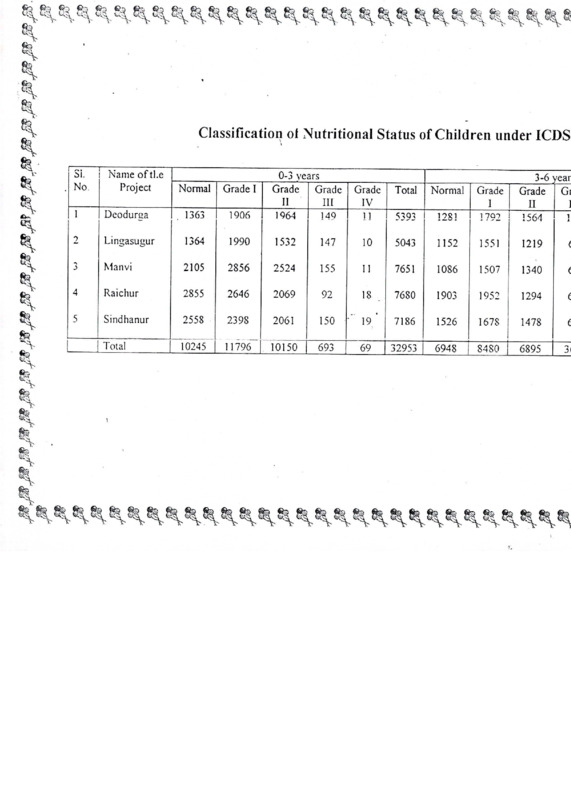
Classification of Nutritional Status of Children under ICDS
Item
- Title
- Classification of Nutritional Status of Children under ICDS
- extracted text
-
Bi
Classification of Nutritional Status of Children under ICDS
r^~
No.
Name of tl.e
Project
Normal
Grade I
1
Deodurga
1363
1906
0-3 years
Grade Grade
II
III
1964
149
2
Lingasugur
1364
1990
1532
Manvi
2105
2856
4
Raichur
2855
5
Sindhanur
2558
| Total
di.
fe1
fe'
1281
Grade
I
1792
3-6 years
Grade Gr
II
I
ii
1564
5043
1152
1551
1219
6
11
7651
1086
1507
1340
6
92
18
7680
1903
1952
1294
6
2061
150
19
7186
1526
1678
1478
6
10245 | 11796"! 10150
693
69
32953
6948
8480
6895
36
Grade
IV
11
Total
Normal
5393
147
10
2524
155
2646
2069
2398
§^
g^
Population and\ Beneficiaries covered under ICDS Progr
SI.
No.
Beneficiaries
Name of the
D r-/> • /*/-*<
x *y
■q
o
O
•U
*0
6
Z
cL O'
o —
- 5 S
C
5 §'
H-g
H <
6~o
H o 8
£ sy
g
Q
O Q
sU) yu.
.2 _y
>
3
£
CO 3
■S >>
116
CN
i
KO
CM
i
^o
s
Ph
-1
Deodurga
171
176900
35040
188
164
164
3078
3078
2738
2738
855
2
Lingasugur
220
262000
41652
191
182
126
4365
3763
4605
2431
1100
Manvi
266
269300
51210
171
164
171
5852
3724
5586
3192
1330
4
Raichur
362
35SSOO
56578
156
142
*113
5847
5847
7312
6028
1733
5
Sindhanur
289
284S00
52822
172
159
135
5344
5876
6100
5616
1445
Total
1308
135180
0
237302
878
811
709
24486
22288
28339
20003
6463
K
%
5
■v
— on
3to
L
i
fe>
tt
£
r
♦
doC■}
CHILD SURVIVAL & SAFE MOTHERHOOD PROGRAMME
GUIDELINES
FOR
OPERATIONALISING
FIRST REFERRAL UNITS ( FRUs )
CSSM PROGRAMME DIVISION
DEPARTMENT OF FAMILY WELFARE
GOVT. OF INDIA
1993
'i
GUIDELINES FOR
OPERATIONALISING
FIRST REFERRAL UNITS (FRUs)
OBSTETRIC CARE (EOC)
FOR
EMERGENCY
INTRODUCTION
The basic strategy for enhancing Safe Motherhood under
the CSSM Programme has the following three components :
I.Essential Obstetric Care for all - will increase the
chances that any complications is detected early.
In
addition,
since foetal and neonatal health is closely
associated with the health of the mother,
improved maternal
health and safe delivery practices will have a positive
impact on child survival.
II.Early Detection of Complications - will increase the
chances of maternal survival.
Many complications require
prompt and appropriate action, which will be more feasible if
problems are quickly recognized.
III,Emergency Obstetric Care - is critical for saving lives,
since the majority of complications leading to maternal death
can not be predicted. Reduction in maternal mortality will
ultimately depend on whether these services are available and
utilized by women who need them.
components
Safe
services,
of
Some
Motherhood
particularly
essential
those which will contribute to
obstetric care for all , are already in existence as a part
of the CSSM Programme in all districts of the country.
The
challenge now in areas such as IFA prophylaxis
TT
,
immunisation and safe delivery is to improve coverage through
better systems of service delivery and demand generation
through communication efforts. These interventions can have a
positive impact on the overall perinatal and maternal health.
The most important measure for reducing the maternal
deaths now , however, is the provision of emergency care for
women with obstetric complications. Since a large proportion
of these complications can not be predicted,
it is essential
that adequate treatment is made available in time. Hence, the
First Referral Units (FRUs) will play a pivotal role in
reducing the maternal mortality by providing timely emergency
care to women with obstetric complications.
WHY SET UP FRUs ?
The 'model plan' for primary health care , adopted
by the country in 1978-79 envisaged that there would be a
Community Health Centre (CHC) for every one lakh population
1
by the end of 7th Plan period. Every CHC is
to have a
minimum of 30 beds and 4 specialists (either qualified or
specially trained to work as Surgeon, Obstetrician, physician
so that it could provide specialised
and Paediatrician)
medical care to the cases referred by the Sub-centres and
Primary Health Centres under its jurisdiction.
However , the CHC set up has remained weak in
terms of
providing the referral support to the outreach
facilities ,particularly in the six States of Assam ,Bihar,
M.P.
,Orissa , Rajasthan and U.P. This has been confirmed by
the data collected under the Health Facility Survey , carried
out in 21 districts of the country in 1992 by the Institute
for Research in Medical Statistics (IRMS), an associate body
of Indian Council of Medical Research (ICMR) . The Survey,
categoried all institutions at block headquarters,
which
and/or those having specialist posts (sanctioned)
as a
potential referral institution , revealed that most of the
block level institutions still remain, in structure, closer
to the concept of a Primary Health Centre, having 6 to• 10
beds, though having an average of 3-5 medical officers, The
main aspects of the findings , in this regard for 6 of the
districts covered in the survey , given below , will
substantiate this observation :
District
Referral hospitals/CHC/Upgraded PHCs/
Popn.
(in lakhs) Block PHCs
Reqd.
Set
up
no.hav no.hav- no.having
ing OBG 30 beds ambulance
specialist
Sanct- in posiioned tion
Gaya, Bihar
Dhar, M.P.
Raisen, M.P.
Jodhpur, Raj.
Kota, Raj.
Banswara; Raj.
26.60
13.00
8.80
21.00
12.00
11.00
27
13
9
21
12
11
20
15
9
16
10
10
0
5
5
5
1
3
5
0
4
1
1
2
2
1
6
4
5
0
5
4
4
5
8
It is in the above context of the poor availability
of specialised emergency care for pregnant women , which has
been a major cause of maternal deaths , that the CSSM
Programme envisages setting up a network of sub-district
first referral units (FRUs) ,through a process of selection
from the existing institutions ( CHCs, Block PHCs, upgraded
PHCs and rural hospitals etc.)
2
SELECTING THE FRUs
Most States , during planning workshops , have
adopted a goal / norm for providing one FRU for every 3 to 5
lakh population which means that the number of instituitons
to be selected for developing the FRU network will range
between 6 to 12 such units per district ,depending upon the
population .
is to be
The identification of FRUs ,as noted above ,
done through a process of selection from amongst existing
CHCs, Block PHCs , Referral Hospitals , Upgraded PHCs and
Rural Hospitals etc.
, with due regard to availability of
physical facilities ( beds reserved for obstretic care and
operation theatre etc.) manpower, particularly OBG specialist
and performance of obstretic care services in the recent
past. The process of identification should also include an
indication
of the strengthening required in terms
of
additional physical facilities and manpower that would be
required for each of the recommended FRUs.
As mentioned earlier , IRMS (ICMR) has conducted a
health facility survey (HFS) which provides details of the
equipment, patient capacity, infrastructure and staff skills
available at all government health institutions in the
district, The States/Districts , who have been provided with
the reports of the HFS done in 21 districts , should review
the survey report, and finalise the institutions that are to
be upgraded as FRUs.
For those districts where no HFS has been carried out,
identification of units to be upgraded as FRUs should be made
on the following criteria:
a)
b)
c)
d)
location; geographical distribution
availability of medical manpower
current utilization of services
basic infrastructure (building, electricity,
water supply)
and
As a minimum,
facilities should have a labour room and
However, in districts where too few
an operation theatre.
facilities meet these criteria, additional units may be
chosen for upgradation in future.
FUNCTIONS OF FRUs
The functions that every FRU must perform and the
minimum skills necessary for each of the functions are given
below:
3
A: SURGICAL FUNCTIONS
SKILLS : - Laparotomy & repair of rupture uterus
- C-Section
- Repair of cervical & vaginal tears
- Uterine evacuation for incomplete
abortion (D&C)
- Amniotomy with or without Oxytocin '
- Surgical treatment of severe sepsis
B: MEDICAL TREATMENT FUNCTIONS
SKILLS : - Use of IV Oxytocin for augmenting
labour
- IV infusion of iron
- Management of severe hypertensive
disorder of pregnancy & eclampsia
- Management of haemorrhagic shock
C: BLOOD TRANSFUSION FUNCTION
SKILLS : - Cross matching of blood
- Bleeding a donor & giving blood
transfusion
D: MANUAL FUNCTIONS
SKILLS : - Version
- Manual removal of placenta
- Forceps delivery
- Vaccum extraction
- Partography
E: ANAESTHESIA
SKILLS:
- General Anaesthesia
Ether
Inhalation
Intravenous
- Spinal Anaesthesia
F: NEONATAL CARE FUNCTIONS
SKILLS:
- Neonatal resuscitation
- Treatment of several pneumonia
- Severe dehydration or shock
D: EOC DRUGS
Certain drugs are generally required to manage common
obstetric emergencies . A minimum list of such drugs has been
compiled and is given below:
4
of
Drug
Essential
Drug Category
Name
Critical
Anaesthetics
Ether
Inj.Atropine
Inj.Diazepam
Oxygen
Inj.Thiopental
Inj.Xylocaine-5%
Inj.Xylocaine-2%
Nitrous Oxide
Inj.Suxamethonium/
Catamine
Analglesics
Inj.Fortwin/
Pentazocine
Inj. Pethidine
Antiallergics
Inj.Decadron/Cortisone
Inj.Phenergan/Promethazine
Inj.Chlorpromazine
Tab. Iron
Inj. Iron
Antianaemia
Antidiabetics
Inj. Insulin
Antihypertensive
& CVS
Tab.Nifedipine
Inj.Mephentine/
Dopamine
Tab./inj. Digoxin
Propranolol
Antibiotics
Inj.Ampicillin
Inj.Gentamycin
Inj.Benzyl Penicillin
Inj.Procaine Penicillin
Inj.Chloramphenicol
Tab.Co-trimoxazole
Tab/inj.Chloroquine
Tab/inj.Quinine
Antimalarials
Diuretics
Inj.Furosemide
I.V. Fluids
Plasma Expanders
Glucose 5%
Glucose Saline/
Normal Saline
Ringer's Lactate
Sodium Bicarbonate
Oxytocics
Inj.Ergometrine
Inj.Oxytocin/Syntocinon
Inj.Tetanus Toxoid
Others
Most of the drugs listed in the above table may already
be on State approved drug lists and may have been supplied
such as
to the districts. However , a few critical ones ,
5
plasma expanders , are rarely provided
Ensuring the
of these essential medicines in
availability
adequate
quantities
each FRU will be necessary
at
if
these
institutions are to be appropriately prepared to cope with
obstetric emergencies when they arise .
OPERATIONALISING FRUs
Action for improving the availability of Emergency
Obstetric Care (EOC) at the identified institutions,} that are
to be developed into a network of FRUs, will be required in
the following major areas :
i)
improving physical facilities
,
if
considered necessary . Resources for this activity will need
to be identified either under the ongoing Area Development
Project or under the Minimum Needs Programme .( Please see
Notes on Funding at the end of this document .)
ii)
ensuring availability of necessary
equipment. While Govt. of India will procure and supply the
equipment to 219 districts ( all districts of Assam, Bihar,
M.P., Orissa, Rajasthan and U.P. and Adilabad of Andhra
Pradesh , Chickmaglure of Karnataka , North Arcot and
Thirunelvelli of Tamil Nadu and South 24 Parganas of West
Bengal ) , procurement for the remaning districts will have
to
using
be
organised by the State Govenments
the
specifications provided by Govt. of India.[ Ref. d.o.letter
No.M-14015/13/91- UIP dated 7th September '92 from Mrs.
Vineeta Rai, Joint Secretary ,MOHFW.]
iii) improving availability of specialists
at the FRUs.
This would include
the
filling up of
specialists'
posts that are available in the concerned
district and reorganisation of specialists available till
additional specialists become available .
improving the EOC skills of non
iv)
specialist staff located at the FRUs . Funds for the skill
development training to be carried out through an attachment
of the FRU staff to the District Hospital or the nearest
Medical College, will be provided under the CSSM Programme
for all districts.
v)
ensuring availability of essential EOC
drugs at the FRUs. Procurement and supply of EOC drugs will
be the responsibility of the State Governments.
vi)
ensuring adequate maintenance of the EOC
services and facilities .
FRUs
vii)
initiating
6
regular monitoring
of
the
Immediate action ,however, must be initiated in the
EOC drugs, skill development
four critical areas namely,
The issues and
training , maintenance and monitoring
aspects that would need to be addressed , for each of these
critical areas, is described in subsequent paragraphs .
EOC DRUGS:
(i)
The
State Govts, should
- ensure that all EOC drugs are included
in the State approved drug list.
- prioritise and rationalise their drug
procurement ploicy to ensure that all critical EOC drugs are
available at the FRUs .
- allow that the drugs procured under
family planning budget head can be used for EOC cases .
- authorise obstetrician/FRU Incharge to
purchase
critical EOC drugs from contingency funds in
emergencies.
Critical EOC drugs must always be available in labour
(ii)
room,
obstetric OT and obstetric emergency management ward.
They should be displayed prominently on a list in the above
areas and sister/staff nurse and M.O. Incharge should monitor
their availability on a daily basis.
(iii)
Quantities of EOC drugs supplied to CMOs and FRU I/Cs
and the funds available for their purchase should be on the
basis of the estimated number of complicated cases expected
in the district/FRU. Each FRU should calculate its first year
requirement on the basis of EOC cases managed in the past and
expected EOC cases in the coming year(s).
SKILL DEVELOPMENT TRAINING:
Those
specialists/medical
sub-district
(i)
officers/paramedical workers who are already performing EOC
functions should be oriented alongwith the district hospital
specialists over a two-day period.
(ii)
EOC skills training should be conducted by attaching
FRU - health personnel to institutions where EOC cases are
being treated. This will allow for appropriate skill-based,
hands-on training.
(iii)
The following institutions are recommended as
for EOC skills training in order of preference:
sites
- District hospital.
- District hospital of a neighbouring district.
- Nearest medical college hospital.
7
(iv)
Initially, skills development training of FRU staff
should be organised. Subsequently, PHC medical officers, LHVs
and MPWs should be trained in basic EOC skills by attaching
them to the FRUs in a phased manner.
(v)
Staff presently in position at FRUs should be
trained on an immediate basis so that FRU become operational
as soon as possible. Categories of FRU staff requiring
laboratory
training include non-specialist medical officers,
technicians and staff nurses.
addition to EOC skills, appropriate FRU staff
In
(vi)
should eventually be trained in management of newborn and
paediatric emergencies also so that the FRUs become a nodal
referral centre/institutiton for the entire range of MCH
services included under the CSSM Programme.
Minimum criteria for hands-on practice should be
(vii)
specifiedL which would have to be satisfied by FRU staff
during training. The following schedule is recommended for
the most comprehensive training requirement:
Personnel
category
Training
duration
Medical Offr.
(in OBG)
3 months
Skills
practice
Minimum hands
on practice
Surgical functions C-Section:
Manual and medical - Observe 15
treatment functions - Assist 15
— Perform at
least 5
Medical Offr.
3 months
(in Anaesthesia)
Anaesthesiogical
functions
Laboratory
Technician
1 month
Blood cross-match- Cross-match
ing and transfusion ing-10
Blood collection-10
Staff Nurse
1 month
OT training
Assisting anaesthetist
Manual procedures
Blood transfusion
Supportive care
Administer:
-G.A.(Boyles)-5
-Spinal-5
-Intubation-5
MAINTENANCE OF EOC FACILITIES:
State Governments should allocate a proportion of their
(i)
existing
drug
budgets to create a
performance-linked
miscellaneous purpose fund for the FRUs.
It is recommended
8
that disbursements from out of this fund should be Rs. 100.00
for each EOC admission to the FRUs and should be released
quarterly on the basis of the monthly performance reports for
the last quarter.
(ii)
Each FRU should be allowed to spend its earning under
the performance-linked miscellaneous purpose fund for the
following items or activities :
- Locally procured consumables for general maintenance
- Disposables for blood transfusion
- Maintenance of OT and beds
- Repair of EOC equipment
- Local purchase of emergency requirements of EOC drugs
MONITORING OF EOC FACILITIES:
To facilitate monitoring at FRUs, a Summary Case Sheet
prototype given at Annex I ) should be introduced for all
maternity admissions at FRUs .
(i)
(
An EOC Monthly Monitoring Report ( prototype given at
(ii)
Annex II ) should also be introduced. This should be filled
by each FRU to capture necessary data. Reports should be
based on data from Summary Case Sheets. 'These tools would be
used to identify deficiencies in EOC coverage and FRU
performance.
(iii)
Standardization of existing records will facilitate
monitoring and identification and gaps in EOC availability.
Specific areas requiring improvement are recording of :
- Time of admission,
register)
diagnosis/complaints
(admission
- Time of intervention (case sheets and OT records)
Whether complicated or normal delivery (labour
register)
room
District/FRU personnel should be briefed in the use of
(iv)
monitoring tools during EOC orientation or skills training.
The briefing should include :
Hands-on practice
available records
in filling forms
using
existing
- Explanation of how data can be used to identify
specific gaps in EOC availability (e.g. equipment,
staff skills, supplies)
9
■< MONITORING OPERATIONALISATION
A regular monitoring of progress on selected milestones
would help in accelerating operationalisation of EOC at FRUs.
The State Governments should , therefore , review the
of operationalisation of FRUs with the State
progress
Programme managers in every quarter . Suggested activities
which may be monitored are the following :
- Assure all sanctioned FRU posts are filled
- Choose sites
for training
of district hospital
personnel
- Issue
guidelines
incorporating
critical
and
essential EOC drugs in State approved drug list
- Allocate a proportion of existing drug budget for
EOC drugs to ensure uninterrupted supply to FRUs.
- Allow
family planning budget head drugs
to be
used for EOC cases also.
- Allocate a proportion of health budget to be used
for maintenance of FRUs.
- Authorize
( if necessary ) non-specialist staff
to
be trained in and carry out EOC functions
- Orient State CSSM core team in plans for EOC skills
upgradation
- Organize two-day orientation for district hospital
specialists and OB-GYN and paediatric specialists
from FRUs.
- Issue guidelines for FRU monitoring using select
indicators.
- Assure
of
existing
standardization
records
(admissions register, case sheets, OT records, labour
room register)
- Publicize availability of EOC at FRUs.
- Include messages on obstetric complications in State
and District IEC activities.
Notes on Funding :
(1)
The CSSM outlays t as they have been approved by
the Govt,
of India ,
include provision of essential
equipment to the identified FRUs of the districts
pertaining to the six States of Assam,Bihar, M.P.,
Orissa, Rajasthan and U.P.
Skill development training
of the medical and paramedical workers of the FRU staff
, however , will be funded under the CSSM Programme for
all districts.
(2)
The identified FRUs may
also need minor
upgardations in terms of physical facilities
like
repair/renovation of operation theatre ,
construction
of latrines , provision of a generator to ensure
10
availability of power during operations etc. The CSSM
programme has not made any provision of funds for such
upgradation. Funds for such upgradation in these states,
which would obviously be institution/district specific ,
the
Area
would
have to be made available from
Development Projects and/or Minimum Needs Programme.
***
27.1.1993
4
11
FRU
Annex .1
District
SUMMARY INDOOR PATIENT SHEET
To be filled upon discharge for all indoor cases of pregnancy, delivery, abortion and puerperum
(This does not replace bedside ticket)
Identification data:
Name
Husband’sName
Age
Policestation
Village/Ward
Parity
Admission info: Date of admission
Referred by: Setf/TBA/Private Doctor/Subcentre
Distance travelled
Time taken
Time of admission
Discharge info: Clinical diagnosis
Delivered in hospital: Yes/No Referred to
Result: expired/cured/reiieved/abscondedor LAMA
Date & time of discharge
Booked/Unbooked
PHC/CHC
Mode of transport
(Fill up reverse)
Classification:
Normal pregnancy
Normal delivery
Normal abortion/MTP
Complic. pregnancy
1:
toxemia/APH/severe
anaemia
others (specify)
____________
Complic. delivery2:obstructed/prolonged/PPH/others (specify)
Complic. abortion:
sepsis/incomplete/others (specify)
Complic. puerperum:
sepsis/PPH/others (specify)
(Stop here if Normal case)
Chief complaints
1.
3.
(in chronology; state
2.
4.
labour pains in hrs)
Condition on admission:
GC: Good/fair/poor/gasping
Pulse
BP
'
Temp
Others
Systemic (Positive findings only):
PA:
PV:
First treatment:
Date
Type (i.eM parenteral drugs & fluids)
Time
Definitive treatment:
Date
Type (i.e., conservative or operative)
Time
Major treatments given:
Surgical procedures
Yes/No
(exclude routine episiotomy)
C-section
Laprotomy
other (specify)
repair pereneal tear
Medical procedures
Yes/No
I.V/I.M. drugs
I.V. fluids
Blood transfusion
Yes/No
# of units
Source
Manual procedures
Yes/No
forceps
vacuum extraction
Anaesthesia
Yes/No
local
: antibiotics
Plasma expander
any pregnancy requiring operative intervention, transfusion, antibiotics,
significant medical condition.
2
oxtocics
uterine evacuation
sedatives
MTP
others
manual removal of placenta
general
spinal
management of hypertension, bleeaing, or any other
any delivery' requiring operative intervention (excluding routine episiotomy), transfusion, antibiotics or management of hypertension, severe
anaemia, unusual bleeding, obstructed/prolonged labour, or unusual presentation (inclucina breech).
P.TO.
t
Referral information
Patient referred to
for following reason(s):
A.
Lack of medicines (specify)
B.
Nonavailability of personnel to perform:
Surgery
Anaesthesia
Manual procedures
Blood transfusion
C.
Lack of equipment needed to perform:
Surgery
Anaesthesia
Manual procedures
Blood transfusion
To be filled by 2nd referral institution:
IPD #
Result: expired/cured/relieved/abscondedor LAMA
Delivered in hospital: Yes/No
Date & time of discharge
Kindly return form to 1st referral institution.
An Hex .H
Emergency Obstetric Care Monthly Monitoring Report
FRU
District
Month/Year
1-month period Cumulative
1.
Total maternity admissions
2.
Total complicated maternity admissions
3.
Total deliveries
4.
Total C-sections
5.
Total complicated abortion cases
6.
Maximum admission-intervention
interval for PPH cases
Total maternal deaths
8.
Total blood transfusions for
obstetric cases.
9.
Referred to other institutions
A. Outdoor maternity cases
B. Indoor maternity cases
C. Total
10.
Outcome of referred cases from previous month
reported referred institution:
A.
Total reported
B.
Total where outcome was
maternal death
CH- U •
1
Technical Comments on the activities of ICDS
programme support from TVS Medical Unit Hosur.
This comment has been written after a single visit to the Anganwadi
center of Government of TN that has the support of TVS unit at Hosur.
Hence it is limited to what had been observed at the time of visit.
The Situation:
The village Kothaguntapalli is about few kms from Hosur Factory. The
Anganwadi is one the centres of ICDS. There was a teacher and an ayah
manning the children, A typical Anganwadi center with lackluster in
various aspects, this is attached to the primary school of the village.
There was a ‘Salter Scale ‘ hanging in the middle of the room, (perhaps
to indicate that the center was an Anganwadi) There were about 25
children, out of enrolment 35. It was about a month since the centre had
been opened for the current year.
The strength of Anganwadi Positive points ;The Govt of TN had
provided the teacher with the chart which is almost a ready- reckoner for
the teacher to classify the children according to the nutritional status.
Naturally the teacher lacked in depth understanding of the purpose of the
chart, She merely records the wt and had mentioned that most of the
children were normal or in grade 1 Similarly the chart had been given for
the weight for the expectant mothers, who are also the beneficiary of the
centre. Both the charts did not show the reference standards. I could not
check the weight recorded as the register was not in the class. The fact
that an effort to help the teacher to record the weight, utilising the
figures provided in the chart shows the concern of the authorities.
The Ration given to the children as per the Governmental instruction is
as under
WEANING FOOD (as found on the label) Composition per 100 g.
Cereal (wheat/Maize/ BajraRagi
Bengal gram
Jaggery
Nutritional facts
52 g
05 g
12 g
30 g
per 100g Calories 350
Protein
8.5 g
2
The ration permitted of the ready mix to the children . The processed
powder is mixed with boiled and cooled water to make into laddoos
50 g ball for the under two yrs and 100 g balls for the above 2 yrs upto
5yrs. As soon as the children arrive the balls are ^served The under twos
have the laddos and return with the mothers while the anganwadi
children get the midday meal as well . The ration per child /day are
as Rice
80 g , dhall 10 g- oil 2 g In addition on Mondays
1 egg while on
potatoes are given, Tuesdays Greengram Thursdays
Wednesdays and Fridays no additional item is provided .
Through this meal as per the calculation the children get 290 calories
and 6.5 g Protein thus during the day with laddo and meal the
anganwadi children get in total 640 calories (RDA 1230)
15 g Protein (RDA 25 g)
The food provided during the day gives about 50% of RDA and is quite
good. According to the ‘consultant’ of the team the normal status
children in the class is to the extent of 70-80% (!) But the Team had also
taken the wt of children who do not attend the anganwas|\di class and the
wt recorded shows children with normal wt also to the extent of 75 %
What is the impact of the meal provided ?
My observations: The support given by the Government of TN in
providing a ready reckoner is a good start. But beyond this there were no
information whether the the children are given any vitamin /mineral
supplements. Whether the medical checkup was done or not.,was not
known. The children looked rather weak and stunted in growth.Though it
is difficult to weigh the children of that age certain care need to be taken
during weight recording. Since we did not see any data of individual
child’s growth rate one does not know whether the normal child is on the
borderline or well above. There was no individual weight card. When the
children are getting the calorie gap filled in with the meal and laddoos,
there should be some difference between the anganwadi and nonanganwadi attending children. Weight alone is inadequate to rate the
child’s nutrtional status. Some of the standards, recommended
maintained in India and elsewhere are stated below.
3
Standards available to assess the nutritional status of the children :
On the recommendations of the WHO the standards of National Centre
for Health Statistics (NCHS)is the reference point recommended in
India. The median value of NCHS is taken as Indian reference standard
(copies enclosed) Normally the classification of nutritional status are
Ht for age wt for age as well as wt for ht.
1. According to Gomez standard the classification details are :
above 90% of Indian standard
Normal
I st degree mal-nutrition
75-90 %
60-75
II nd degree
III rd degree
<60 %
Reference is 50th centile
2 The Indian Academy of Pediatrics (IAP)
Normal
I st degree
II nd
III rd
Ivth
above 80%
70-80 %
60-70
50-60
< 50%
To confirm the nutritional status weight alone is inadequzte. Height for
age is also essential and weight for ht as well as wt for age^refer to the
table) A proper medial checkup need to be done at the beginnng to check
for possible infection or infestation ,other factors that would inhibit the
absorption of the nutrients by the body,
With the average availability of 650 calories even the mal nourished
should be able to show some improvement and move up in the scale.
Since the teacher appears to be not so trained in the technical details
including the weighing of the child in the balance ,A>close observation
whether the children are eating what is served would give more
information about the children and the instruction received from their
mothers.
It is said that every child has the same growth potential if properly
nourished. It us thus necessary as not to accept lower standards as
“Indian “
4
With my handicap of limited information received on the spot, I make
the following suggestion for the TVS team who are graciously
supporting the Government’s effort in the area of child development
The suggestions are:
1. Check the scale used by the Anganwadi as the spring needs to be
strengthened.
2. Weigh the children individually as to wt for age ,measure the ht for
age with reference to the NCHS 50th centile (as per the chart) of
the Anganwadi group and record their status. Measurement of
arm-girth would be also useful if the doctors have the time. This
data of individual child , the team could keep in their office and
not share with the teacher till certain facts could be deduce
3 The teacher can continue her exercise. This can be corrected once
the doctors ares sure of the data. For this reason a close supervision
of the anganwadi school children need to be done’
As to their eating habits alertness and interest. A close observation of
children’s eating habit is required to find out whether they do get
their share and consume the food served. This one of the team
members can do continuously for a week or two during the meal
time The same person should make enquiries about the food that is
given by the mothers at home to compute the food availability for the
growing child
4.
Provide the medical check up for possible corrections if required
5. The children should be weighed periodically (once in three
months) to observe the growth during the period and also see the
difference between Anganwadi and outside.
6. To weigh the other children bathroom scale (platform type)
should be avoided..
7. Conduct under two advisory centers as this age is very crucial to
promote the potential growth factor in the child
8. To conduct this it should be considered as Health-nutrtion
education programme.
Select intelligent mothers and train them on few facts
8.1
of nourishment and health care of the under two yrs,
and make them as para- teachers/mother-teachers to
teach minimum of five mothers in their peer group,
5
8.2
8.3
8.4
Conduct nutrition and health education classes to
give a holistic information on water ,hygiene and food
requirements
The clinical classes should be a positive under two
Programme and not just cater to the sick children
alone. This would enable the mothers to a understand
and help in maintaining the weight chart as well as
provide possible adequate nourishment at home
Encourage the mother- teachers to participate and help
the anganwadi specially during meal time. This can
be done by the selected mother-teachers in turn
A comparative findings of local situation with that
of anganwadi will be useful for other areas
alsowhere anganwadi programme is executed. In TN
With time bound project the TVS team can show the way to
organize Under Twos in Anganwadi centres
The above activities are only a suggestion to improve the condition
of the children and the approach to anganwadi with TVS support.
0
■
K\
Ov#- (^tz^ '
l^o (A/?(jtAz
lAf^AM
V.^^C'K/VVVVYX .
KyV^t^V'^^
p t^xb^ (XJ^a Xa '^IA
(P(> -
W'V-’A^J
- S-ot)
ck&J^
qa Jj /v ^
<----------------
%
154
D. HANUMANTHA RAO AND K. VUAYAR
TEXTBOOK OF HUMAN NUTRITION
Table 2: Median Values (50th percentile) Weight for H
Table 1: MedianValues (50th centiles) of Heights and Weights of
Boys and Girls (0-60 months) — NCHS
Age
Months
0
3
6
9
12
15
18
21
24
27 •
30
33
36
39
42
45
48
51
54
57
60
Years
5.0
5.6
6.0
6.6
7.0
7.6
8.0
8.6
9.0
9.6
10.0
10.6
11.0
11.6
12.0
12.6
13.0
13.6
14.0
14.6
15.0
15.6
16.0
16.6
17.0
17.6
18.0
Giris
Boys
Height
(cms)
50.5
61.1
67.8
. 723
76.1 ‘
79.4
82.4
85.1
87.6
88.1
90.4
.92.7
94.9
97.0
99.1
101.0
102.9
104.8
106.6
108.3
109.9
109.9
113.1
116.1
119.0
121.7
124.4
127.0
129.6
132.2
134.8
1373
140.3
143.3
146.4
149.7
153.0
156.5
159.9
163.1
166.2
169.0
1713
1733
175.2
176.2
176.7
176.8
Weight
(kg)
Height
(cms)
Weight
(kg)
13.0
60
6.0
6.0
104
13.6
14.1
61
6.3
105
62
6.3
6.6
6.6
106
6.9
6.9
7.2
7.5
7.7
8.0
8.3
8.5
8.8
9.0
9.2
9.5
9.7
9.9
7.1
7.4
■ 7.7
7.9
8.2
8.4
8.6
8.9
107
108
109
110
111
18.7
19.7
20.7
21.7
22.9
24.0
25.3
108.4
111.6
114.6
17.7
18.6
19.5
117.6
20.6
29.7
31.4
33.3
35.3
373
39.8
42.3
45.0
47.8
50.8
- 53.8
56.7
59.5
62.1 .
64.4
66.3
67.8
68.9
1413
144.8
148.2
151.5
154.6
157.1
159.0
160.4
161.2
161.8
162.1
162.4
162.7
163.1
163.4
163.7
10.2
10.8
113
11.8
12.4
14.6
16.0
16.4
16.8
17.2
17.7
21.8
23.3
24.8
26.6
28.5
30.5
32.5
34.7
37.0
39.2
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
413
83
43.8
46.1
48.3
50.3
52.1
53.7
55.0
55.9
56.4
56.7
56.7
56.6
84
85
86
87
88
89
90
91
92
Ref: WHO. Measuring change in nutritional status. Guidelines for assessing the nutritional impact of
supplementary feeding programmes for vulnerable groups. WHO, Geneva, 1983.
94
95
100
101
15.1
15.5
129.3
132.2
135.2
138.3
3.4
3.5
3-7
3.9
4.7
5'0
5.3
5.7
97.9
99.8
101.6
103.4
105.1
106.7
108.4
26.4
28.1
3.3
4.7
5.0
5.4
5.7
5.4
7.2
8.9
9.5
126.4
Giris
4.1
3.2
593
65.9
70.4
74.3
77.8
80.9
83.8
86.5
87.0
89.5
91.7
123.5
Boys
Height
(cms)
4.1
4.3
49.9
120.6
Expected Weight (kg)
50
51
52
53
54
55
56
57
58
59
3.3
6.0
7.8
92
I Q.2
10.9
113
12.0
12.3
12.9
133
14.1
14.6
15.2
15.7
16.2
16.7
17.2
17.7
18.2
18.7
93.9
96.0
Height
(cms)
93
3.5
3.7
3.9
4.3
96
97
98
99
102
103
112
113
114
115
9,1
116
9.3
9.5
9.7
117
118
10.1
10.4
10.6
10.0
120
10.2
10.4
122
10.8
11.0
10.6
123
10.8
11.0
124
11.2
11.4
11.6
11.8
12.0
12.3
12.5
12.7
12.9
13.2
13.4
126
11.2
11.5
11.7
11.9
12.1
12.3
12.6
12.8 ’
13.0
13.3
13.5
13.7
14.0
13.6
119
121
125
127
128
129
130
131
132
133
134
135
136
137
Ref : WHO. Measuring change in nutritional status. Guidelines for a
supplementary feeding programmes for vulnerable groups. WHO, Ge
k
I
156
GROWTH CHART
(IAP-Classification - NCHS st
TEXTBOOK OF HUMAN NUTRITION
CLASSIFICATION OF NUTRITIONAL STATUS
Relatively speaking, weight, height and arm circumference have come to be considered
the most sensitive parameters for assessing nutritional status of under fives. Several
methods have been suggested for the classification of nutritional status based on these
measurements.
The anthropometric data can be expressed in a number of ways in relation to. refer
ence data: (a) by the use of mean and standard deviation values, (b) by calculating per
centages of the median value of reference population which is assigned as 100 per cent,
and (c) by comparing with percentiles of the reference data, where median value is the
50th centile.
Weight for Age
18
17
16
15
14
13
12
11
10
9
8
7
6
5
4
3
2
1
0
a
-0
*
Various methods have been suggested to classify children into various nutritional grades
using the body weights. The most widely used classification is the Gomez classification
(Gomez et al., 1956), in which the children are classified as having first, second or third
degree malnutrition if their weight for age is in the range of 75—90%, 60-75% or less
than 60% respectivejy of the reference median. All children whose weight is 90% and
above are categorised as normal. The selection of cut-off levels was based on the clinical/hospital experience in Mexico. Gomez et al. (1956) observed a marked difference in
mortality during first 48 hours between children with second degree malnutrition (6075% of median) and those with third degree malnutrition (< 60% of median). The Indian
Academy of Paediatrics (IAP) recommends the following classification : 80%, 70-80%,
60-70%, 50-60% and < 50% as normal, first, second, third and fourth grade of mal
nutrition respectively (IAP, 1972). This classification is currently used by the Integrated
Child Development Scheme (ICDS) for selecting beneficiaries and growth monitoring
(Chart 1). As such, most of the classifications, based on weight for age use arbitrary cut
off points. Normal growth is considered to encompass values within two standard devia
tions of the mean. Since body weight does not follow Gaussian distribution, use of mean
and standard deviations for classifying children into differenet grades of nutritional
status may not be appropriate. To overcome these problems, Ramnath, el al. (1993),
recommend use of 5th percentile of reference values as the cut-off point to classify
children as normal and malnourished. They suggest that the weight below the 10th per
centile values of the community (ICMR data) may be considered as indicative of severe
degree of malnutrition. When these criteria were used, their analysis indicated that 80%
of NCHS median appeared appropriate to decide whether children were normal or mal
nourished. The current criterion of 60% of reference median for grading the children as
suffering from severe degree of malnutrition and 80% of reference median as cut-off be
tween ’normals’ and malnourished, appears to be the most reasonable. A summary of
these classifications is given in Table-3.
f
■
ill-
’I!
i
0 3 6 9 12 15 18 21 24 27 30 33 36 39 42
Age in months
GROWTH CHART
(IAP classification - NCHS
w
15141312-
I i
J,
11
a 10-
Z 9-
ILL
4
5 8-
£ 7-
t
w. I1
65-
/
A
'H
41
I
inormal
I 111
Illll
i.
21 24 27 30 33 36 39 42
0 3 6 9 12 15 18
k-ff'K fa'
£•
C H - <4 ■
Joe
t
(IC4RNATAIO1 GROUP-1)
UDISHA - A DA WN IN ICDS TRAINING
The Training component of the ICDS Programme has now been recognised as
the most important key to achieving the aims and objectives of the ICDS Training
Programme, with the ultimate aim of moulding the ICDS functionaries into Agents of
social and behavioural change'. Keeping in view the importance of the programme
and its likely impact on the quality of the ICDS scheme, the administrative approval
and guidelines for the implementation of the World Bank assisted ICDS Training
Programme - Project - UDISHA have been issued vide Govt, of India letter No. :1115/98-TR-I dt.lfh May 1999. The Project Implementation Plan (PIP) for a periodfive
yeai's from lsl April 1999 has also been finalised and this is the basic working
document for the implementing states, including Karn ataka.
UDISHA envisages the upward revision offinancial norms, integration and co
ordination of Training of ICDS functionaries and revision of Training Syllabus, The
Southern Regional Centre of the National Institute of Public Co-operation and Child
Development (NIPCCD) located at Bangalore is an apex body catering to the training
needs of senior level ICDS functionaries like Asst. Directors/Progranune
Officers/CDPOs/ACDPOs etc., besides undertaking research and evaluation studies.
During the _current_year NIPCCD has been requested to tak^ up Evaluation of the^
\dch Training Programme for AVtlTs', 'Integrated approach to pre-school
Education Impact ofSupplementary Nutrition in ICDS' etc.
There is only one Middle Level Training Centre (MLTC) at Ujire ( Dakshi&a
Kannada District U^^fTis'catering^ie Training needs of Supervisors^ Ike State has
T3 AngfflTWttdi Workers~Training Centres (AWTCs) which are run by KSCCW and
Helpers. The revised rates of honorarium as
Other NGOs for trailting the AWWs
well as revised course grants as per the UDISHA guidelines have been sanctioned by
the state Govt, during 1999-2000.
TRAINING STATUS OF ICDS FUNCTIONARIES AS ON 01.04.2000:Sanctioned
CDPO
ACDPO
Supervisors
AJIWs
.1IIdis
185
219
1862
40170
40170
In position
| Trilined
Untrained
183
140
660
39277
39890
. 152
107
660
38680
27993
31
33
597
11897
The Physical & Financial progress achieved luider project UDISIIA during 992006 is asfollows:L
PHYSICAL PROGRESS:-
SI.
No.
ICDS Functionary
1.
2.
3.
4.
5.
CDPO
ACDPO
Supervisors
AWWs
Helpers
Trained during 1999-2000
Trained in J TC
Trained in RC
7
13
217
6669
Nil
8
9
Nd
1999
540 (OC)
6. Sandwich Training for A IPJPs in 2 batches. 40+39
79 (AWTCBelgaum)
II.FINANCIAL PROGRESS:Grants
Budget Opening Balance
Released to ML TC/ Balance
Total
released io the grants AU TCs during
Head of as on 1.4.1999
with the
during
available
1999-2000
state
State
Account
as on 1.4.2000
1999-2000
3 UjOtskS lops
2235-02102-0-05
3.26 Crores
1.15 Crores 4.41 Crores ( l‘7Q Crores^)
(^3 ‘71 Crores }
M'v ■•J
inecctsttj
I
_
------ -
STATE LEVEL TRAINING TASKFORCE:The Training conq)onent of LCDS has now been recognised as the most
important key to achieve the aims and objectives of the 1CDS Programme. The
emphasis now is on quality improvement and enrichment of human resources
available, with the ultimate aim of nw^lding jhe^ l^DSfimcnonaries into agents of
social aniLbehiivioural changes, con vincing communicators- 11ho^cah~efieciivetr bring
about the attitudinal changes required. Training of human resource development or
capacity building ( as it is other - nise knonn) assumes tremendous significance.
2
For regular monitoring and evaluation of ICDS training component the State
Govt, has constituted the State Training Task Force vide its order dt. 25.04.98, with the
following members:Director of Women and Child Development
Regional Director, NIPCCD, Bangalore
State Co-ordinator, ICDS, Central Technical Committee
Director, DPEP
Director, DSERT
Director, Health & Family Welfare
Asst. Technical Adviser, Food & Nutrition Board
Representative from KSCCW
Representative from MLTC, Ujire ( on rotation )
Representative from UNICEF, Hyderabad
One CDPO ( on rotation )
One Supervisor ( on rotation )
One Anganwadi Worker ( on rotation )
Joint Director (ICDS )
Chairman
Member
9)
ff
>>
99
Invitee
99
Convenor
So far, three State Level Task Force Committee meetings were convened on
OfJO. 1998. 19.07,1999 and 12.01.2000^under the Ch airnmnship of the Director,
Women and Child Development. Hie Proceedings of the above, meeting are enclosed
h erey vith for reference.
Hie basic futicdon of Tusk Force is the hitegi ute aad co-ui'di;iate all aspects of
ICDS trainhig ar all l^els and to reconmen a changes in the curriculum., strategies
and methodology. 7lie ultimate goal is to reorient and reutilise ICDS training to turn
it into a dynamic responsive human resource development programme.
For regular monitoring and evaluation of the ICDS Training Programme in
the State, a STTF has been constituted vide Govt. Order No. DWCD:257JCD/97
Bangalore dt. 25.04.98, for a period of two years, lite tenure of this Task-Force has
expired on 24.04.2000. Govt, has been requested to renew the same for another three
years, i.e. ugto 31.03.2004. Soon after the re-constilntion /renewal, a meeting will be
convened Si syllabus revision in respect ofSupervisors training is proposed to be taken
up. A sub com milfee has also been constituted under the STEF' to look into the
revision of 30° o module^Jujsed syllabus in respect of training of ICDS functionaries.
The proposed revision in respect of .FTC ofAWWs has already been conveyed to the
Govt of India. ( Copy enclosed)
State Training Action Plan for 1999-2000 included sensitization Programmes
for Asst. Directors of Women & Child Development, Programme Officers of Distilct
ICDS Cells & Heads of MUTC/AWTCs. However formal approval of Govt, of India
for conducting the above programmesis still aw'aited.
J
STATE TRAINING CALENDER:1. 15 CDPOs have been deputed to NIPCCD, Bangalore for Job Training with effect
from 2nd May 2000. ( copy enclosed)
a) Supervisors have been deputed to MLTC Ujire for 2 Refresher Courses
2.
commencing from 24.04.2000 & 08.05.2000 @ 25 per batch, (copy enclosed)
b) The appointment of Supervisors in the State has been delayed, on account
of a pending court decision on additional marks to be allotted to rural
candidates.
3. The Training Calendar for 25 AWTCs, in the State has been finalised for the
first quarter of the current year . ( copy enclosed )
STA TVS OF RE-IMBURSEMENT CLAIMS
1. The reimbursement claims in the prescribed proforma are being finalised in
tivo phases.
a) From
October 98 to 31s1 march 1999.
b) From 1^ April 99 to ifi1 March 2000.
Item wise details of expenditure have been called for from each training Centre /
District Office and mil be sent to Govt, ofIndia shortly.
STATE TRAINING ACTION PLAN FOR 2000-20(^1.
(Other than regular training of ICDS functionaries)
Vertical Workshop & Meeting
( Taskforce ADs & POs meeting, A WTC & MLTC &
other review meeting)
1,00,000
2. Crash course for statistical Assistants in consolidation
of reports
8,00,000
3. Advocacy [irograntme
15,00,000
4. Exposure tour& w
3,00,000
1.
X
1 5. Talukmse training to Anganwadi workers regarding utility
of Activity Bank
12,00,000
4
i.
6. Research study at A WTC/MLTC
6,00,000
7. Training to elected Gram Panchayat JVomen Members
10,00,000 —
8. Developnientj>f Resource Material in local language
45,00,000
Total
1,00,00,000
/_<
Av— t Director
Women and Child Development
Bangalore
5
CU^ ’uc fe. ‘ (" .
),k J ex?
C
J
o
---------- ---------- - --------
^2-^
/<7'7/ C<?= ij-ijo-k
-L-C2-^ rn.Ox>y ^C‘
tP
------ ’—■—:——
yrt ,—
^p^iyLi
L
I-—- // 3
•
7~/^/ ^<<x
l .m—l.i <
C-H
/ £?6
U. tv
doc
(T;
("o
I
, <
^ze^-4
7
^JL^n1-.
J <30
j.
(Lee- o
cx^
E
L l J<2
r
. Lo^.
1 c.^
l O^ ,
c/ J
Lo
2
. p)
LV
-
/3
,- fc
j
L
,.i\'
^.LL
7 1
,LuC^i
ROx
t
e ocv-> u?*™- 4
(2? (L-C* tvA-^
2
O ~
Laj S^
x^n
Jb?
?
4
■-P c?
I
(J
-O L
c
r Pt'^
K
^-pp
®rj>47
(3?. </
(
^C2
■ fc.
>
D >1
A
cts_&-> *i'^
(Lo J
£^:yG'2
kJ P r
j /w
. '3GX-^>
“S1'
1
.
C. O J-L
I
31
J4-^.
(O U
. ,-.J> Kr
P'c.of
C
^Ucu
iM-
.d-C-op u'^
’
<^dJl 7"^
7A-C2_,
<2-^—
1 ^rT< S<J
(Lxxv*^
c^t-
^ .oc Ct u ncr
^Ot_LcJ
P-M
}cJ.
l S-£
^ c.
f
Lx e 1^^-yL. UUh c (
1
4‘
Ss,
CL)
Ct O-t -^i rt=^Ml
t-
Mu
'
■■
j ’
4
PM
jcr>n
1^p
■
,
j Mr
'<
Je^G^
J
p —’M °v ofG- c^Jd-
(p
f /?e-6K
v 3
f ac
Pe«M 7 Jp
/,
z-o^^30
Lft "
-
l^*3- ®M-
I
y<ji_A->^'
■J
j\^ CX_-t-C
CCL-)
JJ.
^c
D c> (L^-d^
Zlc
^C (ZX>^V
U r h* k.o 3
5
-p
feK
Uev-o<?
C
r
m
jl .
:
&
c
e
- l-l&.<^ LfT^c
•4 -
0-2
Vr
■P 1.5/0
’J^P"
u
A Cld)^
I
■J
P
rPl^
!■
—'
r.f Joc^0^ , |
"F"
i
?
lx ZLl td>^ &ALla
I
e
f
C < i> jLCC<CJ-2_j£
L^- AC. C
P, ■/
ij.
>c^cd
"j"^Jc-2 Lo^x <2.
f
ru
-- D-'Sr"
7-7
------
S
- ------
• 1
Of'L'j
,
•■
6vaa < Y
Pa / c ^
i ^P-e'
^■o^' Ovn zaz Li Lt^ >
jB c <5—
------ pp-r .27
D >/
——
72 -/S’
£5 P ~
c^=>-^ ^1d
7^ (^ZAZ—I — i ^T-A
C>-ii
,p)
‘'
uCy!^ f
< b P -r-yi — Az
C
.
c &x^p
i
6vg-
3
J
Q
/ hLm
K 7g
h
^(^xa -x Saa -S
i
*=D.
yp'
■ f-
\L
»
4
U cjo ^
*
/VAU-J^- /-<^Q <<
.
O_p-S^ i S
ft^J' Ne^ -^Zpp
IA^
A-A.
4<^ ^2254
^Jz-t i
U.
:_';c~
c<>Z t
pjjTfljL
qf
coulK
I
-z,
..^■^r-.<X
Ct-Q-i-' Ac
C>—
7) op
i
5A-AQ|
^
• ‘-A-p*
dU^ '*-
p
x^jJ v UPX)
r
<2-1-
/
__4
. . l TPoi
pv
y-
rat
/c?-^
£
g <a 3
<^(l^
Xi
l/J
0^ d
3
|A_zOL?^
<\
' p.
'7> o -^c l - La z
ZlAHiA' .
b
Tc?
ujr
/'r
</>
J
< ^27
c ^L(L^L < |
LUO-
,S
■^1
A'c
7,
(L ^
Lx 1^
2 Q^c.
'Toa Z’
.
-^X,
, X■
U
U^J_.\
Xx G>. <X
Pej^vx^
p
^^-‘-,'<2-0
<<?^
X.
Qf^Lrz
>,.
c-cX
V
o.
-0
X-c’
"' %>s^ 5 eA-'
i
(loeD-
LA2
q
■
r a 4
7^
£ <- /M
OC>2>
d, o-J
)^-tA C-
«<>• - =A‘T
-p
J> ,
•Mo*^
CLa C
K)€O
C-C'^'
1-
[)
Jl<2 J
^6-
<Lp
■■ r
—c
' •- G
*
C’ M i
?>
,
. .U^ "Jlss
Xi
-^TPp
p
aj&l
yp
a
p
dd
^C><z
I
/Cc -
)
-^C£.-
■
1}
<<L>-4v-t/''.v_Q_.
C_o
isSL'S-'^-
S-^c -
L
(-x—^
r
I U c—.
d
r
m -JLc - Xa S
.
qI
C2_
c
c_Q-
— ^J-AJ H /
M
aw P^’. _
;i LA
Y^
McxlCtU^
x
b) ^p^^-*'
<?f<
cj
gt
La
La J5^
6) v'J
3
V
’
r-pt'P
ig-^ClxP
f
S
p/' •
"
Ssr
C /’TS^
bj
i^flD , ^l~t 0
•
l j
3rc^
S' ,<£0 6-^
/-/■
^'*
"-s
Lo JTL
. Jj>2-
p
Zg ^
/
3-^ o^
>,'- - Us^i>a 1TT '-^ ■
A.
L-v
< fC-
c >y 8
It
r7^
c- ->
,1r1c:
/Tc
ha—
;’S7T>J^
•3^ ^JtSr
11 A
rU^'
c O^
' P-
5
%<x)
<'-J
7
/ ?7(9
OvJ rv-
i3
PcJ
A
'
CL<^J
I
(
Sdw (Ay
'
1
;- Cr^P
CX-u Li>
' ITAAAtAS
X1B
*—u ^-Q—»
/f^7
/ 2^
:<a _
A-X^-")
^u ^(LHL< GYAA^
><^C=
a.
J :
' J?/
<
Xj =^-S t C -
«?=»
cS>_A
A_J_^ cx^. <!> ^p
J
X
l
" "'Cl ,
x
LuJ 6? I^-',
uOc^l
GPOLA^J'
f
XiXX
c
XT7^^
C:rr^
-
z-r-) “SUc^-a-vX
CZOAAAAe^-
go^d
-kc>->~^
o .UJ^°
'. 4
i ^j CIL"XLt'
., A^X?
j '-H
^! V' **
,Wf x
r’-r
JSz Ooa ^-
f.
k
.AM •
>£• —
.
X 0
t
/
c O
'
xC (~
P\_p‘
.cu
t
-
r
r, I
,1^
^.oXC*
°- "
>
i/^'(-‘
? ?S"X ■
1
4U-S^
A^
C2 'a K-v-
p£? ’A
6 c^
of
r^v Xc-^0^
»J -'®' Ti
'*4.
/jA^- /
i)
go^J '
'. , L L’—LO-
J -,'
)H
/? c
/<J
oJi-Cp <2
'£
■P^c^
.^.auo Cnxxaa
(3)
-^kl
S ,u^°
uxJ z)
o t jj /v) i c (2 r, C
-
X
jc-^5^
<
cJL^ ^'
^ <L^oC/
■' 4
ZAq
>-
kc J.
L> rC
A Ka Io " -yir jXJ
KJ L>
(.A-K { AJO ^A -. A tM^e^0
M la fS tIT<4c^n
jo -—i
/fc *->-a . /oUua' S i-i7
^Jo, Ur-.^cJ
(>H c
a
&•
&Y f-p_e c
d<2f
y
/^e-o^
^Jj Cc Ls
J
r
11
1
©<xf
/?c r ■'
c yr/ (^<J- Cut
CH -
-
Results of National Evaluation oF ICDS (Various studies)
Nutrition:
*
Adequate intake of all nutrients except Vit. A(1981, Singhal)
Intake of protein was low (Joshi 1977)
Caloric gap of 400-500 (Jyoti Kumari 1985)
Improvement in severe malnutrition but not much impact on mild and
m o derate malnutrition.
Rapid decline in Xerophthalmia over a period of two years in Tamil Nadu
(Chandra 1984) due to ICDS.
Malnutrition was attributed to various factors like poor socio-economic
conditions, inadequate health & nutrition education, faulty weaning
practices, lack of ante-natal care, low birth weight, repeated pregnancies,
superstitions and beliefs, large sized families and insanitation (Bapat
1983)
90% had very poor home stimulation in terms of availability of toys,
games and reading materials and provision of affection and warmth
(Jyothi Kumar i 1985)
Taste important factor in quality of supplement consumed.
The nutritional status of pre-school children improved and their level of
Hb increased after deworming and or introducing suppl. Nutrition and iron
therapy (Soundarajan 1985)
Breast feeding, weaning at an early age and 'complete immunization
identified as important determinants of nutritional status (Kaniala 1985) &
protection against diseases, 1MR in every breast-fed and weaned infant
was low (Mathur 1983).
Anthropometric measurements indicated chronic malnutrition among the
expectant mothers. 75% showed nutritional deficiency and 93% anemic
and had inadequate intake of mineral and vitamins.
bnmunizauon
Only 52% mothers adhered to the immunization schedules. Reasons were
ignorance, indifferent attitude, lack of awareness regarding schedule, non
availability of vaccines, fear of side effects, inconvenient timings (& fixed
days) and long distances to be travelled (Khanna 1983)
* Not much studies on IT coverage of women.
Health And Nutrition Education (HNE)
It was reported that HNE rai'ely conducted by AWW and only a small
percentage of AWWs were rated satisfactoiy on skills in planning and
implementation of HNE (Sharma 1986).
Treatment by mothers of diarrhea improved where ORS was used or home
based fluids.
\
Tackle the following issues:
♦
♦
®
♦
Women’s low status and lack of decision making power -> Empowerment.
Information to recognize the signs of complications
Health education.
Able to access care when complications develop -> referral.
Resources to reach an appropriate care facility in time -> transportation.
Key lessons ofpast decade.
9
Risk approach does not help to predict which women will develop
complications and which women will not.
« Use of family planning methods does reduce unwanted pregnancies.
4»
Training of TBA’s has not reduced MMR as they cannot handle
emergenci e s/c omp 1 i c ati ons.
The limited procedures carried out in the name of ANC and PNC have had
little impact in lowering Maternal Mortality and morbidity. These services
are more for the infants than for women, (paradigm shift to avoid turning
two sets of distinct and legitimate needs into competing demands for
appropriate care.
More resources on ANC than into delivery and immediate post partum
cai e, emergency obs. care and safe abortions.
Making every nuiternal death count:
®
•
•
•
•
•
Improving / upgrading emergency obs.services.
Training of professionally recognized community and facility based
midwives, (including post partum care).
Provision of safe, legal abortion services, (reason fori in 6 global maternal
deaths).
Strengthening of private care to improve women’s general health,
beneficial ANC, PPC, FP, HE on pregnancy and its complications.
Gradually replace TBA’s with trained midwives n the community.
Chronic maternal morbidity also to be tackled (poor repair of episiotomy
and perineal tears, vesico-vaginal fistula and utero-vaginal prolapse)
Measuring Maternal Mortality (impact indicator)
©
Sisterhood method/surveys (asking respondent about sister’s birth histories,
number reaching adulthood, number who have died, age at death, year in
which death occurred, and years since the death, etc)
Verbal autopsy.
RAMOS (Reproductive age Mortality study)
Confidential enquiries (ideal)
Maternal Death Review (recommended by WHO for selected health
facilities).
Impact indicators difficult to measure. So process indicators, which provide information
on the actions to be taken to improve the situation. They are affordable and reflect
changes immediately (responsiveness).
Table 1 (pg 26)
Improvement in safety of caesarians
Legalization of abortions and provision of safe seivices.
Leadership of midwives and obg. Specialists for better training and services.
Maternal deaths audits.
Community Partidpation
•
♦
*
•
Low or marginal community participation.
ICDS functionaries also did not perceive the importance of community
participation.
Low level of community participation was attributed to lack of awareness
and knowledge of ICDS scheme, ignorance, poverty, lack of time on the
part of villagers, inadequate training of AWW, lack of transport facilities,
etc (Ramdev 1982).
Factors considered critical for strengthening and promoting community
participation were, skills of the worker in eliciting community
participation, existence of coordination committees, frequency of their
meetings and involvement of local organizations. (Sharma A. 1986)
Source : Preventing Maternal Mortality Evidence, Resources, Leadership, Action.
Safe Motherhood Initiatives, RH Matters 1999.
j Vaiernal A/ oriality
Inter national conference on Population and Development in Cairo 1994, ICPD 4- 5 in
1999 at New York decided that Governments agree to reduce MMR by year 2000 of half
of
k. vcls and ai Ul I) . kuiher half.
.. ... ............^4j ;o Iics , paivticaral.iK.dru^o, paiunteral anticonsulsants, manual removal of placements, removal or related products and assisted
regional delivery, (could be provided at community level also).
Comprehensive EOC above and surgery (caesarian) and blood transfusion.
Reasons for decline in Developed countries.
J, Levels of poverty
T Living conditions
Better nutrition
Greater autonomy of women
T Standards of OBG.
Aseptic practices in assisting deliveries.
Drugs to combat sepsis, eclampsia & Haemorrhage
Lower fertility rates by birth control
- Media
 SDA-RF-CH-4.23.pdf
SDA-RF-CH-4.23.pdf
Position: 1903 (6 views)