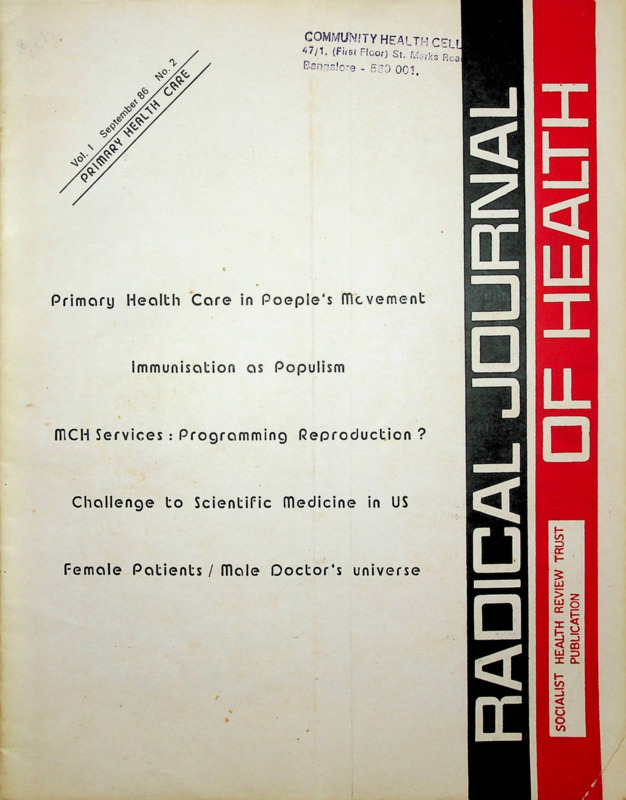
Radical Journal of Health 1986 Vol. 1, No. 2, Sep.: Primary Health Care
Item
- Title
- Radical Journal of Health 1986 Vol. 1, No. 2, Sep.: Primary Health Care
- Date
- September 1986
- Description
-
Primary health care in people’s movement
Immunisation as populism
MCH Services: programming reproduction?
Challenge to scientific medicine in US
Female patients / male doctor’s universe - extracted text
-
COMMUHfTY HEALTH CEl I
'■•7/1. (First Floor) St. Mjrks Roa
Bangalore - 530 OCI,
Primary Health Care in People's movement
immunisation as Populism
mCH Services : Programming Reproduction ?
Challenge to Scientific medicine in US
Female Patients / male Doctor's universe
Yol I
Sept 1986
No. 2
HEALTH
CARE
PRIMARY
41
Editorial Perspective
Working Editors :
Amar Jesani, Manisha Gupte,
Padma Prakash, Ravi Duggal
Editorial Collective :
Ramana Dhara, Vimal Balasubrahmanyan (AP),
Imrana
Quadeer, Sathyamala C (Delhi),
Dhruv Mankad (Karnataka), Binayak Sen,
Mira
Sadgopal
(M P),
Anant
Phadke,
Anjum Rajabali, Bharat Patankar, Jean D'Cunha,
Srilatha Batliwala (Maharashtra) Amar Singh
Azad (Punjab), Smarajit Jana and Sujit Das
(West Bengal)
Editorial Correspondence :
Radical Journal of Health
C/o 19 June Blossom Society,
60 A, Pali Road, Bandra (West)
Bombay - 400 050 India
Printed and Published by
Dr. Amar Jesani for
Socialist Health Review Trust from C-6 Balaka
Swastik Park, Chembur Bombay 400 071
POLITICS OF PRIMARY HEALTH CARE
Imrana Quadeer
43
SOCIAL DIALECTICS OF PRIMARY HEALTH
Guy Poitevin
52
IMMUNISATION AS POPULATION : A REPORT
Asha Vohuman
55
PROGRAMMING REPRODUCTION ?
MATERNAL HEALTH SERVICES
Manisha Gupte
59
THE HOLISTIC ALTERNATIVE TO SCIENTIFIC
MEDICINE: HISTORY AND ANALYSIS
Howard S Berliner and J Warren Salmon
66
UPDATE - News and Notes
Printed at :
69
Omega Printers, 316, Dr. S.P. Mukherjee Road,
Belgaum 590 001 Karnataka
FEMALE PATIENTS VERSUS
MALE DOCTORS' UNIVERSE
Jytte Willadsen
Annual Subscription
Rates
:
Rs. 30/- for individuals
Rs. 45/- for institutions
Rs. 500/- life subscription individual
US dollars 20 for the US, Europe and Japan
US dollars 15 for other countries
We have special rates for developing
countries.
SINGLE COPY : Rs. 8/(All remittances to be made out in favour of
Radical Journal of Health. Add Rs. 5/- on
outstation cheques)
73
Dialogue
ORGANISING DOCTORS: A DIFFERENCE IN
APPROACH Sujit Das
LIGHT ON BLIND SPOTS: UN Jagoo
ECT AND DRUG THERAPY: IS THERE AN
ALTERNATIVE : A R
The views expressed in the signed articles do
not necessarily reflect the views of the editors.
Editorial Perspective
Politics of Primary Health Care
SINCE the seventies, in many national and international
circuits of health bureaucracies, Primary Health Care (PHC)
has become a panacea for all the evils of the poorer nations.
The WHO has projected it with all its convictions and the
member nations have accepted, it with equal vigour.
According to the Alma Ata declaration.'
Primary Health Care is essentia! health care based on practical, scienti
fically sound and socially acceptable methods and technology made
universally accessible to individuals and families in the community
through their full participation and at a cost that the community and
country can afford to maintain at every stage of their development
in the spirit of self-reliance and self-determination. It forms an integral
part both of the country’s health system of which it is the central
function and main focus, and of the overall social and economic
development of the community.
Today when this strategy has been accepted by such a large
number of countries, there is a need to examine its potential
strengths and weaknesses.
The idea that health is closely related to people’s living
and working conditions and that it is an outcome of their
socio-economic environment was vocalised by men in
different fields like John Snow, Engels and later Virchow in
the West. It manifested itself in the sanitary movement of
the 19th century. In India and other parts of the East it had
much deeper roots, visible in the method of ancient medical
science itself and in the cultures of Harappa and Mohenjodaro. In India during the struggle for Independence, a
demand for comprehensive health care was a part of the
national movement. Why then this sudden fervour now for
projecting PHC as a new concept by international and
national official circles?
To understand the politics of PHC one has to understand
the role that UN and WHO have played in the overall politics
of the world. Always supporting the interests of the
imperialist nations, these organisations have used the liberal
tools of aid, support and providing consultancy to diffuse,
control and direct crisis situations. The effort to develop an
alternative World Economic Order in the 70s was one such
spurious exercise and as a part of it, was proposed the notion
of alternative health care for the third world.
The motives behind it were to check impending destruc
tive and costly reactions from and within third world nations
whose poverty, disease and squalor were becoming threats
to stability. PHC was the baby of the liberals in the
imperialist camp and WHO projected it as the solution to
poor nations’ health problems—with full promise of help
and support, but a clear understanding that the local political
structures alone will give shape to the implementation of
Primary Health Care! Such an international strategy which
offers free help without any political price is obviously
seeking change in health situation with or without the
political will of the local government. It is interesting that
the international terms of trade are in total contradiction to
this attitude. Even though one knows that some liberals have
their hearts in the right places, this conflict in international
strategy needs serious analysis to understand the reasons for
this special concession to health.
September 1986
At the national level the concept of PHC acquires multiple
dimensions. Given the particular hue of the government, the
implications have varied from Africa to south cast Asia and
Eastern Mediterranean regions. The issue is what use docs
a national government make of the concept? Does it use it
as the concept is presented by the Alma Ata declaration and
make it a part of its effort to develop an integrated strategy
for the betterment of its people, as in Angola, Tanzania and
Mozambique or does it allow the concept to degenerate into
a slogan behind which the same old strategies with some new
features continue to be implemented—at a faster rate perhaps
with the additional inputs from the international fund
givers—as in India and Pakistan?
A grasp on the national politics of PHC requires an.
understanding of the country’s socio-economic and political
structure and the nature of its government and health service.
structures. Only such an understanding allows one to assess
the potentialities or limitations of the system to achieve PHC.
An example of the interplay between PHC and politics is
the level at which it is integrated into the planning process
of a country. Thus, the Chinese and Vietnamese incorporated
PHC in the very process of national planning right from the
period of their independence without giving it a name. In
contrast, India made so much fuss and then relegated PHC
to the care of the health ministry while the overall planning
processes took its own directions. Yet another example is the
implementation and outcome of programmes introduced
under the banner of PHC. These programmes which may
have a potential of providing much needed services are over
taken by the local power elite through their links with the
health and administrative bureaucracies. The nature of the
latter thus becomes the primary determinant of the outcome.
The Community Health Guides scheme and the drinking
water supply through borehole hand pumps in India arc two
such examples.
Another dimension of the PHC efforts at the national level
is the setting of priorities and the selection of technology.
In India despite the official acceptance of implementing PHC
by 2000 AD, the heavy emphasis on urban-based services and
curative approach in rural areas continues with heavy
dependence on expensive equipment and drugs. The drug
policy needed to provide PHC is yet to be formulated. Can
issues of priorities and technology be then isolated from
politics? A simple but revealing example is the supply of
“electrolyte” packets in the Community Health Guides’ kits!
Does it not show links between the health administrators and
the drug industry who know that addition of so many salts
to the basic mixture only increases cost and not effectivity?
If the concept of PHC is getting distorted in the hands
of the not-so-democratic government and is becoming a4ool
for creating two types of services, one for the rich and the-'
other for the poor, should it be criticised, rejected, accepted
as an unavoidable distortion or used to broaden the base of
democratic movements? These are some of the questions
which need to be answered by those who are working in the
41
interest of people’s health. Can PHC as a concept become
an inspiration for those involved in people’s struggle for their
rights? If PHC is an outcome of total development then it
should be. And what have people’s democratic and left
movements done about it?
There are many small or regional projects experimenting
with implementation of primary health care. What is the role
of such projects in focussing upon the issue of PHC or in
diluting it?
In academic circles, in the name of professionalism and
the need to achieve results, a concept of “selective PHC”
has been circulated which means let us not talk of compre
hensive development but do what we can without disturbing
the existing balances. This is attractive to those who would
like to go back to singing praises to powers of technology
and managerial competence. There is need to examine such
concepts threadbare to show their reactionary ideology as
well as non-feasibility.
Are there any lessons that we can draw from the ex
periences of the socialist countries which have tried to
provide health care not in isolation, but as a part of their
total developmental processes? These are the major questions
which need to be addressed when one is dealing with the
bipronged weapon of Primary Health Care.
and perspective of the maternal and child health programme
and points out that without a questioning of the role of the
women in society, any such programme would be ineffective.
Asha Vohuman reports on the mass immunisation pro
gramme which was launched with such fanfare in Bombay
in 1983, not so much because of its potential impact on the
health of the children but because the minister in charge
needed a visibly successful campaign to consolidate her
political gains. The reprinted article from International
Journal of Health Services provides a historical background
of the concept of public health and raises some questions
about holistic health alternatives emerging in the US. And
in the non-theme section we have Jytte Willadsen discussing
the question of the sexist bias in medicine. As a doctor herself
she also touches upon the problems encountered in bring
ing about any changes in the very male oriented medical
establishment in Denmark.
We have as usual the Update and Dialogue sections. Sujit
Das continues the discussion on the role of doctors; Ulhas
Jajoo responds to Anant Phadke’s review of his book When
the Search Began (RJH, I: I) and AS questions if drug
therapy in psychiatric problems does not have a place in the
present socio-political context.
This issue examines some of the problems raised in the •
editorial. Guy Poitevin describes his experiences in taking
up health issues as a part of larger movement for socio
economic change. Manisha Gupte comments on the ideology
Centre for Community Health and Social Medicine
Jawaharlal Nehru University
New Mehrauli Road
New Delhi.
inirana qadeer
XIII Annual Meet of MFC
Medico Friend Circle will hold its XIII Annual Meet at Seva Mandir Training Centre, Kaya (near Udaipur),
Rajasthan, on 26lh and 27th of January 1987.
The theme chosen for discussion this time is “Family Planning in India: Theoretical Assumptions, Implementation
and Alternatives”. Family Planning has generally been considered an important part of Primary Health Care, but over
the past two decades, it has come to occupy a key place amongst the country’s development strategies. Is its elevation to
the level of a panacea, for the problems facing the people, based on well examined theoretical assumptions? What effects
has the policy of incentives and coercion had on the performance of other health programmes? Out of the existing contra
ceptive methods which is the least harmful? Do some of these methods need to be rejected outright? Are there safer alter
natives? These are some of the issues to be discussed at the Meet.
As usual there will be no reading of papers. Background papers on related topics will be circulated beforehand to facilitate
discussions. They include: (a) Problem of population versus resources (b) Theoretical assumption of FP policy in China
(c) Critical examination of the FP policy in the context of the child survival hypothesis (d) Comparative analysis of the
dangers of pregnancy and contraception (e) Women as the main targets of FP policy (f) The paradox of higher FP perfor
mance in tribal areas (g) Incentives and coercions—effects on Primary Health Care (h) Pattern of resource allocation in
bur Five Year Plans (i) Evaluation of the existing FP methods 0) Natural Family Planning methods as safer alternatives.
We invite you to attend the Meet and share your views and experiences. We also invite you to write background papers
on any other topic to the theme. Your note/paper should reach the Convenor’s office by the 31st November.
Participants are as usual expected to pay for their own travel. Simple boarding and lodging facilities will be available
at the venue, on a payment of Rs. 20/- per day per person. We charge a small registration fee to cover the cost of the
cyclostyled background papers. Return reservation facilities are also available. If you wish to attend, please write to:
Dhruv Mankad, Convenor, Medico friend Circle, 1877, Joshi Galli, Nipani-591 237. We will then send you the venue
details and background papers.
42
Radical Journal of Health
Social Dialectics of Primary Health
guy poitevin
This article presents some socio-psychological observations and conclusions drawn from a social study made
of a limited voluntary health programme undertaken by a sinall NGO in remote rural areas of Maharashtra (Sahyadri
Range). This qualitative study is concerned with health as a social process. Health practices are examined as
components of over-all socio-cultural dynamics and the foundations of a people's health movement sought within
the context of a wider attempt of socio-political awakening and people's organisation.
SEVERAL voices raise to draw our attention on primary health status, the planning of alternative or integrated health
health issues as components of local socio-cultural dynamics. 'services among deprived rural population and the related
This perception prevails, for instances, as a conclusion of welfare, educational or developmental issues, in a more or
the assessment of the working of the Rural Health Scheme less static way. Health is examined here as a social process
made by the Population Research Centre of the Institute of from within a marginalised population, v/z., as a dimension
Economic Growth: “His (Community Health Volunteer, of an overall dynamics of socio-cultural and socio-political
CHV) role as a public health worker is more social than awakening and people’s organisation. The study is concerned
medical. It would require of him to create health con with the conditions of a possibility-of an effort of health
sciousness within the community and to prepare and organise by the people which actually cares for all, bas^d on a critical
the community effort to carry out all the necessary steps of appraisal by those concerned -i e those deprived of health
improving sanitation within the settlement, cleansing up the care facilities—of the present health system and motivated
surrounding areas and imparting health education to all its by a will to try out self-reliant ways. This case study is partial
members. This work within the community is in fact the contribution towards answering some of the following ques
fundation upon which the whole health care delivery system tions: the need for a strategy for enlisting community par
must rest” (Bose A, 1983: 53-80). P B Desai concludes a ticipation, the task of generating social health awareness,
general evaluation of the CHV Scheme in India with the securing of the cooperation of women more than of men,
following assessment: “The most crucial shortcomings of this generating appropriate health practices, organising collective
kind of approach is the failure to upgrade the capabilities health actions, etc. We may even piously wish or dream that
’of individuals, families and communities to take upon
“if we succeed in organising the community for giving to
.themselves the responsibility of attaining and maintaining itself-a primary health care system of its own choice, it may
conditions for healthy living within their jurisdictions. In • become all the more practicable to carry forward this process
•other words, the central issue of the promotion of self-care of self-reliant development into all fields of social and
’is left unresolved” (1983: 7). He then stresses the point that economic progress” (Desai, 1983: 8). But the crucial ques
the definition of the objectives drawn in the Alma Ata tion remains unanswered beyond the many evaluations of
•Declaration (1978) to resolve this central issue is ‘holistic’ in the shortcomings and failures of the CHV Scheme: what does
nature, as t^eir formulation insists on a full community parti it mean methodologically to “organise the community” for
cipation and a spirit of self-reliance and self-determination enabling it to wish, to conceive, to experiment, to chalk out
(WHO-UNICEF, 1978: 3), and the “task of delivering health and to give itself a health system appropriate to its concrete
•care must begin with this non-medical, social endeavour of needs. What does this mean in terms of strategies of social
achieving the necessary social transformation at the grassroot action?
level.”
Primary health care as the subject of social science research.
If such is the case, once we have acknowledged and really should therefore be examined and evaluated by focusing on
perceived the social role of the CHV and measured the ’ the dialectical relation obtaining between the level of health
import of the ‘holistic’ perspective with which we should conciousness and the forms of collective organisation on
approach primary health issues, a corollary immediately health issues on the one hand, and on the other, the local
follows, that health development schemes should seek the socio-cultural, administrative and power structures, including
help and the critical insights of social scientists, anthro those of the public health care system itself. If health status
pologists and psychologists. And this is all the more is rightly considered as an index of social development, health
necessary when we are concerned with provision of primary consciousness—as expressed in relevant renewed perceptions
health education and care based on efforts of self-reliance and representations and consequent forms of collective
among the most underdeveloped sections of the rural popula action—should be rightly considered as a component and
tion, whether these efforts be undertaken by government an index of the socio-cultural, and politcal awakening of a
agencies or NGOs. If these efforts are to be.“viable, dynamic given population.
and positive instruments of social progress” (P B Desai), then*.
The health education and care programme carried out by
primary health schemes should first of all become the subject. the voluntary organisation Village Community Development
matter of social science investigation and critical analysis.. Association (VCDA) in the remote hilly areas of the talukas
. We present here below some/socio-psychological observa of Mulshi and Velhe (Sahyadri Range) was considered as pro
tions and conclusions drawn from a social science study of viding an adequate field of observation for such a scientific
a limited voluntary health programme undertaken by a small investigation by the Centre for Co-operative Research in
NGO in remote rural areas of Maharashtra. The study is not. Social Sciences, Pune which conducted the study with a grant
directly concerned with such objectives as the raising of from the ICSSR. The health programme under study is part
September 1986
43
of a wider educational programme (called “School without of autonomous self-determination as well as develop the
Walls” and comprising mainly non-conventional program theoretical ability of the group of health workers.
The validity of in-depth studies is not to be undermined
mes of cultural action for children and women directed
towards children’s and women’s organised collective action) with regard to the needs of those concerned with macro
which is itself a part of a much wider programme of “con- planning and large scale policies. Macro-level planning
scientisation” and organisation of the deprived sections of cannot with impunity overlook the conclusions of in-depth
the population of several rural talukas around Pune. The analyses. Planning remains a futile exercise whenever it does
health programme is carried out in areas deprived of any not take into account the dynamics operating at thegrassymedical services. Quite recently, the government made an root level.
The scheme under study not being a medical care scheme,
effort to implement its CHV Scheme. A few private practi
tioners sometimes visit the area to give injections and to make sampling methods do not suit the objectives of the investiga
money from the population. Medical officers of the PHC tion. The changes.occuring in health preceptions, practices
(Velhe and Paud) do rarely visit the area, except for enlisting and conditions are evaluated by several types of qualitative
“cases” (tubectomy operations). Sanitary conditions arc procedures. One of the most significant is the so-called
particularly bad. Animals are kept inside the houses. Many “sociological intervention”: The sociologist and his assistants
villages are cut off by the monsoon rains. In the dry season, intervene at the time of seminars and analytical exercises,
very few villages are directly connected by a bus to the taluka in-depth interviews of individuals and groups of health
centres. The scarcity of land»does not permit a sufficient and workers on a specific theme; personal interviews of villagers;
balanced diet. Traditional representations about diseases and inquiries made by some trained health workers, personnel
narratives; minutes and reports of usual meetings and free
their treatment are generally prevalent.
The main aim of the study was, to document a few pos discussions among the health workers; and role-plays. No
sible ways of reciprocal determination, among marginalised questionnaire nor schedules were used; only guide-lines were
rural population deprived of elementary health services, of always carefully prepared for conducting discussions. The
study was spread over two and a half years (1983-1986) as
three series of processes:
(1) The spread of medical knowledge and the consequent a sort of continued analytical effort following and accom
improvement of health conditions among marginalised rural panying the evolution of the action programme.
population;
Awareness of Identity among Health
(2) The process of socio-cultural and socio-political
Animators (HAs)
awakening especially with reference to the representations
about health and body and the present disfunctions of the
The most decisive step consists in generating a basically
health care system, with the consequent people’s collective new approach through a sort of cultural labour prompting
initiatives of organisational attempts to deal with health the volunteers to discover their identities as HAs in a way
problems as well as other related issues;
quite different from their own expectations obviously model
(3) Autonomous and alternative efforts to promote led after the social patterns and the collective representations
attitudes and concrete attempts of collective self-help in shared by the population at large.
respect of primary health education and care among the same
After two to three years of health training and practice,
weaker sections.1
HAs unanimously acknowledge their complete unawareness
The assumption underlying and motivating the study was at the beginning of what health might'mean. The contrast
the conviction of the necessity of such a reciprocal deter between the perceptions acquired during many months of
mination: failing this, no health development scheme—be continuous training and involvement and the remaining
it of a minor scale—can significantly contribute to the radical memories of the initial understanding leads to an evaluation
changes needed in this field. The aim of the qualitative study of what happened.at the begining. First of all, the idea, let
was to describe and establish the nature, the extent and some alone the wish, of any health activity being undertaken by
forms of this mutual positive correlation.
the population itself, did not emerge of its own from the
A second aim was to draw observations and conclusions people concerned or involved as HAs or as beneficiaries.
relating to and bearing i4>on concepts and procedures of What then was the motivating factor prompting them to
development—and especially of health development— of undertake health tasks? People from the lower sections
processes of cultural, social and political awakening and volunteered to undertake a health activity on account of the
organisation of the marginalised sections of rural popula moral authroity that their organisation Garib Dongari
tion. These latter processes are obviously leading towards Sanghatna (GDS) had acquired and of the trust they had
redefining the epistemology of development. The case study already put on the external social agents who floated the ideal
sheds some light on these theoretical issues with regard to (the main animators acting as catalysts of GDS). It is obvious
underdeveloped rural masses the health needs of which have that without the on-going organisational process such a
been consistently neglected.
prompt response, would have been impossible. Without such
Three aspects characterise the methodology: The analysis a collective social support with its components of moral
is jointly and cooperatively carried out at all stages, with authority and confidence, neither the. idea of a health task*
those concerned and involved in the scheme, resorting to would have been effectively welcomed by a deprived popula
methods of collective self-analysis and research-action. Such tion nor any man, let alone a woman, from lower sections
a methodological approach is expected to promote a better would have dared to volunteer.
critical consciousness and consequently to foster the process
Secondly, in the absence of an awareness of the urgency
44
Radical Journal of Health
of health issues, what representations defined and accom cess to, the sharing and circulation of. medical knowledge
panied the idea of a health task? The possibility of some among rural lower sections. Secondly, a health scheme is
honorarium was a very strong constituent; the vague desire bound in the first instance to be specifically ‘recognised’ or
of some sort of ‘employment’ was also there; “to become understood, from a socio-psychologically point of view,
a doctor!” was a widely shared expectation; “to distrubute through the established patterns of representation concerning
medicines and pills, to give injections, or to become a dai”: doctors, health and therapies. There may be therefore some
such was the most substantial content discretly related to naivety on the part of action groups to resort to health as
health; some had really no idea of what could be the task an entry point if this means that health, as such, on account
expected from them; there was a strong apprehension, of its urgency, is expected to easily generate radical social
especially among illiterate women, about their ability to com insights. The prevalent unawareness about health as a
prehend; some daring pushed ahead all of them and some personal as well as social issue and the deeply imbibed preliking too. When we. compare these initial representations critical and unconscious cognitive structures in this respect
with those brought about after three years of experience, make health one of the most deceptive and difficult ‘entry
three main shifts appeared to occur in the preceptions. Firstly, points’ if one looks forward to it as a lever for radicalising
from static notions of social status and prestige position rural populations.
In such circumstances, a main concern of a health scheme
associated with the health profession and the expectation of
an employment, the approach evolved towards activist consists in defining the role of the HA. This had been and
attitudes, became action-oriented and conceived in terms of remains one of the main themes of the regular and con
actual achievement. The systemic outlook was altered into tinuous training programmes of HAs in the VCDA scheme.
a dynamic attitude. Secondly, from self-preceptions in terms As a result of discussions among all those concerned by the
of ignorance, fear and inferiority feelings, there was a shift scheme, doctor, activists and mainly HAs, the following write
towards self-confidence, boldness. Their ability to assimilate up was prepared as a basic chart of the HA’s role, as an
knowledge enhanced the self-image. Inhibition gave way to operational model.
self-assertion. Thirdly, from an individualistic outlook and
Our Health Work: Why and How?
wishes of private profit, there was a shift towards a social
—We and our children fall sick every now and then.
understanding.
—When we fall sick, we never get medicines soon, nor do we get good
The interest was hence motivated at the start by the hope
medicines.
of a small honorarium (discontinued later on), by the wish
/. Why du we fall sick so often?
to be a ‘doctor’, by the desire to escape deceptive practices
The
reasons
are
that:
of the private doctors, by the pleasure of getting informa
1 We do not get enough to eat nor is the food good. Then, as a result,
tion “when we realised that we could understand it”. The
we become weak.
interest of those who had no specific liking for the topic was
2 We do not get enough of water, nor clean and pure water. As a
result in the dry season, scabies increase and in the rainy season, diar
raised when they learnt something new and delivered a few
rhoeas increase.
pills. After two or three years, four main motivations are ex
3 Our living quarters are small and not clean. We keep our cattle
pressed as follows at the time of health seminars: Let us give
inside our houses.
information to the people. Let us sit together and educate
4 During the rainy season, we work exposed to cold winds and we
people. Let us organise the people. Let us be self-reliant. Later
have not enough clothes to put on.
5 Our work is dangerous, instruments arc primitive and insufficient.
new-comers, all women, all illiterate, who joined a scheme
As a result, accidents occur; we are overworked; we quickly tire and
which they had observed, give ,the following reasons for
we do not pay attention to our health condtion.
taking up this responsibility: to get a new education and
6 Many times, we are overwhelmed by difficulties: as a consequence,
training; if they fall sick, to be able to do something by
our mind does not remain sane. The pressure of the male domina
tion upon women is epccially heavy.
themselves; the good results of the medicines circulated by
7 The government has no money the government people do not give
the HAs; no money to buy medicines from private doctors,
us information. But it takes great care of a handful of privileged
but cheap pills available from the HAs, even on credit;
people.
doctors take a lot of money and do not treat unless paid
8 Bad habits: alcoholism, tobacco etc.
beforehand; interest in this topic; if they now learn, their
9 Frequent pregnancies.
10 No vaccination.
children can be taught... To the question that such interest
If we could get rid of these difficulties,.then we would not fall sick
may not be sufficiently strong when male pressure is raised
so often. But, today, these difficulties cannot be removed. As a con
against women taking the lead, the answer is that: “We have
sequence, the frequency of diseases cannot immediately come down.
been selected by a group of people during a meeting. We have
2. Why do we not get proper medicines when we fall sick?
the support of people”.
1
There are no doctors in our area; the ‘medicine men’ are many, they
As a matter of fact, external support is not sufficient. The
deceive us.
female new-comers maintain their involvement out of a
2 The doctors who come iqto our area, behave like 'medicine men’;
strong inteYnal conviction: “We have seen the earlier ones.
for instance, for no reason, they put on a very serious face, use difficult
They committed themselves to this work. They have not
words which they pronounce like mantras and create an atmosphere of
mystery. Although there is no need, they give injections and prescribe
eloped or have been taken away by men! The provision of
useless medicines. The medical profession is being converted in to a
a health education scheme, to succeed or fail for many
business like any other business. It is a profession consisting of selling
reasons absolutely alien in nature to the health issues tackled
medicines. The more money you give, the belter treatment you .will
by the scheme. One of them has been suggested above con
receive. A doctor is no different from an agent of a drug company.
cerning the social factors conditioning the desire for, the ac
Doctors behave like dealers:.they store the knowledge as shopkeepers
September 1986
45
store the commodities ano make us more expensive. There is a com
petition for consumers, (as among dealers) to obtain more consumers
and gain more money.
Where is ’humanity’?
3
What is clear about today’s doctors!
Doctors do just sell treatments. Moreover, oh account of the doctors’
behaviour, some ideas are firmly embedded in our minds, for example:
money is everything; the knowledge of the doctor is very complicated.
We shall never be able to understand anything of it; Our health depends
upon doctors; Doctors’ work is intellectual and of a much higher grade
than our labour in the fields.
4
tices of medical care; 4) al raising the level of socio-political
awareness of the whole population in this respect through
health education, self-reliant practices and collective health
action as levers, thus contributing, in its own way, to
strengthen the overall health movement; 5) at resorting to
operational concepts and criteria of evaluation of a social
and cultural nature instead of giving priority to and taking
only as operative norms the quantitative medical im
provements in the health status of a given population,
objective that at any rate the NGOs are unable to achieve—
particularly the small ones—on a suficicntly large scale.
What is rhe use of our health work!
Selection of HAs
We cannot bring about important changes in our condition, so
exposed to diseases with our health activities. The reasons are as
A general model remains futile without its operational con
follows: Our health condition depends much more on many other
cepts. The selection of HAs is one of them. With rare ex
factors of our whole environment than on medical factors; the
ceptions of selection being made by the external main
knowledge that we can get about health as health animators is limited.
animators of GDS, the HAs of VCDA were regularly selected
The pills and medicines that we give are simple and not many.
What then is the use of our health work?
by local groups of GDS during their meetings (with the ‘per
We want to bring, at this primary level, a new concrete way of under
mission’ of the husband or parents for the female HAs). A
taking health work. An example will make it clear. What is the
few women were selected at the start on account of their
difference in the health work, between the method that is usually
activity as teachers in a voluntary nursery school of GDS.
followed today, and our method? This will be clearly understood from
the following example
Sometimes special meetings were called to deal with this issue
Let us suppose that a lady health animator from our group attends
and several meetings were necessary to make a selection. In
a child suffering from summer diarrhoea, what will she be able to
the course of time, when new volunteers joined, they were
achieve?
all co-opted by the local groups of GDS. The selection was
Change in the body. We shall be able to win over the disease which
affects the body of the child.
not a sort of casual appointment but the result of group
Change at the economic level'. A good treatment can be given at a
discussion and exchanges among the assembled people.
very small cost. We can demonstrate it.
When the health workers look back and consider the pro
At the level of health consciousness: The health animator can change
the ideas of the people. What will she/he tell them?
cedures of their initial selection, they come to the following
1 Why diarrhoea occurs, what is the treatment, and if it can be conclusions.
prevented. This techincal knowledge about diarrhoea will be given.
At the beginning, without any experience of procedures
2 Why diarrhoea occurs much more often among the poor and
of collective determination, “We had no idea of the method
in the villages. How the proper preventive treatment of diarrhoea
depends upon a proper water supply. Why today’s doctors and drug
followed, and we did not understand its importance’’, confess
companies lake pleasure in treating diarrhoea with very expensive
all of them. The cooptation process from within a group for
medicines. This is social knowledge that the health animator is giving.
a task to be carried out. in the name of a group or mass
3 How there is no need for a doctor to treat simple and minor
organisation
was a procedure absolutely unknown. They did
ailments and what is the opposition of the private doctors to this
not realise the meaning of this process. Three years later in
statement.
4 How we can deliver people from the exploitation of private 1984, all of them except one woman who dropped out express
doctors.
the firm conviction that it is proper to make the selection
5 How in our health work there is no domination of the doctor.
from within a group of assembled people taking a common
We don’t give him undue importance.
6 Why, despite so many promises and announcements on the part decision.
of the government, this latter cannot seriously undertake genuine
The reason are the following:
health work of that sort.
The selection should be made according to the ideas that
7 This health work is going on in a nice way, because we arc
the people have about it. Their ideas should be taken into
awakened, organised. Our health work will progress to the extent our
consideration; A private selection is a mistake; when there
awakening and our organisation will grow.
8 Still, as long as food, water, shelter, education, cloth, etc. are not is a decision of a group, the selected person feels responsible
available, we shall not stop falling sick time and again.
to the group and the group responsible to the individual. This
This definition of the HA’s role tries to give a concrete
design to a specific concept of health work among and by
marginalised rural population. This concept ought to be
made explicit. The health work in such a context is conceived
as aiming 1) at forging a collective health consciousness based
on a critical perception of the relation obtaining between
people of lower social strata and their actual physical en
vironment and specific social constraints; 2) at making ex
perimental attempts which constitute perse a practical criti
que of the prevailing methods and structures of the health
care system; 3) at projecting in an embryonic form a sort
of miniature model revealing the feasibility conditions of
alternative values, norms, organisational patterns and prac
46
is bound to generate a reciprocal questioning of both of
them. And such habit should exist; in the case of a private
selection, people will not feel like cooperating with the one
selected, nor give him/her their support. When a meeting
is called, everbody will find an excuse for remaining absent.
The model to be followed in the future is as follows:
“In a new village or a hamlet, we shall hold a meeting on
health and give some information about it. Then, we should
tell the people: To tackle your problems in this respect you
should select your own man/woman for that”.
Why should this procedure be followed? This process
induces the awareness of a reciprocal responsibility; It avoids
the danger of pressures of vested interest and the criticism
Radical Journal of Health
attending training course ih health or undertaking health
tasks. Only women upon whom husbands and family could
not keep a firm control were so allured. Their volunteering
showed their lack of social restraint and fear. “Men and
women sit together!” “Women just like to follow their
whims!” It was almost out of lust that they had volunteered!
4 The fourth image was that through this scheme, a dispen
sary would be set up, medicines and pills would be made
available. In this respect, as people were saying that “an
educated man is needed to give medicines”, women had
doubts about their ability to prescribe medicines, as they were
conscious of their ignorance and absence of education.
These data show that two main and anti-thctic socio
cultural cognitive structures gave readymade referential yard
sticks to understand and evaluate the event. The first
reference relates to the women’s roles and image: a woman
should never go outside of the home where she is confined
to subordinate and non-prestigious tasks. The second
reference relates to the prestigious function and role of a
doctor as a supplier of medicines and health services. As the
health animators were considered as doctors, these two
referential factors clashed and as a consequence, the women
were derided, for assuming a role of high rank and superior
knowledge!
The basic and spontaneous point of view was not a
technical or practical approach, but a social reading; and
this reading was no conceptual insight nor analytical appre
hension. It was a judgement. The cognitive structures
worked, as a judicial recognition, not as an act of cognition.
How Villagers Perceive Health Animator
If this is likely to be the case in any transfer, its sucess depends
Another determining factor, mainly at the initial stage, is upon the will and the ability to develop a conceptual
the perception of the beneficiaries and their expectations. understanding and to refrain from any hasty and spon
Four types of reaction characterise these altitudes, in the taneous interpretation by referring to the in-built structures
perception of HAs, which symbolise four cognitive struc of recognition which can lead nowhere but to a judgement
tures through which villagers spontaneously approach this which is only a reduction to the same. This seals the
health experiment.
impossibility of any progress.
This is obvious in our case. If the judicial recognition turns
1 “The village has got a big ‘doctorin’!” This derogatory
into
a judgement against illiterate women and ignorant men
remark related to the women health animators. It points out
firstly, that the health worker is considered as a ‘doctor.’! And taking up the role of a ‘doctor*, as this is simply a contradic
secondly, that the prestige and honour implied in this image tion, still a women may be considered as positively motivated
serve conversely, to ridicule people—, especially the women, to take up this task for the reason that she wants to bring
or the illiterate workers—volunteering for the scheme being home some income, for the benefit of her husband and her
projected so suddenly to such a high position! People did children, as the source of wealth of the house {dhana). This
not react mainly in terms of the concrete advantages of the is also a very clear cognitive structure regarding the role of
scheme, but with regard to the social image of the doctor a woman. The understanding of her desire to become a health
and to the concept of health as a doctor’s commodity both animator is therefore either, negatively, a will to escape her
of them turned into arguments meant to throw discredit upon duties at home and the control of her husband, or positively
ignorant people pretending to be more clever than they were a justifiable intention of bringing home (to her owner, for
the benefit of her house) some wealth, as she is a lakshmi.
to involve themselves in these tasks!
or the mockery against the one who is chosen; this process
assures cooperation, support and participation; there cannot
be any real work by an individual alone.
What do these procedures aim at?
These procedures impart information to the people
(doctors never impart information about health and thrive
upon the ignorance in which they keep the patients; people
get a chance to assemble, exchange and make an effort to
solve their own difficulties; the objective is to become selfreliant, “to stand on our own feet”; this helps to strengthen
and spread the organisation GDS; the intention is to put an
end to the deceptive practices of doctors and of the local
miscreants who act hand in hand with the doctors; this brings
a health knowledge to the village level; this develops a health
consciousness; this gives the women an opportunity of having
some role and stand in society; this offers a chance to
everybody of speaking out.
Let us draw one clear operational conclusion from these
data: the perception of health as a collective issue that
confronts the whole community is generated here through
a social process of cooperation, by the group, of a volunteer.
It is not the perceptions of health as a community problem
which comes first and leads to a renewed social practice. Il
is a renewed social practice which helps developing a new
approach towards health, as it could have been with any other
issue. There cannot be any real consciousness of collective
responsibility unless it takes the form of an appropriate
pattern of social relation or a cooperative social formation.
2 This work was looked at as sort of employment for the
One operational conclusion can be drawn from this. If a
volunteers. As the possibility of an initial honorarium of health scheme aims at engineering a process of social change,
Rs 50 was known, the task was considered as resorted to by vfz, a transformation in the patterns of relationship and
the volunteers under the motivation of this material incen values, it should and it could boldly create a situation which
tive. The women would then be able to bring their contribu will directly challenge the cognitive structures mentioned. For
tion to the maintainance of their husband and children, as that purpose a health scheme should not start with doctors
they are the dhana of the house, its source of wealth, its and medical services run by doctors: health should not firstly
lakshmi.
' ,
be looked at as a technical task. Secondly, the leading role
3 The third understanding is that this task was just a in the implementation of the health activities should be given
chance offered to the women’s eagerness for being ‘set free’, to those women whose health is the most affected by the
abandoning the household duties under the pretext of present health system. These activities should mainly and
September 1986
47
basically consist in imparting elementary health education
to women and more technical knowledge should come as a
secondary dimension. A health animation activity under
taken by women of the lower social sections, taking the initi
ative of visiting and educating village population is likely
to prove one of the most effective levers of social change in
the rural areas, as this practice breaks off strongly built-in
cognitive structures which have a definitive repressive role
and are very significantly responsible for the perpetuation
of a particularly degraded health status among women: the
partiarchal patterns of relationship and values, and the undue
prestigious status of the (male) doctors as the only ones
capable of dealing With health and medicines.
Socio-cultural Pressures Against Health
Animation
Between 1981 and 1984, out of an initial group of 30 HAs
(14 men, 16 women), 17 dropped out (6 men, 11 women),
while 18 new comers volunteered (1 man, 17 women). Those
who remained involved had collectively analysed the reasons
why so many dropped out—26 answers-could be specifically
given for the defection of 17 HAs. These answers arc
classified into 9 categories as follows: .
1:3 male and 3 female HAs abandoned as they did not
obtain the expected financial profit. The honorarium was
considered too meagre; even this was discontinued and
substituted by small help given on the basis of the days spent
on house visits and meetings held, etc. Motivations were put
to the test.
2:5 female HAs left under the social repression obtaining
against women’s assertiveness.
3:2 men and 1 women left for reasons of economic pressure
and poverty.
4:3 men left out of diffidence about their own ability and
social inhibition.
5:1 man and 1 woman were frustrated in their expectation
of a higher status sought through this activity.
6:3 left on account of personal reprehensible behaviour.
7:2 women left because they could not cope up with
the task.
8:1 woman could not bear the clash between the knowledge
received and her traditional beliefs.
9:1 woman left out of lack of proper motivation.
These reasons are indicative of the difficulties and of the
nature of the psycho-social determination of those who
maintain their involvement with a renewed conciousness. It
is obvious that almost all HAs joined the scheme with the
thought that they would get a sort of paid employment thus
improving their low social status. As a matter of fact, if all
of them could secure through this programme somehow
better social position, a qualified social recognition and some
social respect—and self-respect—, paradoxically would
remain more involved in the scheme than those who were
usually deprived of such social respect, often denied the right
to talk in the open and assert themselves, while those who
already enjoyed some social prestige left an activity which
appeared to them as not enhancing their dominant social
position, or even countering it.
One should be fully aware of the basic difficulties which
any attempt of popular health movement among under-
developed rural population has to overcome before becom
ing a strength. If we are convined that there is no alternative
to such a movement for bringing about significant structural
changes in the health care system, wc ought to be still more
aware of the socio-cultural challenges this implies in the first
instance. Two testimonies may convey the magnitude of the
challenge. The first one is the testimony of a woman HA
whose potentialities as organiser are totally repressed by her
husband.
I was conducting a balwadi under the sponsorship of VCDA since
one year. On this account, 1 was, therefore, going from house to house
to fetch the children. ! found many people sick during the monsoon.
Althogh they were suffering from simple ailments they were going
to the doctors and taking injections. Doctors were coming from outside
and knew how to take advantage of this situation; they collected and
lot of money from the population for this. I thought, let us do
something about these minor ailments, through health education. Then
I volunteered to become a health animator
Private doctors do not give information on about diseases, they
just give medicines. They come to our villages only to raise money
from the population. I started telling people thus and trying to con
vince them. Six women came together and, through the Association,
wc requested Dr. Phadkc to come and impart health education. The
doctor used to come twice a month in the beginning and gave us infor
mation about the children’s and women’s health. We were getting Rs
50 as honorarium.
In the beginning, women called me names. But, later on, opposi
tion become less. People trusted the information that wc were giving
them and followed our prescriptions. Similarly, they could observe
by themselves how the government doctors functioned.
When I had to go and attend a meeting (training camp) and spend
one night outside, my husband would object. “Who will look after
our daughter who has reached the age of marriage? The younger
children are going to school: who would look after them?’’
I have now after three year accepted the job of becaning health
worker of the government so that the health education that I received
during these years is not wasted. They organise only one meeting per
month. When VCDA stopped giving the Rs 50 honorarium for
the health work, my husband became completely opposed to my parti
cipation in these activities. This is the reason I accepted government
work. And I continued this health activity with the same motivations
that I got from VCDA training
With the government we do not hSv’i the freedom to function as
we think right; we have to do the wortonly in a very particular way.
Although I have accepted the wor^’of the government I like to at
tend the meetings and the camps for women of the VCDA My ex
perience with the government is very different. People get absolutely
no health education from them. Only one thing matters: to distribute
pills and to keep monthly records. This is what the health officers
consider good and important health work.
Should b®.abI.c 10 slud>' as we were doing which quesons the women shou d think over and take up. For instance, women
educatioanmOVCment
drinking Watcr’ as a resuk of thal
fn
^ond testimony is the account of the difficulties
!fpvddnf d heby l \e 8r°U0 Of HAs from panshet whose
level of deprivation makes difficulties more acute. 1) The first
t^teaeh*
°nrT d^^ 3b°Ut °ne’S 0<Vn abilitv lo folloW
a^d
W? s' dOClOr’ “We Sha11 not be ab* to learn
ana stuay: \\e were not educed»• >
anything about health, dispensary medicines ” Therewas
no conviction of one’s ahiltrv
‘ 1 nere "as
of the doctor. None of the HAs had
COrre?ll:‘'
!essons
anv meetinn nr ...
.
LVer previous!.- attended
any meeting o expressed himself in a group “For three
months I just kept silent in the meetings'”
as "any XZXdSXZ hUT beinSS- “ mUCh
48
Journal of Health
and cattle. Where is the government? How to go and meet in the HAs and in the organisation a direct challenge to their
them? We did not have any idea about it. We had no idea authority. “They arc not Dhanagars (in one area, many HAs
that we had also rights. HAs were requested to commit were from this caste), they are foreigners: they come to collect
themselves to assume a social role when they had hardly a girls and send them abroad where there is a want of girls.
clear consciousness of their own identity of social beings. One should not vote for them. If they can get four votes,
No wonder this generates a strong feeling of self we can still have ten of them... Listen to the head-men of
diffidence. “I am afraid that people will not come and attend the village. This is not proper. Our women should not talk
our meetings, nor listen to us.” Still, “I am convinced that with men from outside!” “The HAs get plenty of money:
going out to attend meetings, I shall learn something. How this is the reason why they roam about”. “They get medicines
long should we continue to submit and surrender to the free of charge and take money from us!” As expected, the
same leaders make capital of caste feelings to object to the
leaders?”
Going alone from house to house to give information fact that HAs of different castes assemble together, and do
about health was seen as a great difficulty by some. Some not listen to the caste elders.
A few drunkards come to disturb the meetings, teasing,
felt it was easier to impart health education in a meeting,
within a group, when people are assembled together, because shouting, raising their voices with the result that people
there can be exchanges and discussions, and those who cannot express freely their difficulties, despite their genuine
desire to do so. In the beginning we did not know how to
understand can help others to learn.
There was the reluctance to listen to women: “They cannot handle these trouble makers”.
even behave themselves in the society and look after them
selves! How should they come and teach us! Men teased the
Dynamics of Self-Assertion
female HAs, especially after having had their drink, “We
The
interviews
of the new-comers—all women who happen
shall, all of us, now, become doctors!” “Why make everyone
to
join
the
existing
groups of HAs reveal the following
a doctor also like you!”
The pressure of the authority of elders especially upon processes:
Personal acquaintances and a prolonged time of “wait
l)
women makes these latter still more shy and inhibited to
undertake something new and unusual. Men complain and see” attitude preceded any decision. The example and
against women that they attend meetings and report there the concrete testimony of some one else are necessary as a
about the drunkards of the village and all their stupid and preliminary step.
bad behaviour, and first of all about their insults against the
2) A clear invitation to join was made, not to elicit a purely
HAs. The pressure of the more influential male leaders was individual move but a commitment tp participate in a col
and remains a serious difficulty for the women who volunteer lective effort.
or would like to volunteer.
3) The initial step were met with laughter, counter
The countter propaganda objected that outsiders had come
propaganda,
lack of appreciation on the part of the
and trained HAs who immediately listen to them and follow
them, falling a prey to them. “We should only look after our population.
fields, eat peacefully our pancakes of millet. Women should
4) The decision to join was personal and motivated by a
just go to the fields or to the forest for their tasks, earn a will to achieve something and dedicate oneself to a task
few rupees for the house; this is better than attending meeting whose relevance was understood.
and roaming about, everywhere, doing nothing, whiling the
5) This understanding increaseed the strength of the
time in useless activities which do not yield any income. What
will you get (money) from this work? What will these people personal motivation and developed progressively a wider and
realistic social consciousness.
give you?” Aren’t they already ‘social workers’ in our village?
6) The motivation takes momentum, against objectidns,
(leaders who are supposed to care for the welfare of the com
munity). Local leaders do often call women names because out of one’s own effective commitment to tasks which arc
they follow people from outside instead of going to work experienced as beneficial. Action generates self-assertion.
to bring home a few rupees, listening only to them and
7) The group proves to be the best support for the personal
keeping a submissive attitude towards them.
efforts and commitment: A small group of like-minded
Another type of counter-propaganda says: “What did you
people is the essential structural factor.
obtain and what did you give us after three years?” The
8) The elements of general personality development (self
understanding behind the objection is that the organisation
should immediately bring in some material improvements assertion, ability to express oneself and talk in front of a
to show its credentials, to the population, free of charge and group, capability to understand a knowledge considered as
without any effort on their part. The reason motivating the difficult, etc,...) work as an encouragement.
objection is also that the organisation “of the poor of the
9) When money is seen as the main motivating factor, no
mountain” is approaching directly the administration and effective health animation can be sustained. Monetary com
demanding the implementation of the government schemes pensation may not go against a real interest in health and
for the benefits of the needy, independently of the local health education, but once such an interest is maintained by
leaders who have a vested interest in the poor depending upon monetary incentive only, we cannot expect it to develop into
them.
a social concern and commitment for health animation and
HAs insist upon the reactions of the local leaders who see community organisation on health issues.
September 1986
49
shows their superiority and “if we ask, we arc left with the
following answer: “You are ignorant! What can you under
stand! Don’t you have confidence in me?... I told you once,
HAs wished to co-operate with the government health I shall not repeat... and so on they simply do not care
services rather than compete with them. A voluntary scheme for whether we understand or not: nor why we cannot
is no substitute to public health sevices. The several attempts understand.
^A second feature consists in not giving information about
made by VCDA to operate jointly with the government servi
ces met with only a little success. As our concern here is with any disease: they would just hand over medicines. They never
the local socio-cultural processes, we shall consider only the impart nor show any readiness to impart knowledge about
psycho-sociological dynamics obtaining between HAs and health qnd disease. Mainly concerned with cases of family
PHC personnel rather than the possible forms of co-opera planning, they do not give due attention to the sick. Expecta
tion. Let us give due attention to the perceptions of HAs con tions regarding money are another main feature of their
cerning the behaviour and the attitudes of th;'government behaviour. The question may often be raised, from the start.
personnel, as articulated in health seminars^by HAs.
If there is no money, the patient may be sent back or adviced
1. Government doctors are to be seen at the taluka centre to come later, or another day... Money and injections are
and in the villages only in the specific places where com two main aspects of the doctors* behaviour. •
modities and facilities are available. Government doctors will
The doctors would also easily entrench themselves behind
always be seen in the company of a limited, restricted and the laws and rules of the government. They do not appear
specific category of people: with the sarpanch, the patil, the as responsible towards the population; they are not answer
teachers, and sometimes the talathi and the kotwal. Their able to the people.
social place is with the leaders, the rich, the notables, “with
These frustrations and clashes with regard to the medical
those who talk”. They will behave with them with civility. practices of the government personnel lead to conclusions
They will be attentive and considerate with the established already often drawn but naturally stressed by HAs in their
notables andje’aders. They will be seen in their home places. analysis.
They will accomodate them immediately when these latter
1) The doctor’s services are alien to the needs themselves.
come to meet tham and they will attend to them without “Our main expectations is that the government doctors reach
delay, and show them small courtscys. The government us, the poor, who need them. They don’t. They never come
accordingly behave also as local leaders.
to the houses of the rural poor”. “We don’t know what the
2. The attitudes which motivate their way of talking and word nurse mean. If it a thing to be eaten, or an animal?”
their behaviour lead them to make a show of their superiority “We asked the PHC officer to send us a nurse: he just
a^d importance. Their arrogance is resented by the people; promises but nobody has ever come”. Once, at Sakhari,
they do not let others talk and express themselves. They speak thanks to the firm insistance of HAs, doctors came and HAs
fast and loudly over the voice of others as to frighten the helped them to vaccinate the children. HAs motivated and
people. Their manners show that others are not worth assembled the people. Then the doctors promised to come
attention, being all ignorant people. “They consider the poor to another village, Dudhavan, under the pressure of the HAs.
as stupid and childish”. With the poor, they are, insulting But they never did. The false promises of doctors to the HAs
and offending their feelings; they do not give answer if poor are a permanent matter of tension, diffidence and disgust
people ask questions.
about the government health care system, and its personnel.
3. A few features characterise their language and ways'of Another area of tension is the insistance of the government
addressing the common people. They often use words (some personnel that HAs should bring to them women for being
special or English words) that people cannot understand^ sterilised. The government CHV are supposed to do it, why
with the purpose of not being understood. This language should the HAs not give priority to this too? HAs answer:
Chart
Antagonistic Perceptions and Conflicting
Practices
We HAs
The Government Health 'Personnel
— We go antf visit the poor at home
— We arrange for few cheap and good medicines being
supplied to people
— We give priority to the people
—We educate people
— We look at the patient and give the appropriate
medicine
— We think of the whole environment and situation
— We select HAs taking into account the ideas of the
people
— We organise people for collecting action oq health
problem
— We promote health consciousness
— Health is a public issue and a political question
— They enter only in the house of important people
— They give importance to medicines
50
-t They give importance to money
— They just distribute medicines
They don’t give all the medicines required to cure
the patient
They don’t bother for the whole environment
— They make private choices
— They don’t try to assemble the people
- They don’t bother about health awareness
- Health is a private problem to be solved by doctors
Radical Journal of Health
Conclusion
“You don’t give any protection to our childre. Four live and
four die. First come and attend to our children, save them
and we shall bring you plenty of cases. Otherwise, why should
we undergo operations?”
Strategies of “Health For AU” will prove effective when
we succeed in translating them into alternative social prac
tices of “Health by the People”.iThe chart on p 50 is an
2) The health system is not directed towards the people. attempt made by HAs of VCDA, on the basis of.their
Those HAs who were absorbed in the government scheme: experience, to define antithetically, these alternative health
“During the training meeting organised by the government practices required as a foundation of a people’s health move
every month, doctors and their CHV pretend that doctors ment among rural marginalised population.
In view of the magnitude of countervailing forces, there
are ready to go anywhere. If HAs protest that they have never
seen them, that doctors make promises which they never is little likelihood of such alternative health practices gaining
keep... Government doctors and their CHVs look down on their own a significantly large and lasting momentum
upon us, repress us as women who talk too much and had unless (1) they are locally part and parcel of an appropriate
better shut up in front of them! When we asked the doctors: wider peasant movement putting out similar roots,
“Why do you take money from people, regularly, although (2) externally backed by and related to, other branches and
you are paid by the government?”, doctors reply angrily: • forces of the national health movement and (3) internally
“Why don’t you take money yourself also from the people?” born by a permanent self-learning exercise addressing the
Doctors insisted and added, addressing a dai “before doing anthropological, socio-cultural and ideological dimensions
any delivery, you must first ask for money from the people”. of the primary health issues. For lack of space, we did not
Doctors advise their CHV: “You had better stay at home. . deal here with these pedagogical, anthropological and
Do not visit houses.” We, HAs, tell the people: “Go and see ideological components as essential to any effort towards
the CHV of the government.” People reply: “They do health by the people.
nothing. They do not inform us. They do not come and
References
attend us. They tell us nothing, they just give a pill”. We tell
people: “It is your right to go and meet them and avail from Alma Ata 1978: Primary Health Care. Report of the International Con
ference on Primary Health Care, Alma Ata USSR, WHO-11978.
them their services. It is a government service.” People reply:
“We prefer to come and see you. No improvement is gained Bose A and Desai P B, Studies in Social Dynamics of Primary Health
Care, Hindustan Publishing Corporation, New Delhi, 1983.
from them. They are of no use”. Doctors tell us: “You want
Djurfeldt, Goran and Lindberg, Pills Against Poverty, London, Curzon,
conflict... You organise demonstrations... We shall also
1975.
organise such demonstrations... You cannot even sign your Health for All: An Alternative Strategy, Report of a Study Group set
name and you'immediately strongly reply and object to what
up jointly by ICSSR and ICMR, Indian Institute of Education, Pune,
1981.
we say!”
3) The selection of CHV serves vested interests. In Panshet
area, when the CHV scheme started, HAs insisted that
women should also be taken, and not only men, and even
illiterate women. Some were appointed but no further co
operation could materialise in'other places, despite the
readiness of the HAs to help goverment officers in the selec
tion and implementation of the scheme.
Jobert B: La Participation populaire au development sanitaire: le cas
des volontaires de la same en Inde, Pevue Tiers Monde, t XXIII,
91; Juillet-Septembre 1982, Paris.
Poitevin G and con der Weid D, Roots of a Peasant Movement,
Shubhada-Saraswat Publications Private Ltd, Pune, 1981.
Guy Poitevin,
Centre for Co-operative Research in Social Sciences
Rairkar Bungalow
884 Deccan Gymkhana, Pune 411 004.
Economic and Political Weekly
A journal of current affairs, economics and other social sciences
Every week it brings you incisive and independent comments and reports on current problems plus a number of well-researched,
scholarly articles on all aspects of social science including health and medicine, environment, science and technology, etc.
Some recent articles:
Mortality Toll of Cities—Emerging Pattern of Disease in Bombay: Radhika Ramsubban and Nigel Crook
Famine, Epidemics and Mortality in India—A Reappraisal of the Demographic Crisis of 1876-78: Ronald Lardinois
Malnutrition of Rural Children and Sex Bias: Amartya Sen and Sunil Sengupta
Family Planning and th^ Emergency-An Unanticipated Consequence: Alaka M Basu
Ecological Crisis and Ecological Movements: A Bourgeois Deviation?: Ramachandra Guha
Environmental Conflict and Public Interest Science: Vandana Shiva and J^Bandhyopadhyay
Geography of Secular Change in Sex Ratio in 1981: Ilina Sen
Occupational Health Hazards at Indian Rare Earths Plant: T V Padmanabhan
Inland Subscription Rates
Institutions/Companies One year Rs 250, Two years Rs 475, Three years Rs 700
Individuals Only One year Rs 200, Two years Rs 375, Three years Rs 550
Concessional Rates (One year): Students Rs 100; Teachers and Researchers Rs 150
(Please enclose certificate from relevant academic institution)
[All remittances to Economic and Political Weekly. Payment by bank draft or money order preferred. Please add Rs 14 to
outstation cheques for collection charges]
A cyclostyted list.of selected articles In EPW on health and related subjects Is available on request.
---------- ----------------- ------------------------- ;----------- COMMUNITY HCALT! I ClJ L
September 1986
47/1, (First Floor) St. Marks
Bangalore - 560 001.
Immunisation as Populism
A Report
aslia vohunian
A mass polio immunisation campaign was launched in Maharashtra in May 1983 with much fanfare. The war
on polio' was meticulously planned and 6,000 volunteers mobilisedfthe All India Institute of Physical Medicine
and Rehabilitation acting as medical advisers. By the end of July two-thirds of the slum colonies were supposed
io have been covered. The article takes a closer look at the campaign and discovers shocking lapses. The
campaign it is pointed out, was merely a gimmick created to aid and abet the then health minister s political
ambitions.
THE use of health in populist politics is as old as the ends. She did not bring in unnecessary .rhetoric about which
rationale was reserved for public consumption: such as one
Emperor Ashoka. But it is difficult to find as blatant an
example as the mass Polio Immunisation Campaign launched of the printed “public appeals” which said: “Of all these
in May, 1983, by the then health minister of Maharashtra diseases, polio is the most dreadful... (it) not only causes
whose “War on Polio” campaign warrants close study for death but also produces permanent disabilities of varying
its sheer ambitiousness, and its unabashed use of a health
degrees, which not only makes the life of the children and
parents miserable but also burdens.. .Society. This problem
intervention to achieve a tawdry political end.
Before one describes the programme or rather, “cam is more acutely felt in the case of female children due to the
paign”, it is vital to understand the motivating factors behind
problem of difficulty in marriages.. .”
it. The appointment of this particular health minister had
“.. .There is no specific treatment for this disease, that is
been violently opposed even from within her own ruling party why it is extremely important to protect every child by
ranks. Within weeks of her appointment, there were several
immunisation as early as possible”.
moves to oust her for “incompetence” and being for “an
Having chosen her medico-political weapon in March
embarassment to the cabinet”. The Chief Minister apparently
1983, the health minister planned the war with a metiwarned her that she had to do something to effectively silence culousncss which would do credit to a Field Marshal. It was
her opponents or he would have no choice but to replace decided to launch the campaign on May 1, Maharashtra Day,
her. Evidently, a considerable part of the furore over her (ironically, Labour day as well) with maximum fanfare. The
appointment was caused by communal factors, since the planners then worked backwards, systematically plotting and
health minister was a South Indian by birth (though
preparing each step.
domiciled in Maharashtra for over 30 years) and her Bombay
With 30 years’ experience as a family physician the minister
constitutency was also predominantly South India. Yet
knew that if the cafeteria approach would work immunisa
another source of political pressure on the minister was the tion would have to be taken to the dorrstep of every eligible
falling popularity of her party especially among the poor,
family. Existing health manpower in the city was not touched
who had, in the previous elections, voted largely for overtly because their routine duties should not suffer, but
actually because they were unlikely to cooperate and even
Opposition candidates.
Thus it was that the beleaguered health minister had to. if they did, it would not ensure that the credit went to the
find a quick means of securing her own position in the minister’s party and party workers.
Thus a broad spectrum of organisations and institutions
Cabinet as well as improve the party image among the City’s
poor and a means which was within the confines of her port were approached—colleges and schools (whose students were
folio. She hit upon the idea of the “War Against Polio” as promised extra marks in return for their participation),
the proverbial stone which would kill both birds. We shall
“social organisations” (which were by and large communal
see why this was a brilliant choice.
and caste groups interested in “public service”), clubs like
Consider first of all how beautifully polio immunisation
the Lions, Rotary, and Giants, political parties, and associain a image compaign fits the bill:
tioifs of the medical fraternity like the IMA. The Directorate
When asked “Why polio?” the health minister reportedly said of Health Services and the Bombay Municipal Corporation
“other vaccines like triple, the child gets fever. The parents . was asked to provide support services in the form of vehicles
are upset and don’t bring the child back for second dose.■ vaccines and equipment but were otherwise kept on the
Also, these reactions would be used by our opponents to periphery. The All India Institute of Physical Medicine and
spread fear and make the compaign fail. With polio doses, Rehabilitation (AIIPMR) acted as medical advisors to the
we were confident that this would not happfen.”
programme. Even the Bombay Restaurant and Hotel Owners’
“I had to have a programme which would take my party Association was-approached to provide cold-storage facilities
workers into the slums, doing a good community service, to and ice to immunisation teams to maintain the cold chain
improve the image of the party among the poor!’
at the field level. Within a month, not a single source of help
“Another thing—anyone could give polio (sic) because it and support was left untapped. By May 1, some 6000
need not be injected. So with polio, I need not depend on volunteers were standing by.
medical people to help me. I could use our party people and
Meanwhile, the problem of identifying the target areas and
volunteers”.
members was taken up. In consultation with the AIIPMR
Several observers of the programme commented on how it was decided that the campaign should aim to cover only
candid the health minister, was, privately, about her political 0-5 years old living in slums with 3 doses of vaccine. To
52
Radical Journal of Health
determine exactly where and how many, the polio-endemic
identified in a survey conducted by the AIIPMR in 1981 were
superimposed on ward-wise maps of the city. Teams of
student volunteers accompanied by party workers then
fanned out into these areas to survey the number of un
immunised under-5-’s and within weeks delivered the target
figure: 1,00,000 children. This enabled the organisers to
promptly obtain adequate supplies of the vaccine from the
Haffkine Institute.
The campaign plan was now further elaborated and
entrustead to a team of ‘campaign managers’ each with a
specific set of responsibilities: e g, manager-volunteers
(enlistment, deployment, supervision); manager-vaccines
(cold chain maintenance, supply, distribution); manager
publicity (printing, media, etc), manager-transport (com
mandeering, co-ordination, deployment), etc, etc. Each
campaign manager was a trusted party lieutenant of the
minister’s, personally loyal to her. In addition, a “Ward
Chief” (again a trusted party worker) was appointed to'
co-ordinate and supervise all activities at the ward level.
Publicity came next. By early April, thousands of poster,
banners and hand bills were flooding the target areas. Party
workers addressed hundreds of local public meetings to
spread awareness of the campaign and to enlist more
volunteers. But the minister’s coup-dc-etat was undoubtedly
her “padayatra” through the slums accompanied by polioaffected children. In each locality, the crippled child was
made to address the people, appealing to them to immunise
their children and prevent them suffering a similar fate.
Simultaneously, immunisation cards were printed in
thousands to be filled in by the vaccinators and handed over
to the parents as a record, to ensure completion of the doses
and prevent double immunisation of the same child.
The problem of supplying thousands of flasks to the
immunisation teams was solved by asking the volunteers to
bring their own flasks. Hotels ahd restaurants near each
target area were alerted a day before to kep supplies of ice
feady for the teams. The vials were themselves deployed.to
there focal points the day before and kept in their deep
freesers.
An intelligence system was also set up to achieve an
efficient, up-to-the-minute flow of information regarding
immunisations performed (area-wise, dose-wisp), vaccine
supply, member of volunteers and their deployment, and the
transport position. The campaign would start on the first
Sunday of every month (to enable the maximum member
pf volunteers to participate) with mop-up operations for each
bose on the following Sunday.
This is only the bare bones of the campaign’s organisa
tion, since a detailed description would take up a book. But
if is clear that little was left to chance of accident—far too
much was at stake, politically, for any risks to be taken. One
pbserver records that the team-spirit and hardwork put in
by the minister, managers and wardchiefs was most impres
sive; but also very aggressive, as if daring anyone to criticise
pr better their efforts.
• The “War Against Polio” bdgan on May 1, 1983, with the
then Governor of Maharashtra symbolically immunising the
first child from a central city slum at 8 am. By 7 pm some
70,000 immunisations had been performed, or 70 per cent
pf the target figure. The second round was conducted on
September 1986
June 5, with 85,000 doses being administered—60,000 second
doses and 25,000 first doses. By end of July, a total of
I 35,000 0-5 years old had received first doses, 50,000 had
received two doses, and 85,000 children had received all three
doses. Two-thirds of all slum colonies'in the city were
supposed to have been covered under the campaign. This,
of course, is the Gospel according to the health minister’s
cohorts, and is quite open to interpretation, as we shall sec.
Having understood the motivations for the campaign, and
the plan of action, we can now take a closer look at what
actually happened.
As pointed out earlier, virtually none of the considerable
health resources directly under the health minister’s com
mand were utilised in the campaign. The role of the state
Directors of Health Services, for instance, was limited to
ensuring supplies of vaccines and vehicles for transport
(though the latter were apparently withdrawn by the Direc
torate after the first round), printing the publicity material
and forms, and “arranging” meetings (though not attending
them). One Assistant Director of Health Services is reported
to have said: “This is another political tamasha. We are here
always; we have to serve the people and face them through
out. These people come and go, so they have to make a
tamasha while they are in power”. He was also bitter that
the Directorate had been ignored. entirely because the
campaign organisers wanted none of the credit to accrue to
anyone else.
Notwithstanding this, a sizeable number of public health'
service doctors and officers actively participated in the
campaign in their personal capacities. They-were frankly
seeking political favours by associating themselves with the
campaign. One municipal health officer apparently absented
himself from his normal duties for the duration of the
campaign, knowing his superiors could not touch him
without risking political retribution.
As for the much-proclaimed involvement of “voluntary
organisations”, they were conspicuous by their absense. Not
a single secular or progressive grassroots agency working in
the slums was approached to assist the campaign, despite
their initimate knowledge of the. local people and their
extensive networks. The health minister was dismissive about
this, telling an observer “They have done nothing all these
years. If they had, we would not have to do this now”. An
aide was evidently more blunt: “We approached mainly the
South India social organisations; we ourselves being South
Indian, we felt that they would give a better response. The
North Indian organisations we approached did not takemuch interest. But on the whole, very few of these organisa
tions have done very much... That is why we are relying
mostly on our own party workers.” In response to why they
did not involve grassroots agencies working in slums, the
same aide reportedly said, “Why should we ask them? We
wanted to show what (our) party could give the people—
and have succeeded. Why should someone else take the
credit? Can they run the country?” The defence rests.
The poor involvement of medical organisations, parti
cularly IMA members, was interesting. This was apparently
because several leading paediatricians advised the health
minister not to launch the campaign in May, since epjdemiologically this is a peak period for poliomyelitis. 'Mass
immunisation at this time could, in their opinion, actually
53
increase the incidence of the disease. Other members sheered
at the whole campaign as a political tamasha with which they
had no wish to associate. The organisers, however, ascribed
a different motive to the attitude of the private practitioners:
that they couldn’t care less about the slum dwellers.
Let us now turn from the medical fraternity to the legion
of volunteers (mostly college .students) mobilised into
vaccination teams. These were the “front-line” of the
campaign and therefore vital to this success. It is shocking
in the extreme therefore that a campaign in which so much
detailed planning and preparation went into every aspect,
no one bothered about training the volunteers for their tasks.
On the morning of each of the campaign days, hundreds
of student volunteers would be milling around the health
minister’s residence, without a clue as to why or what they
were there for. The majority did not know, until they were
actually taken to the sites, that they were to perform
immunisations, much less which vaccine was involved. To
ask if they were aware of polio, and the concept and
importance of the cold chain, was an exercise in futility. One
journalist got the following response from scores of students
when he asked them if they knew what they were going to
do that day: “They said they would explain everything when
we reached the place. They haven’t told us anything. The
college also said these people would tell us what to do”.
One eye-witness reported that the entire gamut of infor
mation to the volunteers—from maintenance of the cold
chain (“Keep the vial in the flask. After you. open it keep
it in the saucer with ice”), how to measure and administer
each dose, what questions to ask the parents, and some
contra-indications—was packed into a five-minute lecture at
the entrance to the slum, before the teams were give their
vials and told to fan out. The claim made by the organisers
that each team was accompanied by a doctor, nurse, medical
student or student nurse was more fantasy then reality.
Qualified observers who accompanied the teams were
horrified at the repeated breaks in the cold chain, and the
administration of the vaccine to children with several contra
indications. For example, unopened vials of the vaccine were
carried in handbags (not in flasks) for hours together in 38°
C.temperature (May being the hottest month of the year);
opened vials were exposed to sunlight for nearly an hour,
with all the ice around it melted away, and then the same
vial used to “immunise” more children; infants with-coughs,
colds, diarrohoeas were immunised; infants were breast-fed
within seconds of swallowing the vaccine. This bizarre
scenario was compounded by the fact that the same
.volunteers were rarely present at the next round of the
programme. The high turnover of volunteers ensured that
each round was as bad as the previous one. No one thought
it worthwhile to train these volunteers in even basic pro
cedures to ensure cold-chain maintenance and effective
immunisation. But then, this was not really the objective of
the exercise.
The-real objective of the campaign was well achieved, in
the words of one aide: “Our party workers are acompanying every vaccination team to tell the people that this service
is coming from the. (name of the party). I am confident that
in the next election, these sections will vote for
our.', .candidate—these shims will be behind our party from
now on”. One consultant observing the programme con
54
firmed this: “In two slums 1 visited, I asked whether polio
vaccine had been provided by the government. The answer
was “No, not by government—by party”.
Let us now examine the role played by the medical advisory
institution which was assisting the campaign as the.r
technical watchdogs. Far from watching, they followed a
“see-hear-speak no evil” policy which destroyed any chance
of this politically-motivated campaign achieving some social
good. Either the Director of the Institute or a senior associate
was present on all the campaign days. But while they
admitted their fears about the programme in private, they
were far too intimidated by the presence of political power
to do so publicity, not even directly to the health minister
and her aides. They simply joined the ranks of yes-men
surrounding any politician—rendering the Hippocratic oath
into a hypocritical one.
What about the people themselves? If reports of the cam
paign arexto be believed, they were far too wise to reject any
gratuitous offering, even though few knew what it was. The
vast majority of mothers when asked, had no idea that their
children had received a vaccine against polio, thinking it was
against tuberculosis, measles, smallpox, or tetanus-but none
refused. This was simply because in most slums, no one had
actually seen a polio-affected child (except in the padayatra)
and those who had could not see the connection between
the physical disability of a 7 year-old and the pink drops
given to the 7-month-old. This is not surprising in view of
the fact that the AIIPHR survey itself had found the
incidence of poliomyelities to be highest in the lower middle
class group and not among slum dwellers. The publicity cam
paign which the organisers had designed to “create an
awareness” was clearly aimed at an awareness of things other
than the causes, symptoms, effects and prevention of polio.
As for actual coverage, there was considerable evidence
that the elaborate system worked out by the organisers for
“initial attack” and “mop-up” phases broke down rapidly
under the sheer weight of the tamasha being enacted upon
it: entire pockets of “target” slufns had not been touched—
the teams had covered the peripheries and left; more often,
people complained that one round had been completed with
the promise to return next month, and the teams were never
seen again; in other areas, two rounds had been done before
the disappearing act; in some of the poorest areas, cynical
parents told a visiting observer “May be them came-may be
they didn’t. How do we know? Why should we care?”.
Consequently, experts who closely monitored the cam
paign feel that not more than 25 per cent of target children
actually received three doses of vaccine, and that under the
prevailing conditions, only about half of these were
effectively protected against polio.
However high our eyebrows rise, the fact that the health
minister retained her place in the cabinet-for the duration
of that particular ministry, at any rate-is now history. Heady
with the “success” of the “War Against Polio”, she quickly
abandoned the campaign to her lieutenants to complete as
best they could, and moved on to new pastures: viz a “War
Against Leprosy”. But for the battle-weary poor, one question
remains: Will the wars against them ever cease? Q
Asha Vohuman
C/o Radical Journal of Health
Radical Journal of Health
Programming Reproduction?
Maternal Health Services
manisha gupte
In the absence of a basic questioning of women's status and role in society, birth control, abortions and even
maternal health care end up merely replacing an old set of traditions with new ones. Do maternal and child health
services as they exist today have the potential to emancipate or to further bind a woman to her traditional role
albeit in subtler ways? The article contends that the entire primary health programme reflects social attitudes
towards women, viewing them primarily as mothers or as potential mothers.
even in the face of unmasked oppression. Separation and
IT is no more a disputed fact that working class women
consequently living single or with the children and without
participate in production with men and that like the latter
a man, often means a drastic drop in the standard of living
are alienated from the means of production. What makes
for women, if not abject impoverishment.
their position still worse is that women participate more
With enforced backwardness, it is also easy to push women
actively in reproduction than men do and yet unfortunately
out of the labour force more easily than it is to push men
the former are alienated from the means of reproduction as
out, be it due to automation, unemployment or the omni
well. Juliet Mitchell argues that as in capitalist production
present and omnipotent reproductive duties. Women thus
the social product is confiscated by capital, so is the child
become a reserve army which will work at half pay and who
snatched away from a woman (Mitchell, 1966). Not strictly
will be reabsorbed by the family if there is unemployment
speaking, perhaps so. In patriarchial society, the child, a
(Rowbotham, 1973). Underpaid outdoor work, invisible
result of physiological and emotional interaction is seen as
property, and male property at that. Concepts of illegitimacy
domestic labour and conjugal duties therefore leave a woman
and patriarchial lineage are examples. A child, created so
vulnerable to be doubly exploited. Unfortunately, though the
actively by a woman, grows up in a capitalist and sexist
condition of working class women is ideal for the creation
milieu, and alienation occurs through the conditioning and
of a powerful political force, their realisation of exploita
values that she or he absorbs since infancy. Physical aliena tion dissipates instead of being sharpened. The shunting from
tion does not usually occur because both women and children
reproduction to production and back to reproduction acts
are conditioned socially not to question or to rebel inside
as a safety valve to smoothen conflict.
the family. When women do so, physical alienation too does
The changing role of the family also determines the
occur in the form of custody in divorce, since custody is more reproductive potential of the woman. The family in turn is
often than not in favour of the male.
governed by historical inevitability, market compulsions and
The changing role of the family further determines the often by the prevailing political will where reproduction is
newer roles that a woman performs within and outside the concerned. In peasant households with .considerable land
family. The institution of marriage too on the exterior holdings it might be desirable to have as many extra pairs
becomes rather destabilised, say for example through a of hands as possible; similar may be the case in not so
divorce or through voluntary rejection of marriage by a advanced capitalism, where the quantity of workers needs
sexually involved couple. However, the psychological and to be maintained at a high level so that their exploitation
sociological functions and grip of the family remains the through underpayment is possible. With the decline of
same—it creates the ‘masculine’ and the ‘feminine’, resulting labour-intensive industry and with the emergence of capitalin a ‘man’s world’ and a ‘woman’s world*. It also conditions intensive industrialisation however, the main economic task.
the newly born infant to accept and appreciate the ‘security of the family would no longer be to produce a large number
and stability’ that the bourgeois family has to offer.
‘of children, since then quality rather than quantity would
The prescribed role model of the husband-wife-child deter be important in the labour market (Morton Peggy, quoted
mines and influences the roles that men and women perform in Mitchell, 1966). The family adapts itself accordingly, and
within and outside the family. As a vivid example, one may in turn monitors the reproductive ability of the woman to
quote the doctor-nurse-patient relationship being analogous suit the requirements of the contemporary wage market.
to the earlier mentioned hierarchal familial triangle. Looking
The woman in question therefore, is only seemingly
deeper, these role models by virtue of their predecided status liberated to become a wage earner. In truth, however she
determine the extent of food, health facilities, education and holds no real power in either structure; in fact forces that
employment opportunities that men and women will receive are alien, incomprehensible and beyond her control monitor
in relation to each other. Therefore, even though women do her, both inside and outside the family. In the existing
enter the production force with vigour and corppulsidn, they context, birth control, abortions or even good- maternal
inevitably land up doing jobs that are qualitatively and thus health care, in the absence of the* basic questioning of a
economically inferior to those performed by men.
woman’s role in society, end up merely replacing an old set
The wage system continues to be structured according to of traditions with new ones. Not only does the woman
the assumption that a wornan’s wage is only supplementary.
perform the necessary functions that the traditional orthodox
Women are thus seen as economic attachments to men, not set up demands from her, but she also faces the ‘consequence*
as free labourers who participate equally (Rowbotham, 1973).
of being the modern, sexually liberated bohemian woman.
Women are thus financially compelled to stay with their men
It is in the light of this framework that we have to view
September 1986
55
the ideology of maternal and child health (MCH) services;
whether they do liberate a woman even marginally, say from
the risk of maternal and child mortality, whether a healthy
pregnancy and childbirth coupled with birth spacing gives
her more choice and more control over her body or whether
the existing MCH programme in form and in content, ends
up merely making her a more healthy and well programmed
baby making machine. In short, whether MCH as it exists
today has the potential to emancipate or to further bind a
woman to her traditional role, albeit in subtler ways, calls
for examination.
MCH: Sexist Bias in Planning
total workload, the daily and seasonal patterni of
access to health care and so on. Neither are p
. .
affect women more severely, such as maln°“r'sh"’®"‘;
anaemia and occupational hazards, or t osc
,
women specifically, such as abortion or spouse abuse
considered (ibid).
,
. , ..
MCH activities, in an informal manner, began in Ind a
around the turn of the nineteenth century: mostly voluntary
efforts ranging from enrolling women students in medical
colleges to training of midwives and Lady Health Visitors.
The first transition of the official control over voluntary
direction in MCH came in 1938. In 1953, following the
introduction of training courses for Auxiliary Nurse
Midwives (ANMs) and public health nurses, most voluntary
health schools closed down (Sethna, 1978).
The Indian government’s official MCH package includes
the antenatal, perinatal and postnatal care, the Integrated
Child Development Scheme (ICDS), the National Pro
gramme for Control of Blindness, the Programme for
Control of Diarrhoeal diseases and Family Planning.
There exists undoubtedly a role, however limited, that
MCH can play in a woman’s and child’s life, provided it is
universally available and is of high quality. However, in the
absence of a woman’s control over her own reproduction,
a culturally and socially conditioned inability within her to
be able to vocalise her gynaecological problems to a health
worker, especially male, and the latter’s reluctance to bridge
the communication gap by demystifying pregnancy, make the
MCH a watered down programme, reduced to a mechanical
distribution of iron-folic acid tablets, a mindless target
oriented approach towards immunisations and endless
weighing of children to identify the ‘at risk’ individuals in
an already malnourished population.
In a patriarchial world, it is no great surprise that male
hegemony would exist in all aspects of health care—at the
policy level, at the implementation stage and throughout the
delivery of this care. Women as a group therefore have to
receive health care that is designed in their own favour.
Effective health care, provided free of cost and which is
accessible to all, especially to women during pregnancy,
delivery and the post partum period should be considered
a fundamental right. We must fight to see that no woman
or child is at the risk of dying, especially during those crucial
months. But we must also emphasise that mere MCH will
not do. Motherhood is only one of the roles that a woman
may voluntarily wish to perform during her lifetime. She may
accept it or reject it and in spite of opting out of motherhood
or marriage she is a full human being. Health services must
be available to women irrespective of their childbearing role.
The entire primary health programme reflects social
attitudes towards women, viewing them primarily as mothers
or as potential mothers; in fact health services for women
have been termed as MCH services (ICSSR/ICMR, 1981).
The same report notes that there is positive evidence to
The lack of control over one’s own body is experienced
conclude that the health status of Indian women has declined by many women in the clinic approach to pregnancy and
over the past thirty five years in spite of improved MCH childbirth. Most often, questions that bother a woman deeply
programmes, mainly due to the fact that women are more remain unasked. The concept that pregnant women should
‘at risk’ nutritionally and yet that they utilise health services swallow tablets or receive injections for their own benefit
less than men do. They are of interest to the health services without any active partcipation from their own end reveals
only when.they conceive or when they have reached the upper the ambiguity and myth of ‘people’s participation’ so loftily
limit of child bearing permitted by the government’s family considered the basis of the Family Welfare programme in
planning (FP) programme.
India. In fact, passivity is a fundamental feature of the
The infant mortality rates too are highly unflattering relationship between the providers and users of maternity
(114 per 1000 live births in 1980 as compared to 129 in 1971) services (Graham and Oakley, 1981).
and there has been no appreciable improvement in the
Growth charting, accepted so enthusiastically by our
nutritional level of children, in spite of programmes directed health care system is yet another instance of mystification.
towards them, neither has primary education become When less than ten percent of under five children in deprived
universal.
sections are nutritionally normal, expensive growth monitor
To shift resources towards women as a group, it is necessary ing is unnecessary. If 50 per-cent of underfives in India
for policy makers to be firstly convinced that women con (amounting to 55 million children) were to be covered
tribute greatly towards world production—within the family, through growth monitoring charts, this activity of weighing
in the agricultural sector, in traditional as well as modern and charting alone would require 110,000 workers annually
sector industries and also in commerce. An estimate of 18-30 and would incur an expenditure of US $ 27.5 millions for
per cent of the world’s families are solely supported by salaries, $ 20.0 million for Salter scales (one per 100 under
women, while in many others the woman’s financial con fives) and additional expenditure for repairs, replacements
tribution is a substantial component (Wayne, 1985). Statistics maintenance, transport and new growth charts (Gopalan and
unfortunately miss family and informal sector activities, Chatterjee, 1985).
resulting in this contribution to the overlooked. Within the
Such luxurious and unnecessary activity in fact detracts
health care system, factors that contribute towards women’s from motivational and educational work which is of nrimarv
ill health are not considered—their socio-economic status, importance in child health and nutrition programmes
56
Radical Journal of Health
(Snlatha, 1984). In a country with limited resources for child
care, a social g>oup that faces a high risk of nutritional
problems needs to be identified and standard intervention
is necessary to all their members (Nabarro, 1984).
MCH and Population Control
. The scope of the already small package of MCH services
is urther reduced by making it a screen to achieve family
planning targets. There is constant talk of ‘integration of
MCH and FP’ and under this euphemistic slogan, a cur
riculum for undergraduate students of medicine and interns
has been prepared by an expert committee. The training pro
gramme has already been adopted by three teaching colleges.
In one year, three courses were conducted, which nine teams
of twentyseven professors attended (GOI, 1985, p 125).
In the minds of policy makers, MCH figures not as an
independent programme but as a means to reduce fertility.
The Annual Report (1984-85) of the Ministry of Health and
Family Welfare (MHFW) states that ‘to reach a couple pro
tection rate (CPR) of 60.0 per cent of eligible couples by 2000
AD, it is essential that the younger group of eligible couples
be motivated to accept spacing and the small family norm
... Moreover, use of spacing methods ... has a significant
impact not only on curbing the population growth, but also
on the health of the mother and chilcT (p 116).
The Ministry’s own assessment states that the crude birth
rate (CBR) at the end of 1984 should have been 32.6 per 1000
population, whereas actually it was slightly higher—33.6.
Whereas 29.4 per cent of couples were ‘protected’ by the end
of 1984 (sterilisations accounted for 23.7 per cent of these),
a CPR of 60.0 per cent is desired by the turn of the century;
To give the FP programme a boost, especially in backward
areas, partial assistance from DANIDA, ODA(UK), UNFPA,
USAID and the World Bank has been received to cover 63
districts in 14 states as ‘Area Projects’ for intensive develop
ment of health and family welfare. ‘The objectives are
reduction of fertility and reduction of maternal and child
mortality’ (GOI, 1985, p 150).
The government has introduced the concept of Net
Reproduction Rate Unity (NRR-1) in its FW programme ...
“after considerable experience in this regard (need to control
population growth), the country has set before itself the long
term demographic goal of achieving NRR unity by 2000 AD,
with a birth rate of 21.0, death rate of 9.0 (life expectancy
at birth being 64.0 years) and infant mortality rate less than
60.0. In order to achieve this goal, the National FW
programme has been and will be strengthened. It is a
voluntary programme ..(GOI, 1985, p 164).
In the context of these new goals'set by the Indian govern
ment, the stranglehold of FP over MCH can be fully
understood. In fact, the first UN Advisory Mission, as early
as 1966 had gone as far as to insist that ANMs should be
‘relieved from other responsibilities .such as MCH and
nutrition’ so as to concentrate efforts on FP. This mission
stated that “This recommendation is reinforced by the fear
that the (FP) programme may be otherwise used in some
states to expand the much needed and neglected maternal
and child welfare services” (UN Advisory Mission, 1966).
The first double-edged tool within the FP programme
came in the form of the Medical Termination of Pregnancies
(MTP) Act in the early seventies. Regarded by feminists as
September 1986
a mucn-desired means to control one’s fertility, the legalisa
tion of abortions is in itself welcome. However, the govern
ment’s interest in this legalisation becomes clear when one
notes that by the end of March 1984, in all 4,553 institutions
were rendering MTP services as compared to 4,170 at the
end of March 1983. In Bombay city alone, 50,000 MTPs are
registered annually (Karkal, 1984).
The official acceptance of NRR-1 by the government is
especially sinister because in lay person’s terms it spells that
only one daughter should replace her mother. Thus female
foeticide through sex determination (amniocentesis,
chorionic villi biopsy) or through sex pre-selection (Ericsson,
Japanese method) is inbuilt within the government’s popula
tion control (PC) policy.
The government’s emphasis on ‘child survival’ rings
another ominous bell. Welcome in itself, the slogan is reduced
to ‘spacing methods’. The earlier mentioned Report of the
MHFW states that “since child survival is amongst the
foremost factors which induce the couple to adopt the two
child norm, MCH programme has been given due im
portance.” The strategy becomes clearer when along with the
slogan of ‘child survival’, the government has markedly
increased its budget for FP in the Seventh Five Year Plan
period and the emphasis will now be on spacing methods
for women. It is estimated that by 1990, spacing methods
will account for 20.0 per cent of ‘protected’ couples against
the present level of 5.5 per cent. A Contraceptive Marketing
Organisation has been registered to promote spacing methods
(GOI, 1985; p. 107).
The government now admits that one-third of all lUCDs
ever inserted are removed and one fifth are expelled. The
officially accepted dropout rate for lUCDs therefore is 53.3
per cent (GOI, 1986). Naturally, the proponents of popula
tion control would be desperate to design a centralised and
foolproof system that leaves little or no control in the
women’s hands to withdraw the contraceptive and it is in this
context that the importance of injectable contraceptives (ICs)
or implants should be understood. Though ICs as yet do not
form a fcart of the FP programme, a Programme-introduc
tory Study on ICs (Net-En) at PHCs attached to 15 medical
colleges is underway. Based on the results of this pilot project
it is hoped to introduce this spacing method soon. In fact,
according to official plans it was to b^ introduced in 1984-85.
The ICMR is also conducting its sti ’ies with Norplant—
an implant for women. An appropriai version of this contra
ceptive was to be available by the ei of 1985 to start the
programme introduction studies aH th PHCs (GOI, 1985;
p.107).
It has been decided to intitiate a two million corps of
women trained to motivate for FP. These corps will be
nonpaid and interestingly, acceptors of FP methods them
selves. Another significant move by the government in the
near future is to disband all male community health
volunteers. Through the IUCD programme, it has been learnt
that male motivators cannot do the job where spacing
methods are concerned. Male health workers have experien
ced embarrassing consequences while having to explain
Copper-T insertions to a woman or to her husband. To close
all loopholes therefore women motivators exclusively would
approach women targets henceforth.
57
Motivation: Distortion of Human Relationships
The state’s emphasis on women targets and women
motivators is a cause of feminist concern for the distortion
of human relations which the coercive, target-oriented
campaign brings along. When motivators are women, be they
the health staff or primary school teachers, they are con
stantly threatened with dire consequence such as job
transfers, sexual harassment, humiliation and delayed salaries
it they fail to fulfil their targets. The dangerous limits are
reached when these women are the major or only source of
livelihood for their families, when they are single, living in
an alien village and are unable to complete targets. Recently,
in March 1986, Manda Padwal, a female health functionary
(an ANM) in Talasari PHC of Thane district committed
suicide after reprimand and order from the doctor in charge
to sterilise twenty tribals (Barse, 1986).
These women, with the proverbial sword hanging over their
heads, are forced to_see every other woman in the village as
a potential target. All their conservation, whether at the
doorstep or at the village well, invariably ends with motiva
tion for FP. Little surprising therefore that the village women
resent these motivators and consider them as scheming nags.
The entire fabric of woman-to-woman relationships is eroded
• in this situation, with each party outsmarting the other
whenever possible and harbouring deep rooted resentment
mutually.
This distortion of basic human relations and support
systems has dangerous political consequences. Sexist bias,
international conspiracy and the government’s population
control policy are responsible for the inhuman family plan
ning campaign. Targets are planned outside the micro
environment in which the masses live Dangerous contracep
tives are dumped by ruthless, profit-hungry multinationals.
Yet, all of these are invisible to the rural working class.
The only visible oppressor they see is a poor ANM like
Manda Padwal; most often the latter being from their own
class and a victim of the present system as well. Therefore,
the anger directed towards another helpless victim helps the
ruling class through a divide and rule strategy. Not only does
it break working class solidarity, but it also diverts the issues,
allowing the real enemy to escape without confrontation. It
makes the rulers seem like paternal and benevolent Caliphs
out of the Arabian Nights.
As regards the delivery of health services, the ‘integration’
of FP with primary health care has in fact had an adverse
effect on the utilisation of health care at PHCs. A substantial
majority of the rural population utilises the private practi
tioner in times of illness and the major reason for non
utilisation of government, services is the absurd emphasis of
the latter on family planning. Women still prefer to be
delivered at home by traditional dais or relatives, one reason
being that any perinatal or postpartum contact with a woman
is immediately seized for target completion in a PHC.
Immunisation camps suffer because covertly many such
camps are used to gather young mothers for Copper—T
insertions.
The overshadow of the population control programme
over all other essential public health services is resented by
people and results in poor utilisation of all these basic
services. It is angering that ptibljc-bcallii services, especially
maternal and child services are used as a bait to lure people
towards reducing population growth, without any considera
tion for the existing socio-economic conditions, the help essness and the inability of the oppressed sections to rebel. In
fact coercion thrives on these very conditions, and it is only
a conscious, organised working class that can focus on con
tradictions, unearth the intricate conspiracies and then
demand that the health services be geared in their own favour.
The conspiracy of the ruling class and the inhuman
strategies employed by them, often in sugar-coated pills such
as maternal and child health or as emancipation through
birth control, works to control the'lives of already exploited
populations. Patriarchy, which has the art of adapting itself
it/mew situations, in fact of moulding new situations to suit
its end, prevails in policy making research, medicine and
science. Our own demands, be they of safe deliveries, of our
children’s survival and their well being, or birth control, of
abortions and the like are snatched away from us and given
back to us blunted and decolourised.
Under the guise of giving us the choice, we are made
spectators of our own oppression, be it through dangerous
contraception, female foeticide, sex selection, surrogate
motherhood or the perpetual tight rope walk where our
productive and reproductive duties are concerned. It is
therefofe, necessary to constantly expose this design and to
build a strong women’s movement that attacks both class
and patriarchial control over the various institutions that
govern our lives. We have to relate the personal to the political
and should constantly question our role as women within
and outside the family.
References
Barse, Sheela: The Afternoon Despatch and Courier, April 21, 1986.
Gopafan C and Meera Chatterjee: Use of growth charts for promoting
child nutrition: A Review of Global Experience, Nutrition Founda
tion of India, 1985.
Government of India: Ministry of Health and Family Welfare, Annual
Report, 1984-85, 1985.
Government of India: Evaluation Report on Family Planning Pro
gramme, Planning Commission, p. 173, 1986.
Graham Hilary and Ann Oakley: “Competing ideologies of reproduc
tion: Medical and maternal perspectives on pregnancy” in Women,
Health and Reporduction, (Ed. Helen Roberts), pp. 50-74, Routledge
and Kegan Paul, London, 1981.
Indian Council of Social Science Research (ICSSR) and Indian Council
of Medical Research (ICMR): Health For All: An Alternative
V f 7 J5>; PP’„3 ' 40; Indlan lnslituIe of Education, 1981.
Karkal, Mahm, Personal communication, 1984
Mitchells Ju'iet: Women's Estate. 1966 (Penguin Books. 1971).
Morton, Peggy: Quoted in above.
7
Naharro David: (1984) Quoted in Gopalan and Chatterjee. 1985.
Books3,mi973.el a: °mon's Co^ciousness. Man's World, Penguin
^st’ituieo"^^^
"’“la. All India
i r •,
» Hygiene and Public Health, Calcutta 1978
“ a"nd Famil?Pli5'°n-(,96<* Qu°'«» m B9nerji Debabar,
N^ Delh” 1985
.
V. Srilatha: Nutrition Foundation nf inri>e> ivaWayne, Stinson: Salubritas, Vol 8 No 2 An^H
1984>
by the American
aLL-.•
2’ Apr,,Junc 1985, (Published
A^soclatiwis)*030
^SS°C,at,On and World Federation of PH
Manislia Gupte
58
Radical Journal of Health
The Holistic Alternative to Scientific Medicine
History and Analysis
Howard s berliner and j warren salmon
The resurgence of the holistic health movement in the US in the 1970s can in part be attributed to increasing)
consumer dissatisfaction with the present system of medical care delivery. This article traces the rise and decline
of modern medicine and the concept of public health by analysing the assumption of hegemony by scientific
medicine and its practitioners. Then it describes the challenges that holistic medicine's theories and therapies cur
rently pose to scientific medicine's organisational form and practical content. Holistic medicine is assessed in
terms of its organisational and conceptual basis, and the relationship between haTstic medicine and the needs
of advanced capitalist society is discussed. The article is reprinted in a slightly editedform from the International
Journal of Health Services, 10: 1, 1980.
IN an era of concern over the costs of medical care and
disarray in the health-care delivery system, the rise oh a
countertendfcncy centering on a quest for health deserves
attention. A resurgence in the healing arts, manifested
through a diverse collection of “holistic health practices,” is
underway in the United States and Western Europe (1).
Movements and theories such as humanistic medicine,
transpersonal psychology, parapsychology, folk medicine,
herbalism, nutritional therapies, homeopathy, yoga, massage,
mediation, and the martial arts have spread widely over the
last five years (see for example, reference 2-6). (See also
reference 7 and 8).
To grasp the complexity of the emergence of this move
ment as a social phenomenon today, it is necessary to explore
the historical and theoretical dimensions of both the holistic
tradition itself as well as the tradition to which i: is now in
opposition. We begin by describing how the rise of scien
tific medicine in the late 19th century led to the demise of
a'prior holistic understanding of health and medicine. Next,
we relate the re-emergence of holistic health thought to the
broader economic crisis that currently confronts
technologically based forms of medicine, as well as to the
inability of Western medicine to adequately address the
health problems of advanced societies (see refs 9, 10, 11).
Medical Theories and the Rise of Capitalism
In early to mid-19th century Europe, two different theories
arose to explain the nature of origin of disease. The first,
known as contagionism, postulated that some disease were
contagious, spreading via commerce and population migra
tion. the strategic consequence was the quarantine, and the
system of quarantine enforcement was intended to shut down
commerce and trade to keep disease away from non-infected
areas. The second theory, known as anticontagionism,
postulated that disease instead resulted from local sources
and arouse out of “miasmas” —clouds of rotting matter and
filth activated by certain meteorological conditions. The prac
tical outcome of this story was to leave ports and commerce
alone, and to eliminate filth and swamps in the disease-laden
areas. What makes these previous medical theories of more
than marginal interest is their direct association With distinct
political perspectives. As Ackerknecht point out (12):
Contagionism was not a mere theoretical or even medical problem.
Contagionism had found its material expression in the quarantines
and their bureaucracy, and the whole discussion was thus never a
discussion on contagion alone, but always on contagion and quaran
tines. Quarantines meant, to the rapidly growing class of merchants
September 1986
and industrialists, a source of losses, a limitation
expansion, a
weapon of bureaucratic control that it was no longer wilA-g to tolerate,
and thjs class was quite naturally with its press ana deputies, its
material, moral, and political resources behind those who showed that
the scientific foundations of quarantine were naught, and who anyhow
were usually sons of this class. Contagionism would, through its
associations with the old bureaucratic powers, be suspect to all liberals,
trying to reduce state interference to a minimum. Anlicontagionists
were thus not simply scientists, they were reformers, fighting for the
freedom of the individual and commerce against the shackles of
despotism and reaction.
The high point of anticontagionism occured just before the
political revolutions of 1848. It lost its strength in tne wake
of the subsequent reaction, while contagionism remained
dominant untill its reformation into germ theory in the 1870s.
The leaders of the contagionist movement, primarily hi?hranking royal military or naval physicians, were politically
unified. The anlicontagionists were split between liberals ana
radicals. Opposing quarantine and state bureaucracy, the
liberals favoured sanitary reform by cleaning up filth, puri
fying drining water, and controlling refuse disposal as solu
tions to disease eradication. This position attributed disease
to a primarily biological condition: the miasma. The radicals
instead saw disease (and the miasma) as arising from broader
social conditions: the poverty, filth, malnutrition, and
oppression bred by nascent capitalism. The liberal position,
typified in Britain by Edwin Chadwick’s report of 1842,
recommended environmental and sanitary reforms that left
untouched the production system and its social relations
(13-15). On the other hand, the radical position, as typified
by Friedrich Engels’s The Condition of the Working Class
in England in 1844 (16), fully implicated the developing
capitalist system and its class relations for disease, as well
as for the class-related incidence and distribution of
morbidity (17).
In France and Germany, radical anticontagionists formu
lated “social medicine”, the core of which maintained that
resistance to disease was not purely biological but depended
on class and social position (18, 19). This orientation implied
that the human body could resist or become more susceptible
to disease, and that prevention of disease was possible
through adjustments or change in the social structure. Thus,
in reporting on a typhus epidemic in 1948, Rudolf Virchow,
a social medicine physican (and founder of pathology in his
later years), called for measures such as free public education,
separation of church and state, higher wages, progressive tax
ation, cultural autonomy for national minorities, agricultural
collectivies, and full employment (20). With the defeat of the
59
revolutions of 1848 in Europe, social medicine was virtually
obliterated. As the anticontagionists lost power and prestige,
contagioniss*’ was revived as the leading medical theory.
Nevertheless, anticontagionism had lefts its mark, and the
movement of sanitary reform went forward from England
to other European countries and America. Between the late
1840s and the 1880s, centralised water supplies, sewage
systems, ventilated housing, and improvements in factory
construction were all introduced (21). Health standards began
to improve. Better transportation between town and country
enabled larger quantities of fresh food to reach people. Im
proved standards of living resulted from successful efforts
to gain higher wages and from the general deflation in
Europe due to lower production costs (22). Death rates began
.tQxp’ummet. Not ony did sanitary reform improve health
status, but it had secondary benefits for capital as well. Cen
tralised water supplies, for instance, removed locational
dependence upon rivers, fostering industrialisation. More
over, water supplies allowed for the design of effective fire
fighting techniques that could reduce the unplanned destruc
tion of capital and lower fire insurance costs. The sanitary
movement also assisted in the creation of new industries such
as refuse disposal; by the end of the 19th century, trash had
become private property—and was collected only when one
paid (23). That sanitary reform was controlled by the
bourgeoisie meant that it emphasised benefits to capital more
than to other social groups. Although far removed from
revolutionary class struggles, it was nonetheless progressive.
While the sanitary revolution, as it is called, was pro
ceeding, medical theory was being greatly influenced by
technical developments which allowed the visualisation of
bacteria. The germ theory of disease emerged in France and
Germany during the 1870s and 1880s and became the means
for constructing new conceptions of disease and health—
conceptions that are still maintained with slight alterations
today under the rubric of “scientific medicine.”(22)
Germ theory and the theory of specific etiology (single
cause of disease) served as the basis for a total transforma
tion of medicine. When germ theory produced its first prac
tical success (vaccines for cholera, rabies, diphtheria, an
thrax), popular acclaim mounted. As these discoveries were
being made, death rates throughout Europe were falling
dramatically, to an extent that was publicly noticeable. Yet,
ironically, this decline in death rates was erroneously attri
buted to germ theory advances, rather than to the sanitary
reforms and higher living standards that had actually caused
the decline. Studies of death rates for virtually all infectious
diseases show them declining precipitously after the intro
duction of sanitary measures, and well before specific
therapeutic interventions occurred (25). Nevertheless, scien
tific medicine took the credit. The end result was the reifica
tion of germ theory, which came to be employed as a total
expansion, rather than as a theory that could explain some
things—but not everything—about disease. Environmental
and social factors were no longer considered very relevant
to the understanding or causation of disease.
Implications of the Imposition of Germ Theory
Gem theory and the concept of specific etiology were
tremendously progressive steps for the development of
medicine. Although scientists at the time exaggerated the im60
portancc of specific etiology and neglected much previous
knowledge about infectious diseases, the importance of these
advances cannot be doubted. Germ theory was deeply in
fluenced by the social context in which it developed. The
growing strength of the labour movement in Europe, as well
as in America, had helped to focus attention on health
hazards'in the workplace, but germ theory s placement of
blame for most sickness and disease on microorganisms
served to exculpate industry for responsibility. Scientific
medicine, as opposed to the social medicine of the 1840s
tended to focus ori the b.ological problems of the individual
in order to understand and treat most diseases. The diagnosis
of illness was made o.a an individual basis and treatment or
therapy was .also individually prescribed.
There are serious problems with this approach, which still
dominates contemporary medicine. The physician deals with
an individual patient (already a socially determined process)
(27). The patient is not an abstract being, but of a certain
age, sex, race, and clsss, and has internalised a specific
historical experience from childhood to adulthood (28, 29).
The taking of a purely medical history individuates the
patient; however the disease or injury from which the patient
is suffering is received as part of a collective experience in
a particular historical, cultural, and social setting. These
latter circumstances are as much a part of the cause, and
should be part of the treatment, as are purely medical facts.
(The medical facts themselves are social-historical facts.)
Thus the essence of scientific medicine’s treatment of disease
discourages a proper understanding of disease by excluding
from consideration the most relevant internalisation of the
external world by the patient. As WartoTsky (30) puts it:
“Human ontology cannot be reduced to an asocial or
ahistorical biology without doing violence to the very
specificity of human biological structure and function itself!’
By abstracting disease from its social framework and
reducing it to the biological sphere, social conditions could
be and were ignored. Scientific medicine became consistent
with, and indeed legitimated, capitalist development by inte
grating a model of healing with the social structure; in so
doing, scientific medicine has obscured the relationship
between disease and the form of social development. Today
heart disease, cancer, and auto accidents are posited as
“diseases of civilisation.”(31). They are conceived of as
necessary consequence of economic growth and indus
trialism, when it is uncertain that this is so (32).
The greatest decline in the death rate has come from the
reduction in infant mortality, attributable mostly to public
health measures and not to medical advances. Life expec
tancy has increased in the United States only when the reduc
tion of infant mortality is included in the statistics—in other
words, a man of 60 in 1900 had virtuall/the same remaining
life expectancy as a man of 60 today (33). Despite the fact
the expenditures for medical care now constitute almost 10
per cent of the Gross National Product in the United States
and are growing at a rate almost twice that of the rest of
the economy, it is not at all clear that health is improving.
Medicine is largely ineffective against the leading causes of
death for those under 45 (accident, suicide, and homicide)
as well as those over 45 (heart disease, cancer, and stroke)
not so much because the biological origin (if any) of these
problems is misunderstood as that their social aspects have
Radical Journal of Health
been relatively unexplored and unincorprated into medical
arc in some sense so complicated and so multifactorial, as the term
goes, that they have something to do with the stress and pace of
practice.
modern living—that we can’t do anything about them until society
Success in finding specific causative agents for infectious
itself is remade... I simply can't take that point of view yerv
diseases led to a particular understanding of causation: the
seriously—not as long as we are as ignorant about the mechanisms
view that a specific biological agent was responsible for a
of those diseases as we arc. We really don’t know anything at a dog's
level about the mechanism of heart disease, or cancer, or stroke, or
specific disease. This assumption remains at the heart of
rheumatoid arthritis. We can make up stories about them and it could
modern epidemiology, even for the study of chronic diseases.
be, I suppose, that they do have multiple causes, and arc due to things
Epidemiological research, especially after World War II
we can’t control in the environment. If that’s true—if that should turn
in the United States and Europe, has attempted to link social
out to be true—that would be quite a piece of news. Because it has
never happened before. Every disease that wc do not know about,
and economic factors to morbidity and mortality distribuand for which wc have really settled the issue, so that we can cither
'ztion. Social epidemiology, as this type of reserach is called,
turn it off, switch if off or prevent it once and for all—every such
received emphasis during the War on Poverty programmes
disease turns out to be a disease in which there is one central
of the early 1960s and, at the same time, gave some scientific
mechanism. ... In the case of pneumonia, it’s the pncumonocciccus,
and in the case of tuberculosis, it’s the tuberculc bacillus, and in
justification for their inauguration and continuance (34, 35).
pcllcgra, it’s a single vitamin deficiency, and I have a hanch, of'course,
Studies indicated differences in occurrence, severity, and
I can’t prove it, that it will turn out to be that way for cancer.
length of specific illnesses based upon a person’s income,
For all the billions that have gone into cancer research,
race, age, and especially class. While these findings become
widely accepted within the discipline of epidemiology, they no single etiological agent has been found. But the WHO
never had a substantial impact on medical education. (In fact, claims that 80-90 per cent of all cancer is environmental or
most health workers, including physicans, are not taught occupational in origin, hence preventable in some way (38).
epidemiology.). Yet, just associating a relationship between Although there are constant pronouncemnts on the cause
social characterstics, disease incidence, and health status docs of heart disease (e.g. highfat diet, excessive sodium intake),
not fully explain the totality of that relationship. To the extent none appears to be specifically responsible. The most fruitful
that social epidemiology was content to remain on a descrip approach to the control of heart disease may be the altera
tive lex'el, it became merely a form of demography (36). While tion of the social environment (i.e. stress reduction) (39).
social epidemiology allows for the use of “multifactorial” Suicide and homicide are obviously not amenable to bio
explanations for disease occurrence, it still tends to rely upon logical answers, despite the protestations of the so<;ioa notion of specific etiology and sees social and economic biolog'ists (40).
Therefore, the present understanding of medicine and
factors as contributive rather than causative.
disease
spread is most valuable for infectious diseases—ones
The search for a specific cause tends to preclude a
thorough and exact analysis of the particular societal con that have largely been brought under control in the advanced
text. This problem can be illustrated by the relation between capitalist world. For diseases that are not infectious,, there
smoking and lung cancer. While smoking is clearly related does not seem to be specific etiology, or a single cure; it is
to lung cancer and people who smoke are far more suscep these diseases that constitute most of the morbidity and
tible, there is no known agent transmitted from the cigarette mortality in the United States.
into the lungs which can be said to specifically cause the Popular Disaffection with Scientific Miedicine
disease. It cannot be maintained by remaining within accept
It is through the study of chronic diseases, the,- so-called
able grounds of epidemiological thought that cigarette smok
diseases of civilisation, that one confronts the ineffectiveness
ing causes cancer, although a high correlation between
smoking and lung, cancer incidence exists. In other words, of scientific medicine. It was not until the discovery off sulpha
where causality is multiple and/or approximate, no firm con drugs and antibiotics in the 1930s and 1940s that modern
clusions can be drawn that are generally acceptable within medicine could intervene in the disease process in a ‘specific
way with a relatively guaranteed result (excluding s.urgcry,
the scientific community.
of course). However, this seeming success with inf ectious
If this is true of cigarette smoking, where the effects are
. disease both increased the expectation of medicine’s
relatively apparent, image the difficulty in trying to establish
capabilities and, al the same time, wreaked havoc with the
the causative nature of industrial pollutants, occupational
demographic profile of the Western world by incireasing
chemicals, or excessive noise-all of which clearly fall outside
longevity. Thus, millions of cases of chronic degenerative
the notion of cause that is accepted by classical epidemiology.
disease resulted in people who would not previously have
Consider the difficulty in firmly establishing the causative
lived past childhood.
nature of specific social, economic or political factors, given
Since the 1960s, a growing disaffection regarding medicine
these limitations! The methodological emphasis on determining* a"direct causative link limits the study of many of ’ has been noticeable. There are several compounding facets
the more pressing problems of illness in advanced Western to this: (a) doubts regarding the value of a modi cine which
society by its reductionist orientation. Moreover, research prolongs life to old age, but often in hospital or nu rsing home
scientists, as opposed to epidemiologists, often try not to settings and in a manner which tends to deprive people of
think in terms of multiple causation. The following quote their human dignity; (b) ethical questions arising from the
(cited in reference 37, p 29) from Lewis Thomas, M.D., inequitable access to and allocation of extremely scarce
president of the Memorial Sloan-Kettering Cancer Center medical resources, e g, artifical organs, dialysi.s machines,
and certain surgical procedures; (c) an awareness f that modern
in New York, is indicative:
It has become something of a popular notion to say that the diseases medicine has been unable to cure and reduce th-e number -of
we are left with, now that we have got nd of the major infections, cases of certain diseases, despite the large sums of monkey
September 1986
61
spent on research; (d) the realisation that much disease results
directly from the degradation of the physical environment,
the workplace, and the individual, coupled with a sense that
medicine does not adequately address prevention on either
the social or the individual level; and (c) the explosion in
the costs of the provision of medical care to individuals, the
government, and employers. This section will expand on these
points and relate them to an explanation of the rise of holistic
medicin^ in the 1970s.
While there has been relatively little change in life expec
tancy rates for those already over 50 in the United State since
the turn of the century, there has been a significant increase
in the number of people, and the percentage of the popula
tion, living to an older age In 1900 there were only 3.1 million
people 65 years and older, but by 1975 there were 22.4 million,
with a population projection of 3.18 million aged by the year
2Q00—perhaps a conservative estimate (33). This will create
a pool of largely unemployed elderly, dependent on a social
security system warcked with financial dliemmas and a
private pension system unable to maintain parity with
inflation. Needless to say, the economic plight of the elderly
adversely affects their health stauts. Given that the elderly
consume more health resources than other segments of the
population, this demographic change implies greatly expan
ded medical care costs. Currently, 68 per cent of the care
fpr the aged is financed by public monies through legislatively
guaranteed benefit packages (41). Medicare has continually
had the most inflationary outlays due to current hospital
behaviour and failings in the largely proprietary nursing
home industry. It is not difficult to grasp why the issue of
passive and active euthanasis is now under discussion and
why a concern over dignity in dying (and even a life after
death) is being promoted in this decade (42, 43).
A somewhat related problem stems from the ethics of
allocating scarce medical resources in a demoractic society.
As sophisticated medical technology becomes evermore ex
pensive, the question of how to decide who should have
access to that technology and on what basis allocative
decisions should be made pose a series of critical bioethical
issues. A whole set of dilemmas have arisen to further
complicate this problem. For example, in the United States
tpday all people with kidney disease can get their treatment
reimbursed through the end-stage and renal dialysis pro
gramme of Medicare, yet poor women have been denied
access to legal abortions through Medicaid.
A third facet of the growing dissatisfaction with medicine
comes from the ineffectiveness of medical research in
adequately answering the most pressing disease problems
tpday. Results of a curative nature from cancer and heart
disease research have been negligible, let alone significant
in alleviating these problems. While there have been advances
qn an individual clinical level (44), the morbidity-mortality
data demonstrate how limited these have been. In the face
of a population apparently not getting healthier, palliative
therapies abound for a wide gamut of current disease
conditions. For example, the huge consumption of psycho
active drugs in the United States has been given wide
attention. One can only speculate on thfnumbers of people
vyho use some form of medication or drug (e.g. alcohol) to
get them through the day (45).
Another facet of the overall problem results from the
62
mounting evidence that much disease, especially heart disease
and cancer, results from the degradation of the physical and
social environment. Air and water pollution, radiation
exposure and additives to food substances have all been
implicated in the disease process and clearly must be addres
sed if social prevention strategies are desired. Further,
occupational stress and health hazards in the workplace
reveal additional social origins of disease (38, 46-49). Millions
of workers have been exposed to chemicals whose long-term
effects on health were previously considered inconsequential
(or in some case known to be hazardous but used anyway).
Greatly increased cancer death rates among certain categories
of workers will emerge over the next two decades. Moreover,
the degradation of the individual citizen through lack of
exercise, inadequate or inappropriate diet, heightened anxiety
and chronic social stress, and other aspects of alienation from
labour and life adversely affect health status indicators and
drive up the utilisation of health services. What is of special *
importance about all these factors is that, by definition, they
are preventable. Yet, medicine, medical research, and the
medical care system continue to ignore the possibility of
prevention by not addressing the social occupational, and
environmental origins of our current disease structure.
Each of the above points has an underlying economic
aspect. The cost explosion in medical care today has
established cost containment as the overriding priority in
most decisions. With the US economy facing severe problems
of inflation and intermittent recession, both corporations
(who purchase the bulk of health insurance for their
employees) and the Federal Government (which funds
services for the poor and aged) are calling into question the
amount of money being spent on medical care services (50).
The cost of medical care and other associated health services
(such as environmental and workplace clean-up require
ments) has increased at an exponential rate over the last three
decades, making the health sector a leading growth industry.
From the‘corporate perspective, these health benefit costs
might have their own justification if the present array of
services returned an even larger increase in the labour force
productivity via improved heath. But the past two decades
have brought significant change in health status, despite this
escalation of expenditure. Complicating this problems is the
fact that the major portion of health expenditures flows out
of the corporate sector and State into the hands of profes
sionals and hospitals. Thus health care expenditure appear
unequivocally as a major factor limiting capital accumula
tion, and a corporate strategy to reduce inflation in health
costs is currently becoming evident (51). Replacement of
costly, high-technology medicine with cheaper, nontechnological therapies is a major redirection advocated by
proliferating medical-care evaluation studies (52, 53).
Corporations have developed an interest in holistic health
as Forbes magazine notes, “because it emphasises more
money-saving prevention and patient responsibility?’(54)
In addition to the extent that the provision of successful
medical care has become a source of legitimacy in advanced
capitalism, increasing popular dissatisfaction with current
medical practice will become a chief focus of the State (It
has become clear for instance, that right-wing political groups
have latched on to the public disaffections with medicine
through the promotion of anti-abortion crusades, laetrile
Radical Journal of Health
legalisation campaigns, etc.).
All of these problems have led to a heightened concern
with health in recent years. The holistic health movement
has arisen in part out of this concern and in part has helped
to generate it.
Holistic Health Movement
There are problems in defining the holistic health move
ment beyond grouping together all practitioners who place
themselves against or outside the mainstream of modern
medicine. Further, it is difficult to distill commonalities from
the potpurri of alternative therapies, since such a diversity
has been linked as a movement by its organisational
advocates (1,57-59).
The positive health orientation of holistic therapy has two
separate components. The first is the perception of health
as a value in and of itself; the second is the notion of health
as a praxis—the active participation of the individual in the
ongoing maintenance of his/her own helth. Holistic therapies
also assume a unity between mind, body, and spirit, the
major implication of which is that illness is regarded as more
than just physical disease and is assumed to have causes and
dimensions beyond the purely biological. The separation of
mind and body has long been a philosophical issue in
Western thought, and the elimination on downplaying of the
mind as a component of the disease process has been con
sidered as of the cardinal success of scientific medicine. The
critique of the mind-body duality and the reintroduction of
elements of spirtuality in holistic medicine form a strong
counter to the crude materialism of scientific medicine in
its narrow emphasis on what it takes to be the physical and
biological source of disease.
The holistic health movement has philosophically set itself
in direct opposition to some of the basic tenets of scientific
medicine. The potential power of the “mind” over the
“body” is being tested in the treatment of various diseases
as practices such as meditation, biofeedback, autogenic train
ing, and hypnosis become quite popular. The exploration of
psychic phenomenon (e.g. clairvoyance, telepathy, pre
cognition, psychokinesis, and extrasensory perception) may
encourage a new understanding of pathophysiology and
ongoing health maintenance. Other practices (such as yoga
and the various forms of martial arts) are promoted a£ aids
in forming an integrated view of the individual’s health and
a greater consciousness of health.
Although it is challenging the taboos of scientific medicine,
holistic medicine has not yet established itself as scientific.
Holistic therapies primarily have relied upon ancedotal
evidence, with “proof” of efficacy to be found in individual
testimony. Since scientific theory prides itself on repeatability
and universality medicine orientations easily fall prey to
charges of quackery and hucksterism. Several factors,
however, complicate the picture. For one thing, a number of
scientifically established medical procedures and therapies
have been found in many cases to be no more effective than
treatment by a placebo. This applies not only to certain drugs,
but also to various surgical and medical treatments. Indeed,
several recent Government reports have criticised the scien
tific medical establishment for choosing many of its prac
tices more by intuition than by science or study. Most notable
is the recent survey by the Office of Technology Assessment,
September 1986
an agency of the US Congress on the safety and efficacy of
17 common medical practices (52). The implication of this
orientation is apparent: if scientific medicine were to subject
itself to the same rigorous testing that it demands for holistic
medicine, many of its forms of intervention would not fare
too well cither! One may conclude that science, as we
presently know it, is insufficiently developed to properly
understand the interactions of body, mind, and spirit over
the course of the disease process. At the same time, this line
of reasoning should not suggest immediate acceptance of
holistic medicine and its various therapies without some
proof of efficacy.
By concentrating on individuals and tailoring therapies to
individual needs and desire, holistic medicine achieves a great
degree of client satisfaction. Interpersonal sensitivity and
responsiveness to patient’s needs ans values which are
generally operationalised in the holistic practitioner-patient
interface. Since the patient is held responsible for his/her
own health (and in many cases, the results of therapy), people
arc loathe to blame failure of the invervention or the therapy
itself. Rather, it is usually assumed that the patient has not
tried hard enough, “it’s not the time yet,” or that the search
must continue for the real root-cause of the illness. Often,
the power of suggestion and belief plays a dominant role in
therapy. For the most part, then practitioners of holistic
medicine tend to generate loyal followings for their particular
theory and therapy among their clientele. In an era of
growing disenchantment with modern medicine, one finds
in holistic therapy a popular modality’upon which to center
one’s hope for alleviation, if not elimination, of a plaguing
health problem. It is less invasive and dangerous than scien
tific medicine; it tends to use natural or symbolically ritual
medicines or drugs; and because it employs more intimate
forms of treatment such as touching, holistic medicine is
usually enjoyable and pleasant.
As public support wavers for the scientific establishment,
various forms of holistic health care are generating atten
tion and hope from both those suffering from maladies and
those wishing to grow in new dimensions of their lives. Never
theless one finds in the holistic health movement many of
the same organisational and social patterns that predominate
in the present health care system: solo, fee-for-service entre
preneurial practice; knowledge or skill sold to “consumers”
in commodity forms elitist and sexist behaviour on the part
of the practitioners; a concentration of availability of services ■
to middle-class, white people able to play; and a clear separa
tion between practitioners and those who are served. Most
practices also tend to be focussed on the individual, as in
scientific medicine, and lack virtually any focuss on the larger
social grouping.
In the midst of the growing narcissism in the United States
today, holistic health practices are being explored as part of
strivings toward self-growth and self-actualisation (60). In
addition, some corportions are beginning to seek increased
employmee productivity by offering training in practices such
as mediation for stress reduction (61-63). While taking a
positive step by including the mind as a causative as well as
a healing agent, most holistic practices continue to exclude
the external social world from their attempts at healing,
failing to provide strategies for changing economic and social
relations. Some practices are serving to further commodify
63
alienation “personal” problems arc temporarily relieved as
a particular practice lends io adjust the individual to the
society from which the pathology has arisen. Thus, this
adjustment of the individual may become a prominent
tendency (64).
Most holistic practices contain heavy doses of mysticism
and charismatic elitism. Their Eastern (and precapitalist)
origin often results in an authoritarian elitism that has taken
interesting—and—disturbing—forms as these age-old prac
tices have been transplanted into America. The most glow
ing deficiencies of holistic practices, as they currently exist,
arise out of their intense individualism and limited notion
of totality. Most assume that they are totalistic by stressing
the unity of the body, mind, and spirit. However, this ignores
the larger social world outside the body from which much
of disease originates. Meditation, fpr instance, can relieve
the effects of stress on an individual, but it does not remove
the stress source. When one stops meditating, the social stress
is still there. A readily apparent weakness of many of the
holistic medicine practices is that they ignore politics, declin
ing to connect disease to existing social relations. When these
connections are made, the problem is often defined in terms
so general—“the West,” “modern society’—as to suggest that
the only sensible course is exclusive concentration on healing
the individual in a chaotic and brutal world. The philo
sophical thrust of holistic medicine assumes emotional and
spiritual dimensions of the individual transcending the
physical body. Yet even this expansion still centers on the
internal dynamics of the individual to the exclusions of
external reality. This, of course, differs from the social
medicine of the 19th century, which defined the totality to
include the physical and social environment as well as the
human organism.
Conclusions
Various holistic medicine therapies are rapidly becoming
popular alternatives to scientific medicine. In just a few years,
holistic medicine has been able to achieve significant public
support in the Western world, as well as the nascent support
of both corporations and the Federal Government. It is
imperative that health policy analysts and health practitioners
understand the nature and content of holistic medicine and
the social dynamics out of which it arises.
That holistic medicine poses challenges to the hegemony
of scientific medicine cannot be denied. One example is the
pressure for the National Cancer Institute in the United
States to hold controlled clinical trials to test the alleged
efficacy of laetrile in cancer treatment. Some 17 state
legislatures have legalised the prescription and sale of lactrile within their borders, a decision made in spite of the
almost unanimous opposition of the medical profession.
Chiropractic therapy now receives reimbursement from
several Medicaid plans and from Medicare. Court cases regar
ding the rights of people to choose a holistic therapy (i.e,
nutritional therapy or laetrile) against the wishes of their
physicians, who. advocate either chemotherapy or some
invasive treatment, have been heard with mixed results to date
(see, for example, refernce 65). It seems apparent, though
that many more such issues will be fought out in the legal
arena. Meanwhile, a groundswell of investigation into alter
natives to scientific medicine has been occurring as patients
64
seek out therapies suggested by the multiplicity of articles in
the popular press. Bookstores have been devoting higher and
higher percentages of shelf space to sections on health,
psychology, and the occult; many of the ideas gleaned from
this recent explosion in publishing arc used by people as
supplements—it not direct alternatives—to what scientific
medicine-oriented physicians suggest.
Its non technological nature and extreme emphasis on indi
vidual responsibility for health are aspects of holistic
medicine that imply cheaper modalities of care than the
present, medical care system offers. Those social groups
advocating cost containment in hclth care have an obvious
interest, then, in the explosion, growth, and spread of holistic
health care. As noted earlier, medical care inflation has been
running at a rate almost twice that of the rest of the economy,
and the likelihood of its being slowed down dramatically is
quite limited in the absence of major cutbacks in care, which
seem politically infeasible at this time. Given this reality, there
is a definite political and economic necessity for new
approaches to hcalt and health care problems. Holistic
medicine just may fill that need.
Similarly, a changing ideological focus is being promoted
in health today. A medical care system emphasising the indi
vidual’s role in maintaining his/her own health and
promoting a signifient lessening of absenteeism among
employees would be of considerable value to the corporate
sector. It the infusion of holistic medicine modalities into
the workplace could keep people on the job and improve their
individual productivity by making them cither objectivity
healthier or at least believing they arc healthier, it would serve
to address one of the most pressing problems in America
today (as defined by corporations): low productivity due to
worker alienation. Thus holistic medicine could be of great
utility to our present malfunctioning system of economic
production.
Finally, if holistic medicine should succeed in giving people
a sense of caring for themselves and being the decision
making subject in their lives rather than just an object; if
it should succeed in promoting dramatic changes in current,
unhealthy lifestyles; it if does provide a more meaningful
justification for living in a relatively unpleasant world; then
it most certainly will be utilised by greater numbers of people
in our society. Yet, by achieving such results, holistic medicine
may then become a part of corporate and state strategies for
cost constainmcnt in health care. Also holistic medicine could
easily be formulated into a social mechanism for allaying
criticism of present inadequacies in health care delivery and
the social production of disease (66).
We have attempted to demonstrate that the resurgence of
the holistic health movement in this decade is no social
accident, but clearly arose in response to degenerative social
and psychological conditions of the day. Holistic therapies
arc addressing some of the crises that lhavc been created by
the ongoing demise of scientific medicine. It should be noted
that scientific medicine is far from dead at the moment,
however, and may, with some propitious discoveries, regain
its hegemony. At the same time,we have tried to indicate that
holistic medicine, to the extent that it focuses solely on the
individual and ignores political and social dimensions, is not
the entire answer for health either. Nevertheless, holistic
medicine is an up-and-coming social movement gaining wide
Radical Journal of Health
SVoT
0"- r as such> dcmands attention
th' "o^ers anti policy analysts (67-69).
This from all
US 1979-77. US Government Printing Office, Washington, DC, 1978.
Hurcly, R. The health care crisis of the poor. In The Social Organisa
tion of Health, edited by H P Dreitzel. MacMillan, New York, 1971.
35 Susscr, M W. and Watson, W. Sociology in Medicine. Oxford
University Press, New York, 1962.
36 Tiesman D. The Institute of Psychiatry sackings: Ideology, science
References
and the organised scientific worker. Radical Science Journal 5, 1977.
37 Sontag, S. Disease as political metaphor. New York Review of Books,
’ And/Or
HCa“h Ha“p 29, February 23, 1978.
And/Or Press, Berkeley,
2 fheS?.1lCtraLZ’""f"'?nt °f
Medicine. Institute for 38 Epstein, S. The Politics of Cancer. Charles Scribners Sons, New York, 1978.
■t Th T TJ f Human,stlc Medicine, San Franscisco, 1975.
39 Eyer, J. Hypertension as a disease of modern society. Int J Health
3 tan, T. Tmnspcrsonal Psychologies. Harper Colophon, New York 1977
Service 5 (4): 539-558, 1975
4 Cousins, N The mysterious Placebo: How mind helps medicine work '
40
Caplan, A L. The Sociobiology Debate. Harper and Row, New York, 1978.
Saturday Review, pp 9-16, October 1, 1977.
nt wont.
41 Cambridge Research Institute. Trends Affecting the US Health Care
5 The Journal of Holistic Health, 1977-1979.
System. Aspen System Germantown, Md, 1976.
6 Carlson, R, The End of Medicine. John Wiley and Sons, New York, 1975.
7 Hec/^’p SI 7<J!7h°IiSlic hcahh rcvolut»on. Journal of Holistic 42 Kubler-Ross, E. On Death and Dying. MacMillan, New York, 1973.
43 Veatch, R M. Death, Dying and the Biological Revolution: Our Last
Hope. Yale University Press, New Haven, 1976.
8 Carlson, R, Frontiers of Science and Medicine. Henry Regncry
44 Israel, L. Conquering Cancer. Random House, New York, 1978.
Company, Chicago, 1975.
45 Waldron, I. Increased prescribing of Valium, Librium, and other
9 Berliner, H A, Larger perspective on the Flexner Report. International
drugs: An example of the influence of economic and social factors
Journal of Health Services 5 (4): 573-592, 1975.
on the practice of medicine. Int H Health Service 7 (1): 37-62, 1977.
10 Sigerist, H. Landmarks in the History of Hygiene. Oxford University
46 National Cancer Institute. Estimating the Fraction of Cancer in the
Press, Longdon, 1956.
United States Related to Occupational Factors. Washington, DC,
11 Rosen, G, .4 History of Public Health. MD Publications, New York
September 15, 1978.
1958.
47 Brodeur, P. Expendable Americans. Viking, New York, 1974.
12 Ackerknecht, E, Anticontagionism between 1821 and 1967. Bull Hist
48 Stellman, J, and Daum, S. Work is Dangerous to Your Health.
Med 22 (5): 562-593, 1948.
Vintage, New York, 1975.
13 Chadwick, E, Report on an Inquiry into the Sanitary Conditions 49 BerMan, DM. Death on the Job. Monthly Review Press, New York,
of the Laboring Population of Great Britain. Edinburgh University
1978.
Press, Edinburgh, 1965.
50 Salmon, J W. Corporate Attempts to Restructure the American
14 Chadwick, E, The Health of Nations. Longmans, Green, and
Health Care System. Unpublished dissertation, Cornel University,
Company, London, 1887.
Ithaca, 1978.
15 Finer, S, The Life and Times of Sir Edwin Chadwick. Methuen and
51 Salmon, J W. Monopoly capital and the reorganisation of the health
Company, London, 1952.
sector. Review of Radical Political Economics 9 (1, 2): 1-44, 1977.
16 Engels, F, The Condition of the Working Class in England in 1844.
52 US Congress Office of Technology Assessment. Assessing the Safety
Progress Publishers, Moscow, 1973.
and Efficacy ofMedical Technologies. US Gvernment Printing Office,
17 Marcus, S, Engels, Manchester and the Working Class. Vintage,
Washington, DC, 1978.
New York, 1975.
53 Cochrane, A L. Effectiveness and Efficiency: Random Relections
18 Rosen, G. What is social medicine? A genetic analysis of the con
on Health Service Nuffield Provincial Hospitals Trust, London, 1972.
cept. In From Medical Police to Social Medicine, pp 60-119. Science
54 Physician Heal Thyself.. .or Else. Forbes, p 95, October 1, 1977.
History Publications, New York, 1974.
55 Culbert, M L. Vitamin B-17: Forbidden Weapon Against Cancer.
19 Galdston, I. The Meaning of Social Medicine. Harvard Univesty
Arlington House, New York, 1974.
Press, Cambridge, 1952.
56 Harton, H, editor. The Truth About Laetrile. Public Affairs Press,
20 Ackerknecht, E. Rudolf Virchow: Doctor, Statesman, Anthropologist.
New York, 1977.
University of Wisconsin Press, Madison, 1953.
57(CaPatra, J. Healing. LcGraw-Himm, New York, 1978.
21 Ringen, K. Edwin Chadwick: The market ideology and sanitary 58 Walker, M. Total Health: The Holistic Alternative To Traditional
Medicine. Everest House, New York, 1978.
reform. Int J Health Service 9 (1): 107-120, 1979.
22 Ringen. K. The Development of Health Policy: Norway, England 59 Kaslof, L J,-editor. Wholistic Dimensions in Healing: A Resource
and Germany. Unpublished dissertation, Johns Hopkins University
Guide. Doubleday and Company, New York, 1978.
60 Lasch, C. The Culture of Narcissism. Norton, New York, 1978.
School of Public Health, Baltimore, 1977.
23 Stern, B. Society and Medical Progress. McGrath Publishing Com 61 Relaxation breaks instead of coffee breaks lower employees’ blood
pressure. Wall Street Journal, p 1, December 1, 1977.
pany, Washington, DC, 1970.
24 Ackerknecht, H. A Short History of Medicine. The Ronald Press, 62 Drew, D R. Transcendental meditation and productivity. Academy
of Management Journal 17: 362-368, 1974.
New york, 1968.
63 Flanagan, W. Reducing stress through transcendental meditation.
25 Powles, J. On the limitations of modern medicine. Sci Med Man 1
Business Week, pp 101-102, October 26, 1974.
(1): 1-30, 1973.
.
.
64 Crawford, R. You are dangerous to your health: The ideology and
26 Renaud, M. On the structural constraints to state intervention in
politics of victim blaming Int J Health Service 7 (4): 663-680, 1977.
health. International J Health Service 5 (4): 559-572, 1975.
27 Waitzkin, H, and Stoeckle, J. The communications of information 65 Follow-up on the Chad Green case. New York Times, P 33, January
21, 1979.
about illness. Adv Psychosom Med 8: 180-215, 1972.
28 Reich, W. The Mass Psychology of Fascism. Farrar Strauss and 66 Berliner, H S, and Salmon, J W. The new realities of health policy
and influence of holistic medicine, c/o Journal of Alternative Human
Giroux, New York, 1970.
..
•
Services 5 (2): 13-16, 1979.
29 Reich, W. Character Analysis, 3rd edition, Simon and Schuster, New
67 Ullman, D. Holistic health as a model for personal and social change.
’^artofsky, M. Organs, organisms and disease: Human ontology■and
c/o Journal of Alternative Human Services 5 (2): 9-12, 1979.
68 Burlage, R. New health care alliance could build new system.
medical practice. In Evaluation and Explanation in the
Democratic Left, pp 9-12, June 1979.
Sciencezed'Md by H T Engelhardt, Jr, and S Spicker, pp 67-83.
69 Salmon, J W, and Berliner, H S. Health policy implications from
D Reidel Publishing Companym, Boston, 1975.
the holistic health movement. Journal of Health Politics, Policy and
Knowles, J H. Introduction to Doing Better and Feeling Worse.
31
Law (forthcoming).
Health in the United States. Norton, New York, 197/.
32 Eyer. J, and Sterling, P. Stress-related monalily and socta^organisa- 70 Salmon, J W, and Berliner, H S. Can Holism Tbrn Left? Paper
presented at the 107th Annual Meeting of the American Public
tion. Review of Radical Political Economics 9 (1, 2M^. W?Health Association, New York City, November 7, 1979,
33 US Department of Health, Education and Welfare. Healt .
, —j attention
hould, hopefully, be directed toward uniih.
uniting people in the
transformation of their social conditions
------ 3 necessary for
improved health (70).
34
65
September 1986
UPDATE
News and Notes
Privatisation of Medicare: Help from GIC
THE General Insurance Corporation (GIC) has an
nounced the introduction of a medical insurance
scheme, named Mediclaim, with effect from November
3. The introduction of medical insurance should
ordinarily have been welcomed as an important step
towards extending the benefits of modern health cafe
to the mass of the people. However, the scheme
announced by GIC through a high-powered advertise
ment campaign should instead be expected to, and is
indeed intended to, give a strong fillip to the privatisa
tion of health care in the country—and this not
withstanding the fact that the GIC itself is a wholly
government-owned corporation. In fact, we have here
another instance of how the government and public
sector organisations closely collaborate with private
busyiess for the advancement of the latter’s interests.
The manner in which the GIC has chosen to adver
tise its Mediclaim scheme tells its own tale. The adver
tisements read very much as if what is being advertised
is a sort of lottery: “Claim medical expenses upto
Rs 17,600 a year by paying just Rs 250”, the GIC pro
claims. Also noteworthy is the prominence given in the
advertisements to th£ fact that the premium paid on
Mediclaim policies will be deductible from taxable
income under section 80D of the Income Tax Act,
making it clear that the GIC is aiming the scheme
mainly, if not wholly, at income tax payers Who con
stitute some three per cent of the country’s population.
be meaningful medical insurance must cover the whole
family. Taking a family of five members, the two
cheapest policies, which cover tf.edical expenses only
in case of hospitalisation,
cost Rs 1,125 and
Rs 1,575 per annum, respectively (after allowing for
the 10 per cent discount which the GIC is offering
where one or more dependenis a e also covered). At
the other end, the premium cn the more expensive
policies, which alone cover the cost of domiliciary
hospitalisation, vary betwe^nj^s 2,700 and Rs 5,850
per annum—quite large sums even for those in the up
per income brackets. No wonder that the GIC has
realised that it desperately needs the crutch of tax
deductibility of premium payments to be able to sell
Mediclaim. Incidentally, by its very nature, private
medical, insurance of the type being offered by GIC
tends to be expensive. As a result, it can be meant on
ly for a small select section of the population. Even
in a country like the UK, according to one estimate,
whereas nearly a quarter of professionals have private
health insurance cover, for semi-skilled and unskilled
workers the coverage is less than two per cent.
If, on the one hand, Mediclaim is meant to cater to
upper-income income-tax payers, on the other hand,
it is intended to cover the cost of medical treatment
in the exclusive private hospitals set up as corporate
business enterprises, the rapid proliferation of which
has been one of the major developments in the area
of
health care in the country in the last few years. This
In any case, the terms of the Mediclaim scheme are
such that there is no possibility of anyone except the is evident from the fact that the hospital room charges
very well-off benefiting from it. The GIC is offering • that Mediclaim allows for are Rs 550 and Rs 350 per
five classes of policies. The annual premium on the day for the two most expensive policies and Rs 250 per
least-priced two are Rs 250 and Rs 350 and entitle the day for the remaining three types of policies. Of course,
insured person to claim 80 per cent of the cost of there is in this country a class of people who can
medical treatment in hospitals subject to a maximum without batting an eyelid pay for treatment at the new
of Rs 17,600 and Rs 25,500, respectively. Under these private hospitals at these or even higher rates. But it
policies the GIC will pay nothing if the medical is naturally a small class. So if the private sector
expenses are not incurred in a hospital but on treat hospitals are to continue to attract the required large
ment at home. Then there are three other more expen investments and their number is to continue to grow
sive classes of policies, costing Rs 600, Rs 840 and and their profits are to keep rising, the demand for
• Rs 1,300 per annum, which entitle the insured person their services needs to be enlarged beyond that pro
to reimbursement of hospitalisation expenses upto vided by the above-mentioned class of the very rich.
Rs 37,750, Rs 52,750 and Rs 82,500, respectively; in This is precisely what GIC’s Mediclaim scheme aims
addition, under these policies medical expenses incur to do with the direct help of the government in the
red on treatment at home too will be reimbursed upto form of tax exemption for premiums paid under the
scheme, which amounts, roughly speaking, to between
Rs 5,250, Rs 7,400 and Rs 11,500, respectively.
one-third and one-half of the private hospitals’ charges
At first sight, the premium rates may not appear being paid out of the public exchequer in the form of
excessive. The catch lies, however, in the fact that to tax revenue forgone. It should by now be clear how
66
Radical Journal of Hea!^
the government and the public sector GIC are aiding
the privatisation of medical care in India.
The GIC’s Mcdiclaim scheme is only one of a series
of recent moves by the government to help privatisa
tion of medical care. In December last year the Income
Tax Act was amended so that reimbursement by
employers of medical expenses such as operation fees,
hospitalisation charges, cost of medicines and tests, etc,
incurred by employees and their families is no longer
treated as a perquisite. In other words, the amounts
so reimbursed are not now added to the taxable income
of the employees. The term ‘employees’, it has been
specifically provided, is to include “managers/dircctors” (with their families). The Income Tax Act 1961
already permitted government employees to receive
such tax-free reimbursement of medical expenses. This
benefit has now been extended to those working in the
private sector and in public sector undertakings.
The change in the tax treatment of expenditure on
medical expenses has to be seen together with some
other decisions of the government to appreciate its full
import. Under the scheme to encourage non-resident
Indians (NRI) to invest in India, hospitals have been
included among the areas qualifying for NRI invest
ment upto 74 per cent. Later the definition of hospitals
was enlarged to include ‘diagnostic centres’ as well in
order, as the government press note on the subject put
it, “to facilitate the inflow of NRI expertise and
investment in the area of medical diagnosis through
specialised and sophisticated equipment not readily
available in India’’. Apollo Hospitals in Madras was
the first to come up in response to the government
scheme, as a public limited company with non-resident
jnj^stment. Others have since followed in its wake.
In addition to these specific measures to facilitate
their growth, the government is only too ready to give
theprivate corporate hospitals legitimacy and respec
tability. For instance, while inaugurating its Diabetes
Foundation, the Vice-President of India acclaimed
Apollo Hospitals as “the first fully-equipped, cor
porate, multi-speciality hospital in India” and added,
“I have had the privilege of being associated with the
development of this unique all-round medicare faci
lity”. What followed was even more explicit under
writing of private medical care at the cost of the
facilities provided in government hospitals. The VicePresident said that to depend on the government alone
for health services would be to reconcile oneself to
mediocrity and paucity of such services. In other
•'"'us, because government health services are of in
different quality and inadequate, the government needs
to support private establishments such as Apollo
Hospitals.
This is a piece of deliberate misrepresentation, for
the high-cost private sector hospitals with their high-.
September 1986
powered doctors, their sophisticated diagnostic
machines and therapeutic aids provide an altogether
different type of medical care from that provided by
the government health services and to an altogether
different class of people. Far from making up for the
undoubted deficiencies of the public health services,
privatisation of medical care with the active support
of the government is bound to further distort the
priorities of the government’s health policies and
thereby further choke the flow of resources and
qualified medical personnel to the government health
services, rendering them even more unequal to the task
of providing health care for the mass of the people.
K R
Legislation of Abortion in Yugoslavia
Yugoslavia is a.country where abortion is legal and
very simple. It is sufficient that the woman chooses
the hospital and the gyneacologist, pays about 50
guilders for the whole treatment including the
anesthesia, and she is back home the next day. All this
is due to the very good laws and to a struggle that the
women of Yugoslavia won fighting against the conser
vative behaviour and practice. The struggle for various
women’s rights including the right ro decide about her
own childbirth, dates in Yugoslavia from the second
world war. In 1952 the interruption of pregnancy was
legalised but only for medical reasons. The social
reasons were accepted too. From 1960-1978 the
abortion had to be approved by a commission, instead
of the woman herself. Various- commissions had
different opinions, which made it impossible for
women to use their legal rights. Although the com
mission approved of 97 per cent of the petitions, in
order to lessen the tension for women and to liberate
them from the haste, and all the waiting in the medical
clinics, women still made further efforts to liberalise
the law even more.
A new law was passed in 1978 and according to it
the decision about childbirth is a personal matter. A
part of the law is about contraception: the rights of
people to learn about contraception and the planning
of the family is acknowledged. Sterilisation is allowed
for persons older than 35 or if there are other medical
reasons. The main feature of the law about abortion
is that every woman has the right to ask for it, that
they are safe financially, and institutions are available,
which is very important. And that abortion can be
refused for medical reasons. The law makes it possible
for a woman to have the abortion after a medical
examination on her request, till the 10th week of
pregnancy. From the 10th to 20th week and later it is
possible only if the commission finds it not dangerous
for the women’s health. Persons under age can also ask
for it, but with the agreement of parents or the person.
responsible.
67
After bringing up the tree law the number of
abortions has increased a great deal, which is alarm
ing considering that Yugoslavia has about 22.5 million
inhabitants and the number of abortions done annually
is about 300,000. There arc some parts of Yugoslavia
where the number of abortions is larger than the
number of births. In Scrvia there is one birth to 1.4
abortions, in Croatia one birth to 0.75 abortions. And
it is still increasing.
In Yugoslavia contraception is not very popular,
there are not enough services for it and young people
are not well-informed about it. Although the number
of services is increasing, only 40 per cent of the women
use contraception. A lot of women still use abortion
as the only method of contraception together with the
traditional methods—39,000 abortions have been done
on married women out of 40,000 that were done in
Croatia. The figures tell us that the planning of the
family is not valued. Sterilisation is very unpopular,
men do not ask for it at all.
i
Tokyo, Isis WICCE, Dispensaire des Femmes, and the
Boston Women’s Health Book Collective.
For further information please write to:
CEFEMINA, Apdo 5355, San Jose 1000, Costa Rica.
Ills of Public Hospitals
Recent events have drawn fresh attention to the
atrocious state of public hospitals all over the coun
try. The glycerol tragedy which is unfolding every
day in the courts in Bombay can well serve as
a case study of the degree of inefficiency in these
hospitals. Even more disconcerting is the fact that the
doctors and the officials appear to be exhibiting a
degree of nonchalance which can only be termed
inhuman and callous. Officials have admitted that no
action was taken other than issuing a routine alert, and
that after a delay, even though several similar deaths
had occurred in a single ward; doctors have confessed
that they did not deem it important to read circulars
marked urgent; and units have been found to have con
[Abridged from Women's Network on Reproductive Rights
tinued to use the same batch of suspect glycerol for
Newsletter]
48 hours after an order was issued to impound the
Fifth International Women and Health Meet batch.
It was around this time that the doctors at KEM
WOMEN health activists, researchers, and practi
hospital in Bombay went on unique strike with the sole
tioners form all over the world will gather in San Josd,
objective of highlighting the utter lack of adequate and
Costa Rica next spring for the Fifth International
necessary facilities in the hospital. And what they had
Women and Health Meeting. The Centre Feminista de
to tell the patients was indeed a revelation—sub
Informacioh y Acciori (CEFEMINA) is co-ordinating
standard equipment, operating theatres with fungus
the planning for the conference, which is scheduled to
growth on the walls, machines sitting idle for want of
take place from May 23 to 28, 1987. This marks the
simple repairs, shortages of drugs, and so on.
first time the meeting will be held in a Third World
However, all this attention on the inefficiencies of
country; the previous four meetings have been held in
public hospitals has given rise to a feeling that the only
European cities.
choice then is to make use of private practice facilities,
The conference will focus on five main themes:
even if one has to foot the fabulous bills later on. In
population policies and reproductive rights; com
fact, state governments, like Uttar Pradesh have already
munity health; environmental health hazards; drugs;
set in motion, plans to hand over rural health care to
and the health care system. The organisers welcome
z private sector.
any suggestions for specific workshops to be organised
There cannot be a more mistaken notion than this.
under these categories as well as general input into the
The roots of the malady in public hospitals probably
planning of the conference. Meetings will be held in
Spanish, French or English, with simultaneous transla lie in the proliferation of private practice and private
hospitals. And it is these hospitals which have received
tion available for plenary sessions. Childcare facilities
enormous support and patronage from the government
for participants’ children will be provided.
even as the government-run institutions have lacked
The conference organisers also urge women who
both finance and other support. There is need to look
want to attend to begin fund raising immediately to
more closely and critically at the relationship between
cover travel costs and expenses. Those who can are
the private and public institutions. Today the state is
encouraged .to help raise funds for women who cannot
openly admitting its inability to provide welfare
cover their own costs.
Eleven national and international women’s organisa services such as health and seeking to move its respon
sibility to the private and voluntary agencies. Can the
tions, including Isis International and the Latin
American and Caribbean Health Network which we government abdicate its responsibility to provide
‘welfare’-—even if it is rudimentary? Have we as health
co-ordinate, are sponsoring the conference. The others
activists been altogether more concerned about evol
art Peru Mujer, Centro Ecuatoriano para la Promocidn
ving alternatives than with pressurising the government
y Accidn de la Mujer, Women’s Global Network on
to be accountable?
Reproductive Rights, International Baby Food Action
Network, Health Action International, SOSHIREN
—P P
68
Radical Journal of Health
Female Patients versus Male Doctors’ Universe
jyttc willadsen
How does medicine view women’s health problems? In recent years the women’s movement has posed many
questions to medicine which has in turn set the medical establishment thinking. This article is an ’insider’s view
by a Danish woman psychiatrist and discusses how bias influences both the diagnosis and the treatment of women’s
problems.
SCIENCE is unscientific in the way it analyses and treats
women. Virginia Woolf says, “Science it would seem is not
sexless, she is a man, a father and infected too”.
It is very important and essential to confront the medical
world with feminist viewpoints. You may then be able to
explain many otherwise unintelligible problems and
treatments. If we raise the consciousness about this con
frontation we can go ahead in a much wiser way and other
wise we will obtain impossible results in the treatment of
women patients. In the industralised part of the world women
live about seven years longer than men do. Why is it so? On
the other hand, depressions are much more widespread in
our societies among women, and women are depressed
between three and six times as often as men. What’s the
explanation of this? Women go to see their doctors twice
as often as men. Is this good or bad? Women are drugged
twice as often as men, and many healthy women are
constantly under the control of an artificial intake of sexhormones, while healthy men as a rule don’t take hormones.
Why is it that men most often abuse alcohol and drugs? Why
is it that nearly exclusively, men are imprisoned?
Women’s Biology
Women have a wonderful biology. Our life is cyclic and
cyclicity is an underestimated richness. From puberty the
woman is constantly changing. She is influenced by a
hormonal balance which all the time changes quietly, little,
just like the moon and in the same pace as the moon. Every
28th day women menstruate and after this, in the middle of
the period, we are in ovulation. After this and before the
next menstruation we have the premenstrual phase, where
many women feel extra energy, extra power and vitality.
During menstruation many women feel their womanhood
confirmed and sealed. Some times the female cyclicity takes
other forms. When you are pregnant you are in a long cycle
of nine months, where you feel new changes, new hormone
balances controlling your organism and from moment to
moment you and your child are in quiet change and move
ment towards birth. The birth itself is a series of oscillations
and the labour begins quietly and slowly. As the labour
continues the oscillations become more and more intense,
until the child is born. Afterwards a new cyclicity arises and
you find a new hormone balance with new experiences. When
you nurse the child, your breast slowly fills up and after
wards your love to the baby slowly and peacefully empties
the breast again. This sort of cyclicity continues until you
again return to the ordinary cyclicity and the ordinary
menstrual cycle. May be after more pregnancies with ordinary
cyclicity in between, you at last reach the ‘large cycle, the
climacteric, where you experience the menopause and your
organism again reaches a new hormone balance in quiet pace.
September 1986
For some years you then will go on this balance until old
age and death.
The female doctor and psychoanalyst Thercse Benedek
wrote a paper, ‘Climacterium a Developmental Phasc’(1950).
She found that psychodynamically the female sexual cycle
involves a greater integrative capacity within the personality.
Thus when the approaching menopause diminishes the
fulctuations of the sexual drive, the ego is flexible enough
to use the energies released from previous tasks for new
integrations. In other words, the female cyclicity is an
advantage because it creates flexibility to manage new life
situations and use the energies in a new and satistying way,
as may happen in the climacteric.
Margaret Mead talked about the postmenopausal zest and
as you know she herself enjoyed her zest and many of her
world famous works were made in her postmenopausal
phase.
Karen Blixen, Danish female author, wrote in The
Caryatids, an Unfinished Tale (1957), “He watched the figure
of his wife, sunk in musing in the carriage seat. He recognised
the thoughtful mood which had come over her, the wave
motion of her being, following the rhythm of the moon like
the tidal waves of the sea. It was as if a weight was being
gathered grain by grain, within the depth of her, balancing
down her vitality into a new calm and a deeper under
standing. Sometimes she would disappear from him
altogether for a day or two, but only to come back, radiant,
as from a flight into a distant world from which she brought
with her fresh flowers to adorn her home? When we talk
about the female cyclicity, the phases in our lives, in this way,
it is difficult for many of us to recognise ourselves. Also in
my daily life, femininity is quite different from the way I have
tried to describe it here.
Menstruation
You see the problems clearly in advertisements. An ad from
a Danish paper “Girls! Be balanced every day! Menstrual
days and the climacteric don’t need to be problems! Take the
new Melbrosia.pill every day!’ The advertiser trusts in our
imbalance and especially in that we feel it.
In an ad for doctors, the drug company offers hormone
therapy for premenstrual syndrome (PMS) and the pill is said
to remove irritability, crimes, accidents, breast tenderness,
emotional turns, headache and so on. This is an audacious
claim by the drug company, because premenstrual syndrome
lacks scientific proof. In connection with this ad we had a
debate in the Danish media. Fhmale doctors emphasised that
crime and accidents primarily are male problems and that
it was farfetched to believe that women should need treat69
ment with hormones to prevent crime. After a long debate
the company at last admitted that the ad was not objective
arid it was then withdrawn. In a mass-circulating newspaper
a cartoonist showed his new understanding—his cartoon
showed a battered woman calling the drug company, “Can’t
you produce some similar hormones for my husband—but
they have to work every day!’ Menstrual troubles' Symptoms,
course of disease, treatment, is the title of an informative
book for all women. It was published after the debate, and
the author is one of our prominent gynaecologists. From an
illustration in the book you see the endometrium changing
through the period. At the top of the picture is an illustration
showing how the woman feels*. She looks free and well until
the last days before menstruation. Then she is shown to be
sitting down and she looks like a person who is unable to
do reasonable things. It is interesting to look at this picture
and at the same time be conscious of the fact that this is
never scientifically shown to be a normal situation for
women. Some healthy women can feel negative sensations
in the days before menstruation, but other women can feel
the opposite or nothing and this is totally forgotten in
medicine.
In medicine a woman is regarded as a handicapped man.
It is considered a negative factor that she may be
premenstrual or menstrual or in ovulation and that she may
be pregnant or in puerperium and for a certain period she
may be nursing and later she will experience the worst, the
menopause. A women is thus always in a ‘special condition'.
She is never okay, but what about the original model, the
man?
Some female doctors have studied ‘the man’ and we plan
to publish a book with the title, Testosteron troubles:
Symptoms, course of disease, treatment. As yet nobody has
taken care of the poor man with this strained condition. We
will stress, that the level of the man’s testosteron concentra
tion in blood is nearly always the same, and as everybody
knows, men are always in the same spirit. But many men
suffer from testosteron poisoning, and they are in the same
aggressive condition all the time. We hope very much that
we can help them, but until now we have no sure and certified
method of doing it.
Giving Birth
In Denmark nearly all women give birth in hospitals and
both the labour and the condition of the child are monitored
in several ways. It is difficult to imagine how women giving
birth will be able to experience the many sensations and great
moments in their lives, when they are treated as patients in
the hospital milieu. We know that women nowadays are at
a larger and larger risk of having to undergo Caesarian
sections so that their experience of giving birth will be an
experience of being under narcosis. 'And what about the
children? Is it good for them to come into the world and
live without the normal experience of birth? Of course it is
advantageous that w'e have the possibility of a Caesarian
section when it is really necessary, but is it with advantage
that we perform the operation more and more?
Climacteric
In ads for the climacteric the drug companies tell us that
we can do something for this otherwise hopeless situation.
70
Hdrmonc therapy solves the problems. The atmosphere in
illustrations is depressing and resigned and often against the
background of rainy weather or autumn.
In Denmark two well-established male gynaecologists have
written an ‘informative’ book about the climacteric. It is
issued in the same series as the book about PMS mentioned
above. The title is, The Climacteric: Symptoms, Courses,
Treatment. The book has illustrations presenting the woman
before and after the menopause. You see a profound change
between these illustrations. The postmenopausal woman is
fat and her appearance is totally without charm. We must
wonder why male doctors want us postmenopausal women
with zest to identify ourselves with such pictures of women.
The diagnosis of the menopausal syndrome was first
introduced to English-speaking doctors late in the last
century; and it became an instant success. Joel Wilbush (1981)
in an article, “What’s in a name? Some linguistic aspects of
the climacteric ’’ views the diagnosis of menopause as a
‘wastebasket’ and the introduction of this diagnosis in the
last century gave little offence. It was an excellent label which
satisfied doctors and patients alike.
It is important to stress the lack of proof of the connection
between mental illness and menopause. In Sweden Tore
Hallstrom (1973) undertook a thorough epidemiologic study
of 800 women and found no correlation between the
menopause and mental disorder. In Denmark, a study
including all patients in the psychiatric institutions has shown
no peak in the number of patients in the middle years per
number of inhabitants in the same age group. Weissman and
Kierman (1977) in a comprehensive review of the literature
concluded that there was no evidence that women are at
greater risk of depression during menopausal period.
Many men and women feel that menopause is the worst
experience in the life of a woman. And some even claim, that
it will leave her as a castrata for the rest of her life. In the
treatment of menopause the most important task of the
doctor is to give the women careful and factual information.
It is necessary to distinguish facts and.myths. I would like
to stress once again that no mental disease has ever been
proven to be caused by the menopause. Therefore hormonal
treatment cannot be expected to, and has never been proven
to alleviate such diseases. When the woman is well informed
it is up to her to choose whether and for how long she wishes
to have hormone therapy. The informed choice of the woman
is much preferable to an authoritarian decision by the doctor.
Depression, Thy Name is Woman
Now let us take a look at depression. Depression is a
‘woman’s disease’ and it is up to six times as common among
women as men. Today most psychiatrists and psychologists
agree that we see quite smooth transitions from the normal
sorrow to very deep and serious depressions. The psychiatric
diagnostic apparatus is here, as in many other places quite
uncertain and unstable. In all the professional textbooks you
find the description of the depressive person as passive with
lack of initiative, lack of self-confidence, introjection of
aggression with subsequent feeling of guilt and with a lack
of sexual desire and performance, men are impotent and
Radical Journal of Health
women frigid. Here it’s essential and interesting to remember
Freud’s description of the normal woman and after him,
many other identical descriptions. Freud tells us that the
normal woman is passive with lack of initiative, lack of selfconfidence, as a rule she introjects her aggression and she
cannot show her anger, is inclined to feeling guilt and sexually
she is masochistic. As you can see the two descriptions arc
rather alike. Indeed they are nearly in accordance word by
word. Yet thd normal woman is labelled as masochistic, which
I think many feel is worse than the depressive woman’s
frigidity.
Freud’s and other description of the woman is, I’m sorry,
current also today. Women’s sex role is a norm which in many
ways demands passivity. When passivity is pronounced,
depression will follow. It is more than hypothesis that the
female sex role in many cases is the same as mild depres
sion. And when the woman experiences psychological
traumas, strain and so on, she overplays her female role as
a defence and then she develops a more severe depression
(Willadscn, 1983).
The bringing up of girls is an upbringing to passivity, to
potential depression. In many situations it can be easy to
be passive and it is important to understand the tempting
aspect of convenience of the female sex role. You can identify
female passivity and helplessness in many ways.
Have a look at the language. Sheila Rowbothan says in
Womqn’s Consciousness, Man's World'. “As soon as we learn
words we find ourselves outside them. We need a language
which constructs the reality of women’s strength, women’s
power. When you arc angry and want to express your strength
and power, you have not your own words for it”.
The normal result of the normal upbringing of a girl, is
a mild, attractive and kind woman and whatever happens
she will stay by her man. Often she cannot manage to accept
this normal sex role, and cannot -find her psychic balance,
and then, nowadays, very frequently she ends up a depressed
woman. The depression is for her a flight from an intolerable
life situation and in the depression she can relate to her
surroundings although in a negative way.
Hysteria
In other cases the women ends in another exaggeration
of the female role, the so-called hysterical personality. In the
leading Danish textbook of psychiatry our first psychoanalyst
(Vanggaard 1985) as late as last year writes about the classical
hysterical personality, “A known, example is the colourful,
lively, attractive and seductive woman, but it turns out that
she is not serious. In intimate sexual relationships she is
frigid. Even outside the narrow erotic sphere the inviting,
charming and seemingly emotional attitude of these persons
can impress people—often resulting in disappointment at a
larger moment!’ The editors of the textbook, five other male
Danish psychiatrists, all in high positions, have not com
mented on this outpouring. You see the alarming distance
from women’s reality. It’s the same in many well-known
international textbooks.
In the USA’s diagnostic statistical manual, the commonly
September 1986
used diagnostic system in the States, DSM III, the term
hysterical personality is abandoned and it is now called
‘histrionic personality disorder’. In the description in the
manual you sec that the histrionic personality is described
in the light of the usual oppressive concept of women. There
you read that histrionic personality disorder is diagnosed far
more frequently in females than in males. Such individuals
arc typically attractive and seductive, superficially charming
and appealing. They arc demanding, egocentric, and
manipulative. They may be sexually unresponsive and in both
sexes overt behaviour often is a caricature of femininity. All
these pejorative descriptions are known in all sorts of
psychiatric literature. The hysterical or histrionic woman is
accused directly of looking lovely and being attractive and,
at the same time, of being unreliable in their sexual
accessibility for men. They bypass the traditional norms and
are accused of using the femininity in order to manipulate
the surroundings. The textbooks forget the simple fact that
behaviour that is rewarded will be promoted. The behaviour
of the hysterical women is, of course, determined by their
living conditions. The essential issue is the deleterious lack
of real female life realisation. Hysterical symptoms act as
a substitute and they can be regarded as a caricature of the
demands to women’s behaviour in general and her sexual life
in particular. Hysterical symptoms are distorted communica
tion with the surroundings and an attempt at protest against
the conditions. The hysterical person lives under the motto,
“Don’t* think, don’t know, don’t feel”. You have to act as
another alien person and to satisfy the needs of other instead
of your own, and at that be so kind as not to see through it.
In the Danish textbook the psychoanalyst also writes about
the spouses of the hysterical patients. He finds it surprising
what many spouses are willing to acccept the hysterical
personality. There is really no basis for surprise. Lawrence
Durrell formulates so shrewdly: “We get the partner who
corresponds to our own inner ugliness, i e, when we look
for a partner, our negative aspects will be decisive, while the
positive aspects will be without any consequences, because
they will be accepted by everybody. The hysterical woman
will often marry a special type of man, superficially he is
clever and permissive in relation to her, but if you analyse
the relation, you will often understand that he plays his own
game. For his own good he keeps to the hysterical because
he experiences himself as strong and important and as safe
as possible in his male role. At the same time he ‘fixes’ her
symptoms because he can’t do without.
The label frigidity is often linked to the hysterical.
Sexologists have tried to replace frigidity with general sexual
dysfunction of the female. They have tried to be progressive,
but in vain. Frigidity is essentially the women’s skewed protest
against participation in the traditional sex life, when
everything is dictated by the wishes and needs of the man.
She experiences all of it as an attack against her integrity.
Many womens suffer from lack of sexual life realisation. The
woman’s common inclination to passivity explains that she
often finds herself to be, what we call, frigid or suffers from
sexual dysfunction.
I have read Sheila Kitzinger’s Women's Experience of
71
Sex (1983) with great profit, and in many ways I agree with
her. She writes in the postscript that she has learned much
from writing tile book. Before writing the book she took it
more or less for granted, that sex therapists must be right
when they talk about female sexual dysfunction and when
they often use therapies to help women adapt without ques
tioning the social values and codes which impose on us par
ticular kinds of sexual behaviour and assumptions about sex.
It’s a fact that nearly all diseases occur with a skewed
sex-distribution. In every textbook you find the unequal sex
distribution mentioned. But without any analysis and
without recommendations for prevention and cure of the
diseases in this light. Drugs are used widely and it is alarming
that many, many healthy women arc medicated in several
ways. In gynaecology, hormones, as I mentioned before, are
often used in the treatment based on myths about women’s
biology and sexual life. The same happens in some cases of
gynaecological operations. In general practice the treatment
very often is a drug treatment and it is the general practi
tioners who prescribe most of the psychotropic durgs. Most
of them are sedatives but they also issue many prescriptions
for antidepressives and neuroleptics.
The pharmaceutical industry is aware of the sex of the
doctor and the sex of the patient,. In the ads you often find
the attractive woman, with a nice hairdo, make-up and
posture and the elderly grandfather-like doctor—he usually
has grey hair and a bald spot on top of his head just to inspire
confidence. If his patient is a hysteric who cannot manage
her frigidity or a depressive who suffers from passivity and
lack of self-confidence, where can she go for better treat
ment, than to the psychotherapist?
Many patients feel that the psychotherapist puts them back
in their box and not to a worthy life outside the fixed
conventional role. The male society makes its demands. A
woman has to be the good wife and mother and at the same
time she is expected to be attractive and be able to manage
competition from pornography.
Can men (as psychiatrists or doctors) treat women? It is
a difficult question, because it depends on the scope of the
treatment. In the treatment of the weakest patients it
necessary to work with very limited purpose. It’s a sort of
camp hospital treatment at times where you cannot free the
patient from war. If the possibilities are better and the woman
has resources and can depend on a supportive social network,
then she can go ahead and develop her personality. I’m sure
she needs help from others who understand her suppression.
Some few male doctors do, and honestly many female
doctors do not. We are educated in the male medical world
and we have internalised so much.
Voluntary helpers and sejf-help groups sometimes can be
good solutions for women with psychic problems, but often*
they have very few resources. It can be difficult to offer the
necessary steady help. The society should on one side support
the pioneering initiatives and on the other side, learn from
them and transform the established treatment apparatus
accordingly. More importantly than appropriate treatment,
we need to raise the woman from childhood to a realistic
concept of her own biology and psychology. Then she will
appreciate her cyclicity and not be apt to biologise her
problems, and more or less unconsciously overplay the
72
normal sensations in the female biological cycles. We need
to be conscious of our problems and try actively to solve
them. We will define our femininity ourselves rather than
to accept the traditional definition put forth by men.
When we meet psychic problems, it’s necessary in the
earliest phases to be active, to take responsibility for
ourselves, to use our anger and aggression and not to
introject all of it. In every way we have to counteract the
objectification of women in our society. I think our sex life
is most important. We must be aware of our sexual position.
Clara Thompson (1942) wrote, “The characteristics and
inferiority feelings which Freud considered to be specifically
female and biologically determined can be explained as
developments arising in and growing out of western woman’s
historic situation of underprivileg, restriction of develop
ment, insincere attitude toward the sexual nature, and social
and economic dependency. The basic nature of woman is still
unknown!’ The basic nature of woman is still unknown, we
must acknowledge. We owe our children, our species to
discover it. We need to think, to know, to feel, if we dare,
and if we manage it will give our species a much-needed
survival value.
[Paper read in a slightly modified form at the 2nd Inter
national Feminist Bookfair, Oslo, June 21-27, 1986]
References
Bcncdck, Thercse, Climacterium: A Developmental Phase, The
Psychoanalytic Quarterly, 1950; T9: 1-27.
Blixen, Karen, The Caryatids, An Unfinished Talc, in Isak Dinesen,
(edited by Karen Blixen) (Last Tales), Putnam, London, 1957.
Hallstrom, Tore, Mental Disorder and Sexuality in the Climacteric: A
Study in Psychiatric Epidemiology, (DISS), Goteborg, 1973.
Kitzinger, Sheila, Woman's Experience of Sex, Dorling Kindcrsley,
London, 1983.
Thompson, Clara, Cultural Pressures in the Psychology of Women,
Psychiatry, 5, 1942: 331-9.
Vanggaard, Thorkil, Ncuroser, 1 Weiner J, Reisby N, Lupn V, Rafaclsen
OJ. Schulsinger F (eds): Psykiatri: En tekslbog, FADL, Kobcnhavn,
1985.
Weissman, Myrna M and Klcrman, G L, Sex Differences and the
Epidemiology of Depression, Arch Gen Psychiatry, 1977; 34: 98-111.
Wilbush, Joel, What’s in a Name? Some Linguistic Aspects of the
Climacteric, Maturitas, 1981; 3: 1-9.
Willadscn, Jyttec, Depression, dit navan er kvinde: Mandsvadde. or
helbred, Lindhardt and Ringhof, Kobcnhavn, 1983.
Jyttce Willmlsen, M I)
Copenhagen County Psychiatric Hospital
Nordvang
DK-2600 Glostrup
Denmark
RADICAL JOURNAL OF HEALTH
Forthcoming Issues
December 1986: Vol I no 3 : State Sector in
Health Care
March 1987: Vol I no 4
: Medical Technology
June 1987: Vol II no 1
: Agrarian Development
and Health
September 7 987: Vol II no 2 .■ Health Issue in
People's Movement
Radical Journal of. Health
Dialogue
Organising Doctors: A Difference in Approach
Sujit Das
ANANT PHADKE (SHR, II (3) p 151-2) in his critique of
my article (SHR, II p 57-66) has chosen to employ rude
words e g, “shame-faced defence of the interests of the doc
tors”. Rude words may have their appropriate uses but,
as I am inclined to believe, are never known to be good
substitute for argument. To confess, my article has not been
intended to be any sort of defence of anyone and I have not
happened to feel any sort of shame in informing certain
aspects of a certain section of the medical profession which
is yet ill-understood. Reading Phadke’s own article (SHR,
II (3) p 198-50) on the same topic I find I can identify the
difference between our basic approaches to the problem but
before that let me clarify a few minor points raised by him.
Phadkc takes me to task for my original title “Medical
Profession in Health Care” which the working editors
thoughtfully changed to “Doctors in Health Care” in order
to, I presume, save me from ignominy. Phadke claims that
the “medical profession being only doctors” is a popular but
mistaken notion and it should include nurses, social health
workers, etc. On the other hand, I had no intention to sud
denly change a popular category of almost.universal usage
and if I did, I am sure, would have invited another, irrele
vant debate. I do not feel much enthusiasm to emulate the
purists’ example of using the word ‘doctor’ for only medical
doctors which is also a popular but thoroughly mistaken
category. Phadke insists that general practitioners should be
said to be involved in “petty commodity relations” and not
“precapitalist mode of production” because the former is
a “part of a capitalist social formation”. Frankly, I do not
understand the significance of the difference between the two.
The production relation of the GP is neither capitalist nor
post-capitalist and further, it is also a part of pre-capitalist
social formation.
In his own article, Phadke deals with the subject from
the traditional and over-worked idealistic approach to which
I alluded in my article: “The profession has hardly beenlooked into as what it is, but often analysed on the basis of
what it should be.” That is why, Phadke wants to organise
the doctors towards the end of fulfilling the tasks set by his
own lofty ideal. He starts by uncritically superimposing the
formulation of a particular western school of analysts on
the Indian situation. This school categorises the highly skilled
wage earners of advanced capitalist society as “new middle
class” and Phadke adopts this formulation to place'the:
Indian wage-earning doctors to that class and therefore
attributes them similar contradictory role towards social
revolution.
ThiS he does without even a cursory glance to the Indian
reality. By no stretch of imagination could the Indian society
be labelled as an advheed capitalist society. The section of
Indian wage-earning doctors is yet to be consolidated in a
well-defined social layer. In my article, I have briefly narrated
the social events which tend to show that this section of doc
tors is in the process of consolidating towards a distinct social
layer, quite different from the other sections, under the in
Sep tember 1986
fluence of objective forces—particularly economic and
political—despite individual tendencies to the contrary.
Again, I find that Phadke’s assignment of these doctor’s role
in the function of Capital (according .to the same formula
of new middle class of developed capitalism) is at variance.
with reality. I have not found these doctors, as a class, per
forming “the function of capital, of supervising, extracting
work from the paramedics” in order to earn a part of the
surplus value (from unidentified source). In fact, the current
trend shows different picture. In Bihar, UP and West Bengal,
this newly organising band of doctors has joined hand with
the already unionised hospital workers in common struggle
on common demands—particularly trade union—and
democratic rights. Phadke’s estimate that these doctors earn
a “comparatively high salary” also appears, devoid of
clarification, to be another borrowed assumption. With
whom has this comparison been made? With employees of
the lower hierarchy, or with employees of the same hierarchy
or with their work value/utitlity value/market price?
From this dubious promise, Phadke asks the left “to
determine its strategy of .organising’this layer of doctors”
He castigates the leadership of the doctors’ organisations for
organising them on a trade union platform; discounts trade
unionism itself as unworthy because this will only consolidate
their already earned privilege; laments that there is no “well
thought out strategy in organising doctors; and calls for
appealing towards a small section of enlightened doctors “on
the basis of comprehensive revolutionary medical programme
which asks doctors to throw away their privileges as elite doc
tors in return for the promise of decent, meaningful work
ing life.”
Weil, there may not be nobler ideal and more
humanitarian appeal to the heart and conscience. But such
idealistic approaches have never helped. Trade unionism does
not owe its origin and development to anyone’s desires and
wishes. Trade unionism develops from objective compulsions.
Economism is one of the primary driving force behind trade
unionism. Forgetting that we live in a country where even
the mature organised working class itself is bogged down
in economism, Phadke is so angry with doctors’ trade
unionism that he admonishes me for giving importance to
the West Bengal doctors’ movement in 1974 which did not
raise any slogan in the peoples’ interest. I do not understand
why narration of fact or event should be taken as shame
faced defence? Rather I believe it is of no use theorising
without a look at facts and events. TYue to his disinclination
to face facts, Phadke has missed an entire paragraph in my
article where I narrated the subsequent events revealing how
the doctor’s organisation later came to. understand the linkage
between economic aspirations and egalitarian health care ser
vice and raised, an entirely new’set of demands voicing
people’s interests.
Contrary to Phadke’s assumption, I have not tried to
determine doctor’s role in social revolution—certainly not
at this stage. I wanted to draw an eventful picture of a sec
73
tion of the medical profession in the perspective of hard myth of noble profession, step out of our idealistic world
reality. Because I found that the observers almost always of believe and turn a fresh look towards doctors as just a
dealt with the medical profession from individual presump social layer with the relevant particularities. We have to col
tions and pre-determined positions without bothering to sift lect real life data and analyse them. We have to know how
empirical findings. Even the bitter critics of doctors have the doctors practise medicine in the state hospitals, how they,
fallen prey, perhaps unwittingly, to the concept of noble pro as a class or interest group, interact with the recipients, non
fession and, for no coherent reason at all, expect the doctors doctor workers and the employer. In this context, discussion
to remain unaffected by the nuances of the commercial on professionalism, role expectation, role performance, as
society and to conduct themselVes as holy men. Hence, the well as agitative movenjents become relevant.
exploitative practice of the doctors which is an utter con
When we do this, we may be able to understand and
tradiction to the ideal of noble profession, shocks them. Whv
determine the service-doctors’ role on the basis of their own
should the noble doctors behave as other wage-earners do?
conduct and not through any wishful thinking. Then only
Why should they indulge in trade unionism and economism
will we be in a position to determine their relationship with
as the common workers do? Why should they demand
a people’s health movement for a just health care service. The
8-hours duty as everyone does? Why shouldn’t they, as noble
relationship—I quote Thompson again - "must always be
ones, "throw away their privileges as elite doctors in return
embodied in real people and in a real context".
for promise of decent, scientific, meaningful working life’’,
as the other commoners'do not do? When these doctors do
Without going into details, I may draw attention to the
not oblige. Phadke goes searching for a "small critical mass experience of USSR and China. There, in the post
of doctors’’ who may persuaded to raise a sufficiently strong revolutionary period, the state had to deal with the entire
clamour for "a revolutionary change" in the medical system., medical profession in reshaping health care service. Revolu
I have little hope* he will find one and even if he is for tionary exhortations were found to be inadequate. The
tunate to find them, his ideal may remain unrealised. One instrument of incentive and disincentive was ultimately
thing is certain. We cannot run a medical system without resorted to and it brought results. The problem has yet to
doctors—certainly not by a small critical mass of revolu be resolved. Professionalism, job satisfaction, econornism,
tionary doctors. Before jumping ahead to determine the role role expectation, role performance, private practice,
of doctors in social revolution, let us try to understand and technocratic scienticism etc, are still living problems.
determine their role in health care. What role do we envisage
References
for the doctors in today’s health care? What are they perfor
Phadke,
A:
’
One
sided
defence
of professional interests’, SHR, II (3),
ming? What are the nature and cause of short-comings in
151-2.J985.
role performance? What changes should we demand and
K: ‘Doctors in Health Care: Their role and class location’, SHR,
strive for in the medical system and what will be the role Das^S
II, (2), 57-66, 1985.
of the doctors in such dynamic situation? In order to find Phadke, A: ‘Organising Doctors: Towards What End?, SHR, II (3)
answers to these questions we have to purge ourselves of the
148-50, 1985.
Light on ‘Blind Spots’
u n jajoo
ANANT PHADKE in his review (RJH, June I: 1) of our
book FFAen the Search Began contends that: "It is not clear
from their account as to why the response to this scheme
was better than to the earlier one. No economic or political
activity has been reported. Perhaps the support of the
medical college including the doctor’s monthly visit made
this difference."
This and other such statements need some clarifications.
The insurance scheme demanded Rs 3/person/year as con
tribution from 75 per cent of the village population and
offered hospital services at 75 per cent subsidised cost (See
Introduction). Though highly subsidised, hospital charges
were beyond the reach of poor villagers. The Jwar Insurance
Scheme provide free hospitalisation for all unexpected
illnesses and thus provided a sense of security. It was essen
tially this modification which attracted people and not any
economic or political activity.
Regarding Phadke*s comments on cost analysis, a close
took. at the cost analysis will reveal the following:
Hospital indoor admission rate per year = One per 10 population
Government expenditure for 10 people 28x10 * Rs 280/year
74
Contribution from the people = Meets the cost of peripheral health
infrastructure plus spares Rs 18.50
Therefore the amount which can be spared for hospitalised treatment
per patient = Rs 280 plus Rs 18.50 Rs 298.50
With a proper referral established between the hospital and
the specialised care hospital, I feel that.with the amount
available, and health insurance coverage for indoor admis
sions can be provided. It is futile to compare this cost-analysis
with existing government PHC set-up where distribution of
funds provides only 12 paise/person/year towards drug cost.
What is important I believe is that the alternative strategy
appears feasible.
Elsewhere Phadke comments that the increase in percen
tage coverage for health insurance from 46.5 in the first year
to 71.5 per cent in the third year does not tally with the earlier
claim. The data quoted earlier is from village Nagapur—
the village where by trial and error health insurance scheme
evolved over the years. The data on increase in coverage (on
page 14) is pooled information from the new villages where
health insurance scheme was introduced and then imple
mented once it was found feasible. The strategy of our entry
Radical Journal of Health
in village life was totally different.
As lor the ‘blind spots’ the search continues. We began
with what was possible in the given social structure, invol
ving people to the maximum, without corrupting them with
blind charity. The ‘blind spots’ can only be eliminated when
really democratic health services evolve. What matters today
is whether there are attempts towards the democratisation
process.
We did try towards decentralisation, e g, village contribu
tion is now collected by villages and is kept in the village
as a village fund. Its utilisation is now decided by gram
sabha, thereby controlling the village health workers perfor
mance. The attempts towards appropriate health education
was the natural corallary but the extent to which attempts
towards ‘conscientisation’ can breed ‘health actions’ is a
question we have yet to answer.
It must be understood that for me goal of democratisa
tion to be achieved the consumer should be participating.
For people’s participation to emerge, a felt need has io exist.
The needs cannot be created. If need-based participation
ensues, it has to be guided towards democratisation, the value
which under-privileged section rarely visualises. It is here that
the role of activist lies. The vision of democratisation is
perceived by those individuals who can see beyond the
immediate gains, i e, people who join the struggle through
conscious committment.
As far as health work is concerned it is a moot question
whether the consumers arc motivated enough to actively par
ticipate. In case they arc not, health work remains “for the
people’’ and not “by the people? The experience narrated
in the book describes our march towards “for the people?
Though conscious of the goal “health by the people’’, we
stumbled against the reality, that health is not a priority need
of the people and hence we did not sec community participa
tion emerging.
One should not compare the strategy of work at organised
sector like the Chattisgarh Mines Shramik Sangh and among
unorganised rural agrarian population. Running a hospital
by contributions from the beneficiaries is not new. What
matters is how far the democratisation has been inculcated
in health actions. Il will be a nice idea if someone from
Rajhara hospital shares his/her experiences of the demo
cratisation process in health action, its feasibility and failures.
U iX Jajoo
Department of Medicine
Medicial College
Sevagram, Wardha disc
Maharashtra
MERIND
MERIND LIMITED
New India Centre, 17, Cooperage Road.
BOMBAY-400 039.
September 1986
75
ECT and Drug Therapy: Is There an Alternative?
AR
IT is true that medicalised attitude towards psychiatric
problems is a misdirected one and we have to look at psychic
disorders in a holistic way (SHR II: 4). But can we totally
reject the use of drugs or even electro-convulsive therapy in
psychiatric illnesses? The articles tend to suggest this by
denouncing psychiatry in toto, without giving an adequate
basis for such a total rejection.
To begin with, we must distinguish schizophernia
(madness) from neuroses (“queer behaviour’’). It has been
well-established that there is some genetic factor involved in
schizophrenia. Moreover, some schizophrenics become
violent cither to others or to themselves; many cannot take
care of their bodily functions. It is almost impossible to keep
such a person in one’s house without treating him/her with
powerful drugs or electuroconvulsive therapy (ECT). Like
any other medical therapy, ECT may have its own risks and
disadvantages. If the medical establishment is hiding these,
or glorifying ETC, we must oppose it. We need a better mode
of treatment then ECT. The scientific basis of how and why
of ECT was not at all clear when it was started and is still
not clear today. But this empirically established form of
treatment is on the whole quite helpful in tiding over crises,
and in reducing hospitalisation and in the absence of a better
alternative, cannot be rejected. Are there any alternatives
better methods of treatment available? Where is the proof?
Similarly, powerful psychotropic drugs also reduce
hospitalisation. These methods of treatment many-a-time
convert the schizophrenic into a passive, dull individual. A
few who do not require long-term treatment may become
almost normal but many others loose vitality in their life.
But again—is there a better alternative?
Schizophrenia is not simply “deviant*’ behaviour. It is quite
troublesome and often may be dangerous to others. If it is
considered as a revolt against the society, how should society
react to it? In a social political revolt, there are certain definite
demands. But the schizophrenic does not have any such
demands.
What is precisely wrong in conventional psychiatry is the
medicalised conception of schizophrenia. ECT and drugs are
not looked upon as temporary resorts in extreme conditions,
but as the solution. Though there are genetic factors involved,
stressful life situations, continued tensions and humiliations
are often responsible for converting a genetic potential into
the reality of madness. Instead of being sympathetic to the
patients for the sorry state to which the society has brought
them, the victims then are blamed, castigated and the role
played by social-cultural conditions in creating this illness
is forgotten. Unlike neuroses, a change in the family or
work-environment may not bring the schizophrenic back to
complete normalcy. In this regard, one is tempted to compare
schizophrenia with byssinosis (a bronchitis-like condition
found in cotton-mill-workers which is caused by continuous
exposure to cotton-dust; once developed, it cannot be cured).
Like byssinosis and many cancers, schizophrenia can be
prevented. But once the damage is done, it can rarely be
reversed. The real solution to schizophrenia is to create a
society which would not create such stressful situations which
foster schizophrenia. Even then, there may be a few people
going mad, but to be sure, the incidence can be brought down
considerably. But in the present circumstances, all that the
medical people can do is to be sympathetic to the patient,
to use urugs, and so on when essential and identify the family
and society as an important cause of this malady.
In neuroses, the family and the society at large are
completely responsible for a person’s neurosis; there being
no genetic factors involved. Early detection of “strange
behaviour’’ and identifying the cause in the immediate
interpersonal, social surrounding may help a lot. If the
situation around such a person continues in the same fashion,
the person may end up with serve neurosis and then the
person may never revert back to complete normalcy; years
of illness-creating-environment create a change which cannot
be easily reverted. Drugs can only be useful to tide over a
crisis. But by no means are they the real solutions.
In the absence of a holistic view of mental health and
illness, and also due to vested professional or business
interests of psychiatrists, and the drug-companies, psychiatry
has been overused, abused. This fits well into a society where
there is a culture of scienticism, compartmentalism. This
overuse, misuse of psychiatry has to be opposed. We need
to create a countertendency in addition, which identifies
concretely pathogenic interpersonal and social practices, their
economic-political basis. Such a countertendency has also
to evolve and practice ‘an alternative, healthy culture to
demonstrate an alternative. The seed for socialist, healthy
culture has to be sown today! But I doubt whether ECT or
drug therapy for those who are already ill can be totally
rejected.
SUBSCRIPTION RENEWALS
Is this your last subscribed issue? A prompt renewal from
you will ensure that your copy is mailed directly from the
Press. Many of our issues have sold out fasti So book your
copies by renewing your subscription now!
Our new subscription rates:
For individuals—Rs. 30/- (four issues)
For institutions—Rs. 45/- (four issues)
Foreign subscriptions: US $ 20 for US, Europe and Japan
US S 15 for all other countries
(special rates for developing
countries)
Life subscription: Rs. 500/-
D D s cheques, IPOs to be made out to Radical Journal
of Health. Kbay. Please write your full name and correct
address legibly. And please don't forget to add Rs. 5/- on
outstation cheques.
Radical Journal of Health
76
Why don't you write for us ?
This periodical is a collective effort of many individuals active or interested in the
field of health or interested in health issues. The chief aim of the journal is to provide a
forum for exchange of ideas and for generating a debate on practical and theoretical
issues in health from a radical or Marxist perspective. We believe that only through
such interaction can a coherent radical and marxist critique of health and health care be
evolved.
Each issue of the journal highlights one theme, but it also publishes (i) Discussions
on articles published in earlier issues (ii) Commentaries, reports, shorter contributions
outside the main theme.
Our forthcoming issues will focus on : Medical Technology, Agricultural Develop
ment and Health, Health in People's Movements.
If you wish to write on any of these issues do let us know immediately. We have
to work three months ahead of the date of publication which means that the issue on
Medical Technology is already being worked on. A full length article should not exceed
6,000 words and the number of references in the article should not exceed 50. Unless
otherwise stated author's names in the case of joint authorship will be printed in
alphabetical order. You will appreciate that we have a broad editorial policy on the
basis of which articles will be accepted.
We have an author's style-sheet and will send it to you on request. Please note that
the spellings and referencing of reprint articles are as in the original and are NOT as per
our style.
We would also like to receive shorter articles, commentaries, views or reports. This
need not be on the themes we have mentioned. These articles should not exceed 2,000
words. Please do write and tell us what you think of this issue.
All articles should be sent in duplicate. They should be neatly typed in double
spacing on one side of the sheet. This is necessary because we do not have office
facilities here and the press requires all material to be typed. But if it is impossible for
you to get the material typed, do not let it stop you from sending us your contributions
in a neat handwriting on one side of the paper. Send us two copies of the article
written in a legible handwriting with words and sentences liberally spaced.
The best way to crystallise and clarify ideas is to put them down in writing. Here's
your opportunity to interact through your writing and forge links with others who are,
working on issues of interest to you.
WORKING EDITORS
Please send me Radical Journal of Health for one year (four issues). I am
sending Rs. _____________________ as subscription and/or donation by Demand
Draft/Cheque. (D D and cheque in favour of Radical Journal of Health and
for cheque add Rs. 5, if outside Bombay).
Name
Address
my sin ••••analgin
those were the last dying gasps,
(or so it seemed then),
that were kept 'alive' with galloping agony,
that pushed my life into hopeless despair
fever juxtaposed with spasmodic chills
and that soar throat that quenched my voice
into oblivion,
was signal enough
to let loose
tiny, horrendous microbes,
in tens of thousands, millions and billions,
to pounce on my flesh,
in an effort to strip me to my skeleton.
the healing messiahs,
gathered around me
(in a state of helplessness)
pumped desparately blood into me,
to replenish the granulocytes,
that had vanished from my blood,
thanks to the pain-killer,
which i was prescribed.
i survived somehow.
they said i was lucky.
"it's a miracle,
50 percent don't see through."
' pain-killer? driving me to^the height of agony ?
plunging me into misery ? dragging me to death?
why make such a monster ? "i cried
with a voice that had barely returned.
and the messiahs said,
there were 'profits' in making this monster
"profits"?" i was puzzled.
"profits" they said,
"for companies which manufacture it,"
"profits for the governments which allow it,"
’'profits for the messiahs who prescribe it,"
"but what of me" i said,
"i was pushed into the doors of death."
' oh !" they said,
"you are just one that gets into such a mess,
after everyjhundred thousand."
i wished i was amongst
those 50 percent who did not see through,
for this callousness
was more agonising than the disease.
"but what was my crime,...what was my sin. '
they laughed cynically... "you ingested analgin."
anil pilgaokar
Position: 798 (16 views)