. To quote a WHO document
The conclusion to be drawn from these re
suits is quite fantastic; they imply that a single
examination performed on person using a bad
technique has the same genetic consequences as
the same examination jperformed using a good
technique on 22,000 persons of the
...j same sex
and life expectancy."
Genetic Hazards
The genetic effects of X-rays are randomly
distributed and their clinical consequences are late
in occurrence. The changes they produce in germ
cells (sperms and ova) are either chromosome
mutation or gene mutation. While chromosomal
mutations are mostly lethal for the germ cells,
their only effect is a reduced birth rate. However,
some of these of chromosome mutations
-------------- > lead io
very serious hereditary diseases in the first
generation.
Gene mutations or point mutations are
"microscopically invisible changes in the structure
of DNA, the chemical substance responsible for
heredity. The majority of point mutations are re
cessive, and a hereditary diseass connected with
such a mutation will become evident only when
two germ cells (a male and a female) bearing
similar mutations unite by chance. The chance
of this event obviously depends on the muta
tions present in the 'gentic pool' rather than the
mutations in the germ cells of an individual
person. The genetic pool includes germ cells of
all individuals in the population who have a
given probability of becoming parents. Persons
9
1A
rvDV(:.ri nt K
BEWARE OF X-RAYS
THE DANGEROUS DIMENSIONS OF DIAGNOSTIC X-RAYS.
X-RAYS ARE HIGHLY HAZARDOUS : HANDLE THEM WITH CARE.
IMPROPERLY USED X-RAYS ARE DEATH RAYS
Dr. S. G. KABRA
It is plain to even the most crsual observer
that "Diagnostic Clinics" or "X-ray Clinics" pepper
the streets of urban, and a good deal of semi-urbam
India. More often than not, these clinics ara
independent of hospitals and have maoe X-ray
facilities as readily available as photocopying
services. In fact, there has been a phenomenal
increase in the number of diagnostic X-ray units
in xthe country. From an estimated 1C,400 units
in 1975, the number now exceeds 30,000, acco
rding to a report of the Bhabha Atomic Research
Centre (BARC). This proliferation of X-ray services
is apt to be regarded as " sign of progress"
and public awareness of X-rays is such that an
X-ray examination offers a tremendous psycho
logical boost to a patient much the same way
as an injection would. It is not infrequent fora
patient himself to suggest to his treating physi
cian that he be X-rayed and the compliance oj
the physician in this respect assures the patient
that his problem is receiving serious attent on I
Only individuals in the younger age groups
are considered since the effects of radiation are
Of the 9
manifest only decades after exposure.
crore persons X-rayed in the country in any given
year, roughly 55% or 5 crore are 30 years of age
or less.
★ Estimated number of diagnosti :
30,000
X-ray units in India
★ Presumed (for the sake of
:
10
calculation) that the number of
patients X-rayed per day per unit
★ Number of patients X-rayed
per day
:
30,000 x 10
—
300,000
300
★ Number of working days in
a year
What is not generally known is that diagnostic
X-rays todny constitute, as a whole, the biggest man
made source of ionising radiation, whose potential for
harm equals that of ionising radiation emanating from
a nuclear explosion. Judiciously and safely used
X-rays are, of course, of immense value in mo
dern medicine. Used otherwise. X-rays cause more
harm than good, not only to patients, but clso
to the public at, large and their future generations.
ionising radiation in any form and in any dose increases
the risk, in exposed persons, of developing cancer
and their progeny of being born malformed.
★ Number of patients X-rayed
per year
:
300,000 x 300
90,000,000
—
★ Number of such patients aged : 55%of 90,000,000
30 yrs or less
50,000,000
—
Below are the estimates of cancers and con
genital anomalies that would
occur in
these 5
crore persons in their lifetime and their progeny
respectively over and above
what
would
have
occurred had they not been X-rayed. Since the
Risk Estimates from Diagnostic X*rays
risks vary according to the type
For estimating such, the population X-rayed
in ONE YEAR is taken into account. It is pre
sumed that these persons will receive X-rays
only once in their lifetime.
of
X-ray and
the part of the body exposed, the different types
of X-rays that would have been carried out on
these 5 crore people are also presumed in these
calculations.
j
7
>
Type or Diagnostic
X-ray
Plain Chest and Ribs
Plain Abdomen
Barium Meal
Barium Enema
Oral Cholecystography
IVP
Hip and Femur
Lumbar Spine
TOTAL
Additional Cancers
Additional Hereditary
Defects
No: Persuns
X-rayed
(lakhs)
No: who will develop cancer
Bone
Breast
Marrow
(Women)
Additional
No : Hereditary Defects via
Mother
Father
Lung
130
10
39
26
10
10
120
72
12
10
576
288
30
39
15
2
120
15
30
45
6
24
162
51
40
12
4
3
10
2
50
25
135
7
500
200
50
25
3
3
220
900
50
40
30
7
380
120
500
268
244
82
1978
1586
: 594
: 3586
Note : These estimates are based on the following sources :
(I) UN Scientific Committee on the Effects of Atomic Radiation, Report to
the General Assembly.
United Nations, NY, 1977
(II) Diagnostic Radiography : What are the risks ? Drug and Therapeutics Bulletin 1980; 18.49-50
The above estimates are for X-ray machines
which are properly maintained and monitored, and
operated with all the prescribed safety precau
tions. The situation in our country, however, is
quite the opposite, according to a report of the
Division of Radiological Protection ( DRP ) of
BARC.
The DRP, entrusted with the task of sur
veying X-ray units in the country to detect, and
advise about, radiation hazards, found it impossible
to keep up with the explosive increase in the
number of these units.
ber 1983 is now estrused with the responsibility
of developing and implementing appropriate regu
latory measures aimed at ensuring radiation safety
in all applications involving ionising radiations
envisaged in the Atomic Energy Act, 1962.
The status of radiological protection in small
hospitals and clinics that constitute 95% of the
total diagnostic units in the country "is so poor
that most of the excessive
reported from them"
DRP.
exposure
cases are
says the survey report of
Though started in 1957, DRP had, till 1976,
surveyed only 9%, i. e. 946, of the estimated 10,400
X-ray units in existence at that time. The situation
has only worsened over the year.
are improper layout of these installations (85%
The Atomic Energy Regulatory Board (AERB)
constituted by the Government of India in Novem-
protection measures in 25% to 90% of the smal]
units.
The causes of excessive exposures detected
of the small hospitals
and clinics surveyed and
and 60% of [the large hospitals),
8
and
lack of
It
*
Q f'
rtt- cg-115
Emerging Medical Culture — i
pared to sputum acid fast tubercular bacillus, X-ray
chest gets a positive nod for investigating tubercu
losis of lungs; blood sugar estimation is considered
more sophisticated than simple urine sugar exami
nation; blood urea gets an upper hand for diagno
sis of kidney disorders when compared with urine
albumin and microscopy and urine bilirubin and
urobilinogen are seldom considered important when
compared to a battery of biochmical liver function
tests.
Too often investigations are advised with
out close scrutiny of the outcome that one expects
out of them. For a case of head injury X-ray skull
is quite often advised to judge brain injury, while
scientific data suggests that bedside examination
is a better guide and contribution offered by an
observable fracture of the skull in management of
a patient is nil. X-ray cervical spine is invariably
advised for suspected case of cervical spondylo
sis, while it is the clinical examination which alone
dictates the mode of treatment. And so on.
Out of a battery of tests available for pro
per diagnosis in a given patient, the clinician has
to select the accurate, safe and cheap procedure.
He must be aware of the inherent limitations of
each test i.e., the sensitivity of an investigative
procedure to pick up the disease and specificity
of the procedure for a definitive diagnosis of the
same disease.
Patholgical investigations, like planned ad
vertising campaigns, often create wasteful wants.
A doctor can earn much more from them than what
he can earn through a simple consultation. Ring
practice-in the current commercial medical jargonis acquiring new significance it had never assumed
before. A patient in the ring is just a defenceless
pawn—too meek to make a move — ’as he passes
through the check-posts of specialists, each squeez
ing his harde’arned money.
The human body is treated like a machine .
The human element in treatment of the patient is
fast vanishing. We have learned to look at the
heart, kidney, liver........ and have forgotten the
human being who harbours all of them.
How relevant are those immortal words of
Sir Robert Hutchinson in this context:
From inability to let well alone;
From too much zeal for what is new
And contempt for what is old.
From putting knowledge before wisdom
Science before an art, and cleverness before
common sense;
From treating patients as cases;
and from making the cure of the disease
more grievous than its endurance
Good Lord deliver us!
Ulhas Jajoo
Too Miusy Investigations:
Open up any text book of modern medi
cine, and you find^ a growing, rapidly enlarging,
list of investigations. Take any disease from com
mon cold to cancer and you see a physician order
ing a battery of investigations. Being trained in
the traditional western style of medical education,
a young medico lends a deaf ear to the patient’s
history, turns a blind eye to the vital examination
and relies entirely on complex investigations as
if they would, like Aladdin’s lamp, always solve the
clinical problems, With computers having already
made a significant dent in medical technology a
day is not far off when blue chips would replace
human grey matter. Let us start with a simple in
vestigation—an electrocardiogram. A basic investi
gation for recognising various heart diseases. ‘We
must not forget however, that an electro-cardiogram
does not solve all the problem’, writes J. Willis
Hurst in his magnum opus of cardiology.’ and
tliat many problems may be created by its use’,
(emphasis my own). Nothing can be more of an eyeopener than the view of Frank Wilson, father of
modern electrocardiogaphy who writing the preface
of his son-in-law’s book in 1951 warns:
Tn the last two decades, there has been a
tremendous growth of interest in the ECG diagno
sis and the number and varieties of ECG in use.
In 1914, there was only one instrument of this
kind in the state of Michigan and this was not in
operation; there were no more than a dozen ECG
machines in the1 whole United States. Now there is
one or more in about every village of any size, and
there are comparatively fewer people who are not
in danger of having their peace and happiness
destroyed by an erroneous diagnosis of cardiac ab
normality based on faulty interpretation of an
EGG than of being injured or killed by an atomic
bomb.’
Frank Wilson’s prophecy is certainly sound
ing true in 1984. An ECG strip, innocent and im
pressive though it appears, is capable of stripping
the poor man’s money, happiness and tranquility.
Roentgen rays are no longer the rays of hope to a
diseased patient. The indiscriminate use of Roent
genology may offset the very advantages it offers.
Come what may, an X-ray occupies the num ero uno
position in diagnostic work up of a busy practitioner,
who believes more in Roentgen’s tubes than on
Laennec’s stethoscope.
‘Look before you leap to a lab’ should be
the most candid advise to a busy practitioner.
The phenomenal rise in laboratory investigations
in the last decade reflects the blind faith of doc
tors in’ the numbers game.’ The sufferer is the
ordinary man. In his vain hope to get rid of suff
erings, he spends his hard-earned money over un
necessary investigations which do not have a be’aring
on his treatment. Simple investigations which pro
vide important clues to the diagnosis are ignored
while costly investigations are advised. Thus com-
Dept, of Medicine, MGIMS, Sevagramu
(Extracted from an article written by tha
author for creating awareness in the lay media. The
article is entitled— The Emerging Medical Culture).
5
Position: 3962 (2 views)