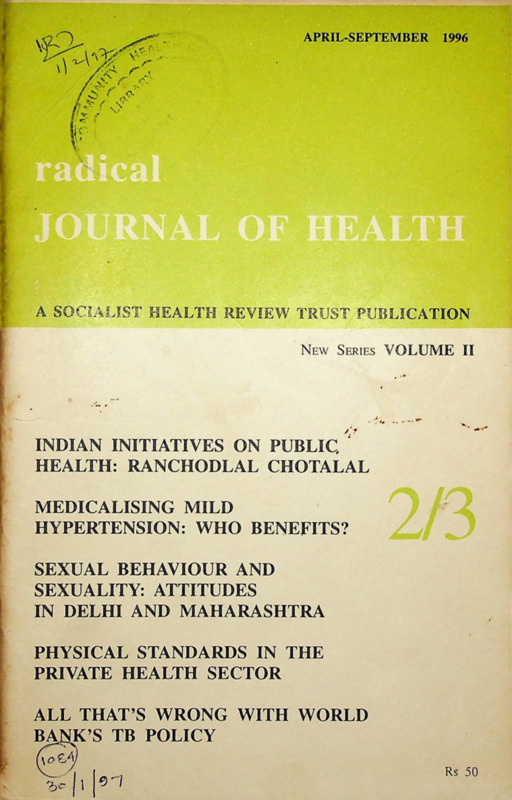
Radical Journal of Health 1996 Vol. 2, No. 2/3, April – Sep.
Item
- Title
- Radical Journal of Health 1996 Vol. 2, No. 2/3, April – Sep.
- Date
- September 1996
- Description
-
Indian initiatives on public health: Ranchodlal Chotala
Medicalizing mild hypertension: WHO Benefits?
Sexual behaviour and sexuality: Attitudes in Delhi and Maharashtra
Physical standards in the private health sector
All that’s wrong with world bank’s TB policy - extracted text
-
APRIL-SEPTEMBER
1996
A SOCIALIST HEALTH REVIEW TRUST PUBLICATION
New Series VOLUME II
INDIAN INITIATIVES ON PUBLIC, ''
HEALTH: RANCHODLAL CHOTALAL
MEDICALISING MILD
HYPERTENSION: WHO BENEFITS?
SEXUAL BEHAVIOUR AND
SEXUALITY: ATTITUDES
IN DELHI AND MAHARASHTRA
PHYSICAL STANDARDS IN THE
PRIVATE HEALTH SECTOR
ALL THAT’S WRONG WITH WORLD
BACK’S TB POLICY
(u>£/y
Rs 50
'b
Consulting Editors:
Amar Jesani.
CEHAT. Bombay
Binayak Sen, Raipur, MP
Dhruv Mankad,
VACHAN, Nasik
K Ekbal,
Medical College, Kottayam
Francois Sironi, Paris
Imrana Quadeer,
JNU, New Delhi
Leena Sevak,
London School of Hygiene and
Tropical Medicine, London
Manisha Gupte,
CEHAT. Pune
V R Muraleedharan,
Indian Institute of
Technology, Madras
Padmini Swaminathan,
Madras Institute of
Development Studies, Madras
Sandhya Srinivasan,
Harvard. USA
C Sathyamala. New Delhi
Thelma Narayan,
Community Health Cell,
Bangalore
Veena Shatrugna, Hyderabad
The Radical Journal of Health is an
interdisciplinary social sciences
quarterly on medicine, health and
related areas published by the Socialist
Health Review Trust. It features
research contributions in the fields of
sociology, anthropology, economics,
history, philosophy .psychology,
management, technology and other
emerging disciplines. Well-researched
analysis of current developments in
health care and medicine, critical
comments on topical events, debates
and policy issues will also be
published. RJH began publication as
Socialist Health Review in June 1984
and continued to be brought out until
1988. This new series of RJH begins
with the first issue of 1995.
Editor. Padma Prakash
Editorial Group: Aditi. Iyer, Asha
Vadair, Ravi Duggal, Sandeep
Khanvilkar, Sushma Jhaveri,
Sunil Nandraj, Usha Sethuraman.
Production Consultant: B H Pujar
Publisher: Sunil Nandraj for
Socialist Health Review Trust.
All communications and
subscriptions may be sent to :
Radical Journal of Health,
19, June Blossom Society,
60-A Pali Road, Bandra,
Bombay 400 050.
EMail: rjh@nrp.ilbom.emet.in
Typsetting and page layout at the Economic and Political Weekly.
Printed at Konam Printers, Tardeo, Bombay 400 034.
Volume II
New Series
Numbers 2/3
April-September 1 996
Letter to Editor
94
Editorials: Shocking Negligence
Padma Prakash
Is Social Insurance Around the Corner? Ravi Duggal
Ranchodial Chotalal: Pioneer of Public Health in Ahmedabad
Mridula Ramanna
99
Sexuality: Differing Perceptions
Mira Savara, C R Sridhar
113
Sexual Behaviour of Women in an Urban Resettlement
Colony in Delhi
Tania Nayar, S C Chawla
133
Physical Standards in the Private Health Sector
Sunil Nandraj, Ravi Duggal
141
Communications
Medicalising Mild Hypertension
Who Benefits?
Anil Gurtoo
185
Discussion Paper
World Bank’s Blind Spot
Revised National Tuberculosis Control Programme
Debabar Banerji
*
189
Facts and Figures
193
RJH
(New Series)
Vol II: 2/3
1996
Letter to Editor
Appeal for Medical Equipment
THE Sambhavna Trust is a registered charitable trust set up for the
welfare of the survivors of the December 1984 Union Carbide disaster
through medical care, research, education and information dissemcnation.
The initial funds for the activities of the institution which have been
set up have been raised through individual contributions . Efforts are
on to generate more resources. The trust has set up a clinic with a
complement of allopathic, ayurvedic doctors, a yoga instructor and health
workers and a documentation centre. We are desperately in need ol
equipment for diagnosis and rehabilitation of people who come to us
for help. We cannot afford to buy these. We would be grateful for
donations of used equipment as long as they are in working condition
The following arc urgently needed: Pneumoscope for lung function tests;
bronchoscope for internal examination of lungs; slit lamp apparatus:
duedenoscope: electrophysiological equipment; light optical microscope
with camera attachment. We also need a computer system for installing
apatient record system. If you can help us please contact the undersigned.
We would be happy to answer any queries regarding the clinic and its
functioning too.
Satinath Sarangi
Bhopal People’s Health and Documentation
Centre,44, Sant Kanwar Ram Nagar
Bhopal 462 01
Telephone: 0755-530914
Subscription Rates
Inland
(In Rupees)
two years
five years
life
360
1000
Individuals
180
—
—
3000
Institutions
(In US S)
Foreign
All other countries
Asia(excluding Japan)
Africa and Latin America
one year
one year
two years
25
25
Individuals
15
60
Institutions
30
50
Remittances may be by cheque or draft and may be made out to Radical
Journal of Health. Please add Rs 20 for outstation cheques. Subscriptions
rates are per volume and will begin with the first issue of the volume.
one year
100
150
94
RJH
(New Series)
Vol 11:2/3
7996
Shocking Negligence
For all the committees and their recommendations the FDA remains
bogged down in bureaucratic tangles; its unconcern for the consumer
and the unstated bias towards industry' becoming increasingly evident.
THE pathetic lack of control the FDA has over drug companies has been
amply demonstrated by recent events with regard to the contaminated
tablets of Comsat Forte manufactured by Boehringer Mannheim. The
tablets, a widely used, broad spectrum antibiotic combination of
sulfamethaxozolc and trimethoprim distributed to patients who had
undergone cataract surgery al an eye camp at Ahmednagar on August
16 produced adverse drug reaction and more than 62 people had to be
hospitalised three days after. Incredibly,the FDA which seized the
remainder of the drugs, made no move to make public this information
or order a stoppage of sales of the drug until further investigation. It
took almost 15 days to analyse the material: the tablets were found to
have been contaminated with an anti-diabetic drug, glibenclamide which
drastically reduces blood sugar levels and is administered to diabetics.
Only then did it issue a notification to Boehringer Mannheim India to
recall the drug within 72 hours. That the contaminant which can cause
hypoglycemia is potentially life threatening was publicly acknowledged
by the FDA commissioner.Yet when the company pleaded its inability
to set the recall process in motion in 72 hours, it was granted an extension.
There were al lhai lime, over four lakh tablets in the market in India.
(liven the fact that it was a widely used drug and that in India an adverse
drug reaction machinery docs not exist, an immediate alerl should have
been sent out with notices in the media warning people about Comsat
1 orte. Nothing of that sort was done—instead, the company (and it would
jppear the FDA) did its best to keep the issue under wraps.
Meanwhile the company set in motion its own outflanking man
oeuvres. It made several confusing public statements; most importantly
that its own tests ofcontrol samples did not reveal anything incriminating.
But even by September 5, the extended deadline for recall, it was reported
that 20 per cent of the tablets were still in circulation.
Meanwhile, in Kolar at yet another surgical camp for cataract treat
ment, two people died and 11 others became seriously ill after consuming
ihese tablets. Il remains and probably will remain a mystery how these
tablets were purchased after presumably the recall notices had been sent
by the company to all its distributors.
Another lethargic nine days passed before the FDA decided to issue a
show cause notice to the company seeking an explanation about the
contaminated tablets. Only on September 21, almost a month after the
RJH
(New Series)
Vol ll: 2/3
1996
95
adverse reactions were reported did the company hah production of its
entire Thane unit near Mumbai, one of those manufacturing Comsat
Forte. Why did the FDA not insist on the company issuing a notification
about the product immediately in the media? Secondly, clearly the
company did not act in the interest of the consumers: even i f the tests that
it had conducted contradicted the FDA's findings, as a measure of safety.
resorted to by other companies in similar situations, it should have, if
public safety was a concern, made the facts known to the public ai
whatever cost. Would the situation have arisen in the home country of the
MNC where both public reaction and the state machinery would hawensured othcrwise?Fourthly, had the FDA and its inspectors been doing
their job would such a situation have arisen? Was Boehringer Mannheim
following the good manufacturing practices which the drug controller.
the industry and especially the OPP1 and the MNCs have been so
vociferously advocating? The MNC's old argument has been that no
Indian company, certainly not small ones, can match the quality control
of MNCs. In the circumstances, one can only hope that it is true.
A glaring feature in all this is the lack of concern for the consumer.
those who were taken ill and those potentially at risk of consuming the
contaminated tablets. Neither the MNC nor the FDA issued any public
notification warning the people against purhasing the drug. Nor for that
matter was any notification issued to public hospitals who may have bulk
purchased the drug.
-Padma Prakash
Is Social Insurance Around the Corner?
While the centre has made some provision towards the beginnings
of social insurance, they may remain only on paper, yet.
UNDER the new dispensation at the centre Insurance and Sickness
Funds, which were the beginnings of universal coverage today in many
western countries, are being mooted for the first time in government
policy and budgets. In the 1996-97 budget a small beginning has been
made. First, a National Illness Assistance Fund with a corpus of Rs 50
million has been set up and this fund is expected to attract other fund''
since contributions to it will give the donor 100 per cent tax deduction.
Similarly, another Rs 250 million has been allocated to enable stale
governments to set up similar funds in the stales.
These funds will provide assistance to lhe poor for surgeries.
hospitalisations and ireatment of catastrophic illnesses such as heart
diseases, kidney problems, cancers, AIDS etc. While such a provision is
96
RJH
(New Series)
Vol 11:2/3
7996
welcome, the problem is how will the poor (the criteria for eligibility) be
identified ; will its fate not be similar to other such programmes like IRDP
where this will become a system for granting largesse? Inevitably it will
become another money-making device for politicians and bureaucrats.
The target set must necessarily be the entire population so as to avoid any
screening process, and of course those who have the capacity to pay must
do so indirectly through systems designed to collect revenues on a
progressive basis. As yet, this scheme is only on paper and with a measly
allocation. One has to wait and see how it gets implemented in the states—
especially in states where the coalition partners are in power. Further,
hospitalisation is only one aspect of health care, no doubt the more
pauperising one as indebtedness surveys have amply shown. But the
requirements for treatment of minor ailments is as important, and for the
poor here too there is severe indebtedness but it does not show as
dramatically as the one for hospitalisation.
Second, the budget has roped in the GIC to come out with a voluntary
insurance plan called Jan Arogya wherein for an annual premium of Rs
70 an individual can get a cover of upto Rs 5000 for medicare (and a
family of four a cover of Rs 20,000 with a premium of Rs 240). The
scheme sounds interesting, especially for the middle classes, but its
details too are not as yet available. Will it cover all routine illness care ?
If the answer to this is yes then I think this is a radical step in health
insurance and could become the foundation stone for universal social
insurance in India. Further, if all routine care is covered then the state
governments must be made to pay for atleast half the population who fit
an objective criteria of poverty — agricultural labourers, marginal peas
antry, the unemployed, the urban daily wager, etc — and the other half can
contribute through taxes, levies, etc on a progressive scale. But again one
has to wait for this scheme to be finalised.
And it is precisely this absence of the mechanics of the schemes which
makes one feel that these schemes could be mere eyewash. Past experi
ence shows that the bureaucracy will be unable to deliver the goods as
envisaged by policy. However, for those who work in the arena of
advocacy for the problems of the poor another stick is now available to
beat the stale with. Another positive impact is that the debate for a more
progressive health insurance policy will get a boost and studies and
research on these issues will be undertaken with a new enthusiasm.
So far nothing has been said about private insurance and the recom
mendations of the Malhotra Committee but this is something which is
impending and it will be difficult for even this government (even though
backed by communist parties) to prevent such insurance from coming in.
Therefore it is extremely important for public insurance to set up the
benchmarks for health care insurance which are strongly equitable and
pro-poor.
RJH
(New Series)
Vol II: 2/3
1996
97
Finally, large scale insurance would also imply regulation and controls
over the functioning of the private health sector. There is nothing so far
in the offing. Even the process of adopting the Nursing Home and
Hospitals Regulation Acts in their present toothless form is very slow as
is evident in the recent attempt of the Bihar government in pushing
through this bill where the private health sector is up in arms against
passing of this Act. All said and done, without any comprehensive
measures which tackle the totality of health care issues, health care for all
will only remain a dream.
Ravi Duggal
Subscribe to
Medical Ethics
Journal of Forum for Medical Ethics Society
A quarterly publication dealing with ethical issues in
medical practice and health care services.
Subscription rates:
Inland
one year
two years
life
Individual
60
100
1000
Institutional
100
150
2000
International:
Developed Countries: (Annual) Individuals: US $ 15
Institutional: US $ 20
Developing countries: (Annual) Individual: US $ 10
Institutional: US $ 20
(Two years)lndividual: US $ 20
Institutional: US'$ 40
Cheques/MOs/Drafts in favour of Forum for Medical Ethics. Add
Rs 20 for outstation cheques.
Send subscriptions to 310 Prabhu Darshan, S S Nagar,
Amboli Andheri(W), Bombay 400 O58.Tel/Fax: 625 0363.
98
RJH
(New Series)
Vol II: 2/3 . 1996
Ranchodlal Chotalal
Pioneer of Public Health in Ahmedabad
Mridula Ramanna
Indian response to western ideas of sanitation under colonial
rule were not always negative as has been generally assumed. The
efforts of Ranchodlal Chotalal, the chairman of the Ahmedabad
Municipality and a textile magnate in the last two decades of the
19th century provide a glimpse of a different dimension in the
interactions between the colonial powers and Indians.
THIS paper focuses on the efforts of Ranchodlal Chotalal, chairman of
the Ahmedabad Municipality and a textile magnate, in promoting public
health measures in that city in the last two decades of the 19th century.
He campaigned for a better water supply and sewage system in the face
of opposition from Ahmedabad’s citizens, including leading educated
reformers and the public. His initiative is significant as it shows that
Indian responses to western ideas of sanitation were not always negative,
but ambivalent. In other cities there had been resistance. Thus Indian
Municipal Commissioners in Bombay city, supported by the health
officer, Thomas Blanery, had opposed the underground drainage system
for financial and socio-religious reasons [ 1 ]. The Sanitary Commissioner
of Bombay considered the apalling sanitary condition of Nasik to be
an “index of the little interest” that the Municipal Commissioners took
“in the sanitation of their picturesque city” [2]. The Madras Municipal
Council’s scepticism of the efficacy of certain medical interventions has
been shown by V R Muraleedharan and D Veeraraghavan [3]. In this
context, Ranchodlal Chotalal’s contribution is important.
Ranchodlal also funded dispensaries in the city for the poor and for
women and children. Indian Philanthropists had financed medical facili
ties in Bombay Presidency since mid 19th century. Premabhai Huttesing
and Bechurdass Ambaidass had established a hospital and dispensary at
Ahmedabad earlier. Medical Philanthrophy has been seen as “a part of a
strategy of accommodation” with the ruling power [4]. Ranchodlal’s
anxiety to start the Victoria Jubilee Dispensary for Women and Children
in the year of Queen Victoria’s Jubilee is apparent in his correspondence
with the Collector of Ahmedabad and the government of Bombay. He had
been made CIE in 1883 and given the title of Rao Bahadur. Nevertheless,
his concern for improving his city and his pursuit of this goal, single
handedly, is noteworthy.
Ranchodlal was born in 1823 in a nagar brahmin family. He received
elementary education in Gujarati and then studied Persian and English
RJH
(New Series)
Vol II: 2/3
1996
99
with Rao Bahadur Bhola Nath Sarabhai. He continued his studies at the
Subscription English School, a private institution, maintained by a
Portuguese gentleman. Like other English educated young men of his
time, Ranchodlal entered government sService as a clerk [5] He rose
swiftly to be daftardar and assistant political agent [6] Subsequently
Ranchodlal left government service and joined the mill as a Manager. He
soon became a leading cotton manufacturer and entrepreneur. He made
a large fortune, and came to be regarded in the words of his biographer as
“the father of the mill industry”. He was nominated a member of the
Ahmcdabad Municipality in 1869, chairman in 1883 and president two
years later [7].
It was as chairman that Ranchodlal prepared an elaborate memoran
dum, dated December 8, 1883, on the deteriorating public health in
Ahmcdabad; and made suggestions to be circulated among his colleagues
in the corporation. He compared the city’s high mortality rate, with other
cities’ in the Presidency: while Ahmedabad’s death rate was 44 per 1000
in 1880-81, Bombay’s was 27.87 Poona's 25.1 and Calcutta’s 30 per
1000. Ahmedabad had the dubious distinction of having the highest
number of deaths from fever in the same years too, viz. 35.65 per 1,000.
as .against 33.96 in Kanpur, 8.60 in Calcutta and 8.29 in Bombay [8].
The high mortality rates and the poor sanitary condition of Ahmedabad
had been repeatedly pointed out by the Collector, Alfred Borradaile since
1874. He had represented before each Governor who visited the city [9].
Subsequently, the Sanitary Commissioner, Hewlett made an adverse
report, which was widely circulated, on the preponderance of fevers in the
city, in contrast to Bombay. He recommended the appointment of a health
officer Borradaile piqued by the report, contended that there was nothing
to prove Ahmedabad was “exceptionally unhealthy” and that any com
parison with Bombay was fallacious. He pointed out that despite its sweet
water, pure air, wide streets, qualified health officer and controlled
cremation ghats and graveyards, hundreds were dying of cholers in
Bombay. Besides, Bombay had a large floating population of men in the
prime of life who went there, to seek their fortunes, and relumed home to
die [ 10]. However, the British officials were in agreement on the fact that
the poor supply and deficient sanitation were responsible for the high
death rates in Ahmedabad.
Water Supply and Drainage Schemes
Ranchodlal analysed these issues in detail in his memo. He held that
with a large river like the Sabarmati, a tank like the Kankaria (with a depth
of 10 feet and an area of 72 acres) and good potable spring water and wells,
Ahmedabad had an abundant supply of water, but of poor quality. The
sewage from houses was collected in cess pits or khalcooas, which were
100
RJH
(New Series)
Vol //: 2/3
J996
dug close to the houses to a depth of 15 to 20 feet. Houses, since the sub
soil was porous, the khalcooa water found its way into the water supply.
The well and spring water was also polluted by the khalcooas. The river
water was used for bathing and for washing and cleaning of animals,
making it unclean [11] A pumping plant had been erected in 1847 from
the City Walls Restoration Fund, Four years later, piped supply, pumped
by the Persian Wheel provided water from the river.
This had proved to be ineffective. Other schemes had been put forward
by Hatherly in 1876, Borradaile in 1878, Potlinger (Executive Engineer
for irrigation in Gujarat) also in 1878, Playford Reynolds in 1883, and
Executive Engineer, S B Doig in 1884, but these had not been imple
mented [12], One hundred and thirty three thousand gal Ions of water were
raised by steam pumps from the river Sabarmati but the spot selected for
water was at the lowest point of the town, where the river had already been
fouled by the washing activity upstream. The water was raised at night by
two small engines of five and six horse power, respectively, when the
river was relatively less free of impurities. After being raised, the water
passed through a filter tank and was distributed partly by earthen pipes
and partly by iron pipes [13]. However, this was inadequate and a great
number depended on cisterns, underground reservoir or tankass, in which
inhabitants stored water during the monsoons [14].
According to Ranchodial, the problem could be tackled through more
efficient filteration of river water as had been done in the River Hooghly
at Calcutta. Since there was a spring in the neighbourhood of the city, he
recommended that a well, 63 or 78 feet in depth, could be sunk. Besides,
there were the tankass, wherein people stored rain water, which had been
found to be superior to river or well water on chemical analysis. There
fore, all that was needed was for that these be cleaned out [15].
As for drainage, Ranchodlal contended that there was ‘no system’ at
all. In 1872, the Municipality had prohibited the construction of deep well
privies and in 1879, closed the existing ones [16]. There were only the
khalcooas. He estimated that out of 41,000 houses in Ahmedabad, 8,800
had khalcooas and the remainder no privies al all [17]. Those houses
which had no provision for removal of sewage, threw it in front of their
houses. Since the lanes on which they were situated were narrow, the
sun’s rays did not reach them. As a result, dampness prevailed in the
locality and malaria was rampant. The marks of decay visible in the walls,
in the bricks and chunam were called loona, locally, and was proof of the
‘unwholesome’ state of the sub soil. He endorsed the suggestion of the
Army Sanitary Commission that the khalcooa system should be replaced.
Some arrangements had to be made to carry away sewage for those who
had no khalcooa through public toilets, stricter sanitary inspection, use of
disinfectants, re-location of night soil depots and town sweepings, from
their position at the Jamalpur and Shahpur gates to a distance of two miles
RJH
(New Series)
Vol 11: 2/3
1996
101
to the south-east of the City and the construction of a light railway, as at
Amritsar, to carry them there. His other suggestions included filling up of
hollow spaces near city walls where water stagnated, the removal of
offensive trades, the widening of narrow streets and the regulation of
cattle stables. He pointed out that while the principal roads were well
drained and metalled, the roads in thepols were unsatisfactory. They were
devoid of even surfaces and storm water drains. Being constantly sodden,
they were “a fertile soil for cholera” [18]
The other issue Ranchodial tackled in his memo was the density of the
population in the city. He suggested that the evils of overcrowding could
be explained to the people through tracts and lectures. The government
and the municipality could adopt the following measures:- (1) induce
people to build houses outside the city; (2) not sell land located in
overcrowded places; and (3) open up new spaces and thoroughfares. His
suggestions also included welfare schemes, viz. the building of chawls for
the poor and provision of medical facilities for the poor middle castes,
who out of prejudice and honest pride, could not afford to pay for
competent medical attendance and were unwilling to go the hospitals
used by the ‘poor’ [19].
Ranchodlal also estimated the cost of these improvements at Rs
15,00,000 and recommended that the Municipality could obtain a loan for
this amount at five per cent interest, repayable in fifty years. To meet this
expenditure, he proposed a special tax amounting to twelve annas per
head which, he contended, would be less than what they would have to
pay for the upkeep of khalcooas and tankas [20] To prevent the cess from
being a burden on the poorest, he suggested that the Municipality should
make a general valuation of all immovable property in the city and
regulate the incidence of the tax on the basis of that valuation. He appealed
to the Government to advance a loan by conceding to the municipality the
right to receive sale proceeeds of the occupancy rights of all unoccupied
lands within municipal limits, and by paying the Municipality compen
sation for the loss of octroi fees on country liquor, which had resulted
from the government acquiring the monopoly over liquor in 1881 [21].
While appealing to his fellow Commissioners and the people of
Ahmedabad to take seriously the subject that involved the lives of
thousands of citizens, he recognised that the question of funds might
come in the way. However, he said that “when the importance of the
subject is well understood, I hope the difficulty will soon be removed
[22]. The memorandum had been prepared by Ranchodlal after taking
into account the experience of other cities. He consulted the lectures of a
sanitary officer of Manchester, who had proposed that the old sewers
should be used for surface water and new watertight sewers for liquid
refuse, which could then be conveyed to farm lands. Many English towns
had carried out this system. He referred to a Gujarati essay on agricultural
102
RJH
(New Series)
Vol 11:2/3
1996
improvements, wherein the use of human manure had been suggested
[23]. He also visited the Calcutta exhibition and got estimates from firms
which had built the light railway in the Punjab [24]. Ranchodlal had even
corresponded with Florence Nightingale who was in contact with Lord
Reay, Governor of Bombay, about the Bombay Village Sanitation Act,
which aimed at educating each village on sanitary matters [25].
Responses to the Schemes
The Sanitary Commissioner commended Ranchodlal’s memorandum
as a “remarkable document for a native gentleman’’ as it exhibited, “a
breadth of view and a masterly appreciation of some of the main question
that affect public health in that city” [26]. The Army Sanitary Commis
sion also hailed it as a remarkable Sanitary report, which threw additional
light on the cause of fever in Indian towns [27] It was more difficult
convincing Ranchodlal’s colleagues in the Municipality and continuous
meetings of the Managing Committee were held in the first year of his
office. He succeeded in obtaining sanctions for certain improvements like
dealing with street sweepings and garbage, the construction of open
gutters to carry away storm water and the erection of reservoirs of water
for use by cattle [28].
At Ranchodlal’s request, the Bombay Government used the services
of Col. Walter M Ducat R E, who was Executive Engineer, Poona. Ducat
made suggestions to improve the water supply and recommended the
establishment of an underground drainage scheme.29 Ducat’s plans were
received with great hostility, both by Ranchodlal’s fellow Municipal
Commissioners and the public, who regarded the proposals as impracti
cable and expensive. Daily protest meetings were held, presided over by
Ranchodlal ’s opponents. The press fanned the opposition. Despite rumours
that there would be violence if he went to the mass meeting at Tanksal to
protest against the plans, Ranchodlal braved the hostility and attended.
However, he was refused a hearing and, according to his biographer, was
pelted with garbage and stones, and had to be escorted home by the police
[30]. In June 1886, the report was rejected by the Municipality. Gillian has
attributed the opposition, to religious prejudice (since piped water supply
would be available to all) to jealously of Ranchodlal and to a fear that
increase in taxes would follow the introduction of these schemes. The
opponents included leading social reformers like Mahipatram Rupram
and others like Kewasji Mancherji Karanjawala, Bechurdass Ambaidass,
Padshahi Diwan Mirza Najaf Ali Khan, Valade Mirza Nawab, Ardeshir
Kewasji Karanj-Awala, Maganlal Sarupchand [31].
Ranchodlal had gathered the views of Dr Blaney, Bombay’s Health
Officer, who had opposed a similar suggestion in the Bombay Municipal
Corporation. Blandey had, in a letter to the Bombay Gazette, shown the
RJH
(New Series)
Vol II: 2/3
1996
103
unfavourable results of the system when it was implemented in Kamtipura.
In his reply to Ranchodlal. Blaney had referred to the deaths of four
labourers from asphyxiation, when they had been sent down to clean out
a sewer only nine days after its construction. Besides, the system most
suitable to Ahmedbad had to be worked out with reference to that city’s
needs [32].
In order to convince his colleagues about the value of the rejected
proposals, Ranchodlal even improvised a water supply scheme from the
Sabarmati for his own mills, laid down small drainage works and a model
farm in the compound of his house. But his opponents remained adamant
and received unexpected support from Sir Theodore Hope, who was
formerly Collector of Ahmedabad and, al the time, a member of the
Viceroy's Executive Council. Hope wrote a long minute from Simla in
October 1886, condemning Ducat’s schemes. His views were circulated
in Ahmedabad and published in the Bombay Gazette. He recommended
the removal of sewage by hand and the surface removal of sullage.
Ranchodlal realised that Hope had been misled by hasty generalisations,
based on the different conditions at Lahore, and defended his proposals
in an elaborate memo, which was circulated among his colleagues and the
public. He wrote letters to the press, countering the theories of his
opponents and justifying Ducat’s schemes. Ducat himself wrote a caustic
refutation of Hope’s views [33].
Regarding improvements to the water supply, Ducat had recom
mended a more efficient use of the Sabarmati, though Doig had been in
favour of bringing water from Kharee, a smaller river. Ranchodlal studied
the relative costs and showed that if twenty gallons of water was the
requirement per head, there would be a saving in the Sabarmati project.
which would cost Rs 20,594; while the Kharee project, would cost Rs
45,880. Ducat had emphasised the need for ventilation in the water
channels, based on his knowledge of Kolhapur, where four men, sent to
clean out the channels containing pure drinking water, were killed as the
air inside had become deadly. Hope too had favoured the Sabarmati as the
source of water supply and preferred iron over masonry for pipes. He also
suggested that reservoirs should be constituted in distinct sections each of
moderate size [34]. Ranchodlal followed Ducat’s suggestion by sinking
a trial well, 25 feet in diametre in the river bed at Dudheswar, and
demonstrated that double the daily quantity of water could be raised by
machinery from a single well [35].
After a long discussion, the Municipal Commissioners passed a
resolution, 16 to 10, moved by Professor Abaji Visnu Kathavate and
seconded by Hugh Fraser that a modified version of Ducat’s scheme be
adopted [36]. A well was constructed in the bed of the river at Dudheswar
at a cost of Rs 10,000. The object was to get naturally filtered water and
save the expense of the construction of filtering and settling beds [37].
104
RJH
(New Series)
Vol 11:2/3
1996
The cost was raised from Rs 500,000 estimated by the sub committee, to
Rs 600,000 to provide for iron pipes of a larger diametre. In April 1887,
the Municipality gave its approval to raise the loan of Rs 600,000. The
Bombay government gave its sanction quickly but the Government of
India passed its orders only in May 1888. The work commenced in March
1889. On June 1891 the Governor of Bombay, Lord Harris, opened the
completed works which comprised of a pumping plant capable of supply
ing, in 12 hours working, 1,300,000 gallons of water and 51 miles of
piping. On completion the cost came to worked out to Rs 7,50,000 and
was carried on, under the supervision of Doig and his assistant Fardunji
of the Public Works Department. A second high level reservoir, with a
capacity of 318,000 gallons was built subsequently and a third, in 1898,
which could deliver 1800 gallons per minute to the high level reservoir
[38].
The question of drainage proved to be more contentious. The system
of removal of night soil, by hand, to the Jamalpur and Shahpur gates was
replaced by its removal, in a tram, to a place outside the city walls, known
as Bagh Firdaus. As president of the municipality, Ranchodlal reported,
with great satisfaction, that the number of deaths had consequently
reduced from 6729 in 1885 to 4773 in 1886, particularly noticeable in the
areas, where the night soil depots had been located. The labour of the
bhangis had been reduced to keeping the privies clean [39]. A sub
committee, which was appointed in November 1886 to discuss the
question, recommended the removal of sullage water by pipes as a
temporary measure. The municipality declined to sanction this proposal
and declared its support for Hope’s suggestion of removal of sullage by
hand. However, the collector, commissioner of the Northern Division, the
Sanitary Commissioner and the Government of Bombay rejected the
suggestion as expensive and inefficient. Another sub-committee ap
pointed by the municipality, recommended, in its report of 1887, a system
of main drains or sewers to carry off sullage water from the city. However,
this was not accepted by the Municipality who reverted to their original
proposal of removing sullage and foul water by hand. The Government
emphatically rejected this move and issued a resolution requiring the
Municipality to implement this underground drainage scheme [40].
Since a number of members voted in favour of the proposal, the local
press alleged that the commissioners had been pressurised td do so.
Among the papers were the Gujarati, the Ahmedabad Times, Gujarat
Gazette, Hitechu, Bombay Samachar, Gujarat Darpan, and Yajdan
Parast. The Nyayadarshak, Praja Mat and Ahmedabad Times even
welcomed rumours of Ranchodlal’s resignation from Presidentship of the
Municipality which were, however, untrue [41]. The citizens then sub
mitted a petition to the Viceroy claiming that the Government resolution
infringed on their rights to self government. The petitioners maintained
RJH
(New Series)
Vol II: 2/3
1996
105
that underground sewerage was yet a matter of experiment, even in
England, and experts were disagreed as to its value. In Calcutta, the
sewerage works had not proved “an unmixed good". They contended that
unless the trapping in ever)' house connection and street opening was
completed, an underground drainage system was sure to become a
nuisance and an active source of disease. The petitioners supported the
removal of sullage by a pail system which had long worked in Manchester
and Glasgow. The petition was approved of by Hope, Blaney and others.
signed by 7,000 persons and adopted at a public meeting [42]. The Rast
Goftar, in a newsletter from Ahmedabad, noted that except for some
agitators, very few in Ahmedabad cared whether the drainage works were
constructed or not. It held that those who wished to push forward their
names to public notice, pretended that they had consented, owing to the
threats held out by the new collector, James and by the City Magistrate
Dastur Firuz [43]. The petitioners decided that a deputation should
proceed to Calcutta to meet the Viceroy and to explain how difficult and
impractical was the scheme. However, it seems that their inability to
procure a map led to the plan being dropped. The Governor General, in
his reply to the petition, declined to interfere with the Bombay
Government’s Orders [44].
Since many adverse opinions had been expressed against underground
drainage, it was decided that the system be tried, in a part of the town,
before making further extensions [45]. Designs were made by Baldwin
Latham and the work was carried out by Public Works Department
officers, Doig Maj H D Olivier, R E, and Fardunji Cooverji Taraporewala
.
[46]
Even while pipes were being laid, the public remained hostile and
would refer to the pits as graves. Abuses were particularly heaped on
Ranchodial, women outvying men in doing so [47]. It was the success of
the water works which gradually changed the opinion of Ahmedabad’s
citizenry. By 1897, there was a demand for the extension of drainage to
other parts of the city and under the direction of Ranchodlal, plans were
made involving an expenditure of Rs 800,000. However, the approval of
Government and the sanction for raising the loan was received, only after
Ranchodlal’s death in 1898 [48].
Promotion of Medical Facilities
Ranchodlal’s interest in public health predated his assumption of
positions in the municipality. In 1879, he submitted a proposal to the
government endowing a building for the establishment of a charitable
dispensary in the railway suburb just outside the city. This location was
specially chosen so that patients from Kathiawar could avail of the
services offered at the dispensary [49]. A dharmashala for relatives
attending on patients was also to be established. However, the govern
106
RJH
(New Series)
Vol 11:2/3
1996
ment turned down Ranchodlal’s request and wanted the municipality to
pay the salary of the assistant surgeon. Earlier too, the government had
been reluctant to subsidise medical salaries: in 1860, when Jagannath
Shankar Shet had offered to extend the facilities of the Charitable
Dispensary at Girgaum, in Bombay, and in 1862, when Bechurdass
Ambaidass had offered to endow a dispensary in Ahmcdabad [50].
Ranchodlal was, however, not deterred and by 1881, had secured the
services of a doctor for his dispensary, and was sanctioned Grant-in-aid
[52]. It was consequently transferred to the charge of the Municipality,
and Ranchodlal donated a sum of Rs 20,000 for its maintenance. Subse
quently, he provided more funds for the extension of its buildings, to
admit indoor patients and increase hospital staff [52]. He frequently
visited the dispensary which was in the charge of assistant surgeon,
Nilkant Dayabhai, L M and S [53]. Surgical operations were increasingly
carried on at the dispensary. The numbers rose rapidly from 51 in 1894
to 1028 in 1896. The Surgeon General, who inspected the dispensary in
the 1890s when S F Ghandy was managing it found it in “good condition”
[54].
In 1885, Ranchodlal offered Rs 20,000 for the establishment of a small
hospital for women and children, provided the government undertook
charge of it and appointed a qualified lady doctor, half of whose salary he
would bear for a period of four years [55]. That Ranchodlal wished to
support the scheme in view of the Empress interest in medical aid for
women in India is obvious. He wanted the establishment of the institution
to coincide with Queen Victoria’s Jubilee, and met Lady Reay, Vice
Patroness of the Countees of Dufferin Fund, in this connection. Surgeon
General Moore interpreted this offer of Ranchodlal’s as a desire to gain
the credit for establishing a female hospital, without providing for
adequate facilities [56]. The government, as usual, dragged its feet on the
subsidy. The Surgeon General had estimated the cost of its maintenance
at Rs 5,626 per annum [57]. But the Municipality was willing to contrib
ute no more than Rs 600 per annum for four years and Rs 1,200 per annum
thereafter [58]. On the collector’s persuasion, the government finally
agreed to a grant of Rs 2,000 per annum [59]. The Local Fund Board
provided Rs 300 per annum while the remaining was financed by the
interest earned on the Fund of Rs 15,469, which had been collected for the
support of the institution [60]. Ranchodlal agreed to finance the construc
tion of the building, and government provided the land.
After considerable search for the services of a lady doctor, C Blim was
selected. A Parisian by birth, Madame Blim, as she is referred to in the
records was a widow who had come to India as governess to the two young
daughters of General Sir Michael Biddulph. After the premature death of
her charges, Blim trained as a mid-wife at the Grant Medical College,
Bombay. Then she moved to Madras, where she studied the curriculum
RJH
(New Series)
Vol II: 2/3
1996
107
of the L M and S Degree of that University but was not awarded the
degree, because she was not a matriculate, which was the prescribed
requisite. Her qualifications were, therefore, on par with those of an
Apothecary. Blim knew Hindustani and assured the authorities that she
would soon learn Gujarati [61]. The dispensary opened on April 1, 1889
and was named Victoria Jubilee Dispensary,'with provision for eight beds
[62]. The management committee comprised of the Collector HEM
James, Civil Surgeon, president of the municipality Ranchdolal himself,
K B Shapurji Ratanji, vice-president of the local board and Sheth Jehangir
Pestonji who was on the Victoria Jubilee Fund Committee [63].
Blim served for a very short period and was replaced by Motiben
Kapadia, a certified practitioner from Grant Medical College [64]. Being
a Gujarati, Motiben proved to be popular, the attendance at the dispensary
was 11,347 patients, including 7,415 women and 4,022 children, in 1898
[65]. The Annual Inspection Reports of the dispensary for the 1890s
.records that it was in “excellent order”, the most common diseases being
treated were malarial fevers, diseases of the skin, eye, ear and respiratory
system [66].
Hindus constituted the majority of the patients in the Ranchodlal and
Victoria Jubilee Dispensaries, the other communities being Muslims,
Parsis, Indian Christians, Europeans and Eurasions [67].
Yet another medical facility financed by Ranchodlal was the Medical
Home Relief Scheme, 1894, for poor patients who were unable to go to
a dispensary. The scheme particularly benefitted bed ridden patients. The
services of a retired first class hospjtal assistant, Laxman Singh were
engaged and for the first year of its working, the total cost was borne,
equally, by Ranchodlal and the Municipality. Thereafter, Ranchodlal
made an endowment of Rs 25,000 and handed over the maintenance to the
latter [68]. Men, women and children availed of this facility, their number
being 608 in 1898 [69].
The Lord Harris Travelling Dispensary was also established by
Ranchodlal in 1895, in the Daskroi Taluka. The services of a Doctor and
a Compounder were provided. Initially Phirozsha Edalji Bharucha,
Hospital Assistant and Later Narayan Rao Jeram Rao were in charge [70].
They distributed medicines among the villages of the taluka. In 1898,
5,099 patients availed of this facility including 4,983 Hindus, Ill Muslims
and five Indian Christians [71].
Concluding Remarks
• Ranchodlal Chotalal’s involvement with public health was so com
plete that Gillian has pointed out that there was a decline in city
improvements after Ranchodlal’s death in 1898 [72]. Whatever he
achieved was in the face of the hostility of Ahmedbad’s citizenry, which
108
RJH
Series)
Vol II: 2/3
1996
was led by the western educated champions of social reform, like
Mahipatiam Rupram, Vishwanath Narayan Mandlik in Bombay had
opposed the underground drainage scheme and favoured open sewers on
the ground that not enough water had been provided to make the former
effective Mandlik noted in the Bombay Gazette, March 31, 1870 “Our
houses are supposed to be rebuilt our habits changed and our old customs
of centuries on which we are all so stiff was led away. At least this has been
done on paper in our Secretariat” [73]. Like Ranchodlal’s opponents in
Ahmedabad who saw the new schemes and the government’s decision to
implement them as an infringement on the rights to self government,
Mandlik felt that the whole question of drainage was handled in a high
handed manner by the administration of Sri Richard Temple in Bombay.
He contended that municipal administration ought to be “untramelled by
the fetters of officialism” [74].
Ranchodial was doubtless ‘accommodating’ to the British and named
the women’s dispensary after the Queen; but the fact remains that the
municipal improvements he initiated led to a decline in annual mortality
rates in Ahmedbad. Focus, at the micro level, on efforts such as
Ranchodlal’s are necessary for an overall analysis of Indian attitudes
towards western medicine and colonial conceptions of public health.
References
[The author wishes to thank Makrand Mehta for his valuable guidance in the
preparation of this paper; and acknowledge Devbala Sanghvi’s assistance in
translating Ranchodlal’s Biography from Gujarati to English.]
[1] Mark Harrison Public Health in British India: Anglo Indian Preventive
Medicine 1859-1914, New Delhi, Cambridge University Press, 1994, p
171.
[2] Report of the Sanitary Commissioner, Bombay, 1888, p 60.
[3] Muraleedharan V R and D Veeraraghavan (1995): ‘Disease, death and
Local Administration: Madras City in the Early 1900s’ in Radical Journal
of Health, New Series, January 1, p 23.
[4] Arnold David (1993): Colonising the Body, Berkeley, p 271.
[5] Badshah Bhagwanlal R (1989): Rao Bahadur Ranchorelal Chhotalal CIE,
Ahmedabad, 1899, pp 5-8.
[6] Representative Men of Bombay Presidency, Philadelphia, 1900, p 204.
[7] Badshah, Ranchodial, p 37.
[8] General Department Volumes, Government of Maharashtra Archieves,
(GD) 104, 1884, p 89.
[9] GD97, 1876, pp 107-8.
[ 10] Ibid, pp 117-118, 125 The population of the City, at the time comprised of
58,477 males and 58,396 females, ibid, p 129.
[11] GD, 104, 1884, p 90.
[12] S M Edwardes, A Memoir of Rao Bahadur Panchhodlal Chhotalal, CIE,
Exeter, 1920, p 32.
RJH
(New Series)
Vol II: 2/3
1996
109
GD 148, 1885, p 254.
G D 13, 1884, Annual Report of the Municipality' of Ahmedahad (ARM)
1882-1883. pp 61-62.
[15] GD 104, 1884. p 90.
[16] Kenneth Gillian, Ahmedbad, A Study in Indian Urban History', University
of California Press. 1968 p 133.
[17] GD26, 1884, A/?Af, 1883-1884, p 26.
[18] GD, 104. 1884. pp 90-91.
[19] Ibid.
[20] G D, 26, 1884, ARM. 1883-1884, p 28.
[21] Edwardes, Memoir, p 31.
[22] GD, 104, 1884, p 91.
[23] Badshah, Ranchodlal. pp 84-86.
[24] GD, 26, 1884, p 27.
[25] Gillian, Ahmedabad, p 138; Cecil Woodham Smith, Florence Nightingale,
London, 1950, p 565.
[26] GD, 104, 1884. p 83.
[27] G D, 148. 1885, pp 256-257.
[28] Edwardes, Memoir, p 30.
[29] GD, 148, 1885, p 185.
[30] Edwardes, Memoir, p 33.
[31] Gillian, Ahmedabad, p 137.
[32] Badshah, Ranchodlal, pp 44-45.
[33] Edwardes,Afe/no/r, pp 35-7.
[34] Badshah, Ranchodlal, pp 47. 63.
[35] Edwardes, Memoir, p 35.
[36] Edwardes, Memoir, p 36.
[37] G D, 13, 1889, ARM, 1887-1888, p 2.
[38] Edwardes, Memoir, pp 36-37.
[39] G D, 8, 1888, A R M, 1886-87; p 27. Ranchodlal showed the relative fall in
death rates in his covering letter, forwarding the Report of the Ahmedabad
Municipality', 1887-1888.
Number of Deaths
Rates per 1,000
Average of Deaths, (1877-78 to 1886-1887)
6,040
49.49
Average of Deaths, (1883-83 to 1886-1887)
5,310
41.74
In 1887-88 4,719
37.09
GD, 13, 1889, p 1.
[40] GD 103, 1889, pp 130-131.
[41] Report of Native Newspapers, 1888 (R N N).
[42] GD, 103, 1889, pp 93-103.
[43] R N N, 1888, Rast Goftar, June 3 1888.
[44] GD, 103, 1889, p 103, p 141.
[45] GD, 13, 1889, A RM, 1887-88, p 3.
[46] G D, 45, 1893, p 108.
[47] Badshah, Ranchodlal, p 89.
[48] Edwardes, Memoir, p 40.
[49] Badshah, Ranchodlal, p 50.
[50] GD, 7, 1860, p 237; GD8 A, 1864, p 113.
[13]
[14]
110
RJH
(New Series)
Vol 11:2/3
1996
Confidential Vol, 16, 1885, p 390.
Edwardes, Memoir, p 53.
Report of Civil Hospitals and Dispensaries, Bombay, 1883, App 1, p 39.
Administration and Progress Report on (he Mofussil Civil Hospitals and
Dispensaries, Bombay, 1893-1898, (ARCH D).
[55] GD, 45, 1886, pp 30-31.
[56] G D, 40, 1887, p 67.
[57] G D, 47, 1888, pp 95-98.
[58] GD, 45, 1886, p 47.
[59] G D, 47, 1888, p 99.
[60] G D, 40, 1887, p 208.
[61] GD, 54, 1889, pp 119-121.
[62] G D, 40, 1887, pp 56-57. Out of a total population of 124, 767, there were
63,088 females, and 61,679 males ibid.
[63] G D, 54, 1889, p 206.
[64] GD, 54, 1889, p 207.
[65] A R C H D, 1896, p xxxii, A R C H D, 1898, pp 128-129.
[66] Ibid, 1896, p xxxii.
[67] Ibid, 1893-1898.
[68] Ibid, 1898, p 70, Edwardes, Memoir, p 54.
[69] ARCHD, 1898, p 70.
[70] Badshah, Ranchodial, p 2543, ARCHD, 1896, p 67
[71] Ibid, 1898, p 69; pp 128-129.
[72] Gillian, Ahmedabad, p 142.
[73 ] Writings and Speeches of Late Honourable Rao Saheb Viswanath Narayan
Mandlik edited by N V Mandlik, Bombay, 1896, p 416.
[74] Ibid, p 425, Letter to Bombay Gazette, May 31,1883.
[51]
[52]
[53]
[54]
Dr Mridula Ramanna
Department of History
SIES College
Mumbai 400 022
Note to Contributors
We invite contributions to the RJH. Original research
articles, perspectives, field experiences, critiques of policies
and programmes in health care, medicine and allied areas are
welcome. Please send manuscripts, preferably typed in
doublespace. If the material is on a word processor, please
send us a hard copy along with the matter on a diskette
preferably in WS4. Address all communications to the editor
at the address on the inside front cover.
RJH
(New Series)
Vol 11: 2/3
1996
111
Medico Friend Circle
Publications
In Search of D/agnos/s edited by Ashwin Patel, pp 175,1977
(reprinted 1985). Rs 12. (Currently out of stock)
Health Care: Which Way to Go? Examination of Issues
and Alternatives edited by Abhay Bang and Ashwin Patel,
pp 256, 1982 (reprinted 1985), Rs 15. (Currently out of
stock)
Under the Lens: Health and Medicine edited by
Kamala Jayarao and Ashwin Patel, pp 326, 1986, Rs 15
(Currently out of stock)
Medical Education Re-Examined edited by Dhruv Mankad,
pp 214, paperback Rs 35, hardcover Rs 100.
Bhopal DisasterAftermath: An Epidemiological and Socio
medical Study, pp 76, 1985.
Distorted Lives: Women’s Reproductive Health and Bhopal
Disaster, October 1990, Rs 10.
Medico Friend Circle Bulletin’. Bi-monthly, Individual
subscription: Rs 30.
For enquiries
Ravi Duggal, Convenor, Medico Friend Circle,
Building 4, Flat 408, Wahatuk Nagar, Amboli, Andheri(W),
Bombay 400 058. Phone/Fax: 621 0145.
112
RJH
(New Series) 'Vol 11:2/3
1996
Sexuality: Differing Perceptions
Survey in Maharashtra
Mira Savara
C R Sridhar
There is no one common understanding of ‘sexuality’ and different
cultures have widely varying notions and attitudes to it. With the
advent of AIDS there is a tendency to take the ‘scientific’ under
standing of sexuality, as defined within a western paradigm, to
be the inalienable norm. Consequently, sex education designed on
this basis is -often misread and miscarries in other cultures. This
enquiry into sexual attitude and behaviour in two cities ofMaharashtra
reveals that there exists a culture-specific understanding which offers
an opportunity for devising a more positively oriented education
programme.
THE past decades have seen profound changes in India’s socio-economic
structure: growing urbanisation, increased consumerism, an increase in
women workers, growth of nuclear families, increase in marriage age
and increased use of sex in advertising. All these factors point to a
situation where there is a growing tendency towards freer social rela
tionships outside of the immediate family, village or caste control [Savara
1992].
People never thought that HIV/AIDS would be a serious problem in
India. According to The National AIDS Control Organisation (NACO),
as of December 31, 1994 there have been 24,30,645 samples screened;
and 17,124 confirmed by western Blot, and so far 1017 cases of AIDS in
India. This gives a seropositivity rate of 7.05 per thousand. No state has
been untouched; cases have been detected in every slate of India. Leading
in HIV cases is Maharashtra with 5428, followed by Manipur with 2758
and Tamil nadu 27,66. The small state of Pondichery has over a thousand
confirmed by the western blot. The major route of transmission in India
is through sex. However despite this and despite decades of a family
planning programme there has been no research on sexual behaviour in
India.
This report describes the findings of a survey on sexual bahaviour and
beliefs in 1992-93. Some 2500 men and women from a number of
occupational groups were surveyed, mainly students, industrial workers,
white collar workers, migrant workers, using in-depth interviews and
focus group discussions were surveyed. Given that this was one of the first
studies on sexual behaviour in India, we had no precedents to go by. The
RJH
(New Series)
Vol II: 2/3
1996
113
study raised many questions and issues. Sexual behaviour research is
difficult and raises problems unique to itself.
We have learnt a lot from our two years’ work. We stumbled, made
mistakes. We hope that sharing these will assist those who plan to take up
such research in the future. We also hope by sharing we will be able to
extend our work into other areas, and to network with people and
institutions interested in sexuality in the Indian context. We also hope that
our learning will be useful to those working in the areas of Family
Planning. STD’s and AIDS prevention.
Initial Fears
People said that we would not be able to do such a survey. The topk
is too sensitive. In India people do not talk about such matters. We had to
create an atmosphere for research. Through our work we have found that
it is possible to do such research. Interviewers need to be well trained.
They must understand why they are asking the questions, so that they can
remove their own, and respondents doubts and confusions.
The objectives of our study were: (a) To understand the ways in which
people talk about sexual matters and the role of sexuality in people’s
everyday life, (b) To understand how to approach questions on sexuality.
(c) To decide the best approach to a sexual behaviour study in India, (d)
To test the instrument and the method of filling out questionnaires,
especially in the context of high illiteracy, (e) To access the relevant
questions for behaviour such as homosexuality, paid sex, pre and post
marital sex. Other questions would also be raised and some answers along
the way.
Our methodology was designed with the following stages:
First stage, mapping of one town and interviews with two men and two
women in four groups (students, migrant workers, factory workers, office
workers) to learn how they talk about sexual matters; second stage, Ptetest structured questionnaire; third stage, administration of question
naires in one cenre; fourth stage administration of questionnaires in other
centres; fifth stage, coding and analysis and sixth stage, focus groups. To
find our respondents we used the technique of city mapping. City
mapping consisted of interviewing government officials in hospitals.
surveying doctors, blood banks; meeting up with NGO’s working in the
area. We chose Nasik as our first centre. This was done in consultation
with the Maharashtra government AIDS cell. A letter from them was
extremely important in establishing the legitimacy of our work. Approxi
mately 30 men and women were interviewed, in Marathi. Our in-depth
interviews began with questions related to (a) marriage, (b) myths from
India which have some sexual reference, (c) photographs and iconogra
phy from Indian temples which show sexual intercourse, (d) health, and
114
KJ II
(New Series)
Vol 11:2/3
1996
then sexual behaviour. We wanted to test out what would be the best
approach to use for getting into questions related to sex.
We found that the most suitable approach was through health issues.
Marriage was inappropriate since a significant proportion of our respon
dents were unmarried, and questions related to marriage were of little
interest. Myths posed a difficulty, because each different caste and local
group had different myths, different versions of the same myth, and hence
comparison was difficult. The photographs of iconography made most of
the women respondents hesitant and bashful. Hence it was decided to use
the approach of health. The in-depth interviews also gave us an idea of
what terms to use in the structured questionnaire.
A structured questionnaire was developed and translated. We first
evolved a two part questionnaire. The questions not related to sexual
behaviour was asked by the interviewer; and the part on sexual behaviour
was to be self-administered. In pretesting we found that having a two-part
questionaire led to more confusion and embarrassment. So we decided on
a one part questionnaire. We developed two questionnaires - one for men,
one for women.
According to Catania el al, (1990) “A common assumption is that
question sensitivity should increase progressively across items: subjects
are then gradually desensitised to more intimate items. Sensitive items
presented too early may lead to measurement error.” After much testing
we decided on the following order: background information, health
related questions, questions related to attitudes towards sexuality, ques
tions related to sexual behaviour, contraception and problems of condom
use. Our questions on sexual behaviour were kept very simple, since we
had no bench mark survey. We were interested in the age of first
intercourse, with whom it was, the number and identity of partners in pre
marital and post-marital sex, number of homosexual and paid sex expe
riences. For condom use, we were interested in whether there was pain,
as verbal communication had suggested that uncircumcised men faced
more problems with condoms, because of the pull on the foreskin. Also
we were interested in the extent of tears and breakages experienced, and
in the use of lubricants.
On attitudes towards sexuality, we were attempting to test to what
extent Indian texts and beliefs had a following amongst everyday people.
According to ay urveda semen is the most precious substance in the human
body, and loss of semen takes a heavy on the body. To gauge to what
extent this is believed in the population, we asked whether people
believed one drop of semen is equal to 100 drops of blood implying to
much sex can lead to weakness. As Kakad 91989, 118) explains,
Physical and mental strength and mental power have their source in Vitya, a
word that stands for both sexual energy and semen. Virya, in fact is identical
with the essence of maleness. Virya can either move downward in sexual
RJH
(New Series)
Vol 11: 2/3
1996
115
intercourse, where it is emitted in its gross physical form as semen or it an move
upward through the spinal chord and into the brain in its subtle form known as
• Ojas. Hindus regard the downward movement of sexual energy and its
emissions as enervating, a debilitation waste of vitality and essential energy.
Of all emotions, it is said, lust through the physical system in to the greatest
chaos, with every violent passion destroying millions of red blood cells. Indian
metaphysical physiology maintains that food is converted into semen in a 30day period by successive transformations (and refinements) through blood.
flesh, fat, bone and marrow till semen is distilled - forty drops of blood
producing one drop of semen”.
In an attempt to understand the belief we included the following state
ments:
- I believe that one drop of semen equals hundred drops of blood yes/
no
- I feel that too much sex leads to physical weakness: yes/no
Much of Indian mythology revolves around the sexuality of the
Indian gods. One hypothesis was that whilst in the west, sex was seen
in the context of pleasure and reproduction, in India it was possibly also
seen in the context of spiritual development. We also felt that there may
be a difference in the way that sex was perceived. In the west, there was
an undercurrent of sex being equated with sin. We hypothesised that
given the tradition of Tantra and Yoga this may not be the case in India.
It was within this context that we asked the responses to the statements
below:
I believe that one can develop spiritually by channeling the sex drive;
I feel sex is a natural act which even the gods do; I feel there is something
sinful about sex; In addition we asked the responses to the following
questions too; Do you think you can get sick because of sexual inter
course? What type of sickness can you get: weakness fever STD’s
Each questionnaire consisted of the questions asked in English and
Marathi. For those who could not read, an interviewer filled out the form.
Self-administered questionnaires have been extensively used in sexual
behaviour studies. The fact that we had to use a mixture of methods-self
administered for the literates and face-to-face for those who could not
read could affect our findings. To guarantee confidentiality, the question
naire, once completed, was put into a specially made envelope and sealed
in front of the respondents. After each interview/self administered ques
tionnaire the interviewer filled out an interviews feedback form, which
gave feedback on where the form was filled, to what extent it was self
administered and what difficulties were faced. In addition, interviewers
completed a daily report which gave feedback on response rate (number
approached and numbers who agreed for interviews, in-depth and focus
groups) plus information on any problems encountered during the day
and/or any insights.
116
RJH
(New Series)
Vol 11:2/3
1996
We decided to recruit local investigators, since we felt they would be
more familiar with the local situation. We had women interviewing
women, men interviewing men. Our efforts at recruiting married men and
married women were not successful because men were usually employed
and married women were hesitant to get involved in the study after seeing
the questionnaire. All interviewers were given a two-day training
programme. This consisted of having a discussion on the physiological/
biological aspects of sex. Initially both men and women were together.
Then separate sessions were held. Each interviewer then filled out the
questionnaire. A detailed session was then held on the questionnaire, and
clarifying any doubts. The second day interviewers were sent on a field
to fill out two to three questionnaires each. In the afternoon a session was
held to discuss the problems faced and to clear any doubts. Each
interviewer was given an identification card with photograph and leaflets
about Shakti. We feel after our experience that the training sessions
should start with a more cultural approach. Perhaps taking up the
Kamasutra and Khajuraho. Besides the physiological approach to sexu
ality, we feel it is important to have a session on how sexuality is seen in
ayurveda, since this the reference point that most of the non-English
speaking people relate to.
Contact was initially made with those in leadership positions in the
sector chosen. For students this would be the college principal, for
workers it would be the owners of the industry or the top management, or
the association of industries, or labour unions; for migrant workers the
labour contractors. The purpose of the study would be explained, and
cooperation sought. Most often after explaining the reason for the study,
the people contacted would ask if we would come and give a lecture or
educate them on AIDS. This became the manner in which we made
contact for our further focus group discussions.
There were a few problems. In one area, a local women’s group
objected to our study and took delegations to the local politician to
prevent us from asking questions on sexual behavious. The local politi
cian was met, and the survey explained. A letter from the government
AIDS cell, introducing us and our work was shown. The local politician
then appeased the women ’ s group who no longer prevented our work. The
biggest hurdle was posed by the poorer respondents who thought we were
from the family planning department. It was only after convincing them
that wc had no pills, etc, for distribution did they allows us to do the
interview. The particular groups were contacted at their location and
quota sampling done. Respondents covering the age range required were
taken serially till the required number was covered.
About a third of the forms were self-administered. The average time
taken to fill out the questions was about 20 minutes. A majority respon
dents found it simple and easy to answer. How does occupation make a
RJH
(New Series)
Vol 11: 2/3
1996
117
difference in sexual behaviour and altitudes? Briefly, the findings show
differences in sexual behaviour in lhe occupational groups. The biggest
determinant of premarital sex was age of marriage. As age of marriage
increased, the tendency to go for premarital sex increased. Approxi
mately 25 per cent had sex before marriage. As lhe following table
indicates, there is a tendency for increase in premarital sex amongst the
younger, unmarried population. Il is commonly presumed that commer
cial sex workers is the only avenue for having pre marital sex. Ramasuban
(1992)says:
There is general censure of young men engaging in premarital sex and early
arranged marriages are one mechanism by which the avoidance of such
liaisons are sought. However, peer pressures can work strongly among
adolescents in this respect. Visiting prostitutes is the commonest way ol
gaining such experience, since patriarchal family norms place very strict
controls on lhe participation of adolescent girls in such experiment.
Our data tells us otherwise and indicates that the first sexual experi
ence is most likely to be a friend in all categories of respondents. The
highest incidence of going for paid sex is generally amongst the middle
class white collar workers.
Occupation and Marital Status
The unmarried show a similar trend. Though friends remain the largest
category, there is an increased tendency to go for paid sex (Tables 2
and 3).
Some 7-11 percent of our respondents admitted that they had sex with
someone other than their wives after marriage. This was most likely to be
a paid sex worker or a relative. As table indicates there is vast difference
by occupation. However, since there is a difference in methodology
amongst these groups we cannot definitely compare these groups. The
incidence of homosexual contacts also range between 1-6 per com
amongst the married. There seems to be less homosexual experience
amongst lhe unmarried. However, it occurs al a lower age. We feel that
this is an under repre
sentation. Our question
Table 1: Premarital Sex-Occupational Groups
on homosexuality was
Had sex before Had sex but
unclear. Since many of Respondent
Category
Marriage
unmarried
the acts performed in ho
—
mosexual behaviour eg Students
18.9
29.9
24.6
anal penetration was not Blue Collar Worker
. 34.9
26.7
necessarily understood Migrant Worker
26.2
by lhe respondents to be White Collar Worker 26.4
10.4
14.3
a same sex encounter. Loom Workers
118
RJH
(New Series)
Vol II: 2/3
1996
Our experience says (hat this question needs substantial clarification and
reworking.
We founds less variation in altitudes on sex by occupation. Few of our
respondents felt that sex leads to sickness. Sex was seen in a positive light.
as a source for spiritual development, and linked to a natural act which
gods do. The belief that one drop of semen equals hundred drops of blood,
and sex leads to physical weakness was high amongst our respondents.
Most married men avoid sex during a woman’s menses and pregnancy.
We found vast differences in awareness of AIDS and usage of
condoms. Awareness was high amongst the educated; but almost negli
gible amongst illiterate groups like migrant workers. Workers reported
having used a condom in their lifetime. Similarly, al leasl half lhe blue and
white collar workers admitted to using a condom once in their life. Usage
amongst the migrant workers was extremely low. The usage of condoms
is higher among lhe unmarried compared to lhe married respondents.
\mong the unmarried men who have experienced sex, students blue
collar workers and white collar workers show a high usage of condoms.
However usage by migrant workers remains low. This indicates that
whilst the condom message is well received by the more educated,
messages to lhe poorer, the illiterate is still low.
Since we have used a quota sample of occupational groups, aggrega
tion of these without appropriate wights usually is not lhe best method to
draw a complete sample. However we felt that given lhe lack of informa
tion, even though there were significant differences in occupation, lhe
aggregate information docs provide insight on sexual behavour amongst
Table 2: First Sexual Experience, Age and Person: Married
Respondent Category
Avg Yrs
Age Friend Relative
Blue Collar Worker
Migrant Worker
White Collar Worker
Loom Worker
22.7
18.8
23.3
19.4
16.7
19.8
14.4
12.9
3.2
1.5
—
1.4
Same Wife Prostitute
Sex
N
75.4
73.3
73.6
85.7
126
131
125
70
1.6
0.8
5.6
-
4.0
6.1
10.4
1.4
Table 3: First Sexual Experience, Age and Person: Unmarried
Respondent Category
Avg Yrs
Age
Friend Relative Same
Sex
Student
Blue Collar Worker
Migrant Worker
While Collar Worker
Loom Worker
16.6
18.3
17.2
19.4
14.2
12.6
23.6
26.1
16.9
1.5
3.1
1.5
1.6
0.8
1.5
RJH
Vol 11: 2/3
1996
(New Series)
0.8
—
—
—
-
Wife Prostitute
—
—
—
—
1.6
4.7
7.9
14.6
3.0
N
127
127
126
130
67
1 19
the population at large. More than half of the men were in the reproductive
age group of20-30 years. The majority were from within Maharashtra and
were Hindus. Caste wise, kshatriyas and shudras were the largest groups.
Most were educated; only 18 per cent had no schooling. A little less than
half were married and 45 per cent of the men travelled out of town for
work. The modal monthly household income range was Rs 1000-2000.
Of the respondents, 45 per cent were married. Most had arranged
marriages. Age at marriage for many respondents and their partners was
15-25. About half of the married respondents had children. About equal
numbers lived in nuclear and in joint families. We found that in the
general population one in four had donated blood. Quite a large number
of respondents had taken injections. Extra-marital relationships was the
perceived as the majorreason for getting STDs. Weakness and STDs were
seen as being caused by sexual intercourse. Almost 70 per cent of the
respondents believed that condoms are useful in avoiding STDs.
We see very low levels of the other risk behaviours. Given the low
level of response to questions of blood donation. TB and the cliched
responses to questions related to injections, we feel that this approach was
not too useful in conditioning the respondent, and making his/her more
relaxed for the future questions. If anything, it created a negative, fearful
attitude. The questions related to attitudes on sexuality were received
very well, and increased the respondents’ interest in the questionnaire.
The responses to these questions were:
- sexual feelings develop between 15-20 years of age (57 per cent); sexual
drive helps develop personality (62.4 per cent); sex is a natural act (76.6
per cent);
- One drop semen is equal to hundred drops of blood (61.5 per cent).
Some 62 per cent had sexual intercourse; of these individuals, the
majority first experienced intercourse in the age group, 15 to 20; and their
first sexual partner was their wife. Only 7.2 per cent said that they always
used condoms and 9 per cent said they use oil or cream when using
condoms. About a quarter of the respondents admitted they had had
premarital sex; 15 per
cent admitted going to
Table 4:Extra Marital Sex
prostitute even after mar
Respondent Prostitute Relative Anyone N
riage and 2.3 per cent to Category
other than
having homosexual re
wife
lationships after mar
riage. The percentage Blue Collar
Worker
126
5.6
4.8
11.1
who admi tied havi ng had
131
Migrant Worker 6.9
3.8
11.5
homosexual experience
White Collar
was 6.9 per cent before
7.2
125
Worker
3.2
1.6
marriage. One of the Loom Workers
1.4
70
2.9
issues of concern is
120
RJH
(New Series)
Vol 11:2/3
1996
whether people know the correct usage of condoms, and (he quality of
condoms available in the market. To what extent do they tear? Respon
dents reported tearing of condoms. There was widely differing rales of the
different groups requires further investigation. Il would be the quality of
condoms being bought, ortho better usage. A small minority said that they
added cream, oil whilst using condoms.
One of our testing hypothesis was whether intercourse was painful
with condoms for circumcised men. This docs not seem to be the case and
one of the respondents said they did not experience pain.
We wanted to find out what differences existed among the men in our
survey in terms of levels of sexual activity and degree of at-risk sexual
behaviour. What background factors are associated with different levels
of sexual activity? Are different levels of sexual activity associated with
variation in altitudes and behaviour? In this survey we asked about sex
within marriage, pre-marital sex, extra-marital sex, sex with PSW and
homosexual sex. In what ways, if any, are men who engage in more of
these types of sexual behaviour different from men who only engage in
marital sex?
To explore these questions we constructed an index of sexual behaviour
for those men who had experienced intercourse. Men who only had sex
with their wives were scored ‘O’, men who engaged in one other type of
sexual activity (pre-marital, exira-marilal, PSW, or homosexual sex)
were scored ‘ 1 ’ and men who engaged in two or more of these other types
of sexual activity were scored *2’ on our index of sexual activity. This
analysis was conducted on the 992 men who had experienced intercourse.
Of these:
- 480 fell in the category of not engaging in risk behaviour
- 342 had done one risk behaviour
- 169 had done more than one risk behaviour
How do these groups different? factors lead to different levels of
sexual activity, (a) Age al which sexual feelings develop: Among the
male respondents who had experienced intercourse, those who believe
that sexual feelings develop at a younger age were likely to engage in
more types of sexual activity than those who believe that sexual feelings
develop at an older age.
Those who went to vernacular schools scored lower on the index of
sexual activity than those who attended English-medium schools. There
was a weak relationship between the index of sexual activity and the
amount of formal education they had. As education increased, index of
sexual activity increased slightly. There was a weak relationship between
index of sexual activity and age.
As the age of marriage increases, the index of sexual activity increases,
as shown in the table below. While 84 per cent of the men who married
before they were 16 had sex with their wives only, this was true for 63 per
RJH
(New Series)
Vol 11: 2/3
1996
121
cent of the men w ho married at age 25 and above. Some 11 percent of the
men who married before 16 engaged in two or more other types of sexual
activity; this w as the case for 26 percent of the men who married al 25 and
above. Thus the tendency to engage in at-risk sexual behaviour is greater
among the men who marry later. In the survey vast majority of the men
had arranged marriages. However, those men who had not had arranged
marriages were more likely to have engaged in more types of sex.
There were differences in levels of sexual activity among men who
were in different living arrangements. Some of the living arrangements
that allowed more freedom were associated with higher indices of sexual
activity, but there were no clear patterns. Men who were paying guests
reported the highest indices of sexual activity. Both men who lived alone
and men in joint families reported the lowest levels of sexual activity. As
income increased, the tendency to engage in more types of sexual activity
increased.
Men who have sex outside of marriage are more likely to name
pleasure as the reason for sexual intercourse than are men who don’t have
sex outside of marriage. When asked what they thought sexual inter
course was for. the first answer given by 42 per cent of the men scoring
zero on the index and by 69 per cent of the men scoring two was pleasure.
Some 55 per cent of the men scoring zero on the sexual activity index
answered ’reproduction’, and this was the case for 28 percent of the men
scoring two. Among the married men, those with higher scores on the
sexual activity index, indicating sex outside of marriage, are also likely
to have sex more often with their wives than men with lower scores on the
sexual activity index. From our data it is evident that not all men are al
risk. Approximately half of the men say that they do not engaeg in high
risk behaviour.
We therefore feel that educational material should not say that all men
are at risk and should clearly specify the risk behavior and clearly say that
behavior change can make a person not at risk with HIV. This could
provide a motivational leverage to change behavior.
Sexual Behaviour: Women
We know from sexual behaviour studies worldwide that it is more
difficult to get responses from women. If a calculation is made from the
numbers of affairs men in.our survey say they have with friends, the
number is much larger than the number of women admitting to having had
affairs themselves. Our data also indicates that getting reliable responses
from woman posses problems. Women seem to require a more sensitive
approach.
Half of the woman were in the reproductive age group 15-25, with
most coming from Maharashtra. They were primarily Hindu, though all
122
RJH
(New Series)
Vol 11:2/3
1996
communities were covered-including Sikhs and Parsis. Caste-wise, the
largest groups were kshatriyas and shudras. Only 23 per cent had no
schooling; 16 per cent were graduates. Most had attended co-educational
schools in the vernacular language. Three quarters were living in nuclear
families; 60 per cent were married. The modal monthly family incomes
were in the Rs 1,000 to 3.000 range. Some 12 per cent traveled out of town
for their work, half of these on regular basis. Half had married between
the age of 15-20, with the partner’s age being between 20-25. Most had
arranged marriages and had children.
Three-quarters of our respondents had their menstruation start be
tween 12-14, and 97 per cent were still menstruating at the time of survey.
Thirty-seven per cent said they never had painful menstruation; 43 per
cent said they had pain sometimes. For 93 per cent the period was regular.
Over three quarters said they used cloth during their menses, and 80 per
cent said they followed no rituals. Only 6 per cent had ever donated blood;
only 4.8 per cent said they had received blood. Eighty-two per cent had
taken injections. Injections were taken primarily for fever (60 per cent)
and pain (35 per cent). A miniscule number said they had an STD. The
major reasons given for getting an STD was their husbands going to
another woman or them going to another man 13 per cent said they did not
know.
A third of them said that sexual intercourse could cause illness; of these
most believed it could cause weakness. Half felt that sexual feelings
develop between the age 15-20. About half believed that one drop of
semen equals 100 drops of blood, and that sex leads to physical weakness.
18 per cent felt that sex is a sinful act. Half know that condoms are useful
in avoiding STDs, three quarters had heard of AIDS. Half avoided sex
during menstruation.
Of those who had sex, almost all (97.5 per cent) had it first with their
husbands. Only 1.9 per cent admitted to having extra-marital sex. One
woman said she had had a homosexual relation; 1 per cent said they had
been molested. Less than half said they had used a birth control method,
with 34 per cent mentioning condoms. Surprisingly the contraceptive
method currently being used most was the condom; 20 per cent said they
had a miscarriage or abortion. From our responses it seems that the
incidence of pre marital sex and post-marital affairs is quite low amongst
females. It is difficult to say whether this is a reflection of reality or a
hesitation in questionnaire resposne. From ourdata it seems that if women
are at risk from STD’s and HIV/AIDS, it is going to be from the male
behaviour patterns and not their o\9n. It is interesting to note the relatively
high response to condom usage, something which can be built upon.
We note also that there is a considerable difference in the various
occupational groups of woman’s age of marriage is much less amongst
the uneducated, the tribals and migrant workers. It is also this group which
RJH
(New Series)
Vol 11:2/3
1996
123
shows no awareness of AIDS or of the condom being useful in avoiding
STD's. These groups do not read, do not watch TV much, or listen to the
radio. A communication package to reach these groups is essential.
However, it was in this groups that we received maximum hostility to
the survey, because we were perceived to be family planning pe
rsonnel. Research is required as to how to reach these sections of the
population.
Ver}' few women said that they had premarital sex or a post marital
affair. It indicates that it is rarely women’s sexual behaviour that puts hcr
at risk. It is clearly male sexual behaviour which puts a woman at risk, and
this provides some insight as to our educational work regarding AIDS.
However the data on pre and extra marital sex from women is suspect. It
seems to us that there is societal sanction for woman to say no to sex under
certain conditions.
Talking about the African context, Orubuloye et al (1992) maintain:
In terms of women’s control over their sexuality, it is important to note that the
culture has long expected women to shoulder the responsibility for ensuring
that no sexual relations take place, no matter how importuning husbands or
other partners may be. during menstruation and the post partum period, and
after becoming a grandmother or reaching menopause. These periods totaled
over 60 per cent of a women’s time between menarche and menopause.
Although the main responsibility is on the woman to maintain these periods.
she is helped by the societal consensus that they are proper and necessary and
that ignoring the post partum prescription on sexuality may result in the death
of their children, and by the overseeing of this period and even physical
intervention by relatives.
It seems to us that these situations where woman can say no and is
supported by family and society should be highlighted. This would
empower women. By highlighting that it is all right for a woman to sa\
no when her husband shows signs of ill health would create a atmosphere
of societal approval.
We had 20 group discissions with men and women of the four
occupational groups, in Thane and Nasik. Some of our findings are:
1 Marriage is seen as a normal event which requires little prior
information
Q Why do people get married? or what do they do after they get married.
Do you have any idea? Did your parents tell you anything? (Men)
- Everyone knows what to do after getting married. There is no need
in asking parents.
- Parents do not tell anything.
- Parents do not tell anything, we already know everything.
Q What did you know about marriage before getting married? (M)
- We know that after getting married we have to earn money for the
family.
124
RJH
(New Series)
Vol 11:2/3
1996
- Wc know that after getting married we have to carry on our generation.
2 The father plays a very minimal role in imparting sex education to
his sons
Q Do you talk to your father about such matters?
- My father does not give much attention to these kind of talks.
- Some people are scared of their father, so they don’t ask.
- My father was very strict, so wc never asked him.
- Most of the time my father is at work, so we ask our mother since
she is at home most of the time. (Male student)
Q Mothers tell their daughters about this, but fathers do not tell their
sons anything, do you think so?
- Mothers only tell a lot.
- Mother only tell the daughters but fathers don’t.
- Sometimes one asks the mother but not to the father (male white collar).
In general, it appears that taboos set against discussing sex at home
automatically eliminate the father, the head of the household, as the
primary source of sex education for sons. Much of this knowledge on sex
was from friends who had married or already had sexual experience. The
father as a source of information about sex was not even contemplated.
Most respondents were defensive, saying that fathers were too busy, they
had more important matters on hand, etc.
Mothers are the primary source of information about sex for daugh
ters.
The relationship between mother and daughter tends to be a little
closer than that between father and son in matters related to sex. The
beginning ofcducation related to sex starts with the girl attaining puberty.
The mother tells the daughter about becoming a "woman.” She tells her
about menstruation and warns her against pregnancy.
Q What is your feeling at the time of first MC (menses)?
- My mummy informed me about MC. And also suggested that I don’t
keep contact with boys (female student).
- For those who can read and write, books and novels are a source of
information about relations between the sexes and sex.
~ At the time of marriage too, a woman is told a few things about sex:
that first intercourse could be painful, there could be some bleeding,
and these are temporary inconveniences.
Q What was your feeling at time of marriage?
- When I married I was 15 years and my husband was 19 years and
my mother had already told me about sex. My mother told me that don’t
frightened when your husband touches your body. My friends and me
always talk about married life and sex. Because of them I have infor
mation about sex. (female blue collar)
- I married in joint family There were only two rooms in my house.
At first night my husband called me into another room. 1 was frightened,
RJH
(New Series)
Vol II: 2/3
1996
125
but I don’t tell anybody. At the lime of sex my husband was suffering
with bleeding. But my mother told me it was good indication. Means
my husband did not have any relation with other woman, (female white
collar)
4
Sex is seen in terms of attraction
Q What do you think of sex?
- To have relation with opposite sex or getting heat on seeing some
man. If a man touches a female, she feels like getting current in body
and get attracted, (female white collar)
Q What do you feel after having sex with your husband?
- Satisfaction, (female blue collar)
Q Does the relation between you and your husband or boyfriend depend
on season?
- Yes, more frequent during rainy season as we go out and I need sex
more often, (female white collar)
Q Are you satisfied by such relations?
- Yes, I get my physical desires satisfied, otherwise I get irritated, (female
white collar)
5
Sex is important and has specific benefits
Q What do you think about the sex drive?
- Sex is essential to be a mother, (female blue collar)
- I think sex as important only for giving birth to a child and carrying
on the family. To gain more information about sex, one should approach
doctor, (female white collar)
- I feel that 16-18 years, is an age when one should control one self
and if one is able to pass this age without getting off-track, then he or
she able to carve out a better life, (female student).
- In college, girls do fashion to attract boys. But actually, even boys
don’t like to see girls from good families in Bermuda’s and in short
pants. That shows that the girl is not decent. Mostly girls wear all
revealing type of clothes to attract boys but decent boys lend to choose
girls who are well dressed in churidar’s or sarees. (female student)
Q When did you get the information about sex first time?
- When I was in 1 Oth, my friend came with his girl friend in class room.
He removed all other boys from class room and asked me to wail outside
of the class room. Then something happened between them. When I asked
him, what they were doing he explained in brief about sex. (female while
collar)
Q How important is sex to you?
- Sex is at its place. After marriage it comes automatically. It is a part
126
RJH
(New Series)
Vol 11:2/3
1996
of life bul it is not essential. I have many friends but our relation is
friendly, (female while collar)
- I feel happy when my husband has sex with me, but I don’t regard
sex as an import part of life, (female blue collar)
- My husband knows a lot about sex but I am ignorant about it. I don’t
read about it. My husband often discusses sex with his friends. But he
has never told me about oral sex. (female while collar)
6 Women in focus groups expressed a wide range offeelings about the
sexual life.
Q What is your altitude towards sex?
- This is very beautiful. One time in a week is happy. 2/4 times a week
is joy ful but not more than this. We have contact once a week on husbands
holiday, (migrant workers)
Q Do you ever ask for sex?
- No, women generally do not ask for sex. Yes, I ask my husband. Yes,
I ask, but we both sleep in common bed and have contact daily, (female
white collar)
7 It is doubtful whether the physiology or the psychology of sex, as is
known to westerns or the urban educated, is ever explained to the
daughters. The education is imparted in unsystematic but culture-related
terms.
Q What is the meaning of Shivalinga?
- Means Shiva’s ling (penis) and pind (vagina). Ling belongs to Shiva,
Pind belongs to Parvati. What which comes from ling goes into pind.
Al Shivratri time, we go to the Shiv temple. Before that we do puja
of our husband, because for us he means Shiv.
8 Extra-marital affairs are dealt with at a community level
Q If there is a man who after marriage is involved with another woman,
how does your community deal with this?
- This is not accepted in our community.
- When we have one wife there is no question of such relationships.
- If we come to know that a man is having a relation with some other
woman, we go and tell his wife about it and then she decides whether
she wants to live with him or not.
- If a man has such relations then our panchayats deals with it. Our
panchayat will ask this particular man whether he want to divorce his
wife. If he wants to divorce his wife, the divorce takes place in front
of the panchayat. There is no need of going to court, (tribal males)
Q Does your husband have any contact with call girls?
- Yes, sometimes. His friends told me.
- My neighbours told me.
- If a woman has sexual relation with another man, it is not good.
RJH
(New Series)
Vol JI: 2/3
1996
127
Society hales her. It may be bad for health if he has any relation with
call girls.
I will not allow my husband to have relation with other women. It is
injurious to our family, (female blue collar)
9 Sex is taken in a matter-of-fact, routinefashion rather than as a subject
that demands serious speculation.
- Most married men did not believe that there was any need to get
extensive knowledge on sex. Very few were scared of meeting their
partners in bed soon after marriage.
Q Do you think that knowledge after marital life is important or not?
- Information is important but because of family restrictions, not one
gives information.
- It is important.
- Information about how to carry our generation is necessary.
I don’t think this information is required because we gel this information
from the house.
10 Questions About Sex
Q Do you want to ask any questions?
- Each and every' information
_ Who has more tension? Man or woman?
- Both are having same sex feeling.
-Why is woman a more attentive towards her husband? Why does women
attract men? We think that woman has more sex power than man?
- How many days after having a child can't you have intercourse with
your wife?
- How many days after having a child can a woman get pregnant again?
- Can there be a problem after having loo many intercourses like
reduction in semen?
- Without getting officially married can you keep relations with a woman
as a wife?
- What type of sickness can you get by sex?
- What disease are classified as sexually transmitted diseases?
- What happens when that person is having AIDS?
- How does one know whether a person has AIDS or not? or is a HIV
carrier?
- What are the symptoms of AIDS?
- How does one delect AIDS?
- How did AIDS come into humans?
- Can cows get infected by AIDS?
- Suppose a woman has delivered a child and if she gets affected by
AIDS virus after her delivery and if the child has its mother’s milk, will
the child gel affected?
The focus group discussions were very active and two aspects became
clear. The AIDS campaign has created fear in the minds of people, and it
128
RJ11
(New Series)
Vol 11:2/3
1996
has raised many questions which people do not know wheic to get
answered. It also revealed a big interest in discussions. One of the
commonest responses is that “If we had known why (his survey earlier,
we would have taken it more seriously.’’ Hence it seems that a better
conditioning is required for the respondents and interviewers need to be
more trained to answer any questions which respondents may have
regarding sexuality, and also on AIDS.
Self administered questionnaire seem to be a viable means for getting
responses from the literate male population. Our own conclusion is that
we need to lest our several more and different methodologies with the
non-lilerates to guage the reliability of the responses. Such approaches
could include having discussions prior to the interview to remove any
fears and apprehensions. A greater understanding of what we are trying
to do may increase response and reliability.
The length of the questionnaire approximately 10-15 minutes is an
acceptable length for self administered questionnaires. The sequence of
questions needs to be tested further. Our sequence for the questions on
sexual behaviour went from pre-marital, to post-marital to marriage
experience. Our apprehension is that for those respondents who have not
been involved in pre or post marital affairs, the interest could be lost by
(he time they reach the questions on marriage. Hence, questions on
marriage need to be addressed first. A further change is the need to
develop separate questionnaire for the married and unmarried. It seems
essential (hat we incorporate into the questionnaire design, questions
regarding how different people and groups respond io the interview
situation itself. Abramson (1992:114) says:
Rutters argues that social measures usually fail to recognise the significance
of the instrument taking situation. Forcxamplc, if theory would predict certain
differences in behaviour in the presence of authority most social science
measures ignore their importance in (he instrument taking situation. Thus
instrument behaviour must be fully conceptualised within the specific instru
ment testing situation itself.
From our preliminary analysis we see that there is variation in sexual
behaviour patterns depending on: (a) occupational groups, (b) age of
marriage, (c) education. We see a higher degree of premarital sex amongst
the higher occupational, educational groups and those who have a higher
marriage age. White collar workers were the group which showed the
highest percentage of those going to paid sex workers.
Levels of post marital affairs was approximately 10 per cent with about
5 per cent going for paid sex. Homosexuality rales was low. Approxi
mately 5 per cent said that they had been engaged in group sex, with the
highest percentages again the white collar workers. By comparing the
married and unmarried we see the changes which are occurring with age.
RJH
(New Series)
Vol ll: 2/3
I99#$C'
129
Firstly, there is a change in social structure with an increase in educa
tional levels and more differentiation within caste and occupational
group. There also was an increase in marriage age. All this was reflec
ted in an increase in premarital sex. Premarital sex is in the range of 1
in 4 amongst blue collar workers migrant workers and while collar
workers.
Implications for AIDS work
Awareness differs within the different occupational groups and com
munication regarding STDs condoms and AIDS is especially low amongst
the migrant workers. We would extrapolate from this that amongst the
illiterate, there is a need for specific directed programmes. We feel that
education and access to communication media (TV, radio) is of consid
erable importance. These groups are being left out of the current commu
nication channels, and despite being in the urban areas these groups have
not been covered. In the groups where there was an awareness that such
a thing called AIDS exists, we found a lot of interest in discussing and
finding out more about it. The communication channels currently being
used seem to have created an awareness that such a thing exists, and the
messages have generated a lot of fear. Besides the awareness of the name
AIDS, we found that people had little idea about anything else.
This association of fear with AIDS is something which is considerable
concern, since we know that fear leads to denial and is not a motivator for
behaviour change. Since these messages have been received through the
current media approaches, these approaches need to be questioned. Our
research also points for the need for greater studies of the communication
being done, especially those target groups who do not have access to other
forms of information.
There is no one sexuality in the world and different cultures have
related to sexuality in different ways. One of the fears is that with the
advent of AIDS, there is a tendency to lake the ‘scientific’ understanding
of sexuality, scientific as defined within a western paradigm, as a ‘truth’.
And the way and means, the messages which are given, are often picked
up in toto by other cultures. As Greer (1984), says:
My objection is that the sex knowledge so called is actually sex belief and
includes a system of values which are appropriately only to a bureaucratic,
consumer society.
The altitudes towards sexuality in India indicate a positive view and
there is no association of sex with sin, guilt and disease. It is evident that
sex is seen within a spiritual context, and this perhaps points to the way
in which sexual messages may be more positively communicated and
received. Our survey confirms that the Indian population which does not
speak English is more governed by an Indian understanding of the body.
130
RJH
(New Series)
Vol II: 2/3
1996
health, sexuality. Some of the concepts which have come to us are as
follows:
(a) The notion of the body: How one looks at sex is fundamentally
related to how one sees the body. And Indian concepts of the body,
healing and sex differs quite fundamentally from those in the West. We
found that the predominant explanation of the body in the west secs the
body as a clearly differentiated mass and explanations derived primarily
from biology. In India, the people see a rich interaction between the body
and the environment, including astrology and the stars. Most Indians
believe that natural effects, especially the state of one’s mind have great
effects on the human body. Hence the effect of planetary constellations
and Indian preoccupation with astrology; the effect of earth, magnetic
fields, phase of the moon, seasonal and daily rhythms, precious stones and
metals, the effect of sound and mantras. In terms of reasons for ill health,
there are many different levels of beliefs and knowledge, often contradic
tory, that are held simultaneously or consecutively by individuals.
Many of the rituals in Indian society also have to do with the
celebration of sexuality. One, done by millions, every Monday, is the
pouring of milk on the lingam (symbolic of light and also the penis) which
is placed within a yoni (the female generative organ). On a conscious
verbal level, people may say it is symbolic of creation, they may not say
it is symbolic of the sexual act of union. But at the subconscious level, the
imagery is so obvious. Does it need to be spelt out? Perhaps the spelling
it out removes the magic and mystery? There is not much talk about sex
in India. This has led many who are in the business of talking about sex,
to say that sexuality is repressed in India. Sex has never been taboo.
Khajuraho, and its erotic sculptures have become world famous. How
ever, such images are not peculiar to Khajuraho, and many of our temples
show explicit sexual imagery. The yoni, the female reproductive organ,
is often shown, in miniscule detail, stylised, in a design, as a pattern, but
very obvious. Does one need to talk about genitalia when it is there for all
to see?
This continuity of symbols, texts, sex is evident at a street level too. On
the street outside of a Bombay suburban station is a man, who sells books.
They are spread out on a sheet on the payment. On one side are film songs,
next to it are books on the various gods, mythological stories like
Mahabharata, next to them are the Kamasutra, the other shastras relating
to desire, like Kokshastra, Ritushastra. Next to them are books and
manuals on sex. And then porno books.
How different from the porno bookshops of the west, where you only
get sex, sex and more sex. It is not only old art which depicts sexuality and
spirituality. A folk wall painting on bamboo bark shows seven different
circles each with a different god. Open the flap and there arc different
dance poses. Open it once again and there are different positions for
RJH
(New Series)
Vol 11:2/3
1996
131
sexual intercourse. The way of discourse, of learning, of information has
generally other avenues of symbols and art. This has many implications
on issues like sex education and communication strategies for STDs and
AIDS. Il is crucial that we approach these questions within our own
cultural framework, which 1 believe is positive and which sex as a natural
phenomena, into which one grows naturally. How one communicates is
.important. And it is crucial that we do not repeat what they are finding out
in the west. At the annual meeting of the Society for the Scientific Study
of Sex, the report slates that there is concern that sex education concen
trates on negative aspects of sex like AIDS. Such an approach, they
maintained, makes many people see sex as shameful, dirty and dangerous
(Indian Express, November 9, 1993).
References
Catania, J C et al (1990): ‘Methodological Problems in AIDS Behavioural
Research: Influences of Measurement Error and Participation Bias in Studies
of Sexual Behaviour’, Psychological Bulletin, Vol 108(3). 339-362.
Orubuloye, I O et al (1992): ‘African Women’s Control over Their Sexuality in
the Era of AIDS’, Australian National University.
Ramasuban Radhika (1992): ‘Sexual Behaviour and AIDS in India; Potential
Risks for HIV Transmission in India’, Sexual Behaviour and Networking: An
Anthropological and Socio-Cultural Study in Transmission of HIV, Belgium.
Derouauxordine.
Savqra, M (1992): ‘Sexuality in the Indian Context’, Seminar, 396, New Delhi.
Dr Mira Savara
Shakti
B 10 Sun n Sea
25 J P Road, Versoa
Andheri (W), Mumbai 400 061
We invite reports on current developments field surveys,
conferences and seminars for the ‘communications’
section. The ideal length would be about five pages
of the RJH including tables and references. Please keep
references and tables to a minimum. We would
appreciate the material in a wordprocessed format
with a floppy.
132
RJH
(New Series)
Vol 11:2/3
1996
Sexual Behaviour of Women in an Urban
Resettlement Colony of Delhi
Tania Nayar
S C Chawla
In view of the special vulnerability of women to HIV/AIDS, a
community-based study was carried out in Kalyanpuri, an urban
resettlement colony of Delhi, to study the sexual behaviour and
practices of women in the reproductive age group. The study reveals
a high prevalence of RTls among these women. It records that
a majority of the women have no choice in the matter of sexual
activity, and knowledge of STDs and AIDs among the women was
abysmal. Gynecological morbidity and sex education are issues
requiring urgent attention.
IN India, as in other developing countries, explosive urbanisation,
population pyramids heavily weighted with young individuals, the low
status of women, low levels of adult, and particularly, female, literacy,
lack of adequate health information and socially sanctioned male pro
miscuity expose people to the very real risk of acquiring HIV infection.
Women are less able to prevent exposure to sexually transmitted infec
tions (and HIV) because of the lack of available female-controlled barrier
methods. Also, the power-dynamics in sexual relationships in India arc
such that women have limited or no ability to negotiate the conditions
under which sexual intercourse occurs.
For anatomic reasons, transmission of HIV following exposure ap
pears to be more efficient from male to female than vice versa. These
lacts, plus the high prevalence of undetected reproductive tract infections
(RTIs) in the women (knowing that a breach in (he mucosal barrier
increases the chances of acquiring HIV infection by three to five times)
have profound implications for HIV transmission.
The only solution to the problem of HIV is prevention through
education aimed at behaviour modification. To begin thinking of modi
fication. we must first have some data which reflects a true picture of the
pievailing sexual behaviour and practices. Hardly any studies are avail
able on sexual behaviour of urban communities. More so in India, where
people have great difficulty in confronting issues relating to sexuality.
Women of reproductive age were studied as they arc the most at risk of
acquiring HIV infection.
A community-based descriptive epidemiological study (cross-sec
tional) was carried out at Kalyanpuri. an Urban Resettlement Colony of
RJH
(New Series)
Vol 11: 2/3
1996
133
Delhi between October 1992 and June 1993. Cluster sampling technique
was adopted. All women between 15-45 years residing in one block of (he
area (Block 18) which was chosen randomly, were the study population.
The women were interviewed by house to house visits through a struc
tured, pre-tested questionnaire. They were called to the health centre nun
by the Lady Hardinge Medical College) in the area on the subsequent day
where a general physical examination, speculum examination, bimanual
pelvic examination and investigations were carried out on them. All
women found to have the disease were offered treatment. The total
women interviewed was 111 (104 married and seven unmarried). The
data was analysed using software package EpiInfo version 5.0.
This was predominantly a migrant population living as nuclear I amilies. The women ranged from 15 to 45 years of age, with a mean age of
27.7 years. Some 75 per cent of the study population was less than 30
years of age that is, a largely young population.
They were predominantly (88.5 per cent) Hindus. Generally (70 per
cent) women’s education was below class V while about half had no
education at all. The average family income was low and in (he majority
it was less than Rs 1,500 per month.
Sexual Debut
About half the women had had their first sexual encounter by 16 years
of age and more than 80 per cent were sexually active by 18 years of age.
Unlike the west, however, the sexual debuts were almost entirely postmarital. Only two women out of the 1 11 admitted to having had premarital
sex. Of these, one had had premarital sex with her future husband and the
other with a lover. The mean age at sexual debut of these women was 16 3
years. This is almost five years younger (han (he mean age of (heir partners
(husbands), which was 21.34 years at the time of the women’s sexual
debut.
Early age at sexual debut has been associated with increased risk of
cervical cancer [Edibiri 1990], viral infections, including herpes simplex
virus (HSV) infection [Stavraky et al 1983; Kjaer ct al 1990] and human
papilloma virus (HPV) infections [Reeves et al 1987], and bacterial
infections, including those due to gonorrhea and chlamydia [Philips et al
1988]. This is because early initiation of sexual activity means a longer
period of unprotected intercourse and greater possibility of exposure to
multiple sex partners [Aral 1992].
Back Volumes of Radical Journal of Health and Socialist Health
Review are available at Rs 150 per volume
134
RJH
(New Series)
Vol 11:2/3
1996
Reproductive tract infections (RTIs) had an alarmingly high preva
lence rale among the women studied. Nearly half the women examined
had cervicitis, 18.9 per cent had vaginitis, and 40 per cent had pelvic
inflammatory disease (PID). Several women had more than one RTI. The
average number of RTIs per woman was higher in those who had an early
sexual debut. The average RTIs per woman was 1.7 in those who had their
first sexual encounter at less than 15 years of age and 1.2 in those whose
sexual debut was after 15 years of age. Similar high rates of prevalence
nf RTIs were found in a study done in two villages in India [Bang ct al
1989]
About 15 per cent of the women studied said that they have intercourse
almost everyday. Some 38 per cent said they have intercourse couple of
limes a week, 43.2 per cent said ‘‘couple of times a month” and 4 per cent
said they had intercourse less often than that. Among women whose
frequency of intercourse is high (almost everyday) acute infection - acute
cervicitis (45 per cent) and acute vaginitis (27.3 per cent) were seen. In
women with lower frequency of intercourse (couple of times a month or
less) chronic cervicitis (68.7 per cent) and chronic PID (53 per cent)
prevailed.
Frequency of intercourse has not received much attention as a risk
factor for STDs. The limited data available points to frequency of
intercourse as a risk factor for PID [Lee et al 1991], and acquiring HIV
infection [Pandian el al 19901. The probability of transmission of a
pathogen during a single episode of sexual intercourse is variable for
different pathogens and not 100 percent for any of them [Aral 1992].
Thus, if an individual has an infected sex partner, the risk of acquiring
infection would be directly associated with the frequency of intercourse
with that partner.
The findings related to the frequency of intercourse in the present
study are explained thus: those with acute infections are younger and have
more frequent intercourse. They have been sexually active for a shorter
Mine and hence have acquired infections from their partner or during
childbirth more recently. Hence acute infections are seen predominantly.
The group with lower frequency of intercourse having chronic infec
tions is probably an older age group having been exposed to and
harbouring infections for a longer time. The reduced frequency of
intercourse may be due to older age and hence lower sex drive. Also,
chronic infections and PID in particular cause dyspareunia, making
sexual activity painful and therefore less indulged in.
In the Indian context, where male promiscuity has a social sanction,
information about sexual partners may be the most important factor
influencing STD-risk for most women. For, most Indian women have a
I united number of life-time sex partners - and this is usually only one. As
many as 61 per cent of the women said that their husbands had had
RJH
(New Series)
Vol 11: 2/3
1996
135
premarital sex; 28 per cent of the women said (hat (heir husbands were
having sex outside marriage currently. Of the women whose husbands
had had premarital sex, 94 per cent had one or more RTIs. All of the
women whose husbands were having sex outside marriage currently had
one or more RTIs.
In this population, where the mean age of the partners al sexual debut
of the females is almost five years higher, the chances of males seeking
premarital sex partners is very high. This is a migrant population, where
males migrate to cities, leaving (heir wives behind and getting them to the
city only later. Gender-specific morbidity of this type predisposes males
to seek other avenues for sexual relations [Larsen 1989].
Some 42 per cent of the women said they often had sex even if they
don’t feel like it and 40 per cent said that they have sex even if they don't
feel like it occasionally. Some 83 per cent of the women were found to
have little or no choice in the matter of sexual activity. Only 17 pcr cent
of the women could firmly say that they don’t have sex if they don’t feel
like it. Only 26 per cent of the women said that they ever initiate sexual
activity, and only 7 per cent said that they do so often.
As many as 94 per cent of the women said that they never feel like
having an affair, while among men. almost 30 per cent are having extra
marital sex currently (and these are only the ones where the wives know!).
However, six women did admit that they feel like having an affair as a
reaction to their husbands’ infidelity.
The social status of women in a society and the predominant gender
power relations influence sexual behaviour and STD rates in very
important ways. In societies (such as ours) where a womans status is
defined only in terms of her relationship to men; as a mother, daughter.
sister and wife, sexual double standards prevail which place an over
whelming majority of the women at increased risk for STDs because
of the sexual behaviour of their partners [Aral and Holmes 1990|.
This problem is com
pounded by the high Table 1: Age at Sexual Debut of Women Studii i>
prevalence of RTIs Number Percentage
Cumulative
which further predis Age
Percentage
pose them to acquiring
sexually transmitted
12
3
2.9
2.9
4
13
3.8
6.7
infections (and HIV).
14
7.7
14.4
8
Poor levels of education
15
20
19.2
33.7
and low socio-economic
16
20
19.2
52.9
status, as are character
17
15.4
16
68.3
istic of this study popu
82.7
18
15
14.4
lation, are also associ
=>19
18
17.3
100.0
ated with higher risk of
Note'. N = 104, all married women interviewed
STDs.
136
RJH
(New Series)
Vol 11:2/3
1996
Figure I: Awareness of Sexually Transmitted Diseases among Women
N= 111
I
Women who do not
know about STDs 55
Women who know they
can acquire STDs from
their husband/partner 56
Claim to know how to
protect themselves from
acquiring an STD
33 (29.7 per cent)
J__ .
I
Don’t know how to
protect themselves
from acquiring an STD
23 (20.7)
Protective Method Known
Abstinence 26
Condom 4
Other 3
Note : The figures in the brackets indicate percentage out of the total study
population.
Figure 2: Knowledge of AIDS among Women Studied
N= 111
I
Women who have
not heard of AIDS
90
Women who have
heard of AIDS
r
i
21
i
Knowledge about AIDS
- STD
11
- Just know the name
8
- A disease transmitted by touch I
- A killer disease
I
Note : The figures in (he parentheses show percentages out of the total.
RJH
(New Series)
Vol II: 2/3
1996
137
Almost half the study population had no knowledge that sexualIv
transmitted diseases exist. Among the other half only 33 women claimed
to know how to protect themselves from acquiring such an infection
(Figure 1). Of these 26 women (which is less than a quarter of the
population) said that abstinence was a good method of protection from
STDs (- but for how long?) Three women felt that getting their husbands
treated would prevent them from getting infected. This would depend
upon the husband’s willingness to admit a sexual contact other than his
wife and to get treated. Also, unless from a reliable source, how can
effectiveness of treatment be guaranteed? Only four of the 111 women
knew that condoms were effective protection against STDs. Thus, knou Iedge of STDs and how to protect oneself against them was abysmal in this
study population. As Figure 2 shows, the knowledge of AIDS among this
group of women was virtually non-existent.
In view of the very real threat of AIDS, sexual behaviour and practices
of people need to be studied. Areas requiring specific interventions for
behaviour modification need to be identified and addressed. Large-scale
rural to urban migration is creating resettlement colonies and slums where
living conditions pose several health risks to people.
In the context of HIV transmission, women as a group, and particularly
those of reproductive age are especially vulnerable - both, because of the
risks posed by their living conditions and their socio-cultural set-up. A
high prevalence of undetected reproductive tract infections among the
women further adds to this risk.
Sex education and health education for women are imperative to
prevent HIV transmission. Also, gynecological morbidity among women
- particularly for RTIs, needs to be looked into and addressed urgently as RTIs make women extremely vulnerable to HIV infection.
References
Edibiri A A (1990): ‘Cervical Intra Epithelial Neoplasia: The Role of Age al
First Coitus in its Etiology’, J Reprod Med, 35: 256-9.
Stavraky K M, Rawls W E, Chiavetta J, Donner A P, Wanklin J M
(1983): Sexual and Socio-economic Factors Affecting the Risk of
Past Infections with Herpes Simplex Virus Type 2’. Am J Epidemiol, 1IX:
109-21.
Kjaer S K,G Engholm, C Teisen et al (1990): ‘Risk Factors for Cervical
Human Papilloma virus and Herpes Simplex Virus Infection in Greenland
and Denmark: A Population-based Study’. Am J Epidemiol, 131: 669-82.
Reeves W C, D Caussy, LA Brinton et al (1987): ‘Case Control Study of
Human Papilloma Viruses and Cervical Cancer in Latin America’, Ini ./
Cancer, 40: 450-4.
Philips R S, P A Hanff, A Wertheimer, M D Aronson (1988): ‘Gonorrhea in
138
RJH
(New Series)
Vol 11:2/3
1996
Women Seen for Routine Gynecological Care: Criteria for Testing’, Am
J Med,
Aral S O(-1992): ‘Sexual BehaviourasaRiskFactorforSexuallyTransmitted
Disease’ in A Germain, J N Wasserheit, K K Holmes, Reproductive Tract
Infections: Global Impact and Priorities for Women's Reproductive
Health, Plenum Press, New York, 185-98.
Bang R A, A T Bang, M Baitulc, Y Chaudhary, S Sarmukaddam, O Tale
(1989): ‘High Prevalence of Gynecological Diseases among Rural Indian
Women’, Lancet, 1: 85-6.
Lee N C, G L Rubin, D A Grimes (1991): ‘Measures of Sexual Behaviour and
the Risk of Pelvic Inflammatory Disease’, Obstet Gynecol, 77: 425-30.
Padian N S, S C Shibaski, N P Jewell (1990): ‘Heterosexual HIV Transmis
sion and Frequency of Intercourse’, J Infect Dis, 161: 883-7.
Larson A (1989): ‘Social Context of Human Immunodeficiency VirusTransmission in Africa: Historical and Cultural Cases of East and Central
African Sexual Relation’, Rev Infect Dis, 11: 716-31.
Aral S O, K K Holmes (1990): ‘Epidemiology of Sexual Behaviour and
Sexually Transmitted Diseases’ in Holmes K K, P A Mardh, P F Sparling,
P J Weisner (eds). Sexually Transmitted Diseases, second edition. New
York; McGraw Hill, 19-36.
Dr Tanya Nayar
Department of Health Service Studies
Tata Institute of Social Sciences
Trombay
Mumbai.
Note to Advertisers
The RADICAL JOURNAL OF HEALTH is a multi
disciplinary quarterly on health and medicine aimed at pro
viding a rational, humane and critical perspective on these
topics. Our readership is made up of academics, activists,
journalists, students, NGOs, research and documentation
institutions. We also have a small, growing circulation
abroad. For information write to Sushma Jhaveri, RJH,
C/o 19 June Blossom Society, 60-A Pali Road, Bandra,
Bombay 400 050.
RJH
(New Series)
Vol 11: 2/3
1996
139
ECONOMIC
AND
POLITICAL
WEEKLY
SPECIAL NUMBER
September 1996
Sociology and Common Sense
...Andre Beteille
Agricultural Modernisation and Education
... Krishna Kumar
Vcrricr Elwin and the Tribal Question in
Late Colonial India
... Ramachandra Guha
Politics of Ecology: Wildlife and People
...Mahesh Rangarajan
Sexual Violence. Discursive Formations and the State
...Veena Das
Should Domestic Prices Be Equated to
World Prices?
Export-Oriented Agriculture and Food Security
...Prabhat Patnaik
...Utsa Patnaik
Agricultural Development: Imperatives of
Institutional Reform
... A Vaidyanathan
Economic Reforms. Employment and Poverty
...Abhijit Sen
India’s Checkered History in Fight Against Poverty:
Are There Lessons for the Future? ...Martin Rava11ion, Gaurav Datt
Poverty Estimates and Indicators: Importance of
Data Base
...M H Suryanarayana
Minimum Needs of Poor and Priorities
Attached to Them
...V Sitaramam, S A Paranjpe,
T Krishna Kumar, A P Gore, J G Sastry
Economic Reform and Rate of Saving
...EPW Research Foundation
Savings Rate in Indian Economy since 1991
...Pidapre Balakrishnan
Explaining Post-Reform Industrial Growth
...CP Chandrasekhar
Foreign Direct Investment and Domestic
Savings-Investment Behaviour ...Biswajit Dhar, Saikat Sinha Roy
Capital Market Growth: Trends.
Explanations and Evidence
Too Little in the Wrong Places? Efficiency
and Equity in Indian Urbanisation
pp 224
...R Nagaraj
...Sanjoy Chakravorty
Price: Rs 70; 5 20
For copies write to
Circulation Manager
Economic and Political Weekly
Hitkari House, 284, Shahid Bhagat Singh Road. Mumbai 400 001.
140
RJH
(New Series)
Vol 11:2/3
1996
Physical Standards in the Private
Health Sector
Sunil Nandraj
Ravi Duggal
The rampant, unregulated, unplanned and largely unmonitored
growth of the private health sector has resulted in the current
situation of poor and unreliable quality of care. This article
documents systematically the nature of care available to people in
the Satara district of Maharashtra. The poor implementation of
existing legislation and lack of standardisation in health insti
tutions is brought into sharp focus.
I
Introduction
IN India, provision of health care services is complex. It is provided
mainly by the public and private sectors. The public sector provides
health services through the central government, state governments.
municipal corporations and other local bodies. The private health sector
consists of the ‘not-for-profit’ and the ‘for-profit’ health sector. The notfor-profit health sector which is very small includes various health
services provided by non government organizations (NGOs), charitable
institutions, missions, trusts, etc. Health care in the for-profit health
sector is provided by various types of practitioners and institutions. Tin
informal’ sector consists of practitioners not having any formal quali
fications, like the tantriks, faith healers, bhagats. hakims, vaidyas and
priests who also provide health care.
The private sector is a large and important constituent in the country’s
health care delivery system. It has expanded greatly in the post indepen
dencc period, especially in (he 1980s. Various studies conducted by
organisations such as National Sample Survey Organisation (NSSO).
Foundation for Research in Community Health (FRCH). Kerala Shashtra
Sahitya Parishad (KSSP) and National Council of Applied Economic
Research (NCAER) bring out the fact that between 60 and 80 per cent of
people utilise private health facilities in the country in both rural and
urban areas |NSSO, 1987, Duggal. R. Amin. S 1989. Kannan. K P. el al.
1991, NCAER. 1992. George, A, et al. 1993]. The findings also show that
a substantial financial burden is borne by households for meeting health
care needs. Compared to public expenditures on health the private
household expenditure are nearly four to five times more.
RJH
(New Series)
Vol 11: 2/3
1996
14.
Data on sectoral distribution of doctors is not easily available. Many
stales do not file the required information to the appropriate authorities.
A listing of health establishments and practitioners in Ahmcdnagar
district. Maharashtra, was done by FRCH. This study identified a total of
3060 doctors in the district belonging to all systems of medicine and 92
per cent of them were found to be practising in the private sector
(including a very small percentage in the voluntary sector). Of the total
doctors identified 51 percent were in urban areas and the rest in rural areas
[FRCH, 1993]. The 1981 census economic tables which list occupational
distribution also show a more or less similar pattern. Thus of all doctors
in the country 59 per cent were in urban areas (73 per cent for allopathic)
[Census, GOI 1981].
With regard to hospitals in the country, during 1974 16 per cent of the
hospitals and 21.5 per cent of the hospital beds were in the private sector
and rest were in the public sector. This increased in 1990 to 57.95 per cent
of hospitals and 29.12 percent hospital beds in the private sector [CBHI,
Table 1 :Basic Characteristics of Sample Practitioners by Location
Practitioner Characteristic
EBA
EDA
Total
All Practitioners
Location
(a) Urban
(b) Rural
Gender
(a) Male
(b) Female
Age
(a) < 35 years
(b) 35-45 years
(c) > 45 years
# Mean Age (years)
Qualifications
(a) Accredited Degree
(b) Unqualified
System Accredited
(a) Allopathic
(b) Homoeopathic
(c) Indian Systems
(d) Unqualified
Valid Registration
(a) Yes
(b) No
(c) Unqualified
41.50
58.50
100.00
13.64
86.36
83.87
16.13
54.7
45.3
95.45
4.55
93.55
6.45
94.3
5.7
50.00
36.36
13.64
36.00
35.48
35.48
29.04
39.00
41.5
35.9
22.6
37.7
54.55
45.45
90.32
9.68
75.5
24.5
4.54
9.10
40.91
45.45
48.39
3.22
38.71
9.68
30.2
5.7
39.6
24.5
45.45
9.10
45.45
61.29
29.03
9.68
54.7
20.8
24.5
Note'. EDA=economically developed area; EBA=economically backward area
(Figures, except #, are in percentages, columns=100 )
142
RJH
(New Series)
Vol 11:2/3
1996
Table 2: General Features of Practice
Practice Characteristic
Type of Practice
(a)Allopathic
(b) Allopathic + other
(c) Ayurveda
Years of Practice
(a) upto 5 years
(b) 6 - 10 years
(c) 11 - 20 years
(d)>20years
# Mean years
Clinic Ownership
(a) Owned
(b)Rented
Multiple Practice
(a) Single clinic
(b) 2 or more clinics
Indoor Care Facility (ICF)
(a) Yes
(b) No
(c) Other clinic
Number of Beds as per cent of (ICF)
(a) One
(b) Two or more
(Sample : actual number)
# Mean Days/week clinic open
Laboratory Services
(a) Yes
(b) No
(c) Refers local area
(d) Refers nearby town/villagc
Telephone Facility
(a) Yes
(b) No
(c) Care off
Practice Caseload
# Mean Hours per day
Practice Characteristic
# Mean Cases per day
- last day actuals
- during monsoon
# Mean Cases in last week
# Mean cases in last month
- old cases
- new cases
Contact with Med.Reps
(a) No contacts
(b) < 5 per week
(c) 5 & more per week
Maintaining Case Records
(a) Yes
(b)No
Sample Size (actual numbers)
EBA
EDA
TOTAL
86.36
9 09
4.55
74.19
16.13
6.45
79.24
15.09
3 77
31.82
36.36
13.64
9.09
8.45
35.48
12.90
29.04
22.58
12 00
33.96
22.64
22.64
16.98
10.50
48.39
51 61
39 62
60.38
68.18
31.82
70.97
29.03
69.81
30.19
50.00
50.00
—
22 58
67.74
9.68
33.96
60.38
5.66
63.64
36 36
(H)
6.50
28 57
71.43
(7)
6.29
50.00
50.00
(18)
6.38
—
9.09
45.45
40.91
6.45
3.23
70.97
16.13
3.77
5.66
60.38
26.42
9.09
68.18
22.73
64.52
19.35
16.13
41.51
39 62
18.87
12.09
8.77
10.11
22.18
36.50
140.86
493.89
160.67
333.22
18.55
31.12
113.52
342.17
140.71
201.46
20.05
32.61
124.87
399.39
148.52
250.87
27.27
45.46
27.27
6.45
51.61
41.94
15.09
49.06
35.85
40.91
59.09
22
35.48
64.52
31
37.74
62.26
53
27.27
72.73
•
Note. Where per cent totals don’t equal 100 the balance are ‘no - responses’
(Figures, except #, are in percentages, columns=100 )
RJH
(New Series)
Vol II: 2/3
1996
143
various years]. There are reasons to believe (hat the number of hospitals
in the private sector is much larger than the available data suggests.
Health Information of India 1992, shows that there were only 1.319
private and voluntary hospitals in Maharashtra. Bui the Bombay Munici
pal Corporation listed 907 private hospitals and nursing homes in Bombay
city alone (excluding Thane), on the basis of its registration data which is
also an underestimate. Another instance of under reporting of data is
brought out by a survey undertaken by Andhra Pradesh Vaidya Vidhana
Parishad, which found the existence of2.802 private hospitals and 42.192
private hospital beds in Andhra Pradesh in 1993 as against only 266
private and voluntary hospitals and I 1,103 private hospital beds accord
ing to official figures [Mahapatra P. 1993]. The survey also showed that
67.60 per cent of the private hospitals were located in urban areas (which
were state capital, divisional HQ, district HQ and taluka HQ). The bed
population ratio in private hospitals was 6.37 beds per 10,000 population
as compared to public hospitals which was 5.12 per 10.000.
The expectation of the public for quality medical care is very high,
especially of the middle classes. There is a growing pressure on health
care providers and professionals to maintain and improve the quality of
health care with emphasis on cost effectiveness. This is reflected in a
concern accorded by policy makers, planners, administrators, doctors,
researchers and consumers to the aspect of quality of care in the delivery
of health care services.
Quality and Standards in Health Care
There are different aspects and dimensions of quality. The Oxford
English Dictionary defines quality as a noun meaning ‘degree of excelTable 3: Practitioner Qualification vis-a-vis their Actual Practice
Type of Practice
_____________________ Qualification____________
Allopathy
Indian System
Homoeopathy
Unqualified
EBA EDA Total EBA EDA Total EBA EDA Total EBA EDA Total
Allopathy
Allopathy+other
Ayurveda
Crosspracticc Rale
Sample Size:
100.0 93.3 93 8 88.9 50.0 66.7 50.0 100.0 66 7 90.0 33.3 76.9
— 6.7 6.2 — 33.3 19.0 50.0 - 33.3 10.0 33.3 15.4
— —
— 11.1 16.7 14.3 — — — — —
—
0
7
6 800 499 599 9900 9900 9900 NA NA NA
2
15
9
1
16
12 21
1
3
3
10
13
Noles ::) where per cent totals don’t equal 100 the balance are ’no - responses'
ii) the crosspractice rale has been calculated by indexing 'qualification' = 100
and dividing it by the percent who actually practice their original system.
multiplying this by 100 and from the product obtained subtracting 100. For
example, for the ISM qualified in the EDA: [ 100*( 100/16.7)1- 100=499. In
the case of homoeopaths wc have taken the denominator as I. NA = Not
Applicable.
(Figures are in percentages, columns = 100).
144
RJH
(New Series)
Vol 11:2/3
1996
lence’. The Bureau of Indian Standards defines quality as ‘the totality of
features and characteristics of a product or service that hear on its ability
to satisfy stated or implied needs*. They use the term quality with a
qualifying adjective such as ‘quality level’ ‘relative quality’. The quality
revolution with its emphasis on total quality, quality leadership, and total
quality management has resulted in its usage even in human services.
Concepts of quality of life (QOL) quality enhancement and quality
assurance, total quality management, quality level are currently having a
significant impact on human services like health and education.
In developed countries quality as an issue has been in the forefront for
management of various types of institutions. Various systems and meth
odologies have been developed to study different dimensions of quality.
These were developed first in the industrial setting and then later in the
health care sector. The same trend is being followed in India.
Quality medical care involves methodology used to assess and ensure
quality, development of guidelines regarding appropriate methods of
quality assessment to improve care provided and increase overall access
to health care of high quality. There are systems and processes for
guaranteeing quality. The measures include reducing unnecessary admis
sions, assessing the appropriateness of average length of stay, the number
Table 4: Some Observations of Condition of Clinics: Positive Features
Features Observed
EBA
EDA
TOTAL
Noise Level (quietness)
Condition of Wall (good)
Height of Ceiling (above 8 fl.)
Ceiling Type (cemented)
Condition of Ceiling (good/clean)
Type of Floor (filed)
(’ondition of Floor (good/clean)
Natural Light (sufficient)
\ rtificial Lighting (sufficient)
Ventilation (adequate)
Seating for Patients (adequate)
Water Availability (present)
Display of Registration
Environment (uncongcstcd)
Dustbin (present)
Examination Table (present)
Condition of Ex .Table (good/clean)
Medicine Tray (present)
Pharmacy (present)
Sample Size (actual numbers)
27
22
59
18
14
77
36
68
23
9
18
14
5
36
18
95
50
55
29
61
81
45
58
90
58
58
65
26
81
32
81
48
23
84
81
77
28
47
72
34
40
85
49
62
47
19
55
25
13
43
21
89
68
68
22
31
53
Note', (figures are percent positive to total): EDA=economically developed Area;
EBA=economically backward area.
RJH
(New Series)
Vo! 11:2/3
1996
145
of consultations and the number of days spent in hospitals. The outcomes
include such things as rate of avoidable deaths, preventing hospital
infection, avoiding surgeries and invasive procedures when not neces
sary. and reducing the instances of post operative complications and
readmissions.
Avcdis Donabcdian (1988). the guru of quality assurance, in his
contribution to the assessment of health care lays emphasis not only on the
technical domain (defined as knowledge, judgement and skill of provid
ers) but also on the interpersonal. This consists of patient communication
to the physician for purposes of both diagnosis and the determination of
preference for treatment and physician communication to the patient for
purpose of information on the nature and management of the illness.
Explicitattention tothe defini
tion and measurement of quality
Table: 4a: Equipment Found in GP
of care on the pan of the internaClinics
tional health community can be
Equipment
EBA EDA
attributed to the widespread dis
semination of the writings of Gauze swabs
9.1
83.9
71.0
Bruce and her colleagues (1990) Sterile pads
54.5
64.5
who have initiated activities to Scissors
—
12.9
operationalise what had previ Adult weighing machine
ously been thought a rather elu Children’s weighing
—
machine
3.2
sive concept. Bruce has devel
Kidney tray
45.5
61.3
oped a conceptual framework Antiseptic solution 1
90.3
3.6
which defines quality of care for Syringes
81.8
90.3
family planning and related re Needles
81.8
90.3
productive services. The frame Oxygen cylinder
4.5
6.5
—
work defines quality in terms of X-ray viewers
19.4
—
6.5
six elements and associated indi Slides
9.1
45.2
cators. These are choice of Test lube
13.6
38.7
method, provider-client informa Spirit Lamp
—
6.5
tion exchange, provider compe Haemoglobin test set
Steriliser
4.5
3.2
tence, interpersonal relations,
51.6
Bowls
22.7
mechanisms to encourage conti Bed sheets
—
4.5
nuity and appropriate constella Towels and napkins
22.7
54.8
tion of services.
—
Revolving stools
12.9
The conceptual framework Ordinary stools
—
51.6
19.4
9.1
provided by Bruce on quality of Examination table
—
9.7
care is rather narrowly defined. Step stool
—
3.2
The framework does not include Screen stands or curtains
Refrigerator
16.1
the health infrastructure. This di
—
9.7
mension clearly cannot be ignored Wash basin with tap
—
Wall clocks
12.9
when evaluating services. Bar
bara Mensch (1990) mentions two Note. Percentage existing.
146
RJH
(New Series)
Vol 11:2/3
1996
parts to a comprehensive assessment of services. The first is a description
of programs which arc considered part of the infrastructure (i c. equip
ment and facilities, staff and training, supervision, record-keeping, and
supplies). If all of these arc functioning, the necessary, although not
sufficient, conditions for adequate services can be said to be in place. In
other words, a facility might be clean, reasonably equipped, and staffed
with trained personnel, but still treat women poorly both from the medical
and personal standpoint. Similarly, a family planning clinic might have
a decent contraceptive logistics system with an adequate range of sup
plies, but not provide balanced information or a full range of methods.
The existence of a large supply of any one method may simply indicate
that that particular method is rarely offered.
Inevitably, emphasis on quality of care leads us to the discussion of
standards. Standards assist us in defining the meaning of quality as it
relates to health care delivery. The first step in improving quality of care
is an articulation of standards that are needed for the provision of care.
The key concepts for the definition of standards arc firstly it notes that
standards are a degree of excellence, secondly it suggests that standards
serve as a basis of comparison, thirdly that standards arc a minimum with
which a community may be reasonably content and finally that it is
recognised as a model for imitation.
Standards arc classified broadly as written or explicit standards,
written or implicit standards and unwritten or implicit standards.
Explicit standards are defined as specific for care. Implicit standards
are defined as usual and customary in practice. Implicit standards can
also be written such as a general checklist of items. Ideally standards
should be written and explicit as these allow both the data collection
process and the assessment of care
Table 4b: Type of Equipment
to be based on clearly delineated
agreed upon bench marks rather Equipment
EBA EDA
than relying on the discretion of
86.4
90.3
assessors [Fooks and Rachlis Stethoscope
BP Instrument
81.8
93.5
1990]. Donabcdian (1988) states Thermometer
48.4
36.4
that standards may be directed Tongue Depressor
31.8
58.1
towards structure, process or Scalpel
13.6
12.9
outcome. Structure standards Speculum ENT
—
22.6
apply to the things such as Valselum
9.7
4.5
3.2
4.5
human, financial and physical re Reflective mirror
29.0
Artery forceps
sources. Process standards apply
—
6.5
to activities that constitute care, Auroscope
86.4
83.9
service or management. Outcome Dressing material
—
12.9
Knee hammer
standards refer to the end results
9.1
58.1
Sutures and ligatures
of care, clinical as well as nonNote'. Percentage existing.
ciinical.
RJH
(New Series)
Vol II: 2/3
1996
147
In 1985 (he deliberations of a WHO expert committee resulted in a
report entitled The Hospiro! curl Health for All. This report highlighted
the need for suitable infras'iuciurc lorthc hospital and for the organisation
of resources across various levels of service. Il further suggested a need
for an appropriate management system to be in place, that hospitals
determine their scope oi
Table 5: Hospital Prohiij
service with reference to a
EBA EDA Total
community based informa
tion system. 'Inc commit AU Institutions
36.70 63.30 100.0
Location
tee recommended that
a) urban
55.6 90 3 77 6
WHO develop indicators of
44 1
b) rural
9.7 22 4
performance as well as
Yen: of establishment
methods and materials re
a) 1968 to 1978
II 1
12.9 12 2
h) 1980 to 1990
50.0 41 9 44 9
lated to facility planning and
C) 1991 to 1995
38.9 45.2 42.9
maintenance for hospitals.
Ou nership
In 1990a WHO study group
a) individual prop
100.0 600 91 8
al Geneva brought out a re
—
b i partnership
97
6 1
c) any other-1002.0
port which recommended
to WHO to continue to de Ownership of premises
a) owned
61.1
83.9 75.5
velop guidelines on essen
h) rented
33 2
16.1 22.4
tial procedures, technolo
— 2.05
c) long term lease
5.6
gies and standards for first
Functioning
a) only self patients
100.0 77.4 85.7
referral hospital functions.
b) open NH
22.6 14.3
It furiherrecommended that
Doctor-Owner
national and international
Administrator
100 100
100
non-governmcnl
Qualification of doctor-owner
a) Allopathy
61.1
77.4 71.4
organisations should im
b) Ayurveda
22.2
12.9 16.3
prove the existing standards
9 7 10.2
c) Homeopathy
II.1
of management. The report
— 2.0
d) LMP/LSM
5.6
w'ent into the specific of el
Sex of Owner
ements of standards such as
a) Male
88 9 935 91.8
b) Female
111
8.2
6.5
information system, refer
Age of Owner
ral systems, human re
a) < .35 j r.
50.0 35.5 40.8
sources. continuous moni
16.7 41.9 32.7
b) 35 - 45 yr.
toring and evaluation of
c)>45yr.
33.3 22.6 26.5
39 11 39 12 39.12
performance, quality of care
# Average age
and effectiveness and effi Number of Beds
44.4
129 24.5
a) 3 to 5
ciency as well as its physi
50.0 64.5 59.2
b) 6 to 15
cal structure and equipment
19.4 14 3
55.6
c) 16 to 2
[WHO. 19901.
2.0
3.2
d)above 25
# Average number of beds
755 12.29 10.55
Many
countries
49
18
31
# Total
recognise the need for stan
dards for hospitals. Some
Note: Figures are percentages with column =
countries have established
100. except those marked #.
148
RJH
(New Series)
Vol! I: 2/3
/996
national standards and are continuously improving (hem. some of them
have established national programs to monitor the compliance of indi\idual hospitals and other lypes of health care facilities with national
standards. Scrutiny of hospital based services is required on (he grounds
that a sound organisation is necessary for the delivery of high quality
clinical care and a high quality of services for the user.
There arc various levels of standards. There are minimum standards
which generally represent a level of acceptability. Minimum standards
are a must to meet. Beyond the minimum there arc desirable or optimal
standards. A hospital while meeting a minimum standard should seek to
achieve a desired or optimum standard. Minimum standard should be
achievable by all, optimal standards on the other hand represent a degree
of excellence. If good quality service involves ‘conformity to specified
requirements’ wc have to ask whose requirements and whose standards
are to be met. Standards have to be developed and maintained. This is
done based on collective judgments. This includes both the organisation
and management standards, standards for clinical/professional practice.
Governments have an important role of establishing standards for the
delivery of health care services.
In 1984 a regional committee of the WHO adopted 38 targets fo;
attainment of health for all by the year 2000. Target 31 is specifically on
quality, and reads: “By 1990 all member slates should have built effective
mechanisms for ensuring quality of patient care within their health care
systems'*. The target book included establishing methods and procedures
for systematically monitoring the quality of care given to patients, by
making assessment and regulation a permanent component of health
professionals’ regular activities, and by providing all health personnel
with training in quality assurance. It also emphasized the need for clear
country policies on quality assurance. Such policies should state which
procedures were to be assessed, how the assessment should be organised.
how health providers, politicians and consumers should co-ordinate their
Table 6: Care Provided
Number of OPD cases and Indoor admissions
Total
EBA
EDA
Out patient department (OPD)
Average cases treated
Last day (number)
Last week (number)
Indoor admissionsAdmissions
last week (number)
Admissions last month (number)
Length of stay (last month) (days)
Occupancy rate (last month) (percent)
RJH
(New Series)
Vol! 1:2/3
34.72
161.06
43.29
199.03
40.14
185.58
11.06
44.35
6.90
54.68
12.06
40.85
16.38
48.98
11.68
42.20
13.32
50.81
/ 996
149
efforts, and what the practical consequences of quality assessment would
be. Policies would have to be formulated to ensure the involvement and
cooperation of providergroups, researchers, public health authorities and
consumers. No member state claimed to have established a comprehen
sive programme for quality assurance. Three countries had incorporated
into law the requirement to include quality assurance [WHO 1990).
In recent times there is an increase interest not only in formulation of
standards but also in the process of measurement of compliance with
them. This is generally refrered to as accreditation. Accreditation is a
process wherein standards arc set and compliance with them is measured.
CE Lewis gives a useful working definition of accreditation as profes
sional and national recognition reserved for facilities that provide high
quality health care. This means that the particular health care facility has
voluntarily sought to be measured against high professional standards
and is in substantial compliance with them [Lewis 1984]. In many
countries accreditation systems are in place for the monitoring of stan
dards in hospitals. The countries with the most firmly established accredi
tation systems are the US, Canada and Australia. In the US there were
three clear phases in the evolution of the accreditation process : the era ol
minimal standards 1917-1965. the era of optimal achievable standard
1966-1987, and the era of performance evaluation and beyond from 198S
[Brooks 1990].
In developing countries the issue of quality assumes a different
dimension, that of accessibility and availability of health services. In
India the access to service is very limited and until the present the
government's attention was focused on the expansion of services, namely
opening of primary health centre's and sub-centre’s for the rural popula
tion. This expansion was carried on without giving emphasis to the
quality aspect. This resulted
in the government primaTable 7. Staffing
rily concerned with meet
EBA EDA Total
ing targets of infrastructure
Qualified
and humanpower. This is Q Docs full lime (allop)
14
32
46
especially true of family Q Docs full time (oih sys)
13
10
23
planning services. The ex- VC (Total)
38
52
90
0
3
3
pansion of the family plan- Q Nurses
Q Technicians
2
6
8
nine infrastructure in rural
Sweepers
29
40
11
areas which the country has Ward attendants
3
15
18
undertaken in the last few Receptionists
9
1
8
years will become effective Others
19
17
36
only if corresponding im Unqualified
71
15
86
provement in the quality of Nurses
17
Pharmacists
28
II
service lakes place. Perceiv
2
2
Technicians
0
ing quality to be luxury in
150
RJH
(New Series)
Vol H: 2/3
1996
resource poor settings, international donors, national policy makers and
local providers have directed their attention to expansion of services
ignoring for the most part the nature of these services. Not surprisingly
then researchers investigating the health sector in developing countries
rarely focus explicitly on the assessment of existing services [Barbara
1990].
There have been very few studies of institutional based health care
services and practitioners and even fewer on the private providers of
health care. The application of the concept of quality is relatively new to
the Held of health. In the overall scenario no significant impression has
been made on the issue of quality with regard to the country's health care
services. Nevertheless in a short period a number of studies have been
undertaken on the aspect of quality.
Only recently there have been studies conducted on the aspect of
quality. A search of the studies conducted in India post-1985 using the key
word ‘quality’ identified 30 studies. This was due to the fact that quality
as a term has been used rather loosely to mean many things. The various
studies on quality were baseline and evaluation studies, which looked at
specific components of service delivery and programmes. Majority of the
studies restricted themselves to the family welfare programme. These
studies were too narrow and focused in their approach. The studies mainly
dealt with the client perception of quality, utilisation, acceptance, role of
demand and supply factors. These studies have shown several shortcom
ings in the programme operations. There were a few major studies which
focused primarily on the aspect of quality. To mention few, the ICMR
conducted a study evaluating the adequacy of facilities, humanpower and
quality of family welfare services offered by 398 primary health centres.
Table 8: Qualifications of Doctors and Place of Practice
Doctor’s Practice
Residence
a) same premises
b) does not reside
#Total
Doctor-owners operating alone
a) MBBS
b) Specialists
c) Other Systems of Medicine
Doctor-owners with Visiting Consultants
a) MBBS
b) Specialists
c) Other Systems of Medicine
# Total
EBA
EDA
Total
83
16
18
71
29
31
75
25
49
6
6
28
10
29
—
8
21
10
50
—
10
18
6
32
23
31
22
21
18
49
Note. (Figures are percentages with column = 100, except those marked #).
RJH
(New Series)
Vol II: 2/3
1996
151
selected across IS stales and 1 union territory [ICMR 1991). Another
comparative study undertaken by the Operations Research Group in three
states examined functioning of PHC/SC. its coverage, quality of service
and main bottlenecks, perceptions of people about functioning of PHC/
SC and reasons lor not utilising it [Khan and Tamang 1987). Recently the
International Institute of Population Studies also conducted a study in 3
states on the quality of family welfare services. The study examined the
perspeeption of clients and providers on quality of family planning
services provided and the relationship between perception of quality and
utilisation of services [Verma. Roy and Saxena 1994].
There have been very few studies conducted on the private health
sector in India. Two studies on knowledge and awareness among doctors
regarding treatment of tuberculosis and leprosy were conducted in
Bombay. Il was found that for treating tuberculosis patients. 100 private
doctors prescribed 80 different regimens, most of which were inappropri
ate and expensive [Uplekar. Shepard 1991 ]. In the study with regard to
leprosy, it was found lhal there was a gross lack of knowledge and
awareness among private doctors about leprosy and aboui the National
Leprosy Control Programme [Uplekar. Cash 1991]. Another study exam
ined the use of irrational medicines and injections by the doctors in the
private health sector. Out of a total of 633 prescriptions analysed from 27
private clinics it was found that 28.9 per cent were of irrational drug
combinations, 9.6 per cent were for hazardous drugs. 45.7 per cent were
unnecessary drugs and 26.5 per cent were unnecessary injections [Phadke
cl al 1995]. Another study conducted by H Vishwanathan and J E Rhode
on diarrhoea brought out sharply that 62 per cent of ‘doctors’ identified
by local respondents had no formal medical qualifications [Vishwanathan
and Rhode 1990]. The presence of these ‘doctors' is prominent especially
in the remote rural areas of the country. A study conducted in Madhya
Pradesh showed that of all those treated in a private facility, 52.24 per cent
of the illness episodes in
T,\ble 9: Services Provided
rural areas were treated by
EBA EDA Total
licentiaJes/RMPs and in Types of cases treated
contrast in urban areas 17.83
Obstretics and
per cent were treated by
Gynecological
14
17
13
such practitioners [George
Medical
22
19 20
—
et al, 1993]. The Medico
Surgical
16
26
19
16
Friend Circle conducted a Gynecological and Medical 22
Surgical and Medical
8
6
10
public survey to understand
4
11
• patient’sexpericnces, views Gynecological and Surgical
19
All types oi cases
22
16
and perceptions on the pri49
#
Total
Hospitals
18
31
vate health care system. The
findings bring out various Note: (Figures, except #. arc in Percentages,
aspects of the private prac- columns=100 )
152
RJH
(New Series)
Vol 11:2/3
1996
litioners functioning in terms of waiting period, treatment provided,
reasonability of charges among others [Medico Friend Circle 1990].
With regard to hospital-based studies with specific reference to qual
ity, Mahapalra and Berman conducted two studies based on secondary
Table 10: Examinations. Emergency and Accidents
Pathology Lab Present
Referral for path, exams
a) Same villagc/town
b) Different villagc/town
Blood Bank Present
Referral lor blood
a) Pvt. Blood bank
b) Cottage Hospital (Karad)
c) Pvt Teaching hospital (Karad)
d) Refer the case elsewhere
Emergency cases
a) Treat the cases
b) Preliminary treat, given & refereed
c) Refer directly
d) Do not admit
Place refereed
a) Refer to Private Hospitals
b) Refer to specialists
Treat for minor accident cases
a) Treat the case
b) Preliminary treatment and refereed
c) Refer to private hospitals
d) Refer to public hospitals
c) Do not admit
Treat for road accident cases
a) Treat the case
b) Preliminary treatment
c) Refer to Private hospitals
d) Refer to Public
c) Do not admit
Treat for domestic accident cases
a) Treat the case
b) Give preliminary treatment
c) Refer to private hospital
d) Refer to public hospital
e) Do not admit
# Total
EBA
EDA
Total
11
23
18
61
16
0
24
—
0
35
3
0
11
0
67
22
26
10
32
13
20
6
45
16
—
11
56
6
3
16
19
6
2
14
33
6
61
6
32
3
45
4
33
17
11
11
28
68
6
3
23
55
10
6
4
25
6
28
11
6
28
26
16
13
6
39
18
20
12
6
34
11
11
28
50
18
48
6
6
6
32
31
35
8
14
4
38
49
Note'. Where per cent totals don't equal 100 the balance are ‘No - responses’
(Figures arc percentages, except #. column =100).
RJH
(New Series)
Vol 11: 2/3
1996
153
data of 108 secondary level public hospitals in Andhra Pradesh. The first
study looked at the utilisation and productivity, the second study dealt
with the performance service-mix ratios [Mahapatra. Berman 1990 and
1992]. Nandraj conducted a study of 24 randomly selected private
hospitals and nursing homes in Bombay city. Il documents their poor
condition and an absolute lack of concern for any minimum standard
[Nandraj 1994].
Presently, as mentioned earlier in India there are no standards <r
guidelines being enforced for the running of private hospitals and nursing
homes. For the running of government hospitals there are basic require
ments and guidelines laid down. Various government and non-government bodies have attempted and evolved standards for minimum require
ments in hospitals and nursing homes. The various government bodies
which have some standards for private hospitals are the Municipal
Corporation of Bombay. Delhi Development Authority and Karnataka
Government. The standards incorporated in the legislations do not cover
various aspects of the hospital functioing are very limited in scope of
monitoring private hospitals. In most of the places these are not being
implemented for various reasons. The Bureau of Indian Standards (BIS)
have laid down standards for hospitals ranging from 30 to 250 beds. The
standards which are laid down are applicable to both private and public
sectors. National Institute of Health and Family Welfare (NIHFW) has
laid down standards but largely for 50 and more than 50 bedded hospitals
and that too only for equipment. Most of the standards laid down by BIS,
NIHFW etc. are meant for relatively larger hospitals located in major
urban areas. In Maharashtra the government hospitals have to follow the
Hospital Administration Manual for the running of the hospitals. Andhra
Pradesh Vaidya Vidhana Parishad has laid down standards for secondary
level hospital in the soveminent sector which Table No 11: Services Proved by Facilities
comes under it. One of the
objectives of the present
study was to document and
review various guidelines
available in the government,
NGO and private sectors for
the minimum physical stan
dards necessary for provi
sion of health care of vari
ous kinds.
In the present study we
selected two talukas of
Satara district in Maha
rashtra. one economically
154
Major Minor Labour Sterlisation
OT
OT Room
Room
OB/Gyn
5
Medical
3
Surgical
8
OB/Gyn
and Medical 6
Surgical
and Medical 3
OB/Gyn
and Surgical 2
All care
9
Total
36
2
2
2
-
4
1
3
1
3
1
-
2
1
2
8
1
3
20
3
8
7Vb/e:(Figures are percentages column =100).
RJH
(New Series)
Vol 11:2/3
1996
developed and one economically backward, and in them a sample of
general practitioners and nursing homes / hospitals to explore their
existing status and how they fit into a framework of minimum standards
for provision of health care. The framework of minimum standards
for quality care have been evolved on the basis of existing informa
tion discussed as per the findings and its critique at a workshop orga
nised by CEHAT to facilitate the placement of findings of the present
study.
In developed countries quality as an issue has been in the forefront for
management of various types of institutions. Various systems and meth
odologies have been developed to study different dimensions of quality.
These were developed foremost in the industrial setting and (hen later in
the health care delivery systems. The same trend follows in India. Indus
trial units look up the issue of quality and began developing quality
standards in their production, sales, operations, management systems,
among others. The entry of multinationals, the opening of the Indian
economy and the increased pur
Table 12: Operation Theatre/ Labour
chasing-power and consciousness
Room
in the middle class consumer have
73
Operation theatre present
been some of the factors which
Area adequate
11
have raised quality awareness.
Labour room present
16
‘Quality’ is the new buzz word
Condition of the walls
with International Standards Good clean
36
Organisations (ISO) certifications
64
Dirty and Bad
2
being chased by an increasing
Height below 8 feel
98
above 8 fl
number of organisations. As re
Condition of ceiling
gards health care services as yet
51
Clean
nosignificant impression has been
Bad/Dirty/ Leaking/ Paint peeling 49
made on the issue of quality in this Condition of Floor
country.
54
Clean
For the present study we had to
Dirty/ dusiy/Cracked/ Uneven
46
Lights
evolve a study design and use
55
different methodologies for col Sufficient
45
Not sufficient
lecting the required information.
71
Operation table present
1'his was due to the limited amount
Lithotomy present
37
of information and the secretive
Placement of equipment
nature of the functioning of the
43
Organised
57
private health sector in the coun
Unorganised
49
try. Studies on public health ser Trolley for instruments present
39
vices arc relatively easier to con Shadowless lamp present
Wash basin with long handle tap
duct since the data is available,
35
Present
though often its accuracy is ques
tionable. The present study is ex Note: (Figures are percentages, except
#, column =100).
ploratory in nature and mainly an
RJH
(New Series)
Vol II: 2/3
1996
155
enquiry into the existing nature and physical infrastructure available with
the practitioners and hospitals operating in the domain of private health
care.
Maharashta is considered one of the more developed states in India.
The average per capita income in the slate was Rs 3.168 during 1982-83
to 1984-85. ranking second only to Punjab. Though majority of the
population is engaged in agriculture, it is one of the industrially more
developed stales in the country. A word of caution about Maharashtra
being a more developed state in India - if the Bombay-Thane-Punc bell
is excluded the state income may even fall below the average income for
the country as a whole. Thus the stale is characterized by uneven
development among its various regions. This pattern of development
gets reflected within the districts [George and Nandraj 1993J. Using
the CMIE scores for districts we categorised them into developed.
average, and underdeveloped. Shortlisting all the average districts and
Tilling oilier criteria like logistics, resources, short time frame, and the
nature of the study we selected Satara district randomly from a final list
of six districts.
T^ble 13: Equipment and Instruments
The district of Satara reflects a
in all Hospitals
trend like in many of the districts
Total
in lhe country where some of the Equipment and Instruments
regions are developed and some B.P Instrument
98
63
underdeveloped. There are around Larangyscopc Adult
53
4356 co-operative societies of all Larangyscope Child
Refrigerator
39
sons in the district, a large num ECG monitor
10
ber of them being connected and Sterliser
65
dependent on the sugar industry Stretcher
51
49
which is controlled by politicians; # Total
16.13 per cent of the irrigated Note: (Figures are percentages, except
land is used for sugarcane, oil #. column =100).
seeds, and cotton cultivation.
Table 14: Equipment and Instrument*
From among the 11 tchsils in
in OB/Gyn Hospitals
Satara district, we selected Karad
and Patan lehsil. Karad being a Equipment and Instruments
Total
developed tchsil and Patan un
81
derdeveloped. This was on the Suction machine
Oxygen cylinder with valves
52
basis of broad socio-economic OB forceps
81
indicators.
Labour table with U-Cut
As this was an exploratory
Lithotomy
7-4
74
study we used a combination of Baby Weighing Machine
59
methodologies. Firstly from lhe M.T.P Sets
# Total
27
sources such as District Statisti
cal Handbook, District Gazetteer,
Note: (Figures are percentages, except
Census documents, offices of the #. column =100).
156
RJH
(New Series)
Vol JI: 2/3
J996
district health officer and the block development officer, documents of
the various medical councils and associations, etc we collected basic
information on the district. There was paucity of information on private
health facilities with the government bodies, including the DHO’s office.
No compilation of their number, size, care provided, facilities available
was available in the district. There was no information on the number of
doctors practising in the district. Registration of the hospitlas in the
district was not being done in spite of the fact that in Maharashtra under
the Bombay Nursing Home Registration Act (BNHRA) of 1948 it is
mandatory to register with the local body.
The team had to make use of various handbooks, and membership lists
compiled by different local associations of doctors, chemists and medical
representatives. These were available for the tehsil of Karad and Palan
town. These were deficient in many respects since some of them had only
names of their members, some had restricted it to the system of practice,
others had names of only those who had paid the subscription. There was
inadequate information on the doctors practising in the Indian systems of
medicine.
From the lists provided by the various local associations and the
Medical Council list, the lists were cross-checked and in addition key
informants such as drug stores, senior doctors, government health offi
cials, etc were contacted for updating the list. After this exercise a final
list was compiled of the practitioners and institutions in the two selected
tehsils of the district. Care was taken to include practitioners from
different systems of medicine and specialties. The names of those persons
practising without any qualifications were collected through informal
discussion with kev informants in the villages such as shopkeepers,
PHC doctors, private qualified
doctors,
local
voluntary
Table: 15 Select equipment and
Instruments for Surgical hospitals
organisationsetc. Ouraltempt was
to cover around 50 practitioners Equipment and Instruments
Total
and 50 hospitals and nursing
Shadowless
Lamp
65
homes from both the tehsils. This
Oxygen Cylinder with Valves
56
was considered a fairly sufficient
Lahem Table
26
sample to understand the func Electro cautrey unit
39
tioning and examine the physical
Ventilator
13
standards available in them.
Defribilator
9
57
The final sample consisted of X-ray viewers
39
53 practitioners and 49 hospitals. X-ray machines
91
In Palan tehsil 18 hospitals and 22 Autoclave
Boyle's apparatus
0
practitioners were covered under # Total
23
the sample. In Karad which was
the developed tehsil 31 practitio Note: (Figures are percentages, except
ners and 31 hospitals and nursing #, column =100).
RJH
(New Series)
Vol 11: 2/3
1996
157
homes were covered. The selected sample in the two tehsils was roughly
proportionate to the actual number as found in our compilation The
sample with regard to practitioners consisted of those qualified and
also those not qualified and from various systems of medicine, to
whatever extent possible in the same proportion as in the population.
and different regions in the tehsil. Il was done in order to capture the
variations in size and spread across various socio-economic divisions
within the tehsil.
The sample for both the tehsils was from the tehsil headquarters, the
villages where the hospitals were located and one PHC village and its sub
centre (SC) village and a remote village in each tehsil. Care was taken to
interview those doctors practising in remote villages which had no public
health facility.. In the rural sample care was taken to select GP’s from the
PHC village. SC village and a remote village of the particular SC village.
This gave us a diverse sample. An effort was also made to interview
doctors during bazar day in the village bazar. (The terms hospitals and
nursing homes have been used synonymously and henceforth will be
mentioned in the text as hospitals).
The data collection was undertaken during January, February and
March 1995. As this was during the winter season the doctors were
relatively free, since the morbidity load according to them is fairly low
during this season. The tools of data collection consisted of a structured
interview schedule along with an observation schedule and checklist for
equipment.
Contrary to our expectations the response of the doctors practising and
of hospital owners was quite positive. Initially there was some apprehen
sion like some were under the impression we were from the income tax
department, many of them were exposed to a research study for the first
time and did not know how to react, a few were openly hostile and did not
give the information etc. But this was mainly in Karad laluka. The
positive side was that many doctors especially in smaller towns and
villages were friendly and went out of their way to assist us in many ways.
The persons who feared and were worried were those practicing without
any qualification. In one instance the respondent who did not have proper
qualification informed his brother who was a sub-inspector in the Bombay
police to make inquiries about us.
A one-day workshop was held on ‘Minimum Physical Standards for
Private Hospitals and Nursing Homes’ in Bombay for researchers.
government officials, doctors from the public and private hospitals from
urban and rural areas. A consultant was appointed to evolve minimum
standards for the hospitals taking into consideration various aspects of
functioning. A background document ‘Proposed Minimum Standards for
Private Hospital and Nursing Homes: Upto 30 bedded unit Providing
Mcdical/Surgical/Maternity Care’ was was discussed in the workshop.
158
RJH
(New Series)
Vol 11:2/3
1996
Various valuable suggestions and comments where emerged have been
incorporated in the final document. The document evovled was an
independent excersise from the field based study. While efforts were
made to collect substanial information from the field based study and
compare it with the standards evovled, it was not possible to examine all
the aspects of the standards evovled due to the nature of the study. (Eg
Information was collected on the sources of supply of water and its
storage but we did not collect information on the amount availble per
day).
There were various problems faced by the researchers during the
conduct of the study. The most important was that of inadequacy of data
on the size, functioning and nature of the private health sector. This was
compounded by the fact that there few studies available on private
health facilities and the few studies that were available dealt with only
the urban setting. This becomes more frustrating when neither the
government nor medical associations/councils have any kind of informa
tion on this sector. The second problem related to the size of the
institutions which ranged from the three beds to 500 bedded hospitals.
This made the task of categorising different aspects related to physical
standards between two extremes difficult for analysis. It was difficult to
study such a wide variation in the present study. The third problem was
in terms of defining the various units under study and their various
functions. Practitioners in the district ranged from the road side quick
fix operator to the super specialists. In between we had persons claim
ing to be doctors and practising. Further there were those qualified in
a formal system and those trained by tradition. A related problem was
with reference to defining qualitative terms for the observation schedule.
We have come to the conclusion that the observations are subjective
since we did not standardize various definition such as clean, adequate,
proper etc.
Another problem was with the instruments and their numbers. We
went into details of certain instruments such as scissors, scalpel sets,
gauze, kidney trays. In some of the bigger hospitals they would laugh at
us for asking such questions, since many of them were having it by the
dozens but on the other hand smaller setups would not have them in
sufficient quantities. Another problem was that all the researchers
involved in the data collection were from the social science backg
round. It was difficult for the researchers to grasp especially when
clinical terms were used and with the names of, drugs, instruments
and equipment. We feel that a study of this kind should have a person
with a medical background. Two other major limitations of the study was
that it covered only aspects of physical standards (which included
staffing) and that it was not possible to check records of the hospital in
most cases.
RJH
(New Series)
Vol II: 2/3
1996
159
II
Private General Pactice: Nature and Status
Provision of routine medical care for a wide range of diseases and
symptoms is mostly in the private sector. While government health
centres exist across the length and breadth of the country they have failed
to provide the masses with the basic health care which the latter expect
The scope of this document does not permit a detailed analysis as to why
the government health care has failed. It will suffice to say that a fairly
large investment by the public sector in health care is being wasted due
to improper planning, financing and organisation of the health care
delivery' system - the national public sector health expenditure today is Rs
10.000 crore per year being spent on 4800 hospitals. 11.100 dispensaries.
23,000 PHCs, 140,000 subcentres and various preventive and promolive
programs, including family planning. The state employs 125.000 doctors
and also runs 108 medical colleges. But the services provided by the
state do not meet the expectations of people and as a consequence the
latter are forced to use private health care whatever be its quality and / or
effectiveness.
Private medical practice flourishes almost everywhere. The range ol
providers are also varied, from the herbal and witch doctor to the modern
unqualified or quasi-qualified ’quack’, and to the qualified practitioners
of different systems of medicine, many of whom also indulge in quackery.
There is no firm data available on the entire range of practitioners. Even
the medical councils of the various systems of medicine have failed to
maintain a complete register of active practitioners. The census is another
source but the latest available census data for occupations is for 1981
Hence estimates from various studies or indirect extrapolations arc the
only methods for fixing a proximate size of medical practitioners.
Ourestimate based on indirect extrapolation using the assumption that
all doctors (compiled from lists of the various medical councils) minus
government doctors is equal to the private sector. Today there are about
11,25,000 practitioners registered with various system medical council'
in the country and of these 125,000 are in government service (including
those in administration, central health services, defence, railways, stale
insurance, etc). This leaves 10,00,000 doctors of various systems ol
medicine floating in the private sector and one can safely assume that
atleast 80 percent of them (800,000) are economically active and aboui
80 percent (640,000) of the latter arc working as individual practitioners
Apart from this there are as many unqualified practitioners as estimated
by the UNICEF/SRI-IMRB study in Uttar Pradesh, and if we accept this
estimate then the total medical practitioners active becomes about
13,00,000, that is one such practitioner per 750 population [Hema and
Rhode 1994]. Another study in Ahmednagar district showed that the
160
RJH
(New Series)
Vol! 1:2/3
1996
c
district had 3060 active medical practitioners [FRCH 1993]. Ahmednagar
being an economically average developed district, if we multiply this
figure by 452 districts we get a proximate figure of 13.8 lakh practitioners
(or the country as a whole which is quite similar to the earlier estimate.
The latest census figures were not available, and in Satara district we were
unable to do a complete listing of medical practitioners because of the
limited objectives of the present study and the constraint of time and
resources. Apart from this no other information about the size of the
health sector is available. This problem of poor availability of informa
tion, especially about the private health sector calls for intervention to
make the various medical councils and the local bodies more accountable
and to improve their recording and information systems.
Unlike the estimate which was possible in the Ahmednagar study
ncnlioned earlier the limited scope of the present study did not allow the
time nor had the resources to throw our nets wider to collect information
on the size of the private health sector. The objectives of the study are
limited to the existing status and nature of the practice and how it
conforms to accepted minimal standards or quality of care. In Satara
district from the two sample units, one a developed taluka and another a
backward taluka, 31 and 22 medical practitioners were selected, respec
tively, to explore the nature of general practice.
Profile of Medical Practitioners
The number of medical practitioners in the EDA is expected to be
much larger than those in the EBA since medical practitioners tend to
concentrate in developed markets and our sample reflects that. The same
is true for the urban/rural distribution in the two areas, though this may be
closer to the actual proportion. The EBA is almost wholly rural except for
the taluka headquarters which we have classified as an urban area. The
EDA has well developed urban centres and thus even has a private
teaching hospital, making for a much larger concentration of medical
practitioners in urban centres. Urban concentration of health care provid
ers is a well known fact - 59 percent of the country’s practitioners as per
1981 census (73 per cent allopathic) are located in cities, and especially
metropolitan ones (Census 1981). For instance, of all allopathic medical
graduates in Maharashtra 60 per cent are located in Bombay city which
has only 11 per cent of the state’s population (see Table 1).
This selective concentration of health care providers then becomes a
major concern to be addressed to, especially since the health care market
is supply induced and when people fall ill they are wholly vulnerable and
forced to succumb to the dictates of such a market. The consequence of
this is that access to health care providers gets restricted to those living in
urban and developed pockets and the vast majority of the rural and EBA
RJH
(New Series)
Vol II: 2/3
1996
161
populace have lo make do with quacks or travel to the EDAs forsalisfymg
their health care needs. In fact, studies have shown that those living in
EBAs spend about as much on health care as those in EDAs [Duggal.
Amin 1989: George el al 1993] and hence relocation can become
economically viable for qualified private practitioners. Thus the state and
the local bodies must intervene to restrict the number of practitioners from
setting up practice in EDAs. This calls for some locational policy which
can establish a relative socio-geographic equity.
The gender and age distribution show a very high male concentra
tion in both the areas and as one would expect a larger proportion of
women practitioners are located in the EDA. Macro data also show
that the proportion of women doctors is abysmally low. For instance
the 1981 census reveals that women constitute only 10.8 per cent ol
all doctors (4 per cent in rural areas). This overwhelming male domi
nance of the medical profession has had its adverse impact on health
care of women, especially of care specific to women. Further the women
who become doctors also tend to locale themselves in the larger urban
centres.
As regards age distribution of the active doctors, the mean age of the
sample is 37.75 years and 42 per cent of them are below 35 years. The
mean age of the EDA practitioner is higher and this is perhaps indicative
of the push factor in EDAs as a consequence of over concentration which
is forcing new practitioners to move gradually into EBAs (half of EBA
practitioners are below 35 years) in larger numbers. If this is happening
it is a welcome trend and a policy to encourage youngsters to move into
underserved areas and conversely a policy to discourage new entrants into
the profession from selling up shop in overserved areas would be helpful
— lhe local governments have an importani role to play here.
When we launched on ihis study the first question which confronted us
was how to determine who was a qualified practitioner. After much
debate and consultation we decided to ‘qualify' those practitioners who
had obtained a degree or diploma from a recognised university or
statutory board of allopathy, homeopathy, ayurveda. unani and siddha.
All others who did not fit the above definition have been regarded as
unqualified and this includes lhe so called group of registered medical
practitioners (RMPs), unless of course lhe latter had an actual registration
with a recognised board or council (some very old practitioners in
Maharashtra, for instance do have such a registration).
Thus in our sample we have ‘recognised’ two categories, one called
‘accredited degree or diploma' and the other called ‘unqualified’. We
would like to note here that by labelling this group as unqualified we are
in no way commenting on their abilities and skills in providing care. Our
perception being coloured by modern science we have only made catego
ries to facilitate our analyses.
162
RJH
(New Series)
Vol 11:2/3
1996
In our sample of practitioners we see that one-fourth of them are
unqualified and the difference between the EDA and EBA on this count
is very large. The EBA has unqualified practitioners nearly five times
that of EDA. This reflects not only the fact that (he unqualified arc
largely located in EBAs but also that EBAs have weak markets (low
purchasing power) and probably no concern at all for regulation. The
EDAs with large concentration of practitioners arc also well developed
markets and some unwritten regulatory mechanisms operate due to forces
of demand and supply but as is well known these forces vis-a-vis the
health sector are very weak because health care has always been a supply
induced market.
Of all the qualified practitioners in the total sample 40 per cent are
allopaths, 52.5 per cent from Indian systems and only 7.5 per cent from
homeopathy. Between the EDA and EBA again a vast difference as per
the pattern discussed above prevails. Thus in the EDA of all qualified 53.6
per cent are allopaths and 42.9 per cent from Indian systems, and in the
EBA conversely only 8.3 pcr cent arc allopaths (over six times less than
EDA) and a whopping 75 pcr cent from Indian systems.
Further, we see that those qualified in modern medicine tend to locale
in EDAs and in our sample the EDA has six times more allopaths than the
EBAs. The Indian system practitioners which is the largest group of
practitioners in the country, as also in our sample, is more or less equally
distributed in the EBA and EDA. The 1981 census also indicates a similar
pattern - the allopaths in urban areas (EDA) are three limes more than in
the rural areas (EBA), and the Indian system doctors distribution is
more or less similar, 55 pcr cent in rural areas and 45 per cent in urban
areas (if we exclude govternment doctors from the census data then the
similarity with our sample becomes very close) (Census 1981). The
findings of the Ahmednagar study also support the findings in Salara
district. In Ahmednagar 77 per cent of allopaths were in EDAs and 23 per
cent in EBAs and for Indian systems the percentage distribution was
68 and 32. respectively [FRCH 1993]. And in our sample of all the
allopaths 94 per cent were in EDAs and of all Indian systems 43 per cent
were in EBAs.
The diversity and complexity discussed above becomes a serious
concern in the context of the fact that an overwhelming majority of them,
including unqualified, are practising allopathy. Thus, a major question
which needs to be addressed is how do we view practitioners of different
systems of medicine, how should they be distributed in the population and
what type of care should each group be allowed to administer. While
recognising the advantages that each system may have, overall it is
generally accepted that modern medicine deserves the priority it com
mands today and hence it should become the basic system of medicine
(until another system establishes its ‘superiority’) and hence medical
RJH
(New Series)
Vol II: 2/3
1996
163
education must produce a single stream of basic doctors trained in modern
medicine and those who wish to acquire knowledge and skills of other
systems should have the necessary facilities to pursue those as electives
or specialisations. We strongly feel that this is an important issue of
concern for policy makers. If some steps in the direction suggested are
not undertaken with due seriousness then the existing system hier
archies (with allopathy as dominant and homoeopathy and ayurveda
qualifications serving as a legitimacy to practice modern medicine or as
alternate to allopathy for the patient when the latter fails to cure) will
continue and quality care or care with basic minimum standards will
never be achieved.
Related to having an accredited qualification is the question of regis
tration with the appropriate authority and renewing the registration
periodically. Legally speaking registration gives the qualified practitio
ner the right to practice medicine and it is the duty of the concerned
authority to assure the consumers of such health care that no practitioner
without appropriate registration is treating patients. For instance, the
Maharashtra Medical Council registers all doctors qualified in allopathy
and permits them to set up medical practice in the state. Similarly each
state or region has such a council. The Indian systems and homeopathy
also have their respective councils and give registrations for practising the
relevant system of health care. The registrations given arc not permanent
and are usually for five years and it is the responsibility of every
practitioner to renew their registration at the appropriate lime failing
which the council can prevent the practitioner from practising. It is well
known that the various medical councils have been lax and negligent and
have not been performing their statutory duties. As a consequence the
medical practitioners have also become lax and a large number of them
are practising today not only without proper registration but also without
the requisite qualifications. All this then becomes a threat to the patient
who is thrown at the mercy of ‘doctors’ who may not have the necessary
skill and practice with half baked knowledge. Thus, even something for
which there is a law and an authority to administer it, it is being neglected.
It is the responsibility of the State to see that its own constituted
authorities are carrying on with their responsibilities effectively.
In our study sample we found that only 55 per cent of the practitioners
had the appropriate registration and even from among all the qualified
practitioners only 72.5 per cent were registered. Between the EDA and
EBA the former had 61 percent of practitioners registered and the latter
45 per cent and from those qualified the percentages for the two areas
were 68 and 83. respectively. Of course, as mentioned earlier the EBA has
nearly five times more unqualified practitioners than the EDA. All this
clearly demonstrates both the laxity of the concerned authorities and the
unconcern of the medical profession for proper standards and quality care
164
RJH
(New Series)
Vol ii: 2/3
1996
(or treatment of patients. The health care administration needs to pull up
its bootstraps on the one hand and the concerned medical professionals
must lake a lead to pul lheir own house in order on the other hand.
When people fall i 11 the first line of contact is usually the neighbourhood
general praclilioner (GP) or some government facility like a dispensary
or primary health centre or a hospital. That the GP is the most sought after
health care provider has been confirmed now by a number of studies, and
this ranges from 60 per cent to 85 per cent of all non-hospital care which
patients seek [NSSO 1987; Duggal, Amin 1989; Kannan, 199I;NCAER
1992; George et al 1993]. But we have already seen above that many GPs
are there in the market place, and more so in the EBAs where the majority
of the population resides, who may be more a risk than help to patients
seeking care (see Table 2).
While modern medicine has simplified treatment of most illnesses and
symptoms to a few drugs (even making many of us self-prescribcrs) its
commercialisation has brought in more problems than the benefits it has
created. The pharmaceutical industry and the medical equipment industry
.have both caused much harm to the character of the medical profession.
Their marketing practices have lured a large majority of medical profes
sionals (and not the unqualified quacks alone) to increasingly resort to
unnecessary and irrational prescriptions of drugs, the overuse of diagnos
tic tests, especially the modern ones like CAT Scan, ultrasound, ECG, etc
and uncalled for references to specialists and superspecialists (for all of
which a well organised kickback system operates - the givers and
beneficiaries calling it commission’). These issues, while they fall within
the context of standards and quality of care, are extremely difficult to
study and hence only anecdotal information is available. However,
through indirect methods some amount of information may be derived as
was done in one study in Satara district of drug supply and use. This study
lends credence to the anecdotal evidences we so far had about unneces
sary and irrational drug prescription and use. We conclude that there is a
very high proportion of use of unnecessary, irrational, hazardous drugs
and unnecessary injections, especially in the private sector, to the extent
that 69 per cent of expenditure on prescriptions is a waste [Phadke et al,
1995]. In the present study such an exercise has not been possible because
we have focused largely on the supply side and not looked al usage.
In the preceding section we discussed the qualifications of the practi
tioners and even mentioned that the non-allopathic and unqualified are in
reality largely practising modern medicine even when they are not trained
for it. This fact is clearly borne out amongst the sample practitioners
where we see that as many as 79 per cent are practising only allopathy as
against 30 per cent of the doctors in the sample who are qualified
allopaths. If we add to this those practising allopathy alongwith their own
system in which they are trained then the total of those actually practising
RJH
(New Series)
Vol II: 2/3
1996
165
allopathy becomes 94 per cent. The trend in both the EDA and EBA is
similar with the EBA having a slightly larger proportion of those who
practice allopathy alone - in the context of the fact that it has only 4.5 per
cent qualified allopaths amongst its practitioners the difference assumes
added significance.
When we cross-tabulate the actual practice data with the practitioner’s
actual qualification we see that almost all the allopaths practice only
allopathy, only 14 per cent of the ayurveds practice solely their own
system, none of the homoeopaths practised their own system independent
of allopathy and 77 per cent of the unqualified are practising purely
allopathy. The patterns in the EDA and EBA are similar. A proxy cross
practice rate reveals that the qualified allopaths have an insignificant
volume of crosspractice as against the ISM and homoeopath practitioner
As suggested in the preceding section something needs to be done at the
policy level about this crosspractice and the large presence of unqualified
practitioners. Action has to begin from reorienting medical education to
create a basic doctor in rational modern medicine and strengthening
regulation and control of medical practice by getting the regulatory
bodies to become active and committed to the cause of quality and
standards of health care.
The mean number of years of practice in the overall sample is 10.5
years. There is a significant difference between the EDA and EBA with
the former having practitioners with a greater number of years of
experience as compared to the latter. While the EBA has 68 per cent
practitioners with 10 or less years of practice the EDA has 64 per cent of
its practitioners who have worked for over ten years. In the sample 60 per
cent of the practitioners are working in rented clinics. In the case of EBA
practitioners 73 per cent have rented clinics in comparison to 52 per cent
in EDA. Further, in both the areas about 30 per cent of the practitioners
run clinics in more than one place. (For those having multiple clinics all
data pertains to the clinic in which the practitioner was interviewed). Onethird of the practitioners had indoor care facilities and in the EBA this
facility was there in one-half of the clinics. This difference is understand
able because the EBA is less likely to have nursing homes and hospitals
and hence individual practitioners do maintain some provision for day
care (usually saline drips) or for observation of a serious patient. In the
EDA this is not necessary because of easy access to hospitals and nursing
homes. Of all those who have indoor facilities half of them have one bed
and the other half two or more beds. The EBA has more of the former and
the EDA more of the latter. As regards laboratory services very few
doctors in either area have them and they usually refer to the nearest one
available. In the EDA a large majority of the doctors have their own
telephone connection whereas in the EBA very few do. A large majority
of the clinics are open six days of the week, however the EBA has many
166
RJH
(New Series)
Vol 11:2/3
1996
clinics open for all seven days of the week, and the average number of
hours the clinic is open everyday is 10.11 hours with a large difference
between the EDA (about 9 hours) and the EBA (12 hours) (in fact two
practitioners from the EBA staled that theirclinic runs for 24 hours !].The
differences due to location arc as expected and reflects the nature of
supply of services in the two areas, clearly establishing that the supply is
related to potential of making profits. Thus, the EBA docs not have
laboratory services because a minimum volume of such cases perhaps
does not exist or more properly cannot be induced in the EBA market
whose purchasing capacities are much more limited to make such an
investment in the EBA viable.
The number of cases or patients seeking care from practitioners has
been recorded in a number of different ways so that it can gives us some
methodological insight. Thus, we first recorded the number of cases
treated on the preceding day, then questioned about cases treated during
last week, further during the last month new cases (incidence) and old
cases continuing from the earlier month into the last month (the latter two
together constituting the monthly caseload), and the number of cases
treated per day during the monsoon months. Since case records arc not
maintained properly by most practitioners the figures most often are those
reported by the practitioner him/herself. Therefore, recall plays its role.
Our assessment is that the preceding day’s figures and previous week’s
figures are the most accurate and the others are approximate. Wherever
possible monthly figures were checked against records available at the
clinics and our judgement is that the monthly figures are quite accurate,
though an underestimate. Of course, the most appropriate would have
been to sit through the entire work-day of the practitioner and record the
actual attendance, but this has not been possible due to the limited lime
and resources on our hands.
The data on workload shows that practitioners are seeing 20 patients
per day, 125 patients per week and 400 cases per month. During the
monsoon months they estimate that their work load increases by 63 per
cent to a daily average load of 32 patients. The difference between the
EDA and EBA is substantial. The EBA practitioner is treating on an
average more patients than the EDA practitioner. The difference is 20 per
cent on a daily basis and 24 percent on a weekly basis. This is perhaps due
to the fact that EDA has a greater concentration of practitioners as against
the EBA. This then allays the apprehension of doctors that patients are not
available in the backward and rural areas. The EBAs and rural areas have
as much a demand for health care as the EDAs and hence there is much
sense in implementing a policy of locational restriction in overserved
areas and locational encouragement in underserved areas through, for
instance, fiscal and lax related measures. Further, the question of a lack
of purchasing power, which is very valid, can also be overcome by
l\.IH
(New Series)
Vol II: 2/3
1996
167
involving the qualified practitioners into a stale sponsored universal
health care system which assures them a clientiele and income through a
system of family practice. For the latter to be successful a statute backed
locational policy for setting up medical practice becomes essential.
Along with this regulation, standards and quality care are necessary
features.
Visits by medical representatives (MRs) to clinics and other health
care establishments is an important feature of the health sector economy.
MRs from pharmaceutical companies are the lifeline of the drug industry
on the one hand and a source of information or misinformation for the
practitioners on the other hand. The network of MRs is so wel 1 entrenched
that even in the EBA as many as 73 per cent of practitioners are visited by
them. As is expected the EDA based practitioners are subjected to more
frequent contacts by the MRs because of the medical market and espe
cially the drug market being concentrated in urban and developed areas.
With the irrational and unnecessary drug prescriptions being-very high,
and the role of the pharmaceutical industry in perpetuating this calls for
policy intervention in regulating MR practices on one hand and creating
a mechanism for rational continuing medical education for medical
practitioners on the other hand.
Another disturbing feature of medical practice is the lack of maintain
ing case records by the practitioners. Only 38 per cent of the practitioners
had some semblance of a record but even these were not case records in
the true sense. The records were usually just what medicines they
administered and the charges to be paid by the patient and it was mostly
the latter so that they could keep track of which patient owed them what
- most of these’were maintained in dairies or notebooks. This is again an
important area of policy concern and practitioners must be legally
made liable for maintaining a proper record of a patients diagnosis,
treatment given, prescriptions, charges levied, etc. Proper records are a
must both from the perspective of the patient as a right to information as
well as for the doctor’s own protection to evaluate his/her interventions
especially when there are charges of negligence and malpractice against
him/her.
While carrying out the field study the investigators were provided with
an observation checklist to record qualitative aspects of the clinic. The
listing in Table 3 gives the percentage of clinics which ‘scored’ positive
on the feature observed. For instance noise level refers to clinics which
were not noisy or condition of floor refers to clean and well kept and type
of floor means tiled or display of registration means ‘Yes’ or pharmacy
means it exists as a separate entity etc. The findings arc self-explanatory
and show that overall conditions are not very conducive and that the EDA
clinics are a little belter off in some of the features. To improve these
general conditions the role of a regulatory authority becomes manifest.
168
RJH
(New Series)
Vol JI: 2/3
1996
There is an urgent need to have provisions as to where, how, what features
etc. a clinic must have in the interest of good medical practice and that of
the patients.
Like the observation checklist we had a checklist for equipment and
instruments. This list was developed in consultation with a number of
medical practitioners in Bombay. While this list may not be complete it
may also have some items which sound frivolous to ask and enlist.
Nevertheless, this list may be assumed to be a proxy minimum require
ment that any GP clinic must meet. The results arc evident in Table 4.
Again one sees that certain crucial requirements are lacking and the
difference between the EDA and EBA in some cases is sharp. Overall the
existing situation is quite bad - things like sterilisers, thermometers,
examination table, weighing machine, bed sheets, towels and napkins,
wash basin, etc. arc grossly lacking. Again a need to formulate a minimum
list of equipment which a general practice clinic must have in the interest
of good medical practice becomes necessary. Clinics without the agreed
upon basic minimum must not be granted permission to be set up.
Ill
Hospitals
Care in institutions like hospitals could be for the purposes of exami
nation, diagnoses of diseases, curing, surgical interventions, recuperat
ing, maternity and related purposes, among others. One can broadly
classify these institutions on the basis of their (i) bed strength, (ii)
location, (iii) ownership and (iv) services and facilities provided. Institu
tions range from those having five beds or below to corporate hospitals
having more than 500 beds, which are set up by corporate bodies as
business ventures. In addition to these there are companies who have their
hospitals to provide medical care to their employees. Lastly there are
hospitals which are run by NGOs and private charitable trusts.
There is under-estimation of data and the quality of data available from
official sources is unreliable. There are reasons to believe that the number
of hospitals in the private sector is much larger than what the available
data suggests. Health Information of India 1992, claims that there were
only 1,319 private and voluntary hospitals in Maharashtra, and the
Directory of Hospitals brought out by the ministry of health listed 1,174
hospitals in Maharashtra [CBHI, 1992]. But the Bombay Municipal
Corporation listed 907 private hospitals in Bombay city alone (excluding
Thane), on the basis of its registration data which again is an underesti
mate. Another instance of under reporting of data is brought out by a
survey undertaken by Andhra Pradesh Vaidya Vidhana Parishad, which
found the existence of 2,802 private hospitals and 42,192 private hospital
beds in Andhra Pradesh in 1993 [Mahapatra P 1993]. According to data
RJH
(New Series)
Vol II: 2/3
1996
169
available with GOI as on January 1 1991, however Andhra Pradesh had
only 266 private and voluntary hospitals and 11,103 private hospital beds
[CBHI 1992, op oil]. There is little information available at the district
level of the total number of health establishments. The data available is
of the same quality as available at the state and national level. The
Directory of Hospitals, 1988 lists only 47 hospitals and 1728 beds in
Ahmednagar district [CBHI 1988]. A listing of hospitals in the district in
1992 found that there were 274 institutions having indoor facilities. Out
of them 18 were government run, 224 from the private sector and 12 from
the voluntary’ sector [FRCH 1993]. Primary health centre’s were not
included in the listing. Data for hospitals from official sources is ver>
scanty and unreliable. Many stales do not file the required information
and the data that is provided is incomplete. Due to inadequate and
unreliable nature of data, planning for the health system becomes inaccu
rate and faulty.
Location
There were 49 hospitals involved in the study sample. From the EDA
31 hospitals were selected and 18 hospitals from the EBA. As expected
nearly three fourths of the institutions were located in the urban areas.
which consisted of the two tehsil head quarters and one other town.
Majority of them were from the EDA area namely Karad. This was due
to the fact that geographically the town of Karad is well connected with
other surrounding districts and tehsils, located on the national highway
and boasts of a private teaching hospital. In the EBA more than 50 percent
of the hospitals were located in Patan town. The findings reveal that
majority of private hospitals are located in urban areas of the developed
taluka. This is reinforced by other studies which looked at the location ol
private hospitals. A listing of institutions in Ahmednagar found that oui
of the 274 institutions 201 were located in urban areas and 71 were in rural
areas of the district [FRCH 1993]. Another study conducted in Andhra
Pradesh found that the highest concentration of hospitals homes were in
the towns and cities of the advanced districts. Even in the backward
districts they were restricted to major towns The private sector functions
in areas where there is a paying capacity. The growth of the private sector
in health care is directly related to the level of economic development.
This link is logical because it is the economically developed areas which
not only provide the market for these services but also the surplus to invest
in commercial enterprises [Baru R 1993].
The majority of the hospitals were established during the post 1980s
and these were in the urban areas of the developed district. Between 1968
to 1978 there were 12.2 per cent hospitals established, between 1980 to
J 990 44.9 per cent hospitals were established and 42.9 per cent hospitals
170
RJH
(New Series)
Vol JI: 2/3
1996
between 1991 to 1995. More than eighty percent of the hospitals in the
sample were established in the 1980s anti 1990s period. During this
period the private sector increased it’s presence and this growth look
place al a rapid pace. In the Ahmednagar study too it was found that out
oi 75 hospitals in the sample 51 percent of them were established between
1983 to 1991 [FRCH 1993]. The growth of private hospitals can be
noticed al the National level also. In India, during 1974, 16 per cent of the
hospitals and 21.5 per cent of the hospital beds were in the private sector
and rest were in the public sector. This proportion increased in 1992 to
57.42 per cent of the hospitals and 32.22 per cent hospital beds in the
private sector [CBHI, various years]. This clearly bears out that the
private sector increased its presence and became more dominant in the
last two decades even in the hospital sector.
The findings with regard to the type of management revealed that 92
per cent of them were individual proprietorship, 6 percent were run on
partnership basis, one was on a cooperative basis by doctors. All the
partnership run hospitals were in the EDA. Three-fourths of the hospitals
in the sample were operating from premises which was owned by
i hemselves. The doctor was the admimstrator/solc inchargc of the insti:ution for all the hospitals in the sample. The Ahmednagar study found
that out of 75 hospitals 93 percent of them were individual proprietorship
and 4 per cent were run on partnership basis. With regard to ownership of
premises 81 per cent of the premises were owned by the doctor running
it and in only 19 per cent it was on a rental basis [FRCH 1993]. The
findings on the type of management and ownership of premises clearly
brings out the fact that many of the medical practitioners are progress
towards building their own hospitals. The phenomena of individual
proprietorship of the hospitals by the doctors has been due to the
increasing number of doctors passing out from the medical colleges and
the fast returns on the investment in the health field. There is an increasing
tendency to start self-owned hospitals.
More than 90 per cent of the doctors running the hospitals were males.
There were only four female doctors in the sample running the hospitals
independently. In most cases the team found that it was the husband and
wife team running the hospital. The phenomena of husband and wife
running the hospital is quite unique. Discussions with the medical
fraternity and a glance al the matrimonial advertisements reinforce the
fact that in lhe medical profession spouses look out for partners with a
hospital in mind, therefore the specialization of the spouse becomes an
important factor. This requires a more detailed sociological study.
Further examination revealed that in 85.7 per cent of lhe hospitals
patients were admitted only by the doctor-owner and only in 14.3 percent
of the hospitals other doctors could admit their patients. This was more so
in lhe EDA, whereas in lhe EBA all of them were admitting only their own
patients. The findings on the type of management, ownership of the
premises and admission of patients, clearly brings out the fact that
many of the medical practitioners progress towards building their own
hospitals.
With regard to the qualification of doctor/owner it was found that 71.4
percent of them were qualified in the allopathy system of medicine. Out
of them lOwereMBBS. 10 were specialists with MD or MS and five were
MBBS with some diploma. Out of the 10 specialists nine were located in
the EDA of the district. This shows that the doctors with specialisation
prefer to set up hospitals in a developed area. There were 16.3 per cent and
10.2 per cent of the doctors who were trained in ayurveda and homeopa
thy systems of medicine respectively. Those qualified in other systems of
medicine were located in the EBA of the district. All the hospitals owned
by doctors from other systems in the sample were also providing care in
the Allopathy system. This is of serious concern as these doctors qualified
in homoeopathy and Indian systems of medicine are not trained in
allopathy. This has taken place since there are no monitoring mechanisms
or a regulator}’ authority operating in the country
None of the hospitals were being registered by local authorities or any
authority for that matter. In Maharashtra hospitals are legally required to
register with the local governing authority under the Bombay Nursing
Home Registration Act (1949). The act is applicable to the whole of
Maharashtra, however it is not being implemented. Many of the local
bodies did not have enough information regarding the Act and the bye
laws were yet to be formulated in some. Except for Delhi, Bombay and
Karnataka none of the states have any rules, laws, regulations or even data
for private hospitals and nursing homes. In Delhi there is the Delhi
Nursing Home Registration Act (DNHRA), 1953. In the above states the
various acts are not being implemented for various reasons. In most of the
states in India there are no regulations for private hospitals and nursing
homes. Despite having one of the largest private health sectors in the
world, providing 70 per cent of care in India, the fact that it should
function practically unregulated is a matter of grave concern.
The average number of beds was 11 beds per hospital in the study
sample. In the EDA the average was 12 beds as compared to 8 beds in the
EGA. More than fifty percent of the hospitals had a bed strength in the
range of 6 to 15 beds. Nearly a quarter of the hospitals in the sample
had a bed strength between three to five beds, most of them were
located in the EBA. It was generally found that the majority of the
hospitals located in the EBA had bed strength of less than 15 beds. In the
studies conducted in Bombay and Ahmednagar it was found that the
average bed size of a private hospital/nursing home was 10[FRCH 1993;
Nandraj 1994]. This raises issues of efficiency and effectivity of running
smaller hospitals.
172
RJH
(New Series)
Vol 11:2/3
1996
AH the hospitals in the study had OPDs. This was cither for a new
cases, consultancy or for followup of the indoor treatment provided
earlier. The average number of OPD cases was collected for the previous
day, last week and last month. On an average a hospital was attended to
40.14 OPD cases per day and 185.58 cases in a week. The OPD attendance
was higher in the EDA by about 25 per cent. Data collected for the month
could not be compared with actual records and hence there were substan
tial problems in reporting by the respondents because of the long recall
period and hence the data is not usable. The higher attendance of OPD
cases in the EDA is because people prefer to come to the developed/ urban
area in case of major ailments as specialists are available mostly in the
EDA and also due to rcferals by practitioners and institutions from the
rural areas. (See Table 6).
Admissions for indoor patients on an average in a hospital forlhe last
week worked out to 11 and for the last month 42 patients. The average
length of stay of patients in the hospitals was about 13 days for patients
under care during the month. The number of days’ stay was higher in the
EDA, about 16 days as compared to seven days in EBA. This could be
because the investment in the EDA for setting up a hospital is higher and
therefore to maximise returns the hospitals would be keeping the patient
for longer period of time. This could also be that for major ailments,
illnesses, surgeries, etc people prefer to go to hospitals located in the urban
centres in the developed areas which have specialists and other supportive
structures such as blood bank, laboratories and diagnostic facilities. The
other reasons are that many patients come from the periphery to the
developed areas for treatment. The occupancy rate for the month was on
an average 51 per cent of the beds available in the sample hospitals.
There are diverse categories of personnel who run the hospitals. They
could be broadly classified as those with qualification and those without
any formal qualification. The personnel could be further classified based
on the role they perform. There are doctors, nurses, paramedics, pharma
cist, various types of technicians to handle the equipment and conduct
various tests and the other supportive staff like ward boys, ayahas, recep
tionist, typist, security personnel, etc. The availability of human power in
the hospitals is of prime importance. Data regarding the staffing pattern
was collected with regard to the various categories of personnel employed,
their number and their qualification. Data on visiting consultants was also
collected. The full time staff generally consisted of medical and paramedi
cal workers. They were doctors, nurses, technicians, wardboys/ayahbais,
receptionist and others. These are the staff mainly running the hospitals
and those who are employed in the institutions. (See Tables 7 and 8).
Information on the place of residence of the doctor was collected. It
was found that out of 49 hospitals 38 of the owner doctors resided in the
same premises and of those not residing in the same premises nine
RJH
(New Series)
Vol II: 2/3
1996
173
stayed at a walking distance of five to 10 minutes from the hospital
There were a total of 69 full time doctors in the hospitals of the sample.
46 were qualified in modem medicine and 23 were from oilier systems of
medicine. More than 60 percent of them in the EDA. Out of a total of 23
doctors trained in other systems 57 per cent were in the EBA.
Out of a total of 49 hospitals 39 per cent of them were being run by the
doctor-owner without any assistance from other doctors or visiting con
sultants; of these only half had any specialist qualifications and one-fourth
of them (all from the EBA) did not have a qualification in modern
medicine. An issue of grave concern is that as many as 29 per cent of the
hospitals were run by doctors trained/qualified in the other systems ol
medicine and were providing care using allopathic cures. The BNHRA
(1949) clearly mentions that the hospital should be under the management
of a qualified medical practitioner or a qualified nurse. It was generally
found that MBBS doctors prefer to practice with the aid of eithera full time
doctor or a visiting consultant. In Bombay it was found that out of 24
hospitals and nursing homes only 1 hospital had employed a post graduate
doctor, whereas 10 of them had doctors trained in other systems. Few
hospitals had provision for the doctors to be present round the clock.
Majority of the nursing homes utilised the services of visiting consultants
[Nandraj 1994].
The majority of the consultants were anaesthetists, followed by
surgeons and those trained in general medicine. The services of the
visiting consultants were mainly utilised by the those performing surger
ies. In the EBA the visiting consultants would visit the hospital on a
particular date. Usually the planned operations were performed on that
day. Most of the hospitals that utilised visiting consultants were located
in the EDA. In some hospitals the consultants were called when required
and in some they were visiting on a regular basis.
Qualified nurses were in short supply. There were only three
qualified nurses in the entire sample. Most of them were employing
unqualified nurses. They were usually women with some formal educa
tion trained by the doctors themselves. Many doctors claimed that the
nurses trained by them were also assisting them in the OT. Informal
discussions with them also revealed that they were performing other tasks
in the hospitals such as sweeping, dispensing of drugs etc.. Their hours of
work was very long and working conditions miserable, with poor remu
neration. The BNHRA (1949) states that a maternity home should have
on their staff a qualified mid-wife. In the study in Bombay it was found
with regard to qualified nurses only seven had employed them that loo
only one nurse each. Most of them had employed unqualified nurses who
were either trained by the doctor or had received training for about three
to six months from various private training institutes which have also
sprung up to meet the needs of private hospitals [Nandraj 1994].
174
RJH
(New Series)
Vol 11:2/3
1996
Other staff present in the hospitals were technicians, ward attendants.
sweepers and a category of personnel who performed all the jobs (OT
issistant, pharmacists, technician, ward attendant, sweeper, receptionists
etc.) in the hospital. Thus generally we see that employment of qualified
staff is an issue of serious concern in private hospitals. It was generally
tound that the availability of staff was in adequate and many of those
employed were not properly qualified. Many hospitals functioned with
doctors trained in other systems of medicine who administer allopathy
treatment in these hospitals.
There have been very few studies conducted on the services and
facilities provided by private hospitals. Data and information with regard
to the functioning of private sector is not forthcoming. Figures regarding
cases treated, diagnosis, type of treatment provided, amount charged etc.
are not easily obtainable from private hospitals (See Table 9).
Hospitals providing care could be of a general nature providing basic
care or interventions or may be restricted to certain specialties. They could
be classified as medical, surgical, obstetrics and gynecological, paediatric,
orthopaedic, ophthalmic, etc, or a combination of them. The services could
include maternity, medical termination of pregnancy (MTP), baby care,
intensive care services (ICU), surgery, day care and other types of services.
The responses with regard to the services provided by the hospitals for
indoor admissions were open ended under the broad categories of medical,
surgical and ob/gynaecology (maternity). This gave a broad spectrum of
type of cases admitted in the hospitals. Some of the hospitals were
providing care in certain specialties such as orthopaedics. Ob/gyn were the
single largest service provided in the sample hospitals with 55 per cent of
hospitals providing the service. Il was provided exclusively by 14 percent
of the hospitals. The main services consisted of care for normal delivery,
cesarean, hysterectomy, abortion, MTP, DNC, infertility. STD, etc. The
major services being provided was medical care. The cases treated were
mostly for illness such as tuberculosis, malaria, gastroenteritis, typhoid,
diarrhea, dysentery, jaundice, asthma and various kinds of fevers such as
rheumatic fever, enteric fever, etc. Medical services were being provided
exclusively in 20 per cent of the hospitals. In 18 per cent and 8 per cent it
was being provided alongwith ob/gynaecology and surgical services
respectively. Hospitals providing exclusive surgical services comprised
16 per cent of the sample, all of them located in the EDA.
IV
Minimum Standards
In this section the findings of the study are compared in the context of
the standards developed for private hospitals having a bed strength of upto
30 beds. As mentioned earlier in the review of literature private hospitals
RJH
(New Series)
Vol II: 2/3
1996
175
in the country function without any regulation or adhering to standards.
Standards are not prescribed nor are being enforced either through
legislation, bye-laws or professional organizations/associations.
One of the major objectives of the study was to evolve standards
for the smaller private hospitals functioning in small towns and rural
areas. A medical doctor, well-aquainted with hospital administration
was consulted to evolve standards for private hospitals having a bed
strength upto 30 beds. A document on the physical standards for private
hospital was prepared. This was based on existing material, visits to
private hospitals, discussion with owners of hospitals and other doctors.
These standards covered minimum requirements for running a hospital
in terms of services offered, space, humanpower, facilities available
with regard to equipment and instruments. They were evolved keeping
in mind both scientific principles as well as patients’ minimum comfort.
For the smooth functioning of the hospital certain basic requirements
arc needed. The environment and infrastructure related factors are mainly
those connected with the physical structures of the unit, its location, size,
condition, etc. It also includes communication facilities such as phone,
ambulance for the transport of patients, continuous power and water
supply etc.. The facility related factors are operation theatre, labour room,
sterilisation room, equipment and instruments. In this section the findings
have been presented under the following broad heads : Functional
programme; humanpower available; facilities available and space re
quirements and equipment and instruments.
Functional Programme
As per the physical standards would for hospitals certain basic facili
ties need to be provided by the hospitals irrespective of the services being
provided.
Emergency Care: The standards clearly mention that every hospital
should be in a position to provide first aid to stabilize a victim's condition
for transportation to a higher or appropriate service in case of emergency.
The hospitals should provide emergency services for cases such as road,
minor, domestic accidents and those involving medico legal victims. In
the field based study we found that private hospitals were unwilling to
treat emergency cases and those involving accident cases. Only 2 per cent
of the hospitals were treating emergency cases. In 14 per cent hospitals
preliminary treatment was given and the cases were referred elsewhere.
In 33 per cent hospitals the cases were not admitted at all but referred
directly. In the EBA majority of the hospitals do not admit the patients.
With regard to accidents cases majority of them treat only accidents
which are of a minor nature. They do not admit cases involving road and
domestic accidents. The doctors like to play it safe and not get involved
176
RJH
(New Series)
Vol 11:2/3
1996
in medico legal cases. This is in clear violation of the ethics of the doctors
and amounts to negligence on the part of the doctor. They do not want to
even provide first aid and refer the patient to bigger institution. Most of
them complain that it is because of the various formalities and procedures
involved.
Pathology: There should be provisions in hospitals or nearby location
for minimum pathological tests to be performed on site or at a nearby
facility. Of all hospitals only 18 per cent had facilities for pathological
examination. These were mainly located in the EDA and they did routine
tests such as blood, urine and stools. Most of the hospitals were referring
the patients to the private laboratories in the same village or town. In
another district we found that persons from the laboratory would come
and collect the samples from the hospital and bring back the results. This
practice was not found in Satara district [FRCH 1993]. Hospitals located
in the rural areas of EBA were referring them to laboratories located in
another village or town.
During data collection we found that many of the pathology laborato
ries functioning in small towns or bigger villages had unqualified persons
to conduct the tests. Many of them conducting the tests were not qualified
to carry out the tests recommended. In rural areas it would be quite
appropriate for the hospital to have facilities for conducting certain basic
tests, otherwise proper treatment in such cases could be delayed. It would
also save the patient unnecessary transport to an urban areas. The referrals
for examination mainly for diagnostic tests has had an unhealthy nexus.
There is a system of cut system operating. In Bombay, Pune, Nasik the
laboratory/ diagnostic centre gives a cut of the charges to the doctor
referring the patient. We were not able to collect information on this
aspect in our study as the data was not forthcoming. In Karad informal
discussions with the doctors revealed that sonography was being con
ducted rampantly. At one end in rural areas there are no facilities to
conduct simple tests in the hospitals and at the other end we find
unnecessary investigations and examinations being conducted more out
of economic reasons.
Blood transfusion facilities should be available within half to one
hour for hospitals providing maternity and surgical services. None of
the hospitals had facilities of a blood bank. Blood banks were located
in Karad and Satara towns of the district. In Karad it was available in
the private teaching hospital and the cottage hospital run by the zilla
parishad. Majority of the hospitals informed the patient to make their
own arrangement in procuring blood for either surgery or transfu
sion. This is major problem which the patients face as in case of a
planned surgery or transfusion the patient has to run around to procure
blood. In case of emergency the problem is worse especially in the
rural areas.
RJH
(New Series)
Vol 11: 2/3
1996
177
Power Supply: For the running of a hospital the availability of power
supply is of utmost importance. Those of non availability of continuos
power supply a generator should be available. With regard to continuous
power supply it was found that only in a quarter of the hospitals power
was available without any interruption. Only 24 per cent of the hospitals
in the sample had of a generator. The non-availability of continuous
power supply to the hospital is of concern as in certain situations it
could mean life and death for a patient. The patient is put to a grave risk
if power fails.
Water: the majority of the hospitals were getting water which was
supplied by the municipal/grampanchayat authority and were having
storage facility either underground or in an overhead tank.
Communication: Three fourths of all hospitals had facilities of a
telephone but in the EBA only 50 per cent of them did so. A quarter of the
hospitals in the sample were depending on a care-off number which was
either in a nearby shop or situated close to the hospital. Hospitals which
did not have the facility of a telephone were mainly located in the rural
areas of the EBA. The non-availability of a telephone for the functioning
of hospitals is of serious concern as in case of_an emergency the
communication between the doctor and the supportive services and with
patients is not present.
None of the hospitals had an ambulance available. Many of the doctors
expressed surprise at this question as it was assumed by them that
transportation of the patients was their own responsibility. It should be the
responsibility of the hospital to provide proper transportation facilities
to the patients especially when they are referred by the hospitals. In the
EBA most of the patients were transported in a passenger jeep for those
who could afford. It became more difficult for patients from rural areas
and in case of emergencies. In the EDA, private ambulances were
available. It is possible for some of the smaller hospitals to come together
and have one which could be used by all of them. This would be more
beneficial in the rural areas due to the transportation facilities being poor.
Communication and transport facilities should be a prerequisite for the
functioning of a hospital as the time for providing any intervention is
often critical.
Firefighting: Fire fighting equipment was available only in 22 percent
of the hospitals, all of them were located in the EDA.
Humanpower
As seen earlierthe availability of staff for the running of hospitals was
grossly inadequate, and of those available majority of them were not
qualified. Here we examine the availability of humanpower especially
doctors and nurses in relation to the standards laid down.
178
RJH
(New Series)
Vol 11:2/3
1996
Doctors: The standards laid down were that there should be one duty
medical officer available for every 20 indoor beds or part thereof in every
eight hour shift. In hospitals where the qualified owner doctor is resident
the requirement could be scaled down.
As noted earlier 39 per cent hospitals were functioning without either
a full-time doctor or a visiting consultant for the care of the patients.
Assuming that the owner-doctor is resident, it is not possible for him/her
to work for 24 hours. The situation could become dangerous when the
doctor goes out of the hospital even for a short while. A qualified doctor
is a must for proper care to be provided to the patient. Out of the 19
hospitals which were run by the doctor-owner alone, 29 per cent of the
hospitals were being run by doctors trained in other systems and in 10 per
cent they were operating alone. Out of a total of 14 hospitals who had a
doctor-owner qualified in other system, two of them were providing
services in ob/gyn and medical services, three hospitals in medical care,
and one surgical services. It was surprising to note that one of the doctors
was providing care in surgical services. The practice of doctors trained in
other systems of medicine providing care in Allopathy system of medi
cine needs to be banned.
Such a situation has arisen because there arc no regulations for the
functioning of private hospitals in the country. Anybody can open a
hospital and start practicing and providing care even if they arc not
qualified to do so. With regard to the doctors who were only had a MBBS
it was found that three of them were providing care for all types of services
and two were providing even ob/gyn. Out of the 24 specialists six of them
were providing care in Medical services, four for all types of care and
three each for only ob/gyn and ob/gyn alongwith medical care. There
were 46 qualified allopaths totally available on afull time basis who were
either employed or running the hospitals themselves. If we exclude the
owner-doctors of the 19 hospitals functioning without any full-time
doctor we find that only 27 doctors were available on a full time basis for
the rest of the 30 hospitals. This practically means that full-time doctors
were not available on a shift basis.
This clearly brings out the fact that the hospitals are not willing to
employ full-time qualified doctors to run them. The hospitals were being
run on a purely individual basis by the doctors with some additional help
from other persons trained by them. This has come about due to the fact
that there is no accountability and monitoring system. It is also because
the practice of medicine had become commercialised with fast returns by
not employing qualified staff. Visiting consultants were not taken for
analysis as many of them were visiting more than one hospital.
Nurses: The standards specify that there should be one nurse available
for every seven beds for every eight hour shift. For hospitals offering
maternity facilities and emergency surgical facilities two more operation
RJH
(New Series)
Vol II: 2/3
1996
179
theater nurses are required on shifts. In the study the availability of
qualified nurses it was found to be grossly inadequate. Only two hospitals
had three qualified nurses between them. There were 14 hospitals who did
not have either qualified or unqualified nurses. Comparing them with the
recommendations of nurses to be available in shifts, even taking into
consideration unqualified one the availability was only two nurses per
hospital.
Facilities and Space
A hospital should have certain basic facilities in terms of various
zones for the provision of treatment. These are the waiting room,
dispensary/pharmacy counter, toilets, bathrooms, consulting room, wards
among others. Those providing surgical services and maternity services
should have a operation theatre, labour room, sterlisation room, changing
room etc..
Location and Premise: In the study it was found that 82 per cent of the
hospitals were located near a market place and in 66 per cent of them were
functioning from an independent building. The noise level in 55 per cent
of them was disturbing. The location and premise of the hospitals play a
very vital role in the recuperation of the patient. The location of the
hospitals near a market place is due to the fact that the hospitals would like
to attract patients and be known. Hospitals in a residential complex pose
a number of problems for the residents living in the locality. For instance,
the garbage is dumped in the common dumping ground, which could lead
to spread of infections. Also the residential premises are not suitable for
hospitals as the purpose for a dwelling place is much different from that
providing indoor care, with its wards, OT, etc. The study in Bombay
found that 62.50 per cent of the private hospitals were located in
residential premises, and 12.50 per cent were run from sheds which had
roofs of asbestos, tin. etc. and only 8.33 per cent had an independent
building of their own. The study further found that 50 per cent of the
hospitals were located in poorly maintained buildings or were in a
dilapidated condition. In Bombay the development rules clearly state that
hospital should have a separate entrance as it would not disturb other
residents of the building.
Pharmacy/dispensary: Usually in private hospitals it is generally
found that in the waiting room premises a place is there for the dispensing
of the drugs. In 27 per cent of the hospitals there was a place for a
dispensary but the space provided was inadequate for all the hospitals.
Waiting Room: The waiting and consultancy room are the first entry
points of a patient visiting the hospital. Certain basic facilities need to be
provided for the comfort of a patient during his waiting. The environment
of the waiting room should be such that it is pleasing and not congested.
180.
RJH
(New Series)
Vol 11:2/3
1996
Various types of information need to be provided. The doctor’s qualifi
cation, registration in the council and schedule of fees should be displaye'd
in the waiting room prominently. There should be a proper system of entry
to the doctors chambers. Enough space should be provided for the patients
and their relatives to sit in the waiting room. The environment in the
waiting room was reasonable in 82 per cent of the hospitals.
Consultancy Room: The majority of the hospitals in the sample had
facilities of a consulting room. Only in 28 per cent of the hospitals the area
was found to be adequate. The consulting room needs to have certain
basic equipment and instruments, fixtures for diagnosis of the patient’s
illness or complaints. It was found that 92 per cent of those who had a
consulting room an examination table was present and of those 71 per cent
of them had a bedding on the examination table. Further it was revealed
that in 47 per cent of the consulting room did not have a stool and only 8
per cent had a revolving stool. The privacy of the patient is of utmost
importance, especially for women. There was neither a screen, curtain or
a separate room for examination of patients in 65 per cent of the hospitals.
The privacy of patients was not given adequate importance. It is impera
tive that there is a wash basin and with sufficient water as the doctors
examine different types of patients. A wash basin with tap was available
in 59 per cent of the hospitals, and out of these 49 per cent there was no
water available in the wash basin.
Wards: The major standards recommended were that wards should
be separate for male and female patients, infectious and non-infectious
diseases. There should be a minimum of 70 sq ft per bed with a minimum
distance of 2.2 sq ft between centres of two beds. The findings with
regard to the wards was conducted of the general ward. This was done
since the observation of a special room would provide a different picture
all together. It was generally found that the walls in the wards were bad,
there was sufficient light, ventilation was not proper, distance between
beds not sufficient, width of the door less than 3 ft, etc.. Three fourths not
having a screen and of those having a screen it being dirty in nearly most
of the hospitals. Surprisingly in 71 per cent the bed pans were not
available.
Beds: The conditions of the beds were observed. It was found that in
only 6 per cent of the hospitals the space per bed was adequate. It was
generally noticed that private hospitals as far as possible try to make the
maximum utilisisation of the space available. This is done usually at the
cost of patient comfort. The space between beds is kept as little as possible
so that more number of beds could be put. In 57 per cent of the hospitals
the distance between two beds was less than 3 ft. This has other conse
quence such as the spread of various infectious diseases within the
hospital. In more than 50 per cent of the hospitals the bedsheets and
pillows were found to be dirty.
RJH
(New Series)
Vol II: 2/3
1996
181
Operation Theater (OT)/Labour Room: Hospitals providing surgical
services should have a facility of an operation theatre. The standards
evolved do not differentiate between a minor and Major OT. Out of 49
hospitals 36 were having facilities of an OT. There were totally 23
hospitals providing care in surgical services cither exclusively or in
addition with ob/gyn and medical services. All of them had OT facilities
except one hospital which was providing services for surgical and
medical care.
There were 27 hospitals providing care in ob/gyn services, seven
exclusively, others in addition to medical and surgical services. One
hospital neither had an OT or a labour room. In 13 hospitals there were no
facilities for a labour room, the OT was used as a labour room. In four
hospitals facilities were present of only for a labour room. All the four
hospitals were providing services in addition with medical services.
Though most of them had facilities of an OT the area was found to be
adequate in only 11 per cent of the hospitals of those who had an OT. The
minimum requirement of space for the provision of an OT was 350 sq.ft.
The conditions of the OT and labour room were very bad. OT table was
present in only 71 percent of the hospitals having OT facilities. Shadowless
lamp was present in only 39 percent of them. Lithotomy was present in
37 per cent of the hospitals. In 64 per cent of them the wall were dirty and
in 49 per cent the ceiling was leaking and paint peeling off. The equipment
was kept in an unorganised manner in 57 per cent of the OTs.
Equipment and Instruments: Standards evolved have dealt with equip
ment and instruments in great detail inclusive of minor and major
instruments and their number. The standards have recommended that a
portable ECG facilities should be available in all hospitals round the
clock. In hospitals providing surgical facilities X-ray facilities should be
available. For the purpose of analysis of availability of equipment and
instruments, not all of them were analysied. It was generally found that
a ECG monitor which is a must for all hospitals, only 10 per cent of them
had the facility. A steriliser was available in 65 per cent of the hospitals.
The findings reveal that basic instruments and equipment was available
in more that 50 percent of the hospitals.
In hospitals providing OB/Gyn sendees nearly a quarter of them did
not have equipment and instruments which was a basic requirement. A
oxygen cylinder was available in 52 per cent, labour table in 74 per cent
and a suction machine in 81 per cent of the hospitals. With regard to
hospitals providing surgical services only 39 per cent had a X-ray
machine. Oxygen cylinder was available in 56 per cent of the hospitals.
A Electro cautrey unit was available in 39 per cent of the hospitals. None
of them had a Boyles apparatus.
The availability of equipment and instrument is of vital concern. They
should be available in sufficient numbers and be in a working condition.
182
RJH
(New Series)
Vol 11:2/3
1996
They should be well maintained. In the study we found in some hospitals
that they were kept in an unorganised manner. Basic cleanliness was not
maintained with regard to the equipment and instruments. Except for a
few hospitals who were storing them in a cupboard with glass doors, most
of them were leaving it open. In some hospitals there was more than
sufficient number of smaller instruments such as needles, thermometer,
dressing material, kidney trays, scalpel sets. In fact the respondent would
laugh at the investigators for asking such things but at the other end there
were hospitals which were not even these in sufficient quantity.
The private health sector has grown to be the most dominant one in the
health sector. This sector’s growth has been unregulated, unplanned and
is not accountable. This has taken place been the state did not regulate,
monitor to make the private health sector accountable. Surprisingly, the
functioning of this sector has been the least examined. There are no
minimum standards laid down for the functioning of private hospitals in
the country. Even where regulation exists in paper it is not being
implemented. In the US where the market forces play a dominant role,
there are stringent regulations for setting up private practice and hospi
tals.
Action needs to be taken to bring about reforms in this sector. The
suggestions made are not exhaustive, but touch upon some areas which
need to looked at in the prevailing situation. As a first step people should
be made aware of their rights and duties vis vi the health care system. With
regard to private practitioners, the state and medical councils should
ensure that only properly qualified persons practice. The government
should endeavor through licensing and encouragement the proper geo
graphical distribution of practitioners and hospitals in the country to
prevent over-concentration in certain areas. There should be regular
medical and prescription audits. The renewal of license and registration
should be dependent on it. Records should be maintained properly and the
patients should have access as a matter of right. Minimum standards and
requirement for various types and kinds of hospitals and nursing homes
should be laid down and be made legally binding.
References
Baru R (1993): ‘Inter-Regional Variations in Health Services in Andhra Pradesh’,
Economic and Political Weekly, May.
Bhore J (1946): Report of the Health Survey and Development Committee, 4
Vols., GOI, New Delhi.
Brooks T (1990): Standards and Accreditation : Quality Assurance Program,
Kings Fund Centre for Health Service Development, Hospital Management
International Hospital Federation, Sterling Publications. Bruce J (1990):
‘Fundamental Elements of the Quality of Care: A Simple Framework,
Studies’ in Family Planning, Vol 21, No 2, March-April.
RJH
(New Series)
Vol II: 2/3
1996
183
Operation Theater (OT)/Labour Room: Hospitals providing surgical
services should have a facility of an operation theatre. The standards
evolved do not differentiate between a minor and Major OT. Out of 49
hospitals 36 were having facilities of an OT. There were totally 23
hospitals providing care in surgical services either exclusively or in
addition with ob/gyn and medical services. All of them had OT facilities
except one hospital which was providing services for surgical and
medical care.
There were 27 hospitals providing care in ob/gyn services, seven
exclusively, others in addition to medical and surgical services. One
hospital neither had an OT or a labour room. In 13 hospitals there were no
facilities for a labour room, the OT was used as a labour room. In four
hospitals facilities were present of only for a labour room. All the four
hospitals were providing services in addition with medical services.
Though most of them had facilities of an OT the area was found to be
adequate in only 11 per cent of the hospitals of those who had an OT. The
minimum requirement of space for the provision of an OT was 350 sq.ft.
The conditions of the OT and labour room were very bad. OT table was
present in only 71 percent of the hospitals having OT facilities. Shadowless
lamp was present in only 39 per cent of them. Lithotomy was present in
37 per cent of the hospitals. In 64 per cent of them the wall were dirty and
in 49 percent theceiling was leaking and paint peeling off. The equipment
was kept in an unorganised manner in 57 per cent of the OTs.
Equipment and Instruments: Standards evolved have dealt with equip
ment and instruments in great detail inclusive of minor and major
instruments and their number. The standards have recommended that a
portable ECG facilities should be available in all hospitals round the
clock. In hospitals providing surgical facilities X-ray facilities should be
available. For the purpose of analysis of availability of equipment and
instruments, not all of them were analysied. It was generally found that
a ECG monitor which is a must for all hospitals, only 10 per cent of them
had the facility. A steriliser was available in 65 per cent of the hospitals.
The findings reveal that basic instruments and equipment was available
in more that 50 percent of the hospitals.
In hospitals providing OB/Gyn services nearly a quarter of them did
not have equipment and instruments which was a basic requirement. A
oxygen cylinder was available in 52 per cent, labour table in 74 per cent
and a suction machine in 81 per cent of the hospitals. With regard to
hospitals providing surgical services only 39 per cent had a X-ray
machine. Oxygen cylinder was available in 56 per cent of the hospitals.
A Electro cautrey unit was available in 39 per cent of the hospitals. None
of them had a Boyles apparatus.
The availability of equipment and instrument is of vital concern. They
should be available in sufficient numbers and be in a working condition.
182
RJH
(New Series)
Vol II: 2/3
1996
They should be well maintained. In the study we found in some hospitals
that they were kept in an unorganised manner. Basic cleanliness was not
maintained with regard to the equipment and instruments. Except for a
few hospitals who were storing them in a cupboard with glass doors, most
of them were leaving it open. In some hospitals there was more than
sufficient number of smaller instruments such as needles, thermometer,
dressing material, kidney trays, scalpel sets. In fact the respondent would
laugh at the investigators for asking such things but at the other end there
were hospitals which were not even these in sufficient quantity.
The private health sector has grown to be the most dominant one in the
health sector. This sector’s growth has been unregulated, unplanned and
is not accountable. This has taken place been the state did not regulate,
monitor to make the private health sector accountable. Surprisingly, the
functioning of this sector has been the least examined. There arc no
minimum standards laid down for the functioning of private hospitals in
the country. Even where regulation exists in paper it is not being
implemented. In the US where the market forces play a dominant role,
there are stringent regulations for setting up private practice and hospi
tals.
Action needs to be taken to bring about reforms in this sector. The
suggestions made are not exhaustive, but touch upon some areas which
need to looked at in the prevailing situation. As a first step people should
be made aware of their rights and duties vis vi the health care system. With
regard to private practitioners, the state and medical councils should
ensure that only properly qualified persons practice. The government
should endeavor through licensing and encouragement the proper geo
graphical distribution of practitioners and hospitals in the country to
prevent over-concentration in certain areas. There should be regular
medical and prescription audits. The renewal of license and registration
should be dependent on it. Records should be maintained properly and the
patients should have access as a matter of right. Minimum standards and
requirement for various types and kinds of hospitals and nursing homes
should be laid down and be made legally binding.
References
Baru R (1993): ‘Inter-Regional Variationsin Health Services in Andhra Pradesh’,
Economic and Political Weekly, May.
Bhore J (1946): Report of the Health Survey and Development Committee, 4
Vols., GOI, New Delhi.
Brooks T (1990): Standards and Accreditation : Quality Assurance Program,
Kings Fund Centre for Health Service Development, Hospital Management
International Hospital Federation, Sterling Publications. Bruce J (1990):
‘Fundamental Elements of the Quality of Care: A Simple Framework,
Studies’ in Family Planning, Vol 21, No 2, March-April.
RJH
(New Series)
Vol II: 2/3
1996
183
Bureau Of Indian Standards (1992): Quality Systems-Vocabulary, Indian Stan
dards Institution. New Delhi. Third Reprint April.
Crawford, DG (1914): A History' of the IMS 1600-1913. Vol II, W Thacker and
Co, Calcutta.
Donabedian, A (1988): ‘The Quality of Care: How Can it be Assessed?’ Journal
of the American Medical Association 260 (12) 1743-1748.
Duggal R (1990): *A Review of the Bhore Committee, 1946 and Its Relevance’,
.FRCH Newsletter IV 1-2, January-April 1990.
Duggal, R. S Amin (1989): ‘Cost of Health Care, Survey of an Indian District’,
FRCH, Bombay 1989.
Duggal R, S Nandraj (1991): ‘Regulating the Private Health Sector’, Medico
Friend Circle Bulletin No 173-174, July/August.
Fooks C and M Rachlis (1990): ‘Assessing Concepts of Quality of Care: Results
of a National Survey of Five Self Regulating Health Professions in Canada’,
CHEPA working paper series, Mcmaster University, Canada 90-7 May.
FRCH (1993): ‘Health Sector Resources. Investment and Expenditure in a
District’. FRCH, Pune, Draft Report, 1993.
George A and S Nandraj (1993): ‘State of Health Care in Maharashtra’,
Economic and Political Weekly, Bombay. Vol XXVIII Nos 32 and 33,
August 7-14.
George, A, I Shah, S Nandraj (1993): ‘A Study of Household Health Expenditure
in Madhya Pradesh’, FRCH, Draft Report, 1993.
Indian Council of Medical Research (1991): Evaluation of Quality of Family
Welfare Services of Primary Health Centre Level, New Delhi.
Jaggi O (1979): Western Medicine in India, Vol XIV, Alma Ram, New Delhi.
Kannan, K P, K R Thankappan. V Raman Kutty and K P Aravindan K P (1991):
Health and Development in Rural Kerala, KSSP, Thiruvananthapuram.
Khan, M E and A K Tamang (1987): Quality of Health Services in Rural India,
A Comparative Study of Three States, ORG, 1987.
Lewis C E (1984): ‘Hospital Accreditation in New Zealand’, Hospital 68, 8, pp
15-17 quoted in Tessa Brooks, Standards and Accreditation : Quality Assur
ance Program, Kings Fund Centre for Health Service Development, Hospital
Management International Hospital Federation, Sterling Publications, Lon
don, pp 130-133, 1990.
Mahapatra P, P Berman (1992): ‘Evaluating Public Hospital Performance:
Service mix Ratios of Secondary Level Hospitals in Andhra Pradesh’
Hyderabad, 1992.
Mahapatra P, P Berman ‘Evaluating Public Hospital Performance: Combined
Utilization and Productivity’, Hyderabad, 1990
Medico Friend Circle (1990): ‘Patient Provider Interface: A Public Survey’.
Mensch B (1990): ‘Quality of Care: A Neglected Dimension’, Studies in Family
Planning, Vol 21, No 2 61-91.
Sunil Nandraj
CEHAT
S S Nagar
Andheri (W), Mumbai
184
RJH
(New Series)
Vol 11:2/3
1996
Communications
Medicalising Mild Hypertension
Who Benefits?
Today hypertension has emerged as the most ferequent reason
for visits to physicians as well as the leading indication for pre
scribing drugs. Could it be this redefinition of ‘mild hypertension ’
and the medicalisation of its treatment is driven less by science
and more by the deeper structural interests of professional power
in alliance with the pharmaceutical industry?
TWO trends emerging in parallel mark the therapeutic advance of
anti-hypertensive thcrapy:(l) a progressive lowering of the cut-off
level at which the blood pressure gets labelled hypertension in need
of drug treatment (from diastolic pressure of 105 mm Hg in 1977
through 95 mm Hg in 1985 down to the present day level of 90 mm
HG. with 84-89 mm HG regarded as high normal), and (2) a pro
liferating diversity of ever ‘newer’ drugs, each claiming therapeutic
ascendancy over its predecessor, inundating each of the five classes
of anti-hypertensive drugs. The two together account for the fact
that today hypertension has emerged as the most frequent reason for
visits to physicians as well as the leading indication for prescribing
drugs.
To what reality do these trends refer? Could it be that this
redefinition of ‘mild hypertension ‘ and then medicalisation of its
treatment is driven less by science and more by the deeprer structural
interests of : professional power in alliance iwth the pharmaceutical
industry? Not that IU intend to proose a commercial conspiracy
underpinning the trend but only suggest that the shifts in the content
and the boundaries of the medical course on hypertension while
facilitating the posing of certain problems and issues also masks and
excludes many others from its confines. It is to the questions not
raised and the issues masked that I wish to turn. Why is it that even
after a decade of accumuulating evidence seriously questioning the
rationale of drug treatement for mild hypertension [Cutler et al 1989]
(defined as diastolic BP between 9 and 104 mm Hg) more than 70 per
cent of physicians continue to institute drugs as the first line of therapy
for le-veels of diastlic BP between 90 and 100 mm HG and in the US
as many as 20 per cent doctors even treat patients with diastolic BP
RJH
(New Series)
Vol ll: 2/3
1996
185
below 90 mm HG [Veterans Administration 1970]. Why is it that
instead of framing a new research paradigm questioning the value of
treating ’mild hypertension' at all, the profession continues to invest
all its resources on the need to develop ever newer drugs? Is it through
mere coincidence that even as the tightness of BP control has been
absolutised intoa therapeutic end in itself, the far more vital
epidemiologic goal viz, modification of the cardiovascular risk factor
profile, as a whole, of which hypertension is but one component
(others being: life style modification, diet, obesity, alcohol, smoking)
been relegated to the sidelines?
While the issue of ‘quality of life under medication' has been com
manding research priorities, the very real possibility of drug withdrawal
after a period of control and the efficacy of non-drug therapies (exercise,
diet and relaxation) are glossed over. All these questions arise. The claim
to improved quality of life with newer drugs even though valid at one
level, when set up against the larger epidemiologic backdrop also takes
on the features of an ‘ideology’ that seems to expost-facto rationalise the
interests of the dominant ‘medical-industrial complex’.
One way it does so is by progressively lowering and fusing the
threshold of diagnosis for ‘mild hypertension’ with the threshold of
initialing drugs and thus transforming the earlier problematic focused
on the clinical question of ‘to treat or not to treat’ into the straight
jaccket of ‘screen, detect and shoot with drugs anything higher than
diastolic 90 mm Hg’. What could be the structural origins of such an
ideology? I begin by tracing the origins of the professional discourse.
What does it begin?
Sometime in the mid-50s when anti-hypertensive drugs were just
being discovered and as Kawachi and Wilson have shown the efficacy of
the new found drugs was so convincing in reversing severe forms of
hypertension (diastolic BP exceeding 130 mm Hg), it was thought
unnecessary to conduct randomised trials. The success of a new therapy
in one group of hypertensives, viz, severe forms led ineluctably to its
uncritical universalisation to patients with far milder forms of hyperten
sion via a process well known to anthropology as ‘professional adoption’
and fuelled no doubt by agressive marketing. Even though randomised
clinical trials focused on ‘mild HT’ were still in progress and were beging
to cast doubt upon the need to treat it, by 1980s drug treatment for diastol ic
BP ranging from 85 mm Hg to 100 mm Hg had already been elevated to
the status of a ‘standard procedure’. Thus we can see how the emerging
‘critical thinking’ and ‘doubt’ over the need to treat mildren forms were
erased and professional consciousness socialised into the narrow con
fines of equating mild HT with drug treatment. This ongoing reification
of raised blood pressure into a ‘disease’ and its progressive abstraction
from the curve of normal distribution of blood pressure in a population
186
RJH
(New Series)
Vol II: 2/3
1996
(which is continuous and unimodal) led to leh creation of what George
Pickering in his textbook has called ‘the arbitrary dichotomisation of
normal BP and hypertension’. Such an abstraction gave bilh to the widely
prevalent professional proclivity to the conceptualise hypertension as if
at some fixed point in the continuous normal distribution curve of blood
pressure, the abrormal level abruptly separates off and the risk of
cardiovascular disease abruptly shoots up. Quite the contrary, the rela
tionship between blood pressure and the risk of complications in curvilin
ear. Under the gaze of this discourse, the very radical agenda of Framingham
Report got diverted from the emerging conception that views hyperten
sion not as a disease, but as one of the several markers of cardiovascular
risk for which drug treatment is just one of the several more important
non-drug therapies into a commodified ‘disease’ of hypertension in need
of drugs.
Without commercial advocacy the non-drug therapies have been
unable to compete with the agressively funded pro-drug compaigns.
Moreover, physicians having been accullurated as part of our medical
training rites of passage, lend to value the immediate over the long term
and certainly over ambiguity and thus instinctively favour immediate
‘action’ with drugs over the invisible and slower non-drug therapies.
However, all this did not go unchallenged. The year 1985 marked a radical
shift in our understanding of ‘mild HT’. That year the MRC trial, the
single largest randomised trial on treating mild HT destroyed the myth of
mild HT in need of agressive medical treatment. Il found no overall
difference in total mortality or coronary disease incidence between
placebo and active treatment groups of ‘mild hypertensives’. These MRC
results signalled a very radical restructuring of the professional discourse
on mild HT involving a shift from the curative to the preventive, from
drug to non-drug therapies and from a diagnosis based on a single raised
reading to one based on multiple high readings (in order to avoid the
wrong labelling of a common phenomenon of transiel and volatile
hypertension that need only be observed). While all this mass of new
information should have catalysed new thinking, nothing really changed.
Instead an opposing view point vigorously began to deny the validity of
extrapolating from the results of a trial to formulate treatment guidelines.
The issue was again shrouded in confusion. They overlooked the histori
cal fact that the initial adoption of anti-hypertensive therapy was itself
based upon the results of earlier and far less precise trials. The new
findings were thus blocked and prevented from being transmitted into the
rationality of every day practice which continues to equate mild HT with
drug treatment. But who gains from the power to treat with drugs all
patients with mild HT?
The question brings the role of the pharmaceutical industry on to
the centre stage. Several studies have indicated that physicians pre
RJH
(New Series)
Vol JI: 2/3
J996
187
scribing behaviour is directly influenced by (he promotional activities
of drug companies, viz use of sales reps, direct mailings of literature,
the donation of free drug samples, advertisements in medical journals
and sponsorship of seminars and conferences. Besides, the practitio
ners, in the absence of any alternative source of continuing education,
often end up being passive receptors of promotional messages. One of
the major strategy in the industry’s response to the attempted
rationalisation of treatment of HT has been to shift the discourse
towards the issue of ‘quality of life under medication’ by subsidising
clinical trials to propagate newer drugs as means to improve the
‘quality of life under medication'. The result: a progressive displace
ment of the consumer from the participative realms of the therapeutics
and his/her being labelled into a ‘sick role’ and placed into a passive
dependent relationship vis a vis the ‘medical-industrial complex’.
The point is not against the use of drugs (they are in fact vital for severe
HT with diastolic BP exceeding 115 mm Hg and for most cases of
moderate HT at 105 to 114 mm Hg), but against the system of entrenched
vested interests that prevents their more rational use, particularly for
milder forms of HT (90-140 mm Hg).
But perhaps this issue is but a small reflection of a far bigger trend of
progressive abstraction and isolation of the medical discourse from its
socio-economic context and its increasing cooperation with the pharma
ceutical industry. Counterpoint can only develop through a consumer
driven democratisation of the ‘medical-industrial complex’.
Bibliography
Cutler J A, MacMohan S W and Furberg C D (1989): Controlled clinical trials
of drug treatment for HT. A review. Hypertension 13 (Suppl I): 1-36.
Veterans Administration, ‘Cooperative Study Group on Anti-Hypertensive Agents:
Effects of Treatment or Morbidity in HT: Results in Patients with Diastolic
BP Averaging 90 Through 114mmHg’. JAMA 213:1143, 1970.
-Anil Gurtoo
Associate Professor
Department of Medicine
Jawaharlal Institute of Postgraduate Medical
Education and Research
Pondicherry-605006. India
Have you renewed your subscription to RJH2
188
RJH
(New Series)
Vol 11:2/3
1996
Discussion Paper
World Bank’s Blind Spot
Revised National Tuberculosis Control Programme
Debabar Banerji
The World Bank’s proposed new programmefor tuberculosis control
quite ingnores the fact that among the main reasons for the failure
of the earlier programme was the unnecessary interference from
international agencies. It also shows little perception of the relevant
contributions of indigenous research to the control strategies.
THE World Bank’s proposal for what they call the ‘Revised National
Tuberculosis Control Programme’ (RNTCP) for India is going to have
very damaging consequences for the development of health services of
the country. The Voluntary Health Association of India (VHAI) and the
Nucleus for Health Policies and Programmes have got together to
produce this document, which contains a scientific analysis of the
RNTPC to draw attention to its infirmities and to formulate an alternative
proposal for strengthening the National Tuberculosis Programme (NTP)
of India. While the RNTCP will be analysed in detail at a later stage,
it will be worthwhile here to note that the infirmities belong to three
categories. The most important among them is that the RNTCP has been
developed without paying adequate attention to the process of formu
lation of the NTP and the factors which have come in the way of its
implementation over the more than three decades since it was adopted
by the Government of India. Secondly, in considering the conceptualisation
of the RNTCP as an outcome of an interdisciplinary study, adopting
a systems approach, there are very serious flaws in project formulation
in terms of system optimisation, epidemiological and sociological
analyses, managerial and technological perspectives, coverage, epide
miological impact, repayment of the World Bank loan, replicability of
the RNTCP, and other such considerations. Thirdly, the World Bank
promoted RNTCP as a part of the sequence of what are termed as
‘international initiatves’ thrust on the country from outside at the instance
of international agencies backed by strong support from many powerful
western countries, which make substantial contributions to the budgets
of the former. Ironically, as will be demonstrated later on, it is these
international initiatives which have been proved to be the major hurdles
in the way of implementation of the NTP all these years. The RNTCP
thus appears as a not well thought out operation performed by persons
RJH
(New Series)
Vol ll: 2/3
1996
189
from the very same group who. in the first place, have been responsible
for the damage done to the NTP.
Even from this very broad mention of the RNTCP it is possible to
discern an underlying streak of dogmatism among the exponents of the
RNTCP, which has impelled them to ‘forget’ the enormous and very
substantial public health research in tuberculosis conducted within the
country and put enormous pressure on the national authoities to submit to
‘models’ developed by them outside the country. Apart from very serious
conceptual flaws, these western models are technocentric, imposed on the
people from above and make the country dependent on assistance from
outside. ‘Forgetting’ ideas developed indigenously has thus become
almost a prerequisite for taking international initiative in health fields; the
fields gets closed to scientific discussions and only those ‘natives’ whodo
not question them, or are incapable of doing so, are allowed entry into the
privileged group by the international syndicate. Soon after the poor
countries of the world had dared to make a declaration of self-reliance in
health in the Alma-Ata Declaration of 1978, the affluent countries
‘invented’ what they called Selective Primary Health Care , which was
almost immediately followed by the unleashing of a series of interna
tional initiatives in health. Significantly, there has been little protest from
the concerned community of public health scholars even in the affluent
countries to such brazen forms of manipulation of science to impose
programmes on ‘defenceless’ countries, from outside. The World Bank
backed RNTCP is a particularly unfortunate example of imposition of
such international initiatives.
The drive towards globalisation of the economy and polity has made
the poor countries even more vulnerable to manipulation by the rich
countries. In the so-called global village, the poor countries are con
demned to serve as bonded hirelings of the rich kulaks and cowboys. A
dialectical outcome of this form of international relations is for the
oppressed peoples to make conscious efforts to prevent the dominant
powers to ‘forget’ their historical heritage. To adapt a quotation from
Milan Kundera, it becomes a struggle between memory and forgetful
ness. Just as ahistoricity becomes an important weapon in the hands of
those who would fight to continue to monopolise the control over the bulk
of the resources of the world, breaking into their consciousness to
‘remind’ them about the history they try to forget becomes a weapon in
the hands of the oppressed to fight oppression.
At a time when a concerted effort is being made by World Bank
officials to promote RNTCP in this country, this document may be
considered as a modest effort to ‘remind’ them as well as the concerned
authorities in the country about the very significant work that has been
done in India to deal with tuberculosis as a public health problem. No
apologies will be offered here for consciously taking the side of the people
190
RJH
(New Series')
Vol 11:2/3
1996
by bringing out well researched data which had formed the basis of the
NTP some three and a half decades ago. A very deliberate effort is made
here to describe the work rather extensively. The ‘battle lines’ are clear:
on one side are the indigenous research efforts made to fomulate a
nationally applicable, socially acceptable and epidemiologically effec
tive tuberculosis programme, and on the otherside is a ‘foreign inspired’,
prepackaged programme that is sought to be thrust on the country by
powerful countries and international organisations.
The above account shows how a well researched and reasonably
simple and straightforward programme can get hopelessly confounded
due to the interplay of a variety of social, political and economic forces.
NTP essentially involved offering diagnosis and treatment to the very
substantial portion of tuberculosis patients who were actively seeking
treatment in various health institutions, both in rural and urban areas.
These institutions were offered a referral support system which extended
right up to the supper-specialists in post-graduate teaching hospitals.
State Tuberculosis Centres and NTI and other tuberculosis research and
teaching institutes were meant to provide support to the programme in the
form of training, monitoring, evaluation and operational research.
But as pointed out by Halfdan Mahler, “Even the simplest technology,
if it is not properly deployed and utilised by the infrastructure, just will not
move, will not control tuberculosis, will not meet people’s felt-needs.”
This is what has befallen on NTP. The infrastructure has been grievously
damaged because of sharp decline up of key public health posts by the
persons who do not have technical competence, by imposition of target
oriented specialised programmes on an already weak infrastructure and
correspondingly sharp fall in the quality of administrators and research
personnel in the field of tuberculosis.
From the basic premises presented above, some important suggestions
are being made below:
1 While tuberculosis workers cannot take on themselves the onerous
task of rejuvenating the moribund health and family planning services
system, the crisis has become so profound that there arc good chances that
the political leaders will have to wake up to it. A detailed programme for
rejuvenation of the health services is given in the author’s B C Dasgupta
Oration of the Indian Public Health Association in 1988 . Some important
components are:
(a) Building up a critical mass of public health workers in the fields
of education, training, research and practive.
(b) Restructuring the cadre structure to place competent public health
specialists in key public, health positions.
(c) Concurrent removal of the square pegs in the round holes of the
system.
(d) Making ‘conditional’ integration of the special target oriented family
RJH
(New Series)
Vol 11: 2/3
1996
191
planning and other programmes ‘unconditional’. This will lead to
according much higher substantial pan of the total suffering caused
by health problems as a whole.
2 Tuberculosis workers can help in the process of rejuvenation of the
health and family planning service systems by insisting that this
process is critical for providing good tuberculosis services.
3 On its own, even considering the constraints of the general health services
as given, there is still considerable scope for improving the NTP system
through use of operational research and systems analysis. The Surajkund
Conclave recommendations can serve as a starting point.
4 The very improvement in the NTP system might stimulate improve
ment in the wider health and family planning services systems, by
providing an example.
5 NTI can be rejuvenated by bringing together a competent interdis
ciplinary team of workers, so that it can play a role in strengthening
the NTP. It can even extend its activities to serve as one of the many
institutions which would be necessary to strengthen the general
health services.
6 Concurrently, competent tuberculosis workers are placed as heads
of tuberculosis wings of the central and state health services.
7 Other tuberculosis institutions, such as TRC, should be tuned to serve
the NTP, i e, the problem they deal with must emerge from the field
situation, and not the other way round, as is often the case at present.
8 The idea of task force or a similar set up which is vested with power
and resources to act as a watchdog for the implementation of NTP, very
well blends with the other suggestions for improving NTP given here.
9 Again, there is considerable scope for optimising the urban com
ponents of the NTP.
10 The Tuberculosis Association of India and its branches can be
revamped to perform a complementary role in strengthening of NTP.
In sum, the suggestion is that we take steps to unleash the social forces
which ensure that simple and efficacious technology developed in India
is made accessible to the hundreds of thousands of sputum positive cases,
who are actively seeking relief from suffering but who are still being
thrown out of the health institutions with a bottle of useless cough
mixture. Sociologically, it is contended that the very meeting of the felt
needs generates more needs, and, if that does not happen, active educa
tional steps are taken to generate more needs to reach a level when it starts
having an epidemiological impact. This epidemiological impact will
occur in consonance with the impact that might occur as a result of
changes in the natural history of tuberculosis in India.
-Debabar Banerji
Nucleus for Health Policies and Programmes
B 43 Panchsheel Enclave, New Delhi 110 017
192
RJH
(New Series)
Vol 11:2/3
1996
Facts and Figures
Housing and Other Amenities
The availability and quality of housing, water supply, fuel and
sanitation has a direct influence on the health status of populations.
This is increasingly evident in the spread of diseases hitherto assumed
to have been under control—many of these are waterborne and spread
rapidly in overcrowded and unhealthy living and working environ
ments.
Data on housing and other amenities was collected during the 1991
Census operations. Like the preceding censues, questions were asked
on the roofing matcrialm, wall and floor, as well as on drinking water
supply and availability of electricity.The 1991 census collected data
on availability of toilet facilities for the first lime.
We present here selected few tables from Housing and Amenities:
A Brief Analysis of the Housing Tables of 1991 Census.
The number of census houses in India has gone up by 82 per cent
since 1961, giving an increase of 85.89 million houses. There were
190.33 million houses in India in 1991. While the increase in houses
was 62 per cent in rural areas, it was 178 per cent since 1961. the
lislribution with regard to quality of houses is as in Table 1. The fact
that the proportion of pucca houses have increased should be read with
care. Il is a fact that building activity inurban areas, mainly catering
to the growing middle class has been on the increase, and this figure
may only indicate that more housing unaffordable by the poor is being
built.
A shocking fact is that only 62.72 percent of houscolds have access
to safe drinking water, notwithstanding that the proportion has almost
doubled since 1981. Equally disturbing is the fact that only 23.55 per
cent of households have reported having toilet facilities, with only
11.16 and 7.22 scheduled caste and scheduled tribe respectively
having such facilities. Some 28 per cent of SCs and 45 per cent of STs
have none of the facilities that is, electricity, safe drinking water or
toilets. These are ominous trends which will increasingly affect health
status.
!H
(New Series)
Vol 11: 2/3
1996
193
Table 1: Percentage Distribution of households living in Pucca, Semi Pucca
and Kutcha Holses. 1981-91
India/State/
Union Territory
1
India*
India**
State
Andhra Pradesh
Arunachal Pradesh
Assam
Bihar
Goa
Gujarat
Haryana
Himachal Pradesh
Jammu and Kashmir
Karnataka
Kerala
Madhya Pradesh
Maharashtra
Manipur
Meghalaya
Mizoram
Nagaland
Orissa
Punjab
Rajasthan
Sikkim
Tamil Nadu
.Tripura
Uttar Pradesh
West Bengal
Union Territory
Andman and Nicobar
Island
Chandigarh
Dadara and Nagar
Heveli
Daman and Diu
Delhi
Lakashadweep
Pondicherry
1981
2
Pucca
1991
3
32.67
32..73
Semi--pucca
1981
1991
4
5
Kutcha
1981
1991
6
7
41.61
42.30
33.29
33.24
30.95
31.36
34.04
34.03
26.22
7.48
NA
23.64
32.45
48.96
39.82
43.94
26.20
29.33
38.80
25.02
39.63
3.42
11.29
7.30
10.18
13.00
58.12
49.08
18.16
36.62
3.61
29.29
28.40
38.41
14.94
I4..62
30.18
50.70
56.93
50.14
53.03
NA
42.55
55.97
30.47
52.20
5.40
13.30
19.10
12.62
18.71
76.97
56.13
26.95
45.54
5.50
41.03
32.61
24.18
11.64
NA
40.10
57.44
42.12
35.85
45.14
40.01
44.89
20.33
66.30
40.22
18.89
26.87
22.72
21.92
18.53
16.11
25.14
35.51
18.15
8.41
35.37
26.03
22.58
11.72
15.16
36.00
44.47
39.01
35.73
40.99
NA
40.90
19 13
64.87
36.14
40.65
33.72
45.52
36.47
22.06
11.07
22.94
39.11
18.03
20.71
30.34
29.38
49.60 39.01
80.88 73.34
N A 70..22
36.26 33.82
10.11
4.82
8.92
4.06
24.33 14.13
10.92
5.99
33.79
NA
25.78 16.55
40.87 24.90
8.68
4.66
20.14 11.67
77.69 53.95
61.84 52.98
69.98 38.38
67.90 50.91
68.47 59.23
25.77 11.96
25.78 20.93
77.00 33.94
45.23 36.44
87.98 73.79
35.62 28.63
45.57 38.01
4.00
84.42
10.40
82.49
43.43
8.61
47.25
8.42
52.57
6.97
42.35
9.10
18.47
67.84
88.73
61.17
37.48
20.80
79.80
85.60
88.84
44.88
5.02
21.41
6.08
34.90
9.25
22.54
17.33
4.61
9.04
12.16
76.51
10.75
5.19
3.92
53.27
56.66
2.87
9.79
2.12
42.96
27.44
26.33
* India excludes Assam in 1981 and India excludes Jammu & Kashmir in
1991
** Excluding Assam and Jammu and Kashmir.
194
RJH
(New Series)
Vol 11:2/3
199'1
Table 2: Percentage of Households Having Safe-drinking
Water - 1981 and 1991
India/State/
I nion Territory
1
1981
2
Total
1991
3
38.19’
India
37.91
India*1
Vtate
\ndhra Pradesh
25.89
\runachal Pradesh
43.89
NA
Assam
37 64
Bihar
Goa
22.50
52.41
Gujarat
1 laryana
55.11
Himachal Pradesh
44.50
Jammu and Kashmir 40.28
Karnataka
33.87
Kerala
12.20
M.tdhya Pradesh
20.17
42.29
Maharashtra
19.54
Manipur
Meghalaya
25.11
Mizoram
4.88
Nagaland
45.63
14.58
Orissa
84.56
Punjab
27.14
Rajasthan
30.33
Sikkim
43.07
Tamil Nadu
27.33
Tripura
33.77
Uttar Pradesh
West Bengal
69.65
Union Territory
Andman and Nicobar
51.64
Island
Chandigarh
99.09
Dadara and Nagar
19.35
Hevcli
54.48
1 )aman and Diu
92.97
1 )elhi
Lakashadweep
2.19
80.59
Pondicherry
1981
4
1991
5
Urban
1991
1981
7
6
62.30"'
62.72
26.50'
26.34
55.54"
55.92
75.06' 81.38"
74.13 81.59
55.08
70.02
45.86
58.76
43.41
69.78
74.32
77.34
NA
71.68
18.89
53.41
68.49
38.72
36.16
16.21
53.37
39.07
92.74
58.96
73.19
67.42
37.18
62.24
81.98
15.12
40.16
NA
33.77
8.57
36.16
42.94
39.56
27.95
17.63
6.26
8.09
18.34
12.91
14.26
3.57
43.43
9.47
81.80
13.00
21.70
30.97
22.17
25.31
65.78
48.98
66.87
43.28
56.55
30.54
60.04
67.14
75.51
NA
67.31
12.22
45.56
54.02
33.72
26.82
12.89
55.60
35.32
92.09
50.62
70.98
64.28
30.60
56.62
80.26
63.27
87.93
NA
65.36
52.31
86.78
90.72
89.56
86.67
74.40
39.72
66.65
85.56
38.71
74.40
8.79
57.18
51.33
91.13
78.65
71.93
69.44
67.92
73.23
79.78
73.82
88.20
64.07
73.39
61.71
87.23
93.18
91.93
NA
81.38
38.68
79.45
90.50
52.10
75.42
19.88
45.47
62.83
94.24
86.51
92.95
74.17
71.12
85.78
86.23
67.87
97.73
36.35
94.39
59.43
98.11
91.95
99.39
90.91
97.68
45.57
71.42
95.78
11.90
88.75
16.85
46.42
62.26
0.97
76.88
41.17
56.87
91.01
3.41
92.86
54.35
67.04
94.91
3.65
84.18
90.97
86.76
96.24
18.79
86.05
Rural
(& Excluding Assam and Jammu and Kashmir.
* Excludes Assam.
** Excludes Jammu and Kashmir.
RJH
(New Series)
Vol ll: 2/3
1996
195
Table 3: Percentage of Scheduled Caste, Scheduled Tribe and •Others’
Households Having None of the Facilities, ie. Electricity,
Safe-Drinking Water and Toilet - 1991
India/State/
Union
Territory
1
SC
2
India’
28.06
Stale
Andhra
Pradesh
33.34
Arunachal
Pradesh
18.94
Assam
35.40
Bihar
41.53
Goa
15.59
Gujarat
11.32
Haryana
15.43
Himachal
Pradesh
7.70
Karnataka
14.90
Kerala
49.82
Madhya
Pradesh
25.14
Maharashtra 14.58
Manipur
31.55
Meghalaya
28 67
Mizoram
11.70
—
Nagaland
Orissa
49.12
Punjab
4.43
Rajasthan
34.17
Sikkim
21.87
Tamil Nadu
19.45
Tripura
15.30
Uttar Pradesh 41.88
West Bengal 15.31
Union Territory
Andman and Nicobar
Island
Chandigarh
1.24
Dadara and
Nagar Heveli 7.42
Daman and Diu 0.67
Delhi
3.40
—
Lakashadweep
Pondicherry
5.79
Total
ST Others
SC
Rural
ST Others
SC
Urban
ST Others
3
4
5
6
7
8
9
10
45.30
21.37
32.14
48 06
28 65
9 62
15.70
4.46-
44.34
23.19
37.07
46.81
29.84
11.73
18 63
5.98
15.71
56.18
65.85
34.38
40.83
-
21.67
31.30
32.66
9 22
10.67
8.90
20.68
39.46
43.52
19.69
15.39
17.93
16 63
58.02
68.54
42.31
43.93
—
28.11
35.42
36.54
12.21
16.04
12.39
13.40
9 02
21 29
10 13
4.29
3 47
2.48
15.05
32.76
31.43
11.53
4.21
4.95
10.25
4.95
2.83
0.86
9.73
19.29
69.95
4.07
14.91
32.21
8.14
17.22
54.46
10.14
21.6S
72.93
4.58
20.48
39.14
1.50
5 99
27 33
0.78
7.11
18.34
0.84
3.86
12.75
44 58
31.13
33.46
50.88
19.00
16.95
61.14
47.45
13.80
37.54
52.31
22.61
38.31
27.59
11.27
18.34
19.42
7.29
15 28
41.33
1.38
29.37
15.36
13.82
10.05
31.06
8.39
28.19
19 48
37.52
41.83
33.99
—
51.90
5.24
40.13
24.05
21.08
17.67
45.68
16.95
45.89
34.50
36.67
57.92
31.55
18.67
62.59
49.59
15.04
42.63
53.40
28.97
40.30
37.03
18 44
24.19
39.72
26.90
23.47
48 12
1.91
38.98
16.98
18.93
13.18
38.08
11.87
13 14
3.98
18.73
2 87
3 52
25.19
1.47
8.86
3.96
12.87
2.59
13.72
7.24
21.21
8.39
3.29
5.32
4.38
9.29
36.26
—
13.72
0.88
13.61
1 15
9.39
14.54
6 35
2.08
8.78
2.05
5.39
8.82
10.70
0.32
4.41
1.39
4.34
0.55
5.73
2.05
43.44
—
16.26
0.41
0.13
45.73
—
22.1 1
0.36
1.41
6.10
—
1.59
0.42
40.74
7.94
—
1.05
-
8.16
1.13
1.05
1.68
2.85
8.58
1.08
9.21
4.34
41.87
7.87
1.45
—
10.63
1.75
3.82
7.04
2.89
0.00
0.00
2.75
—
8.02
7.25
8 27
—
0 67
-
0.32
0.58
0.79
0.25
2.85
Vol! I: 2/3
1996
—
* Excludes Jammu and Kashmir.
196
RJH
(New Series)
THE INDIAN JOURNAL OF LABOUR ECONOMICS
I
D
3
0
D
D
fl
fl
fl
B
fl
D
Q
B
I
D
B
[1
B
D
[1
D
B
fl
'I'he Journal, in print since 1958, is published quarterly as the organ of the
Indian Society of Labour Economics which is a broad-based organisation in
which all schools of analysis are welcome to participate. The chief aim of the
Journal is to promote scientific studies in labour economics, trade unionism,
industrial relations and related topics. Apart from peer-reviewed articles and
research notes, the Journal publishes communications of seminars and
conferences, documentation of important Government reports/rescarch studies
concerning labour, selected labour statistics, and book reviews.
Recent articles include :
o
Employment, Labour Market Flexibility and Economic Liberalisation
in India — Amit Hhadari
o
Health, Poverty and Labour — T.N. Krishnan
O
Workforce Restructuring, Wages and Want : Recent Events, Interpretations and
Analysis — Sheila llhnlla
The Informal Sector Reconsidered — /an Urcman
Policies for Rural Labour : From Relief to Structural Change — VM. lino
o
O
O
Employment and Labour under Structural Adjustment :
India Since 1991 — /ayalhi Ghosh
Organising the Unorganised Labour : Some Issues — Abdul Aziz
Safety Nel of the National Renewal Fund : Some Basic Issues — Indira Hirway
O
O
O
Unemployment and Large-Scale Industries : A Historical Study of the Roots of
Labour Surplus in the Jute Industry — Arjan dr: Haan
O
Attack on Poverty and Deprivation : Role of Structural Change and
Structural Adjustment — CH. I lanumanlha Hao
A Note on Measurement and Use of Poverty Estimates — Yogindcr K. Alagh
fl
fl
D
0
D
D
D
D
B
B
D
D
D
D
fl
I
I
L,
o
Development and Employment — S U Hashim
o
o
o
Labour Market Flexibility and the Indian Economy — Ajil K. Chose
O
Economic Reforms and Employment in India : Projections for the Year
2001-02 — H N. Agarwal and II.N. Gaidar
Government Interventions and Social Security for Rural Labour — S’. Mahendra Dev
Annual Subscription Rates
Individual
Institutional
India
Abroad
Rs. 150
US $35
Rs. 300
US $55
Payments in the form of bank draft/
choquo may bo sent in favour of The
Indian Journal of Labour Economics.
Rs. 12./US S3 should be added extra in
tho case of outstation cheques.
All editorial and business correspondence should be made with the Editor/Managing
Editor, The Indian Journal of Labour Economics c/o Institute of Applied Manpower
Research, 1:P. Estate, Mahatma Gandhi Marg. New Delhi-110002. India.
Phone/Fax: 3319909
I
I
I
I
I
a
i
a
i
i
fl
i
i
■
a
i
D
I
I
I
I
I
fl
I
I
I
I
I
I
I
I
i
I
I
I
I
I
I
I
I
1
I put a sheet of paper on my table,
Clean, snowy white,
And at its side a pencil, black as sable,
With which I’ll write.
The one and only thing that now remains
Is to commence.
Yet wait, my hand, don’t hurry and leave stains,
Uncouth and dense.
I
i
i
Clean paper! Fire or ice - What does it hide?
Just like a baby
Sti-11 in the Womb - does joy await outside
Or sorrow, maybe?
i
1 1
j,
What can’t a pencil trace upon its space,
Led by a man’s hand There’s nothing, as the Russian proverb says,
Paper won’t stand.
((
1
Glad tidings, sense and nonsense, trite and new
Ideas men write.
Death sentences are written on it too
In black and white.
(Translated by Dorian Rottenberg
in Voice of Friends: Soviet Poets)
-Mustai Karim
(Bashkir Poet)
i
I
h
'
\
Position: 6251 (1 views)